Abstract
Background
Studies show uneven access to Medicare-approved lung cancer screening (LCS) programs across the United States. The Veterans Health Administration (VA), the largest national US integrated health system, is potentially well positioned to coordinate LCS services across regional units to ensure that access matches distribution of need nationally.
Research Question
To what extent does LCS access (considering both VA and partner sites) and use match the distribution of eligible Veterans at state and regional levels?
Methods
In this retrospective analysis, we identified LCS examinations in VA facilities between 2013 and 2019 from the VA Corporate Data Warehouse and plotted VA facilities with LCS geographically. We compared estimated LCS rates (unique Veterans screened per LCS-eligible population) across states and VA regional units. Finally, we assessed whether the VA’s new partnership with the GO2 Foundation for Lung Cancer (which includes more than 750 LCS centers) closes geographic gaps in LCS access.
Results
We identified 71,898 LCS examinations in 96 of 139 (69.1%) VA facilities in 44 states between 2013 and 2019, with substantial variation across states (0-8 VA LCS facilities per state). Screening rates among eligible Veterans in the population varied more than 30-fold across regional networks (rate ratio, 33.6; 95% CI, 30.8-36.7 for VA New England vs Veterans Integrated Service Network 4), with weak correlation between eligible populations and LCS rates (coefficient, –0.30). Partnering with the GO2 Foundation for Lung Cancer expands capacity and access (eg, all states now have ≥ 1 VA or partner LCS site), but 9 of the 12 states with the highest proportions of rural Veterans still have ≤ 3 total LCS facilities.
Interpretation
Disparities in LCS access exist based on where Veterans live, particularly for rural Veterans, even after partnering with the GO2 Foundation for Lung Cancer. The nationally integrated VA system has an opportunity to leverage regional resources to distribute and coordinate LCS services better to ensure equitable access.
Key Words: access, lung cancer, lung cancer screening, preventive medicine, rural, veteran
Abbreviations: LCS, lung cancer screening; LDCT, low-dose CT; VA, Veterans Health Administration; VISN, Veterans Integrated Service Network
FOR EDITORIAL COMMENT, SEE PAGE 34
Lung cancer screening (LCS) with low-dose CT (LDCT) scanning of the chest has been shown to reduce lung cancer mortality in large randomized trials.1,2 Since December 2013, the US Preventive Services Task Force has recommended LCS for high-risk individuals (those 55-80 years of age who currently smoke cigarettes or quit within the past 15 years, with at least 30 pack-years total smoking history), and Medicare reimburses LCS for eligible beneficiaries if screening occurs in approved LCS centers that meet quality standards.3,4 In response, many hospitals developed LCS programs, but faced several barriers and had few incentives to coordinate services or share resources. Perhaps in part because of a lack of coordination across regions, unequal distribution of resources to provide screening, and other reasons, the distribution of Centers for Medicare and Medicaid Services-approved LCS centers across the country remains uneven.5 Unfortunately, populations with increased risk of lung cancer incidence and mortality, such as rural and socioeconomically marginalized communities, typically have lower access to this preventive service.6, 7, 8
By contrast, the Veterans Health Administration (VA) is uniquely positioned as the largest nationally integrated US health care system to assess need and resources across the system and to leverage VA regional networks to plan services to ensure equitable access. Recognizing the increased risk of lung cancer in the Veteran population, the VA was an early adopter of LCS, beginning with a demonstration project in eight VA facilities from 2013 through 2015.9 Since then, a growing number of VA facilities have begun offering LCS, but screening rates remain low nationally in the VA (a challenge observed outside of the VA as well).10, 11, 12 To improve LCS uptake, in June 2020, the VA entered a partnership with the GO2 Foundation for Lung Cancer. This public-private partnership is intended to allow Veterans enrolled in the VA health care system to access LCS at more than 750 GO2 Foundation for Lung Cancer screening centers, to raise awareness among Veterans and VA providers about LCS, and to share best practices for LCS implementation.13
To date, it remains unclear how well access to LCS and screening rates within the VA match the geographic distribution of LCS-eligible Veterans in the population and the degree to which the new GO2 Foundation for Lung Cancer partnership will address existing gaps in LCS access. In this study we sought: (1) to assess the geographic distribution of VA facilities that offer LCS relative to need in the population (determined by estimated LCS-eligible populations per state), (2) to compare estimated LCS rates (numbers of unique Veterans screened among the estimated LCS-eligible population) across states and VA service regions to assist with future planning and allocation of resources, and (3) to characterize the extent to which locations of GO2 Foundation for Lung Cancer partner sites address geographic gaps in LCS availability. Given the heightened lung cancer risk in rural populations,14 we were particularly attentive to availability of LCS through the VA or GO2 Foundation for Lung Cancer partnership sites in rural areas.
Methods
This study was approved by the VA Bedford (Identifier: RW0008H) and the VA Boston (Identifier: 1590535) Institutional Review Boards.
Study Population: Veterans Who Underwent Initial LCS in a VA Facility
To determine the number of unique Veterans who underwent LCS during the study period, we identified initial episodes of LCS among Veterans 55 to 80 years of age that occurred in VA facilities from 2013 through 2019 from the VA’s Corporate Data Warehouse.15 We captured initial LCS examinations by these criteria: (1) a Current Procedural Terminology code corresponding to LDCT scanning for LCS (G0297, S8023), (2) LDCT scan or noncontrast CT scan of the chest with a Lung CT Screening Reporting & Data System16 category included in the radiology report, or (3) clinical reminder in the VA’s electronic health record indicating that the Veteran agreed to undergo LCS followed by chest CT scan within 90 days. We then calculated the number of unique Veterans who underwent initial LCS, aggregated to each VA medical center.
Geographic Distribution of LCS Services
We mapped locations of all 139 VA medical centers in the United States (excluding US territories) using the Microsoft Excel 365 ProPlus 3D-Map tool (Microsoft), indicated whether we found evidence of LCS at the facility, and graphically displayed LCS volume at each VA facility using heatmaps. We considered VA facilities that screened fewer than 25 unique Veterans from 2013 through 2019 as performing “sporadic LCS.” We subsequently mapped locations of GO2 Foundation for Lung Cancer LCS programs, as listed on the GO2 Foundation for Lung Cancer website17 as of December 14, 2020. We used data on percent of rural Veterans enrolled in the VA system by state and by VA facility from the VA Office of Rural Health’s Fiscal Year 2015 Rural Veterans Health Care Atlas, which categorizes rurality based on Rural-Urban Commuting Area classifications of the US census tract corresponding to the Veteran’s residence.18,19
Estimated Rates of LCS Among Eligible Veterans
We estimated LCS rates and 95% CIs by state and VA service region (numerator, number of unique Veterans with evidence of LCS in that geographic unit; denominator, estimated LCS-eligible Veterans in the population of that geographic unit). We used data on the 2018 Veteran population by state and VA regional service unit from the VA National Center for Veterans Analysis and Statistics.20 We further refined these denominators to account for age and smoking history to approximate LCS-eligible populations, as described subsequently herein. Of note, the VA National Center for Veterans Analysis and Statistics reports data on all living Veterans, not just those enrolled in the VA health care system, so our denominators (and consequently our estimated LCS rates within the VA system) are imprecise. However, our focus is on relative differences in estimated LCS rates across geographic units (ie, rate ratios comparing LCS rates in different geographic units, correlation between estimated LCS rates and need in the population), rather than absolute LCS rates; our estimates are suitable for this purpose.
By State
We used 2018 Behavioral Risk Factor Surveillance System data from the Centers for Disease Control and Prevention21 to estimate proportions of LCS-eligible Veterans for each state based on age and smoking history (55-79 years of age and smoked within prior 10 years, criteria that approximate Triplette’s validated criteria for identifying likely LCS-eligible individuals22); see e-Appendix 1 for details. We then multiplied these proportions of LCS-eligible Veterans by each state’s Veteran population to determine estimated populations of LCS-eligible Veterans in each state. To calculate LCS rates by state, screened Veterans were assigned to their state of residence, which in some cases differed from the state in which they underwent LCS, because our estimated state denominators (Behavioral Risk Factor Surveillance System sampling and Veteran populations) were based on state of residence.
By VA Service Region
The national VA system comprises 18 regional service networks (ie, Veterans Integrated Service Networks [VISNs]), with each VA facility assigned to one VISN.23 We estimated LCS-eligible populations per VISN in a three-step process: (1) first, we approximated the 55- to 80-year-old population from the overall Veteran population per VISN by adding 50% of the 45- to 64-year-old age group to 75% of the 65- to 84-year-old age group; (2) next, we multiplied this number for each VISN by the estimated proportion of Veterans in this age range who would meet LCS smoking pack-year criteria (we used 32%, informed by VA calculations for planning the VA LCS demonstration project24); and (3) finally, we multiplied this number by a factor to account for differences between national and VISN-specific smoking rates, using data from the 2018 Survey of Veteran Enrollee’s Health and Use of Health Care.25
Results
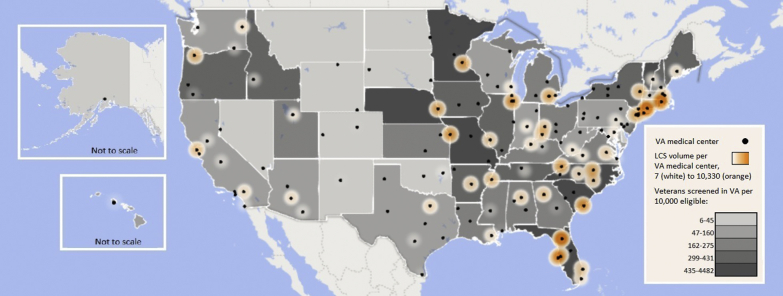
We identified 71,898 Veterans who underwent LCS in a VA facility between 2013 and 2019. We identified LCS examinations in 96 of 139 VA facilities (69.1%) in 44 states, with substantial variation in distribution across the country (Fig 1). Volume of LCS within facilities varied widely, including 20 facilities that offered only sporadic LCS (< 25 unique Veterans screened between 2013 and 2019) and 40 facilities that each screened > 500 Veterans during the study period (LCS volume indicated by heatmap in Figs 1 and 2). Whereas several states had multiple VA facilities that performed LCS, six states had none, despite an estimated 86,893 LCS-eligible Veterans living in these states (Delaware, 3,839; North Dakota, 7,249; South Dakota, 9,979; Montana, 13,626; Kansas, 24,846; and Iowa; 27,354) (Table 1). Every VA service region had VA facilities that performed LCS, but the number of screening facilities was not distributed evenly according to estimated populations of eligible Veterans (Table 2). For example, we identified more than twice as many VA facilities that perform LCS in VISN 12 (VA Great Lakes Health Care System) compared with VISN 15 (VA Heartland Network), despite similar estimated populations of LCS-eligible Veterans (VISN 12, five LCS facilities for an estimated 123,837-person population; VISN 15, two LCS facilities for an estimated 121,213-person population).
Figure 1.
Heatmap showing LCS in VA medical centers in the United States, 2013 through 2019: locations of VA medical centers and Veterans screened in VA centers per 10,000 eligible by state. LCS = lung cancer screening; VA = Veterans Health Administration.
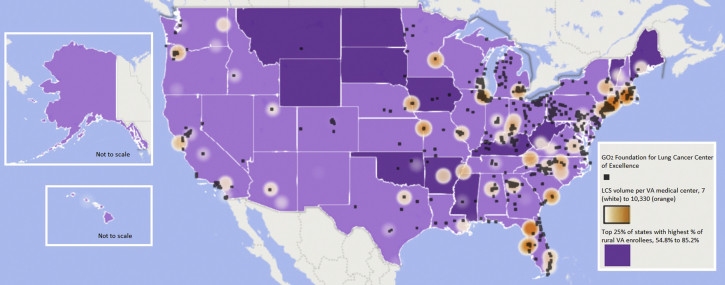
Figure 2.
Heatmap showing LCS in VA medical centers in the United States, 2013 through 2019: location of GO2 Foundation for Lung Cancer Partner sites and top 25% of states with highest percent of rural enrollees. LCS = lung cancer screening; VA = Veterans Health Administration.
Table 1.
Estimated LCS Rates and Screening Facilities by State
| US Census Region or State | Veterans Screened | Estimated Eligible Population | Estimated LCS Rate | VA Facilities With Any LCS | VA LCS Facilities After Removing Sites With < 25 Veterans Screened | GO2 Foundation for Lung Cancer Partner Sites |
|---|---|---|---|---|---|---|
| Northeast | ||||||
| Connecticut | 5,149 | 21,779 | 23.6 (23.0-24.3) | 1 | 1 | 9 |
| Maine | 558 | 14,282 | 3.9 (3.6-4.2) | 1 | 1 | 2 |
| Massachusetts | 2,671 | 36,627 | 7.3 (7.0-7.6) | 2 | 2 | 20 |
| New Hampshire | 333 | 11,040 | 3.0 (2.7-3.4) | 1 | 1 | 3 |
| New Jersey | 1,079 | 35,914 | 3.0 (2.8-3.2) | 1 | 1 | 25 |
| New York | 3,304 | 108,648 | 3.0 (2.9-3.1) | 4 | 4 | 47 |
| Pennsylvania | 591 | 125,686 | 0.5 (0.43-0.51) | 5 | 4 | 87 |
| Rhode Island | 2,689 | 6,000 | 44.8 (43.1-46.5) | 1 | 1 | 7 |
| Vermont | 234 | 5,326 | 4.4 (3.8-5.0) | 1 | 1 | 0 |
| Total Northeast | 16,608 | 365,300 | 4.5 (4.5-4.6) | 17 | 16 | 200 |
| Midwest | ||||||
| Illinois | 3,150 | 77,234 | 4.1 (3.9-4.2) | 3 | 2 | 35 |
| Indiana | 1,068 | 70,905 | 1.5 (1.4-1.6) | 2 | 1 | 28 |
| Iowa | 818 | 27,354 | 3.0 (2.8-3.2) | 0 | 0 | 5 |
| Kansas | 638 | 24,846 | 2.6 (2.4-2.8) | 0 | 0 | 2 |
| Michigan | 1,619 | 84,936 | 1.9 (1.8-2.0) | 4 | 1 | 37 |
| Minnesota | 2,252 | 47,532 | 4.7 (4.5-4.9) | 2 | 1 | 5 |
| Missouri | 2,892 | 66,445 | 4.4 (4.2-4.5) | 2 | 2 | 15 |
| Nebraska | 1,192 | 17,005 | 7.0 (6.6-7.4) | 1 | 1 | 8 |
| North Dakota | 5 | 7,249 | 0.1 (0.02-0.16) | 0 | 0 | 2 |
| Ohio | 2,415 | 142,008 | 1.7 (1.6-1.8) | 4 | 2 | 57 |
| South Dakota | 7 | 9,979 | 0.1 (0.03-0.14) | 0 | 0 | 1 |
| Wisconsin | 666 | 57,416 | 1.2 (1.1-1.3) | 1 | 1 | 21 |
| Total Midwest | 16,722 | 632,908 | 2.6 (2.6-2.7) | 19 | 11 | 216 |
| South | ||||||
| Alabama | 1,030 | 56,263 | 1.8 (1.7-1.9) | 3 | 1 | 16 |
| Arkansas | 1,253 | 29,042 | 4.34.1-4.6) | 2 | 1 | 1 |
| Delaware | 12 | 3,839 | 0.3 (0.2-0.5) | 0 | 0 | 1 |
| District of Columbia | 23 | 10,552 | 0.2 (0.1-0.3) | 1 | 1 | 3 |
| Florida | 10,330 | 236,493 | 4.4 (4.3-4.5) | 6 | 5 | 59 |
| Georgia | 2,227 | 93,173 | 2.4 (2.3-2.5) | 2 | 2 | 33 |
| Kentucky | 895 | 55,197 | 1.6 (1.5-1.7) | 2 | 2 | 33 |
| Louisiana | 556 | 34,179 | 1.6 (1.5-1.8) | 2 | 1 | 6 |
| Maryland | 389 | 43,052 | 0.9 (0.8-1.0) | 1 | 1 | 11 |
| Mississippi | 576 | 32,119 | 1.8 (1.7-1.9) | 2 | 2 | 4 |
| North Carolina | 4,035 | 77,137 | 5.2 (5.1-5.4) | 3 | 3 | 40 |
| Oklahoma | 207 | 45,983 | 0.5 (0.39-0.52) | 1 | 1 | 2 |
| South Carolina | 2,461 | 55,917 | 4.4 (4.2-4.6) | 1 | 1 | 13 |
| Tennessee | 3,159 | 75,939 | 4.2 (4.1-4.3) | 3 | 3 | 9 |
| Texas | 1,110 | 174,891 | 0.6 (0.60-0.67) | 4 | 3 | 14 |
| Virginia | 1,874 | 82,739 | 2.3 (2.2-2.4) | 3 | 3 | 35 |
| West Virginia | 430 | 27,080 | 1.6 (1.4-1.7) | 1 | 1 | 2 |
| Total South | 30,567 | 1,133,597 | 2.7 (2.67-2.73) | 37 | 31 | 282 |
| West | ||||||
| Alaska | 13 | 9,733 | 0.1 (0.07-0.23) | 1 | 0 | 0 |
| Arizona | 905 | 60,374 | 1.5 (1.4-1.6) | 2 | 2 | 1 |
| California | 2,969 | 185,042 | 1.6 (1.5-1.7) | 7 | 6 | 33 |
| Colorado | 46 | 44,458 | 0.1 (0.08-0.14) | 1 | 1 | 13 |
| Hawaii | 101 | 13,573 | 0.7 (0.6-0.9) | 1 | 1 | 0 |
| Idaho | 450 | 14,832 | 3.0 (2.8-3.3) | 1 | 1 | 2 |
| Montana | 8 | 13,626 | 0.1 (0.03-0.12) | 0 | 0 | 1 |
| Nevada | 31 | 36,848 | 0.1 (0.06-0.12 | 1 | 0 | 6 |
| New Mexico | 39 | 24,367 | 0.2 (0.11-0.22) | 1 | 1 | 0 |
| Oregon | 1,843 | 45,818 | 4.0 (3.8-4.2) | 2 | 2 | 13 |
| Utah | 328 | 11,933 | 2.7 (2.5-3.1) | 1 | 1 | 1 |
| Washington | 932 | 67,604 | 1.4 (1.3-1.5) | 3 | 3 | 5 |
| Wyoming | 22 | 6,754 | 0.3 (0.1-1.3) | 2 | 0 | 0 |
| Total West | 7,687 | 534,962 | 1.4 (1.41-1.47) | 23 | 18 | 75 |
| National total | 71,584a | 2,666,766 | 2.7 (2.67-2.70) | 96 | 76 | 773 |
Data are presented as No. or percentage (95% CI). States in the highest quartile when ranked by proportion of rural Veterans among all enrolled Veterans are shown in boldface. LCS = lung cancer screening; VA = Veterans Health Administration.
Excludes 314 Veterans who were screened in a VA facility, but who lived outside the United States or whose state of residence was missing.
Table 2.
Estimated LCS Rates and Screening Facilities by VA Service Region
| Veterans Integrated Service Network | Veterans Screened | Estimated Eligible Population | Estimated LCS Rate | VA Facilities With LCS |
|---|---|---|---|---|
| 1: VA New England Healthcare System | 11,837 | 113,787 | 10.4 (10.2-10.6) | 7 |
| 8: VA Sunshine Healthcare Network | 10,890 | 183,604 | 5.9 (5.8-6.0) | 6 |
| 23: VA Midwest Health Care Network | 4,704 | 121,804 | 3.9 (3.8-4.0) | 3 |
| 2: New York/New Jersey VA Health Care Network | 4,447 | 118,374 | 3.8 (3.6-3.9) | 5 |
| 9: VA MidSouth Healthcare Network | 4,851 | 150,128 | 3.2 (3.1-3.3) | 5 |
| 6: VA Mid-Atlantic Health Care Network | 5,560 | 173,659 | 3.2 3.1-3.3) | 6 |
| 15: VA Heartland Network | 3,865 | 121,213 | 3.2 (3.1-3.3) | 2 |
| 12: VA Great Lakes Health Care System | 3,291 | 123,837 | 2.7 (2.6-2.7) | 5 |
| 7: VA Southeast Network | 5,358 | 212,981 | 2.5 (2.4-2.6) | 6 |
| 20: VA Northwest Network | 3,219 | 168,713 | 1.9 (1.8-2.0) | 7 |
| 10: VISN 10: VA Healthcare System | 4,945 | 303,904 | 1.6 (1.6-1.7) | 9 |
| 21: VA Sierra Pacific Network | 2,161 | 144,369 | 1.5 (1.4-1.6) | 6 |
| 22: VA Desert Pacific Healthcare Network | 1,826 | 203,440 | 0.9 (0.86-0.94) | 6 |
| 5: VA Capitol Health Care Network | 864 | 106,023 | 0.8 (0.76-0.87) | 3 |
| 16: South Central VA Health Care Network | 1,849 | 247,328 | 0.7 (0.71-0.78) | 6 |
| 17: VA Heart of Texas Health Care Network | 1,124 | 165,287 | 0.7 (0.64-0.72) | 4 |
| 19: Rocky Mountain Network | 578 | 132,381 | 0.4 (0.40-0.47) | 5 |
| 4: VA Healthcare—VISN 4 | 529 | 170,781 | 0.3 (0.28-0.33) | 5 |
Data are presented as No. or percentage (95% CI). LCS = lung cancer screening; VA = Veterans Health Administration.
We observed marked variation in LCS rates across states and VA regional networks (Fig 1, Tables 1, 2), with only weak correlation between estimated LCS rates and need, determined by estimated LCS-eligible Veterans in the population (state-level correlation coefficient, –0.044; VISN-level correlation coefficient, –0.30). Overall, Northeastern states showed the highest estimated LCS rates and Western states showed the lowest rates, with variability across Midwestern states. In 15 states (seven in the West, five in the South, two in the Midwest, one in the Northeast), we estimated that < 1% of eligible Veteran residents had undergone LCS, whereas in two Northeastern states (Connecticut and Rhode Island), we estimated that > 20% of LCS-eligible Veteran residents had undergone screening. Estimated LCS rates varied more than 30-fold across VA service regions, ranging from < 0.5% in VISN 4 (Pennsylvania and Delaware) and the Rocky Mountain network (VISN 19) to 10.4% (95% CI, 10.2%-10.6%) in the highest-screening region (VISN1, VA New England; rate ratio, 33.6 [95% CI, 30.8-36.7] for VA New England vs VISN 4).
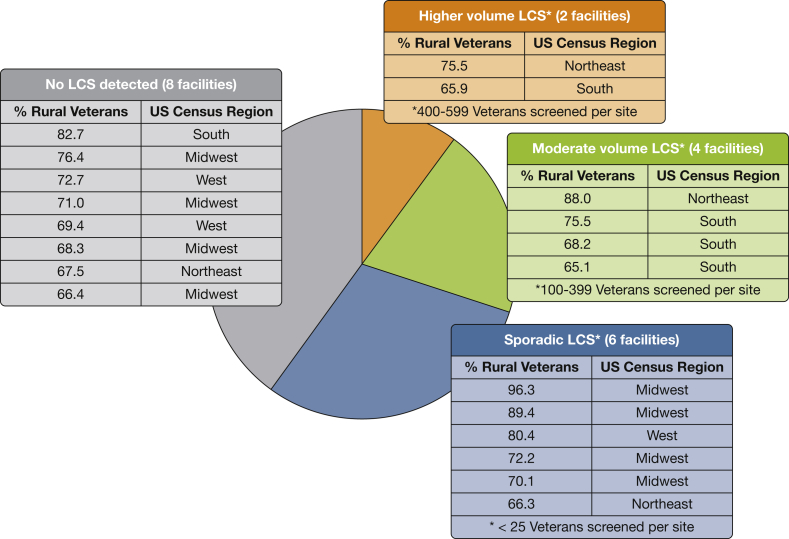
Access to LCS was limited for Veterans living in rural areas. Among the 20 VA medical centers that serve the highest proportion of rural Veterans, six facilities (30%) screened > 100 unique Veterans between 2013 and 2019, whereas an additional six facilities performed only sporadic LCS (Fig 3). Among the 12 states that serve the highest proportions of rural Veterans (boldface values in Table 1), only nine VA facilities performed more than sporadic LCS. By visual inspection, distribution of GO2 Foundation for Lung Cancer partner sites largely mirror concentration of VA LCS services, with many sites along the East Coast and in major West Coast cities, and fewer screening centers in Midwestern and Western plains and mountain states (Fig 2). Of note, partner sites provide some, albeit in places limited, access in states where the VA has yet to establish LCS programs: with the VA and GO2 Foundation for Lung Cancer partnership, every state now has at least one site where eligible Veterans can access LCS. However, among > 750 GO2 Foundation for Lung Cancer sites, only 50 are located in the 12 states with the highest proportion of rural Veterans, and 33 of these are in a single state (Kentucky; see boldface values in Table 1).
Figure 3.
Pie chart showing LCS volume at the top 20 rural-serving Veterans Health Administration medical centers. LCS = lung cancer screening.
Discussion
In this first national analysis comparing rates of LCS among estimated eligible Veteran populations in each state and VA regional service unit, we found that LCS rates and number of VA sites that performed screening varied dramatically across both state and VA regional service units. Importantly, our study was able to identify critical gaps in LCS access across states that could be masked when data are aggregated to the regional or national level. To the best of our knowledge, we are also the first to characterize the distribution of the LCS screening centers added by VA’s new partnership with the GO2 Foundation for Lung Cancer, which expands LCS access for Veterans to several hundred sites outside of the VA network. We found that both VA and GO2 Foundation for Lung Cancer LCS sites occur largely in metropolitan areas in the East, Midwest, and along the Pacific coast, with far fewer LCS sites for Veterans living in rural areas in the central plains and Rocky Mountain states.
We note that the geographic distribution of screening facilities and the number of Veterans screened does not always seem proportionate to state or regional need. For example, Arkansas, Mississippi, and Louisiana are among the states with the highest lung cancer incidence and mortality in the United States, but VISN 16 has among the lowest estimated LCS rates among VA regional units.26 Despite the known higher lung cancer risk among rural populations,14 Veterans in rural areas have less access to LCS in the VA system, via the GO2 Foundation for Lung Cancer partnership, and through Medicare than individuals in urban areas, demonstrating continued disparities in this marginalized population.7,8 Expansion of access via the GO2 Foundation for Lung Cancer partnership provides some additional rural LCS locations and certainly increases LCS capacity in many densely populated urban areas with high concentrations of eligible but unscreened Veterans. However, by visual inspection, a number of states, including several in the highest quartile of proportion of rural Veterans enrolled, have comparatively limited LCS access even after the addition of GO2 Foundation for Lung Cancer sites.
Although LCS has increased over time in the national VA system,10 overall LCS rates remain unacceptably low. In both the VA system and outside of the VA, less than 5% of eligible individuals have been screened for lung cancer nationally,10,11 compared with 65% to 85% of Veterans screened for colorectal cancer in Medicare and the VA, respectively.27 The VA and GO2 Foundation for Lung Cancer partnership represents a step in the right direction and likely will increase LCS rates by augmenting capacity, which has been associated with LCS rates in other studies.11,28 However, by visual inspection and by the number of LCS sites added in states with high proportions of rural Veterans, the GO2 Foundation for Lung Cancer partnership does not seem to address fully the rural disparities in LCS access. Moreover, the extent to which Veterans and VA providers will capitalize on the option to obtain LCS through GO2 Foundation for Lung Cancer screening centers remains unknown. Even if there is robust use by Veterans of LCS through GO2 Foundation for Lung Cancer sites, successful care coordination across health-care systems is challenging because of the lack of a shared electronic medical records, imaging systems, or well-established relationships between providers.29,30 Breakdowns in communication and fragmentation of care create the potential for lower-quality care, higher costs, and worse outcomes for patients.31 Thus, the VA also should pursue other options beyond the GO2 Foundation for Lung Cancer partnership to ensure equitable LCS access. One promising strategy to increase LCS access and uptake in underserved rural areas is to offer screening through a mobile LDCT imaging scanner unit,32,33 which then can transmit images to a VA facility in the region with an existing LCS program for interpretation and recommendations for next steps.
A precedent exists for coordinating LCS services at the regional level in the VA system. In 2017, the VA New England Healthcare System (VISN 1) approved a policy to support and coordinate LCS services across the eight VA facilities in the regional network using a hub-and-spoke model. The VISN provided resources to support LCS implementation in the region, including funding for LCS nurse coordinators (effort supported depended on projected LCS-eligible Veterans served by the facility) to champion LCS and coordinate care before and after LCS; provided support to activate standardized clinical reminders for LCS in the VA’s electronic medical record; provided support to implement software to track LCS findings and any needed evaluation; and provided a regional LCS council including LCS coordinators and physician leads that holds regular calls to share best practices across sites and to troubleshoot barriers to implementation. Likely in part because of this concerted effort to support and coordinate LCS services across the region, VISN 1 achieved estimated LCS rates substantially higher than any other VA regional service unit, and even the two states in New England that rank in the highest quartile of proportion of rural Veterans showed estimated LCS rates well above the VA’s national average (estimated LCS rates: Vermont, 4.4% [95% CI, 3.8%-5.0%]; Maine, 3.9% [95% CI, 3.6%-4.2%]; United States, 2.7% [95% CI, 2.67%-2.70%]).
Our study has limitations. We may have misestimated the numerator of screened Veterans if LCS examinations were miscoded as diagnostic CT scans or vice versa. We may have misestimated the denominator of LCS-eligible Veterans if self-reported smoking histories in survey data were inaccurate or if age across the 45- to 85-year-old range was distributed unequally. Critically, these inaccuracies are unlikely to affect specific geographic units disproportionately, increasing confidence in the relative differences we observed. Most conclusions about geographic distribution and gaps in services were based on visual inspection, rather than spatial analysis methods. Because our analysis is focused on VA services, our estimated LCS rates do not account for Veterans screened outside the VA; we do not include Veterans who may have been screened in GO2 Foundation for Lung Cancer sites, because we captured LCS performed through 2019 and the VA and GO2 Foundation for Lung Cancer partnership did not begin until June 2020. Of note, the true rate of LCS among Veterans likely is higher than what we report, given that some Veterans may have undergone screening in the private sector (ie, our numerator may be too low) and that not all Veterans included in our Veteran population estimates receive their care through the VA system (ie, our denominator is too high).
Interpretation
As a nationally integrated health system with potential for service coordination across regional units, the VA is uniquely positioned to provide high-quality LCS, to address observed inequalities in LCS access to mitigate disparities in rural and underserved areas, and ultimately to reduce lung cancer mortality. An early adopter and innovator in the field of LCS from the time of the carefully planned and coordinated eight-site VA LCS demonstration project,9 the VA has developed best practices for high-quality LCS (eg, standardized clinical reminders for use in the VA’s common electronic medical record, VISN 23’s pulmonary nodule evaluation tracking software system, VA Portland’s centralized LCS program model) and has leveraged its national network successfully to spread these best practices to other VA sites.24,34,35 To continue to improve LCS quality, access, and uptake among eligible Veteran populations, critical next steps include raising awareness among Veterans and VA providers about LCS, including the option for screening at GO2 Foundation for Lung Cancer partner sites; setting goals and incentives for providers to offer LCS to eligible Veterans; continuing to expand LCS access by coordinating services across regional units using successful hub-and-spoke models such as VA New England’s; and supporting facilities that offer LCS with resources and infrastructure to promote high-quality screening, evaluation of screen-detected abnormalities, and downstream cancer care.36,37 With the new multimillion-dollar VA Lung Precision Oncology Program, which will provide funding for 18 VA medical centers across the country to expand and coordinate LCS and precision oncology services within their VISNs, the VA again demonstrates its commitment to ensuring equitable access to reduce lung cancer mortality for all Veterans.38
Take-home Points.
Study Question: From 2013 through 2019, during which time the VA encouraged implementation of VA LCS programs, to what extent has LCS access in the VA and additional partner sites matched the distribution of eligible Veterans at state and regional levels?
Results: Among the 71,898 LCS examinations identified in 69.1% of VA facilities, screening rates varied across states (0-8 VA LCS facilities per state) and regional networks (rate ratio, 33.6 [95% CI, 30.8-36.7] for VA New England compared with the VA service region in Pennsylvania and Delaware) and demonstrated weak correlation between eligible populations and LCS rates (coefficient, –0.30), leaving gaps in rural areas where neither VA facilities nor GO2 Foundation for Lung Cancer partnership sites offer LCS.
Interpretaion: Although partnering with the GO2 Foundation for Lung Cancer expands LCS capacity and access, geographic disparities persist in rural areas and those without strong programs, leaving the nationally integrated VA system with an opportunity to leverage regional resources to distribute and coordinate LCS services better to ensure equitable access.
Acknowledgments
Author contributions: J. H. B., T. J. C., D. R. M., and R. S. W conceived and designed the study. J. H. B. and S. Q. acquired the data: J. H. B., T. J. C., D. R. M., S. Q., and R. S. W. analyzed and interpreted the data. J. H. B. drafted the manuscript. J. H. B., T. J. C., D. R. M., E. R. N., S. Q., and R. S. W. provided critical revision of the manuscript for important intellectual content. R. S. W. obtained funding. R. S. W. supervised the study and is the guarantor of the study data.
Financial/nonfinancial disclosures: R. S. W. serves as Co-Chair of the VISN1 lung council screening council, but does not receive financial compensation for this role. None declared (J. H. B., D. R. M., S. Q., E. R. N., T. J. C.).
Role of sponsors: The funding organizations had no role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript.
Other contributions: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Additional information: The e-Appendix can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: This study was funded by VA HSR&D IIR 18-075, and with resources from the VA Bedford Healthcare System, the VA Boston Healthcare System, and the VA Ann Arbor Healthcare System. Dr Nunez was supported by the National Institutes of Health [Grant T32 HL-007035].
Supplementary Data
References
- 1.National Lung Screening Trial Research Team. Aberle D.R., Adams A.M., et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Koning H.J., van der Aalst C.M., de Jong P.A., et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503–513. doi: 10.1056/NEJMoa1911793. [DOI] [PubMed] [Google Scholar]
- 3.Moyer V.A., U S Preventive Services Task Force Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(5):330–338. doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare and Medicaid Services Decision memo for screening for lung cancer with low dose computed tomography (LDCT) (CAG-00439N). Centers for Medicare and Medicaid Services website. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274
- 5.Sahar L., Douangchai Wills V.L., Liu K.K., Kazerooni E.A., Dyer D.S., Smith R.A. Using geospatial analysis to evaluate access to lung cancer screening in the United States. Chest. 2021;159(2):833–844. doi: 10.1016/j.chest.2020.08.2081. [DOI] [PubMed] [Google Scholar]
- 6.Kale M.S., Wisnivesky J., Taioli E., Liu B. The landscape of US lung cancer screening services. Chest. 2019;155(5):900–907. doi: 10.1016/j.chest.2018.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eberth J.M., Bozorgi P., Lebron L.M., et al. Geographic availability of low-dose computed tomography for lung cancer screening in the United States, 2017. Prev Chronic Dis. 2018;15:E119. doi: 10.5888/pcd15.180241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiener R.S., Rivera M.P. Access to lung cancer screening programs in the United States: perpetuating the inverse care law. Chest. 2019;155(5):883–885. doi: 10.1016/j.chest.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 9.Kinsinger L.S., Atkins D., Provenzale D., Anderson C., Petzel R. Implementation of a new screening recommendation in health care: the Veterans Health Administration’s approach to lung cancer screening. Ann Intern Med. 2014;161(8):597–598. doi: 10.7326/M14-1070. [DOI] [PubMed] [Google Scholar]
- 10.Lewis J.A., Samuels L.R., Denton J., et al. National lung cancer screening utilization trends in the Veterans Health Administration. JNCI Cancer Spectr. 2020;4(5):pkaa053. doi: 10.1093/jncics/pkaa053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fedewa S.A., Kazerooni E.A., Studts J.L., et al. State variation in low-dose CT scanning for lung cancer screening in the United States [published online ahead of print November 12, 2020]. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djaa170
- 12.Okereke I.C., Nishi S., Zhou J., Goodwin J.S. Trends in lung cancer screening in the United States, 2016-2017. J Thorac Dis. 2019;11(3):873–881. doi: 10.21037/jtd.2019.01.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Veterans Affairs Office of Public and Intergovernmental Affairs VA and GO2 Foundation for Lung Cancer partner to improve outcomes for veterans at risk of lung cancer. United States Department of Veterans Affairs website. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5468
- 14.Atkins G.T., Kim T., Munson J. Residence in rural areas of the United States and lung cancer mortality. Disease incidence, treatment disparities, and stage-specific survival. Ann Am Thorac Soc. 2017;14(3):403–411. doi: 10.1513/AnnalsATS.201606-469OC. [DOI] [PubMed] [Google Scholar]
- 15.United States Department of Veterans Affairs Health Services Research & Development VA informatics and computing infrastructure. Corporate Data Warehouse (CDW). United States Department of Veterans Affairs website. https://www.hsrd.research.va.gov/for_researchers/vinci/cdw.cfm
- 16.American College of Radiology Lung CT Screening Reporting & Data System (Lung-RADS). American College of Radiology website. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads
- 17.GO2 Foundation for Lung Cancer Screening centers. GO2 Foundation for Lung Cancer website. https://g02foundation.org/risk-early-detection/screening-centers/
- 18.U.S. Department of Veterans Affairs Office of Rural Health. Rural veterans health care atlas FY 2015. United States Department of Veterans Affairs website. https://www.ruralhealth.va.gov/aboutus/rvhc_atlas_fy2015.asp
- 19.United States Department of Agriculture Economic Research Service Rural-urban commuting area codes. United States Department of Agriculture website. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
- 20.United States Department of Veterans Affairs National Center for Veterans Analysis and Statistics Veteran population. United States Department of Veterans Affairs website. https://www.va.gov/vetdata/Veteran_Population.asp
- 21.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System survey data. Centers for Disease Control and Prevention website. https://www.cdc.gov/brfss/index.html
- 22.Triplette M., Donovan L.M., Crothers K., Madtes D.K., Au D.H. Prediction of lung cancer screening eligibility using simplified criteria. Ann Am Thorac Soc. 2019;16(10):1280–1285. doi: 10.1513/AnnalsATS.201903-239OC. [DOI] [PubMed] [Google Scholar]
- 23.United States Department of Veterans Affairs Interactive US map. United States Department of Veterans Affairs website. https://www.va.gov/directory/guide/map.asp
- 24.Kinsinger L.S., Anderson C., Kim J., et al. Implementation of lung cancer screening in the Veterans Health Administration. JAMA Intern Med. 2017;177(3):399–406. doi: 10.1001/jamainternmed.2016.9022. [DOI] [PubMed] [Google Scholar]
- 25.Veterans Health Administration VA survey of veteran enrollees’ health and use of health care. United States Department of Veterans Affairs website. https://www.va.gov/health/survey.asp
- 26.Centers for Disease Control and Prevention United States cancer statistics: data visualizations. Centers for Disease Control and Prevention website. https://gis.cdc.gov/Cancer/USCS/DataViz.html
- 27.United States Department of Veterans Affairs Quality of care: prevention—colorectal cancer screening. United States Department of Veterans Affairs website. https://www.va.gov/QUALITYOFCARE/initiatives/compare/Prevention_Colorectal_Cancer_Screening.asp
- 28.Charkhchi P., Kolenic G.E., Carlos R.C. Access to lung cancer screening services: preliminary analysis of geographic service distribution using the ACR Lung Cancer Screening Registry. J Am Coll Radiol. 2017;14(11):1388–1395. doi: 10.1016/j.jacr.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anderson E., Wiener R.S., Resnick K., Elwy A.R., Rinne S.T. Care coordination for veterans with COPD: a positive deviance study. Am J Manag Care. 2020;26(2):63–68. doi: 10.37765/ajmc.2020.42394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zuchowski J.L., Chrystal J.G., Hamilton A.B., et al. Coordinating care across health care systems for veterans with gynecologic malignancies: a qualitative analysis. Med Care. 2017;55(suppl 7, suppl 1):S53–S60. doi: 10.1097/MLR.0000000000000737. [DOI] [PubMed] [Google Scholar]
- 31.Frandsen B.R., Joynt K.E., Rebitzer J.B., Jha A.K. Care fragmentation, quality, and costs among chronically ill patients. Am J Manag Care. 2015;21(5):355–362. [PubMed] [Google Scholar]
- 32.Raghavan D., Wheeler M., Doege D., et al. Initial results from mobile low-dose computerized tomographic lung cancer screening unit: improved outcomes for underserved populations. Oncologist. 2020;25(5):e777–e781. doi: 10.1634/theoncologist.2019-0802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lam A.C.L., Aggarwal R., Cheung S., et al. Predictors of participant nonadherence in lung cancer screening programs: a systematic review and meta-analysis. Lung Cancer. 2020;146:134–144. doi: 10.1016/j.lungcan.2020.05.013. [DOI] [PubMed] [Google Scholar]
- 34.Shelver J., Wendt C.H., McClure M., et al. Effect of an automated tracking registry on the rate of tracking failure in incidental pulmonary nodules. J Am Coll Radiol. 2017;14(6):773–777. doi: 10.1016/j.jacr.2017.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.VA Portland Healthcare System Oregon veterans among first in VA to take part in innovative lung cancer screening program now going national. VA Portland Healthcare System website. https://www.portland.va.gov/features/Portland_Innovative_Lung_Cancer_Screening_Program.asp
- 36.Wiener R.S., Gould M.K., Arenberg D.A., et al. An official American Thoracic Society/American College of Chest Physicians policy statement: implementation of low-dose computed tomography lung cancer screening programs in clinical practice. Am J Respir Crit Care Med. 2015;192(7):881–891. doi: 10.1164/rccm.201508-1671ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mazzone P., Powell C.A., Arenberg D., et al. Components necessary for high-quality lung cancer screening: American College of Chest Physicians and American Thoracic Society Policy Statement. Chest. 2015;147(2):295–303. doi: 10.1378/chest.14-2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collins C. VA research: the VA National Precision Oncology Program. Building a system of excellence for cutting-edge cancer care. Defense Media Network website. https://www.defensemedianetwork.com/stories/va-research-the-u-s-department-of-veterans-affairs-national-precision-oncology-program/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.