Abstract
Background
The majority of living organ donors are women, but few are deceased organ donors, which increases risks associated with sex mismatched organs. We sought to identify reasons for sex disparities in organ donation and strategies for equity.
Methods and Results
Using Amazon's Mechanical Turk, we examined US adults' perceptions regarding donation in a mixed‐methods survey study. Results were compared by sex with Fisher's exact test and T‐tests for quantitative results and qualitative descriptive analyses for write‐in responses. Among 667 participants (55% women), the majority of men (64.8%) and women (63.4%) self‐identified as registered donors. Women's willingness to donate their own organs to family members (P=0.03) or strangers (P=0.03) was significantly higher than men. Donors from both sexes were guided by: desire to help, personal experience, and believing organs would be useless to deceased donors. Non‐donors from both sexes were guided by: no reason, medical mistrust, contemplating donation. When considering whether to donate organs of a deceased family member, women were equally guided by a family member's wishes and believing the family member had no further use for organs. Men had similar themes but valued the family member's wishes more. Among non‐donors, both sexes would consider donation if more information was provided.
Conclusions
In a national survey, both sexes had similar reasons for becoming and not becoming an organ donor. However, compared with men, women were more willing to donate their organs to family members and strangers. Improving education and communicating wishes regarding organ donation with direct relatives may increase sex equity in deceased organ donation.
Keywords: organ donation, sex disparities, women's health
Subject Categories: Transplantation, Ethics and Policy, Health Services
Nonstandard Abbreviations and Acronyms
- MTurk
Amazon's Mechanical Turk
Clinical Perspective
What Is New?
Both sexes had similar reasons for donating organs.
Compared with men, women were significantly more willing to donate organs to a family member and to a stranger.
Men valued the wishes of a family member more than women when making decisions about donating a direct relative's organs.
What Are the Clinical Implications?
There may be a miscommunication between men and women about their wishes to donate organs, and this can be addressed by discussing wishes to donate organs with direct relatives.
There are opportunities to improve organ donation through public education about the process of becoming an organ donor.
Sex disparities in the living and deceased organ donor pool continue to exist. 1 The majority of living organ donors are women (60%), but less than half of deceased organ donors are women (40%). 1 These sex differences in organ donation have persisted for over 25 years 1 and may be influenced by the rate of donation refusal. A 2013 study found an 11.1% refusal rate amongst family members considering organ donation of a recently deceased individual. 2 The majority of family members that refused donation were women. This is problematic because sex disparities in organ donation contribute to sex mismatch in transplant recipients, which is associated with worse outcomes among transplant recipients. 3 , 4 Women represent more than 40% of candidates awaiting many organs available through deceased organ donation. 1 Thus, achieving an equitable sex deceased donor pool is a priority.
Sex differences in deceased organ donation rate may be related to the cause of death. The main causes of death for deceased organ donors include stroke (35.7%) and trauma (28.5%). 1 Among donors, more women die from strokes, and more men die from trauma. 1 In addition, there was a rise in the number of deceased organ donors due to the opioid crisis in the US. From 2000 to 2016, there was an over 11% increase in drug overdose‐induced deaths, and the majority of these deaths were comprised of men (61.2%). 5 , 6 However, these differences do not fully explain sex differences in deceased organ donation rates.
Understanding the reasons behind organ donor registration can contribute to strategies to diversify the donor pool. A 2014 study suggested that organ donors registered because they value altruism. 7 Another study identified insufficient information regarding organ donation processes as the main reason for not registering to become a donor. 8 Fear of unethical organ procurement is also known to impact the decision to donate. 8 Additional studies suggest that age, socioeconomic position, religious beliefs, geography, and race or ethnicity can contribute to the disparity between registered donors across the sexes. 9 , 10 , 11 Though a variety of sociodemographic factors are known to impact donor status, major reasons for differences in organ donor registration by sex have not been extensively addressed.
Using Amazon's Mechanical Turk (MTurk), we performed a simultaneous mixed‐methods quantitative and qualitative survey among adults residing in the US. We sought to identify reasons for disparities in deceased organ donation between sexes and strategies to increase the number of deceased organ donors. Since the majority of living organ donors are women, we wondered whether there may be (1) a disconnect in honoring or sharing women's wishes of organ donation with next of kin that could impact deceased organ donation, or (2) sex differences in motivation for organ donation, such as deciding who will receive the organ with a live organ donation but not deceased organ donation.
Methods
The data that supports the findings of this study are available upon request from the corresponding author.
Survey Design
The study team performed an extensive literature search to identify known factors contributing to organ donation registration among the general public 8 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 and developed a survey that would specifically examine differences in organ donation by sex among the general public. Survey questions focused on personal decisions regarding individual organ donation including motivation to donate, communication of wishes with family, and whether or not guiding who (family member or stranger) the organ was going to mattered as this could be a critical distinction between decisions for live and deceased organ donation. Deceased organ donations often go to strangers, and live donations often go to family members. Since family members typically make the final decision for deceased organ donation, survey questions focused on relationship status, knowledge of organ donor registration status for family members, and willingness to donate organs of a deceased family member, particularly a spouse. Non‐donors were specifically asked about methods to reconsider the decision to donate. The survey was created and uploaded on Qualtrics XM, a survey platform. Then surveys were iteratively pre‐tested among a sample of more than 15 laypersons and healthcare workers in Arizona to assure clarity in both questions and categorical response choices. The survey was finalized when there were no additional recommendations for changes to the survey. The final survey was expected to take under 10 minutes to complete.
Survey Instrument
Categorical questions included demographics (age, sex, race, ethnicity, marital status, education, state of residency), donor registration status (participant and participant's family), relationships with organ donation (do you know someone that is: organ recipient, registered donor, dialysis patient, organ transplant list, none of the above) (Figure, Data S1). Following these questions, Likert scale questions regarding participant's willingness to donate to a family member or a stranger were asked (rating: 1=being very unlikely to 5=very likely).
Figure 1. Key survey components.
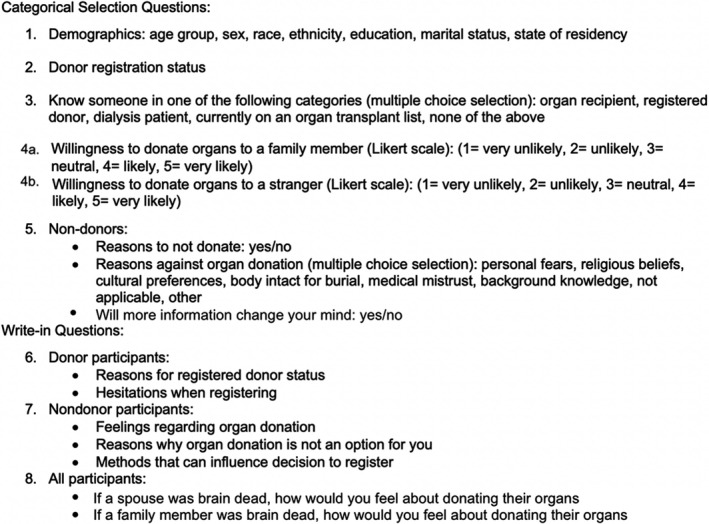
Survey questions included categorical selection questions and write‐in questions.
Skip logic was performed for remaining questions according to participants' self‐identified donor status. Among self‐identified non‐donors, categorical questions included whether or not they had reasons to not donate organs (yes/no), multiple choice selections included possible reasons against organ donation (personal fears, religious beliefs, cultural preferences, body intact for burial, medical mistrust, background knowledge, not applicable, and other), and asked whether or not more information would change their mind (yes/no). Write‐in questions for non‐donors included discussing their feelings regarding organ donation, reasons why organ donation is not an option, and describing methods that may change their decision regarding donor registration. Among donor participants, write‐in questions included reasons for registering as an organ donor and for any hesitations they experienced when registering. Among all participants, write‐in questions included discussing their feelings regarding organ donation in the setting of brain death of their spouse if applicable, and family members if applicable.
Data Source
MTurk was used to recruit participants for the survey study. MTurk is a global crowdsourcing marketplace owned by Amazon that is used to recruit survey participants for a fee. Scientists can select inclusion and exclusion participant criteria for surveys that limit which surveys are available for participants through MTurk. Eligible participants may choose to participate based upon interest in the title and description of survey as well as compensation. Then participants are directed to a survey platform to complete the survey, which was located at Qualtrics XM. Scientists and survey developers do not have access to the data of participants in MTurk, and participants do not have access to the data of scientists and survey developers. A denominator of eligible participants is not made available to scientists.
Surveys completed through MTurk are an established mechanism for obtaining reliable convenience survey data. 18 MTurk is being increasingly used for electronic surveys since participants can be quickly identified, and subsequently survey studies are completed rapidly. 18 , 19 While MTurk participants are similar to participants from other electronic surveys, important differences exist between MTurk participants and the general public. The majority of MTurk participants are women, born after 1970, single, White race, have below average income but higher education compared with the general population. 20 , 21 Given the need to examine women's reasons for and against becoming an organ donor, MTurk was considered a reasonable source for this study.
Study Design and Participants
A mixed‐methods simultaneous quantitative and qualitative convenience survey study was performed September 2019. Inclusion criteria were created on MTurk to only allow participants access to the survey if they were 18 years of age or older and residents of the US. Participants were excluded for survey responses that were nonsensical (n=56), plagiarized from transplant or organ donor websites (n=29), incomplete (n=77), or repetitive identical responses to differing study questions (n=48). Among 887 participants, a total of 210 were excluded, resulting in a final cohort of 667 participants. Participants provided consent for survey participation and received compensation of $1.00 after survey completion. This study was approved by the University of Arizona Institutional Review Board.
Statistical Analysis
Quantitative Analyses
Demographics were descriptively compared. Nominal categorical variables were compared using Fisher's exact tests. T‐tests were used to compare willingness to donate organs to strangers and family members by sex. As a secondary analysis, data were stratified by marital status (married or not married) since decisions regarding deceased organ donation among married individuals often defaults to the spouse. Willingness to donate to family or a stranger was compared by sex among married and non‐married using T‐tests. A P value threshold of 0.05 was considered statistically significant. All analyses were executed using R version 3.6.3. 22
Qualitative Analyses
Inductive qualitative descriptive analyses were performed for write‐in survey responses. Survey results were examined for common, repetitive patterns—themes that explained reasons for and against organ donation. Analysts were masked or blinded to participant demographics and donor registration type (donor versus non‐donor). First, 2 team members (E.Y., B.D.) independently performed open coding for all survey responses, describing the main idea of each of the participant responses. The main ideas were organized into themes (patterns) until saturation (no new themes) were achieved. Second, team members met with the primary investigator (K.B.) to consolidate themes into broader patterns and arbitrate differences between team member's findings during a series of research meetings. Third, themes were unmasked to participant sex and donor registration type and categorized by participant sex and donor registration type. Themes repeated by at least 10% of the participant group were maintained as main themes. Illustrative (exemplar) quotes were selected to demonstrate the main themes in a table.
Rigor for qualitative analyses was established according to Lincoln and Guba's Evaluative Criteria for qualitative research. 23 , 24 Credibility and triangulation were achieved through validation of participant write‐in responses with the Likert scale survey questions. Transferability included debriefing with the primary investigator, an advanced heart failure and transplant cardiologist, and with the study team members. Confirmability was attained via trained team members who performed the qualitative descriptive analyses (E.Y., B.D.) in conjunction with supervision by the primary investigator. Dependability was accomplished by maintaining a decision trail of the coding process throughout the analyses. No existing relationships were present between study team members and participants. The entire study team consisted of women.
Results
Primary Analysis: Sex Differences
Quantitative Survey Results
Among 667 participants, 55% were women (Table 1). The majority of participants were in the 18‐ to 40‐year age group (63%). Most participants were Non‐Hispanic White (women 72%, men 66%), Hispanic (women 9%, men 15%), and Non‐Hispanic African American (women 7%, men 10%) racial and ethnic groups. Participants resided among 49 US states plus D.C., and a higher proportion resided in the South and West regions of US. A higher proportion of women than men completed high school or received a GED (women 31%, men 25%), and a higher proportion of men attained a bachelor or associate degree (women 48%, men 56%). A lower proportion of both men (37%) and women (48%) participants were married.
Table 1.
Participant Demographics
| Variable |
Men N=301 (45.1%) |
Women N=366 (54.9%) |
|---|---|---|
| Registered donor | 195 (64.8%) | 232 (63.4%) |
| Age group | ||
| 18–30 y | 112 (37.2%) | 96 (26.2%) |
| 31–40 y | 99 (32.9%) | 114 (31.1%) |
| 41–50 y | 49 (16.3%) | 66 (18.0%) |
| 51–60 y | 27 (9.0%) | 58 (15.8%) |
| 61–70 y | 10 (3.3%) | 31 (8.5%) |
| 71+ y | 4 (1.3%) | 1 (0.3%) |
| Race and ethnicity | ||
| Non‐Hispanic White | 198 (65.8%) | 264 (72.1%) |
| Non‐Hispanic African‐American | 31 (10.3%) | 26 (7.1%) |
| Hispanic | 45 (15.0%) | 34 (9.3%) |
| Non‐Hispanic Asian | 22 (7.3%) | 23 (6.3%) |
| American Indian | 1 (0.3%) | 5 (1.4%) |
| Other* | 4 (1.3%) | 14 (3.8%) |
| Education | ||
| Less than high school | 0 (0.0%) | 1 (0.3%) |
| Some high school, no diploma | 6 (2.0%) | 16 (4.4%) |
| Completed high school/GED | 74 (24.6%) | 115 (31.4%) |
| Associate's/Bachelor's degree | 169 (56.1%) | 175 (47.8%) |
| Master's/Doctorate degree | 52 (17.3%) | 59 (16.1%) |
| Marital status | ||
| Single, never married | 165 (54.8%) | 138 (37.7%) |
| Married | 110 (36.5%) | 175 (47.8%) |
| Divorced | 21 (7.0%) | 43 (11.7%) |
| Separated | 3 (1.0%) | 6 (1.6%) |
| Widowed | 2 (0.7%) | 4 (1.1%) |
| Region of residency | ||
| Northeast | 44 (14.6%) | 68 (18.6%) |
| Midwest | 52 (17.3%) | 69 (18.9%) |
| South | 114 (37.9%) | 122 (33.3%) |
| West | 88 (29.2%) | 105 (28.7%) |
| Unknown | 3 (1.0%) | 2 (0.5%) |
Other refers to additional Racial/Ethnic Groups.
The majority of men (65%) and women (63%) were registered organ donors (Table 1). There were no significant differences by sex in donor status of participants' family members (Table 2). However, over 20% of men and women stated that they did not know the donor status of family members. There were no significant differences by sex among participants' acquaintances with individuals who were donors, transplant recipients, awaiting transplant, or requiring dialysis. Among non‐donors, there were no significant differences by sex in reasons to not donate, and likelihood that more information will change their mind. Among all participants, women were more willing than men to donate organs to a family member (Likert Scale rating: 1=being very unlikely to 5=very likely; women: 4.15 [95% CI: 4.04–4.26]; men: 3.97 [95% CI: 3.85–4.09]; P=0.03) and to a stranger (women: 3.35 [95% CI: 3.23–3.48]; men, 3.13 [95% CI: 2.99–3.28]; P=0.03) (Table 2).
Table 2.
Quantitative Survey Responses
| Variable |
Men N=301 (donors: N=195; non‐donors: N=106) |
Women N=366 (donors: N=232; non‐donors: N=134) |
P value |
|---|---|---|---|
| Family member registered donor | 0.80 | ||
| Yes | 188 (62.5%) | 227 (62.0%) | |
| No | 45 (15.0%) | 61 (16.7%) | |
| Don't know | 68 (22.6%) | 78 (21.3%) | |
| Know someone in these categories | |||
| Organ recipient | 57 (18.9%) | 75 (20.5%) | 0.63 |
| Registered donor | 176 (58.5%) | 202 (55.2%) | 0.43 |
| Dialysis patient | 56 (18.6%) | 85 (23.2%) | 0.15 |
| On transplant list | 34 (11.3%) | 42 (11.5%) | 1.00 |
| None of the above | 90 (29.9%) | 110 (30.1%) | 1.00 |
| Willingness to donate | |||
| Willing to donate to a family member | 3.97 (3.85–4.09) | 4.15 (4.04–4.26) | 0.03 |
| Willing to donate to a stranger | 3.13 (2.99–3.28) | 3.35 (3.23–3.48) | 0.03 |
| Married participants willingness to donate* | |||
| Willing to donate to a family member | 3.97 (3.78–4.17) | 4.23 (4.09–4.37) | 0.04 |
| Willing to donate to a stranger | 3.20 (2.98–3.42) | 3.45 (3.28–3.63) | 0.08 |
| Non‐married participants willingness to donate † | |||
| Willing to donate to a family member | 3.97 (3.82–4.13) | 4.08 (3.92–4.25) | 0.30 |
| Willing to donate to a stranger | 3.09 (2.91–3.28) | 3.26 (3.08–3.45) | 0.22 |
| Non‐donors: have reasons to not donate | 0.09 | ||
| Yes | 35 (33.0%) | 59 (44.0%) | |
| No | 71 (67.0%) | 75 (56.0%) | |
| Non‐donors: reasons against organ donation | |||
| Personal fears | 51 (48.1%) | 69 (51.5%) | 0.70 |
| Religious beliefs | 20 (18.9%) | 28 (20.9%) | 0.75 |
| Cultural preferences | 10 (9.4%) | 11 (8.2%) | 0.82 |
| Body intact for burial | 22 (20.8%) | 23 (17.2%) | 0.51 |
| Medical mistrust | 39 (36.8%) | 47 (35.1%) | 0.79 |
| Background knowledge | 33 (31.1%) | 45 (33.6%) | 0.78 |
| Not applicable | 12 (11.3%) | 20 (14.9%) | 0.45 |
| Other | 9 (8.5%) | 12 (9.0%) | 1.00 |
| Non‐donors: more information will change willingness to donate | 1.00 | ||
| Yes | 43 (40.6%) | 55 (41.0%) | |
| No | 63 (59.4%) | 79 (59.0%) | |
Married participants willingness to donate: (men: N=110; women: N=175).
Not Married participants willingness to donate: (men: n=191; women: n=191).
Qualitative Survey Results
Donor participants
Among self‐identified donor participants from both sexes, 3 themes emerged to support their registration as organ donors (Table 3). Donors expressed (1) a desire to help others. Donors believed that (2) their personal experience with organ donors and recipients who have been through the process contributed to their decisions. Donors believed that (3) their organs had no use to the donor following death. They felt that organs would go to waste if the participant did not donate them following death.
"It is an easy way for me to help others at literally no cost or inconvenience to myself” (Male Donor)
“I have a friend and a family member that was saved by a donated organ” (Male Donor)
“If I ended up dying, I’d want my organs to go to good use” (Female Donor)
Table 3.
Themes With Exemplar Quotations
| Theme |
Men N=301 (donors: N=195; non‐donors: N=106) |
Women N=366 (donors: N=232; non‐donors: N=134) |
|---|---|---|
| 1a. Donors: willingness to donate | ||
| Desire to help others |
“I have just always thought it was important to help others in need, and if something were to happen to me, I would want someone else to benefit from the use of my organs. It would make me feel like I was truly making a difference by giving someone else the gift of life.” N=135 |
“I want to help people if they can use my organs.” N=181 |
| Personal experience with organ donors/recipients |
“I have close friends who have (1) received organ donations and (2) survived as a result of organ donations.” N=23 |
“My mother needed a donation and the person who donated to her saved her life. We were so grateful and this person was so kind. I decided I want to give back and help someone if I can.” N=44 |
| Believing organs would have no use to the donor once dead |
“I want to be able to give what I don't have a use for anymore.” N=60 |
“I won’t need my organs when I am dead, other people who are still living would put them to good use.” N=75 |
| 1b. Donors: hesitations when registering | ||
| No hesitations |
“I did not have any hesitations becoming an organ donor.” N=162 |
“No hesitations at all. I was happy to sign up to be an organ donor.” N=178 |
| Medical mistrust |
“Yes, I've read that sometimes organs are harvested while you're still alive and that if doctors know you're an organ donor your life might not be top priority.” N=23 |
|
| Organ donation is unsettling |
“The thought of being dissected and harvested for your organs is a little unsettling even if you're already deceased.” N=30 |
|
| 2a. Non‐donors: feelings regarding deceased organ donation | ||
| No desire to donate |
“I don’t intend on becoming a registered deceased organ donor.” N=28 |
“I really do not want to be an organ donor. I know it could save lives. I just don't like the idea of being all cut up.” N=22 |
| Considering donation |
“It is amazing thing after our death our organs will help other people it is very useful and nice thing so I feel happy.” N=35 |
“I think it is one of the most selfless things you can do. if something happened to me I would like to know that my organs could help save someone else.” N=53 |
| Uncertainty about feelings |
“Personally I'm still unsure and quite uncertain about it because I fear that my organs might go to someone that is undeserving or I fear mishandling of my organs by people.” N=36 |
“I feel unsure about it.” N=61 |
| 2b. Non‐donors: reasons against deceased organ donation (Why?) | ||
| No reason (don’t want to donate) |
“I don't even like to think about it; I want to help, but I could never get up the courage to volunteer for organ donation.” N=49 |
“I just don't want to be an organ donor.” N=54 |
| Medical mistrust |
“Sometimes people are not "dead" yet. I've read articles and heard stories about this. It scares me, as I used to be a donor.” N=20 |
|
| 2c. Non‐donors: methods to change decision about donation | ||
| More information |
“Just more information so [that] I can give fully informed consent or denial.” N=43 |
“Learning more about donations and what it all means and how it all works.” N=63 |
| More trust in medical system |
“Concrete absolute proof that the person is totally dead before being cut on. Also, the doctors should not be able to coerce a family member into donating before it's known if the person even has a 1% chance of recovery.” N=19 |
|
| 3. Feelings regarding donation of family member’s organs | ||
| My decision depends on my family member's wishes |
“It depends on their wishes. I would take that into consideration first. If I didn't know how they felt, I might be inclined to donate their organs.” N=134 |
“I do not know. I would only donate their organs if they had already given me permission to do so.” N=146 |
| My family member will not need their organs after death and should be used to help others |
“Absolutely, I would. If my family member wasn't going to recover and had no use for their organs, someone else should be able to live and carry out a normal life; my family member's organ/s would be a life‐giving gift.” N=80 |
“Yes, I would donate their organs. The family member’s organs aren’t going to benefit them after death, but it might greatly benefit someone else.” N=149 |
| 4. Feelings regarding donation of spouse’s organs | ||
| My decision depends on my spouse's wishes regarding donation |
“I would if she was willing to. I wouldn't want to go against their wishes.” N=74 |
“I would accept. I think he trusts me to make that decision for him and that I would do as he wished.” N=87 |
| My spouse will not need their organs after death |
“Yes. I would not keep her alive per our agreement. The organs will be more useful to someone that needs them.” N=44 |
“Yes, I'd donate his organs because he doesn't need them and he wouldn't want to live as a brain dead vegetable.” N=76 |
The number of participants describing the themes may be higher than the total participants since a single participant may express more than one theme. Themes were maintained after unmasking participant sex if the theme was repeated among at least 10% of the population of donor men or women, or non‐donor men or women, or of all‐comer men or women.
Self‐identified donor participants were prompted to focus on hesitations upon deciding to register for organ donation. Among female donor participants, the following themes emerged: (1) no issues or hesitations with organ donation; (2) organ donation is unsettling, believing that the organ donation process was uncomfortable to process; and (3) medical mistrust, believing that the medical system and healthcare personnel do not act ethically when treating potential donors. Male participants only expressed the first theme of no hesitation.
“No, it was very clear what I should do” (Female Donor)
“Yes because I thought the idea of being cut open and having different organs being in different people was weird and creepy to say the least” (Female Donor)
“I was hesitant that I would be declared dead and not resuscitated if I was to be an organ donor” (Female Donor)
Non‐donor participants
Self‐identified non‐donor participants from both sexes expressed opinions regarding deceased organ donation (Table 3). Themes included: (1) no desire to donate organs; (2) considering donating organs; and (3) uncertainty about donating organs.
“I do not want to be an organ donor” (Female Non‐Donor)
“I think it’s a noble thing to do. It’s something I (would) consider doing. It’s a little bit anxiety provoking, but I think it is worthwhile as one can potentially save people’s lives by signing up” (Female Non‐Donor)
“I’m not sure; I haven’t given it much thought” (Male Non‐Donor)
Self‐identified non‐donor participants’ reasons against deceased organ donation included the following themes among women: (1) no clear reason; and (2) medical mistrust. Men only shared the first theme of no clear reason.
“I don’t feel comfortable with it for some reason, but I don’t really know why.” (Female Non‐Donor).
“I think, and have read, that sometimes doctors will decide to pull the plug just to be able to harvest the organs. I have also read that organs have to be removed while the person is still alive but brain dead. Not sure if that’s true though.” (Female Non‐Donor)
Non‐donor participants were asked to provide methods that could change their mind about their donor status. Women participants’ answers reflected two themes: (1) more information, believing that additional information about organ donation could influence the participant’s decision; and (2) more trust in the medical system, believing that being informed about the medical personnel and learning about the protocols in place to care for patients who are donors will not differ from non‐donors. Men shared the first theme of requesting more information.
“Speaking to recipients of organ donors or talking to doctors more about the process/whether or not there are any risks” (Female Non‐Donor)
“I would have to have more trust with the medical doctors and lessen my own personal fears” (Female Non‐Donor)
All participants
All participants were asked to express how they felt about donating a family member’s organs in the case of brain death (Table 3). Themes were similar across sexes, but importance of themes varied by sex. Men found the following theme more important than women: (1) my decision depends on my family member’s wishes, believing that communicating with family members prior to death about their wishes regarding deceased organ donation would impact the participant’s decision to donate the family member’s organs. Women found the first and second theme equally important: (2) my family member will not need their organs after death and thus should be used to help others.
“I would only donate the organs of a family member if that was their wish and I would not want to make a decision in which they did not approve prior to such a tragedy.” (Male Non‐Donor)
“Yes, I would donate their organs. The family member’s organs aren’t going to benefit them after death, but it might greatly benefit someone else” (Female Donor)
Secondary Analyses: Marital Differences by Sex
Quantitative Survey Results
In secondary analysis, married women were more willing than married men to donate organs to a family member (women: 4.23 [95% CI: 4.09–4.37]; men: 3.97 [95% CI: 3.78–4.17]; P=0.04) (Table 2). No significant differences were observed by sex among non‐married participants’ willingness to donate to a family member (women: 4.08 [95% CI: 3.92–4.25]; men: 3.97 [95% CI: 3.82–4.13]; P=0.34). There were no significant sex differences in willingness to donate to strangers when stratified by marriage (P=0.08 married; P=0.22 non‐married).
Qualitative Survey Results
Among married participants, no sex differences were observed regarding views about donation of a spouse’s organs in the case of brain death (Table 3). Non‐married participants responded “not applicable” to this question. Themes among married participants included: (1) my decision depends on my spouse’s wishes; and (2) my spouse will not need their organs after death.
“I would if she was willing to. I wouldn’t want to go against their wishes.” (Male Donor)
“I would accept. It would be important to my husband to have a part of him live on, and to help others if he could no longer use his organs” (Female Donor)
Discussion
In a crowdsourcing MTurk study of US adults, the majority of male and female participants self‐identified as registered organ donors. Categorical selections revealed that women were more willing to donate their own organs to family members and strangers than men with the former also being true among married women. Among non‐donors, there were no significant sex differences in reasons to donate nor in likelihood of changing mind.
Qualitative analyses revealed similarities by sex in reasons for donating among donors and general feelings about donation among non‐donors. Sex differences were present on remaining questions. Among donors, both sexes had no major hesitations to registering, but women also endorsed concerns of medical mistrust and discomfort with donating. Among non‐donors, both sexes believed that more information might change their mind, and women also thought that a more trustworthy medical system would help. Among all participants, men were most influenced by their family member’s wishes to donate in the setting of a family member’s brain death. Women were equally influenced by family member’s wishes and belief that their family member no longer needed their organs. Overall, this study suggests that deceased organ donation of women may be increased by encouraging women to share their plans and beliefs with family members, particularly to any men in their families, by improving public education of the transplant process, and by developing a more trustworthy medical system.
Reasons why individuals become organ donors are well studied; however, reasons for low deceased organ donation in women are not known. 25 Low donor rates of various populations have been attributed to levels of education, socioeconomic factors, and religious beliefs. 26 Studies have also shown that differences in donation between sexes could be attributed to the majority of deceased organ donor deaths due to the increase in drug overdose related deaths and blunt trauma. 1 , 5 Our study is unique due to detailed investigation of specific reasons for deceased organ donation among men and women, and important since low proportion of deceased organ donors that are women can reduce the survival of those who receive sex mismatched organs. 27 The large number of participants sharing their views on this issue is a major strength to our study and adds weight to the depth of the discussion.
Upholding a family member’s wishes has been identified as a major reason for organ donation in other studies. 28 , 29 In one US study of deceased organ donors’ next of kin, the family member’s wishes was one of the most important factors contributing to their decision to donate their family member’s organs. 30 Another US study from 2012 demonstrates that women (45.5%) and men (39.7%) are very willing to discuss their wishes regarding organ donation with their families. The majority of women in that study knew about the family member’s wishes for organ donation, and a minority of men knew about their family member’s wishes to donate. 31 A study conducted in Europe had similar findings, where the next of kin wanted to follow the wishes of their family member and struggled making decisions when they did not know their family member’s wishes. 32 Our study suggests that this is the most important value for men when deciding about whether or not to donate the organs of their family members. Thus, indecision about knowing a family member’s wishes may contribute to the sex disparity in organ donation when the family member is a woman. Since women generally supported organ donation for themselves and their family members, sharing their wishes early in life among next of kin could attenuate the sex disparity among deceased organ donors.
Concerns about whether or not a healthcare system is trustworthy enough to make ethical decisions in the setting of pre‐death registration for organ donation has been another ongoing issue observed in multiple studies. In another European study, they estimated that 10% of residents would likely opt out of organ donation due to concern of unethical treatment during clinical care that would promote organ donation rather than life preservation. 33 These notions are not unfounded. Unethical organ procurement has been documented in African American patients in the US in the 1960s and among prisoners in other countries. 34 , 35
Our study suggested that women would be more open to donating if the medical system was more trustworthy, and both sexes would be amenable to donating if more information was provided. In alignment with the Belmont Report, multiple ethical policies are in place to prevent unethical organ procurement. In the US, transplant centers must adhere to policies of the Organ Procurement and Transplantation Network (OPTN) in order to maintain accreditation. Ethical Principles in the Allocation of Human Organs from the OPTN include “respect for persons,” where programs must respect the decisions of potential donors and those that do not consent to donate, and transparency must be maintained throughout the process. 36 In addition, international consensus was convened under the World Health Organization, which details “Guiding Principles on Human Organ Transplantation” that also share the necessity of consent to proceed with organ procurement. 37 Improved public dissemination of these ethical policies may restore trust in the medical system. Implementation studies led by patient stakeholders may be an appropriate next step toward achieving equity in donor registration by sex.
Limitations
This study was subject to several limitations. First, more women than men participated in this survey study, and the majority identified their ethnicity as non‐Hispanic White and had some form of a college education. A greater proportion of the excluded participants were of Hispanic ethnicity and married than those in the included cohort (Table S1). Systemic racism and bias are known issues affecting patients of color, 38 and socioeconomic status also impacts likelihood of donation. 39 This study lacks the viewpoint of these important intersectional groups. However, since fewer women become deceased organ donors, having more women than men participate is a strength of this study. Second, prevention of repeat participation cannot be guaranteed, but this was avoided using Qualtrics XM prevent ballot box stuffing selection, which uses cookies to identify repeat participants. The survey link was selected as unavailable for indexing on search engines using Qualtrics XM. Only unique MTurk participants meeting study inclusion criteria were able to access the Qualtrics XM survey link. Third, differences between adult age groups was not addressed in this study. The survey population was mostly comprised of adults between the ages of 18 and 40, and thus there was not enough power to investigate the difference between those of younger and older ages. Last, as a convenience survey, which inherently lacks randomized sampling and a denominator, results are not representative of the entire US population; however, participants are well represented throughout all four regions of the US.
Conclusions
In a US MTurk study, women were more willing than men to donate organs to a family member and to a stranger. Compared with married men, married women were more willing to donate organs to a family member. Both male and female donors revealed similar themes for becoming donors. When making decisions about donating organs of deceased family members, men valued family member’s wishes as the most important theme guiding their decision. Women placed equal value on the family member’s wishes and the desire to help others. Eliminating sex inequity in deceased organ donation will likely require more public education and communication of post‐humous wishes regarding deceased organ donation. Systematic changes and strategies to build trust in the medical system were also identified as means to change the stance of non‐donors from both sexes.
Sources of Funding
Dr Breathett received support from National Heart, Lung, and Blood Institute K01HL142848, R25HL126146 subaward 11692sc, and L30HL148881; University of Arizona Health Sciences, Strategic Priorities Faculty Initiative Grant; University of Arizona, Sarver Heart Center, Novel Research Project Award in the Area of Cardiovascular Disease and Medicine, Anthony and Mary Zoia Research Award; and Women As One. Ms Duarte received support from University of Arizona, Focusing Research on the Border Area (FRONTERA) Program. Dr Carnes’s research on scientific workforce diversity is funded by National Institute of General Medical Sciences (NIGMS) R35GM122557.
Disclosures
None.
Supporting information
Data S1
Table S1
For Sources of Funding and Disclosures, see page 11.
References
- 1. National data—OPTN [Internet]. Available at: https://optn.transplant.hrsa.gov/data/view‐data‐reports/national‐data/#. Accessed February 6, 2020.
- 2. Traino HM, Siminoff LA. Attitudes and acceptance of First Person Authorization: a national comparison of donor and nondonor families. J Trauma Acute Care Surg. 2013;74:294–300. doi: 10.1097/TA.0b013e318270dafc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Saidi RF, Hejazii Kenari SK. Challenges of organ shortage for transplantation: solutions and opportunities. Int J Organ Transplant Med. 2014;5:87–96. [PMC free article] [PubMed] [Google Scholar]
- 4. Khush KK, Kubo JT, Desai M. Influence of donor and recipient sex mismatch on heart transplant outcomes: analysis of the International Society for Heart and Lung Transplantation Registry. J Heart Lung Transplant. 2012;31:459–466. doi: 10.1016/j.healun.2012.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hickman L, Killian JT, Windham ST. Despite the growing impact of the american opioid epidemic on organ donation, a small percentage of drug intoxication deaths result in organ donation. Transplantation. 2018;102:S334. doi: 10.1097/01.tp.0000543066.99410.c0 [DOI] [Google Scholar]
- 6. Increases in Drug and opioid overdose deaths—United States, 2000–2014 [Internet]. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm#tab. Accessed December 10, 2020.
- 7. Irving MJ, Jan S, Tong A, Wong G, Craig JC, Chadban S, Rose J, Cass A, Allen RD, Howard K. What factors influence people’s decisions to register for organ donation? The results of a nominal group study. Transpl Int. 2014;27:617–624. doi: 10.1111/tri.12307 [DOI] [PubMed] [Google Scholar]
- 8. Feeley TH, Reynolds‐Tylus T, Anker AE, Evans M. Reasons for (not) signing the state registry: surveying Department of Motor Vehicles customers in New York state. Prog Transplant. 2014;24:97–105. doi: 10.7182/pit2014390 [DOI] [PubMed] [Google Scholar]
- 9. Boulware EL, Ratner LE, Cooper LA, Sosa JA, Laveist TA, Powe NR. Race and gender differences in willingness to donate blood and cadaveric organs: understanding disparities in donor behavior. Med Care. 2002;40:85–95. doi: 10.1097/00005650-200202000-00003 [DOI] [PubMed] [Google Scholar]
- 10. Mocan N, Tekin E. The determinants of the willingness to donate an organ among young adults: evidence from the United States and the European Union. Soc Sci Med. 2007;65:2527–2538. doi: 10.1016/j.socscimed.2007.07.004 [DOI] [PubMed] [Google Scholar]
- 11. Sehgal NKR, Scallan C, Sullivan C, Cedeño M, Pencak J, Kirkland J, Scott K, Thornton JD. The relationship between verified organ donor designation and patient demographic and medical characteristics. Am J Transplant. 2016;16:1294–1297. doi: 10.1111/ajt.13608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rodrigue JR, Cornell DL, Jackson SI, Kanasky W, Marhefka S, Reed AI. Are organ donation attitudes and beliefs, empathy, and life orientation related to donor registration status? Prog Transplant. 2004;14:56–60. doi: 10.1177/152692480401400109 [DOI] [PubMed] [Google Scholar]
- 13. DuBois JM, Anderson EE. Attitudes toward death criteria and organ donation among healthcare personnel and the general public. Prog Transplant. 2006;16:65–73. doi: 10.1177/152692480601600113 [DOI] [PubMed] [Google Scholar]
- 14. Reynolds‐Tylus T, Quick BL, King AJ, Moore M. Illinois Department of Motor Vehicle customers’ reasons for (not) registering as an organ donor. Prog Transplant. 2019;29:157–163. doi: 10.1177/1526924819835838 [DOI] [PubMed] [Google Scholar]
- 15. Morgan SE, Harrison TR, Afifi WA, Long SD, Stephenson MT. In their own words: the reasons why people will (not) sign an organ donor card. Health Commun. 2008;23:23–33. doi: 10.1080/10410230701805158 [DOI] [PubMed] [Google Scholar]
- 16. Sanfey H. Chapter 55—gender‐specific issues in organ transplantation [Internet]. In: Legato MJ, ed. Principles of Gender‐Specific Medicine. 2nd ed. Academic Press; 2010:657–675. Available at: https://www.sciencedirect.com/science/article/pii/B9780123742711000551. Accessed April 11, 2021. [Google Scholar]
- 17. Gyllström Krekula L, Forinder U, Tibell A. What do people agree to when stating willingness to donate? On the medical interventions enabling organ donation after death. PLoS One. 2018;13:e0202544. doi: 10.1371/journal.pone.0202544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk: a new source of inexpensive, yet high‐quality, data? 2011. [Internet]. Available at: https://journals.sagepub.com/doi/abs/ 10.1177/1745691610393980. Accessed April 9, 2021. [DOI] [PubMed]
- 19. Goodman JK, Cryder CE, Cheema A. Data collection in a flat world: the strengths and weaknesses of Mechanical Turk samples. J Behav Decis Mak. 2013;26:213–224. doi: 10.1002/bdm.1753 [DOI] [Google Scholar]
- 20. Difallah D, Filatova E & Ipeirotis P Demographics and dynamics of Mechanical Turk workers [Internet]. In: Proceedings of the Eleventh ACM International Conference on Web Search and Data Mining—WSDM ’18. Marina Del Rey, CA, USA: ACM Press; 2018:135–143. Available at: http://dl.acm.org/citation.cfm?doid=3159652.3159661. Accessed March 18, 2020.
- 21. Walters K, Christakis DA, Wright DR. Are Mechanical Turk worker samples representative of health status and health behaviors in the U.S.? PLoS One. 2018;13:e0198835. doi: 10.1371/journal.pone.0198835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. R. Core Team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2020. Available at: https://www.R‐project.org. Accessed December 2, 2020.
- 23. Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Approaches. SAGE Publications, Inc; 2013. [Google Scholar]
- 24.RWJF—Qualitative Research Guidelines Project | Lincoln & Guba | Lincoln and Guba’s Evaluative Criteria [Internet]. Available at: http://www.qualres.org/HomeLinc‐3684.html. Accessed April 9, 2021.
- 25. Reibel M, Olmo C, Andrada S, Koertzen J. Deep demographics: understanding local variation in donor registration. Prog Transplant. 2016;26:191–198. doi: 10.1177/1526924816640670 [DOI] [PubMed] [Google Scholar]
- 26. Shacham E, Loux T, Barnidge EK, Lew D, Pappaterra L. Determinants of organ donation registration. Am J Transplant. 2018;18:2798–2803. doi: 10.1111/ajt.15025 [DOI] [PubMed] [Google Scholar]
- 27. Kittleson MM, Shemin R, Patel JK, Ardehali A, Kawano M, Davis S, Moriguchi JD, Kobashigawa JA. Donor‐recipient sex mismatch portends poor 10‐year outcomes in a single‐center experience. J Heart Lung Transplant. 2011;30:1018–1022. doi: 10.1016/j.healun.2011.03.018 [DOI] [PubMed] [Google Scholar]
- 28. Siminoff LA, Gordon N, Hewlett J, Arnold RM. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA. 2001;286:71–77. doi: 10.1001/jama.286.1.71 [DOI] [PubMed] [Google Scholar]
- 29. Siminoff LA, Traino HM, Gordon N. Determinants of family consent to tissue donation. J Trauma. 2010;69:956–963. doi: 10.1097/TA.0b013e3181d8924b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transplant. 2006;6:190–198. doi: 10.1111/j.1600-6143.2005.01130.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. 2012 national survey of organ donation attitudes and behaviors. 124. 2013 U.S. Department of Health and Human Services. Available at: https://www.organdonor.gov/sites/default/files/organ‐donor/professional/grants‐research/national‐survey‐organ‐donation‐2012.pdf. Accessed December 4, 2020.
- 32. de Groot J, van Hoek M, Hoedemaekers C, Hoitsma A, Smeets W, Vernooij‐Dassen M, van Leeuwen E. Decision making on organ donation: the dilemmas of relatives of potential brain dead donors. BMC Med Ethics. 2015;16:64. doi: 10.1186/s12910-015-0057-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Miller J, Currie S, O’Carroll RE. ‘What if I’m not dead?’—Myth‐busting and organ donation. Br J Health Psychol. 2019;24:141–158. doi: 10.1111/bjhp.12344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Iacobucci G. Chinese doctors admitted in undercover calls that harvested organs were available, informal tribunal finds. BMJ. 2020;368:m859. doi: 10.1136/bmj.m859 [DOI] [PubMed] [Google Scholar]
- 35. Jones S. The Organ Thieves: The Shocking Story of the First Heart Transplant in the Segregated South. Illustrated ed. Gallery/Jeter Publishing; 2020. [Google Scholar]
- 36. Ethics—ethical principles in the allocation of human organs—OPTN [Internet]. Available at: https://optn.transplant.hrsa.gov/resources/ethics/ethical‐principles‐in‐the‐allocation‐of‐human‐organs/. Accessed December 4, 2020.
- 37. WHO | International perspectives on the ethics and regulation of human cell and tissue transplantation [Internet]. WHO. Available at: https://www.who.int/bulletin/volumes/85/12/06‐038703/en/. Accessed December 4, 2020. [Google Scholar]
- 38. Breathett K, Jones J, Lum HD, Koonkongsatian D, Jones CD, Sanghvi U, Hoffecker L, McEwen M, Daugherty SL, Blair IV, et al. Factors related to physician clinical decision‐making for African‐American and Hispanic patients: a qualitative meta‐synthesis. J Racial Ethn Health Disparities. 2018;5:1215–1229. doi: 10.1007/s40615-018-0468-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shah MB, Vilchez V, Goble A, Daily MF, Berger JC, Gedaly R, DuBay DA. Socioeconomic factors as predictors of organ donation. J Surg Res. 2018;221:88–94. doi: 10.1016/j.jss.2017.08.020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Table S1


