Abstract
As the lifespan increases, special attention has been given to the supportive care needs of the elderly. Frailty is an important issue in third age, since it is related to poor quality of life and mortality. The prevalence of pathological conditions related to sodium levels, specifically hyponatremia, is also present in the elderly. Yet, it is unclear, if hyponatremia and frailty are related to each other. This review summarizes the current state of knowledge regarding hyponatremia and frailty and analyzes five independent studies which searched for an association between those two parameters. As indicated by this study results, hyponatremia consists a risk factor for frailty. This could be explained by an effect of hyponatremia on sarcopenia and on cognitive function, which consist components of frailty. Thus, it is essential to monitor sodium levels in the elderly and to develop related interventions (e.g. using arginine vasopressin antagonists) in order to prevent frailty.
Keywords: Cognitive function, Frailty, Hyponatremia, Sarcopenia, Sodium
Introduction
Until the middle of the 19th century, people were divided into two age groups: childhood and adulthood. However, it was not recognized that people who differed in age have divergent needs[1]. Aging has been studied in modern times not only in terms of the life expectancy of elderly people, but also in terms of how they age[2]. It is claimed that although life expectancy is increasing, disability-free years are also decreasing due to the increase in the incidence of chronic diseases. Therefore, modern people live longer, but are affected by several chronic diseases. For this reason, the study of aging is of increased interest[2].
Normal aging is characterized by the process during which the functionality of the individual is progressively reduced. The effects of old age become apparent after some time during the life of the individual. Thus, the person’s abilities decrease at all levels[3,4].
In that context, the aim of the present study was to investigate frailty and hyponatremia and to search for an association between those two parameters, as well as for related explanations. This study is a non-systematic literature review, carried out in Scopus and Pubmed, using related search terms.
Hyponatremia explained
Water is of most importance for human health. The total amount of water in the body differs between men and women, and decreases with age. It accounts for 50% of body weight (BW) in women and 60% of BW in men, aged 18-40 years. 2/3 (40% of BW) is intracellular, while 1/3 (20% of BW) is extracellular. 1/4 of extracellular water (5% of BW) is in the intravascular space[5,6]. Fluid loss can occur from both the intercellular and extracellular space. The finding of changes in the total amount of water in the body is done, more reliably, by measuring BW. In order to clinically establish an increase in extracellular space (swelling), at least 4-5 L of fluid should be retained. Assessment of active circulating blood volume can be done by physical examination and measurement of static (blood pressure, heart rate) and dynamic (pulse pressure, pulse volume variability) indicators, using invasive (right cardiac catheterization with Swan-Ganz catheter) or non-invasive (echocardiography) methods[5,6].
To clarify the cause of electrolyte disorders, knowledge of the history, underlying diseases and medication taken by the patient is needed. The concentration of electrolytes in the urine indicates whether the kidney responds prematurely by retaining or excreting this electrolyte. In addition to measuring its concentration and total amount in urine, which is considered the “Golden Rule”, a more convenient method for investigating the management of an electrolyte by the kidney is fractional excretion of the electrolyte (FE), calculated as follows:
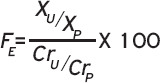
Where U and P concentrations in urine and plasma, electrolyte (X) and creatinine (Cr). Reduced fractional excretion means renal resorption, while high fractional excretion means renal loss. In oliguria specific, fractional excretion Na+ >2% indicates renal impairment, while <1% indicates prorenal oliguria[5,6].
The osmolality of a solution (for example plasma) is expressed by the total concentration of dissolved substances in mmol per L of solution or per kg of water, calculated in milliosmoles (mOsm)/L or mOsm/kg. When the plasma concentrations of dissolved substances are normal, the osmolarity of the plasma is 285-295 mOsm/L. Liquids with an osmolarity greater than the normal plasma are called hypertonic, while when the osmolality is less than normal they are called hypotonic. Tonality refers to active osmolarity and is created by dissolved substances that do not pass freely through the cell membranes and, as a result, lead to difference (inclination) of concentration and movement of fluids between the two sides of the membrane (osmosis phenomenon)[5,6]. Increasing tonicity stimulates the feeling of thirst and the secretion of antidiuretic hormone (anti-Diuretic Hormone, ADH). Substances that freely pass through cell membranes (urea, ethanol) increase the osmolarity, but not the tonicity of the plasma and do not cause fluid movement (non-active osmols). Plasma osmolality (Omega) can be calculated from the concentrations of the main dissolved substances in the plasma, i.e. Na+, glucose and urea, as follows[5,6]:
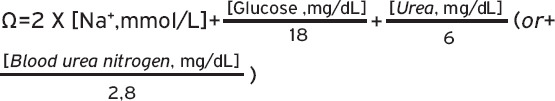
The concentration of Na+ is the same whether measured in mmol/L or mEq/L, because it is a monovalent ion. The doubling of the concentration of Na+ is done because Na+ is a strong electrolyte, fully dissociated in plasma conditions by the co-existing anions (mainly chlorine, Cl-)[5,6]. Physiologically, the measured osmolality (the measurement is made by estimating the descent of the freezing point) is higher than the calculated, because there are other dissolved substances in the plasma besides Na+, glucose and urea. This difference is called osmotic plasma gap and is normally 10 mOsm/L. Difference greater than 10 mOsm/L is an index of existence and other, uncalculated, dissolved substances, such as mannitol and ethanol[5,6].
Because the differences in osmolarity between intracellular and extracellular space are quickly balanced by the movement of water from the plasma membrane passages (aquaporins), the concentration of dissolved substances as a whole must be the same inside and outside the cells.
Hyponatremia is defined as a decrease in serum Na+ concentration to <135 mEq/L. In hyponatremia, plasma osmolarity may be low (hypotonic hyponatremia), normal (isotonic hyponatremia) or elevated (hypertonic hyponatremia)[5,6].
Isotonic hyponatremia is observed in cases of severe hyperlipidemia and hyperproteinemia. Na+, as an electrolyte, is distributed in the aqueous phase of the plasma. Usually, in the laboratory the measurement of its concentration is calculated in the total volume of plasma[5,6]. Since the non-aqueous phase is only a small part of the total volume of plasma, the difference from its actual concentration in the aqueous phase, where it is normally distributed, is small. However, at high concentrations of lipids (chylomicrons, triglycerides and cholesterol) and proteins, the measurement of Na+ concentration is affected, resulting in incorrect low values (pseudohyponatremia), while osmolarity is not affected. Newer measurement methods, using special electrodes for ions, measure Na+ in the aqueous phase of the plasma, and this laboratory error is not observed[5,6].
Hypertonic hyponatremia is observed in hyperglycemia and mannitol administration. Significantly increased glucose (or mannitol) concentration causes osmotic movement of water from intracellular to extracellular space. Moving water reduces the concentration of Na+ in plasma (this is not pseudohyponatremia). Na+ concentration is reduced by 1,7 mEq/L for every 100 mg/dL increase in glucose concentration[5,6].
Most cases of hyponatremia are hypotonic. Most liquids are hypotonic relative to plasma (have a lower concentration of Na+). With furosemide administration, the concentration of Na+ in excreted urine is increased up to 75 mEq/L[5,6]. Apart from this case, further other sub-categories such as euvolemic, hypovolemic and hypervolemic are also observed, referring to decrease in total body water with greater decrease in total body sodium, normal body sodium with increase in total body water and increase in total body sodium with greater increase in total body water respectively. Yet, these cases are less frequent compared to hypotonic hyponatremia[5]. In addition, hyponatremia might be related to SIADH, which is characterized by excessive unsuppressible release of antidiuretic hormone, and might be caused by various chronic diseases, such as cancer, and related treatments[7].
The concept of frailty
The definition of frailty is variably defined, but Fried et al proposed a definition according to which, frailty is a clinical syndrome consisting in the coexistence of at least three of the following five criteria: weight loss, exhaustion, vulnerability, slow walking speed and low physical activity[8-11]. Fried et al, as well as other studies related to frailty, have investigated whether it could validly contribute to the prognosis of mortality from a multitude of chronic diseases[11-14]. In general, frailty is an age-related medical syndrome, and leads to greater risk of adverse health effects, including disability, hospitalization, post-operative complications and even death[10-15]. Many chronic diseases have been studied in relation to frailty. Remarkably, frailty and disability are often correlated[16] and frailty can be regarded as pre-disability[17]. Indeed, it has been suggested that these two conditions share common pathogenic mechanisms and that certain ways of treatment, such as physical exercise, benefit both[18-20].
Frailty was determined according to the criteria proposed by Fried et al as follows: (1) Looseness: determined by the time used to pass a 4-meter gait test. The cut-off point was adjusted for gender and height, and those in the lower quintet were identified as having slow gait speed[11]. (2) Grip strength: measured using a hand dynamometer. Three measurements were made on both hands, and the highest was retained. The cutoff point was adjusted for body mass index and gender, and those in the lowest quintet were determined to have the poorest grip strength[11]. (3) Physical activity: defined using the physical activity scale for the elderly, which is an instrument that measures the level of physical activity for older adults[11]. (4) Exhaustion: elderly with a negative answer to the following 2 questions are exhausted: “Do you feel full of energy?” and “do you have enough energy for your daily life?”[11]. (5) Weight Loss: determined using the self-reporting of weight loss (5 kg) during the last 6 months[11]. Those who meet 3 or more of the criteria were considered frail, while those who meet 1 or 2 criteria are considered pre-vulnerable[11].
Studies associating hyponatremia with frailty
Few studies have investigated the association between hyponatremia and frailty. In a relevant study in France, 696 patients were assessed as for their frailty and hyponatremia (mean age 86.1 years old). As indicated by the analysis, the prevalence of falls was 27.9% and the prevalence of mild hyponatremia 15.9%[21]. The prevalence of mild hyponatremia was 13.2% in patients without falls and 26.1% in patients with falls. The association between mild hyponatremia and falls was statistically significant (Odds Ratio 3.02, p<0.001). Thus, this study indicates a strong association between hyponatremia and falls[21].
In another study in the United States, 608 community elderly (mean age 84.3) were followed for 41.5 months and assessed for their frailty and hyponatremia. During the follow-up, frailty was observed in 44.4% of the participants. It was also found that hyponatremia is a significant independent predictor of frailty levels[22].
In another study in the United States, a cohort of 1.062.467 individuals aged ≥55 years were assessed as for their serum sodium levels and as for their hyponatremia, defined as sodium <135 mEq/L with sub-acute (<30 days) and chronic (≥30 days)[23]. The aim of the study was to investigate the association between frailty and those two types of hyponatremia. As found by the statistical analysis, any hyponatremia duration compared to normonatremia had a serious falls/hip fractures HR (95%CI) of 1.18 (1.15, 1.22), with sub-acute and chronic hyponatremia having HR of 1.38 (1.33, 1.42) and 0.91 (0.87, 0.95), respectively[22]. Examined separately, the serious falls HR was 1.37 (1.32, 1.42) and 0.92 (0.88, 0.96) in sub-acute and chronic hyponatremia, respectively. Hip fracture HR were 1.52 (1.42, 1.62) and 1.00 (0.92, 1.08) for sub-acute and chronic hyponatremia, respectively, compared to normonatremia. In overall, early/sub-acute hyponatremia is more strongly associated with falls and hip fractures[23].
In an additional study in Canada, 8.911 responders were assessed as for their frailty and dysnatremia levels, as part of the National Health and Nutrition Examination Survey[24]. Frailty Index was calculated from each respondent and associated with dysnatremia. Dysnatremia was significantly associated with frailty[24]. In addition, the higher the degree of frailty, the higher the proportion of dysnatremia. In addition, when adjusted for frailty the association between age and dysnatremia was insignificant, indicating that the effect of age is attributed to frailty, not in age itself[24].
In another study in Japan, 3.555 hospitalized patients with heart failure was prospectively assessed between October 2014 and March 2016 as for frailty and hyponatremia[25]. Additional risk factors for frailty were also assessed. In this study, it was found that patients with hyponatremia had 1.49 higher odds for frailty compared to those without hyponatremia[25].
The interplay mechanism between hyponatremia and frailty
Of note, the mechanism leading from hyponatremia to frailty is quite unclear. As noted by Bhandari et al who carried out the largest study in hyponatremia patients (N=1.062.647 individuals followed for 18 years), it is yet unclear if hyponatremia is a marker of frailty or is a causative factor of frailty. Yet, a few explanations for this association are possible[23].
Pathophysiologically, hyponatremia can be caused by a decrease in the body content of sodium or potassium and/or an increase in the body content of water. Sarcopenia is an ageing-related progressive and general loss of musculoskeletal mass and strength that leads, particularly in the vulnerable and frail elderly, to low physical ability[26]. Since muscle mass is the main body store of potassium, this disorder which is associated closely with frailty syndrome, normally reflects a decreased potassium content in the body. On the other hand, hyponatremia, on its own, can induce sarcopenia and enhance frailty, as a result of gait instability and further muscle inactivity. So, it seems these two conditions can give feedback to each other and subserve frailty[26].
Another related mechanism has to do with cognitive decline which is present among the frail. Low levels of sodium are associated with cognitive deficits. Thus, it could be possible that the effect of hyponatremia on frailty is also explained by the negative effects of low sodium levels on cognitive function[27].
Another attribution has to do with the effect of diuretics[28,29]. Indeed, the elderly frequently use diuretics, which could therefore lead to hyponatremia. Since higher medication used is also associated with frailty, it could be possible that frailty and hyponatremia are not causatively associated, but that they are both a result of high diuretic use[28,29]. Several other drugs, frequently used by the elderly, also lead to hyponatremia. For example, psychotropic medication can also be associated with hyponatremia[29,30].
Clinical applications
As indicated by the results of the studies included in this review, hyponatremia seems to be a causative factor of frailty. It is therefore essential to improve sodium levels in order to prevent frailty in the elderly. The therapeutic armamentarium available to physicians has been increased by the arginine vasopressin antagonists, vaptans, which can lead to improvement of sodium levels and have a positive impact on frailty levels[31]. Thus, it is essential to routinely monitor the sodium levels of the elderly and to find those who experience low sodium level and to apply related interventions[32].
Conclusion
Frailty is a significant issue in elderly, which deserves increasing attention due to population aging. This study investigated frailty and hyponatremia, which also occurs in third age, and examined studies associating these parameters. As indicated by the study results, all the relevant studies demonstrated that hyponatremia has a causative effect on frailty. Nevertheless, it is yet unclear how this effect could be explained. It is possible that this is attributed to the induction of further hyponatremia in elderly due to sarcopenia, which leads to functional decline and frailty. In addition, it could be argued that hyponatremia also leads to cognitive impairment for the elderly. As hyponatremia therefore affects the development of sarcopenia and cognitive problems, it is highly likely that these two mechanisms explain the development of hyponatremia in the elderly. However, it should be noted that the effect of hyponatremia on frailty could be not only a causative factor, but also a prognostic factor, meaning it could reflect an overall functional decline. Future studies are warranted to further understand this mechanism. Finally, it is necessary to develop interventions for the treatment of hyponatremia, in order to protect the elderly against the development of frailty.
Footnotes
Edited by: Yannis Dionyssiotis
References
- 1.Wold GH. Basic Geriatric Nursing. Athens: Parisianou Publications; 2017. [Google Scholar]
- 2.Ryff CD, Singer B. Bengston V. L, Gans D, Pulney N. M, Silverstein M. Handbook of theories of aging. Springer Publishing Company; 2019. Understanding healthy aging: Key components and their integration; pp. 117–144. [Google Scholar]
- 3.Harman D. Aging: overview. Annals of the New York Academy of Sciences. 2001;928(1):1–21. doi: 10.1111/j.1749-6632.2001.tb05631.x. [DOI] [PubMed] [Google Scholar]
- 4.Harman D. The aging process. Proceedings of the National Academy of Sciences. 1981;78(11):7124–7128. doi: 10.1073/pnas.78.11.7124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chawla R, Todi S, Agarwal DK. Singapore: Springer; 2020. Hyponatremia. In ICU Protocols; pp. 3–15. [Google Scholar]
- 6.Peri A, Thompson CJ, Verbalis JG. Disorders of Fluid and Electrolyte Metabolism: Focus on Hyponatremia. Karger Medical and Scientific Publishers. 2019 [Google Scholar]
- 7.Castillo JJ, Vincent M, Justice E. Diagnosis and management of hyponatremia in cancer patients. The oncologist. 2012;17(6):756. doi: 10.1634/theoncologist.2011-0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthanet S, et al. Frailty:an emerging research and clinical paradigm - issues and controversies. The Journals of Gerontology Series A:Biological Sciences and Medical Sciences. 2007;62(7):731–737. doi: 10.1093/gerona/62.7.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gobbens RJ, Van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JM. The Tilburg frailty indicator:psychometric properties. J Am Med Dir Assoc. 2010;11(5):344–355. doi: 10.1016/j.jamda.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Rockwood K. What would make a definition of frailty successful? Age and ageing. 2005;34(5):432–434. doi: 10.1093/ageing/afi146. [DOI] [PubMed] [Google Scholar]
- 11.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults:evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):146–157. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 12.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, et al. Frailty and risk of falls, fracture, and mortality in older women:the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62(7):744–751. doi: 10.1093/gerona/62.7.744. [DOI] [PubMed] [Google Scholar]
- 13.Cawthon PM, Marshall LM, Michael Y, Dam TT, Ensrud KE, Barrett-Connor E, et al. Frailty in older men:prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007;55(8):1216–1223. doi: 10.1111/j.1532-5415.2007.01259.x. [DOI] [PubMed] [Google Scholar]
- 14.Mitnitski A, Song X, Skoog I, Broe GA, Cox JL, Grunfeld E, et al. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc. 2005;53(12):2184–2189. doi: 10.1111/j.1532-5415.2005.00506.x. [DOI] [PubMed] [Google Scholar]
- 15.Kostakopoulos NA, Karakousis ND. Frailty assessment and postoperative complications in urologic oncology operations. J Frailty Sarcopenia Falls. 2020;5(3):57. doi: 10.22540/JFSF-05-057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan H, Kalogeropoulos AP, Georgiopoulou VV, Newman AB, Harris TB, Rodondi N, et al. Frailty and risk for heart failure in older adults:the health, aging, and body composition study. Am Heart J. 2013;166(5):887–894. doi: 10.1016/j.ahj.2013.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodríguez-Mañas L, Fried LP, Vellas B. Physical frailty:ICFSR international clinical practice guidelines for identification and management. The journal of nutrition, health &aging. 2019;23(9):771–787. doi: 10.1007/s12603-019-1273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldwater DS, Pinney SP. Frailty in advanced heart failure:a consequence of aging or a separate entity? Clin Med Insights:Cardiol. 2015;9:19698. doi: 10.4137/CMC.S19698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldfarb M, Sheppard R, Afilalo J. Prognostic and therapeutic implications of frailty in older adults with heart failure. Cur Cardiol Rep. 2015;17(11):1–7. doi: 10.1007/s11886-015-0651-3. [DOI] [PubMed] [Google Scholar]
- 20.Schopfer DW, Forman DE. Cardiac rehabilitation in older adults. Can J Cardiol. 2016;32(9):1088–1096. doi: 10.1016/j.cjca.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Boyer S, Gayot C, Bimou C, Mergans T, Kajeu P, Castelli M, et al. Prevalence of mild hyponatremia and its association with falls in older adults admitted to an emergency geriatric medicine unit (the MUPA unit) BMC geriatrics. 2019;19(1):1–6. doi: 10.1186/s12877-019-1282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ganguli A, Mascarenhas RC, Jamshed N, Tefera E, Veis JH. Hyponatremia:incidence, risk factors, and consequences in the elderly in a home-based primary care program. Clin Nephrol. 2015;84(2):75. doi: 10.5414/CN108453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhandari SK, Adams AL, Li BH, Rhee CM, Sundar S, Krasa H, et al. Sub-acute hyponatraemia more than chronic hyponatraemia is associated with serious falls and hip fractures. Internal Med J. 2020;50(9):1100–1108. doi: 10.1111/imj.14684. [DOI] [PubMed] [Google Scholar]
- 24.Miller AJ, Theou O, McMillan M, Howlett SE, Tennankore KK, Rockwood K. Dysnatremia in relation to frailty and age in community-dwelling adults in the National Health and Nutrition Examination Survey. J Gerontol A Biol Sci Med Sci. 2017;72(3):376–381. doi: 10.1093/gerona/glw114. [DOI] [PubMed] [Google Scholar]
- 25.Yaku H, Kato T, Morimoto T, Inuzuka Y, Tamaki Y, Ozasa N, et al. Risk factors and clinical outcomes of functional decline during hospitalisation in very old patients with acute decompensated heart failure:an observational study. BMJ open. 2020;10(2):e032674. doi: 10.1136/bmjopen-2019-032674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bertini V, Nicoletti C, Beker BM, Musso CG. Sarcopenia as a potential cause of chronic hyponatremia in the elderly. Med hypotheses. 2019;127:46–48. doi: 10.1016/j.mehy.2019.03.029. [DOI] [PubMed] [Google Scholar]
- 27.Grundmann F. Electrolyte disturbances in geriatric patients with focus on hyponatremia. Z Gerontol Geriatr. 2016;49(6):477–482. doi: 10.1007/s00391-016-1117-y. [DOI] [PubMed] [Google Scholar]
- 28.Hanotier P. Hyponatremia in the elderly:its role in frailty. Rev Med Brux. 2015;36(6):475–484. [PubMed] [Google Scholar]
- 29.Liamis G, Elisaf M. Hyponatremia induced by drugs. In Hyponatremia. New York, NY: Springer; 2013. pp. 111–126. [Google Scholar]
- 30.Sahoo S, Grover S. Hyponatremia and psychotropics. J Geriatr Ment Health. 2016;3(2):108. [Google Scholar]
- 31.Morley JE. Dehydration, Hypernatremia, and Hyponatremia. Clin Geriatr Med. 2015;31(3):389–399. doi: 10.1016/j.cger.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 32.Bourdel-Marchasson I, Laksir H, Puget E. Interpreting routine biochemistry in those aged over 65 years: a time for change. Maturitas. 2010;66(1):39–45. doi: 10.1016/j.maturitas.2010.02.004. [DOI] [PubMed] [Google Scholar]


