Abstract
Background
Breast cancer screening utilization steeply dropped at the start of the coronavirus disease 2019 (COVID‐19) pandemic. However, the effects on breast cancer screening in lower income populations are unknown. This study examined changes in breast cancer screening rates (BCSRs) during the pandemic among 32 community health centers (CHCs) that provided health care to lower income populations.
Methods
Secondary data from 32 CHCs participating in an American Cancer Society grant program to increase breast cancer screening services were used. BCSRs were defined as the percentage of women aged 50 to 74 years who had a medical visit in the past 12 months (142,207 in 2018, 142,003 in 2019, and 150,630 in 2020) and received a screening mammogram within the last 27 months. BCSRs in July 2020, July 2019, and June 2018 were compared with screening rate ratios (SRRs) and corresponding 95% confidence intervals (CIs).
Results
BCSRs significantly rose by 18% between 2018 and 2019 (from 45.8% to 53.9%; SRR, 1.18; 95% CI, 1.17‐1.18) and then declined by 8% between 2019 and 2020 (from 53.9% to 49.6%; SRR, 0.92; 95% CI, 0.92‐0.93). If the 2018‐2019 BCSR trends had continued through 2020, 63.3% of women would have been screened in 2020 in contrast to the 49.6% who were; this potentially translated into 47,517 fewer mammograms and 242 missed breast cancer diagnoses in this population.
Conclusions
In this study of 32 CHCs, BCSRs declined by 8% from July 2019 to 2020, and this reversed an 18% improvement between July 2018 and 2019. Declining BCSRs among CHCs during the COVID‐19 pandemic call for policies to support and resources to identify women in need of screening.
Keywords: access, breast cancer screening, community health centers, coronavirus disease 2019 (COVID‐19), disparities, neoplasm
Short abstract
In this study of 32 community health centers, breast cancer screening rates declined by 8% from July 2019 to 2020. This reverses an 18% improvement between July 2018 and 2019.
Introduction
The emergence of the coronavirus disease 2019 (COVID‐19) pandemic in the United States in the first quarter of 2020 caused delays in health care procedures, including cancer screening. 1 , 2 Recent reports have noted steep drops in breast cancer screening utilization at the start of the COVID‐19 pandemic. 2 , 3 However, the pandemic's effects on breast cancer screening in populations with lower incomes are not yet known. This is important because these populations have longstanding barriers to accessing care, lower breast screening rates, and higher breast cancer mortality rates 4 , 5 and are especially vulnerable to health care disruptions. In this study, we examined changes in breast cancer screening rates (BCSRs) during the pandemic among 32 community health centers (CHCs) that provide health care to people who are medically underserved. 6
Materials and Methods
This study used secondary data from 32 CHCs participating in the American Cancer Society's Community Health Advocates Implementing Nationwide Grants for Empowerment and Equity (CHANGE) grant program to increase BCSRs and follow‐up care. Beginning in August 2018, the CHANGE program funded clinics for 2 years, including 2020, to implement at least 3 evidence‐based client‐directed interventions (patient navigation, reminders, and education) and provider‐directed interventions (feedback and electronic medical record enhancements). CHCs periodically reported clinic‐level BCSRs throughout the 2‐year project period, which were defined as the percentage of women aged 50 to 74 years who had a medical visit within the past 12 months and received a screening mammogram within the last 27 months. There were 142,207, 142,003, and 150,630 women who had a medical visit in the past 12 months and were included in the 2018, 2019, and 2020 BCSR denominators, respectively. We compared overall BCSRs as of July 2020 versus July 2019 versus June 2018 and according to the regions, urban/rural status, and demographic characteristics of clinics with screening rate ratios (SRRs) and corresponding 95% confidence intervals (CIs). In ad hoc analyses, the numbers of potentially missed mammograms and breast cancer diagnoses were estimated under 2 scenarios: 1) if the 2018‐2019 trend extended through 2020 and 2) if 2019 rates remained level. 7 The number of potentially missed breast cancers was computed by multiplying the projected number of missed mammograms with the previously reported average cancer detection rate (5.1 breast cancers detected per 1000 mammograms). 7 The numbers of missed ductal carcinomas in situ and invasive breast cancers were similarly computed with their respective detection rates (1.6 and 3.5 per 1000 mammograms). 7 Analyses were conducted with SAS version 9.4. This study did not involve human subjects according to Emory University's institutional review board.
Results
Among women aged 50 to 74 years in 32 CHCs, BCSRs significantly rose by 18% between 2018 and 2019 (from 45.8% to 53.9%; SRR, 1.18; 95% CI, 1.17‐1.18) and then declined by 8% between 2019 and 2020 (from 53.9% to 49.6%; SRR, 0.92; 95% CI, 0.92‐0.93; Table 1). If 2018‐2019 BCSR trends had continued through 2020, 63.3% of women would have been screened in 2020 in contrast to the 49.6% who were; this translated into potentially 47,517 fewer mammograms and 242 missed breast cancer diagnoses, including 166 invasive breast cancers and 76 ductal carcinoma in situ cases (Figs. 1 and 2). If BCSRs had remained flat at 53.9% between 2019 and 2020, there would have been 6477 fewer mammograms, and this would resulted in 33 missed breast cancer diagnoses.
TABLE 1.
Breast Cancer Screening Rates Among 32 Community Health Centers, 2018‐2020
| No. of Clinics | 2018 (n = 142,207) a | 2019 (n = 142,003) a | 2020 (n = 150,630) a | 2019 vs 2018 | 2020 vs 2019 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| BCSR, % b | SRR | 95% CI c | SRR | 95% CI c | ||||||
| Total | 32 | 45.8 | 53.9 | 49.6 | 1.18 | 1.17 | 1.18 | 0.92 | 0.92 | 0.93 |
| Urban/rural | ||||||||||
| Rural | 4 | 23.0 | 36.5 | 35.1 | 1.59 | 1.53 | 1.65 | 0.96 | 0.93 | 0.99 |
| Urban | 28 | 48.3 | 55.4 | 51.3 | 1.15 | 1.14 | 1.15 | 0.93 | 0.92 | 0.93 |
| Region d | ||||||||||
| Midwest | 8 | 38.5 | 48.6 | 43.7 | 1.26 | 1.24 | 1.29 | 0.90 | 0.88 | 0.92 |
| Northeast | 6 | 65.5 | 64.4 | 56.4 | 0.98 | 0.97 | 0.99 | 0.88 | 0.87 | 0.89 |
| South | 11 | 33.4 | 45.8 | 45.4 | 1.37 | 1.35 | 1.39 | 0.99 | 0.98 | 1.00 |
| West | 7 | 51.5 | 59.6 | 53.8 | 1.16 | 1.14 | 1.18 | 0.90 | 0.89 | 0.91 |
| % Uninsured e | ||||||||||
| Low (<13.3%) | 12 | 59.4 | 62.4 | 53.1 | 1.05 | 1.04 | 1.06 | 0.85 | 0.84 | 0.86 |
| Medium (13.3%‐26.2%) | 9 | 37.3 | 52.2 | 50.2 | 1.40 | 1.38 | 1.42 | 0.96 | 0.95 | 0.97 |
| High (≥26.3%) | 11 | 37.0 | 43.4 | 42.0 | 1.17 | 1.15 | 1.20 | 0.97 | 0.95 | 0.98 |
| % Hispanic e | ||||||||||
| Low (<10%) | 10 | 31.0 | 45.1 | 41.5 | 1.46 | 1.42 | 1.49 | 0.92 | 0.90 | 0.94 |
| Medium (10%‐32%) | 11 | 49.1 | 52.2 | 47.7 | 1.06 | 1.05 | 1.08 | 0.91 | 0.90 | 0.92 |
| High (≥33%) | 11 | 48.6 | 57.9 | 54.1 | 1.19 | 1.18 | 1.20 | 0.93 | 0.92 | 0.94 |
| % Black e | ||||||||||
| Low (<22%) | 10 | 40.2 | 52.5 | 49.9 | 1.31 | 1.29 | 1.33 | 0.95 | 0.94 | 0.97 |
| Medium (22%‐50%) | 11 | 46.8 | 53.9 | 49.7 | 1.15 | 1.14 | 1.16 | 0.92 | 0.91 | 0.93 |
| High (≥51%) | 11 | 49.9 | 55.3 | 48.9 | 1.11 | 1.09 | 1.12 | 0.88 | 0.87 | 0.90 |
Abbreviations: BCSR, breast cancer screening rate; CI, confidence interval; SE, standard error; SRR, screening rate ratio.
The n value is the number of women in the denominator (defined as women aged 50‐74 years who had a medical visit within the past 12 months).
BCSRs were defined according to the Centers for Medicare and Medicaid Services Measurement Identification Number 125 (CMS‐125) measure as the percentage of women aged 50 to 74 years who had a medical visit within the past 12 months and received a screening mammogram within the last 27 months. The 2018, 2019, and 2020 BCSRs were as of June 2018, July 2019, and July 2020, respectively.
SEs were determined with a delta method–derived formula:
where p is the proportion of women screened and n is the number of women eligible (those aged 50‐74 years who had a medical visit in the past 12 months) for comparison years. For example, for the 2020‐2019 SRR, p1 was the proportion screened in 2020, n1 was the number of eligible women in 2020, p2 was the proportion screened in 2019, and n2 was the number of eligible women in 2019.
Based on US Census regions.
Low, medium, and high were defined according to tertile ranks with the ranges presented in the table. For example, low for the percentage uninsured included clinics with the lowest proportion of uninsured patients. There were 12 clinics with a low proportion of uninsured because of a tie in the proportion uninsured.
Figure 1.
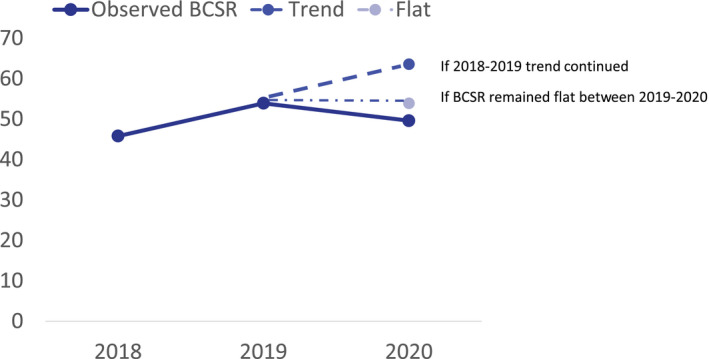
Observed BCSRs among 32 community health centers: 2018, 2019, and 2020. The observed BCSRs were defined according to the CMS‐125 measure as the percentage of women aged 50 to 74 years who had a medical visit within the past 12 months and received a screening mammogram within the last 27 months. The observed 2018, 2019, and 2020 BCSRs were as of June 2018, July 2019, and July 2020, respectively. Hypothetical 2020 BCSRs were projected under 2 scenarios: 1) if the 2018‐2019 trend extended through 2020 and 2) if 2019 rates remained level. BCSR indicates breast cancer screening rate.
Figure 2.
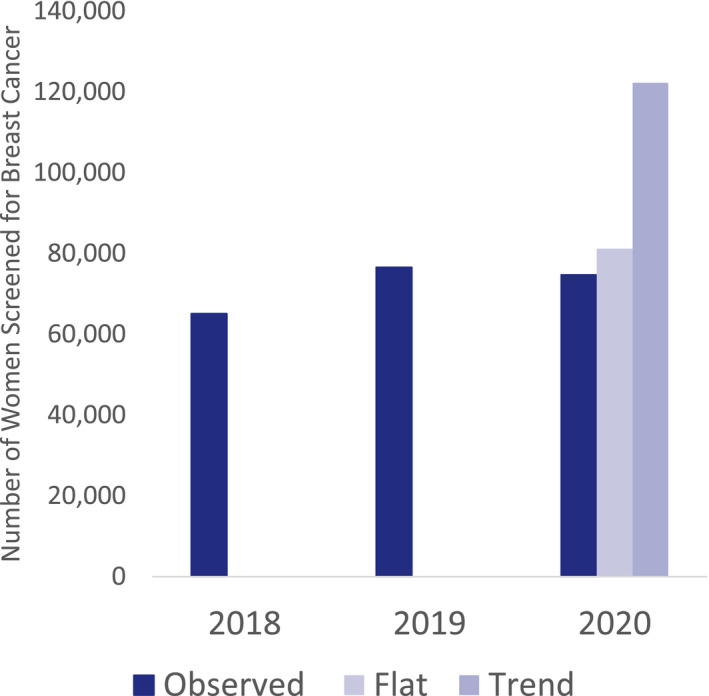
Observed and projected numbers of women screened among 32 community health centers: 2018, 2019, and 2020. Observed numbers of breast cancer screenings were computed as of July 2018, 2019, and 2020. The number of breast cancer screenings was projected under 2 scenarios: 1) if the 2018‐2019 trend extended through 2020 and (2) if 2019 rates remained level.
The pattern of BCSR increasing and then decreasing between 2018‐2019 and 2019‐2020 was generally observed across clinic characteristics, although magnitudes varied. Between 2019 and 2020, CHCs with a higher proportion of Black patients (SRR, 0.88; 95% CI, 0.87‐0.90) and a lower proportion of uninsured patients (SRR, 0.85; 95% CI, 0.84‐0.86) experienced greater declines, and there were no significant changes among clinics located in the South.
Discussion
In this study of 32 CHCs, BCSRs declined by 8% from July 2019 to 2020, and this reversed an 18% improvement between July 2018 and 2019. Modeling analyses have estimated that a 75% decline in the BCSR over 6 months could lead to an excess of 5000 breast cancer deaths by 2030 nationally. 8 It is not known how negative outcomes will be distributed or whether breast cancer mortality disparities will widen. We observed generally consistent declines across CHCs, although magnitudes were greater in clinics serving a higher proportion of Black patients. Southern clinics maintained BCSRs, and this possibly reflected lower baseline rates or impact of stay‐at‐home orders; further study is warranted.
The magnitude of the BCSR declines in our study was less than the 30% decline between June 2020 and 2017‐2019 and an earlier 94% drop in March/April 2020 according to an electronic health record research network report. 2 Within a large Boston metro‐area health system, BCSRs nearly rebounded in June to September 2020 to prepandemic levels after an initial steep drop during the spring of 2020. 3 Although these studies were based on electronic health record and billing data that track data on a more frequent basis (eg, daily or monthly), our data included reports from a single month (July), and our screening metric included a 27‐month look‐back period that captured a period before the COVID‐19 pandemic. This is among the study limitations, which include a lack of individual‐level data and the unknown representativeness of the 32 out of 1385 CHCs in the United States. 6
We also note that the CHANGE program–funded interventions, which were established before and were continued through 2020, may have mitigated the pandemic's effects on breast cancer screening services among the 32 CHCs that were studied. Further investigation of BCSRs among additional CHCs will further inform where targeted interventions (eg, client reminders and education on a return to screening) are most needed.
This is one of the first studies to examine BCSRs during the pandemic specifically among clinics providing care to communities of color and lower income populations, groups with lower utilization of and greater barriers to breast cancer screening. 9 Declining BCSRs among CHCs during the COVID‐19 pandemic call for policies to support and resources to identify women in need of screening. These actions will be critical for returning to and surpassing prepandemic BCSRs in CHCs and the lower income populations that they serve.
Funding Support
Funding for the Breast Health Equity Community Health Advocates Implementing Nationwide Grants for Empowerment and Equity (CHANGE) grant was provided by the National Football League (NFL) in partnership with the American Cancer Society. Funding provided by the NFL helped to execute and sustain activities at all project sites in addition to supplementing administrative salaries to support the CHANGE grant program. The NFL was not involved in the writing of this research article. The funders had no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; in the preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication.
Conflict of Interest Disclosures
All the authors are employed by the American Cancer Society, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside the submitted work. The salaries for Kristen A. Wehling and Karla Wysocki are partially funded by Pfizer grants for projects outside the scope of this article. Stacey A. Fedewa, Megan M. Cotter, Richard Killewald, and Laura Makaroff are not funded by or key personnel for any of these grants, and their salaries are solely funded through American Cancer Society funds. Fedewa also reports National Cancer Institute honoraria for a Cancer Epidemiology Education in Special Populations talk (August 2019), which were donated to the American Cancer Society, and Makaroff has served on an advisory board for the University of New Mexico project ECHO.
Author Contributions
Stacey A. Fedewa: Full access to all of the data in the study and responsibility for the integrity of the data and the accuracy of the data analysis; acquisition, analysis, or interpretation of the data; statistical analysis; supervision; concept and design; drafting of the manuscript; and critical revision of the manuscript for important intellectual content. Megan M. Cotter: Concept and design; acquisition, analysis, or interpretation of the data; drafting of the manuscript; and critical revision of the manuscript for important intellectual content. Kristen A. Wehling: Concept and design; administrative, technical, or material support; drafting of the manuscript; and critical revision of the manuscript for important intellectual content. Karla Wysocki: Concept and design; administrative, technical, or material support; drafting of the manuscript; and critical revision of the manuscript for important intellectual content. Richard Killewald: Concept and design; acquisition, analysis, or interpretation of the data; administrative, technical, or material support; drafting of the manuscript; and critical revision of the manuscript for important intellectual content. Laura Makaroff: Concept and design; acquisition, analysis, or interpretation of the data; supervision; drafting of the manuscript; and critical revision of the manuscript for important intellectual content.
Fedewa SA, Cotter MM, Wehling KA, Wysocki K, Killewald R, Makaroff L. Changes in breast cancer screening rates among 32 community health centers during the COVID‐19 pandemic. Cancer. 2021. 10.1002/cncr.33859
See editorial on pages 4365‐4367, this issue.
We thank the National Football League for its support of the Community Health Advocates Implementing Nationwide Grants for Empowerment and Equity (CHANGE) program as well as the American Cancer Society regional staff managing the extensive relationships with all health systems involved with the project.
References
- 1. Czeisler ME, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID‐19–related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250‐1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mast C, del Rio AM. Delayed cancer screenings—a second look. Epic Health Research Network. Published July 17, 2020. Accessed February 10, 2020. https://www.ehrn.org/articles/delayed‐cancer‐screenings‐a‐second‐look [Google Scholar]
- 3. Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh QD. Cancer screening tests and cancer diagnoses during the COVID‐19 pandemic. JAMA Oncol. 2021;7:458‐460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American Cancer Society . Cancer Prevention & Early Detection Facts & Figures 2019‐2020. American Cancer Society; 2019. [Google Scholar]
- 5. Withrow DR, Berrington de Gonzalez A, Spillane S, et al. Trends in mortality due to cancer in the United States by age and county‐level income, 1999‐2015. J Natl Cancer Inst. 2019;111:863‐866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. National Health Center data. Health Resources and Services Administration. Accessed December 7, 2020. https://data.hrsa.gov/tools/data‐reporting/program‐data/national [Google Scholar]
- 7. Lehman CD, Arao RF, Sprague BL, et al. National performance benchmarks for modern screening digital mammography: update from the Breast Cancer Surveillance Consortium. Radiology. 2017;283:49‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sharpless NE. COVID‐19 and cancer. Science. 2020;368:1290. [DOI] [PubMed] [Google Scholar]
- 9. Schootman M, Jeffe DB, Baker EA, Walker MS. Effect of area poverty rate on cancer screening across US communities. J Epidemiol Community Health. 2006;60:202‐207. [DOI] [PMC free article] [PubMed] [Google Scholar]


