1. INTRODUCTION
Specialist Palliative Care Needs Rounds (SPCNR) in residential aged care (RAC, or care homes), led by in‐reach specialist palliative care nurse practitioners, are an evidence‐based approach that improves the quality of death and dying by strengthening end‐of‐life care planning. 1 SPCNRs consist of Needs Rounds meetings (monthly triage and risk stratification meetings, hereafter ‘Needs Rounds’), multidisciplinary case conferences and clinical work.
In April 2018, and in the absence of a nurse practitioner, Needs Rounds were introduced by a palliative medicine physician (SR) into 2 RAC facilities in one Australian rural town. The detail around methods and intervention are published elsewhere. 2 , 3 Needs Rounds increased the uptake of end‐of‐life care plans and strengthened staff confidence in providing end‐of‐life care. In 2019, due to limited resources and a focus on a larger multidisciplinary case conference hybrid implementation‐effectiveness study (Phase 1), 4 Needs Rounds meetings were temporarily suspended. As part of that larger study, in January 2020, Needs Rounds were reintroduced into routine clinical care, with the potential to expand into additional RAC facilities (Phase 2).
In order to scale up Needs Rounds for other rural and remote areas, where specialist palliative care is often limited, 5 alternative delivery platforms need exploring. Telehealth, the delivery of health care services via communications technologies, is one option to reduce inequities in access to specialist health services in rural, remote and regional areas. 6 , 7 However, the uptake of telehealth has often been slow due to limited reliable infrastructure (equipment or connectivity) and support, and concerns regarding rapport and cybersecurity. 8 , 9
In March 2020, the World Health Organization declared COVID‐19 to be a pandemic. Older people, especially those in RAC, were considered to be amongst the most vulnerable groups. 10 , 11 To safeguard residents from COVID‐19, RAC visitors in many countries, including Australia, have been restricted. In some jurisdictions, non‐essential visitors (including some specialist services) were temporarily restricted while in others, full lockdowns prevented any entrants. 12 This provided opportunity to immediately trial Needs Rounds via teleconferencing.
This short report presents data collected in Phase 2 of the larger study pertinent to the use of telehealth from the perspectives of RAC staff who participated in the Needs Rounds. The aim was to test whether telehealth is an acceptable and useful option to facilitate palliative care Needs Rounds triage meetings in rural RAC.
2. METHODS
2.1. Design
This was Phase 2 of a larger (hybrid type‐3 effectiveness‐implementation) study. Detail around Phase 1 methods and results is published elsewhere. 4 This study design 13 tests an implementation intervention/strategy (in this case, Needs Rounds via telehealth) while collecting data on the intervention's impact on relevant outcomes (documented end‐of‐life care plans including anticipatory medications and place of death).
2.2. Measures
Primary measures include (a) total number of Needs Rounds; (b) number of residents discussed in Needs Rounds; and (c) degree of satisfaction of staff in using telehealth. Secondary measures include (d) documentation of end‐of‐life care plans including charting of anticipatory medications; and (e) place of death. We hypothesised that if telehealth is as effective as face‐to‐face Needs Rounds, these meetings would continue on a monthly frequency with similar numbers of residents discussed.
2.3. Setting
Three RAC facilities in the rural Snowy‐Monaro region of NSW, Australia, participated. Two facilities (Sites 1 and 2) had participated in previous face‐to‐face Needs Rounds and multidisciplinary case conference studies. 2 , 3 , 4 Prior to the pandemic declaration, the third facility, located in a small town 60 km away (Site 3) and with no prior relationship to the specialist, had agreed to implement Needs Rounds.
2.4. Model
2.4.1. Intervention
Monthly Needs Rounds, led by a palliative medicine physician (SR) and attended by RAC staff (described elsewhere), 2 , 3 were adapted for delivery via online videoconference using Zoom. Using the Needs Round checklist criteria 14 (prognosis of 6 months or less, physical or cognitive decline or symptom exacerbation in the last 3 months, no end‐of‐life care plan, family conflict regarding goals of care or resident transferred to RAC for end‐of‐life care), residents identified by staff as being at greatest risk of dying without a plan in place or with a high symptom burden were discussed. Individual end‐of‐life care plans were developed through case‐based education. General practitioners (GPs) and families did not normally attend; however, on 2 occasions, Needs Rounds were adapted to urgently include a family member. Individual summaries and action plans were completed by the physician and emailed to the facility. These guided follow‐up discussions, between RAC senior staff and GPs, to complete end‐of‐life management plans.
2.4.2. Implementation
The palliative medicine physician (SR), working from home, had access to a private corporate Zoom licence, ensuring all communication was encrypted. Each facility decided which residents to discuss and staff members to attend. Content consistency was maintained through a checklist template. 14
Facilities had different levels of technical preparedness, leading to some being able to immediately support videoconferencing, while others transitioned from telephone conferencing. The Needs Rounds implementation strategy is illustrated in Figure 1. Videoconferences were organised differently at each facility. Site 1 had a large meeting room in an adjacent off‐site building. Participating staff attended together while maintaining COVID‐19 physical distancing requirements. Once visiting restrictions were eased, face‐to‐face meetings resumed, initially in the off‐site building. With further easing of restrictions, face‐to‐face Needs Rounds were conducted on‐site with one senior staff member continuing to join off‐site via Zoom. Participants in Sites 2 and 3 attended Zoom meetings from an office in the RAC facility.
FIGURE 1.
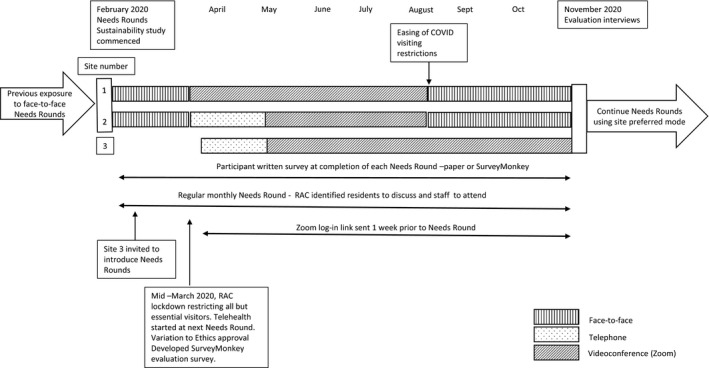
Telehealth Needs Rounds implementation strategy
2.4.3. Evaluation
Implementation and intervention effectiveness were assessed using the Standards for Reporting Implementation Studies (StaRI) guidelines (Figure 2). 15
FIGURE 2.
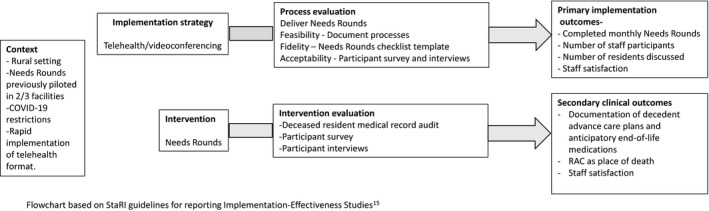
Telehealth Needs Rounds implementation and effectiveness evaluation
2.5. Data collection and analysis
Qualitative and quantitative data were collected concurrently from participating RAC staff at each site to optimise the sample and enhance understanding of the data. 16
2.5.1. Staff surveys
At completion of each Needs Round, all participants were invited to complete either a paper (face‐to‐face) or online (telehealth) 6‐item survey addressing the usefulness of Needs Rounds (intervention effectiveness) and perspectives on different implementation modes (implementation). Sixty surveys were distributed; 29 were returned (response rate 48%); survey return implied consent.
2.5.2. Staff interviews
All Needs Round attendees were invited by SR to participate in an interview. Willingness to participate was indicated by return of a written consent including individual contact details (mobile phone number or email address) and permission to forward contact details to the interviewer (SHD; a non‐local registered nurse and experienced qualitative researcher). Seven participants (2 managers [M], 4 registered nurses [RN] and one care assistant) provided written consent to participate in a telephone interview; however, one registered nurse and the care assistant rescinded consent when contacted. Semi‐structured interviews, lasting 28‐50 minutes (mean 38 minutes), were audio‐recorded and professionally transcribed. Both implementation and effectiveness questions were included. Active listening was used to confirm correct understanding; transcripts were not returned.
2.5.3. Review of decedent records
As part of the larger study, data (documented evidence of an end‐of‐life care plan, anticipatory medications and place of death) were collected by SR from the health record of all residents who died during the study period.
Survey and chart review quantitative data were analysed using descriptive statistics (SR). Interview data were coded and analysed thematically, by SR and SHD, using the approach of Braun and Clarke (data familiarisation, generating initial codes, searching for themes, reviewing themes, defining and naming themes). 17
2.6. Ethics approval
This study was approved by the Australian National University Human Research Ethics Committee through a variation to protocol 2017/933, dated 25/03/2020.
3. RESULTS
Twenty‐five Needs Rounds (15 telehealth, 10 face‐to‐face) were conducted between 3 February and 2 November 2020. Forty‐seven residents were discussed at least once; 23 RAC staff (10 registered nurses, 9 care assistants, 4 managers) attended at least one Needs Round.
3.1. Effectiveness and Implementation
Table 1 presents the effectiveness of using telehealth and the perspectives of staff on Needs Rounds and different implementation modes. During the study period, 21 RAC residents who had been discussed in a Needs Round died (21/31 of all RAC deaths at the time). This included 14 who were discussed via telehealth. Of these 14, all had a documented end‐of‐life care plan, 86% had anticipatory medications charted, and 93% died in their facility.
TABLE 1.
Telehealth Needs Rounds outcome measures (effectiveness and staff satisfaction)
| Delivery Method | Telehealth | Face‐to‐face | |
|---|---|---|---|
| Videoconference | Teleconference | F2F | |
| Total number of Needs Rounds | 11 | 4 a | 10 b |
| Total number of residents discussed | |||
| New | 16 | 8 | 23 |
| Follow‐up | 22 | 6 | 7 |
| Mean residents discussed at each NR, range | 3.8 [2‐6] | 3.25 [2‐5] | 3.5 [1‐6] |
| Total staff | 13 | 3 | 18 |
| Mean staff at each NR, range | 3 [2‐7] | 1.5 [1‐2] | 3.9 [1‐6] |
| NR cancelled | 0 | 0 | 2 c |
| Decedent medical file review (N = 21) | n = 10 | n = 4 | n = 7 |
| Documented end‐of‐life care plan | 10 (100%) | 4 (100%) | 5 (71%) |
| End‐of‐life medications charted | 9 (90%) | 3 (75%)d | 4 (57%) |
| Died in RAC | 10 (100%) | 3 (75%)d | 6 (86%) |
| Staff survey questions relevant to telehealth e |
All RAC staff responses (N = 29) Median [range] |
Responses from staff who attended telehealth NR f (n = 11) |
Responses from staff who attended F2F NR (n = 18) |
|---|---|---|---|
| This needs round was helpful in planning end‐of‐life care for the residents discussed | 4 [3‐5] | 4 [3‐5] | 4.5 [4‐5] |
| I was able to make a worthwhile contribution | 4 [2‐5] g | 4 [3‐5] | 4 [2‐5] g |
| Needs rounds will improve the coordination of care for the residents discussed | 4 [4‐5] | 4.5 [4‐5] | 4.5 [4‐5] |
| Satisfaction with this telephone/videoconferencing (or if F2F NR, satisfaction with previous telehealth NR compared with this F2F NR) | 3 [1‐5] h | 4 [3‐5] h | 2.5 [1‐5] i |
This study was not powered sufficiently to show differences between the different delivery methods.
Abbreviations: F2F, face‐to‐face; NR, Needs Round; RAC, residential aged care
Telehealth delivery method: videoconference (Zoom); teleconference (telephone).
Poor Zoom connectivity during one Needs Round so switched to phone.
One off‐site staff member joined via Zoom on 2 occasions.
Cancelled due to workforce shortages.
At request of family, one resident transferred to hospital at midnight for management of acute symptoms, died in hospital on same day.
Items were rated on a scale of 1 (not confident/satisfied) to 5 (completely confident/satisfied).
Telehealth—9 videoconference, 2 telephone.
Score 2 was given by a manager who had been in the position for less than 1 wk.
Higher rates of satisfaction were given when only one or 2 participants attended via Zoom.
n = 11; no response received from 7 participants who had not participated in a telehealth NR; score of 1 indicated low satisfaction with telehealth compared with F2F; score of 5 indicated greater satisfaction with telehealth.
3.2. Infrastructure
Telehealth required access to compatible equipment, ‘My computer screens don't have the camera’ (RN01‐Site2), and a stable Internet connection. Frequent ‘dropouts’ and ‘time lags’ were frustrating.
3.3. Commitment and flexibility
Residential aged care staff were committed to continuing Needs Rounds and found ways to overcome system failures,
We've had a couple of technical hiccups, but we just rang [the specialist] on the phone and it went perfectly fine. (RN02‐Site3)
3.4. Sharing documents
All participants identified at least one implementation deficiency for telehealth. For one participant, it was the inability to peruse the same documents in real time,
It's just handy to be able to all look at the same documents together, you know, looking at primary medication charts or care directives all together and discussing it face‐to‐face rather than Zoom. (RN01‐Site2)
On the other hand, another participant found videoconferencing helpful in managing the paperwork,
Zoom works for everybody because there's no extra travel for anyone and we can sort of sit down with our files. (M02‐Site3)
3.5. Communication
Consistent with the survey data, the 2 interviewees who had previously attended face‐to‐face meetings felt that ‘face‐to‐face for that sort of discussion is much better’ (M01‐Site1) as spontaneous dialogue was inhibited when using telehealth, especially with larger groups.
Regardless of the platform used, Needs Rounds strengthened relationships between the specialist and staff. Over time the increased familiarity with, and confidence in, telehealth had other clinical benefits and provided access to specialist advice after‐hours:
So, on Sunday, I just took my laptop up to the man that was dying, and it was beautiful. [The specialist] could talk to him, she could talk to his daughter. She was able to see him, [and] instruct me about what she wanted me to do. So, taking the two‐hour round trip off her and just doing it by Zoom I think's a good compromise. (RN02‐Site3)
4. DISCUSSION
4.1. Main findings
We have reported the first study to conduct telehealth Needs Rounds triage meetings in rural RAC. While face‐to‐face meetings were preferred, videoconferencing was readily implemented and an acceptable compromise; telephone was a suitable backup. Telehealth proved to be an effective platform 18 to continue Needs Rounds in existing sites and initiate them in new ones, while enabling our larger effectiveness‐implementation study to continue. Telehealth Needs Rounds were useful in facilitating end‐of‐life care planning. Consistent with a COVID‐19 study in metropolitan RAC, 19 telehealth delivery was as effective as face‐to‐face modes, in terms of numbers of attendees and residents discussed, and completion of end‐of‐life care plans.
Access to specialist palliative care, including Needs Rounds, should be available to all RAC residents regardless of their location. Telehealth has the potential to provide access to specialist services, including Needs Rounds, where local resources are limited by distance (rural, remote and developing countries) or restricted during local infectious disease outbreaks or pandemics. 6 , 8 , 19 , 20 , 21 Globally, the rapid uptake of telehealth, spurred by COVID‐19, was embraced by clinicians, consumers and health services. 22 The acceptance of, and satisfaction with telehealth reported by the RAC staff in this study, is consistent with the findings of a recent literature review. 22 However, the success and sustainability of telehealth are dependent on reliable and secure equipment and connectivity, commitment by the clinician and RAC staff to support telehealth and flexibility especially during system failures. 18 , 21 , 22
4.2. Strengths and weaknesses
Consistent with current COVID‐19 palliative care research, 23 this study is limited by its small size, but strengthened by the mixed‐methods approach. 16 As this was an opportunistic study, it is insufficiently powered to show differences between the modalities and we were reliant on participants' existing telehealth skills and equipment, with no time for training. During this study, there was no local community‐acquired COVID‐19; it is difficult to know if commitment to telehealth Needs Rounds would have increased or decreased in priority had there been active COVID‐19 in these 3 RAC facilities. 19
In conclusion, while this was a small study, there is sufficient evidence to recommend and encourage telehealth Needs Rounds as routine in rural areas lacking specialist resources. Larger multi‐centre rural studies on the use of telehealth in RAC are also encouraged.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest with respect to the research, authorship or publication of this article.
AUTHOR CONTRIBUTIONS
All authors made a substantial contribution to the study design. SR was the chief investigator for the study being responsible for study administration, management, leading the Needs Rounds, and collection and analysis of survey and decedent health record data. SHD conducted the interviews. SR and SHD analysed the qualitative data. SR wrote the draft paper; all authors revised it critically for important intellectual content. All authors read and approved the final manuscript.
SUPPLEMENTARY DATA AND MATERIALS
Data is available to bona fide researchers by contacting the corresponding author.
Rainsford S, Hall Dykgraaf S, Phillips C. Effectiveness of telehealth palliative care Needs Rounds in rural residential aged care during the COVID‐19 pandemic: A hybrid effectiveness‐implementation study. Aust J Rural Health.2022;30:108–114. 10.1111/ajr.12789
Funding information
This project was supported by funding from COORDINARE—South Eastern New South Wales Primary Health Network through the Australian Government's Primary Health Network Program. The funder had no role in the conduct of the study or interpretation of the results
REFERENCES
- 1. Forbat L, Liu W‐M, Koerner J, et al. Reducing time in acute hospitals: a stepped‐wedge randomised control trial of a specialist palliative care intervention in residential care homes. Palliat Med. 2020;34(5):571‐579. [DOI] [PubMed] [Google Scholar]
- 2. Rainsford S, Liu W‐M, Johnston N, Glasgow N. The impact of introducing palliative care Needs Rounds into rural residential aged care: a quasi‐experimental study. Aust J Rural Health. 2020;28(5):480‐489. [DOI] [PubMed] [Google Scholar]
- 3. Rainsford S, Johnston N, Liu W‐M, Glasgow N, Forbat L. Palliative care needs rounds in rural residential aged care: a mixed‐methods study exploring experiences and perceptions of staff and general practitioners. Prog Palliat Care. 2019;28(5):308‐317. [Google Scholar]
- 4. Rainsford S, Hall Dykgraaf S, Kasim R, Phillips C, Glasgow N. Strengthening advance care planning in rural residential aged care through multidisciplinary educational case conferences: a hybrid implementation‐effectiveness study, Prog Palliat Care. 2021;29(4):199–208. 10.1080/09699260.2021.1872136 [DOI] [Google Scholar]
- 5. NSW Auditor General . New South Wales Auditor‐General’s report – performance audit: planning and evaluating palliative care services in NSW. Sydney: Audit Office NSW; 2017. www.audit.nsw.gov.au/sites/default/files/pdf‐downloads/01_Palliative_Care_Full_Report.pdf. Accessed February 18, 2020. [Google Scholar]
- 6. Moffatt J, Eley D. The reported benefits of telehealth for rural Australians. Aust Health Rev. 2010;34(3):276‐281. [DOI] [PubMed] [Google Scholar]
- 7. Health informatics — Telehealth services — Quality planning guidelines. ISO 13131. 2021. https://www.iso.org/standard/75962.html. Accessed July 30, 2021.
- 8. Fisk M, Livingstone A, Pit S. Telehealth in the context of COVID‐19: changing perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res 2020;22(6):e19264. 10.2196/19264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Collier A, Morgan D, Swetenham K, To T, Currow D, Tieman J. Implementation of a pilot telehealth programme in community palliative care: a qualitative study of clinicians' perspectives. Palliat Med. 2016;30(4):409‐417. [DOI] [PubMed] [Google Scholar]
- 10. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Holt NR, Neuman JT, McNeil JJ, Cheung AC. Implications of COVID‐19 in an ageing population. Med J Aust. 2020;213(8):342‐344.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Communicable Diseases Network Australia CDN Coronavirus (COVID‐19) Guidelines for Outbreaks in Residential Care Facilities. CDNA National Guidelines for the Prevention, Control and Public Health Management of COVID‐19 Outbreaks in Residential Care Facilities in Australia version 4.0. 2021. https://www.health.gov.au/sites/default/files/documents/2021/03/cdna‐national‐guidelines‐for‐the‐prevention‐control‐and‐public‐health‐management‐of‐covid‐19‐outbreaks‐in‐residential‐care‐facilities‐in‐australia_0.pdf. Accessed July 2021.
- 13. Curran GM, Bauer M, Mittman L, Pyne JM, Stetler C. Effectiveness‐implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Forbat L, Chapman M, Lovell C, Liu WM, Johnston N. Improving specialist palliative care in residential care for older people: a checklist to guide practice. BMJ Support Palliat Care. 2018;8:347‐353. [DOI] [PubMed] [Google Scholar]
- 15. Pinnock H, Barwick M, Carpenter C, et al. Standards for Reporting Implementation Studies (StaRI) statement. BMJ. 2017;356: i6795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Farquhar M, Ewing G, Booth S. Using mixed methods to develop and evaluate complex interventions in palliative care research. Palliat Med. 2011;25(8):748‐757. [DOI] [PubMed] [Google Scholar]
- 17. Braun V, Clarke V. Using thematic analysis in Psychology. Qual Res Psychol. 2006;3:77‐101. [Google Scholar]
- 18. Jess M, Timm H, Dieperink K. Video consultations in palliative care: a systematic integrative review. Palliat Med. 2019;33(8):942‐958. [DOI] [PubMed] [Google Scholar]
- 19. Samara J, Liu W‐M, Kroon W, Harvie B, Hingeley R, Johnston N. Telehealth palliative care needs rounds during a pandemic. J Nurse Pract. 2021;17(3):335‐338. [Google Scholar]
- 20. O'Kane G. Telehealth—improving access for rural, regional and remote communities. Aust J Rural Health. 2020;28:419‐420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bradford NK, Caffery LJ, Smith AC. Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. Rural Remote Health. 2016;16:4268. [PubMed] [Google Scholar]
- 22. Hall Dykgraaf S, Desborough J, de Toca L, et al. “A decade's worth of work in a matter of days”: the journey to telehealth for the whole population in Australia. Int J Med Inform. 2021;151(104483):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Walshe C. Perspectives on COVID‐19 and palliative care research. Palliat Med. 2021;35(1):4‐5. [DOI] [PubMed] [Google Scholar]


