Abstract
This study aimed to investigate the perceptions of patient-centered care (PCC) among inpatients in Guangdong Province (GD), China. Based on these perspectives, we sought to understand existing PCC practices in medical institutions and identify the impacts of inpatients’ sociodemographic status on their perceived PCC. A self-developed PCC questionnaire was used to investigate inpatients’ perceptions of PCC. A cross-sectional survey was conducted in nine tertiary-level hospitals across five cities in GD. Descriptive statistics was used to describe the levels of PCC in GD. The differences in PCC levels across different sociodemographic groups were assessed using analysis of variance and multivariate linear regression. Valid responses were provided by 1863 inpatients. The mean overall PCC score was 8.58 (standard deviation [SD] = 1.36); inpatients from the Pearl River Delta and eastern GD area reported significantly higher scores than those from western and northern GD area (P<.01). Inpatients from rural areas tended to report lower PCC scores than their urban counterparts. Among the PCC questionnaire sub-domains, inpatients scored highest and lowest in “patient experience” (mean = 8.96, SD = 1.34) and “medical insurance” (mean = 7.93, SD = 2.05), respectively. This study provided a comprehensive overview of inpatients’ perceptions of PCC in the public healthcare system in GD, China. Our findings highlighted that a majority of inpatients were satisfied with the PCC in public healthcare system; however, a significant discrepancy between inpatients with different sociodemographic status remained.
Keywords: patient-centered care, inpatient, sociodemographic status, public healthcare system, China
Introduction
The primary goal of patient-centered care (PCC) is to empower patients to become active participants in their healthcare and improve individual health outcomes. This makes PCC an approach worth promoting in almost any healthcare delivery system. 1 The number of studies featuring the term “patient-centered care” has been continuously increasing over the past 3 decades, 2 and PCC is now recognized as an essential characteristic of high-quality healthcare services.3,4 In particular, themes such as biopsychosocial perspective, coordinated care, integrated and continuous care, proactive and prepared care teams, shared decision-making, and individual needs are commonly associated with PCC.5-7 Additionally, under the traditional healthcare system, clinicians mainly focus on treating the disease, rather than providing holistic care for the patient, and focus on using advanced technology, rather than respecting patients’ preference. However, modern medicine is complicated; an increasing number of studies have shown that PCC can effectively address this limitation, 8 reshape the humanistic nature of medical services, 9 and improve the quality and efficiency of healthcare services.10,11
The practice of PCC enjoys global consensus, as all top-performing medical systems worldwide promote PCC. 12 This trend is especially notable in China, whose healthcare system has undergone rapid and profound changes. 13 In recent years, the Chinese government has paid greater attention to promoting healthcare system reforms, such as strengthening investment in primary healthcare to improve the accessibility of medical services, 14 reforming the public medical insurance payment system to control increasing burden of medical expenses, improving the medical legal system, and providing medical professionals with remuneration that reflects the value of their services. 15 These efforts have considerably enhanced patients’ medical treatment experience and their perception of PCC. However, the current understanding of PCC’s connotation is not uniform across countries,16,17 and inpatients’ perception of PCC remains unknown in GD.
With decades of rapid economic development as its foundation, China currently has the largest number of middle-income earners in the world. This implies that Chinese people’s consumption of healthcare has become more refined; that is, people’s perceptions of health care have changed from being subsistence-based to quality-based. 17 In this context, patients develop a desire to be more involved in their medical treatment, concomitantly expecting to have better healthcare experiences, more satisfactory medical treatment environments, friendlier medical professionals, and safer and more efficient medical services. 18 These emergent patient preferences are the core characteristics of PCC19,20; therefore, it is necessary to investigate to what extent the patients’ needs have been met.
Although the benefits of PCC have been recognized by China’s medical community, 21 there has been no specific research into inpatients’ perception of PCC in China, especially in GD. Consequently, the PCC best practices for hospitals remain unclear. 22 Therefore, this study aimed to investigate the inpatients’ perspectives on PCC and identify the influential role of sociodemographic variables on their perceived PCC levels in GD, China.
Methods
Study Design
A cross-sectional survey was conducted from November 2019 to January 2020 in nine tertiary-level hospitals across five central cities in GD. The target cities represent the province’s four economic regions. This ensured that the respondent sample was balanced and representative of the demographic characteristics of the sample area. The survey was conducted with a large sample of inpatients in GD to investigate their perceived issues with PCC (eg, problems in communication with medical professionals and medical expenditure) and identify the impact of inpatients’ sociodemographic status on their perception of PCC.
Setting
GD has the largest economy in China, with a population of approximately 113 million. In 2018, its gross domestic product (GDP) was 9727.8 billion RMB (US$ 1393.3 billion) and its gross health expenditure was 519.9 billion RMB (US$ 74.4 billion). 23 However, similar to the unbalanced development in different regions of China, the development levels in GD vary across regions. 24 For example, GDP per capita of the Pearl River Delta (PRD) region was US$ 18,928 in 2018, which was equivalent to that of upper-middle-income countries, and was over three times higher than that of the western and northern GD that remain extremely underdeveloped. 25 The PRD region is ranked the highest in development, followed by the western, eastern, and northern regions. 23 The per capita GDP of the PRD region was more than three times that of western GD in 2018. This variation in development among the regions indicates that considering samples from each region and the differences in their respective perspectives would be helpful for a better understanding of the status quo of PCC in China.
Sampling
We selected a total of nine tertiary-level hospitals (the highest level of hospital grading in China) from five central cities located across the four economic regions of GD. For each city, one to three of the largest and most comprehensive tertiary general hospitals were selected as investigation sites; this was done to ensure that the respondents were strongly representative of the area. The number of hospitals surveyed in each region was determined based on the number of permanent residents of that region. The target cities were Guangzhou (PRD, 3 hospitals selected), Shenzhen (PRD, 3 hospitals selected), Meizhou (east, 1 hospital selected), Shaoguan (north, 1 hospital selected), and Zhanjiang (west, 1 hospital selected).
The minimum sample size needed for this study was approximately 1,443, which was determined using a frequently used sample size calculator. 26 The key parameters used in the calculation are as follows: confidence level, 95%; confidence interval, 2.58; and population of GD, 113 million. The anticipated minimum sample sizes for each of the four regions (PRD, east, north, and west) were 807, 212, 212, and 212, respectively; these were determined based on the proportions of their respective permanent resident populations.
All inpatients present in the general wards of the target hospitals during the survey period were invited to participate in the survey anonymously. The inclusion criteria were as follows: (1) aged ≥18 years; (2) able to read and speak Mandarin; (3) no cognitive problems; and (4) able to provide informed consent.
Measurement
A self-developed PCC questionnaire was used to investigate the perception of PCC among the inpatients in GD. The questionnaire was developed based on a literature review, semi-structured focus group interviews, and expert consultation.
First, we conducted a literature review to ensure that the questionnaire contained the universal elements of classic PCC models applied worldwide, including those of the World Health Organization, 27 the Picker institute, 28 the King’s Fund, 29 and other existing models. Subsequently, we conducted semi-structured group interviews about PCC across five cities in GD. Focus group interviews were conducted with different stakeholders, which included 55 patients, 21 doctors, and 17 nurses, from orthopedics, rehabilitation medicine, endocrinology, oncology, geriatrics, and traditional Chinese medicine departments. After the interviews, domains and items of the PCC questionnaire were confirmed, and opinions of the three key participants in medical service were included in the questionnaire. Finally, expert consultation was conducted to ensure the content and face validity of the questionnaire.
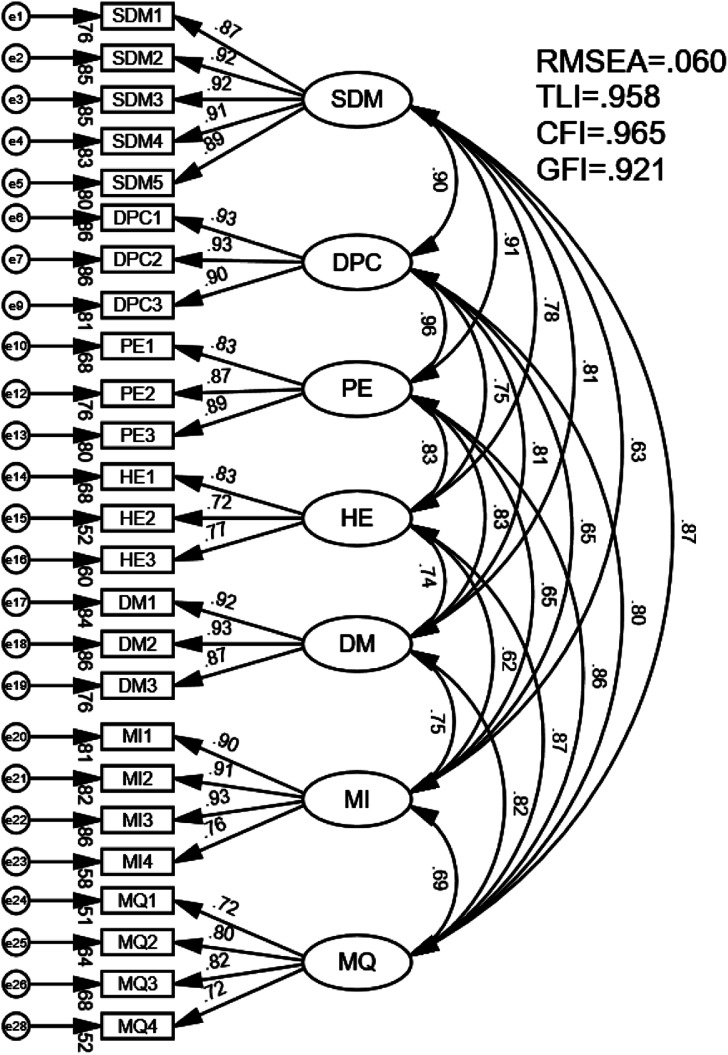
The final questionnaire comprised 25 items across seven domains of PCC (Table 1). Each item in the PCC questionnaire related to a specific patient concern, and scores were given on a scale ranging from 1 to 10, representing the worst to best levels of PCC, respectively. The total was then divided by 25 to obtain the overall mean score. The reliability test showed that the Cronbach’s α values of the overall PCC questionnaire and its seven domains were all above .750. Moreover, we used the Amos Graphics software to conduct confirmatory factor analysis (CFA) based on structural equation modeling to verify the questionnaire’s seven-domain structure (see Appendix A). CFA was performed to examine the structure of the PCC questionnaire. The model fit was determined by four indicators, root mean square error of approximation (RMSEA: .060, fair), the comparative fit index (CFI: .965, good), the Tucker–Lewis index (TLI: .958, good), and goodness of fit index (GFI: .921, good). 30 These tests indicate that the PCC questionnaire is a valid and reliable instrument.
Table 1.
The Seven Domains of the Patient-Centered Care Questionnaire and Their Definitions.
| Domains | Explanations |
|---|---|
| Shared decision-making | Patients and their family members and other relatives actively engage in decision-making, and all decision-making is centered on patients’ preferences, values, and needs |
| Doctor–patient communication | The doctor–patient partnership should feature a collaborative approach to addressing diseases, and doctors should provide understandable explanations of diseases and meet patients’ personalized needs in a timely and effective manner |
| Patient experience | This refers to patients’ perceptions of the medical treatment process, their degree of trust in the hardware- and software-related aspects of the medical institutions, and whether the patients perceive that they are receiving heartfelt care and comfort from medical professionals |
| Hospital environment | The medical institution’s environment is clean and has effective logistics that make the patient feel comfortable, and self-service is facilitated |
| Disease management | This variable relates to the provision of positive and professional health education covering hospitalization to discharge as well as severe chronic disease management to ensure that patients live healthier lives |
| Medical insurance | The reimbursement rate of medical insurance is perceived as reasonable and equal for all patients, self-paid medical expenses can be effectively reduced, and the reimbursement scope and proportion of expensive yet necessary drugs can be improved |
| Medical quality | Treatment results conform to patients’ expectations, hospitals’ internal departments are integrated well, and all examinations are performed based on sufficient evidence |
Data Collection
To ensure a consistent level of quality regarding data collection, an investigation team comprising six recruited research assistants was formed to conduct the fieldwork for the face-to-face inpatient survey. All the field-investigation team members were provided prior specialized training in administering the questionnaires and communicating with patients. The investigators, assisted by local medical professionals, visited the wards of the target hospitals and distributed paper-based questionnaires to inpatients. Participants were asked to rate the items based on their own experience of medical service access. The investigators assured inpatients that the questionnaire would not have any impact on their use of medical services. All participants provided verbal informed consent prior to participation. This study was conducted in accordance with the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee.
Statistical Analysis
Descriptive statistics, analysis of variance (ANOVA), and linear regression models were employed to analyze the data. We described inpatients’ sociodemographic characteristics using counts and proportions. Different groups were created based on sociodemographic information, and PCC scores were calculated for each group. The scores for different groups were compared using an ANOVA test. Multivariable regression models were then used to explore the influence of sociodemographic characteristics on PCC and its seven domains.
For the grouping of sociodemographic characteristics, we adopted both common and official grouping methods. For example, groups of economic regions were determined using the official Guangdong Statistical Yearbook. “Hukou” referred to whether the respondents’ permanent address was in a rural or urban area. Medical insurance was divided into 4 groups: (1) medical insurance for urban employees (public medical insurance for people living in urban areas and employed by companies or organizations); (2) medical insurance for urban residents (public medical insurance for people living in urban areas and not employed by any company or organization); (3) people covered by the New Rural Cooperative Medical System (NCMS); and (4) other (people with no public medical insurance). We divided income level into three groups: “average” represented the middle-income range defined in the 2019 Guangdong Statistical Yearbook; “below average” represented incomes below this range; and “above average” represented incomes above this range. SPSS software was used to perform the data analyses, and P-values less than .05 were considered to indicate significance.
Results
A total of 2028 inpatients completed the questionnaire. Of these, responses from 165 were excluded because of missing information regarding sociodemographic characteristics or items from the PCC questionnaire. Consequently, 1863 valid questionnaires were included in the analysis. Of these 1863 valid responses, 1,066, 434, 151, and 212 were collected from the PRD, eastern, western, and northern areas of GD, respectively. All of these exceeded the respective minimum sample sizes for the regions and were consistent with the proportion of permanent resident populations in each region.
Descriptive statistics regarding the sociodemographic characteristics of the survey sample and a comparison of their respective mean scores are presented in Table 2. In this study, 48.36% of the respondents were male, while 51.64% were female; respondents’ average age was 49.01 years; 35.80% had received college education; 50.08% lived in rural areas; and 57.22% lived in Guangzhou and Shenzhen in the PRD, which matched the proportion of permanent residents in the PRD when compared to the rest of GD. The survey also obtained information on the number of hospitalizations, income, and medical insurance.
Table 2.
Sociodemographic Characteristics of the Respondents and Comparison of Mean PCC Scores.
| PCC | ||||||
|---|---|---|---|---|---|---|
| Groups | N = 1863 | %=100 | Mean | SD | F-Value | P-value |
| Age (mean, SD) | (49.01, 16.73) | |||||
| Gender | ||||||
| Male | 901 | 48.36 | 8.60 | 1.30 | 4.83 | .51 |
| Female | 962 | 51.64 | 8.56 | 1.42 | ||
| Education level | ||||||
| Primary school | 379 | 20.34 | 8.65 | 1.38 | 1.42 | .24 |
| Middle school | 817 | 43.85 | 8.60 | 1.40 | ||
| College | 667 | 35.80 | 8.51 | 1.31 | ||
| Hukou a | ||||||
| Rural | 933 | 50.08 | 8.61 | 1.32 | 3.26 | .36 |
| Urban | 930 | 49.92 | 8.55 | 1.41 | ||
| Region b | ||||||
| PRD | 1066 | 57.22 | 8.64 | 1.27 | 18.65 | <.001 |
| Eastern | 434 | 23.30 | 8.75 | 1.32 | ||
| Western | 151 | 8.11 | 7.85 | 1.76 | ||
| Northern | 212 | 11.38 | 8.43 | 1.41 | ||
| Number of hospitalizations | ||||||
| First time | 616 | 33.06 | 8.58 | 1.35 | 4.91 | .01 |
| 2-3 times | 816 | 43.80 | 8.49 | 1.39 | ||
| >3 times | 431 | 23.13 | 8.74 | 1.31 | ||
| Medical insurance c | ||||||
| Urban employee | 659 | 35.37 | 8.54 | 1.34 | 1.14 | .33 |
| Urban resident | 546 | 29.31 | 8.52 | 1.42 | ||
| NCMS | 502 | 26.95 | 8.66 | 1.29 | ||
| Other | 156 | 8.37 | 8.64 | 1.48 | ||
| Income level d | ||||||
| Below average | 643 | 34.51 | 8.55 | 1.48 | .48 | .62 |
| Average | 510 | 27.38 | 8.55 | 1.31 | ||
| Above average | 710 | 38.11 | 8.62 | 1.29 | ||
| Severity of disease | ||||||
| Very serious | 414 | 22.22 | 8.64 | 1.37 | 1.48 | .22 |
| Serious | 389 | 20.88 | 8.45 | 1.48 | ||
| Not very serious | 517 | 27.75 | 8.58 | 1.22 | ||
| Not serious | 543 | 29.15 | 8.61 | 1.40 | ||
aHukou: Location of the respondent’s permanent residence.
bRegion: The method for distinguishing the economic regions in Guangdong Province was based on the official approach applied in the Guangdong Statistical Yearbook. The ranking of the regions in terms of per capita gross domestic product is Pearl River Delta (PRD)>western>eastern>northern.
cMedical insurance: (1) Public insurance for urban employee: people living in urban areas who are employed by companies or organizations; (2) Public insurance for urban resident: people living in urban areas who are not employed by any company or organization; (3) NCMS: people covered by the New Rural Cooperative Medical System; (4) other: people with no public medical insurance.
dIncome level: “Average” represents the middle-income range of residents as defined by the “2019 Guangdong Statistical Yearbook.” “Below average” indicates incomes below this range, and “above average” indicates incomes higher than this range.
PCC: patient-centered care; SD: standard deviation.
The overall mean PCC score was 8.58 (standard deviation = 1.36). Significant differences in scores were found between the economic regions and based on the number of hospitalizations (P < .05). Comparisons using the least-significant difference revealed that the overall PCC scores for PRD and eastern GD were higher than those of western and northern GD (P < .05). Moreover, inpatients with more than 3 hospitalizations scored higher than those with 2 or 3 hospitalizations and first-time inpatients (P < .05).
To further examine the specific sources of the overall PCC scores, we calculated the scores for each of the 25 items and 7 domains. Table 3 shows the scores for the 25 PCC sub-items along with descriptions of the focus of each item. Mean scores of all the 25 items exceeded 7. PE1 (first item of patient experience), representing “attitude of the medical professionals,” received the highest score, with a mean of 9.07, whereas MI3 (third item of medical insurance), representing “fairness of reimbursement policy,” received the lowest score, with a mean of 7.74. Items with high scores were concentrated in the patient experience domain, while items with low scores were concentrated in the medical insurance domain. Items with low scores tended to be accompanied by a high coefficient of variation. The scores for the 7 domains are shown in Table 4; the results showed that the patient experience domain (8.96) was rated the highest, whereas the medical insurance domain (7.93) was rated the lowest.
Table 3.
Scores for the 25 Individual Items of the PCC Questionnaire.
| Domains | No | Item | Mean | SD | CV, % |
|---|---|---|---|---|---|
| SDM | SDM1 | HCW provides alternative choices | 8.61 | 1.74 | 20.25 |
| SDM2 | HCW listens to the patient | 8.77 | 1.63 | 18.61 | |
| SDM3 | HCW adheres to the patient’s preferences | 8.84 | 1.56 | 17.69 | |
| SDM4 | The patient and HCW discuss the disease together | 8.80 | 1.65 | 18.79 | |
| SDM5 | HCW understands the patient’s needs | 8.75 | 1.69 | 19.28 | |
| DPC | DPC1 | HCW fully communicates information regarding the illness | 8.80 | 1.60 | 18.15 |
| DPC2 | HCW provides an understandable explanation of the illness | 8.88 | 1.54 | 17.35 | |
| DPC3 | HCW effectively responds to the patient’s needs | 8.92 | 1.54 | 17.26 | |
| PE | PE1 | Attitude of the medical professionals | 9.07 | 1.42 | 15.63 |
| PE2 | Patients’ confidence in the medical technology | 9.01 | 1.37 | 15.18 | |
| PE3 | HCWs emotionally comfort the patient | 8.79 | 1.61 | 18.30 | |
| HE | HE1 | Comfortable environment | 8.57 | 1.65 | 19.26 |
| HE2 | Good logistics support | 7.97 | 2.15 | 27.03 | |
| HE3 | Convenient self-service | 8.96 | 1.43 | 16.00 | |
| DM | DM1 | Positive health education | 8.30 | 1.87 | 22.57 |
| DM2 | Efficient health education | 8.49 | 1.74 | 20.49 | |
| DM3 | Disease management after discharge | 8.72 | 1.64 | 18.86 | |
| MI | MI1 | Reasonable medical reimbursement | 7.93 | 2.25 | 28.40 |
| MI2 | Reasonable self-pay level | 8.08 | 2.10 | 25.99 | |
| MI3 | Fair reimbursement policy | 7.95 | 2.26 | 28.45 | |
| MI4 | Reimbursement of expensive but necessary drugs | 7.74 | 2.47 | 31.90 | |
| MQ | MQ1 | Stable supply of drugs | 8.96 | 1.58 | 17.64 |
| MQ2 | Evidence-based medical examination | 8.52 | 1.81 | 21.19 | |
| MQ3 | Good medical results | 8.54 | 1.61 | 18.88 | |
| MQ4 | Highly efficient medical process | 8.42 | 1.91 | 22.62 |
PCC: Patient-centered care; SD: Standard deviation; CV: coefficient of variation; SDM: Shared decision-making; DPC: Doctor–patient communication; PE: Patient experience; HE: Hospital environment; DM: Disease management; MI: Medical insurance; MQ: Medical quality; HCW: Healthcare worker
Table 4.
Overall PCC Score and Scores for its Seven Domains.
| Domains | Mean | SD | CV, % |
|---|---|---|---|
| SDM | 8.76 | 1.53 | 17.44 |
| DPC | 8.87 | 1.48 | 16.63 |
| PE | 8.96 | 1.34 | 14.91 |
| HE | 8.50 | 1.50 | 17.63 |
| DM | 8.50 | 1.64 | 19.30 |
| MI | 7.93 | 2.05 | 25.91 |
| MQ | 8.61 | 1.43 | 16.61 |
| PCC (overall) | 8.58 | 1.36 | 15.90 |
The maximum score for each domain was 10. PCC: Patient-centered care; SD: Standard deviation; CV: Coefficient of variation; SDM: Shared decision-making; DPC: Doctor–patient communication; PE: Patient experience; HE: Hospital environment; DM: Disease management; MI: Medical insurance; MQ: Medical quality
To further examine the factors affecting inpatients’ perception level of PCC, we constructed a multivariable linear regression model. This model considers PCC and its 7 domains as dependent variables. The independent variables of this model were education level, Hukou, economic region, medical insurance, income level, severity of disease, and number of hospitalizations. The results indicated that inpatients covered by the NCMS had higher overall PCC scores. Moreover, inpatients from western and northern GD had lower overall PCC scores than that of PRD and eastern GD (P < .001). Furthermore, inpatients living in rural areas and those with a “serious” disease tended to rate most of the PCC domains lower (P < .05). Additionally, inpatients who had more hospitalizations tended to rate most of the PCC domains higher (P < .05). Finally, college-educated inpatients scored lower in the domain of disease management (P = .03), while high-income inpatients scored higher in the domain of medical insurance (P = .001). More details are shown in Table 5. The regression models showed that gender, age, and chronic disease had no significant effect on PCC scores (P > .05), whereas Hukou, region, medical insurance, income level, severity of disease, and number of hospitalizations had significant effects on PCC scores (P < .05).
Table 5.
Sociodemographic Characteristics Associated With Mean Scores for PCC and its Domains.
| Overall | SDM | DPC | PE | |||||
|---|---|---|---|---|---|---|---|---|
| Model | β(95% CI) | P-value | β(95% CI) | P-value | β(95% CI) | P-value | β(95% CI) | P-value |
| Education | ||||||||
| Primary and below | Ref | Ref | Ref | Ref | ||||
| Middle school | −.06 (−.24.0.11) | .464 | −.04 (−.24.0.16) | .696 | −.04 (−.23.0.15) | .654 | .01 (−.16.0.18) | .898 |
| College | −.16 (−.38.0.05) | .139 | −.11 (−.35.0.14) | .385 | −.12 (−.36.0.12) | .319 | −.05 (−.26.0.16) | .642 |
| Hukou | ||||||||
| Urban | Ref | Ref | Ref | Ref | ||||
| Rural | −.17 (−.33,−.01) | .041 | −.17 (−.35.0.01) | .062 | −.13 (−.30.0.05) | .159 | −.19 (−.35,−.03) | .018 |
| Region | ||||||||
| PRD | Ref | Ref | Ref | Ref | ||||
| Eastern | .12 (−.05.0.28) | .170 | .17 (−.01.0.36) | .069 | .20 (.02.0.38) | .028 | .15 (−.02.0.31) | .082 |
| Western | −.74 (−.98,−.51) | <.001 | −.49 (−.76,−.23) | <.001 | −.42 (−.68,−.16) | .001 | −.42 (−.65,−.19) | <.001 |
| Northern | −.19 (−.39.0.02) | .071 | −.14 (−.37.0.09) | .244 | −.09 (−.31.0.13) | .423 | −.17 (−.37.0.03) | .088 |
| Medical insurance | ||||||||
| Urban employee | Ref | Ref | Ref | Ref | ||||
| Urban resident | .04 (−.12.0.21) | .609 | .00 (−.18.0.19) | .960 | .06 (−.12.0.24) | .543 | .00 (−.16.0.16) | .980 |
| NCMS | .21 (.01.0.42) | .040 | .24 (.01.0.46) | .044 | .29 (.07.0.51) | .009 | .29 (.09.0.49) | .004 |
| Others | .14 (−.09.0.38) | .237 | .15 (−.11.0.42) | .260 | .22 (−.04.0.48) | .102 | .16 (−.08.0.39) | .190 |
| Income level | ||||||||
| Below average | Ref | Ref | Ref | Ref | ||||
| Average | .08 (−.09.0.25) | .356 | .11 (−.08.0.30) | .264 | .19 (.00.0.37) | .048 | .12 (−.05.0.28) | .172 |
| Above average | .14 (−.05.0.32) | .142 | .07 (−.14.0.28) | .506 | .14 (−.06.0.34) | .161 | .08 (−.10.0.26) | .375 |
| Severity of disease | ||||||||
| Very serious | Ref | Ref | Ref | Ref | ||||
| Serious | −.19 (−.38.0.00) | .050 | −.25 (−.46,−.03) | .023 | −.33 (−.53,−.12) | .002 | −.25 (−.43,−.06) | .009 |
| Not very serious | −.05 (−.23.0.13) | .582 | −.17 (−.38.0.03) | .096 | −.14 (−.34.0.05) | .153 | −.11 (−.29.0.07) | .220 |
| Not serious | .00 (−.18.0.18) | .993 | −.11 (−.31.0.10) | .315 | −.12 (−.32.0.08) | .245 | −.03 (−.21.0.15) | .746 |
| Number of hospitalizations | .04 (.01.0.07) | .008 | .05 (.02.0.09) | .003 | .04 (.01.0.08) | .012 | .04 (.01.0.07) | .007 |
PCC: Patient-centered care; CI: Confidence interval; HE: Hospital environment; DM: Disease management; MI: Medical insurance; MQ: Medical quality; Hukou: Location of the respondent’s permanent residence; PRD: Pearl River Delta; NCMS: New Rural Cooperative Medical System. SDM: Shared decision-making; DPC: Doctor–patient communication; PE: Patient experience.
Discussion
This study was the first to provide insights into the perceived levels of PCC among inpatients in China. In general, we found that inpatients reported high satisfaction with PCC during their hospitalization. To make medical services more patient-friendly in recent years, the Chinese government developed ambitious programs, such as the “Action Plan for Further Improvement of Health Services 2018–2020” 31 As a result, hospitals in GD have made great efforts to provide high-quality medical services to improve patients’ experiences of using public healthcare services. Our study was the first to assess the efficiency and effectiveness of these policies and confirmed that the quality of medical services has improved inpatients’ perception of PCC considerably.
Among the domains of the PCC questionnaire, the medical insurance domain was rated the lowest by the inpatients in this study. This suggests that, even though satisfaction improved, inpatients still experienced issues related to certain basic components of the healthcare system, such as unfair reimbursement policies from public medical insurance systems and limited breadth and depth of reimbursement. 32 For example, some frequently used drugs were not covered by the medical insurance, and the reimbursement rate of some expensive drugs was also very low. 33 This dissatisfaction with medical insurance indicates that inpatients' perceived disease burden requires further improvement.
Inpatients, who came from western GD, an economically developed region, reported a lower PCC level of than those from eastern GD, which is an economically under-developed region. As such, economic development levels may not be the primary factor affecting inpatients’ perception of PCC, but rather the relative extent of government investment in the medical system and the patients’ perceived level of medical technology. 34 To address this, the relative extent of government investment in hospitals to improve the medical system plays a key role in the improvement of inpatients' perception of PCC. Furthermore, this study found that the higher the number of hospitalizations experienced by patients, the higher their PCC scores. There is no research on the relationship between number of hospitalizations and patients’ PCC scores; this may be because patients reporting more hospitalizations show greater understanding and tolerance to medical staff. However, the specific reasons need to be confirmed by further empirical studies.
This study found that inpatients from rural areas got a lower PCC mean score compared with those from urban areas. Although the China General Office of the State Council issued guidelines on promoting the development of a hierarchical medical system in 2015, 35 in this study, 51.02% (n = 476) of the rural inpatients who rated their health status as “not very serious” also reported visiting tertiary-level hospitals. The main reasons for this phenomenon may be the low quality of and patients distrust in doctors' skills at rural healthcare facilities, which led to wastage of time, and higher costs.36,37 Therefore, additional resources need to be invested to improve the doctors’ skills in rural medical institutions. Conversely, inpatients covered by the NCMS scored PCC higher than those covered by the public medical insurance for urban employees. However, rural patients can only avail the NCMS, which covers permanent rural residents, and its overall financing and reimbursement levels are lower than those covered by public urban medical insurance. This unusual finding indicates two things. First, in recent years, GD has invested considerable resources into improving its primary healthcare system, especially in rural areas. 38 Nevertheless, compared to urban patients, lower overall PCC scores indicated that rural inpatients have greater dissatisfaction with medical services. Second, compared to the medical insurance schemes for urban patients, in recent years, the Chinese government has increased the reimbursement rate for patients who are covered by the NCMS 39 ; thus, rural residents’ disease burden has been significantly reduced. 40 This key development strategy has greatly improved rural patients’ expectations, as stated by most participants in our study, who reported that they can access medical services more conveniently and at affordable rates.
In this study, a self-developed questionnaire was used to measure the PCC, which provided empirical evidence to assess the quality of healthcare services from Chinese patients’ perspective. As we know, currently, there is no instrument that assesses PCC, developed for the Chinese context.35,41 All the existing PCC-related instruments have been developed in the context of Western healthcare systems; their validity and reliability have never been assessed in the Chinese population, and thus, their findings may not be generalizable to the Chinese context. In this study, the PCC questionnaire was developed based on a rigid process in the context of GD, one of the most populous regions in China, while also considering the socioeconomic disparities within the province. More importantly, this study directly investigated the patients’ perspective on PCC’ thus, providing novel insights for future PCC studies and enriching the existing knowledge on PCC in China. However, despite the psychometric properties of the questionnaire being satisfactory, its performance needs further assessment in the other regions of the country.
Despite these significant contributions, several limitations need to be addressed. First, this was a cross-sectional study; thus, no causal relationships between sociodemographic characteristics and PCC could be established. In future studies, longitudinal data should be collected and analyzed. Second, items and mean scores showed ceiling effects to some extent, which is a common problem in patient experience and outcome measures. Some inpatients in this study may not have been completely convinced by our repeated assurances that their responses to the survey will not affect their access to medical services; thus, it is possible that some participants may have scored some items too high. In the future, researchers should take effective steps to control the ceiling effect of patient scores. Third, inpatients living in rural areas tended to report a poor PCC; however, since all the inpatients investigated in this study were selected from hospitals in big cities, their ratings may be less comprehensive in terms of the primary healthcare system. Therefore, further research should be conducted in primary healthcare institutions.
Conclusion
This study provided a comprehensive overview of inpatients' perceptions of PCC in tertiary-level hospitals in GD, China, and found that inpatients reported high satisfaction with PCC during their hospitalization. Inpatients from rural areas perceived a lower level of PCC compared to those from urban areas, whereas inpatients covered under the NCMS reported higher PCC score than those under the public medical insurance for urban employees. Moreover, inpatients in western GD reported a lower PCC score than those in eastern GD. Heterogeneity in PCC between different sociodemographic status groups indicates that, despite a high level of PCC reported by inpatients in this study, some fundamental issues regarding PCC are need to be improved.
Appendix 1.
Figure A1.
Confirmatory factor analysis based on the structural equation model of the patient-centered care questionnaire. PCC: Patient-centered care; SDM: Shared decision-making DPC: Doctor–patient communication; PE: Patient experience; HE: Hospital environment; DM: disease management; MI: medical insurance; MQ: medical quality; RMSEA: root mean square error of approximation; TLI: Tucker–Lewis index; CFI: Comparative fit index; GFI: Goodness of fit index.
TableA1.
Reliability Test of the PCC Questionnaire and its Seven Domains
| Domains | PCC | DPC | SDM | PE | HE | DM | MI | MQ |
|---|---|---|---|---|---|---|---|---|
| Value of Cronbach’s α | .971 | .941 | .956 | .895 | .800 | .928 | .924 | .845 |
PCC: Patient-centered care; DPC: Doctor–patient communication; SDM: Shared decision-making PE: Patient experience; HE: Hospital environment; DM: Disease management; MI: Medical insurance; MQ: Medical quality.
Footnotes
Author Contributions: Conceptualization: DW; Methodology: LZ and RX; data collection: LZ, YX, and JC; statistical analysis: LZ; Writing—Review and Editing: LZ and RX. All authors have read and agreed to the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the “Guangdong Basic and Applied Basic Research Foundation (2021A1515011973); a grant from Philosophy and Social Sciences of Guangdong College for the project of “Public Health Policy Research and Evaluation” Key Laboratory (2015WSYS0010), The Natural Science Foundation of Guangdong Province, and Public Health Service System Construction Research Foundation of Guangzhou, China.
Ethical Approval: The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Second Affiliated Hospital of Guangzhou Medical University (Project identification code: 2019-ks-28).
Data Availability: The data might be achieved by contacting the correspondence author.
ORCID iD
Ling-ming Zhou https://orcid.org/0000-0002-0989-2071
References
- 1.Bergeson SC, Dean JD. A systems approach to patient-centered care. J Am Med Assoc. 2006;296(23):2848-2851. doi: 10.1001/jama.296.23.2848 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Framework on Integrated, people-centred health services[EB/OL]. (2016-4-15)[2020-9-20]. http://www.who.int/servicedeliverysafety/areas/people-centred-care/en/ [Google Scholar]
- 3.Scholl I, Zill JM, Härter M, Dirmaier J. An integrative model of patient-centeredness - a systematic review and concept analysis. PLoS One. 2014;9(9):e107828. doi: 10.1371/journal.pone.0107828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greene SM, Tuzzio L, Cherkin D. A framework for making patient-centered care front and center. Perm J. 2012;16(3):49-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vennedey V, Hower KI, Hillen H, Ansmann L, Kuntz L, Stock S. Patients’ perspectives of facilitators and barriers to patient-centred care: insights from qualitative patient interviews. BMJ Open. 2020;10(5):e033449. doi: 10.1136/bmjopen-2019-033449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brickley B, Sladdin I, Williams LT, et al. A new model of patient-centred care for general practitioners: results of an integrative review. Fam Pract. 2020;37(2):154-172. doi: 10.1093/fampra/cmz063. [DOI] [PubMed] [Google Scholar]
- 7.Raja S, Hasnain M, Vadakumchery T, Hamad J, Shah R, Hoersch M. Identifying elements of patient-centered care in underserved populations: a qualitative study of patient perspectives. PLoS One. 2015;10(5):e0126708. doi: 10.1371/journal.pone.0126708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sultan WIM, Sultan MIM, Crispim J. Palestinian doctors’ views on patient-centered care in hospitals. BMC Health Serv Res. 2018;18(1):766. doi: 10.1186/s12913-018-3573-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiorio CV, Gorli M, Verzillo S. Evaluating organizational change in health care: the patient-centered hospital model. BMC Health Serv Res. 2018;18(1):95. doi: 10.1186/s12913-018-2877-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein RM, Street RL, Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103. doi: 10.1370/afm.1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luxford K, Safran DG, Delbanco T. Promoting patient-centered care: a qualitative study of facilitators and barriers in healthcare organizations with a reputation for improving the patient experience. Int J Qual Health Care. 2011;23(5):510-515. doi: 10.1093/intqhc/mzr024 [DOI] [PubMed] [Google Scholar]
- 12.van Dulmen SA, Lukersmith S, Muxlow J, Santa Mina E, Nijhuis-van der Sanden MWG, van der Wees PJ. Supporting a person-centred approach in clinical guidelines. a position paper of the allied health community - guidelines international network (G-I-N). Health Expect. 2015;18(5):1543-1558. doi: 10.1111/hex.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blumenthal D, Hsiao W. Lessons from the East - China’s rapidly evolving health care system. N Engl J Med. 2015;372(14):1281-1285. doi: 10.1056/NEJMp1410425 [DOI] [PubMed] [Google Scholar]
- 14.Xu W, Zhang F, Zeng B, Yang T, Wang H. Spatial access to medical services in the underdeveloped region of northwestern china: a case study in lanzhou city. Sustainability. 2019;11(23):6786. [Google Scholar]
- 15.Luo D, Du J, Wang P, Yang W. Urban‐rural comparisons in health risk factor, health status and outcomes in Tianjin, China: a cross‐sectional survey (2009‐2013). Aust J Rural Health. 2019;27(6):535-541. doi: 10.1111/ajr.12562 [DOI] [PubMed] [Google Scholar]
- 16.National Bureau of Statistics . Annual Statistics Data of China[EB/OL; 2019. https://data.stats.gov.cn/easyquery.htm?cn=A01 [Google Scholar]
- 17.Su M, Zhang Q, Lu J, et al. Protocol for a nationwide survey of primary health care in China: the China PEACE (patient-centered evaluative assessment of cardiac events) mpp (million persons project) primary health care survey. BMJ Open. 2017;7(8):e016195. doi: 10.1136/bmjopen-2017-016195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.OECD . Caring for Quality in Health: Lessons Learnt from 15 Reviews of Health Care quality[EB/OL; 2017. http://www.oecd.org/els/health-systems/Caring-for-Quality-in-Health-Final-report.pdf [Google Scholar]
- 19.Sun J, Hu G, Ma J, et al. Consumer satisfaction with tertiary healthcare in China: findings from the 2015 China national patient survey. Int J Qual Health Care. 2017;29(2):213-221. doi: 10.1093/intqhc/mzw160 [DOI] [PubMed] [Google Scholar]
- 20.Ree E, Wiig S, Manser T, Storm M. How is patient involvement measured in patient centeredness scales for health professionals? A systematic review of their measurement properties and content. BMC Health Serv Res. 2019;19(1):12. doi: 10.1186/s12913-018-3798-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou H, Bai G, Gao J, et al. The development of indicator measure for monitoring the quality of patient-centered care in China’s tertiary hospitals. PLoS One. 2018;13(10):e0205489 . doi: 10.1371/journal.pone.0205489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu G, Chen Y, Liu Q, et al. Patient experience of hospital care in China: major findings from the Chinese patient experience questionnaire survey (2016-2018). BMJ Open. 2019;9(9):e03161. doi: 10.1136/bmjopen-2019-031615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Statistics Bureau of Guangdong Province . Statistical Yearbook of Guangdong[M]. China: Statistics Press, 2018. [Google Scholar]
- 24.People’s Government of Guangdong Province . Briefing on Health Resources and Medical Services of Guangdong Province in 2019 [EB/OL]. (2020). http://www.gd.gov.cn/zwgk/sjfb/sjfx/content/post_3017297.html [Google Scholar]
- 25.Woo J, Kwok T, Sze F, Yuan H. Ageing in China: health and social consequences and responses. Int J Epidemiol. 2002;31(4):772-775. doi: 10.1093/ije/31.4.772 [DOI] [PubMed] [Google Scholar]
- 26.Viechtbauer W, Smits L, Kotz D, et al. A simple formula for the calculation of sample size in pilot studies. J Clin Epidemiol. 2015;68(11):1375-1379. doi: 10.1016/j.jclinepi.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization . People-Centred Health Care: A Policy Framework[EB/OL; 2007. -9-13)[2020-9-25] https://iris.wpro.who.int/bitstream/handle/10665.1/5420/9789290613176_eng.pdf [Google Scholar]
- 28.Picker Institute . Eight Dimensions of Patient-Centred Care[EB/OL; 2015. -5-15)[2020-7-8] https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ [Google Scholar]
- 29.The King’s Fund . How to Deliver High-Quality, Patient-Centred, Cost-Effective care[EB/OL]; 2010. http://kingsfund.org.uk/sites/files/kf/how-to-deliver-high-quality-patient-centred-cost-effective-care-16-september-2010-kings-fund.pdf [Google Scholar]
- 30.Hu Lt., Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model: A Multidisciplinary J. 1999;6(1):1-55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- 31.Action Plan for Further Improvement of Health Services 2018-2020 [EB/OL].(2010). Available: http://www.gov.cn/gongbao/content/2018/content_5299607.htm [Google Scholar]
- 32.Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192-1204. doi: 10.1016/S0140-6736(19)32136-1 [DOI] [PubMed] [Google Scholar]
- 33.Diao Y, Qian J, Liu Y, et al. How government insurance coverage changed the utilization and affordability of expensive targeted anti-cancer medicines in China: an interrupted time-series study. Journal of Global Health. 2019;9(2):020702. doi: 10.7189/jogh.09.020702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang X, Sun X, Birch S, et al. People-centred integrated care in urban China. Bull World Health Organ. 2018;96(12):843-852. doi: 10.2471/BLT.18.214908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu X, Hou Z, Towne SD, Jr, et al. Knowledge, attitudes, and practices related to the establishment of the national hierarchical medical system (NHMS) among outpatients in Chinese tertiary hospitals. Medicine. 2018;97(35):e11836. doi: 10.1097/MD.0000000000011836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yuan B, Jian W, He L, Wang B, Balabanova D. The role of health system governance in strengthening the rural health insurance system in China. Int J Equity Health. 2017;16(1):44. doi: 10.1186/s12939-017-0542-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hu D, Zhu W, Fu Y, et al. Development of village doctors in China: financial compensation and health system support. Int J Equity Health. 2017;16(1):9. doi: 10.1186/s12939-016-0505-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen Y, Yin Z, Xie Q. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. Int J Equity Health. 2014;13:34. doi: 10.1186/1475-9276-13-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu H, Dai W. An empirical study on the benefits equity of the medical security policy: the China health and nutrition survey (CHNS). Int J Environ Res Publ Health. 2020;17(4):1203. doi: 10.3390/ijerph17041203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ta Y, Zhu Y, Fu H. Trends in access to health services, financial protection and satisfaction between 2010 and 2016: has China achieved the goals of its health system reform? Soc Sci Med. 2020;245:112715. doi: 10.1016/j.socscimed.2019.112715 [DOI] [PubMed] [Google Scholar]
- 41.Hu L, Zhou BP, Liu S, Wang Z, Liu Y. Outpatient satisfaction with tertiary hospitals in china: the role of sociodemographic characteristics. Int J Environ Res Publ Health. 2019;16(19):3518. doi: 10.3390/ijerph16193518 [DOI] [PMC free article] [PubMed] [Google Scholar]