Abbreviations
- ADRD
Average Daily Red Cell Demand
- CBS
Canadian Blood Services
- DoH
Days on Hand
- IVIG
intravenous immune globulin
- NAC
National Advisory Committee on Blood and Blood Products
- NEBMC
National Emergency Blood Management Committee
- PEBMC
Provincial Emergency Blood Management Committee
- PPRP
plasma protein and related products
- P/T
provincial and territorial
- RBC
red blood cell
1. INTRODUCTION
Security of supply is a priority for the blood system and must include consideration of inventory held by the manufacturer and held and utilized by hospital transfusion laboratories. 1 Blood shortage planning is an essential aspect of this system, to ensure preparedness for handling emergent and unexpected periods of inventory instability, and to mitigate against potentially associated adverse health consequences. 2 Disaster preparedness plans that include consideration of blood shortages should be developed in times of good supply and be available for implementation during periods of supply concern or constraint. 3 , 4
In Canada, we benefit from a well‐defined construct between three key elements of our blood system: the manufacturer, the provincial governments, and the hospitals. In this article, we use red blood cell (RBC) data as an illustrator to summarize our experience of national blood supply and demand‐associated challenges with inventory management in Canada (exclusive of Quebec) during the initial 6 months of the COVID‐19 pandemic and highlight the benefits of operating within such an effective framework.
2. THE CANADIAN BLOOD SYSTEM
There are two blood operators in Canada responsible for collecting blood from voluntary donors, manufacturing blood components, and managing the supply and distribution of blood components and plasma protein and related products (PPRP) to hospitals within their respective jurisdictions. Canadian Blood Services (CBS) serves all provinces and territories except Quebec, which is served by Héma‐Québec. These nonprofit organizations are funded by the Ministries of Health of provinces and territories they serve. Although they do not routinely share inventory, they are able to do so if needed.
In the fiscal year 2019/2020, CBS distributed over 700,000 RBC units, 166,000 platelet doses, 105,000 transfusable plasma doses, and almost 50,000 units of cryoprecipitate; a further 500,000 units of plasma were collected and sent for fractionation. These products were donated by over 400,000 volunteer donors across the country. Pre‐pandemic, approximately 60% of donations were collected at fixed donor centers located in large urban areas across the county, with the remainder collected at mobile sites. CBS issued 23.8 RBC units and 4 platelet units per 1000 population to hospitals in 2019. National weekly RBC issues average 14,000–15,000 units, with notable variation in regional practice.
CBS collection plans are informed by future demand projections leveraging historical data of blood components issued to hospitals. In times of usual operations, system‐wide demand has been relatively stable and is a reliable predictor of future hospital demand. An established electronic inventory reporting structure enables routinely weekly reports of hospital RBC and platelet inventory to CBS, providing “a snapshot” of the entire national inventory in the country for these two blood components. This combined blood operator and hospital inventory data, allowing CBS to detect signals of potential supply challenges. In addition, CBS routinely consults with the hospital transfusion medicine community and with members of the National Advisory Committee on Blood and Blood Products (NAC) to understand system‐wide patterns of demand. The NAC is a standing interprovincial technical committee that acts as an advisory group to CBS and the provincial and territorial (P/T) Ministries of Health.
3. NATIONAL BLOOD SHORTAGES PLANNING
Blood supply may be compromised by external threats including natural or man‐made disasters, which could be local, regional, or national in their scope. Drops in demand due to catastrophic events may be regional in nature and lead to mobilization of supply to the remaining intact blood system. Over a decade ago, the NAC recognized the need for an effective and equitable response to any actual or potential crisis, which could impact the blood supply. This led to the development of the Canadian National Plan for Shortages of Labile Blood Components 4 (the Plan) in 2009. The sentinel implementation element of the Plan is the potential to convene the National Emergency Blood Management Committee (NEBMC), a congress of approximately 50 people, consisting of NAC members, provincial and territorial government official, and leadership from CBS medical, supply chain, and government relations groups (see Appendix S1 for the NEBMC Terms of Reference).
In times of blood inventory constraint, the NEBMC determines if the declaration of an inventory shortage phase is required (Table 1), recommends actions necessary to mitigate inventory challenges, and coordinates communications to be disseminated to hospital laboratory and clinical stakeholders. The Plan provides a framework for blood supply management during a nationwide shortage to ensure a consistent and collaborative mechanism through coordinated, open discussion. It is an expectation that P/T Ministries of Health and their regional jurisdictions will develop jurisdictional blood shortage management plans in alignment with the Plan.
TABLE 1.
Inventory shortage phases as defined in the Canadian National Plan for Shortages of Labile Blood Components (the Plan)
| Phase | Description |
|---|---|
| Green | Normal blood component inventory levels exist and supply general meets demand |
| Green Advisory | Persistent limited blood component supply, which may serve as a warning of imminent shortage risk, prompting review of hospital inventory levels and enhanced national visibility of hospital inventory serving as a signal for hospitals and provinces to implement any potential conservation strategies to help avoid a shortage |
| Amber | National blood inventory is insufficient to continue with routine transfusion practices, and implementation of specific measures is required to reduce blood usage |
| Red | Blood inventory levels are insufficient to ensure patients with non‐elective indications will receive transfusion |
| Recovery | Blood component inventories have begun to increase and are expected to be maintained at a level, which would enable gradual return to green phase. |
As a complementary document to the Plan, the NAC created an Emergency Framework for Rationing of Blood for Massively Bleeding Patients during a Red Phase Blood Shortage, 5 which has served as a model for blood shortage planning in other countries. 6 To date, it has not been activated in Canada. Since 2015, there have been six Green Phase Advisory declarations for RBC (primarily due to reduced group O‐negative RBC supply), two Amber Phase declarations for platelets, and no Red Phase declarations.
4. THE ROLE OF INVENTORY TRACKING
CBS uses a Days on Hand (DoH) metric to track inventory levels of RBC and platelets. The calculation is based on usual historical demand patterns and denotes the number of days that can be supplied from the national inventory to all hospitals should all collections cease.
Hospitals routinely report RBC and platelet inventories to CBS once per week. RBC inventory demand patterns are based on daily utilization with an Average Daily Red Cell Demand (ADRD) indicator. This indicator includes all units transfused, outdated, and wasted in a defined period of time, which is divided by a timeline denominator (e.g., 365 days). Platelet inventory is reported based on actual units in hospital. Overall, data from the blood operator and hospital inventories are used to provide a full perspective of available RBC and platelet inventory nationwide.
During a blood shortage phase declaration by the NEBMC, hospitals are required to report RBC and/or platelet inventory to CBS daily. Visibility of the total national inventory facilitates NEBMC discussion and provides guidance to CBS. As the national blood supplier, CBS can divert blood products to areas of greatest need or direct jurisdictions to redistribute blood between hospitals if required to meet urgent patient needs.
5. UNIQUE PREPARATIONS FOR POTENTIAL BLOOD SHORTAGES DURING THE COVID‐19 PANDEMIC
A summary of RBC and platelet supply and demand determinants during the COVID‐19 pandemic is shown in Figure 1. Shortly after the novel SARS‐CoV‐2 virus was identified in early 2020, CBS began monitoring its impact on the blood supply in countries affected by the virus. Specifically, reports of decreased blood donor attendance and supply challenges 7 led to concern regarding blood inventory system stability. In the days following the declaration of COVID‐19 as a global pandemic on March 11, 2020, all Canadian provinces declared states of emergency, which led to business closures and population‐wide sheltering in‐place. As detailed later, CBS experienced an almost immediate reduction in collections, a phenomenon which has also been reported by other international operators. 8 , 9 , 10 , 11 , 12
FIGURE 1.
Balance of blood component supply and demand determinants in Canada during the COVID‐19 pandemic
On March 16, 2020, the NEBMC met to discuss concerns about the security of Canada's national blood supply. Although inventory levels were sufficient at the time, forecasting data and international observations suggested an impending inability to meet hospital demand based on the precipitous decline in collections, which was expected to be sustained for weeks to come. Therefore, the NEBMC declared a Green Phase Advisory applicable to all blood components and PPRP. 13
Given the unique and sustained nature of the crisis, physician specialists from national organizations with high transfusion need patients, including critical care, hemoglobinopathy, and stem cell transplant disciplines, were invited to participate as guests in NEBMC meetings. This ensured direct dialogue with clinical experts and opinion leaders managing these patient populations who were otherwise not well described in the Plan or its companion documents. In preparation for RBC and platelet shortages, representatives from the subspecialty disciplines were asked to rapidly develop clinical practice guidance statements to help inform blood transfusion for patients with blood needs. 14 , 15
The NEBMC initially met weekly (for approximately 3 months) to maintain a framework for effective coordination, consensus building, common messaging, and rapid decision‐making during this sustained period of demand and supply volatility.
6. INITIAL IMPACT OF THE COVID‐19 PANDEMIC ON BLOOD COLLECTIONS
During the week of March 9, 2020, CBS experienced a sudden and unanticipated reduction in donor attendance of approximately 20%. This was further compounded by a reduction in collections capacity of 10%–12% in each of the subsequent 3 weeks, related primarily to the cancellation of mobile events in public community settings, which represented 40% of the collection network at that time. Mobile event cancellations were driven by multiple factors, including organizations not wanting to hold a public event in their facility, an inability to maintain physical distancing during the planned collection event, the need for review of disinfection procedures between donors, and fear of staff or donor infection from attending donation events in these communities.
As CBS rapidly moved to address these challenges and rebuild capacity, trends in donor behavior were closely monitored with resources mobilized to augment donor engagement and confidence. As part of this endeavor, CBS engaged with the Council of Medical Health Officers of Canada, with public health and provincial officials, to ensure that public instructions to quarantine were not in opposition to messaging that blood donation was safe and necessary to sustain the blood supply for patients. There was subsequently a national public announcement by the Prime Minister of Canada during a daily media update on March 19, 2020, and a resultant surge in donor attendance at available collection sites.
During this time, CBS activated its pre‐existing Business Continuity Management and Pandemic Preparedness Plans, which enabled rapid adoption of necessary measures to maximize operations within a modified collections network focusing on fixed donor sites. These included extending hours for donation at permanent sites, increasing staff, and implementing safety measures (wellness checkpoints, use of personal protective equipment, physical distancing).
7. INITIAL ACTION BY HOSPITAL TRANSFUSION SERVICES
Following the NEBMC Green Phase Advisory announcement, hospital transfusion services began aggressively promoting restrictive transfusion practices or the use of alternatives to transfusion to minimize the anticipated negative impact on blood inventory related to the rapid decline in donations and collections. Educational initiatives were coordinated and disseminated through both local and national organizations and included the use of available posters from “Choosing Wisely Canada” promoting restrictive RBC transfusion policies and the adaptation of patient blood management poster templates (see Appendix S2 for poster examples). Local and jurisdictional presentations on the risk of blood shortage in Canada aligning with NEBMC messaging were delivered to clinicians and hospital administrators. In support of these hospital‐based approaches, CBS also actively engaged with patient organizations to proactively dialogue regarding inventory challenges and mitigation measures.
Further, in accordance with the Plan, Provincial Emergency Blood Management Committee (PEBMC) activations facilitated local discussions about blood supply monitoring and management. This NEBMC–PEBMC engagement was essential to create awareness of the need to consider blood supply since jurisdictions were invoking healthcare resource restrictions of variable degrees to protect hospital capacity for potential pandemic‐related demand surges.
8. IMPACT ON NATIONAL BLOOD SUPPLY AND DEMAND
Figure 2A demonstrates the dramatic impact of the COVID‐19 pandemic on national RBC inventory supply and demand trends. Figure 2B shows the Canadian COVID‐19 case load relative to RBC demand over the same time period. As a direct consequence of the pandemic, CBS initially experienced a reduction in its planned mobile collection sites to approximately 33% of its collection capacity, which led to a drop in overall RBC collections during March (with a nadir approximately 25% lower than originally planned). A prominent drop in RBC issues to hospitals (demand) is also seen in March, aligning with the timing of healthcare system closures, followed by a gradual upturn in demand in early April.
FIGURE 2.
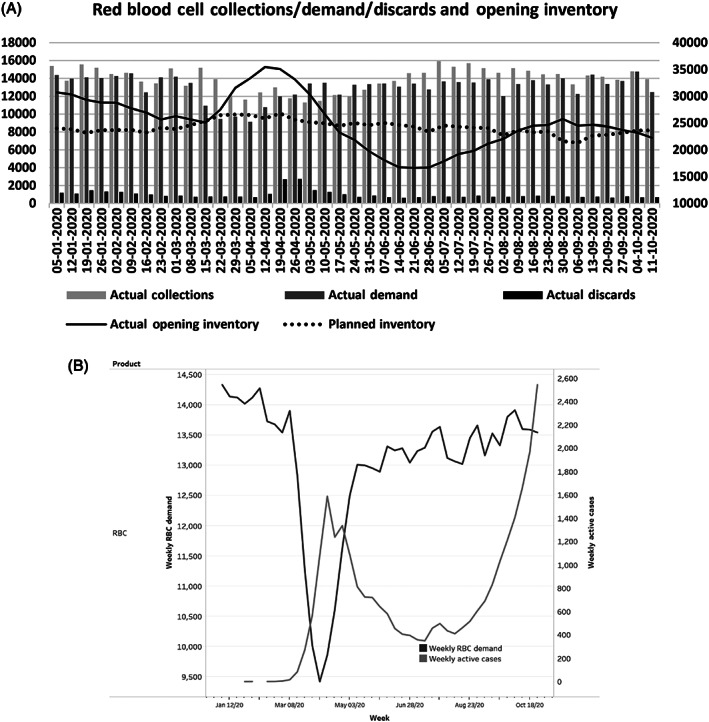
(A) Canadian Blood Services (CBS) red blood cell (RBC) inventory from January 5, 2020 to October 11, 2020. This figure illustrates the number of RBC units actually collected, discarded onsite, and issued to hospitals (demand) from CBS indicated by the bars (y‐axis left). The solid and dotted lines represent actual and planned total number of RBC units in inventory at CBS (y‐axis right). (B) National weekly RBC demand versus population COVID‐19‐positive active case load: February 2020 to October 2020. This figure demonstrates the impact of the first wave of the pandemic on RBC demand in Canada. The left axis and heavy black line demonstrate the early drop in national RBC demand due to initial healthcare system closure, followed by a resumption of urgent care hospital services and return to a reduced but stable RBC demand. The right axis and gray line show the concurrent weekly active COVID‐19 cases in Canada. Despite the gradual growth in COVID‐19 cases nationally into the autumn months, RBC weekly demand remained stable
The reduction in CBS collections driven by the pandemic was offset by a significantly greater reduction in demand than had been expected. National weekly demand for RBC dropped to a nadir of 36% relative to anticipated demand before beginning to recover in early April, aligning with the nadir of 25% in collection reduction relative to planned collections. A parallel platelet supply–demand pattern was also observed (data not shown). Therefore, the total blood system inventory remained sufficient to meet the needs of the population.
Given the reverse inflection observed between supply and demand during the first month of the COVID‐19 pandemic, there was a paradoxical growth of national blood inventory from late March and throughout April 2020, resulting in an unprecedented increase in RBC outdates (discards) at both the blood operator and hospital levels by the end of April. Figure 3 illustrates these trends in greater detail and underscores the early challenges of managing a volatile national inventory. Due to their short 7‐day shelf‐life, excess outdates of platelet inventory were not seen (data not shown).
FIGURE 3.
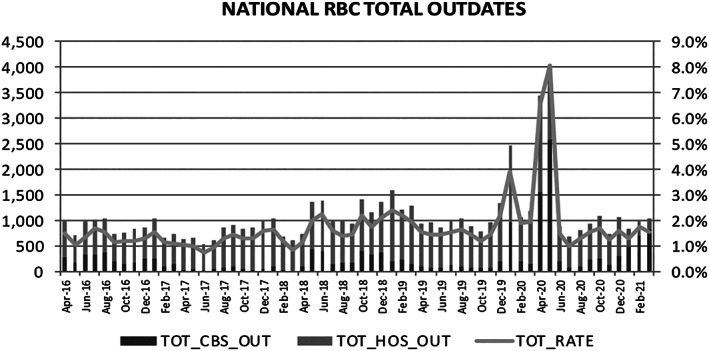
Red blood cell (RBC) discards due to national blood system outdates (including hospital and Canadian Blood Services [CBS] data). Total outdates (line) for RBC is relatively stable with a notable spike April and May 2020 and subsequent return to previous rates. Black bars show outdates that occurred at CBS (prior to issue) and the gray bars show outdates that occurred at hospitals
Hospital inventory reporting data in Figure 4 show that from March 2020 through June 2020, hospitals were stocking inventories about 12% below baseline inventory, reaching a nadir of 22% below usual inventory levels during the week of June 17, 2020. Despite the low inventory held by CBS in June and decreased overall hospital inventories relative to pre‐COVID utilization, RBC supply within hospitals remained adequate to meet the needs of patients. The stabilization of hospital demand and increase in CBS collection subsequently allowed national supply to rebuild to optimal levels between 22,000 and 27,000 units by August 2020.
FIGURE 4.
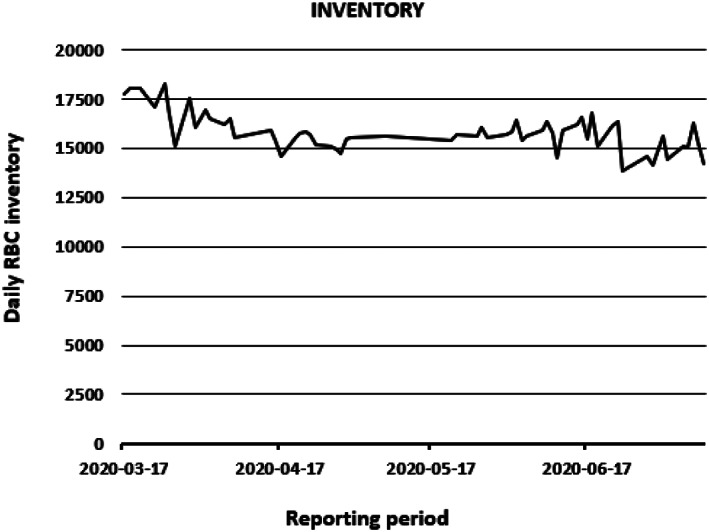
Hospital red blood cell (RBC) inventory reports March 17, 2020 to July 12, 2020. This figure shows the number of units reported to Canadian Blood Services (CBS) from 302 Canadian hospitals during the mandatory inventory reporting period in the Green Phase Advisory. Hospital reporting compliance varies from 52% to 87% throughout the time period listed (data not shown)
In summary, the decline in both blood supply and demand early in the pandemic afforded time for CBS to augment its collection capacity and implement COVID‐19 safety measures. Urgent clinical transfusion needs in hospitals led to increasing demand trends during April and May. However, CBS had not yet reached its reengineered collection capacity, thus CBS inventories fell dramatically in May, reaching a nadir of approximately 18,000 units during the week of June 21. The visibility of blood inventory available within hospitals confirmed an adequate supply for patient care while CBS inventory recovered.
9. THE NEBMC AND ESSENTIAL COMMUNICATIONS
The first 6 months of the COVID‐19 pandemic was a time of great supply–demand instability. Regular discussions at the NEMBC were critical to facilitate an open forum of understanding jurisdictional healthcare system reopening plans and transfusion behaviors. Guests invited to meetings from specialties with high transfusion rates enhanced the NEBMC understanding of essential clinical patient needs. The healthcare system intelligence enabled more accurate demand forecasting and informed CBS reconfiguration of its short‐ and long‐term collection plans.
As the pandemic progressed, ongoing engagement between NEBMC and PEBMC members ensured system visibility of the fresh blood component inventory. The strong RBC inventory resulting from the greater‐than‐expected decrease in hospital demand led the NEBMC to transition from Green Phase Advisory into Recovery Phase for all blood components on May 6, 2020. Monitoring of the overall national RBC and platelet inventories within the blood system and the frequent communication by CBS regarding collection process modifications and timelines—particularly throughout June 2020—provided the NEBMC with reassurance throughout that the blood supply was secure to meet the needs of hospitals.
While NEBMC discussions were heavily focused on RBC and platelet inventory, the NEBMC was also kept apprised of the PPRP supply within CBS inventory. The overall PPRP supply remained stable due to the long product shelf‐life and sufficient inventory existing in‐country, while demand remained at baseline.
On July 14, 2020, the NEBMC notified hospitals of the transition to Green Phase (normal inventory operations) but emphasized the need for continued partnership between the blood operator and hospitals, with each to remain vigilant in their actions to mitigate the potential for any blood shortages. The NEBMC strongly recommended adherence to restrictive transfusion practices and continued vigilance of utilization monitoring within hospitals, given the dynamic and evolving nature of this pandemic.
Core NEBMC members continued to meet regularly throughout the summer months while CBS inventory recovered to baseline levels with implemented collection process changes. Hospitals continued to provide more frequent inventory and demand reporting. On August 25, 2020, activation of the Plan was discontinued, as labile component supply and demand had stabilized.
10. DISCUSSION AND LESSONS LEARNED
A national shortage of labile blood component shortages was avoided in Canada during the first wave of the COVID‐19 pandemic. This was achieved through activation of the National Plan for Shortages of Labile Blood Components (the Plan) and leveraging the NEBMC as a vital collaborative body integral to the Plan. Our success can be attributed to the compliance of all blood system partners with NEBMC recommendations, as well as the commitment of the transfusion medicine community to enhance blood utilization strategies.
During the initial 8 weeks of the pandemic, there were clear signs that CBS collections would not meet forecasted inventory. However, the decline in hospital demand for blood components due to the restriction of hospital services (including reduced surgeries, stem cell transplantation, and outpatient infusion clinic services) and decrease in trauma presentations allowed time for CBS to re‐engineer and implement modifications to collection operations. In the subsequent 6 weeks when hospital demand had stabilized, CBS collections had not yet reached maximal capacity in the context of needed modifications. The visibility of hospital inventory by the NEBMC, together with a sustained communication regarding reduction of baseline inventory at hospitals and high‐level intelligence sharing regarding healthcare system reopening, underpinned confidence that demand would not outpace available blood supply, which would impact patient care. This confidence can be directly attributed to the prolonged engagement of the NEBMC, which ensured that the equitable distribution of RBC would be achieved despite potential jurisdictional variability in healthcare system reopening. The Plan does not restrict provincial health services' activities unless there is a resultant national inventory constraint that impacts the national blood supply. The centralized approach afforded by the NEBMC and the national inventory provided by the blood operator allow for regional precision in a country where the impact of the pandemic has been felt in different ways with differing cadences.
There were notable unanticipated benefits of the pandemic on the blood system. Discussions surrounding RBC and platelet inventory constraints led to an enhanced adherence to patient blood management principles, which aligns with published calls for enhanced compliance with patient blood management practices to reduce strain on the blood system. 16 , 17 Given the demonstrated overall health system benefits of patient blood management interventions, we presume that there is a high likelihood of jurisdictions continuing with program activities such as enhanced use of intravenous iron rather than blood transfusion for anemia management.
With an enhanced awareness of the need to optimize transfusion practices during times of blood supply concern, transfusion optimization practices based on screening of RBC and platelet orders by hospital laboratory technologists (e.g., issue of 1 unit RBC at a time and monitoring pre‐transfusion thresholds in stable inpatients) were implemented in several jurisdictions. This approach was based on principles expanded to sites that were not formal participants within the successful Canadian multicenter project evaluating the effectiveness of lab‐based RBC order screening. 18
In addition, the NEBMC construct and recommendations for actions at the jurisdictional level ultimately led to specific attention focused on the availability of blood by jurisdictional pandemic planning committees during system reopening discussions. For example, surgical service resumption checklists that were implemented in the province of Ontario (which receives almost 50% of the overall national RBC and platelet supply) were revised to include sufficient blood inventory as a criterion for increasing surgical capacity. British Columbia has also recently published their experiences on actions taken as a result of NEBMC recommendations. 19
Activation of the Plan in the context of the COVID‐19 pandemic has highlighted gaps in its design and execution and provides an opportunity to address these going forward. Firstly, while the concepts regarding decreased ability to collect blood in a pandemic were considered in the development of the Plan, the extent of a subsequent reduction of clinical services and trauma presentations decreasing RBC demand was not appreciated and ultimately led to an excess in RBC outdates, which does not appear to have been reported elsewhere. Our recent experiences, and parallel experiences reported by other hospitals during this pandemic, 20 highlight the need for the blood operator and hospital transfusion services to reframe this balance in the Plan. Other estimates of the impact of an influenza pandemic on demand for blood have been reported previously; the AABB Task Force on Pandemic Influenza and the Blood Supply predicted that demand for blood may decrease by 10%–40% based on estimates of the variability of RBC use for elective versus urgent or emergent transfusion. 21 The World Health Organization estimated that a 20%–50% planned reduction in blood usage can often be achieved in jurisdictions where at least a certain amount of blood is used in routine, planned situations. 22 As such, the Plan should be refined to allow for agility to respond to both surges and ebbs in demand to reduce outdates and safeguard donors while simultaneously ensuring sufficient supply.
Secondly, upon activation of the NEBMC, it became apparent that most Canadian hospitals had never trialed implementation of the Plan or its principles in the context of provincial or local emergency shortage management plans. The COVID‐19 pandemic provided an opportunity for NEBMC and PEBMC members to engage and collaborate with hospital administrators to ensure plans were developed and/or implemented in their regions and institutions. This broader uptake highlighted a gap in the Plan with respect to specific patient populations with high transfusion needs, including those with hemoglobinopathies, bone marrow failure syndromes, and recipients of stem cell transplantation. While the Plan itself does not address these patient groups, the NEBMC construct allowed for inclusion of clinical representation and input of these treaters to ensure that the needs of their patients were included in inventory management discussions. These learnings will be incorporated into future revisions of the Plan.
Thirdly, the pandemic raised two novel challenges that had not previously been considered in the Plan. One challenge was the prolonged, globally broad nature of a potential blood shortage versus a brief, transient regional event. The other was the possible increase in demand for RBC associated with extracorporeal life support as a therapeutic intervention for COVID‐19‐associated respiratory failure, which could have a significant impact on blood utilization. Fortunately, the Plan allowed for flexibility in the frequency and duration of NEBMC meetings where these gaps were addressed in real time by members and external subject matter experts. These learnings will also be captured in the next iteration of the Plan.
Lastly, the Plan was written with a specific focus on the management of shortages of labile blood components. It had been recognized by the NEBMC that PPRP supply had been stable in the initial months of the pandemic. However, future supply of specific high utilization of human plasma protein products like intravenous immune globulin (IVIG) could be at significant risk with a pandemic‐induced decline to already declining global plasma collections. As such, a dedicated interim strategy to manage IVIG shortages has been developed in Canada at the request of the NEBMC. 23
11. CONCLUSION
The COVID‐19 pandemic has been a test of Canada's blood shortages planning framework. The sustained communication between NEBMC members and collaboration of the NEBMC with jurisdictional partners and national patient care organizations dependent on blood transfusion support contributed to our success in mitigating a blood component shortage. Although the degree to which both supply and demand fell was unanticipated and RBC outdates increased, patients were not adversely impacted by a lack of product availability. A careful analysis of blood component utilization trends by CBS and a review of actions within provincial and hospital jurisdictions will inform revisions to the Plan, including the addition of a specific section on pandemic planning to ensure optimization of processes in the future.
CONFLICT OF INTEREST
The authors have disclosed no conflicts of interest.
Supporting information
Appendix S1. Supporting Information.
Appendix S2. Supporting Information.
ACKNOWLEDGMENTS
The authors extend their sincere appreciation to NEBMC members for their participation and contribution to discussions during activation of the Plan. We thank Mr. Richard Forester and Mr. Tom Courtney for their assistance with data acquisition and figure formatting, and to Ms. Jennifer Delorme for her assistance with manuscript preparation.
Prokopchuk‐Gauk O, Petraszko T, Nahirniak S, Doncaster C, Levy I. Blood shortages planning in Canada: The National Emergency Blood Management Committee experience during the first 6 months of the COVID‐19 pandemic. Transfusion. 2021;61:3258–3266. 10.1111/trf.16661
REFERENCES
- 1. Najafe M, Ahmadi A, Zolfagharinia H. Blood inventory management in hospitals: considering supply and demand uncertainty and blood transshipment possibility. Oper Res Health Care. 2017;15:43–56. [Google Scholar]
- 2. Simonetti A, Ezzeidin H, Walderhaug M, Anderson SA, Forshee RA. An inter‐regional US blood supply simulation model to evaluate blood availability to support planning for emergency preparedness and medical countermeasures. Disaster Med Public Health Preparedness. 2018;12(2):201–10. [DOI] [PubMed] [Google Scholar]
- 3. Gschwender AN, Gillard L. Disaster preparedness in the blood Bank. Clin Lab Sci. 2017;30(4):250–7. [Google Scholar]
- 4. The National Plan for Management of Shortages of Labile Blood Components . National Advisory Committee on Blood and Blood Products and Canadian Blood Services. Available at: https://www.nacblood.ca/resources/shortages-plan/20200320%20The%20National%20Plan%20for%20Management%20of%20Shortage%20of%20Labile%20Blood.pdf. Accessed 25 May 2021.
- 5. National Blood Shortage Plan . National Advisory Committee on Blood and Blood Products. Available at: https://nacblood.ca/resources/shortages-plan/index.html. Accessed 25 May 2021.
- 6. Doughty H, Green L, Murphy F. Triage tool for the rationing of blood for massively bleeding patients during a severe national blood shortage: guidance from the National Blood Transfusion Committee. Br J Haematol. 2020;191(3):340–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cai X, Ren M, Chen F, Li L, Lei H, Wang X. Blood transfusion during the COVID‐19 outbreak. Blood Transfus. 2020;18(2):79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grandone E, Mastroianno M, Caroli A, Ostuni A. Blood supply and transfusion support in southern Italy: findings during the first for weeks of the SARS‐CoV‐2 pandemic. Blood Transfus. 2020;18(3):230–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pagano MB, Hess JR, Tsang HC, Staley E, Gernsheimer T, Sen N, et al. Prepare to adapt: blood supply and transfusion support during the first 2 weeks of the 2019 novel coronavirus (COVID‐19) pandemic affecting Washington State. Transfusion. 2020;60(5):908–11. [DOI] [PubMed] [Google Scholar]
- 10. Gniadek TJ, Mallek J, Wright G, Saporito C, AbiMansour N, Tangazi W, et al. Expansion of hospital‐based collections in the face of COVID‐19 associated national blood storage. Transfusion. 2020;60(7):1470–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang Y, Han W, Pan L, Wang C, Liu Y, Hu W, et al. Impact of COVID‐19 on blood centres in Zhejiang province China. Vox Sang. 2020;115(6):502–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yahia AIO. Management of blood supply and demand during the COVID‐19 pandemic in King Abdullah Hospital, Bisha, Saudi Arabia. Transfus Apher Sci. 2020;59(5):102836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Canadian Blood Services Inventory Advisories . Available at: https://www.blood.ca/en/hospital-services/customer-service/communications/inventory-advisories. Accessed 25 May 2021.
- 14. Singh G, Nahirniak S, Arora R, Légaré J‐F, Kanji HD, Nagpal D, et al. Transfusion thresholds for adult respiratory extracorporeal life support: an expert consensus document. Can J Cardiol. 2020;36(9):1550–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CTTC Canada – COVID‐19 Position Statement on COVID‐19. 2020 Mar 26. Available at: https://cdn.ymaws.com/www.cttcanada.org/resource/collection/42604803-5F1C-4368-AFA9-2A56102AEF8B/CTTC_COVID19_March_26,_2020_v02.pdf. Accessed 25 May 2021.
- 16. Shander A, Goobie SM, Warner MA, Aapro M, Bisbe E, Perez‐Calatayud AA, et al. Essential role of patient blood management in a pandemic: a call for action. Anesth Analg. 2020;131(1):74–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schlesinger T, Kranke P, Zacharowski K, Meybohm P. Coronavirus threatens blood supply: patient blood management now! Ann Surg. 2020;272(2):272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kron AT, Collins A, Cserti‐Gazdewich C, Pendergrast J, Webert K, Lieberman L, et al. A prospective multi‐faceted interventional study of blood bank technologist screening red blood cell transfusion orders: the START study. Transfusion. 2021;61(2):410–22. [DOI] [PubMed] [Google Scholar]
- 19. McGinnis E, Guo R, Marcon KM, Berry B, Coupland R, Meneghetti V, et al. Adaptations of transfusion systems to the COVID‐19 pandemic in British Columbia, Canada: early experiences of a large tertiary care center and survey of provincial activities. Transfusion. 2021;61(4):1102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gehrie E, Christopher AT, Sanford KW. Transfusion service response to the COVID‐19 pandemic. Am J Clin Pathol. 2020;154:280–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandemic Influenza Resources. Available at: https://www.aabb.org/about-aabb/organization/disaster-response/interorganizational-task-force-on-pandemic-influenza-and-blood-supply. Accessed 25 May 2021.
- 22.Maintaining a Save and Adequate Blood Supply during Pandemic Influenza. Available at: https://www.who.int/bloodsafety/publications/WHO_Guidelines_on_Pandemic_Influenza_and_Blood_Supply.pdf. Accessed 25 May 2021.
- 23.The National Plan for Management of Shortages of Immunoglobulin Products (Ig) – Interim Guidance. Available at: https://www.nacblood.ca/resources/shortages‐plan/The%20National%20Plan%20for%20Management%20of%20Shortages%20of%20Immunoglobulin%20Products%20(Ig)%20%20Interim%20Guidance_July%2027%202020.Published.pdf. Accessed 25 May 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information.
Appendix S2. Supporting Information.


