Abstract
Background
Globally, type 2 diabetes has continued to increase, now accounting for over 90% of all diabetes cases. Though the magnitude of uncontrolled glycaemic levels in patients with type 2 diabetes is steadily rising, evidence showed that effectively controlled glycaemic levels can prevent complications and improve the quality of life of these patients. As little is known about the effect of educational interventions on this population, this systematic review and meta-analysis evaluated the effectiveness of educational interventions versus standard care on glycaemic control and disease knowledge among patients with type 2 diabetes.
Methods
PubMed, Google Scholar, Cochrane Library, Scopus, African Journals Online and Wiley Online Library were searched. Two authors independently assessed within-trial risk of bias in each included study using revised Cochrane risk-of-bias tool for randomised trials. A random-effects model was employed to estimate combined effect sizes. Subgroup analyses were employed to investigate possible sources of heterogeneity between studies. The overall certainty of the evidence was evaluated using the Grading of Recommendations Assessment, Development and Evaluation approach.
Results
A total of 19 trials with 2708 study participants were included in the review. Primary outcomes (glycaemic control) were reported in 18 trials. The pooled estimated impact of educational intervention on glycaemic levels using the random-effects model was −0.83 (95% CI: −1.17 to –0.49, p<0.001). Subgroup analyses revealed greater A1c reductions in those studies with intervention duration of up to 3 months and with empirical intervention designs. Educational interventions led to significant increases in participants’ knowledge of type 2 diabetes (standardised mean difference: 1.16; 95% CI: 0.71 to 1.60; I2=93%).
Conclusion
In the current review overall, educational interventions can potentially lead to improved glycaemic control levels in patients with type 2 diabetes despite heterogeneity across the studies. Besides, the findings showed that educational interventions could increase disease knowledge among patients with type 2 diabetes.
PROSPERO registration number
CRD42020205838.
Keywords: education & training (see medical education & training), diabetes & endocrinology, general diabetes
Strengths and limitations of this study.
This systematic review will provide a comprehensive search of the literature, the effect of educational intervention on glycaemic control and knowledge of type 2 diabetes.
An extensive search of multiple databases and search engines (ie, PubMed, African Journals Online, Web of Science, Scopus and Google Scholar) was performed to ensure a comprehensive review; nevertheless, potentially relevant articles from other/additional databases may be missed.
We only used English-language articles, although our target was global, which could be in several other languages such as Spanish, French or Portuguese.
Background
Diabetes mellitus (DM) is increasingly becoming an extensive non-communicable health problem, leading to significant morbidity and mortality.1 Globally, a recent estimate showed that approximately 422 million adults are living with DM.2 According to the International Diabetes Federation projection, approximately 629 million people will be affected by 2045.3 Of these, approximately 80% of affected individuals live in low-income countries.4 In particular, type 2 DM (T2DM) is responsible for more than 90% of all diabetes cases.5 The increasing burden is due to several risk factors such as sedentary behaviours, obesity, unhealthy diet, lack of exercise, family history and age.6–8
Maintaining optimal glycaemic levels is vital to diabetes control.9 However, evidence showed that poor glycaemic control (glycosylated haemoglobin (HbA1c) ≥7%) contributes to kidney failure, myocardial infarction, stroke, retinopathy, hypertension, increasing costs for patient care and reduced quality of life.10–14 The aims of T2DM management are to attain glycaemic targets, minimise adverse events and prevent complications.15 16 Therefore, lifestyle modifications, such as diet and exercise, have been reported to reduce the complications of uncontrolled glycaemic levels in patients with T2DM.17
Evidence has revealed that self-management education can reduce the glycaemic level by 30%–80%.18 Besides, diabetes education can improve glycaemic control, change people’s behaviours, promote self-care, and reduce complications and progression of the disease.19–21 Moreover, numerous studies suggest that diabetes educational interventions can increase knowledge of diabetes22 23 and medication compliance,24 decrease readmissions,25 26 reduce length of stay and mortality rate,25 and improve glycaemic control.27 28 In addition, the American Diabetes Association (ADA) position statement provides the evidence and strategies for the provision of education and support services to all adults living with T2DM.29 Moreover, the consensus report showed that there are four critical times to provide diabetes self-management education and support: (1) at diagnosis, (2) annually and/or when not meeting treatment targets, (3) when complicating factors develop, and (4) when transitions in life and care occur.30
Though knowledge about diabetes has paramount benefit to patients’ self-care management, insufficient diabetes knowledge is unfavourable to the patients’ health due to most of the complications that arise can be prevented through self-care practice.31 32 However, numerous studies have shown that improving patient knowledge about T2DM and its complications has substantial benefits to maintain optimal glycaemic levels, enhance treatment adherence, reduce treatment cost and decrease the progression of disease.33–35 Previously, several reviews on the effect of self-management interventions for patients with T2DM exist.36–38 However, most reviews included inadequate number of articles, did not address the effects of education on knowledge of diabetes and included interventions which were poorly described. Thus, research is required to estimate the effects of educational interventions on sufficient methodological quality and substantive statistical analysis. Hence, the present review and meta-analysis aimed to evaluate the effect of educational interventions on glycaemic control and disease knowledge in patients with T2DM.
Review questions
Does a structured educational intervention increase diabetes knowledge in patients with T2DM?
Does a structured diabetes educational intervention reduce HbA1c levels among patients with T2DM?
Methods
Protocol and registration
Initially, PROSPERO was searched to confirm for other reviews on the effect of educational interventions on glycaemic control and disease knowledge among patients with T2DM. But no such reviews were identified. Thus, the protocol was registered on PROSPERO (www.crd.york.ac.uk/PROSPERO/) as recommended by the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement.39
Search strategy and data sources
We did a comprehensive systematic search to collect all relevant articles using the Peer Review of Electronic Search Strategies for systematic reviews.40 The search was limited to studies published in peer-reviewed journals from January 2000 to August 2021 (as authors were interested in up-to-date data). The PRISMA guidelines were used to conduct and report the present review.39 The literature was searched in PubMed, Scopus, Google Scholar, African Journals Online, Cochrane Library and Wiley Online Library. The keywords used for the review included “educational”, “behavioral”, “knowledge”, “glycemic control”, “glycosylated hemoglobin”, “HbA1c”, “Type 2 diabetes mellitus”, “Type 2 diabetes” and “T2DM”. Boolean operators like ‘AND’ and ‘OR’ were used to combine search terms. The Medical Subject Headings (MeSH) terms employed in the PubMed search engine in various combinations are shown in table 1. To access all articles on this topic, we manually review all references to reduce publication bias. Searches were performed on 20 August 2020. The search was restricted to full texts, human studies and English-language publications. In the present review, the Patient/Population (P); Intervention (I); Comparison (C) and Outcomes (O) question was as follows: is educational intervention (I) in people with T2DM (P), when compared with people who had not taken part in the educational intervention or had standard care (C), associated with improved glycaemic control and disease knowledge (O)?
Table 1.
PubMed search history
| Search | Search terms | Hits |
| #1 | Type 2 diabetes[tw] OR Type 2 diabetes mellitus[tw] OR T2DM[tw] OR insulin non dependent diabetes [tw] | 199 276 |
| #2 | Education [tw] OR intervention [tw] OR behavioral intervention[tw] OR self-management [tw] | 1 587 693 |
| #3 | Glycemic control [tw] OR glycosylated hemoglobin[tw] OR HbA1c[tw] | 65 114 |
| #4 | Knowledge [tw] OR behavioral outcomes [tw] | 851 164 |
| #5 | #1 AND #2 AND #3 AND #4 | 5428 |
| #6 | #5; limits: studies done with humans, English language, full text, RCT and publication year (2000–2020) | 496 |
RCT, randomised controlled trial.
Eligibility criteria
Types of participants
This review takes into consideration studies that included adult patients (≥18 years old) with T2DM in outpatient health settings, primary care settings, diabetes clinics and hospitals within the catchment. Those articles focusing on or including children or those with T1DM were excluded from the review.
Types of interventions
The review considered any educational intervention provided to adult patients with T2DM in diabetes care settings receiving standard or routine care. Intervention could be provided by any healthcare provider, involved any medium (written, oral, video and computer), delivered at the individual or group level, focused on theory-based or empirical content, and of varying duration. Studies lacking an education intervention, unclear information respecting the intervention and insufficient data on the main outcome variable were considered criteria for exclusion.
The comparator in this study was the delivery of the usual care/routine care for T2DM. Routine care refers to diabetes care that healthcare staff usually and normally provides in their daily care. Articles were excluded if they did not implement a comparison with routine care.
Types of studies
In the present review, studies were included if they were randomised controlled trials. Full-text articles were included, whereas studies published with only abstract or unpublished data were excluded. Of note, non-randomised controlled trials, quasi-experimental, before and after, cohort, case–control and cross-sectional studies were excluded because uncontrolled trials and observational studies lead to greater risk of biased estimates of effect size.41
Type of outcome
This review included the following outcome measures: glycaemic control as the primary outcome of the meta-analysis, and knowledge of diabetes considered as the secondary outcome. A study was excluded if outcomes were not measured or data could not be extracted.
Study selection
After database exploration, all recognised studies were uploaded into EndNote V.8, and duplicate articles were removed. Predefined selection criteria were used to select relevant full-text articles during the screening process. Three authors (WSS, PMP and YAA) independently screened the title, abstract and keywords of the studies identified for possible eligibility in the review. Afterward, all full-text articles were evaluated carefully for inclusion and data extraction. Further screening of full text was done by two (TY and YAA) independent authors to select the studies which satisfied the eligibility standards. The possible justification for the exclusion of full-text studies was documented and reported in the systematic review. Any uncertainties about study eligibility were discussed between authors.
Data extraction
After identifying studies for eligibility, data abstraction was conducted by two (AMK and WSS) independent authors using Microsoft Excel (version 10) for Windows. The first author undertook the data abstraction, whereas the second author assumed control for the quality of extracted and entered data. The data extracted from each study included first/corresponding author, year of publication, study setting, education provider, duration of intervention, intensity of intervention, components of the intervention, number of participants in each arm (intervention and standard care group), intervention design, outcome measures, before and after intervention HbA1c levels, and knowledge scores. The outcome measures in this review were reported as the variation from starting point to closing date of follow-up in the intervention and standard care groups. If the SD of mean difference (MD) was not reported in an included study, the values were recalculated according to the guideline in the Cochrane Handbook.42
Assessment of risk of bias in included studies
Two (MD and PMP) independent authors assessed within-trial risk of bias in each included study using revised Cochrane risk-of-bias tool for randomised trials (RoB 2).43 The Cochrane’s RoB 2 tool evaluation domains used to evaluate validity and bias in studies of clinical trials were applied regarding randomisation, allocation sequence concealment, blinding, incomplete outcome data, selective outcome reporting and other biases. For this review, the overall risk of bias was rated as high/low/some concerns, in agreement with the RoB 2 tool. Any disagreement was resolved through discussion and consensus.
Assessment of certainty of the evidence
To evaluate the quality of the evidence, the authors used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.44 GRADE pro-GDT was employed to summarise the quality of evidence.45 The certainty of the evidence encompasses consideration of the within-study risk of bias which comprises methodological worth, indirectness of evidence, unexplained heterogeneity, imprecision and probability of publication bias. The GRADE approach has four levels of quality such as high-quality evidence that recommends that additional study is very unlikely to change our confidence in the estimate of effect size; moderate quality reflects further research as likely to have a vital impact on the estimate of effect size and may alter the estimate; low quality reveals that further research is very unlikely to have a significant influence on the current estimate of effect size and is likely to change the estimate; and very low quality suggests one is precise indeterminate about the estimate.
Data synthesis and analysis
The primary and secondary outcomes were reported as MD and standardised MD (SMD) with a 95% CI, using a random-effects model,46 respectively. Degree of heterogeneity was examined with the I2 statistic, which expresses the amount of heterogeneity between studies.47 To interpret the effect sizes, authors followed Cohen’s guidelines where d≤0.2 was small, d≈0.5 was medium and d>0.8 were large variation among intervention and control groups.48 We performed subgroup analyses to reduce the level of heterogeneity for the primary outcomes using duration of intervention and intervention design. Publication bias was visually evaluated using the funnel plot, supplemented by Egger’s regression test.49 50 Sensitivity analysis was performed due to the high degree of heterogeneity and risk of bias. Review Manager of the Cochrane Collaboration (RevMan V.5.4, Cochrane Organization) was used to perform the meta-analysis.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
Selection of studies
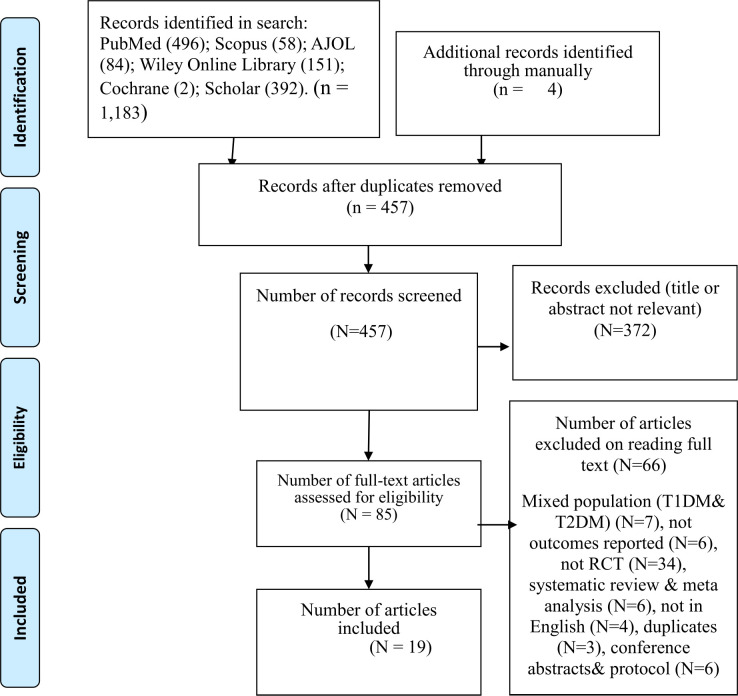
The search of the six databases yielded 1183 articles, and 4 articles were retrieved manually through a review of reference lists. After eliminating duplicates, 457 articles remained. Three hundred seventy-two studies were removed after reading the abstract and title, leaving 85 articles for full screening. Following 66 exclusions at the full-text level (mainly due to non-randomised controlled trials (n=34), or reporting mixed population (type 1 and type 2 diabetes) (N=7)), 19 studies were incorporated in the final review. The flow diagram for study selection is shown in figure 1.
Figure 1.
PRISMA flow chart for selection of studies. PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analysis; RCT, randomised controlled trial; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Characteristics of the included studies
In the current meta-analysis, a total of 19 articles met the inclusion criteria with 2708 study participants. Of these, nine included articles reported glycaemic control and knowledge of diabetes as a common outcome variable. Regarding location, two were from Brazil,51 52 three from China,53–55 two from Germany,56 57 five from Iran,58–62 two from Malaysia,63 64 two from Sweden,65 66 and one each from Thailand,67 Sri Lanka,68 and Australia.69 The sample size varied from 6053 to 300 participants.55 Educational interventions in the review were guided by the following theories or models: three studies used the theory of self-efficacy,54 63 67 three studies56 61 66 used empowerment theory, two studies60 68 used theory of self- efficacy and motivational interviewing, and one study used either chronic care model,55 PRECEDE-PROCEED model,62 BASNEF model59 or behavioural theory.64 However, the remainder of the articles51–53 57 58 65 69 used non-theory or model-based approaches.
The educational interventions comprised of face‐to‐face counselling,54 55 63 68 69 diabetes education sessions,51 52 55 60 63 67 group discussion,56 58–60 67 telephone follow‐ups,54 60 63 67 69 home visits,67 demonstrations,53 54 59 as well as questions and responses58 59 as among the most common approaches. The control groups of all studies were the current standard of care. The duration of educational interventions varied from 4 weeks54 58 59 to 12 months.52 66 Intervention groups obtained the information by different healthcare professionals such as physicians,54 55 66 nurses,52 56 58 67 69 nutritionists,61 64 health managers,55 public health assistants55 and pharmacists.51 In most included studies, intervention processes were group-based education52 54–63 65–67 and combined education53 68 69; however, in the remainder, web-based64 and individual-based51 education approaches were used. The main results and features of the selected studies are presented in table 2.
Table 2.
Characteristics of the included studies
| Authors | Country | Number of subjects (baseline) |
Health education provider |
Theory/model used | Group/ individual |
Intervention | Components of intervention | Duration of intervention | Outcome measures | Outcome indicators |
| Wichit et al67 | Thailand | I=70 C=70 |
Trained nurse | Self-efficacy | Group | Education classes (3 sessions), discussions, a home visit and a telephone follow-up | Programme focused on: meal planning, foot hygiene, physical activities, problem-solving, diabetes-related complications, enhancing competence and diabetes knowledge | 9 weeks | At baseline, week 5 and week 13 | ①②④⑤⑥ |
| Fan et al69 | Australia | I=138 C=138 |
Trained nurse | Empirical | Mixed | Face-to-face counselling over 1 hour, self-care plan, a 10 min telephone call before the appointment, a 3-month forum for about 2 hours | Education emphasises on diet modification, exercise, SMBG, psychological and adherence to medication | 6 months | At each follow-up and the end of 6 months | ① |
| Grillo et al 52 |
Brazil | I=68 C=68 |
Trained generalist nurse | Empirical | Group | Structured diabetes self-management education; the course consisted of weekly 2-hour meetings for 5 weeks, reinforcement meetings every 4 months (7 sessions) | The course content included: (1) identification of modifiable risk factors for T2DM, (2) non-pharmacological treatment, emphasising diet and exercise, (3) pharmacological therapy, (4) an overview of chronic diabetes complications and (5) foot care |
12 months | At baseline, 4, 8 and 12 months | ①④ |
| Cani et al51 | Brazil | I=37 C=41 |
Pharmacist | Empirical | Individual | Diabetes education (5 sessions), pharmacotherapeutic care plan and written guidance | Education on acute and chronic complications, the importance of lifestyle changes, foot care, the importance of home blood glucose monitoring and other topics, advice focused on the indication, proper dosage, side effects and adequate storage of medication |
6 months | At baseline and 6 months | ①③④⑥ |
| Zheng et al53 | China | I=30 C=30 |
Therapist guidance |
Empirical | Mixed | Two-session diabetes self-management education which is theory and practical course, lecture, video, exercise, food simulation model and vivid models | Theory course focuses on knowledge of diabetes and self-management strategies, such as diet guidance, exercise guidance, and knowledge of hypoglycaemia treatment, foot care, medication, and blood glucose monitoring; the practice course focuses on one-on-one nutrition guidance and individualised exercise guidance |
3 months | At baseline and 3 months | ①③⑤ |
| Jiang et al54 | China | I=133 C=132 |
Trained nurses and physicians | Self‐efficacy | Group | Structured education programme, patients’ experience sharing, peer modelling, demonstration; the intervention was given 4 weekly sessions for 1 month and then face‐to‐face/telephone meetings every 3 months | Diabetes‐related knowledge and diabetes self-management skills based on self‐efficacy theory | 4 weeks | At baseline, 3 and 6 months | ①②③④⑤ |
| Kong et al55 | China | I=150 C=150 |
Physician, health manager and public health assistant | Chronic care model (CCM) | Group | Pamphlets and face-to-face communication, continuous medical education; education was 9 sessions every month | Received the five components CCM-based intervention, awareness of the chronic disease management; self-management support included goals setting, planning, doing, checking and assessing |
9 months | At baseline and 9 months | ①③⑥ |
| Braun et al57 | Germany | I=83 C=72 |
Not stated | Empirical | Group | Diabetes teaching and treatment programme, 7 educational classes of 45 min duration | Self-monitoring, diabetes treatment | 6 months | Before (t0), immediately after (t1) and 6 months after (t2) |
①④⑤ |
| Hermanns et al56 | Germany | I=92 C=92 |
Certified diabetes nurse | Empowerment self-management approach |
Group | Lecture, discussion and a nutrition game; the education is given for 10 lessons of 90 min each, 5-week period, 2 sessions per week | Lifestyle modification, blood glucose self-monitoring, metabolic risk factors, individual goals of diabetes treatment, nutrition game, physical exercise and complications | 5 weeks | At baseline and 6 months after the intervention | ①②③④⑤⑥ |
| Didarloo et al58 | Iran | I=45 C=45 |
Trained nurse | Empirical | Group | Interactive approach such as discussion, brainstorming, question-and-response techniques for 60 min/week for 4 weeks; used specific training such as verbal persuasion and modelling | Promoting self-efficacy of diabetics, the educator used specific training approaches such as verbal persuasion, modelling and performance accomplishments Definition, signs, symptoms, and consequences of T2DM and diet |
4 weeks | At baseline and 3 months after the end of the intervention | ①②③④⑥ |
| Askari et al59 | Iran | I=54 C=54 |
Researcher | BASNEF model | Group | Training in 8 sessions (2 sessions in a week); each session lasted for 70 min; question and answer, exercise, discussion, image and messages were sent to the patients each week |
Presented content was about diabetes, signs and symptoms, diet, food composition tables, partitioning, proper use of fruits, vegetables, and grains as sources of dietary fibre |
4 weeks | At baseline and 3 months after the end of the intervention | ①②③④⑤ |
| Ebrahimi et al61 | Iran | I=53 C=53 |
Nurse with the endocrinologist and nutritionist |
Empowerment model | Group | Education training, 5–7 weekly regular meetings were held for about 60–90 min | The content of education was diet, exercise, medication and foot care The structural model was perceived threat, self-efficacy and evaluation |
8 weeks | Baseline and 3 months after the end of the intervention | ① |
| Nejhaddadgar et al62 | Iran | I=43 C=43 |
Trained professional | PRECEDE-PROCEED model | Group | The education programme with 8 weekly sessions; training workshops were also conducted among patients’ families and health workers | Education based on the variables of the PRECEDE model such as predisposing factors are genetic and environmental factors such as knowledge, attitudes and self-efficacy |
8 weeks | Baseline and 6 months after the education programme | ②③④⑤ |
| Azami et al60 | Iran | I=71 C=71 |
Trained nurse | Self-efficacy and motivational interviewing |
Group | Usual care plus a 12-week nurse-led diabetes self-management education, booklet, watching movie clips, group-based educational session, telephone follow-up calls | Self-care behaviours, including healthy eating, being active, monitoring, taking medication, problem-solving, reducing risk and healthy coping are the core components of the intervention |
12 weeks | At baseline, and 12 weeks and 24 weeks post-randomisation |
①②⑤⑥ |
| Tan et al 63 |
Malaysia | I=82 C=82 |
Not stated | Self-efficacy | Group | Structured education consisted of monthly sessions for 3 months about 30 min each session, 2 were face-to-face individual education sessions and 1 was a telephone follow-up; printed educational materials |
The first session, healthy eating, being active, medication adherence and self-monitoring of blood glucose; the second and third sessions on problem-solving skills related to hyperglycaemia, hypoglycaemia, sick day and emotional episodes |
3 months | At baseline and 12 weeks | ①②④ |
| Ramadas et al64 | Malaysia | I=66 C=62 |
Nutritionist | Behavioural theory |
Web-based | Web-based dietary intervention, 12 lesson plans were made available to the patients one after another for 6 months with updates every fortnight |
The dietary lesson plans in the intervention package were personalised according to the patients’ dietary stages of change and were expected to improve their diabetes, knowledge, attitude, and behaviour; the participants also send their queries to the study nutritionist via the website | 6 months | At baseline, 6 months post-intervention and 12-month follow-up |
①②③④ |
| Adolfsson et al 66 |
Sweden | I=50 C=51 |
Nurse and physician | Empowerment | Group | Empowerment group education, counselling using videotaping, presentation and discussion, 1 follow-up session was given within 7 months | About the disease, treatment, prevention of complications, blood glucose monitoring, diet, physical activity and daily foot care | 12 months | At baseline and at 1-year follow-up | ①②④⑥ |
| Hörnsten et al65 | Sweden | I=44 C=60 |
Nurse with special education in diabetes care | Empirical | Group | Education and group discussion with 10 2-hour group sessions over 9 months |
Patients’ understanding of the illness | 9 months | Before and each year after the intervention | ① |
| Jayasuriya et al68 | Sri Lanka | I=43 C=42 |
Medical officer and trained nurse | Self-efficacy and motivational interviewing | Mixed | Self-management education through face-to-face meeting and lecturing The first four sessions within 6 weeks, following monthly (4 weekly) for 5 more visits |
Physical activity and healthy dietary intake and more recently in ‘avoidance behaviours’ to reduce unhealthy eating |
6 months | At baseline and at 6 months | ①②⑤ |
Outcome indicators: ① metabolic controls, ② self-efficacy, ③ behaviour, ④ knowledge, ⑤ other psychological indicators and ⑥ quality of life.
C, control; I, intervention; SMBG, Self Monitoring of Blood Glucose; T2DM, type 2 diabetes.
Risk of bias in the included studies
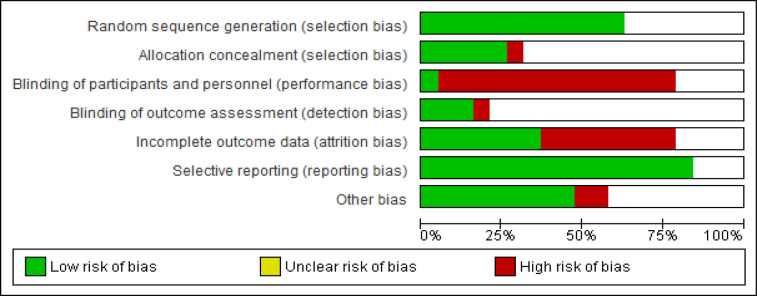
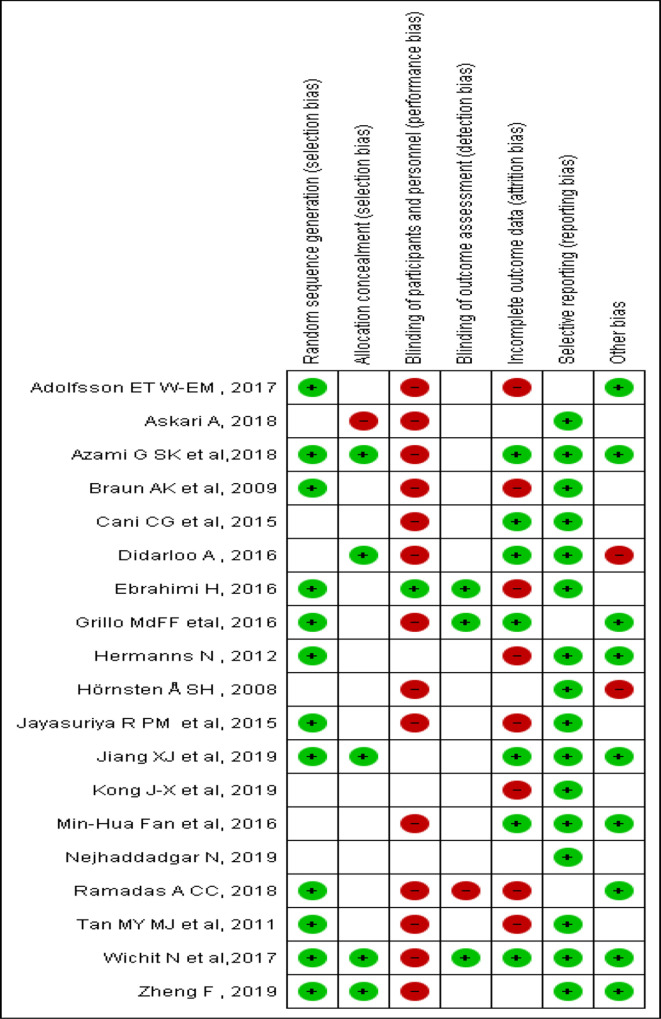
The random sequence generation for allocation was evaluated as low risk of bias in 12 studies,52–54 56 57 60 61 63 64 66–68 with 7 studies measured as having some concerns of bias.51 55 58 59 62 65 69 Allocation concealment was a low risk of bias in five studies.53 54 58 60 67 On the other hand, a high risk of allocation bias was reported in one study.59 The remaining studies51 52 55–57 61–66 68 69 were evaluated to have some concerns of bias. Blinding of participants and educators was considered a problem in such interventions; however, one study blinded participants and educators.60 Outcome assessors were blinded in three studies.52 61 67 Regarding incomplete outcome data reporting, seven studies51 52 54 58 60 67 69 were evaluated as low risk of bias. The risk of bias due to selective reporting was confirmed low for 16 studies51 53–63 65 67–69; however, there were some concerns of bias in three studies.52 64 66 Nine studies52–54 56 60 64 66 67 69 were evaluated as low risk of other potential biases, two studies58 65 were confirmed to be high risk of bias and eight studies51 55 57 60–63 68 were evaluated to have some concerns of bias. The risk of bias for studies overall is summarised in figure 2 and the risk of bias in each study is reported in figure 3.
Figure 2.
Risk of bias graph: review of authors' judgements about each risk of bias item presented as percentages across all included studies.
Figure 3.
Risk of bias summary: review of authors' judgements about each risk of bias item for each included study.
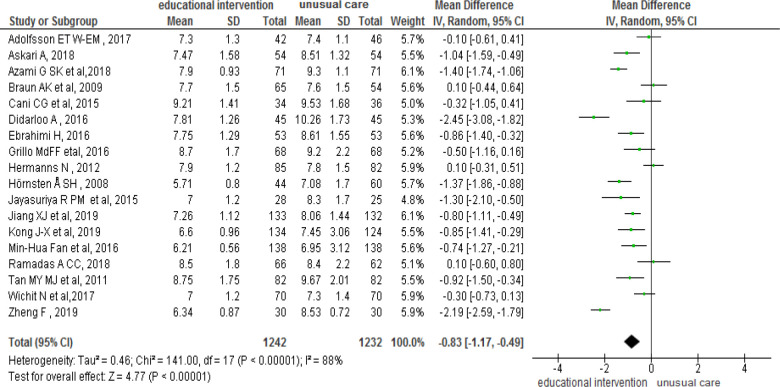
Effect of educational intervention on glycaemic control
The effects of educational interventions on glycaemic (HbA1c) level reduction are presented in figure 4. The results of the meta-analysis using random-effects model revealed that educational interventions significantly decreased HbA1c levels (MD: −0.83%; 95% CI: −1.17% to –0.49%; p<0.001, I2=88%) compared with standard care groups. A sensitivity analysis was employed by omitting three studies53 56 58 because of high risk of heterogeneity. When these studies were omitted, the results demonstrated that the pooled effect on HbA1c reduction remained statistically significant with an MD of −0.70% (95% CI: −0.96% to −0.44%, p=0.001). The I2 statistic among the studies was 73%, indicating a moderate risk of heterogeneity.
Figure 4.
The pooled effect of education interventions on HbA1c levels in patients with T2DM. HbA1c, glycosylated haemoglobin; T2DM, type 2 diabetes mellitus.
Subgroup analysis
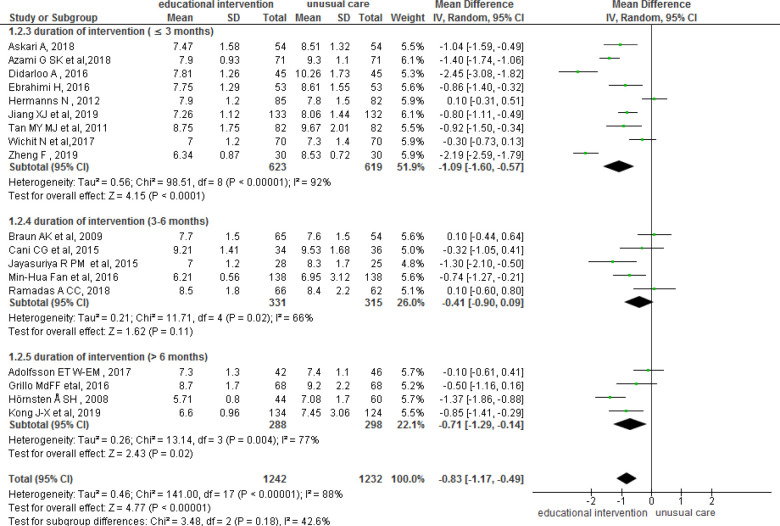
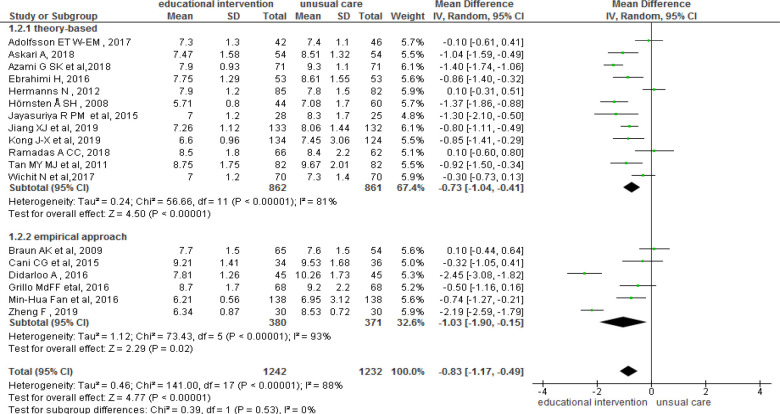
In the present review, subgroup analysis was conducted based on the duration of intervention and intervention design (theory-based vs empirical approach) to explore the potential source of heterogeneity between trials. The results of the subgroup analysis showed that the greater effect size was reported in studies with intervention duration of ≤3 months (MD: −1.09, 95% CI: −1.60 to –0.57, p<0.00) with a significant evidence of heterogeneity among studies (I2=88%) (figure 5). Additionally, the results of the subgroup analysis revealed that interventions with an empirical approach had greater effects in terms of reducing glycaemic levels (MD: −1.03, 95% CI: −1.90 to –0.15, p<0.00). Because of a significant degree of heterogeneity between studies (I2=88%), a random-effects analysis was used (figure 6).
Figure 5.
Subgroup analysis based on the duration of the intervention.
Figure 6.
Subgroup analysis based on intervention design.
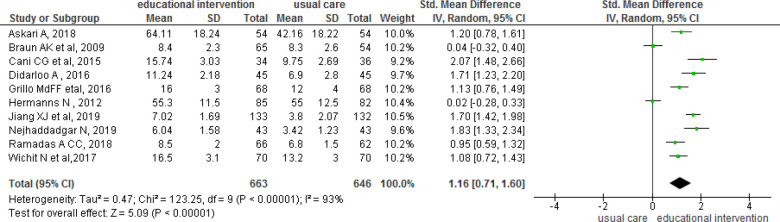
The effect of educational interventions on diabetes knowledge
Ten out of the 19 studies reported knowledge of diabetes as an outcome variable.51 52 54 56–59 62 64 67 The pooled effect size of the 10 trials demonstrated an improvement in knowledge of T2DM (SMD: 1.16, 95% CI: 0.7 to 1.60, p<0.001; figure 7) compared with standard care groups. A random-effects model was used because of significant heterogeneity. The Dietary Knowledge Questionnaire64 and the Diabetes and Medication Knowledge Questionnaire52 54 57 58 67 were used to estimate the level of knowledge in individuals with T2DM. The number of items was between 862 and 24 items.67 There was a significant variation in knowledge of T2DM scores across different studies.
Figure 7.
The pooled effect of education interventions on disease knowledge in patients with type 2 diabetes.
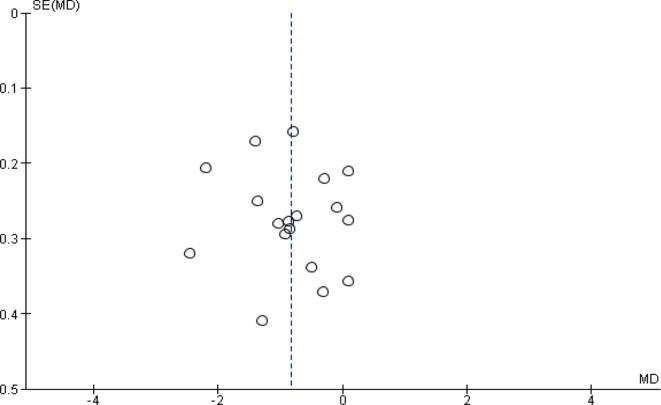
Publication bias
The presence of publication bias was visually evaluated using a funnel plot for the primary outcome (glycaemic control), and the results also reported there was no publication bias (figure 8). Likewise, Egger’s test also showed no publication bias (p=0.732). On the other hand, there were insufficient data to generate funnel plots to assess for the potential presence of publication bias for the second outcome (knowledge about T2DM).
Figure 8.
Funnel plot for HbA1c results. HbA1c, glycosylated haemoglobin; MD, mean difference.
Overall quality of the evidence
The overall quality of evidence was assessed using the GRADE approach and the results are presented in the summary of findings for the main comparison. Findings showed that the overall certainty of the evidence for glycaemic control was moderate, which suggests further studies will increase our confidence in the estimate of effect size. The quality of evidence for diabetes knowledge was low, which reflects that the effect size is limited and the true effect may be substantially different from the estimate of the effect size (table 3).
Table 3.
GRADEpro level of quality evidence assessment
| Educational intervention compared with usual care for patients with type 2 diabetes | ||||||
| Patient or population: patients with type 2 diabetes Setting: Intervention: educational interventions Comparison: usual care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) |
Number of participants (studies) |
Certainty of the evidence (GRADE) |
Comments | |
| Risk with comparison | Risk with intervention | |||||
| Glycaemic control (HbA1c) measured with difference in mean HbA1c level after intervention Scale from 1 month to 12 months |
– | MD 0.83 lower (1.17 lower to 0.49 lower) |
– | 2474 (19 RCTs) |
⨁⨁⨁◯ Moderatea, b |
|
| Diabetes knowledge assessed with diabetes and medication knowledge Scale from 1 month to 12 months |
– | SMD 1.16 SD higher (0.71 higher to 1.6 higher) |
– | 1309 (10 RCTs) |
⨁⨁◯◯ Lowc, d |
|
GRADE Working Group grades of evidence: high certainty—we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty—we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty—our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect. Very low certainty—we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect.
*The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
GRADE, Grading of Recommendations Assessment, Development and Evaluation; HbA1c, glycosylated haemoglobin; MD, mean difference; RCTs, randomised controlled trials; SMD, standardised mean difference.
Discussion
Currently, diabetes has emerged as a public health problem that needs effective educational interventions which apply across age, ethnicities and socioeconomic levels. Evidence showed that appropriate self-management education is a vital component of clinical care to improve glycaemic levels and change behavioural outcomes.70 In the current meta-analysis, to generate high-quality evidence, only clinical trial studies were included.
This review summarises 19 RCT studies of educational interventions involving 2708 study participants with T2DM that took place in different global regions and health systems. In the present meta-analysis, findings demonstrated that educational intervention has a promising effect on glycaemic control and diabetes knowledge. The finding revealed that educational interventions reduced HbA1c levels by 0.83% (95% CI: 1.17 % to 0.49%) among patients with T2DM. This finding has a substantial degree of heterogeneity (I2=88%) indicating variation between included studies. However, there was a slight reduction of MD after sensitivity analysis, 0.70% (95% CI: 0.96 % to 0.44%), with a moderate degree of heterogeneity (I2=73%). Our findings are supported by previous meta-analyses, which reported that behavioural and self-management education have a significant benefit in the reduction of HbA1c levels in patients with diabetes.28 37 38
The improvement in glycaemic levels is considered to be clinically essential. The UK Diabetes Study revealed that with each 1% reduction in HbA1c, there is a likelihood of reducing the risk of diabetes complications by 21%.71 Similarly, a previous study showed that achieving optimal glycaemic level is likely to reduce the risk of deaths from diabetes complications, such as cardiovascular and cerebrovascular problems.72 Moreover, the ADA recognises that diabetes self-management has a vital role in improving glycaemic levels and reducing diabetes-related complications.73
In the current meta-analysis, a subgroup analysis was conducted based on the duration of the educational interventions. Concerning duration of interventions, there was a variation between <3 months, 3–6 months and >6 months in the reduction of HbA1c levels. In this meta-analysis, the pooled effect size for short educational interventions (duration ≤3 months) was better than the effect size of longer interventions (duration 3–6 months and >6 months), −1.09 (95% CI: −1.60 to –0.57, p<0.001). One possible explanation may be associated with the initial motivation of the participant to be empowered to obtain positive results in a short period.74 In contrast, previous studies reported that longer duration of interventions was more likely related to a significant reduction in HbA1c levels.28 75 76 Similarly, a meta-analysis study showed that more contact hours were associated with a reduction of HbA1c level.33 Moreover, evidence also supported that the duration of contact hours between trainer and patient has a substantial impact on HbA1c levels.18 The current findings reflect that the duration of intervention would influence the effectiveness of the educational intervention among patients with T2DM. Therefore, this disparity should be considered when developing future educational interventions.
In the present review, a subgroup analysis was conducted based on intervention design (theory-based vs empirical educational). Our study indicated that educational interventions benefited all patients regardless of the intervention design. In the current findings, empirical educational intervention showed improvement in glycaemic control level, −1.03 (95% CI: −1.90 to –0.15, p<0.001). Similarly, evidence showed that interactive self-management interventions through evidence-based approaches and structured curricula are crucial to improve glycaemic control and behavioural outcomes.77 However, another review indicates that in patients with T2DM, theory-based self-management educational interventions improved HbA1c.36 Although one-third of the included studies used an empirical approach in designing interventions, and favourable results on glycaemic control were obtained, their specific role in educational interventions has been debated.
In this review, diabetes knowledge showed a significantly higher standardised mean score of correct knowledge of diabetes among the intervention group as compared with the standard care group (SMD=1.16; 95% CI: 0.71 to 1.60, p<0.001). Similarly, educational interventions were associated with significant improvements in knowledge of diabetes being reported in the previous meta-analyses.78 79 Moreover, there is evidence that education improves knowledge and subsequently promotes behavioural changes among patients with end-stage renal disease.80 Though significant changes were observed in diabetes knowledge, this finding should be interpreted with caution due to the significant degree of heterogeneity among included studies.
Limitations
Our study has some limitations that need to be considered in the future. First, studies published in the English language were only considered for this systematic review. Second, there was variation in the included studies in terms of healthcare providers, component of interventions, outcome measures and intervention methods. Third, global representativeness must be considered as it was not possible to identify evidence from all countries of the globe. Fourth, although all the included studies were randomised controlled trials, some trials had biases, such as lack of allocation concealment, blinding and intention-to-treat analysis.
Conclusion
This systematic review adds to the body of knowledge that suggests that structured diabetes self-management education and support contribute to improving glycaemic outcomes and diabetes knowledge. Therefore, clinicians could make an effort to provide such care to ensure glycaemic control and to improve knowledge of T2DM. Further research is needed to determine the clinical significance of these improvements and their cost-effectiveness.
Implications for practice
Overall, these data revealed that educational interventions provide a basic benchmark to reduce glycaemic levels and to improve knowledge of T2DM. Importantly, to implement a successful education intervention, it is necessary to consider the duration of intervention and intervention design (empirical education is more effective) in patients with T2DM. Therefore, clinicians should use educational interventions to improve glycaemic control and diabetes knowledge among patients with T2DM. However, before making a practice decision based on the current review, further information from other reviews considering how the role of educational intervention reduced glycaemic level and improved diabetes knowledge should be taken into account. Hence, the certainty of this evidence is not adequate to conclude that interventions will be effective among patients with T2DM.
Implications for research
Further research is likely to change the estimated effect size of educational interventions in glycaemic control and knowledge of patients with T2DM. Knowledge of diabetes was assessed using different tools, outcome data were measured in heterogeneous ways. Based on this review, future studies of educational interventions would increase our certainty of evidence whether these interventions improve knowledge of diabetes or not by overcoming limitations of existing studies. Therefore, future educational intervention studies should be designed to evaluate individual-centred outcomes and become new priorities to support in clinical decision-making.
Supplementary Material
Footnotes
Contributors: WSS, YAA and TY developed the protocol and were involved in the design, selection of study, data extraction, statistical analysis and developing the initial drafts of the manuscript. AMK, WSS, PMP and MD were involved in data extraction, quality assessment, statistical analysis and revision. WSS and YAA prepared and edited the final draft of the manuscript. All authors read and approved the final draft of the manuscript. WSS has taken the full responsibility for the work and/or the conduct of the study, had access to the data and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information. All relevant data are within the paper and supporting information files. There is no separate data set to share.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Fan W. Epidemiology in diabetes mellitus and cardiovascular disease. Cardiovasc Endocrinol 2017;6:8–16. 10.1097/XCE.0000000000000116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roglc G, Varghese C, Cowan M. Global report on diabetes (World Health Organization). WHO Library Cataloguing-in-publication Data, 2016. [Google Scholar]
- 3.Cho NH, Shaw JE, Karuranga S, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 2018;138:271–81. 10.1016/j.diabres.2018.02.023 [DOI] [PubMed] [Google Scholar]
- 4.International diabetes federation . IDF diabetes atlas teB, Belgium. International Diabetes Federation, 2015. [Google Scholar]
- 5.Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 2018;14:88–98. 10.1038/nrendo.2017.151 [DOI] [PubMed] [Google Scholar]
- 6.Lyles CR, Grothaus L, Reid RJ, et al. Communication about diabetes risk factors during between-visit encounters. Am J Manag Care 2012;18:807–15. [PubMed] [Google Scholar]
- 7.Meng X-H, Huang Y-X, Rao D-P, et al. Comparison of three data mining models for predicting diabetes or prediabetes by risk factors. Kaohsiung J Med Sci 2013;29:93–9. 10.1016/j.kjms.2012.08.016 [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . Global report on diabetes, 2016. [Google Scholar]
- 9.American Diabetes Association . 6. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care 2020;43:S66–76. 10.2337/dc20-S006 [DOI] [PubMed] [Google Scholar]
- 10.Gibbons CH, Goebel-Fabbri A. Microvascular complications associated with rapid improvements in glycemic control in diabetes. Curr Diab Rep 2017;17:48. 10.1007/s11892-017-0880-5 [DOI] [PubMed] [Google Scholar]
- 11.Haghighatpanah M, Nejad ASM, Haghighatpanah M, et al. Factors that correlate with poor glycemic control in type 2 diabetes mellitus patients with complications. Osong Public Health Res Perspect 2018;9:167–74. 10.24171/j.phrp.2018.9.4.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dutta T, Kudva YC, Persson X-MT, et al. Impact of long-term poor and good glycemic control on metabolomics alterations in type 1 diabetic people. J Clin Endocrinol Metab 2016;101:1023–33. 10.1210/jc.2015-2640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lau CY, Qureshi AK, Scott SG. Association between glycaemic control and quality of life in diabetes mellitus. J Postgrad Med 2004;50:189–93. [PubMed] [Google Scholar]
- 14.Degli Esposti L, Saragoni S, Buda S, et al. Glycemic control and diabetes-related health care costs in type 2 diabetes; retrospective analysis based on clinical and administrative databases. Clinicoecon Outcomes Res 2013;5:193–201. 10.2147/CEOR.S41846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Control Group, Turnbull FM, Abraira C, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia 2009;52:2288–98. 10.1007/s00125-009-1470-0 [DOI] [PubMed] [Google Scholar]
- 16.Hemmingsen B, Lund SS, Gluud C, et al. Intensive glycaemic control for patients with type 2 diabetes: systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. BMJ 2011;343:d6898. 10.1136/bmj.d6898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharifirad G, Najimi A, Hassanzadeh A, et al. Application of BASNEF educational model for nutritional education among elderly patients with type 2 diabetes: improving the glycemic control. J Res Med Sci 2011;16:1149–58. [PMC free article] [PubMed] [Google Scholar]
- 18.Norris SL, Lau J, Smith SJ, et al. Self-Management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159–71. 10.2337/diacare.25.7.1159 [DOI] [PubMed] [Google Scholar]
- 19.Ellis SE, Speroff T, Dittus RS, et al. Diabetes patient education: a meta-analysis and meta-regression. Patient Educ Couns 2004;52:97–105. 10.1016/S0738-3991(03)00016-8 [DOI] [PubMed] [Google Scholar]
- 20.Deakin TA MC, Cade JE, Williams R. Group based training for self‐management strategies in people with type 2 diabetes mellitus. Cochrane database of systematic reviews 2005;18:CD003417. 10.1002/14651858.CD003417.pub2 [DOI] [PubMed] [Google Scholar]
- 21.Soundarya M, Asha A, Mohan V. Role of a diabetes educator in the management of diabetes. Int J Diabetes Dev Ctries 2004;24:65–8. [Google Scholar]
- 22.Berikai P, Meyer PM, Kazlauskaite R, et al. Gain in patients' knowledge of diabetes management targets is associated with better glycemic control. Diabetes Care 2007;30:1587–9. 10.2337/dc06-2026 [DOI] [PubMed] [Google Scholar]
- 23.Hartz A, Kent S, James P, et al. Factors that influence improvement for patients with poorly controlled type 2 diabetes. Diabetes Res Clin Pract 2006;74:227–32. 10.1016/j.diabres.2006.03.023 [DOI] [PubMed] [Google Scholar]
- 24.Rhee MK, Slocum W, Ziemer DC, et al. Patient adherence improves glycemic control. Diabetes Educ 2005;31:240–50. 10.1177/0145721705274927 [DOI] [PubMed] [Google Scholar]
- 25.Hussain Z, Alkharaiji M, Idris I. Evaluating the effect of inpatient diabetes education on length of stay, readmission rates and mortality rates: a systematic review. Br J Diabetes 2020;20:96–103. 10.15277/bjd.2020.256 [DOI] [Google Scholar]
- 26.Healy SJ, Black D, Harris C, et al. Inpatient diabetes education is associated with less frequent Hospital readmission among patients with poor glycemic control. Diabetes Care 2013;36:2960–7. 10.2337/dc13-0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bukhsh A, Khan TM, Sarfraz Nawaz M, et al. Association of diabetes knowledge with glycemic control and self-care practices among Pakistani people with type 2 diabetes mellitus. Diabetes Metab Syndr Obes 2019;12:1409–17. 10.2147/DMSO.S209711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Azami G, Soh KL, Sazlina S-G, et al. Behavioral interventions to improve self-management in Iranian adults with type 2 diabetes: a systematic review and meta-analysis. J Diabetes Metab Disord 2018;17:365–80. 10.1007/s40200-018-0376-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American diabetes association, the American association of diabetes educators, and the Academy of nutrition and dietetics. The Diabetes Educ 2017;43:40–53.28118121 [Google Scholar]
- 30.Powers MA, Bardsley JK, Cypress M, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Sci Diabetes Self Manag Care 2021;47:54–73. 10.1177/0145721720987936 [DOI] [PubMed] [Google Scholar]
- 31.Bos M, Agyemang C. Prevalence and complications of diabetes mellitus in northern Africa, a systematic review. BMC Public Health 2013;13:387. 10.1186/1471-2458-13-387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Somannavar S, Lanthorn H, Deepa M. Increased awareness about diabetes and its complications in a whole city: Effectiveness of the “prevention, awareness, counselling and evaluation”[PACE] Diabetes Project [PACE-6]. J Assoc Physicians India 2008;56:495–502. [PubMed] [Google Scholar]
- 33.Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns 2016;99:926–43. 10.1016/j.pec.2015.11.003 [DOI] [PubMed] [Google Scholar]
- 34.Schapira MM, Swartz S, Ganschow PS, et al. Tailoring educational and behavioral interventions to level of health literacy: a systematic review. MDM Policy Pract 2017;2:238146831771447–74. 10.1177/2381468317714474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murugesan N, Snehalatha C, Shobhana R, et al. Awareness about diabetes and its complications in the general and diabetic population in a City in southern India. Diabetes Res Clin Pract 2007;77:433–7. 10.1016/j.diabres.2007.01.004 [DOI] [PubMed] [Google Scholar]
- 36.Zhao F-F, Suhonen R, Koskinen S, et al. Theory-based self-management educational interventions on patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. J Adv Nurs 2017;73:812–33. 10.1111/jan.13163 [DOI] [PubMed] [Google Scholar]
- 37.Hildebrand JA, Billimek J, Lee J-A, et al. Effect of diabetes self-management education on glycemic control in Latino adults with type 2 diabetes: a systematic review and meta-analysis. Patient Educ Couns 2020;103:266–75. 10.1016/j.pec.2019.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aquino JA, Baldoni NR, Flôr CR, et al. Effectiveness of individual strategies for the empowerment of patients with diabetes mellitus: a systematic review with meta-analysis. Prim Care Diabetes 2018;12:97–110. 10.1016/j.pcd.2017.10.004 [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McGowan J, Sampson M, Salzwedel DM, et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 2016;75:40–6. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 41.Higgins JP. Cochrane Handbook for systematic reviews of interventions version 5.0. 1. The Cochrane Collaboration, 2008. http://wwwcochrane-handbookorg [Google Scholar]
- 42.Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration, 2011. [Google Scholar]
- 43.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 44.Guyatt GH, Oxman AD, Kunz R, et al. What is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995–8. 10.1136/bmj.39490.551019.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.GRADEpro G . GRADEpro guideline development tool [software], 2015. McMaster University
- 46.Borenstein M, Hedges LV, Higgins JPT, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010;1:97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 47.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cohen J. Statistical power analysis for the behavioral sciences. Academic press, 2013. [Google Scholar]
- 49.Egger M, Smith GD, Schneider M. Bias in meta-analysis detected by a simple, graphical test. increase in studies of publication bias coincided with increasing use of meta-analysis. BMJ 1997;316:629–34. [Google Scholar]
- 50.Sterne JAC, Sutton AJ, Ioannidis JPA, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 51.Cani CG, Lopes LdaSG, Queiroz M, et al. Improvement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital. Clinics 2015;70:102–6. 10.6061/clinics/2015(02)06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.MdFF G, Neumann CR, Scain SF, et al. Diabetes education in primary care: a randomized clinical trial. Cadernos de Saude Publica 2016;32:e00097115. 10.1590/0102-311X00097115 [DOI] [PubMed] [Google Scholar]
- 53.Zheng F, Liu S, Liu Y, et al. Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: a randomized controlled trial. J Diabetes Res 2019;2019:1–7. 10.1155/2019/1073131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jiang X-J, Jiang H, Lu Y-H, et al. The effectiveness of a self-efficacy-focused structured education programme on adults with type 2 diabetes: a multicentre randomised controlled trial. J Clin Nurs 2019;28:3299–309. 10.1111/jocn.14908 [DOI] [PubMed] [Google Scholar]
- 55.Kong J-X, Zhu L, Wang H-M, et al. Effectiveness of the chronic care model in type 2 diabetes management in a community health service center in China: a group randomized experimental study. J Diabetes Res 2019;2019:1–12. 10.1155/2019/6516581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hermanns N, Kulzer B, Maier B, et al. The effect of an education programme (MEDIAS 2 ICT) involving intensive insulin treatment for people with type 2 diabetes. Patient Educ Couns 2012;86:226–32. 10.1016/j.pec.2011.05.017 [DOI] [PubMed] [Google Scholar]
- 57.Braun AK, Kubiak T, Kuntsche J, et al. SGS: a structured treatment and teaching programme for older patients with diabetes mellitus--a prospective randomised controlled multi-centre trial. Age Ageing 2009;38:390–6. 10.1093/ageing/afp056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Didarloo A, Shojaeizadeh D, Alizadeh M. Impact of educational intervention based on interactive approaches on beliefs, behavior, hemoglobin A1c, and quality of life in diabetic women. Int J Prev Med 2016;7:38. 10.4103/2008-7802.176004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Askari A, Jeihooni AK, Kashfi SM, et al. The effect of educational program based on belief, attitude, subjective norm, and enabling factors model on changing the metabolic indices in elderly patients with type II diabetes. Int J Prev Med 2018;9:74. 10.4103/ijpvm.IJPVM_308_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Azami G, Soh KL, Sazlina SG, et al. Effect of a nurse-led diabetes self-management education program on glycosylated hemoglobin among adults with type 2 diabetes. J Diabetes Res 2018;2018:1–12. 10.1155/2018/4930157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ebrahimi H, Sadeghi M, Amanpour F, et al. Evaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial study. Prim Care Diabetes 2016;10:129–35. 10.1016/j.pcd.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 62.Nejhaddadgar N, Darabi F, Rohban A, et al. The effectiveness of self-management program for people with type 2 diabetes mellitus based on PRECEDE-PROCEDE model. Diabetes Metab Syndr 2019;13:440–3. 10.1016/j.dsx.2018.08.016 [DOI] [PubMed] [Google Scholar]
- 63.Tan MY, Magarey JM, Chee SS, et al. A brief structured education programme enhances self-care practices and improves glycaemic control in Malaysians with poorly controlled diabetes. Health Educ Res 2011;26:896–907. 10.1093/her/cyr047 [DOI] [PubMed] [Google Scholar]
- 64.Ramadas A, Chan CKY, Oldenburg B, et al. Randomised-controlled trial of a web-based dietary intervention for patients with type 2 diabetes: changes in health cognitions and glycemic control. BMC Public Health 2018;18:716. 10.1186/s12889-018-5640-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hörnsten A, Stenlund H, Lundman B, et al. Improvements in HbA1c remain after 5 years--a follow up of an educational intervention focusing on patients' personal understandings of type 2 diabetes. Diabetes Res Clin Pract 2008;81:50–5. 10.1016/j.diabres.2008.02.005 [DOI] [PubMed] [Google Scholar]
- 66.Adolfsson ET, Walker-Engström M-L, Smide B, et al. Patient education in type 2 diabetes: a randomized controlled 1-year follow-up study. Diabetes Res Clin Pract 2007;76:341–50. 10.1016/j.diabres.2006.09.018 [DOI] [PubMed] [Google Scholar]
- 67.Wichit N, Mnatzaganian G, Courtney M, et al. Randomized controlled trial of a family-oriented self-management program to improve self-efficacy, glycemic control and quality of life among Thai individuals with type 2 diabetes. Diabetes Res Clin Pract 2017;123:37–48. 10.1016/j.diabres.2016.11.013 [DOI] [PubMed] [Google Scholar]
- 68.Jayasuriya R, Pinidiyapathirage MJ, Jayawardena R, et al. Translational research for diabetes self-management in Sri Lanka: a randomized controlled trial. Prim Care Diabetes 2015;9:338–45. 10.1016/j.pcd.2015.01.014 [DOI] [PubMed] [Google Scholar]
- 69.Fan M-H, Huang B-T, Tang Y-C, et al. Effect of individualized diabetes education for type 2 diabetes mellitus: a single-center randomized clinical trial. Afr Health Sci 2016;16:1157–62. 10.4314/ahs.v16i4.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.American Diabetes Association . Standards of Medical Care in Diabetes-2019 Abridged for Primary Care Providers. Clin Diabetes 2019;37:11–34. 10.2337/cd18-0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405–12. 10.1136/bmj.321.7258.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Association AD . Implications of the diabetes control and complications trial. Diabetes Care 2002;25:S25–7. 10.2337/diacare.25.2007.S25 [DOI] [PubMed] [Google Scholar]
- 73.American Diabetes Association . (4) foundations of care: education, nutrition, physical activity, smoking cessation, psychosocial care, and immunization. Diabetes Care 2015;38 Suppl:S20–30. 10.2337/dc15-S007 [DOI] [PubMed] [Google Scholar]
- 74.Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes 2004;22:123–7. 10.2337/diaclin.22.3.123 [DOI] [Google Scholar]
- 75.McEwen MM, Pasvogel A, Gallegos G, et al. Type 2 diabetes self-management social support intervention at the U.S.-Mexico border. Public Health Nurs 2010;27:310–9. 10.1111/j.1525-1446.2010.00860.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Glazier RH, Bajcar J, Kennie NR, et al. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care 2006;29:1675–88. 10.2337/dc05-1942 [DOI] [PubMed] [Google Scholar]
- 77.Rickheim PL, Weaver TW, Flader JL, et al. Assessment of group versus individual diabetes education: a randomized study. Diabetes Care 2002;25:269–74. 10.2337/diacare.25.2.269 [DOI] [PubMed] [Google Scholar]
- 78.Creamer J, Attridge M, Ramsden M, et al. Culturally appropriate health education for type 2 diabetes in ethnic minority groups: an updated cochrane review of randomized controlled trials. Diabet Med 2016;33:169–83. 10.1111/dme.12865 [DOI] [PubMed] [Google Scholar]
- 79.Cheng L, Sit JWH, Choi K-C, et al. Effectiveness of interactive self-management interventions in individuals with poorly controlled type 2 diabetes: a meta-analysis of randomized controlled trials. Worldviews Evid Based Nurs 2017;14:65–73. 10.1111/wvn.12191 [DOI] [PubMed] [Google Scholar]
- 80.Tsay S-L, Hung L-O. Empowerment of patients with end-stage renal disease--a randomized controlled trial. Int J Nurs Stud 2004;41:59–65. 10.1016/S0020-7489(03)00095-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information. All relevant data are within the paper and supporting information files. There is no separate data set to share.