Highlights
-
•
The prevalence of regular alcohol use was the highest among adolescents in Zambia but the lowest in Senegal.
-
•
The prevalence of problematic alcohol use was higher in Argentina and Colombia than in any other low- and middle-income countries.
-
•
The prevalence of regular and problematic alcohol use was the lowest in countries with Muslim and Buddhist religions.
-
•
Samoa had the highest prevalence of smoking as well as in marijuana and amphetamine consumption.
Keywords: Adolescents, Substance use, Country-specific risk factors, Global School-based Student Health Survey, Low-and middle-income countries
Abstract
Introduction
Adolescence is a critical developmental stage for the initiation of substance use worldwide. However, the prevalence of various types of substances consumed by adolescents living in low- and middle- income countries (LMICs) across different continents is not fully understood.
The aims of the present study were to estimate the prevalence of regular and problematic substance use among adolescents in 73 LMICs across different continents and to explore the role of country-specific factors on this prevalence.
Method
Data of 314,187 adolescents (52.79% girls; median age = 15 years old) who participated in the Global School-based Student Health Survey (GSHS) were analysed. After estimating the weighted prevalence for each country, multilevel models were used to examine the influence of country-specific factors on the prevalence of substance use across 73 LMICs.
Results
The results indicated that problematic alcohol use was more prevalent in LMICs with higher income levels. The prevalence of regular alcohol use was the highest in Zambia. Regular and problematic alcohol use was the least prevalent in Senegal and Myanmar. The findings also revealed that smoking and the consumption of marijuana and amphetamine were the most common among adolescents in Samoa, whereas the prevalences for these substances were the lowest in Laos.
Conclusion
Economic wealth, religion and geographical factors seem to have a role in determining the prevalence of substance use among adolescents in LMICs.
1. Introduction
Adolescence is a critical developmental stage for the initiation of substance use (United Nations Office on Drugs and Crime; UNODC, 2018). As recently reported by the World Health Organization (WHO, 2021), substance use is one of the main risk taking behaviours during adolescence which could have an impact on adolescent’s mental and physical well-being. Moreover, it is well-documented the elevated costs asociated with adolescent substance use, in terms of healthcare service utilisation, criminality rate, and school truancy (Maynard et al., 2017, Miller and Hendrie, 2008). The most commonly used substances during the adolescence period are tobacco and alcohol; these substances tend to be consumed first before illicit drugs (Degenhardt, Stockings, Patton, Hall & Lynskey, 2016).
Drinking alcohol among adolescents is a major concern in many countries. It is often associated with an increase of risky behaviours, such as unsafe sex or dangerous driving and is an underlying cause of injuries, violence and premature deaths (Gillman et al., 2018, Hagström et al., 2018, Hohl et al., 2017). Worldwide, more than a quarter of young people aged 15–19 years are current drinkers, which is estimated to affect 155 million adolescents (WHO, 2021). The prevalence of heavy episodic drinking among adolescents aged 12–18 years ranged between 5% and 20%, observing higher rates with age (Jang et al., 2017, Wartberg et al., 2018). However, the prevalence of alcohol use varied across countries. According to the report by the Pan American Health Organization [PAHO], (2015), adolescents in the Americas had higher prevalence of alcohol consumption than adolescents in other countries; however, it is important to note that although adolescents in the Americas, on average, drink less frequently, they consume more per occasion when they drink.
Adolescent tobacco and illicit drug use are also of health concerns worldwide. Approximately 80% of adult smokers have their first cigarette prior to the age of 18 years (WHO, 2021). In relation to illicit drug use, cannabis/ marijuana is considered as the most commonly used drug among adolescents (Weier and Gary, 2016). Other illicit drug such as amphetamine is also commonly used among adolescents (15–16 year old) in most parts of the world (e.g., Europe, Middle East, Asia and North America) (UNODC, 2018). Our knowledge on the prevalence of substance use in adolescents is mostly related to specific substance (e.g., marijuana) and in a specific country, however, little is known about the prevalence of the various types of substances consumed by adolescents living in low- and middle- income countries (LMICs) across different continents.
Although adolescence is associated with the initation of substance use, contextual factors (e.g., geographical location, economic factors, religion) have also been identified as risk factors for substance consumption in this age group. For example, the data from World Bank in 2017 showed that individuals from LMICs had higher prevalence of smoking than those in high-income countries (Marquez & Moreno-Dodson, 2017). By 2030, more than 80% of the world’s tobacco-related deaths are projected to occur in LMICs (WHO, 2017). The major reasons of higher prevalence of tobacco use in LMICs were related to intensive tobacco farming and to the lack of tobacco monitoring systems and programmes to prevent young people from smoking (World Health Organization (WHO), 2017, Yin et al., 2019). As reported by Pengpid and Peltzer (2019) 8.1% of pre-adolescents (aged less than 12 years old) from LMICs (e.g., Laos, Philippines, Thailand) smoked tobacco, and 8.1% consumed alcohol and 4% have tried other drugs (i.e., marijuana and amphetamines).
Other factors which have been linked to a high prevalence of substance use in LMICs were the geographical location (UNODC, 2018). Most of these LMICs were in the continents (e.g., Oceania, East and South-East Asia) which have the fastest-growing methamphetamine markets and are located on the drug trafficking routes (Ranada, 2016; UNODC, 2018). Religion also seems to have an important role on substance consumption (e.g., Adamczyk and Palmer, 2008, Adesina et al., 2020, Ford and Hill, 2012, Hoffmann and Bahr, 2014, Silva et al., 2006). Specifically, the prevalence of alcohol use has been reported to be less prevalent among adolescents from Muslim than adolescents from Christian background; this finding was explained in terms of substance use being explicitly condemned and that alcohol use is restricted or even forbidden in Islam (Adesina et al., 2020, Bolakale and Markus, 2015, Silva et al., 2006).
Due to the negative impact of substance use among adolescents (e.g., associated with unsafe sex or dangerous driving, violence and premature deaths) (WHO, 2021), it is important to identify its prevalence among adolescents in a wide range of LMICs. While the previous studies have provided information on the prevalence of substance use in some LMICs, it is unclear whether these findings could be generalizable to LMICs in different continents. Thus, the aim of the present study was to estimate the prevalence of regular and problematic substance use (30-day regular alcohol drinking, binge drinking, heavy drinking, smoking and marijuana use; and lifetime amphetamine use) among adolescents from 73 LMICs. Another aim was to explore the extent to which the prevalence of substance use is associated with country-specific factors, including geographical location, economic factors, and religion.
2. Method
2.1. Study sample
This original study used data from the Global school-based Student Health Survey (GSHS) which is a school-based survey conducted among students aged 13–17 years from LMICs across the world. The overall aim of the GSHS was to collect data on leading causes of morbidity and mortality among children and adults worldwide (i.e., dietary behaviours and lifestyle routines, drug use, hygiene and other protective and risk factors). The survey was developed by the World Health Organization (WHO) in collaboration with the United States Centers for Disease Control and Prevention (CDC) and other United Nations allies. Data and further details on the GSHS study protocols are publicly available data at: http://www.who.int/chp/gshs and http://www.cdc.gov/gshs.
The GSHS presented a hierarchical structure in terms of field study implementation. In this regard, the CDC served as a project coordinator centre. An official country-level agency oversaw survey delivery, data collection and storage. Survey procedures were designed to ensure participants' privacy by allowing for anonymous and confidential participation.
The GSHS relies on a 2-stage (i.e., schools and classrooms) cluster sampling to obtain nationally representative estimates. Participating schools were randomly selected upon the census of government schools at a country level. Classrooms were also randomly selected within schools. All the adolescents from the selected classrooms were eligible to be enrolled. Adolescents whose parents (or legal guards) handed in the signed consent were surveyed. Participants completed a self-administered survey on a regular class day. Country level ethics review boards approved the GSHS, and informed consent was obtained from the students, parents and/or school officials before the administration of the survey.
The present study analysed data of adolescents from 73 LMICs, according to the World Bank income level classification (31.51% African countries, 27.40% American countries, 31.51% Asian countries, and 9.59% Oceanian countries) (see: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups) when the survey was conducted between 2003 and 2017. The total sample size comprised 314,187 adolescents (52.79% girls; median age = 15 years old). Details on sample features and survey year by country are displayed in Table 1.
Table 1.
Sample features by country.
| Country | n | Survey year | Sex (% girls) | Age (median) |
|---|---|---|---|---|
| Afghanistan | 2579 | 2014 | 57.94 | 15 |
| Algeria | 4532 | 2011 | 51.97 | 14 |
| Argentina | 28,368 | 2012 | 52.25 | 15 |
| Bangladesh | 2989 | 2014 | 60 | 14 |
| Belize | 2112 | 2011 | 52.81 | 14 |
| Benin | 2536 | 2016 | 45.73 | 16 or older |
| Bhutan | 7576 | 2016 | 54.81 | 16 or older |
| Bolivia | 3696 | 2012 | 49.31 | 14 |
| Botswana | 2197 | 2005 | 55.05 | 15 |
| Cambodia | 3806 | 2013 | 52.79 | 16 or older |
| China | 9015 | 2003 | 51.02 | 14 |
| Colombia | 9907 | 2007 | 54.72 | 14 |
| Costa Rica | 2679 | 2009 | 51.78 | 14 |
| Djibouti | 1777 | 2007 | 42.9 | 15 |
| Dominica | 1642 | 2009 | 56.41 | 14 |
| Ecuador | 5524 | 2007 | 51.43 | 13 |
| Egypt | 2568 | 2011 | 53.32 | 13 |
| El Salvador | 1915 | 2013 | 46.2 | 14 |
| Eswatini | 3680 | 2013 | 52.36 | 16 or older |
| Ghana | 3632 | 2012 | 46.24 | 16 or older |
| Grenada | 1542 | 2008 | 55.06 | 14 |
| Guatemala | 4374 | 2015 | 50.58 | 14 |
| Guyana | 2392 | 2010 | 56.22 | 14 |
| Honduras | 1779 | 2012 | 52 | 14 |
| India | 8130 | 2007 | 44.33 | 14 |
| Indonesia | 11,142 | 2015 | 54.19 | 14 |
| Iraq | 2038 | 2012 | 43.51 | 14 |
| Jamaica | 1667 | 2017 | 54.38 | 15 |
| Jordan | 2197 | 2007 | 43.8 | 15 |
| Kenya | 3691 | 2003 | 51.34 | 14 |
| Kiribati | 1582 | 2011 | 56.41 | 14 |
| Laos | 3683 | 2015 | 54.4 | 16 or older |
| Lebanon | 5708 | 2017 | 59.12 | 15 |
| Liberia | 2744 | 2017 | 47.55 | 16 or older |
| Libya | 2242 | 2007 | 57.05 | 14 |
| Malawi | 2359 | 2009 | 53.45 | 14 |
| Malaysia | 25,507 | 2012 | 49.99 | 15 |
| Maldives | 3493 | 2014 | 57.6 | 15 |
| Mauritania | 2063 | 2010 | 52.58 | 15 |
| Mauritus | 3012 | 2017 | 52.84 | 15 |
| Mongolia | 5238 | 2013 | 56.67 | 15 |
| Morocco | 6745 | 2016 | 46.93 | 15 |
| Mozambique | 1918 | 2015 | 46.67 | 16 or older |
| Myanmar | 2838 | 2016 | 53.73 | 14 |
| Namibia | 4531 | 2013 | 52.71 | 16 or older |
| Nauru | 578 | 2011 | 58.12 | 14 |
| Nepal | 6529 | 2015 | 53.04 | 14 |
| Pakistan | 5192 | 2009 | 24.83 | 14 |
| Paraguay | 3149 | 2017 | 52.45 | 15 |
| Peru | 2882 | 2010 | 51.05 | 15 |
| Philippines | 8761 | 2015 | 54.44 | 15 |
| Samoa | 2418 | 2011 | 58.65 | 14 |
| Senegal | 3154 | 2005 | 45.13 | 14 |
| Solomon Islands | 1421 | 2005 | 48.12 | 15 |
| Sri Lanka | 3262 | 2016 | 55.68 | 15 |
| Santa Lucia | 1276 | 2007 | 57.53 | 14 |
| Saint Vincent | 1333 | 2007 | 52.71 | 14 |
| Sudan | 2211 | 2012 | 61.34 | 15 |
| Suriname | 2126 | 2016 | 50.76 | 15 |
| Syria | 3102 | 2010 | 59.93 | 14 |
| Tajikistan | 9714 | 2006 | 49.95 | 15 |
| Tanzania | 3793 | 2014 | 52.06 | 14 |
| Thailand | 5894 | 2015 | 56.88 | 14 |
| Timor Leste | 3704 | 2015 | 53.6 | 16 or older |
| Tonga | 3333 | 2017 | 54.11 | 14 |
| Tunisia | 2870 | 2008 | 51.31 | 14 |
| Tuvalu | 943 | 2013 | 51.5 | 14 |
| Uganda | 3215 | 2003 | 48.6 | 15 |
| Vanuatu | 2159 | 2016 | 56.41 | 15 |
| Venezuela | 4415 | 2003 | 55.3 | 13 |
| Vietnam | 3331 | 2013 | 53.13 | 15 |
| Zambia | 2257 | 2004 | 51.14 | 15 |
| Zimbabwe | 5665 | 2003 | 55.43 | 15 |
Note. The upper bound of the age variable (i.e., 16 years or older) was collapsed to make a common metric across countries.
n = Number of participants.
2.2. Substance use and risk factors
Regular alcohol use was defined by consuming alcoholic drinks 20 or more days a month. It was measured by using the question, “During the past 30 days, on how many days did you have at least one drink containing alcohol?”
Problematic alcohol use: In line with the U.S. Department of Health and Human Services and U.S. Department of Agriculture (2015), two forms of problematic alcohol use were examined: (a) binge drinking (i.e., engaging in episodes of 4 or more drinks for women and 5 or more drinks for men), and (b) heavy drinking (i.e., having binge drinking episodes on 5 or more days in the past month).
Regular smoking was defined by smoking 20 or more cigarettes in the last month. The participants were asked the following question, “During the past 30 days, on how many days did you use any tobacco products other than cigarettes, such as shisha/hookah, electronic cigarettes, snuff, chewing tobacco, pipe, curut, cigar, cigarillo, or bidis?”.
Other drugs: Regular marijuana use was considered when adolescent reported a use of 10 times or more in a month. Marijuana use was measured by the question, “During the past 30 days, how many times have you used marijuana?” Finally, lifetime amphetamine use was defined as using amphetamines 10 times or more in the entire life (Peltzer & Pengpid, 2017).
Risk Factors: All the data related to risk factors were taken for the survey year across countries. First, the continent was used as a measure of geographical location of country. The income level (defined as the gross domestic product in $; collected from the World Bank database, see: https://data.worldbank.org/indicator/ NY.GDP.MKTP. KD.ZG) and health expenditure (i.e., percentage of gross domestic product devoted to health care services; data taken from the WHO database, https://apps.who.int/nha/database) were considered as economic risk factors. The study also included urbanity rate (i.e., percentage of country citizens that live in urban areas); urbanity data were collected from the United Nations Department of Economic and Social Affairs report (2019). Finally, predominant religion in each country was derived from the Pew Research Center Religion & Public Life (2015) report.
2.3. Data analysis
Weighted prevalence was estimated for each country, using the weights provided by the GSHS data curators to ensure generalisation of results to the entire target population (see Centers for Disease Control and Prevention & World Health Organization, 2013).
Meta-analytic techniques were used to summarise the results that were derived from pooling country-specific weighted prevalence estimates. The overall weighted prevalence was estimated for each of the outcome (i.e., 30-day regular alcohol drinking, binge drinking, heavy drinking, smoking and marijuana use; and lifetime amphetamine use) under random-effects models, using the Freeman-Tukey double-arcsine transformation to asymptotically stabilise country-specific variance (Rücker et al., 2009). The z-based statistic was used to test whether the overall prevalence estimate was significantly different from zero.
Meta-analytic random-effects regression was used to analyse the role of risk factors (i.e., continent, income level, health expenditure, urbanity rate, and predominant religion) in explaining the overall prevalence estimates. The odds ratio estimate was provided as a predictor loading. The R2 estimate was used to account for outcome heterogeneity explaining by predictors.
Overall prevalence and regression parameters were estimated using restricted maximum likelihood algorithms (see Schwarzer et al., 2014). All the analyses were conducted using the R software (R Core Team, 2017), with packages meta, metafor, Hmisc, and psych.
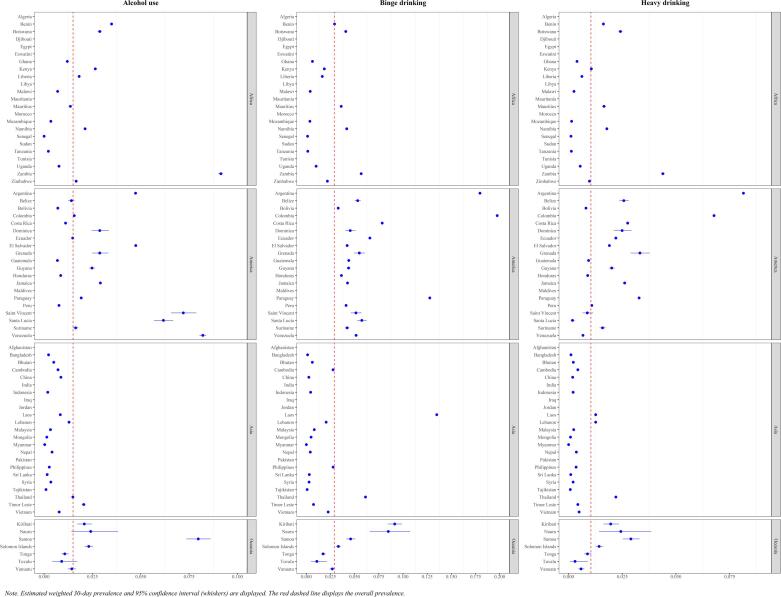
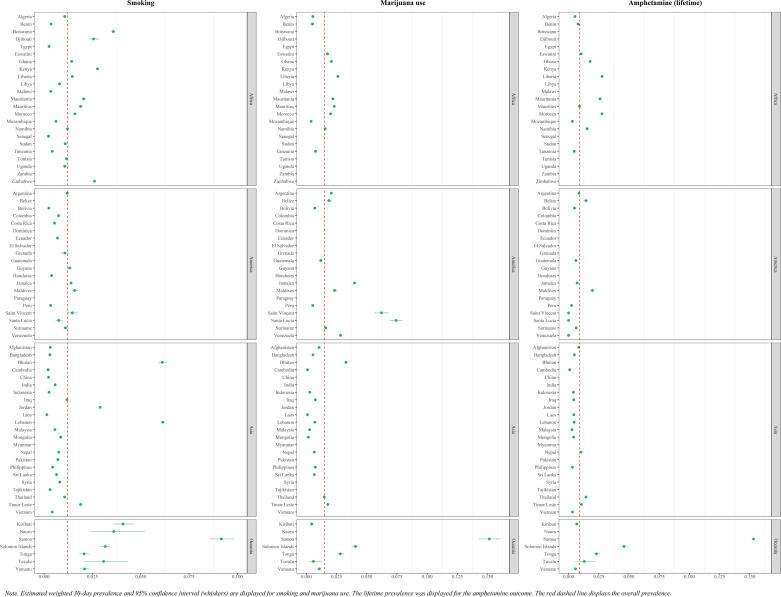
3. Results
Weighted prevalence of substance use by country was displayed in Fig. 1 (alcohol use) and Fig. 2 (smoking, marijuana use, and lifetime amphetamine use). The prevalences of regular alcohol use were estimated to range from 0.00 (Senegal) to 0.09 (Zambia). The prevalence of binge drinking was estimated to range from 0.00 (Myanmar) to 0.20 (Colombia). On the other hand, heavy drinking estimates oscillated between 0.00 (Myanmar) to 0.08 (Argentina). With regards to regular smoking, the lowest prevalence estimates were shown in Laos (0.00) but the highest estimates were in Samoa (0.09). Similarly, for marijuana use, the lowest prevalence estimates were found in Laos (0.00) and the highest prevalence was found in Samoa (0.15). Finally, the country with the highest lifetime prevalence of amphetamine use was Samoa (weighted prevalence = 0.15).
Fig. 1.
Estimated prevalence for alcohol outcome. Note. Estimated weighted 30-day prevalence and 95% confidence interval (whiskers) are displayed. The red dashed line displays the overall prevalence.
Fig. 2.
Estimated prevalence for smoking, marijuana and amphetamine outcomes. Note. Estimated weighted 30-day prevalence and 95% confidence interval (whiskers) are displayed for smoking and marijuana use. The lifetime prevalence was displayed for the amphetamine outcome. The red dashed line displays the overall prevalence.
Overall prevalence estimates were displayed in Table 2. All the estimated prevalence rates were significantly different from zero. The overall prevalence of alcohol use in the last 30 days was 0.015 (CI95 = 0.010, 0.017). The prevalence of problematic alcohol use was slightly higher than the prevalence of binge drinking (overall prevalence = 0.029, CI95 = 0.021, 0.039) and a slightly lower prevalence of heavy drinking (overall prevalence = 0.010, CI95 = 0.007, 0.014). The results suggested that 1.5% of adolescents from the LMICs drink alcohol on a regular basis in the last month. Almost 3% of adolescents engaged in binge drinking, and 1% were engaged in heavy drinking.
Table 2.
Overall prevalence across substance use outcomes.
| k | Prevalence | LBCI95 | UBCI95 | Z | |
|---|---|---|---|---|---|
| Alcohol | |||||
| Use | 58 | 0.015 | 0.010 | 0.017 | 13.49 |
| Binge episode | 58 | 0.029 | 0.021 | 0.039 | 12.94 |
| Heavy drinking | 58 | 0.010 | 0.007 | 0.014 | 13.03 |
| Tobacco smoking | 65 | 0.012 | 0.009 | 0.015 | 16.35 |
| Marijuana use | 44 | 0.015 | 0.010 | 0.020 | 11.79 |
| Amphetamine use (lifetime) | 43 | 0.009 | 0.006 | 0.013 | 9.69 |
Note. Overall 30-day prevalence (except for amphetamine use) was estimated under random effects model.
k = Number of countries in analysis. LBCI95 = 95% confidence lower bound. UBCI95 = 95% confidence upper bound. Z = Contrast statistic (all significant with p < .01).
With regards to smoking, 1.2% of adolescents reported smoking on a regular basis in the last month (overall prevalence = 0.012, CI95 = 0.009 0.015), and 1.5% of adolescents reported smoking marijuana (overall prevalence = 0.015, CI95 = 0.010, 0.020). The overall lifetime prevalence for amphetamine use was relatively low, being 0.009 (CI95 = 0.006, 0.013).
The meta-regression models provided some evidence on country factors with a significant loading on the weighted prevalence (see Table 2, Table 3). Regarding alcohol consumption, countries in which Muslim religion was predominant showed lower prevalence than countries in which Christian religion was majority (OR between 0.88 and 0.94, p < .05). Moreover, income level was associated with higher prevalence of binge drinking (OR = 1.03, CI95 = 1.01, 1.04; p < .01) and heavy drinking (OR = 1.02, CI95 = 1.01, 1.04; p < .01). Oceanian countries showed a higher prevalence of regular smoking (OR = 1.08, CI95 = 1.03, 1.14; p < .01) and a lifetime prevalence of amphetamine (OR = 1.10, CI95 = 1.03, 1.19; p < .01), in comparison to Asian countries. Finally, the prevalence of marijuana use was associated with higher income level (OR = 1.02, CI95 = 1.00, 1.04; p < .05) and lower urbanity rate (OR = 0.97, CI95 = 0.95, 0.99; p < .05) (see Table 4).
Table 3.
Factors to predict prevalence of alcohol-related prevalence.
| Alcohol |
Binge episode |
Heavy drinking episode |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | CI95 | Z | OR | CI95 | Z | OR | CI95 | Z | |
| Continent (ref. = Asia) | |||||||||
| Africa | 1.01 | 0.95, 1.07 | 0.18 | 0.98 | 0.91, 1.06 | −0.52 | 1.01 | 0.96, 1.05 | 0.25 |
| America | 1.01 | 0.94, 1.09 | 0.32 | 1.05 | 0.96, 1.14 | 0.97 | 1.02 | 0.96, 1.07 | 0.53 |
| Oceania | 1.03 | 0.96, 1.10 | 0.75 | 1.03 | 0.94, 1.13 | 0.67 | 1.01 | 0.96, 1.07 | 0.48 |
| Income level | 1.02 | 1.00, 1.04 | 1.71 | 1.03 | 1.01, 1.06 | 2.58** | 1.02 | 1.01, 1.04 | 3.19** |
| Health expenditure | 1.00 | 0.98, 1.02 | 0.34 | 1.00 | 0.98, 1.03 | 0.31 | 1.01 | 0.99, 1.02 | 0.77 |
| Urbanicity | 1.00 | 0.98, 1.02 | 0.13 | 1.02 | 1.00, 1.05 | 1.59 | 1.01 | 0.99, 1.03 | 1.21 |
| Religion (ref. = Christian) | |||||||||
| Muslim | 0.92 | 0.85, 0.98 | −2.51* | 0.88 | 0.81, 0.96 | −2.80** | 0.94 | 0.89, 0.99 | −2.40* |
| Other | 0.95 | 0.89, 1.00 | −1.88 | 0.97 | 0.90, 1.04 | −0.87 | 0.97 | 0.93, 1.01 | −1.46 |
| R2 | 0.30 | 0.50 | 0.46 | ||||||
Note. The outcome was the country-specific prevalence, under loglinear transformation.
OR = Odds ratio. CI95 = 95% confidence interval for the OR. Z = Z-based contrast test.
* p < .05; ** p < .01.
Table 4.
Factors to predict prevalence of smoking-related and amphetamine prevalence.
| Tobacco smoking |
Marijuana smoking |
Amphetamine (lifetime) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | CI95 | Z | OR | CI95 | Z | OR | CI95 | Z | |
| Continent (ref. = Asia) | |||||||||
| Africa | 1.00 | 0.97, 1.04 | 0.10 | 1.03 | 0.98, 1.09 | 1.08 | 1.04 | 0.99, 1.10 | 1.53 |
| America | 0.96 | 0.92, 1.01 | −1.47 | 1.07 | 0.99, 1.14 | 1.79 | 1.00 | 0.93, 1.06 | −0.13 |
| Oceania | 1.08 | 1.03, 1.14 | 3.10** | 1.07 | 0.99, 1.15 | 1.74 | 1.10 | 1.03, 1.19 | 2.65** |
| Income level | 1.01 | 1.00, 1.03 | 1.71 | 1.02 | 1.00, 1.04 | 2.12* | 1.01 | 0.99, 1.03 | 1.28 |
| Health expenditure | 1.01 | 0.99, 1.02 | 0.78 | 0.99 | 0.98, 1.01 | −0.58 | 1.00 | 0.98, 1.02 | −0.08 |
| Urbanicity | 1.01 | 0.99, 1.02 | 0.98 | 0.97 | 0.95, 0.99 | −2.52* | 0.98 | 0.96, 1.01 | −1.39 |
| Religion (ref. = Christian) | |||||||||
| Muslim | 0.99 | 0.95, 1.02 | −0.83 | 0.99 | 0.93, 1.04 | −0.47 | 1.02 | 0.96, 1.07 | 0.54 |
| Other | 0.98 | 0.94, 1.02 | −0.87 | 0.97 | 0.91, 1.03 | −0.91 | 0.99 | 0.93, 1.05 | −0.31 |
| R2 | 0.29 | 0.28 | 0.24 | ||||||
Note. The outcome was the country-specific prevalence, under loglinear transformation.
OR = Odds ratio. CI95 = 95% confidence interval for the OR. Z = Z-based contrast test. GNI = Gross national income per capita.
* p < .05; ** p < .01.
4. Discussion
The present study examined the prevalence of substance use (i.e., 30-day regular alcohol drinking, binge drinking, heavy drinking, regular smoking and regular marijuana use; and lifetime amphetamine use) among adolescents in LMICs from various geographical locations and continents. The major strength of this study was its large sample size, consisting of data of 314,187 adolescents from 73 LMICs in four different continents (i.e., Africa, America, Asia and Oceania).
Our findings showed variation in the prevalence of different types of substance use (i.e., regular alcohol use, binge and heavy drinking, smoking, marijuana and amphetamine) within and between the LMICs in different continents. In line with previous research (e.g., PAHO, 2015), there was a higher prevalence of problematic alcohol use in the Americas which could be related to their increasing economic wealth in recent years that is associated with more production, marketing and easier access to alcohol in this region. For example, Argentina is characterized as a wine-industry and that wine is never taxed which in turn contributes to the highest per-capita alcohol consumption. Moreover, alcohol policy issues deserve mentioning to explain the increased prevalence of alcohol use outcomes among Argentinian adolescents. In this regard, some studies have found a relationship between problematic alcohol use and early alcohol initiation among Argentinian adolescents and the higher alcohol exposure through movies, advertisements and other media sources observed in this country (Mejia et al., 2016, Probst et al., 2018). Similarly, in Colombia, alcohol consumption begins early since it is mostly seen as a normal practice within the community (Gomez, Scoppetta & Alarcon, 2011).
An interesting finding was the differences in the prevalence of regular alcohol consumption across LMICs in Africa, which could potentially be explained in terms of the contextual differences. For example, the prevalence of regular alcohol use was the highest in Zambia but the lowest in Senegal. In contrast to the finding that problematic alcohol use was more prevalent in economically developing regions such as the Americas, the prevalence of regular alcohol use was the highest in Zambia although it has the highest levels of poverty and inequality globally (The World Bank, 2021). In this sense, other factors should be considered at a community and public health level. First, this finding could be related to the fact that social drinking is a widely accepted behavior in Zambian culture (e.g., Hammerstein et al., 2017). Second, the relaxed policy on direct marketing of alcohol products undertaken by the Zambian government in the times of GSHS implementation may also be behind this higher alcohol outcome prevalence (Swahn, Ali, Palmier, Sikazwe, & Mayeya, 2011).
The lowest prevalence of regular alcohol consumption was in Senegal which could be explained by the religion in Senegal where large majority of the population is Muslim. This finding supported previous research which indicated low level of alcohol use in Muslim societies since alcohol use is restricted or even forbidden in Islam (Adesina et al., 2020, Bolakale and Markus, 2015, Silva et al., 2006). The low prevalence of both binge and heavy drinking in Myanmar could also be related to religion. The major religion in Myanmar is Buddhism which forbids the consumption of alcohol and drugs (Htin et al., 2014).
Our findings revealed that Samoa had the highest prevalence of smoking and marijuana and amphetamine consumption. One possible reason of this finding could be that Samoa is located in East Asia and Pacific, which has the fastest-growing methamphetamine markets (UNODC, 2018; The World Bank, 2021). The estimates by the Institute for Health Metrics and Evaluation (IHME, 2012) also revealed that 20% of people in the world smoke tobacco but the regions where many people smoke are clustered in South-East Asia and Pacific regions. In these regions, adolescents have easy access to substances via production and marketing. Another reason could be that high population of people who are smoking and/or using marijuana/amphetamine might serve as a role model (e.g., parents, peers) for adolescents to develop addictive behaviours (Brooks et al., 2012, Pratt et al., 2010).
In contrast to some previous studies (e.g., Pengpid & Peltzer, 2019), the lowest prevalence of smoking, marijuana and amphetamine use was in Asia and mostly in Laos. This finding would be related to increasing investments in education and health sector in relation to the prevention of substance use (The World Bank, 2021) and that majority of the people in Laos belong to Buddhism which forbids substance consumption (Htin, et al., 2014).
Some limitiations of this study should also be considered when interpreting our findings. GSHS data were based on self-report questionnaires which might be affected by social desirability and reporting biases because the use of substances particularly illicit drugs are highly stigmatised in some LMICs. Therefore, it is likely that the adolescents did not report the full account of their substance use. To overcome this methodological limitation, future studies should include some objective measures to test the consumption of illicit drug such as urine test. Furthermore, the GSHS data were collected in a cross-sectional design, which limits to draw a causal direction in findings which arises the need for more longitudinal studies on the multi risk factors of substance use among adolescents in LMICs. On the other hand, the GSHS relies on a school-based design. Unfortunately, an elevated number of adolescents does not attend school in LMIC (UNESCO Institute for Statistics, 2018). Therefore, the results from this study should be taken cautiously and limited to schooled adolescents. Further studies using more inclusive designs should be conducted to make a wider picture on substance use prevalence among LMIC adolescents. Finally, some country-specific GSHS surveys were delivered almost 20 years ago (e.g., the Uganda or Senegal survey). Further studies should provide prevalence estimates relying on more recent surveys to have an updated picture on substance use epidemiology across LMIC.
Overall, this study has demonstrated that substance use among adolescents in LMICs in specific countries in Asia, Africa, Americas and Oceania is a common public health problem. The findings also drew attention for the urgent need to develop or strengthen the prevention/intervention programmes, drug policies and professional support with the aim of reducing substance use among adolescents in these countries. Public policies to restrict substance exposure (e.g., alcohol advertisement) may become decisive to hinder the escalition of problematic substance use among adolescents from LMIC. Moreover, reducing barries to accessing mental health care by providing practical facilities (e.g., telehealth) may help tackle the lure of problematic substance use in a vulnerable population, as adolescent population is. It is hoped that future research will expand on these findings and will draw a more clear profile of multifactorial risks of substance use among adolescents in more LMICs with more diverse sociocultural, economic and religious profiles.
Author Agreement
All authors have seen and approved the final version of this manuscript. We confirm that the article is our original work, has not received prior publication and is not under consideration for publication elsewhere.
CRediT authorship contribution statement
ADL: Conceptualization, Undertook the analyses and interpreted the results, review & editing. FO: Conceptualization, Writing - original draft, Writing - review & editing. CAE: Review & editing, Critique the output for important intellectual content, provided theoretical support.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This paper uses data from the Global School-Based Student Health Survey (GSHS). GSHS is supported by the World Health Organization and the US Centers for Disease Control and Prevention.
References
- Adamczyk A., Palmer I. Religion and initiation into marijuana use: The deterring role of religious friends. Journal of Drug Issues. 2008;38(3):717–741. [Google Scholar]
- Adesina B.O., Adebayo A.M., Iken O.F. Factors associated with psychoactive substance use among in-school adolescents in Zaria local government area, Kaduna State, Nigeria: A cross-sectional study. International Journal of School Health. 2020;7(1):14–22. [Google Scholar]
- Bolakale A.S., Markus B.Y. Factors influencing drug use and abuse among undergraduate sudents of a tertiary institution in Nigeria. International Journal of Science and Research. 2015;6(8):2012–2018. [Google Scholar]
- Brooks F.M., Magnusson J., Spencer N., Morgan A. Adolescent multiple risk behaviour: An asset approach to the role of family, school and community. Journal of Public Health. 2012;34(suppl 1):i48–i56. doi: 10.1093/pubmed/fds001. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, & World Health Organization. (2013). 2013 GSHS Data User’s Guide. Retrieved from https://www.cdc.gov/gshs/pdf/gshs-data-users-guide.pdf.
- Degenhardt L., Stockings E., Patton G., Hall W.D., Lynskey M. The increasing global health priority of substance use in young people. Lancet Psychiatry. 2016;3(3):251–264. doi: 10.1016/S2215-0366(15)00508-8. [DOI] [PubMed] [Google Scholar]
- Ford J.A., Hill T.D. Religiosity and adolescent substance use: Evidence from the national survey on drug use and health. Substance Use & Misuse. 2012;47(7):787–798. doi: 10.3109/10826084.2012.667489. [DOI] [PubMed] [Google Scholar]
- Gillman A.S., Yeater E.A., Feldstein Ewing S.W., Kong A.S., Bryan A.D. Risky sex in high-risk adolescents: Associations with alcohol use, marijuana use, and co-occurring use. AIDS and Behavior. 2018;22(4):1352–1362. doi: 10.1007/s10461-017-1900-9. [DOI] [PubMed] [Google Scholar]
- Gómez A.P., Scoppetta O., Alarcón L.F. Age at onset of alcohol consumption and risk of problematic alcohol and psychoactive substance use in adulthood in the general population in Colombia. The Journal of International Drug, Alcohol and Tobacco Research. 2011;1:19–24. [Google Scholar]
- Hagström H., Hemmingsson T., Discacciati A., Andreasson A. Alcohol consumption in late adolescence is associated with an increased risk of severe liver disease later in life. Journal of Hepatology. 2018;68(3):505–510. doi: 10.1016/j.jhep.2017.11.019. [DOI] [PubMed] [Google Scholar]
- Hammerstein N., Paul R., Ncheka J. Increasing problem of alcohol abuse among the Zambian population in the psychiatric setting. Health Press Zambia Bull. 2017;1(4) [Google Scholar]
- Hoffmann J.P., Bahr S.J. Parenting style, religiosity, peer alcohol use, and adolescent heavy drinking. Journal of Studies on Alcohol and Drugs. 2014;75(2):222–227. doi: 10.15288/jsad.2014.75.222. [DOI] [PubMed] [Google Scholar]
- Hohl B.C., Wiley S., Wiebe D.J., Culyba A.J., Drake R., Branas C.C. Association of Drug and Alcohol Use With Adolescent Firearm Homicide at Individual, Family, and Neighborhood Levels. JAMA Internal Medicine. 2017;177(3):317–324. doi: 10.1001/jamainternmed.2016.8180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Htin K., Howteerakul N., Suwannapong N., Tipayamongkholgul M. Smoking, alcohol consumption and betal-quid chewing among young adult Myanmar laborers in Thailand. Southeast Asian Journal of Tropical Medicine and Public Health. 2014;45(4):926–939. [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation . IHME; WA: 2012. Financing Global Health 2012: The end of the golden age? Seattle. [Google Scholar]
- Jang J.B., Patrick M.E., Keyes K.M., Hamilton A.D., Schulenberg J.E. Frequent Binge Drinking Among US Adolescents, 1991 to 2015. Pediatrics. 2017;139(6) doi: 10.1542/peds.2016-4023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez P.V.M., Moreno-Dodson B. At the Crossroads of Health and Development. 2017. Tobacco Tax Reform. [Google Scholar]
- Maynard B.R., Vaughn M.G., Nelson E.J., Salas-Wright C.P., Heyne D.A., Kremer K.P. Truancy in the United States: Examining temporal trends and correlates by race, age, and gender. Children and Youth Services Review. 2017;81(May):188–196. doi: 10.1016/j.childyouth.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejia R., Pérez A., Abad-Vivero E.N., Kollath-Cattano C., Barrientos-Gutierrez I., Thrasher J.F., Sargent J.D. Exposure to alcohol use in motion pictures and teen drinking in Latin America. Alcoholism: Clinical and Experimental Research. 2016;40(3):631–637. doi: 10.1111/acer.12986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, T., & Hendrie, D. (2008). Substance abuse prevention dollars and cents: A cost-benefit analysis. In Substance Abuse and Mental Health Services Administration (Issue DHHS Pub. No. (SMA) 07-4298).
- Pan American Health Organization (PAHO). (2015). Regional Status Report on Alcohol and Health in the Americas. Washington, DC. Retrieved from https://www.paho.org/hq/dmdocuments/2015/Alcohol-Report-Health-Americas-2015.pdf.
- Peltzer K., Pengpid S. Cannabis and amphetamine use among adolescents in five Asian countries. Central Asian Journal of Global Health. 2017;6(1) doi: 10.5195/cajgh.2017.288. Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pengpid S., Peltzer K. Early substance use initiation and psychological distress among adolescents in five ASEAN countries: A cross-sectional study. Psychology Research and Behavior Management. 2019;12:1003–1008. doi: 10.2147/PRBM.S223624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center Religion & Public Life. (2015). The Future of World Religions: Population Growth Projections, 2010-2050. Retrieved from https://www.pewforum.org/2015/04/02/religious-projections-2010-2050/.
- Pratt T.C., Cullen F.T., Sellers C.S., Thomas Winfree L., Madensen T.D., Daigle L.E.…Gau J.M. The empirical status of social learning theory: A meta-analysis. Justice Quarterly. 2010;27(6):765–802. [Google Scholar]
- Probst C., Monteiro M., Smith B., Caixeta R., Merey A., Rehm J. Alcohol policy relevant indicators and alcohol use among. Journal of Studies on Alcohol and Drugs. 2018;79(1):49–57. [PubMed] [Google Scholar]
- R Core Team. (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing. Retrieved from https://www.r-project.org/.
- Ranada, P. (2016). A Look at the State of Crime, Drugs in the Philippines. Retreived from https://www.rappler.com/nation/crime-drugs-philippines.
- Rücker G., Schwarzer G., Carpenter J., Olkin I. Why add anything to nothing? The arcsine difference as a measure of treatment effect in meta-analysis with zero cells. Statistics in Medicine. 2009;28(5):721–738. doi: 10.1002/sim.v28:510.1002/sim.3511. [DOI] [PubMed] [Google Scholar]
- Schwarzer, G., Carpenter, J. R., & Rücker, G. (2014). Meta-analysis with R. Springer International Publishing Switzerland. Retrieved from https://doi.org/10.1007/978-3-319-21416-0_5.
- Silva, L. V., Malbergier, A., Stempliuk, V. D. A., & Andrade, A. G. D. (2006). Factors associated with drug and alcohol use among university students. Revista de saúde pública, 40(2), 280-288. [DOI] [PubMed]
- Swahn M.H., Ali B., Palmier J.B., Sikazwe G., Mayeya J. Alcohol marketing, drunkenness, and problem drinking among zambian youth: Findings from the 2004 global school-based student health survey. Journal of Environmental and Public Health. 2011;2011:1–8. doi: 10.1155/2011/497827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNESCO Institute for Statistics. (2018). One in five children, adolescents and youth is out of school. In UNESCO Institute for Statistics Sustainable Development Goals Report: Vol. Fact Sheet (Issue 48). http://uis.unesco.org.
- United Nations. Department of Economic and Social Affairs report. (2019). World Urbanization Prospects. The 2018 Revision. New York. Retrieved from https://population.un.org/wup/Publications/Files/WUP2018-Report.pdf.
- United Nations Office on Drugs and Crime (UNODC) (2018). World Drug Report 2018. Vienna.
- Wartberg L., Kriston L., Thomasius R. Depressive Symptoms in Adolescents. Deutsches Arzteblatt international. 2018;115(33–34):549–555. doi: 10.3238/arztebl.2018.0549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weier, M., Gary, Chan, G.C.K., Quinn, C., Q., Hides, L., & Hall. W. (2016). Cannabis use in 14 to 25 years old Australians 1998 to 2013. Centre for Youth Substance Abuse Research Monograph No. 1 (Brisbane, Australia, Centre for Youth Substance Abuse, 2016). Retrieved from https://ncysur.centre.uq.edu.au/files/405/Cannabis%20technical%20report.pdf.
- The World Bank Prevalence of deaths through substance abuse, mental health and road accidents differ by region. 2021. https://blogs.worldbank.org/opendata/prevalence-deaths-through-substance-abuse-mental-health-and-road-accidents-differ-region Retrieved from.
- World Health Organization (WHO) (2017). WHO report on the global tobacco epidemic 2017: Monitoring tobacco use and prevention policies. Retrieved from: https://www.who.int/tobacco/global_report/2017/en/.
- World Health Organization (WHO) (2021). Fact Sheet: Adolescent and Young Adult Health. Retrieved from https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions.
- Yin, S., Ahluwalia, I. B., Palipudi, K., Mbulo, L., & Arrazola, R. A. (2019). Are there hardened smokers in low- and middle-income countries? Findings from the Global Adult Tobacco Survey. Tobacco induced diseases, 17(11). Retrieved from https://doi.org/10.18332/tid/100631. [DOI] [PMC free article] [PubMed]