Abstract
Introduction
The dynamic interplay between parent depressive symptoms and child internalizing behavior over time is not well understood.
Methods
We used data from a prospective parent-offspring adoption design (N = 561) to examine associations between adoptive parent depressive symptoms and child internalizing behavior when children were ages 18 months, 27 months, 4.5 years, and 6 years, and subsequent child psychiatric disorder symptoms when children were between the ages of 6 to 8 years. Models also accounted for the contributions of birth parent psychopathology, birth mother depressive symptoms during pregnancy, and infant negative emotionality. Bidirectional associations between adoptive parent depressive symptoms and child internalizing behavior were examined using a random-intercept cross-lagged panel model.
Results
There was evidence for associations between child internalizing behavior and adoptive parent depressive symptoms over time, with mothers’ depressive symptoms being a more salient risk factor for child internalizing behavior than fathers’. We found one significant cross-lagged association from adoptive mother depressive symptoms at child age 18 months to child internalizing behavior at age 27 months. Infant negative emotionality (i.e., emotional liability) at age 9 months predicted both child internalizing behavior and adoptive parent depressive symptoms.
Conclusion
Results suggest that postnatal maternal depressive symptoms confer specific risks for child internalizing behaviors in toddlerhood and childhood and depressive symptoms in childhood.
Keywords: Psychopathology, Risk Factors, Depression, Prospective Studies, Parents, Child Behavior
The dynamic interplay between parent depressive symptoms and child behavior problems on child psychiatric disorders: An adoption study
One out of six children age 2–8 has been diagnosed with a mental, behavior, or developmental disorder (Cree et al., 2018), and disorders often co-occur (Danielson et al., 2018; Ghandour et al., 2019). Psychiatric disorders that begin earlier in life are associated with long term deficits in social functioning (Donohue et al., 2020; Finsaas et al., 2020) and are challenging for children and their caregivers. They also place a significant burden on health care systems (Zima et al., 2016). The continuation of child internalizing behaviors to child psychiatric disorders is partially explained by rearing environment influences (Wichstrøm et al., 2017). Specifically, parent depression and depressive symptoms are a known environmental risk factor for internalizing behaviors and psychiatric disorders in early childhood (Bufferd et al., 2014; Netsi et al., 2018; Psychogiou et al., 2017; Wolford et al., 2017) and in middle childhood even after accounting for genetic risk (Gouze et al., 2021; Kerr, et al., 2013; Lewis et al., 2011; Natsuaki et al., 2014; Netsi et al., 2018). Genetics also play an important role in the transmission of risk (Flint & Kendler, 2014). Therefore, it is important to consider genetic influences when examining the environmental role of parent depressive symptoms on child symptoms. One method to isolate the postnatal, environmental transmission of parent depressive symptoms on child symptoms from genetic and prenatal effects is to use an adoption design where children are placed with non-relative adoptive parents around the time of birth. This study uses a parent-offspring adoption design, enrolling children who were placed with non-relative adoptive parents shortly after birth. Because the adoptees were reared by parents who were not genetically related to them, we can study the effects of postnatal environmental risks separate from genetic and prenatal influences.
Postnatal exposure to parent depressive symptoms consistently confers risk for child internalizing behaviors (Côté et al., 2018; Goodman et al., 2011; Kendler et al., 2008). For maternal depressive symptoms, one meta-analysis found small, yet consistent, effects of maternal depressive symptoms on child internalizing behavior and on general child psychopathology (Goodman et al., 2011). Most often, associations between maternal depressive symptoms and child internalizing behavior emerge when maternal depressive symptoms are assessed as a chronic exposure (i.e., aggregated over an extended period; Grabow et al., 2017; Pemberton et al., 2010) versus a time-specific exposure (Hails et al., 2018). This pattern is consistent with extant findings in which persistent maternal depressive symptoms are associated with increased risk for child internalizing behavior in early childhood and depression in adolescence (Netsi et al., 2018). Collectively, these studies indicate that persistent (between-person) and time-specific (between-dyad) maternal depressive symptoms should be examined to identify developmental periods during which the risk for internalizing problems is seeded.
Within this literature, fathers’ depressive symptoms have received substantially less attention than mothers’ depressive symptoms (Feldman et al., 2020; Taraban et al., 2020). This gap in research is important to fill because fathers experience higher rates of depression compared to the overall male population (10% vs. 5%), and up to 25% of fathers report experiencing postpartum depression during the first year of fatherhood (Paulson & Bazemore, 2010). Moreover, fathers’ depressive symptoms predict child internalizing behavior and psychiatric disorders, and effect sizes are similar to those of mothers’ (Goodman et al. 2011). Analyses based on our sample have found associations between adoptive father depressive symptoms during infancy and children’s behavior problems during toddlerhood (Pemberton et al., 2010) and internalizing symptoms at age 6 (Hails et al., 2018). In other samples, father depression has also been associated with child psychiatric disorders seven years later, in particular, Oppositional Defiant Disorder (ODD; Ramchandani et al., 2008). Moreover, paternal depressive symptoms are related to maternal depressive symptoms (Paulson & Bazemore, 2010), and when both parents experience heightened depressive symptoms, children are more likely to exhibit behavior problems (Volling et al., 2018). Thus, it is important to account for both parents’ depressive symptoms in studies of child internalizing behavior.
While we have summarized the potential heightend importance of chronic rearing parents’ depressive symptoms over time, there are opportunities for time-specific influences between parents and children throughout development. Transactional models of development propose that children and their environments affect each other (Sameroff & Mackenzie, 2003). Child exposure to maternal depression during the first year of life is a particularly salient risk factor for child internalizing behavior (Allen et al., 1998; Pratt et al., 2017; Verbeek et al., 2012). In toddlerhood, there is evidence that child internalizing behaviors predict maternal depressive symptoms, and improvements in child behavior are related to reductions in maternal depressive symptoms (Chazan-Cohen et al., 2007; Hails et al., 2018; Pemberton et al., 2010). Throughout childhood and adolescence, similar and more exaggerated patterns emerge such that maternal depressive symptoms predict child internalizing behaviors, and child internalizing behaviors exacerbate maternal depressive symptoms (Sellers et al., 2016; Yan & Dix, 2014). Moreover, child psychiatric disorders predict parent psychiatric disorders. For example, child depression in middle childhood (7–15 years) predicts parent depression approximately two years later (Wesseldijk et al., 2018). Thus, we expected to find associations between parent depressive symptoms in infancy (9 months) with toddler internalizing behaviors and concurrant associations between maternal depressive symptoms and child internalizing behaviors in childhood at age 6, based on pronounced associations that are evident in later childhood in prior studies.
Most studies of associations between child internalizing behavior and parent depressive symptoms include genetically related individuals. In such studies, it is unclear whether associations are explained by a shared genetic predisposition. Few models using a genetically-sensitive design have modelled transactional associations using a longitudinal latent variable design that can control for trait-like stability in parent depressive symptoms and child internalizing behaviors. Those that have used this approach have included few time points and have used regression approaches that do not account for trait-like stability in constructs (e.g., Chazan-Cohen et al., 2007; Pemberton et al., 2010), making it challenging to assess trait-like characteristics and sensitive points for changes over time. For example, Chazan-Cohen et al. (2007) assessed child behavior and maternal depressive symptoms at child ages 14, 24, and 36 months and two years later in prekindergarten. They used a regression mediation to identify child behavior improvements resulting from the intervention as a mediator of improved maternal depressive symptoms. Pemberton et al. (2010) used an adoption design, allowing for a separation estimates from the rearing environment and biological transmission, but only looked at child externalizing behaviors out to 27 months. Other examples of models exist but none to our knowledge have used a design that allows for the separation of depressive symptoms in the rearing environment from those that are transmitted due to genetic and prenatal risk, while also using a modelling approach that separates out trait-like stability to allow for an examination of contributions of parent depressive symptoms on child outcomes at specific time points.
The cross-lagged panel model (CLPM) has been previously used to estimate lagged influences in developmental models. However, prior research has highlighted that the CLPM does not adequately control for the trait-like or time-invariant nature of each construct, and thus leads to biased estimates of cross-lagged paths. To address limitations of the traditional CLPM, we use a random-intercept cross-lagged panel model (RI-CLPM). The RI-CLPM has been proposed as an anecdote to this dilemma because it allows for accurate estimates of reciprocal processes over time at the within-dyad level (Hamaker et al., 2015). Thus, the RI-CLPM provides an ideal approach to model the dynamic interplay between postnatal parent depressive symptoms and child behavior problems (Mund & Nestler, 2018) because it allows for an examination of reciprocal relations between parent depressive symptoms and child behavior problems as they unfold over time, while delineating within- and between-person effects (Hamaker et al., 2015).
Current Study
We used a prospective parent-offspring adoption design to examine the bidirectional paths between adoptive parent depressive symptoms (postnatal environmental influences) and child internalizing symptoms from age 9 months to age 6 years, and ultimately, how these influences jointly contributed to predict general child psychopathology and risk for residual psychiatric disorder symptoms. We accounted for contributions of birth parent psychopathology (genetic influences), birth mother depressive symptoms during pregnancy (prenatal risks), and infant negative emotionality. We used a RI-CLPM to enable the separation of between-person effects from time-specific effects. Therefore, we were able to separate associations between trait-like chronicity (e.g., between-person effects) from time-specific effects that examine changes in child symptoms as a function of parent symptoms over time, and vice versa (within-dyad effects).
We tested the following hypotheses: 1) adoptive mother and father chronic depressive symptoms (modelled respectively as latent constructs of depressive symptoms from age 9 months to age 6 years) would be related to the latent construct of child internalizing behavior and child psychiatric disorder symptoms from 18 months to age 6 years (between-person effects); 2) adoptive mother and father depressive symptoms during infancy (when children are 9 months of age) would be associated with child internalizing behavior at 18 months); and 3) child internalizing behavior at age 6 would demonstrate a time-specific association with concurrent adoptive parent depressive symptoms for both mothers and fathers.
Method
Participants
This study used data from the Early Growth and Development Study (EGDS; Leve et al., 2019). EGDS is a prospective, longitudinal study consisting of 561 linked sets of adoptive families (adopted child, adoptive parents, and birth parents), with data collected in two cohorts of 361 and 200 linked sets, respectively. Participants were recruited via 45 adoption agencies in 15 states across the United States (see Leve et al., 2019, for further description). Individuals were eligible for participation if: (1) the adoption was domestic, (2) the infant was placed with a non-relative adoptive family, (3) the infant was placed before 3 months of age (M = 7.11 days, SD = 13.28), (4) the infant had no known major medical conditions, and (5) the birth mother and adoptive parents could read or understand English at least at an eighth-grade level.
At the time of the adoptee’s birth, adoptive parents’ median total household income was between $100,000 and $125,000 and median educational attainment for adoptive mothers and adoptive fathers was at least a 4-year college degree (40% and 40%, respectively). Adoptive mother and adoptive father mean ages were 37.43 (SD = 6.03) and 38.28 (SD = 5.83) years old, respectively. Most adoptive mothers and adoptive fathers were White (92% and 90%, respectively), and the remainder were African American (4% and 5%, respectively), Latinx (2% and 2%, respectively), and “other” (2% and 3%, respectively). Adoptive parents were assessed in-person at the same time points as adoptees.
For birth parents, the median total household income was between $25,001 and $40,000 and the median educational attainment was a high school diploma (measured at 3 to 6 months post-partum). Birth parents typically had household incomes of less than $25,000. Birth mothers and birth fathers were 24.35 (SD = 6.03) and 26.05 (SD = 7.75) years old at the time of birth of the child, respectively. The majority of birth mothers and fathers were White (70% and 70%, respectively), and the remainder were African American (13% and 12%, respectively), Latinx (7% and 10%, respectively), and “other” (10% and 9%, respectively). Birth parents were assessed in-person when adoptees were ages 3 to 6 months, age 18 months, and again between ages 4 to 7 years old.
Measures
Adoptive parent depressive symptoms
Adoptive mothers and fathers self-reported their depressive symptoms when children were 9 months, 18 months, 27 months, 4.5 years, and 6 years of age. The Beck Depression Inventory (BDI; Beck et al., 1988) or Center for Epidemiologic Studies-Depression Scale (CES-D; Lewinsohn et al., 1997) was used at each time point. Scores were converted to z-scores for ease of comparison. The BDI was administered when children were 9 months (Cronbach’s α = .73, .73; adoptive mother and adoptive father, respectively), 18 months (Cronbach’s α = .79, .81), and 27 months (Cronbach’s α = .83, .86). The original BDI contains 21 items, but an item about suicidal ideation (item 9) was not included in the assessment. Scores on the BDI range from 0–60 with higher scores indicating greater severity of depression. The CES-D was administered when children were 4.5 years (Cronbach’s α = .86, .83) and 6 years (Cronbach’s α = .90, .85). The CES-D is 20 items, each rated on a scale of 0 to 3 for a range of scores from 0 to 60, with higher scores indicating a greater severity of depression.
Child internalizing behavior
Adoptive parents completed the Child Behavior Checklist (CBCL) to measure internalizing behavior at age 18 months, 27 months, 4.5 years, and 6 years. For children in Cohort I and children under age 6 in Cohort II, the preschool version of the internalizing scale was used (CBCL/1½‐5; Achenbach & Rescorla, 2000). For children in Cohort II who were age 6, the school age version was administered (CBCL/6‐18; Achenbach & Rescorla, 2001). Raw scores of total internalizing behaviors were converted into z-scores to create comparable factors. When available, adoptive mother and father report were averaged (r’s: 18 months = .42, 27 months = .51, 4.5 years = .29, 6 years = .44) at each time point prior to z-scoring (Cronbach’s α for adoptive mothers and fathers, respectively: 18 months = .73, .77; 27 months = .78, .80; 4.5 years = .86,.85; 6 years = .83, .83).
Child psychiatric disorder symptoms
When children were between 6 – 8 years of age, adoptive parents reported on their children’s psychiatric symptoms during the last three months, using the Preschool Age Psychiatric Assessment (PAPA). The PAPA is a developmentally-appropriate structured parent interview lasting approximately 100 minutes. It includes sections on a range of psychiatric symptoms (Egger et al., 2006). As a structured interview, it has the advantage of being keyed to DSM diagnostic criteria, improving the likelihood of accurate diagnosis as compared to the CBCL, which is considered a screening measure and often provides a basis for referral (Lavigne et al., 2016). Four variables were created from the PAPA: Depressive Disorder symptoms (DD), anxiety disorders symptoms (AD), Attention Deficit/Hyperactivity Disorder symptoms (ADHD), and Conduct Disorder and Oppositional Defiance Disorder symptoms (CD/ODD), each representing a continuous symptom count. DSM-IV symptom counts were derived using algorithms created by the instrument’s developers. For the full PAPA assessment summary score, interrater reliability was computed with percent agreement between two raters on 17% of the 396 PAPA assessments (IRR = 93%). A latent variable was estimated by loading all symptom variables onto a common child psychopathology higher order factor to account for overall child psychopathology and disorder-specific symptoms.
Covariates
Birth parent psychopathology.
An overall factor of birth mother and father psychopathology (‘p’ factor) was used to estimate overall liability or genetic risk for child internalizing behavior and psychiatric disorders (Marceau et al., 2019). This construct is a higher-order factor based on factor scores for two lower-order factors: internalizing problems and externalizing problems. Each of the lower order factors was computed using four indicators collected from birth parents at 18- and 54-months post-adoption: symptom count, diagnosis count, age of onset, and first-degree relatives with a disorder. For the first three indicators, the Composite International Diagnostic Instrument (Kessler & Üstün, 2004) and the Diagnostic Interview Schedule (Robins et al., 1981) were used to create birth parents counts for (a) number of disorders on the diagnostic interview, (b) number of symptoms endorsed on the diagnostic interview, and (c) age of onset of each disorder. For internalizing disorders, the diagnostic categories assessed included major depression, brief recurrent depression, dysthymia, separation anxiety, adult separation anxiety, social phobia, agoraphobia (with and without panic), panic disorder, specific phobia, and generalized anxiety. For externalizing disorders, the diagnostic categories assessed included CD, antisocial personality disorder, alcohol abuse and dependence, drug abuse and dependence, and tobacco dependence. For both externalizing and internalizing scores, episodes of prenatal symptoms were excluded. The fourth indicator was the proportion of first-degree relatives with either internalizing or externalizing problems. This indicator was calculated as the maximum proportion of first-degree relatives [mother, father, and up to three siblings] the birth parent rated as having externalizing problems, internalizing problems and/or substance use problems. Indicators were entered into a principal component analysis separately for each disorder and extracted factor scores were aggregated to create a composite score for internalizing symptoms and for externalizing symptoms and aggregated again to create the higher order, p factor. For additional information, see Marceau et al. (2019).
Infant negative emotionality.
At 9 months, the Infant Behavior Questionnaire (IBQ; Rothbart, 1981) was used to assess infant negative emotionality with the 20-item Distress to Limitations scale (Cronbach’s α = .83 and .83, adoptive mother and father report, respectively) and the 20-item Fearfulness scale (Cronbach’s α = .73 and .72, respectively) to control for symptoms before the first administration of the CBCL. When ratings from both adoptive mother and father were available (87% of the sample), a mean score was computed (r = .56 and .55, p < .05) for each scale. The Distress to Limitations scale and Fearfulness scales were then standardized and averaged to arrive at the final indicator for infant negative emotionality.
Prenatal and perinatal risk.
Birth mother depressive symptoms during pregnancy were collected at 3–6 months postpartum using 5 items from the Beck Depression Inventory (BDI; Beck et al., 1988; Cronbach’s α = .93). Additional prenatal and perinatal risk variables were assessed using the Perinatal Risk Index (PRI) developed for this study (Marceau et al., 2016) based on a modified version of the McNeil-Sjostrom Scale for Obstetric Complications (McNeil et al., 1994). The PRI includes birth mother self-report data collected at 3–6 months postpartum and from data extracted from prenatal care and delivery records.
Openness of adoption.
Degree of openness in adoption was assessed when children were 5–9 months of age using perceptions of the degree of contact between parties, as rated by the birth mother, adoptive mother, and adoptive father, to control for similarities that may result from contact between birth and adoptive families. Each participant rated the degree and nature of contact and communication with their counterpart (IRR = .66–.81, ps <.001) For additional information see Ge et al. (2008).
Child sex.
Child sex (coded as 0 for male and 1 for female) was included as a covariate given that girls typically experience more internalizing symptoms and disorders whereas boys typically experience more externalizing symptoms and disorders (Liu, 2004). However, sex differences were not examined as a primary hypothesis because sex differences in prevalence rates for internalizing disorders do not emerge until adolescence (Crawford et al., 2001; Martel, 2013).
Analytic Plan
Missing data were evaluated using Little’s test of missing data (Little, 1988) to identify if there were patterns in missing data. Little’s test of missingness was significant. Attrition analyses revealed that, compared to baseline characteristics, there were no differences between children, adoptive mothers, and adoptive fathers who were retained in the study compared to those who did not complete the final assessment. There were also no differences on birth mother variables for birth fathers who did and did not participate. Thus, it is unclear whether there was a mechanism for missingness. When data are not missing at random, full information maximum likelihood with structural equation modelling accounts for item measurement error and typically performs similarly to multiple imputation (Little et al., 2013), and was, thus, used in this study.
The RI-CLPM includes a latent intercept term to account for trait-like stability in parent depressive symptoms and child internalizing behavior (between-person effects), and, thus, provides an unbiased examination of reciprocal relations between parent depressive symptoms and child internalizing behavior as they unfold over time (within-dyad effects; Hamaker et al., 2015; Mund & Nestler, 2018). Using a RI-CLPM, we modelled the reciprocal transaction between adoptive parent depressive symptoms and child internalizing behavior while controlling for the trait-like stability of each construct. We included birth parent psychopathology, recalled birth mother prenatal depressive symptoms, and infant negative emotionality as predictors of the random intercepts of adoptive parent depressive symptoms and child internalizing behavior, the latent variable representing child psychopathology symptoms, and the residual symptoms, specific to each psychiatric disorder. The random intercepts of adoptive parent depressive symptoms and child internalizing behavior were also modelled to predict child psychopathology and residual disorder symptoms. We used a robust maximum likelihood to estimate the RI-CLPM because of the non-normal, positively skewed, residual distribution of the variables of interest (e.g., depressive symptoms; Kline, 2016). The RI-CLPM was run twice to examine distinct patterns between adoptive mother and father depressive symptoms and child internalizing behaviors: first, examining the reciprocal relations between adoptive mother depressive symptoms and child internalizing behavior, controlling for an observed composite of adoptive father depressive symptoms (adoptive mother RI-CLPM), and second, examining the reciprocal relations between adoptive father depressive symptoms and child internalizing behavior whilst controlling for an observed composite of adoptive mother depressive symptoms (adoptive father RI-CLPM).
Results
Table 1 presents correlations among study variables. Results from both models are presented in parentheses in the text and in Table 2, with adoptive mother RI-CLPM results first and adoptive father RI-CLPM results second. Figure 1 presents the adoptive mother RI-CLPM and Figure 2 presents the adoptive father RI-CLPM. Fit indices for the adoptive mother RI-CLPM indicated good fit to the data (Robust Comparative Fit Index (CFI) = .98; Standardized Root Mean Square Residual (SRMR) = .04; Robust Root Mean Square Error of Approximation (RMSEA) = .03) by standards reported in Hu and Bentler (1995). Indicators of adoptive mother depressive symptoms loaded onto a random intercept (std. coefs. = .59– .64) as did indicators of child internalizing behavior intercept (std. coefs. = .57– .61). Child psychiatric disorder symptoms loaded onto a common child psychopathology factor (DD std. coef. = .67, CD/ODD std. coef. = .48, ADHD std. coef. = .66, ANX std. coef. = .67). The second model specified correlations and cross-lagged paths between adoptive father depressive symptoms and child behavioral problems in the same manner as previously described for the adoptive mother RI-CLPM. Fit indices for the adoptive father RI-CLPM indicated good fit to the data (Robust CFI = .96; SRMR = .04; Robust RMSEA = .04). In this model, indicators of adoptive father depressive symptoms loaded onto a random intercept (std. coefs. = .68– .75) as did indicators of child internalizing behavior intercept (std. coefs. = .57– .61). Child psychiatric disorder symptoms loaded onto a common child psychopathology factor (DD std. coef. = .70, CD/ODD std. coef. = .47, ADHD std. coef. = .67, ANX std. coef. = .62).
Table 1.
Correlations Among Main Study Variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. BF p | |||||||||||||||||||||
| 2. BM p | .17* | ||||||||||||||||||||
| 3. BM pre dep | .18* | .07 | |||||||||||||||||||
| 4. Negative emo 9m | −.05 | −.00 | .06 | ||||||||||||||||||
| 5. AM dep 9m | .01 | .05 | −.03 | .12* | |||||||||||||||||
| 6. AM dep 18m | .01 | .02 | −.05 | .04 | .63* | ||||||||||||||||
| 7. AM dep 27m | .09* | .03 | −.04 | .09 | .56* | .62* | |||||||||||||||
| 8. AM dep 4.5y | −.03 | .01 | −.07 | .04 | .42* | .37* | .49* | ||||||||||||||
| 9. AM dep 6y | −.05 | −.05 | −.07 | .11* | .38* | .36* | .45* | .56* | |||||||||||||
| 10. AF dep 9m | .05 | −.01 | .02 | .14* | .10* | .11* | .10* | .02 | .02 | ||||||||||||
| 11. AF dep 18m | .07 | .06 | .03 | .11* | .10* | .17* | .19* | −.00 | .12* | .65* | |||||||||||
| 12. AF dep 27m | .04 | .07 | .01 | .03 | .07 | .11* | .22* | .04 | .20* | .58* | .73* | ||||||||||
| 13. AF dep 4.5y | .06 | .07 | .03 | .17* | .15* | .10 | .13* | .11* | .14* | .51* | .54* | .45* | |||||||||
| 14. AF dep 6y | .04 | .02 | .08 | .17* | .18* | .13* | .13* | .10 | .20* | .47* | .56* | .54* | .61* | ||||||||
| 15. Child int 18m | .03 | .01 | −.01 | .32* | .15* | .16* | .11* | .10* | .18* | .17* | .15* | .12* | .17* | .12* | |||||||
| 16. Child int 27m | .07 | .10* | −.01 | .24* | .17* | .21* | .25* | .10* | .18* | .18* | .15* | .14* | .10 | .11* | .64* | ||||||
| 17. Child int 4.5y | .01 | .07 | −.00 | .18* | .14* | .07 | .09 | .16* | .17* | .15* | .15* | .11* | .08 | .05 | .44* | .47* | |||||
| 18. Child int 6y | .01 | .10* | .06 | .10* | .15* | .12* | .16* | .15* | .26* | .12* | .15* | .18* | .05 | .13* | .35* | .45* | .64* | ||||
| 19. Child anxiety | .02 | .01 | −.01 | .10 | .07 | .06 | .13* | .21* | .20* | .06 | .11* | .06 | .06 | .04 | .23* | .19* | .38* | .42* | |||
| 20. Child dep | −.01 | −.01 | .02 | .09 | .21* | .23* | .26* | .22* | .31* | .04 | .11* | .15* | .01 | .01 | .19* | .21* | .31* | .39* | .60* | ||
| 21. Child ADHD | .05 | −.02 | .08 | .07 | .10 | .09 | .13* | .08 | .14* | .05 | .04 | .07 | −.01 | −.01 | .09 | .08 | .25* | .26* | .47* | .51* | |
| 22. Child ODD/CD | .02 | −.01 | .02 | .12* | .08 | .03 | .04 | .14* | .19* | −.05 | .03 | .04 | −.00 | .07 | .16* | .13* | .31* | .33* | .42* | .43* | .40* |
Note. BF = birth father, BM = birth mother, AM = adoptive mother, AF = adoptive father, p = psychopathology, anxiety = anxiety symptoms, dep = depressive symptoms, int = internalizing behavior, ODD/CD = Oppositional Defiant Disorder/Conduct Disorder symptoms, ADHD = Attention Deficit/Hyperactivity Disorder symptoms. Childhood disorder symptoms from the PAPA were collected between ages 6–8. Correlations were estimated after accounting for covariates (prenatal risk, openness of adoption, child).
indicates p < .05.
Table 2.
Results from RI-CLPMs for Predictors of Child Psychaitric Disorders
| Adoptive Mother RI-CLPM | Adoptive Father RI-CLPM | |||||
|---|---|---|---|---|---|---|
| Std coef | SE | p | Std coef | SE | p | |
| Child int | ||||||
| BM p | 0.06 | 0.03 | 0.342 | 0.06 | 0.03 | 0.329 |
| BF p | 0.10 | 0.03 | 0.080 | 0.09 | 0.03 | 0.103 |
| BM pre dep | −0.03 | 0.01 | 0.630 | 0.00 | 0.01 | 0.991 |
| Infant neg emo | 0.34 | 0.04 | 0.000 | 0.34 | 0.04 | 0.000 |
| AF/AM dep | 0.17 | 0.06 | 0.027 | 0.31 | 0.06 | 0.000 |
| AM/AF dep | ||||||
| BM p | 0.03 | 0.03 | 0.586 | 0.06 | 0.03 | 0.274 |
| BF p | 0.02 | 0.02 | 0.717 | 0.03 | 0.03 | 0.504 |
| BM pre dep | −0.08 | 0.01 | 0.128 | 0.02 | 0.01 | 0.748 |
| Infant neg emo | 0.12 | 0.04 | 0.022 | 0.12 | 0.05 | 0.031 |
| AF/AM dep | 0.16 | 0.07 | 0.057 | 0.24 | 0.07 | 0.002 |
| Infant neg emo | ||||||
| BM p | −0.07 | 0.03 | 0.101 | −0.07 | 0.03 | 0.108 |
| BF p | 0.01 | 0.03 | 0.868 | 0.00 | 0.03 | 0.954 |
| BM pre dep | 0.06 | 0.01 | 0.185 | 0.08 | 0.01 | 0.077 |
| Child CD/ODD | ||||||
| BM p | 0.00 | 0.04 | 0.964 | 0.00 | 0.04 | 0.996 |
| BF p | −0.01 | 0.04 | 0.778 | −0.01 | 0.04 | 0.784 |
| BM pre dep | −0.03 | 0.02 | 0.534 | −0.03 | 0.02 | 0.552 |
| Infant neg emo | 0.02 | 0.08 | 0.716 | 0.01 | 0.07 | 0.795 |
| Child int | 0.19 | 0.17 | 0.032 | 0.22 | 0.19 | 0.022 |
| AM/AF dep | −0.05 | 0.11 | 0.446 | −0.08 | 0.10 | 0.257 |
| AF/AM dep | −0.03 | 0.10 | 0.634 | −0.05 | 0.08 | 0.308 |
| Child ADHD | ||||||
| BM p | 0.01 | 0.04 | 0.337 | 0.01 | 0.04 | 0.347 |
| BF p | −0.01 | 0.04 | 0.473 | −0.01 | 0.03 | 0.504 |
| BM pre dep | 0.02 | 0.01 | 0.074 | 0.02 | 0.01 | 0.079 |
| Infant neg emo | 0.01 | 0.06 | 0.710 | 0.00 | 0.06 | 0.748 |
| Child int | −0.01 | 0.17 | 0.689 | −0.01 | 0.20 | 0.673 |
| AM/AF dep | 0.00 | 0.09 | 0.979 | 0.00 | 0.09 | 0.872 |
| AF/AM dep | −0.01 | 0.07 | 0.583 | −0.01 | 0.06 | 0.611 |
| Child depressive symptoms | ||||||
| BM p | −0.06 | 0.05 | 0.212 | −0.06 | 0.05 | 0.228 |
| BF p | 0.01 | 0.04 | 0.874 | 0.00 | 0.04 | 0.960 |
| BM pre dep | −0.02 | 0.02 | 0.732 | −0.02 | 0.02 | 0.627 |
| Infant neg emo | −0.05 | 0.08 | 0.361 | −0.05 | 0.09 | 0.381 |
| Child int | 0.12 | 0.24 | 0.283 | 0.14 | 0.28 | 0.280 |
| AM/AF dep | 0.18 | 0.14 | 0.008 | −0.01 | 0.14 | 0.901 |
| AF/AM dep | −0.04 | 0.09 | 0.476 | 0.13 | 0.10 | 0.021 |
| Child anxiety symptoms | ||||||
| BM p | −0.02 | 0.05 | 0.727 | −0.01 | 0.05 | 0.795 |
| BF p | 0.01 | 0.04 | 0.890 | 0.00 | 0.04 | 0.965 |
| BM pre dep | −0.08 | 0.02 | 0.090 | −0.07 | 0.02 | 0.122 |
| Infant neg emo | −0.05 | 0.07 | 0.326 | −0.05 | 0.07 | 0.362 |
| Child int | 0.25 | 0.21 | 0.021 | 0.27 | 0.25 | 0.031 |
| AM/AF dep | −0.07 | 0.12 | 0.264 | −0.06 | 0.12 | 0.462 |
| AF/AM dep | 0.05 | 0.09 | 0.423 | −0.01 | 0.08 | 0.804 |
| Child psychiatric disorder symptoms | ||||||
| BM p | 0.03 | 0.05 | 0.698 | 0.03 | 0.05 | 0.676 |
| BF p | −0.09 | 0.04 | 0.155 | −0.09 | 0.04 | 0.147 |
| BM pre dep | 0.12 | 0.02 | 0.111 | 0.11 | 0.02 | 0.151 |
| Infant neg emo | −0.05 | 0.09 | 0.565 | −0.06 | 0.09 | 0.479 |
| Child int | 0.45 | 0.23 | 0.003 | 0.50 | 0.26 | 0.002 |
| AM/AF dep | 0.15 | 0.14 | 0.105 | −0.10 | 0.13 | 0.341 |
| AF/AM dep | −0.13 | 0.09 | 0.122 | 0.05 | 0.10 | 0.520 |
Note. Estimates for the adoptive mother RI-CLPM are listed in columns on the left and adoptive father RI-CLPM are on the right. BF = birth father, BM = birth mother, AM = adoptive mother, AF = adoptive father, p = psychopathology, ODD/CD = Oppositional Defiant Disorder/Conduct Disorder symptoms, ADHD = Attention Deficit/Hyperactivity Disorder symptoms.
Figure 1.
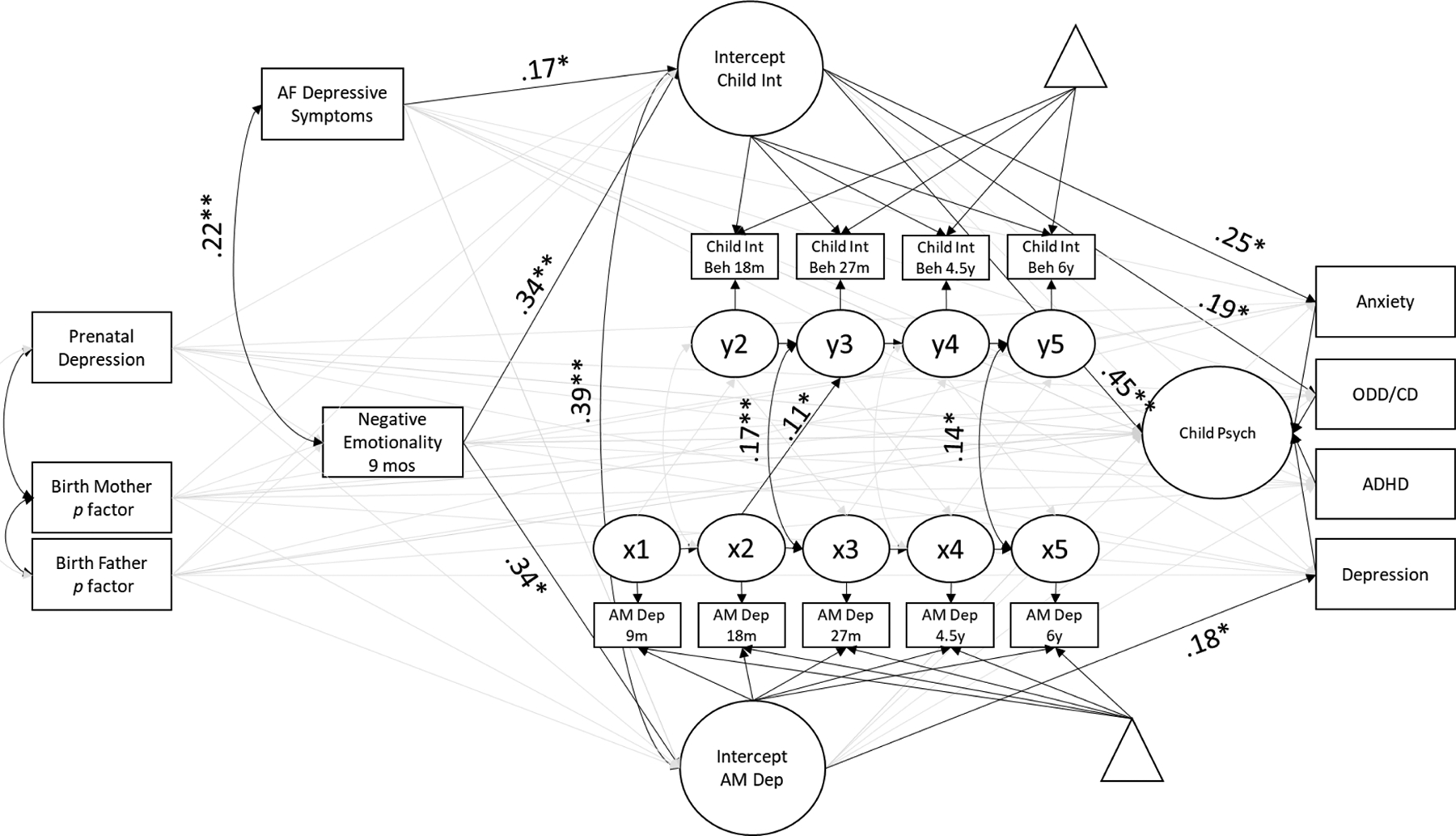
Random Intercept Cross-Lagged Panel Model between adoptive mother depressive symptoms and child behavior problems. Significant paths are depicted in black. Triangles represent mean structure. AM = adoptive mother, AF = adoptive father, Int = internalizing behavior, Dep = depressive symptoms, anxiety = anxiety symptoms, depression = depressive symptoms, int = internalizing behavior, ODD/CD = Oppositional Defiant Disorder/Conduct Disorder symptoms, ADHD = Attention Deficit/Hyperactivity Disorder symptoms.
Figure 2.
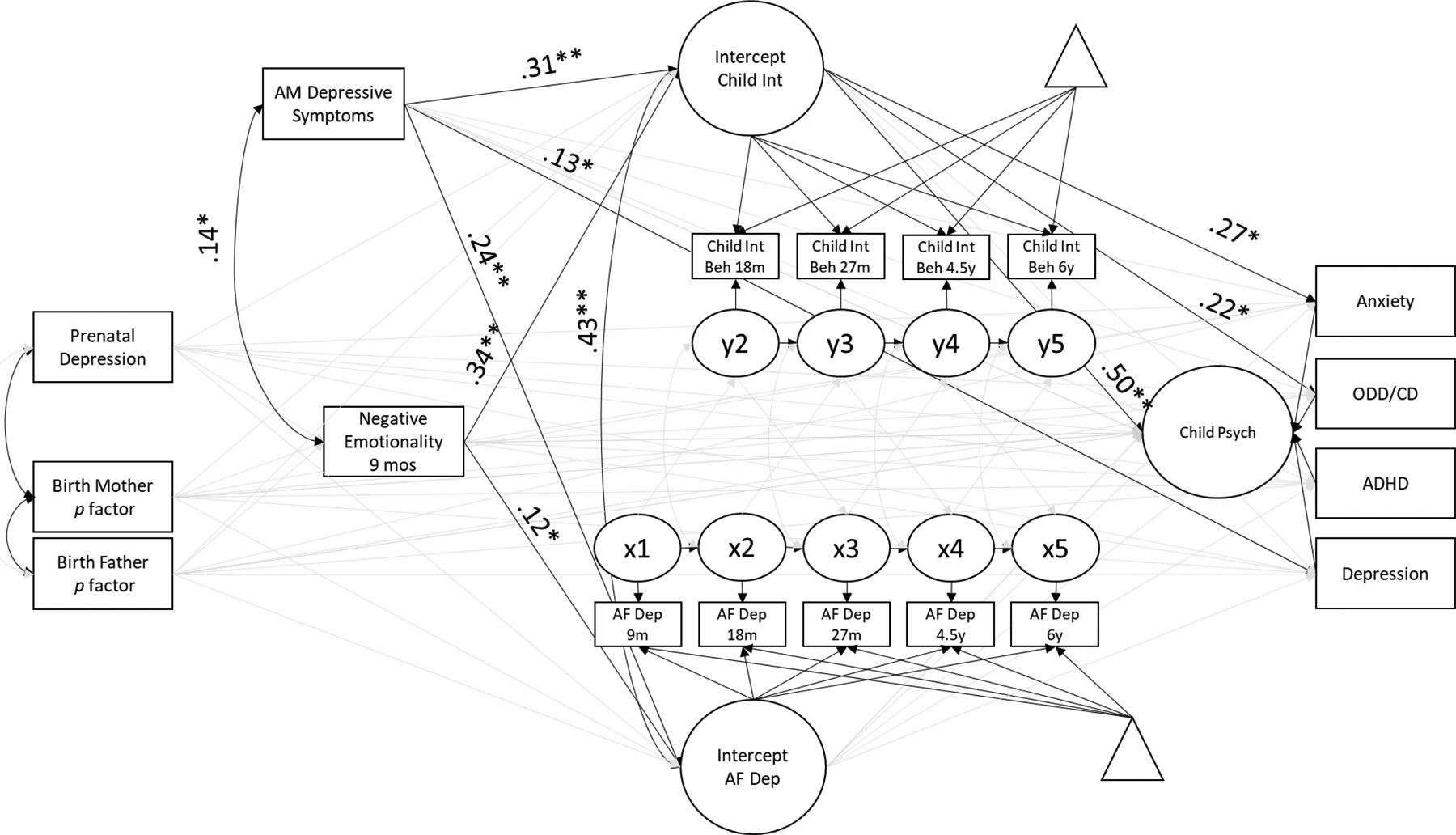
Random Intercept Cross-Lagged Panel Model between adoptive father depressive symptoms and child behavior problems. Significant paths are depicted in black. Triangles represent mean structure. AM = adoptive mother, AF = adoptive father, Int = internalizing behavior, Dep = depressive symptoms, anxiety = anxiety symptoms, depression = depressive symptoms, int = internalizing behavior, ODD/CD = Oppositional Defiant Disorder/Conduct Disorder symptoms, ADHD = Attention Deficit/Hyperactivity Disorder symptoms.
Results identified significant between-person effects as demonstrated in Table 2: adoptive mother and adoptive father chronic depressive symptoms when children were age 9 months through 6 years were related to chronic child internalizing behaviors from 18 months through 6 years (std. coef. = .31, .17; p < .01, p = .03). These findings provide partial support for hypothesis 1. Adoptive mother depressive symptoms from this latent composite predicted child DD (std. coef. = .18, p < .01). No other significant associations emerged between parent depressive symptoms and child psychopathology and child psychiatric disorder symptoms.
Our second hypothesis, that adoptive parent depressive symptoms at child age 9 months would demonstrate a cross-lagged association with child behavioral problems at 18 months, was not supported, as depicted in Figures 1 and 2; however, maternal depressive symptoms at child age 18 months predicted child internalizing behavior at age 27 months (std. coef. = .11, p = .04). No other cross-lagged associations from adoptive mother and father depressive symptoms to child internalizing behavior were significant, nor were associations from child internalizing behavior to adoptive parent depressive symptoms.
Regarding the specificity of child internalizing behavior at age 6 and concurrent adoptive parent depressive symptoms, there was partial support for hypothesis 3 for maternal depressive symptoms but not for father depressive symptoms (see Figures 1 and 2). Co-occurring associations between maternal depressive symptoms and child internalizing behavior were significant at ages 27 months (std. coef. = .17, p < .01) and 6 years (std. coef. = .14, p = .03). There were no significant time-varying associations between adoptive father depressive symptoms and child internalizing behavior.
Discussion
This study examined transactional associations between adoptive parent depressive symptoms and child internalizing behavior. We examined how these constructs predicted child psychiatric disorder symptoms. By using a parent-offspring adoption design, we were able to account for some of the possible genetic and prenatal influences on children’s symptoms. As children did not share a rearing environment with their biological parent, this design allowed for separate estimates for genetic and prenatal risk for psychopathology, insofar as genetic risk was indexed by our computation of birth parent psychopathology, and prenatal risk was indexed by birth mother internalizing symptoms during pregancy. Moreover, the use of RI-CLPMs separated trait-like stability in child internalizing behavior and parent depressive symptoms from time-specific changes in these constructs. This allowed for unbiased estimates of the cross-lagged paths between adoptive parent depressive symptoms and child internalizing behavior. To date, we are unaware of any other studies that have gone beyond the traditional CLPM. Thus, associations found from prior work are likely overestimated due to the continuity of both rearing parent depressive symptoms and child internalizing behavior over time. Additionally, the use of two separate models that considered mothering and fathering separately, while accounting for the other, allowed for a broader picture of the rearing environment to understand how mothers and fathers contribute uniquely to child internalizing behavior and child psychopathology. Overall, results suggested that child internalizing behavior predicts overall child psychopathology and child ODD/CD and ANX symptoms, but not child DD or ADHD symptoms. Environmental exposure to chronic maternal depressive symptoms may confer specific risk for child expression of depressive symptoms.
Parents’ Postnatal Depressive Symptoms as an Environmental Risk
In line with hypotheses, adoptive mother and father chronic depressive symptoms (as indicated as a higher latent intercept) covaried with consistent child internalizing behavior (between-person effects); the standardized association was medium in magnitude. These findings echo those from previous work. Specifically, rearing mother depressive symptoms, considered as a composite, are typically associated with child internalizing behavior (Grabow et al., 2017; Netsi et al., 2018; Pemberton et al., 2010), suggesting that rearing mothers with chronic, rather than acute, symptoms should be prioritized for intervention. We identified a similar pattern of results for adoptive father depressive symptoms, although it was smaller in magnitude. This father effect held even when controlling for the effect of adoptive mother depressive symptoms. The findings from this study provide clear evidence that at the between-person level, father’s depressive symptoms are associated with children’s internalizing behavior.
However, adoptive mother’s depressive symptoms predicted both child internalizing behavior and adoptive father depressive symptoms, whereas adoptive father depressive symptoms only predicted child internalizing behavior (Table 2). Recent findings have suggested that, although father depressive symptoms are related to child internalizing behavior, the absence of father depressive symptoms alone cannot compensate for the presence of maternal depressive symptoms (Pietikäinen et al., 2019). Taken together, our results suggest that maternal depressive symptoms are a possible driver of both paternal depressive symptoms and child internalizing behavior. However, in the absence of an experimental design, we cannot infer causality.
Although adoptive mother and father chronic depressive symptoms were related to child internalizing behavior, the only association between adoptive parent depressive symptoms and child psychopathology or specific disorder symptoms was between adoptive mother depressive symptoms and child depressive symptoms (Table 2). This finding is contrary to prior work that has established associations between rearing mother and father depressive symptoms and child psychopathology (Goodman et al., 2011; Harold et al., 2011; Tully et al., 2008). The specificity of risk from chronic maternal depressive symptoms to child depressive symptoms, beyond what was accounted for by general child psychopathology, is in line with the idea that environmental exposures differentiate the manifestation of disorder types (Kendler et al., 2011; Rhee et al., 2015).
Contrary to findings from Pemberton et al. (2010), Verbeek et al. (2012), and Pratt et al. (2017), our second hypothesis was not supported, as there was not a cross-lagged association between maternal or paternal depressive symptoms at child age 9 months and child internalizing behavior at age 18 months (Figures 1 & 2). These null findings may be because maternal depressive symptoms in infancy more reliably predict internalizing behaviors during the preschool and school-age years when behavior problems are more stable (Allen et al, 1998; Braungart-Rieker et al., 2010; Hernández et al., 2018; Sallquist et al., 2009) or because the chronicity of depressive symptoms (i.e., associations between intercepts) accounts for associations over time. There is also a need to include parent depressive symptoms earlier than age 9 months. At the time of birth, infants begin to understand the nature of their caregiving environment, by approximately 2 months, they begin smiling, and by 4 months they can time their smiles to elicit a social response from their mother (Ruvolo et al., 2015). It has been demonstrated that rearing mothers experiencing heightened depressive symptoms are more likely to display blunted sensitivity to infant cues (Muzik et al., 2017; Newland et al., 2016). Experimentally, differential patterns of interactions emerge between infants whose mothers are depressed and other adults as early as 3 months of age (Field et al., 1988). Thus, an examination of parent depression before child age 9 months and similar modelling approach is warranted. The use of a genetically sensitive design would help bolster confidence that the effects of parent depressive symptoms postnatally are due to rearing effects, rather than genetic transmission.
A cross-lagged association emerged between adoptive mother depressive symptoms at child age 18 months and child internalizing behavior at age 27 months. There were within-time associations at age 27 months and 6 years between adoptive mother depressive symptoms and child internalizing behavior, but no time-varying associations for adoptive fathers. For adoptive fathers, there may have been less variance in fathers’ depressive symptoms over time compared to mothers’. Prior work has identified that father depressive symptoms may peak during child infancy, return to baseline levels after the early postpartum period, and then remain somewhat stable (Volling et al., 2018), whereas maternal depressive symptoms exhibit a variety of trajectories throughout a child’s development such as low-stable, moderate-stable, moderate-increasing, and high-decreasing (Ahmed et al., 2019). The within-dyad associations between adoptive mothers and their children indicated that deviations from the person-specific mean in maternal depressive symptoms (as captured by the random intercept) were accompanied by deviations in the person-specific mean in child internalizing behavior at child age 27 months and 6 years. Associations at child age 6 years were expected as child internalizing behavior in later development (childhood and adolescence) is typically accompanied by maternal depressive symptoms (Gjerde et al., 2017; Sellers et al., 2016). Additional research is needed to understand the mechanism underlying environmental transmission from maternal depressive symptoms to child internalizing behavior in toddlerhood. Potential candidates include maternal negative affect and/or maternal modelling and reinforcement of internalizing behaviors as a coping style (Muzik et al., 2017). It is also possible that extraneous factors drive associations between maternal depressive symptoms and child internalizing behaviors (Pelham III et al., 2020). These may include correlates of maternal depression at 18 months which may impact a child’s later behavior such as childcare enrollment, or the introduction of a sibling (Lemay et al., 2012; Stewart et al., 1987).
Limitations and Future Directions
Limitations include the timing of data collection, potential reporter bias, and design limitations. Specifically, other studies of parent depressive symptoms and child internalizing behavior have measured depressive symptoms between three to six months postnatal (Gutierrez-Galve et al., 2019; Netsi et al., 2018). We were unable to measure the early postpartum period because the first assessment of adoptive parent depressive symptoms in this study was child age 9 months, which may have limited our ability to detect effects of parent depressive symptoms in infancy. Additionally, future studies may consider if maternal depressive symptoms measured on a smaller timescale (e.g. daily or weekly basis) are more strongly associated with child symptoms than those taken with greater spacing (e.g., months to years apart). Another limitation is that adoptive parents reported both their depressive symptoms and their child’s behavior problems. Use of the same reporter and the same method tends to inflate associations (i.e., shared method variance; LaGrange & A Cole, 2008; Xerxa et al., 2020). This issue was partially accounted for by using both parent’s estimates of child internalizing behavior, when available, but some bias may still exist because parents’ depressive symptoms also influence each other (Volling et al., 2018). Finally, some of the effects of birth and rearing parents’ depressive symptoms may not emerge until later in child development, as the prevalence of mental health disorders increases in adolescence (Costello et al., 2003). Thus, future analyses should apply similar methodologies with adolescent populations.
Limitations also exist in the sample. The majority of birth father data was imputed when the psychopathology construct was created because of the reduced number of birth fathers in the study. Thus, it is possible that variance explained by birth mother psychopathology explained most of the variance associated with birth father psychopathology for child internalizing behavior. Additionally, birth parents may be at higher risk than the population norms, as the majority had moderately low income and low educational attainment at each study period (Leve et al., 2019). Adoptive parents typically had higher income and educational attainment than the general population, which typically reduces a child’s risk for behavior problems (Hodgkinson et al., 2017; Larson et al., 2015). Adoptive parents in our study also had a lower prevalence of a major depressive episode (17% for adoptive mothers, 6% for adoptive fathers) compared to birth parents (37% for birth mothers, 26% for birth fathers) and compared to the general population (25% for the general female population, 18% for the general male population; National Comorbidity Survey, 2007). The majority of the adoptive parents identified as White, which limits the generalizability of our study to more diverse populations.
Additional limitations possible include type I and type II error. For type I error, we estimate multiple crossed-lagged paths and while the RI-CLPM is more conservative than a traditional CLPM, it is possible that some of our results could have emerged due to chance. For type II error, because the RI-CLPM we used was more conservative and can inflate standard errors, it is also possible we may not have detected associations that actually exist at a population level. Replicability is a critical element of hypothesis testing, thus additional research using a similar design and modelling approach is needed to confirm our findings (Banerjee et al., 2009).
This study did not have power to evaluate simultaneous interactions between adoptive mothers and fathers and child internalizing symptoms but future research may consider the combined effect of mother and father depressive symptoms utilizing a three way RI-CLPM to estimate whether there are distinct but additive contributions of rearing mother and father depressive symptoms (respectively) at sensitive developmental time points. The RI-CLPM is also well-suited to estimate whether similar patterns emerge for associations between parent depressive symptoms and child externalizing behaviors.
Conclusion
Limitations notwithstanding, there are several key contributions from this study. Namely, we examined environmental exposure to parent depressive symptoms while separating out the influences of birth parent psychopathology and recalled prenatal depressive symptoms. We used an RI-CLPM to account for trait-like stability over time, which enabled us to identify sensitive developmental time points. Using this model, we found associations between rearing mother depressive symptoms and child internalizing behaviors at several time points. Findings indicated the presence of genetic transmission of child internalizing behavior but not overall psychopathology or specific child psychiatric disorders. Adoptive mother depressive symptoms were more associated with child internalizing behavior than were adoptive father depressive symptoms, although fathers’ depressive symptoms were still significantly associated with child internalizing behavior. Moreover, results suggested that the within-dyad variability was limited to a cross-lagged association between maternal depressive symptoms at 18 months and internalizing behavior at 27 months and correlations between maternal depressive symptoms and child internalizing behavior when children were 27 months and 6 years. Early intervention to reduce the onset and chronicity of depressive symptoms is warranted for both mothers and fathers to reduce the child’s risk for developing behavior problems. Clinicians should simultaneously screen for parents’ depressive symptoms and child internalizing behavior to prevent maladaptive child outcomes (Beach et al., 2008; Shaw et al., 2009). Validated supports that target parental depression include parent training and cognitive-behavioral approaches for parents (Waddell et al., 2007).
Data Availability Statement
The de-identifieid data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Acknowledgements:
This work was supported by the 2019–2020 University of Oregon Graduate School, College of Education Dissertation Research Fellowship. This project was supported by grant R01 HD042608 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the National Institute on Drug Abuse, NIH, U.S. PHS (PI Years 1–5: David Reiss, MD; PI Years 6–10: Leslie Leve, PhD). This project was also supported by grant R01 DA020585 from the National Institute on Drug Abuse, the National Institute of Mental Health and OBSSR, NIH, U.S. PHS (PI: Jenae Neiderhiser, Ph.D.; grant R01 MH092118 from the National Institute of Mental Health, NIH, U.S. PHS (PIs: Jenae Neiderhiser, Ph.D. and Leslie Leve, Ph.D.); grant R01 DK090264 from the National Institute of Diabetes and Digestive and Kidney Disease, NIH, U.S. PHS (PI: Jody Ganiban, Ph.D.); grant R01 DA035062 from the National Institute on Drug Abuse, NIH, U.S. PHS (PI: Leslie Leve, Ph.D.); grant R56 HD042608 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, NIH, U.S. PHS (PI: Leslie Leve, PhD), and grant UH3 OD023389.from the Office of The Director, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health & Human Development nor the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors have no conflict of interest in relationship, financial, or otherwise to disclose.
REFERENCES
- Achenbach TM, & Rescorla L (2001). Manual for the ASEBA school-age forms & profiles : an integrated system of multi-informant assessment. [Google Scholar]
- Achenbach T, & Rescorla L (2000). Manual for the ASEBA Preschool forms & profiles. In Burlington: University of Vermont, Research Center for Children, Youth & Families. [Google Scholar]
- Ahmed A, Bowen A, Feng CX, & Muhajarine N (2019). Trajectories of maternal depressive and anxiety symptoms from pregnancy to five years postpartum and their prenatal predictors. BMC Pregnancy and Childbirth, 19(1), 26. 10.1186/s12884-019-2177-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen NB, Lewinsohn PM, & Seeley JR (1998). Prenatal and perinatal influences on risk for psychopathology in childhood and adolescence. Development and Psychopathology, 10(3), 513–529. 10.1017/S0954579498001722 [DOI] [PubMed] [Google Scholar]
- Banerjee A, Chitnis UB, Jadhav SL, Bhawalkar JS, & Chaudhury S (2009). Hypothesis testing, type I and type II errors. Industrial Psychiatry Journal, 18(2), 127–131. 10.4103/0972-6748.62274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach SRH, Kogan SM, Brody GH, Chen Y-F, Lei M-K, & Murry VM (2008). Change in caregiver depression as a function of the Strong African American Families Program. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 22(2), 241–252. 10.1037/0893-3200.22.2.241 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100. 10.1016/0272-7358(88)90050-5 [DOI] [Google Scholar]
- Braungart-Rieker JM, Hill-Soderlund AL, & Karrass J (2010). Fear and anger reactivity trajectories from 4 to 16 months: The roles of temperament, regulation, and maternal sensitivity. In Developmental Psychology (Vol. 46, Issue 4, pp. 791–804). American Psychological Association. 10.1037/a0019673 [DOI] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Olino TM, Dyson MW, Laptook RS, Carlson GA, & Klein DN (2014). Predictors of the onset of depression in young children: a multi-method, multi-informant longitudinal study from ages 3 to 6. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 55(11), 1279–1287. 10.1111/jcpp.12252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chazan-Cohen R, Ayoub C, Pan BA, Roggman L, Raikes H, Mckelvey L, Whiteside-Mansell L, & Hart A (2007). It takes time: Impacts of Early Head Start that lead to reductions in maternal depression two years later. Infant Mental Health Journal, 28(2), 151–170. 10.1002/imhj.20127 [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, & Angold A (2003). Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Archives of General Psychiatry, 60(8), 837–844. 10.1001/archpsyc.60.8.837 [DOI] [PubMed] [Google Scholar]
- Côté SM, Ahun MN, Herba CM, Brendgen M, Geoffroy M-C, Orri M, Liu X, Vitaro F, Melchior M, Boivin M, & Tremblay RE (2018). Why is maternal depression related to adolescent internalizing problems? A 15-year population-based study. Journal of the American Academy of Child & Adolescent Psychiatry, 57(12), 916–924. 10.1016/j.jaac.2018.04.024 [DOI] [PubMed] [Google Scholar]
- Crawford TN, Cohen P, Midlarsky E, & Brook JS (2001). Internalizing Symptoms in Adolescents: Gender Differences in Vulnerability to Parental Distress and Discord. Journal of Research on Adolescence, 11(1), 95–118. 10.1111/1532-7795.00005 [DOI] [Google Scholar]
- Cree RA, Bitsko RH, Robinson LR, Holbrook JR, Danielson ML, Smith DS, Kaminski JW, Kenney MK, & Peacock G (2018). Health care, family, and community factors associated with mental, behavioral, and developmental disorders and poverty among children aged 2–8 years — United States, 2016. MMWR. Morbidity and Mortality Weekly Report, 67(5), 1377–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, & Blumberg SJ (2018). Prevalence of parent-reported ADHD diagnosis and associated treatment among u.s. children and adolescents, 2016. Journal of Clinical Child and Adolescent Psychology : The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 47(2), 199–212. 10.1080/15374416.2017.1417860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue MR, Tillman R, & Luby J (2020). Early socioemotional competence, psychopathology, and latent class profiles of reparative prosocial behaviors from preschool through early adolescence. Development and Psychopathology, 32(2), 573–585. 10.1017/S0954579419000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, & Angold A (2006). Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA). Journal of the American Academy of Child & Adolescent Psychiatry, 45(5), 538–549. 10.1097/01.chi.0000205705.71194.b8 [DOI] [PubMed] [Google Scholar]
- Eley TC (1997). General genes: A new theme in developmental psychopathology. Current Directions in Psychological Science, 6(4), 90–95. 10.1111/1467-8721.ep11512831 [DOI] [Google Scholar]
- Field T, Healy B, Goldstein S, Perry S, Bendell D, Schanberg S, Zimmerman EA, & Kuhn C (1988). Infants of depressed mothers show “depressed” behavior even with nondepressed adults. Child Development, 59(6), 1569–1579. 10.2307/1130671 [DOI] [PubMed] [Google Scholar]
- Finsaas MC, Kessel EM, Dougherty LR, Bufferd SJ, Danzig AP, Davila J, Carlson GA, & Klein DN (2020). Early Childhood Psychopathology Prospectively Predicts Social Functioning in Early Adolescence. Journal of Clinical Child and Adolescent Psychology : The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 49(3), 353–364. 10.1080/15374416.2018.1504298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flint J, & Kendler KS (2014). The genetics of major depression. Neuron, 81(3), 484–503. 10.1016/j.neuron.2014.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X, Natsuaki MN, Martin DM, Leve LD, Neiderhiser JM, Shaw DS, Villareal G, Scaramella L, Reid JB, & Reiss D (2008). Bridging the divide: Openness in adoption and postadoption psychosocial adjustment among birth and adoptive parents. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 22(4), 529–540. 10.1037/a0012817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, & Blumberg SJ (2019). Prevalence and treatment of Depression, Anxiety, and Conduct Problems in US children. The Journal of Pediatrics, 206, 256–267.e3. 10.1016/j.jpeds.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjerde LC, Eilertsen EM, Reichborn-Kjennerud T, McAdams TA, Zachrisson HD, Zambrana IM, Røysamb E, Kendler KS, & Ystrom E (2017). Maternal perinatal and concurrent depressive symptoms and child behavior problems: A sibling comparison study. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 58(7), 779–786. 10.1111/jcpp.12704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Grabow AP, Khurana A, Natsuaki MN, Neiderhiser JM, Harold GT, Shaw DS, Ganiban JM, Reiss D, & Leve LD (2017). Using an adoption-biological family design to examine associations between maternal trauma, maternal depressive symptoms, and child internalizing and externalizing behaviors. Development and Psychopathology, 29(5), 1707–1720. 10.1017/S0954579417001341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grattan A, Sullivan MD, Saunders KW, Campbell CI, & Von Korff MR (2012). Depression and prescription opioid misuse among chronic opioid therapy recipients with no history of substance abuse. Annals of Family Medicine, 10(4), 304–311. 10.1370/afm.1371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Burwell RA, & Nagin DS (2009). Transactional processes in child disruptive behavior and maternal depression: a longitudinal study from early childhood to adolescence. Development and Psychopathology, 21(1), 139–156. 10.1017/S0954579409000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez-Galve L, Stein A, Hanington L, Heron J, Lewis G, O’Farrelly C, & Ramchandani PG (2019). Association of maternal and paternal depression in the postnatal period with offspring depression at age 18 years. JAMA Psychiatry, 76(3), 290–296. 10.1001/jamapsychiatry.2018.3667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hails KA, Reuben JD, Shaw DS, Dishion TJ, & Wilson MN (2018). Transactional associations among maternal depression, parent–child coercion, and child conduct problems during early childhood. Journal of Clinical Child & Adolescent Psychology, 47(sup1), S291–S305. 10.1080/15374416.2017.1280803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker EL, Kuiper RM, & Grasman RPPP (2015). A critique of the cross-lagged panel model. Psychological Methods, 20(1), 102–116. 10.1037/a0038889 [DOI] [PubMed] [Google Scholar]
- Harold GT, Rice F, Hay DF, Boivin J, van den Bree M, & Thapar A (2011). Familial transmission of depression and antisocial behavior symptoms: Disentangling the contribution of inherited and environmental factors and testing the mediating role of parenting. Psychological Medicine, 41(6), 1175–1185. 10.1017/S0033291710001753 [DOI] [PubMed] [Google Scholar]
- Hernández MM, Eisenberg N, Valiente C, Thompson MS, Spinrad TL, Grimm KJ, VanSchyndel SK, Berger RH, Silva KM, Pina AA, Southworth J, & Gal DE (2018). Trajectories of the expression of negative emotion from kindergarten to first grade: Associations with academic outcome. Journal of Educational Psychology, 110(3), 324–337. 10.1037/edu0000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkinson S, Godoy L, Beers LS, & Lewin A (2017). Improving mental health access for low-income children and families in the primary care setting. Pediatrics, 139(1), e20151175. 10.1542/peds.2015-1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1995). Evaluating model fit. In Hoyle RH (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 76–99). Sage Publications, Inc. [Google Scholar]
- Huaqing Qi C, & Kaiser AP (2003). Behavior problems of preschool children from low-income families: Review of the literature. Topics in Early Childhood Special Education, 23(4), 188–216. 10.1177/02711214030230040201 [DOI] [Google Scholar]
- Kendler KS, Gardner CO, & Lichtenstein P (2008). A developmental twin study of symptoms of anxiety and depression: Evidence for genetic innovation and attenuation. Psychological Medicine, 38(11), 1567–1575. 10.1017/S003329170800384X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler Kenneth S, Aggen SH, Knudsen GP, Røysamb E, Neale MC, & Reichborn-Kjennerud T (2011). The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. The American Journal of Psychiatry, 168(1), 29–39. 10.1176/appi.ajp.2010.10030340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr DCR, Leve LD, Harold GT, Natsuaki MN, Neiderhiser JM, Shaw DS, & Reiss D (2013). Influences of biological and adoptive mothers’ depression and antisocial behavior on adoptees’ early behavior trajectories. Journal of Abnormal Child Psychology, 41(5), 723–734. 10.1007/s10802-013-9711-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, & Üstün TB (2004). The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93–121. 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2016). Principles and practice of structural equation modeling, 4th ed. In Principles and practice of structural equation modeling, 4th ed. (pp. xvii, 534–xvii, 534). Guilford Press. [Google Scholar]
- LaGrange B, & A Cole D (2008). An Expansion of the Trait-State-Occasion Model: Accounting for Shared Method Variance (Vol. 15). 10.1080/10705510801922381 [DOI] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, & Rathouz PJ (2011). Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry, 68(2), 181–189. 10.1001/archgenpsychiatry.2010.192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson K, Russ SA, Nelson BB, Olson LM, & Halfon N (2015). Cognitive ability at kindergarten entry and socioeconomic status. Pediatrics, 135(2), e440–e448. 10.1542/peds.2014-0434 [DOI] [PubMed] [Google Scholar]
- Laurent HK, Leve LD, Neiderhiser JM, Natsuaki MN, Shaw DS, Fisher PA, Marceau K, Harold GT, & Reiss D (2013). Effects of parental depressive symptoms on child adjustment moderated by hypothalamic pituitary adrenal activity: Within- and between-family risk. Child Development, 84(2), 528–542. 10.1111/j.1467-8624.2012.01859.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavigne JV, Meyers KM, & Feldman M (2016). Systematic Review: Classification Accuracy of Behavioral Screening Measures for Use in Integrated Primary Care Settings. Journal of Pediatric Psychology, 41(10), 1091–1109. 10.1093/jpepsy/jsw049 [DOI] [PubMed] [Google Scholar]
- Lemay L, Bigras N, & Bouchard C (2012). Educational Daycare from Infancy and Externalizing and Internalizing Behaviors in Early Childhood: Differential Effect by Children’s Vulnerability. Procedia - Social and Behavioral Sciences, 55, 115–127. 10.1016/j.sbspro.2012.09.485 [DOI] [Google Scholar]
- Leve LD, Neiderhiser JM, Ganiban JM, Natsuaki MN, Shaw DS, & Reiss D (2019). The Early Growth and Development Study: A dual-family adoption study from birth through adolescence. Twin Research and Human Genetics, 1–12. 10.1017/thg.2019.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Shaw DS, Ganiban J, Natsuaki MN, & Reiss D (2013). The Early Growth and Development Study: A prospective adoption study from birth through middle childhood. Twin Research and Human Genetics : The Official Journal of the International Society for Twin Studies, 16(1), 412–423. 10.1017/thg.2012.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, & Allen NB (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. In Psychology and Aging (Vol. 12, Issue 2, pp. 277–287). American Psychological Association. 10.1037/0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- Lewis G, Rice F, Harold GT, Collishaw S, & Thapar A (2011). Investigating environmental links between parent depression and child depressive/anxiety symptoms using an assisted conception design. Journal of the American Academy of Child and Adolescent Psychiatry, 50(5), 451–459.e1. 10.1016/j.jaac.2011.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83(404), 1198–1202. 10.1080/01621459.1988.10478722 [DOI] [Google Scholar]
- Little TD, Jorgensen TD, Lang KM, & Moore EWG (2013). On the joys of missing data. Journal of Pediatric Psychology, 39(2), 151–162. 10.1093/jpepsy/jst048 [DOI] [PubMed] [Google Scholar]
- Liu J (2004). Childhood externalizing behavior: Theory and implications. Journal of Child and Adolescent Psychiatric Nursing : Official Publication of the Association of Child and Adolescent Psychiatric Nurses, Inc, 17(3), 93–103. https://www.ncbi.nlm.nih.gov/pubmed/15535385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marceau K, Rolan E, Leve LD, Ganiban JM, Reiss D, Shaw DS, Natsuaki MN, Egger HL, & Neiderhiser JM (2019). Parenting and prenatal risk as moderators of genetic influences on conduct problems during middle childhood. In Developmental Psychology (Vol. 55, Issue 6, pp. 1164–1181). American Psychological Association. 10.1037/dev0000701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM (2013). Sexual selection and sex differences in the prevalence of childhood externalizing and adolescent internalizing disorders. In Psychological Bulletin (Vol. 139, Issue 6, pp. 1221–1259). American Psychological Association. 10.1037/a0032247 [DOI] [PubMed] [Google Scholar]
- McNeil TF, Cantor-Graae E, & Sjöström K (1994). Obstetric complications as antecedents of schizophrenia: Empirical effects of using different obstetric complication scales. Journal of Psychiatric Research, 28(6), 519–530. 10.1016/0022-3956(94)90042-6 [DOI] [PubMed] [Google Scholar]
- Meadows SO, McLanahan SS, & Brooks-Gunn J (2007). Parental depression and anxiety and early childhood behavior problems across family types. Journal of Marriage and Family, 69(5), 1162–1177. 10.1111/j.1741-3737.2007.00439.x [DOI] [Google Scholar]
- Mund M, & Nestler S (2018). Beyond the cross-lagged panel model: Next-generation statistical tools for analyzing interdependencies across the life course. Advances in Life Course Research. 10.1016/j.alcr.2018.10.002 [DOI] [PubMed] [Google Scholar]
- Murphy BC, Eisenberg N, Fabes RA, Shepard S, & Guthrie IK (1999). Consistency and change in children’s emotionality and regulation: A longitudinal study. Merrill-Palmer Quarterly, 45(3), Palmer Quarterly, 1999, Vol.45(3). [Google Scholar]
- Muzik M, Morelen D, Hruschak J, Rosenblum KL, Bocknek E, & Beeghly M (2017). Psychopathology and parenting: An examination of perceived and observed parenting in mothers with depression and PTSD. Journal of Affective Disorders, 207, 242–250. 10.1016/j.jad.2016.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Comorbidity Survey. (2007). 10.4135/9781483365817.n885 [DOI]
- Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, & Stein A (2018). Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry, 75(3), 247–253. 10.1001/jamapsychiatry.2017.4363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newland RP, Parade SH, Dickstein S, & Seifer R (2016). The association between maternal depression and sensitivity: Child-directed effects on parenting during infancy. Infant Behavior & Development, 45(Pt A), 47–50. 10.1016/j.infbeh.2016.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulson JF, & Bazemore SD (2010). Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. JAMA, 303(19), 1961–1969. 10.1001/jama.2010.605 [DOI] [PubMed] [Google Scholar]
- Pemberton CK, Neiderhiser JM, Leve LD, Natsuaki MN, Shaw DS, Reiss D, & Ge X (2010). Influence of parental depressive symptoms on adopted toddler behaviors: An emerging developmental cascade of genetic and environmental effects. Development and Psychopathology, 22(4), 803–818. 10.1017/S0954579410000477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietikäinen JT, Kiviruusu O, Kylliäinen A, Pölkki P, Saarenpää-Heikkilä O, Paunio T, & Paavonen EJ (2019). Maternal and paternal depressive symptoms and children’s emotional problems at the age of 2 and 5 years: A longitudinal study. Journal of Child Psychology and Psychiatry, n/a(n/a). 10.1111/jcpp.13126 [DOI] [PubMed] [Google Scholar]
- Pratt M, Goldstein A, Levy J, & Feldman R (2017). Maternal depression across the first years of life impacts the neural basis of empathy in preadolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 56(1), 20–29.e3. 10.1016/j.jaac.2016.10.012 [DOI] [PubMed] [Google Scholar]
- Psychogiou L, Moberly NJ, Parry E, Nath S, Kallitsoglou A, & Russell G (2017). Parental depressive symptoms, children’s emotional and behavioural problems, and parents’ expressed emotion - Critical and positive comments. PLoS ONE, 12(10). 10.1371/journal.pone.0183546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchandani PG, Stein A, O’Connor TG, Heron JON, Murray L, & Evans J (2008). Depression in men in the postnatal period and later child psychopathology: A population cohort study. Journal of the American Academy of Child & Adolescent Psychiatry, 47(4), 390–398. 10.1097/CHI.0b013e31816429c2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee SH, Lahey BB, & Waldman ID (2015). Comorbidity among dimensions of childhood psychopathology: Converging evidence from behavior genetics. Child Development Perspectives, 9(1), 26–31. 10.1111/cdep.12102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice F, Harold GT, Boivin J, van den Bree M, Hay DF, & Thapar A (2010). The links between prenatal stress and offspring development and psychopathology: Disentangling environmental and inherited influences. Psychological Medicine, 40(2), 335–345. 10.1017/S0033291709005911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice Frances, Harold G, & Thapar A (2002). The genetic aetiology of childhood depression: A review. Journal of Child Psychology and Psychiatry, 43(1), 65–79. 10.1111/1469-7610.00004 [DOI] [PubMed] [Google Scholar]
- Ringoot AP, Tiemeier H, Jaddoe VWV, So P, Hofman A, Verhulst FC, & Jansen PW (2015). Parental depression and child well-being: Young children’s self-reports helped addressing biases in parent reports. Journal of Clinical Epidemiology, 68(8), 928–938. 10.1016/j.jclinepi.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Roben CKP, Moore GA, Cole PM, Molenaar P, Leve LD, Shaw DS, Reiss D, & Neiderhiser JM (2015). Transactional patterns of maternal depressive symptoms and mother-child mutual negativity in an adoption sample. Infant and Child Development, 24(3), 322–342. 10.1002/icd.1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, & Ratcliff KS (1981). National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Archives of General Psychiatry, 38(4), 381. 10.1001/archpsyc.1981.01780290015001 [DOI] [PubMed] [Google Scholar]
- Rothbart MK (1981). Measurement of temperament in infancy. Child Development, 52(2), 569–578. 10.2307/1129176 [DOI] [Google Scholar]
- Ruvolo P, Messinger D, & Movellan J (2015). Infants time their smiles to make their moms smile. PloS One, 10(9), e0136492–e0136492. 10.1371/journal.pone.0136492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallquist JV, Eisenberg N, Spinrad TL, Reiser M, Hofer C, Zhou Q, Liew J, & Eggum N (2009). Positive and negative emotionality: Trajectories across six years and relations with social competence. Emotion (Washington, D.C.), 9(1), 15–28. 10.1037/a0013970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff AJ, & Mackenzie MJ (2003). Research strategies for capturing transactional models of development: The limits of the possible. Development and Psychopathology, 15(3), 613–640. 10.1017/S0954579403000312 [DOI] [PubMed] [Google Scholar]
- Sellers R, Hammerton G, Harold GT, Mahedy L, Potter R, Langley K, Thapar A, Rice F, Thapar A, & Collishaw S (2016). Examining whether offspring psychopathology influences illness course in mothers with recurrent depression using a high-risk longitudinal sample. Journal of Abnormal Psychology, 125(2), 256–266. 10.1037/abn0000080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, & Gardner F (2009). Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology, 21(2), 417–439. 10.1017/S0954579409000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart RB, Mobley LA, van Tuyl SS, & Salvador MA (1987). The Firstborn’s Adjustment to the Birth of a Sibling: A Longitudinal Assessment. Child Development, 58(2), 341–355. 10.2307/1130511 [DOI] [PubMed] [Google Scholar]
- Sullivan PF, Neale MC, & Kendler KS (2000). Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry, 157(10), 1552–1562. 10.1176/appi.ajp.157.10.1552 [DOI] [PubMed] [Google Scholar]
- Thapar A, Collishaw S, Pine DS, & Thapar AK (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. 10.1016/S0140-6736(11)60871-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tully EC, Iacono WG, & McGue M (2008). An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. The American Journal of Psychiatry, 165(9), 1148–1154. 10.1176/appi.ajp.2008.07091438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeek T, Bockting CLH, van Pampus MG, Ormel J, Meijer JL, Hartman CA, & Burger H (2012). Postpartum depression predicts offspring mental health problems in adolescence independently of parental lifetime psychopathology. Journal of Affective Disorders, 136(3), 948–954. 10.1016/j.jad.2011.08.035 [DOI] [PubMed] [Google Scholar]
- Volling BL, Yu T, Gonzalez R, Tengelitsch E, & Stevenson MM (2018). Maternal and paternal trajectories of depressive symptoms predict family risk and children’s emotional and behavioral problems after the birth of a sibling. Development and Psychopathology, 1–18. 10.1017/S0954579418000743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waddell C, Hua JM, Garland OM, Peters RD, & McEwan K (2007). Preventing mental disorders in children: A systematic review to inform policy-making. Canadian Journal of Public Health, 98(3), 166. 10.17269/cjph.98.812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Gammon GD, John K, Merikangas KR, Warner V, Prusoff BA, & Sholomskas D (1987). Children of depressed parents: Increased psychopathology and early onset of Major Depression. JAMA Psychiatry, 44(10), 847–853. 10.1001/archpsyc.1987.01800220009002 [DOI] [PubMed] [Google Scholar]
- Wesseldijk LW, Dieleman GC, van Steensel FJA, Bleijenberg EJ, Bartels M, Bögels SM, & Middeldorp CM (2018). Do parental psychiatric symptoms predict outcome in children with psychiatric disorders? A naturalistic clinical study. Journal of the American Academy of Child & Adolescent Psychiatry, 57(9), 669–677.e6. 10.1016/j.jaac.2018.05.017 [DOI] [PubMed] [Google Scholar]
- Wichstrøm L, Belsky J, & Steinsbekk S (2017). Homotypic and heterotypic continuity of symptoms of psychiatric disorders from age 4 to 10 years: a dynamic panel model. Journal of Child Psychology and Psychiatry, 58(11), 1239–1247. 10.1111/jcpp.1254 [DOI] [PubMed] [Google Scholar]
- Wolford E, Lahti M, Tuovinen S, Lahti J, Lipsanen J, Savolainen K, Heinonen K, Hämäläinen E, Kajantie E, Pesonen A-K, Villa PM, Laivuori H, Reynolds RM, & Räikkönen K (2017). Maternal depressive symptoms during and after pregnancy are associated with attention-deficit/hyperactivity disorder symptoms in their 3- to 6-year-old children. PloS One, 12(12), e0190248–e0190248. 10.1371/journal.pone.0190248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan N, & Dix T (2014). Mothers’ early depressive symptoms and children’s first-grade adjustment: a transactional analysis of child withdrawal as a mediator. Journal of Child Psychology and Psychiatry, 55(5), 495–504. 10.1111/jcpp.12189 [DOI] [PubMed] [Google Scholar]
- Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, & Berry JG (2016). Psychiatric disorders and trends in resource use in pediatric hospitals. Pediatrics, 138(5), e20160909. 10.1542/peds.2016-0909 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The de-identifieid data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


