Abstract
Antigenic drift refers to the evolutionary accumulation of amino acid substitutions in viral proteins selected by host adaptive immune systems as the virus circulates in a population. Antigenic drift can substantially limit the duration of immunity conferred by infection and vaccination. Here, I explain the factors contributing to the rapid antigenic drift of the SARS-CoV-2 spike protein and receptor proteins of other viruses and discuss the implications for SARS-CoV-2 evolution and immunity.
Antigenic drift refers to the evolutionary accumulation of amino acid substitutions in viral proteins selected by host adaptive immune systems as the virus circulates in a population. Antigenic drift can substantially limit the duration of immunity conferred by infection and vaccination. Here, I explain the factors contributing to the rapid antigenic drift of the SARS-CoV-2 spike protein and receptor proteins of other viruses and discuss the implications for SARS-CoV-2 evolution and immunity.
Basic concepts in antigenic drift
The estimated 1033 viruses that constitute the virome are earth’s most abundant self-replicating entity. Viruses have small genomes that are quickly replicated upon viral proliferation, facilitating rapid adaptive evolution. Viral genomes encode relatively simple proteomes that are still sufficient to hijack host cell biosynthetic machinery and produce up to a million offspring viruses from a single infectious cycle in a single day. Viral DNA or RNA polymerases exchange accuracy for efficiency, generating nucleotide substitutions at rates upward of 1 substitution per 5,000 copied nucleotides (mutation rate of 2 × 10−4 per base pair; by comparison, the error rate in replicating the human genome is 6,000 times lower). This typically results in each progeny virus having at least one point mutation per genome. Viral genetic variation is further enhanced by codon deletions and/or insertions and recombination between viral genomes, a feature common in coronaviruses (CoVs), and occasionally between viral and host genomes.
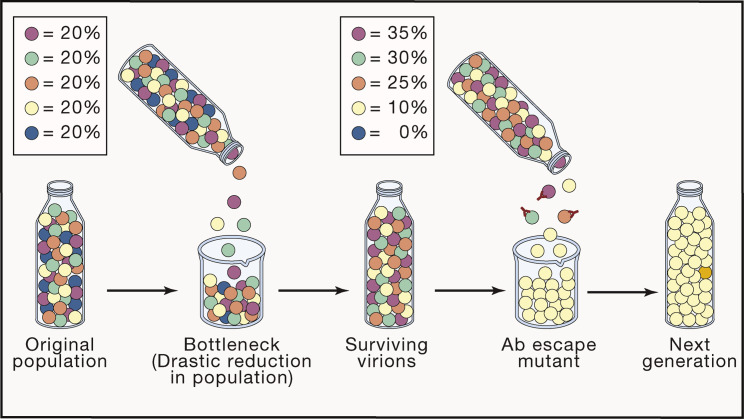
Infected humans can produce 1012 virions—infectious viral particles—during a respiratory virus infection. For the many viruses with high mutation rates, this swarm includes viruses with mutations at each position in the genome and even viruses with all possible nucleotides at any two positions. Such continuously generated robust genetic diversity allows viruses to evolve rapidly under host immune pressure. It is important to distinguish this “genetic drift” from antigenic drift (Figure 1; see Box 1 for terms defined). Genetic drift is the inevitable consequence of high viral mutation rates. Mutations that do not compromise viral replication and transmission are randomly propagated and “fixed” in a virus population when a small number of virions (sometimes just one) transmits the infection to a new host.
Figure 1.
Genetic versus antigenic drift
Nearly every virus generated in a host (depicted as a metaphorical bottle) possesses at least one point mutation. Transmission of a very limited number of viruses between hosts (bottlenecking, 5 different mutants in the figures) results in the random selection of mutants that compete in the new host (generating a hierarchy as shown, with the blue virus becoming extinct with the purple virus at the top), all the while generating a new repertoire of mutants that are bottlenecked in transmitting to the next host. This results in the steady accumulation of mutants as a virus circulates. In the presence of neutralizing Abs, viruses with mutations that enable escape from neutralization are rapidly selected, resulting in antigenic drift. Ab selection can occur either in the transmitting host or the recipient host. In the latter case, this will be a very infrequent event because so few viruses are transmitted, but given enough transmission events to immune individuals, it can contribute to antigenic drift. Note that in the Figure, the yellow mutant is less fit in non-immune host (losing the competition to the other mutants) but much more fit when Ab neutralization is added to the various selection factors.
Box 1. Glossary.
Adaptive immunity: immunity acquired by previous exposure to the immunogen. To be compared with innate immunity, which requires no previous exposure.
Affinity: the thermodynamic measure (binding constant) of the monomeric interaction between two substances. This contrasts with avidity, the binding constant of the interaction between multimeric substrates (such as Abs, which possess 2–10 Ag binding sites, and viruses, which can possess tens to thousand copies of a given antigen).
Antibody: the original functional term coined by pioneering German (antikorper) and French (anticorp) immunologists for substances induced in the blood after introducing infectious agents and other foreign substances. The very first serum transfer experiments (passive immunity) demonstrated that this activity conferred protection against toxins and infectious diseases. Ab responses typically consist of thousands of different immunoglobulins (see below), complicating analysis of their function. The advent of hybridoma technology in the 1970s enabled studies using single Abs (monoclonal Abs, mAbs), which has now been supplemented by direct cloning of Ab genes from isolated B cells.
Antigen: a substance interacting with a given set of antibodies or T cell receptors. Antigenic site refers to highly immunogenic, physically separated regions of antigen recognized by multiple antibodies.
Antigenicity: the magnitude of the antigen-immune receptor interaction, strictly defined operationally by the nature of the immune receptors.
Antigenic drift: gradual change in the antigenicity of viral proteins, driven by antibody selection of escape mutants. T cells can also drive antigenic drift, but only in chronically infected individuals beause MHC polymorphism severely limits the relevance of a given escape mutation in different individuals.
B cells: lymphocytes that produce antibodies. In birds, they develop in the eponymous bursa. In mammals, B cells principally develop in the fetal liver and bone marrow after birth. Humans possess a repertoire of ∼3 × 109 B cell clones that enable responding to an essentially infinite number of immunogens since even completely artificial organic molecules can induce a specific Ab response. After activation, B cells typically switch their heavy chains from IgM to IgA or IgG, which each exhibit unique biological activities that contribute to anti-viral immunity.
Clonal selection: the process that powers adaptive immunity. Individuals possess enormous repertoires of B and T cells, most of which never encounter activating immunogens, and remain in a naïve state, dividing infrequently (∼every 3.5 years). Once activated, clones divide extremely rapidly (4 to 8 h per cell cycle) to expand up to 106-fold to power the immune response.
Epitope: the residues on an antigen that contact or influence the binding of an Ab or TCR. For TCRs, this is defined by naturally processed short peptides bound to a MHC molecule. For Abs, epitopes on globular domains typically are created from residues present in different surface loops of the protein.
Epistatic: compensatory mutation that restores the fitness of a mutated gene product
Immunodominant: the strong tendency of B and T cells to respond hierarchically to complex antigens at the level of proteins and antigenic sites (Abs) and peptides (T cells) is termed immunodominance. For antibodies, the immunodominance of antigenic sites is similar between different species and even between different types of antibodies (immunoglobulins versus lamprey VLRs), consistent with the idea that immunogenicity is based on physicochemical properties of protein regions that enable interactions with other proteins.
Immunogen: a substance that elicits an immune response.
Immunoglobulin: the protein complex that accounts for antibody activity in jawed vertebrates. Generally consisting of heavy and light chains, with the amino-terminal end of each exhibiting enormous variability based on the large number of variable genes present in genomes that are assembled to create each variable region. The variable region is further diversified by randomly adding additional amino acids during the rearrangement process and by mutating the variable regions during B cell activation and maturation in the lymph nodes. This results from clonal competition for immunogen and selecting clones with the highest affinity Igs. During this process, heavy chain switching occurs, causing the initial IgM Ab response to broaden into Abs with IgA and IgG heavy chains. Antibody affinity to viral antigens generally starts at 1 to 10 nM (dissociation constant) and increases up to 1,000-fold with the process of affinity maturation
Memory: during lymphocyte activation, a fraction of activated cells differentiates into cells that patiently await future exposure to the same or cross-reactive immunogen. Such memory cells are present in lymphoid organs and target organs for the pathogen, and they respond more rapidly and naive cells, providing an immediate boost to immunity. B cell differentiation also leads to the generation of plasma cells, which constitutively secrete Abs for years to many decades following their generation. Plasma cells are perhaps the most important target for effective vaccination.
Naive host: an individual who has not been previously exposed to a given immunogen or antigenically cross-reactive immunogens.
Neutralization: the ability of Abs or other substances to prevent virus infection, as typically measured in cultured cells. Abs that block viral entry usually provide the most potent neutralization in vitro and in vivo. Abs that inhibit the release of nascent virions from infected cells will score as neutralizing in multistep infection assays (such as plaque formation) but will be “non-neutralizing” in single-cycle infection assays, e.g., flow cytometric assays using reporter viruses. Abs that fail to neutralize in vitro can still protect in vivo by interacting with innate immune proteins or cells. If this diminishes viral transmission, it can select for escape mutants despite the absence of classical neutralization activity.
If such mutations generate an amino acid substitution that decreases the antigenicity of an immune target protein, this will phenotypically result in antigenic drift. Antigenic drift reduces the efficacy of existing immune effectors targeting the drifted region of the viral protein. Antigenic mutants exist at minute frequencies in viral populations without selection, but with immune selection for viruses that escape immune-mediated neutralization or destruction of infected cells, they come to dominate the population and replace the original virus. In enabling immune escape, antigenic drift compromises immunity conferred by previous infection or vaccination. As described below, antigenic drift is highly relevant to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) evolution as it circulates globally. It has contributed to the present need for booster shots and will necessitate updating vaccines to match drifting variants, as is practiced for influenza.
Host anti-viral immunity
Host organisms (from bacteria to blue whales), faced with dangerous parasitic viral hordes throughout their evolutionary history, evolved multilayered defenses beginning at the level of individual cells. Bacteria, the first organisms to deal with viruses, developed innate (e.g., restriction enzymes) and adaptive (e.g., CRISPR) anti-viral immune mechanisms. Likewise, nearly all cells in multicellular organisms possess robust anti-viral innate immune sensing and effector functions that limit viral entry, transcription, translation, and assembly. In vertebrates, this includes up to 1,500 genes induced by interferons, cytokines with potent anti-viral activities. Multicellular organisms express soluble proteins and glycans that exhibit anti-viral activity. Anti-viral activity in vertebrates is supplemented by the adaptive immune system, comprised of humoral (B cell-based) and cellular (T cell-based) arms.
B cells generate humoral immunity by secreting immunoglobulins (Igs; also known as antibodies, Abs) that are specifically selected for high-affinity binding to foreign substances. By five or so days after infection or immunization, specific Abs can be detected in serum in the form of IgM heavy chains. Over the next three weeks, Ab levels increase and shift to IgG and IgA heavy chains as antibody affinity increases because of ongoing somatic mutation, reducing the levels of Abs needed for protection. Most IgA Abs are delivered to mucosal surfaces, while IgG Abs typically function in blood, lymph, and tissues. Specific Ab-producing cells persist from weeks to a lifetime depending on the nature of the immunogen.
Abs protect against viral infections in many ways. The simplest and typically most effective mechanism is to bind to virion surface proteins and prevent virus attachment to host cells or viral penetration to the cytosol. The relevant target protein for SARS-CoV-2 and other CoVs is the spike glycoprotein, which gives CoVs their crown in electron micrographs and attaches virions to ACE2 receptors on host cells. Such Ab-mediated “neutralization” is the only adaptive immune mechanism to provide truly sterilizing immunity: i.e., zero virus infection of host cells. The Ig N terminus, known as the Fc domain, functions as a bridge to innate immune effector functions. These include binding to Fc receptors on natural killer cells or macrophages, which, respectively, can kill infected cells displaying bound anti-viral Abs or phagocytose and destroy Ab-decorated virions. Fc also can interact with complement proteins to lyse cells expressing viral surface proteins or enhance the potency of Abs bound to the virion surface.
Abs are complemented by T cells responding specifically to viral peptides presented by major histocompatibility complex (MHC) class I and II molecules. CD8+ T cells are famous for their ability to lyse virus-infected cells expressing class I molecules complexed with viral peptides, but CD4+ T cells can also kill cells that express MHC class II molecules presenting viral peptides. Unlike class I molecules, which are constitutively expressed on nearly all cell types, class II molecules are expressed by immune cells and a few non-immune cells (including type II pneumocytes, a target cell for many respiratory viruses), though they are induced on many cell types by interferons. CD4+ T cells also play an essential role in B cell Ig class switching, somatic mutation, and memory cell formation.
Viral escape from host immunity
Every virus must evolve to evade innate host cellular immunity. This entails dealing with intracellular mechanisms that limit viral transcription and translation and extends in multicellular organisms to evading extracellular proteins that prevent viral entry. The barriers that limit zoonotic virus establishment in a new species are host cell receptor binding and entry, innate immunity, and transmission to the next host. Evolution rapidly optimizes viral genes to maximize transmission during the early phase of viral adaptation to a new species. In a pandemic, it is expected that as tens of thousands of individuals are sequentially infected, a newly introduced virus will reach a near-optimal genotype for humans. Selection of additional mutations can occur as the virus encounters consistent differences in host polymorphic innate immune genes or weather and/or behavioral conditions that influence transmission.
The strongest selection pressure after adaptation occurs, however, when the virus encounters the adaptive immune system. For SARS-CoV-2 and other acute viruses infecting naive hosts, viral transmission is likely to occur before the transmitting host can mount an effective immune response, which requires a week or more following infection. Thus, early in a pandemic, with so many naive hosts available, there will be limited adaptive immune pressure. However, as the vaccinated or previously infected population grows, immune pressure increases, raising the possibility of variants selected by immune escape (Figure 1 ).
Evading Ab recognition
Abs typically interface with protein antigens over a ∼750 Å2 area, consisting of ∼15 interacting amino acids on both Ab and antigen, with five key residues providing the bulk of the free energy that accounts for binding. Substituting any of these critical epitope residues or deletion and/or insertion of residues can reduce Ab affinity by several orders of magnitude, which is usually sufficient to escape from monoclonal Ab (mAb)-mediated neutralization (Figure 2A). Changes outside of the contact region can also enable escape, depending mainly on the conformational dynamics of the viral antigen that can limit access of an Ab to its epitope. Antigenic drift is due predominantly to amino acid substitutions within epitopes that reduce antibody avidity but also results from substitutions that alter protein “breathing”—temperature-dependent gyrations in secondary, tertiary, and quaternary protein structure—to reduce access of an Ab to its epitope and substitutions that add N-linked glycans or other post-translational modifications that reduce antibody binding sterically or chemically.
Figure 2.
Mechanisms of immune escape
(A) Viruses can avoid Ab-mediated neutralization by acquiring point mutations encoding amino acid substitutions that directly reduce Ab binding (top), introduce a N-linked glycan that sterically blocks antibody binding (bottom), induce conformational changes that prevent Ab access to its epitope (not shown), or in the case of “absorptive mutants”, increase receptor binding to shift the equilibrium to favor virus association with the host cell versus the neutralizing Ab (not shown).
(B) Viral proteins subject to antigenic drift navigate a fitness landscape that constrain their evolution. Achieving the highest levels of fitness (blue path) may entail a step of lower fitness, which will greatly slow the process. Moving down a given path limits the available choices of amino acids that improve fitness with the practical effect of preventing accurate predictions of antigenic drift and future vaccine strains.
Viral immune escape is constrained by, first, the mutational space of a single nucleotide substitution in the relevant codon to generate an amino acid substitution that reduces Ab binding energy and, second, the ability of the antigen to accommodate a given amino acid substitution and maintain sufficient function to support viral fitness under the selection conditions. With sufficient immune pressure, viral escape mutants with compromised fitness can continue to replicate and explore additional mutational space to improve fitness from an “epistatic” mutation in a different residue in the same protein or even another viral protein with a complementary function (Figure 2B). For example, selection of influenza A virus (IAV) hemagglutinin (HA) escape mutants can select for compensatory mutations in the viral neuraminidase and vice versa to balance the binding and releasing activities of the two proteins.
As drift proceeds in a given viral protein, each amino acid substitution changes the evolutionary fitness landscape. This includes the effects of future substitutions on escaping antibody binding as well as protein fitness. This, in addition to the randomness of mutation and selection, makes predicting antigenic drift in circulating viruses extremely difficult, if not impossible. This is well illustrated by the reintroduction of a human 1950 IAV in 1977. The parallel HA evolutionary trajectories of the virus lineages from 1950–1957 versus 1977–onward were completely distinct, with few common sites of substitutions and even fewer common substitutions (Figure 2 ). Compounding the difficulty of predicting IAV antigenic drift, an enormous variety of mutants cocirculate at any given time, with one lineage eventually sweeping the world on the scale of months to years.
Selection can occur immediately upon a virus contacting host tissues if Abs present in respiratory secretions do not completely neutralize the virus. Ab responses are polyclonal, comprised of dozens to hundreds of different Abs specific for a given viral receptor protein, but responses are typically biased to antigenic sites that are immunodominant. Further, individuals can have a highly biased response to a single antigenic site. A single amino acid substitution can enable escape from biased responses, particularly when weak, initiating antigenic drift. Since epitopes in and around viral receptor-binding sites (RBS) are frequently both immunodominant and an efficient target of neutralizing Abs, these are often mutated.
Changes in residues in and around the RBS can alter RBS binding affinity and/or specificity (two sides of the same coin). Such “adsorptive” mutations that increase binding to host cells can be directly selected when a virus faces a subneutralizing Ab response balanced across multiple antigenic sites. For viruses that like IAV using sialic acid as receptors, amino acid substitutions that increase the net positive charge of the HA can increase binding to negatively charged sialic acid receptors. Adsorptive mutants are typically less fit in naive hosts or hosts with low Ab levels because such tight binding can compromise viral entry or the release of progeny virus. If so, this will result in selection for mutants with decreased receptor avidity. This ratcheting mechanism acting as virus circulates between immune and naive hosts will generate mutations in the globular domain with each cycle. Since these residues can be in neutralizing epitopes, this process will appear to be classical antigenic drift, illustrating the potential uncertainties in assigning selective forces to fixation of any given mutant.
Receptor proteins of enveloped viruses are almost always glycosylated at multiple asparagine residues. Some glycan locations are highly conserved between strains, and these often are needed for glycoprotein biogenesis and function. Other glycan sites are selected to sterically shield epitopes from neutralizing Abs. This is a highly effective method of escape and, depending on glycan size and location, can reduce the binding of Abs to multiple antigenic sites. Adding glycan sites typically entails high fitness costs that epistatic mutations must offset, limiting their frequency. Even less frequently, epistatic glycan addition can (ironically) offset the fitness costs of standard escape mutations. Influenza virus hemagglutinins (HAs) appear to have a limit for adding glycans with the number of addable glycans specific for each HA subtype. Reaching the limit stifles antigenic drift, paving the way for the introduction of a new zoonotic strain.
Evading T cell recognition
In principle, CD8+ T cells can select for viral escape mutants by limiting viral replication in individual cells. As with antibody escape, single amino acid substitutions can diminish TCR binding to peptide-class I complexes to sub-activating levels. Viral mutations can also limit the generation of antigenic peptides. T cell selection for escape mutants is well established in human chronic infections. In an individual HIV patient, for example, escape can be relatively rapid, robust, and ongoing. In this circumstance, viruses need only to escape from a single set restricting MHC molecules. Such viral escape is likely a significant factor leading to the remarkable polymorphism of MHC class I, which renders escape moot as viruses transmit between MHC disparate individuals. Thus, in genetically diverse populations, viral T cell escape is of limited concern
Antigenic drift in SARS-CoV-2 spike
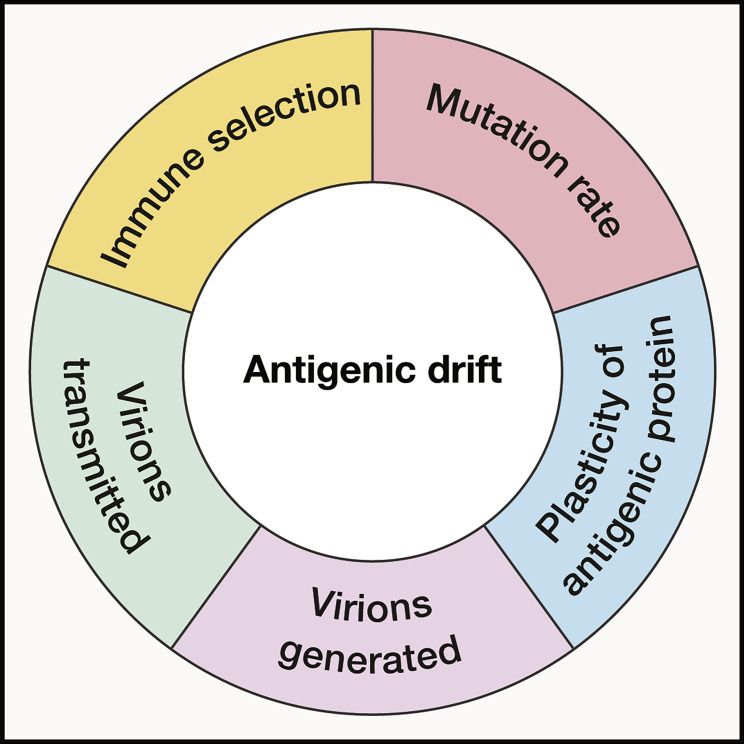
All viral genes derive from a small number of common ancestor genes. Consequently, all viral proteins can genetically diverge and maintain function and, given time, evolve to escape immune or other selection pressures. The key to antigenic drift in viral target proteins, then, is its speed as a virus evolves during host transmission. For any given protein in any given virus, this is related to multiple factors (Figure 3 ). These include:
-
(1)
Intrinsic mutation rate of the viral polymerase and the number of virions generated in an individual that can potentially be transmitted.
-
(2)
Capacity of the viral protein to accept amino acid substitutions that reduce antibody binding while maintaining viral fitness and its ability to increase fitness by epistatic changes. This can vary widely among proteins. For example, measles virus receptor and fusion proteins, which are antigenically invariant, do not easily tolerate random amino acid insertions, in contrast to HA in IAV. The antigenically variable regions of HA and NA are also known to tolerate random mutations and insertions better than antigenically conserved regions in HA or other influenza proteins
-
(3)
Number of virions that initiate infection. This number likely ranges from 1 to 100 or so virions. Ab selection for single amino acid substitutions will occur, given enough transmission events, even with just a few virions. With more virions, selection will be proportionally higher.
-
(4)
Number of viruses generated during infection. More replication means a broader repertoire of mutants for selection.
-
(5)
Nature of the immune selection pressure, particularly the extent to which “Goldilocks” conditions are met, i.e., a moderate response focused on one (or possibly two) antigenic sites.
Figure 3.
Factors contributing to the rate of antigenic drift
The rate of drift is the product of the (1) intrinsic mutation rate of the viral polymerase, (2) capacity of the viral protein to accept amino acid substitutions that reduce Ab binding while maintaining viral fitness and its ability to increase fitness by epistatic changes, (3) number of virions that initiate infection, (4) number of viruses generated during infection, and (5) the nature of the immune selection pressure on antigenic sites.
Until recently, human CoVs were considered antigenically stable. Circulating IAVs, the poster viruses for antigenic drift, accumulate 1 to 1.5 amino acid substitutions per year in their two target proteins (HA and NA), with nearly all substitutions on the protein surface and many in established antigenic sites. Drift in the H3 HA over 22 years has necessitated 16 vaccine updates. Over 32 years, the 229E seasonal CoV spike exhibits 46 substitutions, with many substitutions in regions likely to be recognized by neutralizing Abs. The substitution rate, 1.4 per year, is at the high end of human influenza A HAs and higher than influenza B virus HAs.
Where HA and seasonal CoV spike differ is in N-linked glycan evolution. The 229E spike has 24 predicted N-linked glycans, which are completely conserved over 32 years of evolution in humans. Over 32 years of evolution during the same period, the H3 HA added three glycans to the antigenic regions.
In its brief evolution in humans, the SARS-CoV2 spike has exhibited astonishingly rapid evolution. In less than one year, the delta variant spike (isolated in October 2020) now sweeping the world accumulated a deletion and nine substitutions. As with 229E, the N-linked glycan sites have been highly conserved, with only 1,236 out of 519,035 (0.2%) isolate sequences demonstrating alterations to glycan sites (near all are single-site losses). The recently described omicron mutant, which appears to be becoming dominant in South Africa, possesses 35 amino acid changes in spike. This rate of spike evolution (substitutions per residue per year), approximately 10-fold higher than influenza HA, is unprecedented in an acute virus and prompts serious consideration of reformulating vaccines to induce T cell responses to more CoV2 proteins.
Most naturally selected spike amino acid substitutions, particularly those present in the RBD, also result from mAb selection in vitro, supporting their Ab-based in vivo selection. Curiously, many of these changes occurred during transmission in a largely naive human population. Because viral transmission is likely to occur before the generation of a significant neutralizing antibody response, this suggests that selection may have predominantly occurred in chronically infected individuals with compromised immunity with weak Ab responses that facilitate escape.
Current evidence suggests that while spike antigenic drift facilitates SARS-CoV-2 reinfection, infection and vaccine-induced Ab and T cell responses still provide robust, if imperfect, immunity to serious disease and death from the delta variant. The extent to which this applies to the omicron variant remains to be determined. Based on seasonal CoVs and other human respiratory viruses, it is likely that as immunity wanes following infection and/or vaccination, individuals will be infected every few years with SARS-CoV-2, with serious disease being an unusual outcome. To what extent repeated boosting will remain necessary to prevent moderate to severe disease among different risk groups is an open question. Monitoring the outcome of differential vaccination rates between locales should provide answers over the next few years.
Recap
The high mutation rate of many viruses enables their rapid evolution to increase transmission between individuals. Adaptive immunity to viruses can exert high selection pressure, resulting in antigenic drift in T cell and Ab epitopes. For acute viruses, antigenic drift is essentially limited to Ab-mediated selection for viruses with mutations in virion surface proteins. These mutations reduce the avidity by several logs of Abs capable of reducing viral transmission. Mutations can reduce antibody binding by either changing the amino acids in the epitope, limiting the exposure of the epitope to the Ab, or enabling addition of glycans that limit Ab access to its epitope. Mutations are constrained by their effect on protein function, which epistatic mutations can alleviate in the same or other viral proteins. Viruses demonstrate considerable differences in the rate of antigenic variation based on multiple factors. Antigenic drift in the SARS-CoV-2 spike is occurring surprisingly rapidly compared with other acute viruses, possibly even 10-fold faster than the IAV HA. This will likely necessitate vaccine updating regularly if it continues unabated in future years. Predicting antigenic drift is likely not possible, so vaccine selection will need to be empirical, based on the currently dominating circulating strain. Serious consideration should be given to broadening vaccines to induce responses to multiple CoV2 proteins.
Acknowledgments
J.W.Y. is supported by the Division of Intramural Research, NIAID. The author is grateful to Seth Margolis (Johns Hopkins University) and William Yewdell (Memorial Sloan Kettering Institute) for their thoughtful comments and suggestions.
Recommended reading
- Altman M.O., Angel M., Košík I., Trovão N.S., Zost S.J., Gibbs J.S., Casalino L., Amaro R.E., Hensley S.E., Nelson M.I., Yewdell J.W. Human Influenza A Virus Hemagglutinin Glycan Evolution Follows a Temporal Pattern to a Glycan Limit. MBio. 2019;10:e00204-19. doi: 10.1128/mBio.00204-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angeletti D., Gibbs J.S., Angel M., Kosik I., Hickman H.D., Frank G.M., Das S.R., Wheatley A.K., Prabhakaran M., Leggat D.J., et al. Defining B cell immunodominance to viruses. Nat. Immunol. 2017;18:456–463. doi: 10.1038/ni.3680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das S.R., Hensley S.E., David A., Schmidt L., Gibbs J.S., Puigbò P., Ince W.L., Bennink J.R., Yewdell J.W. Fitness costs limit influenza A virus hemagglutinin glycosylation as an immune evasion strategy. Proc. Natl. Acad. Sci. USA. 2011;108:E1417–E1422. doi: 10.1073/pnas.1108754108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das S.R., Hensley S.E., Ince W.L., Brooke C.B., Subba A., Delboy M.G., Russ G., Gibbs J.S., Bennink J.R., Yewdell J.W. Defining influenza A virus hemagglutinin antigenic drift by sequential monoclonal antibody selection. Cell Host Microbe. 2013;13:314–323. doi: 10.1016/j.chom.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis A.K.F., McCormick K., Gumina M.E., Petrie J.G., Martin E.T., Xue K.S., Bloom J.D., Monto A.S., Bushman F.D., Hensley S.E. Sera from individuals with narrowly focused influenza virus antibodies rapidly select viral escape mutations in ovo. J. Virol. 2018;92:e00859-18. doi: 10.1128/JVI.00859-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eguia R.T., Crawford K.H.D., Stevens-Ayers T., Kelnhofer-Millevolte L., Greninger A.L., Englund J.A., Boeckh M.J., Bloom J.D. A human coronavirus evolves antigenically to escape antibody immunity. PLoS Pathog. 2021;17:e1009453. doi: 10.1371/journal.ppat.1009453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer W., Giorgi E.E., Chakraborty S., Nguyen K., Bhattacharya T., Theiler J., Goloboff P.A., Yoon H., Abfalterer W., Foley B.T., et al. Network for Genomic Surveillance in South Africa (NGS-SA) HIV-1 and SARS-CoV-2: Patterns in the evolution of two pandemic pathogens. Cell Host Microbe. 2021;29:1093–1110. doi: 10.1016/j.chom.2021.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulton B.O., Sachs D., Beaty S.M., Won S.T., Lee B., Palese P., Heaton N.S. Mutational Analysis of Measles Virus Suggests Constraints on Antigenic Variation of the Glycoproteins. Cell Rep. 2015;11:1331–1338. doi: 10.1016/j.celrep.2015.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han A.X., Maurer-Stroh S., Russell C.A. Individual immune selection pressure has limited impact on seasonal influenza virus evolution. Nat. Ecol. Evol. 2019;3:302–311. doi: 10.1038/s41559-018-0741-x. [DOI] [PubMed] [Google Scholar]
- Huang K.Y., Rijal P., Schimanski L., Powell T.J., Lin T.Y., McCauley J.W., Daniels R.S., Townsend A.R. Focused antibody response to influenza linked to antigenic drift. J. Clin. Invest. 2015;125:2631–2645. doi: 10.1172/JCI81104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko S.H., Bayat Mokhtari E., Mudvari P., Stein S., Stringham C.D., Wagner D., Ramelli S., Ramos-Benitez M.J., Strich J.R., Davey R.T., Jr., et al. High-throughput, single-copy sequencing reveals SARS-CoV-2 spike variants coincident with mounting humoral immunity during acute COVID-19. PLoS Pathog. 2021;17:e1009431. doi: 10.1371/journal.ppat.1009431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Boutz D.R., Chromikova V., Joyce M.G., Vollmers C., Leung K., Horton A.P., DeKosky B.J., Lee C.H., Lavinder J.J., et al. Molecular-level analysis of the serum antibody repertoire in young adults before and after seasonal influenza vaccination. Nat. Med. 2016;22:1456–1464. doi: 10.1038/nm.4224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linderman S.L., Chambers B.S., Zost S.J., Parkhouse K., Li Y., Herrmann C., Ellebedy A.H., Carter D.M., Andrews S.F., Zheng N.Y., et al. Potential antigenic explanation for atypical H1N1 infections among middle-aged adults during the 2013-2014 influenza season. Proc. Natl. Acad. Sci. USA. 2014;111:15798–15803. doi: 10.1073/pnas.1409171111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanjuán R., Domingo-Calap P. Mechanisms of viral mutation. Cell. Mol. Life Sci. 2016;73:4433–4448. doi: 10.1007/s00018-016-2299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu N.C., Wilson I.A. Influenza Hemagglutinin Structures and Antibody Recognition. Cold Spring Harb. Perspect. Med. 2020;10:a038778. doi: 10.1101/cshperspect.a038778. [DOI] [PMC free article] [PubMed] [Google Scholar]