Abstract
An invasive moth, Lymantria dispar dispar, also known as the gypsy moth, originates from Europe and first came to Ontario, Canada, in 1969. The moth is a defoliator which feeds on oak and other deciduous trees, and less commonly, conifers. Outbreaks of Lymantria dispar dispar moth infestation occur every 7–10 years with rapid expansion of the population until there is a natural collapse due to pathogens and predators. In addition to the extensive environmental impact of defoliation of the tree canopy, the Lymantria dispar dispar moth larva (caterpillar) is responsible for causing a significant cutaneous eruption in exposed individuals. In our report, we describe six cases of Lymantria dispar dispar dermatitis which occurred in Ontario, Canada, in May of 2021. It is important for dermatologists to be aware of this potential diagnosis and to be aware of local infestation in affected areas.
Keywords: Lymantria dispar dispar, gypsy moth, dermatitis
Introduction
Lymantria dispar dispar (LDD), also known as the gypsy moth, is an invasive species originating from Europe and first found in Ontario, Canada, in 1969. 1 It is a defoliator that feeds on oak, maple, willow, and other broadleaf trees. The larvae of this species are responsible for devouring leaves and present during the months of April through July (Figure 1). Contact with LDD can cause an acute contact dermatitis characterized by erythematous and urticarial papules, often with excoriations. LDD outbreaks occur every 7–10 years and currently Ontario is heavily infested. Defoliation caused by these moths saw a staggering 1200% increase between 2019 and 2020 1 and continues today.
Figure 1.
Lymantria dispar dispar (LDD) larva seen outdoors during the month of May in Ontario, Canada. (a) LDD at an early instar stage. (b) Cluster of LDD larva infesting a tree in southern Ontario. Photo courtesy of A O’Toole (a) and M Hartviksen (b).
Case report
We report six cases of LDD dermatitis that occurred in Ontario, Canada, in May 2021 which presented over the span of 3 days. The cases were reported in central, eastern, and southern Ontario. The first case involved a 52-year-old healthy female from Wellington County who presented with widespread erythematous papules on her arms (Figure 2) and chest. She was removing an infestation of nests from her front porch and had noted caterpillars escaping the nest. Within 24 h, the patient developed erythema, swelling, and pruritus at the exposed sites. After 2 days, she developed extremely pruritic papules and the pruritus woke the patient from her sleep. The patient learned others in her neighborhood were experiencing similar signs and symptoms. She was treated with a tapering course of prednisone over 2 weeks with good effect.
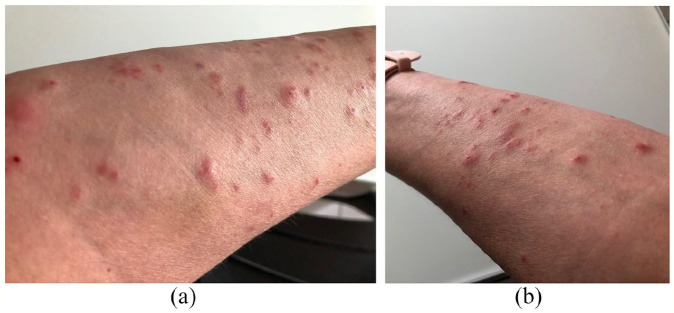
Figure 2.
(a) and (b) Typical eruption of excoriated papules and urticarial lesions on the forearm of patient #1. Photos courtesy of M Gooderham.
The second case involved a 45-year-old healthy female from Northumberland County who presented with numerous excoriated inflammatory papules which were solitary, in groups, or linear and mainly on her forearms. The patient had noticed caterpillars dropping from trees above onto her while she was spending time outdoors with her family. Within days, the eruption spread and was treated with betamethasone valerate 0.1% cream as required.
The third case was a 74-year-old male from Peterborough County with a 1.5-week history of an extremely pruritic and exudative rash involving the posterior neck, forearms, and abdomen. The rash started shortly after doing yardwork in a short-sleeved shirt while exposed to multiple caterpillars. This patient was treated with betamethasone valerate 0.1% cream and was offered a course of prednisone if the papules worsened.
The fourth case also from Peterborough County involved a 63-year-old female who developed multiple extremely pruritic erythematous papules and pseudovesicles on her forearms and abdomen after doing yard work. She has a known infestation of the moths on her property awaiting extermination.
The fifth case reported from Simcoe County involved a healthy 47-year-old male who, while working as a camera operator at an outdoor film shoot, was exposed to approximately 20 caterpillars on his body at one time. Two days later, he developed pruritic erythematous papules on his posterior neck and forearms. He reported similar signs and symptoms in the rest of the film crew as well. The patient’s rash resolved in 2 weeks without specific therapy.
The sixth case from the Ottawa area was a 30-year-old female who lives in a rural location. The patient reported she had an infestation of caterpillars on her property. She was taking care of her lawn and garden when she noted caterpillars on her exposed arms and on her T-shirt. Overnight, she developed pruritic erythematous urticarial plaques and papules on her arms, as well as a serpiginous pattern of papules on her abdomen (Figure 3). She was treated with clobetasol 0.05% twice a day for pruritus and the lesions resolved slowly over the following week.
Figure 3.
(a) and (b) Serpiginous and clustered eruption of pruritic papules in patient #6. Photos courtesy of J Beecker.
Discussion
The etiology of LDD dermatitis has not been fully elucidated. Evidence suggests a delayed-type hypersensitivity to the hairs of the LDD caterpillars is at least partly responsible. 2 The hairs contain thaumetopoein, a type of nettle poison, as well as histamine which can cause the skin to react initially. 2 Increased risk of hypersensitivity can be related to prior history of exposure, direct contact or indirect exposure to a caterpillar (e.g. hanging laundry outside to dry), or a history of hay fever. 3
The first North American cited gypsy moth outbreak occurred in north-eastern United States in 1981. At the time, many cases of dermatitis were reported not only to public health officials but also in the literature. 4 One report at the time by Beaucher and Farnham 2 described eight cases of LDD caterpillar dermatitis as being papular, pruritic, erythematous and at times vesicular rashes located on the arms, legs, back of neck, feet, and flank area, which were similar to our reported cases. Beaucher and Farnham 2 carried out patch testing with the hairs of the LDD caterpillar on all eight patients with a history of LDD dermatitis as well as 11 controls. In all patients with a history of dermatitis, there was a positive patch test result; however, no reaction was observed in 10 out of the 11 controls, confirming a delayed-type hypersensitivity response. In addition, many patients required treatment with systemic corticosteroids after failure of topical treatments and antihistamines, due to the intensity of pruritus, similar to some of our patients. 2 Furthermore, among cases reported in 1981, urticaria after exposure to caterpillar hairs was also documented in addition to dyspnea and rhinitis in some patients.2,4 Interestingly, the reports from 1981 also found that many cases of LDD dermatitis occurred in May, similar to our report, with skin reactions occurring within 12 h after exposure. 4 Another review by Kikuchi et al. 5 in Japan that reported on 229 cases of LDD dermatitis also found that areas primarily affected were the neck and arms and eruptions were less likely in those aged above 70 years old. 5
This report summarizes six cases of LDD dermatitis due to a current outbreak in Ontario. Our cases were strikingly similar to previous reports with erythematous lesions and pruritus developing within 1–2 days in exposed areas including the posterior neck, forearms, and trunk. Dermatologists as well as family physicians should be aware of local infestations of the species as well as the potential dermatological manifestations related to exposure. Improved public and provider recognition can lead to prompt diagnosis and initiation of appropriate treatment. Although outbreaks occur infrequently, they can be associated with a significant public health concern leading to patients seeking medical care due to a significant impact on quality of life.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was obtained for use of clinical photographs.
ORCID iDs: Jennifer Beecker  https://orcid.org/0000-0003-0872-3388
https://orcid.org/0000-0003-0872-3388
Melinda J Gooderham  https://orcid.org/0000-0001-8926-0113
https://orcid.org/0000-0001-8926-0113
References
- 1. Ministry of Natural Resources Forestry. Gypsy moth. Ontario.ca, 2021, https://www.ontario.ca/page/gypsy-moth (accessed 30 May 2021).
- 2. Beaucher W, Farnham J. Gypsy-moth-caterpillar dermatitis. N Engl J Med 1982; 306(21): 1301–1302. [DOI] [PubMed] [Google Scholar]
- 3. Tuthill R, Canada A, Wilcock K, et al. An epidemiologic study of gypsy moth rash. Am J Public Health 1984; 74(8): 799–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shama S, Etkind P, Odell T, et al. Gypsy-moth-caterpillar dermatitis. N Engl J Med 1982; 306(21): 1300–1301. [DOI] [PubMed] [Google Scholar]
- 5. Kikuchi T, Kobayashi K, Sakata K, et al. Gypsy moth-induced dermatitis: a hospital review and community survey. Eur J Dermatol 2012; 22(3): 384–390. [DOI] [PubMed] [Google Scholar]