Supplemental Digital Content is available in the text
Keywords: abdominal injury, computed tomography, diagnostic accuracy, meta-analysis, military setting
Abstract
Background:
It is critical to accurately identify patients with abdominal injury who truly need to undergo laparotomy during the war in timely fashion. The diagnostic utility of computed tomography (CT) for evaluating abdominal injury in the military setting remains uncertain.
Methods:
PubMed, EMBASE, and Cochrane Library databases were searched. Meta-analyses were performed by using a random-effect model. We pooled the area under the summary receiver operating characteristic curves with standard errors, the Q indexes with standard errors, the sensitivities with 95% confidence intervals (CIs), the specificities with 95% CIs, the positive likelihood ratios with 95% CIs, the negative likelihood ratios with 95% CIs, and the diagnostic odds ratios with 95% CIs. The heterogeneity among studies were evaluated by the I2 and P value.
Results:
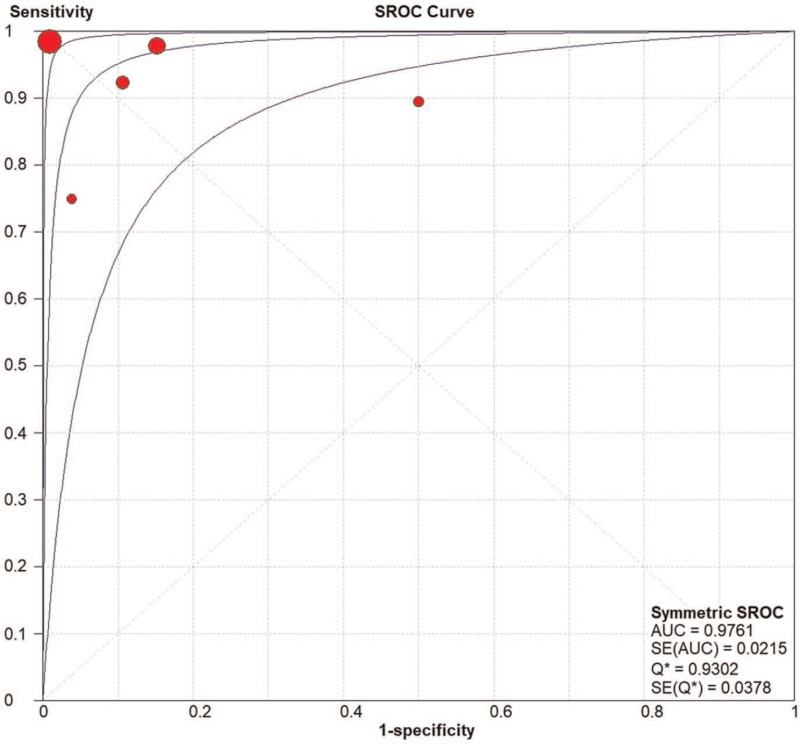
Overall, 5 retrospective studies were included. The area under the summary receiver operating characteristic curve was 0.9761 ± 0.0215 and the Q index was 0.9302 ± 0.0378. The pooled sensitivity was 0.97 (95% CI = 0.92–0.99) without a significant heterogeneity among studies (I2 = 0%, P = .4538). The pooled specificity was 0.95 (95% CI = 0.93–0.97) with a significant heterogeneity among studies (I2 = 90.6%, P < .0001). The pooled positive likelihood ratio was 10.71 (95% CI: 2.91–39.43) with a significant heterogeneity among studies (I2 = 89.2%, P < .0001). The pooled negative likelihood ratio was 0.07 (95% CI = 0.02–0.27) with a significant heterogeneity among studies (I2 = 57.5%, P = .0516). The pooled diagnostic odds ratio was 177.48 (95% CI = 18.09–1741.31) with a significant heterogeneity among studies (I2 = 75.9%, P = .0023).
Conclusion:
Diagnostic accuracy of CT for abdominal injury is excellent in the military setting. Further work should explore how to shrink CT equipment for a wider use in wartime.
1. Introduction
Generally, laparotomy is the first-line treatment option for controlling bleeding and infections in patients with abdominal penetrating wounds.[1,2] However, a proportion of laparotomies are unnecessary and/or inappropriate. The rate of nontherapeutic laparotomy is 27% to 40% in patients who underwent laparotomy.[3–5] Additionally, the incidence of complications related to laparotomy is 22% to 41%, which will prolong the hospital stay and increase the medical burden.[6,7] Therefore, in the military setting, it is important to identify patients with abdominal injury who truly need to undergo laparotomy.
Physical examinations, mainly including vital signs, hemodynamics, and abdominal tenderness and rebound,[8] are performed to initially screen these patients. However, the diagnostic accuracy of injury based on physical examinations alone is poor. Additionally, focused assessment with sonography in trauma (FAST) seems to be a convenient non-invasive tool for evaluating injury in the battle front, but its diagnostic sensitivity is unsatisfactory.[9] During the past 2 decades, computed tomography (CT) has been widely recognized an auxiliary approach for evaluating abdominal injury in the military setting.[10] Herein, we performed a systematic review and meta-analysis to explore the diagnostic performance of CT for evaluating abdominal injury in the military setting.
2. Methods
The current study was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements.[11] Because it was a systematic review and meta-analysis of published data, its ethical approval was not necessary.
2.1. Registration
The current study was registered in the PROSPERO and the registered number was CRD42019138248.
2.2. Literature search
PubMed, EMBASE, and Cochrane Library databases were searched and the last search date was August 28, 2021. Search items as follows: ((Computed tomography) OR (CT)) AND ((Combat) OR (War) OR (Military)) AND ((Injury) OR (Trauma)). There was no language limitation.
2.3. Selection criteria
Included studies should explore the diagnostic accuracy of CT for abdominal injury in the military setting. Exclusion criteria are as follows: duplicates; guidelines, reviews, or meta-analyses; case reports, comments, or letters; experimental or animal studies; studies unrelated to military setting; studies unrelated to CT; studies unrelated to abdominal injury; and relevant data cannot be extracted.
2.4. Outcomes
The major outcome of this study should be the diagnostic performance of CT for evaluating abdominal injury in the military setting.
2.5. Data extraction
The following information were extracted from the included studies: first author; year of publication; country; study design; sample size; inclusion and exclusion criteria; source of patients; CT machines; period of enrollment; characteristics of injured casualties; reference standard for injury; true-positive value; false-positive value; false-negative value; and true-negative value. Disagreement was resolved by a consensus among researchers.
2.6. Study quality assessment
Study quality was assessed by using the quality assessment of diagnostic accuracy studies-2 tool (QUADAS-2).[12] The QUADAS-2 includes 4 domains: patient selection, index test, reference standard, and flow and timing. For the first 3 domains, both risk of bias and applicability concerns are evaluated. For the last domain, only the risk of bias is evaluated. The risk of bias is rated as “low risk,” “high risk,” and “unclear risk.” The applicability concern is rated as “low applicability,” “high applicability,” and “unclear applicability.” Studies with more “low risk” and “high applicability” are of high quality.
2.7. Statistical analysis
In a diagnostic accuracy meta-analysis, the diagnostic threshold effect was firstly evaluated by the Spearman correlation coefficient and P value. The Spearman correlation coefficient,[13] reflecting the linear correlation of thresholds among these included studies, ranges from −1 to +1. The magnitude of this coefficient indicates the extent to which thresholds are scattered. If a coefficient was closer to −1 or +1, the scatter would be less. A coefficient of +1 or −1 indicates a perfect correlation among these thresholds in included studies; and a coefficient of 0 indicates no correlation among these thresholds in included studies. If the diagnostic threshold effect was not statistically significant (P > .05), the area under the summary receiver operating characteristic curves (AUSROCs) with standard errors (SEs), Q indexes with SEs, sensitivities with 95% confidence intervals (CIs), specificities with 95% CIs, positive likelihood ratios with 95% CIs, negative likelihood ratios with 95% CIs, and diagnostic odds ratios (DORs) with 95% CIs would be calculated. If the diagnostic threshold effect was statistically significant (P < .05), only AUSROCs with SEs and Q indexes with SEs would be calculated, avoiding the inaccuracy of statistical results. An AUSROC of >0.9, 0.7 to 0.9, and 0.5 to 0.7 refers to a high, moderate, and low diagnostic accuracy, respectively. The Q index, which is the true positive rate of a diagnostic test, ranges from 0 to 1. If the Q index was higher, a diagnostic test would have a better diagnostic performance. A higher sensitivity suggests that a diagnostic test has a better performance of screening a disease, and a higher specificity suggests that a diagnostic test has a better performance of identifying a disease. For example, if a diagnostic test had a sensitivity of 0.80 and a specificity of 0.90, the possibility of a true disease would be 80% in a patient with a positive diagnostic result, and the possibility of no disease would be 90% in a patient with a negative diagnostic result. DOR reflects the association between a positive diagnostic test and a true disease. A DOR of >1 suggests that a patient with a true disease could have a higher rate of a positive diagnostic test; a DOR of =1 suggests that a positive diagnostic test could not be employed for the diagnosis of a true disease; and a DOR of <1 suggests that a patient with a true disease could have a higher rate of a negative diagnostic test. The heterogeneity among studies was evaluated using the chi-squared test and the inconsistency index I2. P < .1 and/or I2 > 50% were considered as statistically significant heterogeneity. All statistical analyses were performed by Meta-Disc software version 1.4,[14] which has been developed by the Unit of Clinical Biostatistics team of the Ramón y Cajal Hospital in Madrid, Spain.
3. Results
3.1. Study selection
Overall, 4871 papers were identified. Finally, 5 studies were included[15–19] (Fig. 1). The characteristics of included studies were summarized in the Table 1. They were published between 2001 and 2015 and the sample size ranged from 13 to 403. Among them, 3, 1, and 1 study was performed in UK, USA, and Czech Republic, respectively. The inclusion and exclusion criteria of each included study were summarized in the Table S1, Supplemental Digital Content, http://links.lww.com/MD/G517. The outcomes reported by each included study were summarized in the Table S2, Supplemental Digital Content, http://links.lww.com/MD/G518.
Figure 1.
Flow chart of study selection.
Table 1.
Characteristics of included studies.
| First author (year) | Country | Journal | Study design | Sample size | CT machines | Source of patients | Period of enrollment | Characteristics of injured casualties | Reference standard for injury |
| Charvát (2001) | Czech Republic | Ceska Radiologie | Diagnostic accuracy test | 23 | NA. | The Central Military Hospital in Prague, Czech Republic. | July 1996–June 1998 | Blunt liver and spleen injuries. | Laparotomy |
| Beekley (2008) | USA | The Journal of Trauma | Diagnostic accuracy test | 145 | 8-slice Siemens Somatom, plus 4 (Stuttgardt, Germany). | The 31st combat support hospital, in Baghdad, Iraq. | July 2004–January 2005 | Penetrating injury caused by combat fragmentation wounds. | Laparotomy |
| Smith (2010) | UK | Annals of the Royal College of Surgeons of England | Diagnostic accuracy test | 13 | Not reported in details. | A deployed military field hospital in HERRICK 9, Afghanistan. | October 2008–November 2008 | Injury caused by high velocity gunshot wound, blast, and stab. | Laparotomy |
| Morrison (2011) | UK | World Journal of Surgery | Diagnostic accuracy test | 60 | Not reported in details. | The British Military Hospital in Helmand Province, Afghanistan. | October 2007–September 2008 | Penetrating abdominal injury caused by gunshot and fragmentation in the conflict environment. | Laparotomy |
| Smith (2015) | UK | Annals of Surgery | Diagnostic accuracy test | 403 | Not reported in details. | Joint Force Medical Group Role 3 Medical Treatment Facility in Camp Bastion, Helmand Province, Afghanistan. | July 2012–November 2012 | All abdominal injury in the military setting. | Laparotomy |
CT = computed tomography, NA = not available.
3.2. Study quality
The quality of included studies was summarized in the Table S3, Supplemental Digital Content, http://links.lww.com/MD/G519. In the domain of patient selection, 4 studies[16–19] had low risk of bias and high applicability concerns; in the domain of index test, 4 studies[16–19] had low risk of bias and high applicability concerns; in the domain of reference standard, all of 5 studies[15–19] had low risk of bias and high applicability concerns; and in the domain of flow and timing, 3 studies[16,17,19] had low risk of bias.
3.3. Systematic review
In 2001, Charvát et al[15] performed a retrospective study to explore the diagnostic accuracy of CT in 23 patients suspected with abdominal injury in a military hospital. Nineteen patients (82.61%, 19/23) had positive CT findings, but 2 of them (10.51%, 2/19) underwent non-therapeutic laparotomy and were finally confirmed false positive. Four patients (17.39%, 4/23) had negative CT findings, but 2 of them (50.00%, 2/4) were finally diagnosed with liver injury by laparotomy and were confirmed false negative.
In 2008, Beekley et al[16] performed a retrospective study to explore the diagnostic performance of physical examination, FAST, and CT in hemodynamically stable patients with penetrating wounds to the back, flank, lower chest, abdomen, and pelvis in a combat support hospital. In this study, 145 patients were included, of whom 139 had physical examination findings, 114 had FAST findings, and all had CT findings. Sixty patients (41.38%, 60/145) had positive CT findings, but 15 of them (25.00%, 15/60) performed non-therapeutic laparotomy and were finally confirmed false positive. Eighty-five patients (58.62%, 85/145) had negative CT findings, but 1 of them (1.18%, 1/85) was finally diagnosed with biliary-pleural-bronchial-cutaneous fistula by laparotomy and was confirmed false negative. Overall, there were 77 injuries in 45 patients who underwent therapeutic laparotomy. Among them, 55 (71.43%, 55/77), 70 (90.91%, 70/77), and 4 (5.19%, 4/77) injuries were missed by physical examination, FAST, and CT, respectively.
In 2010, Smith et al[17] performed a retrospective study to explore the diagnostic performance of CT for abdominal injury during a 7-week period of Operation HERRICK 9. Thirteen patients underwent CT to evaluate abdominal injury. Among them, 12 patients (92.31%, 12/13) had negative CT findings and avoided laparotomy, and the remaining patient (7.69%, 1/13) was suspected with a diagnosis of thoraco-abdominal injury on CT and was confirmed by laparotomy.
In 2011, Morrison et al[18] performed a retrospective study to explore the diagnostic accuracy of CT in the management of penetrating abdominal injury in the conflict environment. In this study, 143 patients were included, of whom 73 underwent immediate laparotomy and 60 underwent CT to further evaluate the necessity of laparotomy. Seventeen (28.33%, 17/60) patients had positive CT findings, but 5 of them (29.41%, 5/17) performed non-therapeutic laparotomy and were finally confirmed false positive. Forty-three (71.67%, 43/60) patients had negative CT findings, but 1 of them (2.33%, 1/43) was finally diagnosed with gunshot wound in the right upper abdomen and was confirmed false negative.
In 2015, Smith et al[19] performed a retrospective study to explore the role of CT in the assessment of battlefield abdominal injury. In this study, 403 patients underwent abdominal CT. Sixty-eight patients (16.87%, 68/403) had positive CT findings, but 3 of them (4.41%, 3/68) performed non-therapeutic laparotomy and were finally confirmed false positive. Three hundred and thirty-five patients (83.13%, 335/403) had negative CT findings, but only 1 of them (0.30%, 1/335) was finally diagnosed with rectal injury by laparotomy and was confirmed false negative.
3.4. Meta-analyses
The diagnostic threshold effect was not statistically significant (Spearman correlation coefficient = –0.300, P = .624) among the 5 included studies.[15–19] The AUSROC was 0.9761 ± 0.0215 and the Q index was 0.9302 ± 0.0378 (Fig. 2). The pooled sensitivity was 0.97 (95% CI: 0.92–0.99) and the heterogeneity was not significant among studies (I2 = 0%, P = .4538) (Fig. 3). The pooled specificity was 0.95 (95% CI: 0.93–0.97) and the heterogeneity was significant among studies (I2 = 90.6%, P < .0001) (Fig. 3). The pooled positive likelihood ratio was 10.71 (95% CI: 2.91–39.43) and the heterogeneity was significant among studies (I2 = 89.2%, P < .0001) (Fig. 4). The pooled negative likelihood ratio was 0.07 (95% CI: 0.02–0.27) and the heterogeneity was significant among studies (I2 = 57.5%, P = .0516) (Fig. 4). The pooled DOR was 177.48 (95% CI: 18.09–1741.31) and the heterogeneity was significant among studies (I2 = 75.9%, P = .0023) (Fig. 5).
Figure 2.
AUSROC of CT for the diagnostic performance of abdominal injury in military setting. AUSROC = area under the summary receiver operating characteristic curve, CT = computed tomography.
Figure 3.
Sensitivity and specificity of CT for the diagnostic performance of abdominal injury in military setting. CT = computed tomography.
Figure 4.
Positive and negative likelihood ratios of CT for the diagnostic performance of abdominal injury in military setting. CT = computed tomography.
Figure 5.
DOR of CT for the diagnostic performance of abdominal injury in military setting. CT = computed tomography, DOR = diagnostic odds ratio.
4. Discussion
To our knowledge, this study should be the first meta-analysis to explore the role of CT in diagnosing abdominal injury in the military setting. CT had an excellent diagnostic accuracy (AUSROC was 0.9761, sensitivity was 0.97, and specificity was 0.95) among patients with abdominal injury in the military setting. It should be acknowledged that a meta-analysis by Baron et al[20] in 2018 had been performed to explore the diagnostic accuracy of CT for abdominal injury in patients with abdominal stab wounds. Notably, the major population of the Baron study was significantly different from that of our study. In details, the Baron study focused on the civilians admitted to the non-war hospitals; by contrast, our study mainly included the soldiers or injured patients in military setting. Severity, nature, and management of abdominal injury are often different between civilian and military settings. The civilians may have less severe injuries and can receive more timely and comprehensive assessment and treatment of abdominal injuries. By comparison, the soldiers in military setting may have more severe and complex injuries and poor access to diagnostic approaches.
Except for laparotomy, patients with abdominal injury often undergo selective nonoperative management (SNOM), which was firstly proposed by Dr. Shaftan in 1960[21] and has been gradually accepted for management of abdominal injury in civilians since then.[22] In 2014, a large scale study performed in USA, including 1273 soldiers with military injury, showed that only 95 patients underwent SNOM and the incidence of nontherapeutic laparotomy was 32% during the past decade.[23] Nontherapeutic laparotomy not only led to a great waste of medical resources during the war, but also significantly increased the risk of surgical complications. Notably, the operating room in military setting should be limited to the patients who urgently need a therapeutic laparotomy. Accurate and rapid assessment of such candidates is still challenging. Physical examination, FAST, and CT are the mainstay diagnostic approaches to identify the patients who should undergo laparotomy. Physical examination has been widely used to make a judgement to undergo laparotomy, but often unreliabile.[16,24] FAST is characterized as light weight, small size, portability, easy operation, and non-radiation.[25] The role of FAST in the diagnosis of abdominal injury in the military setting is important.[9,26] In some cases, FAST may be sufficient to decide SNOM.[27] However, the 2010 guideline regarding SNOM for penetrating abdominal injury recommended that CT should be considered as an important supplementary diagnostic tool to facilitate initial management decisions in SNOM, but FAST should not be considered for the decision of selecting patients for initial nonoperative management.[28]
Principles and indications of FAST and CT for diagnosis of injury are potentially different. FAST is effective for the diagnosis of injury developing in the abdominal solid organs, such as liver, kidney, and pancreas, but less accurate for hollow organs, such as stomach, small intestine, and large intestine. Stassen et al[29] revealed that FAST had a poor sensitivity of diagnosis of intestinal injury. Therefore, if a patient with penetrating abdominal injury had a positive FAST finding, he or she would undergo laparotomy immediately; otherwise, an additional diagnostic tool would be considered to rule out occult injury.[16,30] By comparison, CT has an excellent diagnostic accuracy of abdominal injury.[16,19] However, it has a large volume, and cannot be flexibly transferred and conventionally applied in the front line. Considering that abdominal injury sustained in military setting is often attributed to higher energy transfer, leading to more extensive wounds, greater risk of bacterial contamination, and prolonged pre-hospital time,[31] CT seems to be inappropriate for rapid screening for these soldiers who need laparotomy. Regardless, it should be reasonable that patients with unstable hemodynamics should undergo laparotomy immediately; patients with stable hemodynamics should undergo physical examination and FAST as preliminary screening tools for abdominal injuries; patients with blast injury, multiple injuries, and suspected gastrointestinal tract injuries should undergo CT scans to reduce a missed diagnosis.[32]
The current meta-analysis had several limitations. First, there was a small number of included studies. But it is often difficult to conduct the studies regarding injury in the military setting. Second, all injured causalities in the military setting were included. Except for the soldiers, the civilians developing injury in war times should also be actively managed. Third, the type of abdominal injury was not specified. In the Charvát study,[15] the major type of injury was blunt liver and spleen injuries; in the Beekley study,[16] the major type of injury was penetrating injuries caused by combat fragmentation; in the Smith study,[17] the major type of injury was injuries caused by high velocity gunshot wound, blast, and stab; in the Morrison study,[18] the major type of injury was penetrating injuries caused by gunshot and fragmentation; and in the Smith study,[19] the type of injury included all abdominal injuries. Fourth, the major data could be extracted from the abstract of the Charvát study, but not its full text.[15]
In conclusion, CT has an excellent diagnostic performance of abdominal injury in military setting, but may be limited due to its large volume. In the future, how to shrink the CT equipment for its wide use during the war needs to be resolved.
Author contributions
Conceptualization: Xingshun Qi.
Data curation: Zhaohui Bai, Bing Wang, Hui Lu, Xingshun Qi.
Formal analysis: Zhaohui Bai, Jing Tian, Zhenhua Tong, Xingshun Qi.
Methodology: Zhaohui Bai, Bing Wang, Jing Tian, Zhenhua Tong, Hui Lu, Xingshun Qi.
Supervision: Hui Lu, Xingshun Qi.
Writing – original draft: Zhaohui Bai.
Writing – review & editing: Hui Lu, Xingshun Qi.
Footnotes
Abbreviations: AUSROC = area under the summary receiver operating characteristic curve, CI = confidence interval, CT = computed tomography, DOR = diagnostic odds ratio, FAST = focused assessment with sonography in trauma, QUADAS-2 = quality assessment of diagnostic accuracy studies-2, SE = standard error, SNOM = selective nonoperative management.
How to cite this article: Bai Z, Wang B, Tian J, Tong Z, Lu H, Qi X. Diagnostic utility of CT for abdominal injury in the military setting: a systematic review and meta-analysis. Medicine. 2021;100:50(e28150).
ZB, BW, JT, and ZT contributed equally to this work.
All authors have made an intellectual contribution to the manuscript and approved the submission.
Data Availability: The data that supports the findings of this study are available in the supplementary material of this article.
The authors have no funding and conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
References
- [1].Moore EE, Moore JB, Van Duzer-Moore S, Thompson JS. Mandatory laparotomy for gunshot wounds penetrating the abdomen. Am J Surg 1980;140:847–51. [DOI] [PubMed] [Google Scholar]
- [2].Demetriades D. Civilian and military trauma: training to successfully intervene and save lives. J Am Coll Surg 2018;227:555–63. [DOI] [PubMed] [Google Scholar]
- [3].Sirinek KR, Page CP, Root HD, Levine BA. Is exploratory celiotomy necessary for all patients with truncal stab wounds? Arch Surg 1990;125:844–8. [DOI] [PubMed] [Google Scholar]
- [4].Leppäniemi A, Salo J, Haapiainen R. Complications of negative laparotomy for truncal stab wounds. J Trauma 1995;38:54–8. [DOI] [PubMed] [Google Scholar]
- [5].Miller FB, Cryer HM, Chilikuri S, Creech P, Richardson JD. Negative findings on laparotomy for trauma. South Med J 1989;82:1231–4. [DOI] [PubMed] [Google Scholar]
- [6].Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma 1995;38:350–6. [DOI] [PubMed] [Google Scholar]
- [7].Renz BM, Feliciano DV. The length of hospital stay after an unnecessary laparotomy for trauma: a prospective study. J Trauma 1996;40:187–90. [DOI] [PubMed] [Google Scholar]
- [8].Salim A, Velmahos GC. When to operate on abdominal gunshot wounds. Scand J Surg 2002;91:62–6. [DOI] [PubMed] [Google Scholar]
- [9].Qi X, Tian J, Sun R, et al. Focused assessment with sonography in trauma for assessment of injury in military settings: a meta-analysis. Balkan Med J 2019;37:03–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Gay DA, Miles RM. Use of imaging in trauma decision-making. J R Army Med Corps 2011;157: (3 suppl 1): S289–92. [DOI] [PubMed] [Google Scholar]
- [11].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. [DOI] [PubMed] [Google Scholar]
- [13].Sedgwick P. Spearman's rank correlation coefficient. BMJ 2014;349:g7327. [DOI] [PubMed] [Google Scholar]
- [14].Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A. Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 2006;6:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Charvát F, Chmátal P, Lacman J. Blunt liver and spleen injuries on the CT image. Ceska Radiologie 2001;55:26–31. [Google Scholar]
- [16].Beekley AC, Blackbourne LH, Sebesta JA, McMullin N, Mullenix PS, Holcomb JB. Selective nonoperative management of penetrating torso injury from combat fragmentation wounds. J Trauma 2008;64: (2 suppl): S108–17. [DOI] [PubMed] [Google Scholar]
- [17].Smith JE, Midwinter M, Lambert AW. Avoiding cavity surgery in penetrating torso trauma: the role of the computed tomography scan. Ann R Coll Surg Engl 2010;92:486–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Morrison JJ, Clasper JC, Gibb I, Midwinter M. Management of penetrating abdominal trauma in the conflict environment: the role of computed tomography scanning. World J Surg 2011;35:27–33. [DOI] [PubMed] [Google Scholar]
- [19].Smith IM, Naumann DN, Marsden ME, Ballard M, Bowley DM. Scanning and war: utility of FAST and CT in the assessment of battlefield abdominal trauma. Ann Surg 2015;262:389–96. [DOI] [PubMed] [Google Scholar]
- [20].Baron BJ, Benabbas R, Kohler C, et al. Accuracy of computed tomography in diagnosis of intra-abdominal injuries in stable patients with anterior abdominal stab wounds: a systematic review and meta-analysis. Acad Emerg Med 2018;25:744–57. [DOI] [PubMed] [Google Scholar]
- [21].Shaftan GW. Indications for operation in abdominal trauma. Am J Surg 1960;99:657–64. [DOI] [PubMed] [Google Scholar]
- [22].Singh N, Hardcastle TC. Selective non operative management of gunshot wounds to the abdomen: a collective review. Int Emerg Nurs 2015;23:22–31. [DOI] [PubMed] [Google Scholar]
- [23].Mitchell TA, Hutchison T, Becker TE, Aden JK, Blackbourne L, White CE. Nontherapeutic laparotomy in American combat casualties: a 10-year review. J Trauma Acute Care Surg 2014;77: (3 suppl 2): S171–5. [DOI] [PubMed] [Google Scholar]
- [24].Demetriades D, Velmahos G. Technology-driven triage of abdominal trauma: the emerging era of nonoperative management. Annu Rev Med 2003;54:01–15. [DOI] [PubMed] [Google Scholar]
- [25].Williams SR, Perera P, Gharahbaghian L. The FAST and E-FAST in 2013: trauma ultrasonography: overview, practical techniques, controversies, and new frontiers. Crit Care Clin 2014;30:119–50. [DOI] [PubMed] [Google Scholar]
- [26].Stengel D, Leisterer J, Ferrada P, Ekkernkamp A, Mutze S, Hoenning A. Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev 2018;12:CD012669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kumar S, Prakash P, Joshi MK, Rathi V. Selective non-operative management of patients with abdominal trauma-is CECT scan mandatory? Indian J Surg 2017;79:396–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Como JJ, Bokhari F, Chiu WC, et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma 2010;68:721–33. [DOI] [PubMed] [Google Scholar]
- [29].Stassen NA, Lukan JK, Carrillo EH, Spain DA, Richardson JD. Abdominal seat belt marks in the era of focused abdominal sonography for trauma. Arch Surg 2002;137:718–23. [DOI] [PubMed] [Google Scholar]
- [30].Udobi KF, Rodriguez A, Chiu WC, Scalea TM. Role of ultrasonography in penetrating abdominal trauma: a prospective clinical study. J Trauma 2001;50:475–9. [DOI] [PubMed] [Google Scholar]
- [31].Champion HR, Bellamy RF, Roberts CP, Leppaniemi A. A profile of combat injury. J Trauma 2003;54: (5 suppl): S13–9. [DOI] [PubMed] [Google Scholar]
- [32].Qi X, Tang C, Tian J, Sun R, Lu H. Current status regarding selective non-operative management of abdominal gunshot wounds. Med J Chin PLA 2020;45:893–6. [Google Scholar]