Colorectal cancer (CRC) incidence and mortality rates have decreased in the United States over the last several decades;1-3 however, CRC incidence rates are increasing in younger adults (age <50 years).2-5 Colonoscopy use in younger adults has also increased,6-7 prompting questions of whether the observed increase in early-onset CRC is an artifact of increased colonoscopy use.
Although prior studies report increasing incidence rates that parallel increases in colonoscopy use in younger adults,6-7 none have investigated these trends in the same population and among individuals with full access to primary and specialty care (e.g., gastroenterology), thus eliminating access to care as a contributing factor. To address this gap in knowledge, we examined CRC incidence, colonoscopy use, colonoscopy indication, and stage at diagnosis among individuals 18-49 and 50-54 years of age from a large, integrated health system.
We conducted a retrospective cohort study of Kaiser Permanente Northern California health plan members age 18-49 or 50-54 years in 1998-2018, who were followed from cohort entry to the earliest of 1) the day before their 50th and 55th birthdays, respectively; 2) CRC diagnosis; 3) membership disenrollment; 4) death; or 5) end of the study period (December 31, 2018). The younger cohort was further divided into four age groups (i.e., 18-29, 30-39, 40-44, 45-49 years). For each age group and year in the study period, we estimated CRC incidence, colonoscopy use, colonoscopy indication, and stage at diagnosis (see Supplementary Methods).
During the 21-year study period, we followed 5,982,616 individuals age 18-49, of whom 151,363 received a colonoscopy and 2,280 received a new CRC diagnosis, and 1,625,690 individuals age 50-54, of whom 181,322 received a colonoscopy and 2,259 received a new CRC diagnosis. See Supplemental Table 1 for cohort characteristics. Of the colonoscopies performed in younger adults, 64.9% were diagnostic, 25.9% were screening, 1.7% were follow-up to a positive fecal test, and 3.4% were surveillance; of colonoscopies performed in older adults, 40.6% were diagnostic, 33.3% were screening, 16.4% were follow-up to a positive fecal test, and 1.9% were surveillance.
Colonoscopy use and CRC incidence rates increased in both age groups over time; however, the drivers of these increases differed between groups. Colonoscopy use increased 6.6% annually in younger adults, from 2.8 per 1,000 person-years (PY) in 1998 to 10.1 per 1,000 PY in 2018 (P<0.001), and increased 7.4% annually in older adults, from 16.7 per 1,000 PY in 1998 to 70.0 per 1,000 PY in 2018 (P<0.001) (Figure 1A). CRC incidence rates increased 1.4% annually in younger adults, from 6.0 per 100,000 PY in 1998 to 8.0 per 100,000 PY in 2018 (P<0.001) and 2.2% annually in the older group, from 42.2 per 100,000 PY in 1998 to 65.1 per 100,000 PY in 2018 (P<0.001); increases in colonoscopy use were associated with the increase in CRC incidence in both groups (Figure 1B). However, the rise in colonoscopy use was driven primarily by an increase in procedures with a diagnostic indication in younger adults but increases in both diagnostic and screening indications in older adults (Figure 1C). Moreover, the rise in CRC incidence was driven by increases in advanced-stage disease in younger adults but increases in early-stage disease in older adults (Figure 1D).
Figure 1. Colorectal cancer incidence, colonoscopy use, and colorectal cancer stage at diagnosis in patients age 18-49 and 50-54 years, 1998-2018.
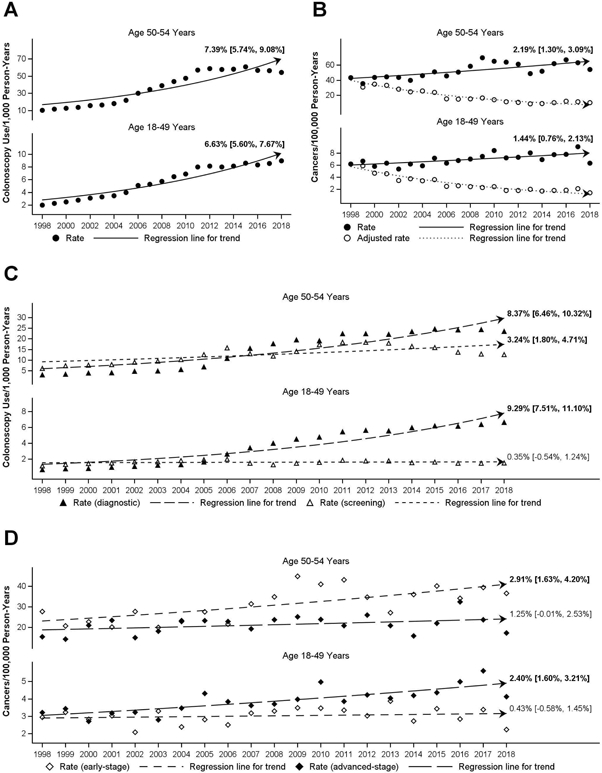
(A) Trends in colonoscopy use per 1,000 person-years. (B) Trends in age-standardized (2000 United States census population) colorectal cancer incidence per 100,000 person-years, crude and adjusted for colonoscopy use. (C) Trends in diagnostic and screening colonoscopy use per 1,000 person-years. (D) Trends in age-standardized (2000 United States census population) early- and advanced-stage colorectal cancer incidence per 100,000 person-years. Regression lines represent annual average percent change.
Approximately 52.2% of early-onset CRC diagnoses occurred in patients age 45-49 (Supplemental Table 1). This subgroup also had the largest increases in CRC incidence, colonoscopy use, and advanced-stage disease, as well as a slight increase in screening colonoscopy use, though this increase was not accompanied by an increase in early-stage disease.
In a large, integrated healthcare system, in which members have full access to primary and specialty care, we observed increases in both CRC incidence and colonoscopy use in younger and older adults, but the two age groups differed dramatically in stage of disease at diagnosis and colonoscopy indication. In younger adults, increases in advanced-stage disease drove the increase in CRC incidence and about 65% of examinations were for diagnostic purposes, indicating the cancers were primarily diagnosed by colonoscopies performed to investigate clinical symptoms rather than primarily by a lowering of the threshold for screening. Among older adults, the increase in CRC incidence was driven by an increase in early-stage disease, a finding which is consistent with the observed increase in screening colonoscopy in this age group, leading to earlier disease detection. Thus, while increasing CRC incidence rates paralleled increases in colonoscopy use – the procedure by which CRC is typically diagnosed – the stark differences in colonoscopy indication and stage of disease at diagnosis support the conclusion that the rise in early-onset CRC is not solely an artifact of increasing colonoscopy use, but likely reflects a true increase in disease burden.
Our findings support prior studies indicating early-onset CRC is on the rise and typically diagnosed at an advanced stage.2-5 Our findings are also consistent with prior studies indicating colonoscopy use is increasing in patients age 18-49,6-7 though this is the first to our knowledge to examine trends in early-onset CRC incidence and colonoscopy use within the same population.
The largest increases in disease burden, including cancers diagnosed at an advanced stage, were observed in those age 45-49 years. Given that advanced-stage CRC has a lower survival probability than early-stage disease,5 lowering the age for CRC screening initiation to 45 years, as recommended by recent guidelines,8 has the potential to substantially reduce early-onset CRC morbidity and mortality through removal of precancerous adenomatous polyps and earlier disease detection.
In conclusion, our findings demonstrate that early-onset CRC is marked by advanced-stage disease, and rates are increasing, even in a medically insured population with access to primary and specialty care. This increase likely reflects a true increase in disease burden rather than an artifact of increasing use of screening colonoscopy. Given that most early-onset CRCs were diagnosed in individuals age 45-49 years, recent recommendations to initiate CRC screening at age 45 rather than 50 has the potential to substantially reduce the burden of early-onset CRC.
Supplementary Material
Grant support:
Jeffrey K. Lee: research support from NCI, K07 CA212057
Caitlin C. Murphy: research support from NCI R01 CA242558
Douglas A. Corley: research support from NCI UM1 CA222035; NCI R01 CA213645
Abbreviations:
- (CRC)
colorectal cancer
- (PY)
person-years
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have no conflicts of interest to disclose
REFERENCES
- 1.Murphy CC, Sandler RS, Sanoff HK, Yang YC, Lund JL, Baron JA. Decrease in incidence of colorectal cancer among individuals 50 years or older after recommendations for population-based screening. Clin Gastroenterol Hepatol. 2017;15:903–9 [e6]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Austin H, Henley SJ, King J, Richardson LC, Eheman C. Changes in colorectal cancer incidence rates in young and older adults in the United States: what does it tell us about screening. Cancer Causes Control. 2014. February;25(2):191–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst. 2017;109(8):djw322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey CE, Hu CY, You YN, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975–2010. JAMA Surg. 2015;150(1):17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang W, Wenbin C, Lin J, Shen Q, Zhou X, Lin C. Incidence and characteristics of young-onset colorectal cancer in the United States: An analysis of SEER data collected from 1988 to 2013. Clin Res Hepatol Gastroenterol. 2019;43:208–215. [DOI] [PubMed] [Google Scholar]
- 6.Fedewa SA, Siegel RL, Jemal A. Are temporal trends in colonoscopy among young adults concordant with colorectal cancer incidence? J Med Screen. 2019; 26(4):179–185. [DOI] [PubMed] [Google Scholar]
- 7.Murphy CC, Lund JL, Sandler RS. Young-onset colorectal cancer: earlier diagnoses or increased disease burden? Gastroenterology. 2017; 152(8):1809–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Preventative Services Task Force. Draft Recommendation Statement. Colorectal Cancer: Screening, https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/colorectal-cancer-screening3#fullrecommendationstart
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


