Abstract
Objectives:
Social and contextual factors underlying the continually disproportionate and burdensome risk of adverse health outcomes experienced by Black women in the US are underexplored in the literature. The aim of this study was to use an index based on area-level population distributions of race and income to predict risk of death during pregnancy and up to one year postpartum among women in Louisiana.
Methods:
Using vital records data provided by the Louisiana Department of Health 2016–2017 (n=125,537), a modified Poisson model was fit with generalized estimating equations to examine the risk of pregnancy-associated death associated with census tract-level values of the Index of Concentration at the Extremes (ICE) – grouped by tertile – while adjusting for both individual and tract-level confounders.
Results:
Analyses resulted in an estimated 1.73 (95% CI:=1.02 – 2.93) times increased risk for pregnancy-associated death for those in areas which were characterized by concentrated deprivation (high proportions of Black and low-income residents) relative to those in areas of concentrated privilege (high proportions of white and high-income residents), independent of other factors.
Conclusions for Practice:
In addition to continuing to consider the deeply entrenched racism and economic inequality that shape the experience of pregnancy-associated death, we must also consider their synergistic effect on access to resources, maternal population health, and health inequities.
Keywords: Maternal Health, Maternal Mortality, Index of Concentration at the Extremes (ICE), Structural Racism
Introduction
Maternal mortality remains a public health crisis in the US where occurrence is far more frequent than in other developed countries. Perhaps of even greater concern, incidence appears to be increasing here while decreasing in other nations (Burgess et al., 2020). Moreover, the experience of loss within the US is deeply disproportionate, with Black women vastly overrepresented among cases of death during pregnancy, childbirth, and postpartum (Creanga et al., 2017).
The scarcity of evidence identifying social contexts underlying women’s risk of death during pregnancy and postpartum is surprising (Wang et al., 2020), given the failure of biomedical interventions and clinical improvements to maternal health care to substantially reduce maternal mortality since the 1950s (Creanga et al., 2014). Explorations of social contexts as drivers of maternal health inequities is perplexingly limited in the literature as well, given scientific repudiation of race as a biological “risk factor” and broader acceptance instead of racism as a fundamental cause of race-based differences in morbidity and mortality (Hoffman et al., 2016; Morning, 2012; Shih et al., 2007; Williams & Collins, 2001). Racial identification alone – a seemingly immutable characteristic – tells us nothing of an individual’s health risks and, importantly, how to mitigate them (Jee-Lyn Garcia & Sharif, 2015; Jones, 2001; Sen & Wasow, 2016). Instead, research is needed to understand the profound health implications of one’s race within a racially-stratified society where access to power and resources is inherently and historically unequal (Jones, 2001).
Dual pathways of neo-materialism and psychosocial environmental stress have been proposed explanations for health inequities within highly unequal societies (Huynh et al., 2005). The neo-materialist theory of income inequality’s effect on health posits that underinvestment in community resources and social infrastructure in unequal communities limits access to educational and employment opportunities, material goods and health care (Smith, 1996). The result is a health disadvantage among poorer segments of the population who lack resources to prevent and treat disease (Link & Phelan, 1995). Structural racism furthers this by positing that historical and contemporary racial oppression experienced by Black Americans (Bailey et al., 2017; Krieger, 2012) constitutes the de jure and de facto disinvestment in Black communities and their exclusion from health-promoting factors (i.e. wealth, income, safe housing, quality education and health care). Racial inequities in health thus become entrenched in society. The psychosocial stress pathway posits that inequities may also result from psychosocial stress, not only induced by living in disinvested communities (Gee & Payne-Sturges, 2004) and comparing oneself to others,(Wilkinson, 1997) but also by the consequences of such conditions such as reduced social cohesion (Kawachi & Kennedy, 1997). Psychosocial stress of community conditions or experiences of racial discrimination may also increase sympathetic nervous system activation and upregulate the HPA axis, increasing physiological wear and tear and elevating the risks of poor health (Geronimus, 1992).
There is a great need for examination of exposures that capture the intersections of pathways through which inequities may be produced within an equal society. The Index of Concentration at the Extremes (ICE) may be one such measure. Advanced by Krieger, et al. (2016b) for public health monitoring of harmful social contexts, the ICE contributes the geographic dimension of both structural racism and income inequality. It can be used to quantify the uneven distribution of privilege (White race and high income) and deprivation (Black race and low income) within a geographic area. The ICE offers a complimentary metric to poverty level – which focuses solely on the disadvantaged – as it simultaneously identifies those unfairly advantaged, thereby revealing the extent of social inequality and the problematic relationships that produce population health inequities (Krieger, Waterman, et al., 2016). Previous studies have associated the ICE with premature mortality, hypertension, cancer, fatal and non-fatal assault, environmental toxins, preterm birth, and infant mortality (Chambers et al., 2019; Krieger, et al., 2015, 2016a, 2016b; Shrimali et al., 2020; Wallace et al., 2019).
This study is based in Louisiana, a state with one of the highest incidences of maternal mortality in the nation and persistent racial socioeconomic and health inequities (Kieltyka et al., 2018). We used the ICE to characterize all Louisiana neighborhoods (census tracts) along a continuum from areas of concentrated deprivation to areas of concentrated privilege. We sought to identify whether the ICE value of maternal residential neighborhood was associated with risk of death during pregnancy and up to 1 year postpartum (pregnancy-associated mortality) and the extent to which the ICE may be exacerbating racial inequities in pregnancy-associated mortality.
Methods
Study population
The Louisiana Department of Health provided data on all verified cases of pregnancy-associated death from 2016–2017 (n=112). These are deaths among pregnant and postpartum (up to 1 year since the end of pregnancy) women due to any cause. Cases were verified as pregnancy-associated if the woman’s death record was linkable to a live birth or fetal death record issued within 1 year of the date of death and/or via the death record pregnancy checkbox indicating pregnancy status of the decedent. Given the potential for misclassification in relying on the pregnancy checkbox alone (Rossen et al., 2020), these cases required additional review and verification by the Bureau of Family Health Regional Maternal and Child Health Coordinators. We created a retrospective analytic cohort of pregnant women in Louisiana from 2016–2017 by combining all live birth records issued to living women (n=125,537), live birth records with linked maternal death records (n=62) and maternal death records where no birth record was available because the decedent was pregnant at time of death (n=32) or linkage was not successful (n=18). Reasons for unsuccessful linkages may include data entry errors on the birth or death certificate variables used in the two-stage linkage procedure (maternal social security number, first and last name, and date of birth) or instances where the infant was put up for adoption.
For all records, address of residence was geocoded using ArcGIS software (ESRI Inc, Redlands, CA). We successfully identified geographic coordinates for all maternal deaths (n=112) and for over 80% of births (n=101,484). Those unable to be located included P.O. boxes (n=479) and records with missing or unknown errors in the house number, street name, or zip code variables (n=23,574). The final analytic sample with georeferenced data (maternal residential census tract Federal Information Processing System number) was 101,596. As all data were deidentified, this study was deemed exempt by the Tulane University Institutional Review Board.
Outcome
Our outcome of interest was pregnancy-associated mortality (death during pregnancy or up to one year from the end of pregnancy, regardless of cause of death), yes/no.
Exposure
We estimated the ICE for every census tract in Louisiana using 2012–2016 American Community Survey (ACS) 5-year estimates of household income by race/ethnicity as a proxy of structural racism. Following the formula described by Krieger et al. (2016b) we calculated the ICE in each census tract by taking the difference between of the number of Non-Hispanic (NH) white persons whose annual household income was greater than or equal to the 80th percentile (>$100,000) minus the number of NH Black persons whose household income was less than the 20th income percentile (<$25,000), divided by the total population with known income in the tract. Values of ICE range from −1 (indicating 100% of the population is concentrated in the most deprived group) to 1 (indicating 100% of the population is concentrated in the most privileged group). Each birth (and/or death) record was linked to its corresponding value of the ICE based on maternal census tract of residence. We categorized the ICE into tertiles in order to compare risk associated with residence in the lower (most deprived), middle, and upper (most privileged) tertiles.
Covariates
Inclusion of individual-level confounders was limited to those available on both birth and death records: maternal age (age at live birth or age at death, if decedent was still pregnant at time of death; ≤25, 25–29, 30–34, ≥35), and educational attainment (less than high school, high school graduate, some college or associate’s degree, bachelor’s degree or higher).
We controlled for tract-level availability of resources (% of families with incomes below the Federal Poverty Level) and an indicator for whether the tract was within an urban vs. rural parish (county equivalent) based on the 2010 US Census designation. We combined “mostly rural” and “completely rural” for a dichotomous urban/rural indicator.
Statistical analyses
We estimated bivariate associations between all covariates and the outcome using chi-square and t-tests as appropriate. We fit a fully-adjusted modified Poisson regression model with generalized estimating equations to accommodate clustering of women within census tracts in order to estimate the relative risk of death associated with residence in the lowest (most deprived) and middle tertiles of the ICE, relative to the top (most privileged) tertile. We fit this model both with and without maternal race/ethnicity as an additional co-variate in order to explore how treating individual race as a “risk factor” may obfuscate the identification of structural racism (the ICE) as a target for intervention.
We applied the framework proposed by Ward et al. (2019) in order to identify the degree to which the ICE may exacerbate racial inequity in mortality. This approach involves exploring racial differences in 1) the outcome 2) the exposure, and 3) magnitude of association between the two. We fit an interaction model to test for effect modification by maternal race/ethnicity and plotted racial differences in risk of death (unadjusted), and proportion of women in the lowest and middle vs. the highest tertiles of the ICE in order to visualize the extent to which the ICE may exacerbate racial inequity in mortality.
Finally, taking a life-course perspective, we sought to identify the degree to which the ICE may be detrimental to women’s health before pregnancy, thereby increasing their risk of an adverse pregnancy experience and ultimately maternal death. We applied a counterfactual approach to mediation analysis to estimate the RR for the natural direct effect (NDE) and natural indirect effect (NIE) of the ICE on mortality mediated through chronic conditions (pre-pregnancy diabetes and chronic hypertension). We fit a mediation model using PROC CAUSALMED in order to test our a priori hypothesis that women living in areas of concentrated deprivation are at increased risk for developing chronic conditions and that these, in turn, may contribute to heightened mortality risk during pregnancy and postpartum. All analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
The descriptive analysis showed that one third of pregnant women from 2016–2017 were age 25 and under, and most had at least a high school education and lived in an urban parish (Table 1). On average, women lived in census tracts where 15% of families were below the poverty line. We identified bivariate associations between maternal death and race/ethnicity, educational-attainment and the ICE (all p<0.05; Table 1). Forty-five percent of the 112 maternal deaths occurred in the bottom tertile of the ICE (neighborhoods of concentrated deprivation). Nearly 60% of maternal deaths were NH Black women, while NH Black women represented only 37% of the total population of pregnant women. The average tract prevalence of pre-pregnancy chronic disease (diabetes and chronic hypertension) was 4.3% among non-cases, and 4.9% among decedents.
Table 1.
Characteristics of pregnant women and their residential census tracts, Louisiana 2016–2017.
| Total | Living women | Maternal deaths | P value | |
|---|---|---|---|---|
|
| ||||
| N (%) | N (%) | N (%) | ||
| 101585 | 101473 (99.89) | 112 (0.11) | ||
| ICE tertiles | ||||
| Concentrated Deprivation | 33886 (33.36) | 33835 (33.34) | 51 (45.54) | .0171 |
| Middle | 33844 (33.32) | 33810 (33.32) | 34 (30.36) | |
| Concentrated Privilege | 33854 (33.33) | 33827 (33.34) | 27 (24.11) | |
| Age | ||||
| =<25 | 34481 (33.94) | 34438 (33.94) | 43 (38.39) | .3445 |
| 25–29 | 31213 (30.73) | 31187 (30.73) | 26 (23.21) | |
| 30–34 | 23918 (23.54) | 23891 (23.54) | 27 (24.11) | |
| 35+ | 11973 (11.79) | 11957 (11.78) | 16 (14.29) | |
| Education | ||||
| LT HS | 15806 (15.65) | 15776 (15.64) | 30 (26.79) | .0007 |
| HS Grad | 32333 (32.02) | 32294 (32.01) | 39 (34.82) | |
| Some College/Associates | 29099 (28.82) | 29068 (28.82) | 31 (27.68) | |
| Bach or higher | 23747 (23.52) | 23735 (23.53) | 12 (10.71) | |
| Race | ||||
| NH White | 51402 (50.60) | 51363 (50.62) | 39 (34.82) | <.0001 |
| NH Black | 37796 (37.21) | 37729 (37.18) | 67 (59.82) | |
| Hispanic, multiple, or other | 12387 (12.19) | 12381 (12.20) | 6 (5.36) | |
| Urbanicity | ||||
| Urban | 86061 (84.72) | 85962 (84.71) | 99 (88.39) | .2795 |
| Rural | 15524 (15.28) | 15511 (15.29) | 13 (11.61) | |
|
| ||||
| Residential census tract characteristics |
Mean (STD) | Mean (STD) | Mean (STD) | |
|
| ||||
| Percent of families below the federal poverty level |
14.95 (3.98) | 14.95 (3.98) | 14.68 (3.76) | .4760 |
| Percent of pregnant women with a chronic condition (pre-pregnancy diabetes or hypertension) |
4.31 (2.91) | 4.31 (2.91) | 4.87 (2.98) | .4006 |
Relative to women in census tracts of concentrated privilege, those in areas of concentrated deprivation were at 1.73 times the risk of maternal death after controlling for all individual and area-level covariates, excluding maternal race (aRR=1.73, 95% CI=1.02 – 2.93) (Table 2). The addition of maternal race to this model reduced the effect estimate and nullified the association between the ICE and mortality (aRR=1.17, 95% CI=0.62 – 2.19). [Table 2]
Table 2:
Adjusted relative risks (RR) and 95% confidence interval (CI) for the association between the ICE and of maternal death in Louisiana, 2016–2017.
| Model 1 | Model 2 | |||
|---|---|---|---|---|
|
| ||||
| RR | 95% CI | RR | 95% CI | |
| ICE Tertile | ||||
| Concentrated Deprivation (−1.00 – −.84) |
1.73 | 1.02 – 2.93 | 1.17 | 0.62 – 2.19 |
| Middle (−.08 – .13) |
1.22 | 0.71 – 2.07 | 1.10 | 0.63 – 1.92 |
| Concentrated Privilege (.14 – .64) |
Ref | |||
| Age | ||||
| =<25 | 1.22 | 0.76 – 1.98 | 1.17 | 0.72 – 1.89 |
| 25 – 29 | Ref | |||
| 30–34 | 1.58 | 0.91 – 2.76 | 1.64 | 0.95 – 2.86 |
| 35+ | 1.87 | 0.99 – 3.49 | 1.99 | 1.06 – 3.75 |
| Education | ||||
| LT HS | 3.76 | 1.84 – 7.68 | 3.90 | 1.81 – 8.43 |
| HS Grad | 2.48 | 1.23 – 5.01 | 2.37 | 1.14 – 4.95 |
| Some College/Associates | 2.18 | 1.09 – 4.35 | 2.04 | 0.99 – 4.16 |
| Bachelor’s or Higher | Ref | |||
| Urbanicity | ||||
| Urban | Ref | |||
| Rural | 0.74 | 0.42 – 1.30 | .76 | 0.43 – 1.37 |
| Family poverty | 0.96 | 0.92 – 1.01 | 0.96 | 0.91 – 1.01 |
| Race | ||||
| Black | - | - | 1.93 | 1.12 – 3.35 |
| Other | - | - | 0.46 | 0.18 – 1.17 |
| White | - | - | Ref | Ref |
Figure 1 depicts the proportion of women, by race, in the top and bottom tertiles of the ICE and the race-specific mortality ratios in the top and bottom tertile.
Figure 1.
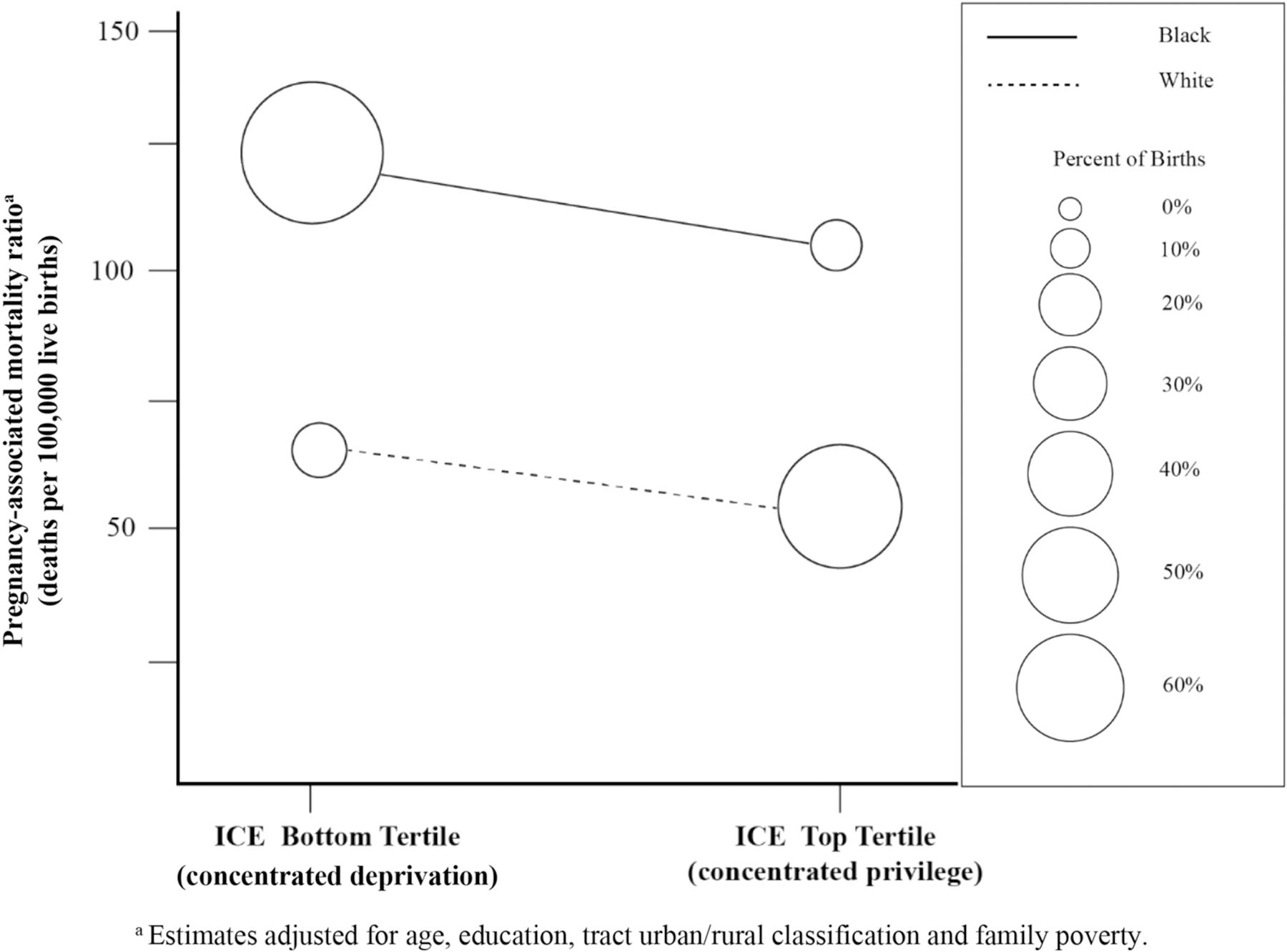
Percentage of births and adjusted pregnancy-associated mortality ratios in the top and bottom tertiles of the ICE, by maternal race
This figure allows for application of the Ward et al. (2019) framework in order to assess the contribution of the ICE as a modifiable exposure that exacerbates racial inequities in mortality. We identified racial differences in 1) the outcome (pregnancy-associated mortality), 2) the exposure (concentrated privilege or deprivation), but not 3) the magnitude of association between the two. Black women were at approximately two-fold greater risk of pregnancy-associated mortality and at both ends of the ICE spectrum compared to white women (adjusted pregnancy-associated mortality ratios among Black women were 123.3 and 105.6 deaths per 100,000 live births in the bottom and top tertiles, respectively, compared to 63.7 and 54.6 deaths per 100,000 live births among white women in the bottom and top tertiles). There were large racial differences in the exposure such that only 12% of white women resided in areas of concentrated deprivation while 63% of Black women resided in these areas (Figure 1). The addition of an ICE by race interaction term in the model was not significant, indicating no racial difference in the magnitude of association between the ICE and mortality (slopes depicted are not significantly different).
Using PROC CAUSALMED in an additional mediation analysis, we assessed the role of pre-pregnancy chronic disease diagnoses in the association between the ICE and maternal death (Table 3). [Table 3] The natural indirect effect (RRNIE) was 2.68 (95% CI = 2.59 – 2.84), indicating that mortality risk among women in areas of concentrated deprivation was elevated more than two-fold as a result of their chronic conditions (pre-pregnancy diabetes and/or hypertension). The natural direct effect (RRNDE) suggested that even if women in areas of concentrated privilege and concentrated deprivation had equal prevalence of chronic conditions, those in areas of concentrated deprivation would still have a 51% higher risk of death (RRNDE=1.51, 95% CI = 1.18 – 2.74).
Table 3.
Estimates of the natural direct, natural indirect and total effect of the association between the ICE and mortality mediated through chronic conditions (pre-pregnancy diabetes and/or chronic hypertension).a
| RR | Bootstrap Bias 95% CI | |
|---|---|---|
| Total Effect | 1.50 | 1.18 2.70 |
| Controlled Direct Effect (CDE) | 1.51 | 1.18 2.74 |
| Natural Direct Effect (NDE) | 1.51 | 1.18 2.74 |
| Natural Indirect Effect (NIE) | 2.68 | 2.59 2.85 |
Model controlled for urban/rural, age, education, poverty, and race.
Discussion
Our study suggests that the spatial social polarization measured by the ICE may contribute to pregnancy-associated mortality and its uneven occurrence across the population. In comparison to women living in neighborhoods of concentrated privilege, those in areas of concentrated deprivation had a significantly greater risk of death during pregnancy and postpartum. A non-significant test for interaction indicated that the magnitude of association between the ICE and mortality did not differ by maternal race, demonstrating the harmful nature of structural racism for all races. However, Black women were significantly more likely to live in the most deprived areas and were at increased risk for mortality compared to white women at every tertile of the ICE (including in areas of concentrated privilege). As a result, even in the absence of a significant race by ICE interaction, these findings implicate the role of structural racism in perpetuating racial inequities in mortality and therefore its salience as a target for interventions to advance health equity. A mediation analysis demonstrated a positive significant natural indirect effect of chronic disease diagnoses on the primary association, meaning that elevated exposures to structural racism may increase likelihood of certain long-term health conditions that may develop prior to pregnancy and increase risk for an adverse event.
Studies have previously found associations between the ICE and other health outcomes – including those pertaining to pregnancy and birth (Chambers et al., 2019; Kandasamyet al., 2020; Krieger et al., 2016b; Shrimali et al., 2020; Shumateet al., 2019; Wallace et al., 2019) – but this study is the first to explore an association between this measure and pregnancy-associated mortality. The geographic racial and economic segregation simultaneously captured by the ICE engenders both advantages and disadvantages by shaping local education, economies, and physical environments within communities, including spatial and economic access to health services (Krieger et al., 2016b). Historic exclusion and exploitation people of color and women in the United States through systemic racism and discrimination – such as redlining (Federal Reserve Bureau, 2017) – has been suggested to underlie modern disparities in chronic disease and birth outcomes (McClure et al., 2019; Mendez et al., 2013). Individual experiences with racism and discrimination have also been shown to have detrimental effects on health. In addition to the increased levels of stress with these experiences, studies have shown that implicit bias among physicians may impact how black women are evaluated and treated in a medical setting (Attanasio & Hardeman, 2019). In the context of maternal health outcomes, this can affect the delivery of screening for pregnancy complications.
We present the final model both with and without maternal race as covariate to demonstrate that, in this instance, treating race as a confounder of the association between the ICE and mortality presents both conceptual and practical problems. Conceptually, our primary independent variable of interest (the ICE) represents an indicator of structural racism. It is a result of structural racism – the hierarchical nature of society that restricts access to power and resources among Black populations – that race becomes a meaningful predictor of one’s health risks. Individual racial identity, as it relates to associations with mortality, therefore follows from structural racism and is not a common cause of either. Moreover, the inclusion of individual race in the model – treating race as a “risk factor” is commonly done to capture by proxy exposure to racial oppression – suppressed the identification of a modifiable target for intervention.
We acknowledge that the magnitude of association detected here is relatively small, and that large racial inequity remained even after accounting for the ICE. Quantitative researchers continue to grapple with ways to measure structural racism for the purposes of documenting its links to population health (Groos et al, 2018). Studies have yet to operationalize a standard measure of structural racism that captures the totality of its reach which extends beyond domains of income and residential segregation captured by the ICE. Indeed, multiple, interconnected systems (not limited to education, media, health care, criminal justice, credit, and benefits) (Bailey et al., 2017) reinforce societal norms and values that dictate how Black women live, reproduce, and are treated at all stages of their lives.
Nonetheless, the racial and economic segregation measured by the ICE can be addressed through policy and programmatic efforts that support investments in non-white communities and equitable redistribution of resources, such as access to fresh and affordable healthy food through food financing initiatives (Giang et al., 2008; Story et al., 2008) or zoning restrictions that may remove problem liquor stores from certain areas (Lee et al., 2020). Positive effects have been seen in interventions of this type. For example, increasing residential greening has been shown to improve birth outcomes (Hystad et al., 2014) and remediation of vacant land in urban areas may lead to reduced crime and violence (Hohl et al., 2019). Such interventions and policy, however, do not address the more fundamental and systemic reasons for disinvestment that we must continue to correct.
Our study has several limitations. Firstly, this is a cross-sectional analysis, and we are not able to account for changes in segregation patterns over time nor the length of time women had been residing in their address at the time of pregnancy. This may be particularly relevant for the mediation analysis, which tests the hypothesis that living in areas of concentrated deprivation may increase risk for chronic conditions which, in turn, elevate risk during pregnancy. While we have no data on mobility in this study, previous work has documented prolonged exposure to impoverished neighborhoods experienced across the life-course by people born into them (Li et al., 2019). Second, not all records were able to be geolocated, for reasons including P.O. Box listings for residential address, and these may be more common among rural women. Relatedly, there are additional factors that may confound the association between the ICE and mortality including geographic access to health care and means of transportation, which we are unable to account for. The small number of maternal deaths also may have limited our statistical power in detecting associations. Also, given the moderately unreliable quality of clinical data derived from birth records (DiGiuseppe et al., 2002), it is possible that the prevalence of chronic conditions in this sample is underreported. Finally, the unique sociopolitical landscape and history of Louisiana prevent us from making conclusions about populations in other state or countries, as well as allows the possibility of additional unmeasured bias.
Conclusion
In the United States, racism has been embedded in institutions, a phenomenon which may influence racial disparities in health outcomes. The ICE index allows us to simultaneously capture racial and income inequality and their association with pregnancy-associated mortality. In addition to interventions that address individual health behaviors, population- level interventions are needed to address these systemic issues and put behavior in context. A paradigmatic shift has been noted as health research becomes increasingly focused on upstream, macro-level change (Carey & Crammond, 2015). By continuing to shift away from behavioral and physical interventions and toward systemic restructuring efforts through policy, we can begin to deconstruct arbitrary and harmful social norms which have consistently detracted from the health and wellbeing of Black Americans.
Significance:
The ICE has previously been used as a proxy of structural racism in other public health studies to assess how population distributions along racial and economic lines can affect health, including maternal health outcomes. This study is unique in that it looks at pregnancy-associated mortality as an outcome while using the ICE to consider the complex social contexts in which these individuals live. Due to the availability of linked data, we are able to model individual-level risk of death associated with an area-based measure of social context despite the fact that death during or immediately after pregnancy is a relatively rare occurrence.
Funding
This work was supported by the National Institute of Child Health and Human Development grant numbers R01HD092653 and R01HD096070. The funding source had no involvement in the conduct of the research or preparation of the article. Its contents are solely the responsibility of the authors and do not necessarily represent the official position of the National Institutes of Health or the Louisiana Department of Health.
Footnotes
Conflicts of interest/Competing interests
Not applicable
Ethics approval
As all data were deidentified, this study was deemed exempt the Tulane University Institutional Review Board.
Consent to participate
Not applicable
Consent for publication
Not applicable
Availability of data and material
Not applicable
Code availability
Not applicable
References
- Attanasio LB, & Hardeman RR (2019). Declined care and discrimination during the childbirth hospitalization. Social Science & Medicine, 232, 270–277. 10.1016/j.socscimed.2019.05.008 [DOI] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, & Bassett MT (2017). Structural racism and health inequities in the USA: Evidence and interventions. Lancet, 389(10077), 1453–1463. 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Burgess APH, Dongarwar D, Spigel Z, Salihu HM, Moaddab A, Clark SL, & Fox K. (2020). Pregnancy-related mortality in the United States, 2003–2016: Age, race, and place of death. American Journal Obstetreics Gynecology, 222(5), 489 e481–489 e488. 10.1016/j.ajog.2020.02.020 [DOI] [PubMed] [Google Scholar]
- Board of Governors of the Federal Reserve System. (2017). Fair Lending Regulations and Statutes: Fair Housing Act Retrieved from https://www.federalreserve.gov/boarddocs/supmanual/cch/fair_lend_fhact.pdf
- Carey G, & Crammond B. (2015). Systems change for the social determinants of health. BMC Public Health, 15, 662. 10.1186/s12889-015-1979-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers BD, Baer RJ, McLemore MR, & Jelliffe-Pawlowski LL (2019). Using Index of Concentration at the Extremes as indicators of structural racism to evaluate the association with preterm Birth and infant mortality-California, 2011–2012. Journal of Urban Health, 96(2), 159–170. 10.1007/s11524-018-0272-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creanga AA, Berg CJ, Ko JY, Farr SL, Tong VT, Bruce FC, & Callaghan WM (2014). Maternal mortality and morbidity in the United States: where are we now? Journal Womens Health (Larchmt), 23(1), 3–9. 10.1089/jwh.2013.4617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creanga AA, Syverson C, Seed K, & Callaghan WM (2017). Pregnancy-Related Mortality in the United States, 2011–2013. Obstet Gynecol, 130(2), 366–373. 10.1097/AOG.0000000000002114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGiuseppe DL, Aron DC, Ranbom L, Harper DL, Rosenthal GE (2002). Reliability of birth certificate data: A multi-hospital comparison to medical records information. Maternal and Child Health Journal, 6. [DOI] [PubMed] [Google Scholar]
- Gee GC, & Payne-Sturges DC (2004). Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environmental Health Perspectives, 112(17), 1645–1653. 10.1289/ehp.7074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT (1992). The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethnicity & Disease, 2(3), 207–221. [PubMed] [Google Scholar]
- Giang T, Karpyn A, Laurison HB, Hillier A, & Perry RD (2008). Closing the grocery gap in underserved communities: the creation of the Pennsylvania Fresh Food Financing Initiative. Journal Public Health Management and Practice, 14(3), 272–279. 10.1097/01.PHH.0000316486.57512.bf [DOI] [PubMed] [Google Scholar]
- Groos M, Wallace ME, Hardeman RR, Theall KP (2018). Measuring inequity: a systematic review of methods used to quantify structural racism. Journal of Health Disparities Research and Practice, 11(2), 13. [Google Scholar]
- Hoffman KM, Trawalter S, Axt JR, & Oliver MN (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences USA, 113(16), 4296–4301. 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hohl BC, Kondo MC, Kajeepeta S, MacDonald JM, Theall KP, Zimmerman MA, & Branas CC (2019). Creating safe And healthy neighborhoods with place-based violence interventions. Health Affairs (Millwood), 38(10), 1687–1694. 10.1377/hlthaff.2019.00707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huynh M, Parker JD, Harper S, Pamuk E, & Schoendorf KC (2005). Contextual effect of income inequality on birth outcomes. International Journal Epidemiology, 34(4), 888–895. 10.1093/ije/dyi092 [DOI] [PubMed] [Google Scholar]
- Hystad P, Davies HW, Frank L, Van Loon J, Gehring U, Tamburic L, & Brauer M. (2014). Residential greenness and birth outcomes: evaluating the influence of spatially correlated built-environment factors. Environmental Health Perspectives, 122(10), 1095–1102. 10.1289/ehp.1308049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jee-Lyn Garcia J, & Sharif MZ (2015). Black lives matter: A commentary on racism and public health. American Journal of Public Health, 105(8), e27–30. 10.2105/AJPH.2015.302706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP (2001). Invited commentary: “Race,” racism, and the practice of epidemiology. American Journal of Epidemiology, 154(4), 299–304; (discussion 305–296). 10.1093/aje/154.4.299 [DOI] [PubMed] [Google Scholar]
- Kandasamy V, Hirai AH, Kaufman JS, James AR, & Kotelchuck M. (2020). Regional variation in Black infant mortality: The contribution of contextual factors. PLoS One, 15(8), e0237314. 10.1371/journal.pone.0237314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, & Kennedy BP (1997). Health and social cohesion: why care about income inequality? BMJ, 314(7086), 1037–1040. 10.1136/bmj.314.7086.1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieltyka L, Mehta P Schoellmann K, Lake C. (2018). Louisiana Maternal Mortality Review Report 2011–2016
- Krieger N. (2012). Methods for the scientific study of discrimination and health: an ecosocial approach. American Journal of Public Health, 102(5), 936–944. 10.2105/AJPH.2011.300544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Gryparis A, & Coull BA (2015). Black carbon exposure, socioeconomic and racial/ethnic spatial polarization, and the Index of Concentration at the Extremes (ICE). Health Place, 34, 215–228. 10.1016/j.healthplace.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Singh N, & Waterman PD (2016a). Metrics for monitoring cancer inequities: residential segregation, the Index of Concentration at the Extremes (ICE), and breast cancer estrogen receptor status (USA, 1992–2012). Cancer Causes Control, 27(9), 1139–1151. 10.1007/s10552-016-0793-7 [DOI] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, & Van Wye G. (2016b). Public health monitoring of privilege and deprivation with the index of concentration at the extremes. American Journal of Public Health, 106(2), 256–263. 10.2105/AJPH.2015.302955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JP, Ponicki W, Mair C, Gruenwald P, & Ghanem L. (2020). What explains the concentration of off-premise alcohol outlets in Black neighborhoods? SSM - Population Health, 12, 10069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M, Johnson SB, Newman S, Wiley AW (2019). Residential mobility and long-term exposure to neighborhood poverty among children born in poor families: A U.S. longitudinal cohort study. Social Science & Medicine, 226 69–76. [DOI] [PubMed] [Google Scholar]
- Link BG, & Phelan J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, (Spec No, 80–94), 80. [PubMed]
- McClure E, Feinstein L, Cordoba E, Douglas C, Emch M, Robinson W, … Aiello AE (2019). The legacy of redlining in the effect of foreclosures on Detroit residents’ self-rated health. Health Place, 55, 9–19. 10.1016/j.healthplace.2018.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez DD, Hogan VK, & Culhane JF (2013). Stress during pregnancy: the role of institutional racism. Stress Health, 29(4), 266–274. 10.1002/smi.2462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morning A. (2012). Everyone knows it’s a social construct: contemporary science and the nature of race. Sociological Focus, 40(4), 436–454. [Google Scholar]
- Rossen LM, Womack LS, Hoyert DL, Anderson RN, Uddin SFG (2020). The impact of the pregnancy checkbox and misclassification on maternal mortality trends in the United States, 1999–2007. National Center for Health Statistics. Vital Health Stat 3(44), 1–61. [PubMed] [Google Scholar]
- Sen M, & Wasow O. (2016). Race as a bundle of sticks: designs that estimate effects of seemingly immutable characteristics. Annual Review of Political Science, 19(19), 499–522. 10.1146/annurev-polisci-032015-010015 [DOI] [Google Scholar]
- Shih M, Bonam C, Sanchez D, & Peck C. (2007). The social construction of race: biracial identity and vulnerability to stereotypes. Cultural Diversity and Ethnic Minority Psychology, 13(2), 125–133. 10.1037/1099-9809.13.2.125 [DOI] [PubMed] [Google Scholar]
- Shrimali BP, Pearl M, Karasek D, Reid C, Abrams B, & Mujahid M. (2020). Neighborhood privilege, preterm delivery, and related racial/ethnic disparities: An intergenerational application of the index of concentration at the extremes. American Journal of Epidemiology, 189(5), 412–421. 10.1093/aje/kwz279 [DOI] [PubMed] [Google Scholar]
- Shumate C, Hoyt A, Liu C, Kleinert A, & Canfield M. (2019). Understanding how the concentration of neighborhood advantage and disadvantage affects spina bifida risk among births to non-Hispanic white and Hispanic women, Texas, 1999–2014. Birth Defects Research, 111(14), 982–990. 10.1002/bdr2.1374 [DOI] [PubMed] [Google Scholar]
- Smith GD (1996). Income inequality and mortality: why are they related? BMJ, 312(7037), 987–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M, Kaphingst KM, Robinson-O’Brien R, & Glanz K. (2008). Creating healthy food and eating environments: policy and environmental approaches. Annual Review of Public Health, 29, 253–272. 10.1146/annurev.publhealth.29.020907.090926 [DOI] [PubMed] [Google Scholar]
- Wallace ME, Crear-Perry J, Green C, Felker-Kantor E, & Theall K. (2019). Privilege and deprivation in Detroit: infant mortality and the Index of Concentration at the Extremes. International Journal of Epidemiology, 48(1), 207–216. 10.1093/ije/dyy149 [DOI] [PubMed] [Google Scholar]
- Wang E, Glazer KB, Howell EA, & Janevic TM (2020). Social determinants of pregnancy-related mortality and morbidity in the United States: A systematic review. Obstet Gynecol, 135(4), 896–915. 10.1097/AOG.0000000000003762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward JB, Gartner DR, Keyes KM, Fliss MD, McClure ES, & Robinson WR (2019). How do we assess a racial disparity in health? Distribution, interaction, and interpretation in epidemiological studies. Annals of Epidemiology, 29, 1–7. 10.1016/j.annepidem.2018.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG (1997). Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? BMJ, 314(7080), 591–595. 10.1136/bmj.314.7080.591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Collins C. (2001). Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep, 116(5), 404–416. 10.1093/phr/116.5.404 [DOI] [PMC free article] [PubMed] [Google Scholar]


