Abstract
Purpose: Pharmacotherapy is one cornerstone of chronic obstructive pulmonary disease (COPD) management. Published U.S. data seldom includes patient-reported COPD medication use and adherence. We add this patient perspective to the commonly reported administrative prescribing and fill data.
Methods: This survey study used inhaler and nebulizer pictures and lists of oral COPD medications to query members of the COPD Foundation Patient-Powered Research Network, a national, self-reported online registry. Medications used, adherence, inhaler education, cost concerns, previous exacerbations, and COPD Assessment Test scores were assessed and summarized using simple descriptive statistics and hazard ratios controlling for age, gender, and disease burden.
Results: Respondents mean age was 68 years, 60% were women, >69% had COPD Assessment Test (CAT) scores >15, and >50% reported 2 or more exacerbations in the past 12 months. Overall, >98% used 1 or more inhaled COPD medications, 7.6% used a rescue inhaler only, 17.8% used long-acting bronchodilator only therapy (11.1% dual), and 72.8% used corticosteroid therapies, including 53% who were on triple therapy. Nebulizers were used by 59.4% and 34.8% used oral COPD medications. Reported adherence rates were high (80.1%), but 41% reported trouble paying for medications, with 20.1% reporting missing medications due to cost.
Conclusions: In this population, COPD had a high burden with >50% of respondents using triple therapy, and 1 in 8 using maintenance oral corticosteroids. Self-reported adherence was high, but with significant cost concerns reported, resulting in missed medications.
Keywords: copd, therapy, medications, inhalers, nebulizers
Introduction
This article contains supplemental material.
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death and disability in the United States, primarily among adults aged 45 years and older.1-2-3-4-5 While up to 50% of COPD appears to remain undiagnosed, 6-7-8-9 COPD that is diagnosed is usually managed within primary care practices.10-11-12 The financial and human burdens for COPD are significant for the U.S. health care system and people and families living with COPD.4,5,13 Many attempts are in progress to expand and enhance current COPD recognition and treatment.14-15-16 Those efforts might be improved with a broader perspective of the current state of COPD management, particularly the patients’ perspective of how they are using COPD medications.
Care for COPD is a combination of non-pharmacologic treatment such as smoking cessation, regular activity, pulmonary rehabilitation, and immunizations in addition to daily pharmacotherapy. Recommendations most relevant to this 2018 survey for initiating and changing pharmacotherapy are summarized in the 2018 Global initiative for chronic Obstructive Lung Disease (GOLD) guidelines.17 Most therapy is aimed at the reduction of symptoms and prevention of exacerbations with limited opportunities to modify underlying disease.
Many reports have reviewed currently prescribed COPD pharmacotherapy and found that it often does not follow GOLD recommendations.18,19 Several studies have reviewed the use of inhaled corticosteroids (ICSs) for COPD management and reported frequent “overprescribing.” 17,20-21-22-23-24 In addition, studies report that patients often fail to take or continue to use the therapies that have been prescribed.25-26-27-28-29-30 A recent study that used data from a large health care system reported that adherence to or continuation of COPD medications was less than 50% over a year and substantially lower than the adherence for other chronic and often asymptomatic chronic conditions such as hypertension or hyperlipemia.31
Other reports on adherence to COPD medications have included information on inadequate inhaler technique, which can adversely impact the effectiveness of poorly used inhalers.32,33 Those studies have shown high rates of 1 or more inhaler use errors and limited patient education to support inhaler use.34-35-36-37-38-39-40 Reports on adequacy and education with nebulized COPD medication are limited, with little published data found.41
Most reports use medical record or administrative prescription and pharmacy fulfillment data and do not include any patient reports of their perceived medication use or adherence rates. The prescription and fulfillment data may be considered more objective than patient reports but fail to include the ultimate step of a patient using or not using the medications they are prescribed or obtain from a pharmacy.3,42 We used a patient survey to ask about medications people with COPD were currently taking. Queries included which inhalers, nebulizers, or oral prescription medications they were using plus any non-prescription therapies. Since COPD control has been repeatedly reported to be impacted by adherence12,34,43 we queried 2 aspects of adherence: (1) patient-reported inhaler and nebulizer technique education and (2) patients’ self-perceived frequency of medication use. In addition, we asked respondents to rate their beliefs regarding the importance and concerns about those medications, their use of supplemental oxygen, and the COPD Assessment Test (CAT) scores.44
The goal of this work is to provide a complementary perspective to large database studies completed from the health care perspective and to try to identify potential medication use patterns and issues with beliefs or concerns that might be appropriate for continued study of medication adherence in COPD management.
Methods
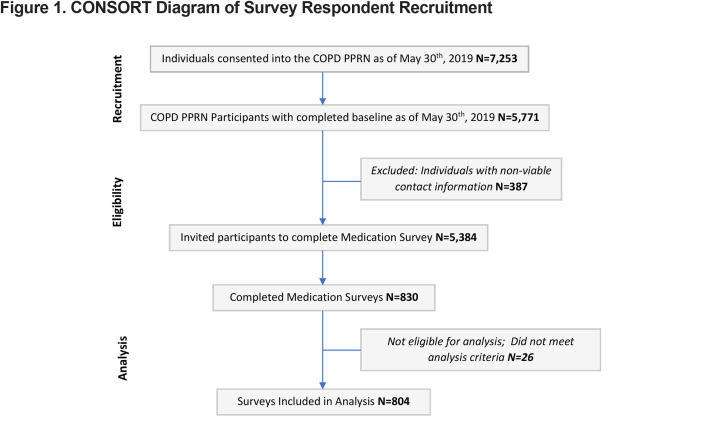
This survey study, launched on March 5, 2019, was conducted among active members of the COPD Foundation Patient-Powered Research Network (COPD PPRN). Such networks have been shown to provide a reliable source of patient-reported data.45 The COPD PPRN was established in 2014 with initial funding by the Patient-Centered Outcomes Research Institute (PCORI). Since the PPRN’s inception in 2014 and the time of this survey launch on March 5, 2019, over 6000 individuals with self-reported COPD (including chronic bronchitis and emphysema) or at high risk of developing COPD had enrolled and consented to be invited to future research studies such as this survey. Of those enrolled, 5771 had provided baseline data and of those, 5384 were sent email invitations between March 5, 2019 and May 30, 2019. A total of 830 completed the survey and 804 met the inclusion criteria of having self-reported COPD. The data from these 804 were included in the data analysis for this study. (See CONSORT diagram, Figure 1) In addition to survey responses, this analysis included information from the baseline surveys (exacerbation occurrences and the CAT) that are completed by those who have enrolled in the PPRN and provided informed consent to be contacted for future studies such as this medication survey.
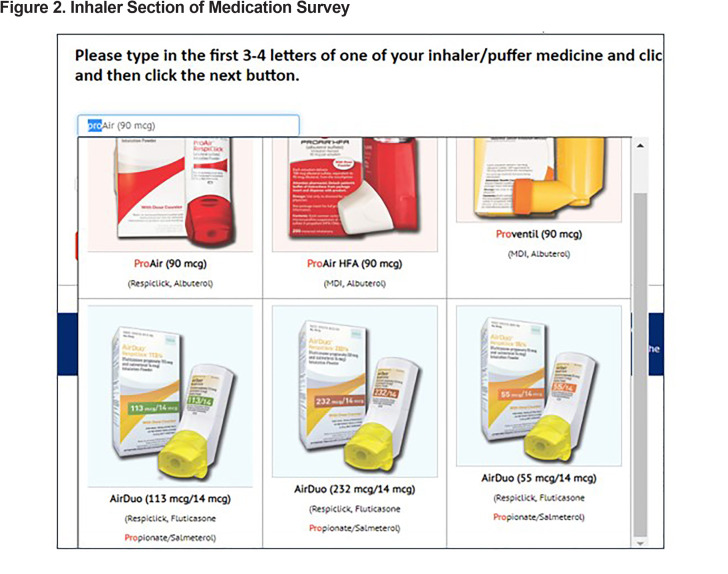
To facilitate reporting, medications were divided into 4 sections–inhalers, nebulizers, pills or liquids, and other over the counter and alternative therapies. Additional questions were included to address adherence, access, and device use education. In the inhaler section, respondents were asked to enter the first 3 to 4 letters of the inhaled medication (brand name or generic name), triggering the appearance of pictures of the corresponding inhalers in all available doses. Figure 2 provides an example of pictures for “pro” or “alb” (albuterol inhalers/specifically Pro-Air).
After each inhaled medication was chosen, respondents were asked several follow-up questions designed to gather information on the frequency of inhaler use, inhaler technique education and teach-back (observation by a health care professional), and issues regarding cost and access to the medication. The supplemental figure in the online supplement provides an example of the questions. Each follow-up question had the name of the chosen medication piped into the question stem. After completing the follow-up questions, participants were asked if they took any other inhalers/puffers. If they answered “Yes,” they completed similar questions for all other inhaled medications. If they responded “No,” they moved on to the Nebulized Medication section which used a similar process to identify medications and answer follow-up questions about each type of nebulized medication.
After completing the information on all nebulizers, or none if that was the case, the respondents moved on to the pills and liquids section. It was not feasible to display images of all available oral medications, and so these questions used only medication names. Following each reported pill or liquid used, questions similar to those following each inhaler were asked.
In the fourth section, queries regarding other non-prescription therapies required responses to open-ended questions with respondents typing in answers. Following a complete listing of their COPD medications, respondents were asked to complete questions about perceived medication adherence and adherence to an overall COPD treatment plan,46 use of over-the-counter COPD medications, ability to manage COPD medications, and medication cost concerns in the past 12 months. Finally, all respondents were asked to complete the CAT.
Information from the respondents’ answers to the COPD PPRN baseline survey was used to supply demographic data such as age and gender, and history of exacerbations.
Statistical Analysis
Descriptive statistics were computed for the respondents' demographic and clinical characteristics. Mean and standard deviation (SD) were calculated for continuous variables, and categorical variables were summarized by frequencies and proportions. Medication use combinations were aggregated across all questions related to the use of inhalers, nebulizers, and oral medications. The frequency and proportions of inhaled, nebulized, and oral medications classes were computed. Stratified analyses of numbers of exacerbations (0, 1, and 2 or more) by the inhaled medication classes and by oral medication classes were performed. Multivariable logistic regression models were fit for the use of nebulized medications, examining the association with the use of oxygen, self-reported exacerbations in prior 12 months, CAT score, and adjusting for age and gender. The significance level was set at 0.05. All statistical analyses were performed using SAS 9.4.
The study was approved by the Western Institution Review Board and all respondents provided e-consent.
Results
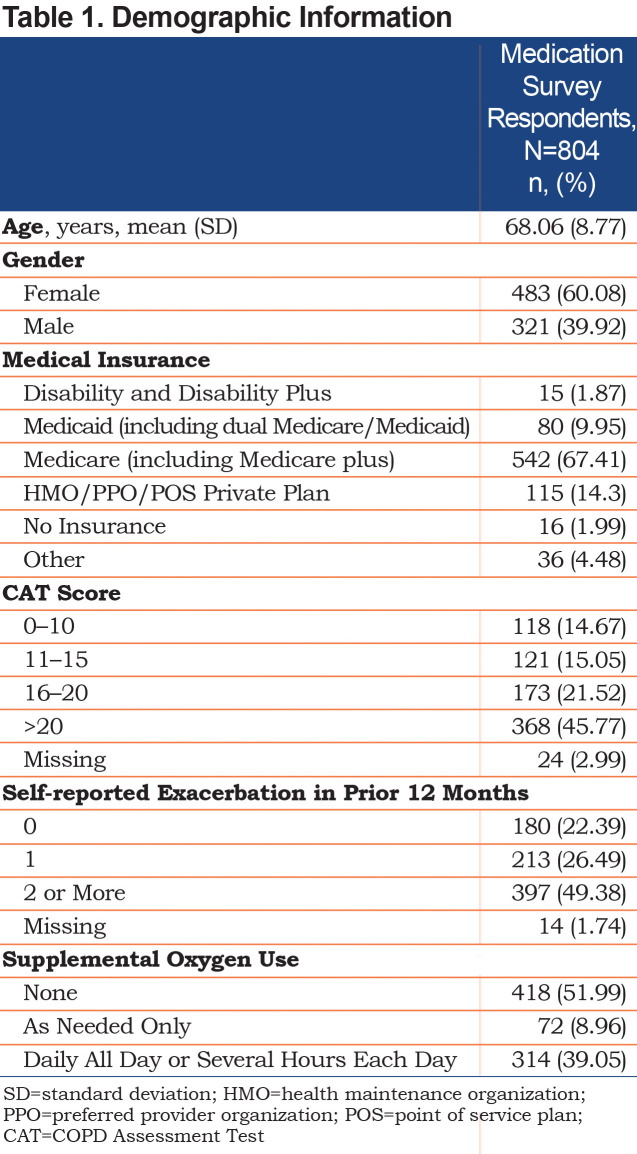
A total of 804 people with self-reported COPD completed the medication survey and were included in the analyses. Respondents' average age was 68 years, and 60% were women. Less than 2% reported having no insurance, with over 77% insured through Medicare or Medicaid. The group was highly symptomatic, with 85% having CAT scores >10 and almost half having scores >20; the majority reported 2 or more exacerbations in the prior 12 months and 48% reported using supplemental oxygen either as needed or daily. (Table 1)
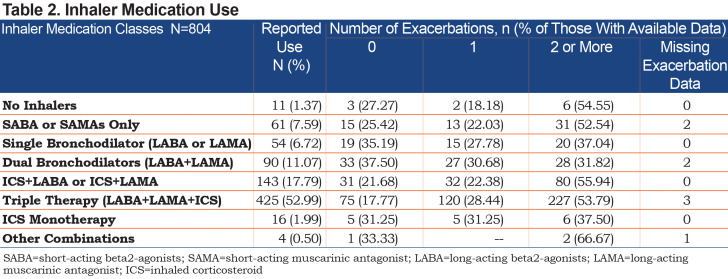
As anticipated in a highly symptomatic population of people with COPD, almost all respondents reported using inhaled medications regularly, with only 1.4% saying they had neither inhaled nor nebulized COPD medications. Another 7.6% reported using only short-acting bronchodilator or quick relief therapy. Treatment limited to either single (long-acting muscuranic antagonists[LAMA] or long-acting beta2-agonists[LABA]) or dual bronchodilator therapy (LAMA+LABA) was used by 17.8% (n=143). Overall, 72.8% of respondents (n=588) reported using therapies that included inhaled corticosteroids (ICSs), primarily in the form of a “triple” therapy of LAMA+ LABA + ICS in 1 or more inhalers (52.99%, n=425). A small number of respondents (2.0%) reported they used ICS mono-therapy for their COPD. Table 2 summarizes the frequency of classes of COPD medications used and exacerbation frequency over the prior 12 months.
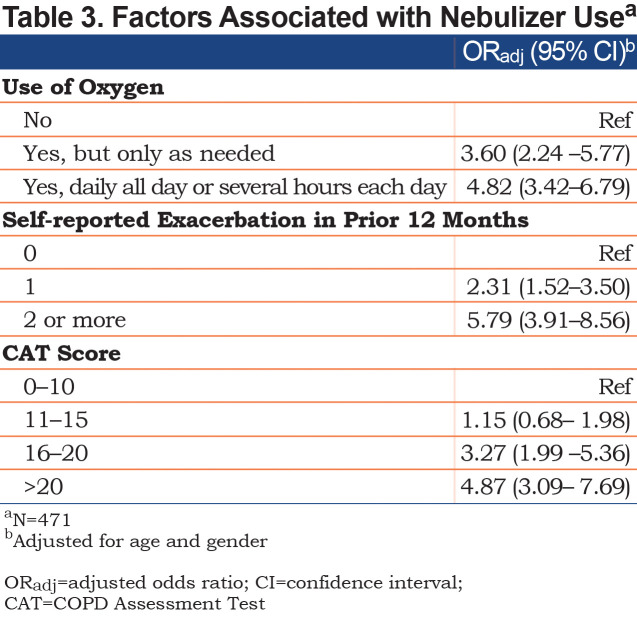
A total of 471 respondents (59.4% of the 793 using inhaled COPD medicines) reported using 1 or more types of nebulized therapy in addition to inhaler therapy. Almost all nebulized therapies were short-acting bronchodilators (n=395, 83.9%). When the reported types of nebulized therapies were compared to classes of inhaler-based therapies, no individual reported using any different class of medications than they had already reported using in an inhaler (data not shown). Adjusting for age and gender, nebulizer use was associated with self-reported oxygen as needed or daily use, having 1, or 2 or more exacerbations in the past 12 months, and CAT scores44 greater than 15 (Table 3).
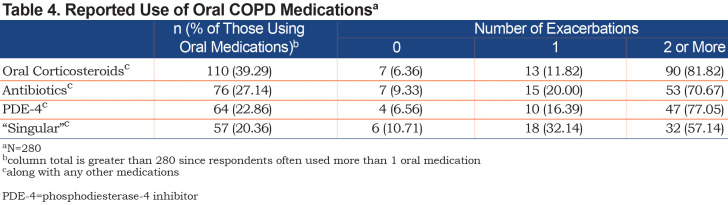
Oral medication use was also not uncommon in this group, with 280 of the 804 (34.8%) reporting use of 1 or more oral maintenance therapies in addition to their inhaled therapies. Oral corticosteroids were the most common, used by 110 (12.4%) of the 804 respondents and 39.3% of those using any oral medications. (Table 4). Of the 110 people using oral steroids “regularly,” 52 (47.3%) used the oral steroids daily with another 2 people (1.8%) using them weekly, and the rest (n= 56, 50.9%) had oral steroids or a prescription for them on hand to use “as needed” with most of these respondents reporting that they had used oral steroids 1 or more times within the past 3 months.
Fewer respondents reported using either daily or weekly antibiotics, primarily azithromycin47 (9.5%, 76 of the 804) or daily phosphodiesterase-4 (PDE-4) inhibitors (8.0%, 64 of the 804) compared to the >12% who regularly used oral steroids. Overall, > 70% of respondents who reported using oral steroids or antibiotics regularly also reported experiencing 2 or more exacerbations in the past 12 months. Slightly over three-quarters (76.6%) of those reporting use of PDE-4 inhibitors48 reported moderate to high burden of cough or phlegm on the CAT.
Overall, 57 (0.7% of the 804 or 20.4% of the 280 using any oral COPD medications) reported using leukotriene receptor antagonists (LTRA), with more than half reporting 2 or more exacerbations in the past 12 months. It is not known how many of the LTRA users had treatable traits consistent with both asthma and COPD.17
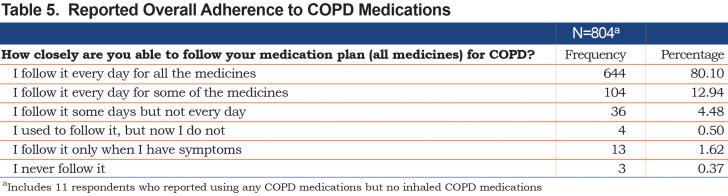
This group of individuals with COPD reported very high levels of adherence to their COPD medication plans. (Table 5) Overall, 91.4% stated that they had no trouble managing all of their COPD inhalers, nebulizers, and oral medications. Yet, many (40.8%, n=328) reported they had difficulty paying for all of their COPD medications, with 21% (n=169) reporting that during the past 12 months, there were times when they did not obtain all of their COPD medications due to being unable to pay for them. When asked in a slightly different way, even more respondents (27.7%, n=223) reported that financial issues resulted in them taking less of their medications than prescribed for some period during the past 12 months.
Adherence is also affected by the adequacy of inhaler technique. While it is not possible to assess proper inhaler technique in an online written survey, respondents were asked if someone had shown them how to use each of the inhalers and nebulizers they reported using. Of the 793 who reported using 1 or more inhalers, 661 (83.35%) reported that someone had shown them how to use at least 1 of their inhalers, but only 246 (31.02%) had been shown how to use all of their inhalers and 380 (47.92%) reported that anyone had asked them to demonstrate how they used even 1 of their inhalers. For the 471 using nebulizers, 339 (71.97%) reported they had received instructions on how to use a nebulizer, but only 168 (35.67%) reported that anyone had observed their nebulizer technique.
Discussion
We asked a group of people with self-reported diagnoses of COPD to report on their COPD medication use and potential barriers to adherence, including costs and receipt of inhaler and nebulizer technique education. The group of individuals was on average close to 70 years of age, had very symptomatic COPD, had about half who reported 2 or more exacerbations in the prior 12 months, and included most reporting being on multiple COPD medications.
The self-reported medications resembled similar patterns to those reported in the literature using pharmacy or medical record data but with higher rates of use of triple therapy, which might be anticipated considering more recent recommendations, clinical trial results, and the high rates of reported exacerbations in the respondents.19,49-50-51-52
Our data appears to confirm earlier reports that suggest some overuse of both inhaled and oral corticosteroids.17,23 For example, 18.2% of respondents regularly using (daily or weekly) oral corticosteroids did not report a history of 2 or more exacerbations in the prior year. Whether this reflects the overprescribing of daily corticosteroids that has been reported by others21,53 or appropriate prescribing that resulted in lower subsequent rates of exacerbations is not known. Similarly, the >40% of respondents taking ICSs but reporting fewer than 2 exacerbations in the past 12 months may represent overprescribing of ICSs that is not consistent with then-current and latest GOLD treatment recommendations17,54 or may also represent individuals with a history of repeated exacerbations in years prior to the past 12 months and physicians’ or other clinicians’ discomfort with recommendations for step down therapy.22,55 This dilemma in interpretation of what is the appropriate use of daily ICSs is seen commonly in the published literature since most recommendations and many studies, including ours, fail to include or assess long-term patterns of exacerbations over multiple previous years. Studies show that while the best prediction of frequent exacerbations is the past history of frequent exacerbations, 17 very limited attention is paid to the long-term pattern of exacerbations over several years when recommending step down therapy.56 It is possible that some of the individuals currently using daily inhaled or oral steroids have had repeated exacerbations prior to the past 12 months, and physicians, or hopefully both patients and physicians, agreed that use of daily ICSs has benefits in preventing those exacerbations that outweigh risks of continued use.7,57-58-59 We do not have many other chronic, potentially progressive conditions in which we recommend discontinuation of successful therapy. It is important to better understand the longer-term trajectory of exacerbations and corticosteroid use before assuming all use of this drug class is inappropriate or overprescribed. Rather than a short-term view in a long-term disease, it may be that recommendations for prescribing and stepping down treatment should be based on a 2- or 3- or even 4-year history of exacerbations.
Similarly, we note that 57 people report using a LTRA (singular) which currently is not approved or recommended for COPD management.54 However, as more attention is given to identifying treatable traits and tailoring therapy to the individual, allergen sensitization, and asthma-like features, the use of LTRA therapy should be re-studied in these subgroups. Positive responses in subgroups may be masked in the analyses of the value of this therapy when looking at the COPD population overall.59
Incomplete or even poor medication adherence rates are a major concern for COPD therapy. Our patient-reported findings are quite different than those reported based on specific refill of COPD medications, which have reported COPD medication persistence rates of as low as 40% over a 1- to 3-year period. 26,31,60 In contrast, over 80% of our respondents report they believe they take their medications according to their treatment plans. This may reflect, in part, the high symptom and exacerbation burden reported by the people we surveyed, with the majority reporting a CAT score of >20 and having 2 or more exacerbations in the prior 12 months. Studies from other groups have included people with a broader range of COPD symptoms and exacerbation severity and frequency, many with low to moderate symptoms and exacerbation burden. In these less severely impacted groups, e.g., those with lower severity, adherence rates may be lower. 31,61,62 In addition to the COPD disease severity, most people with COPD have other multiple morbidities which may impact their adherence to what often becomes poly-pharmacy required to treat all their chronic conditions.55,43,63 We need to continue to try to understand the perceived need of people with COPD of all severity, symptom burden, and risk levels and their self-reported and objectively assessed levels of adherence to daily therapy. It is possible that those with milder symptoms may perceive less therapeutic benefit from prescribed therapies resulting in lower adherence rates while those with high COPD burden are more likely to develop better adherence strategies and habits.64
However, even among these respondents who reported taking medications very regularly, over 40% said they had financial problems obtaining all medications, and over 27% said they had taken less than the prescribed amounts of 1 or more of their COPD medications in the prior year due to costs. This would suggest lower levels of being able to adhere to treatment plans than the patients’ overall adherence assessment suggests. Patients may be reporting their levels of adherence when they have access to the medications. Most studies of drug fulfillment do not include data on why patients did not refill medications, and many studies have been reported from countries with no costs for medications making it difficult to compare to the cost concerns and barriers reported by our respondents. 60,65-66-67 Within the United States, the differences in these self-reported adherence data and that from pharmacy plan-based fulfillment data may, in part, be based on what is being reported. Patients may report adherence when they have medications, and the database studies may report results only among those who obtained the medications, not those prescribed. These differences highlight the importance of obtaining multiple types of data when addressing adherence issues and proposing solutions.
The other issue with adherence that is often overlooked and can seldom be reported from database information relates to the proper use of inhaled and nebulized medications.60,67,68 Inadequate inhaler or nebulizer technique may result in consequences similar to not using the inhaled therapy at all. In our respondents with a heavy symptom and exacerbation burden and high levels of having a specialist as part of their care team, the levels of inhaler technique education were very high for receipt of education for any inhaler but much lower for receiving education regarding each of their different types of inhalers. Levels of having someone observe that inhaler or nebulizer technique were even lower. High levels of inadequate or poor inhaler technique have been identified in the literature for many years, yet remain a gap in COPD care.61,69 Little information is reported in the literature regarding teaching or assessment of nebulizer technique. Several tools have been developed to support inhaler and nebulizer education, including online videos that can be viewed with the patient and family in the office setting and suggested ways to use, and even virtual visits to observe patients’ techniques. Payment for these services remains low with perceived significant documentation burdens. Some attempts to make this type of inhaler technique teaching a quality indicator have been tried, such as the quality indicator suggested by the Minnesota Institute for Clinical Science Improvement70 in 2013. This quality indicator failed and was retired due to the need to review individual medical records (large data collection burden) to assess documentation of such education. Even when these quality indicators were developed, few included teach-back during which the patient’s actual technique is viewed. Telehealth or virtual visits may facilitate increased uptake since the patient is usually at home where they should have inhalers or nebulizers available rather than having to bring the devices to an office visit. Continued work to find ways to incentivize incorporation of teaching and teach-back into COPD management must be completed across the spectrum of COPD care sites—outpatient, urgent care, minute clinic, virtual, emergency department, and hospital visits.
The study has both limitations which with might limit its generalizability and strengths related to adding the patient voice to published COPD medication reports. The overall population who registered for the COPD Foundation’s PPRN are engaged enough in their condition to go online and register for the PPRN. The respondents have higher rates of oxygen use than the general population of people with COPD. The diagnoses of COPD are self-reported but the very high percentage of the group who report receiving daily COPD maintenance medications makes it unlikely that they have not been diagnosed with COPD. How that diagnosis was made or confirmed and the diagnostic accuracy are not known. Our response rate is estimated at 15% and is not high but comparable to response rates for other patient surveys.71,72 Asking for detailed medication use based on both medication names and pictures likely enhanced the accuracy of reporting of both using a COPD medication and the class(es) of medications used. While self-reported adherence was higher than reported in the literature, a significant percentage of respondents did report having problems obtaining all prescribed medications.
Our results highlight continued opportunities to improve and assess COPD pharmacotherapy, even in a group of people with COPD with sufficient motivation to join an online COPD registry and complete a lengthy medication survey. A few respondents had no or only short duration rescue inhalers or ICS mono-therapy for COPD management, appearing to offer easy targets for improvement. The high rate of use of ICSs and oral steroids requires more complex assessment and decision making, including a need to consider rates of exacerbations beyond the 12-month timeframe usually assessed. Superficial data assessment appears to demonstrate high levels of medication adherence as well as high levels of inhaler and nebulizer use education. However, a more in-depth assessment shows that more than 40% of the respondents report financial hardship in obtaining their COPD medications, and 27% report using less medication than prescribed due to these financial barriers. Similarly, rates of receiving education on at least 1 of their inhalers or nebulizers are high, but rates of receiving education or observation of use of all prescribed inhalers and nebulizers are much lower, leaving opportunities for continued care improvement.
Abbreviations
Abbreviations: chronic obstructive pulmonary diseases, COPD; Global initiative for chronic Obstructive Lung Disease, GOLD; inhaled corticosteroid, ICS; COPD Assessment Test, CAT; COPD Foundation Patient-Powered Research Network, COPD-PPRN; Patient-Centered Outcomes Research Institute, PCORI; standard deviation, SD; long-acting muscarinic antagonist, LAMA; long-acting beta2-agonist, LABA; inhaled corticosteroid, ICS; heath maintenance organization, HMO; preferred provider organization, PPO; point of service, POS; short-acting beta2-agonist, SABA; short-acting muscarinic antagonist, SAMA; adjusted odds ratio, ORadj;confidence interval, CI; phosphodiesterase-4, PDE-4; leukotriene receptor antagonists, LTRA
Funding Statement
Novartis Pharmaceuticals provided unrestricted funds to develop a medication survey to be used in this study
References
- 1.Centers for Disease Control and Prevention (CDC). Fact sheets for chronic diseases. CDC website. Updated March 1, 2021. Accessed March 5, 2021. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm [Google Scholar]
- 2.Sullivan J,Pravosud V,Mannino DM,Siegel K,Choate R,Sullivan T. National and state estimates of copd morbidity and mortality - United States, 2014-2015. Chronic Obstr Pulm Dis. 2018;5(4):324-333. doi: https://doi.org/10.15326/jcopdf.5.4.2018.0157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choate R,Mannino DM. Chronic obstructive pulmonary disease: epidemiology, clinical presentation, and evaluation. J Clin Outcomes Manag. 2017;24(4). https://www.mdedge.com/jcomjournal/article/145942/pulmonology/chronic-obstructive-pulmonary-disease-epidemiology-clinical [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC). COPD fact sheets. CDC website. Updated February 21, 2018. Accessed March 5, 2021. https://www.cdc.gov/copd/infographics/copd-costs.html [Google Scholar]
- 5.Iheanacho I,Zhang S,King D,Rizzo M,Ismaila AS. Economic burden of chronic obstructive pulmonary disease (COPD): a systematic literature review. Int J Chron Obstruct Pulmon Dis. 2020;15:439-460. doi: https://doi.org/10.2147/COPD.S234942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ho T,Cusack RP,Chaudhary N,Satia I,Kurmi OP. Under- and over-diagnosis of COPD: a global perspective. Breathe (Sheff). 2019;15(1):24-35. doi: https://doi.org/10.1183/20734735.0346-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruparel M,Quaife SL,Dickson JL,et al. Prevalence, symptom burden, and underdiagnosis of chronic obstructive pulmonary disease in a lung cancer screening cohort. Ann Am Thorac Soc. 2020;17(7):869-878. doi: https://doi.org/10.1513/AnnalsATS.201911-857OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson KM,Bryan S,Ghanbarian S,Sin DD,Sadatsafavi M. Characterizing undiagnosed chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respir Res. 2018;19(1):26. doi: https://doi.org/10.1186/s12931-018-0731-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinez CH,Mannino DM,Jaimes FA,et al. Undiagnosed obstructive lung disease in the United States. Associated factors and long-term mortality. Ann Am Thorac SocE9:F9. 2015;12(12):1788-1795. doi: https://doi.org/10.1513/AnnalsATS.201506-388OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Heart Lung and Blood Institute (NHLBI). COPD: tracking perceptions of the individuals affected and the providers who treat them, 2018 Report. NHLBI website. Published February 2019. Accessed March 11, 2021. https://doi.org/10.1513/AnnalsATS.201506-388OC [Google Scholar]
- 11.Han MK,Steenrod AW,Bacci ED,et al. Identifying patients with undiagnosed COPD in primary care settings: insight from screening tools and epidemiologic studies. Chronic Obstr Pulm Dis. 2015;2(2):103-121. doi: https://doi.org/10.15326/jcopdf.2.2.2014.0152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Press VG,Au DH,Bourbeau J,et al. Reducing chronic obstructive pulmonary disease hospital readmissions. An official american thoracic society workshop report. Ann Am Thorac Soc. 2019;16(2):161-170. doi: https://doi.org/10.1513/AnnalsATS.201811-755WS [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foo J,Landis SH,Maskel J,et al. Continuing to confront COPD international patient survey: economic impact of COPD in 12 countries. PLoS One. 2016;11(4):e0152618. doi: https://doi.org/10.1371/journal.pone.0152618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martinez FJ,O'Connor GT. Screening, case-finding, and outcomes for adults with unrecognized COPD. JAMA. 2016;315(13):1343-1344. doi: https://doi.org/10.1001/jama.2016.3274 [DOI] [PubMed] [Google Scholar]
- 15.Yawn BP,Han M,Make BM,et al. Protocol summary of the COPD assessment in primary care to identify undiagnosed respiratory disease and exacerbation risk (CAPTURE) validation in primary care study. Chronic Obstr Pulm Dis. 2021;8(1):60-75. doi: http://doi.org/10.15326/jcopdf.2020.0155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sogbetun F,Eschenbacher W,Welge J,Panos R. A comparison of five surveys that identify individuals at risk for airflow obstruction and chronic obstructive pulmonary disease. Respir Med. 2016;120:1-9. doi: https://doi.org/10.1016/j.rmed.2016.09.010 [DOI] [PubMed] [Google Scholar]
- 17.Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategies for the diagnosis, management and prevention of chronic obstructive pulmonary disease, 2018 report. GOLD website. Published 2018. Accessed January 25, 2021. https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf [Google Scholar]
- 18.Halpin DMG,de Jong HJI,Carter V,Skinner D,Price D. Distribution, temporal stability and appropriateness of therapy of patients with COPD in the UK in relation to GOLD 2019. EClinicalMedicine. 2019;14:32-41. doi: https://doi.org/10.1016/j.eclinm.2019.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghosh S,Anderson WH,Putcha N,et al. Current and former investigators of the SPIROMICS sites and reading centers. Alignment of inhaled chronic obstructive pulmonary disease therapies with published strategies. Analysis of the global initiative for chronic obstructive lung disease recommendations in SPIROMICS. Ann Am Thorac Soc. 2019;16(2):200-208. doi: https://doi.org/10.1513/AnnalsATS.201804-283OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnes PJ. Inhaled corticosteroids in COPD: a controversy. Respiration. 2010;80(2):89-95. doi: https://doi.org/10.1159/000315416 [DOI] [PubMed] [Google Scholar]
- 21.Saeed MI,Eklof J,Achir I,et al. Use of inhaled corticosteroids and the risk of developing type 2 diabetes in patients with chronic obstructive pulmonary disease. Diabetes Obes Metab. 2020;56(suppl 64):1434. doi: https://doi.org/10.1183/13993003.congress-2020.1434 [DOI] [PubMed] [Google Scholar]
- 22.Yawn BP,Suissa S,Rossi A. Appropriate use of inhaled corticosteroids in COPD: the candidates for safe withdrawal. NPJ Prim Care Respir Med. 2016;26:160-168. doi: https://doi.org/10.1038/npjpcrm.2016.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wedzicha JA,Calverley PMA,Albert RK,et al. Prevention of COPD exacerbations: an ERS/ATS guideline. Eur Respir J. 2017;50(3):1602265. doi: https://doi.org/10.1183/13993003.02265-2016 [DOI] [PubMed] [Google Scholar]
- 24.Criner GJ,Bourbeau J,Diekemper RL,et al. Executive summary: prevention of acute exacerbation of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015;147(4):883-893. doi: https://doi.org/10.1378/chest.14-1677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saxon LA,Doshi A. Editorial commentary: re-inventing chronic disease management as a service - medication adherence solutions are ground zero. Trends Cardiovasc Med. 2019;29(2):118-119. doi: https://doi.org/10.1016/j.tcm.2018.07.013 [DOI] [PubMed] [Google Scholar]
- 26.Cheen MHH,Tan YZ,Oh LF,Wee HL,Thumboo J. Prevalence of and factors associated with primary medication non-adherence in chronic disease: a systematic review and meta-analysis. Int J Clin Pract. 2019;73(6):e13350. doi: https://doi.org/10.1111/ijcp.13350 [DOI] [PubMed] [Google Scholar]
- 27.Parkin L,Barson D,Zeng J,Horsburgh S,Sharples K,Dummer J. Patterns of use of long-acting bronchodilators in patients with COPD: a nationwide follow-up study of new users in New Zealand. Respirology. 2018;23(6):583-592. doi: https://doi.org/10.1111/resp.13235 [DOI] [PubMed] [Google Scholar]
- 28.Davis JR,Wu B,Kern DM,et al. Impact of nonadherence to inhaled corticosteroid/LABA therapy on COPD exacerbation rates and health-care costs in a commercially insured U.S. population. Am Health Drug Benefits. 2017;10(2):92-102. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5470247/ [PMC free article] [PubMed] [Google Scholar]
- 29.Albrecht JS,Park Y,Hur P. Adherence to maintenance medications among older adults with chronic obstructive pulmonary disease: the role of depression. Ann Am Thorac Soc. 2016;13(9):1497-1504. doi: https://doi.org/10.1513/AnnalsATS.201602-136OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campos LF,Glickman ME,Hunter KB. Measuring effects of medication adherence on time-varying health outcomes using Bayesian dynamic linear models. Biostatistics. 2021;22(3):662-683. doi: https://doi.org/10.1093/biostatistics/kxz059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gillespie CW,Morin PE,Tucker JM,Purvis L. Medication adherence, health care utilization, and spending among privately insured adults with chronic conditions in the United States, 2010-2016. Am J Med. 2020;133(6):690-704. E19. doi: https://doi.org/10.1016/j.amjmed.2019.12.021 [DOI] [PubMed] [Google Scholar]
- 32.Molimard M,Raherison C,Lignot S,et al. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: real-life assessment of 2935 patients. Eur Respir J. 2017;49(2):1601794. doi: https://doi.org/10.1183/13993003.01794-2016 [DOI] [PubMed] [Google Scholar]
- 33.Hanania NA,Braman S,Adams SG,et al. The role of inhalation delivery devices in COPD: perspectives of patients and health care providers. Chronic Obstr Pulm Dis. 2018;5(2):111-123. doi: http://doi.org/10.15326/jcopdf.5.2.2017.0168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cho-Reyes S,Celli BR,Dembek C,Yeh K,Navaie M. Inhalation technique errors with metered-dose inhalers among patients with obstructive lung diseases: a systematic review and meta-analysis of U.S. studies. Chronic Obstr Pulm Dis. 2019;6(3):267-280. doi: http://doi.org/10.15326/jcopdf.6.3.2018.0168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yawn BP,Colice GL,Hodder R. Practical aspects of inhaler use in the management of chronic obstructive pulmonary disease in the primary care setting. Int J Chron Obstruct Pulmon Dis. 2012;7:495-502. doi: https://doi.org/10.2147/COPD.S32674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanchis J,Gich I,Pedersen S,et al. Systematic review of errors in inhaler use: has patient technique improved over time? Chest. 2016;150(2):394-406. doi: https://doi.org/10.1016/j.chest.2016.03.041 [DOI] [PubMed] [Google Scholar]
- 37.Wu M,Woodrick NM,Arora VM,Farnan JM,Press VG. Developing a virtual Teach-To-Goal™ inhaler technique learning module: a mixed methods approach. J Allergy Clin Immunol Pract. 2017;5(6):1728-1736. doi: https://doi.org/10.1016/j.jaip.2017.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Griffith MF,Feemster LC,Donovan LM,Spece LJ,Au DH. Reply: effective inhaler training is critical. Ann Am Thorac Soc. 2019;16(11):1460. doi: https://doi.org/10.1513/AnnalsATS.201907-568LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melzer AC,Ghassemieh BJ,Gillespie SE,et al. Patient characteristics associated with poor inhaler technique among a cohort of patients with COPD. Respir Med. 2017;123:124-130. doi: https://doi.org/10.1016/j.rmed.2016.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Griffith MF,Feemster LC,Donovan LM,et al. Poor metered-dose inhaler technique isassociated with overuse of inhaled corticosteroids. Ann Am Thorac Soc. 2019;16(6):765-768. doi: https://doi.org/10.1513/AnnalsATS.201812-889RL [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dhand R,Dolovich M,Chipps B,et al. The role of nebulized therapy in the management of COPD: evidence and recommendations. COPD. 2012;9(1):58-72. doi: https://doi.org/10.3109/15412555.2011.630047 [DOI] [PubMed] [Google Scholar]
- 42.Molimard M,Colthorpe P. Inhaler devices for chronic obstructive pulmonary disease: insights from patients and healthcare practitioners. J Aerosol Med Pulm Drug Deliv. 2015;28(3):219-228. doi: https://doi.org/10.1089/jamp.2014.1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Halpin DMG,De Jong H,Carter V,Skinner D,Price D. Prevalence of comorbidities in established and newly treated patients with COPD according to GOLD 2017 in a UK primary care population. Eur Resp J. 2018;52(3):213-218. doi: https://doi.org/10.1183/13993003.congress-2018.PA3616 [Google Scholar]
- 44.Jones PW,Harding G,Berry P,Wiklund I,Chen W-H,Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648-654. doi: https://doi.org/10.1183/09031936.00102509 [DOI] [PubMed] [Google Scholar]
- 45.Daugherty SE,Wahba S,Fleurence R,et al. Patient-powered research networks: building capacity for conducting patient-centered clinical outcomes research. J Am Med Inform Assoc. 2014;21(4):583-586. doi: https://doi.org/10.1136/amiajnl-2014-002758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morisky DE,Green LW,Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67-74. doi: https://doi.org/10.1097/00005650-198601000-00007 [DOI] [PubMed] [Google Scholar]
- 47.Albert RK,Connett J,Bailey WC,et al. Azithromycin for prevention of exacerbation of COPD. N Engl J Med. 2011;365:689-698. doi: https://doi.org/10.1056/NEJMoa1104623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martinez FJ,Calverley PM,Goehring UM,et al. Effect of roflumilast on exacerbations in patients with severe chronic obstructive pulmonary disease uncontrolled by combination therapy (REACT): multicentre randomized controlled trial. Lancet. 2018;385(9971):857-868. doi: https://doi.org/10.1016/S0140-6736(14)62410-7 [DOI] [PubMed] [Google Scholar]
- 49.Di Martino M,Agabiti N,Bauleo L,et al. Use patterns of long-acting bronchodilators in routine COPD care: the OUTPUL study. COPD. 2014;11(4):414-423. doi: https://doi.org/10.3109/15412555.2013.839646 [DOI] [PubMed] [Google Scholar]
- 50.Brusselle G,Price D,Gruffyd J,et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J Chron Obstruct Pulmon Dis. 2015;10(1):2207-2217. doi: https://doi.org/10.2147/COPD.S91694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rabe KF,Martinez FJ,Ferguson,et al. Triple inhaled therapy at two doses in moderate-to-very severe COPD. N Eng J Med. 2020;383(1):35-48. doi: https://doi.org/10.1056/NEJMoa1916046 [DOI] [PubMed] [Google Scholar]
- 52.Lipson DA,Barnhart F,Breasley N,et al. Once-daily single inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671-1680. doi: https://doi.org/10.1056/NEJMoa1713901 [DOI] [PubMed] [Google Scholar]
- 53.Suissa S,Patenaude V,Lapi F,et al. Inhaled corticosteroids in COPD and the risk of serious pneumonia. Thorax. 2013;68(11):1029-1036. doi: https://doi.org/10.1136/thoraxjnl-2012-202872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategies for the diagnosis, management and prevention of chronic obstructive pulmonary disease, 2021 report. GOLD website. Published 2021. Accessed January 25, 2021. https://goldcopd.org [Google Scholar]
- 55.Rinne ST,Wiener RS,Chen Y,et al. Impact of guideline changes on indications for inhaled corticosteroids among veterans with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1226-1228. doi: https://doi.org/10.1164/rccm.201803-0554LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Magnussen H,Disse B,Rodriguez-Roisin R,et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285-1294. doi: https://doi.org/10.1056/NEJMoa1407154 [DOI] [PubMed] [Google Scholar]
- 57.Lipson Da,Barnacle H,Birk R,et al. FULFIL trials: once-daily triple therapy in patient with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;196(4):438-446. doi: https://doi.org/10.1164/rccm.201703-0449OC [DOI] [PubMed] [Google Scholar]
- 58.Nadeem NJ,Taylor SJC,Eldridge SM. Withdrawal of inhaled corticosteroids in individuals with COPD-a systemic review and comment on trial methodology. Respir Res. 2011;12:107-110. doi: https://doi.org/10.1186/1465-9921-12-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Dijk M,Gan CT,Koster TD,et al. Treatment of severe stable COPD: the multidimensional approach of treatable traits. ERJ Open Res. 2020;6(3):00322-2019. doi: https://doi.org/10.1183/23120541.00322-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Price D,Keininger DL,Viswanad B,Gasser M,Walda S,Gutzwiller FS. Factors associated with appropriate inhaler use in patients with COPD - lessons from the REAL survey. Int J Chron Obstruct Pulmon Dis. 2018;13:695-702. doi: https://doi.org/10.2147/COPD.S178410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Humenberger M,Horner A,Labek A,et al. Adherence to inhaled therapy and its impact on chronic obstructive pulmonary disease (COPD). BMC Pulm Med. 2018;18(1):163. doi: https://doi.org/10.1186/s12890-018-0724-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rogliani P,Ora J,Puxeddu E,Matera MG,Cazzola M. Adherence to COPD treatment: myth and reality. Respir Med. 2017;129:117-123. doi: https://doi.org/10.1016/j.rmed.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 63.Albrecht JS,Park Y,Hur P. Adherence to maintenance medications among older adults with chronic obstructive pulmonary disease: the role of depression. Ann Am Thorac Soc. 2016;13(9):1497-1504. doi: https://doi.org/10.1513/AnnalsATS.201602-136OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Miravitlles M,Ribera A. Understanding the impact of symptoms on the burden of COPD. Respir Res. 2017;18(1):67. doi: https://doi.org/10.1186/s12931-017-0548-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Königsdorfer N,Jörres RA,Söhler S,et al. Adherence to respiratory and nonrespiratory medication in patients with COPD: results of the German COSYCONET cohort. Patient Prefer Adherence. 2019;13:1711-1721. doi: https://doi.org/10.2147/PPA.S223438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.López-Campos JL,Quintana Gallego E,Carrasco Hernández L. Status of and strategies for improving adherence to COPD treatment. Int J Chron Obstruct Pulmon Dis. 2019;14:1503-1515. doi: https://doi.org/10.2147/COPD.S170848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gregoriano C,Dieterle T,Breitenstein AL,et al. Use and inhalation technique of inhaled medication in patients with asthma and COPD: data from a randomized controlled trial. Respir Res. 2018;19(1):237. doi: https://doi.org/10.1186/s12931-018-0936-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.George M. Adherence in asthma and COPD: new strategies for an old problem. Respir Care. 2018;63(6):818-831. doi: https://doi.org/10.4187/respcare.05905 [DOI] [PubMed] [Google Scholar]
- 69.Lareau SC,Yawn BP. Improving adherence with inhaler therapy in COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:401-406. doi: https://doi.org/10.2147/COPD.S14715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Amderson B,Brown H,Bruhl E,et al. Chronic obstructive pulmonary disease (COPD). Diagnosis and management of. Institute for Clinical Systems Improvement (ICSI) website. Published 2016. Accessed January 21, 2021. https://www.icsi.org/guidelines/copd
- 71.Cantuaria ML,Blanes-Vidal V. Self-reported data in environmental health studies: mail vs. web-based surveys. BMC Med Res Methodol. 2019;19(1):238. doi: https://doi.org/10.1186/s12874-019-0882-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Smith MG,Witte M,Rocha S,et al. Effectiveness of incentives and follow-up on increasing survey response rates and participation in field studies. BMC Med Res Methodol. 2019;19(1):230. doi: https://doi.org/10.1186/s12874-019-0868-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article contains supplemental material.