1. Introduction
Approximately 12% of toddlers (i.e., age 3 and younger) in the United States have developmental delays, but up to 90% are not identified at the youngest ages possible (American Academy of Pediatrics, 2018; Rosenberg et al., 2013). Early identification of toddlers who do not meet key developmental milestones is critical to increase early intervention (EI) service use, and maximize functional outcomes (Adams & Tapia, 2013; American Academy of Pediatrics, 2006). Untreated developmental delays can contribute to early school failure and social and emotional problems (American Academy of Pediatrics, 2006). Efforts to improve early identification of developmental delays have primarily focused on pediatricians (Ertem et al., 2009), including the recommendation that pediatricians routinely elicit parental concerns regarding their child’s development (American Academy of Pediatrics, 2001). Although nearly half of parents have concerns about their child’s development, few parents report their pediatrician elicits their concerns (Adams & Tapia, 2013; Marshall et al., 2015; Woolfenden et al., 2015). Furthermore, studies documented parents are unaware of standard developmental milestones, and often lack the language or empowerment to share concerns about their toddlers’ development with their pediatrician (Adams & Tapia, 2013; Woolfenden et al., 2015).
Racial, ethnic (Valicenti-McDermott et al., 2012), and socio-economic (Fountain et al., 2011; Mazurek et al., 2014; Wittke & Spaulding, 2018) disparities exist in screening and identification of delays, access to care, and participation in EI (Zuckerman et al., 2014). Despite similar developmental delay prevalence (Boyle et al., 2011), African American/Black (Black) children are five times less likely to participate in EI services compared to white children at 24 months (Feinberg et al., 2011). Black parents are also more likely than white parents to report unmet therapy needs (Magnusson & Mistry, 2017). In a study about therapy services for developmental delays, low-income Black mothers reported few meaningful conversations with their child’s pediatrician about developmental concerns or EI services (Magnusson & Mistry, 2017), suggesting a need to further understand differences between Black and white parents’ experience identifying a developmental delay and obtaining EI services.
Many systematic factors, often the result of explicit or implicit racial bias (Chapman et al., 2013; Hall et al., 2015), contribute to these disparities including differences in physician referrals, insurance coverage, trust in health care providers and the health care system, and ability to navigate the system (Rosenberg et al., 2008; Zuckerman et al., 2014). These factors are multifaceted, impact racial minority experience with healthcare in the United States, and may contribute to the development of cognitions and emotions that affect how parents understand developmental delays and navigate the EI evaluation and therapy system. For example, Black parents reported fewer concerns about children’s behavior prior to receiving an autism spectrum disorder (ASD) diagnosis, compared to white parents (Donohue et al., 2017).
Exploratory studies about parents’ experiences identifying a developmental delay or obtaining EI services have focused on knowledge of delays (Magnusson & Mistry, 2017; Marshall et al., 2016), or systemic barriers and facilitators (Marshall et al., 2017). However, it is well know that information deficit models do not fully capture processes which influence health behavior (Grimshaw et al., 2001; Marteau et al., 2002) compared with behavioral theory (Glanz & Bishop, 2010). Yet, few leveraged behavior change theories to understand parents’ cognitions and internal processes. Many health behavior models like the Health Belief Model or Theory of Planned Behavior view individuals as rational decision makers, neglect dynamic processes, and fail to provide conceptual explanations for behavior (Cameron & Leventhal, 2003; Leventhal et al., 1980). Theories like the Common Sense Model (CSM), which focus on cognitive and emotional models associated with uptake and adherence to behavior change (e.g., EI uptake) can provide additional insight and a more complete explanation of the cognitive processes underlying parental identification of a developmental delay and EI uptake.
1.2. The Common Sense Model
The CSM is a widely used health behavior theory that provides a framework for a sense-making process whereby an individual perceives and evaluates a health threat and selects a response (Hagger et al., 2017; Leventhal et al., 1980; Leventhal et al., 1984). Specifically, the health threat or stimuli (e.g., information or symptoms) generate a threat schema (i.e., mental model) based on cognitions and emotions, which an individual uses to inform coping strategy selection to manage the threat (Leventhal et al., 1992). Both internal (e.g., somatic changes) and external (e.g., comments from others) stimuli serve as cues to a potential health threat, which initiates parallel but interconnected cognitive and emotional processes and generates representations that drive coping strategies and appraisals to monitor coping strategy effectiveness (Diefenbach & Leventhal, 1996; Hale et al., 2007; Leventhal et al., 1992). Past and present informational inputs from the environment, social structures, or experiences influence mental model development and coping strategy selection.
Cognitive representations are comprised of five domains: 1) identity – the label or description of the condition; 2) timeline – whether the condition is acute or chronic; 3) cause – the instigator of the condition (e.g., genetics, contagion, injury); 4) the potential to control or cure the condition; and 5) consequence – the emotional, social, financial impact (Diefenbach & Leventhal, 1996; Leventhal et al., 1992; Leventhal et al., 1980). Although important to the model, the emotional process of the CSM has received less attention, but includes emotions like fear, worry, and anxiety, and others known to motivate behavior (Cameron & Jago, 2008). Cognitive and emotional representation are thus believed to be significant determinants of health-related behaviors and adherence (Diefenbach & Leventhal, 1996).
Though initially applied to individual beliefs about one’s own illness, the CSM has been used to understand parents’ cognitive and emotional representations of children’s health conditions and pediatric healthcare use (Moran & O’Hara, 2006), including how parents of children with Attention Deficit Hyperactivity Disorder conceptualize and cope with their child’s condition (Wong et al., 2018). However, little is known about how parents of toddlers with developmental delays conceptualize their toddler’s condition. Furthermore, little is known about differences between Black and white parents’ CSM in this context. Given late identification and underutilization of EI services, particularly among Black parents, it is crucial to identify processes that may support parents in the identification of delays and EI service uptake.
The CSM is traditionally used to predict how threat schemas foretell coping. However, over the last few years, Leventhal and colleagues called for a focus on the dynamic processes that underlie action within the CSM (Leventhal, 2019; Leventhal et al., 2016). Leventhal and colleagues (2016) suggest, for example, mechanisms that affect self-efficacy, “a well-known predictor of self-management,” may be an appropriate target. To address these calls, research recently has begun to focus on understanding how representations are formed, and the processes that underlie mental models, as doing so will help to inform future research and intervention development (Leventhal, 2019). For example, scholars noted a lack of focus on social processes (DeLongis & Morstead, 2019), despite the importance of social contextual factors (e.g., culture, media influences, conversations with family/friends) in generating the stimuli and mental model (Leventhal et al., 2016). The current study contributes to this new wave of research by using qualitative methods to identify potential mechanistic targets and explore processes that influence parents’ identification of developmental delays and EI service uptake.
Research employing the CSM has largely capitalized on the availability of validated quantitative measures including the Illness Perception Questionnaire (Weinman et al., 1996), the Revised Illness Questionnaire (Moss-Morris et al., 2002), and the Brief Illness Questionnaire (Broadbent et al., 2006). While useful, such methods may oversimplify the processes within the CSM and obfuscate new ways of theorizing (Revenson & Diefenbach, 2019). In particular, methods that allow for greater understanding of emotional content can provide insight to the influence of emotion and the interactions between cognitive and emotional representations (Revenson & Diefenbach, 2019). A qualitative descriptive approach using the CSM to guide the exploration of participants’ narratives may identify additional processes worthy of further investigation (Sandelowski, 2000; Thorne et al., 1997). Consistent with the cognitive models that underpin the CSM, personal narratives, like those elicited through qualitative methods, integrate past and present experiences and perceptions to create the epistemological frameworks and structures from which an individual makes sense of the world (Petraglia, 2007).
Utilizing the CSM as a framework, this qualitative study explored the cognitive and emotional representations of Black and white parents of toddlers with developmental delays who received EI services. The goals of this study were to identify the framework used by parents to engage with EI services, explore differences between Black and white parents’ frameworks, and identify any underlying processes that may prove fruitful for future CSM research. We intentionally explored exceptional cases, which is to say, parents who obtained EI services. By understanding more about exceptional cases, or those who adopt the desired health behavior, we may be better able to predict the processes and inputs required to achieve outcomes of behavior change and adherence (Leventhal et al., 2016).
2. Methods
2.1. Study design and sample
Following IRB approval at our University, twenty semi-structured in-depth individual interviews were conducted between July 2017 and January 2018. We used a non-probability based purposeful sampling strategy (Patton, 2015) to recruit 50% Black and 50% white participants through our institution’s Early Intervention Research Group (EIRG) registry, posts on the EIRG’s website and social media pages, and flyers distributed to existing network of patients and clinical partners (e.g., pediatric offices, therapy providers, and daycare centers).
2.2. Procedure
Parents had the option to join the EIRG Research Registry or contact the study team via email or phone. Potential participants received an introductory letter with information about the study and, if interested, a screening survey to assess eligibility administered via Research Electronic Data Capture (REDCap; Vanderbilt University). Eligibility criteria for this study included parents: 18 years or older; English-speaking; self-identified as Black or white, non-Hispanic; had a toddler identified with a developmental delay between 18 and 35 months; and were referred to and received, or were receiving, EI services (Table 1).
Table 1.
Parent Sample Characteristics, by Race
| Characteristics | Total (N = 20) | Black (n =10) | white (n = 10) | |||
|---|---|---|---|---|---|---|
| Parent Age M, [SD] | 35.9 | [5.6] | 35.8 | [5.9] | 36.1 | [5.5] |
| Parent Sex | ||||||
| Female | 20 | (100) | 10 | (100) | 10 | (100) |
| Education | ||||||
| < High School | 1 | (5) | 1 | (10) | 0 | (0) |
| High School Graduate | 2 | (10) | 1 | (10) | 1 | (10) |
| Some College (or certificate) | 3 | (15) | 3 | (30) | 0 | (0) |
| College Graduate | 10 | (50) | 5 | (50) | 5 | (50) |
| Post-graduate (MA/S, PhD, MD) | 4 | (20) | 0 | (0) | 4 | (40) |
| Income | ||||||
| < $45,000 | 5 | (25) | 4 | (40) | 1 | (10) |
| $45,000–$89,000 | 4 | (20) | 2 | (20) | 2 | (20) |
| > $90,000 | 10 | (50) | 3 | (30) | 7 | (70) |
| Prefer not to answer | 1 | (5) | 1 | (10) | 0 | (0) |
| Employment Status | ||||||
| Full-time | 8 | (40) | 4 | (40) | 4 | (40) |
| Part-time | 2 | (10) | 0 | (0) | 2 | (20) |
| Homemaker | 7 | (35) | 3 | (30) | 4 | (40) |
| Unemployed | 3 | (15) | 3 | (30) | 0 | (0) |
| Health Insurance Status | ||||||
| Private through workplace | 15 | (75) | 5 | (50) | 10 | (100) |
| Medicare/Medicaid | 5 | (25) | 5 | (50) | 0 | (0) |
| Relationship Status | ||||||
| Married/Domestic Partner/Civil Union | 13 | (65) | 3 | (30) | 10 | (100) |
| Single | 6 | (30) | 6 | (60) | 0 | (0) |
| Living with Partner | 1 | (5) | 1 | (10) | 0 | (0) |
Note. Unless otherwise noted, variables are presented as n (%).
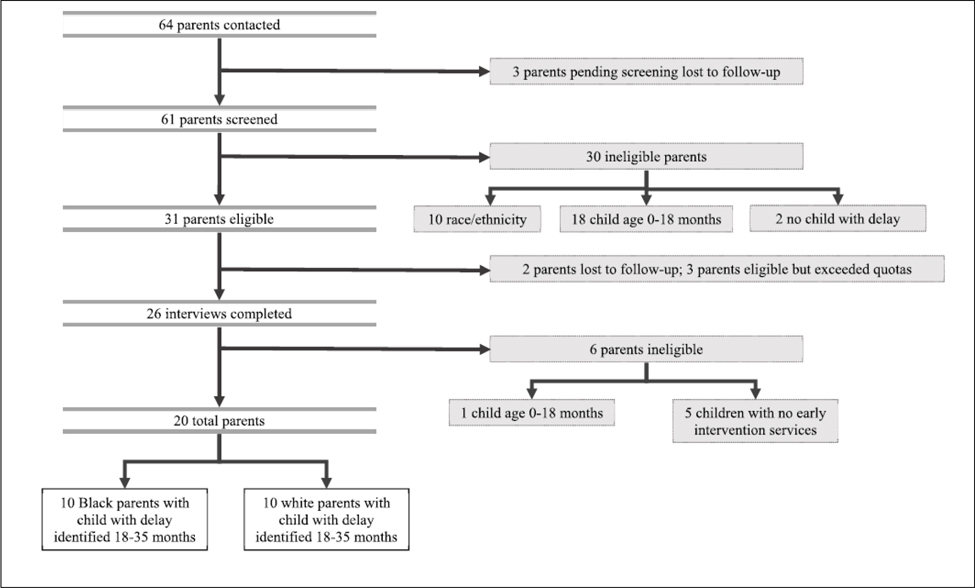
Sixty-one (95%) parents were initially screened for eligibility. Of the 31 (51%) who met eligibility criteria, two were lost to follow-up, and three were eligible after thematic saturation was achieved and quotas for race were met, and therefore did not participate. Twenty-six participants completed interviews: five who did not receive EI services were excluded from this study, and one was deemed ineligible after the interview was complete, which resulted in a final sample of 20 participants (see Figure 1).
Fig. 1.
Recruitment Process. This figure illustrates the recruitment process in this study.
One of three study team members trained in qualitative methods conducted the interviews, with at least one note taker present. The interviewer obtained verbal informed consent prior to each interview. Interviews lasted on average 50 minutes (range 31–72 minutes), were digitally recorded, professionally transcribed, and reviewed by study team members for accuracy and to ensure all names were replaced with pseudonyms. The principle investigator reviewed interviewer notes and transcripts to determine when thematic saturation was achieved. Participants received a $100 gift card in compensation for their time.
2.3. Data collection
The semi-structured interview guide was grounded in the CSM and included questions about parents’ experiences identifying the delay (e.g., When did you first notice something was different about your child’s development?), interaction with their toddler’s pediatrician (e.g., Can you please tell me what happened when you spoke with your child’s doctor?), receiving a referral to intervention services and obtaining and/or completing therapy (e.g., Can you tell me about the referral process to EI therapy services?), beliefs about the cause of the delay (e.g., What do you think caused your child to develop this condition?), emotions and support during the process (e.g., How did learning about your child’s developmental delay make you feel?), expectations for their toddler’s future (e.g., What does this diagnosis mean for your child?), and satisfaction with the referral, evaluation, and therapy process (e.g., How did you feel about the entire process from your first inclination that something was different in your child’s development to where you are today?). Sociodemographic information about parents and their toddlers was captured at the end of the interview.
2.4. Data analysis
Coded transcripts were entered into MAXQDA version 12 (VERBI GmbH Software, Berlin, Germany) for analysis and data management. Descriptive statistics were conducted for sociodemographic data collected during the interview using SPSS 25 (Table 1; IBM Corp., Armonk, New York).
A directed content analytic approach was implemented, as the goal was to examine emergent themes from within the domains and structure of the CSM to further explore and understand the framework itself (Hsieh & Shannon, 2005). Consistent with this approach, three study team members identified key concepts or variables as initial coding categories using the CSM to facilitate the development of operational definitions. Guided by the CSM framework, the initial seven categories included: 1) the stimulus, which triggered parent awareness that something was different about their child’s development, 2) identity, 3) timeline, 4) cause, 5) the potential to control or cure the condition, 6) consequence, and 7) emotional representations (Cameron & Jago, 2008; Diefenbach & Leventhal, 1996; Leventhal et al., 1992; Leventhal et al., 1980). Three study team members independently applied the codes to the transcripts and used a consensus based approach to coding all transcripts, whereby they met to discuss every two transcripts to resolve discrepancies and refine the coding scheme. During this process, pediatrician response to parental concerns was identified as an important theme that could not be coded into the initial categories and was subsequently added to the coding scheme.
3. Results
3.1. Sample characteristics
Sample characteristics for parents are summarized in Table 1. Sample characteristics about their children are summarized in Table 2.
Table 2.
Child Characteristics and Type of Developmental Delay, by Race
| Characteristics | Total (N= 20) | Blacka (n = 40) | whitea (n = 10) | |||
|---|---|---|---|---|---|---|
| Number of Children M, [SD] | 2 | [0.9] | 2 | [11] | 2 | [0.7] |
| 1 | 6 | (30) | 4 | (40) | 2 | (20) |
| 2 | 9 | (45) | 3 | (30) | 6 | (60) |
| 3 | 4 | (20) | 2 | (20) | 2 | (20) |
| 4 | 1 | (5) | 1 | (10) | 0 | (0) |
| Number of Children Identified with a Developmental Delayb | ||||||
| 1 | 16 | (80) | 8 | (80) | 8 | (80) |
| 2 | 3 | (15) | 2 | (20) | 1 | (10) |
| 3 | 1 | (5) | 0 | (0) | 1 | (10) |
| Birth Order of Child with Developmental Delay | ||||||
| First | 15 | (75) | 7 | (70) | 8 | (80) |
| Second | 3 | (15) | 2 | (20) | 1 | (10) |
| Third | 2 | (10) | 1 | (10) | 1 | (10) |
| Type of Delayc,d | ||||||
| Speech and Language | 20 | (100) | 10 | (100) | 10 | (100) |
| Occupational | 15 | (75) | 9 | (90) | 6 | (60) |
| Physical | 2 | (10) | 1 | (10) | 1 | (10) |
| Developmental | 11 | (55) | 6 | (60) | 5 | (50) |
| Autism Spectrum Disorder (ASD) Diagnosise | ||||||
| Yes | 7 | (35) | 5 | (50) | 2 | (20) |
| No or Unknown | 13 | (65) | 5 | (50) | 8 | (80) |
| Child Sex | ||||||
| Male | 14 | (70) | 7 | (70) | 7 | (70) |
| Female | 6 | (30) | 3 | (30) | 3 | (30) |
| Ag Child Identified in Months M, [SD] | 21.5 | [3.9] | 22.3 | [4.3] | 20.8 | [3.6] |
| Time since Identified in Months M, [SD]f | 35.3 | [53.9] | 49.2 | [74.7] | 21.5 | [116] |
Note. Unless otherwise noted, variables are presented as n (%).
Race is based on parent racial identity.
Parents were asked to think about and discuss the first child identified with a developmental delay. In this sample, one parent had twins identified at the same time.
Children could be identified with more than one delay.
Type of delay includes both the developmental delay a child was identified with as well as the therapies a child received. Parents were asked the name of the diagnosis or delay their child was identified with and some responded with the type of therapies the child received instead.
Parents were not asked explicitly about Autism Spectrum Disorder, however some parents stated their child was diagnosed after receiving an Early Intervention evaluation and/or completing Early Intervention therapy.
Number of months since child identified with developmental delay at time of interview.
3.2. Qualitative themes based on CSM domains
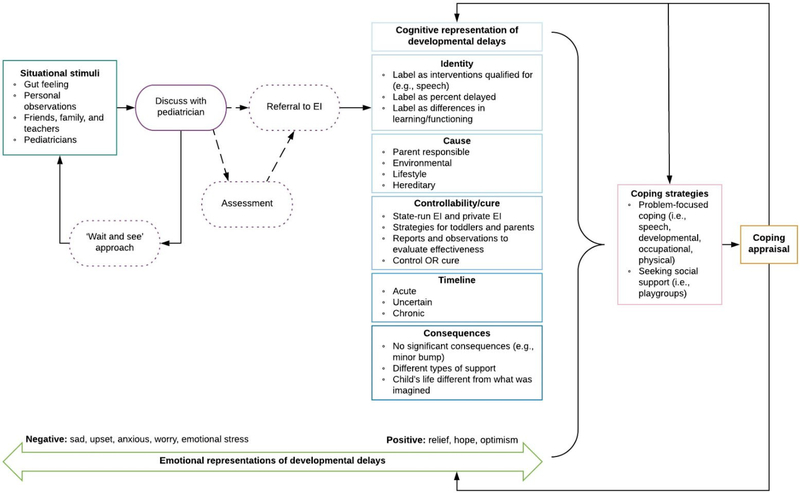
We initially sought to identify differences between Black and white parents, however, few emerged. The term parents refers to both Black and white parents. Race is only explicitly included in the description when differences were identified. Exemplar quotes include parenthetical information about parents’ race (i.e., BP = Black parent; WP = white parent), but should not be interpreted as a belief from one group and not the other, unless explicitly mentioned in the text. We intentionally use the term delay, instead of diagnosis. We recognize that clinical diagnosis is used by a pediatrician when a delay is documented. However, parents understood the process the identification of a delay (not diagnosis) first, until a more specific medical diagnosis (e.g., ASD) is provided, if ever. We present the themes from the qualitative analysis below and in the framework depicted in Figure 2.
Fig. 2.
Parents’ Common Sense Representations of Developmental Delays Model. This figure models pathways and processes associated with identifying a toddler and receiving early intervention. The solid lines in this figure indicate parent decision or action.
Dotted lines indicate pediatrician decision or action. Boxes represents CSM constructs. Ovals represents action based on pediatrician’s response.
Situational stimuli
Situational stimuli was defined as parents’ description of signs and/or symptoms indicating something was different about their toddler’s development. In most interviews (n = 16), parents were the first to notice. In the remaining four cases, all of which were Black parents, the pediatrician was the first to raise concerns about the toddler’s development. Parents’ whose pediatrician raised concerns engaged in retrospective sense-making when asked to describe what they noticed was different about their toddler’s development. They often described milestones their toddler had not achieved. For parents who noticed a difference in their toddlers’ development before the pediatrician, three sources alerted them: a gut feeling, personal observations, and concerns voiced by family members, friends and/or teachers.
First, parents reported a gut feeling or just knowing something was different. In many cases, parents observed unusual or atypical behavior in their toddler over time, but were uncertain if the behavior was something to be concerned about. “Something is going on with this boy. I said, okay, it just kept happening and happening and happening…I just figured something wasn’t right...I just couldn’t put my finger on it. You know?” (BP03). Parents described how their toddler experienced frequent tantrums, frustration, and agitation. Parents also noted changes in behavior or developmental regression. Speech delays seemed easiest for parents to identify and label, but parents’ lacked language to describe or label what was happening for cognitive, adaptive, or fine or gross motor delays beyond a feeling. “There was nothing specific…she just didn’t seem as engaged. She was very alert and observant, but not as engaged as I thought she maybe could’ve been” (WP08).
Second, parents observed their toddlers’ failure to meet specific milestones. Some identified differences in their toddlers’ development by comparing observations of their toddler’s behavior with that of a sibling or other toddlers: “When we first started seeing it for ourselves, he wasn’t making more sounds as other children have made” (WP09). Others observed their toddlers’ failure to meet milestones based on a checklist from their pediatrician or information on parenting websites.
Lastly, observations and feedback from family, friends, or teachers alerted parents to a problem, or supported their concerns regarding their toddlers’ development. However, some described how family, friends, and teachers minimized their concerns. In these cases, parents reported reappraising the situation and continued to monitor their toddler’s development. Teachers would say, ‘Oh, he’s okay. Things are harder for him but it could just be because he’s a boy.’ I think that those comments from other people caused my husband and I to wait even longer before we pursued the early intervention because we thought, okay, maybe people are right. (WP05)
“Boys develop slower” than girls was often used as a rationale by family, friends, teachers, and even pediatricians as a reason to not worry or, ‘wait-and-see.’
Pediatrician response to parental concerns
When parents discussed concerns with their pediatrician, two overarching responses emerged: the pediatrician would provide an EI referral, or suggest a ‘wait-and-see’ approach. Pediatricians who supported or shared parents’ concerns would conduct a clinical evaluation, which led to EI referral, or would simply provide a referral.
She sat down and she talked to him a little bit and I said, ‘Oh, what about the speech?’ And she said, ‘Yeah, I would call about the speech. He seems to not be where we want him to be right now.’ (WP05)
Just under half (n = 7) reported their pediatrician encouraged a ‘wait-and-see’ approach. Pediatricians often normalized different rates of development in the discussion. “Every time I brought it up to my pediatrician, my pediatrician did not think it was an issue. Every time they said, ‘kids develop differently, some have more than others, give it time’” (WP04). When parents were told by the pediatrician to wait, some re-evaluated their concerns, “I’d leave [the pediatrician’s office], and I’d feel better” (WP10). Others felt dismissed or unheard, particularly if they discussed their concerns more than once. In cases when parents brought up their concerns at multiple appointments, most pediatricians would re-evaluate and agree with the parent or acquiesce to their request and provide a referral. One white parent realized she did not need her pediatrician’s referral and called EI directly.
Parents’ cognitive representation of the developmental delay
Identity –
Identity refers to how parents labeled, named, or described their toddler’s developmental delay. When asked what their toddler was diagnosed with, parents clarified that EI does not provide a medical diagnosis; they only provide information about developmental delays. In this study, seven toddlers (five Black and two white) went on to receive an ASD diagnosis. Parents described their toddlers’ initial evaluation as providing information about the type of delay they had, often labeling the delay as the intervention they qualified for, for example, “speech,” “occupational” or “developmental.” Parents described each delay in more detail. Speech delays were described as lacking language or having challenges with expressive language, occupational delays as challenges with sensory or fine or gross motor skills, and developmental delays as not being able to do the things most toddlers can do at that age. Some parents, mostly white parents, described the percentage delay their toddler was diagnosed with: “she was delayed, I want to say 30 or 40%” (WP03). Learning about the delay often gave parents insight into their toddlers’ other behaviors, like frustration, agitation, tantrums, or acting out.
Differences in learning or functioning were also described. Parents emphasized their toddler was not diminished in learning or ability, and often described the delay as a challenge or struggle to overcome when learning new things. “So he’s capable of learning things, and I think he is very intelligent, it’s just a struggle for him to get through that initial phase of learning something” (WP02). Parents whose toddler did not have an ASD diagnosis at the time of the interview (n = 13) were more likely to describe the delay as a “little delay” or explain that their toddler “needs a little help” to learn.
Interestingly, some shared their original perception of what a developmental delay meant before they obtained services, which often was illustrative of severe cases of ASD or even Downs Syndrome. Prior to their exposure to EI services, parents were unaware developmental delays could range from mild to severe, and that some delays could be overcome through therapy.
Cause –
Cause refers to parents’ perceptions of what was responsible for their toddler’s delay. Many parents reported feeling responsible and questioned whether they could have caused or prevented the delay. Some parents stated they just did not know, “there is no answer to that question” (WP12). Many parents speculated the causes could be environmental, lifestyle, hereditary, or something kids are “just born with.” Possible environmental causes included prenatal exposures, preterm delivery or other complications at birth, instability in their home environment, and vaccines. “I’m like, was it the shot [MMR]? Or was it... the [cleaning] chemicals that I was spraying?” (BP03). Of those who shared the belief vaccines may have caused the delay, three Black parents had a toddler diagnosed with ASD, and one white parent had a toddler who had not received an ASD diagnosis. Parents also described lifestyle factors including not paying enough attention to the toddler or not encouraging their toddler to speak. We put a lot of attention on her. Without her even saying anything, we knew it, like, ‘Do you want this?’ We often times didn’t let her speak, not didn’t let her speak, but anticipated her needs before she even had to speak (BP10).
Parents who could identify family members with similar delays were confident in their belief about a hereditary cause for the delay. “I think it was the dad. I really believe it’s something in his gene pool” (BP09). Aside from parents who believed the delay was hereditary, most parents responded with more than one possible cause, indicating ongoing uncertainty.
Controllability/cure –
Controllability or cure refers to the types of interventions the toddler received, the outcomes of the intervention, and the timeline for receiving therapies. Parents described the therapies their toddler participated in through EI including speech, developmental, physical, and occupational. In addition to the state-run EI therapies, some parents sought out private and/or group therapy.
Parents described how therapy provided toddlers with different strategies, “She [therapist] gave him something to do with his hands, like a sign language thing cause he couldn’t talk” (BP03). Therapy also provided strategies for the parent to more effectively relate and interact with their toddler by providing structure or a framework for interactions. “Those sessions were incredibly helpful to us, and they were helpful for us to learn what we needed to do at home and how we needed to speak to her and play with her and work with her” (WP03). Many described working on therapy at home with their toddler by incorporating strategies they learned through EI, their playgroups, support networks, or other parents.
In most cases, parents felt therapies were helping their toddler and described improvements in their toddler’s behaviors. Some parents noticed changes in their toddler immediately, “Once she started early intervention, I would say like within a month. I’ve seen a drastic change. As far as...her speech and everything. She just really took off” (BP08). For others it took some time. Parents often described the progress reports shared by their therapists as a way to track their toddlers’ progress and as evidence therapy was helping. A couple of parents did not believe the therapies were having a noticeable impact on their toddler. “I really didn’t see a difference in anything. I feel like she’s progressing at the rate she would have probably progressed without the therapy” (BP07). Nevertheless, these parents continued with therapy.
When asked if they believed their toddler started intervention early enough, a dialectical tension was present. Most agreed their toddler started at the right time, but wished they had noticed the delay earlier, “I think it was about the right time. I wish … I still think I wished I would have done…you know, noticed he wasn’t speaking a little bit earlier. But I think it was an appropriate time” (BP10). Particularly after seeing the results, parents recognized the value in beginning therapy as early as possible.
Timeline –
Timeline, or parents’ beliefs about how long their toddler will have the delay, was either acute, uncertain, or chronic. Interestingly, there were no differences between parents with a toddler who was diagnosed with ASD and those whose toddler was not. Parents who believed the delay was acute explained that their toddler would age out of therapy or be “mainstreamed” in school, meaning their development was age-appropriate.
Other parents were uncertain about an expected timeline. Uncertainty often led to hope for improvement, however, expectations about the degree of improvement varied. For some, they hoped their toddler could be mainstreamed within a couple of years. “I hope he can outgrow it. I don’t know what to expect, actually. I like to have hope, though, that he can get better or outgrow it” (BP05).
Others believed the condition was chronic, or something their child would deal with for the rest of their life. In these cases, parents hoped their toddler could develop coping strategies. “Hopefully, he’ll find the ways to help himself to be in situations that make him uncomfortable or to increase his focus or whatever he needs moving forward. I definitely think it will be lifelong” (WP05).
Consequences –
Consequences refer to the physical, psychological, social, educational, or financial impact of the condition. A few parents, and in particular those who believed the delay was acute, described it as a “little minor bump” (WP03), with no significant consequences. However, most parents were speculative about expected outcomes. Most focused on the different types of support their toddler would need, “I just need to be more patient with them and understand that they develop at their own rate” (BP09). In a few cases, parents described how their expectations or aspirations for their child had changed. “For your child, you just have this perfect picture of how everything is going to go and then when things don’t go that way it’s hard to accept it and try something different” (BP08). A few parents described the cost of additional therapies and, sometimes, long term care. “We don’t really know where he’s going to be in five years… It means a lot of expensive bills, a lot of therapy, a lot of time” (WP12). Parents also explained how their concerns changed. “I was concerned about just him having relationships with his peers, but it’s gotten much better over the years” (BP10). When discussing the consequences of their toddlers’ delay, parents shared their goals and hopes for their toddler, despite uncertainty about their developmental trajectory.
Parents’ emotional representation of the developmental delay
Consistent with the parallel process in the CSM, parents’ emotional response unfolded with the process of identifying and confirming a delay, and entering therapy. When parents initially thought something was developmentally atypical for their toddler, many described feeling sad, upset, or emotional, especially if they were not expecting it. “I wasn’t upset. I was super emotional…it was like, just new to me that I had a child that was different” (BP02). Sometimes parents had difficulty accepting the delay, which caused emotional stress, especially when they believed they could have been the cause. Others viewed the identification of the delay as a positive or relief-inducing event. Many explained identifying the delay and having a plan helped them cope emotionally because they were able regain control when they previously felt out of control and were experiencing significant uncertainty, “I mean I don’t feel bad about the situation anymore, I feel very hopeful especially since he’s made progress, it’s been such a positive experience” (WP02).
4. Discussion
This qualitative study used the CSM to understand the process by which Black and white parents’ concerns about their toddler’s development led to EI service uptake. Few meaningful differences emerged between Black and white parents’ mental models. By exploring parents’ narratives, we identified additional nuance in the CSM’s theoretical domains and processes.
First, we present theoretical insights, and follow with practical implications.
4.1. Theoretical insights
Leventhal and colleagues encouraged additional work examining the processes underlying the CSM domains (Leventhal, 2019; Leventhal et al., 2016). In this study, we identified several potential underlying constructs, and provide new ways to theorize about the mutual influence of cognition and emotion.
Orbell and Phillips (2019) recently reviewed the potential contributions of automatic processes (i.e., heuristics) within the CSM. Experiences like gut feelings identified in this study are heuristics, made up of “hidden rules of thumb underlying intuition”(Gigerenzer, 2007). In addition to expanding existing work on heuristics, uncovering hidden operations in parent’s gut feelings may uncover new ways to identify developmental delays earlier. Furthermore, research utilizing the CSM consistently finds initial cognitive representations, often established via heuristic reasoning, are based on an acute illness prototype (Leventhal et al., 2016). The default to an acute model is especially likely in younger individuals with no previous health conditions (Leventhal, 2019), and may explain why family, friends, teachers, or pediatricians invalidate parents’ concerns or encourage a ‘wait-and-see’ approach in this study and others (Jimenez et al., 2012; Sices et al., 2009).
We identified interesting insights in the transition points in the model, for example, the transition from stimuli to representation. Consistent with predictions about the model (Leventhal et al., 1980; Leventhal et al., 1984), parents re-evaluated the stimuli when friends, family, teachers, and pediatricians minimized their concerns. In addition to the impact of social processes, Leventhal (2016) suggested additional dynamics, such as self-efficacy, may influence transitions in the CSM. In addition to self-efficacy, the persistence demonstrated by parents repeatedly raising their concerns suggests grit (Duckworth et al., 2007) could be a variable for consideration in future research.
Prior studies focused on the impact of representations on coping as the endpoint, but not on the evaluation of coping strategies (Benyamini & Karademas, 2019). The evaluation of coping strategies is directly related to adherence; therefore, this is a significant shortcoming. In this study, parents’ reflection on their toddlers’ development through goal setting and feedback reports provided by therapists played an important function in parents’ evaluation of the therapies success (coping). Future research should explore whether goal setting and tracking improvements over time by tying coping strategies (e.g., therapies) with outcomes (e.g., developmental milestones) can impact adherence in this context and others.
Most CSM studies have focused on cognitive pathways and neglected emotional representations (Revenson & Diefenbach, 2019). Infused throughout parents’ narratives was a theme of uncertainty and hope. Uncertainty has been defined as the “subjective perception of ignorance” (Han et al., 2011), which in this study resulted from ambiguity, or a lack of knowledge about the trajectory of their toddlers delay. Such ambiguity has recently been linked with the use of ambiguous terms, such as “delay” in the context of a developmental impairment (Grech, 2019). Parents describe what Han and colleagues (2011) refer to as scientific uncertainty about causal explanations or prognosis, and personal uncertainty about the consequences of the delay on their child’s welfare. Although uncertainty is frequently viewed as undesirable (Han et al., 2011), theorizing on uncertainty has encouraged views of uncertainty as an opportunity (Babrow & Kline, 2000). In particular, Brashers’ (2001) work on uncertainty management explicitly links uncertainty with hope—a link consistent with parents’ emotional and cognitive experiences in this study. In particular, uncertainty about the timeline and consequences contained frequent references to hope. As such, further study of the interactions between hope and uncertainty within the domains of the CSM may provide one avenue through which theoretical clarification regarding the relationship between cognitive and emotional representations can be expanded. The identification of cognitive domains that promote favorable coping with uncertainty compared with those that promote maladaptive coping could support recommendations for uncertainty management.
4.2. Practical implications
Examining parent’s mental models highlights several practical implications for healthcare providers including reconsidering the ‘wait-and-see’ approach, and how to talk with parents. In this sample, all except four Black parents were the first to identify their toddler’s delay. Consistent with findings from earlier studies (Marshall et al., 2017; Marshall et al., 2016) parents in this study were are alerted to problems through a combination of observations of their toddler compared with others and developmental milestones, and others’ appraisals of their toddler’s development. Unique to this study, parents described a gut feeling or just knowing something was different. Aside from speech delays, parents had difficulty verbalizing their concerns, which means physicians need to be aware additional probing may be necessary. It may be useful for pediatricians to encourage parents to use validated developmental screening tools, such as the Centers for Disease Control and Prevention’s “Learn the Signs. Act Early” materials or mobile phone application.
Once parents raised their concerns with their pediatrician, many were encouraged to ‘wait-and-see.’ However, parents in this study reported having observed their toddler for some time before discussing it with their pediatrician. Early identification and treatment is critical to maximizing outcomes (Adams & Tapia, 2013; American Academy of Pediatrics, 2006), and state-funded EI services are only available to children under age three. Therefore, the ‘wait-and-see’ approach should be carefully considered. Although parents can call EI directly, parents in this study perceived the pediatrician as a gatekeeper to services (Sices et al., 2009). Asking the parent how long they have had the concern and who else they have discussed their concerns with may elicit additional information that could inform whether a ‘wait-and-see’ approach or referral is more appropriate.
Better understanding the mental frameworks of parents’ who successfully enrolled in EI services may provide guidance for how to talk with parents referred to EI services. For example, once toddlers were enrolled in EI services, parents articulated the delay as the type of services they received and often described the delay in terms of a difference in learning or needing extra support. Healthcare providers may consider adopting parents’ language.
Guilt may be felt prior to or while obtaining EI services. Parents were uncertain about the cause, and unique to our study, uncertainty was linked to feeling guilt they might have done something to cause the delay. On the other hand, some parents described feeling guilty when receiving EI therapy, upon learning how their interactions facilitate or impede development. Pediatricians should be aware of this guilt as it may prevent parents from raising concerns, and may explain why parents do not pursue EI services when recommended. Describing therapies as supporting parents’ interactions with their toddler and giving their toddler tools to cope may alleviate parents’ guilt and uncertainty about what to expect from EI. Therapists may want to reassure, encourage and support parents as they process these feelings.
Parents who were uncertain about how long the delay would last, or believed it was a chronic condition described re-evaluating their expectations for their child. Uncertainty was infused throughout discussions of timelines and consequences, and was connected with hope. Parents sometimes described the initial identification of a delay as a negative emotional experience, but parents quickly re-evaluated the situation and focused on a plan to help their toddler. Realignment from emotion focused coping (i.e., regulating negative emotions) to problem focused coping (i.e., managing the health threat) is a hallmark of functional coping, and as we saw in this study, promoted uptake and adherence to recommended behaviors (Cameron & Jago, 2008). Providers may want to emphasize how entering toddlers into therapy can help parents manage uncertainty, gain a sense of control and cope with the delay. Parents who continue to engage in emotion focused coping (e.g., denial, avoidance) may need referral to counseling services.
4.3. Limitations
All participants in this study received EI intervention services, therefore limited claims can be made regarding the impact of CSM dimensions on coping strategy selection. All participants were drawn from a large metropolitan area and surrounding suburbs, and the relative socioeconomic status of this sample is high compared to the general population. Those of lower socioeconomic status are more reluctant to discuss concerns about their toddler’s developmental delay with their pediatrician (Marshall et al., 2016). Black parents in this sample had lower educational attainment and lower income compared with white parents. This difference was not intentional, but should be noted. A prior study found an interaction between race and SES to impact children’s health outcomes (Chen et al., 2006). Although not the focus of this study, future studies should examine the potential interaction between race and socioeconomic status in the identification of developmental delays. Finally, as parents were recalling their experience obtaining EI services, recall bias may influence their description.
5. Conclusion
Early identification of developmental delays during toddlerhood, and timely intervention is essential to improve functional outcomes and reduce need for long-term treatment and the associated long-term costs (Adams & Tapia, 2013). This study provides several directions for future research using the CSM. First, additional explorations of key transitions between stimuli and cognitive and emotional representations and between behavior and adherence are needed. This study suggests that examining state and trait influences, like self-efficacy and grit, may help identify those more likely to adapt and adhere to coping strategies. Furthermore, messages that emphasize goal setting and link coping with outcomes may provide feedback, which facilitates coping strategy evaluations and promotes adherence. Finally, future research should consider contributions of existing theories on uncertainty to explain the link between cognition and emotion and their impact on adherence.
Future studies should examine links between CSM constructs identified in this study, parents’ sharing of concerns with their pediatrician, and EI service uptake. Additional research should examine the CSM of parents of children who were identified with a developmental delay at an older age to learn more about their cognitive and emotional representations, and to identify differences compared to those who received EI services. Differences in parents’ cognitions and emotions who obtain EI services and those who do not will provide insight to promote parental identification of delays, parent-provider discussions, and ultimately, EI service uptake.
Acknowledgement:
This study was supported by a grant from the Delaney Family Foundation.
References
- Adams RC, & Tapia C (2013). Early Intervention, IDEA Part C Services, and the medical home: Collaboration for best practice and best outcomes. Pediatrics, 132, e1073–e1088. 10.1542/peds.2013-2305 [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics (2001). Developmental surveillance and screening of infants and young children. Pediatrics, 108, 192–195. 10.1542/peds.108.1.192 [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics (2006). Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics, 118, 405–420. 10.1542/peds.2006-1231 [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. (2018). Ages & Stages. [Google Scholar]
- Babrow AS, & Kline KN (2000). From “reducing” to “coping with” uncertainty: Reconceptualizing the central challenge in breast self-exams. Soc Sci Med, 51, 1805. 10.1016/S0277-9536(00)00112-X [DOI] [PubMed] [Google Scholar]
- Benyamini Y, & Karademas EC (2019). Introduction to the special issue on the common sense model of self-regulation. Health Psychol Rev, 1–5. 10.1080/17437199.2019.1644189 [DOI] [PubMed] [Google Scholar]
- Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. (2011). Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics, 127, 1034–1042. 10.1542/peds.2010-2989d [DOI] [PubMed] [Google Scholar]
- Brashers DE (2001). Communication and uncertainty management. Communication and uncertainty management, 51, 477–497. 10.1111/j.1460-2466.2001.tb02892.x [DOI] [Google Scholar]
- Broadbent E, Petrie KJ, Main J, & Weinman J (2006). The brief illness perception questionnaire. J Psychosom Res, 60, 631–637. 10.1016/s1836-9553(12)70116-9 [DOI] [PubMed] [Google Scholar]
- Cameron LD, & Jago L (2008). Emotion regulation interventions: A common-sense model approach. Br J Health Psychol, 13, 215–221.10.1348135910708x288800 [DOI] [PubMed] [Google Scholar]
- Cameron LD, & Leventhal H (2003). Self-regulation, health, and illness: An overivew. In Cameron LD, & Leventhal H (Eds.), The self-regulation of health and illness behavior pp. 1–13). New York, NY: Routledge. [Google Scholar]
- Chapman EN, Kaatz A, & Carnes M (2013). Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. J Gen Intern Med, 28, 1504–1510. 10.1007/s11606-013-2441-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Martin AD, & Matthews K.A.J.A.J.o.P.H. (2006). Understanding health disparities: The role of race and socioeconomic status in children’s health. Am J Public Health, 96, 702–708. 10.2105/ajph.2004.048124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLongis A, & Morstead T (2019). Bringing the social context into research using the common sense model. Health Psychol Rev, 13, 481–483. 10.1080/17437199.2019.1652107 [DOI] [PubMed] [Google Scholar]
- Diefenbach MA, & Leventhal H (1996). The common-sense model of illness representation: Theoretical and practical considerations. J Soc Distress Homeless, 5, 11–38. 10.1007/BF02090456 [DOI] [Google Scholar]
- Donohue MR, Childs AW, Richards M, & Robins DL (2017). Race influences parent report of concerns about symptoms of autism spectrum disorder. Autism, 1362361317722030. 10.1177/1362361317722030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duckworth AL, Peterson C, Matthews MD, & Kelly DR (2007). Grit: Perseverance and passion for long-term goals. J Pers Soc Psychol, 92, 1087. 10.1037/0022-3514.92.6.1087 [DOI] [PubMed] [Google Scholar]
- Ertem IO, Pekcici EBB, Gok CG, Ozbas S, Ozcebe H, & Beyazova U (2009). Addressing early childhood development in primary health care: Experience from a middle-income country. J Dev Behav Pediatr, 30, 319–326. 10.1097/dbp.0b013e3181b0f035 [DOI] [PubMed] [Google Scholar]
- Feinberg E, Silverstein M, Donahue S, & Bliss R (2011). The impact of race on participation in Part C early intervention services. J Dev Behav Pediatr, 32, 284. 10.1097/dbp.0b013e3182142fbd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountain C, King MD, & Bearman PS (2011). Age of diagnosis for autism: Individual and community factors across 10 birth cohorts. J Epidemiol Community Health, 65, 503. 10.1136/jech.2009.104588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gigerenzer G (2007). Gut feelings: The intelligence of the unconscious: Penguin. [Google Scholar]
- Glanz K, & Bishop DB (2010). The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health, 31, 399–418. 10.1146/annurev.publhealth.012809.103604 [DOI] [PubMed] [Google Scholar]
- Grech LB (2019). Developmental delay: An ambiguous term in need of change. Arch Disease Child. 10.1136/archdischild-2019-317522 [DOI] [PubMed] [Google Scholar]
- Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, et al. (2001). Changing provider behavior: An overview of systematic reviews of interventions. Med Care, II2–II45. 10.1097/00005650-200108002-00002 [DOI] [PubMed] [Google Scholar]
- Hagger MS, Koch S, Chatzisarantis NLD, & Orbell S (2017). The common sense model of self-regulation: Meta-analysis and test of a process model. Psychol Bull, 143, 1117–1154. 10.1037/bul0000118 [DOI] [PubMed] [Google Scholar]
- Hale ED, Treharne G, & Kitas G (2007). The Common-Sense Model of self-regulation of health and illness: How can we use it to understand and respond to our patients’ needs? Rheumatology, 46, 904–906. 10.1093/rheumatology/kem060 [DOI] [PubMed] [Google Scholar]
- Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. Am J Public Health, 105, e60–e76. 10.2105/ajph.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Klein WMP, & Arora NK (2011). Varieties of uncertainty in health care: A conceptual taxonomy. Med Decis Making, 31, 828–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh H-F, & Shannon SE (2005). Three approaches to qualitative content analysis. Qual Health Res, 15, 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Jimenez ME, Barg FK, Guevara JP, Gerdes M, & Fiks AG (2012). Barriers to evaluation for early intervention services: Parent and early intervention employee perspectives. Acad Pediatr, 12, 551–557. 10.1016/j.acap.2012.08.006 [DOI] [PubMed] [Google Scholar]
- Leventhal H (2019). Next Steps for examining the common-sense of health behaviour. Health Psychol Rev, 13, 487–489. 10.1080/17437199.2019.1642791 [DOI] [PubMed] [Google Scholar]
- Leventhal H, Diefenbach M, & Leventhal EA (1992). Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cognit Ther Res, 16, 143–163. 10.1007/bf01173486 [DOI] [Google Scholar]
- Leventhal H, Meyer D, & Nerenz D (1980). The common sense representation of illness danger. In Rachman S (Ed.), Contributions to Medical Psychology pp. 7–30). New York: Pergamon Press. [Google Scholar]
- Leventhal H, Nerenz D, R., & Steele, D.J. (1984). Illnes representations and coping with health threats. In Baum A, & Singer J (Eds.), A Handbook of Psychology and Health pp. 219–252). Hillsdale, NJ: Earlbaum. [Google Scholar]
- Leventhal H, Phillips LA, & Burns E (2016). The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J Behav Med, 39, 935–946. 10.1007/s10865-016-9782-2 [DOI] [PubMed] [Google Scholar]
- Magnusson DM, & Mistry KB (2017). Racial and ethnic disparities in unmet need for pediatric therapy services: The role of family-centered care. Acad Pediatr, 17, 27–33. 10.1016/j.acap.2016.06.010 [DOI] [PubMed] [Google Scholar]
- Marshall J, Adelman A, Kesten SM, Natale RA, & Elbaum B (2017). Parents’ experiences navigating intervention systems for young children with mild language delays. J Early Interv, 39, 180–198. 10.1177/1053815117704958 [DOI] [Google Scholar]
- Marshall J, Coulter ML, Gorski PA, & Ewing A (2016). Parent recognition and responses to developmental concerns in young children. Infrants Young Child, 29, 102–115. 10.1097/iyc.0000000000000056 [DOI] [Google Scholar]
- Marshall J, Kirby RS, & Gorski P, A. (2015). Parent concern and enrollment in intervention services for young children with developmental delays: 2007 National Survey of Children’s Health. Except Child, 82, 251–268. 10.1177/0014402915585563 [DOI] [Google Scholar]
- Marteau TM, Sowden AJ, & Armstrong D (2002). Implementing research findings into practice: Beyond the information deficit model. In Haines A, & Donald A (Eds.), Getting Research Findings into Practice pp. 36–42). London: BMJ Publishing Group. [Google Scholar]
- Mazurek MO, Handen BL, Wodka EL, Nowinski L, Butter E, & Engelhardt CR (2014). Age at first autism spectrum disorder diagnosis: The role of birth cohort, demographic factors, and clinical features. J Dev Behav Pediatr, 35, 561. 10.1097/DBP.0000000000000097 [DOI] [PubMed] [Google Scholar]
- Moran TE, & O’Hara MW (2006). Maternal psychosocial predictors of pediatric health care use: Use of the Common Sense Model of Health and Illness behaviors to extend beyond the usual suspects. Clin Eff Nurs, 9, e171–e180. 10.1016/j.cein.2006.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, & Buick D (2002). The revised illness perception questionnaire (IPQ-R). Psychol Health, 17, 1–16. 10.1080/08870440290001494 [DOI] [Google Scholar]
- Orbell S, & Phillips LA (2019). Automatic processes and self-regulation of illness. Health Pscyhol Rev, 1–28. 10.1080/17437199.2018.1503559 [DOI] [PubMed] [Google Scholar]
- Patton MQ (2015). Qualitative Research & Evaluation Methods. Thousand Oaks, CA: SAGE [Google Scholar]
- Petraglia J (2007). Narrative intervention in behavior and public health. J Health Commun, 12, 493–505. 10.1080/10810730701441371 [DOI] [PubMed] [Google Scholar]
- Revenson TA, & Diefenbach MA (2019). New questions about a long-standing model. Health Psychol Rev, 1–3. 10.1080/17437199.2019.1642790 [DOI] [PubMed] [Google Scholar]
- Rosenberg SA, Ellison MC, Fast B, Robinson CC, & Lazar R (2013). Computing theoretical rates of Part C eligibility based on developmental delays. Matern Child Health J, 17, 384–390. 10.1007/s10995-012-0982-2 [DOI] [PubMed] [Google Scholar]
- Rosenberg SA, Zhang D, & Robinson CC (2008). Prevalence of developmental delays and participation in early intervention services for young children. Pediatrics, 121, e1503–e1509. 10.1542/peds.2007-1680 [DOI] [PubMed] [Google Scholar]
- Sandelowski M (2000). Whatever happened to qualitative description? Res Nurs Health, 23, 334–340. [DOI] [PubMed] [Google Scholar]
- Sices L, Egbert L, & Mercer MB (2009). Sugar-coaters and straight talkers: Communicating about developmental delays in primary care. Pediatrics, 124, e705–e713. 10.1542/peds.2009-0286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorne S, Kirkham SR, & MacDonald-Emes J (1997). Interpretive description: A noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health, 20, 169–177. [DOI] [PubMed] [Google Scholar]
- Valicenti-McDermott M, Hottinger K, Seijo R, & Shulman L (2012). Age at diagnosis of Autism Spectrum Disorders. J Pediatr, 161, 554–556. 10.1016/j.jpeds.2012.05.012 [DOI] [PubMed] [Google Scholar]
- Weinman J, Petrie KJ, Moss-Morris R, & Horne R (1996). The illness perception questionnaire: A new mtheod for assessing the cognitive representation of illness. Psychol Health, 11, 431–441. 10.1080/08870449608400270 [DOI] [Google Scholar]
- Wittke K, & Spaulding TJ (2018). Which preschool children with specific language impairment receive language intervention? Langauge, Speech & Hearing Services in Schools, 49, 59–71. 10.1044/2017_LSHSS-17-0024 [DOI] [PubMed] [Google Scholar]
- Wong IYT, Hawes DJ, Clarke S, Kohn MR, & Dar-Nimrod I (2018). Perceptions of ADHD among diagnosed children and their parents: A systematic review using the Common-Sense Model of Illness Representations. Clin Child Fam Psychol Rev, 21, 57–93. 10.1007/s10567-017-0245-2 [DOI] [PubMed] [Google Scholar]
- Woolfenden S, Posada N, Krchnakova R, Crawford J, Gilbert J, Jursik B, et al. (2015). Equitable access to developmental surveillance and early intervention – understanding the barriers for children from culturally and linguistically diverse (CALD) backgrounds. Health Expectations, 18, 3286–3301. 10.1111/hex.12318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Mattox KM, Sinche BK, Blaschke GS, & Bethell C (2014). Racial, ethnic, and language disparities in early childhood developmental/behavioral evaluations: A narrative review. Clin Pediatr, 53, 619–631. 10.1177/0009922813501378 [DOI] [PMC free article] [PubMed] [Google Scholar]