Abstract
Each decade, the American Heart Association (AHA) develops an Impact Goal to guide its overall strategic direction and investments in its research, quality improvement, advocacy, and public health programs. Guided by the AHA’s new Mission Statement, to be a relentless force for a world of longer, healthier lives, the 2030 Impact Goal is anchored in an understanding that to achieve cardiovascular health for all, the AHA must include a broader vision of health and well-being and emphasize health equity. In the next decade, by 2030, the AHA will strive to equitably increase healthy life expectancy beyond current projections, with global and local collaborators, from 66 years of age to at least 68 years of age across the United States and from 64 years of age to at least 67 years of age worldwide. The AHA commits to developing additional targets for equity and well-being to accompany this overarching Impact Goal. To attain the 2030 Impact Goal, we recommend a thoughtful evaluation of interventions available to the public, patients, providers, healthcare delivery systems, communities, policy makers, and legislators. This presidential advisory summarizes the task force’s main considerations in determining the 2030 Impact Goal and the metrics to monitor progress. It describes the aspiration that these goals will be achieved by working with a diverse community of volunteers, patients, scientists, healthcare professionals, and partner organizations needed to ensure success.
Keywords: AHA Scientific Statements, goals, health equity, healthy aging, life expectancy, prevention and control, public health
Each decade, the American Heart Association (AHA) develops an Impact Goal to guide its overall strategic direction and investments in its research, quality improvement, advocacy, and public health programs. Over the past 2 decades, these Impact Goals have driven efforts to reduce mortality from cardiovascular disease (CVD) and stroke, while progressively emphasizing disease prevention and improved cardiovascular and brain health. For the past 2 years, a committee of AHA volunteers and staff, guided by the AHA board, has worked to craft the 2030 Impact Goal. Starting with the AHA’s mission, the new 2030 Impact Goal is anchored in an understanding that to achieve cardiovascular health for all, the AHA must expand its focus and engagement to include overall health and well-being and further address equity. This presidential advisory summarizes the committee’s main considerations and conclusions and outlines the 2030 Impact Goal, the metrics needed to monitor progress, and the aspirations of the AHA to achieve this goal by working with the diverse community of volunteers, patients, scientists, healthcare professionals, the general public, and partner organizations needed to ensure success.
BACKGROUND ON STRATEGIC VALUE PROPOSITION AND EXPANDED MISSION
Supported by 40 million volunteers, a staff of pioneering professionals, and assets of nearly $1 billion, the AHA’s mission is to be a relentless force for a world of longer, healthier lives. Every 10 years since the late 1990s, the AHA commits to a singular Impact Goal for the decade ahead to advance the AHA’s mission. These goals—and the AHA’s mission itself—have become steadily broader (Table 1). This reflects an evolving understanding of the many intertwined conditions that are necessary for all people to live free of CVD and stroke and the AHA’s growing influence as a catalyst within a broader network of fellow stakeholders, in the United States and around the globe. In the next decade, the AHA along with stakeholders will strive for its most ambitious goals:
Table 1.
Evolution of the AHA Mission and Impact Goals
| Era | Mission | Impact Goal |
|---|---|---|
| 1996–2006 | To reduce disability and death resulting from CVD and stroke | By 2010, to reduce coronary heart disease, stroke, and risk by 25% |
| 2006–2019 | To build healthier lives free of CVD and stroke | By 2020, to improve the cardiovascular health of all Americans by 20% while reducing deaths from CVDs and stroke by 20% |
| 2019– | To be a relentless force for a world of longer, healthier lives | Across the United States: “Together, we will equitably increase healthy life expectancy from 66 to at least 68 years by 2030.” Around the world: “Together with global and local collaborators, we will equitably increase worldwide healthy life expectancy from 64 to at least 67 years by 2030.” |
AHA indicates American Heart Association; and CVD, cardiovascular disease.
Across the United States: “Together, we will equitably increase healthy life expectancy from 66 to at least 68 years by 2030.”
Around the world: “Together with global and local collaborators, we will equitably increase worldwide healthy life expectancy from 64 to at least 67 years by 2030.”
Three areas of focus are noteworthy in this new mission and goals. Each is summarized, with further explanation in subsequent sections.
Commitment to wider work. AHA’s expertise has been anchored in cardiovascular and brain health, yet its work with partners encompasses far more. Modern science shows that hearts, bodies, and minds are interconnected and are best able to thrive in a world designed for health and well-being in the broadest sense. Such a world ensures that vital conditions needed to create health and well-being are present for everyone, including societal and structural contributors to health such as housing, education, safety, access to healthy food, meaningful and sufficiently paid work, and clean air and water, as well as healthy environments. To achieve this together, AHA’s partnerships must reflect those working on diverse areas in the United States and around the world.
Equity at the center. Progress must be equitable in both means and ends. All people must have fair opportunities to reach their full potential, without the exclusion of anyone. We can accomplish more to expand health and well-being when all people feel that they belong and can contribute to shape our common world. In fact, the greatest benefits should be among those who have endured the greatest adversities and inequities because of race, ethnicity, income, or other demographic or geographic characteristics.
Unified focus on health and well-being. A unified focus on health and well-being supports connections across sectors and societal circumstances. Efforts to save lives and to prevent premature deaths and disability are thus combined with those aimed at expanding prosperity, a sense of connection and purpose, and other conditions that enhance the experience and productivity of life.
CURRENT PUBLIC HEALTH BURDEN OF CVD AND STROKE AND PROGRESS ON 2020 IMPACT GOAL
Nearly 50% of American adults have some form of CVD, increasing to nearly 60% for non-Hispanic blacks (NHBs).1 CVD and stroke combined remain the leading cause of mortality in the United States for men and women (≈1 of every 3 deaths) and claim more lives each year than all forms of cancer combined. Although there has been steady improvement in cardiovascular mortality in the United States over the past several decades, recent data indicate that progress has stalled and that relatively high age-adjusted mortality persists in many states and counties.1 CVD is also the leading cause of death globally, accounting for >17.6 million deaths in 2016, a number that has been projected to grow to >23.6 million by 2030.2 A recent study focusing on individuals 35 to 70 years of age found that 40% of global deaths were caused by CVD, predominantly in low- and middle-income countries.3
The 2020 Impact Goal was an important step forward for the AHA in helping people live free of CVD and stroke, recognizing the need for an upstream emphasis on cardiovascular health and CVD prevention. It read, “By 2020, to improve the cardiovascular health of all Americans by 20% while reducing deaths from cardiovascular diseases and stroke by 20%.”3a Progress in cardiovascular health was defined on the basis of changes in prevalence of Americans (adults and youth) having poor, intermediate, or ideal levels of 7 fundamental cardiovascular health behaviors and factors; that is, Life’s Simple 7 (tobacco use, dietary quality, physical activity, body mass index, blood pressure, total blood cholesterol, and blood glucose). Over the past decade (NHANES [National Health and Nutrition Examination Survey] 2007–2016), there has been significant progress in the United States toward the 2020 Impact Goal, with less smoking in adults, increased physical activity in adults, improved dietary habits in both adults and youth, lower total cholesterol in adults and youth, and lower blood glucose in adults.1 However, these areas of progress have been offset by adverse forces: increases in high blood pressure and body mass index among adults and youth, higher blood glucose in youth, and lower physical activity in youth. The continued worsening of overweight and obesity rates among adults and youth throughout the decade is especially concerning and largely accounts for worsening blood pressure in adults and youth and fasting blood glucose among youth.
The past decade also saw a substantial 15.1% reduction in age-adjusted mortality due to CVD, a positive achievement but smaller than in previous decades. This slowing decline appears to relate to the decreases in ischemic heart disease and stroke mortality being offset by increases in mortality from other types of CVDs, including hypertensive diseases, heart failure, and atrial fibrillation. In addition, the declines in ischemic heart disease and stroke mortality were likely smaller than would have occurred without the adverse trends in obesity and its corresponding risk factors. Thus, the success of lowering CVD mortality by 15% is tempered by disappointment in not meeting the more ambitious 20% reduction in the 2020 Impact Goal.
Although both cardiovascular health and CVD mortality have improved overall in the United States in the past decade, disparities persist for healthy behaviors, risk factors, and CVD mortality based on race, ethnicity, geography, and income. This is also true globally. Further progress will need a renewed focus on improving health equity and addressing the broader range of factors that contribute to cardiovascular health, as well as overall health and well-being.
SELECTING THE APPROPRIATE 2030 IMPACT GOAL METRIC AND DATA SOURCES
Key Criteria for Selecting the Metric for the 2030 Impact Goal
Starting with the new AHA mission to be a relentless force for a world of longer, healthier lives, and incorporating AHA values of health equity, well-being, and impact across the life course, the committee considered 5 key criteria in selecting the optimal metric and data sources for the 2030 Impact Goal: (1) embodiment of the AHA mission and values, (2) contemporary relevance, (3) validity, (4) modifiability, and (5) data analytic consistency and frequency. In addition, a key characteristic of the final metric and data source was the ability to measure progress at the local and regional levels, including disparities between relevant populations.
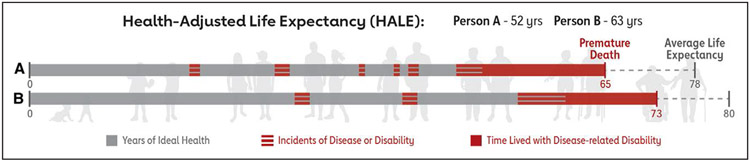
After a careful review of existing metrics and currently available data sources, the committee selected the health-adjusted life expectancy (HALE) metric, commonly referred to as healthy life expectancy, as best meeting the criteria above.4 HALE provides a summary measure of population health that quantifies the number of years that a population can anticipate living in good health. HALE does this by adjusting life expectancy for years lived in less than ideal health and years lost as a result of premature mortality to provide a single measure of the average population health (Figure 1).
Figure 1. Increasing Health-Adjusted Life Expectancy (HALE).
HALE is the number of years living in good health, accounting for years lived with disease or disability and years lost due to premature death. As shown, HALE can be increased through improving health and well-being, preventing or delaying onset and severity of disease, and increasing life expectancy.
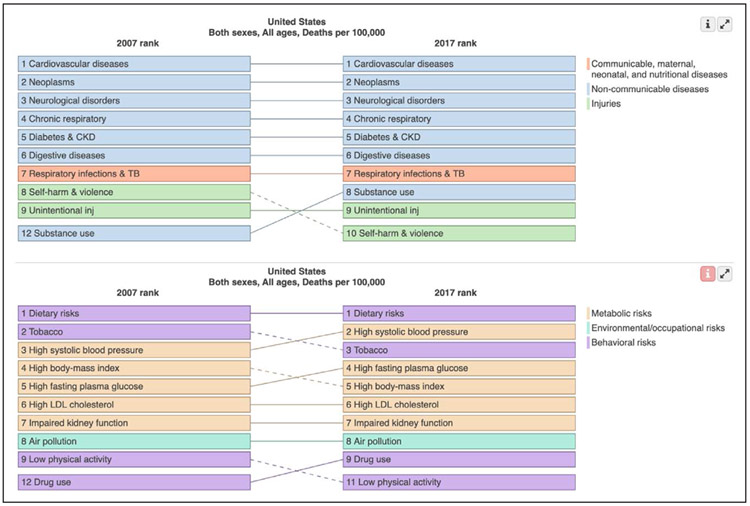
Compared with other population health and surveillance metrics considered, HALE was found to be the most comprehensive single metric that provides an estimate of overall health across the life course and includes several components of well-being in a way that has contemporary relevance to the AHA and many other partnering organizations. In addition, annual national and global HALE estimates provided by the GBD study (Global Burden of Diseases, Injuries, and Risk Factors Study) by the Institute for Health Metrics and Evaluation at the University of Washington provide a data source with relevant validity, consistency, and frequency of reporting.5,6 For example, GBD has ranked the causes of mortality and disability in the United States and their changing rank order between 2007 and 2017.7,8 Although CVD remains the leading cause of death, GBD shows how other conditions such as drug use disorders have risen over this period of time8 (Figure 2).
Figure 2. Comparison of GBD (Global Burden of Diseases, Injuries, and Risk Factors Study) mortality rank order in 2007 and 2017 in the United States, by causes and risk factors.
CKD indicate chronic kidney disease; inj, injury; LDL, low-density lipoprotein; and TB, tuberculosis.
HALE Advantages and Limitations
HALE provides a summary measure of population health that quantifies the number of years that a population can anticipate living in good health and is complementary to estimates of life expectancy alone. HALE has revealed important trends in certain locations such as slower improvements in HALE than in life expectancy; that is, more years being lived but in less than ideal health. HALE is also useful for examining locations where life expectancy is increasing, populations are rapidly aging, and a growing proportion of societal resources are being dedicated to health care through the life course and caregiving in the last years of life.
In this advisory, HALE estimates follow well-established methods,9 as well as approaches and data from the GBD Study 2017.5 The GBD currently produces annual estimates of HALE for the United States and 194 other countries and territories, allowing the use of a common metric for both domestic and international goals. HALE captures both physical and mental health conditions. Although all diagnosable mental health conditions (eg, depression, dementia) are included in the calculation, a limitation is that other aspects of well-being such as emotional, social, economic, and other contextual determinants are not captured. HALE estimates for the United States are also currently available at the national and state levels.8 Additional analyses by GBD are currently underway to produce HALE estimates at a county level and within race and ethnicity groups to help assess measures of health equity and structural determinants of health.
DOMESTIC 2030 IMPACT GOAL
HALE Calculation in the United States
For the 2030 Impact Goal across the United States, HALE was calculated separately by sex on the basis of age-specific mortality rates and years lived with disability per capita for each US state in each year. Years lived with disability were computed for each of 3484 health states (groupings of disease sequelae) by multiplying estimated disease-specific incidence or prevalence by an associated disease-specific disability weight (both from the GBD 2017 study), accounting for multimorbidity with a Monte Carlo simulation, which assumed that comorbidities were independent within age groups.
Forecasting US HALE at Birth in 2020 and 2030
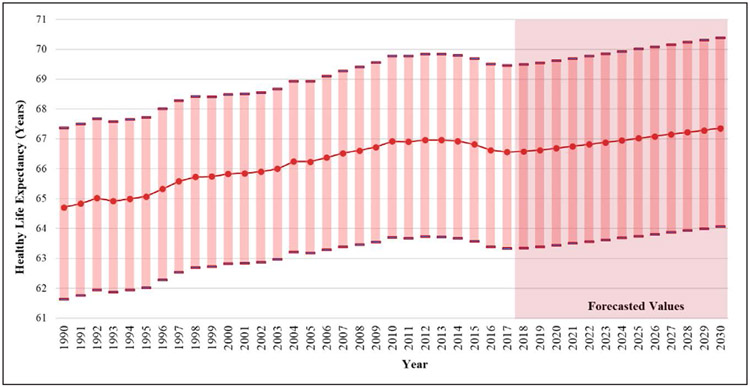
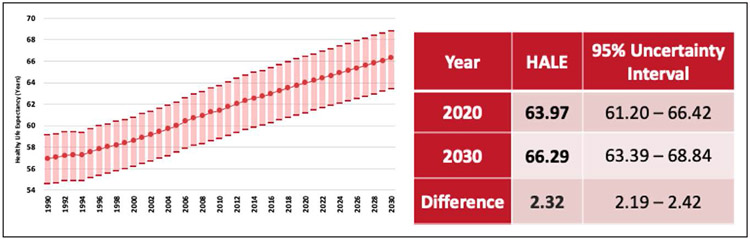
Using GBD estimates of HALE between 1990 and 2017, we forecasted HALE between 2020 and 2030 (Figure 3 and Table 2) using an autoregressive integrated moving average model. This model predicts a value in a response time series as a linear combination of its own past values, past errors, and current and past values of other time series. HALE values and the upper and lower uncertainty intervals were forecasted with PROC ARIMA (SAS version 9.4) on the basis of 1990 to 2017 data.
Figure 3. Forecast for US healthy life expectancy, 2018 to 2030.
Error bars represent 95% uncertainty intervals.
Table 2.
Forecasted US Healthy Life Expectancy in 2020 and 2030 and the Estimated Change Across the Decade
| Year | HALE at Birth | 95% Uncertainty Interval |
|---|---|---|
| 2020 | 66.69 y of age | 63.44–69.62 y of age |
| 2030 | 67.36 y of age | 64.05–70.39 y of age |
| Difference | 0.67 | 0.61–0.77 |
HALE indicates health-adjusted life expectancy.
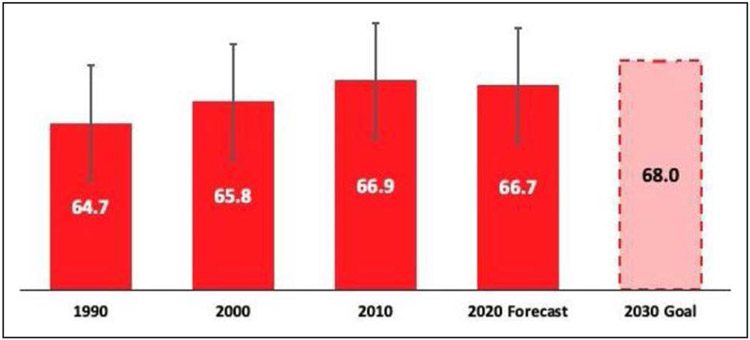
The HALE estimates used for our goal setting were HALE at birth, a standard approach for calculating HALE, and life expectancy by major public health organizations (eg, US Centers for Disease Control and Prevention). These values can be interpreted as the number of years a baby born in the corresponding year can expect to live in good health. From the forecasts in Table 2, the current expected improvement in HALE from 2020 (66.69 years of age) to 2030 (67.36 years of age) is 0.67 years (95% uncertainty interval, 0.61–0.77).
Domestic Goal Language
The 2030 Impact Goal across the United States translates the AHA mission of longer, healthier lives into a specific milestone target while placing both a collaborative approach and health equity at the center: “Together, we will equitably increase healthy life expectancy from 66 to at least 68 years by 2030.”
The goal statement begins with “together” to recognize that coordinated efforts across our nation’s public, private, and nonprofit sectors are needed for success. The AHA will be a relentless force in catalyzing this change through partnerships and inspiring others, in addition to its own work and investments.
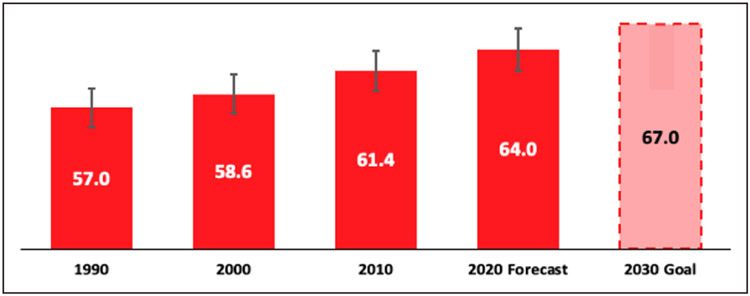
The milestone of “at least 68 years” is a highly ambitious goal, particularly given that it represents reversing declining HALE trends in the United States in the most recent years of data availability (−0.4 years from 2013–2017).1 As outlined previously, the 2030 Impact Goal nearly doubles the forecasted improvement in HALE by 2030 from 0.7 years to 1.3 years. The remaining “stretch” to 68 years of age (0.6 years) represents a major incremental impact objective, one that must be driven by additional improvements in behaviors, prevention, policy, public health, and healthcare systems. Figure 4 graphically represents this.
Figure 4. US health-adjusted life expectancy forecast and goal.
Error bars represent 95% uncertainty intervals.
The goal language also places health equity at the center. Health equity implies that everyone should have an equal opportunity to attain his or her full health potential and that no one should be disadvantaged from achieving this potential throughout life. It is important both to reverse the widening disparities between more and less advantaged groups in our nation and to improve health and well-being outcomes in an absolute sense. Indeed, closing the gap between populations in health and well-being is the only way to ensure sustainability of health improvements for all.
Evolution Between the 2020 and 2030 Impact Goals
The 2030 Impact Goal is a powerful extension from prior years. As described, the 2020 Impact Goal added the novel goal of improving cardiovascular health for all Americans.10 Subsequent research stimulated by the 2020 Impact Goal further highlighted the interrelatedness of cardiovascular health and broader measures of health and well-being.11-18 In other words, improved cardiovascular health across the population can be achieved by improving many circumstances that lead to poor health more generally. These data have motivated the new focus on healthy life expectancy, using the HALE metric that incorporates elements of overall health, disease conditions, quality and longevity of life, and well-being. The 2030 Impact Goal also includes a renewed focus on equity and improvements for all. Finally, in line with the AHA’s mission, a new, separate global 2030 Impact Goal is described below.
GLOBAL GOAL LANGUAGE AND METRIC
The updated Mission Statement explicitly broadens AHA’s scope to create a “world of longer, healthier lives.” Accordingly, the AHA now includes a global Impact Goal for 2030, which parallels domestic language with a stronger emphasis on partnership: “Together with global and local collaborators, we will equitably increase worldwide healthy life expectancy from 64 to at least 67 years by 2030.”
Like the domestic goal, the global Impact Goal is based on the same HALE metric, a widely used summary measure for comparing population health between countries.19,20 The GBD study has calculated HALE for 195 countries by using the prevalence of multiple disease conditions and their sequelae combined with a continuous scale of empirically derived disability weights. In this formulation, HALE becomes a measure that is both consistent over time and sensitive to improvements in health as a result of interventions.
Global HALE was forecast (Figure 5) through 2030 using the same autoregressive integrated moving average method as outlined in the Forecasting US HALE at Birth in 2020 and 2030 section. These projections show global HALE increasing by 2.3 years to reach 66.3 years of age in 2030.
Figure 5. Forecast of global HALE, 1990 to 2030.
Error bars represent 95% uncertainty intervals. HALE indicates health-adjusted life expectancy.
The milestone of “at least 67 years” will add 3 years of healthy life expectancy to the global population of 8.5 billion and represents an ambitious goal and a historic opportunity to improve quality life span across the globe (Figure 6). The target is 0.7 years above the statistical forecast for 2030, and the total increase of 3.0 years represents a significant acceleration from the 2.3 years per decade average since 1990. Bold, innovative initiatives and a broad, multilateral movement are needed to achieve this breakthrough.
Figure 6. Global health-adjusted life expectancy forecast and goal.
Error bars represent 95% uncertainty intervals.
Like the domestic goal, the global Impact Goal emphasizes the need to do this together. Collaboration will be central to the global mission because of the scale of the challenge (global disability-adjusted life-years are nearly 25 times the US total) and the diversity of nations’ health priorities and resources. Expanding our work alongside global and local partners will also further build capacity, share AHA’s expertise, and better support sustainability at the community level.
THE IMPORTANCE OF EQUITY
The World Health Organization defines equity as “the absence of avoidable, unfair, or remediable differences among groups of people.”20a Health equity acknowledges that health and well-being are determined by proximal (biological), intermediate (health behavioral), and distal (contextual) factors, the last often referred to as social or structural determinants of health (SDOH). There is variability within each of these 3 levels in any population, which also influence each other. For example, biological heterogeneity or individual differences in behavior may be influenced by variations in socially patterned group differences in exposure to social and environmental contexts. These systematic differences determine the likelihood of facing risk of harmful versus beneficial outcomes; that is, they are drivers of health inequities. Equitable societies acknowledge this variation and the factors that lead to and perpetuate inequities. They allocate healthcare, public health, social, and economic resources so that all people and communities, not just the socially advantaged, can attain their highest potential for health and well-being.
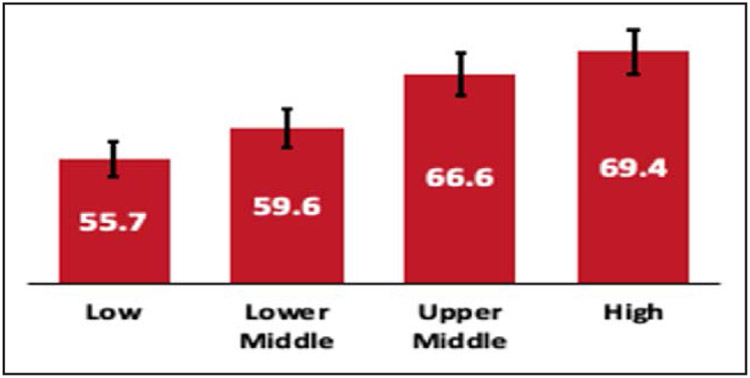
Large disparities (ie, differences) in healthy life expectancy exist across the United States. Across states, for example, the average HALE varied by >7 years in 2017 (Figure 7). Disparities also exist within states along other key dimensions, including, for example, education, income, race/ethnicity, and urban versus rural residence. Addressing these disparities is critical to improving individual lives, the health of communities, and the overall healthy life expectancy across the United States.
Figure 7. Health-adjusted life expectancy (HALE)* across all US states, 2017.

*HALE <1 year of age.
Substantial health inequity also exists at a global level. Despite steady gains in global HALE over the past 30 years, a 14-year difference is seen between the highest and lowest quartiles of nation-specific HALE, a gap that mirrors economic development (Figure 8). Fifty-eight nations representing 2.4 billion people (35% of the global population) currently have HALE of <60 years of age. Many societal, environmental, public health, and healthcare system challenges in lower-income nations are different from those in the United States, but commonalities also exist. CVDs remain the leading cause of death worldwide, and CVD-related disability-adjusted life-years increased most in low- and lower-middle–income countries (L/LMICs) over the past decade, from 9% to 12% of global disability-adjusted life-years from all causes. The last section, A Call to Action: Increasing Healthy Life Expectancy, expands on the call-to-action steps to address both domestic and global health inequities, including developing equity targets to complement the 2030 Impact Goals.
Figure 8. 2017 global average health-adjusted life expectancy grouped by World Bank income group.
BEYOND HEALTH: A FOCUS ON WELL-BEING
Health and well-being are related but distinct. Whereas health refers to a person’s physical and mental status, well-being encompasses additional states of being and aspects of life such as security, prosperity, sense of connection, and purpose.21-24 Such experiences are linked to cardiovascular and brain health and vice versa.25-34 Such ties also appear mutually reinforcing on several scales: neurobiological, behavioral, emotional, socioeconomic, and cultural.35-45
The science of well-being is evolving into an important frontier of knowledge, policy, and practice.46-51 Some nations have designated budgets to expand well-being,52,53 which has also been connected to intergenerational legacies of vital conditions on which all people depend to reach their full potential.54,55 Although much more remains to be discovered, it is clear that well-being matters and can be effectively measured and modified for both individuals and groups.
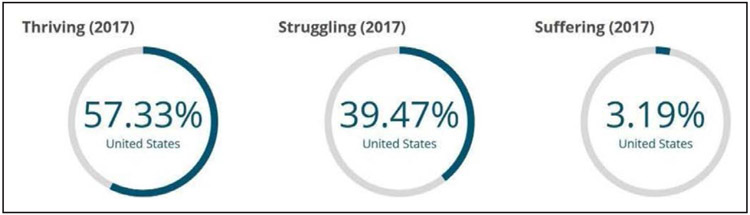
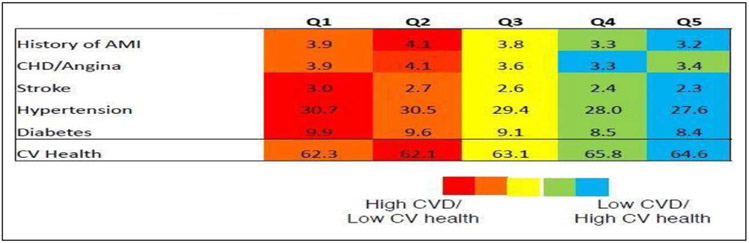
As a complementary measure for the 2030 Impact Goal, the task force identified the Cantril Ladder as an informative summary measure of well-being to chart current status and progress. The Cantril Ladder is a simple, valid, and reliable 2-item scale about how someone feels about his or her life now and in 5 years.56,57 How people feel about their overall life satisfaction strongly predicts how healthy they are, how long they will live, and future healthcare use.57-61 From this metric, it is possible to calculate proportions of the population who feel they are thriving, struggling, or suffering (Figure 9).62,62a Other metrics of well-being show that well-being is strongly correlated with, yet distinct from, conventional measures of cardiovascular health (Figure 10), according to 348 846 respondents in the 2010 Gallup-Healthways survey using their Well-Being Index.
Figure 9. People’s perception of their well-being, United States, 2017.62a.
Figure 10. Correlation of perceived well-being and cardiovascular health.
Rates of cardiovascular risk factors, disease, and health by overall well-being score. Q1=lowest well-being; Q5= highest well-being. AMI indicates acute myocardial infarction; CHD, congestive heart disease; CV, cardiovascular; and CVD, cardiovascular disease. Adapted from Spatz et al.63 Copyright © 2014, American Heart Association, Inc.
Well-being scores are responsive to changes in surrounding circumstances, with shifts in self-report of overall life satisfaction being measurable within 3 to 6 months, and are often used by employers and community initiatives to chart progress over time.56,64-66 The Cantril Ladder is routinely tracked in the United States and globally by groups such as Gallup, the Organization for Economic Cooperation and Development, and the World Happiness Report, which facilitates standardized comparisons over time and geography.67
In addition to the well-being–related components of HALE, the AHA will use the Cantril Ladder to calculate the percentage of people who report that they are thriving, struggling, and suffering across populations. The last section of this advisory, “A Call to Action: Increasing Healthy Life Expectancy,” expands on how the AHA will develop well-being targets for 2030 as a complement to HALE.
THE IMPORTANCE OF STRUCTURAL DETERMINANTS OF HEALTH
For the AHA to achieve its mission and 2030 Impact Goal, it must leverage a wide view of the drivers that contribute to equitable health and well-being. Many of these drivers have been described as SDOH, with increasing appreciation in recent decades that health is driven by far more than health care. Looking ahead to the next decade, the AHA recognizes the importance of these drivers to achieve the environments in which all people have an opportunity to reach their full potential.
Although the term SDOH has helped to galvanize a wider understanding of health drivers, it has a broad and evolving definition encompassing social risk factors, individual social needs, and community/society–level structural determinants.68,69 For example, Healthy People 203070 focuses on establishing a consistent set of vital conditions that all people need all of the time to reach their full potential while also delivering urgent services that an individual under adversity might need temporarily to regain his or her best possible health and well-being.
The AHA recognizes that the multidirectional relationship between these social needs/conditions and equitable health and well-being requires their joint consideration to achieve the 2030 Impact Goal. Whenever possible, measures of HALE stratified by sex, race, ethnicity, geography, and other factors should be prioritized to help identify groups, regions, and communities affected by health disparities and their nonmedical contributors. This is also why the AHA will be working to obtain more detailed demographic and geographic HALE data in the United States and globally.
A CALL TO ACTION: INCREASING HEALTHY LIFE EXPECTANCY
Areas for Focus
Achieving the ambitious goal of equitably increasing healthy life expectancy in the United States and around the world will require a comprehensive understanding of the diverse risk factors and conditions that contribute to lost years of healthy life, a detailed understanding of timing and trends in the burdens of these factors and other contributors, and, guided by this knowledge, a relentless pursuit of targeted reductions in risk factors and improvements in conditions most responsible for overall years of healthy life lost, as well as associated inequities.
Continued Value of the 2020 Goal Constructs of Cardiovascular Health/Life’s Simple 7 and How the 2030 Impact Goal Work Builds on This Foundation
As described, the AHA’s 2020 Impact Goal introduced the concept of cardiovascular health, defining Life’s Simple 7 with 7 components known to strongly and independently improve cardiovascular and brain health, as well as overall health and well-being. This helped shift the AHA from a strong disease focus toward embracing and incorporating health promotion and disease prevention. Yet, not all of the 7 cardiovascular health targets were achieved. In consideration of these successes and limitations, the 2030 Impact Goal and language incorporate a growing appreciation that people’s behaviors influence and are influenced by their overall health and well-being, which in turn are influenced by the environments around them. The choices and opportunities available to people and how they respond to these opportunities help determine their behavioral patterns. To improve individual health, it is important to make the environments in which we live, work, learn, and play equitably supportive of healthy behaviors and well-being. The AHA recognizes that achieving aggressive targets for cardiovascular health, brain health, and overall health and well-being will require addressing SDOH across the life span, particularly to achieve goals for equity. Stated another way, sustainable and meaningful improvements in cardiovascular and brain health of our populations in the United States and globally require that we commit to changing the context that creates health more broadly.
Establishing Targets for Equity in Health and Well-Being
As previously discussed in the introduction, the AHA’s 10-year impact goals guide the organization’s planning for the decade ahead, including its strategic direction, investments, and partnerships. Inherent to the design of the 2030 Impact Goals is the recognition that closing the persistent and unjust differences in health outcomes between subsets of our population is essential if we are to advance cardiovascular and brain health and reach our 2030 domestic and global health life expectancy targets. Consistent with this evidence-based understanding, the AHA will develop specific 2030 targets for both equity and well-being to ensure that the AHA’s broader work is designed, implemented, and monitored in a manner consistent with the central values of the organization. These will help catalyze the 2030 Impact Goals, moving us all toward longer, healthier lives.
Equity Target
To ensure meaningful and impactful targets for equity, the AHA will set up a task force, similar to the process for establishing the overall 2030 Impact Goal, to review the domestic and global equity measures that may be available over the next decade and to analyze the current status and trends to determine specific equity targets for 2030. These targets will be released later in 2020. Domestically, as discussed, the HALE metric currently incorporates county-level and race/ethnicity information to facilitate measurement and tracking of progress in certain aspects of health equity in the United States. This work will be expanded to support wider availability and capacity for target setting and local/regional monitoring and assessment of progress. Globally, the AHA aims to address inequity and the rising relative and absolute burdens of CVD by focusing on accelerating improvements in L/LMICs.
Well-Being Target
As discussed in the Beyond Health: A Focus on Well-Being section, the task force identified the Cantril Ladder as the recommended measurement of well-being for the AHA’s work. Similar to the rigorous process used to create AHA’s 2030 Impact Goal, the AHA will assemble a task force to model and determine a unified 2030 target for well-being. This will include research on how to integrate the Cantril Ladder with HALE to develop a more comprehensive, unified metric of health and well-being. Because HALE is being used for both the domestic and global 2030 Impact Goals, the product of this work will be relevant in the United States and globally. Through this process, we will develop new work, partnerships, and science to address the whole person, caring for cardiovascular health and social needs, and address the underlying SDOH driving poor outcomes and causing people to struggle and suffer.
Burden and Specific Actions to be Taken
A strategy that achieves the overall 2030 targets for HALE will require attention to overall trends and local variations in the causes of low HALE. Although progress has been made in the United States in recent years on certain diseases such as ischemic heart disease and lung cancer, there is much more to do. In recent years, 21 US states have experienced mortality reversals in younger adults linked to substance use, cirrhosis, and self-harm, as well as slower than otherwise expected reductions in CVD and other chronic diseases. Any strategy to increase HALE must appreciate that some areas and populations have markedly worse health trajectories and invest accordingly.
Generally, policy and environmental change strategies to address cardiovascular health and overall health and well-being should10,71 maximize opportunities for healthier eating (eg, economic incentives and disincentives, leveraging of federal feeding programs, strong nutrition standards in schools and workplaces, effective labeling and information, and addressing food insecurity), increase and support outdoor physical activity (eg, bike lanes, attention to planetary health and air pollution), and reduce tobacco use and end the epidemic of youth vaping and alcohol use (eg, smoke-free laws, alcohol and tobacco/e-cigarette taxation and warning labels). Enhancing the effective diagnosis, treatment, and control of existing high-risk conditions such as hypertension, dyslipidemia, diabetes mellitus, and kidney disease, as well as substance use disorders, through increasing the quality and effective broad-scale delivery of evidence-based interventions should be a priority. Care coverage and the costs of medications weigh heavily on both the insured and uninsured in the United States and globally. The global call for Universal Health Coverage, spearheaded by the World Health Organization and incorporated into the United Nations Sustainable Development Goals,72 and related active domestic discussions illustrate the importance of finding a remedy. Expanding affordable housing, living wage employment opportunities, and opportunities to increase educational attainment and improving other SDOH are also essential. Place-specific and population-based approaches that leverage the work environment and target workforces should be rigorously evaluated, with best practices rapidly disseminated.
Ensuring that persistent health inequities are addressed, including but not limited to those related to education, income, race/racism, urban and rural divides, age, and global variation by and within countries, demands careful attention, heightened investments, and strategic variation.
Targeted Populations
Death rates in the United States from CVD and stroke continue to vary by education, income, race/ethnicity, age, place, and other factors. For example, NHBs experience a disproportionate number of deaths from heart disease, stroke, and hypertensive disease, with nearly twice the rate of non-Hispanic whites. Risk for avoidable death is particularly high among NHB men, ≈80% higher than that of non-Hispanic white men and NHB women.73 Compared with non-Hispanic whites, NHBs also have higher prevalence of nonideal cardiovascular health across the majority of components of Life’s Simple 7. In addition, previous studies suggest that the US NHB/non-Hispanic white disparity in avoidable mortality reflects differences in education, income, living conditions, and access to health care. Interventions aimed at addressing these structural determinants of health, in combination with effective treatment and control of risk factors, could help reduce population disparities in avoidable deaths.
Also concerning is the stagnating decline in heart disease mortality among young adults 35 to 44 years of age,74 which has occurred in the context of continuing increases in the prevalence of obesity and diabetes mellitus. The observed increases in heart disease mortality among this working-age population are concerning because these are largely avoidable deaths. Mortality increases were concentrated in medium and small metropolitan areas and in rural counties, which could lead to a widening of the urban-rural disparity that began in the mid-2000s.75 Indeed, this rural-urban gap is not limited to working-age populations. For example, from 2010 to 2017, the rural-urban gap in excess deaths overall increased for cancer, heart disease, and chronic lung disease, and in 2014, life expectancy was >3 years lower in rural compared with urban areas.76 Overcoming these inequities will require increased investment in surveillance, reporting, research, and programs tailored to the structural needs of rural environments and care delivery systems.77 Stroke also shows disturbing trends, with broad and substantial increases in ischemic stroke and stroke risk factors among adults 18 to 54 years of age. NHBs had the highest rate of stroke, whereas Hispanics uniquely had significant increases in ischemic stroke in all age groups.78
Primary prevention of CVD includes health-promoting activities that can occur both within and outside of the traditional healthcare system. The latter may represent a key opportunity for reaching younger, working-age individuals, who may underuse effective preventive health care. A focus of primary prevention on younger adults also represents an opportunity to reduce the cumulative negative effects of CVD risk factors. Similarly, focusing primary prevention efforts outside of large urban counties may be important because the populations in these counties often have a lower prevalence of a number of healthy behaviors.
To ensure that prevention-related interventions for heart disease and stroke events effectively reach these populations, communities and the healthcare and public health systems may require a renewed focus on the identification and effective treatment of not only cardiovascular risk factors, including tobacco use, obesity, diabetes mellitus, hypertension, and hyperlipidemia, but also health behaviors, in particular diet and physical activity, in addition to SDOH. Healthcare systems should be organized to reduce barriers to access and to increase incentives to engage in care early in adulthood such that individuals remain in care as they age. These same efforts, when focused outside of large urban centers, will need to overcome lower access to care in these communities.
A Strategic Approach to the Domestic Goal
To achieve the 2030 Impact goal in the United States, the AHA must work with a range of partners and stakeholders to support both individual- and population-based approaches to improve health and well-being across the life course. These efforts will also require attention to changing systems that perpetuate profound inequities in health and well-being.
To create systems change in the United States, AHA must bring all of its resources to bear, from research and data system expertise to its extensive volunteer network in thousands of communities, its capacity for building leaders, its well-organized policy and advocacy arm, and, above all, its partnerships with organizations across the country. Over the next decade, AHA will create biennial strategic plans to track and measure progress in the HALE metrics to ensure that it stays on track to meet the Impact Goals.
The adapted 100 Million Healthier Lives Community of Solutions framework offers a way to organize these assets, according to levers and activities, into a coherent framework for action (Table 3). Kania, Kramer, and Senge78a outline 6 levers for system change: policies, practices, resource flows, relationships and connections, power dynamics, and mental models. As a whole, this framework offers a systematic approach to improve healthy life expectancy and to position AHA as a pioneer and leader in improving well-being and equity in the country.
Table 3.
Example of an Action Framework to Achieve the AHA’s 2030 Impact Goal, Advancing Equity and Well-Being
| Levers for Systems Change | Activities by AHA | Activities Via Partnerships/With Communities |
Levers for Action |
|---|---|---|---|
| Leading from within (mental models) | Understand how historic and current legacies can create poor health and well-being. Engage all AHA staff and leadership in equity training. |
Engage partners and communities in adopting a well-being and equity approach in pursuing healthy life expectancy as a goal. | Training/education assets internally and externally |
| Leading together (relationships, power dynamics) | Make partnership with communities most affected by health inequities a standard practice in AHA initiatives to address the presidential goal. Support narrative change. Lift up the efforts of communities and partners who are creating effective improvements. |
Map potential partners across sectors and engage in strategic partnerships to advance AHA’s work. Play an active leadership role in aligned networks led by others, such as Well-Being in the Nation, in which multiple organizations are moving forward goals aligned with AHA’s with enough power to influence policy and practice. |
Partnerships Communications |
| Leading for outcomes | Make measurement of healthy life expectancy well-being and equity operational at AHA for routine tracking. Engage in evidence-based strategies to improve healthy life expectancy, wellbeing, and equity. Ensure that all data are disaggregated by equity factors such as race, place, and education. Evaluate the effectiveness of AHA strategies in advancing well-being, equity, and healthy life expectancy. |
Make measurement of drivers of healthy life expectancy, well-being, and equity easy for volunteers working in local communities. Make data visible to local communities. Support communities to measure effectiveness of their initiatives on well-being, equity, and drivers of healthy life expectancy. Support scale-up of approaches that show improved outcomes in healthy life expectancy, well-being, and equity. |
Research and measurement Healthcare delivery Data and technology Volunteer network |
| Leading for structural change (policy, practice, resource flows) | Assess AHA’s policies and practices through a well-being and equity lens. Advocate for global budgets and other policies that promote whole-person, whole-community approaches. Advocate for changes in funds flow and sustainable investment in communities experiencing poor health outcomes. |
Engage partners in communities to take a well-being and equity in all policies approach. Support planning and investment over the life course, with a focus on upstream structural determinants of health, including interventions to reduce toxic stress in childhood. Engage in anchor strategies and funds flow in communities with concentrated poverty. Support desegregation. |
Policy and advocacy Communities |
AHA indicates American Heart Association.
A Strategic Approach to the Global Goal
The global goal of “at least 67 years by 2030” is a major challenge, equaling >25 billion additional healthy years for humankind compared with the prior decade.8 Achieving this will require the skills and resources of the entire worldwide community. The AHA, in accordance with its mission, will be a relentless force in convening, creating, and catalyzing change to realize this outcome.
Although AHA’s international work has grown steadily over the past decade, significant changes in initiative design, operating models, and the scope of collaboration are needed to meet the 2030 Impact Goal. To reflect the health needs of L/LMICs, the AHA has developed programs focused on pediatric care, public training on first aid and trauma stabilization, and the emerging wave of cases of hypertension and diabetes mellitus. Young children (<5 years of age) are a priority because they represent fully 48% of all-age, all-cause disability-adjusted life-years in L/LMICs.8 The Helping Children Survive program provides frontline provider training on treatment of diarrheal and lower respiratory diseases that are 24% of the disability-adjusted life-year burden of this demographic.8 Early treatment of rheumatic fever is another youth-focused priority because rheumatic heart disease afflicts 33 million individuals, primarily in L/LMICs, with lifelong disability.79 Combining first-aid/trauma training with cardiopulmonary resuscitation addresses the road and unintentional injury rate that is 36% higher in L/LMICs relative to high-income countries.8 In addition, the rates of hypertension and diabetes mellitus are growing rapidly in L/LMICs, and roadmaps such as that outlined in Disease Control Priorities, 3rd edition,80 provide direction on how to address these developments.
Collaboration with local medical, community, and regulatory authorities will underpin our approach with each nation. Innovative operating models, using partnerships and licensing combined with emerging technologies, will help address legal and cost barriers.
The AHA will work with local, national, regional, and global partners to address relevant national health priorities. Initiative designs and operating models may differ from those of the United States and require contextualization, with potential focus on global challenges related to tobacco prevention and control, poor-quality diets, pediatric health, rural systems of care, and the diagnosis, prevention, treatment, and control of hypertension, high cholesterol, and diabetes mellitus. The AHA’s equity task force, as discussed, will also review and determine global equity measures and targets for 2030.
Need For Broader Research
Beyond the need for actionable data and active partnerships and the implementation of policies and programs already known to be effective, an expanded repertoire of additional effective interventions is needed. Indeed, as recognized by the AHA through assessment of progress toward past targets, sustainable and meaningful changes in health outcomes, including HALE, will require ongoing scientific research, structural investments, and changes in the way that systems influence health through areas such as housing, neighborhood safety, employment, education, and food security to create a more just and equitable environment for all.
Challenges and gaps remain in identifying priority actions for the AHA, other stakeholders, and the relevant communities to address. To consider these, the AHA will promote further scientific research to better understand models of effective interventions, partnerships, and advocacy for enhancing behaviors, environments, and policies that promote equitable health and well-being. Dissemination of findings and supporting exchanges between communities will be key to uptake of approaches found to be successful.
Cost Considerations
The 2030 Impact Goals appropriately aim to achieve longer, healthier life spans for all people in the United States and all people across the globe. When acting to achieve the 2030 Impact Goals, we need to quantify the health benefits accruing to individuals and to their organizations, communities, and the larger society. In addition, we need to weigh those benefits against the costs of health promotion and disease prevention and treatment decisions required to achieve those goals. The illnesses that need to be addressed to achieve the 2030 Impact Goals consume enormous resources through preventable healthcare expenditures, and corresponding savings in such costs could partly or fully offset efforts needed to improve health and well-being.
The United States lags behind other high-income countries on several measures of health outcomes, healthcare quality, and health equity despite spending roughly double the average amount on health care per person.81 In addition, overall healthy life expectancy in the United States is shorter than that of other high-income economies.82,83
The solution to the growing global burden of disease is not to spend more on sick care but rather to refocus our efforts on prevention and the root causes of poor health, which are often structural in nature. In the United States, most of the dollars spent in health care are directed at the treatment of chronic medical conditions, many of which are preventable. Why not use scarce resources more wisely?
To attain the 2030 Impact Goals, we recommend a thoughtful evaluation of the many intervention options available to the general public, patients, providers, healthcare delivery systems, communities, policy makers, and legislators. We offer that those interventions be judged not only in terms of their health benefits but also in terms of their outright cost, cost-effectiveness, cost utility, and cost benefit. To achieve the “biggest bang for the buck,” we need to do what is humane, what is right, and what is responsible.
Now Is the Moment
Through these 2030 Impact Goals, the AHA is signaling to the domestic and global communities the importance of this moment to build bridges and to work collectively toward a goal that no single organization can achieve alone.
To achieve our goals, we must be prescient in our framing of needs and our design of responses because the world is rapidly changing. For example, the science is clear that changes in our environment will affect contexts relevant to cardiovascular health, longevity, equity, and well-being. The places that we live, the foods that we eat, the way that we seek physical activity, and the economies that employ us all have the potential to evolve to prevent environmental change and to protect our hearts and minds through thoughtful interventions. However, we must design with intention for what the future may bring.
We must also remain nimble to embrace new opportunities that will bring us closer to our 2030 targets as they arise. For example, technology is advancing at a dizzying pace. Investments in information, communication infrastructure and technology, and topical areas such as mobile health, artificial intelligence, and precision medicine portend opportunities in the near future—before 2030, certainly—although they may not be imaginable today. Creating space to act on innovations as they evolve will be essential to achieving our goals.
Perhaps most indelible in the quest to achieve these goals, however, are the strategic liaisons that we will develop across disciplines and sectors working toward these goals. Building on its triad of science, advocacy, and volunteerism with global reach, the AHA brings unique contributions to help move us all toward a world of equitable, longer, healthier lives and well-being.
Footnotes
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
This advisory was approved by the American Heart Association Science Advisory and Coordinating Committee on December 20, 2019, and the American Heart Association Executive Committee on January 22, 2020. A copy of the document is available at https://professional.heart.org/statements by using either “Search for Guidelines & Statements” or the “Browse by Topic” area. To purchase additional reprints, call 215-356-2721 or Meredith.Edelman@wolterskluwer.com.
The American Heart Association requests that this document be cited as follows: Angell SY, McConnell MV, Anderson CAM, Bibbins-Domingo K, Boyle DS, Capewell S, Ezzati M, De Ferranti S, Gaskin DJ, Goetzel RZ, Huffman MD, Jones M; Khan YM, MD, Kim S, Kumanyika SK, McCray AT, Merritt RK, Milstein B, Mozaffarian D, Norris T, Roth GA, Sacco RL, Saucedo JF, Shay CM, Siedzik D; Saha S, Warner JJ. The American Heart Association 2030 Impact Goal: a presidential advisory from the American Heart Association. Circulation. 2020;141:e120-e138. doi: 10.1161/CIR.0000000000000758
The expert peer review of AHA-commissioned documents (eg, scientific statements, clinical practice guidelines, systematic reviews) is conducted by the AHA Office of Science Operations. For more on AHA statements and guidelines development, visit https://professional.heart.org/statements. Select the “Guidelines & Statements” drop-down menu, then click “Publication Development.”
Contributor Information
Sonia Y. Angell, College of Physicians and Surgeons of Columbia University.
Michael V. McConnell, Verily Life Sciences, Google Health, Stanford University.
Cheryl A.M. Anderson, University of California at San Diego.
Kirsten Bibbins-Domingo, University of California, San Francisco.
Douglas S. Boyle, Retired.
Simon Capewell, University of Liverpool (United Kingdom).
Majid Ezzati, Imperial College London School of Public Health (United Kingdom).
Sarah de Ferranti, Children's Hospital Boston.
Darrell J. Gaskin, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins Center for Health Disparities Solutions.
Ron Z. Goetzel, Johns Hopkins Bloomberg School of Public Health.
Mark D. Huffman, Northwestern University Feinberg School of Medicine.
Marsha Jones, Marsha Jones, PNC.
Yosef M. Khan, American Heart Association.
Sonia Kim, Healthier Generation.
Shiriki K. Kumanyika, University of Pennsylvania School of Medicine.
Alexa T. McCray, Harvard University.
Robert K. Merritt, Centers for Disease Control and Prevention.
Bobby Milstein, ReThink Health.
Dariush Mozaffarian, Friedman School of Nutrition Science & Policy, Tufts University.
Tyler Norris, Well Being Trust.
Gregory A. Roth, University of Washington.
Ralph L. Sacco, University of Miami.
Jorge F. Saucedo, Medical College of Wisconsin.
Christina M. Shay, American Heart Association.
David Siedzik, Broad Institute of MIT and Harvard.
Somava Saha, Institute for Healthcare Improvement (IHI).
John J. Warner, University of Texas Southwestern Medical Center.
REFERENCES
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al. ; on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2019 update: a report from the American Heart Association. Circulation. 2019; 139:e56–e528. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 2.Global Status Report on Noncommunicable Diseases. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 3.Dagenais GR, Leong DP, Rangarajan S, Lanas F, Lopez-Jaramillo P, Gupta R, Diaz R, Avezum A, Oliveira GBF, Wielgosz A, et al. Variations in common diseases, hospital admissions, and deaths in middle-aged adults in 21 countries from five continents (PURE): a prospective cohort study [published online September 3, 2019]. Lancet. doi: 10.1016/S0140-6736(19)32007-0. https://linkinghub.elsevier.com/retrieve/pii/S0140-6736(19)32007-0. [DOI] [PubMed] [Google Scholar]
- 3a.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. ; on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 4.Robine JM, Ritchie K. Healthy life expectancy: evaluation of global indicator of change in population health. BMJ. 1991;302:457–60. doi: 10.1136/bmj.302.6774.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369:448–457. doi: 10.1056/NEJMra1201534 [DOI] [PubMed] [Google Scholar]
- 7.US Burden of Disease Collaborators, Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, Lee A, Khan AR, Ahmadi A, Ferrari AJ, et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319:1444–1472. doi: 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Disability-Adjusted Life Years and Healthy Life Expectancy 1990–2017. Seattle, Washington: Institute for Health Metrics and Evaluation (IHME), 2018. http://ghdx.healthdata.org/record/ihme-data/gbd-2017-dalys-and-hale-1990-2017. Accessed January 16, 2020. [Google Scholar]
- 9.Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86:347–354. [PMC free article] [PubMed] [Google Scholar]
- 10.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. ; on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 11.Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. doi: 10.1001/jama.2012.339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Life-time risk and years lived free of total cardiovascular disease. JAMA. 2012;308:1795–1801. doi: 10.1001/jama.2012.14312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, Sweis RN, Lloyd-Jones DM. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018;3:280–287. doi: 10.1001/jamacardio.2018.0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pool LR, Ning H, Huffman MD, Reis JP, Lloyd-Jones DM, Allen NB. Association of cardiovascular health through early adulthood and health-related quality of life in middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Prev Med. 2019;126:105772. doi: 10.1016/j.ypmed.2019.105772 [DOI] [PubMed] [Google Scholar]
- 15.Allen NB, Zhao L, Liu L, Daviglus M, Liu K, Fries J, Shih YT, Garside D, Vu TH, Stamler J, et al. Favorable cardiovascular health, compression of morbidity, and healthcare costs: forty-year follow-up of the CHA study (Chicago Heart Association Detection Project in Industry). Circulation. 2017;135:1693–1701. doi: 10.1161/CIRCULATIONAHA.116.026252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yaffe K, Vittinghoff E, Pletcher MJ, Hoang TD, Launer LJ, Whitmer R, Coker LH, Sidney S. Early adult to midlife cardiovascular risk factors and cognitive function. Circulation. 2014;129:1560–1567. doi: 10.1161/CIRCULATIONAHA.113.004798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kronish IM, Carson AP, Davidson KW, Muntner P, Safford MM. Depressive symptoms and cardiovascular health by the American Heart Association’s definition in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. PLoS One. 2012;7:e52771. doi: 10.1371/journal.pone.0052771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rasmussen-Torvik LJ, Shay CM, Abramson JG, Friedrich CA, Nettleton JA, Prizment AE, Folsom AR. Ideal cardiovascular health is inversely associated with incident cancer: the Atherosclerosis Risk In Communities study. Circulation. 2013;127:1270–1275. doi: 10.1161/CIRCULATIONAHA.112.001183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mathers CD, Sadana R, Salomon JA, Murray CJ, Lopez AD. Healthy life expectancy in 191 countries, 1999. Lancet. 2001;357:1685–1691. doi: 10.1016/S0140-6736(00)04824-8 [DOI] [PubMed] [Google Scholar]
- 20.GBD DALYs, HALE Collaborators, Murray CJ, Barber RM, Foreman KJ, Abbasoglu Ozgoren A, Abd-Allah F, Abera SF, Aboyans V, Abraham JP, Abubakar I, Abu-Raddad LJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–91. doi: 10.1016/S0140-6736(15)61340-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20a.World Health Organization. Health topics: health equity. https://www.who.int/topics/health_equity/en/. Accessed January 16, 2020. [Google Scholar]
- 21.Constitution of the World Health Organization. Geneva, Switzerland: World Health Organization; 1995. [Google Scholar]
- 22.Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73:539–548. doi: 10.1037/0022-006X.73.3.539 [DOI] [PubMed] [Google Scholar]
- 23.Diener E Assessing subjective well-being: progress and opportunities. Soc indicators Res. 1994;31:103–157. [Google Scholar]
- 24.Prilleltensky I Promoting well-being: time for a paradigm shift in health and human services1. Scand J Public Health Suppl. 2005;66:53–60. doi: 10.1080/14034950510033381 [DOI] [PubMed] [Google Scholar]
- 25.Boehm JK, Peterson C, Kivimaki M, Kubzansky L. A prospective study of positive psychological well-being and coronary heart disease. Health Psychol. 2011;30:259–267. doi: 10.1037/a0023124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arora A, Spatz E, Herrin J, Riley C, Roy B, Kell K, Coberley C, Rula E, Krumholz HM. Population well-being measures help explain geographic disparities in life expectancy at the county level. Health Aff (Millwood). 2016;35:2075–2082. doi: 10.1377/hlthaff.2016.0715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. Arch Gen Psychiatry 2004;61:1126–1135. doi: 10.1001/archpsyc.61.11.1126 [DOI] [PubMed] [Google Scholar]
- 28.Riley C, Roy B, Herrin J, Spatz E, Silvestri MT, Arora A, Kell KP, Rula EY, Krumholz HM. Do pregnant women living in higher well-being populations in the USA experience lower risk of preterm delivery? A cross-sectional study. BMJ Open. 2019;9:e024143. doi: 10.1136/bmjopen-2018-024143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caspi A, Harrington H, Moffitt TE, Milne BJ, Poulton R. Socially isolated children 20 years later: risk of cardiovascular disease. Arch Pediatr Adolesc Med. 2006;160:805–811. doi: 10.1001/archpedi.160.8.805 [DOI] [PubMed] [Google Scholar]
- 30.Cohen S Social relationships and health. Am Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- 31.Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C. Purpose in life and reduced risk of myocardial infarction among older U.S. adults with coronary heart disease: a two-year follow-up. J Behav Med. 2013;36:124–133. doi: 10.1007/s10865-012-9406-4 [DOI] [PubMed] [Google Scholar]
- 32.Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2016;78:122–133. doi: 10.1097/PSY.0000000000000274 [DOI] [PubMed] [Google Scholar]
- 33.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–756. doi: 10.1097/PSY.0b013e31818105ba [DOI] [PubMed] [Google Scholar]
- 34.Kubzansky LD, Sparrow D, Vokonas P, Kawachi I. Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the Normative Aging Study. Psychosom Med. 2001;63:910–916. doi: 10.1097/00006842-200111000-00009 [DOI] [PubMed] [Google Scholar]
- 35.Roy B, Diez-Roux AV, Seeman T, Ranjit N, Shea S, Cushman M. Association of optimism and pessimism with inflammation and hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA). Psychosom Med. 2010;72:134–140. doi: 10.1097/PSY.0b013e3181cb981b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roy B, Riley C, Sinha R. Emotion regulation moderates the association between chronic stress and cardiovascular disease risk in humans: a cross-sectional study [published online August 7, 2018]. Stress. 2018:1–8. doi: 10.1080/10253890.2018.1490724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boehm JK, Kubzansky LD. The heart’s content: the association between positive psychological well-being and cardiovascular health. Psychol Bull. 2012;138:655–691. doi: 10.1037/a0027448 [DOI] [PubMed] [Google Scholar]
- 38.Kubzansky LD, Park N, Peterson C, Vokonas P, Sparrow D. Healthy psychological functioning and incident coronary heart disease: the importance of self-regulation. Arch Gen Psychiatry 2011;68:400–408. doi: 10.1001/archgenpsychiatry.2011.23 [DOI] [PubMed] [Google Scholar]
- 39.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005 [DOI] [PubMed] [Google Scholar]
- 40.Tindle HA, Chang YF, Kuller LH, Manson JE, Robinson JG, Rosal MC, Siegle GJ, Matthews KA. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation. 2009;120:656–662. doi: 10.1161/CIRCULATIONAHA.108.827642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roy B, Riley C, Herrin J, Spatz E, Hamar B, Kell KP, Rula EY, Krumholz H. Associations between community well-being and hospitalization rates: results from a cross-sectional study within six US states. BMJ Open. 2019;9:e030017. doi: 10.1136/bmjopen-2019-030017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385:640–648. doi: 10.1016/S0140-6736(13)61489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ryff CD, Singer BH, Dienberg Love G. Positive health: connecting well-being with biology. Philos Trans R Soc Lond B Biol Sci. 2004;359:1383–1394. doi: 10.1098/rstb.2004.1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Steptoe A, Wardle J, Marmot M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proc Natl Acad Sci U S A. 2005;102:6508–6512. doi: 10.1073/pnas.0409174102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Steptoe A, O’Donnell K, Badrick E, Kumari M, Marmot M. Neuroendocrine and inflammatory factors associated with positive affect in healthy men and women: the Whitehall II study. Am J Epidemiol. 2008;167:96–102. doi: 10.1093/aje/kwm252 [DOI] [PubMed] [Google Scholar]
- 46.Diener E The Science of Well-Being: The Collected Works of Ed Diener. Dordrecht, Netherlands: Springer; 2009. [Google Scholar]
- 47.Graham C Happiness for All? Unequal Hopes and Lives in Pursuit of the American Dream. Princeton, NJ: Princeton University Press; 2017. [Google Scholar]
- 48.Kottke TE, Stiefel M, Pronk NP “Well-being in all policies”: promoting cross-sectoral collaboration to improve people’s lives. Prev Chronic Dis. 2016;13:E52. doi: 10.5888/pcd13.160155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robert Wood Johnson Foundation. Advancing well-being in an inequitable world: insights from thought leaders. 2019. https://www.rwjf.org/en/library/research/2019/01/advancing-well-being-in-an-inequitable-world.html. Accessed January 16, 2020. [Google Scholar]
- 50.Diener E, Seligman ME. Beyond money: toward an economy of well-being. Psychol Sci Public interest. 2004;5:1–31. doi: 10.1111/j.0963-7214.2004.00501001.x [DOI] [PubMed] [Google Scholar]
- 51.Stone AA, Mackie C. Subjective well-being: measuring happiness, suffering, and other dimensions of experience. In: Stone AA, Mackie C, eds. Subjective Well-Being: Measuring Happiness, Suffering, and Other Dimensions of Experience. Washington, DC: National Research Council, National Academies Press; 2013. [PubMed] [Google Scholar]
- 52.Roy EA. New Zealand “wellbeing” budget promises billions to care for most vulnerable. The Guardian. 2019. https://www.theguardian.com/world/2019/may/30/new-zealand-wellbeing-budget-jacinda-ardern-unveils-billions-to-care-for-most-vulnerable. Accessed January 16, 2020. [Google Scholar]
- 53.Sturgeon N Why governments should prioritize well-being. 2019. https://www.ted.com/talks/nicola_sturgeon_why_governments_should_prioritize_well_being/transcript?language=en. Accessed January 16, 2020. [Google Scholar]
- 54.Rethink Health. Negotiating a well-being portfolio. 2018. https://www.google.com/search?client=firefox-b-1-d&q=Negotiating+a+well-being+portfolio. Accessed January 16, 2020. [Google Scholar]
- 55.Norris T Reclaiming well-being in America: the vital conditions that make people and places healthier and more resilient. National Civic Review. https://www.nationalcivicleague.org/ncr-article/reclaiming-well-being-in-america-the-vital-conditions-that-make-people-and-places-healthier-and-more-resilient/. Accessed January 16, 2020. [Google Scholar]
- 56.NCVHS measurement framework for community health and well-being, V4. https://www.ncvhs.hhs.gov/wp-content/uploads/2013/12/NCVHS-Measurement-Framework-V4-Jan-12-2017-for-posting-FINAL.pdf. Accessed January 16, 2020. [Google Scholar]
- 57.Cantril H The Pattern of Human Concerns. New Brunswick, NJ: Rutgers University Press; 1965. [Google Scholar]
- 58.Graham C, Laffan K, Pinto S. Well-being in metrics and policy. Science. 2018;362:287–288. doi: 10.1126/science.aau5234 [DOI] [PubMed] [Google Scholar]
- 59.Roy B, Riley C, Sears L, Rula EY. Collective well-being to improve population health outcomes: an actionable conceptual model and review of the literature. Am J Health Promot. 2018;32:1800–1813. doi: 10.1177/0890117118791993 [DOI] [PubMed] [Google Scholar]
- 60.Riley C, Roy B, Herrin J, Spatz ES, Arora A, Kell KP, Rula EY, Krumholz HM. Association of the overall well-being of a population with health care spending for people 65 years of age or older. JAMA Netw Open. 2018;1:e182136. doi: 10.1001/jamanetworkopen.2018.2136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gandy WM, Coberley C, Pope JE, Rula EY. Well-being and employee health-how employees’ well-being scores interact with demographic factors to influence risk of hospitalization or an emergency room visit. Popul Health Manag. 2014;17:13–20. doi: 10.1089/pop.2012.0120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gallup. Understanding how Gallup uses the Cantril Scale. 2012. https://news.gallup.com/poll/122453/understanding-gallup-uses-cantril-scale.aspx. Accessed January 16, 2020. [Google Scholar]
- 62a.Well Being in the Nation Network. Well-being of people: people’s perception of their well-being. https://www.winmeasures.org/statistics/win-measures/us-wellbeing-of-people. Accessed January 22, 2020. [Google Scholar]
- 63.Spatz ES, Herrin J, Riley CL, Roy B, Witters D, Coberley C, Krumholz HM. Population well-being and cardiovascular disease [abstract 335]. Circ Cardiovasc Qual Outcomes. 2014;7:A335. [Google Scholar]
- 64.Goetzel RZ, Ozminkowski RJ, Sederer LI, Mark TL. The business case for quality mental health services: why employers should care about the mental health and well-being of their employees. J Occup Environ Med. 2002;44:320–330. doi: 10.1097/00043764-200204000-00012 [DOI] [PubMed] [Google Scholar]
- 65.Institute for Health and Productivity Studies. Holding company leaders accountable for employees’ health and well-being at Lincoln Industries. 2015. https://www.jhsph.edu/research/centers-and-institutes/institute-for-health-and-productivity-studies/ihps-blog/holding-company-leaders-accountable-for-employees-health-and-well-being-at-lincoln-industries. Accessed January 16, 2020. [Google Scholar]
- 66.Harter JK, Harter J, Rath TH. Wellbeing: The Five Essential Elements: New York, NY: Gallup Press; 2010. [Google Scholar]
- 67.Helliwell J, Layard R, Sachs J. World happiness report 2019. 2019. https://worldhappiness.report/ed/2019/. Accessed January 16, 2020. [Google Scholar]
- 68.National Academies of Sciences, Engineering, and Medicine. Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 69.Castrucci B, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Health Affairs Blog. 2019. https://www.healthaffairs.org/do/10.1377/hblog20190115.234942/full/. Accessed January 16, 2020. [Google Scholar]
- 70.Pronk NP, Kottke T, Milstein B, Rossom R, Stiefel M. Health and well-being: a brief to inform development of Healthy People 2030. 2019. https://webcache.googleusercontent.com/search?q=cache:iMsGkIiMNu4J:https://www.healthypeople.gov/sites/default/files/HP2030_Committee-Combined-Issue%2520Briefs_2019-508c.pdf+&cd=1&hl=en&ct=clnk&gl=us&client=firefox-b-1-d. Accessed January 16, 2020. [Google Scholar]
- 71.Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, Jacobs DR Jr, Kraus WE, Kris-Etherton PM, Krummel DA, et al. ; on behalf of the American Heart Association Council on Epidemiology and Prevention, Council on Nutrition, Physical Activity and Metabolism, Council on Clinical Cardiology, Council on Cardiovascular Disease in the Young, Council on the Kidney in Cardiovascular Disease, Council on Peripheral Vascular Disease, and the Advocacy Coordinating Committee. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.World Health Organization. Health topics: health financing. https://www.who.int/health-topics/health-financing#tab=tab_3. Accessed January 16, 2020. [Google Scholar]
- 73.Centers for Disease Control and Prevention. Vital signs: avoidable deaths from heart disease, stroke, and hypertensive disease-United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2013;62:721–727. [PMC free article] [PubMed] [Google Scholar]
- 74.Vaughan AS, Ritchey MD, Hannan J, Kramer MR, Casper M. Widespread recent increases in county-level heart disease mortality across age groups. Ann Epidemiol. 2017;27:796–800. doi: 10.1016/j.annepidem.2017.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Garcia MC, Rossen LM, Bastian B, Faul M, Dowling NF, Thomas CC, Schieb L, Hong Y, Yoon PW, Iademarco MF. Potentially excess deaths from the five leading causes of death in metropolitan and nonmetropolitan counties–United States, 2010–2017. MMWR Morb Mortal Wkly Rep. 2019;68:1–11. doi: 10.15585/mmwr.ss6810a1 [DOI] [PubMed] [Google Scholar]
- 76.Singh GK, Daus GP, Allender M, Ramey CT, Martin EK, Perry C, Reyes AAL, Vedamuthu IP. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935–2016. Int J MCH AIDS. 2017;6:139–164. doi: 10.21106/ijma.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.The RURAL Cohort Study. http://www.theruralstudy.org. Accessed January 16, 2020. [Google Scholar]
- 78.George MG, Tong X, Bowman BA. Prevalence of cardiovascular risk factors and strokes in younger adults. JAMA Neurol. 2017;74:695–703. doi: 10.1001/jamaneurol.2017.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78a.Kania J, Kramer M, Senge P. The waters of systems change. June 2018. https://www.fsg.org/publications/water_of_systems_change. Accessed January 16, 2020. [Google Scholar]
- 79.Nulu S, Bukhman G, Kwan GF. Rheumatic heart disease: the unfinished global agenda. Cardiol Clin. 2017;35:165–180. doi: 10.1016/j.ccl.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 80.Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, Nugent R, eds. Disease Control Priorities: Improving Health and Reducing Poverty: Volume 9, Disease Control Priorities. 3rd ed. Washington, DC: World Bank; 2018. [PubMed] [Google Scholar]
- 81.OECD. Health at a Glance 2017. 2017. https://www.oecd-ilibrary.orghealth-at-a-glance-2017_5jfqgv50kpjk. Accessed January 16, 2020. [Google Scholar]
- 82.Office of Disease Prevention and Health Promotion. Healthy people 2020: social determinants of health. 2019. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health.Accessed January 16, 2020. [Google Scholar]
- 83.Taylor LA, Tan AX, Coyle CE, Ndumele C, Rogan E, Canavan M, Curry LA, Bradley EH. Leveraging the social determinants of health: what works? PLoS One. 2016;11:e0160217. doi: 10.1371/journal.pone.0160217 [DOI] [PMC free article] [PubMed] [Google Scholar]