Abstract
Background
Polycystic ovary syndrome (PCOS) is a complex condition, impacting cardio-metabolic and reproductive health, mental health and health-related quality of life. The physical health benefits of exercise for women with PCOS are well-established and exercise is increasingly being recognised as efficacious for improving psychological wellbeing. The aim of this review was to summarise the evidence regarding the effectiveness of exercise interventions on mental health outcomes in women with PCOS.
Methods
A systematic search of electronic databases was conducted in March of 2020. Trials that evaluated the effect of an exercise intervention on mental health or health-related quality of life outcomes in reproductive aged women with diagnosed PCOS were included. Methodological quality was assessed using the modified Downs and Black checklist. Primary outcomes included symptoms of depression and anxiety, and health-related quality of life.
Results
Fifteen articles from 11 trials were identified and deemed eligible for inclusion. Exercise demonstrated positive improvements in health-related quality of life in all of the included studies. Half of included studies also reported significant improvements in depression and anxiety symptoms. There was large variation in methodological quality of included studies and in the interventions utilised.
Conclusions
The available evidence indicates that exercise is effective for improving health-related quality of life and PCOS symptom distress. Exercise also shows some efficacy for improving symptoms and/or prevalence of depression and anxiety in women with PCOS. However, due to large heterogeneity of included studies, conclusions could not be made regarding the impact of exercise intervention characteristics. High-quality trials with well reported exercise intervention characteristics and outcomes are required in order to determine effective exercise protocols for women with PCOS and facilitate translation into practice.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-12280-9.
Keywords: Exercise, physical activity, mental health, health-related quality of life, depression, anxiety
Background
Polycystic Ovary Syndrome (PCOS) is a complex and common condition, affecting 8-13% of reproductive aged women [1] and carries a major disease burden across cardio-metabolic and reproductive health. PCOS is characterised by hyperandrogenism, ovulatory dysfunction and polycystic ovary morphology [2] and although not recognised in the diagnostic criteria, insulin resistance is considered a key aetiological feature, contributing to the severity of PCOS features [3]. PCOS is the leading cause of anovulatory infertility among reproductive-aged women [4] and has significant metabolic features including insulin resistance, obesity, and an increased risk of developing type 2 diabetes [5–8]. PCOS is also known to be related to diminished mental health, including increased symptoms of depression, anxiety and lower health-related quality of life, with these comorbidities occurring and having impact across the lifespan [9].
Many chronic illnesses have an impact on mental health and are associated with a reduction in quality of life and an increase in a range of psychological symptoms [9–11]. Given the clinical features of PCOS, it is perhaps not surprising that women with PCOS experience mental health problems and mood dysfunction to a greater degree than women without PCOS [12]. Compared to age and weight matched control women [13, 14], and those with other chronic conditions including diabetes and coronary heart disease [15], women with PCOS have poorer mental health and health-related quality of life with many reporting increased symptoms of anxiety and depression. Fears regarding infertility, body image concerns, low self-esteem and coping with the condition may all contribute to poorer mental health among these women [16]. In addition, the symptoms associated with PCOS often cause distress, leading to a reduced quality of life [17]. Symptom distress is often measured in women with PCOS using the polycystic ovary questionnaire (PCOSQ) which is a reliable instrument for measuring health-related quality of life in women with PCOS [17].
In a healthy population, exercise is an effective means of promoting, improving and managing mental health [18]. This is also the case for populations with chronic conditions [19] and in overweight women [20]. The specific interaction between exercise and mental health in PCOS has not been explored in depth, but the limited existing research indicates a positive effect of exercise for improving mental health and health-related quality of life in women with PCOS [21–24]. Women with PCOS who are more physically active report fewer symptoms of depression than sedentary women with PCOS [9], although active women with PCOS report higher symptoms of depression than active women without PCOS [9].
The current international evidence-based guidelines for the assessment and management of PCOS recommend 150 minutes per week of moderate intensity exercise or 75 minutes per week of vigorous intensity exercise in all women with PCOS, in order to improve general health and quality of life [1]. It is well documented that exercise elicits a number of health benefits including increased insulin sensitivity, increased cardiorespiratory fitness, improved menstrual cyclicity and improved mental health [21, 22, 25, 26]. Despite the positive effects of exercise, low compliance with these guidelines because of general barriers (time limitations, low enjoyment experienced with exercise) and PCOS-specific barriers (low confidence, physical limitations) to exercise [9, 21], means that many women with PCOS remain sedentary or insufficiently active (do not meet the minimum exercise recommendations) [27]. Enhancing engagement in exercise is vital to increase adherence to exercise recommendations and increase the potential health and mental health benefits of exercise [16]. This systematic review will synthesise the existing literature and aim to determine the effectiveness of exercise for improving symptoms of mental health and health-related quality of life in women with PCOS.
Methods
Protocol and registration
This systematic review was registered on the International Prospective Register of Systematic Reviews (CRD42019118657) and conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [28] and
Information sources & search
An electronic database search was initially conducted in December 2018 and updated in October 2021 using Ovid Medline and EBSCOhost (PsycINFO, MEDLINE, SPORTDiscus, CINAHL), with no date or language restrictions. The search strategy included Medical Subject Heading (MeSH) terms and keywords relating to mental health, health-related quality of life, physical activity or exercise interventions and PCOS. An example of a search strategy is reported in Supplementary Table 1 and was adapted for each database. The search terms were broad in order to capture publications that may have included mental health or health-related quality of life as secondary outcomes. Reference lists of relevant articles were searched to identify additional eligible studies.
Eligibility criteria
Included studies involved women of reproductive age (18-45 years of age) and with a diagnosis of PCOS using any established diagnostic criteria (e.g., Rotterdam criteria, National Institute for Health [NIH]). Randomised controlled trials (RCT), non-randomised controlled trials and uncontrolled trials were included. Exercise interventions of two weeks or greater were included in this review (Table 1). Exercise intensity was classified as moderate (55 to <70% HRmax or 40 to < 60% VO2max), vigorous (70 to <90% HRmax or 60 to <85% VO2max) or high intensity (≥90% HRmax or ≥85% VO2max) [29].
Table 1.
Eligibility criteria for study inclusion
| Participants | Intervention | *Comparison | Outcome | Study Design |
|---|---|---|---|---|
|
Diagnosed with PCOS using any established definition Reproductive years, aged 18–45 |
Any intervention that included exercise of: Any type or intensity Duration >2 weeks |
No exercise Alternative therapies (e.g. acupuncture, cognitive behavioural therapy) Medications |
Depression symptoms Anxiety symptoms HRQoL (SF-36) PCOS symptom distress (PCOSQ) |
RCT Non-RCT Cohort Case Control Parallel Clinical trial |
PCOS – Polycystic Ovary Syndrome HRQoL – Health-Related Quality of Life, SF-36 – Short Form 36, PCOSQ – Polycystic Ovary Syndrome Questionnaire, RCT – Randomised Controlled Trial.
*Studies with no comparison were also included in this review.
Outcomes
The outcome measures were health-related quality of life as assessed by either the polycystic ovary syndrome questionnaire (PCOSQ) or the short form 36 (SF-36) questionnaire and symptoms of depression and anxiety assessed by any validated questionnaire (Table 1). Trials that did not report at least one of these outcome measures were not included in this review.
Study selection and data extraction
After duplicates were removed, two reviewers (R.P. and R.B.) independently screened each article by title and abstract. Following removal of irrelevant studies, full-text versions of the remaining publications were assessed for inclusion eligibility. Data relating to study design, participant and intervention characteristics, and outcome measures were extracted independently by reviewers using a pre-determined data extraction form. At each stage of the screening process, discrepancies were resolved by consensus or by a third reviewer (N.S.).. Due to poor reporting of intervention characteristics and outcome measures and large heterogeneity in the interventions, a quantitative synthesis was not feasible. Study results were therefore summarised as statistically significant within group changes (p<0.05).
Risk of bias
The modified Downs and Black checklist for the assessment of methodological quality was used to evaluate the quality of included studies [30] (Supplementary Table 2). Questions regarding blinding of participants were removed as blinding is not possible in exercise intervention trials; however, blinding of outcome assessors was included. This checklist included 21 items with each item receiving a 0 or a 1 response and assesses reporting, internal and external validity or bias, and power. Higher scores indicated better methodological quality. Inter-reviewer discrepancies concerning the methodological quality of included studies were resolved by consensus.
Results
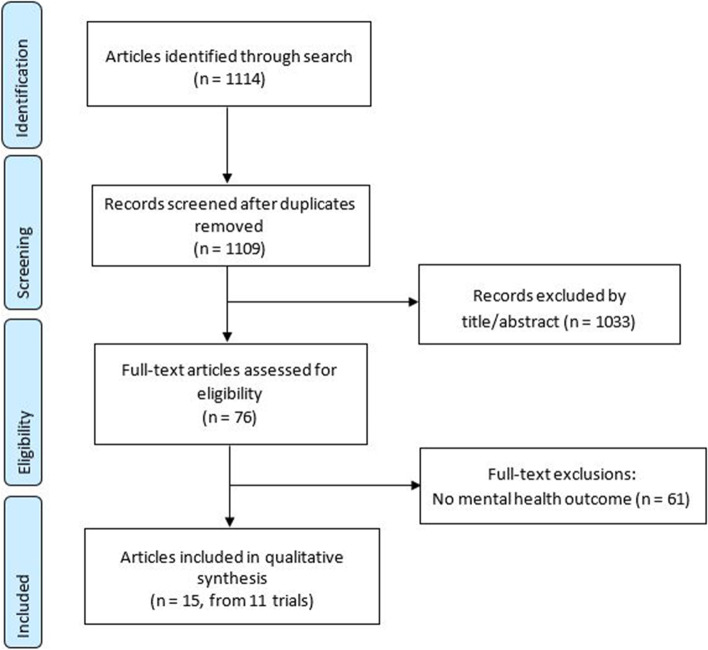
The database searches identified 1114 references. Six articles were removed due to duplication and 1033 articles were deemed irrelevant after title and abstract screening. Of the 76 papers that were deemed eligible for full-text screening, 61 were excluded due to having no relevant outcome measures (Fig. 1). The remaining 15 publications were deemed eligible for inclusion and were assessed for methodological quality, with results reported in Supplementary Table 2. These 15 publications were the result of 11 trials. In cases where multiple publications arose from one trial, data were grouped together. No additional studies were identified from the searches of reference lists of relevant studies. The characteristics of the included trials are presented in Table 2 and summarised below.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) study selection flow diagram
Table 2.
Summary of studies identified for systematic review detailing participant and intervention characteristics, measures used and psychological outcomes.
| Study | QA scorea | Study Design | Exercise Intervention N (total N) | Participant Characteristics | Exercise Intervention(s) Characteristics | Comparison(s) | Measures | Mental health and health-related quality of life outcomes |
|---|---|---|---|---|---|---|---|---|
| Arentz et al. 2017 [31] | 18 | RCT | 62 (122) |
Age: 28.9 ± 5.6 years BMI: 35.2 ± 6.8 kg/m2 PCOS diagnostic criteria: Rotterdam |
Type: Aerobic Frequency: N/R (90-150mins/week) Intensity: 60-90% HRmax Duration: 12 weeks Supervision: Partial |
Herbal medicine + lifestyle intervention |
PCOSQ DASS-21 |
bSignificant improvements were seen for all domains of the PCOSQ and DASS-21 in the herbal medicine plus lifestyle group, significant improvements only for infertility (p=0.001), weight (p=0.01), menstrual problems (p=0.02) and emotions (p=0.04) in the lifestyle only group. No significant changes in DASS-21 scores in the lifestyle only group. |
| Cooney et al. 2018 [32] | 13 | Pilot RCT | 8 (15) |
Age: 32 (27-34) years BMI: 35 (31-40) kg/m2 PCOS diagnostic criteria: NIH |
Type: Aerobic Frequency: N/R (50-175mins/week) Intensity: N/R Duration: 16 weeks Supervision: None |
CBT (weekly 30min CBT sessions) + lifestyle modification |
PCOSQ CES-D |
Clinically but not statistically significant improvements in all domains of the PCOSQ (≥0.5 point increase) with the exception of menstrual problems in the overall group. Statistically significant improvement in depression scores (p=0.01) in the overall group, with no differences between groups (p=0.68). |
| Costa et al. 2018 [33] | 16 | RCT | 14 (27) |
Age: 27.6 ± 4.5 years BMI: 32 ± 4.2 kg/m2 PCOS diagnostic criteria: Rotterdam |
Type: Aerobic Frequency: 3/week Intensity: 60-85% HRmax Duration: 16 weeks Supervision: Full |
No intervention control group | SF-36 | Significant improvements in physical functioning (p=0.004), general health (p=0.012) and mental health (p=0.042) domain scores compared to baseline. |
| De Frène et al. 2015 [34] | 7 | Single arm study | 23 |
Age: 29 (5) years BMI: 33.7 (7.8) kg/m2 PCOS diagnostic criteria: Rotterdam |
Type: Aerobic Frequency: N/R Intensity: N/R Duration: 24 weeks Supervision: None |
None | PCOSQ | Significant positive effect on total PCOSQ score (p=<0.001) as well as emotions (p=<0.01), weight (p=<0.001), body hair (p=<0.05) and infertility (p=<0.001) domain scores. |
| Ladson et al. 2011 [35] | 16 | RCT | 16 (26) |
Age: 28.8 ± 4.6 years BMI: 38.3 ± 8 kg/m2 PCOS diagnostic criteria: NIH |
Type: Aerobic Frequency: ≥2/week Intensity: N/R Duration: 26 weeks Supervision: Partial |
Metformin + caloric restriction & exercise | PCOSQ | Significant improvements in emotions (p=0.008) and weight (p=0.002) domain scores. |
|
Lara et al. 2015 [36] & Ramos et al. 2016 [37] |
12 13 |
Case-control | 43 |
Age: 27.9 ± 5.3 years BMI: 27.9 ± 5.5 kg/m2 PCOS diagnostic criteria: Rotterdam |
Type: RT Frequency: N/R Intensity: 60-85% of 1RM Duration: 16 weeks Supervision: Full |
Non-PCOS |
HADS SF-36 |
Significant improvements in both anxiety (p=<0.01) and depression (p=<0.01) scores over time [36]. Significant improvements in SF-36 physical functioning domain (p=0.02) [37]. |
|
Legro et al. 2015 [24] & Dokras et al. 2016 [38] |
18 12 |
RCT | 49 (149) |
Age: 28.6 ± 3.4 years BMI: 35.1 ± 4.6 kg/m2 PCOS diagnostic criteria: Rotterdam |
Type: Aerobic Frequency: 5/week Intensity: N/R Duration: 16 weeks Supervision: None |
OCP or combined OCP + lifestyle intervention |
PCOSQ SF-36 PRIME-MD |
Significant positive effect on weight (p=<0.0001), infertility (p=<0.0001), menstrual problems (p=0.004) PCOSQ domains [24]. Significant improvement in general health (p=<0.05) and vitality (p=<0.05) domains of the SF-36. Significant decrease in the prevalence of anxiety (15.9 to 4.7%; p=0.02). Non-significant changes in the prevalence of depression (22.7 to 15.9%; p=0.17) [38]. |
| Ribeiro et al. 2019 [39] & Kogure et al. 2020 [40] |
17 17 |
RCT | CAT = 28, IAT = 29 (87) |
CAT = Age: 29.1 (5.3) years BMI: 28.4 (5.6) kg/m2 IAT = Age: 29.0 (4.3) years BMI: 28.7 (4.8) kg/m2 PCOS diagnostic criteria: Rotterdam |
Type: Aerobic Frequency: 3/week Intensity: CAT – 65-80% HRmax IAT – 70-90% HRmax Duration: 16 weeks Supervision: Full |
No intervention control group |
SF-36 HADS |
CAT – Significant improvements in physical functioning (p=0.022), role physical (p=<0.001), general health (p=<0.001), vitality (p=<0.001), social functioning (p=<0.001), role emotional (p=<0.001) and mental health (p=<0.001) domains of the SF-36. IAT – Significant improvements in physical functioning (p=<0.001), role physical (p=0.027), general health (p=<0.001), vitality (p=0.001), social functioning (p=<0.001), role emotional (p=0.011) and mental health (p=<0.001) domains of the SF-36 (36). Significant improvements in anxiety and depression scores (p=<0.05) in both the CAT and IAT groups [40]. |
| Stener-Victorin et al. 2013 [41] | 13 | RCT | 29 (44) |
Age: 29.9 ± 4.4 years BMI: 28.1 ± 7.4 kg/m2 Diagnostic criteria: Rotterdam |
Type: Aerobic Frequency: ≥3/week Intensity: N/R Duration: 16 weeks Supervision: None |
No intervention control group & acupuncture group |
MADRS-S BSA-S PCOSQ SF-36 |
No significant improvements in anxiety or depression. Significant improvements in PCOSQ domains for infertility (p=<0.05) and emotions (p=<0.001) and the role physical (p=<0.001) domain of the SF-36. |
| Thomson et al. 2010 [22] & Thomson et al. 2016 [42] |
12 12 |
RCT |
Aerobic only = 15 Aerobic + RT = 20 (49) |
Age: 29.3 ± 6.8 years BMI: 36.1 ± 4.8 kg/m2 Diagnostic criteria: Rotterdam |
Type: Aerobic only or combined aerobic & RT Frequency: 5/week Intensity: Aerobic = 60-80% HRmax, RT = 50-75% of 1RM Duration: 20 weeks Supervision: Partial |
cDiet only (energy restricted, high protein diet) |
CES-D PCOSQ |
Significant improvement in depression scores in all groups (p=≤0.001) with no effect of treatment (p=0.86). Significant improvements in PCOSQ domain scores for emotions (p=≤0.001), weight (p=≤0.001), menstrual problems (p=≤0.001), and infertility (p=≤0.001) for all groups. |
| Vizza et al. 2016 [23] | 19 | Pilot RCT | 7 (13) |
Age: 26.7 ± 7 years BMI: 41.3 ± 12.5 kg/m2 Diagnostic criteria: Rotterdam |
Type: RT Frequency: 2/week Intensity: N/R Duration: 12 weeks Supervision: Full |
No intervention control group |
PCOSQ SF-36 DASS-21 |
Significant improvements in the RT group compared to the control group for emotions (p=0.003), weight (p=0.04) and infertility (p=0.03) PCOSQ domains. Significant improvements in the RT group compared to the control group for physical functioning (p=0.02), vitality (p=0.02), social functioning (p=0.002), role emotional (p=0.009) and mental health (p=0.009) SF-36 domains. Significant improvements in the RT group compared to the control group for depression (p=0.01) and anxiety (p=0.03). |
Data presented as mean ± SD or median (IQR).
1RM – One Repetition Maximum, BMI – Body Mass Index, BSA-S – Brief Scale for Anxiety, CAT – Continuous Aerobic Training, CBT – Cognitive Behavioural Therapy, CES-D – Centre for Epidemiological Studies Depression scale, DASS-21 – Depression, Anxiety and Stress Scale 21, HADS – Hospital Anxiety and Depression Scale, HRmax – Maximum Heart Rate, IAT – Intermittent Aerobic Training, MADRS-S – Montgomery Åsberg Depression Rating Scale, N/R – Not Reported, OCP – Oral Contraceptive Pill, PCOSQ – Polycystic Ovary Syndrome Questionnaire, PRIME-MD - Primary Care Evaluation of Mental Disorders, QA – Quality Appraisal, RCT – Randomised Controlled Trial, RT – Resistance Training, SF-36 – Short Form 36.
aMethodological quality score from the Downs and Black checklist. Possible range of scores 0-21.
bData provided by author.
cAll groups received the diet intervention.
Study design and participants characteristics
Of the 11 included trials, nine were RCTs [22–24, 31–33, 35, 39, 41], one was a single arm study [34] and one was a case-control study [36]. Sample sizes ranged from 13 to 149 participants. The mean age of participants ranged from 26 to 33 years of age and the mean body mass index (BMI) ranged from 27.9 to 41.3kg/m2. Participants from nine trials were diagnosed with PCOS according to the Rotterdam criteria [22–24, 31, 33, 34, 36, 39, 41] and three trials according to the NIH criteria [32, 35]. Of the included trials, nine recruited only overweight and obese women with PCOS and all studies excluded women with chronic co-morbidities, such as diabetes and cardiovascular disease. One study included only women with a positive screen for depression symptoms [32]. Three studies excluded women who were taking medication treatment for depression [22, 31, 43], five studies did not exclude women who were taking anti-depressant medication [23, 24, 36, 39, 41] and two studies did not report on use of medication for mental health status [34, 35], as shown in Table 2.
Assessment of study quality
Scores from the modified Downs and Black checklist varied greatly with scores ranging from 7 to 19 on a 21-point scale, with a lower score indicating a poorer methodological quality. The most common issues were poor reporting of aspects of the intervention or the characteristics of participants lost to follow-up. The full assessment of methodological quality is presented in Supplementary Table 3.
Intervention characteristics
Aerobic exercise alone was delivered in eight out of the 11 trials [24, 31–35, 39, 41]. One study included an aerobic exercise group, a resistance training group and a combined aerobic and a resistance training group [22] and the final two studies delivered resistance training only [23, 36]. Of the included studies, only four of the interventions had full supervision by an exercise specialist [23, 33, 36, 39], three had partial supervision [22, 31, 35] and four had no supervision [24, 32, 34, 41]. The duration of the interventions varied from 12 to 26 weeks, with the number of sessions ranging from two to five per week. Exercise intensity was only adequately reported in five of the 11 included studies, all of which reported using moderate-vigorous intensity exercise. Adherence, classified as the percent of sessions attended in regards to the expected attendance, was reported in only three of the included studies. Two of these reported an average adherence of 81% [33] and 95% [23] for supervised sessions, with one of these trials also reporting an average of 51% for unsupervised session adherence [23]. The third study reported that on average, only 38% of participants in the lifestyle only group reported meeting their weekly exercise goal [32]. No adverse events were reported as a result of any of the exercise interventions.
Outcomes
Six of the included trials had a primary outcome of mental health and/or health-related quality of life. The remaining five trials included mental health and/or health-related quality of life as secondary outcome.
PCOS symptom distress
Of the studies included, eight used the PCOSQ to assess PCOS related distress, seven of which reported statistically significant improvements in a minimum of two domains. The PCOSQ is a validated questionnaire which assessed the multidimensional concept of health-related quality of life, encompassing five domains; emotions, hair growth, body weight, infertility and menstrual problems. A higher overall score indicates better function, and a change of 0.5 is considered clinically relevant [44]. Six studies reported statistically significant improvements in emotions [22, 23, 31, 34, 35, 41] weight [22–24, 31, 34, 35] and infertility domains [22–24, 31, 34, 41], three reported improvements in the menstrual problems domain [22, 24, 31] and one reported improvements in the body hair domain [34]. The eighth study did not report a statistically significant impact of exercise on PCOS related distress, but did report minimally important clinically significant improvements (≥0.5 point increase), in all domains for the cognitive behavioural therapy plus lifestyle group, and clinically significant increases in the weight and infertility domains for the lifestyle only group [32]. In total, the weight domain had the most clinically significant improvements with six studies reporting improvements ranging from 0.7 to 1.75 point increase in scores. Clinically significant improvements were also commonly reported in the emotions domain, with four studies reporting increases in scores of between 0.5 and 0.8 points. A large proportion of interventions that utilised a range of exercise intensities, doses, types and durations, resulted in significant improvements in multiple domains of the PCOSQ, therefore suggesting that regardless of these factors, exercise can improve health-related quality of life in regards to PCOS symptom distress.
Health-related quality of life
Six studies used SF-36 to determine the health-related quality of life of participants. The SF-36 measures eight dimensions of health; physical functioning, role limitations due to physical problems (role physical) , bodily pain, general health perception, vitality, social functioning, role limitations due to emotional problems (role emotional) and mental health [45]. Four studies reported statistically significant increases in the physical functioning domain [23, 37, 39, 43]. Three studies reported significant increases in general health [38, 39, 43], vitality [23, 38, 39] and mental health [23, 39, 43]. Two studies reported statistically significant improvements in role physical [39, 41], social functioning [23, 39] and role emotional domains [23, 39]. No studies reported statistically significant improvements in the bodily pain domain. Clinically meaningful improvements were most commonly reported for the role physical domain, with 4 studies showing clinically meaningful changes after an exercise intervention [37, 39, 41, 43], reporting increases in scores of 6.3 to 39.3. In regards to the SF-36, a change of score of 5 points or greater is considered clinically meaningful [46]. Improvements were also commonly reported for emotional and mental health domains with increases in scores of between 5.0 to 40.6, and 11.7 to 15.4 respectively. There were three studies that observed large improvements in multiple domains of the SF-36. Two of these studies used an aerobic exercise intervention of moderate to vigorous intensity, delivered three times per week for 16 weeks [39, 43], while the third study conducted a 12 week progressive resistance training program delivered twice per week [23]. In summary, many studies reported improvements in domains of the SF-36 as a result of various exercise interventions, however it appears that there were no common denominators in regards to exercise characteristics.
Depression
Eight studies measured the effect of an exercise intervention on depression symptoms, with five reporting significant reductions in depression scores. Two studies that reported improvements delivered an aerobic exercise intervention [32, 40], two delivered resistance training [23, 36] and the final study compared three interventions (diet only, diet and aerobic exercise and diet and combined exercise) [22], all of which resulted in improved depression scores. There were no obvious common denominators in regards to exercise characteristics between studies that did, and those that did not report improvements in symptoms of depression. One study that used the Depression Anxiety and Stress Scales (DASS-21) questionnaire reported significant changes in depression symptoms at post-intervention, in comparison to a no-intervention control group, after 12 weeks of supervised resistance training [23]. One study, reported significant decreases in depression symptoms following a combined diet and aerobic intervention, with average scores on the CES-D decreasing from 18.6 at baseline to 14.0 post-intervention [22]. A second study that used the CES-D included only women classified as possibly depressed (score of ≥16) at baseline, and reported large decreases in symptoms with average scores decreasing from 24 to 18 [32]. Lastly, both studies that used the HADS questionnaire reported significant improvements in depression scores from baseline, one of which utilised a resistance training intervention [36] and the second study utilised two different aerobic training programs, both of which reported significant improvements [39].
Anxiety
Six studies also examined symptoms of anxiety, three of which reported statistically significant within group reductions in symptoms after an exercise intervention [36, 38, 40]. A third study reported significant reductions in anxiety symptoms compared to a control group with scores reducing from 10.3 at baseline to 7.4 post-intervention [23]. Two studies reported the prevalence of anxiety at baseline and following an exercise intervention. One of these studies reported that 44.1% of participants had anxiety (according to the measures used) at baseline, which decreased to 23.2% after a 16 week resistance training intervention [36]. The second study reported a drop from 15.9 to 4.7% of women considered to have clinical anxiety after a 16 week aerobic exercise intervention [38].
Summary
In summary, exercise interventions reduced symptoms of depression and anxiety in half of the reviewed studies. Due to the large variety of training interventions, conclusions cannot be made regarding the impact of a specific type or intensity of an exercise intervention, compared to another.
Discussion
The current systemic review aimed to determine the effectiveness of exercise on mental health and health-related quality of life outcomes in women with PCOS. Exercise interventions appear to have positive effects on health-related quality of life and associated PCOS symptom distress as assessed by validated measures. The findings for mental health outcomes were less consistent, with a combination of positive and null findings regarding improvements in symptoms of anxiety and depression, although half of the included studies reported improvements in symptoms of anxiety and depression after an exercise intervention. The most common exercise program included various types of aerobic exercise of varying intensities, ranging from moderate to high intensity. Others included some form of resistance training program or a combination of resistance and aerobic exercise. Intervention duration and the inclusion of supervised exercise also varied among interventions. There did not appear to be any common exercise characteristics that could explain differences in symptoms of depression and anxiety, PCOS associated distress, or improvements in health-related quality of life outcomes.
This systematic review expands on an existing review of seven trials that found exercise to be beneficial for improving health-related quality of life, depression and anxiety in women with PCOS [21]. Future research is required however to provide further evidence of these benefits. Observed improvements resulted from various types of exercise, exercise intensities and concurrent therapies, making it difficult to determine the components of the intervention that contribute to improved outcomes. Studies included in this review were largely heterogeneous with varying interventions, concurrent therapies, sample sizes, study designs, comparator groups and methodological quality making the independent effect of any particular type of exercise intervention or characteristics difficult to assess. These variations prevented a meta-analysis from being conducted and limited the ability to form conclusions about the effectiveness of exercise on mental health and health-related quality of life in women with PCOS. In addition, poor reporting of exercise characteristics and the large variety of intensities, duration and frequency, limited the capacity to formulate more specific exercise recommendations for promoting mental health and health-related quality of life in women with PCOS, which limits the translation of these research findings into clinical practice.
The current international evidence based guidelines for the assessment and management of PCOS states that psychological factors, including anxiety and depression, should be screened, assessed and managed [1]. It is important to ensure positive well-being to increase quality of life but also to assist in promoting engagement and adherence to lifestyle interventions. Adherence to exercise interventions has been reported to be low in clinical settings among women with PCOS [35, 47, 48], it is crucial that future studies report measures of adherence to determine interventions that are more effective in maintaining the interest and enjoyment of participants. Very few of the studies reviewed in the current research reported on adherence and compliance to the exercise intervention. In the studies that did report on adherence, supervised sessions had a much greater attendance rate and could ultimately contribute to larger improvements in physical and mental health. Future studies should consider commencing with supervision of all exercise sessions, in order to address initial exercise engagement, followed by a tapering of supervision to include planned, unsupervised exercise, while concurrently promoting and encouraging self-sustainability, to promote long-term maintenance of exercise, following the completion of the intervention.
Given that previous research shows that time limitation is reported as the biggest barrier to exercise participation both in a general population and among women with PCOS [9], the alternative of a vigorous intensity or high intensity interval training may provide a solution to this barrier. Some, but not all, research suggests that individuals may experience greater enjoyment when partaking in high intensity exercise compared to continuous moderate intensity exercise [49–51]. Significant improvements following high intensity interval training have been reported in systematic reviews/meta-analyses for anxiety, depression [49, 52] and quality of life [25, 53] outcomes, however, these benefits have only been reported in patients with chronic conditions other than PCOS. In women with PCOS, there is limited evidence to suggest that high intensity exercise can result in greater health improvements compared to moderate intensity exercise [25]. However the potential effects of high intensity exercise, in particular, on mental health and health-related quality of life outcomes has yet to be thoroughly investigated. Thus, more studies examining the effects of high intensity exercise on mental health outcomes in women with PCOS are needed.
Half of the studies included in this review reported significant reductions in anxiety and depression symptoms after an exercise intervention, especially when considering that the reviewed interventions were primarily aimed at improving the physical health, rather than the mental health, of participants. Designing future interventions with a mental health informed rationale for the exercise intervention may improve engagement and therefore result in greater mental health benefits. For example, multi-component interventions that also include additional therapies such as cognitive behavioural therapy could be considered useful and may aid to increase adherence, retention, engagement as well as the maintenance of a healthy lifestyle to improve all health outcomes in women with PCOS [1]. Although this review was focused on the effects of exercise only, one of the included studies examined a multi-component intervention that included cognitive behavioural therapy, and reported clinically significant improvements in all domains of the PCOSQ and depression symptom scores [32]. Therefore, further examination of multi-component interventions could provide useful information for improving mental health for women with PCOS.
In addition, many of the included trials excluded women who were taking medications for the treatment of clinical anxiety and depression. Given the high prevalence of these two mental health conditions in women with PCOS, excluding these women does not adequately represent the population, and therefore, perhaps the true benefits of exercise for these women. We could benefit greatly from future research that examines the effect of exercise in women with PCOS, who display elevated baseline levels of anxiety and depression. Such research would provide greater insight regarding the efficacy of exercise for improving mental health and health-related quality of life in women with PCOS and would increase generalisability and applicability to real-world clinical practice.
Strengths and Limitations
This review builds on existing knowledge and provides preliminary data to support the inclusion of exercise to manage and improve mental health and health-related quality of life outcomes in women with PCOS. A strength of this review is that it follows the PRISMA guidelines, including double screening of articles, data extraction and quality appraisal of each publication. This review was limited by large variations and poor reporting of exercise characteristics in the included primary studies. This hindered us from being able to conduct a quantitative synthesis of results and limited our ability to form strong conclusions about the effectiveness of exercise, and particular exercise characteristics, on mental health and health-related quality of life in women with PCOS. Future studies should endeavour to adequately report all intervention characteristics, including frequency, intensity, type, format and session duration of exercise interventions and as well as reporting both adherence and compliance to the exercise intervention inform future research.
Conclusions
This review found that exercise results in both clinically meaningful and statistically significant improvements in health-related quality of life in women with PCOS. Exercise also appears to have some benefit for improving symptoms of common mental health concerns with half of studies reporting significant improvements in symptoms of depression and anxiety. However, the heterogeneity of included studies, including methodological quality, and the poor reporting of the characteristics of exercise interventions delivered, limited the ability to make conclusions regarding the effectiveness of specific types of exercise. This also limited the ability to conclude the impact of specific exercise characteristics including intensity, frequency and type of exercise for improving mental health in women with PCOS. It is vital to employ strategies that can both reduce symptoms of anxiety and depression and increase adherence to interventions. Therefore, multi-component interventions that integrate psychological treatment with exercise and address the complex physical and mental health concerns of women with PCOS have the potential for improving mental health outcomes. Future studies should aim to address barriers to exercise participation and determine which intervention characteristics are associated with increased engagement and maintenance of exercise for the promotion of mental health in women with PCOS.
Supplementary Information
Acknowledgements
Not applicable
List of abbreviations
- 1RM
One Repetition Maximum
- BMI
Body Mass Index
- BSA-S
Brief Scale for Anxiety
- CAT
Continuous Aerobic Training
- CBT
Cognitive Behavioural Therapy
- CES-D
Centre for Epidemiological Studies Depression scale
- DASS-21
Depression, Anxiety, Stress Scale-21
- HADS
Hospital Anxiety and Depression Scale
- HRmax
Maximum Heart Rate
- IAT
Intermittent Aerobic Training
- MADRS-S
Montgomery Åsberg Depression Rating Scale
- OCP
Oral Contraceptive Pill
- PCOS
Polycystic Ovary Syndrome
- PCOSQ
Polycystic Ovary Syndrome Questionnaire
- PRIME-MD
Primary Care Evaluation of Mental Disorders
- QA
Quality Appraisal
- RCT
Randomised Controlled Trial
- RT
Resistance Training
- SF-36
Short Form-36
Authors’ contributions
RP conceived the review, conducted the literature search, screened all studies, conducted methodological quality assessment, extracted and interpreted the data, contributed to the preparation and revisions of the manuscript. MP assisted with data interpretation and contributed significantly to the manuscript preparation and revisions. AM assisted with data interpretation and contributed significantly to the manuscript preparation and revisions. RB assisted with screening of studies and conducted methodological quality assessments. NS assisted with the conception of the review, assisted with the search, screening of articles and methodological quality assessment. AP assisted with data interpretation and contributed significantly to the manuscript preparation and revisions. All authors reviewed and approved of the final manuscript.
Funding
The authors declare that they have received no financial support in regards to the publication of this article.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts or competing interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rhiannon K. Patten, Email: Rhiannon.patten@vu.edu.au
Michaela C. Pascoe, Email: Michaela.pascoe@vu.edu.au
Alba Moreno-Asso, Email: Alba.moreno@vu.edu.au.
Russell A. Boyle, Email: Russell.boyle@vu.edu.au
Alexandra G. Parker, Email: Alex.parker@vu.edu.au
References
- 1.Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018;110(3):364–379. doi: 10.1016/j.fertnstert.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rotterdam EA-SPCWG. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Teede HJ, Hutchison SK, Zoungas S. The management of insulin resistance in polycystic ovary syndrome. Trends Endocrinol Metab. 2007;18(7):273–279. doi: 10.1016/j.tem.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Balen AH, Morley LC, Misso M, Franks S, Legro RS, Wijeyaratne CN, et al. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update. 2016;22(6):687–708. doi: 10.1093/humupd/dmw025. [DOI] [PubMed] [Google Scholar]
- 5.Stepto NK, Cassar S, Joham AE, Hutchison SK, Harrison CL, Goldstein RF, et al. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013;28(3):777–784. doi: 10.1093/humrep/des463. [DOI] [PubMed] [Google Scholar]
- 6.Moran LJ, Strauss BJ, Teede HJ. Diabetes risk score in the diagnostic categories of polycystic ovary syndrome. Fertil Steril. 2011;95(5):1742–1748. doi: 10.1016/j.fertnstert.2011.01.133. [DOI] [PubMed] [Google Scholar]
- 7.Cassar S, Misso ML, Hopkins WG, Shaw CS, Teede HJ, Stepto NK. Insulin resistance in polycystic ovary syndrome: a systematic review and meta-analysis of euglycaemic-hyperinsulinaemic clamp studies. Hum Reprod. 2016;31(11):2619–2631. doi: 10.1093/humrep/dew243. [DOI] [PubMed] [Google Scholar]
- 8.Moran LJ, Misso ML, Wild RA, Norman RJ. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2010;16(4):347–363. doi: 10.1093/humupd/dmq001. [DOI] [PubMed] [Google Scholar]
- 9.Banting LK, Gibson-Helm M, Polman R, Teede HJ, Stepto NK. Physical activity and mental health in women with polycystic ovary syndrome. BMC Womens Health. 2014;14(1):51. doi: 10.1186/1472-6874-14-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 11.Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009;190(7 Suppl):S54–S60. doi: 10.5694/j.1326-5377.2009.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 12.Farrell K, Antoni MH. Insulin resistance, obesity, inflammation, and depression in polycystic ovary syndrome: biobehavioral mechanisms and interventions. Fertil Steril. 2010;94(5):1565–1574. doi: 10.1016/j.fertnstert.2010.03.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollinrake E, Abreu A, Maifeld M, Van Voorhis BJ, Dokras A. Increased risk of depressive disorders in women with polycystic ovary syndrome. Fertil Steril. 2007;87(6):1369–1376. doi: 10.1016/j.fertnstert.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 14.Mansson M, Holte J, Landin-Wilhelmsen K, Dahlgren E, Johansson A, Landen M. Women with polycystic ovary syndrome are often depressed or anxious-a case control study. Psychoneuroendocrinology. 2008;33(8):1132–1138. doi: 10.1016/j.psyneuen.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Coffey S, Bano G, Mason HD. Health-related quality of life in women with polycystic ovary syndrome: a comparison with the general population using the Polycystic Ovary Syndrome Questionnaire (PCOSQ) and the Short Form-36 (SF-36) Gynecol Endocrinol. 2006;22(2):80–86. doi: 10.1080/09513590600604541. [DOI] [PubMed] [Google Scholar]
- 16.Banting LK, Gibson-Helm ME, Polman RE, Teede HJ, Stepto NK. Physical activity and mental health in women with Polycystic Ovary Syndrome. BMC Women's Health. 2014;14(51). [DOI] [PMC free article] [PubMed]
- 17.Jones GL, Benes K, Clark TL, Denham R, Holder MG, Haynes TJ, et al. The Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ): a validation. Hum Reprod. 2004;19(2):371–377. doi: 10.1093/humrep/deh048. [DOI] [PubMed] [Google Scholar]
- 18.Stephens T. Physical activity and mental health in the United States and Canada: Evidence from four population surveys. Prev Med. 1988;17(1):35–47. doi: 10.1016/0091-7435(88)90070-9. [DOI] [PubMed] [Google Scholar]
- 19.Kirk AF, Higgins LA, Hughes AR, Fisher BM, Mutrie N, Hillis S, et al. A randomized, controlled trial to study the effect of exercise consultation on the promotion of physical activity in people with Type 2 diabetes: a pilot study. Diabet Med. 2001;18(11):877–882. doi: 10.1046/j.0742-3071.2001.00570.x. [DOI] [PubMed] [Google Scholar]
- 20.Rippe JM, Price JM, Hess SA, Kline G, DeMers KA, Damitz S, et al. Improved psychological well-being, quality of life, and health practices in moderately overweight women participating in a 12-week structured weight loss program. Obesity research. 1998;6(3):208–218. doi: 10.1002/j.1550-8528.1998.tb00339.x. [DOI] [PubMed] [Google Scholar]
- 21.Conte F, Banting L, Teede HJ, Stepto NK. Mental health and physical activity in women with polycystic ovary syndrome: a brief review. Sports Med. 2015;45(4):497–504. doi: 10.1007/s40279-014-0291-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomson RL, Buckley JD, Lim SS, Noakes M, Clifton PM, Norman RJ, et al. Lifestyle management improves quality of life and depression in overweight and obese women with polycystic ovary syndrome. Fertil Steril. 2010;94(5):1812–1816. doi: 10.1016/j.fertnstert.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Vizza L, Smith CA, Swaraj S, Agho K, Cheema BS. The feasibility of progressive resistance training in women with polycystic ovary syndrome: a pilot randomized controlled trial. BMC Sports Sci Med Rehabil. 2016;8:14. doi: 10.1186/s13102-016-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Legro RS, Dodson WC, Kris-Etherton PM, Kunselman AR, Stetter CM, Williams NI, et al. Randomized Controlled Trial of Preconception Interventions in Infertile Women With Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2015;100(11):4048–4058. doi: 10.1210/jc.2015-2778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patten RK, Boyle RA, Moholdt T, Kiel I, Hopkins WG, Harrison CL, et al. Exercise interventions in polycystic ovary syndrome: a systematic review and meta-analysis. Front Physiol. 2020;11(606). [DOI] [PMC free article] [PubMed]
- 26.Benham JL, Yamamoto JM, Friedenreich CM, Rabi DM, Sigal RJ. Role of exercise training in polycystic ovary syndrome: a systematic review and meta-analysis. Clinical obesity. 2018. [DOI] [PubMed]
- 27.Greenwood EA, Noel MW, Kao CN, Shinkai K, Pasch LA, Cedars MI, et al. Vigorous exercise is associated with superior metabolic profiles in polycystic ovary syndrome independent of total exercise expenditure. Fertil Steril. 2016;105(2):486–493. doi: 10.1016/j.fertnstert.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norton K, Norton L, Sadgrove D. Position statement on physical activity and exercise intensity terminology. J Sci Med Sport. 2010;13(5):496–502. doi: 10.1016/j.jsams.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of epidemiology and community health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arentz S, Smith CA, Abbott J, Fahey P, Cheema BS, Bensoussan A. Combined Lifestyle and Herbal Medicine in Overweight Women with Polycystic Ovary Syndrome (PCOS): A Randomized Controlled Trial. Phytotherapy research : PTR. 2017;31(9):1330–1340. doi: 10.1002/ptr.5858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cooney LG, Milman LW, Hantsoo L, Kornfield S, Sammel MD, Allison KC, et al. Cognitive-behavioral therapy improves weight loss and quality of life in women with polycystic ovary syndrome: a pilot randomized clinical trial. Fertil Steril. 2018;110(1):161-71.e1. [DOI] [PMC free article] [PubMed]
- 33.Costa EC, de Sa JCF, Stepto NK, Costa IBB, Farias-Junior LF, da Nobrega Tomaz Moreira S, et al. Aerobic Training Improves Quality of Life in Women with Polycystic Ovary Syndrome. Medicine and science in sports and exercise. 2018. [DOI] [PubMed]
- 34.De Frene V, Verhofstadt L, Lammertyn J, Stuyver I, Buysse A, De Sutter P. Quality of Life and Body Mass Index in Overweight Adult Women with Polycystic Ovary Syndrome During a Lifestyle Modification Program. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN. 2015;44(5):587–599. doi: 10.1111/1552-6909.12739. [DOI] [PubMed] [Google Scholar]
- 35.Ladson G, Dodson WC, Sweet SD, Archibong AE, Kunselman AR, Demers LM, et al. The effects of metformin with lifestyle therapy in polycystic ovary syndrome: a randomized double-blind study. Fertil Steril. 2011;95(3):1059-66.e1-7. [DOI] [PMC free article] [PubMed]
- 36.Lara LA, Ramos FK, Kogure GS, Costa RS, Silva de Sa MF, Ferriani RA, et al. Impact of Physical Resistance Training on the Sexual Function of Women with Polycystic Ovary Syndrome. The journal of sexual medicine. 2015;12(7):1584–1590. doi: 10.1111/jsm.12909. [DOI] [PubMed] [Google Scholar]
- 37.Ramos FK, Lara LA, Kogure GS, Silva RC, Ferriani RA. Silva de Sa MF, et al. Quality of Life in Women with Polycystic Ovary Syndrome after a Program of Resistance Exercise Training. Rev Bras Ginecol Obstet. 2016;38(7):340–347. doi: 10.1055/s-0036-1585457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dokras A, Sarwer DB, Allison KC, Milman L, Kris-Etherton PM, Kunselman AR, et al. Weight Loss and Lowering Androgens Predict Improvements in Health-Related Quality of Life in Women With PCOS. J Clin Endocrinol Metab. 2016;101(8):2966–2974. doi: 10.1210/jc.2016-1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ribeiro VB, Lopes IP, Dos Reis RM, Silva RC, Mendes MC, Melo AS, et al. Continuous versus intermittent aerobic exercise in the improvement of quality of life for women with polycystic ovary syndrome: A randomized controlled trial. Journal of health psychology. 2019:1359105319869806. [DOI] [PubMed]
- 40.Kogure GS, Lopes IP, Ribeiro VB, Mendes MC, Kodato S, Furtado CLM, et al. The effects of aerobic physical exercises on body image among women with polycystic ovary syndrome. J Affect Disord. 2020;262:350–358. doi: 10.1016/j.jad.2019.11.025. [DOI] [PubMed] [Google Scholar]
- 41.Stener-Victorin E, Holm G, Janson PO, Gustafson D, Waern M. Acupuncture and physical exercise for affective symptoms and health-related quality of life in polycystic ovary syndrome: secondary analysis from a randomized controlled trial. BMC complementary and alternative medicine. 2013;13:131. doi: 10.1186/1472-6882-13-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomson RL, Buckley JD, Brinkworth GD. Perceived exercise barriers are reduced and benefits are improved with lifestyle modification in overweight and obese women with polycystic ovary syndrome: a randomised controlled trial. BMC Womens Health. 2016;16:14. doi: 10.1186/s12905-016-0292-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Costa EC, De Sá JCF, Stepto NK, Costa IBB, Farias-Junior LF, Moreira S, et al. Aerobic Training Improves Quality of Life in Women with Polycystic Ovary Syndrome. Med Sci Sports Exerc. 2018;50(7):1357–1366. doi: 10.1249/MSS.0000000000001579. [DOI] [PubMed] [Google Scholar]
- 44.Cronin L, Guyatt G, Griffith L, Wong E, Azziz R, Futterweit W, et al. Development of a health-related quality-of-life questionnaire (PCOSQ) for women with polycystic ovary syndrome (PCOS) J Clin Endocrinol Metab. 1998;83(6):1976–1987. doi: 10.1210/jcem.83.6.4990. [DOI] [PubMed] [Google Scholar]
- 45.Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. British Medical Journal. 1992;305(6846):160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ware J, Snoww K, Ma K, Bg G. SF36 Health Survey: Manual and Interpretation Guide. Lincoln, RI: Quality Metric, Inc, 1993. 1993;30.
- 47.Brown AJ, Setji TL, Sanders LL, Lowry KP, Otvos JD, Kraus WE, et al. Effects of exercise on lipoprotein particles in women with polycystic ovary syndrome. Med Sci Sports Exerc. 2009;41(3):497–504. doi: 10.1249/MSS.0b013e31818c6c0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Randeva HS, Lewandowski KC, Drzewoski J, Brooke-Wavell K, O'Callaghan C, Czupryniak L, et al. Exercise decreases plasma total homocysteine in overweight young women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87(10):4496–4501. doi: 10.1210/jc.2001-012056. [DOI] [PubMed] [Google Scholar]
- 49.Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227. doi: 10.1136/bjsports-2013-092576. [DOI] [PubMed] [Google Scholar]
- 50.Thum JS, Parsons G, Whittle T, Astorino TA. High-Intensity Interval Training Elicits Higher Enjoyment than Moderate Intensity Continuous Exercise. PloS one. 2017;12(1):e0166299. doi: 10.1371/journal.pone.0166299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oliveira BRR, Santos TM, Kilpatrick M, Pires FO, Deslandes AC. Affective and enjoyment responses in high intensity interval training and continuous training: a systematic review and meta-analysis. PloS one. 2018;13(6):e0197124. doi: 10.1371/journal.pone.0197124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beauchamp MK, Nonoyama M, Goldstein RS, Hill K, Dolmage TE, Mathur S, et al. Interval versus continuous training in individuals with chronic obstructive pulmonary disease-a systematic review. Thorax. 2010;65(2):157–164. doi: 10.1136/thx.2009.123000. [DOI] [PubMed] [Google Scholar]
- 53.Ito S, Mizoguchi T, Saeki T. Review of High-intensity Interval Training in Cardiac Rehabilitation. Intern Med. 2016;55(17):2329–2336. doi: 10.2169/internalmedicine.55.6068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.