Abstract
Purpose of review
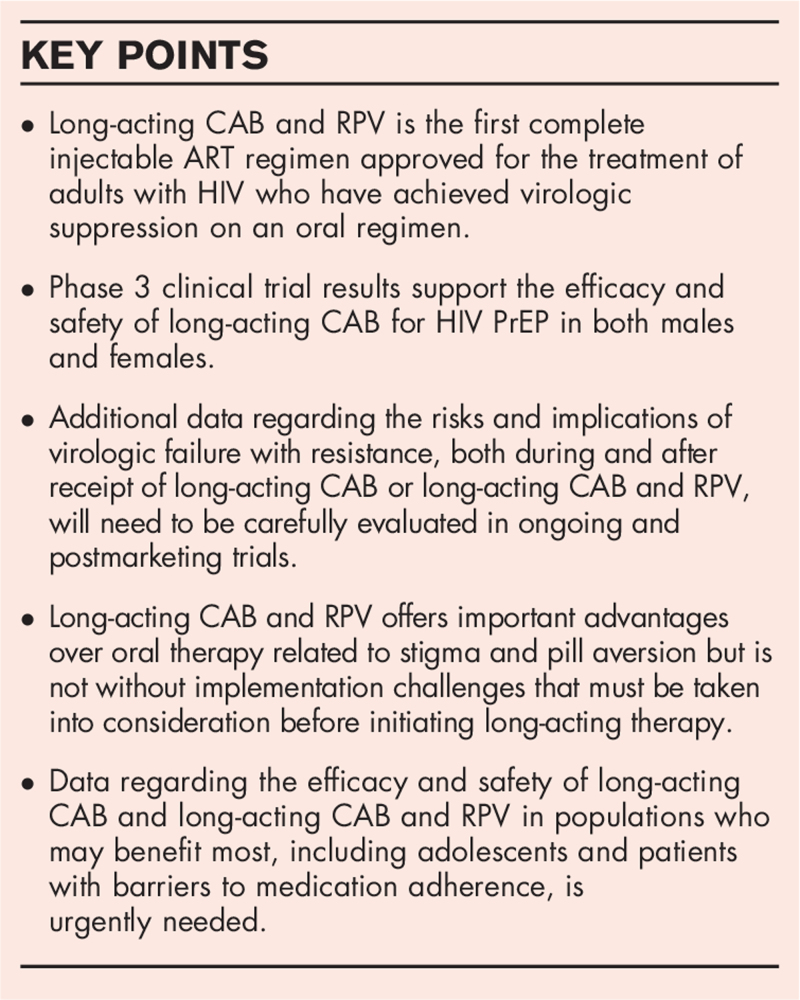
Cabotegravir (CAB) and rilpivirine (RPV) is the first long-acting injectable antiretroviral therapy (ART) option approved for virologically suppressed adults with HIV-1. In addition, long-acting CAB is a promising agent for HIV preexposure prophylaxis (PrEP). This review focuses on phase 3 clinical trial results and implementation considerations for these long-acting ART and PrEP strategies.
Recent findings
Long-acting CAB and RPV administered every 4 weeks demonstrated noninferiority to oral ART through week 96 in both the ATLAS and FLAIR studies, whereas ATLAS-2M found similar efficacy through 96 weeks when the long-acting injectable ART was administered every 8 weeks instead of every 4 weeks. For prevention, two phase 3 trials were stopped early due to fewer incident HIV infections in participants receiving long-acting CAB every 8 weeks compared with daily oral tenofovir disoproxil fumarate–emtricitabine for PrEP. The long-acting therapies were well tolerated across all clinical trials.
Summary
Clinical trial results support the use of long-acting CAB for HIV PrEP and long-acting CAB and RPV as a switch strategy for adults with HIV-1 who are first virologically suppressed with oral ART. Implementation challenges persist, and data are urgently needed in populations who may benefit most from long-acting therapy, including adolescents, pregnant individuals, and those with barriers to medication adherence.
Keywords: antiretroviral therapy, cabotegravir, long-acting injectable antiretroviral, preexposure prophylaxis, rilpivirine
INTRODUCTION
Without a cure or an effective vaccine, antiretrovirals remain the cornerstone of HIV treatment and prevention. Although effective and well tolerated [1], the need for high levels of adherence to daily oral regimens remains a barrier to the success of both treatment and prevention. Challenges related to daily oral adherence include pill fatigue, the need for discretion, self-stigma, and other factors [2▪]. Long-acting injectable antiretrovirals have the potential to improve adherence with less frequent dosing, greater confidentiality/privacy, and reduced risk of undesired disclosure. Further, some adverse effects, drug–drug and drug–food interactions may be minimized with injectable routes of administration. Finally, the availability of multiple methods of drug administration can increase the likelihood that one option would be desirable for an individual through changing needs over their lifespan [3].
Intramuscular formulations of cabotegravir (CAB) and rilpivirine (RPV) became the first long-acting regimen for the treatment of HIV-1 in adults to be approved by Health Canada in March of 2020, the European Medical Agency in December of 2020, and the US Food and Drug Administration in January of 2021 [4–8]. Approval of long-acting CAB for HIV preexposure prophylaxis (PrEP) is anticipated. This review will focus on long-acting CAB and RPV as a two-drug antiretroviral therapy (ART) regimen for the treatment of HIV, and long-acting CAB for the prevention of HIV. Efficacy, safety, and pharmacology data from phase 3 trials are reviewed. In addition, factors regarding patient selection and implementation of long-acting therapy in the clinical setting are discussed.
Box 1.
no caption available
CABOTEGRAVIR AND RILPIVIRINE FOR THE TREATMENT OF HIV
Phase 2b studies of long-acting CAB and RPV, LATTE [9] and LATTE-2 [10], were described in a previous review [11]. Since then, the 5-year results of the LATTE-2 study were published, demonstrating reassuring long-term durability of the injectable regimen in the phase 2b trial [12▪]. These initial studies provided proof of concept that the two-drug oral regimen of CAB and RPV effectively maintained viral suppression of HIV-1 and informed the recently completed phase 3 clinical trials of this long-acting ART strategy. Table 1 describes the phase 3 efficacy and safety trial design, dosing regimen, and virologic outcomes [13▪▪–18▪▪].
Table 1.
Clinical efficacy trials of cabotegravir and rilpivirine for the treatment of HIV
| Study | Trial design | Participant characteristics | Regimens (n for primary endpoint) | Primary endpointaDifference (95% CI) | Final published dataaDifference (95% CI) | Summary |
| ATLAS | Phase 3, randomized, multicenter, open-label, noninferiority switch trial | ART-experienced, virologically suppressed adults with HIV | Daily oral PI, NNRTI or INSTI-based regimen with a 2-NRTI backbone (n = 308)versusOral lead-in: CAB 30 mg daily + RPV 25 mg daily × 4 weeks followed by LA CAB 600 mg IM × 1 + LA RPV 900 mg IM × 1 at week 4 followed by LA CAB 400 mg IM + LA RPV 600 mg IM Q4W beginning at week 8 (n = 308) | Week 48: [13▪▪]0.6% (−1.2%, 2.5%) | Week 96:b,c[14▪▪]100 (23/23) and 97% (28/29) in LA and Switch arms had HIV-1 RNA < 50 copies/ml | Noninferior through week 96 |
| ATLAS-2M | Phase 3b, randomized, multicenter, open-label, noninferiority switch trial | Participants who completed the 52-week comparative phase of the ATLAS trial and had an HIV-1 RNA of <50 copies/ml | LA CAB 400 mg IM + LA RPV 600 mg IM Q4W (n = 523)versusLA CAB 600 mg IM + LA RPV 900 mg IM Q8W (n = 522) | Week 48: [15▪▪]0.8% (−0.6, 2.2%) | Week 96: [16▪▪]1.0% (−0.6%, 2.5%) | Noninferior through week 96 |
| FLAIR | Phase 3, randomized, multicenter, open-label, noninferiority trial | ART-naïve adults with HIV | Induction (all participants):Oral DTG–ABC–3TC daily × 20 weeks (n = 631)Randomized to maintenance strategy:Oral DTG–ABC–3TC daily (n = 283)versusOral lead-in: CAB 30 mg daily + RPV 25 mg daily × 4 weeks followed by LA CAB 600 mg IM × 1 + LA RPV 900 mg IM × 1 at week 4 followed by LA CAB 400 mg IM + LA RPV 600 mg IM Q4W beginning at week 8 (n = 238) | Week 48: [17▪▪]−0.4% (−2.8%, 2.1%) | Week 96: [18▪▪]1.0% (−0.6%, 2.5%) | Noninferior through week 96 |
ART, antiretroviral therapy; CAB, cabotegravir; CI, confidence interval; DTG–ABC–3TC, dolutegravir–abacavir–lamivudine; IM, intramuscular; INSTI, integrase strand transfer inhibitor; LA, long-acting; NNRTI, nonnucleoside reverse transcriptase inhibitor; NRTI, nucleoside/nucleotide reverse transcriptase inhibitor; PI, protease inhibitor; Q4W, every 4 weeks; Q8W, every 8 weeks; RPV, rilpivirine.
Endpoint was HIV-1 RNA of 50 copies/ml or higher unless indicated.
Endpoint was proportion of patients with HIV-1 RNA < 50 copies/ml.
52 Participants transitioned to the extension phase of ATLAS and either continued long-acting therapy (LA arm) or switched from oral to long-acting therapy (Switch arm); these participants were included in the 96-week analysis for which the primary endpoint was proportion with HIV-1 RNA < 50 copies/ml.
Clinical efficacy as a switch strategy
The ATLAS study compared oral ART versus monthly injections of long-acting CAB and RPV for the treatment of HIV-1 among participants who were virologically suppressed for 6 months on oral ART prior to screening [13▪▪]. Participants were randomized to continue oral ART or to switch to injectable long-acting therapy. Participants assigned to long-acting therapy received a 4-week oral lead-in (OLI) of CAB and RPV before transitioning to the injectable regimen. Those who remained virologically suppressed after the OLI received long-acting CAB and RPV every 4 weeks (Q4W) through week 52.
The long-acting therapy was noninferior to oral therapy through the primary endpoint at week 48, with 1.6% (5/308) of participants in the long-acting therapy arm and 1% (3/308) in the oral therapy arm with an HIV-RNA of 50 copies/ml or higher (Table 1) [13▪▪]. Three participants on long-acting therapy had confirmed virologic failure (CVF); two with HIV-1 subtype A/A1 (failures at week 8 and week 20) and one with subtype AG (failure at week 12). RPV resistance-associated reverse-transcriptase mutations were detected in samples from all three participants at the time of failure (E138A; E138K + V108I; E138E/K; and the integrase mutation N155H). Of note, the E138 mutations were present in HIV-1 DNA at baseline in two of the three participants. In comparison, four participants receiving oral ART had CVF with reverse-transcriptase mutations detected in three of these participants (M184I; M184V and G190S; M230M/I).
Participants who completed ATLAS were given the option to withdraw, transition to the ATLAS-2M follow-up study, or enter an ATLAS extension phase in which they either continued long-acting therapy or switched from oral to long-acting therapy. High efficacy rates were observed in 52 participants in the week 96 analysis of the extension phase (Table 1) [14▪▪], with no new CVF or safety signals identified. Most (88%, 502/572) participants transitioned to ATLAS-2M.
ATLAS-2M was designed to evaluate long-acting CAB and RPV given every 8 weeks (Q8W) compared with Q4W [15▪▪]. Virologically suppressed participants from ATLAS had completed the 52-week comparative phase of the trial. Newly recruited participants to ATLAS-2M were virologically suppressed on oral ART for at least 6 months. The two dosing strategies were noninferior, with 2% (9/522) of participants in the Q8W arm and 1% (5/523) in the Q4W arm with an HIV-RNA of 50 copies/ml or higher at week 48 (Table 1) [15▪▪].
In ATLAS-2M, 10 participants had CVF, eight in the Q8W arm and two in the Q4W arm [15▪▪], with the following viral subtypes observed: A (n = 2), A1 (n = 2), B (n = 4), C (n = 1), and complex (n = 1). Archived nonnucleoside reverse transcriptase inhibitor (NNRTI) resistance-associated mutations to RPV, either alone (n = 4) or in combination with a major integrase strand transfer inhibitor (INSTI) resistance-associated mutation (n = 1), were found in five of the eight participants in the Q8W arm. At CVF in the Q8W arm, six participants had RPV resistance-associated mutations and five of these six also had INSTI resistance-associated mutations. Neither of the Q4W participants with CVF had baseline resistance-associated mutations, and both had either RPV resistance-associated mutations, an NNRTI polymorphism, or INSTI resistance-associated mutations at CVF. ATLAS-2M week 96 data were recently presented; noninferiority was maintained (Table 1), but one additional participant developed CVF between weeks 48 and 96 [16▪▪]. The participant was in the Q8W arm and had a baseline RPV resistance-associated mutation.
Clinical efficacy for antiretroviral therapy-naïve adults
Long-acting therapy was evaluated in ART-naïve adults in the FLAIR study [17▪▪], but all participants were first virologically suppressed with oral dolutegravir–abacavir–lamivudine. Participants virologically suppressed after week 16 were randomly assigned to continue oral therapy or switch to Q4W injections of long-acting CAB and RPV following an OLI of CAB and RPV. Through week 48, long acting was noninferior to oral therapy, with 2.1% (6/283) of participants in the long-acting arm and 2.5% (7/283) in the oral arm with an HIV-1 RNA of 50 copies/ml or higher (Table 1) [17▪▪]. At week 96, nine participants in each arm had an HIV-1 RNA of 50 copies/ml or higher, consistent with the noninferiority demonstrated at week 48 [18▪▪].
Four participants in the long-acting arm had CVF through week 48: one participant was withdrawn before initiating long-acting therapy; the other three participants had HIV-1 subtype A1 with an L74I integrase polymorphism at baseline and all three acquired NNRTI and INSTI resistance-associated mutations while on long-acting therapy [17▪▪]. In the oral therapy arm, three participants had CVF but did not develop resistance-associated mutations. No additional participants had CVF between weeks 48 and 96 in the long-acting arm [18▪▪].
Adverse effects
Across both ATLAS and FLAIR, injection site reactions (ISRs) were common, but diminished in severity over time and were well tolerated by participants. In a pooled analysis of week 48 data, a total of 3663 ISRs were reported, representing 25% of all injections administered [19▪]. Less than 1% (n = 34) were grade at least 3 and most (88%) resolved within 7 days (median 3). Injection site pain was the most common ISR, occurring with 21% (n = 3087) of injections. Nodule, induration, and swelling were also reported. The incidence of ISRs was highest with the first dose (week 4) and decreased with time (70% week 4 versus 16% week 48). Only six (1%) participants discontinued treatment due to ISRs.
The most common non-ISR adverse events were nasopharyngitis (18% long-acting arm, 15% oral arm), headache (12% long-acting arm, 6% oral arm), and upper respiratory tract infection (11% long-acting arm, 9% oral arm) [19▪]. The serious adverse events rate was 4% in each arm. Overall, these trials offer reassuring data regarding the safety and tolerability of long-acting CAB and RPV.
Pharmacologic considerations
The pharmacokinetic characteristics of long-acting CAB and RPV were recently reviewed in detail [20▪]. Briefly, sex and BMI contribute to variable pharmacokinetics for both intramuscular CAB and RPV; however, these two factors do not account for most of the variability observed. Both long-acting agents have a half-life of greater than a month (mean: CAB 5.6–11.5 weeks; RPV 13–28 weeks) [5], resulting in prolonged drug exposure after treatment discontinuation, described as the pharmacokinetic tail. This prolonged decay raises concern for emergence of drug resistance as concentrations decline below a minimum effective concentration in individuals who are not virologically suppressed. Therefore, a switch to a suppressive ART regimen after long-acting therapy discontinuation is recommended [1], which is challenging to implement for those who are no longer engaged in clinical care.
One potential advantage of long-acting drug formulations is the reduced risk of adverse drug–drug or drug–food interactions. Indeed, significant absorption related interactions are present for both oral CAB and RPV. Oral CAB, like other INSTIs, is susceptible to poly-valent cation interactions that reduce CAB exposure when given simultaneously [8]. Oral RPV requires administration with a full meal, and acid-reducing agents significantly reduce RPV oral bioavailability [21]. While these interactions remain important during an OLI of CAB and RPV, intramuscular long-acting CAB and RPV successfully avoid these interactions.
Drug interactions related to metabolism remain important for long-acting CAB and RPV [5]. CAB is a substrate of uridine diphosphate-glucuronosyltransferase (UGT) 1A1 and UGT1A9 and RPV is a substrate of cytochrome P450 3A4, and coadministered medications which induce or inhibit these enzymes are expected to influence long-acting CAB and RPV exposure. No drug interaction studies have been conducted with the long-acting formulations to date, but physiologically based pharmacokinetic models were constructed from oral drug-interaction studies to predict the effect of coadministered medications on long-acting formulations. Table 2 illustrates similarities and differences in drug-interaction considerations between oral and intramuscular formulations of CAB and RPV. While drug-interactions are reduced with these long-acting formulations, future studies will be necessary to evaluate potential management strategies, such as the feasibility of supplemental dosing of CAB or RPV to overcome some interactions with moderate enzyme inducers, such as rifabutin.
Table 2.
| CAB | RPV | |||
| Oral | Intramuscular | Oral | Intramuscular | |
| Acid-reducing agents | ||||
| Polyvalent cation containing antacids | ↓CAB expectedSeparate administrationa | ↔ | ↓RPV expectedSeparate administrationa | ↔ |
| H2 antagonists | ↔ | ↔ | ↓RPVSeparate administrationb | ↔ |
| Proton pump inhibitors | ↔ | ↔ | ↓RPVContraindicated | ↔ |
| Anticonvulsants | ||||
| Carbamazepine, Oxcarbazepine, Phenobarbital, Phenytoin | ↓CAB expectedContraindicated | ↓CAB expectedContraindicated | ↓RPV expectedContraindicated | ↓RPV expectedContraindicated |
| Antimycobacterials | ||||
| Rifampin | ↓CAB observedContraindicated | ↓CAB expectedContraindicated | ↓RPV observedContraindicated | ↓RPV expectedContraindicated |
| Rifabutin | ↓CAB observedNo dose adjustment needed | ↓CAB expectedContraindicated because of coadministration with RPVc | ↓RPV observedIncrease RPV dose to 50 mg daily | ↓RPV expectedContraindicated |
| Rifapentine | ↓CAB expectedContraindicated | ↓CAB expectedContraindicated | ↓RPV expectedContraindicated | ↓RPV expectedContraindicated |
| Glucocorticoids | ||||
| Dexamethasone (>1 dose) | ↔ | ↔Contraindicated because of coadministration with RPVc | ↓RPV expectedContraindicated | ↓RPV expectedContraindicated |
| Herbal product | ||||
| St. John's wort (Hypericum perforatum) | ↓CAB possibleContraindicated because of coadministration with RPVc | ↔Contraindicated because of coadministration with RPVc | ↓RPV expectedContraindicated | ↓RPV expectedContraindicated |
| Supplements | ||||
| Polyvalent cations (Mg, Al, Fe, Ca, Zn, multivitamins) | ↓CAB expectedSeparate administrationa | ↔ | ↔ | ↔ |
Al, aluminum; Ca, calcium; CAB, cabotegravir; Fe, iron; Mg, magnesium; RPV, rilpivirine.
Administer antacid or supplement 2 h before or 4 h after oral antiretroviral.
Given H2 receptor antagonists at least 12 h before or 4 h after oral RPV.
Recommendation may be modified if long-acting CAB is approved as a single agent for preexposure prophylaxis.
Predictors and implications of virologic failure
Across all three phase 3 and 3b studies, CVF was rare, occurring in only 1% (n = 17/1636) of participants in the long-acting CAB and RPV arms of each study [22▪▪]. To better identify the factors associated with virologic outcomes in participants receiving long-acting therapy, investigators performed a post-hoc analysis of data from 13 of 1039 participants who developed CVF while on long-acting therapy [22▪▪]. Factors associated with CVF included proviral RPV resistance-associated mutations, HIV-1 subtype A6/A1, BMI at least 30 kg/m2 (associated with week 8 CAB trough concentration), and lower week 8 RPV trough concentrations. Only a combination of two or more of these factors was significantly associated with increased risk of CVF.
The implications of virologic failure with long-acting CAB and RPV are significant because it occurred, albeit rarely, despite good adherence to injection visits in highly motivated participants receiving adherence support through the clinical trials. The risks of virologic failure, including virologic failure with resistance, will likely be higher with real-world use of long-acting therapy. Surveillance is needed to better understand which patients are most at risk of virologic failure, and the implications of the virologic failure that occurs while taking long-acting products that persist for months after discontinuation. The theoretical risk of resistance during the pharmacokinetic tail of long-acting CAB and RPV will need to be carefully evaluated in postmarketing trials.
Patient selection and implementation
Long-acting ART with CAB and RPV is approved as a switch strategy for adult patients who have been virologically suppressed on an oral regimen, with minimal ART experience and no prior virologic failure with resistance. Ongoing studies are evaluating the strategy in important populations, including children, adolescents, and during pregnancy (NCT03497676, NCT04518228). The Q4W administration of long-acting CAB and RPV was approved in the United States and Canada [4,5], while in Europe, both the Q4W and Q8W administration schedules were approved [6,7]. Importantly, long-acting therapy is not yet available outside of resource-rich settings.
Long-acting CAB and RPV offers advantages over oral therapy: it is dosed less frequently, avoids the pill fatigue that many people with HIV experience, is subject to fewer drug interactions, and allows for greater confidentiality and privacy (which in turn leads to decreased likelihood of undesired HIV disclosure). As such, patients who face these barriers may be excellent candidates for long-acting CAB and RPV. However, based on evidence to date, they must achieve virologic suppression on their current oral ART regimens before transitioning to long-acting therapy, and this remains a significant impediment for those who might benefit the most [1,5].
Although long-acting therapy is viewed by many as an opportunity to overcome some barriers to adherence posed by daily oral therapy, all participants in clinical trials completed thus far were enrolled based upon a history of good adherence, indicated by virologic suppression at the start of long-acting therapy. To address this data gap, the AIDS Clinical Trial Group LATITUDE study (NCT03635788) is currently enrolling participants with prior nonadherence. In the meantime, data from the compassionate use program is promising: 28/35 (80%) patients entered the program with detectable viremia and, at the time of analysis, 16/28 (57%) had achieved virologic suppression with long-acting CAB and RPV [23].
Long-acting CAB and RPV are currently recommended with an OLI to ensure the medications are well tolerated before transition to the long-acting formulations. Given there were no safety signals during the OLI in the clinical trials, direct to injection options are currently being evaluated in ongoing studies, and early data suggest that an ART switch to long-acting therapy is safe and effective when administered without an OLI [24▪].
While participant satisfaction with long-acting ART has been largely positive [2▪,25–28], provider enthusiasm has been more cautious. Concerns include the need for patients to adhere to injection visits for treatment to be successful [26]. Several ongoing studies will evaluate implementation strategies, both within existing clinics and using alternative care sites such as infusion centers and pharmacies, to better understand and address these concerns (NCT03856580, NCT04982445, NCT04863261, NCT04399551, NCT04973254, NCT04001803).
Finally, since the long-acting formulations are administered as two separate injections in a Z-track fashion into the gluteus medius, a private space where a patient can comfortably lie down for the injection is ideal. Studies of alternative injection sites, including the vastus lateralis (thigh muscle) are planned [NCT04371380, NCT04484337, and NCT03299049 (substudy)]. A myriad of other implementation factors, including human resource capital to obtain drug, capacity, staffing to support injection monitoring and scheduling, drug product storage (cold-chain storage is required for RPV), inventory management, and cost are current challenges facing widespread posttrial implementation of long-acting CAB and RPV [29]. Approval of the Q8W dosing strategy in the United States and Canada may reduce some of these barriers to implementation.
CABOTEGRAVIR FOR HIV PREVENTION
Daily tenofovir disoproxil fumarate–emtricitabine (TDF–FTC) and tenofovir alafenamide–emtricitabine are well established options for PrEP [30–32]. The safety and efficacy of long-acting CAB as part of ART highlighted its potential as a PrEP strategy. After efficacy was demonstrated in a nonhuman primate model [33,34], long-acting CAB safety, tolerability and pharmacokinetics were assessed in two phase 2 studies [35▪,36]. Recently, results of two phase 3, double-blind studies evaluating long-acting CAB for PrEP were reported (Table 3) [37▪▪,38▪▪].
Table 3.
Clinical efficacy trials of cabotegravir for the prevention of HIV
| Study (phase) | Trial design | Participant characteristics | Regimens (n for primary endpoint) | Primary endpointaHR (95% CI) | Summary |
| HPTN 083 | Phase 2b/3, randomized, double-blind, double-dummy, multicenter, noninferiority trial | Cisgender MSM and transgender women who have sex with men who were at risk for HIV | Oral TDF–FTC daily (n = 2284)versusOral lead-in: CAB 30 mg daily × 5 weeks followed by LA CAB 600 mg IM Q8W (n = 2282) | Week 153 : 2b[37▪▪]0.34 (018, 0.62)52 Participants acquired HIV: 13 in LA CAB arm (incidence 0.41 per 100 person-years) and 39 in TDF–FTC arm (incidence 1.22 per 100 person-years) | LA CAB was superior to daily oral TDF–FTC in preventing HIV infection among MSM and transgender women |
| HTPN 084 | Phase 3, randomized, double-blind, double-dummy, multicenter, noninferiority trial | Cisgender women between 18 and 45 years at 20 sites in 7 African countries who were at risk for HIV | Oral TDF–FTC daily (n = 1610)versusOral lead-in: CAB 30 mg daily × 5 weeks followed by LA CAB 600 mg IM Q8W (n = 1614) | Interim planned analysis:b[38▪▪]0.11 (0.01, 0.31)40 Participants acquired HIV: 4 in the LA CAB arm (incidence 0.2 per 100 person-years) and 36 in the TDF–FTC arm (incidence 1.86 per 100 person-years) | LA CAB was superior to daily oral TDF–FTC in preventing HIV infection among cisgender women |
CI, confidence interval; HR, hazard ratio; IM, intramuscular; LA CAB, long-acting cabotegravir; Q8W, every 8 weeks; TDF–FTC, tenofovir disoproxil fumarate–emtricitabine.
Endpoint was incident HIV infection reported as a HR (95% CI) for LA CAB vs oral TDF-FTC.
Trial was stopped early for efficacy on review of results of the first preplanned interim end-point analysis.
Clinical efficacy trial data
HPTN-083 compared long-acting CAB administered Q8W compared with daily oral TDF–FTC for the prevention of HIV in at-risk, cisgender MSM and transgender women who have sex with men [37▪▪]. The study was halted due to efficacy at the first preplanned interim end-point analysis. Incident HIV infection occurred in 52 participants, 13 of 2282 in the long-acting CAB arm and 39 of 2284 in the TDF–FTC arm (Table 3). This 66% lower risk of HIV infection in the long-acting CAB group was impressive because 72.3% of participants in the TDF–FTC group had TDF concentrations indicative of good long-term adherence, suggesting the greater efficacy of long-acting CAB may extend beyond improved adherence with long-acting therapy. INSTI resistance mutations were detected in four of nine incident cases receiving long-acting CAB. NRTI resistance mutations were detected in four incident cases receiving TDF–FTC.
HPTN-084 compared long-acting CAB administered Q8W compared with daily oral TDF–FTC for the prevention of HIV in at-risk cisgender women [38▪▪]. Like HPTN-083, the study was stopped early for efficacy at the first preplanned interim end-point analysis. Incident HIV infection occurred in 40 participants, four of 1614 in the long-acting CAB arm and 36 of 1610 in the TDF–FTC arm (Table 3). While the complete results have not yet been published, the 89% lower risk of HIV infection in the long-acting CAB group are complimentary to HPTN-083 and offer optimism that long-acting CAB will be a useful prevention strategy for both male and female users.
Adverse events
The frequency of adverse events in HPTN-083 was similar between groups. Serious adverse events were rare (5.3%) and balanced between groups [37▪▪]. ISRs were reported in 81.4% of participants in the long-acting CAB arm and 31.3% of participants in the TDF–FTC arm. Most were mild or moderate in severity and decreased over time. Only 2.4% (50 of 2117) participants who received at least one long-acting CAB injection permanently discontinued the injections due to an ISR. In HPTN-84, 21% of participants experienced any ISR (32% long-acting CAB arm, 9% TDF–FTC arm) and no study discontinuations occurred due to an ISR [38▪▪].
Pharmacologic considerations
The half-life of long-acting CAB was estimated in HPTN-077, where both female sex and higher BMI was associated with a longer CAB half-life [median (range) 42.5 (13.5, 133.9) days in males and 64.6 (19.2, 217.1) days in females] [39]. After discontinuation, CAB was detected of 42.7 (20.4, 134) weeks in males and 66.3 (17.7, 182) weeks in females [35▪]. This prolonged period of CAB exposure after PrEP discontinuation raises concern for INSTI resistance in users with an incident HIV infection. In HPTN-083, three incident HIV infections occurred more than 6 months after the last injection; CAB concentrations were low or undetectable in all three participants, and no resistance was detected [40▪▪]. Similar to long-acting ART, an alternative PrEP strategy should be encouraged after long-acting CAB discontinuation. Ongoing monitoring is essential to understand whether the theoretical risk of INSTI resistance during the CAB tail will be realized in clinical practice.
Incident infections
Despite high rates of prevention, some breakthrough infections during long-acting CAB were observed in both phase 3 trials. In HPTN-084, four participants developed incident infection despite on-time injections and CAB plasma concentrations at least 8× the protein adjusted 90% inhibitory concentration [40▪▪]. Two of four infections in the CAB arm of HPTN-084 occurred during long-acting CAB therapy; one infection occurred in a participant who had not missed a CAB injection, and one occurred after missing a scheduled injection [38▪▪]. Further, a combined four incident infections occurred during the CAB OLI period [38▪▪,40▪▪]. Poor adherence to oral therapy was confirmed by no CAB detected in plasma in one HPTN-083 participant, highlighting that omitting the OLI period may also be advantageous for PrEP. These early findings suggest that, like long-acting CAB and RPV for ART, ongoing studies will need to assess the risk factors for, and implications of, long-acting PrEP failure.
Patient selection
If approved, long-acting CAB will offer a new option for HIV prevention and may increase PrEP uptake, particularly for those who prefer discretion or are unable to adhere to a daily oral regimen. The available results in both males and female adults are encouraging, and substudies of HPTN-083 and HPTN-084 will assess the effectiveness of long-acting CAB in adolescents. During HPTN-083, 29 pregnancies were observed in the CAB arm, which will offer important information on the safety of long-acting CAB early in pregnancy [38▪▪]. Pregnancy represents a unique period of risk for HIV acquisition, and data on the feasibility of continuing PrEP with long-acting CAB during pregnancy will be needed.
Participant perspectives on long-acting PrEP have been positive [41], but similar patient selection and implementation challenges are likely to exist for long-acting PrEP as described for ART. For example, long-acting CAB for PrEP will require clinic visits every 2 months, which is more frequent than currently required with oral PrEP. Lessons from ongoing long-acting ART implementation studies may inform future roll-out and the feasibility of administration outside of traditional clinic settings may increase access to long-acting PrEP.
CONCLUSION
Long-acting CAB and RPV is an effective option and offers a few key advantages over current oral ART options for adults who are virologically suppressed on an oral ART regimen. In addition, if approved, long-acting CAB for PrEP will increase the available prevention options for both male and female individuals at risk for HIV and, with its high efficacy, may play a pivotal role in expanding HIV prevention efforts to achieve the United Nations goal of ending AIDS by 2030. However, in order for us to achieve this goal, long-acting agents will need to be accessible to those who stand to benefit most, including adolescents, people with barriers to medication adherence, and people in resource-limited settings.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
S.H.B. has served as a scientific advisor for Gilead and has received institutional research grants from Gilead, Janssen and ViiV. K.K.S. has received investigator-initiated grant support paid to her institution from Organon, LLC.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Available at: https://clinicalinfo.hiv.gov/sites/default/files/inline-files/AdultandAdolescentGL.pdf. [Accessed 7 October 2021]. [Google Scholar]
- 2▪.Scarsi KK, Swindells S. The promise of improved adherence with long-acting antiretroviral therapy: what are the data? J Int Assoc Provid AIDS Care 2021; 20:23259582211009011. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a recent review of patient satisfaction, potential adherence benefits, as well as challenges related to long-acting therapy.
- 3.Delany-Moretlwe S, Mullick S, Eakle R, Rees H. Planning for HIV preexposure prophylaxis introduction: lessons learned from contraception. Curr Opin HIV AIDS 2016; 11:87–93. [DOI] [PubMed] [Google Scholar]
- 4.Viiv Healthcare ULC. Cabenuva® and Vocabria® [product monograph]. Laval, Quebec: Viiv Healthcare ULC; 2020. [Google Scholar]
- 5.Viiv Healthcare. Cabenuva® prescribing information. Research Triangle Park, NC: Viiv Healthcare; 2021. [Google Scholar]
- 6.Janssen Pharmaceutica NV. Rekambys® product information. Beerse, Belgium; 2021. [Google Scholar]
- 7.Viiv Healthcare BV. Vocabria® product information. Amersfoort, Netherlands; 2021. [Google Scholar]
- 8.Viiv Healthcare. Vocabria® prescribing information. Research Triangle Park, NC: Viiv Healthcare; 2021. [Google Scholar]
- 9.Margolis DA, Brinson CC, Smith GHR, et al. Cabotegravir plus rilpivirine, once a day, after induction with cabotegravir plus nucleoside reverse transcriptase inhibitors in antiretroviral-naive adults with HIV-1 infection (LATTE): a randomised, phase 2b, dose-ranging trial. Lancet Infect Dis 2015; 15:1145–1155. [DOI] [PubMed] [Google Scholar]
- 10.Margolis DA, Gonzalez-Garcia J, Stellbrink HJ, et al. Long-acting intramuscular cabotegravir and rilpivirine in adults with HIV-1 infection (LATTE-2): 96-week results of a randomised, open-label, phase 2b, noninferiority trial. Lancet 2017; 390:1499–1510. [DOI] [PubMed] [Google Scholar]
- 11.D’Amico R, Margolis DA. Long-acting injectable therapy: an emerging paradigm for the treatment of HIV infection. Curr Opin HIV AIDS 2020; 15:13–18. [DOI] [PubMed] [Google Scholar]
- 12▪.Smith GHR, Henry WK, Podzamczer D, et al. Efficacy, safety, and durability of long-acting cabotegravir and rilpivirine in adults with human immunodeficiency virus type 1 infection: 5-year results from the LATTE-2 study. Open Forum Infect Dis 2021; 8:ofab439. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reports results from the LATTE-2 extension period through week 256. Participants were receiving long-acting cabotegravir (CAB) and rilpivirine (RPV) every 4 weeks (Q4W) or every 8 weeks (Q8W) assigned in LATTE-2, or switched to long-acting therapy from oral antiretroviral therapy (ART) after the 96 weeks. 186 (81%) of participants in the randomized long-acting groups and 41 (93%) of participants in the extension-switch groups had an HIV-1 RNA less than 50 copies/ml.
- 13▪▪.Swindells S, Andrade-Villanueva JF, Richmond GJ, et al. Long-acting cabotegravir and rilpivirine for maintenance of HIV-1 suppression. N Engl J Med 2020; 382:1112–1123. [DOI] [PubMed] [Google Scholar]; Primary analysis of the ATLAS trial, which compared the efficacy and safety of long-acting CAB and RPV versus oral standard of care ART as a switch strategy among participants currently virologically suppressed on their current oral therapy. Virologic outcomes were noninferior and safety was similar over 48 weeks.
- 14▪▪.Swindells S, Lutz T, van Zyl L, et al. Long-acting cabotegravir + rilpivirine for HIV-1 treatment: ATLAS week 96 results. AIDS 2021; doi: 10.1097/QAD.0000000000003025. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is follow-up data from the ATLAS trial over 96 weeks in participants who did not discontinue or enroll in ATLAS-2M and demonstrated sustained effectiveness of long-acting CAB and RPV over 96 weeks.
- 15▪▪.Overton ET, Richmond G, Rizzardini G, et al. Long-acting cabotegravir and rilpivirine dosed every 2 months in adults with HIV-1 infection (ATLAS-2M), 48-week results: a randomised, multicentre, open-label, phase 3b, noninferiority study. Lancet 2021; 396:1994–2005. [DOI] [PubMed] [Google Scholar]; Primary analysis of ATLAS-2M, which compared the efficacy and safety of long-acting CAB and RPV given Q8W instead of Q4W as a switch strategy among participants currently virologically suppressed on their current oral therapy or on long-acting therapy in the ATLAS trial. Administering long-acting CAB and RPV Q8W was noninferior to Q4W over 48 weeks.
- 16▪▪.Jaeger H, Overton ET, Richmond G, et al. Long-acting cabotegravir and rilpivirine dosed every 2 months in adults with HIV-1 infection (ATLAS-2M), 96-week results: a randomised, multicentre, open-label, phase 3b, non-inferiority study. Lancet HIV 2021; 8:e679–e689. [DOI] [PubMed] [Google Scholar]; This manuscript reports ongoing noninferiority between Q4W and Q8W administration of long-acting CAB and RPV in ATLAS-2M over 96 weeks.
- 17▪▪.Orkin C, Arasteh K, Gorgolas Hernandez-Mora M, et al. Long-acting cabotegravir and rilpivirine after oral induction for HIV-1 infection. N Engl J Med 2020; 382:1124–1135. [DOI] [PubMed] [Google Scholar]; Primary analysis of the FLAIR trial, which compared the efficacy and safety of long-acting CAB and RPV versus oral standard of care ART among antiretroviral-naïve participants. All participants were virologically suppressed on 20 weeks of oral dolutegravir–abacavir–lamivudine prior to randomization to oral versus injectable ART. Virologic outcomes were noninferior and safety was similar between the oral and injectable therapy over 48 weeks.
- 18▪▪.Orkin C, Oka S, Philibert P, et al. Long-acting cabotegravir plus rilpivirine for treatment in adults with HIV-1 infection: 96-week results of the randomised, open-label, phase 3 FLAIR study. Lancet HIV 2021; 8:e185–e196. [DOI] [PubMed] [Google Scholar]; This is follow-up data from the FLAIR trial over 96 weeks, demonstrating sustained noninferiority of long-acting CAB and RPV compared with oral ART over 96 weeks.
- 19▪.Rizzardini G, Overton ET, Orkin C, et al. Long-acting injectable cabotegravir + rilpivirine for HIV maintenance therapy: week 48 pooled analysis of phase 3 ATLAS and FLAIR trials. J Acquir Immune Defic Syndr 2020; 85:498–506. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the combined FDA snapshot analysis (4% noninferiority margin of HIV-RNA ≥ 50 copies/ml) of ATLAS and FLAIR outcomes at week 48. The article offers a descriptive table of participants with confirmed virologic failure (CVF) during long-acting therapy, including baseline characteristics and resistance mutations at the time of failure.
- 20▪.Hodge D, Back DJ, Gibbons S, et al. Pharmacokinetics and drug–drug interactions of long-acting intramuscular cabotegravir and rilpivirine. Clin Pharmacokinet 2021; 60:835–853. [DOI] [PMC free article] [PubMed] [Google Scholar]; A recent comprehensive review of relevant pharmacology topics related to long-acting CAB and RPV.
- 21.Janssen Therapeutics. Edurant® prescribing information. Titusville, NJ: Janssen Therapeutics; 2019. [Google Scholar]
- 22▪▪.Cutrell AG, Schapiro JM, Perno CF, et al. Exploring predictors of HIV-1 virologic failure to long-acting cabotegravir and rilpivirine: a multivariable analysis. AIDS 2021; 35:1333–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]; Pooled multivariable analysis of virologic failure among participants in ATLAS, ATLAS-2M, and FLAIR. The study evaluates the influence of baseline viral and participant factors, dosing regimen, and drug concentrations on confirmed virologic failure (CVF). Overall, CVF was rare across studies. Presence of at least two of proviral RPV resistance-associated mutations, HIV-1 subtype A6/A1 and/or BMI of at least 30 kg/m2 was associated with increased CVF risk.
- 23.D’Amico R, Moodley R, van Landuyt, et al. Compassionate use of long-acting (LA) cabotegravir (CAB) and rilpivirine (RPV) for patients in need of parenteral antiretroviral therapy. 23rd International AIDS Conference; 6–10 July 2020; Virtual. Poster PEB0263. [Google Scholar]
- 24▪.Orkin C, Bernal Morell E, Tan DHS, et al. Initiation of long-acting cabotegravir plus rilpivirine as direct-to-injection or with an oral lead-in in adults with HIV-1 infection: week 124 results of the open-label phase 3 FLAIR study. Lancet HIV 2021; 8:e668–e678. [DOI] [PubMed] [Google Scholar]; This manuscript describes the first data available on the omission of an oral lead-in period, described as ‘direct to inject’, for long-acting CAB and RPV.
- 25.Chounta V, Overton ET, Mills A, et al. Patient-reported outcomes through 1 year of an HIV-1 clinical trial evaluating long-acting cabotegravir and rilpivirine administered every 4 or 8 weeks (ATLAS-2M). Patient 2021; 14:849–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerrigan D, Mantsios A, Gorgolas M, et al. Experiences with long acting injectable ART: a qualitative study among PLHIV participating in a Phase II study of cabotegravir + rilpivirine (LATTE-2) in the United States and Spain. PLoS One 2018; 13:e0190487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kerrigan D, Sanchez Karver T, Muraleetharan O, et al. A dream come true: perspectives on long-acting injectable antiretroviral therapy among female sex workers living with HIV from the Dominican Republic and Tanzania. PLoS One 2020; 15:e0234666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray M, Antela A, Mills A, et al. Patient-reported outcomes in ATLAS and FLAIR participants on long-acting regimens of cabotegravir and rilpivirine over 48 weeks. AIDS Behav 2020; 24:3533–3544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Collins LF, Corbin-Johnson D, Asrat M, et al. Implementation of long-acting injectable cabotegravir-rilpivirine for HIV-1 treatment at a Ryan White-funding Clinic in the U.S. South. IDWeek, Virtual, 29 September–3 October 2021. [Google Scholar]
- 30.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med 2012; 367:399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010; 363:2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mayer KH, Molina JM, Thompson MA, et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV preexposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, noninferiority trial. Lancet 2020; 396:239–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andrews CD, Spreen WR, Mohri H, et al. Long-acting integrase inhibitor protects macaques from intrarectal simian/human immunodeficiency virus. Science 2014; 343:1151–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dobard C, Makarova N, Nishiura K, et al. Long-acting cabotegravir protects macaques against repeated penile simian-human immunodeficiency virus exposures. J Infect Dis 2020; 222:391–395. [DOI] [PubMed] [Google Scholar]
- 35▪.Landovitz RJ, Li S, Eron JJ, Jr, et al. Tail-phase safety, tolerability, and pharmacokinetics of long-acting injectable cabotegravir in HIV-uninfected adults: a secondary analysis of the HPTN 077 trial. Lancet HIV 2020; 7:e472–e481. [DOI] [PMC free article] [PubMed] [Google Scholar]; This evaluation of the pharmacokinetic tail (or drug decay) of long-acting CAB in the HPTN-077 study describes the duration of drug detection after long-acting CAB discontinuation, as well as the influence of sex and BMI on prolonged exposure during the tail phase.
- 36.Markowitz M, Frank I, Grant RM, et al. Safety and tolerability of long-acting cabotegravir injections in HIV-uninfected men (ECLAIR): a multicentre, double-blind, randomised, placebo-controlled, phase 2a trial. Lancet HIV 2017; 4:e331–e340. [DOI] [PubMed] [Google Scholar]
- 37▪▪.Landovitz RJ, Donnell D, Clement ME, et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med 2021; 385:595–608. [DOI] [PMC free article] [PubMed] [Google Scholar]; Primary analysis of the HPTN-084 trial, which was a double-blind trial to compared the efficacy and safety of long-acting CAB versus oral tenofovir–disoproxil fumarate–emtricitabine as preexposure prophylaxis (PrEP) for MSM or transgender women who have sex with men. The study was stopped early for efficacy after review of results at the first preplanned interim end-point analysis due to fewer incident infections in the long-acting CAB group compared with the oral PrEP group.
- 38▪▪.Delany-Moretlwe S, Hughes JP, Bock P, et al. Long acting injectable cabotegravir is safe and effective in preventing HIV infection in cisgender women: interim results from HPTN 084. HIVR4P (HIV Research for Prevention) Virtual, 27–28 January and 3–4 February 2021. Abstract HY01.02. [Google Scholar]; Primary analysis of the HPTN-083 trial, which was a double-blind trial to compared the efficacy and safety of long-acting CAB versus oral tenofovir–disoproxil fumarate–emtricitabine as PrEP in cisgender women. The study was stopped early for efficacy after review of results at the first preplanned interim end-point analysis due to fewer incident infections in the long-acting CAB group compared with the oral PrEP group.
- 39.Landovitz RJ, Li S, Grinsztejn B, et al. Safety, tolerability, and pharmacokinetics of long-acting injectable cabotegravir in low-risk HIV-uninfected individuals: HPTN 077, a phase 2a randomized controlled trial. PLoS Med 2018; 15:e1002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪▪.Marzinke MA, Grinsztejn B, Fogel JM, et al. Characterization of HIV infection in cisgender men and transgender women who have sex with men receiving injectable cabotegravir for HIV prevention: HPTN 083. J Infect Dis 2021. jiab152.doi: 10.1093/infdis/jiab152. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; This report describes retrospective testing of stored samples from participants in HPTN-083 with incident HIV acquisition. Evaluations included sensitive HIV testing, viral load resting, quantification of study drugs, and HIV drug resistance testing. Important information is provided regarding drug concentrations at the time of incident infections, delays in HIV detection during ongoing PrEP, and drug resistance mutations.
- 41.Murray MI, Markowitz M, Frank I, et al. Satisfaction and acceptability of cabotegravir long-acting injectable suspension for prevention of HIV: patient perspectives from the ECLAIR trial. HIV Clin Trials 2018; 19:129–138. [DOI] [PubMed] [Google Scholar]