Abstract
Background
India has been severely affected by the ongoing COVID-19 pandemic. However, due to shortcomings in disease surveillance, the burden of mortality associated with COVID-19 remains poorly understood. We aimed to assess changes in mortality during the pandemic in Chennai, Tamil Nadu, using data on all-cause mortality within the district.
Methods
For this observational study, we analysed comprehensive death registrations in Chennai, from Jan 1, 2016, to June 30, 2021. We estimated expected mortality without the effects of the COVID-19 pandemic by fitting models to observed mortality time series during the pre-pandemic period, with stratification by age and sex. Additionally, we considered three periods of interest: the first 4 weeks of India's first lockdown (March 24 to April 20, 2020), the 4-month period including the first wave of the pandemic in Chennai (May 1 to Aug 31, 2020), and the 4-month period including the second wave of the pandemic in Chennai (March 1 to June 30, 2021). We computed the difference between observed and expected mortality from March 1, 2020, to June 30, 2021, and compared pandemic-associated mortality across socioeconomically distinct communities (measured with use of 2011 census of India data) with regression analyses.
Findings
Between March 1, 2020, and June 30, 2021, 87 870 deaths were registered in areas of Chennai district represented by the 2011 census, exceeding expected deaths by 25 990 (95% uncertainty interval 25 640–26 360) or 5·18 (5·11–5·25) excess deaths per 1000 people. Stratified by age, excess deaths numbered 21·02 (20·54–21·49) excess deaths per 1000 people for individuals aged 60–69 years, 39·74 (38·73–40·69) for those aged 70–79 years, and 96·90 (93·35–100·16) for those aged 80 years or older. Neighbourhoods with lower socioeconomic status had 0·7% to 2·8% increases in pandemic-associated mortality per 1 SD increase in each measure of community disadvantage, due largely to a disproportionate increase in mortality within these neighbourhoods during the second wave. Conversely, differences in excess mortality across communities were not clearly associated with socioeconomic status measures during the first wave. For each increase by 1 SD in measures of community disadvantage, neighbourhoods had 3·6% to 8·6% lower pandemic-associated mortality during the first 4 weeks of India's country-wide lockdown, before widespread SARS-CoV-2 circulation was underway in Chennai. The greatest reductions in mortality during this early lockdown period were observed among men aged 20–29 years, with 58% (54–62) fewer deaths than expected from pre-pandemic trends.
Interpretation
Mortality in Chennai increased substantially but heterogeneously during the COVID-19 pandemic, with the greatest burden concentrated in disadvantaged communities. Reported COVID-19 deaths greatly underestimated pandemic-associated mortality.
Funding
National Institute of General Medical Sciences, Bill & Melinda Gates Foundation, National Science Foundation.
Translation
For the Hindi translation of the abstract see Supplementary Materials section.
Introduction
India is among the most severely affected countries in the ongoing COVID-19 pandemic, with over 458 000 deaths reported by Nov 1, 2021. However, the true burden of disease is uncertain because of limitations in surveillance. Analyses informed by population-based serosurveys suggest that reported COVID-19 deaths might underestimate true mortality by a factor of seven to ten,1, 2 in agreement with findings from other data sources such as household-based demographic surveys.3 In high-income countries, all-cause mortality data from comprehensive vital registration systems have provided insight into the extent of underreporting of deaths attributable to COVID-19, as well as disparities in pandemic-associated mortality across socioeconomic and demographic groups.4, 5 However, few studies of all-cause mortality have been undertaken in India and other low-income and middle-income countries.6 As the extent of COVID-19 mortality and the effect of lockdown measures on other causes of death might differ in such settings compared with high-income countries, studies of this nature in India remain an important priority.
Chennai is an administrative district within the southern state of Tamil Nadu and the centre of India's fourth largest metropolitan area. The first confirmed COVID-19 cases in Tamil Nadu were reported in Chennai and, throughout the pandemic, Chennai has surpassed all other districts of the state in reported COVID-19 cases and deaths per 1000 population (appendix 2 p 5).7 Although not the wealthiest region of India, Tamil Nadu is known for its effective public health and health-care delivery systems, and it ranks among the states with the highest per-capita health spending and largest health workforce.8 Death registrations captured by the state's Civil Registration System (CRS) closely match mortality estimates from India's demographic survey-based Sample Registration System, making Tamil Nadu one of few Indian states where civil registration systems are considered a reliable basis for mortality surveillance.9
Research in context.
Evidence before this study
We searched the terms “coronavirus disease 2019”, “COVID-19”, “all-cause”, “excess”, “deaths”, “mortality”, and “disparity” in PubMed and Google Scholar to identify studies published in English up to Sept 1, 2021, addressing the effect of the COVID-19 pandemic on deaths due to all causes, across all countries and settings, as well as studies addressing variation in COVID-19 burden across different socioeconomic groups within countries. Multiple studies of excess all-cause mortality have been undertaken in the USA, nationally and within major cities, and within both individual European countries and all countries served by the European Centre for Disease Prevention and Control, at various points in the pandemic. As of June 30, 2021, such settings recorded roughly one to two excess deaths per 1000 people associated with the COVID-19 pandemic. In New Zealand, where widespread SARS-CoV-2 transmission has not occurred, reductions in all-cause mortality have occurred during the COVID-19 pandemic. High-quality studies of excess mortality in low-income and middle-income countries were less widely available; one study generated a real-time, updated database of excess mortality estimates for 103 countries and territories based on publicly available all-cause mortality data, but information on the reliability, timeliness, and completeness of vital registration systems generating the underlying information was not readily available. We found no studies of excess all-cause mortality in India. Lastly, numerous studies have reported on ethnic and socioeconomic disparities in COVID-19 incidence and mortality, primarily in the USA and UK. Expect for large-scale studies addressing community-level predictors of variation in COVID-19 burden in Brazil and one study addressing differences in SARS-CoV-2 seroprevalence in slum and non-slum communities within Mumbai, we found no studies comparing the burden of COVID-19 (including COVID-19 mortality) across socioeconomically distinct communities within low-income and middle-income countries.
Added value of this study
In Chennai, India, where a well functioning civil registration system is in place for mortality surveillance, there were 5·2 excess deaths per 1000 individuals overall through the COVID-19 pandemic; excess mortality was substantially higher in older age groups. We observed greater increases in mortality in communities with lower socioeconomic status during the second wave of infections, but not during the first wave. We also observed reductions in all-cause mortality concentrated among young adult men and within communities of low socioeconomic status immediately after the country-wide lockdown in March 24, 2020, before SARS-CoV-2 transmission was widespread. Although lockdown-associated reductions in adult mortality were transient, we observed reduced mortality among children in Chennai throughout the pandemic.
Implications of all the available evidence
By comparison with higher-income settings, Chennai had substantial excess mortality during the COVID-19 pandemic despite the younger age distribution of its residents, with a more than two-times higher burden of excess deaths per 1000 people. COVID-19 pandemic-associated mortality in this setting is considerably underestimated by deaths reported among confirmed COVID-19 cases. Socioeconomically disadvantaged communities shouldered a greater burden of deaths during the pandemic in Chennai than higher-resource communities, although nonpharmaceutical interventions might have reduced deaths due to certain causes before widespread SARS-CoV-2 transmission was underway.
We analysed comprehensive death records from Chennai district from Jan 1, 2016, to June 30, 2021, with the aim of measuring changes in mortality during the period of the COVID-19 pandemic. We further examined differences in pandemic-associated mortality across socioeconomically distinct communities within Chennai, overall, and during specific periods of the pandemic.
Methods
Death registrations
The CRS operates under the aegis of the Registration of Births and Deaths Act of 1969, which mandates the registration of all births and deaths in India and provides standardised elements for data collection and reporting.9 Throughout India, vital statistics are recorded through a network of local registration units under a decentralised model, which states and districts are expected to customise to develop effective strategies for their distinct contexts. In Tamil Nadu, a Coordinating Committee operates within each administrative district of the state to coordinate vital registration across government departments. Heads of affected households, in conjunction with executive officers of lower administrative subunits (taluks, blocks, or villages), have legal responsibility for notification of births and deaths occurring in the community to their local registration unit, while attendant physicians are responsible for notification of deaths in health-care facilities. Local police and community health workers are responsible for reporting deaths that they are the first to observe; further provisions allow for reporting and verification of deaths by other parties that can come into contact with the deceased, such as operators of crematories or cemeteries. Performance metrics of the CRS across localities are monitored against mortality estimates from India's survey-based Sample Registration System through annual assessments.
Study design and estimation of relative mortality
For this observational study, we estimated pandemic-associated all-cause mortality during the period of the pandemic (defined as the period from March 1, 2020, to June 30, 2021) by comparing reported deaths to predictions of mortality expected under a continuation of trends observed from Jan 1, 2016, to Feb 29, 2020 (pre-pandemic). Additionally, our analyses considered three specific periods of interest: first, the first 4 weeks of India's country-wide lockdown (March 24 to April 20, 2020), before community transmission of SARS-CoV-2 was widespread in Chennai and surrounding areas;7 second, the 4-month period encompassing the first wave of the pandemic in Chennai, from May 1 to Aug 31, 2020, after which cases declined or plateaued at lower levels (appendix 2 p 26);7 and third, the 4-month period encompassing the second wave of the pandemic in Chennai, from March 1 to June 30, 2021, associated with emergence of the delta SARS-CoV-2 variant (B.1.617.2).10
To define predicted mortality, we fitted generalised linear models with a negative binomial link function to time series of the 14-day moving average of daily deaths, stratified by age group (0–9 years, 10–19 years, 20–29 years, 30–39 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years, and 80 years or older bins) and sex, over the pre-pandemic period. The models included age-specific and sex-specific population offsets and accounted for secular and seasonal trends, flexibly represented by harmonic functions (sine and cosine transformations of calendar date) fitted with 12-month, 6-month, 4-month, and 3-month period lengths (appendix 2 p 3). We sampled predicted time series of cases during the pandemic period (and accompanying 95% uncertainty intervals [UIs]) through forward model projections. We propagated uncertainty by drawing from the multivariate normal distribution of regression parameter estimates, as well as the distribution of model residuals for predicted values. We quantified increases or decreases in all-cause mortality with ratios and differences of observed versus expected deaths. Additional details of model fitting and model selection are presented in appendix 2 (p 3).
New district boundaries drawn in 2019 introduced to Chennai district areas not represented by earlier mortality surveillance. We thus limited analyses to postal index number (PIN) code areas within pre-2019 administrative boundaries; our findings should be taken to correspond to this area and population (estimated to be 4 995 398 as of 2020) rather than current district boundaries.
The collection of death registrations is a routine surveillance activity of the CRS. Our secondary data analyses were considered exempt from review by the policies of biomedical research ethics committees of the investigators' institutions.
Demographic measures
We measured changes in life expectancy among residents of Chennai during the calendar years 2020 and 2021 relative to 2019. For analyses of 2021 data, we considered scenarios of a return to age-specific and sex-specific mortality rates consistent with either pre-pandemic (2019-level) or 2020-level observations for the months of July to December. We computed life expectancy at birth for men and women on the basis of observed mortality using life tables accounting for age-specific (within 5-year age intervals) and sex-specific population sizes and deaths. To propagate uncertainty, we modelled the number of deaths within each age and sex stratum as a binomially distributed random variable, parameterised by population sizes and annual probabilities of mortality.
Socioeconomic predictors
We next aimed to determine how changes in all-cause mortality during the pandemic differed across socioeconomically distinct communities. We tabulated deaths by PIN code area and measured 13 distinct socioeconomic attributes of the population within each PIN code area (listed in appendix 2, pp 4, 6) based on the city ward within which the primary post office was contained (154 wards of Chennai, before 2019 redistricting). Within eligible PIN code areas where 1000 or more deaths were observed over the study period, we measured relative mortality during the pandemic using the ratio of observed to expected mortality. We estimated expected mortality according to the negative binomial regression framework described previously for each PIN code area (appendix 2 p 4).
We assessed whether the degree of excess pandemic-associated mortality was associated with community socioeconomic status by fitting regression models relating the outcome of relative mortality (log-transformed ratio of observed to expected mortality), by PIN code area, to each socioeconomic measure as a predictor variable. As a complementary approach aimed at reducing the dimensionality of our socioeconomic measures, we did a principal component analysis of all 13 socioeconomic variables (appendix 2 p 4) and used the same regression framework to estimate unadjusted and adjusted associations of mortality with principal component variables. We did analyses in R software (version 4.0.5).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Between Jan 1, 2016, and June 30, 2021, 336 816 deaths were reported to have occurred in Chennai, including 264 858 among individuals who resided within PIN code areas corresponding to pre-2019 district boundaries. Of the 264 858 deaths, 176 988 occurred before March 1, 2020, and 87 870 (of 88 107 expected with lagged reporting; appendix 2 p 27) occurred during the pandemic period. Under a continuation of pre-pandemic trends, 62 690 (95% UI 62 320–63 030) deaths were expected within the same population (table 1 , figure 1 ). We estimated that 25 990 (25 640–26 360) excess deaths occurred in total during the pandemic period, or 5·18 (5·11–5·25) excess deaths per 1000 people.
Table 1.
Expected and observed deaths during the COVID-19 pandemic in Chennai
| Expected deaths | Observed deaths | Excess deaths | Excess mortality ratio | Excess mortality per 1000 people | |
|---|---|---|---|---|---|
| March 24, 2020 to June 30, 2021 | |||||
| Ages 0–9 years | 980 (950 to 1010) | 668 | −310 (−340 to −280) | 0·68 (0·66 to 0·70) | −0·53 (−0·57 to −0·48) |
| Ages 10–19 years | 910 (860 to 950) | 579 | −330 (−380 to −280) | 0·64 (0·61 to 0·67) | −0·53 (−0·61 to −0·46) |
| Ages 20–29 years | 1720 (1690 to 1760) | 1530 | −190 (−230 to −160) | 0·89 (0·87 to 0·91) | −0·21 (−0·25 to −0·17) |
| Ages 30–39 years | 2930 (2890 to 2980) | 3291 | 360 (310 to 400) | 1·12 (1·11 to 1·14) | 0·40 (0·35 to 0·45) |
| Ages 40–49 years | 5560 (5480 to 5640) | 7350 | 1790 (1720 to 1870) | 1·32 (1·30 to 1·34) | 2·26 (2·16 to 2·36) |
| Ages 50–59 years | 9320 (9190 to 9420) | 13 475 | 4160 (4050 to 4280) | 1·45 (1·43 to 1·47) | 6·63 (6·46 to 6·83) |
| Ages 60–69 years | 12 950 (12 800 to 13 120) | 20 033 | 7080 (6920 to 7240) | 1·55 (1·53 to 1·57) | 21·02 (20·54 to 21·49) |
| Ages 70–79 years | 14 170 (13 990 to 14 360) | 21 687 | 7520 (7330 to 7700) | 1·53 (1·51 to 1·55) | 39·74 (38·73 to 40·69) |
| Ages ≥80 years | 14 150 (13 970 to 14 340) | 19 494 | 5350 (5150 to 5530) | 1·38 (1·36 to 1·40) | 96·90 (93·35 to 100·16) |
| All ages | 62 690 (62 320 to 63 030) | 88 107 | 25 990 (25 640 to 26 360) | 1·41 (1·40 to 1·42) | 5·18 (5·11 to 5·25) |
| Initial lockdown (March 24 to April 20, 2020) | |||||
| Ages 0–9 years | 53 (48 to 60) | 40 | −13 (−20 to −8) | 0·75 (0·67 to 0·83) | −0·02 (−0·03 to −0·01) |
| Ages 10–19 years | 41 (34 to 49) | 25 | −16 (−24 to −9) | 0·62 (0·51 to 0·73) | −0·03 (−0·04 to −0·01) |
| Ages 20–29 years | 100 (90 to 110) | 45 | −50 (−60 to −40) | 0·47 (0·43 to 0·50) | −0·06 (−0·07 to −0·05) |
| Ages 30–39 years | 150 (140 to 160) | 131 | −20 (−30 to −10) | 0·85 (0·80 to 0·91) | −0·03 (−0·04 to −0·01) |
| Ages 40–49 years | 300 (280 to 320) | 264 | −40 (−60 to −20) | 0·88 (0·82 to 0·93) | −0·05 (−0·07 to −0·02) |
| Ages 50–59 years | 500 (470 to 520) | 462 | −30 (−60 to −10) | 0·93 (0·89 to 0·98) | −0·06 (−0·10 to −0·02) |
| Ages 60–69 years | 670 (630 to 700) | 685 | 20 (−20 to 50) | 1·03 (0·98 to 1·08) | 0·05 (−0·05 to 0·16) |
| Ages 70–79 years | 760 (720 to 790) | 767 | 10 (−30 to 50) | 1·02 (0·97 to 1·07) | 0·06 (−0·14 to 0·27) |
| Ages ≥80 years | 730 (690 to 770) | 824 | 100 (60 to 130) | 1·13 (1·07 to 1·19) | 1·79 (1·06 to 2·48) |
| All ages | 3290 (3220 to 3370) | 3243 | −30 (−100 to 50) | 0·99 (0·97 to 1·01) | −0·01 (−0·02 to 0·01) |
| First wave (May 1 to Aug 31, 2020) | |||||
| Ages 0–9 years | 220 (210 to 230) | 157 | −60 (−70 to −50) | 0·72 (0·68 to 0·76) | −0·11 (−0·13 to −0·09) |
| Ages 10–19 years | 220 (200 to 240) | 121 | −100 (−120 to −70) | 0·56 (0·51 to 0·62) | −0·15 (−0·19 to −0·12) |
| Ages 20–29 years | 420 (400 to 430) | 347 | −70 (−90 to −50) | 0·83 (0·80 to 0·87) | −0·08 (−0·10 to −0·06) |
| Ages 30–39 years | 690 (670 to 720) | 683 | −10 (−30 to 10) | 0·98 (0·95 to 1·01) | −0·01 (−0·04 to 0·01) |
| Ages 40–49 years | 1290 (1260 to 1330) | 1522 | 230 (190 to 270) | 1·18 (1·15 to 1·21) | 0·29 (0·25 to 0·34) |
| Ages 50–59 years | 2140 (2090 to 2200) | 3006 | 860 (810 to 910) | 1·40 (1·37 to 1·44) | 1·39 (1·31 to 1·48) |
| Ages 60–69 years | 2940 (2880 to 3010) | 4401 | 1460 (1390 to 1520) | 1·50 (1·46 to 1·53) | 4·39 (4·18 to 4·59) |
| Ages 70–79 years | 3210 (3130 to 3290) | 5023 | 1810 (1730 to 1890) | 1·56 (1·53 to 1·60) | 9·71 (9·28 to 10·14) |
| Ages ≥80 years | 3150 (3070 to 3250) | 4349 | 1200 (1100 to 1280) | 1·38 (1·34 to 1·42) | 22·09 (20·41 to 23·66) |
| All ages | 14 290 (14 130 to 14 450) | 19 609 | 5430 (5270 to 5590) | 1·38 (1·36 to 1·40) | 1·09 (1·06 to 1·12) |
| Second wave (March 1 to June 30, 2021) | |||||
| Ages 0–9 years | 220 (210 to 230) | 139 | −80 (−100 to −70) | 0·63 (0·59 to 0·67) | −0·14 (−0·16 to −0·12) |
| Ages 10–19 years | 210 (190 to 230) | 158 | −50 (−80 to −40) | 0·75 (0·67 to 0·81) | −0·09 (−0·12 to −0·06) |
| Ages 20–29 years | 420 (400 to 430) | 430 | 10 (0 to 30) | 1·03 (0·99 to 1·07) | 0·01 (0·00 to 0·03) |
| Ages 30–39 years | 690 (670 to 710) | 1230 | 540 (520 to 560) | 1·79 (1·73 to 1·84) | 0·60 (0·58 to 0·63) |
| Ages 40–49 years | 1310 (1280 to 1350) | 2795 | 1480 (1440 to 1520) | 2·13 (2·07 to 2·19) | 1·86 (1·81 to 1·90) |
| Ages 50–59 years | 2210 (2150 to 2260) | 5177 | 2970 (2910 to 3030) | 2·34 (2·29 to 2·41) | 4·68 (4·60 to 4·77) |
| Ages 60–69 years | 3040 (2970 to 3110) | 7649 | 4610 (4540 to 4680) | 2·52 (2·46 to 2·58) | 13·51 (13·31 to 13·72) |
| Ages 70–79 years | 3370 (3290 to 3450) | 7944 | 4570 (4490 to 4650) | 2·36 (2·30 to 2·41) | 23·83 (23·41 to 24·26) |
| Ages ≥80 years | 3350 (3270 to 3440) | 6764 | 3410 (3330 to 3500) | 2·02 (1·97 to 2·07) | 60·70 (59·13 to 62·22) |
| All ages | 14 820 (14 650 to 14 990) | 32 286 | 17 700 (17 530 to 17 870) | 2·19 (2·17 to 2·22) | 3·51 (3·48 to 3·54) |
Data are n or value (95% UI). 95% UIs were generated based on parameter uncertainty and stochastic variability in model-based predicted death counts (summed across once per 2 weeks estimates, as presented in figure 1 and figure 2). We present sex-stratified counts and rates of deaths in appendix 2 (pp 7–8). Overall and sex-stratified estimates based on an alternative modelling framework are also presented in appendix 2 (pp 11–13). UI=uncertainty interval.
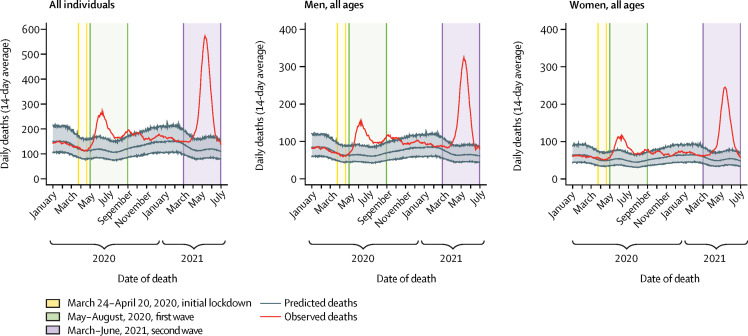
Figure 1.
Excess mortality during the COVID-19 pandemic in Chennai
We plotted 14-day moving average estimates of daily mortality in 2020 and 2021 (observed deaths), corrected for lagged reporting based on 2019 observations (appendix 2 p 27). Grey lines and shaded areas illustrate model-based expectations of the 14-day moving average, according to pre-pandemic observations, together with 95% uncertainty intervals accounting for variation in the fitted model parameters and prediction of uncertainty. Estimates applying an alternative modelling framework to generate predictions, based on pre-pandemic observations, are presented in appendix 2 (p 28).
Total excess deaths numbered 5430 (5270–5590) during the first wave and 17 700 (17 530–17 870) during the second wave (table 1). At the peak of the first and second waves (during 2-week periods surrounding June 9, 2020, and May 10, 2021), observed deaths outnumbered expected deaths by factors of 2·26 (2·01–2·54) in the first wave and 4·75 (4·26–5·36) in the second wave (figure 1). Throughout the pandemic period, Chennai district recorded 8167 deaths among confirmed COVID-19 cases within its full population (inclusive of the PIN code areas included in our analyses and areas annexed in the 2019 redistricting), with 2530 occurring during the first wave and 4037 occurring during the second wave (appendix 2 p 26). Therefore, reported deaths underestimated total pandemic-associated mortality by a factor of at least 3·18 (3·14–3·23) overall, and by factors of at least 2·15 (2·08–2·21) during the first wave and 4·38 (4·34–4·43) during the second wave.
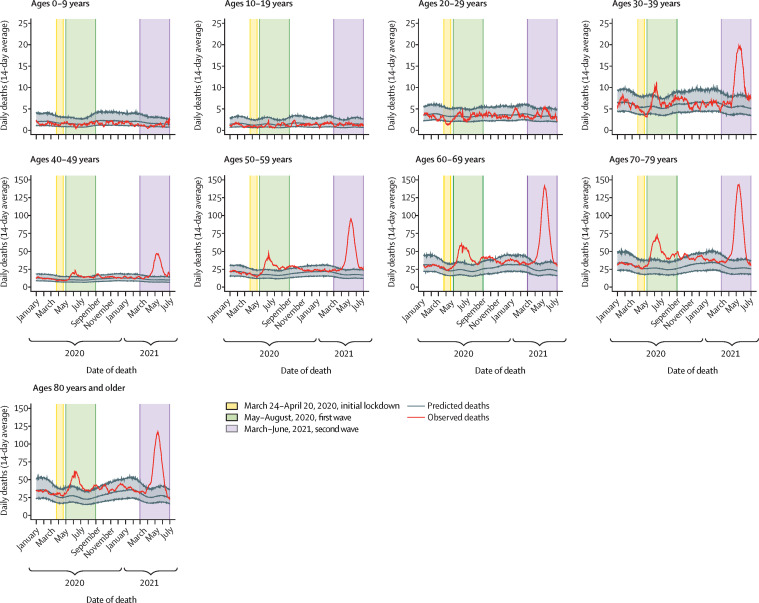
Among men and women, excess deaths numbered 6·07 per 1000 men (5·98–6·17) and 4·26 per 1000 women (4·16–4·35; appendix 2 pp 7–8). Departures from expected mortality differed substantially across ages and by sex (figure 2 ). Although increased mortality was evident for individuals aged 30 years or older, we estimated that 32% (30–34) fewer deaths occurred than expected in children aged 0–9 years, 36% (33–39) among individuals aged 10–19 years, and 11% (9–13) in those aged 20–29 years, on the basis of pre-pandemic mortality rates (table 1). Among children, the greatest reductions in mortality were evident at ages 5–9 years (appendix 2 p 9). At older ages, observed deaths translated to increases in all-cause mortality of between 12% (11–14) at ages 30–39 years and 55% (53–57) at ages 60–69 years, with similar age-specific patterns observed among men and women (appendix 2 pp 7–8). Total excess mortality spanned 0·40 (0·35–0·45) to 96·90 (93·35–100·16) deaths per 1000 individuals between ages 30–39 years and age 80 years or older (table 1).
Figure 2.
Age-specific excess mortality during the COVID-19 pandemic in Chennai
We plotted 14-day moving average estimates of daily mortality in 2020 and 2021 by age (observed deaths), corrected for lagged reporting based on 2019 observations (appendix 2 p 27). Grey lines and shaded areas illustrate model-based expectations of the 14-day moving average, according to pre-pandemic observations, with 95% uncertainty intervals accounting for variation in the fitted model parameters and prediction of uncertainty. Estimates applying an alternative modelling framework to generate predictions, based on pre-pandemic observations, are presented in appendix 2 (p 29), as well as estimates computed from 7-day (appendix 2 p 30) and 28-day (appendix 2 p 31) moving averages. For ease of visualisation, age groups from 0–9 years to 30−39 years have a y-axis scale from 0 to 25 excess deaths per 2-week period, while age groups from 40−49 years to 80 years and older have a y-axis scale from 0 to 150 excess deaths per 2-week period.
Analyses done with an alternative model formulation to account for changes associated with Chennai's 2019 redistricting provided a marginally poorer fit for the pre-lockdown period of 2020 (appendix 2 pp 10, 28–29). Under this analysis approach, overall and age-specific and sex-specific estimates of excess deaths were similar to those of our primary analysis (appendix 2 pp 11–13), as were the results of sensitivity analyses fitting prediction models to time series aggregated with shorter (7-day) and longer (28-day) windows for the moving average (appendix 2 pp 14–15, 30–31).
Increased mortality was apparent for men and women aged 40–49 years and older during the first wave, whereas, during the second wave, increases were evident for men from ages 30–39 years and older and for women from ages 20–29 years and older (appendix 2 pp 7–8). Among individuals aged 20–29 years and 30–39 years, deaths declined immediately after lockdown measures were implemented on March 24, 2020 (figure 2). The greatest reduction in mortality occurred in men aged 20–29 years, with 58% (54–62) fewer deaths than expected during the early lockdown period; reduced mortality was apparent through ages 50–59 years among men during the early lockdown.
On the basis of 2019 mortality data, pre-pandemic life expectancy at birth in Chennai was 70·7 years (70·5–70·8), 68·0 years (67·9–68·2) for men and 73·6 years (73·4–73·8) for women (table 2 , appendix 2 pp 16–19). Observed mortality during 2020 corresponded to a 1·2-year (1·0–1·3) decline in mean life expectancy at birth relative to 2019 levels, whereas in 2021, estimated declines ranged from 3·6 years (3·4–3·8) to 4·2 years (4·1–4·4) under scenarios corresponding to 2019-level or 2020-level mortality during the months of July to December. For individuals who had a pandemic-associated death, mean life-year losses totalled 12·7 years (12·5–13·0) in 2020 and 15·5 years (15·3–15·6) years in 2021 for men, and 15·8 years (15·5–16·2) in 2020 and 17·1 years (16·9–17·4) in 2021 for women (appendix 2 p 20).
Table 2.
Life expectancy losses during the COVID-19 pandemic in Chennai
| Mean life expectancy at birth, years | Decrease in life expectancy relative to 2019, years | |
|---|---|---|
| Overall | ||
| 2019 | 70·7 (70·5–70·8) | (ref) |
| 2020 | 69·5 (69·4–69·6) | 1·2 (1·0–1·3) |
| 2021 (assuming July–December per 2019 baseline)* | 67·1 (67·0–67·2) | 3·6 (3·4–3·8) |
| 2021 (assuming July–December per 2020)† | 66·4 (66·3–66·5) | 4·2 (4·1–4·4) |
| Men | ||
| 2019 | 68·0 (67·9–68·2) | (ref) |
| 2020 | 66·9 (66·8–67·1) | 1·1 (0·8–1·3) |
| 2021 (assuming July–December per 2019 baseline)* | 64·6 (64·4–64·7) | 3·5 (3·2–3·7) |
| 2021 (assuming July–December per 2020)† | 63·9 (63·8–64·0) | 4·1 (3·9–4·4) |
| Women | ||
| 2019 | 73·6 (73·4–73·8) | (ref) |
| 2020 | 72·5 (72·3–72·6) | 1·1 (0·9–1·4) |
| 2021 (assuming July–December per 2019 baseline)* | 70·0 (69·8–70·1) | 3·6 (3·4–3·9) |
| 2021 (assuming July–December per 2020)† | 69·4 (69·3–69·6) | 4·2 (4·0–4·4) |
Data are estimates (95% uncertainty interval). Life tables underlying life expectancy estimates are presented in appendix 2 (pp 13–14) for men and women. Estimated life year losses for individuals who had a pandemic-associated death in 2020 and 2021 are also presented in appendix 2 (p 15).
Estimates apply mortality rates (scaled to 2021 population projections) from 2019 for the months of July to December.
Estimates apply mortality rates (scaled to 2021 population projections) from 2020 for the months of July to December.
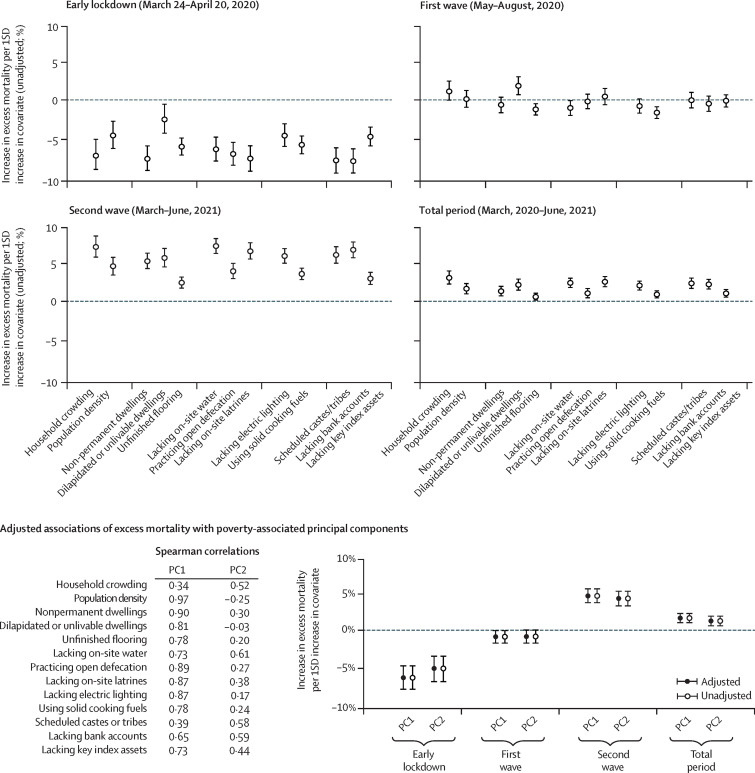
70 PIN code areas had 1000 or more deaths observed over the study period. Observed mortality within each of these PIN code areas ranged from 6·7% (1·2–11·4) lower to 69·7% (58·1–82·2) higher than expected levels during the first wave (appendix 2 p 32), but differences were not consistently associated with socioeconomic attributes of communities (figure 3 , appendix 2 p 21). During the second wave, observed deaths within each PIN code area ranged from 54·6% (47·3–62·8) to 301·8% (250·8–466·8) higher than expected levels. On average, each increase by 1 SD in census-derived measures of community socioeconomic deprivation was associated with a 2·8% to 7·0% increase in mortality over pre-pandemic levels. These socioeconomic disparities in pandemic-associated mortality were likewise evident for the overall pandemic period, with 0·7% to 2·8% higher mortality observed per 1 SD increase in each measure of community socioeconomic deprivation. Similar patterns were evident in analyses of deaths among individuals aged 50 years or older, among whom deaths were more likely to be attributable to COVID-19 (appendix 2 p 22). During the first 4 weeks of the lockdown period, and before SARS-CoV-2 transmission was widespread within Chennai, observed deaths within each PIN code area were between 62·3% (56·3–66·8) lower and 37·9% (23·0–58·0) higher than expected levels. For every increase by 1 SD in measures of community socioeconomic deprivation, PIN code areas had 3·6% to 8·6% lower mortality than expected on the basis of pre-pandemic observations.
Figure 3.
Socioeconomic attributes predicting differences in excess mortality across communities of Chennai
We illustrate differences in excess mortality for the first 4 weeks of the country-wide lockdown, the first wave, the second wave, and the total pandemic period, associated with a 1 SD increase in each measure of community-level socioeconomic deprivation (detailed in appendix 2 p 6). Additionally, we relate pandemic-associated mortality to the first two principal components derived across all 13 socioeconomic variables, alongside measures of Spearman's correlation (ρ) between each principal component and community attributes (additional details on the principal component analysis are presented in appendix 2 p 23). Time series of relative mortality across deciles of community socioeconomic status, as measured by the first principal component, are presented in appendix 2 (p 33). For all panels, lines denote 95% uncertainty intervals based on regression models fit across draws from the distribution of excess mortality measures, with (log-transformed) ratios of observed to expected deaths defined as the outcome variable (further methodological details are presented in appendix 2 p 4). Values are corrected for lagged reporting of deaths based on 2019 observations (appendix 2 p 27). Numerical estimates for all age groups corresponding to values presented in this figure are presented in appendix 2 (pp 21, 24), as well as estimates for individuals aged 50 years or older (pp 22, 25). Deaths are aggregated by PIN code areas; analyses include PIN code areas for which 1000 deaths or more were registered over the study period. Measures of excess mortality by PIN code area are presented in appendix 2 (p 32). PC=principal component.
We identified similar associations in analyses relating pandemic-associated mortality in each PIN code area to principal component variables strongly associated with community-level measures of disadvantage (figure 3, appendix 2 pp 23–25). Plotted estimates of pandemic-associated mortality over time for communities stratified by socioeconomic status decile are presented in appendix 2 (p33).
Discussion
We estimated that 5·2 excess deaths occurred per 1000 residents during the COVID-19 pandemic in Chennai, representing a 41% increase over typical mortality levels. Most excess deaths occurred during the second wave of the pandemic, when mortality peaked at levels 4·75-times higher than pre-pandemic observations. However, fewer deaths were registered among children than expected on the basis of pre-pandemic observations. Communities with lower socioeconomic status had reductions in mortality during the early lockdown, but also had the greatest increases in mortality during the second wave. Therefore, such communities had a disproportionate burden of excess deaths overall. These observations provide insight into the impact of the pandemic across demographic groups in an urban setting within India, where knowledge of morbidity and mortality associated with COVID-19 remains incomplete.
Our estimates of excess mortality during the COVID-19 pandemic in Chennai exceed those from numerous higher-income settings. Although the USA, UK, Italy, and Spain have older populations than that of India, these countries recorded 1·6–2·1 excess deaths per 1000 residents through June, 2021,6 compared with 5·2 in Chennai. Seroprevalence studies in Chennai identified 41% prevalence of antibody reactivity in October–November, 2020,11 and 82% in June–July, 2021,12 at the conclusion of the first and second waves. Our findings show considerable excess mortality associated with this uncontrolled SARS-CoV-2 spread, confirming predictions from early modelling studies13, 14 and underscoring the practical limitations of efforts to mitigate COVID-19 mortality through shielding of older or high-risk individuals amid extensive community transmission.15 The high burden of COVID-19 associated mortality in this setting, and the concentration of excess deaths in socioeconomically disadvantaged communities, casts doubt on hygiene-related hypotheses of reduced SARS-CoV-2 severity in low-income and middle-income countries due to prevalent immunity from other infections.16, 17 Assuming that most observed excess deaths were COVID-19-related fatalities, the infection-fatality ratio in Chennai corresponding to 5·2 deaths per 1000 people and 82% seroprevalence as of July, 2021, would be 0·6%, resembling estimates from demographically similar settings.18
Few studies have addressed socioeconomic disparities in COVID-19 burden within India and other low-income and middle-income countries. Our findings of greater excess mortality in disadvantaged communities, particularly during the second wave, might reflect the need to work outside the home in such communities and the higher risk of transmission within crowded housing. Lower access to care in disadvantaged communities might also contribute to excess mortality, particularly if severe shortages in health-care capacity exacerbated pre-existing disparities in health-care access during the severe second wave. By contrast, we did not identify greater excess mortality in disadvantaged communities during the first wave, potentially reflecting a higher likelihood of SARS-CoV-2 introduction and early spread within communities with greater risk of pre-lockdown SARS-CoV-2 importation through inter-state or international travel. A seroprevalence study in June–July, 2020, identified higher cumulative prevalence of SARS-CoV-2 infection within slum communities of Mumbai than in other neighborhoods.19 Although the study also reported higher estimates of the infection-fatality ratio in non-slum communities, findings should be interpreted cautiously due to differences in the age distribution of slum and non-slum settings and the potential for weaker case-based surveillance in slums.1, 2 Prevalent naturally-acquired immunity in communities hit hard by early waves of SARS-CoV-2 transmission might have affected which settings were most vulnerable to having cases and deaths after the emergence of the delta variant, which is associated with enhanced transmissibility and clinical severity.10 It is important to note that our aggregation of deaths by PIN code area might obscure socioeconomic distinctions across communities in Chennai, where formal and makeshift housing are often closely interspersed. Direct comparisons of outcomes among residents of slum and non-slum communities might yield additional insights into differences in COVID-19 burden at extreme ends of the socioeconomic spectrum.20
The reasons for mortality reductions among children and young adult men during the early lockdown merit consideration. Unintentional injuries are the leading single cause of death among Indian adults younger than 40 years, particularly among men,21 and occur disproportionately in communities of lower socioeconomic status.22 Therefore, our findings might reflect reduced incidence of road accidents, falls, occupational injuries, and other similar causes of death as a result of lockdown-associated measures, including a ban on alcohol sales. Reported increases in the proportion of medically unattended births23 might also help to explain why young adult women and men did not have commensurate changes in mortality during the early lockdown period and first wave in our analyses. We also identified sustained reductions in mortality throughout the pandemic period for individuals aged 0–9 years and 10–19 years, including during the second wave. Communicable diseases are the leading cause of death within these age groups in India and account for 87% of deaths among children younger than 5 years. Reductions in transmission of both respiratory24, 25 and enteric infections26, 27 have been reported elsewhere after implementation of non-pharmaceutical interventions and might explain our observations. Lockdown measures in India have also been associated with decreased access to health care and exacerbation of common non-communicable or chronic conditions28 including cancer,29 diabetes,30 tuberculosis,31 and others.32, 33 Longer-term studies remain important to determine the effect of these changes on mortality.
Although we cannot rule out the possibility that the COVID-19 pandemic interrupted the functioning of civil mortality registration, potentially to different extents across socioeconomically distinct communities, several factors support the external validity of our findings. Expected and observed deaths were in close alignment before the lockdown and during the period between the two COVID-19 waves. During the early lockdown, reductions in mortality were more pronounced among men than among women, whereas Indian vital surveillance systems are generally more susceptible to under-ascertainment of female mortality.34 Lastly, previous analyses have suggested greater degrees of underreporting of COVID-19 deaths among older age groups in India,1, 2 by contrast with the observed concentration of excess all-cause mortality among older age groups at the start of lockdowns and throughout the pandemic period. Deaths among older adults might owe, partly, to delayed presentation to medical facilities, including among individuals with silent hypoxemia.35 Breakdowns in all-cause death registrations would lead our study to underestimate all-cause mortality during the pandemic, leading to conservative conclusions about excess deaths and life-year losses associated with COVID-19. Factors contributing to under-ascertainment of COVID-19 deaths during the pandemic in India merit closer investigation.
Our study has limitations. We analysed deaths due to all causes; determining the proportion of excess deaths attributable to interruptions in care for conditions other than COVID-19 remains a priority, although prospective studies might be needed to support reliable ascertainment of cause of death.16 Chennai residents who died in other districts might be missed by CRS data; however, the combination of inter-state and inter-district travel restrictions during the COVID-19 pandemic7 and the concentration of tertiary health-care facilities in Chennai reduce the likelihood of undercounting due to this factor. Our analyses of differences in mortality across communities relied on socioeconomic data from the most recent census of India, undertaken in 2011. As built environments and standards of living have changed within communities since then, estimated measures of association are probably dampened by misclassification. Community characteristics should be interpreted as indicators of relative disadvantage rather than precise measurements of current conditions.
We identified substantial mortality associated with the COVID-19 pandemic in Chennai, India, exceeding estimates of per-capita excess deaths from higher-income settings despite India's younger age distribution.6 Studies of all-cause mortality provide a valuable opportunity to overcome limitations affecting COVID-19 burden estimates from other data sources, and they provide additional context for estimation of pandemic-associated mortality by incorporating deaths potentially missed by COVID-19 surveillance, deaths attributable to delayed health-care seeking for other conditions, and deaths associated with other conditions occurring secondary to COVID-19.2 Similar assessments should be undertaken in other low-income and middle-income settings, as well as in other parts of India, to understand demographic effects of the pandemic and to inform efforts aimed at enhancing mitigation, including expanded vaccine distribution to populations where access remains inadequate.
Data sharing
Aggregated civil registration system data on births and deaths are available online at the district level for all districts of Tamil Nadu (http://www.crstn.org/birth_death_tn/). Public sharing of disaggregated mortality records used in this analysis was not permitted by the Directorate of Health and Preventive Medicine of Tamil Nadu. Individuals wishing to access these data and accompanying data dictionaries should contact the Directorate of Health and Preventive Medicine of Tamil Nadu (dphpm.tn@nic.in) to share analysis protocols and enter into a formal data access agreement.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
This work was supported by the Bill & Melinda Gates Foundation (INV029062 to RL), the National Science Foundation (CCF1918628 to RL), and the National Institute of General Medical Sciences (MIDASNI2020–3 to JAL).
Contributors
JAL did the literature search. JAL, AM, and RL did the study design. AM, TN, TSS, CMB, and JAL analysed the data. JAL wrote the original draft. All authors contributed to data interpretation and to the review and editing of the manuscript. TSS, TN, and JAL accessed and verified the data. All authors had final responsibility for the decision to submit for publication.
Supplementary Materials
References
- 1.Pons-Salort M, John J, Watson OJ, et al. Reconstructing the COVID-19 epidemic in Delhi, India: infection attack rate and reporting of deaths. medRxiv. 2021 doi: 10.1101/2021.03.23.21254092. published online March 26. [DOI] [Google Scholar]
- 2.Laxminarayan R, Chandra Mohan B, Vinay TG, Arjun Kumar KV, Wahl B, Lewnard JA. SARS-CoV-2 infection and mortality during the first epidemic wave in Madurai, south India: a prospective, active surveillance study. Lancet Infect Dis. 2021 doi: 10.1016/S1473-3099(21)00393-5. published online Aug 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anand A, Sandefur J, Subramanian A. Three new estimates of India's all-cause excess mortality during the COVID-19 pandemic. 2021. https://cgdev.org/sites/default/files/three-new-estimates-indias-all-cause-excess-mortality-during-covid-19-pandemic.pdf
- 4.Weinberger DM, Chen J, Cohen T, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020;180:1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Y-H, Glymour MM, Catalano R, et al. Excess mortality in California during the coronavirus disease 2019 pandemic, March to August 2020. JAMA Intern Med. 2021;181:705–707. doi: 10.1001/jamainternmed.2020.7578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karlinsky A, Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. eLife. 2021;10 doi: 10.7554/eLife.69336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laxminarayan R, Wahl B, Dudala SR, et al. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science. 2020;370:691–697. doi: 10.1126/science.abd7672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parthasarathi R, Sinha SP. Towards a better health care delivery system: the Tamil Nadu model. Indian J Community Med. 2016;41:302–304. doi: 10.4103/0970-0218.193344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rao C, Gupta M. The civil registration system is a potentially viable data source for reliable subnational mortality measurement in India. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Twohig KA, Nyberg T, Zaidi A, et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect Dis. 2021 doi: 10.1016/S1473-3099(21)00475-8. published online Aug 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malani A, Ramachandran S, Tandel V, et al. SARS-CoV-2 seroprevalence in Tamil Nadu in October-November 2020. medRxiv. 2021 doi: 10.1101/2021.02.03.21250949. published online April 3. [DOI] [Google Scholar]
- 12.The Hindu Tamil Nadu's seroprevalence stands at 66·2% 2021. https://www.thehindu.com/news/national/tamil-nadu/tns-seroprevalence-stands-at-662/article35660072.ece
- 13.Walker PGT, Whittaker C, Watson OJ, et al. The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science. 2020;369:413–422. doi: 10.1126/science.abc0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferguson NM, Laydon D, Nedjati-Gilani G, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. 2020. [DOI] [PMC free article] [PubMed]
- 15.Dahab M, van Zandvoort K, Flasche S, et al. COVID-19 control in low-income settings and displaced populations: what can realistically be done? Confl Health. 2020;14:54. doi: 10.1186/s13031-020-00296-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mwananyanda L, Gill CJ, MacLeod W, et al. Covid-19 deaths in Africa: prospective systematic postmortem surveillance study. BMJ. 2021;372:n334. doi: 10.1136/bmj.n334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roy S. Low-income countries are more immune to COVID-19: a misconception. Indian J Med Sci. 2020;72:5–7. [Google Scholar]
- 18.O'Driscoll M, Dos Santos GR, Wang L, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2021;590:140–145. doi: 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- 19.Malani A, Shah D, Kang G, et al. Seroprevalence of SARS-CoV-2 in slums versus non-slums in Mumbai, India. Lancet Glob Health. 2021;9:e110–e111. doi: 10.1016/S2214-109X(20)30467-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murhekar MV, Bhatnagar T, Selvaraju S, et al. Prevalence of SARS-CoV-2 infection in India: findings from the national serosurvey, May–June 2020. Indian J Med Res. 2020;152:48–60. doi: 10.4103/ijmr.IJMR_3290_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Menon GR, Singh L, Sharma P, et al. National burden estimates of healthy life lost in India, 2017: an analysis using direct mortality data and indirect disability data. Lancet Glob Health. 2019;7:e1675–e1684. doi: 10.1016/S2214-109X(19)30451-6. [DOI] [PubMed] [Google Scholar]
- 22.Ram U, Jha P, Gerland P, et al. Age-specific and sex-specific adult mortality risk in India in 2014: analysis of 0·27 million nationally surveyed deaths and demographic estimates from 597 districts. Lancet Glob Health. 2015;3:e767–e775. doi: 10.1016/S2214-109X(15)00091-1. [DOI] [PubMed] [Google Scholar]
- 23.Kumari V, Mehta K, Choudhary R. COVID-19 outbreak and decreased hospitalisation of pregnant women in labour. Lancet Glob Health. 2020;8:e1116–e1117. doi: 10.1016/S2214-109X(20)30319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brueggemann AB, Jansen van Rensburg MJ, Shaw D, et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021;3:e360–e370. doi: 10.1016/S2589-7500(21)00077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang L-P, Han J-Y, Zhou S-X, et al. The changing pattern of enteric pathogen infections in China during the COVID-19 pandemic: a nation-wide observational study. Lancet Reg Health West Pac. 2021;16 doi: 10.1016/j.lanwpc.2021.100268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kraay ANM, Han P, Kambhampati AK, Wikswo ME, Mirza SA, Lopman BA. Impact of nonpharmaceutical interventions for severe acute respiratory syndrome coronavirus 2 on norovirus outbreaks: an analysis of outbreaks reported By 9 US states. J Infect Dis. 2021;224:9–13. doi: 10.1093/infdis/jiab093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh K, Kondal D, Mohan S, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. 2021;21:685. doi: 10.1186/s12889-021-10708-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharma J, Mahajan A, Bakhshi S, et al. The impact of COVID-19 pandemic on access to treatment for children with cancer in India and treating center practices. Cancer. 2021 doi: 10.1002/cncr.33945. published online Oct 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dayal D, Gupta S, Raithatha D, Jayashree M. Missing during COVID-19 lockdown: children with onset of type 1 diabetes. Acta Paediatr. 2020;109:2144–2146. doi: 10.1111/apa.15443. [DOI] [PubMed] [Google Scholar]
- 31.Jain VK, Iyengar KP, Samy DA, Vaishya R. Tuberculosis in the era of COVID-19 in India. Diabetes Metab Syndr. 2020;14:1439–1443. doi: 10.1016/j.dsx.2020.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pati S, Mahapatra P, Kanungo S, Uddin A, Sahoo KC. Managing multimorbidity (multiple chronic diseases) amid COVID-19 pandemic: a community based study from Odisha, India. Front Public Health. 2021;8 doi: 10.3389/fpubh.2020.584408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nasta AM, Goel R, Kanagavel M, Easwaramoorthy S. Impact of COVID-19 on general surgical practice in India. Indian J Surg. 2020;82:1–5. doi: 10.1007/s12262-020-02443-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Basu JK, Adair T. Have inequalities in completeness of death registration between states in India narrowed during two decades of civil registration system strengthening? Int J Equity Health. 2021;20:195. doi: 10.1186/s12939-021-01534-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Etherajan T, Zahir Hussain S, Rajendran K, et al. Profile of COVID-19 patients at zero delay COVID-19 ward, tertiary care hospital in South India. J Prim Care Community Health. 2021;12 doi: 10.1177/21501327211035094. 21501327211035094. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Aggregated civil registration system data on births and deaths are available online at the district level for all districts of Tamil Nadu (http://www.crstn.org/birth_death_tn/). Public sharing of disaggregated mortality records used in this analysis was not permitted by the Directorate of Health and Preventive Medicine of Tamil Nadu. Individuals wishing to access these data and accompanying data dictionaries should contact the Directorate of Health and Preventive Medicine of Tamil Nadu (dphpm.tn@nic.in) to share analysis protocols and enter into a formal data access agreement.