Abstract
Understanding the mechanisms that regulate cancer progression is pivotal for the development of new therapies. Although p53 is mutated in half of human cancers, its family member p73 is not. At the same time, isoforms of p73 are often overexpressed in cancers and p73 can overtake many p53 functions to kill abnormal cells. According to the latest studies, while p73 represses epithelial–mesenchymal transition and metastasis, it can also promote tumour growth by modulating crosstalk between cancer and immune cells in the tumor microenvironment, M2 macrophage polarisation, Th2 T-cell differentiation, and angiogenesis. Thus, p73 likely plays a dual role as a tumor suppressor by regulating apoptosis in response to genotoxic stress or as an oncoprotein by promoting the immunosuppressive environment and immune cell differentiation.
Keywords: immuno-oncology, transcription, p53, p73, tumour microenvironment, epithelial-mesenchymal transition, EMT
1. Introduction
Alterations of p73 activities are associated with cancer hallmarks including cell cycle regulation, replicative immortality, and genomic instability. However, p73-driven changes of these properties are not sufficient for cancer formation per se and can be detected in normal cells as well. The other factors crucial for tumour development is tumour escape from the recognition by immune cells and the formation of the pro-inflammatory tumour microenvironment. It is worth noting that the ability of tumour cells to invade surrounding tissues and metastasise is the main cause of death from cancers.
As extensively described, the tumor suppressor p53, often dubbed as “genome guardian”, is involved in the regulation of these hallmarks of cancer. p53 belongs to the family of transcription factors that comprises three proteins: p53, p63, and p73 [1,2,3]. p63 is the master regulator of epidermal development and homeostasis [4,5,6], a process largely dependent on complex enzymatic processing [2,7,8,9,10,11,12,13]. All three members of the p53 family are present in tumour cells and are expressed as multiple isoforms, which often play opposite functions in tumorigenesis.
While p53 is lost or mutated in most tumours, mutations in the Tp73 gene are relatively rare [14,15,16,17,18,19]. On the other hand, specific p73 isoforms are overexpressed in a variety of malignancies and serve as biomarkers of aggressiveness of the disease [20,21,22,23,24,25,26,27].
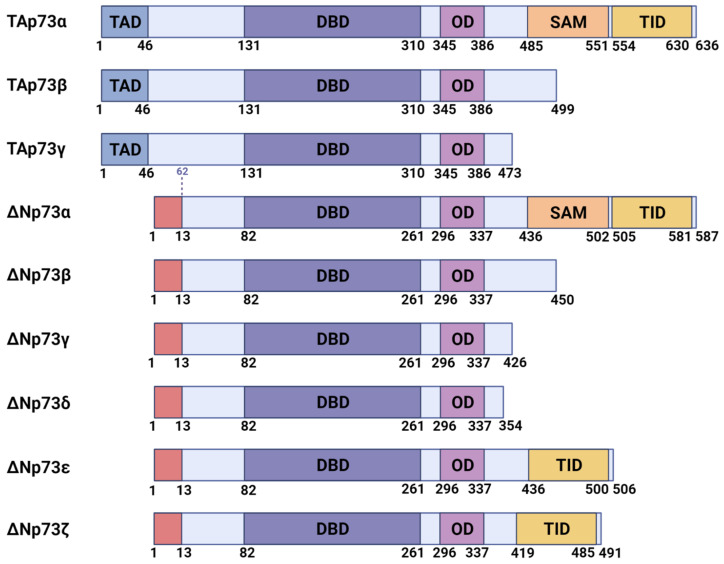
Based on the domain structure, the p73 isoforms can be roughly divided into two classes (Figure 1). Transcriptionally competent p73 isoforms with the full-length N-terminal domain are transcribed from the first external promoter of the Tp73 gene [28,29,30]. The second intragenic promoter of the Tp73 gene produces so-called DN-isoforms (DNp73) lacking the transcriptional activator domain (TAD) but retaining their DNA binding domains. Since the DNA binding domain is conserved within the p53 family, p73 can bind the promoters of the subset of the p53 target genes regulating essential mechanisms in the cell cycle (p21), apoptosis (Bax, Fas, PUMA), and metabolism [31,32,33,34,35,36]. In general, DN-isoforms repress transcription of the p53/TAp73 target genes [37,38,39], but in combination with other proteins, they can activate a set of genes that is very different from those activated by the TAp73 [40,41,42,43,44]. Both TAp73 and p53 activate the DNp73 promoter creating a negative feedback loop [45,46,47].
Figure 1.
Major isoforms of p73 and their domain structure. TAD, transactivation domain, present in the transcriptionally active (TA) isoforms with a full-length N-terminus. N-terminally truncated (DN) isoforms have a distinct N-terminus (the first 13 N-terminal amino acids). DBD, DNA-binding domain; OD, oligomerization domain; SAM, sterile alpha motif; TID, transcriptional inhibitory domain.
Therefore, transcriptionally active p73 isoforms (TAp73) generally possess pro-apoptotic and anti-oncogenic properties, while the N-terminally truncated isoforms (DNp73) tend to be anti-apoptotic and pro-oncogenic [24,48,49,50,51,52,53,54,55].
At the C- terminus of p73, alternative splicing generates a variety of isoforms: α, β, γ, δ, ε, and ζ [26,56] (Figure 1). The full-length p73α isoform contains a distally located sterile alpha motif (SAM) domain that is absent in p53. This domain allows p73 to act both as a transcriptional repressor by preventing interaction with p300/CBP [57] and as a transcriptional co-activator by promoting interactions with c-Jun, Nfkb, and ATF3 transcription factors [58,59,60,61,62,63,64].
Despite certain structural differences, the p73 and p53 proteins have a high degree of homology. Moreover, the signaling pathways that regulate p73 and p53 are also similar [65,66]. For example, the DNA damage response pathway activates both proteins [67]. Furthermore, similar to p53, the p73 transcription activity is repressed by the MDM2 E3 ligase [68,69,70,71]. However, in contrast to p53, this interaction does not result in p73 degradation [72,73,74,75]. Therefore, the loss of p53 functions in cancer can be partially compensated by TAp73 [76,77,78,79].
As a result of their structural similarity, certain p53 mutants interact with p73, causing dysregulation of p73 and hence, affecting the antitumor effect [80,81]. Furthermore, the wild-type p53 has been recently shown to interact with p73 as well, inducing apoptosis via JNK-induced p53 Thr81 phosphorylation [82]. Similarly, TAp73a and the Δ133 isoform of p53 act synergistically to promote the expression of several DNA repair genes (RAD51, LIG4, and RAD52) through binding to the p53-responsive elements in the promoters of these genes [83]. In turn, the DNp73 isoform represses the ATM-p53 mediated DNA damage response directly at the sites of DNA damage [84]. Overexpression of DNp73 in tumours can inhibit the DNA binding and tumour-suppressive functions of p53 leading to cancer progression [48,50,85]. Thus, the precise functional outcome of the p73-p53 interaction depends on which particular isoform of each protein participates in the interaction, thus providing yet another layer of complexity to the regulation of the p73/p53 network in cancer.
The later stages of cancer are associated with well-known cancer hallmarks [86] including induction of angiogenesis to feed the growth of cancer cells [87,88], activation of metastasis driven by the epithelial-to-mesenchymal transition (EMT) [89,90,91], evasion from the immune surveillance, and formation of the tumor microenvironment [92,93,94,95,96,97].
In this review, we summarised the literature data suggesting that while repressing epithelial-mesenchymal transition and metastasis in some cancers, the p73 transcriptional activity can promote cancer growth by modulating the cytokine excretion of cancer and immune cells, thereby promoting polarisation of immune cells to tumorigenic phenotypes in tumour microenvironment and inducing angiogenesis. Thus, we speculate that p73 is likely to play a dual role in tumorigenesis acting as a tumour suppressor by regulating apoptosis in response to genotoxic stress and as an oncoprotein promoting the immunosuppressive environment and immune cell differentiation.
2. Angiogenesis Induction
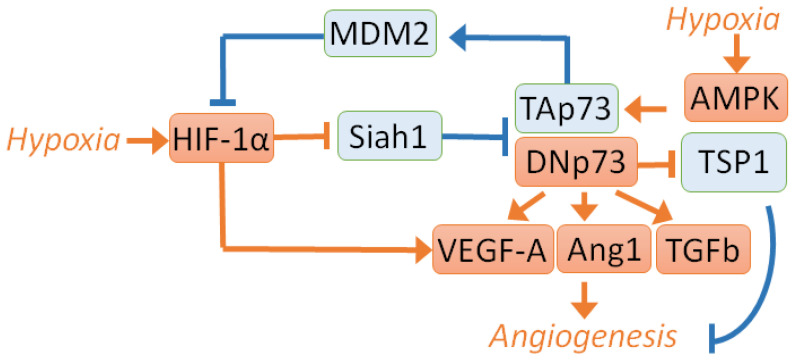
Angiogenesis is the process of forming new blood vessels from pre-existing vessels. This process is vital for tumour development since cancer cells actively proliferate and require ample nutrition and oxygen supply [98]. Several studies assessed the role of p73 in angiogenesis (Figure 2).
Figure 2.
Regulation of angiogenesis by p73. The antiangiogenic signaling is shown in blue, and proangiogenic signalling is shown in red. TAp73 inhibits angiogenesis via MDM2-mediated degradation of HIF-1α [99], whereas the loss of TAp73 and overexpression of DNp73 results in the increased HIF-1α activity and upregulation of proangiogenic cytokines [88]. In turn, TA- and DN- p73 isoforms are stabilised by HIF-1α-dependent suppression of the Siah1-mediated degradation during hypoxia [100]. Similarly, TAp73 can be stabilised by AMPK [104]. Consequently, DNp73 or TAp73 can target VEGF-A, Ang1, and TGFb to promote angiogenesis. On the contrary, TSP-1 is repressed by DNp73, which leads to enhanced angiogenesis in xenograft cancer models [53,102,106].
One of the central angiogenic regulators is the transcriptional factor HIF-1α (hypoxia-inducible factor 1α). Under normoxic conditions, HIF-1a is rapidly degraded due to post-translational modifications and stabilizes upon hypoxia. Importantly, hypoxia is the condition that is prevalent in solid tumors. TAp73 has been demonstrated to inhibit angiogenesis via HIF-1α degradation by an E3 ubiquitin ligase, MDM2 [99]. Another study showed that the loss of TAp73 and overexpression of the DNp73 isoform resulted in elevated angiogenic activity, i.e., augmented HIF-1α-mediated expression of proangiogenic cytokines [88]. These data were obtained using the mice and zebrafish models as well as analysis of publicly available breast cancer RNA sequencing data. These two studies suggest that TAp73 can reduce the HIF-1α activity to attenuate the angiogenic phenotype, which was prevented by DN-p73.
On the other hand, p73 itself is stabilised by different mechanisms upon hypoxia. Experiments on several cancer cell cultures of different origins with different statuses of p53 and p73 revealed that under hypoxic conditions, the TAp73 was stabilised by HIF-1α, which suppressed the E3 ligase Siah1. Siah1 was shown to mediate the p73 degradation [100]. The ChIP assay on MEFs demonstrated that TAp73 bound to the promoter of the proangiogenic VEGF-A (Vascular endothelial growth factor A) gene and activated its expression. In contrast, another study found that under normoxic conditions, p73 inhibited VEGF expression. Importantly, these results were obtained using two p53-deficient cell lines (Hek-293 and Saos2) [101], which raises the question of whether the p53 status plays any role in the outcome of p73 action.
In line with this, the loss of or mutations in the p53 gene induced the antiangiogenic activity of p73. On the contrary, the presence of wild-type p53 leads to the proangiogenic activity of p73 in HCT116 cells [102]. The p73 overexpression increases VEGF production, concomitantly decreasing the expression of one of the major negative regulators of the angiogenesis thrombospondin-1 (TSP-1). TSP-1 repression was observed in p73 overexpressing ovarian carcinoma cells A2780 bearing wild-type p53. Furthermore, p73 overexpressing tumours showed elevated vascularisation. These data are consistent with recent research, which revealed a positive correlation between the expression of TAp73, mutant p53, and vasohibin-1. Vasohibin-1 is an antiangiogenic factor that inhibits the VEGF expression in lung adenocarcinoma [103]. Summarising these studies, it is tempting to speculate that p53 status affects the role of TAp73 in angiogenesis in a compensatory way, but this hypothesis requires additional research.
Besides HIF-1α, an adenosine monophosphate-dependent protein kinase (AMPK), which is activated by hypoxia, also stabilises TAp73 [104]. In hypoxia, blunting the AMPK signaling has been shown to reduce the protein level of TAp73 by allowing Siah1 to ubiquitinylate p73. In contrast, activation of AMPK alone in the absence of hypoxia maintains the TAp73 protein without repressing Siah1. However, the AMPK-mediated stabilisation of TAp73 without hypoxia may be insufficient to induce the tube formation by endothelial cells [104].
Like TAp73, DNp73 can be stabilised under hypoxic conditions [105]. DNp73 was found to be preserved by HIF-1α, a master regulator of transcription under hypoxic conditions. The latter acts upstream of Siah1 to abolish its destabilising activity against DNp73 in hypoxia. HIF-1α regulates the expression of vascular endothelial growth factor, VEGF, which, in turn, controls angiogenesis (Figure 1). Since p73 was implicated in vasculogenesis, it was decided to investigate the regulation of VEGF-A expression by DNp73 [106]. To this end, the researchers studied mouse embryonic fibroblasts lacking the DNp73 protein. The endogenous expression of VEGF-A in these cells was reduced both at the basal level and under hypoxic conditions. After transfection with various p73 plasmids, analysis of endogenous VEGF-A showed that DNp73β was able to induce VEGF-A expression at the level of RNA promoting tumour vascularisation. In glioblastoma, where DNp73 is overexpressed, DNp73 regulates the expression of ANGPT1/Tie2, enhancing angiogenesis and tumour growth, which, in turn, can be inhibited by the treatment with the selective inhibitor of the TIE2 kinase rebastinib [53].
Another study looked at the role of p73 in the formation of the vascular plexus and angiogenesis [106,107]. This paper demonstrated both in vivo and in vitro that DNp73 affected the migration of endothelial cells and tubulogenesis, regulating the expression of VEGF and TGFβ [106]. Moreover, enhanced tumor vascularisation was observed in xenografts of B16-F10 melanoma cells overexpressing DNp73.
An inspection of 112 colon tumour clinical samples and corresponding normal tissues also showed the positive correlation between p73 and VEGF expression [108]. Noteworthy, the expression of VEGF165b, which is considered to perform the antiangiogenic function, was also found to be upregulated by different p73 isoforms. This study also revealed the correlation between ΔEx2p73 and PEDF (Pigment Epithelium-Derived Factor), which plays an antiangiogenic role in many cancer types. Another clinical data analysis showed the correlation between the p73 and VEGF expression as well as the tumour vascular density in colorectal carcinoma [109].
Therefore, the role of p73 in cancer angiogenesis is an important direction of further research. Previous studies have shown that p73 can be stabilised by HIF-1α and AMPK, and that both DNp73 and TAp73 upregulate the expression of proangiogenic genes. Yet, at the same time, TAp73 can induce HIF-1α degradation inhibiting angiogenesis (Figure 2). The angiogenic activity of p73 probably depends on the p53 status. The dominant role of p73 in the HIF-1α-mediated induction of angiogenesis has been suggested to explain an intricate relationship between p73 and angiogenesis [110].
3. Activation of Invasion and Metastasis
Cancer metastasis is a multistep process of invasion, intravasation, dissemination, and extravasation of cancer cells from the primary tumour site followed by the growth at a new location [111]. Metastasis is the leading cause of death among cancer patients. Considering that expression of the pro-oncogenic p73 isoforms often correlates with overall patient survival [55,112,113,114,115], it is possible that p73 also plays a role in metastasis. One of the first steps associated with cancer invasion is the epithelial-to-mesenchymal transition (EMT). During this process, the proteins responsible for tight cell contacts in epithelial tissue are downregulated (E-Cadherin) and substituted for mesenchymal markers, including N-Cadherin, vimentin, and SM-actin. At the same time, the levels of several metal-dependent proteases are augmented to mediate remodelling of the extracellular matrix (ECM). This step is crucial for escaping tumour cells from the site of a primary tumour and invading the adjacent tissues. The key regulators of EMT genes are transcription factors Slug, Snail, Twist, and Zeb1. Surprisingly, the role of p73 in this process is poorly investigated and likely depends on the cancer type (Figure 3).
Figure 3.
The p73-regulated signalling pathways influence EMT, mobility, or invasiveness in cancer models. In blue shown is the EMT repressive and in red—the EMT-promoting signalling. TAp73 inhibits EMT, mobility, and invasion for breast [116], colorectal [89,120,126] or pancreatic cancers [121,122]. However, the induction of DNp73 inhibits EMT and metastasis in melanoma [127,128]. In glioblastoma, total p73 depletion induces an invasive phenotype in the POSTN-dependent manner [135].
In the three-dimensional model of the MCF10A breast cell line, p73 knockdown led to EMT, which was exemplified by downregulation of E-cadherin and concomitant upregulation of EMT transcription factors [116]. In addition, TAp73 depletion resulted in the disruption of normal cell polarity in spheroids, which is critical for the initiation of EMT [116,117,118]. Moreover, using three-dimensional cultures of Madin-Darby canine kidney (MDCK) cells, TAp73, p21, and PUMA were shown to play a critical role in cyst formation while TAp73 knockdown led to EMT by decreasing E-cadherin and increasing Snail and Twist [119].
Consistent with the repressive role of TAp73 in EMT, TAp73 depletion was shown to increase cell migration of colorectal cancer HCT116 and lung carcinoma H1299 cells [120]. Mechanistically, downregulation of the HDAC1-HSP90 signalling promoted the proteasomal degradation of TAp73 [120]. Among the p73 targets is the NAV3 gene, which encodes a microtubule-binding protein that plays a crucial role in the p73-mediated inhibition of cell migration [89]. The EMT markers and metalloproteinases MMP2 and MM9 were also induced by depletion of either NAV3 or p73 [89].
In pancreatic cancer, the gain-of-function mutant p53 induces the PDGFRb expression causing cell invasion in vitro and formation of metastasis in vivo. This happens likely via dissociation of the p73/NF-Y complex [121]. Conversely, the PDGFRb expression is inhibited in the p53-deficient non-invasive cells. Thus, TAp73a inhibits invasion of the pancreatic cancer cells via the protein-protein interaction with NF-Y [121]. Similarly, the TAp73 loss in the murine model of pancreatic ductal adenocarcinoma was associated with EMT induction and shorter survival [122]. Remarkably, EMT induction was mediated by depletion of the secreted protein biglycan (BGN), a TGFb inhibitor. In turn, BGN was induced by TGFb, suggesting a negative feedback loop between them [123]. Moreover, TGFb promoted Treg function and immunosuppression in pancreatic cancer [124].
In the FaDu pharynx squamous cell carcinoma cells and the corresponding xenograft model, the Abrus agglutinin (AGG) treatment induced p73 and suppressed Snail and EMT [125]. Intriguingly, p73 was shown to interact with Snail upon EGF treatment, while AGG inhibited this interaction. This caused cytoplasmic translocation of Snail and its subsequent proteasomal degradation repressing EGF-induced EMT [125].
Ras-dependent activation of phosphatidylinositol-3 kinase (PI3K) signalling was shown to promote a switch from the TA- to DN-p73 isoforms facilitating the anchorage-independent growth of transformed fibroblasts. In line with this, the ectopic expression of either H-RasV12WT, or H-RasV12Y40C repressed TAp73 via the PI3K activation in the HCT116 colon cancer cells [126].
Recently, in melanoma, DNp73 was shown to downregulate EPLIN (Epithelial protein lost in neoplasm), leading to the activation of the IGF1R-AKT/STAT3 pathway, depletion of E-cadherin, induction of Slug, invasion and metastasis [127].
The same group reported a correlation between high levels of DNp73 and aggressiveness of melanoma with hypopigmentation [128]. Mechanistically, DNp73 activates the IGF1R/PI3K/AKT pathway leading to proteasomal degradation of tyrosinase (a key enzyme in the melanin synthesis), induction of Slug, and EMT. These EMT events correlated with higher invasion allowing for stratifying the patients according to their hypopigmentation status [128].
The p73 protein is known to regulate the genes responsible for metastasis, but the direct association is not always established. For example, HMGB1, a putative p73 target that can regulate p73-mediated transactivation [129,130], is associated with EMT, metastasis, and poor prognosis in breast, lung, and other cancer types [55,131,132,133].
In contrast to the role of p73 as a repressor of EMT, in several cancer cell lines p73 was shown to promote expression of the Integrin-β4 gene, which protein product enhances EMT [134]. Further, overexpression of the direct p73 target, POSTN, that encodes the integrin-binding protein restores the invasion ability of glioblastoma cells after p73 depletion [135].
Therefore, the role of p73 in the regulation of EMT and invasion is cancer type-specific. While p73 inhibits EMT and invasion of pancreatic [121,122], colon [89], breast, lung [116,120], and oral carcinoma cells [125], it can also promote invasion of glioblastoma cell lines [135] (Figure 3). In addition, DNp73 induces invasion of hypopigmented melanoma cells [127,128].
4. Tumour-Promoting Inflammation and Evading Immune Destruction
Tumour microenvironment is determined by crosstalk between different signalling pathways taking place in cancer cells, immune cells, and other cancer-associated cells such as fibroblasts [96,136,137,138,139,140,141,142,143].
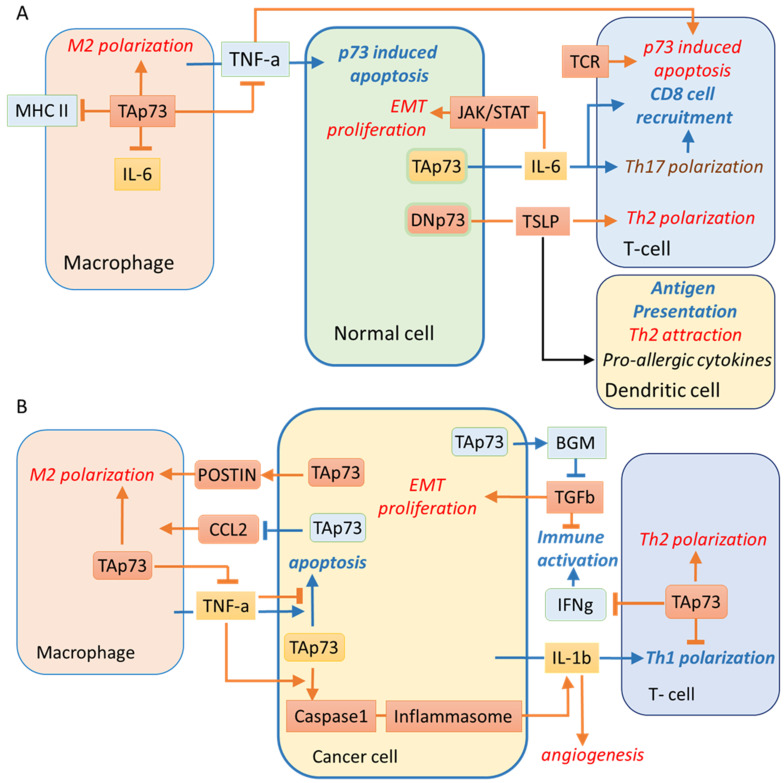
Evidence for the role of p63/p73 in the immune regulation by “non-immune“ cells first came from the study of the autoimmune disease palmoplantar pustulosis. The elevated levels of p63 and p73 proteins were shown to contribute to the enhanced IL-6 production by the reticular crypt epithelial cells that surround lymphoid follicles [144]. The IL-6 mediated activation of the JAK/STAT3 pathway is pro-tumorigenic and also facilitates Th17 T cell differentiation. The latter, in combination with TGFb signaling, can be pro- or anti-carcinogenic by promoting the immune response via the recruitment of CD8 T cells [145]. Both p63 and p73 were demonstrated to activate the IL-6 promoter using overexpression experiments and reporter plasmids. However, functional experiments using p73 depletion were not performed in this study [144].
In light of the role of p73 in the regulation of the immune response, it should be noted that in glioblastomas, p73 regulates POSTN expression [135] which in turn promotes M2 macrophage polarisation and tumour growth [146,147].
The inflammasome is a protein complex that functions as a sensor of pathogen infections [148]. The aberrant inflammasome activation can promote skin and breast cancer but repress colon cancer [149]. The inflammasome signals to the innate immune cells by caspase-1-mediated cleavage and secretion of the IL-1β. Exogenous expression of TAp73b has been recently shown to upregulate the IL-1β expression both at the mRNA and protein levels in H1299 cells [150].
Another report described the role of p73 in atopic dermatitis, a long-term skin inflammation [151]. The DNp73/TAp73 ratio was reported to be increased in the hyperplastic keratinocytes. Paradoxically, this led to enhanced production of the thymic stromal lymphopoietin protein (TSLP), a cytokine that causes Th2 cells-mediated allergic inflammation and also induces the antigen presentation by Langerhans cells [152,153]. In addition, TSLP activation was mediated by exogenous expression of DNp73, concomitantly with an increase of NF-kB, a known p63/p73 coregulator [151,154,155] (Figure 4A). Activation of TSLP signalling promoted the Th2 immune response in breast [92] and pancreatic [156] cancers and was associated with poor prognosis [157].
Figure 4.
The p73-regulated signalling in normal, cancer, and immune cells. TAp73 in cancer cells and immune cells promotes the immunosuppressive cancer environment. In blue shown is cancer-repressing and in red—cancer-promoting signalling, respectively. Arrows represent the positive association, and pointers with blocks are negative associations with green and red anti- and pro-cancerous signalling, respectively. Yellow boxes represent dual signalling molecules with pro- and anticancerous properties. (A) In the normal cells, p73 promotes the IL6 production [144], which can have either pro- [187,188], or anti- cancerogenic effects by inducing Th17 v.s. Treg polarization [189,190]. In skin tissues, p73 regulates TSLR [151] that induces Th2 cell differentiation, thereby promoting chronic inflammation in atopic dermatitis and is associated with poor prognosis in several cancers [157]. (B) In breast cancer, TAp73 represses CCL2 secretion and pro-cancerogenic macrophage recruitment [97]. In contrast, TSLR induces p73 targets VEGF, TSLR, IL-1b, and IL-6 hence promoting breast cancer angiogenesis. In turn, IL1b has a plethora of pro-cancerogenic effects [191]; however, it can also induce the anti-cancerogenic Th1 polarisation [192] and is regulated by the p73/caspase1/inflammasome axis [150,193]. p73-mediated caspase-1 expression is induced by TNFa that also induces a pro-cancerogenic program in SSC [63] but apoptosis in endothelial cells, respectively [165,194,195,196]. The TAp73-induced expression of BGN inhibits the TGFb pro-oncogenic signalling [122]. In contrast, the p73-mediated Warburg effect [197] promotes acidosis, enhanced invasiveness [198], and M2 macrophage polarisation [93]. In turn, the p73 signalling in macrophages promotes M2 polarisation and represses TNF-a production, also promoting phagocytosis and lowering the MHC2 expression [159]. Noticeably, TNFa- or strong TCR-binding-induced apoptosis in T-cells was dependent on p73, but not p53 [163,199]. Moreover, in T-cells, TAp73 and DNp73 repress Th1 polarisation and IFNg production, promoting the immunosuppressive environment [171].
In breast cancer, TSLP induced the anti-apoptotic factors Bcl-2 and Bcl-xL [130] as well as several p73 transcriptional targets related to inflammation, including VEGF, TSLP, IL-1β, and IL-6. These genes were downregulated by the Bcl-2 inhibitor ABT-737 in the activated human mast cell line [158]. Therefore, it is possible that p73 plays a regulatory role in production of these cytokines in immune cells. Further investigations are required to validate this hypothesis.
Another cytokine controlled by p73 is the tumor necrosis factor-alpha (TNFa), which is produced by macrophages [159]. p73 repressed TNFa-induced apoptosis of the immune cells [160,161,162], thereby promoting the immunosuppressive cancer microenvironment. The TNFa-induced apoptosis is mediated via degradation of Rb, thereby leading to activation of the c-Abl/p73 cascade. This mechanism is executed in various cancer cell lines including colorectal carcinoma cells, mice fibroblasts, and thymocytes [163]. In contrast, in the p53 null squamous cell carcinoma cells, TNF-α promoted c-REL nuclear translocation, dissociation of TAp73 from DNp63α, and nuclear export of TAp73 to the cytoplasm [61]. As a result, TNF-α modulates a genome-wide redistribution of the DNp63α/TAp73 and DNp63α/c-REL complexes from the TP53 to AP-1 DNA binding sites to induce an oncogenic gene expression program in squamous cancer cells [63].
As mentioned above, accumulating evidence suggests that TNFa typically promotes apoptosis in normal cells by activating p73. For example, p73 promotes apoptosis induced by the TNFa/IL-1 in the KRT15+ epithelial stem cells [164]. In turn, specific p73 isoforms can also regulate TNFa-induced apoptosis of endothelial cells [165]. The authors demonstrated that TNFa specifically induced the pro-apoptotic TAp73a but at the same time repressed the anti-apoptotic DNp73 form [165]. The p73 −/− mice were used to evaluate the effect of p73 on the TNFa-induced apoptosis [163,164]. p73 −/− mice exhibit a dysregulated immune system and develop chronic inflammation in the epithelial organs, including rhinitis, otitis, periorbital edema, and conjunctivitis [166]. The p73 −/− mice also demonstrated the disrupted development of retinal vasculature. Experiments on cell cultures showed that the absence of p73 affected the production of angiogenic factors to promote the tumour suppressive microenvironment [88,106,141,167,168]. Thus, p73 isoforms regulate apoptosis and differentiation of the innate and adaptive immune cells thereby determining the tumour microenvironment [159,169,170,171,172].
TAp73 depletion in breast cancer cells was associated with their more aggressive growth when xenografted into mice [97]. Mechanistically, this effect was attributed to the TAp73-dependent repression of secretion of chemoattractant Ccl2. This event led to the recruitment of CD204+ and CD206+ pro-carcinogenic macrophages [97].
Collectively, p73 likely affects the tumour microenvironment by regulating the expression of cytokines. However, to unravel the exact effect of p73 on the tumour microenvironment, a comprehensive cytokine profiling of cells with different statuses of p73 is required.
The major factor responsible for tumour promoting inflammation is macrophage polarisation [173,174]. In the course of studying the inflammatory response after lipopolysaccharide (LPS) challenge, it was found that the lack of TAp73 in macrophages prolonged the M1-type macrophage polarisation. These results were obtained using the TAp73 knockout mice and wild-type mice, where endogenous macrophages were substituted by the TAp73-/- ones [159]. In vitro, TAp73-/- macrophages produced more pro-inflammatory cytokines such as TNFa, IL-6 and macrophage inflammatory protein-2. In addition, TAp73-/- macrophages displayed a decreased phagocytosis and increased major histocompatibility complex class II expression. Thus, the lack of p73 prolonged the survival of pro-inflammatory macrophages [159]. These results predict that in tumour-associated macrophages, TAp73 will likely promote M2 polarisation and immunosuppressive tumour microenvironment (Figure 4B).
In adaptive immunity, CD4+ Th1 cells can reprogram M2-like peritoneal exudate cells into the M1 phenotype upon the MHCII-specific interaction. This event enhances an accumulation of M1-polarised tumour-associated macrophages [170]. Th1/Th2 polarization contributes to the immunosuppression environment and progression in gliomas [175,176], hepatocellular carcinoma [177] melanoma [178], and breast cancer [179,180]. Both TA- and DN-isoforms of p73 have been recently shown to negatively affect Th1 differentiation of the naive splenic CD4 T-cells and repress the expression of the IFNg gene [171]. Thereby, it is reasonable to speculate that in the tumour microenvironment, p73 expression in the CD4 T-cells suppresses Th1 polarisation and promotes Th2 polarisation, M2-like macrophages, and immunosuppressive tumour microenvironment.
The same stimuli that activate p53 are likely to activate p73 as well [181]. If true, then p73 should induce the T-cell death and attenuate their well-documented antitumour effects in nearly all cancer types [182,183,184]. Noteworthy, TNFa-induced T-cell apoptosis was dependent on the p73, but not p53 [163]. Importantly, in the cycling peripheral T cells, apoptosis induced by binding of the T-cell receptor (TCR) was independent of p53 but depended on TAp73 [163]. Upon TCR activation, T cell survival was regulated by the MDM2-mediated p73 repression [185]. Inhibiting the MDM2-p73 interaction activated the p73-driven expression of the proapoptotic gene Bim and subsequent apoptosis [185]. Therefore, developing therapeutic strategies that would selectively activate p53 but not p73, would help induce cell death in tumour cells, sparing the T cells from elimination and contributing to the overall anticancer immune response [186].
5. Conclusions
The p53 protein exerts a crucial inhibitory role in cancer development [200,201,202,203,204]. p73 is involved in tissue morphogenesis [205,206] and is rarely mutated in tumours; however, specific isoforms are overexpressed in lung, brain, breast, and other cancer types [207,208]. Here, we reviewed the influence of p73 on the relations between cancer cells and the immune system from the point of view of cancer hallmarks. While the DNA damage response and genomic stability, ability to sustain proliferation, and metabolic control are extensively studied, relatively little is known about the impact of p73 on the ability of cancers to metastasise and the role of p73 in the forming immunosuppressive tumour microenvironment (Table 1).
Table 1.
The cancer hallmarks and p73 functions in specific cancers. The table structure: The rightmost column represents the Tp73 expression in tumour tissue (Tp73Tum) in comparison with the normal tissue (Tp73Norm) as a ratio: log2(Tp73Tum + 1)/log2(Tp73Norm + 1) [209].
| Cancer | Invasion and Metastasis | Angiogenesis | Inflammation | Role of p73 Isoforms in Cancer | Relative tp73 Expression in Cancer Tissue |
|---|---|---|---|---|---|
| Non-small cell lung carcinoma (NSCLC) | [134] | [150] | [210] | [211] | |
| Lung adenocarcinomas | [103] | [193] | [99,212] | 2, 95 | |
| Hepatocellular carcinoma (HCC) | |||||
| Cervix carcinoma | [126] | [213,214,215] | 15, 2 | ||
| Melanoma | [126,128] | ||||
| Osteosarcoma | [99,100,101] | 5, 4 | |||
| Glioblastoma | [126,135] | [135] | [216] | 5, 2 | |
| Medulloblastoma | [217] | --- | |||
| B-cell lymphoma | [88] | [218] | 33, 6 | ||
| Breast cancer | [116] | [88,100] | [150] | [219] | 1, 2 |
| Colorectal cancer | [89] | [88,100,108,109] | [163] | [55,220] | 9, 6 |
| Esophageal adenocarcinoma | [125] | [221] | 1, 1 | ||
| Thyroid cancer | |||||
| Ovarian cancer | [102] | [222] | 4, 1 | ||
| Pancreatic cancer | [121] | [156] | [223,224] | 3, 15 | |
| Neuroblastoma | [135] | ||||
| Squamous carcinoma | [61,63] | [225,226] | 1, 26 |
An analysis of the most recent research reveals that while repressing the epithelial-mesenchymal transition and metastasis in some cancers, the p73 transcriptional activity can promote cancer growth via several mechanisms. For example, p73 directly enhances the Warburg effect stimulating glycolysis in cancer cells. Furthermore, p73 modulates the secretomes of cancer and immune cells to promote the tumour microenvironment. The latter subsequently affects polarisation of immune cells towards the tumorigenic phenotype, culminating in the induction of angiogenesis. Thus, p73 plays a dual role in acting as a tumour suppressor by regulating apoptosis in response to genotoxic stress and as a pro-oncogene by promoting immunosuppressive environment and immune cell differentiation. The experimental evidence reviewed in this study favours the hypothesis that at the advanced stages of cancer development, tumour cells may employ p73 to repress the immune system surveillance explaining why p73 is rarely mutated. This possibility should be taken into account when developing new anti-cancer therapeutic strategies.
Acknowledgments
Authors would like to thank Nickolay Pestov for discussion.
Author Contributions
Conceptualisation, J.M.R., I.B. and A.K.; resources, G.M., N.A.B., A.K. and V.K.; data curation, J.M.R.; writing—original draft preparation J.M.R., A.K., I.Z., D.L., A.B., L.A., A.R. and A.D.; writing—review and editing, J.M.R., I.B., N.A.B. and A.K.; visualisation, J.M.R., S.Z. and A.D.; funding acquisition, G.M., N.A.B. and A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Ministry of Science and Higher Education of the Russian Federation within the framework of state support for the creation and development of World-Class Research Centers “Digital biodesign and personalised healthcare” No. 75-15-2020-913.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to the absence of animal or human research.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Levine A.J., Tomasini R., McKeon F.D., Mak T.W., Melino G. The p53 family: Guardians of maternal reproduction. Nat. Rev. Mol. Cell Biol. 2011;12:259–265. doi: 10.1038/nrm3086. [DOI] [PubMed] [Google Scholar]
- 2.Bernassola F., Federici M., Corazzari M., Terrinoni A., Hribal M.L., De Laurenzi V., Ranalli M., Massa O., Sesti G., McLean W.H.I., et al. Role of transglutaminase 2 in glucose tolerance: Knockout mice studies and a putative mutation in a MODY patient. FASEB J. 2002;16:1371–1378. doi: 10.1096/fj.01-0689com. [DOI] [PubMed] [Google Scholar]
- 3.Bellomaria A., Barbato G., Melino G., Paci M., Melino S. Recognition of p63 by the E3 ligase ITCH: Effect of an ectodermal dysplasia mutant. Cell Cycle. 2010;9:3730–3739. doi: 10.4161/cc.9.18.12933. [DOI] [PubMed] [Google Scholar]
- 4.Candi E., Cipollone R., Rivetti di Val Cervo P., Gonfloni S., Melino G., Knight R. p63 in epithelial development. Cell Mol. Life Sci. 2008;65:3126–3133. doi: 10.1007/s00018-008-8119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Candi E., Terrinoni A., Rufini A., Chikh A., Lena A.M., Suzuki Y., Sayan B.S., Knight R.A., Melino G. p63 is upstream of IKK alpha in epidermal development. J. Cell Sci. 2006;119:4617–4622. doi: 10.1242/jcs.03265. [DOI] [PubMed] [Google Scholar]
- 6.Shalom-Feuerstein R., Lena A.M., Zhou H., De La Forest Divonne S., Van Bokhoven H., Candi E., Melino G., Aberdam D. ΔNp63 is an ectodermal gatekeeper of epidermal morphogenesis. Cell Death Differ. 2011;18:887–896. doi: 10.1038/cdd.2010.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guilluy C., Rolli-Derkinderen M., Tharaux P.-L., Melino G., Pacaud P., Loirand G. Transglutaminase-dependent RhoA activation and depletion by serotonin in vascular smooth muscle cells. J. Biol. Chem. 2007;282:2918–2928. doi: 10.1074/jbc.M604195200. [DOI] [PubMed] [Google Scholar]
- 8.Jones R.A., Kotsakis P., Johnson T.S., Chau D.Y.S., Ali S., Melino G., Griffin M. Matrix changes induced by transglutaminase 2 lead to inhibition of angiogenesis and tumor growth. Cell Death Differ. 2006;13:1442–1453. doi: 10.1038/sj.cdd.4401816. [DOI] [PubMed] [Google Scholar]
- 9.Piredda L., Farrace M.G., Lo Bello M., Malorni W., Melino G., Petruzzelli R., Piacentini M. Identification of “tissue” transglutaminase binding proteins in neural cells committed to apoptosis. FASEB J. 1999;13:355–364. doi: 10.1096/fasebj.13.2.355. [DOI] [PubMed] [Google Scholar]
- 10.Popov Y., Sverdlov D.Y., Sharma A.K., Bhaskar K.R., Li S., Freitag T.L., Lee J., Dieterich W., Melino G., Schuppan D. Tissue transglutaminase does not affect fibrotic matrix stability or regression of liver fibrosis in mice. Gastroenterology. 2011;140:1642–1652. doi: 10.1053/j.gastro.2011.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shweke N., Boulos N., Jouanneau C., Vandermeersch S., Melino G., Dussaule J.-C., Chatziantoniou C., Ronco P., Boffa J.-J. Tissue transglutaminase contributes to interstitial renal fibrosis by favoring accumulation of fibrillar collagen through TGF-beta activation and cell infiltration. Am. J. Pathol. 2008;173:631–642. doi: 10.2353/ajpath.2008.080025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Candi E., Oddi S., Terrinoni A., Paradisi A., Ranalli M., Finazzi-Agró A., Melino G. Transglutaminase 5 cross-links loricrin, involucrin, and small proline-rich proteins in vitro. J. Biol. Chem. 2001;276:35014–35023. doi: 10.1074/jbc.M010157200. [DOI] [PubMed] [Google Scholar]
- 13.Cassidy A.J., van Steensel M.A.M., Steijlen P.M., van Geel M., van der Velden J., Morley S.M., Terrinoni A., Melino G., Candi E., McLean W.H.I. A homozygous missense mutation in TGM5 abolishes epidermal transglutaminase 5 activity and causes acral peeling skin syndrome. Am. J. Hum. Genet. 2005;77:909–917. doi: 10.1086/497707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ikawa S., Nakagawara A., Ikawa Y. p53 family genes: Structural comparison, expression and mutation. Cell Death Differ. 1999;6:1154–1161. doi: 10.1038/sj.cdd.4400631. [DOI] [PubMed] [Google Scholar]
- 15.Alonso M.E., Bello M.J., Lomas J., Gonzalez-Gomez P., Arjona D., De Campos J.M., Gutierrez M., Isla A., Vaquero J., Rey J.A. Absence of mutation of the p73 gene in astrocytic neoplasms. Int. J. Oncol. 2001;19:609–612. doi: 10.3892/ijo.19.3.609. [DOI] [PubMed] [Google Scholar]
- 16.Zaika A.I., Kovalev S., Marchenko N.D., Moll U.M. Overexpression of the wild type p73 gene in breast cancer tissues and cell lines. Cancer Res. 1999;59:3257–3263. [PubMed] [Google Scholar]
- 17.Yokozaki H., Shitara Y., Fujimoto J., Hiyama T., Yasui W., Tahara E. Alterations of p73 preferentially occur in gastric adenocarcinomas with foveolar epithelial phenotype. Int. J. Cancer. 1999;83:192–196. doi: 10.1002/(SICI)1097-0215(19991008)83:2<192::AID-IJC8>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 18.Yasui W., Yokozaki H., Fujimoto J., Naka K., Kuniyasu H., Tahara E. Genetic and epigenetic alterations in multistep carcinogenesis of the stomach. J. Gastroenterol. 2000;35((Suppl. 2)):111–115. [PubMed] [Google Scholar]
- 19.Ganini C., Amelio I., Bertolo R., Bove P., Buonomo O.C., Candi E., Cipriani C., Di Daniele N., Juhl H., Mauriello A., et al. Global mapping of cancers: The Cancer Genome Atlas and beyond. Mol. Oncol. 2021;15:2823–2840. doi: 10.1002/1878-0261.13056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He Y., Fan S., Jiang Y., Xue Z. Expression of ΔNp73 in human NSCLC and clinical implication. Zhongguo Fei Ai Za Zhi. 2006;9:263–266. doi: 10.3779/j.issn.1009-3419.2006.03.11. [DOI] [PubMed] [Google Scholar]
- 21.Dominguez G., Silva J.M., Silva J., Garcia J.M., Sanchez A., Navarro A., Gallego I., Provencio M., España P., Bonilla F. Wild type p73 overexpression and high-grade malignancy in breast cancer. Breast Cancer Res. Treat. 2001;66:183–190. doi: 10.1023/A:1010624717311. [DOI] [PubMed] [Google Scholar]
- 22.Tomkova K., Belkhiri A., El-Rifai W., Zaika A.I. p73 isoforms can induce T-cell factor-dependent transcription in gastrointestinal cells. Cancer Res. 2004;64:6390–6393. doi: 10.1158/0008-5472.CAN-04-2176. [DOI] [PubMed] [Google Scholar]
- 23.Kamiya M., Nakazato Y. The expression of p73, p21 and MDM2 proteins in gliomas. J. Neurooncol. 2002;59:143–149. doi: 10.1023/A:1019633910603. [DOI] [PubMed] [Google Scholar]
- 24.Wager M., Guilhot J., Blanc J.L., Ferrand S., Milin S., Bataille B., Lapierre F., Denis S., Chantereau T., Larsen C.J., et al. Prognostic value of increase in transcript levels of Tp73 DeltaEx2-3 isoforms in low-grade glioma patients. Br. J. Cancer. 2006;95:1062–1069. doi: 10.1038/sj.bjc.6603410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ugur H., Sayan A.E., Ozdamar S.O., Kanpolat Y., Ozturk M. Expression of TAP73 and DeltaNP73 in malignant gliomas. Oncol. Rep. 2004;11:1337–1341. [PubMed] [Google Scholar]
- 26.Inoue K., Fry E.A. Alterations of p63 and p73 in human cancers. Subcell. Biochem. 2014;85:17–40. doi: 10.1007/978-94-017-9211-0_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Engelmann D., Meier C., Alla V., Pützer B.M. A balancing act: Orchestrating amino-truncated and full-length p73 variants as decisive factors in cancer progression. Oncogene. 2015;34:4287–4299. doi: 10.1038/onc.2014.365. [DOI] [PubMed] [Google Scholar]
- 28.Jost C.A., Marin M.C., Kaelin W.G. p73 is a simian [correction of human] p53-related protein that can induce apoptosis. Nature. 1997;389:191–194. doi: 10.1038/38298. [DOI] [PubMed] [Google Scholar]
- 29.Kaghad M., Bonnet H., Yang A., Creancier L., Biscan J.C., Valent A., Minty A., Chalon P., Lelias J.M., Dumont X., et al. Monoallelically expressed gene related to p53 at 1p36, a region frequently deleted in neuroblastoma and other human cancers. Cell. 1997;90:809–819. doi: 10.1016/S0092-8674(00)80540-1. [DOI] [PubMed] [Google Scholar]
- 30.Zeng X., Li X., Miller A., Yuan Z., Yuan W., Kwok R.P., Goodman R., Lu H. The N-terminal domain of p73 interacts with the CH1 domain of p300/CREB binding protein and mediates transcriptional activation and apoptosis. Mol. Cell. Biol. 2000;20:1299–1310. doi: 10.1128/MCB.20.4.1299-1310.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tomasini R., Tsuchihara K., Tsuda C., Lau S.K., Wilhelm M., Rufini A., Tsao M., Iovanna J.L., Jurisicova A., Melino G., et al. TAp73 regulates the spindle assembly checkpoint by modulating BubR1 activity. Proc. Natl. Acad. Sci. USA. 2009;106:797–802. doi: 10.1073/pnas.0812096106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melino G., Knight R.A., Nicotera P. How many ways to die? How many different models of cell death? Cell Death Differ. 2005;12((Suppl. 2)):1457–1462. doi: 10.1038/sj.cdd.4401781. [DOI] [PubMed] [Google Scholar]
- 33.Nepravishta R., Sabelli R., Iorio E., Micheli L., Paci M., Melino S. Oxidative species and S-glutathionyl conjugates in the apoptosis induction by allyl thiosulfate. FEBS J. 2012;279:154–167. doi: 10.1111/j.1742-4658.2011.08407.x. [DOI] [PubMed] [Google Scholar]
- 34.Fazi B., Melino S., De Rubeis S., Bagni C., Paci M., Piacentini M., Di Sano F. Acetylation of RTN-1C regulates the induction of ER stress by the inhibition of HDAC activity in neuroectodermal tumors. Oncogene. 2009;28:3814–3824. doi: 10.1038/onc.2009.233. [DOI] [PubMed] [Google Scholar]
- 35.Sabelli R., Iorio E., De Martino A., Podo F., Ricci A., Viticchiè G., Rotilio G., Paci M., Melino S. Rhodanese-thioredoxin system and allyl sulfur compounds. FEBS J. 2008;275:3884–3899. doi: 10.1111/j.1742-4658.2008.06535.x. [DOI] [PubMed] [Google Scholar]
- 36.Rufini A., Niklison-Chirou M.V., Inoue S., Tomasini R., Harris I.S., Marino A., Federici M., Dinsdale D., Knight R.A., Melino G., et al. TAp73 depletion accelerates aging through metabolic dysregulation. Genes Dev. 2012;26:2009–2014. doi: 10.1101/gad.197640.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ozaki T., Nakagawara A. p73, a sophisticated p53 family member in the cancer world. Cancer Sci. 2005;96:729–737. doi: 10.1111/j.1349-7006.2005.00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tebbi A., Guittet O., Cottet M.-H., Vesin M.-F., Lepoivre M. TAp73 induction by nitric oxide: Regulation by checkpoint kinase 1 (CHK1) and protection against apoptosis. J. Biol. Chem. 2011;286:7873–7884. doi: 10.1074/jbc.M110.184879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vossio S., Palescandolo E., Pediconi N., Moretti F., Balsano C., Levrero M., Costanzo A. DN-p73 is activated after DNA damage in a p53-dependent manner to regulate p53-induced cell cycle arrest. Oncogene. 2002;21:3796–3803. doi: 10.1038/sj.onc.1205465. [DOI] [PubMed] [Google Scholar]
- 40.Liu G., Nozell S., Xiao H., Chen X. DeltaNp73beta is active in transactivation and growth suppression. Mol. Cell. Biol. 2004;24:487–501. doi: 10.1128/MCB.24.2.487-501.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beeler J.S., Marshall C.B., Gonzalez-Ericsson P.I., Shaver T.M., Santos Guasch G.L., Lea S.T., Johnson K.N., Jin H., Venters B.J., Sanders M.E., et al. p73 regulates epidermal wound healing and induced keratinocyte programming. PLoS ONE. 2019;14:e0218458. doi: 10.1371/journal.pone.0218458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sánchez-Carrera D., García-Puga M., Yáñez L., Romón Í., Pipaón C. ∆Np73 is capable of inducing apoptosis by co-ordinately activating several BH3-only proteins. Biosci. Rep. 2015;35:e00198. doi: 10.1042/BSR20150039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nyman U., Vlachos P., Cascante A., Hermanson O., Zhivotovsky B., Joseph B. Protein kinase C-dependent phosphorylation regulates the cell cycle-inhibitory function of the p73 carboxy terminus transactivation domain. Mol. Cell. Biol. 2009;29:1814–1825. doi: 10.1128/MCB.00585-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wildung M., Esser T.U., Grausam K.B., Wiedwald C., Volceanov-Hahn L., Riedel D., Beuermann S., Li L., Zylla J., Guenther A.-K., et al. Transcription factor TAp73 and microRNA-449 complement each other to support multiciliogenesis. Cell Death Differ. 2019;26:2740–2757. doi: 10.1038/s41418-019-0332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grob T.J., Novak U., Maisse C., Barcaroli D., Lüthi A.U., Pirnia F., Hügli B., Graber H.U., De Laurenzi V., Fey M.F., et al. Human delta Np73 regulates a dominant negative feedback loop for TAp73 and p53. Cell Death Differ. 2001;8:1213–1223. doi: 10.1038/sj.cdd.4400962. [DOI] [PubMed] [Google Scholar]
- 46.Nakagawa T., Takahashi M., Ozaki T., Watanabe Ki K., Todo S., Mizuguchi H., Hayakawa T., Nakagawara A. Autoinhibitory regulation of p73 by Delta Np73 to modulate cell survival and death through a p73-specific target element within the Delta Np73 promoter. Mol. Cell. Biol. 2002;22:2575–2585. doi: 10.1128/MCB.22.8.2575-2585.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kartasheva N.N., Contente A., Lenz-Stöppler C., Roth J., Dobbelstein M. p53 induces the expression of its antagonist p73 Delta N, establishing an autoregulatory feedback loop. Oncogene. 2002;21:4715–4727. doi: 10.1038/sj.onc.1205584. [DOI] [PubMed] [Google Scholar]
- 48.Stiewe T., Theseling C.C., Pützer B.M. Transactivation-deficient Delta TA-p73 inhibits p53 by direct competition for DNA binding: Implications for tumorigenesis. J. Biol. Chem. 2002;277:14177–14185. doi: 10.1074/jbc.M200480200. [DOI] [PubMed] [Google Scholar]
- 49.Pozniak C.D., Radinovic S., Yang A., McKeon F., Kaplan D.R., Miller F.D. An anti-apoptotic role for the p53 family member, p73, during developmental neuron death. Science. 2000;289:304–306. doi: 10.1126/science.289.5477.304. [DOI] [PubMed] [Google Scholar]
- 50.Concin N., Becker K., Slade N., Erster S., Mueller-Holzner E., Ulmer H., Daxenbichler G., Zeimet A., Zeillinger R., Marth C., et al. Transdominant DeltaTAp73 isoforms are frequently up-regulated in ovarian cancer. Evidence for their role as epigenetic p53 inhibitors in vivo. Cancer Res. 2004;64:2449–2460. doi: 10.1158/0008-5472.CAN-03-1060. [DOI] [PubMed] [Google Scholar]
- 51.Nakagawa T., Takahashi M., Ozaki T., Watanabe K., Hayashi S., Hosoda M., Todo S., Nakagawara A. Negative autoregulation of p73 and p53 by DeltaNp73 in regulating differentiation and survival of human neuroblastoma cells. Cancer Lett. 2003;197:105–109. doi: 10.1016/S0304-3835(03)00090-9. [DOI] [PubMed] [Google Scholar]
- 52.Oswald C., Stiewe T. In good times and bad: p73 in cancer. Cell Cycle. 2008;7:1726–1731. doi: 10.4161/cc.7.12.6148. [DOI] [PubMed] [Google Scholar]
- 53.Cam M., Charan M., Welker A.M., Dravid P., Studebaker A.W., Leonard J.R., Pierson C.R., Nakano I., Beattie C.E., Hwang E.I., et al. ΔNp73/ETS2 complex drives glioblastoma pathogenesis- targeting downstream mediators by rebastinib prolongs survival in preclinical models of glioblastoma. Neuro. Oncol. 2020;22:345–356. doi: 10.1093/neuonc/noz190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meier C., Hardtstock P., Joost S., Alla V., Pützer B.M. p73 and IGF1R Regulate Emergence of Aggressive Cancer Stem-like Features via miR-885-5p Control. Cancer Res. 2016;76:197–205. doi: 10.1158/0008-5472.CAN-15-1228. [DOI] [PubMed] [Google Scholar]
- 55.Soldevilla B., Díaz R., Silva J., Campos-Martín Y., Muñoz C., García V., García J.M., Peña C., Herrera M., Rodriguez M., et al. Prognostic impact of ΔTAp73 isoform levels and their target genes in colon cancer patients. Clin. Cancer Res. 2011;17:6029–6039. doi: 10.1158/1078-0432.CCR-10-2388. [DOI] [PubMed] [Google Scholar]
- 56.Vikhreva P., Melino G., Amelio I. p73 Alternative Splicing: Exploring a Biological Role for the C-Terminal Isoforms. J. Mol. Biol. 2018;430:1829–1838. doi: 10.1016/j.jmb.2018.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu G., Chen X. The C-terminal sterile alpha motif and the extreme C terminus regulate the transcriptional activity of the alpha isoform of p73. J. Biol. Chem. 2005;280:20111–20119. doi: 10.1074/jbc.M413889200. [DOI] [PubMed] [Google Scholar]
- 58.Oh Y.K., Lee H.J., Jeong M.-H., Rhee M., Mo J.-W., Song E.H., Lim J.-Y., Choi K.-H., Jo I., Park S.I., et al. Role of activating transcription factor 3 on TAp73 stability and apoptosis in paclitaxel-treated cervical cancer cells. Mol. Cancer Res. 2008;6:1232–1249. doi: 10.1158/1541-7786.MCR-07-0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vikhanskaya F., Toh W.H., Dulloo I., Wu Q., Boominathan L., Ng H.H., Vousden K.H., Sabapathy K. p73 supports cellular growth through c-Jun-dependent AP-1 transactivation. Nat. Cell Biol. 2007;9:698–705. doi: 10.1038/ncb1598. [DOI] [PubMed] [Google Scholar]
- 60.Subramanian D., Bunjobpol W., Sabapathy K. Interplay between TAp73 Protein and Selected Activator Protein-1 (AP-1) Family Members Promotes AP-1 Target Gene Activation and Cellular Growth. J. Biol. Chem. 2015;290:18636–18649. doi: 10.1074/jbc.M115.636548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lu H., Yang X., Duggal P., Allen C.T., Yan B., Cohen J., Nottingham L., Romano R.-A., Sinha S., King K.E., et al. TNF-α promotes c-REL/ΔNp63α interaction and TAp73 dissociation from key genes that mediate growth arrest and apoptosis in head and neck cancer. Cancer Res. 2011;71:6867–6877. doi: 10.1158/0008-5472.CAN-11-2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Koeppel M., van Heeringen S.J., Kramer D., Smeenk L., Janssen-Megens E., Hartmann M., Stunnenberg H.G., Lohrum M. Crosstalk between c-Jun and TAp73alpha/beta contributes to the apoptosis-survival balance. Nucleic Acids Res. 2011;39:6069–6085. doi: 10.1093/nar/gkr028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Si H., Lu H., Yang X., Mattox A., Jang M., Bian Y., Sano E., Viadiu H., Yan B., Yau C., et al. TNF-α modulates genome-wide redistribution of ΔNp63α/TAp73 and NF-κB cREL interactive binding on TP53 and AP-1 motifs to promote an oncogenic gene program in squamous cancer. Oncogene. 2016;35:5781–5794. doi: 10.1038/onc.2016.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rozenberg J.M., Rogovaya O.S., Melino G., Barlev N.A., Kagansky A. Distinct p63 and p73 Protein Interactions Predict Specific Functions in mRNA Splicing and Polyploidy Control in Epithelia. Cells. 2020;10:25. doi: 10.3390/cells10010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.De Laurenzi V., Melino G. Evolution of functions within the p53/p63/p73 family. Ann. N. Y. Acad. Sci. 2000;926:90–100. doi: 10.1111/j.1749-6632.2000.tb05602.x. [DOI] [PubMed] [Google Scholar]
- 66.Rozenberg J.M., Zvereva S., Dalina A., Blatov I., Zubarev I., Luppov D., Bessmertnyi A., Romanishin A., Alsoulaiman L., Kumeiko V., et al. The p53 family member p73 in the regulation of cell stress response. Biol. Direct. 2021;16:23. doi: 10.1186/s13062-021-00307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Urist M., Tanaka T., Poyurovsky M.V., Prives C. p73 induction after DNA damage is regulated by checkpoint kinases Chk1 and Chk2. Genes Dev. 2004;18:3041–3054. doi: 10.1101/gad.1221004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gomes S., Raimundo L., Soares J., Loureiro J.B., Leão M., Ramos H., Monteiro M.N., Lemos A., Moreira J., Pinto M., et al. New inhibitor of the TAp73 interaction with MDM2 and mutant p53 with promising antitumor activity against neuroblastoma. Cancer Lett. 2019;446:90–102. doi: 10.1016/j.canlet.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 69.Watson I.R., Blanch A., Lin D.C.C., Ohh M., Irwin M.S. Mdm2-mediated NEDD8 modification of TAp73 regulates its transactivation function. J. Biol. Chem. 2006;281:34096–34103. doi: 10.1074/jbc.M603654200. [DOI] [PubMed] [Google Scholar]
- 70.Nieto A., Hara M.R., Quereda V., Grant W., Saunders V., Xiao K., McDonald P.H., Duckett D.R. βarrestin-1 regulates DNA repair by acting as an E3-ubiquitin ligase adaptor for 53BP1. Cell Death Differ. 2020;27:1200–1213. doi: 10.1038/s41418-019-0406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li X., Guo M., Cai L., Du T., Liu Y., Ding H.-F., Wang H., Zhang J., Chen X., Yan C. Competitive ubiquitination activates the tumor suppressor p53. Cell Death Differ. 2020;27:1807–1818. doi: 10.1038/s41418-019-0463-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rossi M., De Laurenzi V., Munarriz E., Green D.R., Liu Y.-C., Vousden K.H., Cesareni G., Melino G. The ubiquitin-protein ligase Itch regulates p73 stability. EMBO J. 2005;24:836–848. doi: 10.1038/sj.emboj.7600444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Inoue S., Hao Z., Elia A.J., Cescon D., Zhou L., Silvester J., Snow B., Harris I.S., Sasaki M., Li W.Y., et al. Mule/Huwe1/Arf-BP1 suppresses Ras-driven tumorigenesis by preventing c-Myc/Miz1-mediated down-regulation of p21 and p15. Genes Dev. 2013;27:1101–1114. doi: 10.1101/gad.214577.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Di Rita A., Peschiaroli A., Acunzo P.D., Strobbe D., Hu Z., Gruber J., Nygaard M., Lambrughi M., Melino G., Papaleo E., et al. HUWE1 E3 ligase promotes PINK1/PARKIN-independent mitophagy by regulating AMBRA1 activation via IKKα. Nat. Commun. 2018;9:3755. doi: 10.1038/s41467-018-05722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rossi M., Rotblat B., Ansell K., Amelio I., Caraglia M., Misso G., Bernassola F., Cavasotto C.N., Knight R.A., Ciechanover A., et al. High throughput screening for inhibitors of the HECT ubiquitin E3 ligase ITCH identifies antidepressant drugs as regulators of autophagy. Cell Death Dis. 2014;5:e1203. doi: 10.1038/cddis.2014.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chakraborty J., Banerjee S., Ray P., Hossain D.M.S., Bhattacharyya S., Adhikary A., Chattopadhyay S., Das T., Sa G. Gain of cellular adaptation due to prolonged p53 impairment leads to functional switchover from p53 to p73 during DNA damage in acute myeloid leukemia cells. J. Biol. Chem. 2010;285:33104–33112. doi: 10.1074/jbc.M110.122705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Long J.S., Schoonen P.M., Graczyk D., O’Prey J., Ryan K.M. p73 engages A2B receptor signalling to prime cancer cells to chemotherapy-induced death. Oncogene. 2015;34:5152–5162. doi: 10.1038/onc.2014.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kravchenko J.E., Ilyinskaya G.V., Komarov P.G., Agapova L.S., Kochetkov D.V., Strom E., Frolova E.I., Kovriga I., Gudkov A.V., Feinstein E., et al. Small-molecule RETRA suppresses mutant p53-bearing cancer cells through a p73-dependent salvage pathway. Proc. Natl. Acad. Sci. USA. 2008;105:6302–6307. doi: 10.1073/pnas.0802091105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ibrahim N., He L., Leong C.-O., Xing D., Karlan B.Y., Swisher E.M., Rueda B.R., Orsulic S., Ellisen L.W. BRCA1-associated epigenetic regulation of p73 mediates an effector pathway for chemosensitivity in ovarian carcinoma. Cancer Res. 2010;70:7155–7165. doi: 10.1158/0008-5472.CAN-10-0668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gaiddon C., Lokshin M., Ahn J., Zhang T., Prives C. A subset of tumor-derived mutant forms of p53 down-regulate p63 and p73 through a direct interaction with the p53 core domain. Mol. Cell. Biol. 2001;21:1874–1887. doi: 10.1128/MCB.21.5.1874-1887.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Strano S., Munarriz E., Rossi M., Cristofanelli B., Shaul Y., Castagnoli L., Levine A.J., Sacchi A., Cesareni G., Oren M., et al. Physical and functional interaction between p53 mutants and different isoforms of p73. J. Biol. Chem. 2000;275:29503–29512. doi: 10.1074/jbc.M003360200. [DOI] [PubMed] [Google Scholar]
- 82.Wolf E.R., McAtarsney C.P., Bredhold K.E., Kline A.M., Mayo L.D. Mutant and wild-type p53 form complexes with p73 upon phosphorylation by the kinase JNK. Sci. Signal. 2018;11:524. doi: 10.1126/scisignal.aao4170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gong H., Zhang Y., Jiang K., Ye S., Chen S., Zhang Q., Peng J., Chen J. p73 coordinates with Δ133p53 to promote DNA double-strand break repair. Cell Death Differ. 2018;25:1063–1079. doi: 10.1038/s41418-018-0085-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wilhelm M.T., Rufini A., Wetzel M.K., Tsuchihara K., Inoue S., Tomasini R., Itie-Youten A., Wakeham A., Arsenian-Henriksson M., Melino G., et al. Isoform-specific p73 knockout mice reveal a novel role for delta Np73 in the DNA damage response pathway. Genes Dev. 2010;24:549–560. doi: 10.1101/gad.1873910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Vikhanskaya F., D’Incalci M., Broggini M. p73 competes with p53 and attenuates its response in a human ovarian cancer cell line. Nucleic Acids Res. 2000;28:513–519. doi: 10.1093/nar/28.2.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 87.Marin M.C., Marques M.M. Novel role of p73 as a regulator of developmental angiogenesis: Implication for cancer therapy. Mol. Cell. Oncol. 2016;3:e1019973. doi: 10.1080/23723556.2015.1019973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Stantic M., Sakil H.A.M., Zirath H., Fang T., Sanz G., Fernandez-Woodbridge A., Marin A., Susanto E., Mak T.W., Arsenian Henriksson M., et al. TAp73 suppresses tumor angiogenesis through repression of proangiogenic cytokines and HIF-1α activity. Proc. Natl. Acad. Sci. USA. 2015;112:220–225. doi: 10.1073/pnas.1421697112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Uboveja A., Satija Y.K., Siraj F., Sharma I., Saluja D. p73 NAV3 axis plays a critical role in suppression of colon cancer metastasis. Oncogenesis. 2020;9:12. doi: 10.1038/s41389-020-0193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cui X.-P., Wang C.-X., Wang Z.-Y., Li J., Tan Y.-W., Gu S.-T., Qin C.-K. LncRNA TP73-AS1 sponges miR-141-3p to promote the migration and invasion of pancreatic cancer cells through the up-regulation of BDH2. Biosci. Rep. 2019;39:BSR20181937. doi: 10.1042/BSR20181937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bae W.-K., Hong C.-S., Park M.-R., Sun E.-G., Lee J.-H., Kang K., Ryu K.-H., Shim H.-J., Hwang J.-E., Cho S.-H., et al. TAp73 inhibits cell invasion and migration by directly activating KAI1 expression in colorectal carcinoma. Cancer Lett. 2018;415:106–116. doi: 10.1016/j.canlet.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 92.Kuan E.L., Ziegler S.F. A tumor-myeloid cell axis, mediated via the cytokines IL-1α and TSLP, promotes the progression of breast cancer. Nat. Immunol. 2018;19:366–374. doi: 10.1038/s41590-018-0066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen J., Cao X., Li B., Zhao Z., Chen S., Lai S.W.T., Muend S.A., Nossa G.K., Wang L., Guo W., et al. Warburg effect is a cancer immune evasion mechanism against macrophage immunosurveillance. Front. Immunol. 2020;11:621757. doi: 10.3389/fimmu.2020.621757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chang A.L., Miska J., Wainwright D.A., Dey M., Rivetta C.V., Yu D., Kanojia D., Pituch K.C., Qiao J., Pytel P., et al. CCL2 Produced by the Glioma Microenvironment Is Essential for the Recruitment of Regulatory T Cells and Myeloid-Derived Suppressor Cells. Cancer Res. 2016;76:5671–5682. doi: 10.1158/0008-5472.CAN-16-0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fortunato O., Belisario D.C., Compagno M., Giovinazzo F., Bracci C., Pastorino U., Horenstein A., Malavasi F., Ferracini R., Scala S., et al. CXCR4 inhibition counteracts immunosuppressive properties of metastatic NSCLC stem cells. Front. Immunol. 2020;11:02168. doi: 10.3389/fimmu.2020.02168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li L., Yu R., Cai T., Chen Z., Lan M., Zou T., Wang B., Wang Q., Zhao Y., Cai Y. Effects of immune cells and cytokines on inflammation and immunosuppression in the tumor microenvironment. Int. Immunopharmacol. 2020;88:106939. doi: 10.1016/j.intimp.2020.106939. [DOI] [PubMed] [Google Scholar]
- 97.Wolfsberger J., Sakil H.A.M., Zhou L., van Bree N., Baldisseri E., de Souza Ferreira S., Zubillaga V., Stantic M., Fritz N., Hartman J., et al. TAp73 represses NF-κB-mediated recruitment of tumor-associated macrophages in breast cancer. Proc. Natl. Acad. Sci. USA. 2021;118:10. doi: 10.1073/pnas.2017089118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vitali A., Botta B., Delle Monache G., Zappitelli S., Ricciardi P., Melino S., Petruzzelli R., Giardina B. Purification and partial characterization of a peroxidase from plant cell cultures of Cassia didymobotrya and biotransformation studies. Biochem. J. 1998;331:513–519. doi: 10.1042/bj3310513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Amelio I., Inoue S., Markert E.K., Levine A.J., Knight R.A., Mak T.W., Melino G. TAp73 opposes tumor angiogenesis by promoting hypoxia-inducible factor 1α degradation. Proc. Natl. Acad. Sci. USA. 2015;112:226–231. doi: 10.1073/pnas.1410609111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dulloo I., Phang B.H., Othman R., Tan S.Y., Vijayaraghavan A., Goh L.K., Martin-Lopez M., Marques M.M., Li C.W., Wang D.Y., et al. Hypoxia-inducible TAp73 supports tumorigenesis by regulating the angiogenic transcriptome. Nat. Cell Biol. 2015;17:511–523. doi: 10.1038/ncb3130. [DOI] [PubMed] [Google Scholar]
- 101.Salimath B., Marmé D., Finkenzeller G. Expression of the vascular endothelial growth factor gene is inhibited by p73. Oncogene. 2000;19:3470–3476. doi: 10.1038/sj.onc.1203672. [DOI] [PubMed] [Google Scholar]
- 102.Vikhanskaya F., Bani M.R., Borsotti P., Ghilardi C., Ceruti R., Ghisleni G., Marabese M., Giavazzi R., Broggini M., Taraboletti G. p73 Overexpression increases VEGF and reduces thrombospondin-1 production: Implications for tumor angiogenesis. Oncogene. 2001;20:7293–7300. doi: 10.1038/sj.onc.1204896. [DOI] [PubMed] [Google Scholar]
- 103.Wu M., Zhang Z., Ma F., Zhang X., Zhang Z., Tang J., Chen P., Zhou C., Wang W. Association between TAp73, p53 and VASH1 expression in lung adenocarcinoma. Oncol. Lett. 2018;15:5175–5180. doi: 10.3892/ol.2018.7912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Li D., Dulloo I., Sabapathy K. Context-dependent AMPK activation distinctly regulates TAp73 stability and transcriptional activity. Signal Transduct. Target. Ther. 2018;3:20. doi: 10.1038/s41392-018-0020-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dulloo I., Hooi P.B., Sabapathy K. Hypoxia-induced DNp73 stabilization regulates Vegf-A expression and tumor angiogenesis similar to TAp73. Cell Cycle. 2015;14:3533–3539. doi: 10.1080/15384101.2015.1078038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fernandez-Alonso R., Martin-Lopez M., Gonzalez-Cano L., Garcia S., Castrillo F., Diez-Prieto I., Fernandez-Corona A., Lorenzo-Marcos M.E., Li X., Claesson-Welsh L., et al. p73 is required for endothelial cell differentiation, migration and the formation of vascular networks regulating VEGF and TGFβ signaling. Cell Death Differ. 2015;22:1287–1299. doi: 10.1038/cdd.2014.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mauretti A., Neri A., Kossover O., Seliktar D., Nardo P.D., Melino S. Design of a Novel Composite H2 S-Releasing Hydrogel for Cardiac Tissue Repair. Macromol. Biosci. 2016;16:847–858. doi: 10.1002/mabi.201500430. [DOI] [PubMed] [Google Scholar]
- 108.Díaz R., Peña C., Silva J., Lorenzo Y., García V., García J.M., Sánchez A., Espinosa P., Yuste R., Bonilla F., et al. p73 Isoforms affect VEGF, VEGF165b and PEDF expression in human colorectal tumors: VEGF165b downregulation as a marker of poor prognosis. Int. J. Cancer. 2008;123:1060–1067. doi: 10.1002/ijc.23619. [DOI] [PubMed] [Google Scholar]
- 109.Guan M., Peng H.-X., Yu B., Lu Y. p73 Overexpression and angiogenesis in human colorectal carcinoma. Jpn. J. Clin. Oncol. 2003;33:215–220. doi: 10.1093/jjco/hyg045. [DOI] [PubMed] [Google Scholar]
- 110.Sabapathy K. p73: A Positive or Negative Regulator of Angiogenesis, or Both? Mol. Cell. Biol. 2015;36:848–854. doi: 10.1128/MCB.00929-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Blomberg O.S., Spagnuolo L., de Visser K.E. Immune regulation of metastasis: Mechanistic insights and therapeutic opportunities. Dis. Model. Mech. 2018;11:dmm036236. doi: 10.1242/dmm.036236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Concin N., Hofstetter G., Berger A., Gehmacher A., Reimer D., Watrowski R., Tong D., Schuster E., Hefler L., Heim K., et al. Clinical relevance of dominant-negative p73 isoforms for responsiveness to chemotherapy and survival in ovarian cancer: Evidence for a crucial p53-p73 cross-talk in vivo. Clin. Cancer Res. 2005;11:8372–8383. doi: 10.1158/1078-0432.CCR-05-0899. [DOI] [PubMed] [Google Scholar]
- 113.Bunch B., Krishnan N., Greenspan R.D., Ramakrishnan S., Attwood K., Yan L., Qi Q., Wang D., Morrison C., Omilian A., et al. TAp73 expression and P1 promoter methylation, a potential marker for chemoresponsiveness to cisplatin therapy and survival in muscle-invasive bladder cancer (MIBC) Cell Cycle. 2019;18:2055–2066. doi: 10.1080/15384101.2019.1638693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cochrane D.R., Campbell K.R., Greening K., Ho G.C., Hopkins J., Bui M., Douglas J.M., Sharlandjieva V., Munzur A.D., Lai D., et al. Single cell transcriptomes of normal endometrial derived organoids uncover novel cell type markers and cryptic differentiation of primary tumours. J. Pathol. 2020;252:201–214. doi: 10.1002/path.5511. [DOI] [PubMed] [Google Scholar]
- 115.Hua B., Li Y., Yang X., Niu X., Zhao Y., Zhu X. MicroRNA-361-3p promotes human breast cancer cell viability by inhibiting the E2F1/P73 signalling pathway. Biomed. Pharmacother. 2020;125:109994. doi: 10.1016/j.biopha.2020.109994. [DOI] [PubMed] [Google Scholar]
- 116.Zhang Y., Yan W., Jung Y.S., Chen X. Mammary epithelial cell polarity is regulated differentially by p73 isoforms via epithelial-to-mesenchymal transition. J. Biol. Chem. 2012;287:17746–17753. doi: 10.1074/jbc.M112.358143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Persa O.-D., Niessen C.M. Epithelial polarity limits EMT. Nat. Cell Biol. 2019;21:299–300. doi: 10.1038/s41556-019-0284-7. [DOI] [PubMed] [Google Scholar]
- 118.Chatterjee S.J., Halaoui R., McCaffrey L. Apical–basal polarity as a sensor for epithelial homeostasis: A matter of life and death. Curr. Pathobiol. Rep. 2016;4:99–106. doi: 10.1007/s40139-016-0107-5. [DOI] [Google Scholar]
- 119.Zhang Y., Young A., Zhang J., Chen X. P73 tumor suppressor and its targets, p21 and PUMA, are required for madin-darby canine kidney cell morphogenesis by maintaining an appropriate level of epithelial to mesenchymal transition. Oncotarget. 2015;6:13994–14004. doi: 10.18632/oncotarget.4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhang J., Xu E., Chen X. TAp73 protein stability is controlled by histone deacetylase 1 via regulation of Hsp90 chaperone function. J. Biol. Chem. 2013;288:7727–7737. doi: 10.1074/jbc.M112.429522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Weissmueller S., Manchado E., Saborowski M., Morris J.P., Wagenblast E., Davis C.A., Moon S.-H., Pfister N.T., Tschaharganeh D.F., Kitzing T., et al. Mutant p53 drives pancreatic cancer metastasis through cell-autonomous PDGF receptor β signaling. Cell. 2014;157:382–394. doi: 10.1016/j.cell.2014.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Thakur A.K., Nigri J., Lac S., Leca J., Bressy C., Berthezene P., Bartholin L., Chan P., Calvo E., Iovanna J.L., et al. TAp73 loss favors Smad-independent TGF-β signaling that drives EMT in pancreatic ductal adenocarcinoma. Cell Death Differ. 2016;23:1358–1370. doi: 10.1038/cdd.2016.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Groth S., Schulze M., Kalthoff H., Fändrich F., Ungefroren H. Adhesion and Rac1-dependent regulation of biglycan gene expression by transforming growth factor-beta. Evidence for oxidative signaling through NADPH oxidase. J. Biol. Chem. 2005;280:33190–33199. doi: 10.1074/jbc.M504249200. [DOI] [PubMed] [Google Scholar]
- 124.Soares K.C., Rucki A.A., Kim V., Foley K., Solt S., Wolfgang C.L., Jaffee E.M., Zheng L. TGF-β blockade depletes T regulatory cells from metastatic pancreatic tumors in a vaccine dependent manner. Oncotarget. 2015;6:43005–43015. doi: 10.18632/oncotarget.5656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sinha N., Meher B.R., Naik P.P., Panda P.K., Mukhapadhyay S., Maiti T.K., Bhutia S.K. p73 induction by Abrus agglutinin facilitates Snail ubiquitination to inhibit epithelial to mesenchymal transition in oral cancer. Phytomedicine. 2019;55:179–190. doi: 10.1016/j.phymed.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 126.Beitzinger M., Hofmann L., Oswald C., Beinoraviciute-Kellner R., Sauer M., Griesmann H., Bretz A.C., Burek C., Rosenwald A., Stiewe T. p73 poses a barrier to malignant transformation by limiting anchorage-independent growth. EMBO J. 2008;27:792–803. doi: 10.1038/emboj.2008.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Steder M., Alla V., Meier C., Spitschak A., Pahnke J., Fürst K., Kowtharapu B.S., Engelmann D., Petigk J., Egberts F., et al. DNp73 exerts function in metastasis initiation by disconnecting the inhibitory role of EPLIN on IGF1R-AKT/STAT3 signaling. Cancer Cell. 2013;24:512–527. doi: 10.1016/j.ccr.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 128.Fürst K., Steder M., Logotheti S., Angerilli A., Spitschak A., Marquardt S., Schumacher T., Engelmann D., Herchenröder O., Rupp R.A.W., et al. DNp73-induced degradation of tyrosinase links depigmentation with EMT-driven melanoma progression. Cancer Lett. 2019;442:299–309. doi: 10.1016/j.canlet.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 129.Stros M., Ozaki T., Bacikova A., Kageyama H., Nakagawara A. HMGB1 and HMGB2 cell-specifically down-regulate the p53- and p73-dependent sequence-specific transactivation from the human Bax gene promoter. J. Biol. Chem. 2002;277:7157–7164. doi: 10.1074/jbc.M110233200. [DOI] [PubMed] [Google Scholar]
- 130.Uramoto H., Izumi H., Nagatani G., Ohmori H., Nagasue N., Ise T., Yoshida T., Yasumoto K., Kohno K. Physical interaction of tumour suppressor p53/p73 with CCAAT-binding transcription factor 2 (CTF2) and differential regulation of human high-mobility group 1 (HMG1) gene expression. Biochem. J. 2003;371:301–310. doi: 10.1042/bj20021646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chen Y., Cai L., Guo X., Li Z., Liao X., Zhang X., Huang L., He J. HMGB1-activated fibroblasts promote breast cancer cells metastasis via RAGE/aerobic glycolysis. Neoplasma. 2020;68:71–78. doi: 10.4149/neo_2020_200610N620. [DOI] [PubMed] [Google Scholar]
- 132.Okui T., Hiasa M., Ryumon S., Ono K., Kunisada Y., Ibaragi S., Sasaki A., Roodman G.D., White F.A., Yoneda T. The HMGB1/RAGE axis induces bone pain associated with colonization of 4T1 mouse breast cancer in bone. J. Bone Oncol. 2021;26:100330. doi: 10.1016/j.jbo.2020.100330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wu X.-J., Chen Y.-Y., Guo W.-W., Li T., Dong H.-B., Wang W., Xie M., Ma G.-L., Pei D.-S. HMGB1 regulates SNAI1 during NSCLC metastasis, both directly, through transcriptional activation, and indirectly, in a RSF1-IT2-dependent manner. Mol. Oncol. 2020;14:1348–1364. doi: 10.1002/1878-0261.12691. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 134.Xie N., Vikhreva P., Annicchiarico-Petruzzelli M., Amelio I., Barlev N., Knight R.A., Melino G. Integrin-β4 is a novel transcriptional target of TAp73. Cell Cycle. 2018;17:589–594. doi: 10.1080/15384101.2017.1403684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Landré V., Antonov A., Knight R., Melino G. p73 promotes glioblastoma cell invasion by directly activating POSTN (periostin) expression. Oncotarget. 2016;7:11785–11802. doi: 10.18632/oncotarget.7600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Amelio I., Melino G. The p53 family and the hypoxia-inducible factors (HIFs): Determinants of cancer progression. Trends Biochem. Sci. 2015;40:425–434. doi: 10.1016/j.tibs.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 137.Petrova V.S., Barlev N.A. Tumor microenvironment regulation by hypoxia-indicible factors (hifs), and p53 family proteins. Tsitologiia. 2017;59:259–270. [PubMed] [Google Scholar]
- 138.Anqi C., Takabatake K., Kawai H., Oo M.W., Yoshida S., Fujii M., Omori H., Sukegawa S., Nakano K., Tsujigiwa H., et al. Differentiation and roles of bone marrow-derived cells on the tumor microenvironment of oral squamous cell carcinoma. Oncol. Lett. 2019;18:6628–6638. doi: 10.3892/ol.2019.11045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhang Y., Lazarus J., Steele N.G., Yan W., Lee H.-J., Nwosu Z.C., Halbrook C.J., Menjivar R.E., Kemp S.B., Sirihorachai V.R., et al. Regulatory T-cell Depletion Alters the Tumor Microenvironment and Accelerates Pancreatic Carcinogenesis. Cancer Discov. 2020;10:422–439. doi: 10.1158/2159-8290.CD-19-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Garufi A., Traversi G., Cirone M., D’Orazi G. HIPK2 role in the tumor-host interaction: Impact on fibroblasts transdifferentiation CAF-like. IUBMB Life. 2019;71:2055–2061. doi: 10.1002/iub.2144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Beyranvand Nejad E., Labrie C., Abdulrahman Z., van Elsas M.J., Rademaker E., Kleinovink J.W., van der Sluis T.C., van Duikeren S., Teunisse A.F.A.S., Jochemsen A.G., et al. Lack of myeloid cell infiltration as an acquired resistance strategy to immunotherapy. J. Immunother. Cancer. 2020;8:2. doi: 10.1136/jitc-2020-001326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Naserian S., Abdelgawad M.E., Afshar Bakshloo M., Ha G., Arouche N., Cohen J.L., Salomon B.L., Uzan G. The TNF/TNFR2 signaling pathway is a key regulatory factor in endothelial progenitor cell immunosuppressive effect. Cell Commun. Signal. 2020;18:94. doi: 10.1186/s12964-020-00564-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Pallucca R., Visconti S., Camoni L., Cesareni G., Melino S., Panni S., Torreri P., Aducci P. Specificity of ε and non-ε isoforms of arabidopsis 14-3-3 proteins towards the H+-ATPase and other targets. PLoS ONE. 2014;9:e90764. doi: 10.1371/journal.pone.0090764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Koshiba S., Ichimiya S., Nagashima T., Tonooka A., Kubo T., Kikuchi T., Himi T., Sato N. Tonsillar crypt epithelium of palmoplantar pustulosis secretes interleukin-6 to support B-cell development via p63/p73 transcription factors. J. Pathol. 2008;214:75–84. doi: 10.1002/path.2266. [DOI] [PubMed] [Google Scholar]
- 145.Chonov D.C., Ignatova M.M.K., Ananiev J.R., Gulubova M.V. IL-6 Activities in the Tumour Microenvironment. Part 1. Open Access Maced. J. Med. Sci. 2019;7:2391–2398. doi: 10.3889/oamjms.2019.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Guo H., Yang S., Xu L., Li D., Tang J., Wang S., Wei B., Liu Z. Association between the p73 gene G4C14-to-A4T14 single nucleotide polymorphism and risk of cervical cancer by high resolution melting and PCR with confronting two-pair primers in a Chinese population. Oncol. Lett. 2016;12:721–726. doi: 10.3892/ol.2016.4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhou X., Hao Q., Zhang Q., Liao J.M., Ke J.W., Liao P., Cao B., Lu H. Ribosomal proteins L11 and L5 activate TAp73 by overcoming MDM2 inhibition. Cell Death Differ. 2015;22:755–766. doi: 10.1038/cdd.2014.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sharma D., Kanneganti T.-D. The cell biology of inflammasomes: Mechanisms of inflammasome activation and regulation. J. Cell Biol. 2016;213:617–629. doi: 10.1083/jcb.201602089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kantono M., Guo B. Inflammasomes and cancer: The dynamic role of the inflammasome in tumor development. Front. Immunol. 2017;8:1132. doi: 10.3389/fimmu.2017.01132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Vikhreva P., Petrova V., Gokbulut T., Pestlikis I., Mancini M., Di Daniele N., Knight R.A., Melino G., Amelio I. TAp73 upregulates IL-1β in cancer cells: Potential biomarker in lung and breast cancer? Biochem. Biophys. Res. Commun. 2017;482:498–505. doi: 10.1016/j.bbrc.2016.10.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kumagai A., Kubo T., Kawata K., Kamekura R., Yamashita K., Jitsukawa S., Nagaya T., Sumikawa Y., Himi T., Yamashita T., et al. Keratinocytes in atopic dermatitis express abundant ΔNp73 regulating thymic stromal lymphopoietin production via NF-κB. J. Dermatol. Sci. 2017;88:175–183. doi: 10.1016/j.jdermsci.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 152.Soumelis V., Reche P.A., Kanzler H., Yuan W., Edward G., Homey B., Gilliet M., Ho S., Antonenko S., Lauerma A., et al. Human epithelial cells trigger dendritic cell mediated allergic inflammation by producing TSLP. Nat. Immunol. 2002;3:673–680. doi: 10.1038/ni805. [DOI] [PubMed] [Google Scholar]
- 153.Ebner S., Nguyen V.A., Forstner M., Wang Y.-H., Wolfram D., Liu Y.-J., Romani N. Thymic stromal lymphopoietin converts human epidermal Langerhans cells into antigen-presenting cells that induce proallergic T cells. J. Allergy Clin. Immunol. 2007;119:982–990. doi: 10.1016/j.jaci.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 154.King K.E., George A.L., Sakakibara N., Mahmood K., Moses M.A., Weinberg W.C. Intersection of the p63 and NF-κB pathways in epithelial homeostasis and disease. Mol. Carcinog. 2019;58:1571–1580. doi: 10.1002/mc.23081. [DOI] [PubMed] [Google Scholar]
- 155.King K.E., Ponnamperuma R.M., Allen C., Lu H., Duggal P., Chen Z., Van Waes C., Weinberg W.C. The p53 homologue DeltaNp63alpha interacts with the nuclear factor-kappaB pathway to modulate epithelial cell growth. Cancer Res. 2008;68:5122–5131. doi: 10.1158/0008-5472.CAN-07-6123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.De Monte L., Reni M., Tassi E., Clavenna D., Papa I., Recalde H., Braga M., Di Carlo V., Doglioni C., Protti M.P. Intratumor T helper type 2 cell infiltrate correlates with cancer-associated fibroblast thymic stromal lymphopoietin production and reduced survival in pancreatic cancer. J. Exp. Med. 2011;208:469–478. doi: 10.1084/jem.20101876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Corren J., Ziegler S.F. TSLP: From allergy to cancer. Nat. Immunol. 2019;20:1603–1609. doi: 10.1038/s41590-019-0524-9. [DOI] [PubMed] [Google Scholar]
- 158.Kim H.-Y., Jeong H.-J., Kim H.-M. Anti-allergic and anti-inflammatory effects of the Bcl-2 inhibitor ABT-737 on experimental allergic rhinitis models. Eur. J. Pharmacol. 2018;833:34–43. doi: 10.1016/j.ejphar.2018.05.044. [DOI] [PubMed] [Google Scholar]
- 159.Tomasini R., Secq V., Pouyet L., Thakur A.K., Wilhelm M., Nigri J., Vasseur S., Berthezene P., Calvo E., Melino G., et al. TAp73 is required for macrophage-mediated innate immunity and the resolution of inflammatory responses. Cell Death Differ. 2013;20:293–301. doi: 10.1038/cdd.2012.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Carswell E.A., Old L.J., Kassel R.L., Green S., Fiore N., Williamson B. An endotoxin-induced serum factor that causes necrosis of tumors. Proc. Natl. Acad. Sci. USA. 1975;72:3666–3670. doi: 10.1073/pnas.72.9.3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Salomon B.L., Leclerc M., Tosello J., Ronin E., Piaggio E., Cohen J.L. Tumor necrosis factor α and regulatory T cells in oncoimmunology. Front. Immunol. 2018;9:444. doi: 10.3389/fimmu.2018.00444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Qu Y., Zhao G., Li H. Forward and Reverse Signaling Mediated by Transmembrane Tumor Necrosis Factor-Alpha and TNF Receptor 2: Potential Roles in an Immunosuppressive Tumor Microenvironment. Front. Immunol. 2017;8:1675. doi: 10.3389/fimmu.2017.01675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chau B.N., Chen T.-T., Wan Y.Y., DeGregori J., Wang J.Y.J. Tumor necrosis factor alpha-induced apoptosis requires p73 and c-ABL activation downstream of RB degradation. Mol. Cell. Biol. 2004;24:4438–4447. doi: 10.1128/MCB.24.10.4438-4447.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zhan Q., Korngold R., Lezcano C., McKeon F., Murphy G.F. Graft-versus-host disease-related cytokine-driven apoptosis depends on p73 in cytokeratin 15-positive target cells. Biol. Blood Marrow Transplant. 2012;18:841–851. doi: 10.1016/j.bbmt.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Rastogi S., Rizwani W., Joshi B., Kunigal S., Chellappan S.P. TNF-α response of vascular endothelial and vascular smooth muscle cells involve differential utilization of ASK1 kinase and p73. Cell Death Differ. 2012;19:274–283. doi: 10.1038/cdd.2011.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Yang A., Walker N., Bronson R., Kaghad M., Oosterwegel M., Bonnin J., Vagner C., Bonnet H., Dikkes P., Sharpe A., et al. p73-deficient mice have neurological, pheromonal and inflammatory defects but lack spontaneous tumours. Nature. 2000;404:99–103. doi: 10.1038/35003607. [DOI] [PubMed] [Google Scholar]
- 167.Strait A.A., Wang X.-J. The role of transforming growth factor-beta in immune suppression and chronic inflammation of squamous cell carcinomas. Mol. Carcinog. 2020;59:745–753. doi: 10.1002/mc.23196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Larson C., Oronsky B., Carter C.A., Oronsky A., Knox S.J., Sher D., Reid T.R. TGF-beta: A master immune regulator. Expert Opin. Ther. Targets. 2020;24:427–438. doi: 10.1080/14728222.2020.1744568. [DOI] [PubMed] [Google Scholar]
- 169.Hu Y., He Y., Srivenugopal K.S., Fan S., Jiang Y. In vitro antitumor cytotoxic T lymphocyte response induced by dendritic cells transduced with DeltaNp73alpha recombinant adenovirus. Oncol. Rep. 2007;18:1085–1091. [PubMed] [Google Scholar]
- 170.Eisel D., Das K., Dickes E., König R., Osen W., Eichmüller S.B. Cognate Interaction With CD4+ T Cells Instructs Tumor-Associated Macrophages to Acquire M1-Like Phenotype. Front. Immunol. 2019;10:219. doi: 10.3389/fimmu.2019.00219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ren M., Kazemian M., Zheng M., He J., Li P., Oh J., Liao W., Li J., Rajaseelan J., Kelsall B.L., et al. Transcription factor p73 regulates Th1 differentiation. Nat. Commun. 2020;11:1475. doi: 10.1038/s41467-020-15172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Senoo M., Manis J.P., Alt F.W., McKeon F. p63 and p73 are not required for the development and p53-dependent apoptosis of T cells. Cancer Cell. 2004;6:85–89. doi: 10.1016/j.ccr.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 173.Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X., Bucci E., Piacentini M., Ippolito G., Melino G. COVID-19 infection: The perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sanchez-Lopez E., Ghia E.M., Antonucci L., Sharma N., Rassenti L.Z., Xu J., Sun B., Kipps T.J., Karin M. NF-κB-p62-NRF2 survival signaling is associated with high ROR1 expression in chronic lymphocytic leukemia. Cell Death Differ. 2020;27:2206–2216. doi: 10.1038/s41418-020-0496-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Takashima Y., Kawaguchi A., Kanayama T., Hayano A., Yamanaka R. Correlation between lower balance of Th2 helper T-cells and expression of PD-L1/PD-1 axis genes enables prognostic prediction in patients with glioblastoma. Oncotarget. 2018;9:19065–19078. doi: 10.18632/oncotarget.24897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wang H., Zhou H., Xu J., Lu Y., Ji X., Yao Y., Chao H., Zhang J., Zhang X., Yao S., et al. Different T-cell subsets in glioblastoma multiforme and targeted immunotherapy. Cancer Lett. 2021;496:134–143. doi: 10.1016/j.canlet.2020.09.028. [DOI] [PubMed] [Google Scholar]
- 177.Lee H.L., Jang J.W., Lee S.W., Yoo S.H., Kwon J.H., Nam S.W., Bae S.H., Choi J.Y., Han N.I., Yoon S.K. Inflammatory cytokines and change of Th1/Th2 balance as prognostic indicators for hepatocellular carcinoma in patients treated with transarterial chemoembolization. Sci. Rep. 2019;9:3260. doi: 10.1038/s41598-019-40078-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Lauerova L., Dusek L., Simickova M., Kocák I., Vagundová M., Zaloudík J., Kovarík J. Malignant melanoma associates with Th1/Th2 imbalance that coincides with disease progression and immunotherapy response. Neoplasma. 2002;49:159–166. [PubMed] [Google Scholar]
- 179.Tokumaru Y., Le L., Oshi M., Katsuta E., Matsuhashi N., Futamura M., Yoshida K., Takabe K. Association of Th2 high tumors with aggressive features of breast cancer. JCO. 2020;38:e12584. doi: 10.1200/JCO.2020.38.15_suppl.e12584. [DOI] [Google Scholar]
- 180.Zhao X., Liu J., Ge S., Chen C., Li S., Wu X., Feng X., Wang Y., Cai D. Saikosaponin A inhibits breast cancer by regulating th1/th2 balance. Front. Pharmacol. 2019;10:624. doi: 10.3389/fphar.2019.00624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Coppari E., Yamada T., Bizzarri A.R., Beattie C.W., Cannistraro S. A nanotechnological, molecular-modeling, and immunological approach to study the interaction of the anti-tumorigenic peptide p28 with the p53 family of proteins. Int. J. Nanomed. 2014;9:1799–1813. doi: 10.2147/IJN.S58465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Biton J., Mansuet-Lupo A., Pécuchet N., Alifano M., Ouakrim H., Arrondeau J., Boudou-Rouquette P., Goldwasser F., Leroy K., Goc J., et al. TP53, STK11, and EGFR Mutations Predict Tumor Immune Profile and the Response to Anti-PD-1 in Lung Adenocarcinoma. Clin. Cancer Res. 2018;24:5710–5723. doi: 10.1158/1078-0432.CCR-18-0163. [DOI] [PubMed] [Google Scholar]
- 183.Rashed H.E., Abdelrahman A.E., Abdelgawad M., Balata S., Shabrawy M.E. Prognostic Significance of Programmed Cell Death Ligand 1 (PD-L1), CD8+ Tumor-Infiltrating Lymphocytes and p53 in Non-Small Cell Lung Cancer: An Immunohistochemical Study. Turk Patoloji Derg. 2017;1:211–222. doi: 10.5146/tjpath.2017.01398. [DOI] [PubMed] [Google Scholar]
- 184.Rao N., Qiu J., Wu J., Zeng H., Su F., Qiu K., Wu J., Yao H. Significance of Tumor-Infiltrating Lymphocytes and the Expression of Topoisomerase IIα in the Prediction of the Clinical Outcome of Patients with Triple-Negative Breast Cancer after Taxane-Anthracycline-Based Neoadjuvant Chemotherapy. Chemotherapy. 2017;62:246–255. doi: 10.1159/000470900. [DOI] [PubMed] [Google Scholar]
- 185.Busuttil V., Droin N., McCormick L., Bernassola F., Candi E., Melino G., Green D.R. NF-kappaB inhibits T-cell activation-induced, p73-dependent cell death by induction of MDM2. Proc. Natl. Acad. Sci. USA. 2010;107:18061–18066. doi: 10.1073/pnas.1006163107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Qiao H.-B., Li J., Lv L.-J., Nie B.-J., Lu P., Xue F., Zhang Z.-M. The effects of interleukin 2 and rAd-p53 as a treatment for glioblastoma. Mol. Med. Rep. 2018;17:4853–4859. doi: 10.3892/mmr.2018.8408. [DOI] [PubMed] [Google Scholar]
- 187.Uz U., Eskiizmir G. Association Between Interleukin-6 and Head and Neck Squamous Cell Carcinoma: A Systematic Review. Clin Exp Otorhinolaryngol. 2021;14:50–60. doi: 10.21053/ceo.2019.00906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Oh K., Lee O.-Y., Park Y., Seo M.W., Lee D.-S. IL-1β induces IL-6 production and increases invasiveness and estrogen-independent growth in a TG2-dependent manner in human breast cancer cells. BMC Cancer. 2016;16:724. doi: 10.1186/s12885-016-2746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Fiering S.N., Ho G.W. Speed kills: Advancement in th17 cell adoptive cell therapy for solid tumors. Cancer Res. 2020;80:3795–3796. doi: 10.1158/0008-5472.CAN-20-2306. [DOI] [PubMed] [Google Scholar]
- 190.Yang Q., Liu X., Liu Q., Guan Z., Luo J., Cao G., Cai R., Li Z., Xu Y., Wu Z., et al. Roles of mTORC1 and mTORC2 in controlling γδ T1 and γδ T17 differentiation and function. Cell Death Differ. 2020;27:2248–2262. doi: 10.1038/s41418-020-0500-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Nunez N.P., Oh W.-J., Rozenberg J., Perella C., Anver M., Barrett J.C., Perkins S.N., Berrigan D., Moitra J., Varticovski L., et al. Accelerated tumor formation in a fatless mouse with type 2 diabetes and inflammation. Cancer Res. 2006;66:5469–5476. doi: 10.1158/0008-5472.CAN-05-4102. [DOI] [PubMed] [Google Scholar]
- 192.Bent R., Moll L., Grabbe S., Bros M. Interleukin-1 Beta-A Friend or Foe in Malignancies? Int. J. Mol. Sci. 2018;19:2155. doi: 10.3390/ijms19082155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Jain N., Sudhakar C., Swarup G. Tumor necrosis factor-alpha-induced caspase-1 gene expression. Role of p73. FEBS J. 2007;274:4396–4407. doi: 10.1111/j.1742-4658.2007.05969.x. [DOI] [PubMed] [Google Scholar]
- 194.Roberts J.Z., Holohan C., Sessler T., Fox J., Crawford N., Riley J.S., Khawaja H., Majkut J., Evergren E., Humphreys L.M., et al. The SCFSkp2 ubiquitin ligase complex modulates TRAIL-R2-induced apoptosis by regulating FLIP(L) Cell Death Differ. 2020;27:2726–2741. doi: 10.1038/s41418-020-0539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Damgaard R.B., Jolin H.E., Allison M.E.D., Davies S.E., Titheradge H.L., McKenzie A.N.J., Komander D. OTULIN protects the liver against cell death, inflammation, fibrosis, and cancer. Cell Death Differ. 2020;27:1457–1474. doi: 10.1038/s41418-020-0532-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Zhang J., Yang Y., Zhou S., He X., Cao X., Wu C., Hu H., Qin J., Wei G., Wang H., et al. Membrane-bound TNF mediates microtubule-targeting chemotherapeutics-induced cancer cytolysis via juxtacrine inter-cancer-cell death signaling. Cell Death Differ. 2020;27:1569–1587. doi: 10.1038/s41418-019-0441-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Li L., Li L., Li W., Chen T., Zou B., Zhao L., Wang H., Wang X., Xu L., Liu X., et al. TAp73-induced phosphofructokinase-1 transcription promotes the Warburg effect and enhances cell proliferation. Nat. Commun. 2018;9:4683. doi: 10.1038/s41467-018-07127-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Lu J. The Warburg metabolism fuels tumor metastasis. Cancer Metastasis Rev. 2019;38:157–164. doi: 10.1007/s10555-019-09794-5. [DOI] [PubMed] [Google Scholar]
- 199.Lissy N.A., Davis P.K., Irwin M., Kaelin W.G., Dowdy S.F. A common E2F-1 and p73 pathway mediates cell death induced by TCR activation. Nature. 2000;407:642–645. doi: 10.1038/35036608. [DOI] [PubMed] [Google Scholar]
- 200.Mantovani F., Collavin L., Del Sal G. Mutant p53 as a guardian of the cancer cell. Cell Death Differ. 2019;26:199–212. doi: 10.1038/s41418-018-0246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lonetto G., Koifman G., Silberman A., Attery A., Solomon H., Levin-Zaidman S., Goldfinger N., Porat Z., Erez A., Rotter V. Mutant p53-dependent mitochondrial metabolic alterations in a mesenchymal stem cell-based model of progressive malignancy. Cell Death Differ. 2019;26:1566–1581. doi: 10.1038/s41418-018-0227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Li Y., Cao Y., Xiao J., Shang J., Tan Q., Ping F., Huang W., Wu F., Zhang H., Zhang X. Inhibitor of apoptosis-stimulating protein of p53 inhibits ferroptosis and alleviates intestinal ischemia/reperfusion-induced acute lung injury. Cell Death Differ. 2020;27:2635–2650. doi: 10.1038/s41418-020-0528-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Gong L., Pan X., Abali G.K., Little J.B., Yuan Z.-M. Functional interplay between p53 and Δ133p53 in adaptive stress response. Cell Death Differ. 2020;27:1618–1632. doi: 10.1038/s41418-019-0445-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Radine C., Peters D., Reese A., Neuwahl J., Budach W., Jänicke R.U., Sohn D. The RNA-binding protein RBM47 is a novel regulator of cell fate decisions by transcriptionally controlling the p53-p21-axis. Cell Death Differ. 2020;27:1274–1285. doi: 10.1038/s41418-019-0414-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Billon N., Terrinoni A., Jolicoeur C., McCarthy A., Richardson W.D., Melino G., Raff M. Roles for p53 and p73 during oligodendrocyte development. Development. 2004;131:1211–1220. doi: 10.1242/dev.01035. [DOI] [PubMed] [Google Scholar]
- 206.Gonzalez-Cano L., Fuertes-Alvarez S., Robledinos-Anton N., Bizy A., Villena-Cortes A., Fariñas I., Marques M.M., Marin M.C. p73 is required for ependymal cell maturation and neurogenic SVZ cytoarchitecture. Dev. Neurobiol. 2016;76:730–747. doi: 10.1002/dneu.22356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Melino G., De Laurenzi V., Vousden K.H. p73: Friend or foe in tumorigenesis. Nat. Rev. Cancer. 2002;2:605–615. doi: 10.1038/nrc861. [DOI] [PubMed] [Google Scholar]
- 208.Candi E., Agostini M., Melino G., Bernassola F. How the TP53 family proteins TP63 and TP73 contribute to tumorigenesis: Regulators and effectors. Hum. Mutat. 2014;35:702–714. doi: 10.1002/humu.22523. [DOI] [PubMed] [Google Scholar]
- 209.Tang Z., Li C., Kang B., Gao G., Li C., Zhang Z. GEPIA: A web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017;45:W98–W102. doi: 10.1093/nar/gkx247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Uramoto H., Sugio K., Oyama T., Nakata S., Ono K., Morita M., Funa K., Yasumoto K. Expression of deltaNp73 predicts poor prognosis in lung cancer. Clin. Cancer Res. 2004;10:6905–6911. doi: 10.1158/1078-0432.CCR-04-0290. [DOI] [PubMed] [Google Scholar]
- 211.Wang B., Liu X., Liu H., Guo J., Zhang T., Zhou N., Ma Y., Yu H., Chen L., Ren Z., et al. Differential expressions of MDM2 and TAP73 in cancer and cancer-adjacent tissues in patients with non-small-cell lung carcinoma. Pulmonology. 2018;24:155–163. doi: 10.1016/j.rppnen.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 212.Uramoto H., Sugio K., Oyama T., Nakata S., Ono K., Nozoe T., Yasumoto K. Expression of the p53 family in lung cancer. Anticancer Res. 2006;26:1785–1790. [PubMed] [Google Scholar]
- 213.Wakatsuki M., Ohno T., Iwakawa M., Ishikawa H., Noda S., Ohta T., Kato S., Tsujii H., Imai T., Nakano T. p73 protein expression correlates with radiation-induced apoptosis in the lack of p53 response to radiation therapy for cervical cancer. Int. J. Radiat. Oncol. Biol. Phys. 2008;70:1189–1194. doi: 10.1016/j.ijrobp.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 214.Mega Tiber P., Baloglu L., Ozden S., Ozgen Z., Ozyurt H., Eren M., Orun O. The association of apoptotic protein expressions sensitive to apoptosis gene, p73 and p53 with the prognosis of cervical carcinoma. Onco. Targets. Ther. 2014;7:2161–2168. doi: 10.2147/OTT.S71448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Ye H., Guo X. TP73 is a credible biomarker for predicting clinical progression and prognosis in cervical cancer patients. Biosci. Rep. 2019;39:BSR20190095. doi: 10.1042/BSR20190095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Casciano I., Mazzocco K., Boni L., Pagnan G., Banelli B., Allemanni G., Ponzoni M., Tonini G.P., Romani M. Expression of DeltaNp73 is a molecular marker for adverse outcome in neuroblastoma patients. Cell Death Differ. 2002;9:246–251. doi: 10.1038/sj.cdd.4400993. [DOI] [PubMed] [Google Scholar]
- 217.Zitterbart K., Zavrelova I., Kadlecova J., Spesna R., Kratochvilova A., Pavelka Z., Sterba J. p73 expression in medulloblastoma: TAp73/DeltaNp73 transcript detection and possible association of p73alpha/DeltaNp73 immunoreactivity with survival. Acta Neuropathol. 2007;114:641–650. doi: 10.1007/s00401-007-0298-2. [DOI] [PubMed] [Google Scholar]
- 218.Nemajerova A., Petrenko O., Trümper L., Palacios G., Moll U.M. Loss of p73 promotes dissemination of Myc-induced B cell lymphomas in mice. J. Clin. Investig. 2010;120:2070–2080. doi: 10.1172/JCI40331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Gomez L.C., Sottile M.L., Guerrero-Gimenez M.E., Zoppino F.C.M., Redondo A.L., Gago F.E., Orozco J.I., Tello O.M., Roqué M., Nadin S.B., et al. TP73 DNA methylation and upregulation of ΔNp73 are associated with an adverse prognosis in breast cancer. J. Clin. Pathol. 2018;71:52–58. doi: 10.1136/jclinpath-2017-204499. [DOI] [PubMed] [Google Scholar]
- 220.Domínguez G., Peña C., Silva J., García J.M., García V., Rodríguez R., Cantos B., Citores M.J., España P., Bonilla F. The presence of an intronic deletion in p73 and high levels of ZEB1 alter the TAp73/DeltaTAp73 ratio in colorectal carcinomas. J. Pathol. 2006;210:390–397. doi: 10.1002/path.2066. [DOI] [PubMed] [Google Scholar]
- 221.Vilgelm A.E., Hong S.M., Washington M.K., Wei J., Chen H., El-Rifai W., Zaika A. Characterization of ΔNp73 expression and regulation in gastric and esophageal tumors. Oncogene. 2010;29:5861–5868. doi: 10.1038/onc.2010.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Hofstetter G., Berger A., Chamson M., Müller-Holzner E., Reimer D., Ulmer H., Uramoto H., Marth C., Zeimet A.G., Zeillinger R., et al. Clinical relevance of TAp73 and ΔNp73 protein expression in ovarian cancer: A series of 83 cases and review of the literature. Int J Gynecol Pathol. 2011;30:527–531. doi: 10.1097/PGP.0b013e31821ac519. [DOI] [PubMed] [Google Scholar]
- 223.Chen J., Li D., Killary A.M., Sen S., Amos C.I., Evans D.B., Abbruzzese J.L., Frazier M.L. Polymorphisms of p16, p27, p73, and MDM2 modulate response and survival of pancreatic cancer patients treated with preoperative chemoradiation. Ann. Surg. Oncol. 2009;16:431–439. doi: 10.1245/s10434-008-0220-8. [DOI] [PubMed] [Google Scholar]
- 224.Ito Y., Takeda T., Wakasa K., Tsujimoto M., Sakon M., Matsuura N. Expression of p73 and p63 proteins in pancreatic adenocarcinoma: p73 overexpression is inversely correlated with biological aggressiveness. Int. J. Mol. Med. 2001;8:67–71. doi: 10.3892/ijmm.8.1.67. [DOI] [PubMed] [Google Scholar]
- 225.Li J., Jiang X., Zhou X. [Expression and prognosis significance of p73 and PCNA in laryngeal squamous cell carcinoma] Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2005;19:1121–1124. [PubMed] [Google Scholar]
- 226.Choi H.-R., Batsakis J.G., Zhan F., Sturgis E., Luna M.A., El-Naggar A.K. Differential expression of p53 gene family members p63 and p73 in head and neck squamous tumorigenesis. Hum. Pathol. 2002;33:158–164. doi: 10.1053/hupa.2002.30722. [DOI] [PubMed] [Google Scholar]