Abstract
Successful implementation of virtual healthcare depends immensely on patients’ perceptions and satisfaction. This cross-sectional study assessed patients’ perceptions of, and factors associated with, poor and average satisfaction with the outpatient telemedicine clinics in the Kingdom of Saudi Arabia (KSA). This questionnaire-based survey was conducted among 720 patients who attended outpatient telemedicine clinics from different regions of the KSA. Of the sample studied, 54.7% of the participants had high satisfaction and the most common disadvantage perceived by patients was technical issues (53.1%), followed by fewer personal interactions (30.4%). Around 75% of the participants desired to use telemedicine services even after the COVID-19 pandemic. Logistic regression analysis revealed that age group more than 40 years (OR = 1.59; 95% CI = 1.04–2.44, p = 0.031), education less than university level (OR = 1.68; 95% CI = 1.07–2.15, p = 0.025), and first-time participants (OR = 3.28; 95% CI = 2.32–4.65, p < 0.001) were significantly associated with poor and average satisfaction ratings. The concerned authorities must make targeted action plans to circumvent the disadvantages perceived by patients accessing telemedicine. Furthermore, a multicenter, exploratory study that compares the virtual clinic with other telemedicine services in the KSA is warranted.
Keywords: COVID-19, perceptions, satisfaction, Saudi Arabia, virtual clinics
1. Introduction
The World Health Organization (WHO) elucidated telemedicine as “The delivery of healthcare services, where distance is a basic factor, by all medical care experts utilizing information and communication technologies (ICTs), for diagnosis, treatment, and prevention of diseases and infirmities” [1]. Telemedicine incorporates the use of telecommunications in physician–patient interactions [2]. Telemedicine implies a medical care supplier’s utilization of ICTs in the conveyance of clinical medical care administration. In contrast, telehealth alludes to a medical care supplier’s utilization of ICTs to convey clinical, as well as non-clinical, medical services administration [2,3]. Accessibility, equity distribution, quality, and cost-effectiveness are the essential challenges that healthcare systems face worldwide. Modern ICTs, such as smartphones, the internet, and computers, have great potential to address the contemporary health problems of developed and less developed countries [1,4].
The first telemedicine programs were established almost 70 years ago, but the technology grew considerably after 2019 and has become widely interactive in all surgical and medical specialties because of the COVID-19 pandemic and lockdown [5,6,7]. One of the advantages of telemedicine is cost saving because transmitting information is less expensive than transporting people. Other benefits include immediate access to medical expertise regardless of location, more timely diagnoses and treatments than might be possible, and the elimination of long patient commutes from rural communities to urban centers [8,9,10]. Telemedicine has been extensively utilized during the COVID-19 pandemic as it helps in diminishing contact with medical services offices, staff, and patients, and thereby minimizes the danger of COVID-19 spread [11].
Successful implementation of any healthcare delivery, including telemedicine, depends immensely on patient perceptions and satisfaction. Patients are the primary source of information that tells us whether the healthcare is being delivered properly and if the healthcare received meets their expectations [12,13,14]. Dissatisfaction with telemedicine care services would render these services unnecessary and costly. With the surge in worldwide telemedicine services during the COVID-19 pandemic, it is essential to maintain a key quality evaluation indicator of patient satisfaction, regardless of delivery method [15]. Patient satisfaction is the voice of the customer in healthcare and is a growing concern in all aspects of healthcare. Just like the conventional modalities of medical care conveyance, telemedicine depends intensely on feedback from patients [16,17]. A systematic review conducted by Kruse et al. revealed that assessing patients’ satisfaction toward telehealth and its associated factors could help stakeholders to find solutions for specific problems [15]. A recent study by Asma et al. in the Kingdom of Saudi Arabia (KSA) reported that nearly one-third (37%) of patients were highly satisfied with the telemedicine services provided to them during the COVID-19 pandemic [18].
In the KSA, the Ministry of Health (MOH) is concerned with telemedicine through different platforms such as outpatient telemedicine clinics (virtual clinics), 937 call centers, and the Seha smartphone application. In addition, the Saudi Commission for Health Specialties also launched a “telemedicine” training program to train all healthcare professionals to care for patients remotely with the best global practices in telemedicine [19]. Continuous assessment of patients’ perceptions and satisfaction towards telemedicine and its associated factors is essential for the successful implementation of high-quality telemedicine care, especially during pandemics. In the KSA, some authors attempted to find patient satisfaction towards telemedicine [18,20]. However, studies that investigate patients’ perceptions of its advantages and challenges, as well as factors associated with poor satisfaction towards telemedicine, are limited. Therefore, the present study aimed to assess patients’ perceptions of and satisfaction with the Outpatient Telemedicine Clinics, and the association between socio-demographic characteristics and satisfaction scores during the COVID-19 era in the KSA.
2. Materials and Methods
2.1. Study Design and Setting
This analytical, cross-sectional study was performed from 15 June 2021 to 20 October 2021. The present study’s setting was outpatient telemedicine clinics from different departments registered with the MOH, KSA.
2.2. Sample Size Estimation
The research team estimated the required sample size based on the formula n = z2 pq/e2. Here, “n” is the required sample size, “p” is prevalence (37.3% of patients’ satisfaction towards telemedicine) taken from the study done by Nasser et al. [18], q is 1−p (1−0.373) = 0.627, z = 1.96 at 95% confidence interval, and e = 5% margin of error. Applying the values to the above formula, the estimated minimum required sample size for this study was 360 participants. Considering the inclusion of multiple regions of the KSA, we doubled (720) the sample size for this study.
2.3. Sampling Procedure
A consecutive sampling method was applied to select study participants. In this method, the data collectors communicated with the consecutively registered patients after they completed their outpatient telemedicine clinic visits. To get patients from all the days of the week for the survey, we restricted contact to a maximum of 50 patients per day for data collection.
2.4. Inclusion and Exclusion Criteria
The present study included patients attending all the department telemedicine outpatient virtual clinics concerned with the MOH, KSA. Patients who were not willing to participate and private hospital telemedicine clinics were excluded from the present study. Further, this study did not include patients attending other MOH telemedicine care platforms (937 call centers, the Seha app, etc.).
2.5. Ethical Consideration
The present study’s data were collected after ethical committee clearance (no. 089, Qurayat Health Affairs, MOH, KSA) and other necessary approvals were obtained from the concerned authorities. Informed consent was obtained from each participant before proceeding to fill the data collection form.
2.6. Data Collection Procedure
An open-source, structured, and validated questionnaire (Cronbach’s Alpha = 0.89) adapted from a previously published study [18] was sent to the selected patients through their WhatsApp or email immediately after telemedicine consultation, or, at the maximum, the end of that day (by Google form). The questionnaire consisted of three parts. Part 1 collected details about patient socio-demographic characteristics. Part 2 contained details related to patient perception towards telemedicine, including its perceived advantages and disadvantages. Part 3 had eight questions related to patient satisfaction related to telemedicine. The responses in each question were recorded on a 5-point Likert scale as very satisfied to very dissatisfied. The score for each response ranged from 5 (very satisfied) to 1 (very dissatisfied). At the end of the survey, the total score was calculated. A higher score in the patient satisfaction questionnaire indicated higher satisfaction with telemedicine services. Furthermore, patient satisfaction was graded as high (>75% of total score), average (50 to 75% of total score) and poor (<50% of total score).
2.7. Statistical Analysis
Statistical Package for Social Sciences (SPSS) software version 21 (IBM, Armonk, NY, USA) was used for data exported from Excel sheets obtained from Google form. Descriptive statistics for qualitative variables were presented as frequency and percentage, and mean and standard deviation (SD) for quantitative variables. After the Wilk–Shapiro test analysis, we executed independent t test and one way analysis of variance (ANOVA) to find the association between socio-demographic variables and mean satisfaction scores. We performed binomial logistic regression (enter method) analysis to identify the factors associated with poor and average telemedicine satisfaction. In this method, the adjusted independent variables were age category, gender, marital status, education status, employment, Virtual clinic setting, telemedicine before pandemic, and consultation department. A p-value of less than 0.05 and an odds ratio (OR) that did not include the null value were considered as statistically significant.
3. Results
Of the 720 participating patients, the majority (55%) of them were of male gender, married (65%), studied at the university/college level (82.5%), and employed in government settings (63.6%). Further, less than one-third of participants (29%) had experienced a telemedicine consultation before the COVID-19 pandemic (Table 1).
Table 1.
Background details of the study participants (n = 720).
| Variables | Frequency (n) | % |
|---|---|---|
| Age group (in years) (mean ± SD) | 42.9 ± 9.1 | |
| Gender Male Female |
396 324 |
55.0 45.0 |
| Marital status Married Single |
468 252 |
65.0 35.0 |
| Education level Less than University/College University/College |
126 594 |
17.5 82.5 |
| Employment Government Self-employed/Private Unemployed |
458 120 142 |
63.6 16.7 19.7 |
| Telemedicine consultation at PHC General hospital Specialty hospital |
302 340 78 |
41.9 47.2 10.8 |
| Telemedicine consultation experience before the pandemic Yes No |
209 511 |
29.0 71.0 |
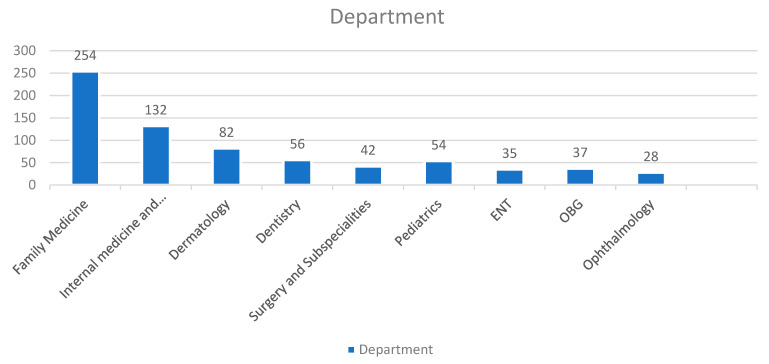
Figure 1 demonstrates the participating patients’ distribution as per the department/specialty outpatient virtual clinics. Of the 720 patients, 254 (35.2%) attended family medicine, followed by 132 (18.3%) in internal medicine and subspecialties, 82 (11.4%) in dermatology, and 56 (7.8%) in dentistry virtual outpatient clinics.
Figure 1.
Patients’ distribution according to department.
The relationship between socio-demographic characteristics and mean satisfaction scores towards virtual clinics is presented in Table 2. The mean satisfaction scores were significantly higher among the age group less than 40 years (mean ± SD = 32.93 ± 4.4, p < 0.001) and the married group (mean ± SD = 32.76 ± 5.4, p = 0.004). No other parameters had shown a significant association.
Table 2.
Comparison of telemedicine scores with patients’ background characteristics.
| Variables | Mean ± SD | p-Value (Two Tailed) |
|---|---|---|
| Age (in years) * ≤40 years >40 years |
32.93 ± 4.4 30.31 ± 4.7 |
<0.01 |
| Gender * Male Female |
31.41 ± 4.9 31.23 ± 3.8 |
0.691 |
| Marital status * Married Single |
32.76 ± 5.4 30.59 ± 6.4 |
0.004 |
| Education * University/College Less than University/College |
31.79 ± 4.1 31.26 ± 5.9 |
0.374 |
| Employment status ** Government Self-employed/Private Unemployed |
31.43 ± 4.3 32.02 ± 3.8 31.75 ± 5.1 |
0.652 |
| Telemedicine consultation at ** PHC General hospital Specialty hospital |
32.46 ± 5.7 32.74 ± 4.9 30.18 ± 5.1 |
0.07 |
| Telemedicine consultation experience before the pandemic * Yes No |
31.23 ± 3.4 32.14 ± 3.7 |
0.105 |
* Independent t test, ** One way ANOVA.
Table 3 presents the patients’ perception of virtual clinics, perceived advantages and disadvantages, and suggestions for improving telemedicine visits. Of the 720 participants, nearly half (45.3%) of them responded that their desire to be seen in person by the healthcare provider has changed during the current pandemic. Nearly two-thirds (68.1%) of the participants were willing to participate in another telemedicine consultation during the pandemic, and 74.4% of patients preferred telemedicine consultation even after the COVID-19 pandemic. The common advantages of telemedicine perceived by patients were convenience (79.3%), time saving (62.8%), and availability of the healthcare provider (45.7%). More than half (53.1%) of the participants responded that technical difficulties was the most common disadvantage perceived by them.
Table 3.
Patients’ perceptions towards virtual outpatient clinic consultation (n = 720).
| Perceptions | Frequency (n) | % |
|---|---|---|
| Has the COVID-19 pandemic changed your desire to be seen in person by a healthcare provider? Yes No Not sure |
326 186 208 |
45.3 25.8 28.9 |
| Do you think anything was missed or not addressed because you were not seen in person? Yes No Not sure |
284 214 222 |
39.4 29.7 30.8 |
| Willingness to participate in another telemedicine consultation during the COVID-19 pandemic Yes No Not sure |
490 124 106 |
68.1 17.2 14.7 |
| Preference towards telemedicine consultation once the COVID-19 pandemic is over. Yes No Not sure |
536 126 58 |
74.4 17.5 8.1 |
| Perceived advantages towards telemedicine Availability of healthcare provider Convenience No time off from work No travel Time saving Safety Visits not rushed None |
329 571 289 128 452 96 85 53 |
45.7 79.3 40.1 17.8 62.8 13.3 11.8 7.4 |
| Perceived disadvantages towards telemedicine Technological difficulties Less personal interaction Poor communication None |
382 219 248 110 |
53.1 30.4 34.4 15.3 |
| Recommendation for telemedicine care improvement Improvement in scheduling/coordination Improved technology Incorporation of diagnostic recommendation None |
281 320 162 91 |
39.0 44.4 22.5 12.6 |
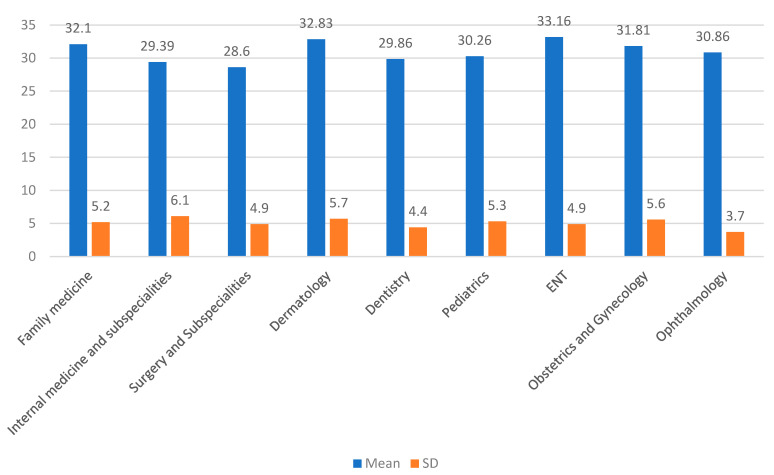
In the present study, the highest mean score was noted in ENT (33.16 ± 4.9), followed by dermatology (32.83 ± 5.7) and family medicine (32.1 ± 5.2) (Figure 2).
Figure 2.
Distribution of patients’ satisfaction scores as per the specialties (mean and SD).
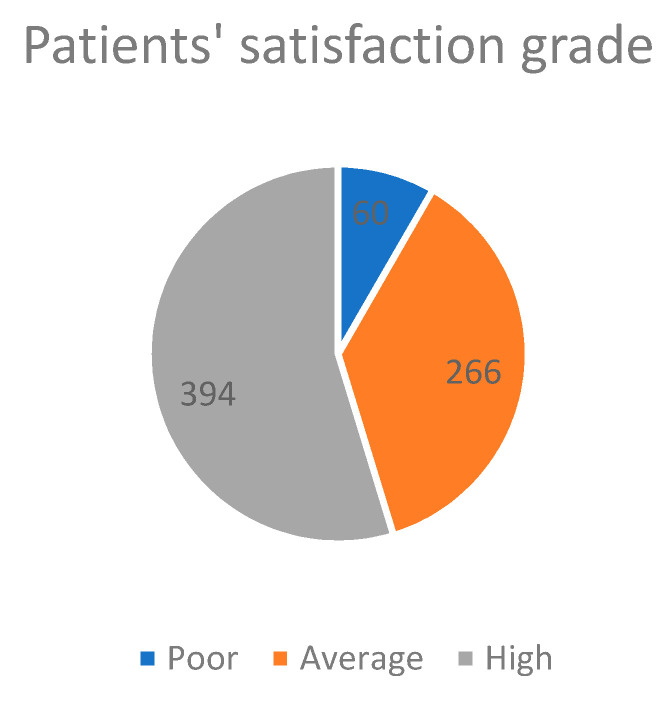
Of the 720 participants, 394 (54.7%) had high satisfaction, 266 (36.9%) had average satisfaction, and 60 (8.3%) had poor satisfaction with the virtual outpatient telemedicine clinics (Figure 3).
Figure 3.
Patients’ satisfaction grade for telemedicine (n = 720).
In the present study, we performed binomial logistic regression analysis to find the associated factors for poor and average patient satisfaction towards telemedicine. The research team executed the logistic regression analysis and, adjusting with other co-variables, the characteristics that were significantly associated with poor and average patient satisfaction scores were age group more than 40 years (OR = 1.59; 95% CI = 1.04–2.44, p = 0.031), education less than University/College level (OR = 1.68; 95% CI = 1.07–2.15, p = 0.025), patients attending a specialty hospital (OR = 1.73; 95% CI = 1.21–2.47, p = 0.03), and patients who had never had a telemedicine experience before (OR = 3.28; 95% CI = 2.32–4.65, p < 0.001) (Table 4).
Table 4.
Logistic regression analysis on patients’ socio-demographic characteristics with poor and average satisfaction towards telemedicine.
| Characteristics | Total Sample (n = 720) |
Poor and Average Satisfaction | Multivariate Analysis * No vs. Yes |
p Value ** | |
|---|---|---|---|---|---|
| No (n = 394) n (%) |
Yes (n = 326) n (%) |
Adjusted OR (95% CI) | |||
| Age (in years) ≤40 years >40 years |
286 434 |
190 204 |
96 230 |
Ref 1.59 (1.04–2.44) |
0.031 |
| Gender Female Male |
324 396 |
174 220 |
150 176 |
Ref 0.55 (0.89–0.63) |
0.554 |
| Marital status Single Married |
252 468 |
166 228 |
86 240 |
Ref 1.51 (0.96–1.91) |
0.072 |
| Education University/College Less than University/College |
594 126 |
326 68 |
268 58 |
Ref 1.68 (1.07–2.15) |
0.025 |
| Employment status Government Self-employed/Private Unemployed |
458 120 142 |
226 72 96 |
232 48 46 |
Ref 1.38 (0.81–2.35) 0.98 (0.56–1.74) |
0.237 0.932 |
| Telemedicine consultation at PHC General hospital Specialty hospital |
302 340 78 |
203 167 24 |
99 173 54 |
Ref 0.57 (0.31–1.05) 1.73 (1.21–2.47) |
0.70 0.03 |
| Previous telemedicine consultation Yes No |
209 511 |
130 264 |
79 247 |
Ref 3.28 (2.32–4.65) |
<0.001 |
| Consultation department Family medicine Internal medicine and subspecialities General Surgery and subspecialties Dentistry Other departments |
254 132 42 56 236 |
156 62 26 18 132 |
98 70 16 38 104 |
Ref 1.52 (0.95–2.43) 1.08 (0.51–2.28) 1.31 (0.92–2.13) 1.48 (0.98–2.24) |
0.081 0.844 0.142 0.061 |
* Variable(s) entered on step 1: age category, gender, marital status, education status, employment, virtual clinic setting, telemedicine before pandemic, and consultation department. ** p value less than 0.05 was considered as statistically significant.
4. Discussion
Globally, healthcare delivery has gone through a paradigm shift during the COVID-19 pandemic, with a sharp increase in virtual care. The promotion of telemedicine care might play a significant role in providing and accessing virtual care and other telehealth services during public health emergencies, such as the COVID-19 pandemic, as stated by the Centers for Disease Prevention and Control [21].
The present study found that 45.3% of participants agreed that the COVID-19 pandemic had changed their desire to see healthcare providers in person. Similar to the present research, Holtz et al. and Khan et al. also found that their study participants changed their desire to see providers [22,23]. This attitude change among patients is due to fear of exposure to COVID-19 patients in healthcare settings, as the world is far from the end of the pandemic.
The present study depicted that only 29% of the participants were involved in any form of telemedicine before the COVID-19 pandemic. However, an increased number of participants (74.4%) expressed their desire to have telemedicine consultations once the pandemic is over. This interesting finding suggests that patients wish to transform their healthcare towards virtual care in necessary situations. On the other hand, a study done by Grossman Z. et al. in 2021 stated that healthcare providers envisage decreasing virtual care after the pandemic [24]. Similar to the current study findings, Lagasse J. also reported that most consumers wished to prefer telemedicine even post-COVID-19 era [25]. In contrast, Nasser A. et al. reported a lesser proportion (48.9%) of patient preference towards telemedicine once the COVID-19 pandemic is over [18]. This striking difference between the different studies could be due to the differences in study settings, inclusion criteria, and the departments involved. The present study included patients from all medical and surgical specialties from regions of the KSA.
Technical difficulties (53.1%), poor communication (34.4%), and less personal communication (30.4%) were the most common disadvantages perceived by the present study’s participants. Similarly, Nasser A. et al. and Alharbi et al. also reported that technical difficulties was the most common disadvantage perceived by patients [18,20]. On the other hand, physicians faced difficulties in making proper clinical diagnoses due to the absence of physical examinations, which was their major perceived disadvantage of virtual care [26].
The present study revealed that more than half (54.7%) of the study participants were highly satisfied with their telemedicine services. Similar to the present survey, a study done in the KSA during the COVID-19 pandemic also revealed that 52% of participants were highly satisfied with telemedicine services [18]. This level of acceptance and satisfaction with telemedicine services in the KSA could be positively influenced by internal or external circumstances. External circumstances refers to the system providing telemedicine care, including government policy towards digital services, availability of trained healthcare providers, and advanced network coverage (4G/5G). At the same time, the internal factors are socio-cultural, education, economic status, and high-level acceptance of innovation [27,28,29]. It is noteworthy to mention that the Saudi Commission for Health Specialties regularly conducts telemedicine training programs for all healthcare professionals to attain telemedicine care at a global level [19]. Other factors responsible for high-level satisfaction in the KSA are the high level of literacy (95.3%) and coverage proportion (90%) of advanced internet in the KSA. The research communities revealed the same high-level satisfaction in other economically developed countries [17,30]. However, the developing and underdeveloped countries’ scenarios could be different due to low literacy rates, poor economies, poor network coverage, unreliable electric power, and restricted resources to implement new technologies [31,32,33].This study aimed to identify the factors associated with poor and average satisfaction towards outpatient telemedicine clinics through binomial logistic regression. The present study revealed that higher age group was one of the significant variables associated with poor and average satisfaction (OR = 1.59; 95% CI = 1.04–2.44, p = 0.031). Similar to the present study findings, several authors also reported that increasing age is a significant factor for poor telemedicine satisfaction [20,23,34,35]. In the era of rising virtual care, aged people find several barriers when accessing it due to inadequate technical competencies and visual and hearing difficulties. This leads to poor acceptance of and dissatisfaction with telemedicine among them. It is noteworthy to mention here that the United Nations observed the international day of older people in 2021 with the theme “Digital Equity for All Ages.” This emphasizes the need for access to care and meaningful involvement in digital healthcare by aged persons [36]. In this study, participants with less than university education levels had significantly lower satisfaction with outpatient telemedicine clinics (OR = 1.68; 95% CI = 1.07–2.15, p = 0.025). Identical to the present research findings, Khan Z. et al. and Alharbi et al. also reported a significant association between patients’ satisfaction with virtual clinics and level of education [20,23]. This could be due to the influence of education on health and ease of using technology among educated patients [37].
The present study depicted that those patients who attended virtual clinic consultations at specialty hospitals had significantly lower satisfaction levels (OR = 1.73; 95% CI = 1.21–2.47, p = 0.03). In the KSA, specialty hospitals generally provide more advanced care for patients. Hence, patients might have preferred to be seen by healthcare providers in person for detailed clinical examinations and laboratory investigations. Another significant variable identified in our study that is associated with the lower satisfaction regarding the virtual clinics is first-time virtual care attendees (OR = 3.28; 95% CI = 2.32–4.65, p < 0.001). Since virtual healthcare delivery is a relatively new concept, patients who attended first-time virtual care might not know how to use it. This finding is supported by a study done in the primary health care settings in the Riyadh region of the KSA [20]. In that research, well-informed patients had significantly higher satisfaction with virtual clinics. Healthcare providers, including physicians, are the essential stakeholders for implementing telemedicine services. A study conducted by Alhajri et al. in 2021 at Abhudhabi reported that physicians perceived that spending less time in documentation and seeing more patients within their duty schedule were the significant advantages of telemedicine. They also perceived that telemedicine could be more effective in follow-up, reordering medications, psychological fields, and essential primary care services. However, a high chance of misdiagnosis due to lack of physical examination and less personal rapport with patients were the disadvantages perceived by the physicians. Furthermore, the physicians were more confident in delivering care with combined audio-video care than with audio care alone [38]. Another study that assessed perceived advantages and disadvantages among Saudi physicians in the Taif region showed that almost a third of the participants believed that telemedicine increased the effectiveness of therapeutic intervention and 44% perceived that virtual care improved patient care. However, the physicians reported that virtual care cannot replace the face-to-face consultation and it can be used for stable patients from remote areas [26]. Some authors explored the integrative advantages and disadvantages perceived by the patients and care providers of telemedicine. They suggested that patient satisfaction and quality of care can be improved by audio-video consultation care, limiting access to such care by stable patients, and referral care for face-to-face examinations where physicians suspect the possibility of misdiagnosis due to lack of physical examination [39,40].
Even though the research team executed this cross-sectional survey with a standard methodology, certain limitations need to be noted while reading the results of this study. Firstly, this study used a non-probability consecutive sampling method to select the study participants. Hence, limitations associated with this method are applicable to the present study. Secondly, this cross-sectional study attempted to find only association, not causation.
5. Conclusions
The present study revealed that more than half of the participants had high satisfaction with outpatient telemedicine clinics. This study depicted several socio-demographic factors associated with poor and average patient satisfaction. Even though the patients perceived some disadvantages, technical issues was the major disadvantage faced by them. Most of the participants desired to use telemedicine services even after the COVID-19 pandemic. This indicates that the COVID-19 pandemic has transformed KSA patients’ desire towards virtual care. However, the concerned authorities must make the necessary and targeted action plans to circumvent the disadvantages perceived by patients regarding telemedicine. Furthermore, a multicenter, exploratory study that compares the virtual outpatient clinic with other telemedicine services provided by the MOH, KSA is warranted.
Acknowledgments
The research team wishes to thank all the participants of this study. We also extend our sincere thanks to the Ministry of Health, Saudi Arabia for their cooperation, especially the virtual clinic nurses, sister Hamedah Moqeem Alrwily and sister Madiha Thane Alrwily, from Prince Mutaib bin Abdulaziz Hospital, Sakaka, Aljouf, Saudi Arabia for their tremendous help in data collection.
Author Contributions
Conceptualization, A.T., N.H.A., T.H.A. and A.H.A.-H.; methodology, A.T., N.H.A., M.J.A. and Z.M.A.; software, A.T., H.A., A.H.A.-H. and T.A.M.A. validation, A.T., N.H.A. and M.G.A.; formal analysis, A.T., N.H.A., M.J.A., Z.M.A., H.A. and T.A.M.A.; investigation, A.T., A.H.A.-H., M.J.A., T.H.A. and T.A.M.A.; resources, A.T., Z.M.A. and H.A.; data curation, A.T., M.G.A., T.A.M.A. and H.A.; writing—original draft preparation, A.T., N.H.A. and A.H.A.-H.; writing—review and editing, A.T., N.H.A., A.H.A.-H., Z.M.A., M.J.A., M.G.A., T.A.M.A., T.H.A. and H.A.; visualization, T.A.M.A. and N.H.A.; supervision, T.A.M.A.; project administration, T.A.M.A., M.J.A., M.G.A., T.H.A. and T.A.M.A.; funding acquisition, A.T. and N.H.A. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the Deanship of Scientific Research at Jouf University under grant No. (DSR-2021-01-03140).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Research Ethics Committee (Reg NO: H-13-S-071), Qurayyat Health Affairs, Ministry of Health, The Kingdom of Saudi Arabia through approval no: 089.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . Telemedicine: Opportunities and Developments in Member States. Report on the Second Global Survey on eHealth. World Health Organization; Geneva, Switzerland: 2010. [Google Scholar]
- 2.Wootton R. Telemedicine. BMJ. 2001;323:557–560. doi: 10.1136/bmj.323.7312.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mechanic O.J., Persaud Y., Kimball A.B. Telehealth Systems. [(accessed on 10 September 2021)];2021 Available online: https://www.ncbi.nlm.nih.gov/books/NBK459384/
- 4.Mamlin B.W., Tierney W.M. The Promise of Information and Communication Technology in Healthcare: Extracting Value From the Chaos. Am. J. Med. Sci. 2016;351:59–68. doi: 10.1016/j.amjms.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Dekker P.K., Bhardwaj P., Singh T., Bekeny J.C., Kim K.G., Steinberg J.S., Evans K.K., Song D.H., Attinger C.E., Fan K.L. Telemedicine in the Wake of the COVID-19 Pandemic: Increasing Access to Surgical Care. Plast. Reconstr. Surg. Glob. Open. 2021;9:e3228. doi: 10.1097/GOX.0000000000003228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galiero R., Pafundi P.C., Nevola R., Rinaldi L., Acierno C., Caturano A., Salvatore T., Adinolfi L.E., Costagliola C., Sasso F.C. The Importance of Telemedicine during COVID-19 Pandemic: A Focus on Diabetic Retinopathy. J. Diabetes Res. 2020;2020:9036847. doi: 10.1155/2020/9036847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lakshin G., Banek S., Keese D., Rolle U., Schmedding A. Telemedicine in the pediatric surgery in Germany during the COVID-19 pandemic. Pediatric Surg. Int. 2021;37:389–395. doi: 10.1007/s00383-020-04822-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boxer R.J. Advantages and utilization of telemedicine. mHealth. 2019;5:12. doi: 10.21037/mhealth.2019.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kichloo A., Albosta M., Dettloff K., Wani F., El-Amir Z., Singh J., Aljadah M., Chakinala R.C., Kanugula A.K., Solanki S., et al. Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA. Fam. Med. Community Health. 2020;8:e000530. doi: 10.1136/fmch-2020-000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gajarawala S.N., Pelkowski J.N. Telehealth benefits and barriers. J. Nurse Pract. 2021;17:218–221. doi: 10.1016/j.nurpra.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monaghesh E., Hajizadeh A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health. 2020;20:1193. doi: 10.1186/s12889-020-09301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dinesen B., Nonnecke B., Lindeman D., Toft E., Kidholm K., Jethwani K., Young H.M., Spindler H., Oestergaard C.U., Southard J.A. Personalized telehealth in the future: A global research agenda. J. Med. Internet Res. 2016;18:e5257. doi: 10.2196/jmir.5257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berger S., Saut A.M., Berssaneti F.T. Using patient feedback to drive quality improvement in hospitals: A qualitative study. BMJ Open. 2020;10:e037641. doi: 10.1136/bmjopen-2020-037641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong E., Mavondo F., Fisher J. Patient feedback to improve quality of patient-centred care in public hospitals: A systematic review of the evidence. BMC Health Serv. Res. 2020;20:530. doi: 10.1186/s12913-020-05383-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kruse C.S., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open. 2017;7:e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hardavella G., Aamli-Gaagnat A., Saad N., Rousalova I., Sreter K.B. How to give and receive feedback effectively. Breathe. 2017;13:327–333. doi: 10.1183/20734735.009917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramaswamy A., Yu M., Drangsholt S., Ng E., Culligan P.J., Schlegel P.N., Hu J.C. Patient Satisfaction With Telemedicine During the COVID-19 Pandemic: Retrospective Cohort Study. J. Med. Internet Res. 2020;22:e20786. doi: 10.2196/20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdel Nasser A., Mohammed Alzahrani R., Al-Falah C.A., Muwafak Jreash D., Talea Almouled N., Salem Bakula D., Abed Ra’Oof R. Measuring the Patients’ Satisfaction About Telemedicine Used in Saudi Arabia During COVID-19 Pandemic. Cureus. 2021;13:e13382. doi: 10.7759/cureus.13382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MOH Telemedicine. [(accessed on 21 September 2021)]; Available online: https://www.moh.gov.sa/en/Ministry/Information-and-services/Pages/Telemedicine.aspx.
- 20.Alharbi K., Aldosari M., Alhassan A., Alshallal K., Altamimi A., Altulaihi B. Patient satisfaction with virtual clinic during Coronavirus disease (COVID-19) pandemic in primary healthcare, Riyadh, Saudi Arabia. J. Fam. Community Med. 2021;28:48–54. doi: 10.4103/jfcm.JFCM_353_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koonin L.M., Hoots B., Tsang C.A., Leroy Z., Farris K., Jolly B., Antall P., McCabe B., Zelis C.B., Tong I. Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. Morb. Mortal. Wkly. Rep. 2020;69:1595. doi: 10.15585/mmwr.mm6943a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holtz B.E. Patients perceptions of telemedicine visits before and after the coronavirus disease 2019 pandemic. Telemed. E-Health. 2021;27:107–112. doi: 10.1089/tmj.2020.0168. [DOI] [PubMed] [Google Scholar]
- 23.Khan Z.A., Zahoor A., Afzal I., Butt U., Siddiqui A.M., Khan Z., Shah I.A., Shah J.A. Evaluation of Patient Perception and Satisfaction Toward the Use of Telemedicine During Pandemic of Novel Coronavirus in Pakistan. Telemed. E-Health. 2021;10:1174–1179. doi: 10.1089/tmj.2020.0343. [DOI] [PubMed] [Google Scholar]
- 24.Grossman Z., Chodick G., Reingold S.M., Chapnick G., Ashkenazi S. The future of telemedicine visits after COVID-19: Perceptions of primary care pediatricians. Isr. J. Health Policy Res. 2020;9:53. doi: 10.1186/s13584-020-00414-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lagasse J. Most Consumers Want to Keep Telehealth after the COVID-19 Pandemic. [(accessed on 24 October 2021)]. Available online: https://www.healthcarefinancenews.com/news/most-consumers-want-keep-telehealth-after-covid-19-pandemic.
- 26.Mubaraki A.A., Alrabie A.D., Sibyani A.K., Aljuaid R.S., Bajaber A.S., Mubaraki M.A. Advantages and disadvantages of telemedicine during the COVID-19 pandemic era among physicians in Taif, Saudi Arabia. Saudi Med. J. 2021;42:110–115. doi: 10.15537/smj.2021.1.25610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park H., Choi S.O. Digital Innovation Adoption and Its Economic Impact Focused on Path Analysis at National Level. J. Open Innov. Technol. Market Complex. 2019;5:56. doi: 10.3390/joitmc5030056. [DOI] [Google Scholar]
- 28.Millan PhD J., Yunda PhD L., Valencia A. Analysis of Economic and Business Factors Influencing Disruptive Innovation in Telehealth. Nova. 2017;15:125–136. doi: 10.22490/24629448.2136. [DOI] [Google Scholar]
- 29.Alsheddi A., Sharma D., Talukder M. Investigating the Determinants of Innovation Adoption in Saudi Arabia. Int. Rev. Bus. Res. Pap. 2019;15:37–59. doi: 10.21102/irbrp.2019.03.151.03. [DOI] [Google Scholar]
- 30.Adams L., Lester S., Hoon E., van der Haak H., Proudman C., Hall C., Whittle S., Proudman S., Hill C.L. Patient satisfaction and acceptability with telehealth at specialist medical outpatient clinics during the COVID-19 pandemic in Australia. Intern. Med. J. 2021;51:1028–1037. doi: 10.1111/imj.15205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scott R., Mars M. Telehealth in the developing world: Current status and future prospects. Smart Homecare Technol. TeleHealth. 2015;3:25–37. doi: 10.2147/SHTT.S75184. [DOI] [Google Scholar]
- 32.Zhang X., Zaman B.U. Adoption mechanism of telemedicine in underdeveloped country. Health Inform. J. 2020;26:1088–1103. doi: 10.1177/1460458219868353. [DOI] [PubMed] [Google Scholar]
- 33.Mittal S., Mehar M. Socio-economic Factors Affecting Adoption of Modern Information and Communication Technology by Farmers in India: Analysis Using Multivariate Probit Model. J. Agric. Educ. Ext. 2016;22:199–212. doi: 10.1080/1389224X.2014.997255. [DOI] [Google Scholar]
- 34.Lam K., Lu A.D., Shi Y., Covinsky K.E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern. Med. 2020;180:1389–1391. doi: 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Orrange S., Patel A., Mack W.J., Cassetta J. Patient Satisfaction and Trust in Telemedicine During the COVID-19 Pandemic: Retrospective Observational Study. JMIR Hum. Factors. 2021;8:e28589. doi: 10.2196/28589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.UN International Day of Older Persons. [(accessed on 20 October 2021)]. Available online: https://www.un.org/en/observances/older-persons-day.
- 37.Raghupathi V., Raghupathi W. The influence of education on health: An empirical assessment of OECD countries for the period 1995–2015. Arch. Public Health. 2020;78:20. doi: 10.1186/s13690-020-00402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alhajri N., Simsekler M.C.E., Alfalasi B., Alhashmi M., AlGhatrif M., Balalaa N., Al Ali M., Almaashari R., Al Memari S., Al Hosani F., et al. Physicians’ Attitudes Toward Telemedicine Consultations During the COVID-19 Pandemic: Cross-sectional Study. JMIR Med. Inf. 2021;9:e29251. doi: 10.2196/29251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weißenfeld M.M., Goetz K., Steinhäuser J. Facilitators and barriers for the implementation of telemedicine from a local government point of view—A cross-sectional survey in Germany. BMC Health Serv. Res. 2021;21:919. doi: 10.1186/s12913-021-06929-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Andrews E., Berghofer K., Long J., Prescott A., Caboral-Stevens M. Satisfaction with the use of telehealth during COVID-19: An integrative review. Int. J. Nurs. Stud. Adv. 2020;2:100008. doi: 10.1016/j.ijnsa.2020.100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.