Abstract
Objective:
Suicidal individuals are a heterogeneous population and may differ in systematic ways in their responsiveness to stress. The primary aim of the present study was to identify whether a different pattern of physiological stress response exists among adult suicide attempters with a history of behavioral problems during childhood and adolescence, which earlier studies have related to both decreased activity of the HPA axis and to suicidal behaviors.
Method:
Seventy-eight participants with Borderline Personality Disorder were assessed using the SCID-II, and completed self-report measures assessing their history of suicide attempts, history of aggressive behaviors, depressive symptoms, history of lifetime abuse and demographics. Participants’ cortisol reactivity was assessed using the Trier Social Stress Test.
Results:
Analyses indicated that suicide attempters with a history of behavioral problems in youth (n=30) had a significantly lower response to stress than both suicide attempters without such a history (n=26) and non-attempters (n=22), when controlling for lifetime history of abuse. The groups did not differ in basal cortisol.
Conclusions:
These findings suggest a unique subtype of suicide attempter among those with Borderline Personality Disorder, characterized by a blunted physiological stress response.
Keywords: Suicidal behavior, Aggression, Behavioral problems, Cortisol, Borderline Personality Disorder
Introduction
Suicide is one of the leading causes of death in the United States (Kochanek, Murphy, Xu, & Tejada-Vera, 2016), claiming 47,173 lives in 2017 alone (Center for Disease Control and Prevention, 2017). However, identifying risk factors for suicide can be problematic, given that suicidal individuals often have different psychiatric diagnoses (Oquendo, Baca-García, Mann, & Giner, 2008) and vulnerability factors may differ significantly from one individual to another (Carballo, Akamnonu, & Oquendo, 2008). For example, patterns of dysregulation of the Hypothalamic-Pituitary-Adrenal (HPA) axis, one of the central neurobiological mechanisms associated with suicidal behavior (Mann & Currier, 2007; Melhem et al., 2017; Oquendo et al., 2014), seem to differ among suicidal individuals. Previous research has yielded inconsistent results, with several studies reporting that individuals with suicidal thoughts and behaviors show hyperactivity of the HPA axis (e.g., Coryell & Schlesser, 2001; Giletta et al., 2015), while other studies report the opposite (O’Connor, Green, Ferguson, O’Carroll, & O’Connor, 2017). Additionally, some researchers observed differences between attempters and non-attempters only in basal cortisol and not in cortisol response to stress (Melhem et al., 2016).
One explanation for these inconsistencies may be the existence of subtypes of suicide attempters, potentially related to different patterns of HPA axis activity (Bernanke, Stanley, & Oquendo, 2017). The human stress system is affected by both genetic and environmental factors (Chrousos, & Gold, 1992; Tackett, Krueger, Iacono, & McGue, 2005). Exposure to stress via aggression or dangerous situations (as a victim or perpetrator) that results in arousal can lead to dysregulation of the stress response system in childhood, adolescence (e.g., Jaffee et al., 2015), or adulthood (Carpenter, Shattuck, Tyrka, Geracioti, & Price, 2011). Such dysregulation may affect the processes that lead to suicidal behavior.
A history of disruptive conduct and behavioral problems during childhood and adolescence may have bearing on HPA axis activity. Studies conducted with children and adolescents have found that those with behavioral problems have lower basal cortisol levels and lower responses to stress as measured by salivary cortisol (McBurnett, Lahey, Rathouz, & Loeber, 2000; Stadler et al., 2011). The latter has been theorized to at least partially result from a cycle encompassing a “fearless stance,” stimulation-seeking, and habituation of the HPA axis following consistent and repeated exposure to stressful situations (Eysenck, 1964; Quay, 1965; Raine, 2013).
Given the contradictory findings regarding HPA axis activity and suicidal behavior, a better understanding of the relationship between cortisol response and suicidal behavior is needed. To our knowledge, no studies have explored a history of behavioral problems and HPA axis activity among suicidal individuals. Therefore, the central aim of the present study was to explore whether suicide attempters with a history of severe behavioral problems in youth (defined here as having problems involving the law/police or hurting someone with a weapon), present with blunted HPA axis activity, compared to both attempters without such history and non-attempters.
This study was conducted within a sample of patients with Borderline Personality Disorder (BPD), a group at high risk for suicide, with suicide attempt rates ranging as high as 75% and suicide deaths rates of approximately 10% (Goodman et al., 2017; Zanarini et al., 2008). Although individuals with BPD share the same diagnosis, there is heterogeneity in the nature of their suicidal behavior when different cohorts are compared (Pompili, Girardi, Ruberto, & Tatarelli, 2005).
Methods
Participants and Procedures
Eighty-four participants were recruited for this study. All participants met criteria for BPD and had a history of a suicide-related behavior or non-suicidal self-injury (NSSI), with continued suicidal ideation or urges to self-injure. Participants were recruited through medical professionals in the New York metropolitan area, newspaper advertisements, and websites. Participants were initially screened over the phone, and later in person, by two doctoral-level clinicians to determine whether they met study inclusion criteria. Exclusion criteria included bipolar I disorder, schizophrenia, delusional disorder, schizophreniform disorder, schizoaffective disorder, psychotic disorder not otherwise specified, intellectual disability, and conditions that required primary treatment (such as severe anorexia or severe primary substance use that could not be managed in an outpatient program). Participants were recruited as part of a six-month treatment study, and only their baseline data were analyzed in the present study. After a complete description of the study was provided, written informed consent was obtained from all participants. The study protocol was approved by the Institutional Review Board at the New York State Psychiatric Institute.
HPA activity assessment
Trier Social Stress Test (TSST).
Measurements of basal cortisol and cortisol reactivity were collected using the TSST, a valid and reliable protocol used to induce moderate psychosocial stress, with associated HPA axis and autonomic nervous system arousal, in laboratory settings (Kirschbaum, Pirke, & Hellhammer, 1993; Dickerson & Kemeny, 2004, for a review). The TSST protocol consisted of a three-minute preparatory period, a five-minute speech, and a ten-minute mental arithmetic task. Participants were instructed to fast beginning two hours prior to the procedure. The TSST required one hour to complete and was administered between 1 p.m. and 4 p.m. to minimize cortisol variability as a result of the time of day. Saliva samples were collected before and at fixed time points after the stress-inducing procedures. A total of five saliva samples per participant were collected serially, one at baseline and four following the administration of the stress procedure (15, 20, 30, and 40 minutes). All cortisol levels were natural log-transformed before further calculations. Three measures of cortisol activity were measured: basal cortisol, peak cortisol change (defined as the difference between the highest cortisol level obtained in the measurement following the stress task and the baseline level), and Area Under the Curve (AUC) with respect to baseline. All three measures were graphed and inspected for outlier values, and outliers were winsorized to the nearest non-outlier value. Six of the 84 subjects had all cortisol data missing and were not included in any analyses.
Clinical assessment
All participants completed an assessment with a doctoral-level psychologist at the start of the study.
The Structural Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM) Axis II disorders (SCID-II; First et al, 1997), a diagnostic structured clinical interview for Axis II personality disorders, based on DSM-IV (1994) criteria, was used to obtain diagnostic information for BPD.
The Columbia Suicide History Form (CSHF; Oquendo et al., 2003), a semi-structured instrument that asks about lifetime suicide attempts, including the method used, lethality of attempt, precipitants, and circumstances surrounding the attempt, was used to record history of suicide attempt(s). A suicide attempt was defined as “an intentional self-injurious act performed with at least some intent to die.”
The Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996), a 21-item multiple choice self-report questionnaire, was used to measure depressive symptoms experienced in the prior two weeks. The BDI is one of the most widely used measures of depression severity. In the current study it evinced good internal reliability (α=.885).
The Brown-Goodwin Lifetime History of Aggression (BGHA; Brown & Goodwin, 1986) is a 33-item assessment scale of lifetime aggressive behaviors. In the current study, the scale was administered in an interview. The participant was asked about the frequency of 11 aggression-related behaviors during childhood, adolescence, and adulthood on a four-point scale (from “never” to “often”). The BGHA was used in the current study to assess for history of significant behavioral problems in childhood and adolescence using six items: (1) trouble with the police during childhood / (2) during adolescence, (3) trouble with the law during childhood / (4) during adolescence and (5) history of hurting someone with a weapon as a child / (6) as an adolescent. Participants who responded affirmatively to any of these six items (any answer other than never) were considered positive for behavioral problems. Because we wanted to evaluate whether aggression in adulthood was a confounding factor, we used this scale to create a variable of aggression history in adulthood – a continuous variable that captures aggression severity (summing the scores of all 11 behaviors in adulthood).
Participants were also interviewed using a psychiatric history and demographic form to assess abuse history (via an item asking whether the participant had been physically or sexually abused) and demographic information. Height and weight (for calculation of BMI), smoking status and psychotropic medication status were also assessed in an interview with the same form.
Statistical Analysis
First, participants were divided into three groups: 1) non-attempters (n=22), 2) suicide attempters with a history of behavioral problems (attempters-B; n=30), and 3) attempters with no history of behavioral problems (attempters-NB; n=26). We did not divide the non-attempter group by behavioral problems as this group was small (n=22) and dividing it would lead to diminished statistical power. In preliminary analyses, we evaluated possible confounding variables of the above predictors, such as age, sex, ethnicity, race, depressive symptoms, BMI, smoking status, psychotropic medication status and aggression history in adulthood, in comparisons among the study groups using one-way ANOVAs and chi-square tests. Then, to evaluate the relationship between attempt (solely) and cortisol response, we conducted three t-test analyses, for basal cortisol, peak cortisol level and AUC. In the main analyses, differences in the three cortisol measures among the three groups were assessed using two-way ANOVA models and a Generalized Least Square model. Having a history of lifetime sexual or physical abuse (yes/no) was entered into the analyses as an additive covariate of the 3-level group variable, with no interaction term. For post-hoc tests, we used t-tests with Bonferroni correction.
Results
Sample Description
Participants (n=78) were predominantly women (92.3%), ranging in age from 18 to 62 (M=29.55, SD=9.70). Most participants (57.7%) were Caucasian. Twenty-three percent of the sample was of Hispanic/Latino origin. Mean total education was 15.32 (SD=2.05). Seventy-six percent of the participants identified as single, 16% separated/divorced and 8% married.
Preliminary Analyses
Results of the three t-tests comparing the three cortisol measures between attempters and non-attempters were non-significant (Basal: t=−1.59, df=76, p=.114; AUC: t=−1.75, df=75, p=.084; Peak cortisol level: t=−1.59, df=76, p=.115). As demonstrated in Table 1, group comparisons showed no differences in any of the potentially confounding factors, except for BMI, that differed within the behavioral-problems-based groups. However, when we assessed its correlation with cortisol measures it was non-significant (p=.065−.099) and therefore we did not include it as a covariate.
Table 1.
Between groups comparisons
| Non-attempters | Attempters - behavioral problems | Attempters – no behavioral problems | Statistics | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | F | df | p | |
| Age | 22 | 28.59 | 6.41 | 30 | 28.63 | 11.48 | 26 | 31.42 | 9.84 | .72 | 2, 75 | .490 |
| BMI | 22 | 24.14 | 6.28 | 30 | 22.85 | 5.70 | 26 | 27.71 | 7.96 | 3.83 | 2, 75 | .026 |
| BDI | 19 | 25.53 | 8.75 | 28 | 30.75 | 10.75 | 24 | 27.58 | 11.67 | 1.45 | 2, 68 | .241 |
| Aggression in adulthood | 22 | 17.59 | 4.01 | 30 | 17.83 | 3.59 | 26 | 15.96 | 3.59 | 1.99 | 2, 75 | .144 |
| N | N with characteristics | % | N | N with characteristics | % | N | N with characteristics | % | X2 | df | p | |
| Sex (females) | 22 | 20 | 90.9 | 30 | 29 | 96.7 | 26 | 23 | 88.5 | 1.53^ | 2 | .568 |
| Race (white) | 22 | 12 | 54.5 | 30 | 16 | 53.3 | 26 | 17 | 65.4 | .95 | 2 | .621 |
| Ethnicity (Hispanic) | 22 | 4 | 18.2 | 30 | 7 | 23.3 | 26 | 7 | 26.9 | .54^ | 2 | .704 |
| Tobacco use | 22 | 9 | 40.9 | 30 | 11 | 36.7 | 26 | 5 | 19.2 | 3.09^ | 2 | .213 |
| Psych med status | 21 | 11 | 52.4 | 29 | 18 | 62.1 | 25 | 16 | 64 | .726 | 2 | 695 |
Cortisol Measures
Between group comparisons on basal cortisol, while controlling for lifetime abuse status, showed non-significant group differences (F(2, 74)=1.72, p=.186), and non-significant effect of abuse (F(1, 74)=.91, p=.343).
When the groups were compared on AUC, differences emerged (F(2)=7.67, p=.001), with the Attempters-B group showing lower cortisol response than the Attempters-NB (M difference=−11.98, SE=3.47, p=.003), and than the Non-attempters (M difference= −11.46 SE=3.60, p=.007), while the differences between the Attempters-NB and Non-attempters were non-significant (M difference= .51, SE=3.03, p=1). The effect of abuse status on AUC was non-significant (F(1)=.00, p=.997).
Group differences emerged also on peak cortisol response (F(2)=8.98, p<.001), with the Attempters-B group showing lower peak cortisol response than the Attempters-NB (M difference=−.38, SE=.11, t=3.45, p=.003), and than the Non-attempters (M difference=−.36, SE=.12, t=3.03, p=.010), while the differences between the Attempters-NB and Non-attempters were non-significant (M difference=−.02, SE=.15, t=.15, p=.880). The effect of abuse on peak cortisol response was non-significant (F(1)=.05, p=.818).
Discussion
The present study sought to explore whether suicide attempters with Borderline Personality Disorder and with a history of severe behavioral problems in youth, had alterations in cortisol response that distinguish them from other suicide attempters and from non-attempters. Our results revealed that BPD suicide attempters with a history of behavioral problems had a significantly lower response to stress than both suicide attempters without such a history and non-attempters, when measured via AUC and peak cortisol response. The groups did not differ in their basal cortisol levels, suggesting that it is their immediate response to stress that differed. These results have two important implications; first, it confirms the notion of the existence of distinct subtypes of suicide attempters, and second, it points to a possible physiological mechanism of the childhood disruptive behaviors – suicidal behavior link.
The differences in cortisol response to social stress between the attempter groups support the notion that there are distinct subtypes of suicide attempters characterized by a different physiological response to stress (Bernanke et al., 2017). These two subtypes appear to be definable by their past history of problematic behavior, a factor known to be related to the stress response system. Blunted cortisol response has been related to maladaptive emotional and behavioral reactions to threat, and to externalizing behaviors in former studies (e.g., Hartman, Hermanns, de Jong, & Ormel, 2013; Quellet-Morin et al., 2011).
Several studies, in turn, have found a link between childhood disruptive disorders and suicidal behavior (e.g., Brent et al., 1993). In a large sample of youth with and without conduct disorder, the former were significantly more likely to attempt suicide prospectively, and to attempt suicide in an earlier age (Wei et al, 2016). The present study’s findings that a lack of stress reactivity is associated with suicide attempters with history of behavioral problems suggest a possible physiological substrate to this connection. The casual mechanisms underlying this association, though, are unclear.
We found no differences among the groups in baseline cortisol. This finding is not consistent with prior studies that found lower basal cortisol in suicide attempters (Keilp et al., 2016; McGirr, Diaconu, Berlim, & Turecki, 2011; Melhem et al., 2016). However, there are a number of differences between these studies and the study reported here. Previous studies’ populations consisted of patients with major depressive disorder (MDD) as well as offspring of MDD probands, and history of prior behavior problems was not characterized. The current study was conducted within a population of individuals with BPD and stratified for the existence of early behavior problems. It is also important to note that all participants here were deemed to be at current high risk for suicidal behavior, endorsing either suicidal ideation or an urge to injure oneself, which attenuated the range of these behaviors and perhaps affected our ability to detect differences.
The current study has several limitations. First, the study sample was comprised of individuals with BPD only, most of them females, limiting the ability to generalize these findings to other populations. Furthermore, the composition of the study sample (i.e., mostly female) may have affected our ability to detect the effect of sex on study variables. Second, the relatively small size of the groups limits its statistical power. Third, groups were defined on the basis of self-report of prior behavior problems that may have been affected by current clinical state or inconsistent recollection. Similarly, other variables, such as BMI and childhood abuse, also relied on self-report measures. Fourth, the study is a secondary analysis of a dataset from a baseline assessment of a treatment study, and therefore, abuse was defined using only one item, and having a behavioral problems history was defined using items from the Brown-Goodwin Lifetime History of Aggression rather than from a measure that was designed to assess behavioral problems. Despite these limitations, this study provides a basis for understanding some of the inconsistencies in the literature regarding differences between attempters and non-attempters in the dysregulation of the stress response system. In addition, it provides support for the notion of subtypes among suicidal individuals, who may require different approaches to risk assessment and treatment. Certain aspects of behavioral history may have a profound effect on current responses to stress, and their contribution to suicidal behavior risk. Suicide prevention interventions with individuals who have such behavioral history and a relatively blunted stress response may be improved by targeting these individuals’ lack of sensitivity to threat and danger, as well as their self-preservation. However, to provide further empirical support for this notion and to better inform therapeutic interventions in other diagnostic populations, future studies should extend the approach taken in this study to other populations at high risk for suicidal behavior.
Figure 1.
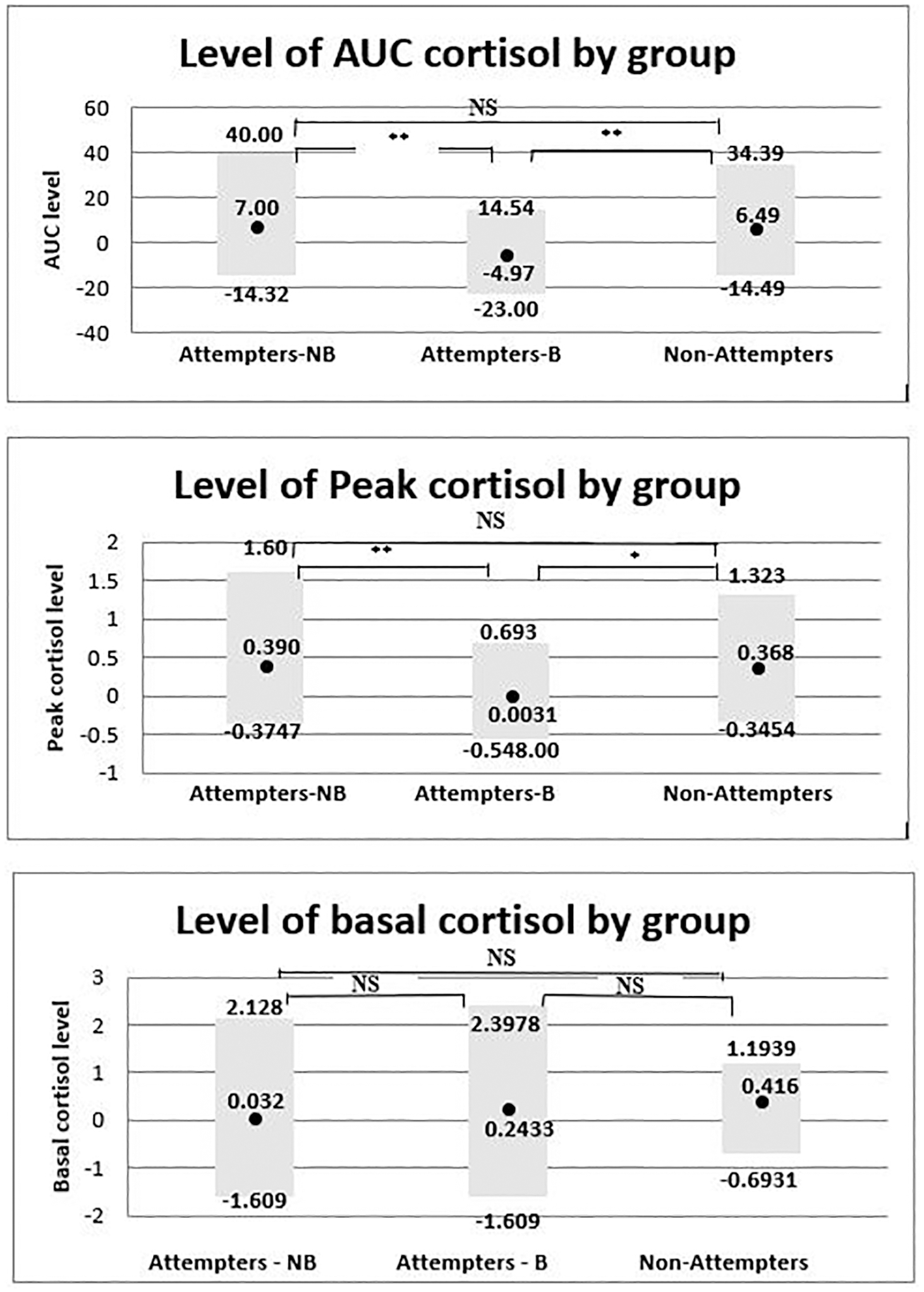
Basal, Peak cortisol and AUC cortisol levels range and average among the three behavioral problems/attempt related groups.
Note: *=p<.05, **=p<.01
Biographical note:
Liat Itzhaky, PhD, John Keilp, PhD, Ilana Gratch, BA, Beth Brodsky, PhD, and Barbara Stanley, PhD, are affiliated with Molecular Imaging and Neuropathology Division, New York State Psychiatric Institute, New York, NY, and Department of Psychiatry, Columbia University, New York, NY. Hanga Galfalvy, PhD, is affiliated with Division of Biostatistics, New York State Psychiatric Institute, New York, NY, and Department of Psychiatry, Columbia University, New York, NY.
References
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: Author. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78(2), 490–8. [Google Scholar]
- Bernanke JA, Stanley BH, & Oquendo MA (2017). Toward fine-grained phenotyping of suicidal behavior: the role of suicidal subtypes. Molecular Psychiatry. doi: 10.1038/mp.2017.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend AMY, Roth C, … & Baugher M (1993). Psychiatric risk factors for adolescent suicide: a case-control study. Journal of the American Academy of Child & Adolescent Psychiatry, 32(3), 521–529. [DOI] [PubMed] [Google Scholar]
- Brown GL & Goodwin FK (1986). Human aggression and suicide. Suicide and Life-Threatening Behaviors, 16(2), 223–243. [DOI] [PubMed] [Google Scholar]
- Carballo JJ, Akamnonu CP, & Oquendo MA (2008). Neurobiology of suicidal behavior. An integration of biological and clinical findings. Archives of Suicide Research, 12(2), 93–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter LL, Shattuck TT, Tyrka AR, Geracioti TD, & Price LH (2011). Effect of childhood physical abuse on cortisol stress response. Psychopharmacology, 214(1), 367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Injury prevention & control: Data & statistics (WISQARS). https://www.cdc.gov/injury/wisqars/. Accessed August 15, 2018.
- Chrousos GP, & Gold PW (1992). The concepts of stress and stress system disorders: overview of physical and behavioral homeostasis. JAMA, 267(9), 1244–1252. [PubMed] [Google Scholar]
- Coryell W, & Schlesser M (2001). The dexamethasone suppression test and suicide prediction. American Journal of Psychiatry, 158(5), 748–753. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, & Kemeny ME (2004). Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychological bulletin, 130(3), 355. [DOI] [PubMed] [Google Scholar]
- Eysenck H (1964). Crime and personality. London: Methuen. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J, & Benjamin L (1997). Structural Clinical Interview for DSM-IV Axis II personality disorders (SCID-II). Washington, DC: American Psychiatric Press. [Google Scholar]
- Giletta M, Calhoun CD, Hastings PD, Rudolph KD, Nock MK, & Prinstein MJ (2015). Multi-level risk factors for suicidal ideation among at-risk adolescent females: the role of hypothalamic-pituitary-adrenal axis responses to stress. Journal of abnormal child psychology, 43(5), 807–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman M, Tomas IA, Temes CM, Fitzmaurice GM, Aguirre BA, & Zanarini MC (2017). Suicide attempts and self‐injurious behaviours in adolescent and adult patients with borderline personality disorder. Personality and mental health, 11(3), 157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman CA, Hermanns VW, de Jong PJ, & Ormel J (2013). Self-or parent report of (co-occurring) internalizing and externalizing problems, and basal or reactivity measures of HPA-axis functioning: A systematic evaluation of the internalizing-hyperresponsivity versus externalizing-hyporesponsivity HPA-axis hypothesis. Biological psychology, 94(1), 175–184. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, McFarquhar T, Stevens S, Ouellet‐Morin I, Melhuish E, & Belsky J (2015). Interactive effects of early and recent exposure to stressful contexts on cortisol reactivity in middle childhood. Journal of Child Psychology and Psychiatry, 56(2), 138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilp JG, Stanley BH, Beers SR, Melhem NM, Burke AK, Cooper TB, … & Mann JJ (2016). Further evidence of low baseline cortisol levels in suicide attempters. Journal of affective disorders, 190, 187–192. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, & Hellhammer DH (1993). The ‘Trier Social Stress Test’–a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology, 28(1–2), 76–81. [DOI] [PubMed] [Google Scholar]
- Kochanek, Murphy, Xu, &Tejada-Vera. (2016). Deaths: final data for 2014. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 65(4), 1–122. [PubMed] [Google Scholar]
- Mann JJ, & Currier D (2007). A review of prospective studies of biologic predictors of suicidal behavior in mood disorders. Archives of Suicide Research, 11(1), 3–16. [DOI] [PubMed] [Google Scholar]
- McBurnett K, Lahey BB, Rathouz PJ, & Loeber R (2000). Low salivary cortisol and persistent aggression in boys referred for disruptive behavior. Archives of General Psychiatry, 57(1), 38–43. [DOI] [PubMed] [Google Scholar]
- McGirr A, Diaconu G, Berlim MT, & Turecki G (2011). Personal and family history of suicidal behaviour is associated with lower peripheral cortisol in depressed outpatients. Journal of affective disorders, 131(1), 368–373. [DOI] [PubMed] [Google Scholar]
- Melhem NM, Keilp JG, Porta G, Oquendo MA, Burke A, Stanley B, … & Brent DA (2016). Blunted HPA axis activity in suicide attempters compared to those at high risk for suicidal behavior. Neuropsychopharmacology, 41(6), 1447–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melhem NM, Munroe S, Marsland A, Gray K, Brent D, Porta G, … & Driscoll H (2017). Blunted HPA axis activity prior to suicide attempt and increased inflammation in attempters. Psychoneuroendocrinology, 77, 284–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor DB, Green JA, Ferguson E, O’Carroll RE, & O’Connor RC (2017). Cortisol reactivity and suicidal behavior: investigating the role of hypothalamic-pituitary-adrenal axis responses to stress in suicide attempters and ideators. Psychoneuroendocrinology, 75, 183–191. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Baca-García E, Mann JJ, Giner J (2008). Issues for DSM-V: suicidal behavior as a separate diagnosis on a separate axis. American Journal of Psychiatry, 165, 1383–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Halberstam B, & Mann JJ (2003). Risk factors for suicidal behavior. Standardized evaluation in clinical practice, 22, 103–129. [Google Scholar]
- Oquendo MA, Sullivan GM, Sudol K, Baca-Garcia E, Stanley BH, Sublette ME, & Mann JJ (2014). Toward a biosignature for suicide. American Journal of Psychiatry, 171(12), 1259–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouellet-Morin I, Odgers CL, Danese A, Bowes L, Shakoor S, Papadopoulos AS, … & Arseneault L (2011). Blunted cortisol responses to stress signal social and behavioral problems among maltreated/bullied 12-year-old children. Biological psychiatry, 70(11), 1016–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompili M, Girardi P, Ruberto A, & Tatarelli R (2005). Suicide in borderline personality disorder: a meta-analysis. Nordic journal of psychiatry, 59(5), 319–324. [DOI] [PubMed] [Google Scholar]
- Quay HC (1965). Psychopathic personality as pathological stimulation-seeking. American Journal of Psychiatry, 122, 180–183. [DOI] [PubMed] [Google Scholar]
- Raine A (2013). The psychopathology of crime: Criminal behavior as a clinical disorder. San Diego: Academic Press, Inc. [Google Scholar]
- Stadler C, Kroeger A, Weyers P, Grasmann D, Horschinek M, Freitag C, & Clement HW (2011). Cortisol reactivity in boys with attention-deficit/hyperactivity disorder and disruptive behavior problems: the impact of callous unemotional traits. Psychiatry research, 187(1), 204–209. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Krueger RF, Iacono WG, & McGue M (2005). Symptom-based subfactors of DSM-defined conduct disorder: Evidence for etiologic distinctions. Journal of abnormal psychology, 114(3), 483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei HT, Lan WH, Hsu JW, Bai YM, Huang KL, Su TP, … & Chen MH (2016). Risk of suicide attempt among adolescents with conduct disorder: a longitudinal follow-up study. The Journal of pediatrics, 177, 292–296. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G, Weinberg I, & Gunderson JG (2008). The 10‐year course of physically self‐destructive acts reported by borderline patients and axis II comparison subjects. Acta Psychiatrica Scandinavica, 117(3), 177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]


