Abstract
Objective
To investigate the effects of one and two doses of intravenous dexamethasone in patients after total knee arthroplasty.
Design
Randomised, blinded, placebo controlled trial with follow-up at 90 days.
Setting
Five Danish hospitals, September 2018 to March 2020.
Participants
485 adult participants undergoing total knee arthroplasty.
Intervention
A computer generated randomised sequence stratified for site was used to allocate participants to one of three groups: DX1 (dexamethasone (24 mg)+placebo); DX2 (dexamethasone (24 mg)+dexamethasone (24 mg)); or placebo (placebo+placebo). The intervention was given preoperatively and after 24 hours. Participants, investigators, and outcome assessors were blinded. All participants received paracetamol, ibuprofen, and local infiltration analgesia.
Main outcome measures
The primary outcome was total intravenous morphine consumption 0 to 48 hours postoperatively. Multiplicity adjusted threshold for statistical significance was P<0.017 and minimal important difference was 10 mg morphine. Secondary outcomes included postoperative pain.
Results
485 participants were randomised: 161 to DX1, 162 to DX2, and 162 to placebo. Data from 472 participants (97.3%) were included in the primary outcome analysis. The median (interquartile range) morphine consumptions at 0-48 hours were: DX1 37.9 mg (20.7 to 56.7); DX2 35.0 mg (20.6 to 52.0); and placebo 43.0 mg (28.7 to 64.0). Hodges-Lehmann median differences between groups were: −2.7 mg (98.3% confidence interval −9.3 to 3.7), P=0.30 between DX1 and DX2; 7.8 mg (0.7 to 14.7), P=0.008 between DX1 and placebo; and 10.7 mg (4.0 to 17.3), P<0.001 between DX2 and placebo. Postoperative pain was reduced at 24 hours with one dose, and at 48 hours with two doses, of dexamethasone.
Conclusion
Two doses of dexamethasone reduced morphine consumption during 48 hours after total knee arthroplasty and reduced postoperative pain.
Trial registration
Clinicaltrials.gov NCT03506789.
Introduction
Total knee arthroplasty is a common procedure. Worldwide, more than 1 000 000 procedures are performed annually, and with ageing populations this number is expected to increase markedly.1 2 3 The procedure is associated with moderate to severe postoperative pain.4 5
Multimodal analgesic treatment is recommended for management of pain after total joint arthroplasty.6 Dexamethasone is often used as part of this treatment and for treatment of nausea after surgery.7 8 The evidence for the adjuvant analgesic effects of dexamethasone after total knee arthroplasty is of very low certainty, however, as the literature is dominated by small underpowered trials and therefore with risks of bias and random errors.9 10 11 12 The potential analgesic effects of glucocorticoids as an adjuvant are probably due to their anti-inflammatory properties, including suppression of proinflammatory cytokines and induction of anti-inflammatory cytokines, reduction of prostaglandin synthesis, and with possible lowering of the excitability of nerve cells.13 14
We therefore conducted the DEXamethasone twice for pain treatment after Total Knee Arthroplasty (DEX-2-TKA) trial to investigate the potential beneficial and harmful effects of one and two doses of intravenous dexamethasone (24 mg) as an adjuvant treatment to a standard non-opioid analgesic regimen in adults after primary total knee arthroplasty. The dose of dexamethasone 24 mg corresponded to that of previous studies in total knee arthroplasty using a single perioperative dose of methylprednisolone 125 mg.10 15 This trial was supported by a review calling for large trials with higher doses of dexamethasone than used for the treatment of nausea and vomiting, which might improve the treatment of pain.16
Our hypothesis was that 24 mg intravenous dexamethasone as an adjuvant to multimodal pain treatment would reduce postoperative opioid consumption and pain, and that two doses would be better than one.
Methods
Trial design and setting
DEX-2-TKA was a multicentre, randomised, blinded, placebo controlled trial in participants undergoing primary total knee arthroplasty, conducted to investigate the effects of dexamethasone on morphine consumption, levels of postoperative pain, adverse events, and serious adverse events.
Our methodology is described in detail in the protocol article,17 in the protocol available at https://www.appraz.dk, and in the statistical analysis plan.18 The trial was conducted at one private and four public Danish hospitals. Written informed consent was obtained from all participants before enrolment. The trial protocol cohered with the SPIRIT statement and was approved by the Regional Committee on Health Research Ethics, Region Zealand, the Danish Medicines Agency, and the Danish Data Registration Agency. The trial was monitored by the good clinical practice units at Copenhagen and Odense University Hospitals, Denmark. Trial reporting was in alignment with the CONSORT (consolidated standards of reporting trials) 2010 guidelines. We take full responsibility for adherence of the trial to the protocol, accuracy, and completeness of data and analyses, and the reporting of adverse events. Two investigators prepared the trial database independently to secure accuracy of the data. Based on the masked results, agreement was reached by members of the steering committee on six possible final abstracts (27 October 2020), before the group identity of the trial was disclosed.
All participants scheduled for primary, unilateral total knee arthroplasty were screened for enrolment. Key exclusion criteria were either contraindications or allergy to the drugs used in the trial. A daily use of opioids up to 30 mg oral morphine equivalents was allowed. Daily use of methadone or use of systemic glucocorticoids within the past three months was not allowed. The full inclusion and exclusion list is provided in eappendix 1.
Intervention
Participants were randomised to one of three intervention groups: DX1 (intravenous dexamethasone (24 mg, 6 mL)+placebo (6 mL saline 0.9%)); DX2 (intravenous dexamethasone (24 mg)+intravenous dexamethasone (24 mg)); or placebo (placebo+placebo), with allocation numbers provided by a web based central database (easytrial.net). The first dose of the trial drugs was administered after onset of spinal or general anaesthesia, and the second dose 24 hours after the end of surgery. Administration of both doses of the drugs was overseen by investigators in the trial.
Randomisation to the three groups in a 1:1:1 ratio was performed by an external trial collaborator, using a computer generated randomised sequence (randomisation.com) with varying block sizes (either three, six, or nine) unknown to the investigators, and with stratification for site. The trial drug was prepared in identical ampoules (efig 1) and was packed and masked by Skanderborg Pharmacy, Denmark. Participants, staff, investigators, surgeons, outcome assessors, statisticians, and those drawing conclusions were blinded to the intervention.17
The type of total knee arthroplasty and surgery was decided solely by the surgeon (16 surgeons, including all sites), and inserted components were either cemented, cement less, or hybrid. All sites used a standard medial parapatellar approach, no standard use of surgical drainage, and started early mobilisation of patients within six hours after surgery. All patients received 1 g of tranexamic acid perioperatively. Participants received spinal (preferred) or general anaesthesia. For spinal anaesthesia, bupivacaine heavy 10-15 mg was used and combined with propofol infusion if sedation was needed. For general anaesthesia, propofol and remifentanil were preferred, and at the end of surgery intravenous sufentanil (0.3 μg/kg) was administered.
All participants were provided with a patient controlled analgesia pump (morphine 1 mg/mL, bolus 2 mg, lock out six minutes, no background infusion) for 24 hours postoperatively. Additional boluses of 2 mg morphine, if requested by the participant, were allowed in the first hour after stopping anaesthesia. During the following 24 to 48 hours the participants had access, on demand, to 10 mg oral morphine tablets. Any other opioid administered during the first 48 hours postoperatively (owing to a mistake, malfunction of the morphine pump, or other circumstances) was converted to intravenous morphine equivalent dose (etable 1) and added to the total intravenous morphine consumption for the primary outcome.17
All participants received a non-opioid pain alleviation regimen according to the protocol, which comprised oral paracetamol 1 g and ibuprofen 400 mg given one hour before, and every six hours after, surgery. In addition, the surgeon injected local infiltration analgesia with 150 mL ropivacaine 1.333 mg/mL into the rear and front capsule, intra-articularly according to a standardised regimen.17 Peripheral regional anaesthesia and any non-protocolised pain medication were not allowed. Treatment that had started before admittance to hospital, with morphine, oxycodone, tramadol, gabapentinoids, or selective serotonin reuptake inhibitors, was continued. These habitually used opioids were not included in the primary outcome.
Outcomes
The primary outcome was total opioid consumption in milligrams of intravenous morphine equivalents 0-48 hours after the end of surgery. Secondary outcomes were levels of pain intensity measured using a visual analogue scale at 24 and 48 hours (score range: 0 mm (no pain) to 100 mm (worst pain imaginable)) during 45° flexion of the knee, at rest, and the highest level of pain experienced during the past 24 hours; and adverse events during 0-24 and 24-48 hours.17
Explorative outcomes were serious adverse events within 90 days (defined according to the International Council for Harmonisation good clinical practice guidelines,19 except “prolongation of stay in hospital”); levels of nausea, sedation, and dizziness reported by participants at 24 and 48 hours (none v mild, moderate, or severe); and number of vomiting episodes, and use of additional antiemetic agents (ondansetron and droperidol) in the periods 0-24 and 24-48 hours.17
Additional explorative outcomes are reported in etable2: total opioid consumption in milligrams of intravenous morphine equivalents 0-24 and 24-48 hours after the end of surgery; pain intensity levels (visual analogue scale) during 45° flexion of the knee, and at rest at six hours; levels of nausea, sedation, and dizziness reported by participants at six hours (none v mild, moderate, or severe); at 24 and 48 hours, the average level of pain experienced during the past 24 hours; quality of sleep assessed at 24 and 48 hours (very/fairly good v fairly/very bad); level of fatigue reported by participants at 24 and 48 hours (none v mild, moderate, or severe); and time for, and maximum pain during, “timed up and go” test at 24 hours. We, furthermore, performed a post hoc analysis to show the level of patient acceptable pain state (visual analogue scale ≤33 mm) in the different trial groups (etable 5).20
The exploratory outcomes—namely, a questionnaire on pain, sleep, and overall satisfaction for postoperative days 3‐7; and the Oxford knee score and EQ-5D-5L at 90 days and one year, will be published elsewhere as separate publications.
Statistical analysis
Because three intervention groups were included, we used an α of 0.0167 (Bonferroni correction; two sided) in the sample size calculation. Hence we predefined our sample size as 486 participants (including a surplus of 15% to take into account the presumed non-normally distributed data) to detect or reject a group difference of 10 mg of intravenous morphine with 90% power.17
We predefined 10 mg of intravenous morphine as minimal important difference, corresponding to a 22% reduction in morphine consumption based on unpublished clinical data from a sample of 46 patients at Næstved Hospital using mean (standard deviation) 45.0 (22.7) mg intravenous morphine.17 A minimal important difference of 10 mm was predefined for pain intensity levels using a visual analogue scale.20
Statistical analyses were performed by two independent statisticians (JCJ and AKN) who were blinded to the trial group assignments. We conducted the primary analysis in the intention-to-treat population, defined as all randomised participants. Analyses of the primary outcome were performed using the non-parametric van Elteren test as pairwise comparisons of the three groups adjusted for site. Group differences were calculated as Hodges-Lehmann median difference and presented with Bonferroni adjusted 98.3% confidence intervals. It was specified post hoc to report Hodges-Lehmann median differences to quantify the effect size of dexamethasone. We chose to report Hodges-Lehmann confidence intervals rather than bootstrapped confidence intervals because they provide a better description of the uncertainty of the result, together with the predefined van Elteren test for significance. Median differences are presented in the etables 7 and 8.
For all other outcomes, the significance level was a P value of <0.05 and accordingly, with no adjustments for multiplicity in the presentation of confidence intervals. We planned to analyse pain intensity levels using linear regression, but because the predefined underlying assumptions (parametric distribution) behind linear regression were not fulfilled, we analysed these data using the van Elteren test.21 Count data were analysed using the van Elteren test, and dichotomous outcomes were analysed using logistic regression. Stata statistical software version 16.1 was used for all analyses. Further details are provided in the statistical analysis plan.18
Patient and public involvement
A panel of three patients have read and commented on the participant information, and representatives for the public in the ethical committee (elected regional politicians) have ethically approved the trial. We did not further involve patients or patient unions in the design of the trial or analyses. The initiative to conduct this trial was based on the researchers’ clinical experience with patients’ pain and their pain treatment after total knee arthroplasty. Thus generating a need to improve the treatment of patients’ pain.
Results
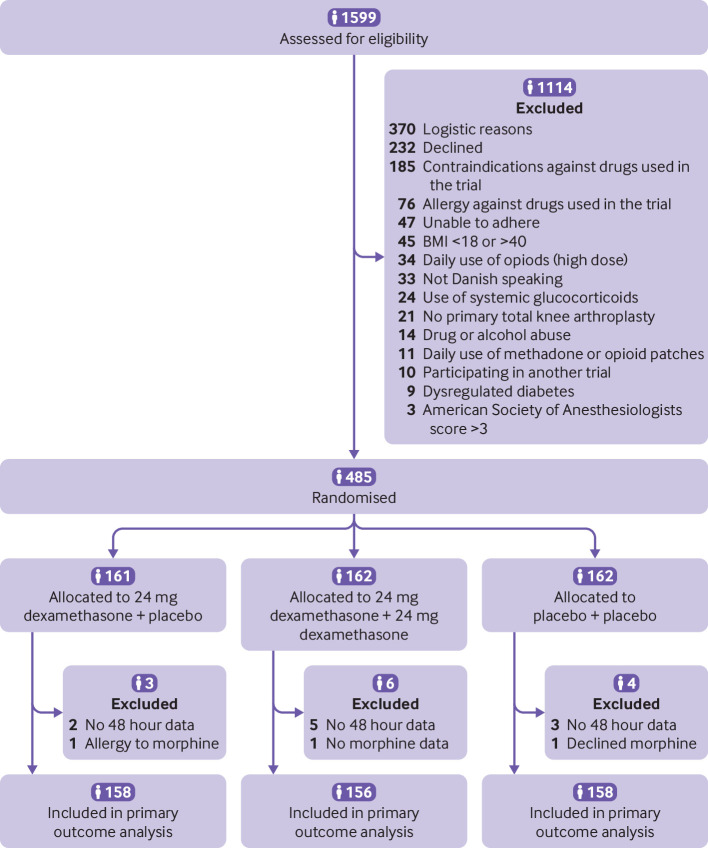
Between 2 October 2018 and 9 March 2020, 485 participants were randomised and included in the intention-to-treat analyses (fig 1). The intervention groups were balanced with respect to baseline data (table 1). The last follow-up data were collected on 7 June 2020. Data completeness was 97.3% for the primary outcome. Missing data are presented in etable 4. According to our statistical analysis plan no imputation was performed.
Fig 1.
Screening, randomisation, and primary outcome population
Table 1.
Patient baseline and perioperative characteristics. Data are number (%) of patients unless stated otherwise
| Intervention group | DX1 (n=161) | DX2 (n=162) | Placebo (n=162) |
|---|---|---|---|
| Baseline characteristics: | |||
| Mean (SD) age (years) | 69 (9) | 67 (9) | 68 (9) |
| Male sex | 80 (50) | 75 (46) | 74 (46) |
| American Society of Anesthesiologists physical status: | |||
| Healthy | 28 (17) | 28 (17) | 19 (12) |
| Mild systemic disease | 102 (63) | 114 (70) | 120 (74) |
| Severe systemic disease | 31 (19) | 20 (12) | 23 (14) |
| Mean (SD) height (cm) | 173 (10) | 172 (9) | 172 (10) |
| Mean (SD) weight (kg) | 86 (17) | 88 (15) | 89 (16) |
| Mean (SD) BMI | 29 (5) | 30 (4) | 30 (4) |
| Type 2 diabetes | 16 (10) | 16 (10) | 17 (10) |
| Insulin treatment | 5 (3) | 3 (2) | 4 (2) |
| Other diabetic treatment | 14 (9) | 14 (9) | 13 (8) |
| Previous daily use (past month) of analgesic drug treatment: | |||
| Paracetamol | 72 (45) | 71 (44) | 75 (46) |
| NSAIDs | 37 (23) | 36 (22) | 38 (23) |
| Gabapentinoids | 3 (2) | 2 (1) | 1 (1) |
| Antidepressants | 4 (2) | 3 (2) | 7 (4) |
| Opioids | 3 (2) | 8 (5) | 5 (3) |
| Morphine | 2 (1) | 5 (3) | 1 (1) |
| Oxycodone | 0 (0) | 1 (1) | 0 (0) |
| Tramadol | 1 (1) | 3 (2) | 4 (2) |
| Median (IQR) amount of opioid used (mg): | |||
| Morphine | 12.5 (11.3-13.8) | 15 (10-20) | 20 (20-20) |
| Oxycodone | NA | 20 | NA |
| Tramadol | 100 (100-100) | 100 (75-125) | 100 (87.5-113) |
| Perioperative characteristics: | |||
| Median (IQR) duration of surgery (min) | 61 (55-71) | 62 (53-73) | 63 (54-71) |
| Type of knee arthroplasty: | |||
| Cemented | 97 (60) | 96 (59) | 94 (58) |
| Cement less | 5 (3) | 2 (1) | 4 (2) |
| Hybrid | 59 (37) | 64 (40) | 64 (40) |
| Type of anaesthesia: | |||
| Spinal | 128 (80) | 131 (81) | 132 (81) |
| General | 30 (19) | 28 (17) | 26 (16) |
| Conversion of spinal to general | 3 (2) | 3 (2) | 4 (2) |
| Mean (SD) amount of sufentanil used if general anaesthesia (μg) | 26.6 (6.1) | 26.2 (4.7) | 27.8 (8.7) |
| Median (IQR) amount of bupivacaine in spinal anaesthesia (mg) | 11 (10-11.5) | 11 (10-12) | 11 (10-12) |
| Median (IQR) intraoperative blood loss (mL)* | 150 (50-250) | 150 (100-200) | 150 (56-250) |
| Administration of 4 mg ondansetron PONV prophylaxis | 140 (87) | 146 (90) | 151 (93) |
| Administration of local infiltration analgesia | 157 (98) | 162 (100) | 161 (99) |
DX1=dexamethasone (24 mg)+placebo; DX2=dexamethasone (24 mg)+dexamethasone (24 mg); IQR=interquartile range; NA=not available; NSAIDs=non-steroidal anti-inflammatory drugs; placebo=placebo+placebo; PONV=postoperative nausea and vomiting; SD=standard deviation.
Intraoperative blood loss was registered at the end of surgery, comprising blood in the suction bottle and gauze.
Primary outcome
Median morphine consumption at 0-48 hours was 37.9 mg (interquartile range 20.7-56.7) in DX1, 35.0 mg (20.6-52.0) in DX2, and 43.0 mg (28.7-64.0) in placebo (table 2 and fig 2). The van Elteren test showed no difference between DX1 and DX2 (Hodges-Lehmann median difference −2.7 mg; 98.3% confidence interval −9.3 to 3.7; P=0.30), but showed a difference between DX1 and placebo (7.8 mg; 0.7 to 14.7, P=0.008), and between DX2 and placebo (10.7 mg; 4.0 to 17.3; P<0.001; table 2). The Hodges-Lehmann median difference reduction of morphine consumption in DX1 compared with placebo was below the predefined minimal important difference, but for reduction of morphine consumption in DX2 compared with placebo was above the predefined minimal important difference. The calculated median difference at a group level between DX2 and placebo was 8 mg, and this difference was below the predefined minimal important difference. All median differences for the primary and secondary outcomes have been calculated and are included in the appendix (etables 7 and 8).
Table 2.
Primary outcome
| Intervention group | DX1 | DX2 | Placebo |
|---|---|---|---|
| Median (IQR) morphine consumption at 0-48 h (mg) | 37.9 (20.7-56.7) | 35.0 (20.6-52.0) | 43.0 (28.7-64.0) |
| DX2 and placebo compared with DX1: | |||
| Difference (98.3% CI), mg | NA | −2.7 (−9.3 to 3.7) | 7.8 (0.7 to 14.7) |
| P value | — | 0.30 | 0.008 |
| Placebo compared with DX2: | |||
| Difference (98.3% CI) mg | NA | NA | 10.7 (4.0 to 17.3) |
| P value | — | — | <0.001 |
DX1=dexamethasone (24 mg)+placebo; DX2=dexamethasone (24 mg)+dexamethasone (24 mg); NA=not available; placebo=placebo+placebo.
Differences between medians are calculated using Hodges-Lehmann. P values are calculated using the van Elteren test.
Fig 2.
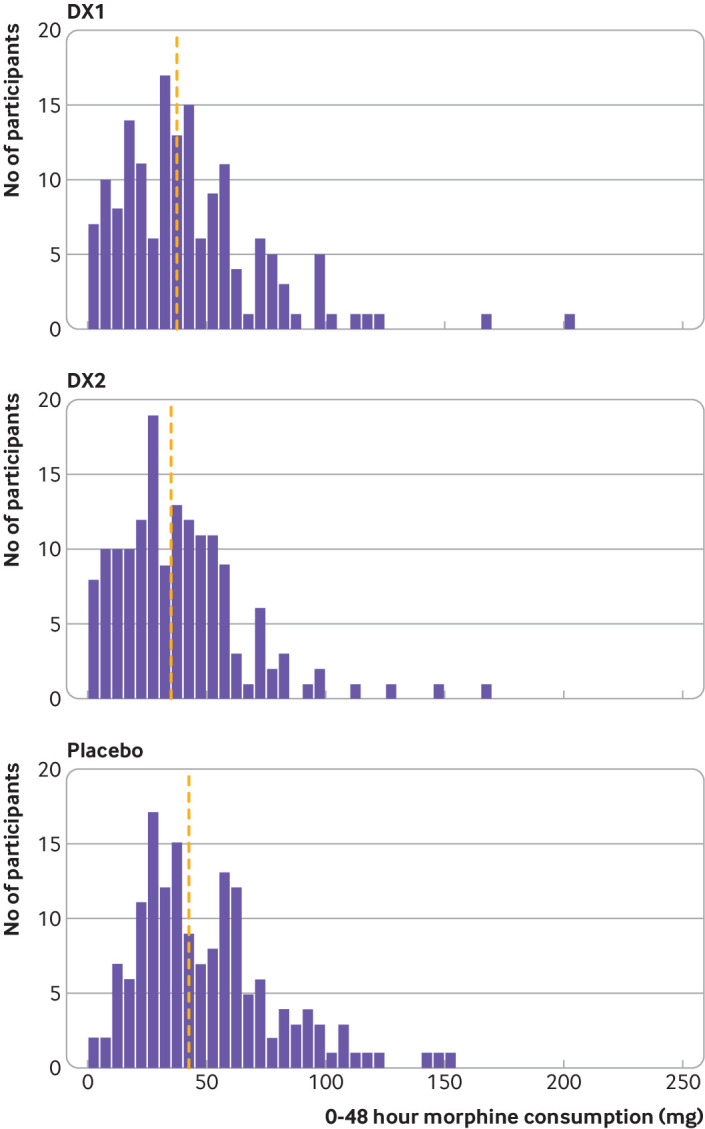
Distribution of morphine consumption according to group 0-48 hours postoperatively. Vertical dashed yellow lines indicate median level of morphine consumption. DX1=dexamethasone (24 mg)+placebo; DX2=dexamethasone (24 mg)+dexamethasone (24 mg); placebo=placebo+placebo
Secondary outcomes
The median pain intensity levels at 24 hours during knee flexion were 50 mm (interquartile range 32-69.5) in DX1, 50 mm (35-68) in DX2, and 60 mm (44-80) in placebo. No difference was found between DX1 and DX2 (table 3). The van Elteren test showed a difference between DX1 and placebo (Hodges-Lehmann median difference 10 mm; 95% confidence interval 4 to 15; P<0.001), and between DX2 and placebo (10 mm; 5 to 15; P<0.001). These reductions of pain in DX1 and DX2 compared with placebo both reached the predefined minimal important difference.
Table 3.
Secondary outcomes. Data are median (interquartile range) unless stated otherwise
| Intervention Group | DX1 | DX2 | Placebo |
|---|---|---|---|
| Pain intensity level; knee flexion at 24 h (mm) | 50 (32-69.5) | 50 (35-68) | 60 (44-80) |
| DX2 and placebo compared with DX1: | |||
| Difference (95% CI), mm | NA | 0 (−5 to 5) | 10 (4 to 15) |
| P value | — | 0.91 | <0.001 |
| Placebo compared with DX2: | |||
| Difference (95% CI), mm | NA | NA | 10 (5 to 15) |
| P value | — | — | <0.001 |
| Pain intensity level at rest at 24 h (mm) | 20 (8-31) | 20 (10-35) | 24.5 (14-45) |
| DX2 and placebo compared with DX1: | |||
| Difference (95% CI), mm | NA | 2 (−1 to 6) | 7 (3 to 11) |
| P value | — | 0.25 | 0.001 |
| Placebo compared with DX2: | |||
| Difference (95% CI), mm | NA | NA | 5 (0 to 10) |
| P value | — | — | 0.031 |
| Level for highest pain intensity 0–24 h (mm) | 70 (50-85) | 69 (50-82) | 80 (66-90) |
| DX2 and placebo compared with DX1: | |||
| Difference (95% CI), mm | NA | 0 (−5 to 5) | 10 (5 to 15) |
| P value | — | 0.81 | <0.001 |
| Placebo compared with DX2: | |||
| Difference (95% CI), mm | NA | NA | 10 (5 to 15) |
| P value | — | — | <0.001 |
| Pain intensity level; knee flexion at 48 h (mm) | 55 (40-70) | 40 (30-50) | 50 (35-63.5) |
| DX2 and placebo compared with DX1: | |||
| Difference (95% CI), mm | NA | −15 (−20 to −10) | −6 (−10 to 0) |
| P value | — | <0.001 | 0.011 |
| Placebo compared with DX2: | |||
| Difference (95% CI), mm | NA | NA | 10 (3 to 11) |
| P value | — | — | 0.003 |
| Pain intensity level at rest at 48 h (mm) | 30 (10-40) | 15 (9-30) | 20 (10-35) |
| DX2 and placebo compared with DX1: | |||
| Difference (95% CI), mm | NA | −10 (−12 to −5) | −3 (−10 to 0) |
| P value | — | <0.001 | 0.01 |
| Placebo compared with DX2: | |||
| Difference (95% CI), mm | NA | NA | 5 (0 to 10) |
| P value | — | — | 0.003 |
| Level for highest pain intensity 24–48 h (mm) | 70 (50-84) | 60 (40-71) | 70 (52-80) |
| DX2 and placebo compared with DX1: | |||
| Difference (95% CI), mm | NA | −10 (−20 to −10) | 0 (−5 to 5) |
| P value | — | <0.001 | 0.89 |
| Placebo compared with DX2: | |||
| Difference (95% CI), mm | NA | NA | 11 (10 to 20) |
| P value | — | — | <0.001 |
| Adverse events 0–48 h, No (%) | 7 (4.3) | 4 (2.5) | 10 (6.2) |
| DX2 and placebo compared with DX1: | |||
| Odds ratio (95% CI) | NA | 0.55 (0.15 to 1.92) | 1.48 (0.53 to 4.09) |
| P value (logistic regression) | — | 0.35 | 0.45 |
| Placebo compared with DX2: | |||
| Odds ratio (95% CI) | NA | NA | 2.75 (0.82 to 9.25) |
| P value (logistic regression) | — | — | 0.10 |
DX1=dexamethasone (24 mg)+placebo; DX2=dexamethasone (24 mg)+dexamethasone (24 mg); NA=not available; placebo=placebo+placebo.
Pain intensity levels as visual analogue scale, 0-100 mm. Differences between medians are calculated using Hodges-Lehmann. P values are calculated using the van Elteren test unless stated otherwise.
The median pain intensity levels at 24 hours at rest were 20 mm (interquartile range 8-31) in DX1, 20 mm (10-35) in DX2, and 24.5 mm (14-45) in placebo. No difference was found between DX1 and DX2. The van Elteren test showed a difference between DX1 and placebo (Hodges-Lehmann median difference 7 mm; 95% confidence interval 3 to 11; P=0.001), and between DX2 and placebo (5 mm; 0 to 10; P=0.031). These reductions of pain in DX1 and DX2 compared with placebo were both below the predefined minimal important difference.
Median levels for highest pain intensity at 0-24 hours were 70 mm (interquartile range 50-85) in DX1, 69 mm (50-82) in DX2, and 80 mm (66-90) in placebo. No difference was found between DX1 and DX2. The van Elteren test showed a difference between DX1 and placebo (Hodges-Lehmann median difference 10 mm; 95% confidence interval 5 to 15; P<0.001), and between DX2 and placebo (10 mm; 5 to 15; P<0.001). These reductions of pain in DX1 and DX2 compared with placebo both reached the predefined minimal important difference.
Median pain intensity levels at 48 hours during knee flexion were 55 mm in DX1 (interquartile range 40-70), 40 mm (30-50) in DX2, and 50 mm (35-63.5) in placebo. The van Elteren test showed (table 3) a difference between DX1 and DX2 (Hodges-Lehmann median difference −15 mm; 95% confidence interval −20 to −10; P<0.001), between DX1 and placebo (−6 mm; −10 to 0; P=0.011), and between DX2 and placebo (10 mm; 3 to 11; P=0.003). These reductions of pain in DX2 compared with both DX1 and placebo reached the predefined minimal important difference.
Median pain intensity levels at 48 hours at rest were 30 mm (interquartile range 10-40) in DX1, 15 mm (9-30) in DX2, and 20 mm (10-35) in placebo. The van Elteren test showed a difference between DX1 and DX2 (Hodges-Lehmann median difference −10 mm; 95% confidence interval −12 to −5; P<0.001), between DX1 and placebo (−3 mm; −10 to 0; P=0.01), and between DX2 and placebo (5 mm; 0 to 10; P=0.003). The reduction of pain in DX2 compared with DX1 reached the predefined minimal important difference.
Median level for highest pain intensity level at 24-48 hours was 70 mm in DX1 (interquartile range 50-84), 60 mm in DX2 (40-71), and 70 mm in placebo (52-80). The van Elteren test showed a difference between DX1 and DX2 (Hodges-Lehmann median difference −10 mm; 95% confidence interval −20 to −10; P<0.001); no difference between DX1 and placebo; and a difference between DX2 and placebo (11 mm; 10 to 20; P<0.001). These reductions of pain in DX2 compared with DX1 and placebo both reached the predefined minimal important difference.
The incidence of adverse events at 0-48 hours was seven in DX1, four in DX2, and 10 in placebo (etable 3). Logistic regression showed no difference between the groups.
Explorative outcomes
The incidence of participants with a serious adverse effect was 21 in DX1, 9 in DX2, and 18 in placebo (table 4). Logistic regression showed a difference between DX1 and DX2 (odds ratio 0.39; 95% confidence interval 0.17 to 0.88; P=0.02; etable 2). Incidences of nausea, sedation, dizziness, vomiting, and antiemetic consumption for the total intervention period were in favour of DX1 and DX2 over placebo (etable 2). At 24 hours DX1 had a lower risk of nausea and sedation than DX2. All other explorative outcomes and the post-hoc analysis of patient acceptable pain state are presented in the appendix (etables 2 and 5).
Table 4.
Types of serious adverse events (follow-up at 90 days). Data are numbers
| Intervention group | DX1 | DX2 | Placebo |
|---|---|---|---|
| Related to surgery: | |||
| Surgical site infection | 2 | 1 | 5 |
| Wound related problems | 2 | — | — |
| Mechanical problems with the prosthesis | 2 | — | 7 |
| Subtotal | 6 | 1 | 12 |
| Medical problems after surgery: | |||
| Pneumonia | — | 1 | — |
| Deep vein thrombosis/lung embolism | 1 | 3 | 1 |
| Dyspnoea | — | 1 | 1 |
| Morphine side effects | 1 | — | — |
| Cardiovascular | 1 | 2 | 1 |
| Cerebral | 2 | — | — |
| Constipation | 1 | — | — |
| Pain | 1 | — | — |
| Hospital admittance >4 days | 1 | — | 2 |
| Low haemoglobin | 1 | — | 1 |
| Subtotal | 9 | 7 | 6 |
| “Not” related to the surgery: | |||
| Infection: not anatomically related | 3 | 1 | — |
| Fracture, not anatomically related | 1 | — | — |
| Cancer | 1 | — | — |
| Unknown | 1 | — | — |
| Subtotal | 6 | 1 | 0 |
| Total | 21 | 9 | 18 |
DX1=dexamethasone (24 mg)+placebo; DX2=dexamethasone (24 mg)+dexamethasone (24 mg); placebo=placebo+placebo.
Discussion
Principal findings
The main finding of this randomised, blinded, multicentre, clinical trial was that both one and two doses of dexamethasone, as an adjuvant to multimodal pain treatment with paracetamol, ibuprofen, and local infiltration analgesia, reduced morphine consumption after total knee arthroplasty, with the effect size of two doses reaching the predefined minimal important difference. We predefined the minimal important difference in intravenous morphine consumption as 10 mg. This choice of minimal important difference of opioid reductions is in line with other postoperative pain trials,22 23 24 25 26 but is arbitrary, as no generally accepted standard exists for a minimal important difference of postoperative morphine sparing. The reduction in morphine consumption of patients found in this trial corresponds to almost 25%, even with dexamethasone as an adjuvant to three non-opioid analgesic interventions. Nevertheless, to avoid overemphasis on statistical significance of trial results that might have questionable importance for patients, it is essential to predefine minimal important differences for all outcomes. All participants received a comprehensive multimodal non-opioid treatment, and the reduction in morphine use with dexamethasone must be considered in this context. Similarly, we predefined a minimal important difference for reduction in pain intensity levels (visual analogue scale) of 10 mm, which is in line with previously reported patient important reductions.20 27 We found patient important reductions of pain for the two groups receiving dexamethasone at 24 hours, but at 48 hours only the group receiving a second dose of dexamethasone displayed such reductions.
In line with several other trials on pain after total joint arthroplasty,28 we chose morphine consumption as our primary outcome. The differences in the opioid use decided by the patient show the differences in pain relief achieved (that is, analgesic efficacy) between the intervention and placebo groups and can therefore be considered as a valid surrogate outcome mirroring patients’ total pain. Furthermore, a reduction in postoperative opioid consumption has potential advantages in reducing opioid related adverse effects.29 Also, a lower perioperative opioid use is important as it might reduce the risk of prolonged opioid use.30
We detected no differences in patient reported adverse events within 0-48 hours between the groups. We found fewer serious adverse events within 90 days for patients receiving two doses of dexamethasone rather than one, but this might be a random finding as our trial was not powered for this outcome. Dexamethasone seemed to reduce postoperative opioid related adverse effects such as nausea, vomiting, sedation, and dizziness.
The benefit we showed of a 48 hour difference of 10 mg of intravenous morphine should, however, always be interpreted, in the light of possible, but rare, serious adverse events—for example, hyperglycaemia, mania, or infections, that might not be disclosed owing to the size of the trial and the duration of follow-up. The safety aspects of perioperative glucocorticoid use have been investigated in other studies. Firstly, Jørgensen et al15 investigated safety aspects of perioperative use of 125 mg methylprednisolone in a prospective cohort of 1442 patients with total knee arthroplasty, and found no association with length of stay of more than four days, readmissions, or infectious complications at follow-up at both 30 and 90 days compared with 2485 patients who did not receive methylprednisolone. Secondly, the long term (12 month) outcomes were also investigated in a randomised trial of 4494 patients undergoing cardiac surgery using 1 mg/kg of intravenous dexamethasone.31 The trial authors concluded that perioperative dexamethasone had no effect on the risk of major adverse events. Thirdly, a recent abridged version of a Cochrane systematic review investigated adverse effects of dexamethasone in patients undergoing surgery and found no association with wound infection, unclear influence on wound healing, and only a minimal increase in blood glucose of 0.7 mmol/L in patients without diabetes.32 A recently published trial of 8725 patients receiving 8 mg dexamethasone or placebo concurs with the aforementioned findings as it showed no difference in surgical site infection and no difference in safety outcomes between the groups.33
Participants in the three trial groups had a minor difference in opioid consumption before surgery (table 1). The number of patients using opioids (morphine, oxycodone, and tramadol) before surgery (at home) was 17, corresponding to 3.5%, and opioid tolerance is probably not a concern for such low doses (<30 mg oral morphine per day).
Comparison with other studies
A recent review of total hip and knee arthroplasties included no low risk of bias trials, but suggested beneficial effects of glucocorticoids, which needed confirmation from further trials.11 Our results concur with most previous, but smaller, trials for the effect of high dose (>20 mg dexamethasone equivalent) glucocorticoid on morphine consumption and pain scores.10 34 35 36 37 38 39 This DEX-2-TKA low risk of bias trial shows a statistically and patient important adjuvant analgesic effect of two doses of high dose dexamethasone, and with follow-up at 90 days.
Strength and limitations
Our trial has several strengths. Firstly, our methodology was predefined before starting the trial, and similarly, the detailed statistical analysis plan was published before the analysis of trial data began. Secondly, participants, staff, investigators, surgeons, outcome assessors, statisticians, and those drawing conclusions were blinded to the intervention. Thirdly, the trial had a pragmatic design and broad inclusion criteria for participation, giving clinical relevance of trial results to patients undergoing total knee arthroplasty. Combined with a multicentre setup, this trial broadly mimics daily clinical routines assuring a high external validity of our findings. Lastly, our primary outcome (48 hour escape morphine use) is a cumulative proxy measure of patients’ total pain, which increases the clinical importance of this outcome.
Our trial also has limitations. Firstly, our results on opioid consumption and pain levels are limited to the first 48 hours after surgery, so the potential long term adjuvant analgesic effects of dexamethasone are unclear based on our results. Secondly, we did not include a quality of recovery measure, which might have increased information on the effect of glucocorticoids on postoperative rehabilitation. Thirdly, we tested the effects of one and two doses of 24 mg dexamethasone and therefore cannot conclude that other doses and treatment regimens of dexamethasone might have adjuvant analgesic effects. Fourthly, as reported in the statistical analysis plan, no previous reliable reports of follow-up data at 48 hours for selected secondary and explorative outcomes exist. Therefore, power estimations of non-primary outcomes in this trial are uncertain. This uncertainty requires reservations about reaching a clear cost-benefit conclusion between the positive effects of the intervention and the possible risk for the patients. Fifthly, the choice of anaesthetic technique was at the discretion of the anaesthetist, which might have affected the outcomes. The type of spinal and general anaesthesia was standardised and according to protocol, however, and was balanced between the three groups (table 1). Sixthly, blood sugar levels were not assessed as an outcome, but in previous trials the rise in blood sugar caused by dexamethasone was shown to be negligible.32 40 41 Thus we excluded only participants with dysregulated diabetes. Seventhly, we recognise that the risk of remifentanil administered to patients operated on under general anaesthesia might result in postoperative opioid induced hyperalgesia, although the clinical effect is debateable.42 43 Eighthly, we did not systematically involve patients or patient unions in the construction of the trial and trial protocol, which might have improved the choice of trial outcomes. Ninthly, the pragmatic design might introduce a small difference in how each patient was treated, from the type of operation to the way in which rehabilitation at the ward was handled. This randomised clinical trial comprised a predefined sample size, which was reached, and the randomisation and stratification for site should result in similar distributions of the surgical and rehabilitative methods in the groups compared. Furthermore, each site followed uniform local standard protocols, and analyses showed no interaction between site and the trial interventions. Tenthly, our measurement of intraoperative blood loss does not allow firm conclusions to be reached about the effects of intervention on perioperative blood loss, as such measurements are complex, and also include, for example, postoperative and hidden blood losses.44 Lastly, our trial does not offer evidence transferable to patients who did not fulfil the eligibility criteria—in particular, patients with BMI above 40 or who used opioids above 30 mg of oral morphine equivalent dose before surgery.
We did not specify how to estimate the median difference we would use to assess if our predefined minimal difference was reached.17 18 The adjuvant analgesic effects of dexamethasone could be tested by comparing medians between groups (at group level). The real interest is the potential adjuvant analgesic effect at the individual level, however, and here the Hodges-Lehmann median difference analysis shows the median differences between individual patients. We (and others45) therefore consider Hodges-Lehmann to be a more relevant analysis, and that analysing data using Hodges-Lehmann leads to more patient relevant results.
Conclusions
In conclusion, two doses of dexamethasone, as an adjuvant to a multimodal pain treatment with paracetamol, ibuprofen, and local infiltration analgesia, reduced morphine consumption and pain after total knee arthroplasty.
What is already known on this topic
Total knee arthroplasty is a common procedure associated with moderate to severe postoperative pain
Dexamethasone is often used as part of a multimodal treatment for pain after surgery, but the evidence for its possible analgesic effects as an adjuvant is sparse, especially for high and repeated doses
What this study adds
Compared with placebo, two doses of 24 mg intravenous dexamethasone administered perioperatively as an adjuvant to multimodal pain treatment resulted in less pain and less morphine consumption
Acknowledgments
We thank patients, relatives, and clinical and research staff at all trial sites. We thank the monitors for their excellent cooperation. No stipend was awarded for participation. The good clinical practice unit was compensated for monitoring the trial according to Danish law.
Web extra.
Extra material supplied by authors
Web appendix: Appendix
Contributors: KSG and DH-P contributed equally to this trial. KSG and OM had full access to all the data in the study, take responsibility and act as guarantors for the integrity of the data and the accuracy of the data analysis. JCJ and AKN conducted, and are responsible for, the data analysis. KSG, DH-P, THL, JCJ, JB, PL, NAP, HMS, KHT, SB, SO, and OM contributed to the study design, data interpretation, editing of the manuscript, and overseeing study conduct. KSG, DH-P, THL, JCJ, and OM contributed to writing the manuscript. CCL, MH, LØV, MA, KJ, MSJ, MJP, JB, PL, NAP, HMS, ML-L, AKN, KHT, SB, and SO contributed to editing the manuscript. KSG, CCL, MH, LØV, KJ, MSJ, NAP, OM and MLL, contributed to patient recruitment and data collection. MA and MJP contributed to data collection. KSG, DH-P, THL, CCL, MH, KJ, NAP, KHT, and OM contributed to creation of the manual of operations. KSG, DH-P, THL, JCJ, AKN, and OM contributed to data analysis. KSG, DH-P, and KHT contributed to creation of the electronic database. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This study was funded by Næstved, Slagelse and Ringsted Hospitals’ Research Fund, and received support from the Department of Anaesthesiology, Næstved, Slagelse and Ringsted Hospitals, Denmark. The funder of the study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from Næstved, Slagelse, and Ringsted Hospitals’ Research Fund and the Department of Anaesthesiology at Næstved, Slagelse and Ringsted Hospitals for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
KSG, the principal investigator, affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and any discrepancies from the study as originally planned and registered have been explained.
Dissemination to participants and related public communities: Recruited participants will be informed (if they consented hereto) about the results of the trial and what intervention they received. A lay summary will be also made available for trial participants at the trial home page. The participating departments will be informed about the trial results. We will draw attention to the trial results and published manuscript on Twitter and LinkedIn. Furthermore, a press release will be submitted to national media.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
This study was approved by the Regional Committee on Health Research Ethics, Region Zealand, Denmark (SJ-695). The trial was conducted in accordance with the declaration of Helsinki and the patients gave informed consent.
Data availability statement
Data will be shared according to the MRC Clinical Trials Unit controlled access approach, based on the following principles: no data should be released that would compromise an ongoing trial or study; there must be a strong scientific or other legitimate rationale for the data to be used for the requested purpose; investigators who have invested time and effort in developing a trial or study should have a period of exclusivity in which to pursue their aims with the data, before key trial data are made available to other researchers; the resources required to process requests should not be underestimated, particularly successful requests that lead to preparing data for release, thus adequate resources must be available to comply in a timely manner or at all, and the scientific aims of the study must justify the use of such resources; and data exchange complies with information governance and data security policies in all the relevant countries. Researchers wishing to access data from the DEX-2-TKA study should contact omat@regionsjaelland.dk in the first instance.
References
- 1. Rupp M, Lau E, Kurtz SM, Alt V. Projections of Primary TKA and THA in Germany From 2016 Through 2040. Clin Orthop Relat Res 2020;478:1622-33. 10.1097/CORR.0000000000001214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S. Projected increase in total knee arthroplasty in the United States - an alternative projection model. Osteoarthritis Cartilage 2017;25:1797-803. 10.1016/j.joca.2017.07.022 [DOI] [PubMed] [Google Scholar]
- 3. Inacio MCS, Graves SE, Pratt NL, Roughead EE, Nemes S. Increase in Total Joint Arthroplasty Projected from 2014 to 2046 in Australia: A Conservative Local Model With International Implications. Clin Orthop Relat Res 2017;475:2130-7. 10.1007/s11999-017-5377-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013;118:934-44. 10.1097/ALN.0b013e31828866b3 [DOI] [PubMed] [Google Scholar]
- 5. Chang CB, Cho WS. Pain management protocols, peri-operative pain and patient satisfaction after total knee replacement: a multicentre study. J Bone Joint Surg Br 2012;94:1511-6. 10.1302/0301-620X.94B11.29165 [DOI] [PubMed] [Google Scholar]
- 6. Wainwright TW, Gill M, McDonald DA, et al. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop 2020;91:3-19. 10.1080/17453674.2019.1683790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wick EC, Grant MC, Wu CL. Postoperative Multimodal Analgesia Pain Management With Nonopioid Analgesics and Techniques: A Review. JAMA Surg 2017;152:691-7. 10.1001/jamasurg.2017.0898 [DOI] [PubMed] [Google Scholar]
- 8. Wu CL, King AB, Geiger TM, et al. Fourth Perioperative Quality Initiative Workgroup . American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Perioperative Opioid Minimization in Opioid-Naïve Patients. Anesth Analg 2019;129:567-77. 10.1213/ANE.0000000000004194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dahl JB, Nielsen RV, Wetterslev J, et al. Scandinavian Postoperative Pain Alliance (ScaPAlli) . Post-operative analgesic effects of paracetamol, NSAIDs, glucocorticoids, gabapentinoids and their combinations: a topical review. Acta Anaesthesiol Scand 2014;58:1165-81. 10.1111/aas.12382 [DOI] [PubMed] [Google Scholar]
- 10. Lunn TH, Kristensen BB, Andersen LØ, et al. Effect of high-dose preoperative methylprednisolone on pain and recovery after total knee arthroplasty: a randomized, placebo-controlled trial. Br J Anaesth 2011;106:230-8. 10.1093/bja/aeq333 [DOI] [PubMed] [Google Scholar]
- 11. Lex JR, Edwards TC, Packer TW, Jones GG, Ravi B. Perioperative Systemic Dexamethasone Reduces Length of Stay in Total Joint Arthroplasty: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Arthroplasty 2021;36:1168-86. [DOI] [PubMed] [Google Scholar]
- 12. Karlsen APH, Wetterslev M, Hansen SE, Hansen MS, Mathiesen O, Dahl JB. Postoperative pain treatment after total knee arthroplasty: A systematic review. PLoS One 2017;12:e0173107. 10.1371/journal.pone.0173107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Romundstad L, Stubhaug A. Glucocorticoids for acute and persistent postoperative neuropathic pain: what is the evidence? Anesthesiology 2007;107:371-3. 10.1097/01.anes.0000279487.27940.5c [DOI] [PubMed] [Google Scholar]
- 14. Myles PS, Corcoran T. Benefits and Risks of Dexamethasone in Noncardiac Surgery. Anesthesiology 2021;135:895-903. 10.1097/ALN.0000000000003898 [DOI] [PubMed] [Google Scholar]
- 15. Jørgensen CC, Pitter FT, Kehlet H, Lundbeck Foundation Center for Fast-track Hip and Knee Replacement Collaborative Group . Safety aspects of preoperative high-dose glucocorticoid in primary total knee replacement. Br J Anaesth 2017;119:267-75. 10.1093/bja/aex190 [DOI] [PubMed] [Google Scholar]
- 16. De Oliveira GS, Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology 2011;115:575-88. 10.1097/ALN.0b013e31822a24c2 [DOI] [PubMed] [Google Scholar]
- 17. Gasbjerg KS, Hägi-Pedersen D, Lunn TH, et al. DEX-2-TKA-DEXamethasone twice for pain treatment after Total Knee Arthroplasty: A protocol for a randomized, blinded, three-group multicentre clinical trial. Acta Anaesthesiol Scand 2020;64:267-75. 10.1111/aas.13481 [DOI] [PubMed] [Google Scholar]
- 18. Gasbjerg KS, Hägi-Pedersen D, Lunn TH, et al. DEX-2-TKA - DEXamethasone twice for pain treatment after Total Knee Arthroplasty: Detailed statistical analysis plan for a randomized, blinded, three-group multicentre clinical trial. Acta Anaesthesiol Scand 2020;64:839-46. 10.1111/aas.13560 [DOI] [PubMed] [Google Scholar]
- 19.ICH Topic E 2 A - Clinincal Safety Data Managements: Definitions and Standards for Expedited Reporting. In London, UK: European Medicines Agency; 1995. https://www.ema.europa.eu/en/documents/scientific-guideline/international-conference-harmonisation-technical-requirements-registration-pharmaceuticals-human-use_en-15.pdf.
- 20. Myles PS, Myles DB, Galagher W, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth 2017;118:424-9. 10.1093/bja/aew466 [DOI] [PubMed] [Google Scholar]
- 21. Conroy RM. What Hypotheses do “Nonparametric” Two-Group Tests Actually Test? Stata J 2012;12:182-90 10.1177/1536867X1201200202. [DOI] [Google Scholar]
- 22. Thybo KH, Hägi-Pedersen D, Dahl JB, et al. Effect of Combination of Paracetamol (Acetaminophen) and Ibuprofen vs Either Alone on Patient-Controlled Morphine Consumption in the First 24 Hours After Total Hip Arthroplasty: The PANSAID Randomized Clinical Trial. JAMA 2019;321:562-71. 10.1001/jama.2018.22039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Martinez V, Beloeil H, Marret E, Fletcher D, Ravaud P, Trinquart L. Non-opioid analgesics in adults after major surgery: systematic review with network meta-analysis of randomized trials. Br J Anaesth 2017;118:22-31. 10.1093/bja/aew391 [DOI] [PubMed] [Google Scholar]
- 24. Fabritius ML, Strøm C, Koyuncu S, et al. Benefit and harm of pregabalin in acute pain treatment: a systematic review with meta-analyses and trial sequential analyses. Br J Anaesth 2017;119:775-91. 10.1093/bja/aex227 [DOI] [PubMed] [Google Scholar]
- 25. Maund E, McDaid C, Rice S, Wright K, Jenkins B, Woolacott N. Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs for the reduction in morphine-related side-effects after major surgery: a systematic review. Br J Anaesth 2011;106:292-7. 10.1093/bja/aeq406 [DOI] [PubMed] [Google Scholar]
- 26. Doleman B, Sutton AJ, Sherwin M, Lund JN, Williams JP. Baseline morphine consumption may explain between-study heterogeneity in meta-analyses of adjuvant analgesics and improve precision and accuracy of effect estimates. Anesth Analg 2018;126:648-60. 10.1213/ANE.0000000000002237 [DOI] [PubMed] [Google Scholar]
- 27. Olsen MF, Bjerre E, Hansen MD, et al. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med 2017;15:35. 10.1186/s12916-016-0775-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Koyuncu S, Friis CP, Laigaard J, Anhøj J, Mathiesen O, Karlsen APH. A systematic review of pain outcomes reported by randomised trials of hip and knee arthroplasty. Anaesthesia 2021;76:261-9. 10.1111/anae.15118 [DOI] [PubMed] [Google Scholar]
- 29. Zhao SZ, Chung F, Hanna DB, Raymundo AL, Cheung RY, Chen C. Dose-response relationship between opioid use and adverse effects after ambulatory surgery. J Pain Symptom Manage 2004;28:35-46. 10.1016/j.jpainsymman.2003.11.001 [DOI] [PubMed] [Google Scholar]
- 30. Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain 2016;157:1259-65. 10.1097/j.pain.0000000000000516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dieleman JM, de Wit GA, Nierich AP, et al. DExamethasone for Cardiac Surgery (DECS) Study Group . Long-term outcomes and cost effectiveness of high-dose dexamethasone for cardiac surgery: a randomised trial. Anaesthesia 2017;72:704-13. 10.1111/anae.13853 [DOI] [PubMed] [Google Scholar]
- 32. Polderman JAW, Farhang-Razi V, van Dieren S, et al. Adverse side-effects of dexamethasone in surgical patients - an abridged Cochrane systematic review. Anaesthesia 2019;74:929-39. 10.1111/anae.14610 [DOI] [PubMed] [Google Scholar]
- 33. Corcoran TB, Myles PS, Forbes AB, et al. PADDI Investigators. Australian and New Zealand College of Anaesthetists Clinical Trials Network. Australasian Society for Infectious Diseases Clinical Research Network . Dexamethasone and Surgical-Site Infection. N Engl J Med 2021;384:1731-41. 10.1056/NEJMoa2028982 [DOI] [PubMed] [Google Scholar]
- 34. Xu B, Ma J, Huang Q, Huang ZY, Zhang SY, Pei FX. Two doses of low-dose perioperative dexamethasone improve the clinical outcome after total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc 2018;26:1549-56. 10.1007/s00167-017-4506-x [DOI] [PubMed] [Google Scholar]
- 35. Wu Y, Lu X, Ma Y, et al. Perioperative multiple low-dose Dexamethasones improves postoperative clinical outcomes after Total knee arthroplasty. BMC Musculoskelet Disord 2018;19:428. 10.1186/s12891-018-2359-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xu H, Zhang S, Xie J, Lei Y, Cao G, Pei F. Multiple Doses of Perioperative Dexamethasone Further Improve Clinical Outcomes After Total Knee Arthroplasty: A Prospective, Randomized, Controlled Study. J Arthroplasty 2018;33:3448-54. 10.1016/j.arth.2018.06.031 [DOI] [PubMed] [Google Scholar]
- 37. Cheng BLY, So EHK, Hui GKM, et al. Pre-operative intravenous steroid improves pain and joint mobility after total knee arthroplasty in Chinese population: a double-blind randomized controlled trial. Eur J Orthop Surg Traumatol 2019;29:1473-9. 10.1007/s00590-019-02469-5 [DOI] [PubMed] [Google Scholar]
- 38. Li D, Zhao J, Yang Z, Kang P, Shen B, Pei F. Multiple Low Doses of Intravenous Corticosteroids to Improve Early Rehabilitation in Total Knee Arthroplasty: A Randomized Clinical Trial. J Knee Surg 2019;32:171-9. 10.1055/s-0038-1636506 [DOI] [PubMed] [Google Scholar]
- 39. Yu Y, Lin H, Wu Z, Xu P, Lei Z. Perioperative combined administration of tranexamic acid and dexamethasone in total knee arthroplasty-benefit versus harm? Medicine (Baltimore) 2019;98:e15852. 10.1097/MD.0000000000015852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dieleman JM, Nierich AP, Rosseel PM, et al. Dexamethasone for Cardiac Surgery (DECS) Study Group . Intraoperative high-dose dexamethasone for cardiac surgery: a randomized controlled trial. JAMA 2012;308:1761-7. 10.1001/jama.2012.14144 [DOI] [PubMed] [Google Scholar]
- 41. Toner AJ, Ganeshanathan V, Chan MT, Ho KM, Corcoran TB. Safety of perioperative glucocorticoids in elective noncardiac surgery: A systematic review and meta-analysis. Anesthesiology 2017;126:234-48. 10.1097/ALN.0000000000001466 [DOI] [PubMed] [Google Scholar]
- 42. Albrecht E, Grape S, Frauenknecht J, Kilchoer L, Kirkham KR. Low- versus high-dose intraoperative opioids: A systematic review with meta-analyses and trial sequential analyses. Acta Anaesthesiol Scand 2020;64:6-22. 10.1111/aas.13470 [DOI] [PubMed] [Google Scholar]
- 43. Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth 2014;112:991-1004. 10.1093/bja/aeu137 [DOI] [PubMed] [Google Scholar]
- 44. Morales-Avalos R, Ramos-Morales T, Espinoza-Galindo AM, et al. First Comparative Study of the Effectiveness of the Use of Tranexamic Acid against ε-Aminocapróic Acid via the Oral Route for the Reduction of Postoperative Bleeding in TKA: A Clinical Trial. J Knee Surg 2021;34:383-405. 10.1055/s-0039-1696722 [DOI] [PubMed] [Google Scholar]
- 45. Conroy RM. What hypotheses do “nonparametric” two-group tests actually test? Stata J 2012;12:182-90 10.1177/1536867X1201200202. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Appendix
Data Availability Statement
Data will be shared according to the MRC Clinical Trials Unit controlled access approach, based on the following principles: no data should be released that would compromise an ongoing trial or study; there must be a strong scientific or other legitimate rationale for the data to be used for the requested purpose; investigators who have invested time and effort in developing a trial or study should have a period of exclusivity in which to pursue their aims with the data, before key trial data are made available to other researchers; the resources required to process requests should not be underestimated, particularly successful requests that lead to preparing data for release, thus adequate resources must be available to comply in a timely manner or at all, and the scientific aims of the study must justify the use of such resources; and data exchange complies with information governance and data security policies in all the relevant countries. Researchers wishing to access data from the DEX-2-TKA study should contact omat@regionsjaelland.dk in the first instance.