ABSTRACT
Background: The mental health burden of posttraumatic stress disorder (PTSD) is high in U.S. military samples. Social support is one of the most robust protective factors against PTSD and a recent meta-analysis indicates that this relationship is even stronger in military samples compared to civilian samples. Yet no meta-analyses have explored factors impacting this association in veterans and military service members (VSMs).
Objective: The current meta-analysis examined demographic, social support, and military characteristics that may moderate the relationship of PTSD severity and social support among U.S. VSMs.
Method: A search identified 37 cross-sectional studies, representing 38 unique samples with a total of 18,766 individuals.
Results: The overall random effects estimate was −.33 (95% CI: −.38, −.27, Z = −10.19, p <.001), indicating that lower levels of social support were associated with more severe PTSD symptoms. PTSD measures based on the Diagnostic and Statistical Manual (DSM)-III had a larger effect size than measures based on DSM-IV or DSM-5. The social support source was a significant moderator such that support perceived from non-military sources was associated with a larger effect size than support perceived from military sources. This finding held after accounting for covariates. Deployment-era, timing of social support, and age were also significant moderators, but were no longer significantly associated with effect size after adjusting for covariates. Although previous meta-analyses have shown social negativity to be more impactful than positive forms of social support, there were too few studies conducted to evaluate social negativity in moderator analyses.
Conclusion: Results suggest that social support received from civilians and in the home environment may play a greater protective role than social support received from military sources on long-term PTSD symptom severity. The literature on social support and PTSD in U.S. VSMs would be strengthened by studies examining the association of social negativity and PTSD symptoms.
KEYWORDS: Posttraumatic stress disorder, social support, military, veterans, active duty
HIGHLIGHTS
• Factors that impact the association of PTSD severity and social support among U.S. military service members are understudied.
• A meta-analysis of 38 cross-sectional samples (N = 18,766) showed that higher levels of social support were associated with less severe PTSD symptoms.
• Social support received from non-military sources had a stronger relationship with PTSD symptoms than support received from military sources.
• Few studies have examined the relationship between social negativity and PTSD severity in military samples despite evidence that social negativity is a more robust predictor than positive forms of support.
Short abstract
Antecedentes: La carga en salud mental del trastorno de estrés post-traumático (TEPT) es alta en muestras militares estadounidenses. El apoyo social es uno de los factores protectores más robustos contra el TEPT, y un meta-análisis reciente indica que esta relación es incluso más fuerte en muestras militares comparada con muestras de civiles. Aunque, ningún meta-análisis ha explorado los factores que impactan esta asociación en veteranos y miembros militares en servicio (VMS).
Objetivo: El presente meta-análisis examinó características demográficas, de apoyo social, y militares que puedan moderar la relación de severidad de TEPT y apoyo social en VMS estadounidenses.
Método: Una búsqueda identificó 37 estudios transversales, representando 38 muestras únicas con un total de 18.766 individuos.
Resultados: La estimación general de efectos aleatorios fue −.33 (95% CI: −.38, −.27, Z=−10.19, p<.001), indicando que niveles más bajos de apoyo social estaban asociados a mayor severidad de síntomas TEPT. Los instrumentos de TEPT basados en el Manual diagnóstico y estadístico de los trastornos mentales (DSM) –III obtuvieron un tamaño de efecto mayor que los instrumentos basados en DSM-IV o DSM-5. La fuente de apoyo social fue un moderador significativo, de tal forma que el apoyo percibido de fuentes no militares estuvo asociado a un tamaño de efecto más grande que el percibido de fuentes militares. Este efecto se mantuvo luego de controlar covariables. La era de despliegue militar, temporalidad del apoyo social, y edad también fueron moderadores significativos, pero no se mantuvieron significativamente asociados al tamaño de efecto luego de controlar covariables. Aunque meta-análisis previos han demostrado que la negatividad social ha tenido más impacto que las formas positivas de apoyo social, existían muy pocos estudios como para evaluar negatividad social en un análisis de moderación.
Conclusión: Los resultados sugieren que el apoyo social recibido de civiles y en el ambiente familiar puede tener un rol protector más relevante que el recibido de fuentes militares en la severidad de síntomas TEPT en el largo plazo. La literatura sobre apoyo social y TEPT en VMS estadounidenses se vería enriquecida por estudios que examinen la asociación de la negatividad social y síntomas TEPT.
PALABRAS CLAVE: Trastorno de estrés post-traumático, apoyo social, militares, veteranos, labour activa
Short abstract
背景: 在美国军人样本中, 创伤后应激障碍 (PTSD) 的心理健康负担很重。社会支持是PTSD最强的保护因素之一, 近期一项元分析表明, 这种关系在军人样本中比平民样本中更强。然而, 尚无在退伍军人和军人(VSMs)中考查这种关联影响因素的元分析。
目的: 本元分析考查了美国VSM中可能会调节PTSD严重程度和社会支持之间关系的人口统计学, 社会支持和军人特征。
方法: 检索确定了37个横断面研究, 包含38个独特样本, 共计18,766人。
结果: 总体随机效应估计值为-.33 (95%CI:-.38, −.27, Z= −10.19, p<.001), 表明较低的社会支持水平与较严重的PTSD症状相关。基于诊断和统计手册(DSM)-III对PTSD的测量, 相较于基于DSM-IV或DSM-5的测量具有更大的效应量。社会支持来源是一个显著的调节因素, 从非军队来源获得的支持与从军队来源获得的支持相比, 具有更大的效应量。这一发现在控制协变量之后仍然成立。部署时期, 社会支持的时机和年龄也是重要的调节因素, 但调节协变量后的效应量不再显著相关。尽管以前的元分析显示, 社会消极感比积极形式的社会支持更具有影响力, 但调节因素分析中评估社会消极感的研究很少。
结论: 结果表明, 就长期创伤后应激障碍症状严重程度而言, 从平民和家庭环境中获得的社会支持可能比从军队来源获得的社会支持起更大的保护作用。可以通过考查社会消极感与PTSD症状之间联系的研究加强美国VSM中社会支持和PTSD的文献。
关键词: 创伤后应激障碍, 社会支持, 军人, 退伍军人, 现役
Posttraumatic stress disorder (PTSD) is one of the most frequently diagnosed disorders following trauma exposure during U.S. military service (e.g., Hoge et al., 2004; Seal, Bertenthal, Miner, Sen, & Marmar, 2007; Vasterling et al., 2010) and risk for PTSD among service members is higher than that of the general U.S. population (Institute of Medicine, 2012). Thus, understanding factors that mitigate PTSD severity among U.S. veterans and service members (VSMs) is critical. Several meta-analyses examining risk factors for PTSD have shown that lower social support is a robust risk factor for the presence of a PTSD diagnosis or higher PTSD symptoms (i.e., Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003; Shand, Cowlishaw, Brooker, Burney, & Ricciardelli, 2015; Wright, Kelsall, Sim, Clarke, & Creamer, 2013; Xue et al., 2015; Zalta et al., 2020), and this association is particularly strong among military samples (Zalta et al., 2020). Meta-analyses in military samples have shown that both lower unit support and lower non-military support (i.e., post-deployment support, family support, social support) are associated with heightened risk for PTSD (i.e., Wright et al., 2013; Xue et al., 2015).
Though previous meta-analyses have shown a clear association between social support and PTSD, only two specifically focused on VSMs (i.e., Wright et al., 2013; Xue et al., 2015). In both of these meta-analyses, social support was only one correlate of PTSD explored, resulting in a narrow pool of only 5–7 studies that were restricted to published papers. Moreover, neither meta-analysis examined possible moderators. Given the fact that social support appears to be a particularly important buffer against PTSD severity among military samples (Zalta et al., 2020), conducting a more thorough review of the literature, including findings observed in unpublished papers, and exploring factors that moderate this association will be important to identify potential targets for further study and intervention.
There are demographic, social support, and military service factors that may moderate the association of PTSD and social support. With respect to demographic factors, the Minority Stress Model (Meyer, 2003) indicates that minorities may experience heightened stress and lower social support in challenging times (e.g., Coleman, Ingram, & Sheerin, 2019; Gibbons, Hickling, Barnett, Herbig-Wall, & Watts, 2012). Women and non-White individuals represent minorities within the military (Department of Defense, 2018), suggesting they may receive less support than their gender and ethic/racial counterparts. For example, relative to men, women service members reported significantly lower unit support (Kline et al., 2013), and lower unit support was associated with higher PTSD symptoms (Polusny et al., 2014). Similarly, racial/ethnic minority women reported lower social support relative to their non-minority women counterparts (Lehavot, Beckman, Chen, Simpson, & Williams, 2019). At the same time, other studies have observed that women veterans and minority veterans report higher support than men and non-minority veterans, respectively (Herbert, Leung, Pittman, Floto, & Afari, 2018), suggesting that race and gender are key moderators to examine. It is further possible that marital status may moderate the association of PTSD and social support such that VSMs who are married or cohabitating will report lower PTSD symptoms and higher social support relative to their non-married counterparts. Indeed, service members who are married report greater access to social support than those who are not married or cohabitating (Herbert et al., 2018). At the same time, there is evidence among military couples that the presence of a diagnosis of PTSD is associated with a higher frequency of negative social exchanges (e.g., Caska et al., 2014), and that separation during deployment may cause a disruption in bonds (Paley, Lester, & Mogil, 2013), suggesting that being married may not be a buffer against PTSD. Finally, younger age is associated with increased risk for PTSD (see review, Brewin et al., 2000), and will therefore be examined as a moderator.
There are also social support characteristics, such as type, source, and timing, that may moderate the relationship between social support and PTSD symptoms among U.S. VSMs. Negative social interactions have been observed to have a stronger relationship with PTSD relative to positive forms of social support (e.g., enacted, perceived, structural; Zalta et al., 2020), suggesting that social support type is a key moderator to explore. Indeed, theories of social support suggest that negative support may be more punitive than the rewarding benefits of positive social support because of the expectation that support received is desired and useful. When it falls on the negative dimension, its receipt may be met with disappointment and concerns about the utility of the relations (Rook & Pietromonaco, 1987). Regarding the source of social support, it is possible that support from fellow service members may be a stronger buffer against PTSD severity due to the sense of a shared understanding of unique job requirements and stressors among service members. This may be particularly true in the U.S where less than one-half of 1% of the U.S. population is active-duty personnel. The timing of support may also be an important factor. Specifically, support received during deployment (vs outside of deployment) may be particularly beneficial in buffering against PTSD symptoms given increases in stress and proximity to traumatic exposures during deployment. Previous research suggests that support received during deployment may enhance coping strategies and build resilience during a challenging time (e.g., Luciano & McDevitt-Murphy, 2017).
Several factors specific to U.S. military service could also impact the association between social support and PTSD symptoms. First, era of service may moderate the association of PTSD and social support. Vietnam veterans faced a lack of public support for this military operation, and many served in Vietnam because they were drafted involuntarily for service (e.g., Ciampaglia, 2019). This may suggest that having social support would be a stronger buffer against PTSD among Vietnam veterans given the societal context of this war. Moreover, service in non-active duty components, such as National Guard or Reserve, may also impact the relationship between social support and PTSD symptoms. Unlike those in active duty service, service members in the National Guard and Reserve components do not live full-time with their fellow service members and may not deploy with their Guard or Reserve units. Evidence suggests that National Guard service members who deploy without their units report lower unit support relative to those that deploy with their units (Granado et al., 2012) and that higher unit support during deployment is protective for Army soldiers but not soldiers in the National Guard (Han et al., 2014). Discharge status may also play a role in that those who are discharged may experience different opportunities for social support due to separation from the military and their unit. None of these military factors have previously been explored in meta-analyses examining the relationship between social support and PTSD.
Finally, it is possible that trauma type may impact the association of PTSD and social support. There has been increasing recognition that military sexual trauma (MST) is a serious problem in the U.S. military with rates of MST among female service members as high as 40% (Wilson, 2018). MST exposure is associated with the presence of a PTSD diagnosis (Kimerling, Gima, Smith, Street, & Frayne, 2007), higher PTSD severity (Blais, Brignone, Fargo, Livingston, & Andresen, 2019), and disrupted interpersonal function (e.g., Blais, 2019; Blais, Geiser, & Cruz, 2018), suggesting that experiences of MST may impact the association of PTSD and social support.
The purpose of the current meta-analysis is to build on previous literature. Namely, prior meta-analyses conducted on VSMs did not focus specifically on the association of PTSD and social support, resulting in a narrow review that was circumscribed to published papers with no examination of possible moderators. The present meta-analysis will explore the association of PTSD and social support as a primary aim, include unpublished data, and explore moderators of this association to better inform possible treatment targets aimed at reducing PTSD symptoms. The current meta-analytic review focused on the U.S. military because the demographic factors (e.g., sex and racial makeup of the military) and military factors (e.g., service era, branch) that we sought to test as moderators may be specific to the U.S. military. Additionally, the current study focused on non-clinical samples to ensure no restriction of range in PTSD symptoms.
1. Method
1.1. Search procedures
The current study is a secondary analysis of a subset of studies from an existing meta-analytic dataset (Zalta et al., 2020 for details). As part of the initial systematic search, electronic databases were searched in three cycles to ensure adequate coverage of research outlets and search terms. In January 2014 and May 2017, searches were conducted in PsycInfo, Embase + Medline, and PILOTS using the following combination of terms: (social support OR instrumental support OR companionate support OR emotional support OR tangible support OR social connectedness OR criticism OR social constraint OR received support OR social integration OR functional support OR structural support OR informational support OR esteem support OR perceived support OR expressed emotion OR hostility OR social network OR cohesion OR social response OR social reaction OR disclosure OR social acknowledgement) AND (PTSD or posttraumatic or post-traumatic). In June 2019, PsycInfo, PubMed1 (includes Medline), PTSDPubs (formerly PILOTS), ProQuest Dissertations & Thesses A&I, and ProQuest Dissertations & Theses Global were searched using the following combination of updated terms: (social support OR instrumental support OR companionate support OR emotional support OR tangible support OR social connectedness OR criticism OR social constraint OR received support OR social integration OR functional support OR structural support OR informational support OR esteem support OR perceived support OR expressed emotion OR hostility OR social network OR cohesion OR social response OR social reaction OR disclosure OR social acknowledgement OR enacted support OR social negativity OR social interaction* OR network support) AND (PTSD or posttraumatic or post-traumatic). In this expanded search, a ‘not’ limiter was included in the PsycInfo, PubMed + MEDLINE, and PTSDPubs searches to avoid redundant research reports already evaluated in the 2014 and 2017 searches. Each of these electronic database searches was restricted to reports available in English, and research conducted on adult human participants. In addition to the database searches, hand searches were also conducted in trauma journals from January 1980 to June 2019 (any issues of Journal of Traumatic Stress, Journal of Anxiety Disorders, Psychological Trauma: Theory, Research, Practice, and Policy, and Anxiety, Stress, and Coping). We also reviewed reference lists of relevant meta-analyses/reviews and included articles. Finally, we solicited data via professional listservs and emails to researchers who were the first, last, or corresponding author on at least two studies deemed to be eligible for the original meta-analysis as these authors were most likely to have relevant ongoing studies or unpublished data.
1.2. Inclusion criteria
The selection of studies for this meta-analysis were limited to: a) full-text reports of a quantitative study; b) written in the English language; and c) published after 1980 following the establishment of the diagnosis of PTSD in the DSM (American Psychiatric Association, 1980). Study subjects had to meet the following criteria to be included: a) at least 18 years of age or older at the time of the study; b) service members or veterans in the U.S. military; and c) trauma exposed or deployed to a combat zone. Treatment studies or studies that recruited participants based on PTSD symptoms or other psychiatric characteristics were excluded because they would potentially represent a biased sample of traumatized individuals and create a restriction of range with regard to PTSD symptoms. With respect to the measurement of PTSD symptoms and social support, the following criteria were applied: a) studies had to utilize a validated self-report PTSD measure that assessed re-experiencing, avoidance, and hyperarousal symptoms, b) symptoms of PTSD had to be assessed at least 30 days following the index trauma to account for differences between PTSD and acute stress disorder (American Psychiatric Association, 2013); c) the social support measure had to include a scale that went in a single direction from lower support to higher support (i.e., scales that were comprised of a single, dichotomous item or scales where optimal support was placed in the centre of the scale were excluded); and d) the study had to report a cross-sectional bivariate correlation (r) between social support and PTSD symptoms. If we were unable to assess these inclusion/exclusion criteria using the article, the information was requested from the corresponding author. If the information could not be collected from the corresponding author, the study was deemed ineligible.
1.3. Selection of studies
The PRISMA flow diagram is shown in Figure 1. Each full-text article assessed for eligibility was read by two independent raters. In cases of disagreement, the two raters first discussed the conflict and came to a consensus. Any remaining questions were brought to the senior author (AKZ) and the study team for discussion until a consensus was reached. If the article did not contain the necessary information to establish inclusion/exclusion or did not report the necessary effect size, the corresponding author was contacted for the necessary information. If the author did not respond to the inquiry or was unable to provide the necessary data, the article was excluded. Of the 150 studies included in Zalta et al. (2020), 113 were excluded because they did not contain a military sample or included a sample that was not based in the U.S. The remaining 37 comprise the current meta-analysis.
Figure 1.
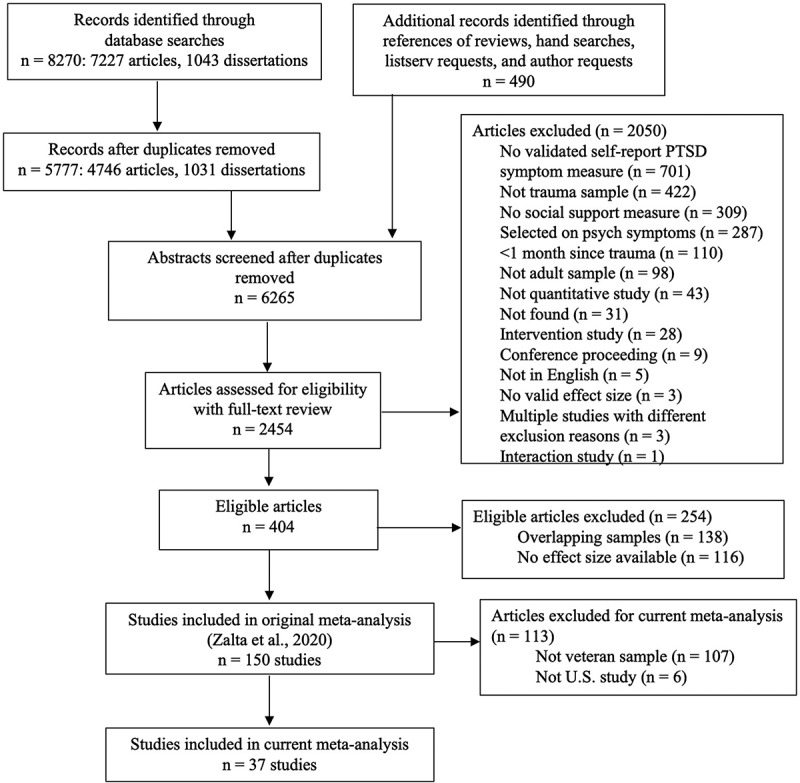
PRISMA flow chart
Note: In the process of retrieving the full text of the reports from the database searches, several additional reports were identified (i.e., reports with very similar titles or additional reports sent to us by authors when reprints were requested). These reports were included in the total number of records identified through database searches.
1.4. Coding of studies
The senior author developed a coding manual (AKZ), and subsequently trained 7 trauma-focused psychologists who were employed at an academic medical centre or university to use the coding manual. The majority of the coders worked to establish fidelity by independently evaluating and rating three articles. They then met to review to achieve consensus. This method was repeated four times (12 articles total) until independent fidelity was observed. Teams of 2 coders were established and the pair of coders reviewed and rated the same set of articles. Rating pairs then compared their ratings and group meetings with the senior author were utilized to discuss and address discrepancies. For the current meta-analysis, we used the same codes established in the parent meta-analysis but also developed codes that were specific to military service (e.g., support received during deployment, support received from military vs non-military sources). The first and senior author were responsible for developing and coding variables specific to military service. These authors coded these variables independently, then met to discuss, and addressed any discrepancies.
Articles that were initially deemed eligible for possible inclusion were coded for these characteristics: publication date, average participant age, sex, percent married/cohabitating, percent identifying as White, publication in a peer-reviewed journal, and use of a validated measure of social support. Types of PTSD measures were also coded to determine if the measure used moderated the association of PTSD and social support. When measures were not commonly used (used in < 5 studies), they were collapsed into an ‘other’ category. We also coded whether the PTSD measure was defined using the Diagnostic and Statistical Manual (DSM), version, III, IV, or 5.
Several social support moderators were coded including the type of social support (perceived, enacted, structural, or social negativity), the source of social support (military v. non-military), and the timing of social support (during deployment v. not during deployment). Of note, all measures included in the current meta-analyses were self-report and therefore all social support types assessed an individuals’ perceptions of support in these different domains. Military-specific moderators included service in National Guard or Reserve (vs non-National Guard/Reserve sample or mixed sample), discharge status (not discharged, discharged, mixed sample), MST exposure (yes/no), and war-era (World War II/Korea, Vietnam, Persian Gulf, Iraq/Afghanistan).
Four quality items were included to assess possible bias: the internal reliability of the social support instrument > .7 (Yes [1] vs. No/Not reported/single item measure [0]); the internal reliability of the PTSD instrument > .7 (Yes [1] vs. No/Not reported [0]); score-level missing data < 20% (Yes [1] vs. No/Not reported [0]); and a suitable approach for managing missing data (scored ‘yes’ [1] if there was no missing data, if the authors used listwise deletion if there was less than 10% missing data, or if the authors used a multiple imputation procedure for more than 10% missing data). The four quality measures were summed to evaluate possible bias. The quality measure developed for this study is included in the coding manual on the Open Science Framework.
For the effect size, bivariate correlations (r) between measures of PTSD severity and social support were coded. Sample sizes were also included in the bivariate correlation code. Correlations were categorized as small (0.10), medium (0.30), or large (0.50; J. Cohen, 1992). If a single study had multiple measures of PTSD and/or social support, all effect sizes were coded. When studies had multiple time points, the first eligible time point (at least 30 days post trauma) where PTSD and social support was assessed was selected because that time point had the largest sample size. All effect sizes were coded such that higher levels of PTSD (i.e., greater severity) were represented by higher scores and higher levels of social support (lower levels of social negativity) were represented by higher scores. As such, the expected direction of the association between social support and PTSD was negative. When articles included effect sizes where poorer social support was represented by higher scores, the reported effect size was reversed for ease of interpretation. When effect sizes were not available, we contacted corresponding authors via email to collect this information.
1.5. Analyses
Comprehensive Meta-Analysis version 3.3.070 was used to calculate weighted effect sizes, heterogeneity, and moderators. We utilized random effects models to tabulate overall weighted effect size because we expected a notable level of heterogeneity. For studies that included total scores and subscale scores for social support, only total scores were utilized in the overall analysis. Heterogeneity of effect sizes was calculated using the Q statistic and the I2 index. The Q statistic was utilized to evaluate the significance of heterogeneity, and the I2 index was utilized to evaluate the proportion of variability among a set of effect sizes that is due to true between-study differences. Percentages of 25, 50, and 75 represented low, medium, and high degrees of between-study variability, respectively (Higgins, Thompson, Deeks, & Altman, 2003). We conducted Grubbs’ test using GraphPad to test for outliers (Grubbs, 1969). Publication bias was evaluated by creating a funnel plot of the overall effect size. Egger’s test of the intercept determined the funnel plot’s asymmetry (Egger, Smith, Schneider, & Minder, 1997) and Duval & Tweedie’s trim-and-fill procedures were utilized when appropriate (Duval & Tweedie, 2000). When there is no evidence of asymmetry in the Egger’s test, the intercept is not significantly different from zero. The trim-and-fill method generates adjusted effect sizes and corresponding confidence intervals that account for missingness based on asymmetry of the funnel plot.
To identify possible covariates (e.g., measurement and quality variables), mixed effect models were utilized to generate analysis of variance for categorical moderator variables and meta-regression analysis for continuous moderator variables. Measurement and quality variables that were significantly associated with effect size at p < .05 were included as simultaneous predictors in a meta-regression to identify which variables were associated with effect size. Variables that remained significant in the meta-regression were retained as covariates in subsequent analyses examining sample, trauma, social support, and military service characteristics.
Finally, we explored whether demographic, social support, and military-service characteristics moderated the association of PTSD and social support using analysis of variance for categorical moderator variables and meta-regression analysis for continuous moderator variables with mixed effects models. In some cases, there were instances in which a single study examined several levels/groups of a single moderator (e.g., a single study measured different types of social support). To account for this in analyses, we utilized the shifting unit-of-analysis approach (Cooper, 2010). When a moderator was significantly associated with effect size, a meta-regression analysis included significant characteristics as covariates. When categorical moderators had more than two categories, we ran the meta-regression analysis with each category as the reference group to conduct all pairwise contrast analyses. This was done for all categories except the category with the smallest neffects.
2. Results
2.1. Descriptive characteristics
Thirty-seven studies were identified with 38 independent samples (see Table 1 for study characteristics). Sixty unique effect sizes were reported. Study sample sizes ranged from 63 to 2,507, resulting in a total of 18,766 individuals. The mean sample age was 35.27 (SD = 7.50; 30 [81.08%] studies reporting), samples were 27.29% female (36 [97.29%] studies reporting), 68.62% White (35 [94.59%] studies reporting), and 57.71% were married/co-habitating (24 [64.86%] studies reporting). The majority of studies were published in peer-reviewed journals (n = 26; 68.42%) and reported the effect size in the manuscript (n = 26; 68.42%). Several self-report measures were used to assess PTSD severity, though versions of the PTSD Checklist (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Weathers, Litz, Herman, Huska, & Keane, 1993; Weathers et al., 2013) were the most common (n = 31; 81.58%). Perceived social support was the most commonly measured social support type (n = 31; 72.09%), and most measures of social support were validated or standardized (n = 30; 83.33%). Social support received outside deployment (n = 33; 75%) was more commonly studied than social support received during deployment. Perceptions of support from non-military sources (n = 32; 66.67%) were more commonly studied than social support received from military sources. The DSM-IV (n = 29; 76.32%) was the most frequently utilized version of the DSM. Most commonly, samples were comprised of both National Guard/Reserve and non-National Guard/Reserve samples (‘mixed’ relative to either National Guard/Reserve or active duty; n = 13; 43.43%) and service members who were not yet discharged from service (n = 14; 48.26%). OEF/OIF/OND was the most commonly represented service era (n = 28; 82.35%). We determined that MST exposure was inconsistently reported, precluding us from including this variable.
Table 1.
Table of study characteristics
| Study Name | N | Age (M) | % F | % White | % Married/ Cohab |
PTSD measure (DSM def) | ES reported | SS type | Military SS | Deployment SS | SS valid | Diss/Unpub | NG/R | War-era | Discharged | ES |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abbas, 2018 | 336 | 27 | 13 | 90 | 55 | PCL (IV) | Yes | P/S | No/Yes | No/Yes | Yes | Yes | Yes | OEF/OIF/OND | No | −.45 |
| Balderrama-Durbin et al., 2013 | 76 | 28 | 8 | 66 | NR | PCL (IV) | Yes | P | No | No | Yes | No | No | OEF/OIF/OND | No | −.36 |
| Boul, 2015 | 127 | 31 | 13 | 57 | 46 | PCL (IV) | Yes | P | No | No | Yes | Yes | Mixed | OEF/OIF/OND | NR | −.56 |
| Britt, Adler, Bliese, & Moore, 2013 | 636 | NR | 4 | 64 | NR | PCL (IV) | Yes | S | Yes | Yes | Yes | No | No | OEF/OIF/OND | No | −.31 |
| Campbell & Riggs, 2015 | 117 | 33 | 16 | 78 | 56 | IES-R (IV) | Yes | P | Yes/No | Yes/No | Yes | No | Mixed | Mixed | Yes | −.16 |
| Davis, Hanson, Zamir, Gewirtz, & DeGarmo, 2015 | 282 | NR | 0 | 89 | 88 | PCL (IV) | Yes | E | No | No | Yes | No | Yes | OEF/OIF/OND | NR | −.12 |
| Day, 2017 | 99 | 33 | 0 | 92 | 100 | PCL (IV) | No | P | Yes/No | No | No | Yes | Yes | OEF/OIF/OND | No | −.19 |
| Dempsey, 2001 | 621 | 47 | 0 | 0 | NR | Mississippi (III) | Yes | P | Yes/No | No | No | Yes | No | VN | Yes | −.51 |
| Dryden, 2012 | 1824 | NR | 20 | 45 | NR | Other (IV) | Yes | P | No | No | Yes | Yes | NR | OEF/OIF/OND | NR | −.03 |
| Gradus, Smith, & Vogt, 2015 | 978 | 35 | 55 | 74 | NR | PCL (IV) | Yes | P | No | Yes | Yes | No | Mixed | OEF/OIF/OND | Yes | −.36 |
| Herbert et al., 2018 | 950 | 31 | 88 | 64 | 41 | PCL (IV) | No | S | No | No | No | No | NR | OEF/OIF/OND | Yes | −.17 |
| Hoyt et al., 2010a | 71 | 31 | 7 | 76 | NR | PCL (IV) | No | P | No | No | Yes | No | Mixed | OEF/OIF/OND | No | −.45 |
| Hoyt & Renshaw, 2014 | 81 | 36 | 2 | 89 | 100 | PCL (IV) | Yes | P | No | No | Yes | No | Yes | OEF/OIF/OND | No | −.44 |
| Kehle et al., 2010 | 418 | 32 | 11 | 92 | 45 | PCL (IV) | No | P | No | No | Yes | No | Yes | OEF/OIF/OND | Mixed | −.51 |
| King, Taft, King, Hammond, & Stone, 2006 | 2249 | 30 | 0 | 90 | NR | PCL (IV) | Yes | P | No | No | Yes | No | Mixed | Persian Gulf | NR | −.18 |
| Kline et al., 2013 | 868 | 30 | 10 | 50 | 40 | PCL (IV) | No | S | Yes | Yes | Yes | No | Yes | OEF/OIF/OND | No | −.23 |
| Koster, unpublished | 203 | 41 | 38 | 64 | 67 | PCL (5) | No | P/E | No | No | Yes | Yes | NR | NR | NR | −.21 |
| Laws, Mazure, McKee, Park, & Hoff, 2016 | 723 | 35 | 40 | 78 | 51 | PCL (IV) | Yes | P | Yes | Yes | Yes | No | NR | OEF/OIF/OND | Yes | −.15 |
| Lisman, Currier, & Harris, 2017 | 90 | 31 | 20 | 93 | 39 | PCL (IV) | Yes | P | No | No | Yes | No | Mixed | OEF/OIF/OND | NR | −.13 |
| Lubens & Silver, 2019 | 176 | 37 | 11 | 63 | NR | PCL (5) | No | S | Yes | Yes | Yes | No | Mixed | OEF/OIF/OND | NR | −.11 |
| Luciano & McDevitt-Murphy, 2017 | 63 | 37 | 18 | 43 | NR | PCL (5) | Yes | P | Yes/No | Yes/No | Yes | No | NR | OEF/OIF/OND | NR | −.42 |
| Mendoza, 2015 | 283 | 44 | 15 | 34 | NR | PCL (IV) | Yes | P | No | No | Yes | Yes | Mixed | Mixed | NR | −.38 |
| Moore et al., 2017 | 1041 | 22 | 0 | 87 | 29 | PCL (IV) | No | P | No | No | Yes | No | No | OEF/OIF/OND | No | −.22 |
| Nayback-Beebe & Yoder, 2011 | 137 | NR | 100 | 54 | 45 | PCL (IV) | Yes | P/N | No | No | Yes | No | No | OEF/OIF/OND | No | −.51 |
| Pietrzak, Johnson, Goldstein, Malley, & Southwick, 2009 | 263 | 35 | NR | 87 | NR | PCL (IV) | No | P/S | Yes/No | Yes/No | Yes | No | Mixed | OEF/OIF/OND | Yes | −.41 |
| Port, Engdahl, Frazier, & Eberly, 2002 | 177 | 76 | 0 | 96 | 79 | Mississippi (III) | Yes | S | No | No | Yes | No | NR | WWII/Korean War | Yes | −.52 |
| Rivet, 2012 | 99 | 33 | 100 | 71 | 48 | PCL (IV) | Yes | P | Yes/No | Yes/No | Yes | Yes | NR | OEF/OIF/OND | NR | −.41 |
| Shaine, 2016 | 221 | 32 | 31 | 76 | 49 | PCL (5) | No | P | Yes/No | Yes/No | Yes | Yes | Mixed | OEF/OIF/OND | Mixed | −.22 |
| Tackett, 2011 | 223 | NR | 5 | 43 | 42 | PCL (IV) | Yes | P | No | No | Yes | Yes | Yes | OEF/OIF/OND | No | −.18 |
| Taft, Stern, King, & King, 1999a | 1156 | 42 | 0 | NR | NR | Mississippi (III) | Yes | P | No | No | No | No | NR | VN | No | −.63 |
| Taft et al., 1999b | 423 | 46 | 100 | NR | NR | Mississippi (III) | Yes | P | No | No | No | No | NR | VN | No | −.47 |
| Vogt, Pless, King, & King, 2005 | 317 | NR | 26 | NR | NR | PCL (IV) | No | P | Yes | Yes | Yes | No | Mixed | Persian Gulf | Yes | −.33 |
| Weber, 2012 | 323 | 30 | 14 | 76 | 47 | PCL (IV) | Yes | P | No | No | Yes | Yes | Mixed | OEF/OIF/OND | Mixed | −.35 |
| Whalen, 2011 | 2507 | NR | 9 | 60 | 54 | PCL (IV) | Yes | S | Yes | No | No | Yes | No | OEF/OIF/OND | No | −.13 |
| Wilcox, 2010 | 83 | 25 | 0 | 87 | 100 | PCL (IV) | No | P | Yes/No | No | Yes & No | No | No | OEF/OIF/OND | No | −.35 |
| Wolfe et al., 1998 | 160 | 28 | 100 | 74 | 34 | Mississippi (III) | Yes | P/E/S | Yes/No | Yes/No | Yes & No | No | Mixed | Persian Gulf | No | −.35 |
| Woodward et al., 2018 | 264 | 39 | 34 | 55 | 80 | PCL (IV) | Yes | P | No | No | Yes | No | NR | OEF/OIF/OND | Mixed | −.45 |
| Wooten, 2012 | 101 | 38 | 100 | 46 | 49 | PCL (IV) | Yes | P | No | No | Yes | No | Yes | OEF/OIF/OND | Mixed | −.25 |
Note: F = female. Cohab = Cohabitating. DSM def = DSM definition of the PTSD measure. ES = Effect size. SS = Social support. Valid = Validated measure. Diss/Unpub = Dissertation/Unpublished. OEF/OIF/OND = Operation Enduring Freedom/Operation Iraqi Freedom/Operational New Dawn. VN = Vietnam. WWII = World War II. PCL = PTSD Checklist. IES-R = Impact of Events Scale – Revised. Mississippi = Mississippi Scale for Combat-Related PTSD. P = Perceived. S = Structural. E = Enacted. N = Social Negativity. NG/R = National Guard/Reserve. NR = Not reported. Mixed = sample is comprised of veterans representing different groups (e.g., National Guard/Reserve and those not in the National Guard/Reserve, Discharged and those not discharged from service).
abThe Taft et al., 1999 study included two independent samples of participants. Sample (a) included 1156 male Vietnam veterans and sample (b) included 423 female Vietnam veterans.
2.2. Overall effect size
The overall random effects estimate was −.33 (95% CI: −.38, −.27, Z = −10.19, p < .001), indicating that lower levels of social support were associated with more severe PTSD symptoms (see Figure 2 for an effect size plot). Grubb’s (Grubbs, 1969) test revealed no outliers. Estimates with one study removed ranged from −.34 to −.32, indicating that any possible outliers had little influence on effect size. Heterogeneity analyses revealed a significantly high degree of heterogeneity in the estimate (Q[df] = 689.08(37), p < .001, I2 = 94.63), indicating that tests of moderation were appropriate. Egger’s test of the intercept was significant (t(36) = 2.14, p = .04; see Figure 3 for the funnel plot). The trim-and-fill procedure using a random effects model revealed that no studies were missing to the right of the mean. These metrics suggest that overall, there was little-to-no impact of publication bias and the asymmetry of the funnel plot was likely due to heterogeneity (Terrin, Schmid, Lau, & Olkin, 2003).
Figure 2.
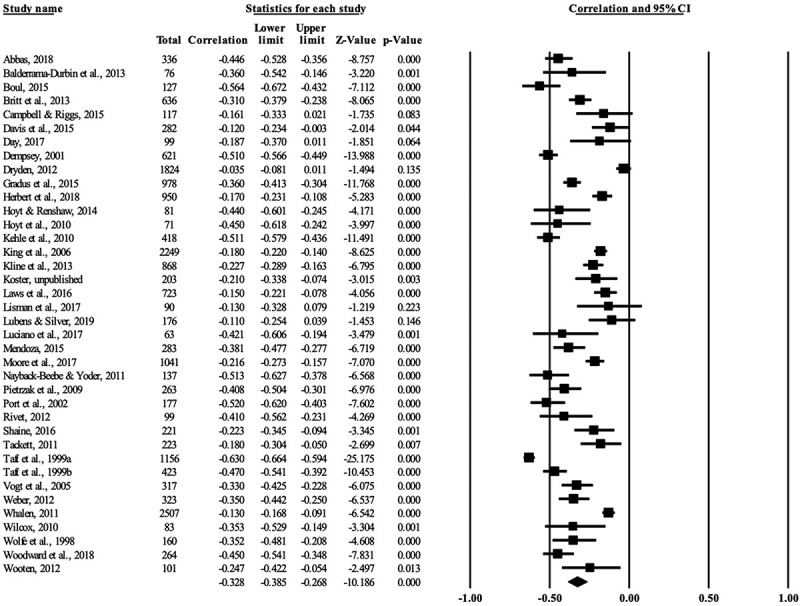
Effect size plot of random effects
Figure 3.
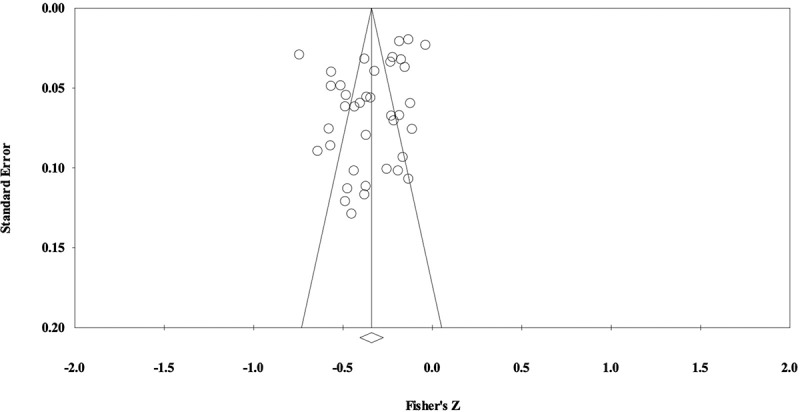
Funnel plot of random effects
2.3. Moderator analyses
2.3.1. Methodological characteristics
Several methodological and measurement moderators were tested to better understand the heterogeneity of the effect size estimate. These methodological moderators were considered to be metrics of data quality and included (1) whether data were published in a peer-reviewed journal, (2) whether the effect size was reported in the manuscript, (3) the year of publication, and (4) the quality measure developed for this study. Measurement moderators included (1) use of a validated measure of social support, (2) version of the DSM used to define PTSD, and (3) PTSD measure used. Categorical moderators are shown in Table 2 and continuous moderators are shown in Table 3. Date of publication was significant such that effect sizes decreased over time (see Figure 4 for a scatterplot). Studies that used the DSM-III definition of PTSD had larger effect sizes relative to DSM-IV or DSM 5. The PTSD measure used was also significant such that the Mississippi Scale for Combat-Related PTSD (Keane, Caddell, & Taylor, 1988; Norris & Perilla, 1996) had larger effect sizes relative to other measures of PTSD. Publication in peer-reviewed journals, whether the effect size was reported in the manuscript, whether the measure of social support was validated, and our quality measure were not significant predictors of effect size.
Table 2.
Moderator analyses of categorical methodological characteristics
| Moderator | Neffects | r | 95% CI | Q (df) |
|---|---|---|---|---|
| Dissertation/unpublished data | 0.20(1) | |||
| Yes | 12 | −0.31 | −0.41, −0.20 | |
| No | 26 | −0.34 | −0.40, −0.27 | |
| Effect size reported in article | 1.44(1) | |||
| Yes | 26 | −0.35 | −0.42, −0.27 | |
| No | 12 | −0.28 | −0.35, −0.21 | |
| DSM definition used | 17.61(2)*** | |||
| DSM-III | 5 | −0.51 | −0.60, −0.41 | |
| DSM-IV | 29 | −0.30 | −0.35, −0.25 | |
| DSM-5 | 4 | −0.22 | −0.31, −0.12 | |
| PTSD measure used | 34.94(2)*** | |||
| PCL | 31 | −0.31 | −0.35, −0.26 | |
| Mississippi | 5 | −0.51 | −0.60, −0.41 | |
| Other | 2 | −0.07 | −0.17, 0.04 | |
| Social support measurea | 0.24(1) | |||
| Validated | 30 | −0.32 | −0.37, −0.26 | |
| Author developed/single item | 6 | −0.37 | −0.56, −0.15 |
Note: PCL = PTSD Checklist, Mississippi = Mississippi Scale for Combat-related PTSD.
aStudies (n = 2) were excluded from this analysis if they included both validated and author-developed/single item measures of social support.
*p <.05, **p <.01, ***p <.001
Table 3.
Meta-regressions of continuous moderators
| Moderator | Neffects | Coef. | SE | Z | p | R2 analog |
|---|---|---|---|---|---|---|
| Publication date | 37 | 0.0140 | 0.0052 | 2.67 | 0.008 | 0.23 |
| Study quality | 37 | −0.0302 | 0.0248 | −1.22 | 0.223 | 0.11 |
| Mean Age | 31 | −0.0069 | 0.0033 | −2.07 | 0.038 | 0.30 |
| % Female | 36 | −0.0003 | 0.0010 | −0.33 | 0.740 | 0.00 |
| % Married/Cohabitating | 24 | −0.0008 | 0.0016 | −0.49 | 0.626 | 0.00 |
| % White | 34 | 0.0009 | 0.0014 | 0.68 | 0.499 | 0.00 |
Figure 4.
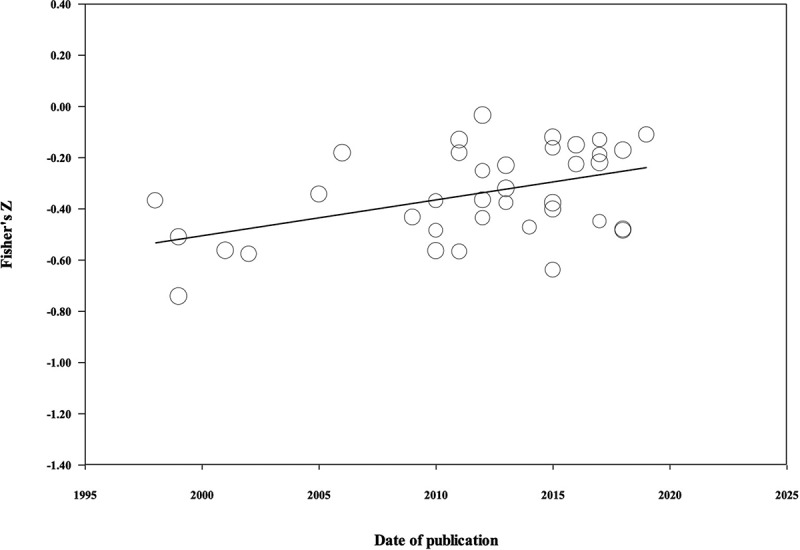
Random effect sizes by publication date
The three significant data quality measures (publication date, version of DSM used to define PTSD, and PTSD measure) were subsequently included as simultaneous predictors in a meta-regression to identify which variables were unique predictors of effect size. The regression was unable to be computed because the predictors revealed a high degree of multicollinearity. A review of the studies revealed that investigations that used the DSM-III definition of PTSD largely used the Mississippi Scale for Combat-Related PTSD and studies that used DSM-IV and 5 definitions largely used versions of the PCL. Moreover, studies published earlier used the DSM-III definition of PTSD and subsequent studies utilized the DSM-IV or 5. Given these overlaps, we opted to covary only for the version of the DSM utilized in subsequent meta-regression analyses. We chose this variable because changes in the actual definition of PTSD was the most theoretically plausible driver of changes in the relationship between social support and PTSD over time.
2.4. Substantive moderator analyses
Next, we conducted substantive moderator analyses examining demographic, social support, and military service characteristics as possible moderators of effect size. We first determined whether the moderator was significantly associated with effect size. Moderators that were significantly associated with effect size were then subjected to a meta-regression adjusted for the version of the DSM used. Continuous moderators are shown in Table 3 and categorical moderators are shown in Table 4.
Table 4.
Moderator analyses of social support and military service characteristics
| Moderator | Neffects | r | 95% CI | Q (df) |
|---|---|---|---|---|
| Social support type† | 4.07(2) | |||
| Perceived | 31 | −0.36 | −0.43, −0.29 | |
| Enacted | 3 | −0.23 | −0.39, −0.07 | |
| Structural | 9 | −0.26 | −0.33, −0.19 | |
| Social support source† | 8.27(1)*** | |||
| Military | 16 | −0.24 | −0.30, −0.18 | |
| Non-military | 32 | −0.38 | −0.45, −0.31 | |
| Social Support Timing | 4.76(1)*** | |||
| During deployment | 11 | −.26 | −.31, −.19 | |
| Outside deployment | 33 | −.36 | −.43, −.29 | |
| NG/R Service | 0.23(2) | |||
| Not NG/R | 7 | −0.24 | −0.26, −0.21 | |
| NG/R | 8 | −0.31 | −0.34, −0.27 | |
| Mixed Sample | 13 | −0.27 | −0.30, −0.25 | |
| Discharged | 0.92(2) | |||
| Not discharged | 14 | −0.32 | −0.39, −0.25 | |
| Discharged | 10 | −0.38 | −0.50, −0.25 | |
| Mixed Sample | 5 | −0.37 | −0.48, −0.25 | |
| Deployment-era | 14.14(2)*** | |||
| Vietnam | 3 | −0.54 | −0.64, −0.43 | |
| Persian Gulf | 3 | −0.28 | −0.40, −0.15 | |
| OEF/OIF/OND | 28 | −0.30 | −0.36, −0.24 |
Note: NG/R = National Guard/Reserve. OEF/OIF/OND = Operational Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn.
†For moderators in which different categories were represented within a single study, we used a shifting unit-of-analysis approach (Cooper, 2010).
*p <.05, **p <.01, ***p <.001
2.4.1. Demographic characteristics
Age was significantly associated with effect size such that as age increased, effect size decreased. A review of the scatterplot revealed the presence of an outlier. When the outlier was removed, the effect only approached significance (p = .07). When age and the version of the DSM utilized were entered into a meta-regression together, age was no longer significantly associated with effect size (coefficient: −.00, standard error [SE]: .00, 95% confidence interval [CI] = −.01, .00, Z = −.82, p = .41). Race, sex, and marital status were not significantly associated with effect size.
2.4.2. Social support characteristics
Perceptions of social support from military versus non-military sources were significantly associated with effect size such that social support perceived from non-military sources (r = −.38) had a larger effect size relative to social support perceived from military sources (r = −.24). This effect remained significant after accounting for the version of the DSM used (see Table 5). Social support timing was also significantly associated with effect size such that perceptions of social support received outside of deployment (r = −.36) had a larger effect size relative to perceptions of social support received during deployment (r = −.26). This effect only trended towards significance (coefficient: .10, SE: .06, 95% CI = −.02, .21, Z = 1.67, p = .09) after accounting for the version of the DSM used. Social support type was not significantly associated with effect size. There was only one study that measured social negativity, precluding us from including social negativity in analyses. Notably, the largest effect size was observed for social negativity (r = −.58).
Table 5.
Meta-regression of Social Support Source Adjusting for Covariates
| Variable | Coef. | SE | 95% CI | Z | p | Q(df) |
|---|---|---|---|---|---|---|
| DSM definition of PTSD measure (ref = III) | 10.35(2)** | |||||
| DSM-IV | 0.20 | 0.07 | 0.07, 0.33 | 3.09 | 0.002 | |
| DSM-5 | 0.24 | 0.09 | 0.05, 0.42 | 2.55 | 0.011 | |
| Social support source (ref = non-military) † | 0.14 | 0.05 | 0.04, 0.24 | 2.79 | 0.005 |
Note: Neffects = 48.
†For moderators in which different categories were represented within a single study, we used a shifting unit-of-analysis approach (Cooper, 2010).
*p <.05, **p <.01, *** p <.001
2.4.3. Military service characteristics
National Guard/Reserve service, discharge status, and deployment-era were examined as predictors of effect size. Deployment-era was significantly associated with effect size. The largest effect was observed for service in the Vietnam era (r = .54), followed by OEF/OIF/OND (r = .30) and Persian Gulf (r = .28). When deployment-era and the version of the DSM utilized were entered into a meta-regression, both DSM and deployment-era were not significantly associated with effect size (see Table 6). National Guard/Reserve service and discharge status were not significantly associated with effect size.
Table 6.
Meta-regression of Deployment Era Adjusting for Covariates
| Variable | Coef. | SE | 95% CI | Z | p | Q(df) |
|---|---|---|---|---|---|---|
| DSM definition of PTSD measure (ref = III) | 0.83(2) | |||||
| DSM-IV | 0.11 | 0.20 | −0.28, 0.50 | 0.55 | 0.58 | |
| DSM-5 | 0.19 | 0.23 | −0.26, 0.63 | 0.83 | 0.41 | |
| Deployment Era (ref = OEF/OIF/OND) | 1.89(2) | |||||
| Vietnam | −0.18 | 0.22 | −0.61, 0.25 | −0.81 | 0.42 | |
| Persian Gulf | 0.06 | 0.11 | −0.16, 0.28 | 0.53 | 0.60 | |
| Deployment Era (ref = Vietnam) | ||||||
| Persian Gulf | 0.24 | 0.19 | −0.13, 0.61 | 1.27 | 0.21 | |
| OEF/OIF/OND | 0.18 | 0.22 | −0.25, 0.61 | 0.81 | 0.42 |
Note: Neffects = 34 OEF/OIF/OND = Operation Enduring Freedom/Operation Iraqi Freedom/Operational New Dawn.
*p <.05, **p <.01, *** p <.001
3. Discussion
Given evidence that social support is a particularly strong buffer against PTSD severity among veterans and military service members (Zalta et al., 2020), we sought to identify moderators of this association within U.S. military samples. The current meta-analysis identified 37 studies for inclusion with 38 unique samples that together comprised 18,766 individuals and 60 effect sizes. Consistent with effect sizes observed in previous meta-analyses not circumscribed to military samples (rs −.27 to −.40; Brewin et al., 2000; Ozer et al., 2003; Zalta et al., 2020), the overall weighted cross-sectional effect size between PTSD symptom severity and social support in the current meta-analysis was moderate, r = −.33, with a fair degree of heterogeneity.
Although support from both military and non-military sources demonstrated a significant relationship between social support and PTSD, support perceived from non-military sources had a significantly larger effect size relative to support received from military sources, even after accounting for covariates. Support received outside of deployment, which was typically assessed from non-military sources, also had a larger effect size than support received during deployment, though this effect was not significant after accounting for methodological covariates. Our results highlight the utility of support received from civilians and challenges assumptions of the Matching Hypothesis (Cohen & Wills, 1985), which suggests that support would be most beneficial when received from a similar other. The benefits of civilian support relative to military supports may also help to explain why service in non-active duty service components (i.e., National Guard/Reserve) was not a significant moderator.
Our analysis of cross-sectional effect sizes prohibits us from determining the direction of the relationship between social support and PTSD. However, the current findings point to several potential clinical implications. Research shows that higher PTSD symptoms can prevent service members from seeking social support from civilians after return from deployment (Blais, Renshaw, & Jakupcak, 2014). Thus, interventions aimed at encouraging VSMs to seek support from their civilian peers and overcoming barriers to support seeking may be beneficial. This may include psychoeducation underscoring the particular utility of civilian peer support or behavioural activation strategies focused on enhancing contact with non-military support sources. Additionally, interventions targeting civilian supporters of VSMs, particularly in the post-deployment period, may help to buffer against the development of PTSD. For example, programmes such as Coaching Into Care, which helps loved ones of VSMs facilitate psychological help-seeking, may be beneficial (Sayers, Hess, Whitted, Straits-Troster, & Glynn, 2020).
Unexpectedly, the type of social support (i.e., perceived, enacted, structural) did not moderate the association of PTSD and social support, which differs from previous research (see review, Finch, Okun, Pool, & Ruehlman, 1999; Zalta et al., 2020). This suggests that VSMs benefit from many different types of support and that more objective forms of support (e.g., enacted support) may be more beneficial among military than civilian populations. This is consistent with the military ethos of taking action in the service of supporting and protecting others. However, it is also important to note that our analysis relied on relatively few studies examining enacted and structural support, contributing to relatively large confidence intervals for these groups. Moreover, only one study that examined negative social support was identified, precluding its inclusion in moderator analyses. The effect size observed in this single study was the largest of all effect sizes, suggesting that negative social support may be particularly damaging for VSMs, consistent with what has been shown in civilian populations (Zalta et al., 2020). Future research in the area of support type, particularly negative social support among VSMs, is warranted.
Initial analyses revealed that service era and age were significantly associated with effect size, but were no longer significant after removing an outlier or covarying for the version of DSM used. Demographic variables of sex, race, and marital status were also not significant predictors of effect size. Of note, we had a fairly good representation of studies with female veterans. On average, studies included 27% of female participants, which represents a larger percentage than the estimated 16.5% of service members who are women (Department of Defense, 2018). We also had a fairly good representation of minorities; on average, studies included 69% White participants with a large standard deviation (21.0%). Marital status was also well-represented in the data with studies ranging from 23–100% of participants cohabitating and an average of 58% married/cohabitating participants across studies. Overall, these null findings highlight that the association of social support and PTSD does not vary meaningfully across specific VSM demographics, suggesting that all VSMs may benefit from efforts to enhance social support.
We identified several methodological variables that were significantly associated with the effect size. Publication date, the DSM version, and the PTSD measure used were significantly associated with effect size such that effect sizes decreased over time, DSM-III had the largest effect size relative to later versions of the DSM, and the Mississippi Scale for Combat-Related PTSD (Keane et al., 1988; Norris & Perilla, 1996) had larger effect sizes relative to other measures of PTSD. However, when all three of these variables were entered into a meta-regression, the regression was unable to be computed because the predictors revealed a high degree of multicollinearity. We expect that these factors were associated with the effect size due to changes in how PTSD was defined over time. The Mississippi Scale for Combat-Related PTSD also queries about conditions associated with PTSD, such as substance misuse, depression, and tendencies towards suicide. Thus, the effect we observed with this scale may be capturing more global distress and dysfunction experienced by VSMs, which may account for the larger effect size.
We had initially sought out to explore the role of exposure to MST as a potential moderator of the association of PTSD and social support, but there were not enough studies that reported rates of MST, and when it was reported, there was little consistency in its measurement. Given the impact of MST on personal and interpersonal function (e.g., Blais et al., 2019, 2018; Kimerling et al., 2007), it is critical that future studies of VSMs more consistently report the proportion of individuals exposed to MST to allow for greater exploration of the role of MST in future meta-analyses. Indeed, extant literature shows that survivors of sexual violence experience negative social reactions to disclosing their traumas and these reactions are associated with higher levels of distress (e.g., Hakimi, Bryant-Davis, Ullman, & Gobin, 2018). Additionally, VSM in particular, have reported not disclosing MST in fear of retaliation or negatively impacting their units during service (Blais, Brignone, Fargo, Galbreath, & Gundlapalli, 2018). Coupled with the observation that social negativity is understudied in VSM samples, a need for research examining how sexual violence experienced during military service relates to PTSD and social support is critically needed.
The current meta-analysis is not without methodological limitations. We focused on PTSD severity instead of diagnoses of PTSD and therefore opted to focus on self-report measures of PTSD and social support. It is possible that the use of clinician administered measures and analyses based on diagnosis may lead to different results. Notably, the two previous meta-analyses conducted on military service members and veterans (Wright et al., 2013; Xue et al., 2015) focused on diagnoses so our approach adds novel information to the literature. We also examined only cross-sectional effect sizes because there were not a sufficient number of longitudinal effect sizes to evaluate moderators; therefore, we cannot determine the direction of causality between social support and PTSD symptoms. Research shows a strong bi-directional relationship between PTSD and social support (e.g., Platt, Lowe, Galea, Norris, & Koenen, 2016; Ullman & Peter-Hagene, 2016). Further research is needed to determine whether the study findings can be replicated with longitudinal data. Some of our moderators (e.g., era of service [Vietnam, n = 3]) had only a few studies to include in statistical analyses. As such, these results may be considered preliminary and worthy of follow-up investigation. Finally, initial kappa scores between raters for quality ratings were not retained. Any discrepancies were discussed between the two raters and when consensus could not be reached, the senior author arbitrated until a rating was agreed upon. Thus, all ratings were consistent across raters before or after arbitration.
We also made specific decisions regarding the inclusion of samples that limit the generalizability of our results. To prevent a restriction of range in PTSD severity which could artificially reduce the correlation between social support and PTSD, we opted not to include clinical studies of individuals with diagnosed PTSD or participants recruited from mental health clinics. That said, it is possible that some participants whose data were included in the current meta-analysis were seeking treatment outside of their respective studies. Since our studies excluded clinical samples, it is possible that the estimate observed does not generalize to clinical samples of VSMs. Future meta-analyses may extend this area by including treatment-seeking as a moderator of the association of PTSD and social support. Studies were also restricted to U.S. VSMs and articles published in English. This means that our findings should not be generalized to non-U.S. samples. It is possible that excluding studies not written in English could have excluded studies that were otherwise eligible for inclusion. The literature on PTSD and social support would be greatly strengthened by a meta-analysis that included non-U.S. military samples and articles published in languages other than English to determine if country of origin or language in which the article was published moderates this association.
Our study is the first meta-analysis to explore moderators of the association between social support and PTSD symptoms among non-clinical samples of U.S. VSMs. Although findings point to important moderating factors (i.e., military v. civilian social support), they also call out some notable gaps in the literature on social negativity and the impact of social support among VSMs exposed to military sexual trauma. Given the particularly robust relationship between social support and PTSD severity among VSMs, including the veterans returning from our ongoing conflicts, these areas of study warrant further exploration.
Acknowledgments
The authors would like to thank Cara Knoeppel, Randy Boley, Jade Cooper, Karyna Bravo, Alexis Blacketer, Laura Cabebe, Jazmin Martinez, Katherine Lucas, Maryam Foroohi, Ramona Martinez, and Kelci Straka for their assistance with the systematic search.
Funding Statement
Philip Held is supported by a career development award from the National Center for Advancing Translational Sciences of the National Institutes of Health (5KL2TR002387-03), and receives grant support from Wounded Warrior Project, and the Boeing Company. Alyson Zalta’s contribution was supported by a career development award from the National Institute of Mental Health (K23 MH103394). The views expressed herein are those of the authors and do not represent the official views of the institutions at which the authors are employed or the institutions that provide funding;NIH [K23 MH103394];NIH [5KL2TR002387-03].
Note
Searches were switched from Embase to PubMed for the updated and expanded 2019 search as Embase was no longer available at Rush University Medical Center or the University of California, Irvine.
Disclosure statement
The authors have no conflicts of interest to disclose.
Data Availability
Data used in the current study can be found here: https://osf.io/2nrj3/?view_only=17ef61829d324634a9100d4e32af1926
References
*References marked with an asterisk indicate studies included in the meta-analysis.
- *Abbas, M. (2018). Examining the dimensions of social support and warfare exposure as predictors of PTSD symptoms among National Guard service members over time (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 10933379). [Google Scholar]
- American Psychiatric Association . (1980). Diagnostic and statistical manual of mental disorders (3rd ed. ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed. ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- *Balderrama-Durbin, C., Snyder, D. K., Cigrang, J., Talcott, G. W., Tatum, J., Baker, M., … Smith Slep, A. M. (2013). Combat disclosure in intimate relationships: Mediating the impact of partner support on posttraumatic stress. Journal of Family Psychology, 27(4), 560–17. [DOI] [PubMed] [Google Scholar]
- Blais, R. K. (2019). Lower sexual satisfaction and function mediate the association of assault military sexual trauma and relationship satisfaction in partnered female service members/veterans. Family Process. doi: 10.1111/famp.12449 [DOI] [PubMed] [Google Scholar]
- Blais, R. K., Brignone, E., Fargo, J. D., Galbreath, N. W., & Gundlapalli, A. V. (2018). Assailant identity and self-reported nondisclosure of military sexual trauma in partnered women veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 10(4), 470–474. [DOI] [PubMed] [Google Scholar]
- Blais, R. K., Brignone, E., Fargo, J. D., Livingston, W. S., & Andresen, F. J. (2019). The importance of distinguishing between harassment-only and assault military sexual trauma during screening. Military Psychology, 31(3), 227–232. [Google Scholar]
- Blais, R. K., Geiser, C., & Cruz, R. A. (2018). Specific PTSD symptom clusters mediate the association of military sexual trauma severity and sexual function and satisfaction in female service members/veterans. Journal of Affective Disorders, 238, 680–688. [DOI] [PubMed] [Google Scholar]
- Blais, R. K., Renshaw, K. D., & Jakupcak, M. (2014). Posttraumatic stress and stigma in active‐duty service members relate to lower likelihood of seeking support. Journal of Traumatic Stress, 27(1), 116–119. [DOI] [PubMed] [Google Scholar]
- Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., & Forneris, C. A. (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. [DOI] [PubMed] [Google Scholar]
- *Boul, S. J. (2015). From combat to classroom: An examination of combat trauma’s effects on military veteran’s relationships and adjustment to college (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 3745534). [Google Scholar]
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. [DOI] [PubMed] [Google Scholar]
- *Britt, T. W., Adler, A. B., Bliese, P. D., & Moore, D. (2013). Morale as a moderator of the combat exposure‐PTSD symptom relationship. Journal of Traumatic Stress, 26(1), 94–101. [DOI] [PubMed] [Google Scholar]
- *Campbell, R., & Riggs, S. A. (2015). The role of psychological symptomatology and social support in the academic adjustment of previously deployed student veterans. Journal of American College Health, 63(7), 473–481. [DOI] [PubMed] [Google Scholar]
- Caska, C. M., Smith, T. W., Renshaw, K. D., Allen, S. N., Uchino, B. N., Birmingham, W., & Carlisle, M. (2014). Posttraumatic stress disorder and responses to couple conflict: Implications for cardiovascular risk. Health Psychology, 33(11), 1273–1280. [DOI] [PubMed] [Google Scholar]
- Ciampaglia, D. A. (2019, March 29). Why were Vietnam War vets treated poorly when they returned? History. https://www.history.com/news/vietnam-war-veterans-treatment
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. [DOI] [PubMed] [Google Scholar]
- Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. [PubMed] [Google Scholar]
- Coleman, J. A., Ingram, K. M., & Sheerin, C. M. (2019). Racial differences in posttraumatic stress disorder symptoms among African American and Caucasian male veterans. Traumatology, 25(4), 297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, H. M. (2010). Research synthesis and meta-analysis: A step-by-step approach (4th ed. ed.). Los Angeles, CA: Sage. [Google Scholar]
- *Dempsey, C. L. (2001). Post-traumatic stress disorder symptomatology among American Indian Vietnam veterans: Mediators and moderators of the stress-illness relationship (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 3021498). [Google Scholar]
- *Davis, L., Hanson, S. K., Zamir, O., Gewirtz, A. H., & DeGarmo, D. S. (2015). Associations of contextual risk and protective factors with fathers parenting practices in the postdeployment environment. Psychological Services, 12(3), 250–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Day, M. A. (2017). The role of social support during post-deployment reintegration in the army national guard (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 10684084). [Google Scholar]
- Department of Defense . (2018). 2018 Demographics Profile, Active Duty Members. Retrieved from: https://download.militaryonesource.mil/12038/MOS/Infographic/2018-demographics-active-duty-members.pdf
- *Dryden, A. E. (2012). The effects of combat exposure on post-deployment coping deficits in OEF/OIF/OND veterans (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 3529752). [Google Scholar]
- Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics, 56(2), 455–463. [DOI] [PubMed] [Google Scholar]
- Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315(7109), 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch, J. F., Okun, M. A., Pool, G. J., & Ruehlman, L. S. (1999). A comparison of the influence of conflictual and supportive social interactions on psychological distress. Journal of Personality, 67(4), 581–621. [DOI] [PubMed] [Google Scholar]
- Gibbons, S. W., Hickling, E. J., Barnett, S. D., Herbig-Wall, P. L., & Watts, D. D. (2012). Gender differences in response to deployment among military healthcare providers in Afghanistan and Iraq. Journal of Womens’ Health, 21, 496–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Gradus, J. L., Smith, B. N., & Vogt, D. (2015). Family support, family stress, and suicidal ideation in a combat-exposed sample of operation enduring freedom/operation Iraqi freedom veterans. Anxiety, Stress & Coping: An International Journal, 28(6), 706–715. [DOI] [PubMed] [Google Scholar]
- Granado, N. S., Zimmermann, L., Smith, B., Jones, K. A., Wells, T. S., Ryan, M. A. K., … Smith, T. C. (2012). Individual augmentee deployment and newly reported mental health morbidity. Journal of Occupational and Environmental Medicine, 54(5), 615–620. [DOI] [PubMed] [Google Scholar]
- Grubbs, F. E. (1969). Procedures for detecting outlying observations in samples. Technometrics, 11(1), 1–21. [Google Scholar]
- Hakimi, D., Bryant-Davis, T., Ullman, S. E., & Gobin, R. L. (2018). Relationship between negative social reactions to sexual assault disclosure and mental health outcomes of Black and White female survivors. Psychological Trauma: Theory, Research, Practice, and Policy, 10(3), 270–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, S. C., Castro, F., Lee, L. O., Charney, M. E., Marx, B. P., Brailey, K., … Vasterling, J. J. (2014). Military unit support, postdeployment social support, and PTSD symptoms among active duty and National Guard soldiers deployed to Iraq. Journal of Anxiety Disorders, 28(5), 446–453. [DOI] [PubMed] [Google Scholar]
- *Herbert, M. S., Leung, D. W., Pittman, J. O. E., Floto, E., & Afari, N. (2018). Race/ethnicity, psychological resilience, and social support among OEF/OIF combat veterans. Psychiatry Research, 265, 265–270. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22. [DOI] [PubMed] [Google Scholar]
- *Hoyt, T., Pasupathi, M., Smith, B. W., Yeater, E. A., Kay, V. S., & Tooley, E. (2010). Disclosure of emotional events in groups at risk for posttraumatic stress disorder. International Journal of Stress Management, 17(1), 78–95. [Google Scholar]
- *Hoyt, T., & Renshaw, K. D. (2014). Emotional disclosure and posttraumatic stress symptoms: Veteran and spouse reports. International Journal of Stress Management, 21(2), 186–206. [Google Scholar]
- Institute of Medicine . (2012). Treatment for posttraumatic stress disorder in military and veteran populations: Final assessment. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Keane, T. M., Caddell, J. M., & Taylor, K. L. (1988). Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: Three studies in reliability and validity. Journal of Consulting and Clinical Psychology, 56(1), 85–90. [DOI] [PubMed] [Google Scholar]
- *Kehle, S. M., Polusny, M. A., Murdoch, M., Erbes, C. R., Arbisi, P. A., Thuras, P., & Meis, L. A. (2010). Early mental health treatment-seeking among U.S. national guard soldiers deployed to Iraq. Journal of Traumatic Stress, 23(1), 33–40. [DOI] [PubMed] [Google Scholar]
- Kimerling, R., Gima, K., Smith, M. W., Street, A., & Frayne, S. (2007). The Veterans Health Administration and military sexual trauma. American Journal of Public Health, 97(12), 2160–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *King, D. W., Taft, C., King, L. A., Hammond, C., & Stone, E. R. (2006). Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology, 36(12), 2980–2992. [Google Scholar]
- *Kline, A., Ciccone, D. S., Weiner, M., Interian, A., Hill, L. S., Falca-Dodson, M., … Losonczy, M. (2013). Gender differences in the risk and protective factors associated with PTSD: A prospective study of national guard troops deployed to Iraq. Psychiatry: Interpersonal and Biological Processes, 76, 256–272. [DOI] [PubMed] [Google Scholar]
- *Koster, M. L. (2019). [Social support, religion, PTSD, and moral injury among service members and veterans]. Unpublished raw data. [Google Scholar]
- *Laws, H., Mazure, C. M., McKee, S. A., Park, C. L., & Hoff, R. (2016). Within-unit relationship quality mediates the association between military sexual trauma and posttraumatic stress symptoms in veterans separating from military service. Psychological Trauma: Theory, Research, Practice, and Policy, 8(5), 649–656. [DOI] [PubMed] [Google Scholar]
- Lehavot, K., Beckman, K. L., Chen, J. A., Simpson, T. L., & Williams, E. C. (2019). Race/ethnicity and sexual orientation disparities in mental health, sexism, and social support among women veterans. Psychology of Sexual Orientation and Gender Diversity, 6(3), 347–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Lisman, R., Currier, J. M., & Harris, J. I. (2017). Religion and cognitive processing of trauma among newly returned US Iraq and Afghanistan veterans. Mental Health, Religion & Culture, 20(7), 603–616. [Google Scholar]
- *Lubens, P., & Silver, R. C. (2019). U.S. combat veterans responses to suicide and combat deaths: A mixed-methods study. Social Science & Medicine, 236, 112341. [DOI] [PubMed] [Google Scholar]
- *Luciano, M. T., & McDevitt-Murphy, M. E. (2017). Posttraumatic stress and physical health functioning: Moderating effects of deployment and postdeployment social support in OEF/OIF/OND veterans. Journal of Nervous and Mental Disease, 205(2), 93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mendoza, M. A. (2015). Predictors of posttraumatic growth among combat veterans (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 3664484). [Google Scholar]
- Meyer, I. (2003). Prejudice, social support, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Moore, T. M., Risbrough, V. B., Baker, D. G., Larson, G. E., Glenn, D. E., Nievergelt, C. M., … Gur, R. C. (2017). Effects of military service and deployment on clinical symptomatology: The role of trauma exposure and social support. Journal of Psychiatric Research, 95, 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Nayback-Beebe, A. M., & Yoder, L. H. (2011). Social conflict versus social support: What is more influential in mental health symptom severity for female service members? Archives of Psychiatric Nursing, 25(6), 469–478. [DOI] [PubMed] [Google Scholar]
- Norris, F. H., & Perilla, J. L. (1996). The Revised Civilian Mississippi Scale for PTSD: Reliability, validity, and cross-language stability. Journal of Traumatic Stress, 9(2), 285–298. [DOI] [PubMed] [Google Scholar]
- Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73. [DOI] [PubMed] [Google Scholar]
- Paley, B., Lester, P., & Mogil, C. (2013). Family systems and ecological perspectives on the impact of deployment on military families. Clinical Child and Family Psychology Review, 16(3), 245–265. [DOI] [PubMed] [Google Scholar]
- *Pietrzak, R. H., Johnson, D. C., Goldstein, M. B., Malley, J. C., & Southwick, S. M. (2009). Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatric Services, 60(8), 1118–1122. [DOI] [PubMed] [Google Scholar]
- Platt, J. M., Lowe, S. R., Galea, S., Norris, F. H., & Koenen, K. C. (2016). A longitudinal study of the bidirectional relationship between social support and posttraumatic stress following a natural disaster. Journal of Traumatic Stress, 29(3), 205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polusny, M. A., Kumpula, M. J., Meis, L. A., Erbes, C. R., Arbisi, P. A., Murdoch, M., … Johnson, A. K. (2014). Gender differences in the effects of deployment-related stressors and pre-deployment risk factors on the development of PTSD symptoms in National Guard Soldiers deployed to Iraq and Afghanistan. Journal of Psychiatric Research, 49, 1–9. [DOI] [PubMed] [Google Scholar]
- *Port, C. L., Engdahl, B., Frazier, P., & Eberly, R. (2002). Factors related to the long-term course of PTSD in older ex-prisoners of war. Journal of Clinical Geropsychology, 8(3), 203–214. [Google Scholar]
- *References marked with an asterisk indicate studies included in the meta-analysis.
- *Rivet, M. A. (2012). An online investigation of the experiences of stress and prevalence of posttraumatic stress disorder for female armed service personnel returning from Iraq and Afghanistan: Understanding their needs and implications for intervention (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 3494838). [Google Scholar]
- Rook, K. S., & Pietromonaco, P. (1987). Close Relationship: Ties That Heal or Ties that Bind? Advances in Personal Relationships, 1, 1–35. [Google Scholar]
- Sayers, S. L., Hess, T. H., Whitted, P., Straits-Troster, K. A., & Glynn, S. M. (2020). Coaching into Care: A VA-funded telephone based service for concerned family members of military veterans. Psychiatric Services. doi: 10.1176/appi.ps.201900113 [DOI] [PubMed] [Google Scholar]
- Seal, K. H., Bertenthal, D., Miner, C. R., Sen, S., & Marmar, C. (2007). Bringing the war back home: Mental health disorders among 103,788 U.S. veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Archives of Internal Medicine, 167(5), 476–482. [DOI] [PubMed] [Google Scholar]
- *Shaine, M. J. D. (2016). Exploring on-campus peer social support as a mediator between attachment and posttraumatic stress in military and veteran students (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 10096687). [Google Scholar]
- Shand, L. K., Cowlishaw, S., Brooker, J. E., Burney, S., & Ricciardelli, L. A. (2015). Correlates of post‐traumatic stress symptoms and growth in cancer patients: A systematic review and meta‐analysis. Psycho‐Oncology, 24(6), 624–634. [DOI] [PubMed] [Google Scholar]
- *Taft, C. T., Stern, A. S., King, L. A., & King, D. W. (1999). Modeling physical health and functional health status: The role of combat exposure, posttraumatic stress disorder and personal resource attributes. Journal of Traumatic Stress, 12(1), 3–23. [DOI] [PubMed] [Google Scholar]
- *Tackett, D. P. (2011). Resilience factors affecting the readjustment of national guard soldiers returning from deployment (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 10807633). [Google Scholar]
- Terrin, N., Schmid, C. H., Lau, J., & Olkin, I. (2003). Adjusting for publication bias in the presence of heterogeneity. Statistics in Medicine, 22(13), 2113–2126. [DOI] [PubMed] [Google Scholar]
- Ullman, S. E., & Peter-Hagene, L. C. (2016). Longitudinal relationships of social reactions, PTSD, and revictimization in sexual assault survivors. Journal of Interpersonal Violence, 31(6), 1074–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasterling, J. J., Proctor, S. P., Friedman, M. J., Hoge, C. W., Heeren, T., King, L. A., & King, D. W. (2010). PTSD symptom increases in Iraq-deployed soldiers: Comparison with non-deployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress, 23(1), 41–51. [DOI] [PubMed] [Google Scholar]
- *Vogt, D. S., Pless, A. P., King, L. A., & King, D. W. (2005). Deployment stressors, gender, and mental health outcomes among Gulf War I veterans. Journal of Traumatic Stress, 18(2), 115–127. [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993, October). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. In Annual convention of the International Society for Traumatic Stress Studies, San Antonio, TX (Vol. 462). [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD. www.ptsd.va.gov
- *Wilcox, S. (2010). Social relationships and PTSD symptomatology in combat veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 2(3), 175–182. [Google Scholar]
- *Whalen, R. J. (2011). Individual- and unit-level coping among combat veterans subject to army force stabilization system personnel policy (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 3469106). [Google Scholar]
- *Weber, D. J. (2012). Academic success and well-being following OEF/OIF deployment (Doctoral Dissertation). ProQuest Dissertations and Theses database (UMI No. 3495315). [Google Scholar]
- Wilson, L. C. (2018). The prevalence of military sexual trauma: A meta-analysis. Trauma, Violence & Abuse, 19(5), 584–597. [DOI] [PubMed] [Google Scholar]
- *Wolfe, J., Sharkansky, E. J., Read, J. P., Dawson, R., Martin, J. A., & Ouimette, P. C. (1998). Sexual harassment and assault as predictors of PTSD symptomatology among U.S. female Persian Gulf War military personnel. Journal of Interpersonal Violence, 13(1), 40–57. [Google Scholar]
- *Wooten, N. R. (2012). Deployment cycle stressors and post-traumatic stress symptoms in army national guard women: The mediating effect of resilience. Social Work in Health Care, 51(9), 828–849. [DOI] [PubMed] [Google Scholar]
- *Woodward, M. J., Morissette, S. B., Kimbrel, N. A., Meyer, E. C., DeBeer, B. B., Gulliver, S. B., & Beck, J. G. (2018). A cross-lagged panel approach to understanding social support and chronic posttraumatic stress disorder symptoms in veterans: Assessment modality matters. Behavior Therapy, 49(5), 796–808. [DOI] [PubMed] [Google Scholar]
- Wright, B. K., Kelsall, H. L., Sim, M. R., Clarke, D. M., & Creamer, M. C. (2013). Support mechanisms and vulnerabilities in relation to PTSD in veterans of the Gulf War, Iraq War, and Afghanistan deployments: A systematic review. Journal of Traumatic Stress, 26(3), 310–318. [DOI] [PubMed] [Google Scholar]
- Xue, C., Ge, Y., Tang, B., Liu, Y., Kang, P., Wang, M., & Zhang, L. (2015). A meta-analysis of risk factors for combat-related PTSD among military personnel and veterans. PLoS ONE, 10(3), 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalta, A. K., Tirone, V., Orlowska, D., Blais, R. K., Lofgreen, A., Klassen, B., ... & Dent, A. L, . (2020). Examining moderators of the relationship between social support and self-reported PTSD symptoms: A meta-analysis. Psychological Bulletin. Advance online publication. doi: 10.1037/bul0000316. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used in the current study can be found here: https://osf.io/2nrj3/?view_only=17ef61829d324634a9100d4e32af1926


