Abstract
Background: The COVID-19 outbreak has major psychosocial consequences on the global population and specialists report that youth may be significantly impacted. Adolescents and young adults, for whom social life is an important protective factor, had to face a new isolation caused by social distancing and home schooling. This study aims to explore youth's profiles of adaptation to COVID-19 pandemic in the province of Quebec, Canada, and the risk factors and strengths associated with each profile.
Methods: A sample of 4936 youth living in Quebec were recruited on social media and filled out an online survey during the lockdown of the first wave of COVID-19. They completed measures of psychological distress, positive adaptation (well-being, resilience), risk factors (alexithymia and emotional dysregulation), COVID-related worries and fear of contamination and COVID-related post-traumatic stress disorder (PTSD).
Results: The results of the latent class analysis showed four patterns of adjustment. The Resilient group (36.6% of the sample) showed the highest probability of a positive adaptation. The High distress class (29.5%) reported clinical distress, low to moderate symptoms of PTSD and fear of contamination and no significant well-being. The Moderate symptoms class (17.55%) showed moderate levels of distress and COVID-related symptoms, with half of the group still showing significant well-being. The Traumatized class (16.35%) reported the worst adaptation. Correlates significantly differentiated profiles.
Limitations: The study relied on a convenience sample and a cross-sectional design.
Conclusion: Disentangling the diversity of adaptation profiles may orient more adapted resources for youth in need during this unprecedented crisis.
Keywords: COVID-19 pandemic, Youth, Psychopathology, PTSD, Resilience
1. Introduction
In December 2019, the government of China identified a new virus spreading in Wuhan. This virus, whose symptoms are similar to those of pneumonia, is from the coronavirus family and is now well known as COVID-19. In January 2020, the World Health Organization (WHO) declared a health emergency, and on March 11, a global pandemic. From that point on, many countries forced quarantine, closed borders and tried to control hospital overcrowding. To date, there have been more than 275 million cases worldwide and the number of deaths has exceeded 5 million (WHO, 2021). Although multiple waves of contamination have now followed the first, it remains important to document the effects of this initial wave as it embodies the beginning of a period of significant and unprecedented uncertainty, prolonged shutdown of services, and the beginning of a lockdown that lasted several months.
In the province of Quebec, Canada, the first case was confirmed on February 28, 2020. When the WHO announced the global pandemic, the provincial government implemented health measures such as the closure of non-essential services (schools, restaurants, stores), restricted access to uncontaminated regions and lockdown for non-essential workers. Essential services stores had a limited number of customers allowed to enter, depending on its size. Family or friend reunions were prohibited unless they lived at the same address and fines were distributed if this was not respected (Institut national de santé publique du Québec 2020).
Besides the physical consequences associated with COVID-19, the pandemic has also affected the mental health of the world population (Xiong et al., 2020). The lockdown, the loss of income, the threat of the virus and restricted access to services caused a lot of distress and anxiety (Dubey et al., 2020). Multiple studies in the world explored the repercussions of the pandemic on the mental health of adults and reported concerning levels of depression, anxiety, stress, and even post-traumatic stress disorder (PTSD; Forte et al., 2020; Liu et al., 2020; Mazza et al., 2020; Zhou et al., 2020).
As COVID-19 pandemic continues to wreak havoc, specialists warn it could affect adolescent and young adults’ mental health (Dubey et al., 2020; Liang et al., 2020). In addition to the worries and uncertainty that are globally experienced, youth are faced with their own set of challenges. Social distancing and online schooling are expected to be particularly harmful for youth mental health, especially since social relationships are crucial in their lives (Orben et al., 2020). As such, the COVID-19 pandemic represents a natural experiment to investigate the outcomes of social distancing. While some preliminary data indicated that online communication could mitigate the effects of social distancing in adolescents (Orben et al., 2020), other findings revealed that more time connecting with friends virtually was related to increased depressive symptoms (Ellis et al., 2020). It appears that the impact of social distancing and the hereby increasing use of online means of communication on youth mental health is not unidimensional, and that different dynamics must be considered in order to fully understand the associations. Moreover, adolescents and young adult preoccupations with the pandemic are not limited to changes in their socialization patterns. They also face a loss of structured occupation, and some young working adults may find themselves in precarious financial situations. Finally, some youth may be forced to stay in harmful, abusive or violent homes, with fewer opportunities to escape maltreatment (Masonbrink and Hurley, 2020). These concerns are likely to negatively affect the mental health and well-being of adolescents and young adults. Current studies have shown that 40 to 45% of adolescents and young adults experienced some form of psychological symptoms (i.e. anxiety, depression), and that between 14 and 32% reported high levels of PTSD symptoms (Liang et al., 2020; Liu et al., 2020; Zhou et al., 2020) during the first wave of the COVID-19 pandemic.
Studies on trauma exposure have taught us that trauma reactions are quite heterogenous within a population. As such, while current studies reveal that a significant proportion of people exposed to the COVID-19 outbreak are dealing with mental health difficulties, some do not develop symptoms of psychopathology. The term resilience is generally conceptualized as a healthy and adaptive functioning within a context of significant adversity (Southwick et al., 2014). Despite the abundant literature on resilience, experts still have not reach a consensual operational definition. Many disagreements persist regarding whether resilience is a stable trait, a dynamic process or an outcome (Luthar, 2006). Moreover, resilience in the sense of a positive adaptation has often been regarded in negative terms (i.e. absence of psychopathology), rather than in positive terms (i.e. happiness, health, well-being). Such a conceptualization is problematic notably because it considers that suffering and happiness are mutually exclusive, which is not necessarily the case (Masten, 2018).
In light of the inconsistencies in the resilience literature, Grych et al. (2015) have developed the Resilience Portfolio Model in an attempt to gain an understanding of the strengths and protective factors that foster resilience. The resilience portfolio encompasses many strengths that are thought to promote a healthy functioning in youth. Individual characteristics that have been more consistently associated to positive and healthy adaptation in the literature (Masten, 2007) were included in the model. These assets are aggregated into three categories: regulatory, interpersonal, and meaning-making strengths. Regulatory strengths encompass self-control and the ability to stay goal-oriented when faced with adversity. The ability to build and maintain supportive relationships has been coined into interpersonal strengths category. Finally, meaning-making strengths pertain to the capacity to find meaning in adverse and even traumatic situations and include optimism, and having a clear set of values and goals. This model was originally developed for children and adults exposed to violence, and, to our knowledge, has not yet been studied in populations exposed to other forms of adversity. Hence, the COVID-19 pandemic represents an opportunity to determine whether it can be applied more widely.
Person-centered statistical approaches are well-indicated for the study of heterogenous populations, such as people exposed to trauma and adverse life events. Latent class analysis (LCA) is a method that can identify unobserved distinct subgroups within a sample, based on their probability to endorse specific items, symptoms or characteristics. LCA has been increasingly used in the social sciences, and more precisely in studies investigating positive and negative adaptation to trauma (Jowett et al., 2020; Kazlauskas et al., 2020).
The current study sought to identify profiles of adaptation to the first wave of the COVID-19 pandemic in youth using LCA. In coherence with the resilience literature, indicators of positive (well-being) and negative (psychopathology) adaptation were included. The second objective aimed to determine whether some risk (alexithymia, emotional dysregulation) and protective factors (resiliency) and some strengths comprised in the Resilience portfolio model were associated to a specific pattern of psychological adaptation. It was expected that lower levels of risk factors, and higher levels of strengths are associated to a healthier pattern of adjustment and vice versa.
2. Methods
2.1. Participants and procedure
An online survey was shared on multiple social media platforms (Facebook, Instagram, Reddit, Snapchat) to recruit a convenience sample of adolescents and young adults aged 14 to 25 years old. To be included, participants had to reside in the Province of Quebec and be French-speaking. To encourage participation of boys, publicity was paid and specifically targeted at them. The recruitment period extended from April 21st to May 25th, 2020. During this period, restrictions varied depending on the geographical area. Because of its high density of COVID cases, the Montreal metropolitan area (population of 4 million) had the strictest restrictions. Non-essential businesses were closed during the duration of the recruitment period, but were allowed to open as of May 4th, 2020 in the rest of the territory. Schools were allowed to reopen on May 11th, except in Montreal, where the schoolyear was canceled. Indoor and outdoor gatherings were prohibited for the most part of the recruitment period (outdoor gathering allowed as of May 22nd, 2020).
Online surveys were completed via the Qualtrics platform, which allows responses to be denominated, and is subject to high security standards. Following completion of the survey, participants were invited to enroll in a contest for a chance to win one of the 50$ gift cards. This study was approved by the Université du Québec à Montréal ethics committee.
Of the initial 7213 responses stored, 489 were excluded because they were invalid (i.e. completed too fast, non-serious answers, same answer to all items) and 1788 had missing data on at least one of the LCA indicators. The total sample was composed of 4936 adolescents and young adults, (64.1% women, 33.6% men, and 2.3% self-identified as belonging to a sexual minority group). The average age of the sample was 19.9 years old (SD = 3.14). Most of the sample identified as Canadian and/or Québécois (91.4%). The majority of responders (72.2%) were students, 22% were on the job market, whereas 5.8% were neither.
2.2. Measures
2.2.1. LCA indicators
The LCA was tested with five indicators reflecting positive and negative adaptation to the COVID-19 pandemic. All indicators were dummy coded (0 = absence, 1 = presence).
2.2.1.1. Psychological distress
The Kessler screening scale (K6; (Kessler et al., 2002)) is a self-administered instrument developed to assess and screen for psychological distress and serious mental health conditions in the general population. The questionnaire prompts on six items using a 5-point Likert scale (1 - All of the time to 5 - None of the time) and the total score ranges from 0 to 24. The cut-off score of the Québec Population Health Survey (EQSP, 2008, 2014–2015) was used in order to assess if the psychological distress was either low (score from 0 to 6) or high (score from 7 to 24). In the present study, the internal consistency was α = 0.82.
2.2.1.2. COVID-related PTSD
The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5; Prins et al., 2016) was used to assess the PTSD symptoms related to COVID-19 pandemic exposure. The instrument usually starts with an item designed to assess whether the participant has been exposed to a specific trauma. In the present study, this item was adapted to “Regarding COVID-19, in the last month, have you…?”. The instrument consists of five items, answered by “yes” or “no”. A cut-off score of 3 and above was found to be optimal to identify participants with clinical levels of PTSD (Prins et al., 2016; α = 0.70).
2.2.1.3. Subjective well-being
Seven items of the Subjective Well-being adapted scale of Hamby et al. (2015) were used to measure one's satisfaction with life. The participants answered on a 5-point Likert scale (1 - Not true about me to 4 - Mostly true about me) and the scores ranged from 1 to 4. A dichotomous score was calculated following the guidelines provided by Hamby et al. (2015). A score of ≥ 0.5 standard deviation of the mean was used to indicate the presence of subjective well-being. The scale was characterized by a good internal consistency (α = 0.88).
2.2.1.4. COVID-related worries and fear of COVID contamination
These indicators were computed from a selection of 25 items from various studies examining adaptation to the COVID-19 pandemic (Satici et al., 2020; Yldirim and Solmaz, 2020). Items were rated on a 4-point Likert scale ranging from 1 - Not true to 4 - Mostly true. An exploratory factor analysis was conducted on the items to extract factors, and two were selected for this study. The COVID-related worries scale was composed of five items, such as “I have trouble concentrating” and “I am affected / troubled by the social distancing measures linked to the pandemic”. The fear of contamination factor was obtained from two items, namely “I am afraid of being infected with COVID-19″ and “I am afraid that someone in my family is infected”. Both variables had adequate internal consistency, respectively α = 0.76 and α = 0.69. Both variables were also dichotomized using a cut-off of ≥ 0.5 SD of the mean.
2.2.2. Covariates
2.2.2.1. Alexithymia
Participants were presented a selection of four items of the Toronto Alexithymia Scale (Bagby, Taylor and Parker, 1994). This scale assesses the ability to identify and describe feelings. Items were selected based on a study conducted by (Heaven, Ciarrochi and Hurrell, 2010). Of the five items initially identified as having superior factor loadings, one was eliminated to avoid redundancy. A Likert-type scale ranging from 1 (False) to 4 (Mostly true) was used to obtain a total averaged score (1–4; α = 0.88).
2.2.2.2. Emotion dysregulation
Emotion regulation problems were assessed with an adapted version of the Difficulties in Emotion Regulation Scale (DERS; Gratz and Roemer, 2004). Four items from the original instrument were used to evaluate one's ability to inhibit and modulate negative emotions. Items are rated on a scale of 1 (Not true about me) to 4 (Mostly true about me), and a total score is obtained by computing the mean of items. The internal consistency for this scale was good in this sample (α = 0.77).
2.2.2.3. Resilience
A two-item version (Vaishnavi, Connor and Davidson, 2007) of the Connor-Davidson Resilience Scale (CD-RISC; Connor and Davidson, 2003) was used to assess resilience, as defined as the ability to bounce back and successfully adapt to change. Items were rated on a scale of 1 (Not true) to 4 (Mostly true) and yielded an average score of 1 to 4, a greater score indicating greater resilience.
2.2.2.4. Strengths
The Resilience Portfolio Questionnaire was developed by Hamby et al. (2018) to better capture the variety of strengths that may be linked to resilience in youth. The complete measure assesses 16 strengths, that can be grouped into three strengths domains, namely regulatory, meaning making, and interpersonal strengths. The current study included scales relating to six strengths, two for each of the three domains. Endurance (psychological) and Recovering positive affect were used as regulatory strengths, Mattering and Relational motivation as meaning making strengths, and social support received and seeking for interpersonal strengths. The Psychological Endurance Scale (5 items; α = 0.64) assesses the ability to persevere despite challenges, whereas Recovering positive affect (6 items; α = 0.83) refers to the ability to retrieve a positive mood after experiencing distress. Mattering (5 items; α = 0.89) is defined as the extent to which one feels important, valued or appreciated by others. The Relational Motivation Scale (3 items; α = 0.74) refers to feeling inspired by important people in one's life. Social support received (5 items; α = 0.85) measures help provided by others in difficult times, whereas social support seeking (6 items; α = 0.90) assesses youth's efforts to obtain such help. All items were given a score of 1 (Not true about me) to 4 (Mostly true about me). Total scores for each scale were obtained by averaging scores of items.
3. Results
3.1. Data analytic plan
Latent class analysis (LCA) is a person-centered approach used to detect qualitatively different groups in an heterogenous population. Groups are unobserved (latent) and are thus inferred from responses on a set of indicators. In the present study, five dichotomous indicators, pertaining to various aspects of psychological adaptation, were used: psychological distress, COVID-19-related PTSD, COVID-19-related worries, fear of contamination, and well-being. Analyses were conducted with Mplus 8 (Muthén and Muthén, 2017). To evaluate the optimal number of classes, relative fit indices, as well as interpretability were compared. The multiple indices available often disagree as to which number of classes best fits the data, and thus need to be examined (Nylund, Asparouhov and Muthén, 2007). Models with the lowest relative fit indices, namely Akaike's information criterion (AIC), Bayes’ information criterion (BIC), and the adjusted BIC (aBIC) suggest the best fit (Sclove, 1987). The Bootstrapped Likelihood ratio test (BLRT) compares the estimated k-number of classes model to a model with k-1 class (e.g. between a three-class and a two-class model). A nonsignificant p-value suggests that the additional class does not significantly improve the fit (Lo, Mendell and Rubin, 2001). Moreover, Lanza and Cooper (2016), among others, have argued that the interpretability of the model should also guide model selection. Finally, an entropy value closer to 1 indicates a better class differentiation; model selection should not, however, rely on entropy.
After selecting the optimal number of classes through the class enumeration process described above, we tested whether the classes significantly differed on their age, and levels of risk (emotion dysregulation, alexithymia) and protective factors (resilience, strengths and assets from the resilience portfolio). The auxiliary function with the BCH method was used to compare the mean of each class on continuous covariates (Bolck, Croon and Hagenaars, 2004). Contrary to an analysis of variance (ANOVA), the auxiliary function accounts for the probabilistic nature of the LCA, by avoiding shifts between the classes (Asparouhov and Muthén, 2014). We also examined whether class belonging was associated to gender following the DCAT method. This method is used with dichotomous variables and provides odds ratios and 95% confidence intervals. Analyses were only conducted on men and women, since only a few participants identified themselves otherwise.
3.2. Descriptive statistics
Descriptive statistics were run with SPSS 27. Two third (67.0%) of the participants surveyed reported high levels of distress and one on five (20.2%) reported clinical levels of post-traumatic stress disorder (PTSD). Only one third (34.7%) of responders reported significant well-being. Overall, 27.9% of participants reported COVID-related worries and 28.2% reported fear of contamination.
3.3. LCA model selection
Latent class models with 1 to 5 classes were tested with five indicators (subjective well-being, COVID-related PTSD, psychological distress, COVID-related worries, and fear of contamination). Table 1 displays the model fit indices for sequential class solutions. With the addition of a fourth class, the AIC, BIC, and sample-adjusted BIC all showed a slight decrease followed by a small increased with the inclusion of a fifth class. Hence, the relative fit indices unanimously favored the four-class solution. The BLRT p-value became non-significant for the 5-class solution, further confirming that the four-class solution better represented the data.
Table 1.
Fit Indices for Latent Class Models with 1 to 5 Classes with the Full Sample.
| Number of profiles | Log likelihood | AIC | BIC | aBIC | Entropy | BLRT p-value |
|---|---|---|---|---|---|---|
| 1 | –14658.581 | 29327.162 | 29359.683 | 29343.795 | N/A | N/A |
| 2 | –13374.992 | 26771.983 | 26843.531 | 26808.577 | .64 | < .001 |
| 3 | –13115.450 | 26264.901 | 26375.474 | 26321.454 | .79 | < .001 |
| 4 | –13083.144 | 26212.288 | 26361.887 | 26288.801 | .65 | < .001 |
| 5 | –13081.427 | 26220.855 | 26409.480 | 26317.328 | .66 | .67 |
Note. AIC = Akaike's Information Criterion; BIC = Bayesian Information Criterion; aBIC = sample-size-adjusted BIC; BLRT = Bootstrapped Likelihood Ratio Test. Boldface indicates the best-fitting model for that particular indicator.
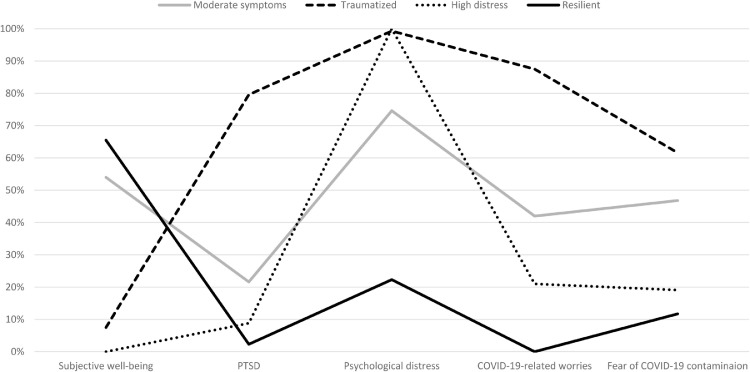
3.4. Description of the classes
The results revealed four patterns of adjustment relative to the COVID-19 global pandemic characterized by distinct endorsement of symptoms of positive (well-being) and negative adaptation (psychological distress, PTSD, worries, and fear). Fig. 1 illustrates the probability of participants from each class to endorse each indicator. The largest class (36.6%) was characterized by the highest probability of subjective well-being, and the lowest probabilities of COVID-related PTSD, psychological distress, COVID-related worries, and fear of contamination. Participants comprised in this class were labeled Resilient. Close to one participant in three (29.5%) belonged to the High distress class. The totality of this group of participants reached clinical levels of distress, and none of them reported significant well-being. They were also characterized by low to moderate PTSD, COVID-related worries and fear of contamination. Participants in the Moderate symptoms class (17.55%) demonstrated moderate levels of all negative adaptation indicators. Interestingly, more than half of participants from this class reported significant levels of subjective well-being. Finally, the Traumatized class was the smallest class, with a prevalence of 16.35% in the sample. This class was characterized by high probabilities of psychological distress and the highest probabilities of PTSD, COVID-related worries and fear of contamination. Moreover, a negligible proportion of participants (7.5%) reported being well. Overall, this class described the poorest adjustment.
Fig. 1.
Expected probability of endorsement in the 4-class model
Note. PTSD: Post-traumatic stress disorder.
Comparing the classes, we found significant differences regarding age, gender, alexithymia, emotion dysregulation, resilience and various strengths from the resilience portfolio. Table 2 displays the mean and standard errors of the classes for the studied covariates. Participants in the Traumatized class were the oldest, whereas participants from the Resilient and High distress classes were younger in average. The DCAT method was used to compare men and women on their probabilities of belonging to each of the four classes. Compared to men, women were almost five times more likely to belong to the Traumatized class (OR = 4.95, 95% CI = 3.61–6.79, p < .001) than to be resilient. They were also more inclined to be classified in the Moderate symptoms class (OR = 6.88, 95% CI = 4.20–11.28, p < .001) and the High distress class (OR = 1.95, 95% CI = 1.47–2.60, p < .001) than to be classified in the Resilient class.
Table 2.
Means and standard deviations for age, risk and protective factors, and strengths across latent classes.
| Resilient (36.60%) | High distress (29.50%) | Moderate symptoms (17.55%) | Traumatized (16.35%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | M | SE | χ2/F | |
| Age of participants | 19.64ab | 0.09 | 19.91b | 0.10 | 20.15a | 0.19 | 20.41c | 0.14 | 25.55⁎⁎⁎ |
| Alexithymia | 1.70a | 0.02 | 2.46b | 0.03 | 1.96c | 0.05 | 2.71d | 0.04 | 940.76⁎⁎⁎ |
| Emotion dysregulation | 1.74a | 0.02 | 2.59b | 0.02 | 2.15c | 0.04 | 2.91d | 0.03 | 1618.83⁎⁎⁎ |
| Resilience | 3.15a | 0.02 | 2.54b | 0.02 | 2.96c | 0.04 | 2.34d | 0.03 | 713.80⁎⁎⁎ |
| Recovering positive affect | 3.08a | 0.02 | 2.38b | 0.02 | 2.94c | 0.04 | 2.35b | 0.03 | 904.42⁎⁎⁎ |
| Endurance | 2.73a | 0.02 | 2.36b | 0.02 | 2.85c | 0.04 | 2.46d | 0.03 | 261.20⁎⁎⁎ |
| Mattering | 3.34a | 0.02 | 2.52b | 0.03 | 3.53c | 0.04 | 2.64d | 0.04 | 992.46⁎⁎⁎ |
| Relational motivation | 3.43a | 0.02 | 3.35b | 0.02 | 3.72c | 0.03 | 3.61d | 0.03 | 103.66⁎⁎⁎ |
| Received social support | 3.00a | 0.02 | 2.57b | 0.03 | 3.33c | 0.05 | 2.92a | 0.04 | 23.84⁎⁎⁎ |
| Sought social support | 2.93a | 0.02 | 2.67b | 0.03 | 3.36c | 0.05 | 2.99a | 0.04 | 147.51⁎⁎⁎ |
Note.
p < .001. Cells with differing subscripts are statistically different from one another at p < .05.
Participants from the Resilient class reported the lowest scores of alexithymia and emotion dysregulation and the highest scores of resilience, followed by the Moderate symptoms class. Comparison on the strengths of the resilience portfolio yielded consistent results for all strengths but the ability to recover positive aspect. For psychological endurance, mattering, relational motivation, and sought and received social support, participants from the Moderate symptoms class consistently reported the highest scores, followed by participants belonging to the Resilient class. Individuals in the High distress class had the lowest levels of strengths. Regarding recovering positive affect, Resilient participants showed the highest scores, followed by participants from the Moderate symptoms class, whereas those in the Traumatized and High distress classes had comparable levels.
4. Discussion
This study aimed to delineate profiles of adaptation in youth affected by the COVID-19 pandemic during the first wave. The world is confronted with an unprecedented situation as individuals are trying to manage and adapt in these uncertain times. The situation may be particularly stressful for youth who are in a critical phase of development. Because of restrictions and confinement, youth have suddenly lost their school or work routine as well as opportunities for leisure and sports which provide contexts for significant social interactions. Physical distancing and social isolation may lead to increased stress which may translate into significant psychological distress (Orben et al., 2020). Yet, the COVID-19 pandemic is unlikely to affect all youth in the same way as past studies have underscored quite diverse patterns of adaptation when individuals are confronted with major stressors, such as the 2003 severe acute respiratory syndrome (SARS) epidemic in Hong Kong, during which adaptation ranged from chronic dysfunction to resilience (Bonanno et al., 2008). Reliance on latent class analysis offers a means to disentangle the diversity of profiles in youth. We used indicators of negative (psychopathology, psychological symptoms) as well as positive adaptation (well-being) to better ascertain the differential patterns in youth.
Results of the LCA revealed four different profiles of adaptation. Findings showed the existence of a class characterized mainly by the presence of clinical levels of psychological distress regrouping 30% of the participants (High distress). A second class (Traumatized class) was characterized not only by clinical levels of psychological distress, but also a high risk of clinical score of PTSD symptoms accompanied by high probabilities of having COVID-19 worries and fear of contamination. Participants from the Moderate symptoms class had moderate probabilities of endorsing indicators of negative adaptation and well-being. Our results also identified a subgroup of Resilient youth that appear to fare better, attesting to the capacities of some youth to overcome adversity. These profiles of adaptation might be linked to prior existing resilience and vulnerability traits that were solicited in the context of the pandemic regulation.
The study also aimed to explore possible risk (alexithymia, emotional dysregulation) and protective factors (resiliency) linked to different profiles of adaptation. In addition, informed by the Portfolio Resilience Model, a selection of regulatory, meaning making and interpersonal strengths were investigated to explore their association with a specific pattern of psychological adaptation. Our findings revealed that these potential correlates significantly differentiated profiles of adaptation. Regarding socio-demographic variables, gender was found to relate to profiles of adaptation as girls were more likely than boys to belong to the classes depicting negative adaptation (Traumatized, High distress and Moderate symptoms) than to be classified into the Resilient subgroup. This result is consistent with past findings showing that girls are more likely to display PTSD when confronted to adverse life events (Nooner et al., 2012) and to experience psychological distress in general (Drapeau, Marchand and Forest, 2014). Age also discriminated groups as participants classified in the Traumatized class were older than participants comprising the three other classes, which might reflect the likelihood of older participants to have added responsibilities (living in an apartment, combining schooling and part-time work, having a child) and ensuing struggles and challenges that may unravel their capacity to cope with the COVID-19 pandemic.
Findings suggest that the classes could be distinguished by some risk and protective factors. It appears that the classes could fall on a spectrum, with, on one end, youth in the Traumatized group likely to show impairment in their capacity to identify and express emotions, emotion regulation and resiliency and, on the other end, of the spectrum youth in the Resilient class showing high resiliency or capacity to bounce back following an adverse event, low levels of alexithymia and emotional dysregulation. This is coherent with findings indicating that emotion regulation is associated to fewer symptoms of psychopathology and that it constitutes a key predictive factor of resilience (Compas et al., 2017). Results are also in line with past meta-analyses concluding that alexithymia or the difficulty to identify and express feelings is associated to a heightened risk of distress including post-traumatic stress disorder and suicidality (Frewen et al., 2008; Hemming et al., 2019) and emotion dysregulation to be linked to an array of mental health difficulties (Aldao, Nolen-Hoeksema and Schweizer, 2010).
Inspection of the results regarding the strengths of the Portfolio model also revealed significant associations with class assignment with lower scores generally found for participants in the High Distress class and higher scores for the Moderate symptoms group. However, a distinct trend was apparent for recovering positive affect, where Resilient participants reported the highest probability, whereas both the Traumatized and the High distress subgroups showed the poorest.
One possible interpretation of the results regarding the two indicators of social support (sought and received) is that participants in the High distress class may not have an available support network and therefore are unlikely to seek social support, while youth in the Moderate symptoms class may have access to social support and use it to cope with the adversity. A parallel can be drawn with the Isolated and Interconnected groups found in a study reported by Hamby et al. (2020). Also based on scales from the Resilience Portfolio Questionnaire, the Isolated group reported little seeking and receiving social support while the Interconnected group had high scores for seeking and receiving support, which respectively corresponds to the High distress and Moderate symptoms classes in the present article. Both groups from Hamby and colleagues’ study (2020) did not differ on their levels of trauma symptoms, as did suggest the comparable probabilities of the Moderate symptoms and High distress groups of the current study to report clinical levels of PTSD.
Coupled with the data on the percentage of participants showing distress and COVID-19 worries and fear, this could suggest that youth in the High distress class show psychological distress that is not specifically associated to the virus, compared to the Traumatized or Moderate symptoms groups. They could be more affected by the lockdown than by the COVID-19 itself, especially if they already had scarce social support resources. Youth in the Moderate symptoms group could be what we could call “active copers”, as they possess more individual and interpersonal resources to help them deal with stressful events. This could also mean that they are not hardened or tolerant towards the stress caused by the virus because they can easily rely on outside help in case of distress (Hamby et al., 2020). Youth in the Traumatized and Resilient classes may not solicit social support as much as youth in the Moderate symptoms class, but for different reasons. The former group because of more limited access to a supportive network, and the latter because they simply do not need to, given their high levels of personal strengths to deal with adversity. Moreover, resilient individuals may display more flexibility in resorting to their strengths depending on the context. For instance, since in-person social contact was discouraged during the confinement, it may be that these youth resorted to their individual strengths to face the situation (i.e. resiliency, emotion regulation, recovering positive affect) rather than strengths relying on how one relates to others (e.g. mattering, relational motivation).
4.1. Limitations of the study
Our study is not without limitations. First, the study relied on a convenience sample recruited through a web-based survey. The absence of random sampling could reduce the representativeness of the sample. Second, while we explored a number of correlates associated with the different classes, important variables that may discriminate profiles of adaptation were not investigated. For example, past trauma and prior psychiatric diagnosis have been linked to worsened psychological symptoms following adverse events, such as the COVID-19 pandemic (Rossi et al., 2020). In addition, only a subset of the strengths and assets proposed by the portfolio model were included in the present study. Similarly, the lack of measures collected before the pandemic did not allow for assessment of other stable factors, such as personality traits, that might be related to differential adaptation patterns in youth. Finally, the data collection was conducted during the first confinement and as such offer a picture of adaptation during the first months of the COVID-19 pandemic. It would be essential to rely on longitudinal studies to explore whether profiles change over time, especially given the pandemic continues to bring its share of uncertainty. Despite these limitations, the current study provides evidence of the immediate effects of the COVID-19 pandemic and the measures that aimed to contain it. Our results corroborate previous findings suggesting that the pandemic is associated with significant distress for youth (Zhou et al., 2020). The present study also extends these findings by identifying different patterns of adaptation while considering not only potential psychological distress and specific COVID-19 related worries and fears, but also indicators of well-being. Indeed, it offers a nuanced picture by showing that while some youth are significantly impacted, others appear to adapt and even thrive through these uncertain times.
5. Conclusion
Given the current pandemic affecting individuals worldwide, research uncovering factors promoting adaptation and fostering resilience should be at the forefront of our preoccupations. These analyses may identify potential targets for interventions that could foster resilience and positive adaptation despite adversity. Strength-based programs could help youth cope with the mental health consequences associated with COVID-19 and the confinement measures. Given the current situation, we need to be innovative to identify strategies to build upon individual and collective strengths to sustain support during the pandemic. This may require ensuring internet access to all and promote the availability of online support groups. In addition, self-help apps (for eg., JoyPop) monitoring daily mood, providing strategies to bolster resilience and positive emotionality (relaxation, mindfulness, journal writing, etc.) can be particularly well-suited to address the needs of youth.
This global pandemic could be viewed as an opportunity to foster solidarity and interconnectedness which will build community resilience enabling societies to push through and to bounce back when the situation is resolved. More than ever, funds should be allocated to improve accessibility of mental health services, especially to vulnerable populations, to prevent the next pandemic from being one of mental health problems.
6. Author contributions
Martine Hébert, Ph.D., Université du Québec à Montréal, Department of sexology: Conception, planning and design of the study, acquisition of data, drafting the manuscript, revising the article critically. Amélie Tremblay-Perreault, Ph.D. candidate, Université du Québec à Montréal, Department of psychology: Contribution to writing, statistical analysis, revising the article critically. Arianne Jean-Thorn, Ph.D. candidate, Université du Québec à Montréal, Department of psychology: Contribution to writing, revising the article critically. Hélène Demers, Ph.D. candidate, Université du Québec à Montréal, Department of psychology: Contribution to literature review, revising the article. All authors approved the final version of the manuscript prior to its submission.
Acknowledgments
Role of funding source
This research was supported by a grant from the Social Sciences and Humanities Research Council (SSHRC) awarded to the first author.
Acknowledgments
The authors wish to thank the youth who participated in the study and Manon Robichaud for data management.
References
- Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Asparouhov T., Muthén B. Auxiliary variables in mixture modeling: using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes. 2014;21:1–22. [Google Scholar]
- Bagby R.M., Taylor G.J., Parker J.D. The twenty-item Toronto Alexithymia Scale—II. Convergent, discriminant, and concurrent validity. J. Psychosomat. Res. 1994;38:33–40. doi: 10.1016/0022-3999(94)90006-x. [DOI] [PubMed] [Google Scholar]
- Bolck A., Croon M., Hagenaars J. Estimating latent structure models with categorical variables: one-step versus three-step estimators. Polit. Anal. 2004;12:3–27. doi: 10.2307/25791751. [DOI] [Google Scholar]
- Bonanno G.A., Ho S.M.Y., Chan J.C.K., Kwong R.S.Y., Cheung C.K.Y., Wong C.P.Y., Wong V.C.W. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: a latent class approach. Health Psychol. 2008;27:659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- Compas B.E., Jaser S.S., Bettis A.H., Watson K.H., Gruhn M.A., Dunbar J.P., Williams E., Thigpen J.C. Coping, emotion regulation, and psychopathology in childhood and adolescence: a meta-analysis and narrative review. Psychol. Bull. 2017;143:939–991. doi: 10.1037/bul0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC) Depress. Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Drapeau A., Marchand A., Forest C. Gender differences in the age-cohort distribution of psychological distress in Canadian adults: findings from a national longitudinal survey. BMC Psychol. 2014;25 doi: 10.1186/s40359-014-0025-4. [DOI] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14:779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52:177–187. doi: 10.1037/cbs0000215. [DOI] [Google Scholar]
- Forte G., Favieri F., Tambelli R., Casagrande M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int J Env Res Pub He. 2020;17:41–51. doi: 10.3390/ijerph17114151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen P.A., Dozois D.J., Neufeld R.W., Lanius R.A. Meta-analysis of alexithymia in posttraumatic stress disorder. J. Trauma Stress. 2008;21:243–246. doi: 10.1037/0021-843X.117.1.171. [DOI] [PubMed] [Google Scholar]
- Gratz K.L., Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Grych J., Hamby S., Banyard V. The resilience portfolio model: understanding healthy adaptation in victims of violence. Psychol. Violence. 2015;5:343–354. doi: 10.1037/a0039671. [DOI] [Google Scholar]
- Hamby S., Taylor E., Mitchell K., Jones L., Newlin C. Is it better to seek or to receive? A dual-factor model of social support. Int. J. Child Adolescent Resilicence. 2020;7:5–31. [Google Scholar]
- Hamby S., Taylor E., Smith A., Blount Z. Resilience Portfolio Questionnaire manual: scales for youth. Sewanee, TN: Life Paths Research Center. 2018 doi: 10.13140/RG.2.2.27296.74243. [DOI] [Google Scholar]
- Heaven P.C., Ciarrochi J., Hurrell K. The distinctiveness and utility of a brief measure of alexithymia for adolescents. Pers indiv differ. 2010;49:222–227. doi: 10.1016/j.paid.2010.03.039. [DOI] [Google Scholar]
- Hemming L., Taylor P., Haddock G., Shaw J., Pratt D. A systematic review and meta-analysis of the association between alexithymia and suicide ideation and behavior. J. Affect. Disord. 2019;254:34–48. doi: 10.1016/j.jad.2019.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institut national de santé publique du Québec . 2020. Ligne Du Temps Covid-19 Au Québec. https://www.inspq.qc.ca/covid-19/donnees/ligne-du-temps/ (accessed August 2020) [Google Scholar]
- Jowett S., Karatzias T., Shevlin M., Albert I. Differentiating symptom profiles of ICD-11 PTSD, complex PTSD, and borderline personality disorder: a latent class analysis in a multiply traumatized sample. Personal Disord. 2020;1:36–45. doi: 10.1037/per0000346. [DOI] [PubMed] [Google Scholar]
- Lanza S.T., Cooper B.R. Latent class analysis for developmental research. Child Dev. Perspect. 2016;10:59–64. doi: 10.1111/cdep.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazlauskas E., Zelviene P., Daniunaite I., Hyland P., Kvedaraite M., Shevlin M., Cloitre M. The structure of ICD-11 PTSD and Complex PTSD in adolescents exposed to potentially traumatic experiences. J. Affect. Disord. 2020;265:169–174. doi: 10.1016/j.jad.2020.01.061. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-.L., Walters E.E., Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32:959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. The Effect of COVID-19 on Youth Mental Health. Psychiat Quart. 2020;91:841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiat Res. 2020;290:1–7. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y., Mendell N.R., Rubin D.B. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. doi: 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- Luthar S.S. Resilience in Development: A Synthesis of Research Across Five Decades. 2006:739–795. second ed. [Google Scholar]
- Masonbrink A.R., Hurley E. Advocating for children during the COVID-19 school closures. Pediatrics. 2020;146 doi: 10.1542/peds.2020-1440. [DOI] [PubMed] [Google Scholar]
- Masten A.S. Resilience in developing systems: progress and promise as the fourth wave rises. Dev. Psychopathol. 2007;19:921–930. doi: 10.1017/S0954579407000442. [DOI] [PubMed] [Google Scholar]
- Masten A.S. Resilience theory and research on children and families: past, present, and promise. J. Fam. Theor. Rev. 2018;10:12–31. doi: 10.1111/jftr.12255. [DOI] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17:31–65. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L.K., Muthén, B.O., 2017. 1998–2017. Mplus user's guide. Muthén & Muthén: los Angeles.
- Nooner K.B., Linares L.O., Batinjane J., Kramer R.A., Silva R., Cloitre M. Factors related to posttraumatic stress disorder in adolescence. Trauma Violence Abus. 2012;13:153–166. doi: 10.1177/1524838012447698. [DOI] [PubMed] [Google Scholar]
- Nylund K.L., Asparouhov T., Muthén B.O. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct. Equ. Model. 2007:535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- Orben A., Tomova L., Blakemore S.-.J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc Health. 2020;4:634–640. doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A., Bovin M.J., Smolenski D.J., Marx B.P., Kimerling R., Jenkins-Guarnieri M.A., Kaloupek D.G., Schnurr P.P., Kaiser A.P., Leyva Y.E., Tiet Q.Q. The primary Care PTSD Screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J. Gen. Intern. Med. 2016;31:1206–1211. doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiat. 2020;11(3):1–6. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satici B., Gocet-Tekin E., Deniz M.E., Satici S.A. Adaptation of the fear of COVID-19 scale: its Association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Ad. 2020:1–9. doi: 10.1007/s11469-020-00294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sclove S.L. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. doi: 10.1007/BF02294360. [DOI] [Google Scholar]
- Southwick S.M., Bonanno G.A., Masten A.S., Panter-Brick C., Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur. J. Psychotraumatol. 2014;5:1–11. doi: 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaishnavi S., Connor K., Davidson J.R. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiat. Res. 2007;152:293–297. doi: 10.1016/j.psychres.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worldwide Health Organization, 2021. Coronavirus disease (COVDIS-19) situation report-205. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200812-covid-19-sitrep-205.pdf?sfvrsn=627c9aa8_2/ (accessed December 2021).
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yıldırım M., Solmaz F. COVID-19 burnout, COVID-19 stress and resilience: initial psychometric properties of COVID-19 Burnout Scale. Death Stud. 2020:1–9. doi: 10.1080/07481187.2020.1818885. [DOI] [PubMed] [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psy. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]