Abstract
There are concerns that involving adolescents bereaved by suicide and other traumatic death in research may cause distress and harm. However, no study has investigated such bereaved adolescents’ research experiences. In addition, no study has looked at the experiences of parents and clinicians as participants in adolescent suicide and traumatic death bereavement research. This study aimed to explore the short-term impact of research participation experienced by adolescents, parents, and clinicians. A total of 61 participants (adolescents, n = 17; parents, n = 12; clinicians, n = 32) filled out a short survey within two weeks of having taken part in a qualitative interview study. Data were analyzed descriptively. Most participants had experienced no distress while participating and no negative effects of participating; rather, participation was experienced as helpful for them and they would highly recommend participating in a study like this to others. A few adolescents and parents reported some distress, related to anxiety about participation and the unpleasantness of grief memories. The study clearly indicates that bereaved adolescents, parents and clinicians can safely participate in research interviews regarding their experiences of grief and help after suicide, generally valuing the opportunity to share their experience. To prevent and mitigate potential distress, training of research staff and implementation of appropriate participant distress protocols are imperative. Future studies could include longitudinal follow-up of participants to assess any longer-term consequences.
Keywords: grief, bereavement, suicide, traumatic death, research participation, ethics, research ethics
1. Introduction
1.1. Rationale
Adolescents who are bereaved by the death of someone close to them, such as a family member or a friend, often experience short-term and long-term impacts regarding their grief, mental health and social functioning [1,2,3,4,5]. Experiencing a death is often an unfamiliar, disruptive and stressful event in their lives, leading to acute grief reactions such as crying, and feelings of numbness, sadness and longing for the deceased person [2,3,4,5]. Compared to other types of bereavement, adolescents bereaved by suicide and other traumatic death can experience more pronounced feelings of shock, guilt, anger, and abandonment [3,4,6]. They can struggle more with “why” questions, finding meaning in the loss, and experience less social support [1,2,3,6]. In addition, they have an increased risk of mental health problems, such as depression, anxiety, posttraumatic stress disorder, and long-term increased risk of suicidal behavior compared to other bereaved and non-bereaved adolescents [7,8,9].
While negative grief reactions are more prominent, there is also emerging evidence of personal or posttraumatic growth in this population [10,11]. The growth is understood as a positive psychological transformation that occurs as the result of a struggle with a traumatic and highly distressing event [12]. Traumatically bereaved adolescents can experience personal or posttraumatic growth in various domains, including increased appreciation of life and relationships, increased maturity and self-care, and finding new opportunities, for example, regarding school or professional career paths [3,11,12]. Nonetheless, bereavement by suicide and other traumatic death among adolescents can disconnect them from their friends and rupture the family equilibrium [13,14,15], which in turn may affect their parents’ and guardians’ capacity to support them and/or refer them to professional help [16].
Given the potential ramifications of bereavement by suicide and other traumatic death in adolescents, conducting research with this population poses important ethical challenges. The Australian National Statement on Ethical Conduct in Human Research (2007) (Updated 2018) [17] places value on principles of research merit and integrity, justice, beneficence, and respect. Researchers are required to minimize and manage potential risks to participants, and risks are only justified when they are outweighed by potential benefits for participants or the community. The National Statement [17] stipulates that research with bereaved minors/adolescents requires specific attention to participants’ capacity to understand the research and consent.
Important concerns regarding participant safety and the potential negative impact of research participation have been voiced in various research fields involving vulnerable populations, including suicide [18,19,20,21], trauma and violence [22,23], palliative care [24], psychiatry [25,26], and bereavement [27,28]. In studies with adults bereaved by suicide, research ethics committees have expressed concerns about potential harm to research participants, particularly that talking about grief experiences may traumatize them and increase their suicide risk [29,30,31]. Further, there are concerns about whether research participants who are negatively impacted will receive enough support [31].
Nonetheless, a recent systematic review found that most participants in suicide bereavement studies experience research participation positively [32]. Positive experiences included gaining insight into their grief experience and providing opportunities for helping others. However, a minority of participants reported unpleasant or negative experiences when participating in studies, such as being reminded of painful experiences, e.g., [27,33]. Despite the importance of these findings, the reviewed studies had several limitations [32]. Most were psychological autopsy studies (in which participants provide information about the deceased person rather than about themselves), and only one study included adolescents in the sample [34]. Hence, little is known about the experiences of adolescents of being involved in research regarding their own grief and help-seeking after a loss by suicide or other traumatic death. In addition, no study has looked at the experiences of parents and clinicians as participants in adolescent suicide and traumatic death bereavement research. This study aimed to address this gap by exploring the short-term impact of research participation experienced by adolescents, parents, and clinicians.
1.2. Background: Original Study
1.2.1. Sampling
The original study, about which participants were then asked about their participation experience, was a qualitative study that examined how to best help adolescents bereaved by suicide and other traumatic death. Although details have been published [13,35], we summarize the original study here to provide context for the current study of participant experiences.
The original study adhered to the COREQ criteria [36] and involved a purposive sample of three groups of participants (adolescents, parents and clinicians) recruited in Australia between October 2019 and March 2020. Adolescents could participate if they had lost a family member or friend through suicide or other cause when they were aged between 12 and 18 years, and had experienced the death between six months and 10 years before participating in the study. Parents could participate if they were the parent of an eligible adolescent. Adolescents and parents could participate whether or not their parents or adolescent children participated. Clinicians could participate if they had at least five years of experience with providing professional help to bereaved adolescents.
Study participants (N = 72) included a total of 20 adolescents, 18 parents and 34 clinicians. The adolescent participants (16 girls, 4 boys) were aged 14 to 26 years (M = 19.50, SD = 2.95). They had lost their father (n = 9), brother (n = 3), sister (n = 2), mother (n = 2), other family member (n = 2), or friend (n = 2), by suicide (n = 18) or by accident (n = 2), on average 4 years previously (M = 3.92, SD = 2.49, range 1 to 10 years).
The parents (18 mothers) were aged 43 to 60 years (M = 53.20, SD = 4.35). The deceased person was the child’s father (n = 10), brother (n = 4) or sister (n = 4), and the person had died by suicide (n = 13), accident (n = 2), manslaughter (n = 1), illness (n = 1) and undetermined (n = 1), on average 5 years previously (M = 5.31, SD = 2.89, range 1.5 to 10 years).
The clinicians (28 females, 6 males) were aged 26 to 71 years (M = 48.47, SD = 11.35). About one in four clinicians had five to nine years of experience (n = 8, 23.5%), 12 others (35.3%) had 10 to 19 years, and 14 (41.2%) had more than 20 years of experience.
1.2.2. Data Collection and Analyses
Participants could choose between taking part in an individual interview by telephone or an in-person group interview [37,38,39,40,41]. We conducted 28 individual interviews, and 11 group interviews with 44 participants. Individual interviews lasted, on average, 46 min (range 19–76), and group interviews were an average of 77 min (range 40–102).
The interview guide was adaptable for individual and group interviews. It consisted of open-ended questions allowing for probes and follow-up questions. The lead questions addressed different aspects of the help (for example: “In your opinion, what help should be provided to a bereaved adolescent?”, “How should the help be provided?”, “How long after the loss?”, “What is the role of professional versus peer support?”, “What are the characteristics that make help helpful?”). Adopting an inductive approach, we analyzed the interview data through a codebook-based thematic analysis [42,43,44].
2. Materials and Methods
2.1. Survey
We created a short survey with five questions to assess the participants’ experiences of taking part in the individual or group interviews. Table 1 lists the survey questions. Participants were asked to answer the first four questions on a 5-point Likert-type scale (1. Not at all; 5. Absolutely). After each question, participants could write a free text comment. Question five was an open-ended question asking the participant if anything important to them was not discussed during the interview. The survey was anonymous, did not collect sociodemographic data, and could be filled out in less than five minutes.
Table 1.
Survey questions.
| Questions |
|---|
|
2.2. Sampling
Participants who took part in an in-person group interview received a hard copy of the survey at the end of the interview, and/or by email, as requested. We emailed the survey to those who had taken part in a telephone interview. We asked all participants to return the survey within two weeks, and 85% (61 out of 72) did so. This included 85% (17 out of 20) of the adolescents, 67% (12 out of 18) of the parents, and 94% (32 out of 34) of the clinicians. This amounted to 96% (n = 42) of group interview participants and 68% (n = 19) of individual interview participants.
Of those who returned the survey, 54% (n = 33) provided at least one comment in the free text boxes of the four survey questions and the open-ended question. This included 41% (n = 7) of the adolescents, 58% (n = 7) of the parents, and 59% (n = 19) of the clinicians. There was no difference between the three groups (χ2 (2) = 1.589, p = 0.452). Additionally, an equal proportion of individual (53%, n = 10) and group participants (55%, n = 23) provided comments (χ2 (1) = 0.024, p = 0.877).
2.3. Analyses
We uploaded all data into SPSS version 26 [45]. We analyzed the quantitative data descriptively and results are presented as frequencies and percentages. Levels 1 and 2 of the 5-point Likert-type scale are considered as low, level 3 is moderate/medium, and levels 4 and 5 are high. We used the Kruskal–Wallis H test to test if there were differences between the three groups of participants. We used Kendall’s tau-b correlation coefficient (2-tailed) to investigate the correlations between the data derived from the four Likert-type questions.
As most comments provided in the free text boxes were short (a few words or a short sentence), we opted to summarize the qualitative data allowing for a quantitative and qualitative report of the findings [46]. The summary applied a deductive approach, based on the survey questions. Two researchers (KA and KK) summarized the data independently and compared their report; there were no discrepancies. The research team discussed the progress and results to maximize consistency throughout the study.
2.4. Ethical Approval
The Human Research Ethics Committee of The University of Melbourne approved the study (ID 1955213). All participants provided written informed consent.
3. Results
3.1. Quantitative Findings
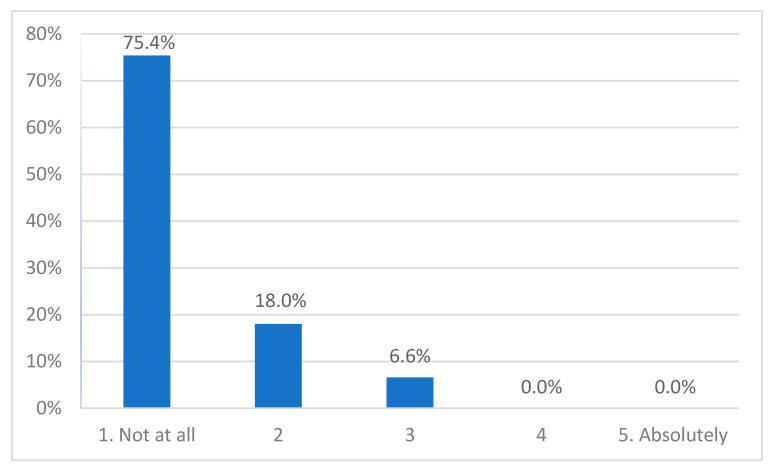
3.1.1. At the Time of Participating, Did You Feel Distressed When You Participated in the Focus Group/Interview?
Most participants (75%, n = 46) reported that they had no or hardly any distress (18%, n = 11) while participating in the interview. Four participants (6.6%, three adolescents, one parent) reported moderate levels, and none reported high levels of distress (Figure 1). The Kruskal–Wallis test indicated a significant difference between the three groups (H(2) = 11.772, p = 0.003). Pairwise comparisons showed that adolescent participants scored higher than clinicians (adj. p = 0.002).
Figure 1.
Experienced level of distress.
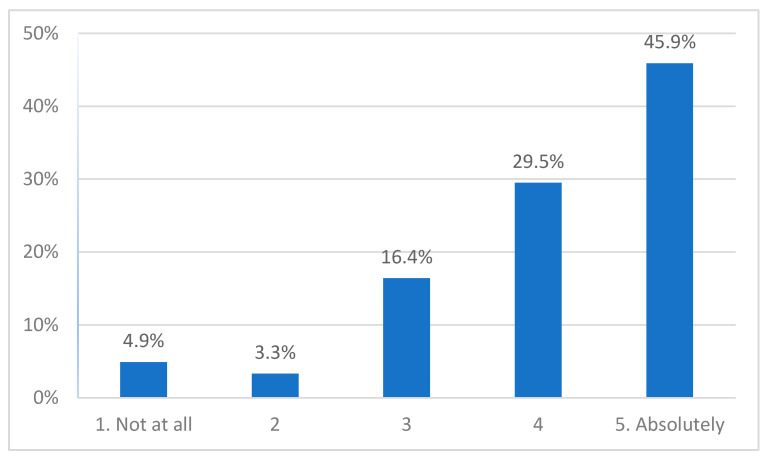
3.1.2. Today, Do You Think That Participating Helped You in Anyway?
About 75% (n = 46) of participants reported they felt that participation was helpful, 16% (n = 10) reported a medium level of perceived helpfulness, and 8% (2 adolescents, 1 parent, 2 clinicians) reported low levels (Figure 2). There was no difference between the three groups (H(2) = 0.210, p = 0.900).
Figure 2.
Perceived helpfulness.
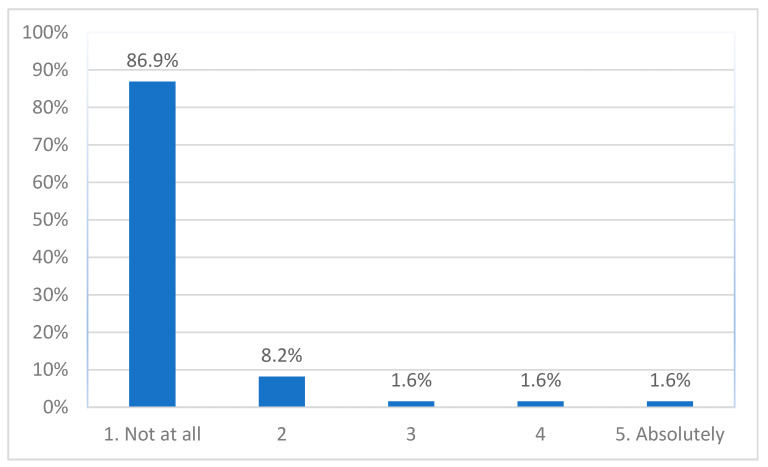
3.1.3. Today, Do You Feel That Participating Had Any Negative Effects for You?
About 95% (n = 58) of participants reported having experienced no or hardly any negative effects of participating (Figure 3); 1.6% (1 adolescent) reported a moderate level, and 3.2% (1 adolescent, 1 parent) a high level of experienced negative effects. The Kruskal–Wallis test found a significant difference between the three groups (H(2) = 11.836, p = 0.003). Pairwise comparisons showed that adolescent participants scored higher than clinicians (adj. p = 0.002).
Figure 3.
Experienced negative effects.
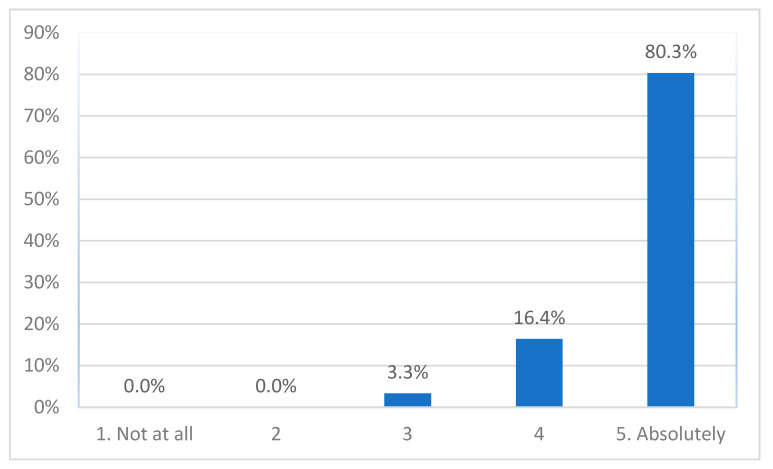
3.1.4. Would You Recommend Participating in a Study Like This to Others?
Almost all participant (97%, n= 59) said they would absolutely or close to absolutely recommend participating in a study like this to others, with the other 3.3% (2 parents) being somewhat likely to recommend (Figure 4). There was no difference between the three groups (H(2) = 0.568, p = 0.753).
Figure 4.
Recommending taking part to others.
3.1.5. Correlation Analysis
Table 2 presents the correlations, showing that there were significant associations between questions 1 and 3 (p = 0.007), and questions 2 and 4 (p = 0.026). This reveals that greater feelings of distress during participation were weakly related to more negative experienced effects of participation, and that greater perceived helpfulness of participation was weakly related to recommending participation to others.
Table 2.
Correlations.
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. At the time of participating, did you feel distressed when you participated in the Focus Group/interview? | 1 | |||
| 2. Today, do you think that participating helped you in anyway? | 0.056 | 1 | ||
| 3. Today, do you feel that participating had any negative effects for you? | 0.335 ** | −0.071 | 1 | |
| 4. Would you recommend participating in a study like this to others? | 0.000 | 0.264 * | 0.077 | 1 |
*. Correlation is significant at the 0.05 level (2-tailed). **. Correlation is significant at the 0.01 level (2-tailed).
3.2. Qualitative Findings
3.2.1. At the Time of Participating, Did You Feel Distressed When You Participated in the Focus Group/Interview?
Six participants provided a comment: 2 adolescents, 1 parent, and 3 clinicians. Two adolescents reported having felt some anxiety but were otherwise fine, as stated by one: “Have anxiety but it was really okay”. One parent reported feeling “distress” after hearing stories of other participants, but the participant continued that this was experienced as a “helpful connection and catharsis”, which helped to reflect “how far” they “had come in their own grief”. Three clinicians reported having felt safe and supported while participating in the interview, as stated by this clinician: [It was] “Very supportive and informative”.
3.2.2. Today, Do You Think That Participating Helped You in Anyway?
Twenty-two participants commented on this question: 5 adolescents, 5 parents, and 12 clinicians. Four adolescents and two parents experienced participating as being helpful for themselves, as stated by this adolescent: “It helped me open up and share my experience”. One adolescent and three parents referred to being able to use their experiences to help others in similar situations, for example, one parent wrote: “I appreciate being able to share to help those behind me”. Eight clinicians commented that participating in the interview was a learning experience, as stated by this clinician: “It’s always beneficial to talk about one’s practice and reflect on the strategies used in your daily work”. Three other clinicians experienced the interview also as a validation and encouragement, as said by this clinician: “It reminds practitioners to continue doing great work”. Still, one clinician commented on the interview as a “one-way conversation”.
3.2.3. Today, Do You Feel That Participating Had Any Negative Effects for You?
Two participants noted a comment (1 adolescent, 1 parent). The adolescent stated that: “It brought up unpleasant memories but not overwhelming”. The parent reported having felt sad and having cried after the interview “particularly after listening to other participants, their loss of their loved ones”.
3.2.4. Would You Recommend Participating in a Study Like This to Others?
Seven participants provided a comment (2 parents, 5 clinicians). The parents emphasized the importance of listening to others “across cultures and genders” to “identify evidence-based approaches that will work”. In addition, it may help us “learn how to best equip and cope with a suicide loss”. The clinicians would recommend participating because it “gives support and facilitates time to reflect, focus, and share ideas about a neglected cohort”. In addition, it can “increase education and awareness” for clinicians, and “support for young people”.
3.2.5. Was There a Topic Very Important to You That You Thought We Should Discuss but Did Not?
Eighteen participants (4 adolescents, 3 parents, 11 clinicians) wrote a comment in the last free text box of the survey, although several comments appeared to be more about what participants thought was important regarding grief and bereavement, rather than about topics that were not addressed in the interviews. Three adolescents emphasized what they saw as crucial for helping bereaved adolescents. One wrote: “trust and knowing that there is good information and discussion out there”, and another highlighted the “need to let the younger teens know it’s not weak to speak and get help”. In addition, one parent elaborated on the “secrecy around suicide” and the tendency of blaming someone for a suicide, which may hinder bereaved adolescents. Subsequently, this parent argued for increased literacy around dealing with grief in society. Two clinicians pointed at cultural sensitivity in providing help, and financial impact of the loss, as important topics for further discussion.
One parent commented on the composition of the group in which she participated. Most participants in her group had lost a husband to suicide and only one participant had lost a child to suicide. Hence, the participant recommended that groups in future studies could be more balanced regarding types of relationship.
Twelve participants (1 adolescent, 2 parents, 9 clinicians) confirmed that everything important had been discussed in their interview, as exemplified by one adolescent who noted: “I believe we covered everything vital”, and participants expressed gratitude for having been involved, as stated by this clinician: “I’m sure there is more, but right now it feels good”.
4. Discussion
This study was a first to investigate the reactions of adolescents, parents, and clinicians regarding their participation in a study on adolescents bereaved by suicide and other traumatic death. Most participants reported that they experienced no distress while participating and no negative effects of participating. Rather, they found participation helpful for them and said they would definitely recommend participating in a study like this to others. These findings reflect results of bereavement studies with parents [47,48], siblings [49], and people bereaved by suicide [30,32], which reported that research participation was mostly a positive experience, with few negative experiences, and participants perceiving participation as being beneficial for themselves and others [30,32,47]. In addition, the correlation analysis showed that there is no contradiction between reporting distress or negative effects of participation and experiencing participation as helpful and recommending it to others. This finding is corroborated by suicide-related research with adolescents and trauma research with adults suggesting that emotional distress can be understood as an indicator of engagement in a data collection process rather than as an indicator of harm [50,51,52].
Although the overall levels of distress and negative effects reported in our study were low, adolescents reported the highest scores, and a few mentioned having experienced anxiety or unpleasant memories. This has also been reported with regard to adolescents participating in health-related studies [53]. As suggested above, these emotional reactions may be due to participants’ engagement with the research project [51], and a study by Hawton and colleagues [34] suggested that this may lead to them benefitting more from participating than adults. However, it may also point to the presence of emotional problems [53,54]. One study in a systematic review [53] examining children’s and adolescents’ reactions to participating in biomedical and health-related studies found that the presence of emotional problems in children was the only variable associated with short-lived negative research participation experiences [55]. Objective variables such as age, gender, methods of data collection, and topic/health condition examined in the studies, were not associated with participants’ appraisals of study participation [53,55]. Another study on pain also reported that age and level of pain did not affect responses regarding experiences of research participation [56]. However, as in our study, young participants still recommended participation to others [56]. Nonetheless, while only a few participants reported negative experiences, the phenomenon needs further investigation in bereaved adolescents, especially since both short-term deterioration and improvement in mood have been reported in adolescent mental health research [54].
Parents in our study were very positive about research participation. This is corroborated by other research with parents who participated in a study concerning the sudden and traumatic death of their children [27]. All parents in that study reported positive experiences and none regretted participating, despite 73% experiencing the interviews as (a little to very) painful [27]. As in our study, having the opportunity to share experiences and being able to help others contributed to a positive experience [27]. Still, one parent in our study reported being emotionally affected, although this parent still perceived participation as helpful. Follow-up data from adults participating in suicide research revealed that participants can be susceptible to short-term deteriorations in mood [57]. However, any negative effects of participation were confined to the days immediately following the study and this temporary deterioration in mood did not increase risk of suicidal thoughts [57].
As with research with bereaved adolescents, research with suicide bereaved adults indicated that objective factors such as gender of participants, their relationship to the deceased, the method of suicide, and time since loss appeared to have little effect on their experiences of participating in a research interview [58]. Moreover, research regarding mental health in adults showed that the presence of mental health problems did not differentiate participants with negative or positive experiences of research participation [59]. Hence, it may be that the presence of emotional problems has a stronger impact on the research experience of children and adolescents compared to adults, though further research is needed to ascertain such differences between children/adolescents and adults.
Clinicians in our study found research participation to be a learning experience. This is supported by findings from studies with clinicians who had lost a patient to suicide, who reported their research participation as a learning and therapeutic experience [60,61]. The finding is also in line with literature on substance abuse research participation [62]. Clinical research participants were more willing to use research findings in practice, especially those with favorable attitudes toward evidence-based practices and whose agencies supported professional growth. The combined findings of our study and others from the literature [60,62] suggest that research participation may reinforce clinicians’ willingness to use research findings in practice, thus contributing to quality of services.
Although our participants expressed gratitude for being involved in the research, a phenomenon also noted in the literature [63], our data suggest that from the three groups of participants, adolescents potentially experience the most distress and negative effects of participation in research interviews. Thus, researchers must inform potential participants, especially adolescents, about both the potential benefits and distress of research participation, and implement appropriate participant distress management protocols. As Parkes [64] pointed out, if a participant becomes distressed, “the needs of the respondent should take priority over the needs of the research” (p. 174). According to such protocols, researchers must provide support to a distressed interview participant according to the level of distress. This can range from allowing them to pause or withdraw from participation, providing emotional support to participants, providing or arranging referral to an appropriate support service (which may include a parent or guardian), or calling medical emergency services.
The literature indicates the important roles of narrating and sharing grief experiences in the processes of meaning-making and personal growth in those bereaved by suicide, which may also contribute to a positive experience as a study participant [10,58]. Interactions with a skilled and empathetic interviewer can also contribute to positive experiences for bereaved study participants [48,65]. While researchers must be sensitive to potential distress in participants, and provide emotional support if needed, they must also be aware of the potential methodological and ethical challenges when research and therapy blur [50,66]. For example, Biddle and colleagues [50] cautioned that participants may share information that they do not want to be used for the research, and researchers may not have the skills or capacity to deal with the distress or unintended shared information from the participant [50,64,66]. Hence, our findings and the broader literature imply that research interviews must be conducted by experienced and properly trained interviewers who can deal with participants’ emotions and make judgements about pausing or continuing an interview, or referring participants to external support [50,64,66]. Further research is needed to clarify the role of the researcher and their approach to participants regarding balancing data collection and being empathic and supportive for the research experience of bereaved participants [48,65,67,68].
To fully understand the study findings, it is important to note that the study involved participants who volunteered to share their experiences, and study participants may not be representative of the population from which they are recruited. In a bereavement study, Akard and colleagues [69] found that those who are motivated and have the capacity to participate tended to respond to the initial researchers’ invitations, and sending more than three invitations hardly increased the response rate [69]. Bereaved people who perceive research participation as too difficult may either decline participation or refuse passively by not responding [69,70]. These findings of the literature indicate the soundness of (potential) participants’ judgements about research participation [50] and indicate that participants make appropriate cost–benefit appraisals of their participation [52]. Research is needed to confirm these observations in adolescents bereaved by suicide, parents or other family members of bereaved adolescents, and clinicians. Nonetheless, researchers and research ethics committees may consider these when designing and assessing research studies in this field. In addition, participants in our study had experienced the bereavement at least six months before participating, which may also have contributed to participants reporting little distress.
Limitations
The study involved a modest sample from a qualitative interview study. Despite the high response rate, the findings may not reflect the experiences of those who were invited to participate and chose not to. It is also not known whether findings apply to participants of other interview studies or studies utilizing other methods of data collection. Further, the survey did not include definitions of ‘distress’ or ‘negative effects’, and data were collected only at one point in time shortly after research participation. Future studies could include pre- and post-measures and longitudinal follow-up to assess any longer-term consequences.
5. Conclusions
The study clearly indicates that bereaved adolescents, parents and clinicians can safely participate in research interviews regarding their experiences of grief and help after suicide and other traumatic death. Participants reported that they experienced little distress and would recommend participation to others. To prevent and mitigate potential distress, training of research staff and implementation of appropriate participant distress protocols are imperative. Future studies could include longitudinal follow-up of participants.
Acknowledgments
We are most grateful to the participants for sharing their experiences, and to the numerous individuals and organizations who helped with recruitment and/or hosted the focus groups, especially: The Compassionate Friends Victoria, Support After Suicide Jesuits Social Services, Standby Support After Suicide, headspace National, Anglicare Suicide Prevention and Grief Support South Australia, Sabrina’s Reach 4 Life, and the Australian Centre for Grief and Bereavement.
Author Contributions
Conceptualization, K.A., D.R. and J.P.; methodology, K.A.; software, K.A.; data collection, K.A. and K.K.; formal analysis, K.A. and K.K.; writing—original draft preparation, K.A.; writing—review and editing, K.A., K.K., D.R. and J.P.; supervision, D.R. and J.P.; project administration, K.A.; funding acquisition, K.A. All authors have read and agreed to the published version of the manuscript.
Funding
K.A. is supported by a National Health and Medical Research Council Early Career Fellowship (GNT1157796) and an Early Career Researcher Grant of The University of Melbourne (ECR1202020). J.P. is funded by a National Health and Medical Research Council Investigator Grant (GNT1173126).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Human Research Ethics Committee of The University of Melbourne (ID 1955213, 8 October 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
According to the ethics approval, data can only be accessed by the members of the research team.
Conflicts of Interest
The authors declare no conflict of interest. The funding bodies had no role in the design of the study, the collection, analysis and interpretation of data, the writing of the manuscript, and the decision to submit it for publication.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Feigelman W., Rosen Z., Joiner T., Silva C., Mueller A.S. Examining longer-term effects of parental death in adolescents and young adults: Evidence from the national longitudinal survey of adolescent to adult health. Death Stud. 2017;41:133–143. doi: 10.1080/07481187.2016.1226990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balk D.E. Dealing with Dying, Death, and Grief during Adolescence. Routledge; New York, NY, USA: 2014. [Google Scholar]
- 3.Andriessen K., Mowll J., Lobb E., Draper B., Dudley M., Mitchell P.B. “Don’t bother about me”. The grief and mental health of bereaved adolescents. Death Stud. 2018;42:607–615. doi: 10.1080/07481187.2017.1415393. [DOI] [PubMed] [Google Scholar]
- 4.De Rosbo-Davies C., Laletas S., Round P. Daughters’ experiences of maternal bereavement during adolescence: A scoping review. Death Stud. 2021:1–11. doi: 10.1080/07481187.2021.1900454. Online ahead of print . [DOI] [PubMed] [Google Scholar]
- 5.Farella Guzzo M., Gobbi G. Parental death during adolescence: A review of the literature. Omega. 2021:1–31. doi: 10.1177/00302228211033661. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 6.Bartik W., Maple M., Edwards H., Kiernan M. Adolescent survivors after suicide—Australian young people’s bereavement narratives. Crisis. 2013;34:211–217. doi: 10.1027/0227-5910/a000185. [DOI] [PubMed] [Google Scholar]
- 7.Brent D., Melhem N., Donohoe M.B., Walker M. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. Am. J. Psychiatry. 2009;166:786–794. doi: 10.1176/appi.ajp.2009.08081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pham S., Porta G., Biernesser C., Walker Payne M., Iyengar S., Melhem N., Brent D.A. The burden of bereavement: Early-onset depression and impairment in youths bereaved by sudden parental death in a 7-year prospective study. Am. J. Psychiatry. 2018;175:887–896. doi: 10.1176/appi.ajp.2018.17070792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Del Carpio L., Paul S., Paterson A., Rasmussen S. A systematic review of controlled studies of suicidal and self-harming behaviours in adolescents following bereavement by suicide. PLoS ONE. 2021;16:e0254203. doi: 10.1371/journal.pone.0254203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levi-Belz Y., Krysinska K., Andriessen K. “To turn a personal tragedy into a triumph”: A systematic review and meta-analysis of studies on posttraumatic growth among suicide survivors. Psychol. Trauma. 2021;13:322–332. doi: 10.1037/tra0000977. [DOI] [PubMed] [Google Scholar]
- 11.Şimşek Arslan B., Özer Z., Buldukoğlu K. Posttraumatic growth in parentally bereaved children and adolescents: A systematic review. Death Stud. 2020:1–13. doi: 10.1080/07481187.2020.1716886. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 12.Tedeschi R.G., Shakespeare-Finch J., Taku K., Calhoun L.G. Posttraumatic Growth: Theory, Research, and Application. Routledge; New York, NY, USA: 2018. [Google Scholar]
- 13.Andriessen K., Krysinska K., Rickwood D., Pirkis J. “It changes your orbit”: The impact of suicide and traumatic death on adolescents as experienced by adolescents and parents. Int. J. Environ. Res. Public Health. 2020;17:9356. doi: 10.3390/ijerph17249356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann W.A., Myburgh C., Poggenpoel M. The lived experiences of late-adolescent female suicide survivors: ‘A part of me died’. Health SA Gesondheid. 2010;15:1–9. doi: 10.4102/hsag.v15i1.493. [DOI] [Google Scholar]
- 15.Cerel J., Jordan J.R., Duberstein P.R. The impact of suicide on the family. Crisis. 2008;29:38–44. doi: 10.1027/0227-5910.29.1.38. [DOI] [PubMed] [Google Scholar]
- 16.Glazer H.R., Clark M.D., Thomas R., Haxton H. Parenting after the death of a spouse. Am. J. Hosp. Palliat. Med. 2010;27:532–536. doi: 10.1177/1049909110366851. [DOI] [PubMed] [Google Scholar]
- 17.The National Health and Medical Research Council, the Australian Research Council and Universities Australia. Commonwealth of Australia; Canberra, Australia: 2018. [(accessed on 11 October 2021)]. National Statement on Ethical Conduct in Human Research 2007 (Updated 2018) Available online: https://www.nhmrc.gov.au/about-us/publications/nationalstatement-ethical-conduct-human-research-2007-updated-2018. [Google Scholar]
- 18.Andriessen K., Reifels L., Krysinska K., Robinson J., Dempster G., Pirkis J. Dealing with ethical concerns in suicide research: A survey of Australian researchers. Int. J. Environ. Res. Public Health. 2019;16:1094. doi: 10.3390/ijerph16071094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andriessen K., Reifels L., Krysinska K., Robinson J., Dempster G., Pirkis J. Ethical concerns in suicide research: Results of an international researcher survey. J. Empir. Res. Hum. Res. Ethics. 2019;14:383–394. doi: 10.1177/1556264619859734. [DOI] [PubMed] [Google Scholar]
- 20.Barnard E., Dempster G., Krysinska K., Reifels L., Robinson J., Pirkis J., Andriessen K. Ethical concerns in suicide research: Thematic analysis of the views of human research ethics committees in Australia. BMC Med. Ethics. 2021;22:41. doi: 10.1186/s12910-021-00609-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hom M.A., Podlogar M.C., Stanley I.H., Joiner T.E., Jr. Ethical issues and practical challenges in suicide research. Crisis. 2016;38:107–114. doi: 10.1027/0227-5910/a000415. [DOI] [PubMed] [Google Scholar]
- 22.McClinton Appollis T., Lund C., de Vries P.J., Mathews C. Adolescents’ and adults’ experiences of being surveyed about violence and abuse: A systematic review of harms, benefits, and regrets. Am. J. Public Health. 2015;105:e31–e45. doi: 10.2105/AJPH.2014.302293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenbaum A., Langhinrichsen-Rohling J. Meta-research on violence and victims: The impact of data collection methods on findings and participants. Violence Vict. 2006;21:404–409. doi: 10.1891/0886-6708.21.4.404. [DOI] [PubMed] [Google Scholar]
- 24.Gysels M.H., Evans C., Higginson I.J. Patient, caregiver, health professional and researcher views and experiences of participating in research at the end of life: A critical interpretive synthesis of the literature. BMC Med. Res. Methodol. 2012;12:1–17. doi: 10.1186/1471-2288-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jorm A.F., Kelly C.M., Morgan A.J. Participant distress in psychiatric research: A systematic review. Psychol. Med. 2007;37:917–926. doi: 10.1017/S0033291706009779. [DOI] [PubMed] [Google Scholar]
- 26.Hiriscau E.I., Stingelin-Giles N., Wasserman D., Reiter-Theil S. Identifying ethical issues in mental health research with minors adolescents: Results of a Delphi study. Int. J. Environ. Res. Public Health. 2016;13:489. doi: 10.3390/ijerph13050489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dyregrov K. Bereaved parents’ experience of research participation. Soc. Sci. Med. 2004;58:391–400. doi: 10.1016/S0277-9536(03)00205-3. [DOI] [PubMed] [Google Scholar]
- 28.Buckle J.L., Dwyer S.C., Jackson M. Qualitative bereavement research: Incongruity between the perspectives of participants and research ethics boards. Int. J. Soc. Res. Methodol. 2010;13:111–125. doi: 10.1080/13645570902767918. [DOI] [Google Scholar]
- 29.Feigelman W., Jordan J.R., McIntosh J.L., Feigelman B. Devastating Losses: How Parents Cope with the Death of a Child to Suicide or Drugs. Springer; New York, NY, USA: 2012. [Google Scholar]
- 30.Omerov P., Steineck G., Dyregrov K., Runeson B., Nyberg U. The ethics of doing nothing. Suicide-bereavement and research: Ethical and methodological considerations. Psychol. Med. 2014;44:3409–3420. doi: 10.1017/S0033291713001670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore M., Maple M., Mitchell A.M., Cerel J. Challenges and opportunities for suicide bereavement research: The experience of ethical board review. Crisis. 2013;34:297–304. doi: 10.1027/0227-5910/a000191. [DOI] [PubMed] [Google Scholar]
- 32.Andriessen K., Krysinska K., Draper B., Dudley M., Mitchell P.B. Harmful or helpful? A systematic review of how those bereaved through suicide experience research participation. Crisis. 2018;39:364–376. doi: 10.1027/0227-5910/a000515. [DOI] [PubMed] [Google Scholar]
- 33.Cooper J. Ethical issues and their practical application in a psychological autopsy study of suicide. J. Clin. Nurs. 1999;8:467–475. doi: 10.1046/j.1365-2702.1999.00276.x. [DOI] [PubMed] [Google Scholar]
- 34.Hawton K., Houston K., Malmbergand A., Simkin S. Psychological autopsy interviews in suicide research: The reactions of informants. Arch. Suicide Res. 2003;7:73–82. doi: 10.1080/13811110301566. [DOI] [Google Scholar]
- 35.Andriessen K., Krysinska K., Rickwood D., Pirkis J. “Finding a safe space”. What makes help helpful for adolescents bereaved by suicide: A thematic analysis. Death Stud. 2021:1–11. doi: 10.1080/07481187.2021.1970049. Online ahead of print . [DOI] [PubMed] [Google Scholar]
- 36.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 37.Heath J., Williamson H., Williams L., Harcourt D. “It’s just more personal”: Using multiple methods of qualitative data collection to facilitate participation in research focusing on sensitive subjects. Appl. Nurs. Res. 2018;43:30–35. doi: 10.1016/j.apnr.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 38.Guest G., Namey E., Taylor J., Eley N., McKenna K. Comparing focus groups and individual interviews: Findings from a randomized study. Int. J. Soc. Res. Methodol. 2017;20:693–708. doi: 10.1080/13645579.2017.1281601. [DOI] [Google Scholar]
- 39.Guest G., Namey E., McKenna K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods. 2017;29:3–22. doi: 10.1177/1525822X16639015. [DOI] [Google Scholar]
- 40.Malterud K., Siersma V.D., Guassora A.D. Sample size in qualitative interview studies: Guided by information power. Qual. Health. Res. 2016;26:1753–1760. doi: 10.1177/1049732315617444. [DOI] [PubMed] [Google Scholar]
- 41.Guest G., Bunce A., Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. doi: 10.1177/1525822X05279903. [DOI] [Google Scholar]
- 42.DeCuir-Gunby J.T., Marshall P.L., McCulloch A.W. Developing and using a codebook for the analysis of interview data: An example from a professional development research project. Field Methods. 2011;23:136–155. doi: 10.1177/1525822X10388468. [DOI] [Google Scholar]
- 43.Braun V., Clarke V., Hayfield N., Terry G. Thematic Analysis. In: Liamputtong P., editor. Handbook of Research Methods in Health Social Sciences. Springer; Singapore: 2019. pp. 843–860. [DOI] [Google Scholar]
- 44.Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 45.IBM Corp . IBM SPSS Statistics for Windows, Version 26.0. IBM Corp.; Armonk, NY, USA: 2019. [Google Scholar]
- 46.Bryman A. Social Research Methods. 4th ed. Oxford University Press; Oxford, UK: 2012. [Google Scholar]
- 47.Butler A.E., Hall H., Copnell B. Bereaved parents’ experiences of research participation. BMC Palliat. Care. 2018;17:1–9. doi: 10.1186/s12904-018-0375-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hynson J.L., Aroni R., Bauld C., Sawyer S.M. Research with bereaved parents: A question of how not why. Palliat. Med. 2006;20:805–811. doi: 10.1177/0269216306072349. [DOI] [PubMed] [Google Scholar]
- 49.Eilegård A., Steineck G., Nyberg T., Kreicbergs U. Bereaved siblings’ perception of participating in research—A nationwide study. Psycho-Oncology. 2013;22:411–416. doi: 10.1002/pon.2105. [DOI] [PubMed] [Google Scholar]
- 50.Biddle L., Cooper J., Owen-Smith A., Klineberg E., Bennewith O., Hawton K., Kapur N., Donovan J., Gunnell D. Qualitative interviewing with vulnerable populations: Individuals’ experiences of participating in suicide and self-harm based research. J. Affect. Disord. 2013;145:356–362. doi: 10.1016/j.jad.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 51.Dyregrov K., Dyregrov A., Raundalen M. Refugee families’ experience of research participation. J Trauma Stress. 2000;13:413–426. doi: 10.1023/A:1007777006605. [DOI] [PubMed] [Google Scholar]
- 52.Newman E., Kaloupek D.G. The risks and benefits of participating in trauma-focused research studies. J Trauma Stress. 2004;17:383–394. doi: 10.1023/B:JOTS.0000048951.02568.3a. [DOI] [PubMed] [Google Scholar]
- 53.Crane S., Broome M.E. Understanding ethical issues of research participation from the perspective of participating children and adolescents: A systematic review. Worldviews Evid. Based Nurs. 2017;14:200–209. doi: 10.1111/wvn.12209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hasking P., Tatnell R.C., Martin G. Adolescents’ reactions to participating in ethically sensitive research: A prospective self-report study. Child Adolesc. Psychiatry Ment. Health. 2015;9:1–12. doi: 10.1186/s13034-015-0074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ellonen N., Pösö T. Children’s experiences of completing a computer-based violence survey: Ethical implications. Child. Soc. 2011;25:470–481. doi: 10.1111/j.1099-0860.2010.00292.x. [DOI] [Google Scholar]
- 56.Hawley K., Huang J.S., Goodwin M., Diaz D., de Sa V.R., Birnie K.A., Chambers C.T., Craig K.D. Youth and parent appraisals of participation in a study of spontaneous and induced pediatric clinical pain. Ethics Behav. 2019;29:259–273. doi: 10.1080/10508422.2018.1463163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Littlewood D.L., Harris K., Gooding P., Pratt D., Haddock G., Peters S. Using my demons to make good: The short-and long-term impact of participating in suicide-related research. Arch. Suicide Res. 2021;25:315–339. doi: 10.1080/13811118.2019.1663330. [DOI] [PubMed] [Google Scholar]
- 58.Dyregrov K.M., Dieserud G., Hjelmeland H.M., Straiton M., Rasmussen M.L., Knizek B.L., Leenaars A.A. Meaning-making through psychological autopsy interviews: The value of participating in qualitative research for those bereaved by suicide. Death Stud. 2011;35:685–710. doi: 10.1080/07481187.2011.553310. [DOI] [PubMed] [Google Scholar]
- 59.Tan D.P., Morgan A.J., Jorm A.F., Reavley N.J. Emotional impacts of participation in an Australian national survey on mental health-related discrimination. Ethics Behav. 2019;29:438–458. doi: 10.1080/10508422.2019.1593844. [DOI] [Google Scholar]
- 60.Hendin H., Lipschitz A., Maltsberger J.T., Haas A.P., Wynecoop S. Therapists’ reactions to patients’ suicides. Am. J. Psychiatr. 2000;157:2022–2027. doi: 10.1176/appi.ajp.157.12.2022. [DOI] [PubMed] [Google Scholar]
- 61.Dransart D.A.C., Treven M., Grad O.T., Andriessen K. Impact of client suicide on health and mental health professionals. In: Andriessen K., Krysinska K., Grad O.T., editors. Postvention in Action: The International Handbook of Suicide Bereavement Support. Hogrefe; Göttingen, Germany: Boston, MA, USA: 2017. pp. 245–254. [Google Scholar]
- 62.Pinto R.M., Yu G., Spector A.Y., Gorroochurn P., McCarty D. Substance abuse treatment providers’ involvement in research is associated with willingness to use findings in practice. J. Subst. Abus. Treat. 2010;39:188–194. doi: 10.1016/j.jsat.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilson A. Consumer participation: Ensuring suicide postvention research counts for end users. Int. J. Nurs. Pr. 2010;16:7–13. doi: 10.1111/j.1440-172X.2009.01811.x. [DOI] [PubMed] [Google Scholar]
- 64.Parkes C.M. Guidelines for conducting ethical bereavement research. Death Stud. 1995;19:171–181. doi: 10.1080/07481189508252723. [DOI] [PubMed] [Google Scholar]
- 65.Caserta M., Utz R., Lund D., De Vries B. Sampling, recruitment, and retention in a bereavement intervention study: Experiences from the Living After Loss project. Omega. 2010;61:181–203. doi: 10.2190/OM.61.3.b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rosenblatt P.C. Ethics of qualitative interviewing with grieving families. Death Stud. 1995;19:139–155. doi: 10.1080/07481189508252721. [DOI] [PubMed] [Google Scholar]
- 67.Kitson G.C., Clark R.D., Rushforth N.B., Brinich P.M., Sudak H.S., Zyzanski S.J. Research on difficult family topics: Helping new and experienced researchers cope with research on loss. Fam. Relat. 1996;45:183–188. doi: 10.2307/585289. [DOI] [Google Scholar]
- 68.Henry M., Greenfield B.J. Therapeutic effects of psychological autopsies: The impact of investigating suicides on interviewees. Crisis. 2009;30:20–24. doi: 10.1027/0227-5910.30.1.20. [DOI] [PubMed] [Google Scholar]
- 69.Akard T.F., Gilmer M.J., Miller K., Steele A.C., Hancock K., Barrera M., Compas B., Davies B., Dietrich M.S., Fairclough D.L., et al. Factors affecting recruitment and participation of bereaved parents and siblings in grief research. Prog. Palliat. Care. 2014;22:75–79. doi: 10.1179/1743291X13Y.0000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Burnell R.H., O’Keefe M. Asking parents unaskable questions. Lancet. 2004;364:737–738. doi: 10.1016/S0140-6736(04)16950-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
According to the ethics approval, data can only be accessed by the members of the research team.