Abstract
Background: Comprehensive geriatric assessment (CGA), as a complex diagnostic process, allows medical specialists to recognize the capabilities and limitations of the patient in older age. This study aimed to evaluate the prevalence and severity of deficits typical of seniors and find relationships between CGA results and selected factors.
Methods: A cross-sectional questionnaire study was performed in Krakow among patients aged 65 years and over visiting their general practitioners (GPs). CGA was conducted using eight scales: the Activities of Daily Living (ADL), Mini-Mental State Examination, Instrumental Activities of Daily Living (IADL), Geriatric Depression Scale, Timed Up and Go Test, Mini Nutritional Assessment Short Form, Clinical Frailty Scale, and Athens Insomnia Scale.
Results: Four hundred and thirty-eight patients, aged between 65 and 96 years, were examined. Most of them received high scores in the assessed aspects. The most common abnormalities were sleep disorders (42 %), symptoms of frailty (33 %), and depressive tendency (32 %). Age correlated with every aspect assessed in CGA and worsened as patients grew older (in all cases p <0.05). Male gender reduced the chance of depressive disorders [odds ratio (OR) =0.6 (0.39-0.92); p =0.02]. The strongest association was found between ADL and IADL scales [OR =153.56 (34.86-676.48); p <0.001].
Conclusions: Even though patients who attended general practices were functioning well in everyday life, after analysis, they manifested deficits in some areas of CGA. The most widespread problems in the geriatric population were depressive symptoms, frailty, and insomnia, and that is why GPs should ask about sleep and mood disorders during visits and assess the occurrence of frailty. HIPPOKRATIA 2020, 24(4): 173-181.
Keywords: General practitioner, primary care, seniors, Central Europe, comprehensive geriatric assessment
Introduction
Comprehensive geriatric assessment (CGA) is a routinely used diagnostic tool in modern geriatric practice1. It is defined as a complex process that allows recognition of a patient’s medical, psychosocial, and functional capabilities and limitations in older age. It can later lead to the formation of a therapeutic plan for them2.
CGA focuses on early screening of risk factors for an unsuccessful model of aging, correct prognosis, and recognition of previously undiagnosed health problems1,2. This method enables tailored treatment of various age-related problems and, in that way, reduces functional decline in older patients and improves their quality of life3. The assessment of a geriatric patient is performed using various questionnaires and scales to analyze their condition in a comprehensive manner2. Regularly performed CGA provides the doctor with feedback on the effectiveness of treatment and allows its optimization.
Until now, CGA has only been evaluated in hospitalised4 and oncological patients5. The research conducted has confirmed the usefulness and effectiveness of CGA in these patient groups. Still, however, there is little information on the use of CGA by general practitioners (GPs) in Europe. Research on this topic has been carried out so far in some countries like Germany6, but, in most cases, not every domain of CGA has been evaluated, which makes the assessment incomplete and not valid for comparisons.
In Poland and other Central and Eastern Europe countries, CGA is an understudied topic, especially in primary care. To the best of our knowledge, no recently published data about the usage of CGA by GPs in Poland are available. Accordingly, there is a need for GPs to have access to information on the most common geriatric deficits among patients registered to their practices and which issues should be given special attention when conducting a geriatric assessment. In our country, CGA is usually initiated and performed by geriatricians7. According to the Ministry of Health, there are only around 450 geriatricians in Poland, which hinders access to specialist services8.
Research on the implementation of CGA in outpatient clinics has not been carried out so far, although GPs have performed some evaluation of the functional status of geriatric patients9. In 2012, the PolSenior project was carried out in Poland, which included the assessment of the health status, general condition, limitations, and deficiencies of older people and analyzed their socioeconomic situation. It allowed the creation of a comprehensive picture of the aging society in Poland10.
Recently, it has been observed that in Poland, as in many other countries, people tend to live longer than previously. According to data from the Central Statistical Office, in 2017, the population in this country was 38.4 million, of whom 6.3 million were aged 65 years and over. Among the elderly, there is a significant increase in the female population of society - there are 160 women per 100 men. The current life expectancy for an average man is 74.0, and for an average woman is 81.8 years. It is predicted that there will be about 5.4 million more people aged 65 and over in 2050 than today11.
Aging is inseparably connected with the accumulation of geriatric deficits, and this indicates why CGA in general practice is of great importance now and in the future10. Due to the rapid aging of society, in our project, we wanted to examine elderly patients attending GPs’ surgeries and receive information about their health using tools from CGA.
The study’s objective was the evaluation of prevalence and severity of functional limitations of basic and complex activities in everyday life, cognitive function problems, mood disorders, risk of falls, malnutrition, frailty syndrome, and insomnia. The next objective was to determine the relationships between CGA results and selected social, economic, demographic, and medical factors.
Material and methods
Design
We conducted a cross-sectional questionnaire study in Krakow and nearby towns and villages among patients aged over 65 years. With over 771 thousand citizens, Krakow is the second-largest and one of the oldest cities in Poland and is situated in the southern part of the country.
Setting
The study was performed in 15 primary care practices randomly selected among all practices cooperating with the Department of Family Medicine at the Jagiellonian University Medical College (n =47). Each primary care practice was assigned a number from 1 to 47. The computer program randomly generated 15 numbers corresponding to the practices, which then participated in the study.
Population studied
We recruited in the study patients aged 65-years-old and above. Other inclusion criteria were: the status of being registered on the list of GP’s patients, the possibility of in-person attendance at the practice, and providing written informed consent to participate in the project. The exclusion criteria were: life expectancy below six months and inability to communicate in Polish. Seniors were divided into three subgroups depending on their age: young-old (65 to 74 years), middle-old (75 to 84 years), and oldest-old (above 84 years). Every subject attending the primary care practices, who met the inclusion criteria, was asked to participate in the study until 30 patients from each practice had enrolled (consecutive sampling).
The study sample was determined by subjective judgment and consensus between one experienced geriatrician and two family physicians. They took into account the number of practices cooperating with the Department of Family Medicine at the Jagiellonian University Medical College (n =47), the number of people over 65 years old in Poland (17 % of the total population), and the number of patients per GP (1,400). Since our study was carried out only in GP surgeries, bedridden patients and permanently housebound patients were not included.
Data collection
The data was collected from April 2018 to April 2019, and all participants completed a questionnaire regarding their personal data. Only the principal researcher knew the name and surname of the patients. Confidential data were not recorded in the individual questionnaires and did not enter into the database. The study’s researchers could not link the patient’s informed consent with the completed questionnaires.
Afterward, a researcher (a trained physician) conducted the process of CGA using the eight various tools described below. The earlier accomplished training consisted of a two-hour session with an experienced geriatrician, during which the theoretical basis of CGA was discussed, and practical training in conducting CGA was carried out.
Research tools and procedure
A questionnaire, developed by the authors, was used to collect essential information and medical data regarding participants. The first section recorded gender, age, biometric parameters, education, habitation, marital status, and professional activity. The second focused on questions about chronic diseases, feeling of pain, medication intake, smoking, physical activity, prophylaxis, and use of medical services. Altogether, the questionnaire consisted of 16 closed and four semi-opened questions. It was tested in a group of 10 patients older than 65 years, who did not submit comments or note difficulties in completing it. The content validity was checked by comparing the questionnaire with other similar tools used in Poland.
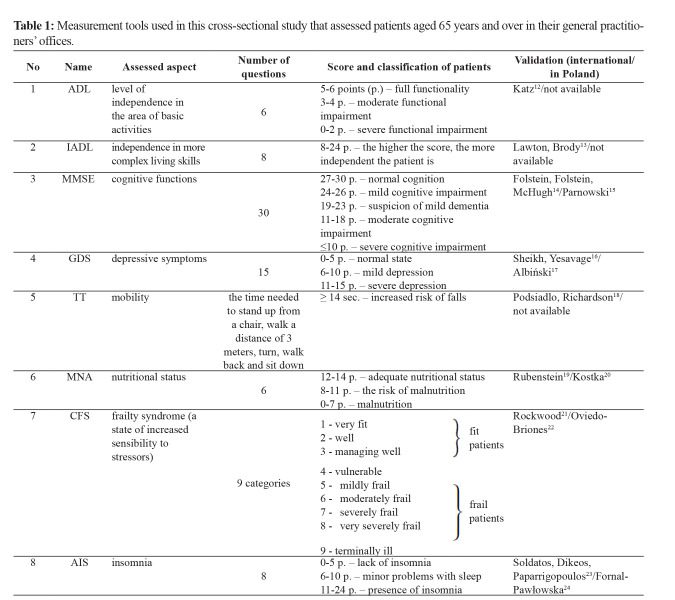
Subsequently, CGA was conducted using eight scales: the Activities of Daily Living (ADL)12, Instrumental Activities of Daily Living (IADL)13, Mini-Mental State Examination (MMSE)14,15, Geriatric Depression Scale (GDS)16,17, Timed Up and Go Test (TT)18, Mini Nutritional Assessment Short Form (MNA)19,20, Clinical Frailty Scale (CFS)21,22 and Athens Insomnia Scale (AIS)23,24. These scales are briefly described in Table 1.
Table 1. Measurement tools used in this cross-sectional study that assessed patients aged 65 years and over in their general practitioners’ offices.
In order to assess trends in the deficiency-indicating results of CGA tests, when a participant had no dysfunctions in any of the areas assessed in CGA, they were assigned 0. When there was only one dysfunction, they scored 1, when two dysfunctions, 2, and so on.
Statistical analysis
Statistical analysis was performed using Statistica, version 13.3 (Statsoft Polska, Kraków, Poland). Data are presented as median with interquartile range (Q1-Q3), besides the results of IADL which are presented as mean score and standard deviation. The Shapiro-Wilk test was used as a normality test. The Chi-square test was used to compare proportions. A logistic regression model was used to define associations between patients’ individual factors and the results of CGA tests. The results are presented in the form of odds ratio (OR) parameter values with a 95 % confidence interval. Statistical significance was set at 0.05.
Ethical considerations
The Bioethical Commission of the Jagiellonian University Medical College approved this study (permission 1072.6120.252.2017), and every participant was given written information and was also verbally informed by the researcher regarding the purposes of this study before signing the informed consent.
Results
Characteristics of the participants
An invitation to enroll in the study was addressed to 582 patients and 438 of these, in the age range of 65 to 96 years, were included (response rate: 75.3 %). The mean age of participants was 75.6 ± 7.9 years (women: 76.0 ± 8.2 years; men: 75.02 ± 7.29 years). Detailed characteristics of the participants are shown in Table 2.
Table 2. Characteristic of the 438 participants, aged 65 years and over.
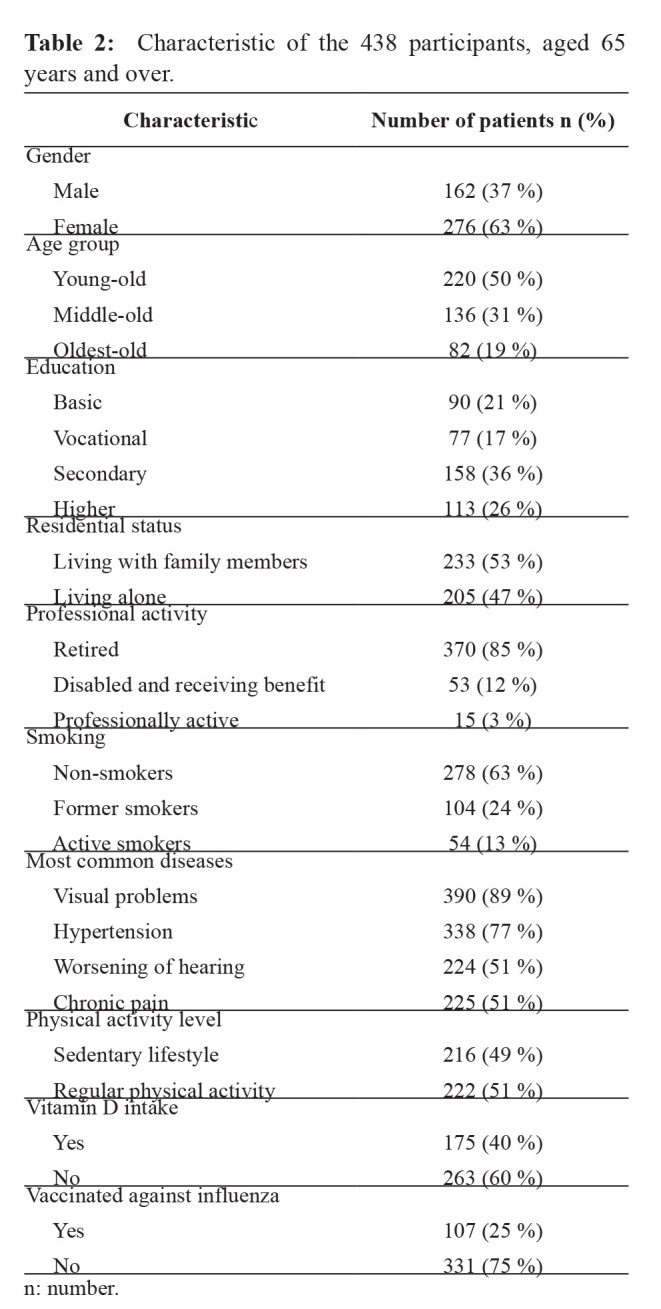
n: number.
Results of particular areas of CGA
Results of particular areas of CGA by age group are shown in Figure 1. Each graph shows the median, lower and upper quartile, and the maximum and minimum results achieved by the study participants. Each of the eight CGA areas analyzed was presented in relation to all patients (first graph element), followed by young-old, middle-old, and oldest-old patients (successive graph elements). Detailed explanations of the scoring of specific scales can be found in the fifth column of Table 1. For example, for insomnia in all patients, the median was five points, the lowest score was zero points (no insomnia), and the highest score was 21 (severe insomnia).
Figure 1. Comprehensive geriatric assessment in 438 patients in general practitioners’ offices by age group. ADL: the Activities of Daily Living, IADL: the Instrumental Activities of Daily Living, GDS: Geriatric Depression Scale, AIS: Athens Insomnia Scale, MNA: Mini Nutritional Assessment Short Form, TT: Timed Up and Go Test, MMSE: Mini-Mental State Examination, CFS: Clinical Frailty Scale.
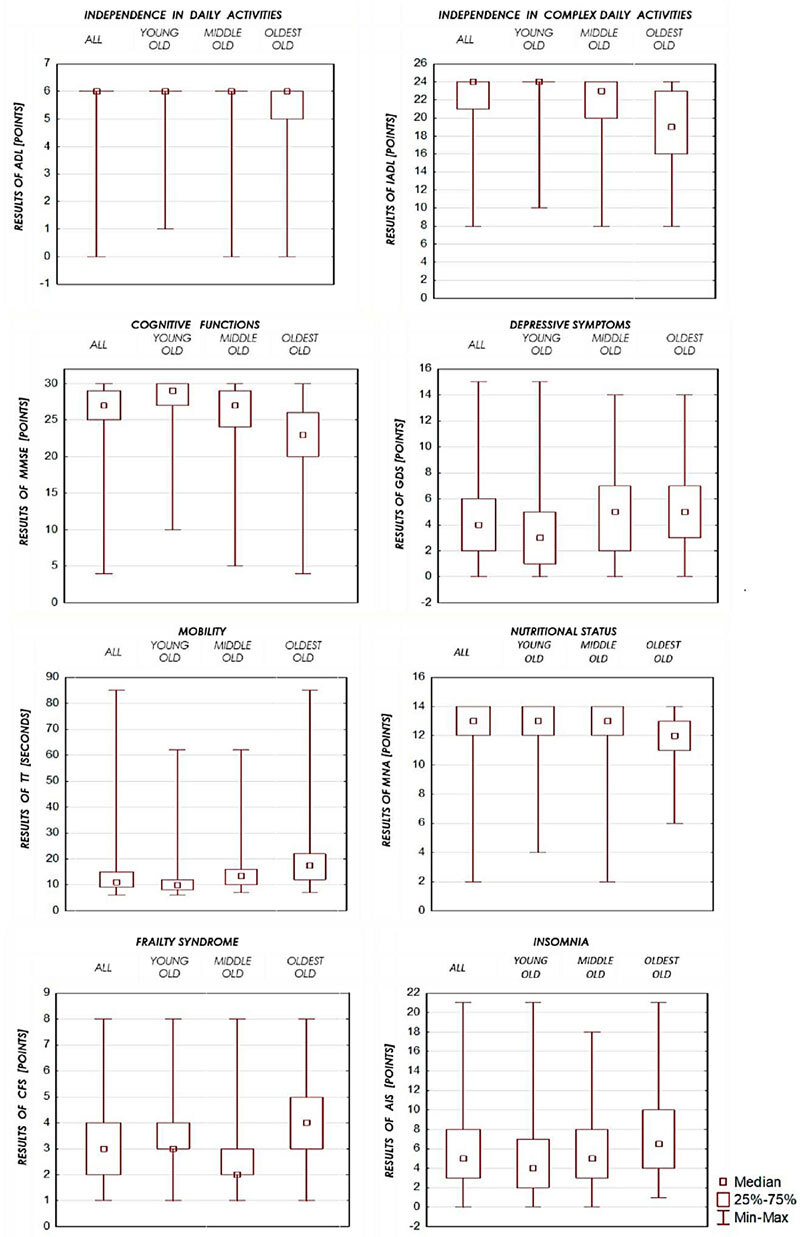
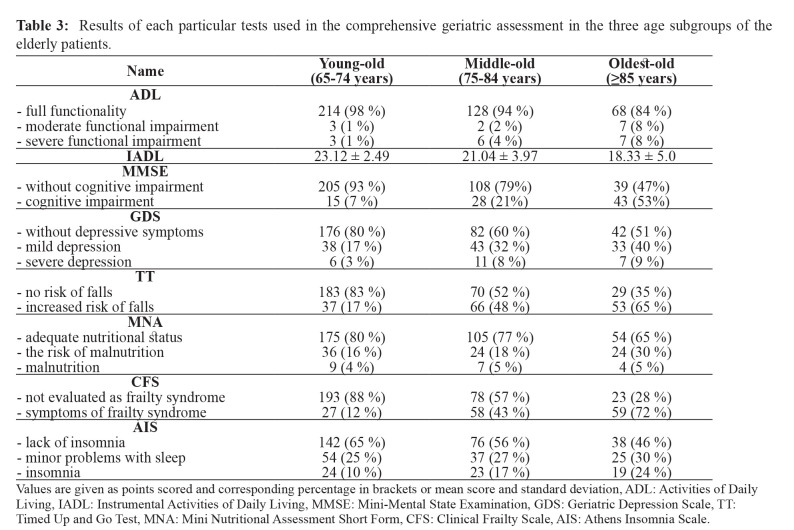
Daily activities
In ADL that assesses self-care, the median (Q1-Q3) was six (6-6) points. The large majority of seniors (410; 94 %) were fully independent (5-6 points in ADL). Twelve people (3 %) had moderate and 16 (4 %) severe functional impairment. The most demanding activity performed by themselves was bathing (44; 10%), while almost all could eat independently (431; 98%).
In the IADL questionnaire, the median was 24 (21-24) points. Maximum scores in this test were obtained by only 241 people (55 %). In most cases, patients had problems with longer walks (121; 27 %) and doing household duties (138; 31 %), while many of them were able to use the phone correctly (371; 85 %).
Mental state
In MMSE, the median was 27 (25-29) points. Most participants of our study did not present cognitive deficits (352; 80 %), whereas the others (86; 20 %) had symptoms of cognitive impairment. Mostly, seniors had problems with naming the exact day of the week (80; 18 %) and counting backward from 100 by serial sevens (131; 30 %).
Regarding psychological status, in GDS, the median was four (2-6) points. Three hundred people (68 %) had no problems with mood, but the rest had mild (114; 26 %) or even severe depressive symptoms (24; 6 %). Mostly, seniors resigned from social life (219; 50 %) and feared for their health (235; 54 %).
Mobility and the risk of falls
The average time taken to perform TT was 13.8 ± 8.7 seconds, and the median was 11 (9-15) seconds. Slightly above one-third of patients had an increased risk of falls (153; 35 %), while others (185; 65 %) achieved better results in this test.
Nutritional status
In MNA, the median was 13 (12-14) points. Most participants in our study were well-nourished according to the questionnaire (334; 76 %). Eighty four people (19 %) were at risk of malnutrition and 20 (5 %) were malnourished. The biggest problems that might had been connected with malnutrition were either serious illness or severe psychological stress (87; 20 %) and neuropsychological disorders (125; 28 %).
Frailty syndrome
In CFS, the median was three (2-4). Of all respondents, 294 (67 %) did not classify as patients with frailty syndrome (stages 1-3 in CFS), while the other 144 (33 %) were evaluated as being frail (stages 4-9 in CFS). Almost one in three participants (125; 29 %) was marked as number three, which indicates ‘managing well’, which is the border between a fit and a frail person.
Sleep disorders
In the AIS questionnaire, the median was five (3-8) points. Sleeping problems were reported by 182 patients (42 %) - either mild (116; 27 %) or severe (66; 15 %). The remainder (256; 58 %) slept well. Respondents complained about delayed falling asleep (263; 60 %) and waking during the night (360; 82 %). Detailed normal and incorrect results of all tests used in CGA in different age groups are shown in Table 3.
Table 3. Results of each particular tests used in the comprehensive geriatric assessment in the three age subgroups of the elderly patients.
Values are given as points scored and corresponding percentage in brackets or mean score and standard deviation, ADL: Activities of Daily Living, IADL: Instrumental Activities of Daily Living, MMSE: Mini-Mental State Examination, GDS: Geriatric Depression Scale, TT: Timed Up and Go Test, MNA: Mini Nutritional Assessment Short Form, CFS: Clinical Frailty Scale, AIS: Athens Insomnia Scale.
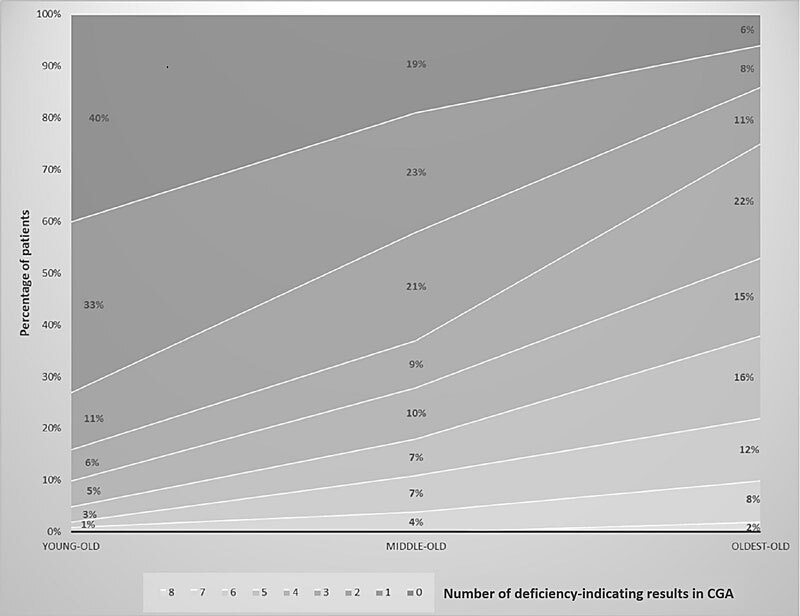
Coexistence of deficiency-indicating results in CGA tests
The number of deficiency-indicating results of tests used in CGA and the proportion of people with coexisting abnormalities in CGA tests increased with age (Figure 2). In the young-old group, 40 % did not present any old-age vulnerabilities, while in the oldest-old group, only 6 % had normal scores in all eight dimensions assessed in CGA (the upper part of the graph marked in the darkest color). The subsequent ranges (from 1 to 8) show the percentage of patients with increasing abnormalities in CGA. The lowest range, showing abnormalities in all eight CGA areas, concerned only 2 % of people in the oldest-old group. The maximum of eight deficits did not occur in either the young-old or middle-old group of patients.
Figure 2. Deficiency-indicating results of eight tests from comprehensive geriatric assessment by age group.
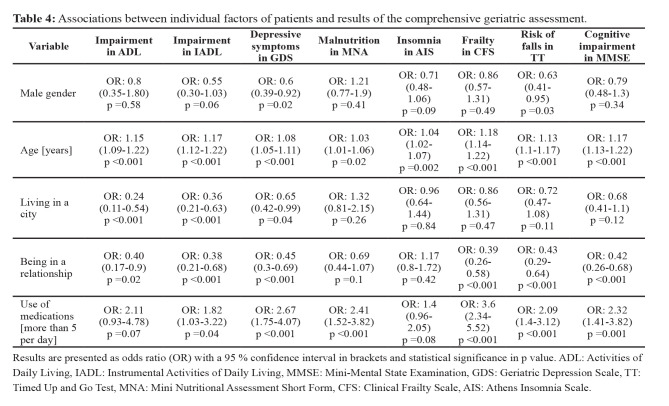
Associations between tests from CGA and individual factors
The associations between patients’ individual factors and CGA tests are shown in Table 4 and Table 5. Male gender was associated with a lower risk of depressive disorders [OR =0.6 (0.39-0.92); p =0.02] and a reduced risk of falls [OR =0.63 (0.41-0.95); p =0.03]. Age correlated with every aspect assessed in CGA and worsened as patients grew older (in all cases p <0.05). There were statistically significant relations between the place of residence and functioning in everyday life and mental state. City-dwellers had a lower risk of functional disabilities in ADL [OR=0.24 (0.11-0.54); p<0.001] and IADL [OR=0.36 (0.21-0.63); p<0.001] and a lower risk of depressive tendencies [OR =0.65 (0.42-0.99); p =0.04]. We found associations between drug intake and six of the assessed aspects of CGA. Taking more than five medicaments per day essentially increased the risk of mood disorders [OR =2.67 (1.75-4.07); p <0.001] but also that of frailty [OR =3.6 (2.34-5.52); p <0.001].
Table 4. Associations between individual factors of patients and results of the comprehensive geriatric assessment.
Results are presented as odds ratio (OR) with a 95 % confidence interval in brackets and statistical significance in p value. ADL: Activities of Daily Living, IADL: Instrumental Activities of Daily Living, MMSE: Mini-Mental State Examination, GDS: Geriatric Depression Scale, TT: Timed Up and Go Test, MNA: Mini Nutritional Assessment Short Form, CFS: Clinical Frailty Scale, AIS: Athens Insomnia Scale.
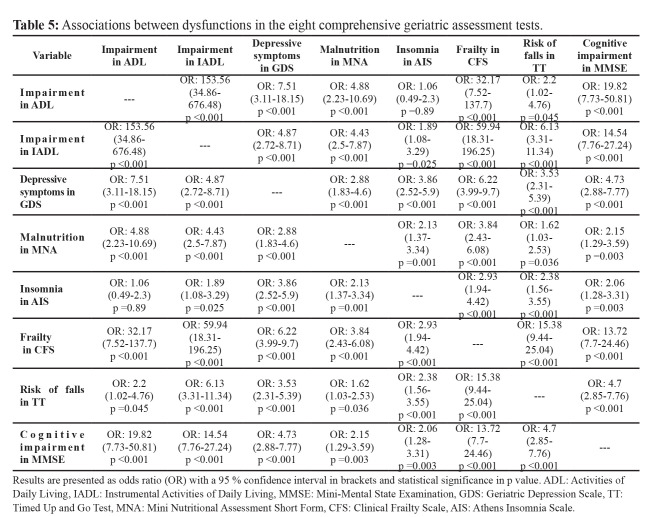
Table 5. Associations between dysfunctions in the eight comprehensive geriatric assessment tests.
Results are presented as odds ratio (OR) with a 95 % confidence interval in brackets and statistical significance in p value. ADL: Activities of Daily Living, IADL: Instrumental Activities of Daily Living, MMSE: Mini-Mental State Examination, GDS: Geriatric Depression Scale, TT: Timed Up and Go Test, MNA: Mini Nutritional Assessment Short Form, CFS: Clinical Frailty Scale, AIS: Athens Insomnia Scale.
Almost all of the tests used in CGA were interconnected (in all cases p <0.05). Such an association was not found only between ADL and AIS results, which indicates that a deficit in one CGA area increased the risk of deficiency in another aspect. The strongest associations were found between ADL and IADL scales [OR =153.56 (34.86-676.48); p <0.001], followed by the CFS and IADL scales [OR =59.94 (18.31-196.25); p <0.001], and CFS and ADL [OR =32.17 (7.52-137.7); p <0.001].
Discussion
Main findings
Our study shows that the majority of the study participants were fully functional according to the results of the ADL and achieved high scores in IADL. Those patients who attended GPs’ surgeries in the Krakow region of Poland were generally functioning well in everyday life. Nonetheless, after a more profound analysis, it turned out that seniors had deficits in various dimensions of CGA. Even when people in the middle-old group had high ADL and IADL scores, half of them had an increased risk of falls and had symptoms of frailty syndrome. Furthermore, as many as 20 % of patients in this age group were at risk of malnutrition or were malnourished. The number of people with geriatric deficits, such as the risk of falls, poor nutritional status, or cognitive impairment, was even higher in the oldest-old age group, although, at first glance, they appeared to be fully functional.
Slightly less than half of the patients had problems with sleeping. One-third of participants had signs of frailty and 32 % symptoms of mild or severe depression. Male gender reduced the chance of depressive disorders and risk of falls. Results of almost all tests in CGA were intercorrelated, and the most robust relationship occurred between ADL and IADL scales.
Comparison with other studies
We revealed that mood, sleep disorders, and frailty are the most common health problems among elderly patients attending GPs in Krakow. A study in the Netherlands (West Friesland) found major and minor depression in 13.7 % and 10.2 %, respectively, of elderly patients who consulted their GPs25. The Faenza Project (Northern Italy) revealed that the prevalence of depression in the elderly population was 25.1 %, with no gender difference26. Among the elderly of the Patras municipality (Greece), 45 % suffered from symptoms of depression, which were more common in women and people living alone or chronically ill27. Another study similarly found that depressive disorders are more common in women28. Jongenelis et al reported that mood disorders were correlated with pain, functional limitations, loneliness, lack of social support, cognitive impairment, and insomnia29. Our study also revealed a high prevalence of depression, diagnosed in 32 % of patients, and it is more common in women, people with insomnia, and those living alone.
The fact that sleep problems are widespread in the elderly was shown by Kamel and Gammack, who estimated their prevalence to be over 50 %30. Another study involving adults aged 65-74 found these issues in 46 % of participants31. The quoted results are very similar to those obtained in the current study.
In a study conducted in GPs’ surgeries in Austria, cognitive impairment was found in 55 % of all participants screened32, which indicates a considerable difference from our study as we revealed fewer (20 %) of these disorders. Our results also differ from Swedish research, which shows that up to 13 % of the elderly had impaired daily activities and were dependent on caregivers33. This percentage is higher than in our study. The presented differences may be attributed to the method of patient selection since we enrolled solely patients who could attend in-person the practices.
No more than partial elaborations, covering selected aspects of geriatric assessment, have been published in Poland, and they did not include people attending GPs’ surgeries. For example, the WOBASZ study34 evaluated only nutrition (MNA questionnaire) in the elderly population. Malnutrition was found in 6 % of men and 7 % of women, which is similar to our study (5 %). Another substantial Polish investigation, “PolSenior”10, was conducted to assess the geriatric population’s health, social, and economic situations. In that study, dementia and loss of independence were more common than in the current. Our study and “PolSenior” indicated depressive disorders and insomnia as important factors in poor functional status.
Strengths and limitations
One of the most important strengths of our study is that it shows a representation of elderly patients who attend GP surgeries, while other studies in Europe were performed in different settings. It is also the first, in Poland, showing the results of CGA in primary care. Another strong point is the use of widely accepted and internationally validated versions of questionnaires. The studied population also corresponded well to the structure of Polish society when it comes to the percentage of people in the three senior subgroups11.
However, some limitations need to be taken into account. The study was performed in only one city and its surroundings which does not allow us to generalize the findings to the entire elderly population in Poland. The study sample was not calculated using statistical methods, but it was determined by subjective judgment and consensus between researchers. Furthermore, we could not exclude sampling bias. Although all general practices were randomly selected, we used consecutive sampling for patient recruitment. We also understand that we have assessed a relatively fit elderly population who could visit their GPs, thus excluding bedridden patients or those with severe disabilities unable to reach the clinics. We used widely accepted versions of questionnaires, and all Polish scales used in the study were derived from a compilation prepared for medical professionals by national geriatrics experts: however, only five (MMSE, GDS, MNA, CFS, AIS) were validated in Poland. Moreover, in our questionnaire, there were no questions about alcohol consumption or illicit drug use. Although these questions are not a routine part of CGA, some authors recommend their inclusion.
Interpretation of the study findings and implications for practice and research
Because aging of society is a growing problem, performing CGA is more important in today’s medicine than in previous years. All physicians, and not only GPs, should be able to perform tests from CGA. Additionally, other staff, such as nurses and paramedics, should be trained in CGA to support doctors in their work.
According to the current study, the most widespread problems in the geriatric population are depressive disorders and insomnia. Both should be diagnosed early due to the possibility of successful treatment, thus improving this group’s quality of life. We believe that during medical consultations of older people for various reasons, GPs should ask about any sleep and mood disorders and administer proper procedures.
Although the study was conducted in one region in Poland, its results may be of international importance. Thirty years ago, other countries in Central and Eastern Europe underwent a transformation of their health services, including primary health care, similar to those in Poland. However, they continue to struggle with poorly developed medical care35. The results of our research can be used not only by Polish doctors but also by neighboring countries to evaluate geriatric patients under their care. In countries where the health care system is provided at a higher level, such as Scandinavia and the United Kingdom, the relevance of our study may be of less significance.
In our study, the results of most of the tests in the youngest subgroup (65-74 years) were within the normal range. In this group, GPs should assess whether performing CGA is reasonable. We can suggest that CGA should be performed only in these seniors if the patient or their caregiver complains about a specific problem. Screening questions or abbreviated tools for geriatric assessment may be helpful in this age group and select the patients most in need of medical attention. On the other hand, people above 85 years old had various medical and social problems; thus, doctors should pay special attention to them and carry out detailed tests in those cases.
CGA, performed in outpatient clinics, creates the possibility of recognizing undiagnosed health problems and optimizing care. It is worth mentioning that CGA results must be interpreted with caution to avoid potential adverse effects like over-diagnosis, labeling, and over-treatment of patients. When a deficit is recognized, it can be treated in various ways - not only pharmaceutically, but also with lifestyle changes.
Conclusions
Patients who attend general practices in Krakow, Poland, manifest only slight deficits in ADL and IADL scales assessing functioning in everyday life. Despite this, in those seemingly healthy seniors, geriatric deficits are revealed after CGA is performed. For this reason, physicians should be watchful, and CGA should be introduced into wider practice. The number of geriatric problems increases with age, so it is more beneficial to perform CGA in older age groups, for example, starting with patients of 75 years and above. Younger patients are expected to have relatively good results in tests assessed in CGA; thus, this kind of assessment is needed when the physician comprehends the relevance of introducing the procedure. CGA reveals that frailty, mood, and sleep disorders are the most common health problems among elderly patients under GPs’ care. Some tests from CGA are more useful in GPs’ surgeries than others, and further research will show which proves to be the best.
Conflict of interest
Tomasz Tomasik has served as a consultant or speaker for Boehringer Ingelheim, Novartis, Shire, Biofarm, and Eli Lilly. The other authors have declared no conflict of interest.
References
- 1.Lee H, Lee E, Jang IY. Frailty and Comprehensive Geriatric Assessment. J Korean Med Sci. 2020;35:e16. doi: 10.3346/jkms.2020.35.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parker SG, McCue P, Phelps K, McCleod A, Arora S, Nockels K, et al. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing. 2018;47:149–155. doi: 10.1093/ageing/afx166. [DOI] [PubMed] [Google Scholar]
- 3.de Vos A, Cramm JM, Van Wijngaarden JDH, Bakker TJEM, Mackenbach JP, Nieboer AP. Understanding implementation of comprehensive geriatric care programs: a multiple perspective approach is preferred. Int J Health Plann Manage. 2017;32:608–636. doi: 10.1002/hpm.2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:CD006211. doi: 10.1002/14651858.CD006211.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Extermann M, Hurria A. Comprehensive geriatric assessment for older patients with cancer. J Clin Oncol. 2007;25:1824–1831. doi: 10.1200/JCO.2007.10.6559. [DOI] [PubMed] [Google Scholar]
- 6.Kruschinski C, Wiese B, Dierks ML, Hummers-Pradier E, Schneider N, Junius-Walker U. A geriatric assessment in general practice: prevalence, location, impact and doctor-patient perceptions of pain. BMC Fam Pract. 2016;17:8. doi: 10.1186/s12875-016-0409-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fedyk-Łukasik M. Całościowa Ocena Geriatryczna w codziennej praktyce geriatrycznej i opiekuńczej. Geriatria i opieka długoterminowa. 2015;1:1–5. [Google Scholar]
- 8.MZ: geriatrów mamy o wiele za mało. MedexpressNewsletter. Available at: https://www.medexpress.pl/mz-geriatrow-mamy-o-wiele-za-malo/73202. date accessed: 14/03/2019.
- 9.Bujnowska-Fedak M, Kumięga P, Sapilak B. Ocena sprawności funkcjonalnej osób starszych w praktyce lekarza rodzinnego w oparciu o wybrane skale testowe. Family Medicine & Primary Care Review. 2013;2:76–79. [Google Scholar]
- 10.Mossakowska M, Więcek A, Błędowski P. Aspekty medyczne, psychologiczne, socjologiczne i ekonomiczne starzenia się ludzi w Polsce. 1st Edition. Termedia Wydawnictwa Medyczne, Poznan, 2012. Available at: http://gerontologia.org.pl/wp-content/uploads/pliki/ol/polsenior.pdf. date accessed: 14.11.2019.
- 11.Główny Urząd Statystyczny. Sytuacja demograficzna osób starszych i konsekwencje starzenia się ludności Polski w świetle prognozy na lata 2014-2050. Available at: https://stat.gov.pl/obszary-tematyczne/ludnosc/ludnosc/sytuacja-demograficzna-osob-starszych-i-konsekwencje-starzenia-sie-ludnosci-polski-wswietle-prognozy-na-lata-2014-2050,18,1.html. date accessed: 14.03.2019.
- 12.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: The Index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 13.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR. “Mini-mental status”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 15.Parnowski T, Gabryelewicz T, Matuszewska E, Jarkiewicz J. Rozpowszechnienie zespołów otępiennych w populacji wielkomiejskiej--badanie pilotażowe. Psychiatr Pol. 1993;27:515–520. [PubMed] [Google Scholar]
- 16.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. Clin Gerontologist. 1986;5:165–173. [Google Scholar]
- 17.Albiński R, Kleszczewska-Albińska A, Bedyńska S. [Geriatric Depression Scale (GDS). Validity and reliability of different versions of the scale--review] Psychiatr Pol. 2011;45:555–562. [PubMed] [Google Scholar]
- 18.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 19.Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF) J Gerontol A Biol Sci Med Sci. 2001;56:M366–M372. doi: 10.1093/gerona/56.6.m366. [DOI] [PubMed] [Google Scholar]
- 20.Kostka J, Borowiak E, Kostka T. Validation of the modified mini nutritional assessment short-forms in different populations of older people in Poland. J Nutr Health Aging. 2014;18:366–371. doi: 10.1007/s12603-013-0393-0. [DOI] [PubMed] [Google Scholar]
- 21.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oviedo-Briones M, Laso ÁR, Carnicero JA, Cesari M, Grodzicki T, Gryglewska B, et al. A Comparison of Frailty Assessment Instruments in Different Clinical and Social Care Settings: The Frailtools Project. J Am Med Dir Assoc. 2021;22:607. doi: 10.1016/j.jamda.2020.09.024. [DOI] [PubMed] [Google Scholar]
- 23.Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48:555–560. doi: 10.1016/s0022-3999(00)00095-7. [DOI] [PubMed] [Google Scholar]
- 24.Fornal-Pawłowska M, Wołyńczyk-Gmaj D, Szelenberger W. [Validation of the Polish version of the Athens Insomnia Scale] Psychiatr Pol. 2011;45:211–221. [PubMed] [Google Scholar]
- 25.Licht-Strunk E, van der Kooij KG, van Schaik DJ, van Marwijk HW, van Hout HP, de Haan M, et al. Prevalence of depression in older patients consulting their general practitioner in The Netherlands. Int J Geriatr Psychiatry. 2005;20:1013–1019. doi: 10.1002/gps.1391. [DOI] [PubMed] [Google Scholar]
- 26.Forlani C, Morri M, Ferrari B, Dalmonte E, Menchetti M, De Ronchi D, et al. Prevalence and gender differences in late-life depression: a population-based study. Am J Geriatr Psychiatry. 2014;22:370–380. doi: 10.1016/j.jagp.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 27.Argyropoulos K, Gourzis P, Jelastopulu E. [Prevalence of depression among the elderly] Psychiatriki. 2012;23:39–45. [PubMed] [Google Scholar]
- 28.Acciai F, Hardy M. Depression in later life: A closer look at the gender gap. Soc Sci Res. 2017;68:163–175. doi: 10.1016/j.ssresearch.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Jongenelis K, Pot AM, Eisses AMH, Beekman ATF, Kluiter H, Ribbe MW. Prevalence and risk indicators of depression in elderly nursing home patients: the AGED study. J Affect Disord. 2004;83:135–142. doi: 10.1016/j.jad.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Kamel NS, Gammack JK. Insomnia in the elderly: cause, approach, and treatment. Am J Med. 2006;119:463–469. doi: 10.1016/j.amjmed.2005.10.051. [DOI] [PubMed] [Google Scholar]
- 31.National Sleep Foundation. Sleep in America Poll. Available at: https://www.sleepfoundation.org/wp-content/uploads/2018/10/2003SleepPollExecSumm.pdf. date accessed: 16/04/2020.
- 32.Mann E, Koller M, Mann C, van der Cammen T, Steurer J. Comprehensive Geriatric Assessment (CGA) in general practice: results from a pilot study in Vorarlberg, Austria. BMC Geriatr. 2004;4:4. doi: 10.1186/1471-2318-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sonn U, Asberg KH. Assessment of activities of daily living in the elderly. A study of a population of 76-year-olds in Gothenburg, Sweden. Scand J Rehabil Med. 1991;23:193–202. [PubMed] [Google Scholar]
- 34.Waśkiewicz A, Sygnowska E, Broda G. Ocena stanu zdrowia i odżywienia osób w wieku powyżej 75 lat w populacji polskiej. Badanie WOBASZ-Senior. Bromat Chem Toksykol. 2012; 3: 614-618. Available at: https://www.ptfarm.pl/pub/File/Bromatologia/2012/3/614-618.pdf. date accessed: 20.04.20.
- 35.Romaniuk P, Semigina T. Ukrainian health care system and its chances for successful transition from Soviet legacies. Global Health. 2018;14:116. doi: 10.1186/s12992-018-0439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]