Abstract
Mental health problems contribute significantly to the global burden of disease. Driven in part by family stressors and insufficient sleep, mental health disproportionately affects low SES urban adolescents. In the United States, American Indian/Alaska Native (AI/AN) youth exhibit excessively high rates of mental health problems. Family functioning is strongly associated with adolescent mental health, and sleep problems may serve as a pathway between family functioning and mental health. Using mixed methods we examine the associations among family functioning, subjective- and actigraphy-measured sleep, mental health (depressive and anxiety symptoms), and cultural identity in a sample of urban AI/AN youth. All participants (N =142) completed surveys; a random subsample (n =26) completed qualitative interviews to assess family and cultural dynamics related to sleep, which informed hypothesized direct and indirect effects that were tested using survey data. Narratives identified mechanisms of family cohesion (e.g., daily interactions that build perceived family togetherness and family-centered traditional activities) and the role that family cohesion plays in sleep (e.g., ensuring stability of sleep environments). Path analysis showed direct effects of improved family functioning on fewer depressive and anxiety symptoms, and indirect effects through lower self-reported sleep disturbance (but not through greater actigraphy-measured sleep duration or efficiency). Cultural identity did not moderate effects in quantitative tests. Our findings illustrate the complex associations among family functioning, sleep, and mental health in AI/AN youth. Family-based interventions to improve adolescent mental health should address modifiable intervention targets such as sleep, and address sources of both risk and resilience relevant to urban AI/AN families, including extended family and cultural practices.
Keywords: mental health, family, sleep, Native American, mixed methods, urban, adolescents, actigraphy
INTRODUCTION
Mental health problems contribute significantly to the global burden of disease,1 with half of all mental health conditions beginning in adolescence.2 Insufficient sleep is core driver of adolescent mental health, often underrecognized as a public health epidemic, but with serious health and social consequences.3 Evidence suggests that, worldwide, adolescent urban dwellers are at an increased risk for sleep and mental health problems, accentuated by poverty, low social capital, and other characteristics of urban environments that are experienced in the home environment and family context.4,5 To address such problems, there have been calls for family-focused public health efforts, acknowledging the role of family context for many health outcomes.6 There may be important lessons to learn about critical opportunities to intervene to effect change in mental health outcomes among vulnerable urban populations.
In the United States, urban American Indian/Alaska Native (AI/AN) youth experience disproportionately high rates of mental health symptoms. For example, compared to other racial/ethnic minorities and non-Hispanic White adolescents, AI/AN adolescents report more depressive symptoms and generalized anxiety.7 Furthermore, the suicide rate among AI/AN youth and young adults is 1.5 times higher than the national average.8 These disparities are related to European contact, forced relocation, and cultural genocide, leading to widespread traumatic experiences and unresolved grief across generations.9 Moreover, approximately 70% of all AI/ANs reside in urban locations far from reservations or tribal lands, and face additional psychosocial and environmental stressors, such as lack of social cohesion and exposure to poverty, that may put them at further risk for mental health problems.10
In the current paper, we focus on two distinct but related dynamics that are associated with adolescent mental health. First, family functioning – that is, family interactions and relationships, including conflict, cohesion, structure, and communication;11 adolescents in well-functioning families report better mental health outcomes, including less depression and anxiety.12 Second, sleep problems often occur during adolescence due to irregular sleep-wake schedules,13 and are a significant contributor to adolescent mental health.14,15 Moreover, poorer family functioning16,17 and lower quality parent-adolescent relationships18 are also associated with sleep problems. Despite high rates of mental health problems among AI/AN youth, no studies to date have examined sleep as a potential mediator of the impact of family functioning on mental health.
In general, there are limited data on how challenges related to cultural disruption influence mental health among urban AI/AN families and youth.19 Urban AI/AN people emphasize that it is often very difficult to be culturally connected given the dispersion of the population and the limited resources.20 Culture can be protective for sleep health;21 however, no studies have assessed whether AI/AN culture may play a role in the relationship between family functioning and sleep, and ultimately on mental health. The current study adds to the literature by examining family functioning and sleep in relation to mental health among urban-dwelling AI/AN youth.
The Role of Biopsychosocial and Contextual Factors
One theoretical framework that is key to understanding the complex interplay between family functioning, sleep, cultural identity, and mental health and draws from a developmental psychopathology framework: the biopsychosocial and contextual paradigm.22,23 In this paradigm, domains of overall health, such as mental health and sleep, are intertwined (through reciprocal relationships) with a range of biological, psychological, social, and contextual factors.22,24 In other words, health outcomes are products of biological characteristics (e.g., circadian rhythm, physical comorbidity, genetic vulnerability), psychological predispositions (e.g., impulsivity, irritability), social factors (e.g., family, peers), and other contextual features (e.g., school, community, culture). In this paradigm health outcomes are also understood to interact with these multi-level factors. Finally, the centrality of each factor or relationship may vary within and across individuals over time.24
The biological dimension of this model provides a rationale for studying the juncture of sleep and mental health in adolescence, especially given the physical growth and neurodevelopmental changes, such as synaptic pruning and developmentally specific changes in circadian rhythms, that occur during this developmental period. 25 Owing in part to the intersection of these neurodevelopmental changes with social stressors (e.g., academic and social pressures and early school start times), adolescents are a high-risk group for sleep problems, including insufficient sleep duration and poor quality sleep.17 In turn, sleep problems are prospectively linked with diverse mental and behavioral health outcomes, including depression, anxiety, and suicide risk.26-28 Yet, very little is known about the association between sleep and mental health in minority groups, such as urban AI/AN youth.
Social factors such as family functioning have been shown to affect adolescent mental health. High family functioning is associated with less depressive symptomatology,29 and adolescents in well-functioning families tend to report better mental health outcomes.12 Several studies have shown, for example, that low family functioning (e.g., increasing stress in the overall family climate) is related to poorer mental health,30 whereas high family functioning (e.g., a safe environment for expressing and understanding emotions) is related to better mental health.31
Family functioning has also been documented to have a significant, though not fully understood role in adolescent sleep.32 For example, family conflict in childhood is longitudinally associated with insomnia in late adolescence,33 and marital conflict predicts childhood sleep disruptions.34 Also, poor family functioning16 and lower quality parent-adolescent relationships are associated with insufficient sleep duration.18 The mechanisms underlying this association include parent-child attachment style,35 parental involvement in setting household rules and sleep routines,36 and family environment attributes, such as safety, which are conducive to a “cessation of vigilance,”37 which supports sleep onset and maintenance. However, gaps remain in understanding these processes, especially in minority populations such as urban Native American families.
Sleep may be an important modifiable pathway between family functioning and mental health.38 One study found that in mostly White adolescents, sleep quality and duration mediated effects of poor family functioning on adolescent mental health. Specifically, when teens reported poor family functioning, this was associated with worse sleep quality and duration, which was then linked to corresponding changes in anxiety and depressive symptoms.39
Finally, the contextual component of the biopsychosocial model underscores the importance of community and cultural factors in family functioning, sleep behaviors, and mental health. Given the history of colonization and collective trauma among AI/AN people and the resulting extreme social and cultural disruption to AI/AN societies and families,40 it is crucial to consider how cultural context, including cultural identity, may affect associations between family functioning, sleep and mental health. For example, among urban AI/AN communities, family functioning may play a key role in buffering the effects of historical trauma.41 Likewise, resilience is often embedded in AI/AN family functioning42 in a dynamic process that includes individual and collective adaptation to overcome stress through nurturing beliefs and values that promote wellbeing.43 For instance, prior work has shown that engagement in traditional practices may decrease anxiety and depression.44 However, the mechanisms linking contextual factors with health outcomes are currently poorly understood, and within-cultural studies may help elucidate such processes. Thus, the current study examines how cultural identity may affect the association between family functioning and sleep, and ultimately mental health.
Current Study
This study addresses several existing knowledge gaps and methodological challenges in the study of sleep, family dynamics, culture, and health in the urban AI/AN population. First, it expands the metrics typically used in studies of family functioning and mental health, incorporating family conflict and cohesion to measure family functioning, depression and anxiety to measure mental health, and both subjective and objective measures of sleep. Prior work on family functioning among AI/AN adolescents has mainly addressed the association between family structure (i.e., parental marital status) and substance use.45-47 For example, compared to adolescents in two-parent AI/AN homes, those living in single-parent AI/AN households were more likely to initiate alcohol, tobacco, and marijuana at earlier ages regardless of parenting practices.45 Less is known, however, about the effects of family dynamics (such as perceived conflict and cohesion) on other behavioral health outcomes among AI/AN youth, such as depression and anxiety.
Second, this study uses mixed-method analysis (complementary and expansion mixed methods)48 to examine the complex associations among family functioning, sleep, and mental health in a sample of urban AI/AN youth. Existing work on family functioning, sleep, and behavioral health among urban AI/AN youth has drawn primarily on quantitative data and analyses, which sometimes struggle to explain the complex mechanisms involved in deeply contextual and interdependent relationships.45,46 Qualitative methods can often shed new light on potential causal associations due to the depth and detail contained in participant narratives.49 In combination, quantitative and qualitative data inform each other to enhance understanding of mechanisms that link contextual with individual-level factors, which can assist with practical intervention development.49 Most prior mixed methods work on family functioning has taken a simple sequential approach, where qualitative analysis preceded quantitative analysis without explicit analytic integration.50 This study’s integrative approach is advantageous because constructs such as family functioning and cultural identity can be explored both through closed-ended survey items and narrative comments; this allows for comparison of results across different types of data, as well as identification of convergence or divergence between survey data and themes from interviews.
Our mixed methods approach leveraged qualitative analysis to generate hypotheses for quantitative testing. Based on thematic content from interviews, we developed several mediation hypotheses: 1) greater family cohesion would be associated with lower depressive or anxiety symptoms, whereas greater family conflict would be associated with greater depressive or anxiety symptoms; and 2) these associations would be mediated by self-reported sleep disturbance, and objectively-measured sleep duration and sleep efficiency. Finally, based on interview findings regarding cultural practices, we used moderated mediation to test whether cultural identity moderated any observed associations between family functioning and sleep. We hypothesized that stronger AI/AN cultural identity would buffer (lessen) the association between poor family functioning and negative sleep outcomes.
METHODS
Overview
We analyzed data from 142 urban AI/AN youth using an integrative mixed methods approach48 to examine pathways among family functioning, sleep, and behavioral health within a cultural context. In step one, we analyzed in-depth interviews and compared themes with our descriptive survey data on similar topics; this approach is known as complementary mixed methods analysis.48 In step two, we used narrative findings from qualitive interviews to formulate a set of hypothesized direct and indirect effects; this technique is known as expansion mixed methods analysis.48
In step three, based on our hypotheses, we examined the direct effects of family functioning (i.e., family cohesion or conflict) on adolescents’ depressive or anxiety symptoms, as well as the indirect effects (mediation) through subjective and objective (via actigraphy) measures of sleep. Based on mixed methods analysis, we hypothesized that greater AI/AN cultural identity might mitigate the negative impact of poor family functioning on sleep (that, in turn, is associated with poor mental health outcomes). Thus, we also explored whether AI/AN cultural identity moderated the indirect path from family functioning to mental health outcomes through sleep.
Sample and Recruitment
We analyzed data from Wave 1 of the Native American Youth Sleep Health and Wellness (NAYSHAW) study; a longitudinal study involving both quantitative (e.g., survey, blood sample, actigraphy) and qualitative (e.g., in-depth interview) data.51 The study benefitted from a community-based participatory approach to engage AI/AN communities, including input from Native elders and community members regarding the recruitment process, sampling approach, survey measures, interview questions, as well as biological (e.g., blood draws) and anthropometric (e.g., height and weight) assessments. We also worked with our community partner, Sacred Path Indigenous Wellness Center (SPIWC), to identify AI/AN recruiters who had worked on our previous projects and had established relationships with communities across California.
AI/AN youth were eligible to participate if they were 12-16 years old, self-identified (or were identified by their parents) as AI/AN (or of AI/AN ancestry) and could read and converse in English. Participants were excluded if a parent reported serious physical or behavioral health conditions such as heart disease, kidney disease, diabetes, sleep disorder, or severe cognitive impairment. We also restricted participation to one adolescent per family due to the nonindependence of sleep and family functioning data within families.
Our quantitative sample includes 142 adolescents living in urban communities in northern, central, and southern California who were recruited via advertisements distributed by community partners. The qualitative sample was a randomly selected subset of 26 interviewees from the quantitative sample.
All data were collected during home visits, and all procedures were approved by RAND Corporation’s internal review board and by the communities that participated in the study. Because all study participants were under age 18, parental consent and adolescent assent were obtained. Participants received $25 for completing the survey and $35 for participating in the qualitative interview.
Qualitative Data Collection
All interviews were conducted during the school year (September 2018 to June 2019). The interview protocol focused on the following topics: (1) sleep environment, including room(s) type and size, sleep arrangements, and sources of lighting and noise; (2) sleep behavior, such as preparing for sleep and daytime napping; (3) quality of sleep; (4) sleep habits and beliefs; and (5) cultural dimensions of sleep. Although we did not directly elicit content related to family functioning, participants described family dynamics frequently during interviews. Supplemental Material 1 provides the full interview protocol.
Quantitative Data Collection
Demographic.
Adolescents reported their age, sex, race/ethnicity, grade, parental education, and parents’ marital status.
Family functioning.
Family functioning was assessed using subscales for family cohesion (seven items) and conflict (six items) from the Brief Family Relationship Scale (BFRS), which has been validated in a sample of Alaska Native youth.52 Prior research has found these scales to be reliable and to show adequate convergent and discriminant validity.53 Respondents rated cohesion on a scale from 0 (not at all) to 2 (a lot; e.g., “in our family there is a feeling of togetherness,” “my family members really support each other”). Conflict was reverse coded and included questions such as “in our family we lose our tempers a lot” and “my family members sometimes are violent.” Higher scores are indicative of better family functioning on each dimension, i.e., more cohesion and less conflict.
Subjective and objective measures of sleep disturbance.
Sleep disturbance was assessed through a validated subscale of the School Sleep Habits Survey of Adolescents.54 This subscale elicits self-reported frequency of indicators of erratic sleep/wake behaviors over the previous 2 weeks (e.g., “stayed up past 3:00 a.m. or later,” “needed more than one reminder to get up in the morning,” “had an extremely hard time falling asleep”). Response options are 0 (never), 1 (once), 2 (twice), 3 (several times), to 4 (every day/night). Higher scores indicate greater sleep disturbance.
We supplemented the self-reported sleep outcomes with actigraphy data, which provides behavioral assessment of habitual sleep patterns and duration.55 Actigraphs are watch-like bracelets, worn on the non-dominant wrist, which may be worn 24 hours per day, including while bathing, swimming, or showering. Actigraphy data were collected at least 7 consecutive days using Actiwatch-2 (Phillips/Respironics®) in order to include sleep parameters for both weekday and weekend nights. A minimum number of 4 nights of actigraphy were used to ensure the reliability of actigraphy sleep outcomes (average 7.35 nights, SD = 1.58, range = 4 - 16). Validated scoring algorithms were used to derive mean levels of sleep duration and sleep efficiency (time spent asleep/ time in bed x 100; expressed as percentage) across 7-days of actigraphy;56 both measures have previously been associated with adolescent mental health outcomes.57
Mental health symptoms.
We used the Patient Health Questionnaire 2-item scale (PHQ2) to measure depressive symptoms. The PHQ2 has been validated in adolescents as a screener for major depression.58 We used the Generalized Anxiety Disorder 7-item scale (GAD7) to measure anxiety symptoms, which has been validated in adolescents for detecting clinically-significant anxiety symptoms.59
Cultural identity.
We used the Multigroup Ethnic Identity Measure (MEIM) to assess AI/AN cultural identity.60 The scale consists of 12 questions rated from 1 (strongly disagree) to 5 (strongly agree). We modified MEIM items to focus on AI/AN heritage (e.g., “I have clear sense of my AI/AN identity and what it means to me”).61
Data Analysis
Stage 1: Qualitative data analysis and complementary survey analysis.
The first stage of analysis involved analyzing family functioning themes from our qualitative data and comparing these findings with similar questions from our survey data. First, we uploaded transcripts to Dedoose, a team-based collaborative software platform for qualitative data management, analysis and interpretation.62 Our qualitative analysis built on a previous study with the same data set.51 The previous study examined all aspects of sleep among AI/AN adolescents, of which family dynamics were a minor component, e.g., parental involvement in sleep behaviors. In contrast, this study focuses primarily on family cohesion and other aspects of family functioning; the family functioning frame drove us to develop 14 new codes specific to this study. Several codes used for the previous study (relating to the sleep environment and sociocultural perspectives) also applied to this study, so we explored them in conjunction with newly developed codes focused on family functioning. We used both inductive and deductive approaches to develop the new codes.63 Two qualitative researchers from the team (AIP and RAB) coded content independently and engaged in several rounds of discussion and reconciliation of differences in coded output. Input from the larger research team helped guide the coding process and rules. The codebook (see Supplemental Material 2) consisted of two main sections, family cohesion and family conflict. As our last step, we compared thematic content with descriptive survey data on similar topics. This allowed us to use survey data to report on the frequency and prevalence of phenomena, and interview data to understand the processes driving and connecting these phenomena.
Stage 2: Mixed methods expansion.
We used results from the Stage 1 qualitative analysis and the extant literature to develop mediation and moderated mediation models for our survey data, using the expansion mixed methods approach - i.e., using themes from interview data to serve as a guide for follow up quantitative investigations. We examined family cohesion and family conflict codes and identified instances that mentioned connections with sleep quality, sleep environment, or sleep behavior. Next, the team examined the explicitly stated or implied role of cultural aspects related to family functioning and/ or sleep, which resulted in us identifying a moderated mediation model for cultural identity in the relationship between family functioning and sleep.
Stage 3: Quantitative data analysis.
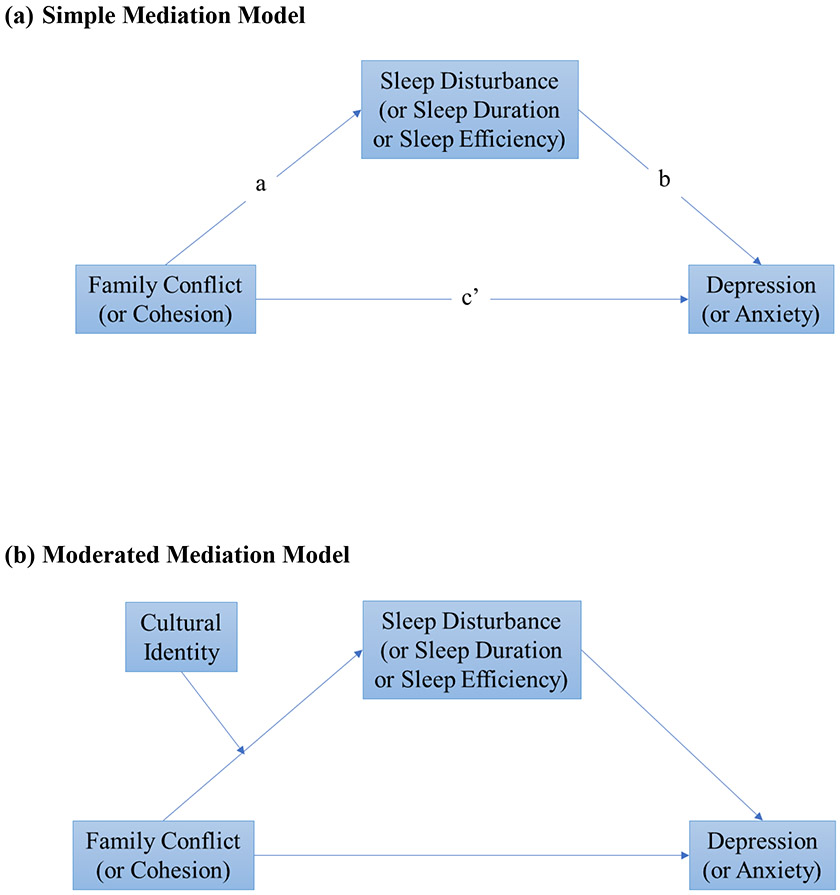
We first conducted descriptive quantitative data analysis using Stata 16.64 We calculated means and standard deviations for continuous variables, as well as counts and percentages for categorical variables. We then conducted mediation and moderation analyses using Mplus 8.65 All models controlled for sex, age, and family structure (i.e., whether or not the adolescent lived in a single parent household), as these control variables are related to both sleep and mental health.66 The data analysis was performed using complete data, and no imputation was performed, given the small amount of missing data. Note that Tables 1 and 2 present the number of observations for each variable. We tested a simple mediation path model (see Figure 1a), examining whether the indirect effect (a*b) of family cohesion or conflict on depression or anxiety was statistically significant. We also tested a moderated mediation model, examining whether AI/AN cultural identity moderated the indirect effects of family conflict/cohesion on depression/anxiety via subjective or objective measures of sleep (see Figure 1b). We provided two sample scripts for the mediation model and moderated mediation model (see Supplemental Material 3). We used a bootstrapping procedure with 10,000 replications to test the statistical significance of the indirect effect as well as the moderated mediation effect. Bootstrap 95% confidence intervals are reported,67 and we used a significance level of 0.05. Model fit for moderated mediation models was evaluated using the combination of the comparative fit index (CFI), Tucker–Lewis index (TLI), the root-mean-square error of approximation (RMSEA), and the standardized root-mean-square residual (SRMR), based on guidelines suggested in the literature: CFI and TLI greater than 0.95 for acceptable fit;68 RMSEA ≤ 0.08 for adequate fit and ≤ .05 for close fit;69 SRMR ≤ 0.08 for acceptable fit.68 Both unstandardized and standardized coefficients (effect sizes) are reported. Standardized coefficients (i.e., standardized with respect to both dependent variable y and independent variable x) indicate the change in y standard deviation units when x changes one standard deviation, and we interpreted them following convention such that 0.20, 0.50, 0.80 are considered small, medium, and large effects, respectively.70
Table 1.
Qualitative and Quantitative Sample Demographics
| Qualitative Sample (N=26) |
Quantitative Sample (N=142) |
|
|---|---|---|
| Age | N (%) | N (%) |
| 12 | 1 (4%) | 23 (16%) |
| 13 | 4 (16%) | 33 (23%) |
| 14 | 11 (42%) | 32 (23%) |
| 15 | 6 (23%) | 25 (18%) |
| 16 | 4 (15%) | 29 (20%) |
| Sex | ||
| Male | 14 (54%) | 58 (41%) |
| Female | 12 (46%) | 84 (59%) |
| Race | ||
| American Indian/Alaska Native | 24 (92%) | 128 (90%) |
| Other | 2 (8%) | 14 (10%) |
| Single Parent Household * | ||
| Yes | 9 (35%) | 66 (46%) |
| No | 17 (65%) | 75 (53%) |
| Missing | 0 (0%) | 1 (1%) |
| Mother Education | ||
| College grad | 7 (27%) | 38 (27%) |
| Some college | 4 (15%) | 30 (21%) |
| High school grad | 6 (24%) | 40 (28%) |
| Didn't finish high school | 5 (19%) | 18 (13%) |
| Don't know | 4 (15%) | 15 (11%) |
| Father Education | ||
| College grad | 2 (7%) | 13 (9%) |
| Some college | 3 (12%) | 17 (12%) |
| High school grad | 8 (31%) | 42 (30%) |
| Didn't finish high school | 9 (35%) | 31 (22%) |
| Don't know | 4 (15%) | 38 (27%) |
Note. One participant missing data on both mother and father education.
Single parent household is defined by parental marital status (Yes = single or never married/ widowed/ separated/ divorced; No = married/cohabitating).
Table 2.
Descriptive statistics of study variables.
| Variable | n | Mean | SD | Range |
|---|---|---|---|---|
| Family cohesion | 142 | 1.63 | 0.33 | 0.43-2 |
| Family conflict | 142 | 0.52 | 0.36 | 0-1.83 |
| Sleep disturbance | 142 | 15.58 | 8.89 | 0-43 |
| Sleep duration (actigraphy; min) | 137 | 425.47 | 54.15 | 275.46-544.64 |
| Sleep efficiency (actigraphy; %) | 137 | 81.09 | 6.87 | 55.49-92.60 |
| Depressive symptoms (PHQ2) | 140 | 1.07 | 1.44 | 0-6 |
| Anxiety symptoms (GAD7) | 141 | 4.73 | 4.83 | 0-20 |
| Cultural identity (MEIM) | 142 | 3.48 | 0.80 | 1.17-5 |
Note. PHQ2 = Patient Health Questionnaire 2-item scale; GAD7 = Generalized Anxiety Disorder 7-item scale; MEIM = Multigroup Ethnic Identity Measure.
Figure 1. Conceptual Diagrams for Mediation and for Moderated Mediation.
(a) This conceptual diagram shows the simple mediation models where we tested whether family functioning (family conflict or cohesion, tested in separate models) had indirect effects on mental health outcomes (depression or anxiety) through sleep (sleep disturbance, sleep duration, or sleep efficiency). The indirect effect is estimated as a*b (the product of paths a and b.
(b) This conceptual diagram shows the moderated mediation models where we tested whether AI/AN cultural identity moderated the indirect effects of family conflict/cohesion on depression/anxiety via subjective or objective measures of sleep. The moderated mediation effect is tested as the product term of the moderating effects and the path between mediator and outcome.
RESULTS
Demographic Characteristics and Other Descriptive Information
Table 1 contains participant demographic characteristics for both qualitative and quantitative samples, showing that the two samples were comparable, except for sex: 54% of interviewees were male in the full sample versus 41% in the qualitative sample. Overall, youth were aged 12-16 (mean = 14.03 years, SD = 1.37 years). All parents identified their participating adolescent child as having AI/AN heritage, and 92% of youth identified as AI/AN, which is consistent with other work in this area.61 Although participants represented roughly 20 different tribes, we do not provide details on tribal affiliation in order to protect confidentiality. Roughly one third said their mother had graduated from college, and 41% reported that their fathers did not finish high school.
We present descriptive information on outcomes variables in Table 2. Scale scores in the full sample (n=142) were comparable to the qualitative subsample (n=26). For example, in the full quantitative sample, average family cohesion was 1.63 (SD=0.33), compared with 1.56 (SD=0.36) in the qualitative subsample. Similarly, the mean for family conflict was 0.52 (SD=0.36) in the full sample and 0.58 (SD=0.35) in the subsample. Actigraphy outcomes showed suboptimal sleep in this sample overall, with an average sleep duration around 7 hours and average sleep efficiency around 81%.
Stage 1: Qualitative Data Analysis and Complementary Survey Analysis
We report two main thematic categories, each with several sub-codes: 1) family cohesion, including daily family interactions, discussing and engaging in traditional activities with the family, and the role of extended family, and 2) family conflict, including disagreements with family members and divorce. Below we describe these themes and illustrate them with supportive quotes. We also indicate how descriptions of the thematic analysis compared with relevant descriptive survey results.
Family Cohesion
Daily family interactions
Sixteen teens (62%) described routine family interactions - such as watching TV or playing computer games with siblings, looking after younger family members, driving/walking to and from school, eating meals with the family, and completing household chores together – as contributing to a sense of togetherness. The following description from a sixteen-year-old AI/AN youth illustrates how family routines create a sense of family warmth: “When my grandma’s here, I like to chill with her. I like to talk to her. I’ll play games, and she’ll be like, ‘Oh, how are you doing in your game?’ I’ll be like, ‘I’m good.’ She’ll be like, ‘Are you winning?’ I’ll be like, ‘Yeah’.” This theme aligns with survey data from two items on the family cohesion scale: 43% of survey respondents said they spent a lot of time doing things together with their family, and 65% said that their family has “a lot” of feeling of togetherness.
Discussing AI/AN heritage and activities with family
Thirteen youth (50%) mentioned family discussions about traditional activities, shared AI/AN beliefs, and AI/AN heritage. Participants indicated that discussions occurred with parents, aunts, uncles and other teens that focused on the meaning of dream catchers, sage burning, historical trauma, and family efforts to enroll in tribes. The following quote helps illustrate this theme: “I try to know some things about my heritage. I would ask my mom on a daily basis, sometimes, if—like anything about my heritage. Like, “Oh, where did my heritage come from?” I don’t really know that much about my heritage. I would love to know more.” (M14)
Eleven youth (42%) described engaging in traditional activities with family members, including powwows, sweat lodges, beading and drumming workshops, events on reservations, and prayers. A fifteen-year-old male had this to say about his experience with powwows: “I’ve been to a couple of pow-wows. They’re pretty cool. I’ve been to some of those little cultural things that they have like where everyone just hangs out and then like the girls, they dance and then like all the guys are like drumming, they sing and that. … I just go with my dad.” (M15)
These themes correspond with the MEIM cultural identity scale. On the MEIM, 41% of youth agreed or strongly agreed that they spent time trying to find out about their AI/AN identity, and 40% agreed or strongly agreed that they often talked to other people about their identity. In addition, 42% of survey respondents endorsed participating in cultural practices of their own AI/AN tribal group.
Role of extended family
Ten youth (38%) made statements about the role of extended family members (grandparents, aunts, uncles, and cousins) in their family life. In particular they spoke about cohabiting (either on a temporary or permanent basis) with other relatives, and how this affected their sleep. Youth mentioned grandparents, cousins, and nephews living with the family, at times affecting sleep quality, as this fourteen-year-old female explained: “My nephew used to live with us and he would cry a lot because he was a baby. When he started teething, that’s when I would mainly stay awake.” Another participant said “When my cousins come over, I don’t get no sleep. They’re usually kicking me off the bed or something.” (F14) Others, however, felt comforted by the presence of family: “I had my grandma staying with us, so she was in the same room with me. So I felt like really happy in a way because I used to live with her when I was younger, so it felt like more complete in a way.” (F14)
We had no survey data for complementary analysis of this theme.
Family Conflict
Disagreements with family members
Ten youth (38%) mentioned mild family disagreements (especially with siblings), although there was little reported conflict with extended family (n=2). Eight of these 10 youth described mild disagreements with immediate family as interfering with sleep or privacy. For example:
“She [sister] knows that on like a school day I want to get my sleep, because we don’t really have that much time. We have to get up early. So she knows that if she annoys me, somebody will walk in here and tell her to stop, because we have to go to bed very early and get up very early and get ready for school so we can get there on time.” (F12)
“I remember I got in a fight with my mom, and I couldn’t sleep the night, not until like 2:00, I think, because I couldn’t sleep, and I was just really sad, angry.” (M16)
Divorce
Six teens (23%) described parental divorce and consequences for sleep, such as having secondary sleeping arrangements due to shared parental custody, foster care, or sleeping with relatives. This statement from a sixteen-year-old male is a typical example: “We moved a lot, because like money problems and stuff. There were times where I would get sent to like a family member’s house because my mom had to work and my dad left. … There were always random periods where like my dad didn’t want to—he didn’t want to talk to me. He didn’t reach out, because he was just too busy, and I understand.” (M16)
Among those who had to share their sleeping environment due to these arrangements, two expressed some negative feelings, including loud noises and discomfort. For example: "Well, [my little brother] is just like dirty, leaves everything around. And sometimes he shakes in the bed and keeps me awake at night sometimes." (M14)
Thematic results on family conflict are consistent with survey responses to items on the family conflict scale as very few (5%) respondents said that their family argues a lot, and 18% said they did not argue at all. Similarly, only 4% said that in their family they are mad at each other a lot, and 54% said the family is not mad at each other at all.
Stage 2. Mixed Methods Expansion Overview
The next stage of our research involved translating our thematic findings and associated survey data into specific hypothesized models that could be tested statistically. This stage also involved consulting the academic literature for corroboration. Based on these processes, we developed the following simple mediation and moderated mediation models, some informed by qualitative findings, whereas others were informed by extant theory, as described below.
Mediation Model Hypotheses
Our thematic content for family cohesion (e.g., being comforted by the presence of family members), led us to hypothesize that greater family cohesion would be associated with lower depressive or anxiety symptoms. Similarly, considering narrative findings for family conflict (e.g., expressions of sadness and anger following family argument), we hypothesized that greater family conflict would be associated with higher depressive or anxiety symptoms. Based on the literature linking family dynamics with sleep, we also hypothesized that these associations would be mediated by lower self-reported sleep disturbance, greater sleep duration, and higher sleep efficiency (see Figure 1a).18,33,38,39,71,72
Moderated Mediation Model Hypotheses
Based on thematic findings describing family participation in cultural practices and academic literature showing protective effects of culture in the AI/AN population, we hypothesized that cultural identity might buffer the effects of family functioning on sleep (see Figure 1b). We used moderated mediation to test whether cultural identity moderated any observed associations between family functioning and sleep.44,73
Stage 3: Quantitative Data Analysis
Unstandardized coefficients are presented in Table 3 and standardized coefficients are presented in Supplemental Material 4 (Table 1). As shown in Table 3, greater family cohesion was significantly associated with lower levels of depressive symptoms (−0.84, 95% CI: [−1.68, −0.06]), and there was a significant indirect effect via lower levels of subjective sleep disturbance (−0.49, 95% CI: [−0.95, −0.10]). In other words, greater family cohesion was associated with lower levels of sleep disturbance, which in turn was associated with lower levels of depressive symptoms. Similarly, greater family cohesion was significantly associated with lower levels of anxiety symptoms (−4.32, 95% CI: [−6.92, −2.14]), and there was a significant indirect effect via lower levels of sleep disturbance (−1.19, 95% CI: [−2.45, −0.25]). Thus, greater family cohesion was associated with lower levels of sleep disturbance, which in turn was associated with lower levels of anxiety problems. Also, greater family conflict was significantly associated with higher levels of depressive symptoms (0.86, 95% CI: [0.19, 1.51]), and there was a significant indirect effect via higher levels of sleep disturbance (0.61, 95% CI: [0.30, 1.04]) such that greater family conflict was associated with higher levels of sleep disturbance, which in turn was associated with higher levels of depressive symptoms. Similarly, greater family conflict was significantly associated with higher levels of anxiety symptoms (4.34, 95% CI: [2.48, 6.43]), and there was a significant indirect effect via higher levels of sleep disturbance (1.38, 95% CI: [0.60, 2.55]) such that greater family conflict was associated with higher levels of sleep disturbance, which in turn, was associated with higher levels of anxiety symptoms. There was no evidence of indirect effects from either family cohesion or conflict to depression or anxiety through actigraphy-measured sleep duration or efficiency. As shown in Supplemental Material 4 (Table 1), the effect sizes were in the small and small-to-medium range for path c’ (shown in Figure 1a) across models with different mediators and outcomes. For the models with sleep disturbance as the mediator, the effect sizes were in the small-to-medium range for path b and in the small range for both path a and the indirect effects (a*b).
Table 3.
Indirect Effects via Self-Reported Sleep Disturbance, and Actigraphy-Measured Sleep Duration and Efficiency.
| path c' (X→Y) | path b (M→Y) | path a (X→M) | Indirect effects (a*b) | |||
|---|---|---|---|---|---|---|
| X | M | Y | coef. (95% CI) | coef. (95% CI) | coef. (95% CI) | coef. (95% CI) |
| Family cohesion | Sleep disturbance | Depression | −0.84 [−1.68, −0.06] | 0.08 [0.05, 0.11] | −6.15 [−10.92, −0.84] | −0.49 [−0.95, −0.10] |
| Family cohesion | Sleep disturbance | Anxiety | −4.32 [−6.92, −2.14] | 0.19 [0.11, 0.28] | −6.15 [−10.92, −0.8] | −1.19 [−2.45, −0.25] |
| Family conflict | Sleep disturbance | Depression | 0.86 [0.19, 1.51] | 0.08 [0.05, 0.10] | 8.14 [4.48, 11.80] | 0.61 [0.30, 1.04] |
| Family conflict | Sleep disturbance | Anxiety | 4.34 [2.48, 6.43] | 0.17 [0.08, 0.26] | 8.14 [4.48, 11.80] | 1.38 [0.60, 2.55] |
| Family cohesion | Sleep duration | Depression | −1.35 [−2.22, −0.51] | 0.001 [−0.003, 0.01] | −4.54 [−31.79, 24.28] | −0.01 [−0.14, 0.04] |
| Family cohesion | Sleep duration | Anxiety | −5.53 [−8.01, −3.03] | 0.01 [−0.01, 0.02] | −4.90 [−32.01, 23.61] | −0.02 [−0.47, 0.14] |
| Family conflict | Sleep duration | Depression | 1.48 [0.75, 2.20] | 0.001 [−0.003, 0.01] | 7.03 [−17.70, 32.41] | 0.01 [−0.03, 0.16] |
| Family conflict | Sleep duration | Anxiety | 5.73 [3.76, 7.77] | 0.004 [−0.01, 0.02] | 7.01 [−17.64, 32.49] | 0.03 [−0.11, 0.51] |
| Family cohesion | Sleep efficiency | Depression | −1.38 [−2.24, −0.53] | −0.02 [−0.06, 0.01] | −0.96 [−4.01, 2.37] | 0.02 [−0.04, 0.17] |
| Family cohesion | Sleep efficiency | Anxiety | −5.53 [−8.08, −2.99] | 0.03 [−0.09, 0.13] | −0.89 [−3.94, 2.45] | −0.02 [−0.43, 0.11] |
| Family conflict | Sleep efficiency | Depression | 1.51 [0.80, 2.23] | −0.02 [−0.06, 0.01] | 0.80 [−2.41, 4.33] | −0.02 [−0.17, 0.04] |
| Family conflict | Sleep efficiency | Anxiety | 5.73 [3.80, 7.76] | 0.03 [−0.08, 0.13] | 0.74 [−2.48, 4.25] | 0.02 [−0.11, 0.37] |
Note. All models controlled for sex and age of the adolescent and single parent household. Boldface indicates statistically significant coefficients (p < .05). 95% CI = 95% bootstrap confidence interval. X = independent variable. M = putative mediator. Y = dependent variable.
As shown in Figure 1, our moderated mediation model tested whether observed indirect effects of family conflict or cohesion on depression or anxiety via self-reported sleep disturbance were moderated by cultural identity. We only ran moderated mediation models for the self-reported sleep disturbance model, given that no indirect effects were found for actigraphy-measured outcomes. Model fit statistics and estimated index of moderated mediation are presented in Supplemental Material 4 (Table 2). Model fit was acceptable (CFIs ≥ 0.95, TLIs ≥ 0.90, RMSEAs ≤ .08, SRMR < .05). We did not find any significant moderated mediation effects, suggesting that indirect effects did not differ significantly at different levels of AI/AN cultural identity.
DISCUSSION
This study addresses several critical gaps in the literature by furthering our understanding of the role of family cohesion and conflict on mental health in urban AI/AN youth. We used an integrative mixed methods approach to examine family functioning and sleep in relation to mental health among urban-dwelling AI/AN youth in the context of cultural identity. To the best of our knowledge, this is the first study to examine these issues in AI/AN populations using both subjective and objective sleep measures. Our findings build on previous research with AI/AN youth, which has focused predominantly on family structure and substance use.45-47,74-77 We added to this work by examining qualitative themes of family functioning to guide us in our quantitative analyses. Although the interviews did not initially set out to explore aspects of family functioning, participants provided numerous unsolicited comments on this topic, highlighting the importance of family dynamics. Combining qualitative and quantitative data helped describe the complex and interdependent associations among family functioning, sleep, and mental health, and the role of cultural identity in these associations.
Qualitative findings illustrated that the urban AI/AN adolescents in our sample perceived a sense of family togetherness, and half commented on the role of daily family interactions in building a sense of family togetherness, AI/AN identity, and family-centered traditional activities. Qualitative findings were supported by youths’ perceptions of family dynamics on the survey, which indicated limited family conflict. Similar to work with other population groups,78,79 youth in this study identified an important role for extended family members in daily family functioning, which mostly occurred via co-habitation. Some youth were comforted by having extended family in their homes; in other cases, they reported negative implications for sleep and health, consistent with previous work in this area.45,46 This highlights the need for family-level interventions focused on balancing kinship and family ties while also recognizing potential constraints of sleeping environments and the challenges of co-habitation.
Consistent with prior literature,12,39,80 our quantitative results indicated that higher family functioning was associated with better mental health through lower levels of self-reported sleep disturbance. However, we did not observe any significant indirect effects of actigraphy-measured sleep duration or efficiency. This may be because the significant associations we observed were due, in part, to shared method variance, as family functioning and mental health were both based on self-report measures. Work in other adolescent samples has also shown stronger associations between self-reported sleep problems, including insomnia, and mental health compared to objective measures of sleep.57,81 Overall, findings suggest that improving sleep quality may be an important target for future, family-based interventions that address improving the mental health in AI/AN youth. We also recommend future longitudinal studies to further our understanding on the role of family functioning and long-term health benefits among urban AI/AN youth.
Previous work has emphasized the important protective role that cultural identity may play in improving mental health in AI/AN individuals.82 However, we did not find that cultural identity moderated associations of family conflict/cohesion, sleep disturbance, and depressive/anxiety symptoms. The lack of significant moderation may be due to the complex, dynamic, and multi-dimensional nature of cultural identity among urban AI/AN youth. 83 Null results may also be explained by the fact that the MEIM scale may not capture the most salient cultural identity factors among urban AI/AN youth. For example, prior work with this scale in AI/AN youth discusses aspects of identity that require additional examination, such as the role of biculturalism in indigenous identity or the role of engagement in specific cultural activities.84 Further research and psychometric evaluations may enhance our understanding of optimal measurement scales for AI/AN cultural identity in the context of complex urban life.
Limitations
The study has several limitations. First, the study sample is not representative of urban AI/AN youth experiences elsewhere in the U.S. because participants were recruited from northern, central, and southern California. Regarding qualitative data, this subsample was randomly selected from the full study sample. Although the two samples were comparable, the relatively small sample size limits generalizability of findings. Another limitation is that the interview protocol did not systematically elicit information on family functioning. The family cohesion and conflict themes in the interview data emphasize the importance of family dynamics for youth; however, the lack of systematic narrative elicitation has likely narrowed prevalence and range of thematic content on this topic. Finally, the mediation and moderated mediation models we tested were based on cross-sectional data, which precludes causal inference. Also, some fit statistics of the moderated mediation models did not reach the recommended cut-off for acceptable fit (i.e., TLIs > 0.90 but did not go above 0.95), raising possible concerns about model misspecification and requiring further examination in a separate, larger sample. The current study was a secondary analysis of the baseline data of the parent study and will need to be replicated in future studies. However, findings are an important first step in understanding these associations among AI/AN youth and can help inform future studies and prevention and intervention efforts for this population.
Conclusions
This study provides an important look at the pathway between family functioning and mental health among AI/AN adolescents, and how sleep and cultural context contribute to these associations. In qualitative interviews, adolescents emphasized distinct aspects of family cohesion, including daily interactions that build a sense of family togetherness, discussions about AI/AN identity, and family-centered traditional activities. Our analysis indicated that better family functioning (i.e., greater cohesion and less conflict) was associated with fewer depressive and anxiety symptoms through lower levels of sleep disturbance. Findings suggest that family-level interventions need to be tailored to balance the importance of kinship and family ties while also recognizing potential constraints of sleeping environments and challenges of co-habitation. Addressing sleep health with families may help improve adolescents’ overall well-being. Finally, research with this population should continue to explore how cultural identity may function to strengthen family cohesion and resilience and ultimately reduce the risk of mental health problems in AI/AN youth.
Supplementary Material
Narratives show family cohesion through family traditional practice
Narratives show role family cohesion plays in sleep, e.g., stable sleep environment
Better family functioning had direct effect on less depression and anxiety
Better family functioning had indirect effects through lower sleep disturbance
Cultural identity was not a significant moderator in the tested pathways
Acknowledgments
This work was funded by a grant from the National Institute on Minority Health and Health Disparities (R01MD012190, PIs: Troxel, D’Amico, and Dickerson). We thank Jennifer Parker, Keisha McDonald, and the RAND Survey Research Group for their help with this study.
Footnotes
CRediT roles for the authors:
Alina I. Palimaru, PhD MPP: formal qualitative and mixed methods analysis; investigation; writing original draft; review and editing.
Lu Dong, PhD: formal quantitative analysis; investigation; writing original draft; review and editing.
Ryan A. Brown, PhD MA: formal analysis; investigation; methodology; writing original draft; review and editing.
Elizabeth J. D’Amico, PhD MA: conceptualization; data curation; funding acquisition; project administration; supervision; investigation; review and editing.
Daniel L. Dickerson, DO MPH: conceptualization; data curation; funding acquisition; project administration; supervision; investigation; review and editing.
Carrie L. Johnson, PhD: project administration; investigation; review and editing.
Wendy M. Troxel, PhD MS: conceptualization; data curation; funding acquisition; project administration; supervision; investigation; review and editing.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Alina I. Palimaru, RAND Corporation, Santa Monica, CA
Lu Dong, RAND Corporation, Santa Monica, CA.
Ryan A. Brown, RAND Corporation, Santa Monica, CA
Elizabeth J. D’Amico, RAND Corporation, Santa Monica, CA
Daniel L. Dickerson, UCLA Integrated Substance Abuse Programs (ISAP), Semel Institute for Neuroscience and Human Behavior, Los Angeles, CA
Carrie L. Johnson, Sacred Path Indigenous Wellness Center, Los Angeles, CA
Wendy M. Troxel, RAND Corporation, Pittsburgh, PA
References
- 1.Reijneveld SA. Mental health as a public health issue. European Journal of Public Health. 2005;15(2):111–111. [Google Scholar]
- 2.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- 3.Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare (Basel). 2018;7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy LE, Jack HE, Concepcion TL, Collins PY. Integrating Urban Adolescent Mental Health Into Urban Sustainability Collective Action: An Application of Shiffman & Smith's Framework for Global Health Prioritization. Front Psychiatry. 2020;11:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudolph KE, Shev A, Paksarian D, et al. Environmental noise and sleep and mental health outcomes in a nationally representative sample of urban US adolescents. Environ Epidemiol. 2019;3(4):e056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanson CL, Crandall A, Barnes MD, Magnusson B, Novilla MLB, King J. Family-Focused Public Health: Supporting Homes and Families in Policy and Practice. Front Public Health. 2019;7:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serfaini K, Donovan DM, Wendt DC, Matsumiya B, McCarty CA. A Comparison of Early Adolescent Behavioral Health Risks Among Urban American Indians/Alaska Natives and their Peers. Am Indian Alsk Native Ment Health Res. 2017;24(2):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. CDC and Indian Country Working Together. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services;2017. [Google Scholar]
- 9.Brave Heart MY, DeBruyn LM. The American Indian Holocaust: healing historical unresolved grief. Am Indian Alsk Native Ment Health Res. 1998;8(2):56–78. [PubMed] [Google Scholar]
- 10.CensusBureau. American Indian and Alaska Native Summary File; Table: PCT2; Urban and rural; Universe Total Population; Population group name: American Indian and Alaska Native alone or in combination with one or more races. . Washington, D.C.: U.S. Census Bureau;2010. [Google Scholar]
- 11.Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT. Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain. 2010;11(11):1027–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scavenius C, Granski M, Lindberg MR, Vardanian MM, Chacko A. Adolescent Gender and Age Differences in Responsiveness to Functional Family Therapy. Fam Process. 2019. [DOI] [PubMed] [Google Scholar]
- 13.Carskadon MA. Sleep in adolescents: the perfect storm. Pediatr Clin North Am. 2011;58(3):637–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang J, Xu Z, Zhao K, et al. Sleep Habits, Sleep Problems, Sleep Hygiene, and Their Associations With Mental Health Problems Among Adolescents. J Am Psychiatr Nurses Assoc. 2018;24(3):223–234. [DOI] [PubMed] [Google Scholar]
- 15.Hysing M, Heradstveit O, Harvey AG, Nilsen SA, Boe T, Sivertsen B. Sleep problems among adolescents within child and adolescent mental health services. An epidemiological study with registry linkage. Eur Child Adolesc Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmeer KK, Tarrence J, Browning CR, Calder CA, Ford JL, Boettner B. Family contexts and sleep during adolescence. SSM Popul Health. 2019;7:004–004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blackham A, McDaniel JR, Chauvin IA, Nelson KL, Buboltz WC. Sleep Disruptions and Disorders in Children and Adolescents: A Review of the Impact of Parents and Family on Sleeping Behaviors. Annals of Sleep Medicine. 2019;2(1). [Google Scholar]
- 18.Haines J, Rifas-Shiman SL, Horton NJ, et al. Family functioning and quality of parent-adolescent relationship: cross-sectional associations with adolescent weight-related behaviors and weight status. Int J Behav Nutr Phys Act. 2016;13:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D'Amico EJ, Dickerson DL, Brown RA, Klein DJ, Agniel D, Johnson C. Unveiling an 'invisible population': health, substance use, sexual behavior, culture, and discrimination among urban American Indian/Alaska Native adolescents in California. Ethn Health. 2019:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kulis SS, Ayers SL, Harthun ML, Jager J. Parenting in 2 Worlds: Effects of a Culturally Adapted Intervention for Urban American Indians on Parenting Skills and Family Functioning. Prev Sci. 2016;17(6):721–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Worthman CM, Brown RA. Companionable sleep: social regulation of sleep and cosleeping in Egyptian families. J Fam Psychol. 2007;21(1):124–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Becker SP, Langberg JM, Byars KC. Advancing a biopsychosocial and contextual model of sleep in adolescence: a review and introduction to the special issue. J Youth Adolesc. 2015;44(2):239–270. [DOI] [PubMed] [Google Scholar]
- 23.Porter RJ. The biopsychosocial model in mental health. Aust N Z J Psychiatry. 2020;54(8):773–774. [DOI] [PubMed] [Google Scholar]
- 24.Lehman BJ, David DM, Gruber JA. Rethinking the biopsychosocial model of health: Understanding health as a dynamic system. Social and Personality Psychology Compass. 2017;11(8). [Google Scholar]
- 25.Campbell IG, Feinberg I. Longitudinal trajectories of non-rapid eye movement delta and theta EEG as indicators of adolescent brain maturation. Proc Natl Acad Sci U S A. 2009;106(13):5177–5180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. 2014;10:679–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier Parental Set Bedtimes as a Protective Factor Against Depression and Suicidal Ideation. Sleep. 2010;33(1):97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agostini A, Centofanti S. Normal Sleep in Children and Adolescence. Child Adolesc Psychiatr Clin N Am. 2021;30(1):1–14. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Huidobro D, Puschel K, Soto G. Family functioning style and health: opportunities for health prevention in primary care. Br J Gen Pract. 2012;62(596):e198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sander JB, McCarty CA. Youth depression in the family context: familial risk factors and models of treatment. Clin Child Fam Psychol Rev. 2005;8(3):203–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Freed RD, Rubenstein LM, Daryanani I, Olino TM, Alloy LB. The Relationship Between Family Functioning and Adolescent Depressive Symptoms: The Role of Emotional Clarity. J Youth Adolesc. 2016;45(3):505–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meltzer LJ, Montgomery-Downs HE. Sleep in the family. Pediatr Clin North Am. 2011;58(3):765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gregory AM, Caspi A, Moffitt TE, Poulton R. Family conflict in childhood: a predictor of later insomnia. Sleep. 2006;29(8):1063–1067. [DOI] [PubMed] [Google Scholar]
- 34.Kelly RJ, El-Sheikh M. Marital conflict and children's sleep: reciprocal relations and socioeconomic effects. J Fam Psychol. 2011;25(3):412–422. [DOI] [PubMed] [Google Scholar]
- 35.Adams GC, Stoops MA, Skomro RP. Sleep tight: exploring the relationship between sleep and attachment style across the life span. Sleep Med Rev. 2014;18(6):495–507. [DOI] [PubMed] [Google Scholar]
- 36.Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. 2015;21:72–85. [DOI] [PubMed] [Google Scholar]
- 37.Dahl RE, El-Sheikh M. Considering sleep in a family context: introduction to the special issue. J Fam Psychol. 2007;21(1):1–3. [DOI] [PubMed] [Google Scholar]
- 38.Zapata Roblyer MI, Grzywacz JG. Demographic and Parenting Correlates of Adolescent Sleep Functioning. J Child Fam Stud. 2015;24(11):3331–3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peltz JS, Rogge RD, O'Connor TG. Adolescent sleep quality mediates family chaos and adolescent mental health: A daily diary-based study. J Fam Psychol. 2019;33(3):259–269. [DOI] [PubMed] [Google Scholar]
- 40.Garcia JL. Historical Trauma and American Indian/Alaska Native Youth Mental Health Development and Delinquency. New Dir Child Adolesc Dev. 2020;2020(169):41–58. [DOI] [PubMed] [Google Scholar]
- 41.Gewirtz A, Forgatch M, Wieling E. Parenting practices as potential mechanisms for child adjustment following mass trauma. Journal of Marital and Family Therapy. 2008;34(2):177–192. [DOI] [PubMed] [Google Scholar]
- 42.Winek JL. Systemic family therapy: From theory to practice. Thousand Oaks, CA: Sage; 2010. [Google Scholar]
- 43.Burnette CE, Boel-Studt S, Renner LM, et al. The Family Resilience Inventory: A Culturally Grounded Measure of Current and Family-of-Origin Protective Processes in Native American Families. Fam Process. 2020;59(2):695–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wright S, Nebelkopf E, King J, Maas M, Patel C, Samuel S. Holistic system of care: evidence of effectiveness. Subst Use Misuse. 2011;46(11):1420–1430. [DOI] [PubMed] [Google Scholar]
- 45.Lonczak HS, Fernandez A, Austin L, Marlatt GA, Donovan DM. Family structure and substance use among American Indian youth: A preliminary study. Families, Systems, & Health. 2007;25(1):10–22. [Google Scholar]
- 46.Tingey L, Cwik MF, Rosenstock S, et al. Risk and protective factors for heavy binge alcohol use among American Indian adolescents utilizing emergency health services. Am J Drug Alcohol Abuse. 2016;42(6):715–725. [DOI] [PubMed] [Google Scholar]
- 47.Rees C, Freng A, Winfree LT Jr. The Native American adolescent: social network structure and perceptions of alcohol induced social problems. J Youth Adolesc. 2014;43(3):405–425. [DOI] [PubMed] [Google Scholar]
- 48.Palinkas LA, Mendon SJ, Hamilton AB. Innovations in Mixed Methods Evaluations. Annu Rev Public Health. 2019;40:423–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yoshikawa H, Weisner TS, Kalil A, Way N. Mixing qualitative and quantitative research in developmental science: uses and methodological choices. Dev Psychol. 2008;44(2):344–354. [DOI] [PubMed] [Google Scholar]
- 50.Povee K, Roberts L, Bourke J, Leonard H. Family functioning in families with a child with Down syndrome: a mixed methods approach. J Intellect Disabil Res. 2012;56(10):961–973. [DOI] [PubMed] [Google Scholar]
- 51.Palimaru AI, Brown RA, Troxel WM, Dickerson DL, Johnson CL, D'Amico EJ. Understanding sleep facilitators, barriers, and cultural dimensions in Native American urban youth. Sleep Health. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fok CC, Allen J, Henry D, People Awakening T. The brief family relationship scale: a brief measure of the relationship dimension in family functioning. Assessment. 2014;21(1):67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moos RH, Moos BS. Family environment scale manual Third ed. Palo Alto, CA: Consulting Psychologists Press; 1994. [Google Scholar]
- 54.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–216. [DOI] [PubMed] [Google Scholar]
- 55.Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Med Rev. 2002;6(2):113–124. [DOI] [PubMed] [Google Scholar]
- 56.Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification from wrist activity. Sleep. 1992;15(5):461–469. [DOI] [PubMed] [Google Scholar]
- 57.Alfano CA, Patriquin MA, De Los Reyes A. Subjective - Objective Sleep Comparisons and Discrepancies Among Clinically-Anxious and Healthy Children. J Abnorm Child Psychol. 2015;43(7):1343–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Richardson LP, Rockhill C, Russo JE, et al. Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. 2010;125(5):e1097–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mossman SA, Luft MJ, Schroeder HK, et al. The Generalized Anxiety Disorder 7-item scale in adolescents with generalized anxiety disorder: Signal detection and validation. Ann Clin Psychiatry. 2017;29(4):227–234A. [PMC free article] [PubMed] [Google Scholar]
- 60.Phinney JS. The Multigroup Ethnic Identity Measure. Journal of Adolescent Research. 2016;7(2):156–176. [Google Scholar]
- 61.Brown RA, Dickerson DL, Klein DJ, Agniel D, Johnson CL, D’Amico EJ. Identifying as American Indian/Alaska Native in Urban Areas: Implications for Adolescent Behavioral Health and Well-Being. Youth & Society. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dedoose [computer program]. Version Dedoose version 8.2.32. Los Angeles, CA: SocioCultural Research Consultants, LLC.; 2019. [Google Scholar]
- 63.Ryan GW, Bernard HR. Techniques to identify themes. Field Methods. 2003;15:85–109. [Google Scholar]
- 64.StataCorp. Stata Statistical Software: Release 16. In. Vol StataCorp LLC. College Station, TX: 2019. [Google Scholar]
- 65.Muthén LK, Muthén BO. Mplus user’s guide. 8th ed. ed. Los Angeles, CA: 2017. [Google Scholar]
- 66.Troxel WM, Lee L, Hall M, Matthews KA. Single-parent family structure and sleep problems in black and white adolescents. Sleep Med. 2014;15(2):255–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mackinnon DP, Lockwood CM, Williams J. Confidence Limits for the Indirect Effect: Distribution of the Product and Resampling Methods. Multivariate Behav Res. 2004;39(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lt Hu, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- 69.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, eds. Testing structural equation models. Beverly Hills, CA: Sage; 1993:136–162. [Google Scholar]
- 70.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 71.Reigstad B, Jorgensen K, Sund AM, Wichstrom L. Prevalences and correlates of sleep problems among adolescents in specialty mental health services and in the community: what differs? Nord J Psychiatry. 2010;64(3):172–180. [DOI] [PubMed] [Google Scholar]
- 72.Owens J, Adolescent Sleep Working G, Committee on A. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Redwood D, Schumacher MC, Lanier AP, et al. Physical activity patterns of American Indian and Alaskan Native people living in Alaska and the Southwestern United States. Am J Health Promot. 2009;23(6):388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Beebe LA, Vesely SK, Oman RF, Tolma E, Aspy CB, Rodine S. Protective assets for non-use of alcohol, tobacco and other drugs among urban American Indian youth in Oklahoma. Matern Child Health J. 2008;12 Suppl 1:82–90. [DOI] [PubMed] [Google Scholar]
- 75.Sapra KJ, Jubinski SM, Tanaka MF, Gershon RR. Family and partner interpersonal violence among American Indians/Alaska Natives. Inj Epidemiol. 2014;1(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention;2011. [Google Scholar]
- 77.Evans-Campbell T, Lindhorst T, Huang B, Walters KL. Interpersonal violence in the lives of urban American Indian and Alaska Native women: implications for health, mental health, and help-seeking. Am J Public Health. 2006;96(8):1416–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Taylor RJ, Chatters LM, Woodward AT, Brown E. Racial and Ethnic Differences in Extended Family, Friendship, Fictive Kin and Congregational Informal Support Networks. Fam Relat. 2013;62(4):609–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reyes AM. The Economic Organization of Extended Family Households by Race/Ethnicity and Socioeconomic Status. J Marriage Fam. 2018;80(1):119–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Robinson M, Kendall GE, Jacoby P, et al. Lifestyle and demographic correlates of poor mental health in early adolescence. J Paediatr Child Health. 2011;47(1–2):54–61. [DOI] [PubMed] [Google Scholar]
- 81.Moore M, Kirchner HL, Drotar D, et al. Relationships among sleepiness, sleep time, and psychological functioning in adolescents. J Pediatr Psychol. 2009;34(10):1175–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Farias M, Underwood R, Claridge G. Unusual but sound minds: mental health indicators in spiritual individuals. Br J Psychol. 2013;104(3):364–381. [DOI] [PubMed] [Google Scholar]
- 83.Brown RA, Dickerson DL, D'Amico EJ. Cultural Identity Among Urban American Indian/Alaska Native Youth: Implications for Alcohol and Drug Use. Prev Sci. 2016;17(7):852–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kulis S, Wagaman MA, Tso C, Brown EF. Exploring Indigenous Identities of Urban American Indian Youth of the Southwest. J Adolesc Res. 2013;28(3):271–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.