Abstract
Simple Summary
Although rare, uveal melanoma (UM) is the most common cancer that develops inside adult eyes. The prognosis is poor, since 50% of patients will develop lethal metastases in the first decade, especially to the liver. Once metastases are detected, life expectancy is limited, given that the available treatments are mostly unsuccessful. Thus, there is a need to find methods that can accurately predict UM prognosis and also effective therapeutic strategies to treat this cancer. In this manuscript, we initially compile the current knowledge on epidemiological, clinical, pathological and molecular features of UM. Then, we cover the most relevant prognostic factors currently used for the evaluation and follow-up of UM patients. Afterwards, we highlight emerging molecular markers in UM published over the last three years. Finally, we discuss the problems preventing meaningful advances in the treatment and prognostication of UM patients, as well as forecast new roadblocks and paths of UM-related research.
Abstract
Uveal melanoma (UM) is the most common malignant intraocular tumour in the adult population. It is a rare cancer with an incidence of nearly five cases per million inhabitants per year, which develops from the uncontrolled proliferation of melanocytes in the choroid (≈90%), ciliary body (≈6%) or iris (≈4%). Patients initially present either with symptoms like blurred vision or photopsia, or without symptoms, with the tumour being detected in routine eye exams. Over the course of the disease, metastases, which are initially dormant, develop in nearly 50% of patients, preferentially in the liver. Despite decades of intensive research, the only approach proven to mildly control disease spread are early treatments directed to ablate liver metastases, such as surgical excision or chemoembolization. However, most patients have a limited life expectancy once metastases are detected, since there are limited therapeutic approaches for the metastatic disease, including immunotherapy, which unlike in cutaneous melanoma, has been mostly ineffective for UM patients. Therefore, in order to offer the best care possible to these patients, there is an urgent need to find robust models that can accurately predict the prognosis of UM, as well as therapeutic strategies that effectively block and/or limit the spread of the metastatic disease. Here, we initially summarized the current knowledge about UM by compiling the most relevant epidemiological, clinical, pathological and molecular data. Then, we revisited the most important prognostic factors currently used for the evaluation and follow-up of primary UM cases. Afterwards, we addressed emerging prognostic biomarkers in UM, by comprehensively reviewing gene signatures, immunohistochemistry-based markers and proteomic markers resulting from research studies conducted over the past three years. Finally, we discussed the current hurdles in the field and anticipated the future challenges and novel avenues of research in UM.
Keywords: uveal melanoma, prognostic factors, biomarkers, metastases, survival, molecular pathology
1. Introduction
Uveal melanoma (UM) is the most common primary malignant neoplasia afflicting the eyes of adults [1,2]. Metastases develop in approximately 50% of patients, who then have a shortened life expectancy [1,2,3]. UM metastasis can develop up to 30 years after the initial diagnosis and treatment [4], and once metastases are detected, the median survival time for UM patients is approximately 12 months, especially because therapeutic options for advanced disease are limited and mostly ineffective [5,6,7]. The identification of robust clinical and molecular biomarkers that can accurately predict the prognosis of patients, namely, the possibility of metastases development, is therefore of extreme relevance and an ongoing challenge in the field [8]. The discovery of robust prognostic biomarkers and/or models has the prospect to positively impact in a personalized UM patient approach, with patient-targeted surveillance and therapeutic strategies [9]. This is particularly pertinent since that there are diverse guidelines for the medical follow-up of UM patients and a definition of which tests are the most effective in detecting early disease relapse is lacking [for example, should patients be followed using only liver ultrasound and/or magnetic resonance imaging (MRI)? Should the MRI be performed with or without contrast medium?] [9,10]. On one hand, the establishment of UM patients with high-risk of disease relapse would lead to a more close monitoring of those patients [11]. On the other hand, the early detection of disease relapse, such as liver metastases, could enable the surgical removal or chemoembolization of those lesions in a premature state, which seems to be the most efficacious strategy currently available to deal with metastatic disease and to extend the life of UM patients with advanced disease [7,10,12]. In addition, liver lobe resection, systemic chemotherapy, radiofrequency ablation or isolated liver perfusion constitute alternative therapeutic approaches for UM metastatic to the liver, however, are essentially unsuccessful at achieving a final cure for the patient [6,12,13]. It is possible that patients who are eligible for metastases resection have a lower burden of disease and a potentially more favourable tumour biology compared with UM patients non-eligible for metastatic ablation [14].
In the present review, we first appraise the main clinical, epidemiological and pathological features of UM. Next, we review the aspects of UM genetics which are at the core of neoplastic transformation and summarize the most relevant knowledge on the currently used prognostic markers in UM, including the updated views on the molecular classification of UM. Afterwards, we review the gene signatures and novel immunohistochemistry-based biomarkers with prognostic relevance in UM published over the past three years. Finally, we discuss the current hurdles in the field, imminent challenges and the promising future research avenues towards a successful and optimized treatment of patients afflicted by this aggressive disease that significantly reduces the quality of life and average life expectancy of patients.
2. Uveal Melanoma: Relevant Epidemiological, Clinical and Pathological Features
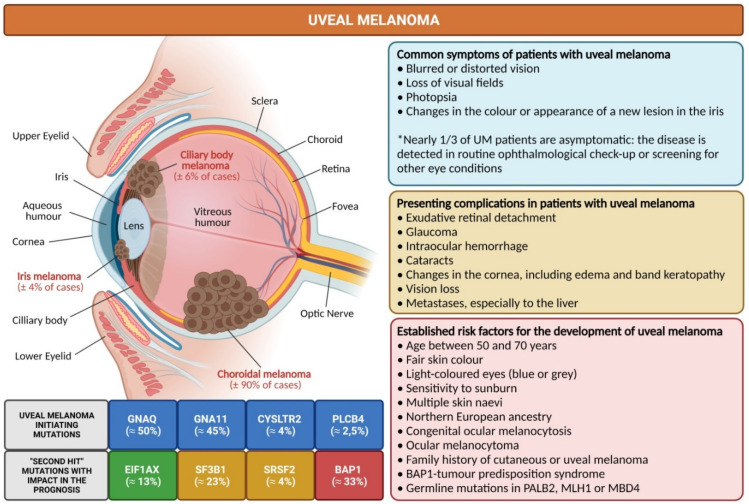
The first known description of the complete natural history of UM dates back to the beginning of the 19th century, when two Scotland-based surgeons, Allan Burns and James Wardrop, described and detailed the clinical history of a 41-year-old woman living in Glasgow, who developed an intraocular lesion that rendered her quickly blind and which became extremely painful and with extrascleral extension only after 4 months [15]. Even though she was enucleated, the patient later evolved with hepatic and abdominal metastases and died in less than a year after the initial medical visit [15]. UM develops from the uncontrolled proliferation of melanocytes in the uveal tract, which comprises the pigmented tissues in both the anterior (iris) and the posterior (choroid and ciliary body) segments of the eye (Figure 1). The disease is usually unilateral and the majority of UM cases have their epicenter in the choroid (≈90%), while nearly 6% of them are restricted to the ciliary body and 4% to the iris (Figure 1) [1,3,16]. The annual incidence in Europe and USA is ≈5 per million population, but worldwide it can range from <1 to >9 per million population per year [17,18,19,20]. Most patients with UM are diagnosed between 50 and 70 years old [18,21]. The symptoms that most commonly prompt UM patients for a medical visit are blurred or distorted vision, loss of visual fields, photopsia and changes in the colour or appearance of a new lesion in the iris (Figure 1) [9,22]. However, in nearly one-third of the UM cases, the patients are asymptomatic and the disease is only detected due to routine ophthalmological check-up or screening for other eye conditions, such as diabetic retinopathy (Figure 1) [9,22]. The most common presenting complications encountered in patients with UM are exudative retinal detachment, glaucoma, cataracts, intraocular hemorrhage, vision loss, changes in the cornea including edema and band keratopathy [21,22,23]. Less than 2% of UM patients have long-distance metastases already at presentation (Figure 1) [24].
Figure 1.
Overview of key facts in uveal melanoma, the most common intraocular primary malignant tumour in adults. Different risk factors are associated with the development of uveal melanoma. The choroid is the most frequent intraocular site of uveal melanoma development, which is detected in routine ophthalmological exams in asymptomatic patients. However, the majority of uveal melanoma patients present with symptoms, such as blurred vision or photopsia. Metastases, especially to the liver, occur in nearly 50% of patients during the first 10 years after diagnosis, but constitute a presenting symptom in only a small fraction of patients (<2%). In the carcinogenic process of uveal melanoma, several tumour-initiating and tumour-promoting mutations have already been identified and characterized. Uveal melanoma patients with mutations in BAP1 (highlighted in red) have been demonstrated to have the worst outcome, while patients with EIF1AX (highlighted in green) have a better prognosis and patients with SF3B1/SRSF2 (highlighted in orange) have an intermediate prognosis. Diagram generated in line with previous literature [1,2,3,9,22,25,26,27,36,37,38,39,40] (Diagram created with BioRender.com, accessed on 15 December 2021).
Over the past years, numerous risk factors have been described as being associated with the development of UM (Figure 1), of which the most established are an age between 50 and 70 years, a fair skin colour, light-coloured eyes (blue or grey), multiple skin naevi, sensitivity to sunburn, northern European ancestry, congenital ocular melanocytosis, ocular melanocytoma, family history of cutaneous melanoma or UM, BAP1 (BRCA1-associated protein 1)-tumour predisposition syndrome and also germline mutations in MBD4 (methyl-CpG-binding domain protein 4), MLH1 (mutL homolog 1) and PALB2 (partner and localizer of BRCA2) [1,9,25,26,27]. Interestingly, in UM there is no evidence of gene signatures indicative of tumours induced by ultraviolet (UV) irradiation, with the only exception being iris melanoma and some residual cases of posterior melanomas [28,29,30].
Once the diagnosis of UM is made, the treatment will aim to treat the tumour, preserve the eye up to its best functional state possible and conserve the vision [9]. Therapeutic modalities include phototherapy (no longer recommended), different forms of radiotherapy (106ruthenium brachytherapy or 125iodine brachytherapy, proton beam therapy or stereotactic radiosurgery) and local resection after radiotherapy for selected lesions [9,31,32,33,34,35]. Besides this, enucleation is the most adequate option for large-sized UMs and cases with advanced local disease, since it allows an enhanced local control with improved quality of life for the UM patient [9,31,32,33,34,35]. Interestingly, previous studies demonstrated superimposable mortality rates when comparing proton beam irradiation versus enucleation for patients with large choroidal melanomas [33]. Local tumour control is achieved in more than 95% of cases, even for large-size tumours [1,9]. Despite the successful local disease control, metastases will develop in nearly 50% of patients during the first 10 years (Table 1) [3,16].
Table 1.
Most frequent anatomic sites afflicted by metastases in uveal melanoma. The estimation of organ involvement was based on the compilation of the data from 1092 patients extracted from 5 relevant previously published studies [24,41,42,43,44,45]. Relative percentages are variable depending on the cohort studied. However, in all studies, the liver is the preferential site of UM metastization.
| Anatomical Site | % of Cases |
|---|---|
| Liver | 85 |
| Lung | 29 |
| Bones | 16 |
| Subcutaneous tissue | 12 |
| Lymph Nodes | 11 |
| Brain | 5 |
| Other sites | 13 |
| Multiple sites | 32 |
Death related with metastases onset is more likely in the first 10 years after UM diagnosis, being scarcely observed beyond 20 years after the initial treatment [46,47,48]. Some studies demonstrate that metastization might occur early in the disease process and that micrometastases can remain in a quiescent state for several years, without the possibility of efficiently detecting them, similarly to other malignant neoplasias [49,50,51]. The liver (≈85%) is the preferred site for metastases development in UM, sometimes constituting the initial presentation of the disease [41,52] (Table 1). Other locations of UM metastasis include the lung (≈29%) and bone (≈16%), among others [24,41] (Table 1). In nearly one-third of the metastatic cases, there is involvement of multiple sites by UM metastases [24,41]. Despite the advances in the understanding of UM biology and the advent of new therapeutic modalities, the 5-year survival rate for UM (≈80%) has remained stable over the past five decades [46,47,48].
3. The Main Genetic Features of Uveal Melanoma
The genetic studies conducted over the past couple of decades allowed the identification of significant mutations in almost a dozen of genes which are relevant for UM development (Figure 1) [36,53]. In contrast to other tumours, including cutaneous melanoma [54] or lung adenocarcinoma [55], the tumour mutational burden (TMB; defined as the number of non-inherited mutations per million of bases of investigated genomic sequence) of UM is normally low [28,36,40]. Indeed, The Cancer Genome Atlas (TCGA) project (http://cancergenome.nih.gov/, accessed on 15 December 2021) showed that TMB for UM was 1,1 per Mb, whereas for cutaneous melanoma it was 18 per Mb [40,56]. In UM, the genes whose studies demonstrated the presence of mutations which are relevant for UM development can fundamentally be grouped into genes with tumour-initiating mutations and genes harbouring mutations with relevant impact in the prognosis of patients (Figure 1) [36,53,57]. Indeed, more than 90% of the patients have activating mutations in GNAQ (Guanine nucleotide-binding protein G(q) subunit alpha, ≈50%) and GNA11 (Guanine nucleotide-binding protein subunit alpha-11, ≈45%) (Figure 1) [36,53]. These mutations are normally mutually exclusive, which means that if a patient carries a mutation in GNAQ, they normally do not harbour a mutation in GNA11 and vice versa [36,58]. GNAQ and GNA11 encode proteins that are both involved in the Gα11/Q pathway, which regulates a myriad of cellular processes, including cell proliferation and growth [58,59,60]. In a restrict number of UM patients, there are tumour initiating mutations in CYSLTR2 (cysteinyl leukotriene receptor 2), which also encodes a G-protein coupled receptor (Figure 1) [61,62], or PLCB4 (1-Phosphatidylinositol-4,5-bisphosphate phosphodiesterase beta-4), which encodes a protein downstream in the GNAQ signalling cascade (Figure 1) [63]. Together, all these tumour-initiating mutations suggest that a dysregulated G-protein signalling is at the core of the carcinogenic process in UM development [58]. However, these mutations do not differentially impact on the prognosis of UM [64]. Recent research proposed that the pathway based on the axis GNAQ/11–PLCβ–PKC–MAPK could be a preferential target in the treatment of tumours with underlying Gαq pathway mutations, such as most of the UM cases [65]. Interestingly, UM normally arise de novo, but they can also develop from choroidal nevi, which frequently contain mutations in GNAQ, GNA11, CYSLTR2 and PLCB4 [62,66].
The process of malignant transformation in UM critically depends on “second hit” mutations, which in addition will also considerably impact on the prognosis of patients (Figure 1) [36,57,67]. Indeed, several studies suggest that metastization in UM is an early event and the ability to develop metastases with clinical impact is directly linked with the “second hit” genetic alterations of the primary tumour [36,57,67]. The most important mutated genes included in this group are BAP1, EIF1AX (eukaryotic translation initiation factor 1A, X-chromosomal), SF3B1 (splicing factor 3B subunit 1) and SRSF2 (serine and arginine rich splicing factor 2) (Figure 1) [36,67]. Nearly 10 years ago, in a breakthrough study, researchers identified in 26 of 31 (84%) metastasizing UM cases inactivating somatic mutations in the gene encoding BAP1 [48], which is located on chromosome 3p and is a deubiquitylase that participates in molecular complexes that are pivotal to the regulation of cell cycle, cellular differentiation, cell death and DNA damage response (DDR), among other key cellular pathways [49]. This study implicated that loss of BAP1 is a major event in the development of UM metastases [48]. Subsequent research demonstrated germline BAP1 mutations with familial clustering in different neoplasias, leading to the discovery of a new cancer syndrome, termed BAP1-tumour predisposition syndrome, which leads to the development of benign and malignant melanocytic skin tumours, malignant mesothelioma, UM and renal cell carcinomas, among other neoplasias [41,49,50,51,52]. BAP1 mutations are identified in nearly one-third of UM cases and loss of BAP1 or partial deletion of chromosome 3 including the BAP1 locus is a stronger predictor of higher risk of metastases and poor survival for UM patients [36,67,68].
The EIF1AX gene is located on chromosome X [53,69] and encodes a protein that interacts with mRNA, being involved in translation initiation, by a combination of recognition of target mRNA and also of ribosome stabilization, preparing mRNA for translation [53,69]. Mutations in EIF1AX, which occur in nearly 13% of UM cases (Figure 1), appear to be mutually exclusive to SF3B1 in UM and lead to altered protein translation processes [36,69]. Patients who harbour theses mutations have a decreased risk of metastases development and, therefore, a considerable better prognosis comparatively to UM patients with BAP1 loss (Figure 1) [36,67,70].
SF3B1 gene is located in chromosome 2 and is responsible for encoding the subunit 1 of the splicing factor 3b protein complex, a large molecular apparatus which is involved in the processing of precursor mRNA (spliceosome) [53,71]. It guarantees that correct splicing occurs through retaining pre-mRNA to define the site for splicing [53,70]. SF3B1 mutations, found in nearly 20% of UM cases (Figure 1), can therefore lead to alternative splicing events for a myriad of genes [69,70]. On the other hand, the SRFS2 gene is located in chromosome 17 and is a member of the serine/arginine (SR)-rich family of pre-mRNA splicing factors, which constitute part of the spliceosome [53,72]. Mutations in SRSF2 are found in up to 4% of UM cases (Figure 1) [36]. Similarly to SF3B1, mutations in SRFS2 lead to alternatively spliced transcripts [70,72]; however, the details of the impact of SF3B1/SRFS2 mutations in UM remain to be entirely understood [53,72]. Patients who harbour SF3B1/SRFS2 mutations have an increased risk of late-onset metastasis and, thus, have an intermediate prognosis comparatively to UM patients with EIF1AX mutations (low-risk) and BAP1 loss (high-risk) (Figure 1) [36,67,70,71].
4. Current Well-Established Prognostic Biomarkers in Uveal Melanoma
The establishment of an accurate prognosis for patients with UM is pivotal [73,74]. In this regard, the prognostic class of a given patient could impact on the specific protocol for surveillance of metastases development [8,11]. In addition, the stratification of patients based on their risk of metastases development or death could be a vital tool to select candidates to be included in clinical trials aiming to test promising adjuvant therapies [8,11,75]. In addition, patients might wish to know their accurate prognosis, which could be important in end-of-life planning, especially in a disease with no currently approved standard therapy for metastatic disease, which normally is associated with an extremely dismal prognosis [5,7,75,76].
Numerous robust prognostic factors for UM were established over the past years and are currently taken into account when evaluating primary UM cases (Table 2). Age could play an important prognostic role in UM, since adults older than 60 years at the time of diagnosis have an enhanced risk of metastases development compared to young and middle-aged adult patients [77,78]. Interestingly, some studies also suggest that gender could influence the prognosis of UM patients, documenting a worse prognosis for males, who have increased rate of metastases development and a decreased survival in the first decade after UM diagnosis [17,79].
Table 2.
Currently well-established prognostic factors in primary uveal melanoma. All the factors highlighted below are associated with a worse prognosis for patients diagnosed with UM.
| Factors Associated with a Worse Prognosis for Uveal Melanoma Patients |
|---|
| Higher age at diagnosis [77,78] |
| Male gender [17,79] |
| Ciliary body location and involvement [9,81,82] |
| Increased tumour size [Largest basal diameter (LBD) and tumour thickness (TT)] [73,82,85] |
| Epithelioid cell morphology [8,80,87] |
| Vascular invasion [83,88] |
| Extraocular spread [84,89] |
| Increased mitotic count [87,90,91] |
| Increased microvessel density [92,93] |
| Presence of tumour-infiltrating lymphocytes (TILs) [94,95,96] |
| Presence of tumour-infiltrating macrophages (TIMs) [94,95,96,97] |
| Presence of necrosis (in non-treated UM) [81] |
| Higher T stage (AJCC, TNM staging) [73,98] |
| Presence of uveal melanoma metastases [7,8,98] |
| Loss of nuclear BAP1 expression/BAP1 mutation [99,100,101,102] |
| PRAME expression [103,104,105,106] |
| Chromosomal abnormalities, especially M3, 8q gain, 6q loss and 1p loss [3,36,39,40,73,107,108,109] |
| Gene Expression Profiling (GEP) Class 2 [110,111,112,113] |
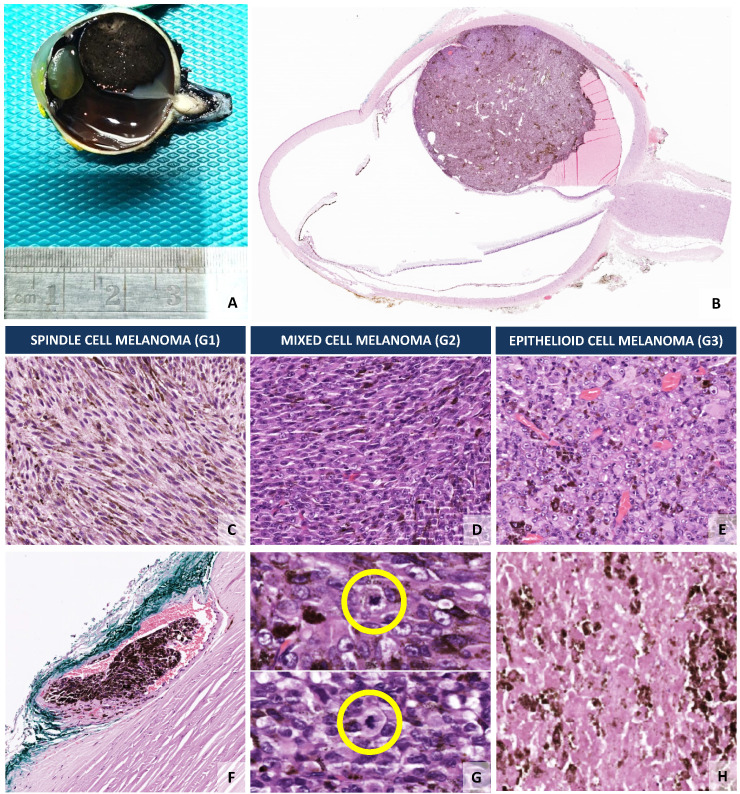
The location of the UM within the eye also has important prognostic implications [16,80]. While UM centred in the ciliary body or involving the ciliary body have the worst mortality rates within 5 years after diagnosis, iris melanoma has the best prognosis, with some studies pointing towards a 10-year mortality below 10% [9,81]. Choroidal melanoma, which is the most frequent type of UM (Figure 2), has an intermediate prognosis between ciliary body and iris melanoma [81]. The best prognosis for iris melanoma can be linked with the fact that the iris is easily visualized and most lesions are detected at an early stage [9,81,82]. Conversely, the ciliary body has a localization that is challenging for clinical examination, which can only be accomplished by slit-lamp examination, ophthalmoscopy, gonioscopy, or transillumination, so that lesions tend to grow larger before they can be detected [9,82]. In addition, the possibility of invasion of the Schlemm’s canal allows an easier and faster route for systemic dissemination of the UM [83,84].
Figure 2.
Uveal melanoma is a primary malignant tumour of the eye with a potential dismal prognosis, since nearly 50% of the patients die because of metastases, preferentially to the liver, which are not curable due to the absence of meaningful therapeutic strategies. The morphological features of uveal melanoma are instrumental to predict the prognosis of patients. (A) Eye specimen containing a pigmented round tumour located in the choroid (posterior segment of the eye), the most frequent anatomic location of uveal melanomas. (B) Whole-slide representative microscopic view of the large-sized choroidal melanoma with evidence of associated exudative retinal detachment (H&E, 2× magnification). (C) Uveal melanomas composed by more than 90% of spindle cells are called spindle cell melanomas (G1; H&E, 400× magnification). (D) Uveal melanomas containing more than 10% of a spindle cell component and less than 90% of an epithelioid component are termed mixed cell melanomas (G2; H&E, 400× magnification). (E) Epithelioid cell melanomas (G3), which are associated with a worse patient prognosis, are composed by more than 90% of epithelioid malignant cells (H&E, 400× magnification). (F) Uveal melanoma disseminates systemically through a preferential haematogenous pathway. The presence of images of vascular invasion is correlated with a worse prognosis for patients (H&E, 200× magnification). (G) The presence of an increased number of mitosis (yellow circle) also hints a worse outcome for uveal melanoma patients (H&E, 200× magnification). (H) The presence of necrosis in non-treated uveal melanoma cases is an additional marker of bad prognosis for patients (H&E, 200× magnification). A summary of all currently well-established markers of bad prognosis in uveal melanoma is presented in Table 2.
The tumour size is among the most robust established prognostic factors in the UM medical literature [8,80]. The largest basal diameter (LBD) and tumour thickness (TT), which are more accurately measured by ultrasonography and fundus photography, help to stratify the size of UM cases in small (T1), medium (T2), large (T3) and very large (T4) tumours, which considerably differ in their survival prognosis [73,82,85]. Some early studies showed that patients with tumours with a LBD above 15 mm have a significantly shorter survival comparatively to patients with tumours smaller than 15 mm [86]. In the international study for validation of the 7th edition of the American Joint Committee on Cancer (AJCC) classification for UM, involving more than 3000 patients, the authors performed Kaplan–Meier metastases-free estimates (5, 10 years), obtaining the following results: T1 (97%, 94%), T2 (85%, 80%), T3 (77%, 68%) and T4 (61%, 5-year only) [85]. In addition, in a previous study involving a large cohort of 8033 UM patients, the authors demonstrated a significant 5% increase in the risk of metastases at 10 years per each millimetre of increased thickness of the UM [16]. Therefore, increased UM size indicates a worse patient prognosis [16,85].
The morphology of the UM cells also has important prognostic implications for ciliary body and choroidal melanoma (Figure 2), whereas in iris melanoma this factor has no prognostic implications [8,80]. Patients with spindle cell UM, which contains more than 90% of spindle cells (G1) have the best survival; while epithelioid cell melanomas, which comprises more than 90% epithelioid cells (G3), have the worst prognosis (Figure 2) [8,114]. The melanomas which contain less than 90% of spindle cells and more than 10% of epithelioid cells (G2), termed mixed cell melanomas, have an intermediate prognosis (Figure 2) [8,114]. Interestingly, some authors demonstrated that the presence of any percentage of an epithelioid component is per se an indicator of a worse outcome [87].
UM preferentially escapes from the eye microenvironment through a haematogenous pathway [115]. The process seems to involve transendothelial migration using complex mechanisms of ameboid blebbing and mesenchymal lamellipodial protrusion, which remain to be fully understood [115]. Dissemination through the lymphatic system only occurs if there is extraocular extension with invasion of the conjunctival lymphatics [116,117]. Therefore, UM spread is intimately linked with the presence of tumour cells in blood vessels (Figure 2) [83], so that the presence of images of vascular invasion in UM (Figure 2), either inside or outside the tumoural area, is associated with a worse prognosis for UM patients and is correlated with other prognostic factors, such as LBD or epithelioid cell phenotype [88]. Additionally, the presence of angiotropism, which is defined as the presence of neoplastic cells disposed along the abluminal surface of vascular structures without intravasation, has also been demonstrated to be a prognostic factor for metastasis and UM-related death [83]. In line with this, microvessel density (MVD), a surrogate marker of angiogenesis which can be easily assessed using antibodies against CD34, became established as a significant prognostic factor in UM nearly two decades ago [92,93]. Higher MVD is independently associated with a poor prognosis and other markers of bad prognosis, such as epithelioid cell morphology and LBD [92,93], as well as with the UM genetic profile, namely, monosomy 3 [complete loss of one copy of chromosome 3 (M3)] and loss of BAP1 expression [118].
Extraocular spread of UM, irrespective of the type of extraocular spread route and dimension of the extraocular tumoural fragment, is a marker of worse prognosis in UM, being correlated with increased rate of metastases development and increased UM-related death [84]. Apparently, it is an indirect sign of enhanced tumour malignancy and for posterior tumours signals a more advanced disease state [84]. Extraocular spread is correlated with other important prognostic factors, such as UM size, tumour location, histologic type and cytogenetics [84,89]. For example, in UM cases with extraocular extension, a gain of chromosomal 8q is associated with increased risk of metastatic disease [89].
Mitotic counts constitute another robust and important classical prognostic factor in UM (Figure 2). In a straightforward manner, in haematoxylin and eosin (H&E) stained sections, mitotic counts are usually performed in 40 fields at high-power (40× objective), with or without the aid of immunohistochemistry (IHC) proliferation markers, such as Ki-67 or PHH3 (phospho-histone 3) [91]. Some pioneer studies demonstrated that mitotic counts were independently associated with metastatic risk and increased mitotic counts were correlated with a shorter survival [87,90].
The absence of a significant immune response against allografts placed within the ocular microenvironment led the pioneer transplantation immunologist Sir Peter Medawar to describe the eye as an immune privileged site nearly 70 years ago [119]. The eye has distinctive anatomical features, namely, a blood barrier analogous to the central nervous system (CNS) blood–brain barrier and lacks a direct lymphatic drainage [119,120]. Besides the anatomical features, novel distinctive immunological and biochemical mechanisms have emerged as plausible explanations for the immunologically unique and privileged microenvironment within the eye [119]. Therefore, unlike in other neoplasias, in UM patients the presence of tumour-infiltrating lymphocytes (TILs) and tumour-infiltrating macrophages (TIMs) is associated with a worse prognosis [94,95,96], with some authors suggesting it is a likely indirect signal of a disruption of the barrier between the eye microenvironment and the rest of the organism [121]. Studies in the early 1990s already demonstrated that patients with UM containing higher amounts of TILs had a worse outcome comparatively to patients with lower amounts of TILs [94,95]. In line with this, pioneer research conducted nearly 20 years ago also demonstrated that patients with UM containing higher amounts of TIMs had a shorter survival [96]. Ensuing studies showed that M2-type macrophages are the predominant macrophage population in UM, being more abundant in M3 UM cases comparatively to disomy 3 (D3) [97]. Interestingly, infiltration by M2-macrophages was linked with a shoddier prognosis for survival [97]. Our understanding of the interplay between the immune infiltrating cells and UM is still in its infancy, but as new knowledge emerges, a better understanding of the role and modulation of TILs and TIMs in UM might lead to innovative robust therapies for UM based on immunotherapy (please see Section 8) [122,123].
Similarly to other neoplasias, the presence of necrosis in non-treated tumours is also associated with an inferior prognosis in UM (Figure 2), with some studies demonstrating an association with other prognostic factors, namely, a correlation between a higher degree of necrosis and a larger tumour size, epithelioid morphology of UM cells or increased number of TIMs [81]. Therefore, the presence or absence of necrosis is a histomorphological feature that is normally assessed by the pathologist during the evaluation of UM cases (Figure 2).
UM is currently staged according to the 8th Edition of the TNM staging system of the American Joint Committee on Cancer (AJCC), which is still the gold standard system for prognostication in UM [73,98]. The TNM staging will help to define the follow-up strategies and the T category was demonstrated to be a robust predictor of UM metastatic disease with increased significant likelihood of metastases development at 5, 10 and 20 years for T1 (8%, 15%, 25%), T2 (14%, 25%, 40%), T3 (31%, 49%, 62%) and T4 (51%, 63%, 69%) stages [73,98]. In line with this, an analogous trend for significant increased risk of death with a higher T stage has also been demonstrated [73,98].
The development of a metastatic disease in UM is among the factors with the biggest impact in the definition of life expectancy of the UM patient [7,8]. Unless metastases are detected early and submitted to ablation therapy, the presence of metastases in UM is a marker of early death, given that effective therapeutic options for the metastatic UM disease are still limited [124,125]. In fact, recent studies demonstrate a median survival time of 17.5 months for M1a (largest diameter of the largest metastasis less than or equal to 3 cm), 9.6 months for M1b (largest diameter of the largest metastasis 3.1–8.0 cm) and 5 months for M1c (largest diameter of the largest metastasis greater than or equal to 8.1 cm) once metastatic UM disease is detected [98].
BAP1 status is one of the most relevant prognostic factors currently evaluated in patients with UM. Indeed, the determination of BAP1 status through IHC in primary UM has become routine in the prognostic evaluation, since it was shown to be highly correlated with gene mutation status [99,100,101,102]. Patients with loss of nuclear BAP1 staining were shown to have an 8-fold higher likelihood of developing metastases comparatively to patients with preserved nuclear BAP1 [100,101]. Therefore, BAP1 quickly became established as a robust independent survival predictor for UM patients, indicating the development of a likely aggressive metastatic phenotype [99,100,101]. Interestingly, a recent study also showed that BAP1 methylation at a single genomic locus is strongly correlated with BAP1 mutations, loss of BAP1 genomic copy and BAP1 protein levels [126]. Besides this, higher levels of BAP1 methylation significantly correlated with worse survival in UM patients [126]. A recent study also put in evidence that BAP1 mutations occur in the early steps of UM neoplastic development, before the tumour is even detected and with a timing that is likely to match the advent of the pioneer micrometastases [127].
Preferentially expressed antigen in melanoma (PRAME) was initially revealed by studies on skin melanoma as an antigen present in tumoural cells and recognized by T cells displaying cytotoxic activity [128]. In melanocytic lesions of the skin and conjunctiva, it is currently used as a helpful and robust adjunct marker to differentiate benign melanocytic lesions from melanoma [129,130]. Furthermore, the increased expression of PRAME is a marker of poor prognosis in different types of neoplasias, namely, breast cancer [131], head and neck squamous cell carcinoma (HNSCC) [132], neuroblastoma [133], osteosarcoma [134], among others. The prognostic significance of PRAME expression in UM emerged from a few studies conducted over the past 5 years, which showed that PRAME expression in UM is associated with an increased tumour volume, enhanced metastatic risk and global inferior prognosis [103,104,105,106].
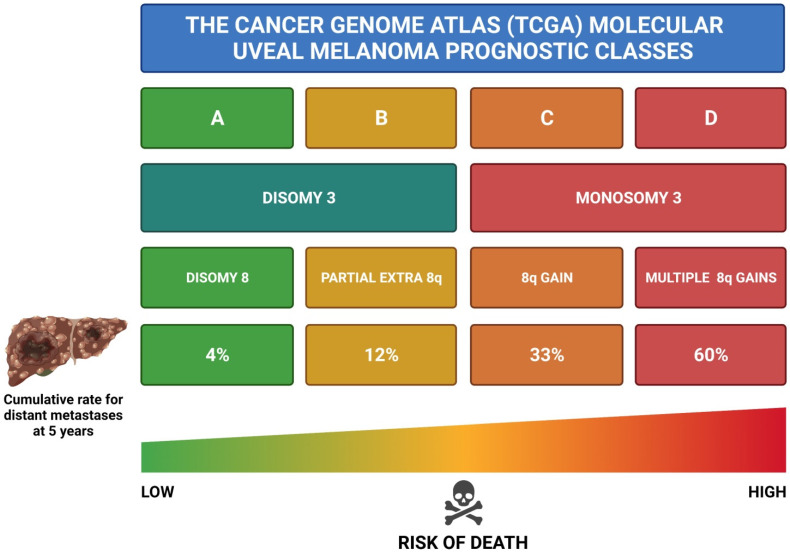
Pioneer cytogenetic studies in the 1990s allowed the identification of important chromosomal abnormalities in UM which influence the prognosis of patients, especially involving chromosomes 1, 3, 6 and 8 [107,108,109]. The most important chromosomal abnormality is M3, which is strongly associated with a higher risk of metastases and, thus, a worse prognosis [40,73,135]. Regarding chromosome 1, total or partial loss of chromosome 1p is also a marker of poor prognosis, irrespective of the presence or absence of M3 [136,137]. As far as chromosome 6 is concerned, the gain of 6p is a robust indicator of good prognosis, since it has a reverse relationship with the metastatic risk [8,138]. On the contrary, the loss of chromosome 6q is correlated with a decreased life expectancy [8,138]. The loss of chromosome 8q is a rare event in UM, while gain of 8q is more common and linked with poor prognosis [8,73]. Interestingly, chromosome 8q gain frequently co-exists with M3 and these patients have the worst prognosis among all (Figure 3) [138,139]. In summary, M3, gain of 8q, loss of 1p and 6q loss are all associated with an inferior prognosis for UM patients [39,138,139]. A novel and more robust molecular prognostic classification of UM is being proposed, which has its backbone on chromosomal abnormalities (Figure 3) [36,40]. The new molecular classification is based on the data gathered from the TCGA project, in which a vast array of 80 UM patients had their primary tumour profiled through a comprehensive analysis involving different molecular methodologies (Figure 3) [39,40]. This new classification comprises four main prognostic classes: class A [D3/Disomy 8 (D8)], class B (D3/partial extra 8q), class C (M3/8q gain) and class D (M3/multiple 8q gains), with progressive increased risk of metastases development and, thus, increased risk of poor prognosis, from class A to class D (Figure 3) [3,36,39,40,73]. This new molecular classification has been demonstrated to be superior to the current gold standard AJCC TNM staging in predicting the risk of metastases and death (Figure 3) [3,36,73,139].
Figure 3.
New molecular prognostic classification for uveal melanoma based on the data generated by the TCGA project involving primary uveal melanoma cases [40]. The new model comprises four main prognostic classes: class A [D3/D8], class B (D3/partial extra 8q), class C (M3/8q gain) and class D (M3/multiple 8q gains). The risk of metastases development increases progressively from class A to class D. Uveal melanoma patients in class D have the least favourable prognosis, with nearly all patients dying within the first decade after diagnosis. Diagram generated in line with previous literature [3,36,39,40,73] (Diagram created with BioRender.com, accessed on 15 December 2021).
The risk of metastatic development for patients with UM can also be predicted using the Gene Expression Profiling (GEP; Castle Biosciences, Phoenix, AZ, USA) of the primary tumour, a commercially available test based on a 15-gene array conducted on a microfluidics quantitative polymerase chain reaction (PCR) platform, which allows accurate UM testing even from small needle biopsy samples [110,111]. A machine learning algorithm is then applied and stratifies UM patients into low metastatic risk (Class 1A), intermediate metastatic risk (Class 1B) and high metastatic risk (Class 2) [111,112,113]. This test has been validated by numerous studies [112,113] and, interestingly, a correlation between class 2 patients and loss of nuclear BAP staining/BAP1 mutation has been found [67,140]. The prognostic accuracy of GEP has been proven to be robust and superior to clinical features, histopathological analysis, TNM staging and evaluation of chromosomal abnormalities [112,141,142].
Worldwide, the usage of GEP and/or chromosomal analysis has been a heterogeneous scenario, with a few centres using both and several centres favouring the usage of one over the other. In centres with less abundance of resources, only the status of BAP1 is tested, through immunohistochemistry, as an indicator of BAP1 mutation and as a surrogate marker for M3. Finally, in a myriad of other centres none of these molecular markers are tested and, thus, UM patient prognostication still relies in classical histomorphological prognostic markers as described above (Table 2).
5. Gene Signatures as Novel Prognostic Biomarkers in Uveal Melanoma
Even though the current therapeutic options are effective in ablating local UM disease, invariably nearly half of the patients will develop metastases in the first decade after the initial diagnosis [9,10]. The ability to accurately predict the patients at high risk of metastases is, thus, of fundamental importance [8,143]. One of the main lines of investigation that the scientific community dedicated to the study of UM has followed is the development of genomic expression signatures of primary UM cases, aiming to find robust ones that can be used to construct reliable prognostic models which can be applied in the follow-up and treatment of patients diagnosed with UM (Table 3). Recently, these efforts were considerably accelerated following the public availability of the clinical and genomic datasets of the TCGA project (http://cancergenome.nih.gov/, accessed on 15 December 2021), in which a vast array of 80 UM patients had their primary tumour profiled [40]; and the datasets within the Gene Expression Omnibus (GEO) database (http://www.ncbi.nlm.nih.gov/geo/, accessed on 15 December 2021), such as GSE22138 (63 UM samples) [144], GSE27831 (29 UM samples) [145], GSE39717 (41 UM samples) [146] and GSE84976 (28 UM samples) [147]. Thus, several UM genomic databases are now available for usage by researchers worldwide, which has helped to significantly leverage genomic research in the UM field (Table 3).
Table 3.
Novel promising prognostic gene signatures in primary uveal melanoma. The novel gene signatures for uveal melanoma described below were published in the past three years.
| Study | Gene Signature | Relevance of the Study |
|---|---|---|
| Wan et al., 2018 [148] | ABTB1, ADPRHL1, NTRK2 and SLC17A7 are hub genes in UM | Important diagnostic and prognostic markers for UM recurrence detection |
| Xue et al., 2019 [149] | AC010442.3, AC023790.2, AC092821.1, AL137784.1, CA12, FABP5P1, FAM189A2, GRIN2A, MGLL, MIR4655, MMP9, PARP8, RNF208, S100A13, SIRT3, TCTN1, ZBED1 and ZNF497 | Early identification of UM patients with poor and good prognosis |
| Ni et al., 2019 [150] | ABHD3, APOM, CALHM2, CENPV, CHAC1, HTR2B, HTRA3, LZTFL1, UBE2W, VCPIP1, ZNF391, ZNF415, ZNF667-AS1 and ZNF835 | Gene signature that allowed prediction of overall survival (OS) and recurrence-free survival (RFS) |
| Choi et al., 2020 [151] | CTNNB1, CYC1, NDUFB9 and NDUFV2 are hub genes in UM | Lower expression of CTNNB1 and increased expression of NDUFB9, NDUFV2 and CYC1 are associated with decreased survival of UM patients |
| Luo et al., 2020 [152] | ANXA2P2, CA12, HMCES, POMGNT2, RNF208, SIRT3, SLC44A3, STPG1, TCTN1 and ULBP1 | High expression of ANXA2P2, CA12 and ULBP1 and a low expression of HMCES, POMGNT2, RNF208, SIRT3, SLC44A3, STPG1 and TCTN1 are associated with higher metastatic risk and a shorter survival |
| Wan et al., 2020 [153] | CREG1, HIST1H4E, LZTS1, NIPA1, SH2D3A and TMEM201 | Low expression of LZTS1 and TMEM201 plus high expression of CREG1, HIST1H4E, NIPA1, SH2D3A are associated with decreased survival of UM patients |
| Tang and Cai, 2021 [154] | EIF1B, MEGF10, PHLDA1, RPL10A, RPL15, SLC25A38, TFDP2 and TIPARP | Robust prediction model of metastases-free survival |
| Jun Liu et al., 2021 [155] | ARPC1B, BTBD6, GUSB, KRTCAP2, RHBDD3 and SLC39A4 | Robust prediction model of OS for UM patients |
In 2018, Wan et al. used the TCGA genomic data involving 10,975 genes from 80 UM patients [148] and performed weighted gene co-expression network analysis (WGCNA) [156,157,158], a popular method frequently employed to ascertain the potential interactions between genes and phenotypes, which has been successfully utilized in studies in neuroscience [159,160,161], cancer [162,163,164,165] and more recently in COVID-19-applied research [166], among other fields [167]. In a simplistic manner, the WGCNA approach transforms the data of gene expression into modules of co-expression, allowing a better understanding of potential signalling pathways that might be strongly linked with phenotypes of interest [158,167]. It is speculated that WGCNA has the important advantage to correlate co-expression modules with clinically relevant traits, perhaps leading to results with a more meaningful biological significance [158,167]. This robust data analysis methodology has also been employed in metabolomics, proteomics and lipidomics studies [168,169]. In the study conducted by Wan et al., using the TCGA data, their WGCNA analysis yielded 21 different and relevant co-expression gene modules in UM [148]. Out of these 21 co-expression modules, four were demonstrated to be correlated with life status of the UM patient, recurrence and recurrence time [148]. The four distinct hub genes identified were ABTB1, ADPRHL1, NTRK2 and SLC17A7 [148]. Given that the four hub genes were basically oncogenes (NTRK2) and genes involved in tumour suppressing pathways (ABTB1, ADPRHL1 and SLC17A7), the authors speculated that they might play a vital role in UM reappearance and, thus, constitute important diagnostic and prognostic markers worth studying for UM recurrence detection [148].
In 2019, Xue et al. used the TCGA genomic data to identify a gene signature that could accurately predict the prognosis of UM patients through a methodology involving glmnet COX model and COX regression analysis [149]. After initially identifying 4388 genes with significant prognostic significance in the 80 UM samples included in the TCGA cohort, they developed a robust model involving 18 genes (AC010442.3, AC023790.2, AC092821.1, AL137784.1, CA12, FABP5P1, FAM189A2, GRIN2A, MGLL, MIR4655, MMP9, PARP8, RNF208, S100A13, SIRT3, TCTN1, ZBED1 and ZNF497), which allowed the early identification of UM patients with poor and good prognosis [149]. The Kaplan–Meier overall survival (OS) curves of the 18 selected genes prognostic genes showed that high expression of AC092821.1, FAM189A2, RNF208, SIRT3, TCTN1, ZBED1 and ZNF497, as well as lower expression of the genes AC010442.3, AC023790.2, AL137784.1, CA12, FABP5P1, GRIN2A, MGLL, MIR4655, PARP8 and S100A13 were positively associated with OS in UM patients; meanwhile, the MMP9 expression levels had no significant influence in the survival of poor and good prognosis patients [149]. Later, the Gene Set Enrichment Analysis (GSEA) allowed the identification, among others, of an enriched p53 signalling pathway in the high risk UM group [149], in line with previous pioneer studies establishing that p53 expression in UM cases tends to be correlated with an unfavourable outcome [170].
In 2019, Ni et al. used the TCGA mRNA expression data and performed WGCNA among other complex analytic methods on a group of 5000 genes, which permitted the generation of potential modules involving co-expressed genes and then correlated those modules with clinical and pathological relevant features [150]. The authors were able to find a selection of groups of genes whose expression was associated with tumour-free survival (ABHD3, APOM, CALHM2, CENPV, CHAC1, HTR2B, HTRA3, LZTFL1, UBE2W, VCPIP1, ZNF391, ZNF415, ZNF667-AS1 and ZNF835) and metastasis status (ABHD3, APOM, ARFGEF1, CALHM2, CHAC1, CENPV, DLL4, HTR2B, LZTFL1, MTUS1, NF835, SLC25A26, UBE2V2, UBE2W, VCPIP1, ZNF391, ZNF415 and ZNF-667-AS1) [150]. Using a Least Absolute Shrinkage and Selection Operator (LASSO) cox regression model, a 14 validated hub-gene model (ABHD3, APOM, CALHM2, CENPV, CHAC1, HTR2B, HTRA3, LZTFL1, UBE2W, VCPIP1, ZNF391, ZNF415, ZNF667-AS1 and ZNF835) was used to build signatures for prediction of OS and recurrence-free survival (RFS), which were later externally validated using the GEO dataset (GSE27831), in which equivalent results were obtained [150]. The authors demonstrated that in comparison to other robust clinicopathological prognostic parameters, such as TNM classification, chromosomal status or LBD; their 14-gene risk model was superior in predicting OS and RFS [150]. For example, a recent in vitro study involving UM cell lines showed that CHAC1 downregulation significantly decreased the proliferation and mobility of UM cells [171]. Another interesting piece of data arising from the Ni et al. study was that the KEGG pathway analysis mainly identified pathways related with immune regulation, showing that chromosome 6p gain and chromosome 8q gain, which are associated with reduced UM survival, could have a correlation with a dysfunctional immune system in UM patients, leading to a worse prognosis [150].
In their study, Choi et al. used the TCGA and GEO data (GSE22138 and GSE39717) cohorts and included only patients who died of UM and excluded patients without information on survival status [151]. In a universe of 159 UM patients [TCGA (n = 67); GSE22138 (n = 63) and GSE39717 (n = 29)], the authors used Kaplan–Meier survival analysis with log-rank test to identify genes of prognostic significance that were common among the three distinct cohorts of UM patients [151]. An initial array of 14 genes that had low expression and 37 genes that high expression was identified as being associated with dismal prognosis [151]. Subsequently, a complex protein-protein analysis was performed, demonstrating that three oncogene-like genes (CYC1, NDUFB9 and NDUFV2) and one tumour suppressor-like gene (CTNNB1) were main hub genes and significant molecular predictors in UM [151]. Across the three independent cohorts, high expression of CYC1, NDUFB9 and NDUFV2, as well as low expression of CTNNB1 were systematically associated with decreased survival of UM patients [151]. For example, CTNNB1 is the gene encoding for β-catenin and the deregulation of the WNT/CTNNB1 (β-catenin) pathway is a well-established event in the carcinogenic process in several neoplasias, including colorectal cancer [172,173,174], hepatocellular carcinoma [175,176,177] and cutaneous melanoma [178,179,180], among others.
In 2020, Luo et al. used the TCGA cohort gene data of 80 UM patients to develop a 10-gene signature based model for UM prognosis, which was later validated using the GSE22138 data, which includes a group of 63 UM patients [152]. Kaplan–Meier survival analysis and univariate COX regression models were initially employed to screen for genes with prognostic value [152]. Afterwards, COX regression analysis coupled with LASSO methodology was used to achieve the minimum 10-gene prognostic (metastases-free survival) signature, which includes the following genes: ANXA2P2, CA12, HMCES, POMGNT2, RNF208, SIRT3, SLC44A3, STPG1, TCTN1 and ULBP1 [152]. In patients classified has having high-risk score and, thus, shorter survival, they observed a high expression of ANXA2P2, CA12 and ULBP1 and a low expression of HMCES, POMGNT2, RNF208, SIRT3, SLC44A3, STPG1 and TCTN1 [152]. This 10-gene signature also robustly predicted metastases-free survival (MFS) in the validation GSE22138 cohort [152]. Besides this, the 10-gene risk model was superior in predicting OS when compared to the normally used clinical prognostic parameters, such as TNM classification or LBD [152]. Furthermore, when correlated with UM chromosomal abnormalities, the 10-gene risk model proposed by Luo et al. was shown to have a positive correlation with chromosome 8q copy number and a negative correlation with chromosome 3, 6q and 6p copy numbers [152]. In the high-risk group, the GSEA analysis showed a gene set enrichment in pathways related with immune response, inflammatory response, p53 signalling, proteasome and natural killer cells, among others [152]. This pointed towards a close relationship with tumour microenvironment, which is a theme of increasing interest in UM, given its relevance in UM carcinogenesis and potential therapeutic strategies (please see Section 8) [152].
In 2020, Wan et al. proposed an even more reduced gene signature model for UM prognostication, which encompasses only six genes (CREG1, HIST1H4E, LZTS1, NIPA1, SH2D3A and TMEM201), with multivariate analysis showing it to be a 5-year independent prognostic factor for OS [153]. In brief, the authors used the genomic information of 80 UM patients in the TCGA database and randomly created two datasets [dataset 1 (n = 39 patients) and dataset 2 (n = 41 patients)] for internal validation [153]. Univariate COX regression analysis allowed the identification of 2010 survival related genes out of a universe of 15,187 genes [153]. Gene functional analysis demonstrated that the identified genes were predominantly connected with mRNA processing, RNA splicing, spliceosome and proteolysis mediated by ubiquitin [153]. A robust likelihood-based survival model methodology was later employed to define the 6-gene signature (CREG1, HIST1H4E, LZTS1, NIPA1, SH2D3A and TMEM201) [153]. High expression of CREG1, HIST1H4E, NIPA1, SH2D3A, as well as low expression of LZTS1 and TMEM201 were demonstrated to be significantly associated with decreased lifetime for UM patients [153]. These results and, thus, the ability of the 6-gene signature to predict 5-year OS in UM patients was also externally validated using two GEO datasets (GSE42656 and GSE84976) [153].
Recently, Tang and Cai generated a model for UM prognosis prediction based on the data of the gene expression microarray GEO data set GSE22138, which comprised a cohort of 63 patients UM patients [154]. Initially, they used WGCNA and identified 41 hub genes that are associated with UM metastases [154]. Afterwards, they applied a LASSO COX regression methodology to identify relevant genes and build a gene expression signature with prognostic significance, which comprises eight genes (EIF1B, MEGF10, PHLDA1, RPL10A, RPL15, SLC25A38, TFDP2 and TIPARP) and named Uveal Melanoma Metastasis Prediction Score (UMPS) [154]. The individual coefficient by LASSO COX regression of RPL10A was demonstrated to be associated with a high risk of metastases, whereas the remainder seven genes were shown to be protective [154]. GSEA analysis showed that the high-risk of metastasis group was associated with complement, E2F targets, G2M checkpoints and unfolded protein response pathways, while no differences in the immune cell proportions were registered between low and high risk groups [154]. The UMPS model was later externally validated using the 80-patient TCGA cohort and the 29-patient GSE27831 cohort of UM patients [154]. The eight-gene expression signature UMPS model was not only able to predict MFS, but was also able to significantly increase the 3-year and 5-year disease-free survival (DFS) prediction accuracy of currently established clinical predictors, such as the AJCC TNM staging [154].
Finally, in a recently published study, Jun Liu et al. proposed a novel six-gene based signature (ARPC1B, BTBD6, GUSB, KRTCAP2, RHBDD3 and SLC39A4) for survival prediction and risk stratification in UM [155]. In brief, using the TCGA database, they initially found that glycolysis and immune response were the most relevant hallmarks for UM related survival [155]. Subsequently, they employed WGCNA, Cox regression analyses and a LASSO algorithm to identify significant hub genes related to glycolysis and immune response, which were used to build the risk model to predict OS of UM patients [155]. The TCGA database constituted the training dataset, while the GEO databases GSE22138 and GSE84976 were used to validate the newly developed prognostic model [155]. Survival analysis demonstrated that the OS of the group with high glycolysis and high immune response Z-scores was lower comparatively to the group with low glycolysis and low immune response Z-scores, respectively [155]. Regarding the immune profile, a higher infiltration of B cells, CD4+ T cells and monocytes was evident in the low-risk group, while the high-risk group had high infiltration by M2-macrophages and myeloid dendritic cells [155]. Their six-gene signature was shown to be an independent and robust prognostic predictor of OS for UM patients [155]. Indeed, ROC curve analysis revealed an AUC above 0.9 for 5-year survival prediction, further validating the six-gene signature as a good model for forecasting the survival of UM patients [155]. Albeit using only six genes, the model was demonstrated to be non-inferior to the 10-gene signature developed by Luo et al. described above for predicting OS [155]. A nomogram based on the six-gene signature was established and might constitute soon, after rigorous validation, a useful tool to develop a personalized therapeutic approach for UM patients [155].
6. Immunohistochemistry-Based Novel Prognostic Biomarkers in Uveal Melanoma
Immunohistochemistry is a powerful laboratory technique that has revolutionized Anatomic Pathology over the past decades [181,182]. It is a relatively affordable method to evaluate protein expression and it is readily available and reproducible in most laboratories worldwide [182]. Similarly to other fields within Pathology, researchers in Ocular Pathology have aimed to find protein markers that can be studied through IHC and that can be of prognostic relevance: as previously mentioned, BAP1 is a good example of such marker [140,183]. In the past three years, approximately 20 novel IHC-based prognostic biomarkers in UM have emerged in the literature (Table 4). A review of these biomarkers and respective research in UM is presented below (Table 4).
Table 4.
Novel promising prognostic immunohistochemistry-based biomarkers in primary uveal melanoma. The new prognostic markers for uveal melanoma highlighted below were published in the past three years.
| Protein | Function | Relevant Conclusions of the Study |
|---|---|---|
|
ABCB5 (ATP-binding cassette sub-family B member 5) [184] |
P-glycoprotein involved in the transport of molecules across membranes Cancer stem cell marker |
Higher expression of ABCB5 is associated with metastases development and worse prognosis |
| Adiponectin [185] | Anti-carcinogenic and insulin-sensitizing actions | Expression of Adiponectin and its receptor Adipor1 was decreased in cases of UM with M3, suggesting that the lower levels of adiponectin could boost the metastatic potential of UM |
|
ATR (ataxia telangiectasia and Rad3-related) [186] |
Member of the DNA damage response (DDR) protein machinery | Loss of nuclear ATR is associated with well-established markers of poor prognosis in UM (epithelioid cell morphology, increased tumour thickness, higher number of mitotic figures and BAP1 loss) |
|
ATM (ataxia-telangiectasia mutated) [187] |
Member of the DNA damage response (DDR) protein machinery | Loss of nuclear ATM is associated with well-established markers of poor prognosis in UM (epithelioid cell morphology, large tumour diameter above 10 mm, TILs and nuclear BAP1 loss) and a significant shorter DFS |
| Beclin-1 [188] | Protein involved in autophagy | Higher expression of Beclin-1 was correlated with a decreased risk of metastases and increased DFS times |
|
BNIP3 (BCL2 19 kD protein-interacting protein 3) [189] |
Mitochondrial protein involved in regulation of cell death, autophagy and cellular protection | Higher expression of BNIP3 was correlated with a shorter survival |
|
BTNL9 (Butyrophilin-like protein 9) [190] |
Modulator of T-cell mediated immune function | Higher expression of BTNL9 was significantly correlated with a better OS |
| c-Rel [191] | Member of the NF-κB pathway, which regulates a large array of genes implicated in cell survival, inflammatory disorders, response to infection, autoimmune disorders and cancer, among other processes | Nuclear expression of c-Rel expression was significantly associated with inferior survival |
|
EphA1 (Eph-A1 receptor, erythropoietin-producing human hepatocellular receptor A1) [192] |
Member of the Ephrin receptors, which are receptor tyrosine kinases (RTKs) that play a myriad of roles during the embryonic development (for example, in axon guidance, cell migration, segmentation and formation of tissue boundaries) and adulthood (for example, in angiogenesis, stem cell differentiation, regulation of the immune system and in cancer development) | Lower expression of EphA1 is associated with a worse prognosis |
|
EphA5 (Eph-A5 receptor, erythropoietin-producing human hepatocellular receptor A5) [192] |
Member of the Ephrin receptors, which are receptor tyrosine kinases (RTKs) that play a myriad of roles during the embryonic development (for example, in axon guidance, cell migration, segmentation and formation of tissue boundaries) and adulthood (for example, in angiogenesis, stem cell differentiation, regulation of the immune system and in cancer development) | Lower expression of EphA5 is associated with a worse prognosis |
|
HDAC-2 (Histone Deacetylase 2) [193] |
Regulation cellular proliferation, differentiation, angiogenesis and cell death, being implicated in neurodegeneration and cancer | Higher expression of HDAC-2 is an independent factor of better survival in UM |
| Nestin [194] | Intermediate filament protein marker of stem cells in the central nervous system and a cancer stem cell marker | Correlation between nestin positivity and well-established markers of bad prognosis (epithelioid cell morphology, higher mitotic counts, M3 and chromosome 8q gain) Nestin positivity in UM is associated with a worse prognosis |
| p50 [195] | Member of the NF-κB pathway, which regulates a large array of genes implicated in cell survival, inflammatory disorders, response to infection, autoimmune disorders and cancer, among other processes | Nuclear immunoreactivity of p50 significantly correlated with metastases development |
| p52 [196] | Member of the NF-κB pathway, which regulates a large array of genes implicated in cell survival, inflammatory disorders, response to infection, autoimmune disorders and cancer, among other processes | Expression of p52 was associated with BAP1 loss Higher p52 expression was associated with worse MFS and OS |
| p65 [195] | Member of the NF-κB pathway, which regulates a large array of genes implicated in cell survival, inflammatory disorders, response to infection, autoimmune disorders and cancer, among other processes | Nuclear immunoreactivity of p65 significantly correlated with metastases development |
|
PARP1 [Poly(ADP-ribose) polymerase 1)] [197] |
Involved in DNA repair and programmed cell death | Higher expression of PARP-1 is associated with decreased DFS and OS |
|
PD-1 (Programmed cell death receptor-1) [198] |
Involved in immune regulation | High expression of PD-1 in UM cells is associated with decreased DFS and OS |
|
PD-L1 (Programmed cell death-ligand 1) [199] |
Involved in immune regulation | PD-L1 immunoexpression was a significant prognostic factor of a reduced DFS |
|
PLK-1 (Polio-like kinase 1) [200] |
Kinase involved in the regulation of cell cycle | Low expression of PLK-1 was correlated with a higher TNM staging and a significantly decreased OS |
|
PRDX3 (thioredoxin-dependent peroxidase reductase) [201] |
Mitochondria protein with a fundamental role in the antioxidant defence of the cell | High PRDX3 expression is correlated with metastatic disease development and reduced OS |
| RelB [196] | Member of the NF-κB pathway, which regulates a large array of genes implicated in cell survival, inflammatory disorders, response to infection, autoimmune disorders and cancer, among other processes | Expression of RelB was associated with BAP1 loss and with inferior MFS |
|
SPANX-C (Sperm protein associated with the nucleus on the X chromosome protein C) [202] |
Belongs to a family of proteins expressed in the testis during spermatogenesis | Higher expression of SPANX-C in primary UM is associated with a decreased MFS |
ATP-binding cassette sub-family B member 5 (ABCB5) is a P-glycoprotein actively engaged in the transport of a myriad of molecules across membranes, including anti-neoplastic molecules [203,204]. ABCB5 is a marker of cancer stem cells and its expression was found increased in different types of neoplasias, including colon cancer [205], cutaneous melanoma [206,207], hepatocellular carcinoma [208] and Merkel cell carcinoma [209]. It is a molecule demonstrated to be implicated in the neoplastic transformation process, tumour expansion and invasiveness [205,207]. For example, in cutaneous melanoma ABCB5 was shown to promote neoplastic invasion and distant metastases through the NF-kB pathway, in a process likely mediated through MMP9, which is involved in cancer invasion and metastasis [207]. In addition, ABCB5 is involved in processes that lead to the resistance of cancer cells to anti-neoplastic agents [204,210]. The expression of ABCB5 was recently evaluated in 32 primary UM cases without associated metastases and 23 primary UM cases with metastases [184]. A higher expression of ABCB5 was observed in the primary UM cases associated with metastases and the authors also showed that these higher levels were correlated with a shorter time to metastases development and, thus, a worse prognosis [184]. Future studies are needed to better understand the role of ABCB5 in UM, its prognostic value and its potential as a therapeutic target.
In the past couple of years, a great interest has been devoted to the expression of Adiponectin in UM, which is a hormone encoded by a gene in chromosome 3, possessing anti-carcinogenic and insulin-sensitizing actions [185]. Tura et al. showed recently that immunoreactivity of Adiponectin and its receptor Adipor1 was decreased in UM cases with M3, suggesting that the lower levels of adiponectin could boost the metastatic potential of UM with that chromosomal abnormality and curb tumour dormancy [185]. Ultimately, adiponectin could be used as a prognostic marker in UM and a potential increase in serum adiponectin levels could be explored as a possible therapy to delay the onset of metastases in UM patients [185]. Interestingly, there was no difference in BAP1 expression between UM cases with low or high levels of Adiponectin and Adipor1 [185].
The role of DDR protein machinery in UM pathobiology remains to be established. The nuclear expression of the ataxia telangiectasia and Rad3-related (ATR) protein, a member of the family of DDR proteins which is encoded in a gene in chromosome 3, similarly to BAP1, was recently evaluated in 69 UM cases [186]. A loss of nuclear ATR expression was documented in nearly 75% of the cases, which was associated with an epithelioid UM cell morphology, increased tumour thickness, increased number of mitotic figures and loss of nuclear BAP1 expression, which are all well-established markers of poor prognosis in UM (Table 2) [186]. This led the authors to conclude that ATR could constitute a novel potential prognostic marker and therapeutic target in UM [186].
Another DDR protein whose expression was recently evaluated in UM is ataxia-telangiectasia mutated (ATM) protein, in a study conducted in 69 UM samples [187]. A loss of nuclear expression of ATM was observed in nearly 65% of the cases and it was significantly correlated with an epithelioid morphology of the UM cells, large tumour diameter above 10 mm, presence of TILs and nuclear BAP1 loss [187]. In addition, patients with absence of nuclear ATM expression had a significant shorter DFS, suggesting that nuclear ATM could constitute a novel biomarker of increased metastatic risk in UM [187]. The correlation between nuclear ATM expression loss with shorter OS could not be established since death was only documented in 2 out of the 69 patients involved in the study [187]. The loss of ATM expression has been observed in other cancer types, namely, breast [211], colon [212] or lung cancers [213], being a strong indicator of a dismal prognosis. Interestingly, the TCGA study showed that DDR proteins were in general upregulated in UM cases with M3 and BAP1 mutations, comparatively to cases preserving two copies of chromosome 3 and harbouring SF3B1 mutations [40].
Autophagy is a natural, homeostatic and complex multi-step cellular process through which the cell eliminates dysfunctional or superfluous components, including lipids, nucleic acids, proteins or organelles, through a lysosome-dependent regulated mechanism [214,215]. Thus, it is fundamental for the orderly degradation and recycling of cellular components, being instrumental for adequate cellular differentiation and survival, as well as tissue development [214,215,216]. Autophagy has a dual role in cancer, since it is important in tumour suppression in early states of the neoplastic development process, while in more advanced neoplastic states it is upregulated leading to a pro-survival and tumourigenic effect in neoplastic cells, enhanced proliferation and metastases [216,217,218]. The role of autophagy in UM development is poorly understood. Recently, the expression of three proteins [autophagy-related gene 7 (ATG7), Beclin-1 and p62] belonging to the vast family of proteins involved in autophagy was assessed through IHC in a cohort of 85 cases of primary UM [188]. Higher expression of Beclin-1 was correlated with a decreased risk of metastases and extended DFS times, establishing Beclin-1 as a significant positive prognostic factor in UM [188]. Contrarily, the expression of ATG7 and p62 did not impact significantly on the prognosis of UM patients [188]. Together, these results open novel avenues towards the evaluation of autophagy-related molecules as prognostic factors in UM and also as potential innovative therapeutic strategies.
BCL2 19 kD protein-interacting protein 3 (BNIP3) is a mitochondrial protein belonging to the BCL-2 family, which has been demonstrated to be involved in the complex regulation of cell death, autophagy and cellular protection [219,220]. Regulation of BNIP3 levels has been implicated in different types of neoplasias, namely, breast cancer [221], lung cancer [222], salivary adenoid cystic carcinoma [223] and skin melanoma [224], being associated with progression of the disease and prognosis. In a recent study, the expression of BNIP3 was evaluated through IHC in a cohort of 47 primary UM cases and the authors demonstrated that higher levels of BNIP3 were correlated with a shorter survival [189]. Given that BNIP3 has both cell death and cell survival promoting effects, novel studies will be needed to elucidate the role of this marker in UM.
Butyrophilin (BTN) and butyrophilin-like (BTNL) family of proteins are structurally related with B7-molecules and like-B7 molecules, being all critical in the modulation of T-cell mediated immune function [225,226]. Even though our knowledge on the regulation of T-cells by BTN and BTNL proteins is still scarce, they appear to be involved in inflammatory diseases and cancer [225,226]. The mRNA expression of BTNL9, one member of the family, was demonstrated to be low in colon cancer comparatively to normal colon [225]. In addition, in a recent study, researchers took advantage of the TCGA database and verified that the expression of BTNL9 was downregulated in breast cancer [226]. The lower expression of BTNL9 in breast cancer was significantly correlated with a worse DFS and OS [226]. Later, by studying breast cancer cell lines they demonstrated that BTNL9 might have an anti-cancer role in breast cancer by inhibiting proliferation and metastasis [226]. A more recent study on breast cancer, involving a multiomics approach, also showed that higher mRNA levels of BTNL9 and of other family members in the BTN/BTNL family were associated with a more favourable DFS and extended OS [227]. The expression of BTNL9 was also recently evaluated in a cohort of 62 primary UM cases [190]. A higher expression of BTNL9 was significantly correlated with a better OS, suggesting that BTNL9 is a marker of good prognosis in UM [190]. This study has opened the prospect of modulating BTNL9 expression as a possible therapeutic option for UM. Comprehensive studies are needed to better understand the role of BTNL9 expression in UM, as well as the possible interplay between BTNL9 expression in UM cells and immune regulation.
The expression of Ephrin receptors has been studied in different tumours with data indicating that they might have an important role as prognostic factors [228,229]. They constitute the largest known subfamily of receptor tyrosine kinases (RTKs), which play critical roles during the embryonic development, such as axon guidance, cell migration, segmentation and formation of tissue boundaries [230,231,232,233]. In addition, during adulthood, they have roles in angiogenesis, stem cell differentiation, immune system regulation and in cancer development, among others [228,229]. Our knowledge on the expression of Ephrin receptors in UM expanded recently with a study where the expression of EphA1, EphA5 and EphA7 was evaluated in 94 UM enucleation samples without previous treatment [192]. A decreased expression of EphA1 and EphA5 was associated with a worse prognosis for UM patients, while a prognostic role could not be firmly established for EphA7 expression [192]. Indeed, a smaller tumour size, decreased mitotic activity and absence of extrascleral extension were positively correlated with increased EphA1 expression, whereas higher EphA5 expression was linked to absence of metastases and decreased likelihood of chromosome 3 loss [192]. This study established that EphA1 and EphA5 are potentially important prognostic markers in UM patients and also opened the prospect of using small molecules addressing the Eph/ephrin signalling as candidate therapies for UM [192,234].
Histone Deacetylases (HDACs) are known to have fundamental roles in the regulation of cellular proliferation, differentiation, angiogenesis and cell death, being implicated in neurodegeneration [235,236] and different forms of cancer, including lung cancer [237,238], skin melanoma [239] and lymphoma [240], among others. Consequently, HDAC inhibitors have constituted promising anti-neurodegeneration and anti-cancer therapies [241,242]. The prognostic significance of HDAC expression in UM was recently evaluated in a study involving 75 UM cases [193]. In line with previous studies, which confirmed HDAC gene [243,244] and protein [245] expression in UM, the authors evaluated HDAC-1, HDAC-2, HDAC-4 and HDAC-6 through IHC and aimed to determine their role as prognostic factors [193]. HDAC-1 and HDAC-2 had both nuclear and cytoplasmic expression, whereas HDAC-4 and HDAC-6 were mostly expressed in the cytoplasm of UM cells [193]. Among the four studied HDACs isoforms, HDAC-2 was the most frequently expressed, with a more significant nuclear expression pattern, and the expression of HDAC-2 the only proven to be an independent factor of better survival in UM [193]. This study provides additional evidence on the potential role of HDACs in UM development and progression, suggesting that inhibition of HDAC could constitute a relevant therapeutic strategy [241]. In a recent phase 2 clinical trial involving 28 patients with metastatic UM, Entinostat (HDAC inhibitor small molecule) was tested combined with Pembrolizumab (inhibitor of PD-1) [246]. Encouraging positive responses in terms of progression-free survival (PFS) and OS were observed in a well-defined subset of mestastic UM patients, namely, patients with BAP1-preserved tumours and one patient with iris melanoma containing a UV-related gene signature [246]. There is an ongoing phase 2 clinical trial in metastatic UM involving the HDAC inhibitor Vorinostat as monotherapy (ClinicalTrials.gov: NCT01587352), which will give us important pilot data on the efficacy of this therapeutic avenue in UM.
Nestin is a well-known intermediate filament protein family member, constituting a putative marker of stem cells in the CNS [247,248], an established cancer stem cell marker [249,250] and a prognostic marker in different tumours, including breast cancer [251], colorectal cancer [252] and lung cancer [253], among others. In fact, the increased expression of nestin in these tumours was associated with an immature stem-cell like phenotype, chemoresistance and enhanced capacity for invasiveness [250,254]. Recently, the team of Sarah Coupland studied the expression of nestin in 141 cases of primary UM and found a correlation between nestin positivity (defined as expression above a cut-off value of ≥10% positively stained UM cells) and well-established factors of bad prognosis in UM, such as epithelioid morphology, higher mitotic counts, M3 and chromosome 8q gain [194]. Besides this, the Kaplan–Meier survival analysis also confirmed that primary UM cases displaying nestin positivity had a worse survival comparatively to nestin-negative cases [194], a finding that has also been corroborated by nestin expression analysis in the TCGA cohort by the same research group [255]. The expression of nestin in UM metastases was also studied and expression of the marker was consistently found in nearly 80% of the cases [194]. Interestingly, the expression of nestin was not observed in the normal choroidal melanocytes, which suggests that in line with other cancer types, the tumourigenic process in UM might involve transformation into a more immature/stem-cell-like phenotype [194]. Together, these results show that high expression of nestin is associated with a more aggressive UM phenotype, displaying enhanced capacity for development of metastases and a significantly decreased survival after diagnosis [194].
The NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) comprises a family of transcription factors that finely regulate a large array of genes involved in cell survival, inflammatory disorders, response to infection, autoimmune disorders and cancer, among other processes [256,257,258]. Five main structurally related members compose that family: p50 (also named NF-κB1), p52 (also named NF-κB2), p65 (also named RelA), RelB and c-Rel [257,258]. A family of inhibitory proteins normally sequesters the different NF-κB proteins in the cytoplasm [257,258]. The adequate activation of the major NF-κB pathway involves two major signalling pathways, the canonical and non-canonical (or alternative) pathways, both being instrumental to regulate the cellular processes governed by NF-κB [256,259]. In the past two decades our knowledge on the NF-κB pathway has considerably expanded, positioning this pathway as an instrumental orchestrator in the regulation of inflammation and in the development of different tumours, including UM [257,260,261]. Using IHC, in 75 UM cases, Singh et al. evaluated the expression of p52 and RelB members of the NF-κB family [196]. They showed that the expression of p52 and RelB was associated with BAP1 loss [196]. Furthermore, in metastatic cases with LBD above 15 mm, tumour thickness exceeding 8 mm and higher tumour staging, the expression of p52 and RelB was significantly increased [196]. The MFS time was decreased in cases positive for p52, RelB, and p52/RelB co-expression [196]. Cases with higher p52 expression and p52/RelB co-expression had worst OS [196]. In another study, they evaluated the expression of three members of the canonical NF-κB pathway in UM: p50, p65 and c-Rel [195]. Nuclear immunoreactivity of p65, p50, and c-Rel significantly correlated with well-established prognostic factors, such as, LBD > 12 mm, tumour height > 8 mm, microvascular density, TILs, TIMs and, more importantly, metastases development [195]. The presence of nuclear p50 and p65 immunorreactivity was associated with a lower survival for UM patients, while the expression of c-Rel was not shown to impact on the OS [195]. The multivariate analysis later established nuclear p50 and p65 expression as independent UM prognostic factors [195]. Interestingly, in a subsequent study, the expression of c-Rel was assessed in 75 UM cases [191]. Nuclear expression of the c-Rel protein, which suggests NF-κB activation, was observed in 56% of the studied UM cases [191]. The nuclear expression of c-Rel was significantly correlated with an epithelioid UM cell morphology, invasion of the ciliary body and iris, as well as scleral invasion [191]. In line with this, patients with nuclear c-Rel expression had an inferior survival [191]. Together, these results show that different proteins in the NF-κB pathway can constitute novel prognostic factors in UM and that promising novel anti-neoplastic approaches in UM might be explored through regulation of this pathway.
Poly(ADP-ribose) polymerases (PARP) constitute an important protein family with fundamental roles in different cellular processes, including DNA repair and programmed cell death, being implicated in cancer development and therapy [262,263]. One of the most extensively studied members of this family is PARP-1, whose expression in UM was recently evaluated through IHC in a study involving 91 enucleation samples [197]. An increased tumour size, higher histopathological grade and higher chromosome 3 loss frequency were significantly correlated with increased expression of PARP-1 [197]. Furthermore, smaller DFS and OS were associated with higher expression of PARP-1, suggesting that this protein could constitute a novel relevant biomarker of poor prognosis in UM [197] and that PARP inhibitory therapies could be evaluated in UM treatment [264].
Immune checkpoint inhibitor therapies have successfully revolutionized the landscape of therapeutic weapons in different types of cancer, namely, lung cancer [265], skin melanoma [266], head and neck cancer [267], among others, and is being envisioned as one of the current most promising strategies to tackle cancer. Programmed cell death receptor-1 (PD-1), one of the best studied and most advanced immune checkpoint inhibition targets, is expressed in lymphocytes (T and B cells), macrophages and natural killer cells and their effector function is halted when it binds its co-ligands programmed cell death-ligand 1 (PD-L1) and programmed cell death-ligand 2 (PD-L2), which are expressed in contacting cells, including antigen-presenting cells, regulatory T-cells and neoplastic cells [268,269]. However, the expression of PD-1 has also been documented in human melanoma cells, even in the absence of a tumour microenvironment, leading to enhancement of tumour growth [270]. Our understanding of the role of immunotherapy in UM is still in its infancy, especially since the blockade of the PD-1/PD-L1 axis has not yielded significant results in this type of tumour [271,272,273] (please see Section 8). The expression of PD-1 in UM was recently evaluated through IHC in a tissue microarray cohort of 82 primary UM cases [198]. Patients with a high expression of PD-1 in the tumoural cells had a smaller DFS and decreased OS [198]. In the same study, the author overexpressed PD-1 in UM cell lines and found that cells had an enhanced proliferative capacity, which was halted when PD-1 expression was downregulated using shRNA [198]. However, in the hands of others [199] and in our hands (data not shown), PD-1 expression in primary UM cases, through IHC, has not been observed, being only present in infiltrating inflammatory cells. In a subsequent study, Singh et al. evaluated the expression of PD-1 and PD-L1 in 71 UM cases [199]. They observed expression of PD-1 in TILs in 30/71 cases, while PD-L1 was expressed mostly in UM cells in 44/71 cases [199]. In the multivariate analysis, PD-1 and PD-L1 immunoexpression were shown to be significant prognostic factors of a reduced DFS [199]. However, in this cohort, patients without TILs displaying PD-L1 expression had an extended DFS and, thus, a better prognosis [199]. This data is in accordance with an earlier study involving 67 primary UM cases, in which PD-L1 expression in more than 5% of tumoural cells was associated with lower number of TILs and a lengthier MFS [274]. Interestingly, expression of PD-L1 in immune infiltrating cells did not significantly impact on the prognosis of the studied cohort [274]. On the multivariate analysis, the UM patient sub-group with PD-L1 expression in more than 5% of UM cells and in immune cells infiltrating the UM had a longer period free of metastasis and, thus, a less adverse prognosis [274]. These results suggest that PD-L1 expression in UM could signal a more positive outcome [274]. Novel studies are needed to further elucidate the role of PD-1/PD-L1 axis in UM development and metastization, as well as to optimize supplementary strategies to turn checkpoint inhibition into an effective therapeutic strategy for UM (please see Section 8).
Polio-like kinase 1 (PLK-1) expression in UM was also recently reported [200]. PLK-1 is a conserved kinase mainly involved in the regulation of cell cycle [275,276,277] and increased expression of PLK-1 was described in breast cancer [278], lung cancer [279] and lymphoma [280], among others, and is being considered a potential molecular target in anti-cancer therapies [281,282]. Berus et al. performed IHC for PLK-1 in 158 UM cases and found that 30% of the tumours had low expression of PLK-1, which was correlated with a higher TNM staging and, thus, a significantly decreased OS [200]. A firm correlation between PLK-1 levels and DFS could not be determined in this study [200]. Even though, contrarily to what was described in other tumours, lower expression of PLK-1 seems to point towards a decreased life expectancy in UM patients [200].
The thioredoxin-dependent peroxidase reductase (PRDX3) is an enzyme localized in the mitochondria which has a fundamental role in the antioxidant defence of cells [283,284]. The enhanced expression of PRDX3 has been reported in different types of cancers [283], but its expression in UM was only recently unravelled [201]. PRDX3 IHC was performed in tissue microarrays of 92 UM samples. A significant strong correlation between high PRDX3 expression and metastatic disease development and reduced OS was demonstrated, proposing that high PRDX3 expression in UM is also a marker of poor prognosis [201].
Sperm proteins associated with the nucleus on the X chromosome (SPANX) family members (SPANX-A, -B, -C and -D) are normally expressed in the testis during spermatogenesis [285,286,287]. Interestingly, numerous studies also demonstrated the involvement of SPANX proteins in cancer development, namely, in breast cancer [288] and cutaneous melanoma [289,290], among others. The role of this protein in cancer development remains to be firmly understood, but the available studies suggest a role in promoting cancer growth and invasiveness [288,289,290]. The expression of SPANX-C was also recently evaluated in 55 primary UM cases [202]. The research team demonstrated a higher expression of SPANX-C in UM that had developed metastases [202]. In addition, patients with a higher expression of SPANX-C in the primary tumour had a decreased MFS [202]. Thus, higher levels of SPANX-C in UM could constitute a new marker of dismal prognosis [202].
7. Additional Novel Promising Molecular Biomarkers in Uveal Melanoma with Prognostic Relevance
Comprehensive proteomic analysis has started to contribute to better define the prognosis of UM patients. The largest study involving proteomic analysis of primary UM patients using a LC MS/MS iTRAQ methodology was unveiled recently, involving 53 metastasizing and 47 non-metastasizing cases [291]. In all studied cases, nearly 3935 different proteins were evaluated and bioinformatics analyses allowed the identification of 191 differentially expressed proteins elevated in metastatic cases and 211 differentially expressed proteins elevated in non-metastatic cases [291]. Reactome pathway analysis of proteins preferentially elevated in metastatic UM showed mostly an overrepresentation of immune system pathways, but also pathways associated with vesicle-mediated trafficking, extracellular matrix organization, metabolism of proteins and homeostasis [291]. On the other hand, in non-metastatic cases, the authors demonstrated a preponderance of pathways connected with metabolism, but also cellular response to external stimuli and developmental biology [291]. Interestingly, the over-representation of proteins of the immune system pathways was more relevant in metastatic cases, while housekeeping pathways were over-represented in non-metastatic cases [291]. This study helped to highlight the immune suppressive nature in primary UM, demonstrating a rather low abundance of immune checkpoint regulator molecules [291]. Yet, some molecules, like CDH1 and HLA-DPA1, as well as 15 kinases and phosphatases emerged as novel candidates for immune checkpoint inhibition therapies [291]. Finally, the authors developed a robust model incorporating 32 proteins which was able to predict metastases development with a 93% discriminatory accuracy [291]. Interestingly, studies like this can lead to the development of innovative immunoassays for the non-invasive UM diagnosis using blood or other biological samples [292,293,294]. Ensuing studies involving larger cohorts of UM patients will be of fundamental value to better define the potential of prognostic protein profiles based on proteomics of primary UM cases.
8. Current Challenges and Future Perspectives in Uveal Melanoma
The comprehensive work carried out in the field of Ocular Oncology over the past years has considerably increased our knowledge on Uveal Melanoma. However, our capacity to prevent UM metastization and UM-related death has not changed considerably over the past years [9,48]. Below, we highlight the most relevant current challenges in UM and anticipate some of the future avenues in UM research and UM patient management.
8.1. Need for Accurate and Robust Models for Prognostication in Uveal Melanoma
In uveal melanoma research, most reported studies involve a limited collection of patient samples, as it became evident, for example, in the description of the novel IHC-based markers that have been reported recently. In addition, the methodology of analysis is also rich and heterogeneous, as it was observed in the recent efforts to find gene signatures with prognostic relevance in UM. Therefore, this poses enormous challenges in the validation and generalization of the obtained results for a wider community of UM patients. One approach could be the stimulation of the widespread sharing of pre-clinical and clinical data, similarly to the history of The Collaborative Ocular Melanoma Study (COMS) initiative, which yielded impactful and groundbreaking contributions to field [295]. The assembly of comprehensive UM patient databases through collaborative efforts could significantly and positively impact on UM research. Indeed, taking advantage of large clinical databases, together with genetic information and pre-clinical data, coupled with artificial intelligence (AI)-based strategies, it will be possible to develop novel robust artificial neural network-based systems to confidently predict patient survival and stratify UM patients for follow-up, therapy and possibly enrolment in clinical trials. Ultimately, this has the prospect to lead to the long-aimed development of a model of UM patient prognostication that is widely accepted and employed by the UM community worldwide. In line with this, among the first successful tools developed is the Liverpool Uveal Melanoma Prognosticator Online (LUMPO), a bioinformatic tool established from the data gathered from patients in the United Kingdom, assembling clinical, histological and genetic data [143,296]. LUMPO is available online, allowing a reliable prognostication of individual UM patients through determination of the risk of metastases and estimation of survival time [143,296]. A subsequent web-based tool created for UM patient prognostication is the Prediction of Risk of Metastasis in Uveal Melanoma (PRiMeUM), established from data obtained mainly from UM patients in the United States of America (USA) [297]. PRiMeUM allows a reliable personalized determination of the metastatic risk at 48 months post-initial diagnosis by combining clinical features (age, sex, tumour location, LBD and TT) and detailed information on chromosomal analysis (chromosome 1p, 3, 6p, 6q, 8p and 8q status) [297]. Even though both tools are able to ascertain the metastatic risk of patients, none can determine accurately when the metastases will develop [143,296,297].
8.2. The Promise of Liquid Biopsies for Uveal Melanoma
Liquid biopsies (LBs) have opened unprecedented avenues in the field of cancer, by allowing a non-invasive approach for diagnosis, identification of relevant mutations, disease progression monitoring, early disease recurrence detection and evaluation of response to therapies, among others [298,299,300]. They are based on the testing of blood or other body fluids (for example, the aqueous humour) and constitute an alternative reproducible method to the classical tissue biopsy, which can be used to detect circulating tumour DNA (ctDNA), circulating tumour cells (CTCs), exosomes, cytokines and microRNAs, among other components [298,300,301]. LBs have been particularly promising in different solid tumours, including lung cancer, with some studies demonstrating encouraging results in their usage in the daily practice [302,303], despite some current technical limitations [304,305,306]. In UM, the LB technology is not yet as developed as it is for other types of cancers and there are no currently available LB systems approved by both the European Medicines Agency (EMA) and Food and Drug Administration (FDA) [298]. However, there is a hope that LBs will become a solid alternative to intraocular biopsies, avoiding the risks of the procedure, including possible tumour dissemination [298,307,308,309]. For example, in a recent published study including 21 patients with UM metastatic disease in a cohort of 135 UM patients, the authors showed that ctDNA was detectable in the plasma of 17 of the 21 metastatic patients [310]. More importantly, by analysing GNAQ/GNA11 mutations using deep amplicon sequencing, in 10 of those UM patients the detection of ctDNA occurred at least 2 months up to 10 months before the clinical detection of metastases, further emphasizing the extraordinary potential of this innovative diagnostic methodology [310].
Previous studies revealed that in UM an inflammatory microenvironment, including infiltration by lymphocytes and macrophages, portends a bad prognosis for patients [122,311]. Knowing that a myriad of proteins can be robustly identified in the anterior chamber fluid and vitreous, Wierenga et al. recently evaluated whether the aqueous humour could be used to measure cytokines and, consequently, define cytokine profiles that could establish an accurate prognosis for UM patients [312]. The analysis of the aqueous humour as a substitute of tumour biopsy has been previous successfully employed in cases of retinoblastoma for diagnosis using cell free DNA [313,314], as well as for detecting the expression of IL-10 and IL-6 as biomarkers for the diagnosis of intraocular lymphoma [315,316]. The study conducted by Wierenga et al. involved 84 UM enucleation samples, from which aqueous humour was immediately collected after surgery [312]. The Proximity Extension Assay (PEA) technology that was employed allowed the detection of 92 proteins using only 1 µL of sample [312]. The study of 84 cytokines in the aqueous humour which were consistently above the limits of detection of the assay, led to the definition of three main clusters: a cluster with few cytokines (cluster 1; n = 37), a cluster with an intermediate number of cytokines expressed (cluster 2; n = 36) and a cluster enriched in several cytokines (cluster 3; n = 11) [312]. Adenosine deaminase (ADA), CD244, CD40, galactin-9 (Gal-9), monocyte-chemotactic protein 3 (MCP-3), PD-L1, tumour necrosis factor receptor superfamily 21 (TNFRSF21) and tumour necrosis factor-related apoptosis inducing ligand (TRAIL) were the most differentially expressed cytokines among the three defined clusters [312]. High levels of CD40, Gal-9, tumour necrosis factor receptor superfamily 9 (TNFRSF9), TNFRSF21 and Fas Ligand (FASLG) were registered in the aqueous humour of patients who had worst survival [312]. Interestingly, the majority of these cytokines are involved in the regulation/induction of apoptosis [312]. When the authors correlated the clinicopathological data with the cytokine cluster analysis, they observed that clusters 2 and 3 were associated with worse prognostic features [312]. Interestingly, cluster 1 patients were shown to have better survival than cluster 2 and cluster 3 patients, while there were no significant survival differences between clusters 2 and 3 patients [312]. Interestingly, in another study involving a cohort of 35 UM patients, the authors found significant higher levels of interleukin-6 (IL-6), interleukin-8 (IL-8), regulated upon activation normal T cell expressed and secreted (RANTES), epidermal growth factor (EGF), basic fibroblast growth factor (bFGF), macrophage migration inhibitory factor (MIF) and monocyte chemoattractant protein-1 (MCP-1) in the aqueous humour of UM patients when compared to control patients [317]. A positive correlation between IL-6 levels and the degree of retinal detachment, as well as between IL-8 levels and tumour thickness was established, which proposes that the levels of these cytokines could hint a more advanced disease stage [317]. Survival analysis was not performed; however, the described pro-inflammatory environment could be linked with an enhanced tumour growth and infiltration by immune cells, which are both associated with a poor survival [317]. Comprehensive studies, with larger cohorts of UM, will be instrumental to define prognostic profiles based on biomarkers present in the aqueous humour. Altogether, these pioneer studies demonstrate that the continuous development in the technological procedures employed in LBs has the potential to soon critically change the paradigm of UM diagnosis and follow-up.
8.3. The Relevance of Non-Coding RNAs (ncRNAs) in Uveal Melanoma
Non-coding RNAs (ncRNAs), which comprise a vast family of very small molecules, including long non-coding RNAs (lncRNAs) and microRNAs (miRNAs), influence and regulate genes at the post-transcriptional level, being involved in different cell types in the fine-tuned control of cell proliferation, cell differentiation and cell death, among other processes [318,319]. Similarly to other cancers, such as lung cancer [320] or cutaneous melanoma [321], in UM ncRNAs constitute emerging molecular players given that aberrations in their expression have been implicated in the development and progression of the disease [322,323]. For example, miRNAs were shown to have both tumour-suppressing and tumour-promoting roles, which are being increasingly unveiled [324,325]. Researchers have tried to uncover miRNAs differentially expressed in cases of primary UM with low and high risk of metastases, with a recent research pooling results from different studies showing consistently in the high-metastatic risk group upregulation of the miRNAs let-7b, miR-20a, miR-124, miR-142, miR-155, miR-199 and miR-224, while only miR-181a and miR-211 were constantly downregulated [324]. The MAPK and PI3K-Akt signaling pathways appear to be altered in light of the dysregulation of the different collection of miRNAs in UM [324,326]. Besides constituting biomarkers of the disease, miRNAs could also become soon promising therapeutic targets in metastatic UM [326,327,328]. Larger studies, involving well-established methodologies will be of fundamental importance to institute meaningful signatures of ncRNAs in UM.
8.4. Dissecting the Role of Tumour Infiltrating Immune Cells in Uveal Melanoma
Mounting evidence points towards a unique biological behaviour in UM, with infiltration by immune cells strongly linked with a tumour growth stimulatory effect, instead of a tumour suppressing effect, which is normally present in other types of neoplasias [272,311,329]. In addition, unlike in cutaneous melanoma, immune checkpoint inhibition has not yielded meaningful results for the majority of UM patients [123,330,331]. Together, these results highlight the presence of a strongly immunosuppressive microenvironment in primary UM, and our knowledge on this distinctive phenomenon remains in its infancy [329,332,333]. Interestingly, an association between BAP1 loss and the infiltration of the tumoural microenvironment by lymphocytes and macrophages, with concomitant overexpression of genes involved in immunosuppression has been established [332]. Classically and well-established checkpoint inhibitor molecules such as CTLA4 and PD-1 seem to be relevant only for limited subsets of UM patients [123,330,331]. On the other hand, a recent study involving single cell RNA sequencing demonstrated that an emerging checkpoint inhibitor molecule, lymphocyte-activation gene-3 (LAG3), is expressed at high levels in most of T-CD8+ cytotoxic UM TILs [334]. Furthermore, increased expression of LAG3 in UM is linked with M3/BAP1 loss (associated with the highest risk of metastasis development) and strongly correlated with a high metastases rate and a worst survival [335]. The expression of LAG3 was proven to be positively correlated with the expression of several of its ligands, namely, Galectin-3 and several molecules in the HLA class II family [335]. LAG3-expressing lymphocytes were also documented in the liver metastases of UM patients [334]. Thus, LAG-3 could be among the most relevant immune checkpoint molecules in UM and, similarly to cutaneous melanoma, anti-LAG3 directed therapies could soon have a role in the treatment of UM patients [334,335].
Cluster of differentiation 47 (CD47) is a transmembrane integrin associated protein of the immunoglobulin superfamily that acts as a “do not eat me” signal for macrophages through binding to the signal regulatory protein (SIRP) on antigen presenting cells [336,337]. The levels of CD47 are normally decreased in damaged or senescent cells, priming their clearance by macrophages [336,337]. In contrast, CD47 was demonstrated to be overexpressed in different cancer types, constituting a strong independent marker of poor prognosis [338,339,340]. The expression of CD47 in UM patients was studied using the TCGA database [341]. Patients with lower CD47 levels had a better PFS, even though there were no major survival differences between patients with low and high CD47 levels [341]. In addition, higher levels of CD47 were associated with a higher immune score, namely, an increase in the number of TILs (CD4+ and CD8+ T cells), proposing that anti-CD47 therapies could also constitute a novel and relevant therapeutic avenue in UM [341,342].
The adequate evaluation of the expression of established (PD-1/PD-L1, CTLA-4) and emerging immune checkpoints molecules [B7 homolog 3 protein (B7-H3), inducible T cell costimulatory (ICOS), indoleamine 2,3-dioxygenase (IDO), LAG3, T cell immunoreceptor with Ig and ITIM domains (TIGIT), T cell immunoglobulin-3 (TIM-3), V-domain Ig suppressor of T cell activation (VISTA), among others] [333,343,344], as well as other immune relevant proteins will be instrumental for the development of novel therapies for UM, which will likely be based on the well-thought combination of different immune blocking antibodies rather than a single miracle antibody approach [273,345]. In this regard, the advent and optimization of laboratory techniques such as multiplexed IHC will critically impact in our ability to identify specific protein markers of interest and/or molecular abnormalities, allowing a more accurate assessment of the in vivo interplay between the different cells of the immune system and tumoural UM cells [346,347].
8.5. Unravelling the Mystery of Preferential UM Metastization to the Liver
The leading cause of death in patients with UM is metastization, which preferentially occurs to the liver (Table 1) [24]. Our knowledge on the mechanisms underlying the exquisitely preference of UM cells for the liver microenvironment is still scarce [9]. In the liver, metastasizing UM cells can display two fundamental patterns of growth: nodular periportal or infiltrative sinusoidal [9,348,349]. The periportal nodular growth pattern is characterized by the presence of UM cells concentrated in the periportal areas, which then become hypoxic, leading to angiogenesis promoted by vascular endothelial growth factor (VEGF), which is produced by the neoplastic cells [348,349]. On the other hand, the infiltrative pattern is characterized by UM cells that occupy the sinusoidal spaces, with a lesser degree of hypoxia and that also develop their own circulation through a process which involves hepatic stellate cells [348,349]. The expression of cMET by UM cells is a plausible explanation for their preferential homing to the liver, since hepatic stellate cells produce the hepatocyte growth factor (HGF), the ligand of cMET [9,350]. Similarly, UM cells also express CXCR4 and hepatic sinusoidal endothelial cells and hepatic stellate cells produce its ligand CXCR12 [9,350]. Interestingly, the blockade of both axes in rodent models also prevented UM metastization [9,350]. Mounting evidence also demonstrates that immune related mechanisms are involved in the promotion of growth of UM cells in the liver microenvironment [291,329]. For example, there is a preponderance of M2-TAMs infiltration in UM metastatic to the liver [329]. Interestingly, the metastatic UM cells in the liver upregulate the expression of an array of genes (BCL2, CD44, CD146/MCAM/MUC18, DUSP4, IGF1R, IRF4/MUM1, LGALS3/Galectin-3, MFGE8/lactadherin, PNMA1 and PRAME), which is likely to contribute to an immunosuppressive tumoural microenvironment [329]. In a recent study, the metastatic tissues of a UM patient with liver metastasis were submitted to a comprehensive single-cell RNA sequencing (scRNA-seq) study, which exposed an extensive intra- and inter-tumoural heterogeneity, further highlighting the diversity and complexity of UM even in a single individual [351]. Interestingly, a high degree of intratumoural heterogeneity has also been demonstrated in primary UM [352,353]. A deeper understanding of the mechanisms involved in the development of liver metastases by UM, including the role of intratumoural heterogeneity, will be fundamental for the generation of robust therapeutic strategies aiming at preventing UM metastases and approaches directed to ablate those metastases with the ultimate aim to significantly increase the life expectancy of patients diagnosed with UM [353].
8.6. Novel In Vitro Cancer Models Will Likely Boost Research Efforts in Uveal Melanoma
The capacity to culture in vitro cells of human origin has dramatically changed the landscape of medical research over the past decades [354,355]. The first human cell line was the HeLa cell line, established in 1951 from a biopsy sample of Henrietta Lacks, who had an aggressive adenocarcinoma of the cervix [356]. Since then, a myriad of different immortalized cell lines and cell culturing approaches from patient-derived tissue have made possible the study of human cells in vitro, both in simple monolayer cultures and in more complex 3D models. Cell lines have been instrumental to unravel important UM biological mechanisms and also allowed the testing of some drugs [357,358,359]. Even though successful culturing in vitro from primary UM cells has been achieved, a standard procedure remains to be established and different groups use their own approaches [357,358,359,360]. Furthermore, reliable animal models remain to be established [361,362]. One appealing strategy can be the usage of human induced pluripotent cells (hiPSCs, efficiently generated from reprogramming of somatic cells obtained from donors), which similarly to human embryonic stem cells (hESCs), are successfully cultured in vitro and are able to differentiate into all three embryonic germ layers (ectoderm, mesoderm and endoderm) and give rise to virtually all cell types of the body in inexhaustible manners [355,363]. In the case of hiPSCs, they retain the genetic background of the donor [363]. Both hiPSCs and hESCs have allowed the study of human cells which are not normally accessible to study in the human body (for example, neurons and glial cells of the human CNS) and, therefore, have boosted the possibilities in medical research employing human cell lines, permitting the study of mechanisms of human development [363,364]; in vitro disease modelling, including in cancer research [365,366,367]; in the development of assays and platforms for drug screening campaigns [355,368,369]; in patient stratification and in the development of cell replacement strategies [355,363]. The pioneer monolayer cultures gave way to organoids, spheroids, organ-on-a-chip approaches and more recently assembloids, which employ single cell types or a multitude of different cellular types [355,360,370,371,372,373]. One such example is the recently developed model of 3D cortico-motor assembloids by Paşca and collaborators, which has brought this technology into a new state of development [374], allowing the efficient combination of 3D structures analogous to the cerebral cortex and/or the hindbrain/spinal cord with human skeletal muscle spheroids, generating a functional nervous circuit in vitro [374]. These innovative 3D cortico-motor assembloids established the conditions for unprecedented opportunities in terms of disease modelling and drug discovery in motor neuron disorders [374,375]. Hopefully, our increased ability to grow different cell types in vitro will lead in the near future to the development of UM 3D models that capture the organization, tumour microenvironment and cellular milieu of the UM patient. Those models will have far reaching impact in our understanding of the disease, in patient stratification and prognostication, as well as in drug discovery and development. In this respect, for example, models of blood–eye barrier and UM-liver co-cultures will offer unprecedented possibilities.
8.7. The Need for Novel Effective Therapeutics for Metastatic Uveal Melanoma
The OS of patients diagnosed with UM has not dramatically changed over the past decades given that there are only limited therapeutic possibilities once widespread metastatic disease develops. In the past year, promising results on the usage of Tebentafusp for UM have been published [376,377]. Tebentafusp is an innovative engineered fusion protein belonging to a new class of promising therapeutic agents termed immune-mobilizing monoclonal T-cell receptors against cancer (ImmTAC) [376,377]. It is a construct composed of a soluble affinity-enhanced HLA-A*02:01–restricted T-cell receptor specific for the glycoprotein 100 (gp100) peptide YLEPGPVTA which is fused to an anti-CD3 single-chain variable fragment [376,378]. Thus, ImmTACs like Tebentafusp, are able to target any protein presented as a peptide–HLA complex on the surface of the target-cell, including intracellular antigens [379,380]. The binding of ImmTAC molecules to their target-cell surface specific peptide–HLA complexes initiates the recruitment and activation of polyclonal T cells, mediated through CD3, which efficiently leads to the release of cytokines and other cytolytic mediators to the target cells [379,380]. In a recent phase 3 clinical trial involving 378 previously untreated HLAA*02:01–positive metastatic UM patients, stratified based on lactate dehydrogenase (LDH) levels, treatment with Tebentafusp was associated with a higher PFS and a 1-year OS of 73%, while in the control group (single agent pembrolizumab, ipilimumab, or dacarbazine) the observed 1-year OS was only 59% [376]. Even though Tebentafusp showed promising results in all UM patients, new studies will be instrumental to better define which UM biomarkers could be helpful to predict an enhanced positive response to this promising drug. Our increased knowledge on the mechanisms underlying UM development, including aspects of metabolomics [381] and of immune checkpoint inhibition, coupled with novel drug screening efforts taking advantage of robust pre-clinical models will hopefully, in the near future, lead to the development of efficacious therapeutic approaches against UM.
9. Conclusions
UM is a rare and complex neoplastic disease with a distinctive biological behaviour. For the majority of patients, the prognosis is dismal after metastases develop in the liver or other sites, since there are currently limited therapeutic strategies for the widespread disease. Indeed, despite extensive research over the past decades our ability to extend the survival of UM patients has not dramatically changed. The continuous efforts to find better estimators of prognosis for UM has led to the recent discovery of novel promising proteins, genomic and proteomic signatures with prognostic implication for UM patients, which complement the list of already well-established prognostic factors in UM. However, a unifying and optimized prognostic model, encompassing clinical and molecular information, widely accepted by the UM community is still lacking. The development of such model is an imminent challenge and could decisively positively impact in a personalized medicine approach, leading to patient-directed surveillance plans and patient-tailored therapies. In this regard, diagnostic methods that allow an earlier disease relapse detection, such as LB, coupled with better pre-clinical models of research which allow a more comprehensive understanding of the UM unique biology, UM metastization and enhanced capacity for in vitro drug testing, as well as a more comprehensive insight on the interplay between different immune infiltrating cells and UM cells will soon help to accelerate the process of therapy development for UM. Hopefully, in the near future we will be able to slow or halt disease progression or even cure UM.
Acknowledgments
N.J.L. would like to thank all members of the Laboratory of Clinical and Experimental Pathology (LPCE), Centre Hospitalier Universitaire de Nice, Nice, France; and all members of the Anatomic Pathology Service, Pathology Department, Centro Hospitalar e Universitário do Porto, Porto, Portugal, especially to José Ramón Vizcaíno (Head of Service), Joana Raposo Alves (Advisor of Pathology Training), André Coelho, David Tente and Francisca Emanuel Costa for their continuous support and help in the development of his knowledge, interest, diagnostic and research skills in the field of Ocular Pathology.
Author Contributions
Conceptualization, N.J.L., S.L. and P.H.; collection and review of the literature, N.J.L., A.M. (Arnaud Martel), S.N.-E., S.G., A.M. (Adam Macocco), C.B., S.L. and P.H.; writing—original draft preparation, N.J.L., S.L. and P.H.; writing—review and editing, N.J.L., A.M. (Arnaud Martel), S.N.-E., S.G., A.M. (Adam Macocco), C.B., S.L. and P.H. All authors have read and agreed to the published version of the manuscript.
Funding
The present manuscript did not receive any specific external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kaliki S., Shields C.L. Uveal melanoma: Relatively rare but deadly cancer. Eye. 2017;31:241–257. doi: 10.1038/eye.2016.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krantz B.A., Dave N., Komatsubara K.M., Marr B.P., Carvajal R.D. Uveal melanoma: Epidemiology, etiology, and treatment of primary disease. Clin. Ophthalmol. 2017;11:279–289. doi: 10.2147/OPTH.S89591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shields C.L., Mayro E.L., Bas Z., Dockery P.W., Yaghy A., Lally S.E., Ganguly A., Shields J.A. Ten-year outcomes of uveal melanoma based on The Cancer Genome Atlas (TCGA) classification in 1001 cases. Indian J. Ophthalmol. 2021;69:1839–1845. doi: 10.4103/ijo.IJO_313_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stalhammar G. Forty-year prognosis after plaque brachytherapy of uveal melanoma. Sci. Rep. 2020;10:11297. doi: 10.1038/s41598-020-68232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rantala E.S., Hernberg M., Kivela T.T. Overall survival after treatment for metastatic uveal melanoma: A systematic review and meta-analysis. Melanoma Res. 2019;29:561–568. doi: 10.1097/CMR.0000000000000575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez-Vidal C., Fernandez-Diaz D., Fernandez-Marta B., Lago-Baameiro N., Pardo M., Silva P., Paniagua L., Blanco-Teijeiro M.J., Pineiro A., Bande M. Treatment of Metastatic Uveal Melanoma: Systematic Review. Cancers. 2020;12:2557. doi: 10.3390/cancers12092557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lane A.M., Kim I.K., Gragoudas E.S. Survival Rates in Patients After Treatment for Metastasis From Uveal Melanoma. JAMA Ophthalmol. 2018;136:981–986. doi: 10.1001/jamaophthalmol.2018.2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaliki S., Shields C.L., Shields J.A. Uveal melanoma: Estimating prognosis. Indian J. Ophthalmol. 2015;63:93–102. doi: 10.4103/0301-4738.154367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jager M.J., Shields C.L., Cebulla C.M., Abdel-Rahman M.H., Grossniklaus H.E., Stern M.H., Carvajal R.D., Belfort R.N., Jia R., Shields J.A., et al. Uveal melanoma. Nat. Rev. Dis. Prim. 2020;6:24. doi: 10.1038/s41572-020-0158-0. [DOI] [PubMed] [Google Scholar]
- 10.Carvajal R.D., Schwartz G.K., Tezel T., Marr B., Francis J.H., Nathan P.D. Metastatic disease from uveal melanoma: Treatment options and future prospects. Br. J. Ophthalmol. 2017;101:38–44. doi: 10.1136/bjophthalmol-2016-309034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dogrusoz M., Jager M.J., Damato B. Uveal Melanoma Treatment and Prognostication. Asia-Pac. J. Ophthalmol. 2017;6:186–196. doi: 10.22608/APO.201734. [DOI] [PubMed] [Google Scholar]
- 12.Comito F., Marchese P.V., Ricci A.D., Tober N., Peterle C., Sperandi F., Melotti B. Systemic and liver-directed therapies in metastatic uveal melanoma: State-of-the-art and novel perspectives. Future Oncol. 2021;17:4583–4606. doi: 10.2217/fon-2021-0318. [DOI] [PubMed] [Google Scholar]
- 13.Bethlehem M.S., Katsarelias D., Olofsson Bagge R. Meta-Analysis of Isolated Hepatic Perfusion and Percutaneous Hepatic Perfusion as a Treatment for Uveal Melanoma Liver Metastases. Cancers. 2021;13:4726. doi: 10.3390/cancers13184726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rowcroft A., Loveday B.P.T., Thomson B.N.J., Banting S., Knowles B. Systematic review of liver directed therapy for uveal melanoma hepatic metastases. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2020;22:497–505. doi: 10.1016/j.hpb.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Kivela T.T. The first description of the complete natural history of uveal melanoma by two Scottish surgeons, Allan Burns and James Wardrop. Acta Ophthalmol. 2018;96:203–214. doi: 10.1111/aos.13535. [DOI] [PubMed] [Google Scholar]
- 16.Shields C.L., Furuta M., Thangappan A., Nagori S., Mashayekhi A., Lally D.R., Kelly C.C., Rudich D.S., Nagori A.V., Wakade O.A., et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch. Ophthalmol. 2009;127:989–998. doi: 10.1001/archophthalmol.2009.208. [DOI] [PubMed] [Google Scholar]
- 17.Alfaar A.S., Saad A., Wiedemann P., Rehak M. The epidemiology of uveal melanoma in Germany: A nationwide report of incidence and survival between 2009 and 2015. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021:1–9. doi: 10.1007/s00417-021-05317-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smidt-Nielsen I., Bagger M., Heegaard S., Andersen K.K., Kiilgaard J.F. Posterior uveal melanoma incidence and survival by AJCC tumour size in a 70-year nationwide cohort. Acta Ophthalmol. 2021;99:e1474–e1482. doi: 10.1111/aos.14847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu Y., Lou L., Wang Y., Miao Q., Jin K., Chen M., Ye J. Epidemiological Study of Uveal Melanoma from US Surveillance, Epidemiology, and End Results Program (2010–2015) J. Ophthalmol. 2020;2020:3614039. doi: 10.1155/2020/3614039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahendraraj K., Lau C.S., Lee I., Chamberlain R.S. Trends in incidence, survival, and management of uveal melanoma: A population-based study of 7516 patients from the Surveillance, Epidemiology, and End Results database (1973–2012) Clin. Ophthalmol. 2016;10:2113–2119. doi: 10.2147/OPTH.S113623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shields C.L., Kaliki S., Furuta M., Fulco E., Alarcon C., Shields J.A. American Joint Committee on Cancer classification of posterior uveal melanoma (tumor size category) predicts prognosis in 7731 patients. Ophthalmology. 2013;120:2066–2071. doi: 10.1016/j.ophtha.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Chattopadhyay C., Kim D.W., Gombos D.S., Oba J., Qin Y., Williams M.D., Esmaeli B., Grimm E.A., Wargo J.A., Woodman S.E., et al. Uveal melanoma: From diagnosis to treatment and the science in between. Cancer. 2016;122:2299–2312. doi: 10.1002/cncr.29727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jovanovic P., Mihajlovic M., Djordjevic-Jocic J., Vlajkovic S., Cekic S., Stefanovic V. Ocular melanoma: An overview of the current status. Int. J. Clin. Exp. Pathol. 2013;6:1230–1244. [PMC free article] [PubMed] [Google Scholar]
- 24.Garg G., Finger P.T., Kivela T.T., Simpson E.R., Gallie B.L., Saakyan S., Amiryan A.G., Valskiy V., Chin K.J., Semenova E., et al. Patients presenting with metastases: Stage IV uveal melanoma, an international study. Br. J. Ophthalmol. 2021 doi: 10.1136/bjophthalmol-2020-317949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Derrien A.C., Rodrigues M., Eeckhoutte A., Dayot S., Houy A., Mobuchon L., Gardrat S., Lequin D., Ballet S., Pierron G., et al. Germline MBD4 Mutations and Predisposition to Uveal Melanoma. J. Natl. Cancer Inst. 2021;113:80–87. doi: 10.1093/jnci/djaa047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abdel-Rahman M.H., Sample K.M., Pilarski R., Walsh T., Grosel T., Kinnamon D., Boru G., Massengill J.B., Schoenfield L., Kelly B., et al. Whole Exome Sequencing Identifies Candidate Genes Associated with Hereditary Predisposition to Uveal Melanoma. Ophthalmology. 2020;127:668–678. doi: 10.1016/j.ophtha.2019.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodrigues M., Mobuchon L., Houy A., Fievet A., Gardrat S., Barnhill R.L., Popova T., Servois V., Rampanou A., Mouton A., et al. Outlier response to anti-PD1 in uveal melanoma reveals germline MBD4 mutations in hypermutated tumors. Nat. Commun. 2018;9:1866. doi: 10.1038/s41467-018-04322-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johansson P.A., Brooks K., Newell F., Palmer J.M., Wilmott J.S., Pritchard A.L., Broit N., Wood S., Carlino M.S., Leonard C., et al. Whole genome landscapes of uveal melanoma show an ultraviolet radiation signature in iris tumours. Nat. Commun. 2020;11:2408. doi: 10.1038/s41467-020-16276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chalada M., Ramlogan-Steel C.A., Dhungel B.P., Layton C.J., Steel J.C. The Impact of Ultraviolet Radiation on the Aetiology and Development of Uveal Melanoma. Cancers. 2021;13:1700. doi: 10.3390/cancers13071700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karlsson J., Nilsson L.M., Mitra S., Alsen S., Shelke G.V., Sah V.R., Forsberg E.M.V., Stierner U., All-Eriksson C., Einarsdottir B., et al. Molecular profiling of driver events in metastatic uveal melanoma. Nat. Commun. 2020;11:1894. doi: 10.1038/s41467-020-15606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reichstein D.A., Brock A.L. Radiation therapy for uveal melanoma: A review of treatment methods available in 2021. Curr. Opin. Ophthalmol. 2021;32:183–190. doi: 10.1097/ICU.0000000000000761. [DOI] [PubMed] [Google Scholar]
- 32.Sikuade M.J., Salvi S., Rundle P.A., Errington D.G., Kacperek A., Rennie I.G. Outcomes of treatment with stereotactic radiosurgery or proton beam therapy for choroidal melanoma. Eye. 2015;29:1194–1198. doi: 10.1038/eye.2015.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Papakostas T.D., Lane A.M., Morrison M., Gragoudas E.S., Kim I.K. Long-term Outcomes After Proton Beam Irradiation in Patients With Large Choroidal Melanomas. JAMA Ophthalmol. 2017;135:1191–1196. doi: 10.1001/jamaophthalmol.2017.3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Beek J.G.M., Buitendijk G.H.S., Timman R., Muller K., Luyten G.P.M., Paridaens D., Naus N.C., Kilic E. Quality of life: Fractionated stereotactic radiotherapy versus enucleation treatment in uveal melanoma patients. Acta Ophthalmol. 2018;96:841–848. doi: 10.1111/aos.13823. [DOI] [PubMed] [Google Scholar]
- 35.Marinkovic M., Horeweg N., Fiocco M., Peters F.P., Sommers L.W., Laman M.S., Bleeker J.C., Ketelaars M., Luyten G.P., Creutzberg C.L. Ruthenium-106 brachytherapy for choroidal melanoma without transpupillary thermotherapy: Similar efficacy with improved visual outcome. Eur. J. Cancer. 2016;68:106–113. doi: 10.1016/j.ejca.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 36.Bakhoum M.F., Esmaeli B. Molecular Characteristics of Uveal Melanoma: Insights from the Cancer Genome Atlas (TCGA) Project. Cancers. 2019;11:1061. doi: 10.3390/cancers11081061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carbone M., Ferris L.K., Baumann F., Napolitano A., Lum C.A., Flores E.G., Gaudino G., Powers A., Bryant-Greenwood P., Krausz T., et al. BAP1 cancer syndrome: Malignant mesothelioma, uveal and cutaneous melanoma, and MBAITs. J. Transl. Med. 2012;10:179. doi: 10.1186/1479-5876-10-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abdel-Rahman M.H., Pilarski R., Cebulla C.M., Massengill J.B., Christopher B.N., Boru G., Hovland P., Davidorf F.H. Germline BAP1 mutation predisposes to uveal melanoma, lung adenocarcinoma, meningioma, and other cancers. J. Med. Genet. 2011;48:856–859. doi: 10.1136/jmedgenet-2011-100156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jager M.J., Brouwer N.J., Esmaeli B. The Cancer Genome Atlas Project: An Integrated Molecular View of Uveal Melanoma. Ophthalmology. 2018;125:1139–1142. doi: 10.1016/j.ophtha.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 40.Robertson A.G., Shih J., Yau C., Gibb E.A., Oba J., Mungall K.L., Hess J.M., Uzunangelov V., Walter V., Danilova L., et al. Integrative Analysis Identifies Four Molecular and Clinical Subsets in Uveal Melanoma. Cancer Cell. 2017;32:204–220.e15. doi: 10.1016/j.ccell.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diener-West M., Reynolds S.M., Agugliaro D.J., Caldwell R., Cumming K., Earle J.D., Hawkins B.S., Hayman J.A., Jaiyesimi I., Jampol L.M., et al. Development of metastatic disease after enrollment in the COMS trials for treatment of choroidal melanoma: Collaborative Ocular Melanoma Study Group Report No. 26. Arch. Ophthalmol. 2005;123:1639–1643. doi: 10.1001/archopht.123.12.1639. [DOI] [PubMed] [Google Scholar]
- 42.Rajpal S., Moore R., Karakousis C.P. Survival in metastatic ocular melanoma. Cancer. 1983;52:334–336. doi: 10.1002/1097-0142(19830715)52:2<334::AID-CNCR2820520225>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 43.Kath R., Hayungs J., Bornfeld N., Sauerwein W., Hoffken K., Seeber S. Prognosis and treatment of disseminated uveal melanoma. Cancer. 1993;72:2219–2223. doi: 10.1002/1097-0142(19931001)72:7<2219::AID-CNCR2820720725>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 44.Rietschel P., Panageas K.S., Hanlon C., Patel A., Abramson D.H., Chapman P.B. Variates of survival in metastatic uveal melanoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2005;23:8076–8080. doi: 10.1200/JCO.2005.02.6534. [DOI] [PubMed] [Google Scholar]
- 45.Jochems A., van der Kooij M.K., Fiocco M., Schouwenburg M.G., Aarts M.J., van Akkooi A.C., van den Berkmortel F., Blank C.U., van den Eertwegh A.J.M., Franken M.G., et al. Metastatic Uveal Melanoma: Treatment Strategies and Survival-Results from the Dutch Melanoma Treatment Registry. Cancers. 2019;11:1007. doi: 10.3390/cancers11071007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aronow M.E., Topham A.K., Singh A.D. Uveal Melanoma: 5-Year Update on Incidence, Treatment, and Survival (SEER 1973–2013) Ocul. Oncol. Pathol. 2018;4:145–151. doi: 10.1159/000480640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singh A.D., Turell M.E., Topham A.K. Uveal melanoma: Trends in incidence, treatment, and survival. Ophthalmology. 2011;118:1881–1885. doi: 10.1016/j.ophtha.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 48.Roelofsen C.D.M., Wierenga A.P.A., van Duinen S., Verdijk R.M., Bleeker J., Marinkovic M., Luyten G.P.M., Jager M.J. Five Decades of Enucleations for Uveal Melanoma in One Center: More Tumors with High Risk Factors, No Improvement in Survival over Time. Ocul. Oncol. Pathol. 2021;7:133–141. doi: 10.1159/000509918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eskelin S., Pyrhonen S., Summanen P., Hahka-Kemppinen M., Kivela T. Tumor doubling times in metastatic malignant melanoma of the uvea: Tumor progression before and after treatment. Ophthalmology. 2000;107:1443–1449. doi: 10.1016/S0161-6420(00)00182-2. [DOI] [PubMed] [Google Scholar]
- 50.Park S.Y., Nam J.S. The force awakens: Metastatic dormant cancer cells. Exp. Mol. Med. 2020;52:569–581. doi: 10.1038/s12276-020-0423-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Neophytou C.M., Kyriakou T.C., Papageorgis P. Mechanisms of Metastatic Tumor Dormancy and Implications for Cancer Therapy. Int. J. Mol. Sci. 2019;20:6158. doi: 10.3390/ijms20246158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Collaborative Ocular Melanoma Study Group Assessment of metastatic disease status at death in 435 patients with large choroidal melanoma in the Collaborative Ocular Melanoma Study (COMS): COMS report no. 15. Arch. Ophthalmol. 2001;119:670–676. doi: 10.1001/archopht.119.5.670. [DOI] [PubMed] [Google Scholar]
- 53.Smit K.N., Jager M.J., de Klein A., Kili E. Uveal melanoma: Towards a molecular understanding. Prog. Retin. Eye Res. 2020;75:100800. doi: 10.1016/j.preteyeres.2019.100800. [DOI] [PubMed] [Google Scholar]
- 54.Kang K., Xie F., Mao J., Bai Y., Wang X. Significance of Tumor Mutation Burden in Immune Infiltration and Prognosis in Cutaneous Melanoma. Front. Oncol. 2020;10:573141. doi: 10.3389/fonc.2020.573141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heeke S., Hofman P. Tumor mutational burden assessment as a predictive biomarker for immunotherapy in lung cancer patients: Getting ready for prime-time or not? Transl. Lung Cancer Res. 2018;7:631–638. doi: 10.21037/tlcr.2018.08.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cancer Genome Atlas N. Genomic Classification of Cutaneous Melanoma. Cell. 2015;161:1681–1696. doi: 10.1016/j.cell.2015.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nahon-Esteve S., Martel A., Maschi C., Caujolle J.P., Baillif S., Lassalle S., Hofman P. The Molecular Pathology of Eye Tumors: A 2019 Update Main Interests for Routine Clinical Practice. Curr. Mol. Med. 2019;19:632–664. doi: 10.2174/1566524019666190726161044. [DOI] [PubMed] [Google Scholar]
- 58.Shoushtari A.N., Carvajal R.D. GNAQ and GNA11 mutations in uveal melanoma. Melanoma Res. 2014;24:525–534. doi: 10.1097/CMR.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 59.Van Raamsdonk C.D., Griewank K.G., Crosby M.B., Garrido M.C., Vemula S., Wiesner T., Obenauf A.C., Wackernagel W., Green G., Bouvier N., et al. Mutations in GNA11 in uveal melanoma. N. Engl. J. Med. 2010;363:2191–2199. doi: 10.1056/NEJMoa1000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Van Raamsdonk C.D., Bezrookove V., Green G., Bauer J., Gaugler L., O’Brien J.M., Simpson E.M., Barsh G.S., Bastian B.C. Frequent somatic mutations of GNAQ in uveal melanoma and blue naevi. Nature. 2009;457:599–602. doi: 10.1038/nature07586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moore A.R., Ceraudo E., Sher J.J., Guan Y., Shoushtari A.N., Chang M.T., Zhang J.Q., Walczak E.G., Kazmi M.A., Taylor B.S., et al. Recurrent activating mutations of G-protein-coupled receptor CYSLTR2 in uveal melanoma. Nat. Genet. 2016;48:675–680. doi: 10.1038/ng.3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nell R.J., Menger N.V., Versluis M., Luyten G.P.M., Verdijk R.M., Madigan M.C., Jager M.J., van der Velden P.A. Involvement of mutant and wild-type CYSLTR2 in the development and progression of uveal nevi and melanoma. BMC Cancer. 2021;21:164. doi: 10.1186/s12885-021-07865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johansson P., Aoude L.G., Wadt K., Glasson W.J., Warrier S.K., Hewitt A.W., Kiilgaard J.F., Heegaard S., Isaacs T., Franchina M., et al. Deep sequencing of uveal melanoma identifies a recurrent mutation in PLCB4. Oncotarget. 2016;7:4624–4631. doi: 10.18632/oncotarget.6614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Koopmans A.E., Vaarwater J., Paridaens D., Naus N.C., Kilic E., de Klein A., Rotterdam Ocular Melanoma Study Group Patient survival in uveal melanoma is not affected by oncogenic mutations in GNAQ and GNA11. Br. J. Cancer. 2013;109:493–496. doi: 10.1038/bjc.2013.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ma J., Weng L., Bastian B.C., Chen X. Functional characterization of uveal melanoma oncogenes. Oncogene. 2021;40:806–820. doi: 10.1038/s41388-020-01569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vader M.J.C., Madigan M.C., Versluis M., Suleiman H.M., Gezgin G., Gruis N.A., Out-Luiting J.J., Bergman W., Verdijk R.M., Jager M.J., et al. GNAQ and GNA11 mutations and downstream YAP activation in choroidal nevi. Br. J. Cancer. 2017;117:884–887. doi: 10.1038/bjc.2017.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Decatur C.L., Ong E., Garg N., Anbunathan H., Bowcock A.M., Field M.G., Harbour J.W. Driver Mutations in Uveal Melanoma: Associations With Gene Expression Profile and Patient Outcomes. JAMA Ophthalmol. 2016;134:728–733. doi: 10.1001/jamaophthalmol.2016.0903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rodrigues M., Ait Rais K., Salviat F., Algret N., Simaga F., Barnhill R., Gardrat S., Servois V., Mariani P., Piperno-Neumann S., et al. Association of Partial Chromosome 3 Deletion in Uveal Melanomas With Metastasis-Free Survival. JAMA Ophthalmol. 2020;138:182–188. doi: 10.1001/jamaophthalmol.2019.5403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Martin M., Masshofer L., Temming P., Rahmann S., Metz C., Bornfeld N., van de Nes J., Klein-Hitpass L., Hinnebusch A.G., Horsthemke B., et al. Exome sequencing identifies recurrent somatic mutations in EIF1AX and SF3B1 in uveal melanoma with disomy 3. Nat. Genet. 2013;45:933–936. doi: 10.1038/ng.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nguyen J.Q.N., Drabarek W., Yavuzyigitoglu S., Medico Salsench E., Verdijk R.M., Naus N.C., de Klein A., Kilic E., Brosens E. Spliceosome Mutations in Uveal Melanoma. Int. J. Mol. Sci. 2020;21:9546. doi: 10.3390/ijms21249546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yavuzyigitoglu S., Koopmans A.E., Verdijk R.M., Vaarwater J., Eussen B., van Bodegom A., Paridaens D., Kilic E., de Klein A., Rotterdam Ocular Melanoma Study G. Uveal Melanomas with SF3B1 Mutations: A Distinct Subclass Associated with Late-Onset Metastases. Ophthalmology. 2016;123:1118–1128. doi: 10.1016/j.ophtha.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 72.Van Poppelen N.M., Drabarek W., Smit K.N., Vaarwater J., Brands T., Paridaens D., Kilic E., de Klein A. SRSF2 Mutations in Uveal Melanoma: A Preference for In-Frame Deletions? Cancers. 2019;11:1200. doi: 10.3390/cancers11081200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shields C.L., Dalvin L.A., Vichitvejpaisal P., Mazloumi M., Ganguly A., Shields J.A. Prognostication of uveal melanoma is simple and highly predictive using The Cancer Genome Atlas (TCGA) classification: A review. Indian J. Ophthalmol. 2019;67:1959–1963. doi: 10.4103/ijo.IJO_1589_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Correa Z.M. Assessing Prognosis in Uveal Melanoma. Cancer Control. J. Moffitt Cancer Cent. 2016;23:93–98. doi: 10.1177/107327481602300202. [DOI] [PubMed] [Google Scholar]
- 75.Sussman T.A., Funchain P., Singh A. Clinical Trials in Metastatic Uveal Melanoma: Current Status. Ocul. Oncol. Pathol. 2020;6:381–387. doi: 10.1159/000508383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Beran T.M., McCannel T.A., Stanton A.L., Straatsma B.R., Burgess B.L. Reactions to and desire for prognostic testing in choroidal melanoma patients. J. Genet. Couns. 2009;18:265–274. doi: 10.1007/s10897-009-9223-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kaliki S., Shields C.L., Mashayekhi A., Ganesh A., Furuta M., Shields J.A. Influence of age on prognosis of young patients with uveal melanoma: A matched retrospective cohort study. Eur. J. Ophthalmol. 2013;23:208–216. doi: 10.5301/ejo.5000200. [DOI] [PubMed] [Google Scholar]
- 78.Shields C.L., Kaliki S., Furuta M., Mashayekhi A., Shields J.A. Clinical spectrum and prognosis of uveal melanoma based on age at presentation in 8033 cases. Retina. 2012;32:1363–1372. doi: 10.1097/IAE.0b013e31824d09a8. [DOI] [PubMed] [Google Scholar]
- 79.Zloto O., Pe’er J., Frenkel S. Gender differences in clinical presentation and prognosis of uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2013;54:652–656. doi: 10.1167/iovs.12-10365. [DOI] [PubMed] [Google Scholar]
- 80.McLean I.W., Foster W.D., Zimmerman L.E. Uveal melanoma: Location, size, cell type, and enucleation as risk factors in metastasis. Hum. Pathol. 1982;13:123–132. doi: 10.1016/S0046-8177(82)80116-0. [DOI] [PubMed] [Google Scholar]
- 81.Albert D.M., Diener-West M., Robinson N.L., Grossniklaus H.E., Green W.R., Vine A.K., Willis J., Frueh B., Kurtz R.M., Elner S., et al. Histopathologic characteristics of uveal melanomas in eyes enucleated from the Collaborative Ocular Melanoma Study COMS report no. 6. Am. J. Ophthalmol. 1998;125:745–766. doi: 10.1016/s0002-9394(98)00040-3. [DOI] [PubMed] [Google Scholar]
- 82.Singh M., Durairaj P., Yeung J. Uveal Melanoma: A Review of the Literature. Oncol. Ther. 2018;6:87–104. doi: 10.1007/s40487-018-0056-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Barnhill R.L., Ye M., Batistella A., Stern M.H., Roman-Roman S., Dendale R., Lantz O., Piperno-Neumann S., Desjardins L., Cassoux N., et al. The biological and prognostic significance of angiotropism in uveal melanoma. Lab. Investig. 2017;97:746–759. doi: 10.1038/labinvest.2017.16. [DOI] [PubMed] [Google Scholar]
- 84.Coupland S.E., Campbell I., Damato B. Routes of extraocular extension of uveal melanoma: Risk factors and influence on survival probability. Ophthalmology. 2008;115:1778–1785. doi: 10.1016/j.ophtha.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 85.Force A.O.O.T. International Validation of the American Joint Committee on Cancer’s 7th Edition Classification of Uveal Melanoma. JAMA Ophthalmol. 2015;133:376–383. doi: 10.1001/jamaophthalmol.2014.5395. [DOI] [PubMed] [Google Scholar]
- 86.Coleman K., Baak J.P., Van Diest P., Mullaney J., Farrell M., Fenton M. Prognostic factors following enucleation of 111 uveal melanomas. Br. J. Ophthalmol. 1993;77:688–692. doi: 10.1136/bjo.77.11.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Damato B., Dopierala J.A., Coupland S.E. Genotypic profiling of 452 choroidal melanomas with multiplex ligation-dependent probe amplification. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2010;16:6083–6092. doi: 10.1158/1078-0432.CCR-10-2076. [DOI] [PubMed] [Google Scholar]
- 88.Ly L.V., Odish O.F., Wolff-Rouendaal D., Missotten G.S., Luyten G.P., Jager M.J. Intravascular presence of tumor cells as prognostic parameter in uveal melanoma: A 35-year survey. Investig. Ophthalmol. Vis. Sci. 2010;51:658–665. doi: 10.1167/iovs.09-3824. [DOI] [PubMed] [Google Scholar]
- 89.Van Beek J.G., Koopmans A.E., Vaarwater J., de Rooi J.J., Paridaens D., Naus N.C., de Klein A., Verdijk R.M., Kilic E. The prognostic value of extraocular extension in relation to monosomy 3 and gain of chromosome 8q in uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2014;55:1284–1291. doi: 10.1167/iovs.13-13670. [DOI] [PubMed] [Google Scholar]
- 90.Lattman J., Kroll S., Char D.H., Ghazvini S., Frigillana H., O’Brien J.M., Elbakri H.R. Cell cycling and prognosis in uveal melanoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 1995;1:41–47. [PubMed] [Google Scholar]
- 91.Angi M., Damato B., Kalirai H., Dodson A., Taktak A., Coupland S.E. Immunohistochemical assessment of mitotic count in uveal melanoma. Acta Ophthalmol. 2011;89:e155–e160. doi: 10.1111/j.1755-3768.2009.01769.x. [DOI] [PubMed] [Google Scholar]
- 92.Foss A.J., Alexander R.A., Jefferies L.W., Hungerford J.L., Harris A.L., Lightman S. Microvessel count predicts survival in uveal melanoma. Cancer Res. 1996;56:2900–2903. [PubMed] [Google Scholar]
- 93.Makitie T., Summanen P., Tarkkanen A., Kivela T. Microvascular density in predicting survival of patients with choroidal and ciliary body melanoma. Investig. Ophthalmol. Vis. Sci. 1999;40:2471–2480. [PubMed] [Google Scholar]
- 94.De la Cruz Jr P.O., Specht C.S., McLean I.W. Lymphocytic infiltration in uveal malignant melanoma. Cancer. 1990;65:112–115. doi: 10.1002/1097-0142(19900101)65:1<112::AID-CNCR2820650123>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 95.Whelchel J.C., Farah S.E., McLean I.W., Burnier M.N. Immunohistochemistry of infiltrating lymphocytes in uveal malignant melanoma. Investig. Ophthalmol. Vis. Sci. 1993;34:2603–2606. [PubMed] [Google Scholar]
- 96.Makitie T., Summanen P., Tarkkanen A., Kivela T. Tumor-infiltrating macrophages (CD68(+) cells) and prognosis in malignant uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2001;42:1414–1421. [PubMed] [Google Scholar]
- 97.Bronkhorst I.H., Ly L.V., Jordanova E.S., Vrolijk J., Versluis M., Luyten G.P., Jager M.J. Detection of M2-macrophages in uveal melanoma and relation with survival. Investig. Ophthalmol. Vis. Sci. 2011;52:643–650. doi: 10.1167/iovs.10-5979. [DOI] [PubMed] [Google Scholar]
- 98.Keung E.Z., Gershenwald J.E. The eighth edition American Joint Committee on Cancer (AJCC) melanoma staging system: Implications for melanoma treatment and care. Expert Rev. Anticancer. Ther. 2018;18:775–784. doi: 10.1080/14737140.2018.1489246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shah A.A., Bourne T.D., Murali R. BAP1 protein loss by immunohistochemistry: A potentially useful tool for prognostic prediction in patients with uveal melanoma. Pathology. 2013;45:651–656. doi: 10.1097/PAT.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 100.Koopmans A.E., Verdijk R.M., Brouwer R.W., van den Bosch T.P., van den Berg M.M., Vaarwater J., Kockx C.E., Paridaens D., Naus N.C., Nellist M., et al. Clinical significance of immunohistochemistry for detection of BAP1 mutations in uveal melanoma. Mod. Pathol. Off. J. United States Can. Acad. Pathol. Inc. 2014;27:1321–1330. doi: 10.1038/modpathol.2014.43. [DOI] [PubMed] [Google Scholar]
- 101.Kalirai H., Dodson A., Faqir S., Damato B.E., Coupland S.E. Lack of BAP1 protein expression in uveal melanoma is associated with increased metastatic risk and has utility in routine prognostic testing. Br. J. Cancer. 2014;111:1373–1380. doi: 10.1038/bjc.2014.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Smit K.N., van Poppelen N.M., Vaarwater J., Verdijk R., van Marion R., Kalirai H., Coupland S.E., Thornton S., Farquhar N., Dubbink H.J., et al. Combined mutation and copy-number variation detection by targeted next-generation sequencing in uveal melanoma. Mod. Pathol. Off. J. United States Can. Acad. Pathol. Inc. 2018;31:763–771. doi: 10.1038/modpathol.2017.187. [DOI] [PubMed] [Google Scholar]
- 103.Field M.G., Decatur C.L., Kurtenbach S., Gezgin G., van der Velden P.A., Jager M.J., Kozak K.N., Harbour J.W. PRAME as an Independent Biomarker for Metastasis in Uveal Melanoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2016;22:1234–1242. doi: 10.1158/1078-0432.CCR-15-2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Field M.G., Durante M.A., Decatur C.L., Tarlan B., Oelschlager K.M., Stone J.F., Kuznetsov J., Bowcock A.M., Kurtenbach S., Harbour J.W. Epigenetic reprogramming and aberrant expression of PRAME are associated with increased metastatic risk in Class 1 and Class 2 uveal melanomas. Oncotarget. 2016;7:59209–59219. doi: 10.18632/oncotarget.10962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cai L., Paez-Escamilla M., Walter S.D., Tarlan B., Decatur C.L., Perez B.M., Harbour J.W. Gene Expression Profiling and PRAME Status Versus Tumor-Node-Metastasis Staging for Prognostication in Uveal Melanoma. Am. J. Ophthalmol. 2018;195:154–160. doi: 10.1016/j.ajo.2018.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schefler A.C., Koca E., Bernicker E.H., Correa Z.M. Relationship between clinical features, GEP class, and PRAME expression in uveal melanoma. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019;257:1541–1545. doi: 10.1007/s00417-019-04335-w. [DOI] [PubMed] [Google Scholar]
- 107.Prescher G., Bornfeld N., Horsthemke B., Becher R. Chromosomal aberrations defining uveal melanoma of poor prognosis. Lancet. 1992;339:691–692. doi: 10.1016/0140-6736(92)90861-V. [DOI] [PubMed] [Google Scholar]
- 108.Horsman D.E., Sroka H., Rootman J., White V.A. Monosomy 3 and isochromosome 8q in a uveal melanoma. Cancer Genet. Cytogenet. 1990;45:249–253. doi: 10.1016/0165-4608(90)90090-W. [DOI] [PubMed] [Google Scholar]
- 109.Prescher G., Bornfeld N., Becher R. Nonrandom chromosomal abnormalities in primary uveal melanoma. J. Natl. Cancer Inst. 1990;82:1765–1769. doi: 10.1093/jnci/82.22.1765. [DOI] [PubMed] [Google Scholar]
- 110.Onken M.D., Worley L.A., Ehlers J.P., Harbour J.W. Gene expression profiling in uveal melanoma reveals two molecular classes and predicts metastatic death. Cancer Res. 2004;64:7205–7209. doi: 10.1158/0008-5472.CAN-04-1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Onken M.D., Worley L.A., Tuscan M.D., Harbour J.W. An accurate, clinically feasible multi-gene expression assay for predicting metastasis in uveal melanoma. J. Mol. Diagn. JMD. 2010;12:461–468. doi: 10.2353/jmoldx.2010.090220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Onken M.D., Worley L.A., Char D.H., Augsburger J.J., Correa Z.M., Nudleman E., Aaberg T.M., Jr., Altaweel M.M., Bardenstein D.S., Finger P.T., et al. Collaborative Ocular Oncology Group report number 1: Prospective validation of a multi-gene prognostic assay in uveal melanoma. Ophthalmology. 2012;119:1596–1603. doi: 10.1016/j.ophtha.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Aaberg T.M., Covington K.R., Tsai T., Shildkrot Y., Plasseraud K.M., Alsina K.M., Oelschlager K.M., Monzon F.A. Gene Expression Profiling in Uveal Melanoma: Five-Year Prospective Outcomes and Meta-Analysis. Ocul. Oncol. Pathol. 2020;6:360–367. doi: 10.1159/000508382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kashyap S., Meel R., Singh L., Singh M. Uveal melanoma. Semin. Diagn. Pathol. 2016;33:141–147. doi: 10.1053/j.semdp.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 115.Onken M.D., Blumer K.J., Cooper J.A. Uveal melanoma cells use ameboid and mesenchymal mechanisms of cell motility crossing the endothelium. Mol. Biol. Cell. 2021;32:413–421. doi: 10.1091/mbc.E20-04-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dithmar S., Diaz C.E., Grossniklaus H.E. Intraocular melanoma spread to regional lymph nodes: Report of two cases. Retina. 2000;20:76–79. doi: 10.1097/00006982-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 117.Van Beek J.G.M., van den Bosch Q.C.C., Naus N., Paridaens D., de Klein A., Kilic E., Verdijk R.M. Absence of Intraocular Lymphatic Vessels in Uveal Melanomas with Extrascleral Growth. Cancers. 2019;11:228. doi: 10.3390/cancers11020228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Brouwer N.J., Gezgin G., Wierenga A.P.A., Bronkhorst I.H.G., Marinkovic M., Luyten G.P.M., Versluis M., Kroes W.G.M., van der Velden P.A., Verdijk R.M., et al. Tumour Angiogenesis in Uveal Melanoma Is Related to Genetic Evolution. Cancers. 2019;11:979. doi: 10.3390/cancers11070979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Taylor A.W. Ocular immune privilege. Eye. 2009;23:1885–1889. doi: 10.1038/eye.2008.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Taylor A.W. Ocular Immune Privilege and Transplantation. Front. Immunol. 2016;7:37. doi: 10.3389/fimmu.2016.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kuchle M., Nguyen N.X., Naumann G.O. Quantitative assessment of the blood-aqueous barrier in human eyes with malignant or benign uveal tumors. Am. J. Ophthalmol. 1994;117:521–528. doi: 10.1016/S0002-9394(14)70015-7. [DOI] [PubMed] [Google Scholar]
- 122.Bronkhorst I.H., Jager M.J. Inflammation in uveal melanoma. Eye. 2013;27:217–223. doi: 10.1038/eye.2012.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wessely A., Steeb T., Erdmann M., Heinzerling L., Vera J., Schlaak M., Berking C., Heppt M.V. The Role of Immune Checkpoint Blockade in Uveal Melanoma. Int. J. Mol. Sci. 2020;21:879. doi: 10.3390/ijms21030879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zane K.E., Cloyd J.M., Mumtaz K.S., Wadhwa V., Makary M.S. Metastatic disease to the liver: Locoregional therapy strategies and outcomes. World J. Clin. Oncol. 2021;12:725–745. doi: 10.5306/wjco.v12.i9.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hoppener D.J., Grunhagen D.J., Eggermont A.M.M., van der Veldt A.A.M., Verhoef C. An Overview of Liver Directed Locoregional Therapies. Surg. Oncol. Clin. 2021;30:103–123. doi: 10.1016/j.soc.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 126.Bakhoum M.F., Curtis E.J., Goldbaum M.H., Mischel P.S. BAP1 methylation: A prognostic marker of uveal melanoma metastasis. NPJ Precis. Oncol. 2021;5:89. doi: 10.1038/s41698-021-00226-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Uner O.E., See T.R.O., Szalai E., Grossniklaus H.E., Stalhammar G. Estimation of the timing of BAP1 mutation in uveal melanoma progression. Sci. Rep. 2021;11:8923. doi: 10.1038/s41598-021-88390-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ikeda H., Lethe B., Lehmann F., van Baren N., Baurain J.F., de Smet C., Chambost H., Vitale M., Moretta A., Boon T., et al. Characterization of an antigen that is recognized on a melanoma showing partial HLA loss by CTL expressing an NK inhibitory receptor. Immunity. 1997;6:199–208. doi: 10.1016/S1074-7613(00)80426-4. [DOI] [PubMed] [Google Scholar]
- 129.Lezcano C., Jungbluth A.A., Nehal K.S., Hollmann T.J., Busam K.J. PRAME Expression in Melanocytic Tumors. Am. J. Surg. Pathol. 2018;42:1456–1465. doi: 10.1097/PAS.0000000000001134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sekoranja D., Hawlina G., Pizem J. PRAME expression in melanocytic lesions of the conjunctiva. Histopathology. 2021;79:989–996. doi: 10.1111/his.14452. [DOI] [PubMed] [Google Scholar]
- 131.Epping M.T., Hart A.A., Glas A.M., Krijgsman O., Bernards R. PRAME expression and clinical outcome of breast cancer. Br. J. Cancer. 2008;99:398–403. doi: 10.1038/sj.bjc.6604494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Szczepanski M.J., DeLeo A.B., Luczak M., Molinska-Glura M., Misiak J., Szarzynska B., Dworacki G., Zagor M., Rozwadowska N., Kurpisz M., et al. PRAME expression in head and neck cancer correlates with markers of poor prognosis and might help in selecting candidates for retinoid chemoprevention in pre-malignant lesions. Oral Oncol. 2013;49:144–151. doi: 10.1016/j.oraloncology.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Oberthuer A., Hero B., Spitz R., Berthold F., Fischer M. The tumor-associated antigen PRAME is universally expressed in high-stage neuroblastoma and associated with poor outcome. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2004;10:4307–4313. doi: 10.1158/1078-0432.CCR-03-0813. [DOI] [PubMed] [Google Scholar]
- 134.Tan P., Zou C., Yong B., Han J., Zhang L., Su Q., Yin J., Wang J., Huang G., Peng T., et al. Expression and prognostic relevance of PRAME in primary osteosarcoma. Biochem. Biophys. Res. Commun. 2012;419:801–808. doi: 10.1016/j.bbrc.2012.02.110. [DOI] [PubMed] [Google Scholar]
- 135.Prescher G., Bornfeld N., Hirche H., Horsthemke B., Jockel K.H., Becher R. Prognostic implications of monosomy 3 in uveal melanoma. Lancet. 1996;347:1222–1225. doi: 10.1016/s0140-6736(96)90736-9. [DOI] [PubMed] [Google Scholar]
- 136.Kilic E., Naus N.C., van Gils W., Klaver C.C., van Til M.E., Verbiest M.M., Stijnen T., Mooy C.M., Paridaens D., Beverloo H.B., et al. Concurrent loss of chromosome arm 1p and chromosome 3 predicts a decreased disease-free survival in uveal melanoma patients. Investig. Ophthalmol. Vis. Sci. 2005;46:2253–2257. doi: 10.1167/iovs.04-1460. [DOI] [PubMed] [Google Scholar]
- 137.Hausler T., Stang A., Anastassiou G., Jockel K.H., Mrzyk S., Horsthemke B., Lohmann D.R., Zeschnigk M. Loss of heterozygosity of 1p in uveal melanomas with monosomy 3. Int. J. Cancer. 2005;116:909–913. doi: 10.1002/ijc.21086. [DOI] [PubMed] [Google Scholar]
- 138.Dogrusoz M., Jager M.J. Genetic prognostication in uveal melanoma. Acta Ophthalmol. 2018;96:331–347. doi: 10.1111/aos.13580. [DOI] [PubMed] [Google Scholar]
- 139.Honavar S.G. Genetics of uveal melanoma—Breed is stronger than pasture. Indian J. Ophthalmol. 2021;69:1643–1644. doi: 10.4103/ijo.IJO_1611_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.See T.R., Stalhammar G., Phillips S., Grossniklaus H.E. BAP1 Immunoreactivity Correlates with Gene Expression Class in Uveal Melanoma. Ocul. Oncol. Pathol. 2020;6:129–137. doi: 10.1159/000502550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Petrausch U., Martus P., Tonnies H., Bechrakis N.E., Lenze D., Wansel S., Hummel M., Bornfeld N., Thiel E., Foerster M.H., et al. Significance of gene expression analysis in uveal melanoma in comparison to standard risk factors for risk assessment of subsequent metastases. Eye. 2008;22:997–1007. doi: 10.1038/sj.eye.6702779. [DOI] [PubMed] [Google Scholar]
- 142.Correa Z.M., Augsburger J.J. Independent Prognostic Significance of Gene Expression Profile Class and Largest Basal Diameter of Posterior Uveal Melanomas. Am. J. Ophthalmol. 2016;162:20–27.e1. doi: 10.1016/j.ajo.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 143.DeParis S.W., Taktak A., Eleuteri A., Enanoria W., Heimann H., Coupland S.E., Damato B. External Validation of the Liverpool Uveal Melanoma Prognosticator Online. Investig. Ophthalmol. Vis. Sci. 2016;57:6116–6122. doi: 10.1167/iovs.16-19654. [DOI] [PubMed] [Google Scholar]
- 144.Laurent C., Valet F., Planque N., Silveri L., Maacha S., Anezo O., Hupe P., Plancher C., Reyes C., Albaud B., et al. High PTP4A3 phosphatase expression correlates with metastatic risk in uveal melanoma patients. Cancer Res. 2011;71:666–674. doi: 10.1158/0008-5472.CAN-10-0605. [DOI] [PubMed] [Google Scholar]
- 145.Gangemi R., Mirisola V., Barisione G., Fabbi M., Brizzolara A., Lanza F., Mosci C., Salvi S., Gualco M., Truini M., et al. Mda-9/syntenin is expressed in uveal melanoma and correlates with metastatic progression. PLoS ONE. 2012;7:e29989. doi: 10.1371/journal.pone.0029989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Worley L.A., Onken M.D., Person E., Robirds D., Branson J., Char D.H., Perry A., Harbour J.W. Transcriptomic versus chromosomal prognostic markers and clinical outcome in uveal melanoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2007;13:1466–1471. doi: 10.1158/1078-0432.CCR-06-2401. [DOI] [PubMed] [Google Scholar]
- 147.Van Essen T.H., van Pelt S.I., Bronkhorst I.H., Versluis M., Nemati F., Laurent C., Luyten G.P., van Hall T., van den Elsen P.J., van der Velden P.A., et al. Upregulation of HLA Expression in Primary Uveal Melanoma by Infiltrating Leukocytes. PLoS ONE. 2016;11:e0164292. doi: 10.1371/journal.pone.0164292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wan Q., Tang J., Han Y., Wang D. Co-expression modules construction by WGCNA and identify potential prognostic markers of uveal melanoma. Exp. Eye Res. 2018;166:13–20. doi: 10.1016/j.exer.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 149.Xue M., Shang J., Chen B., Yang Z., Song Q., Sun X., Chen J., Yang J. Identification of Prognostic Signatures for Predicting the Overall Survival of Uveal Melanoma Patients. J. Cancer. 2019;10:4921–4931. doi: 10.7150/jca.30618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ni Y., Zhang Z., Chen G., Long W., Tong L., Zeng J. Integrated analyses identify potential prognostic markers for uveal melanoma. Exp. Eye Res. 2019;187:107780. doi: 10.1016/j.exer.2019.107780. [DOI] [PubMed] [Google Scholar]
- 151.Choi S., Ha M., Lee J.S., Heo H.J., Kim G.H., Oh S.O., Lee J.J., Goh T.S., Kim Y.H. Novel Prognostic Factor for Uveal Melanoma: Bioinformatics Analysis of Three Independent Cohorts. Anticancer. Res. 2020;40:3839–3846. doi: 10.21873/anticanres.14373. [DOI] [PubMed] [Google Scholar]
- 152.Luo H., Ma C., Shao J., Cao J. Prognostic Implications of Novel Ten-Gene Signature in Uveal Melanoma. Front. Oncol. 2020;10:567512. doi: 10.3389/fonc.2020.567512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wan Q., Tang J., Lu J., Jin L., Su Y., Wang S., Cheng Y., Liu Y., Li C., Wang Z. Six-gene-based prognostic model predicts overall survival in patients with uveal melanoma. Cancer Biomark. Sect. A Dis. Markers. 2020;27:343–356. doi: 10.3233/CBM-190825. [DOI] [PubMed] [Google Scholar]
- 154.Tang Z., Cai K. A Novel 8-Gene Prognostic Signature for Survival Prediction of Uveal Melanoma. Anal. Cell. Pathol. 2021;2021:6693219. doi: 10.1155/2021/6693219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Liu J., Lu J., Li W. A Comprehensive Prognostic and Immunological Analysis of a Six-Gene Signature Associated With Glycolysis and Immune Response in Uveal Melanoma. Front. Immunol. 2021;12:738068. doi: 10.3389/fimmu.2021.738068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhang B., Horvath S. A general framework for weighted gene co-expression network analysis. Stat. Appl. Genet. Mol. Biol. 2005;4 doi: 10.2202/1544-6115.1128. [DOI] [PubMed] [Google Scholar]
- 157.Langfelder P., Horvath S. Eigengene networks for studying the relationships between co-expression modules. BMC Syst. Biol. 2007;1:54. doi: 10.1186/1752-0509-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Langfelder P., Horvath S. WGCNA: An R package for weighted correlation network analysis. BMC Bioinform. 2008;9:559. doi: 10.1186/1471-2105-9-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sato K., Mano T., Matsuda H., Senda M., Ihara R., Suzuki K., Arai H., Ishii K., Ito K., Ikeuchi T., et al. Visualizing modules of coordinated structural brain atrophy during the course of conversion to Alzheimer’s disease by applying methodology from gene co-expression analysis. NeuroImage. Clin. 2019;24:101957. doi: 10.1016/j.nicl.2019.101957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Saris C.G., Horvath S., van Vught P.W., van Es M.A., Blauw H.M., Fuller T.F., Langfelder P., DeYoung J., Wokke J.H., Veldink J.H., et al. Weighted gene co-expression network analysis of the peripheral blood from Amyotrophic Lateral Sclerosis patients. BMC Genom. 2009;10:405. doi: 10.1186/1471-2164-10-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Xie Y., Luo X., He H., Tang M. Novel Insight Into the Role of Immune Dysregulation in Amyotrophic Lateral Sclerosis Based on Bioinformatic Analysis. Front. Neurosci. 2021;15:657465. doi: 10.3389/fnins.2021.657465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ren J., Yang Y., Li C., Xie L., Hu R., Qin X., Zhang M. A Novel Prognostic Model of Early-Stage Lung Adenocarcinoma Integrating Methylation and Immune Biomarkers. Front. Genet. 2020;11:634634. doi: 10.3389/fgene.2020.634634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Niemira M., Collin F., Szalkowska A., Bielska A., Chwialkowska K., Reszec J., Niklinski J., Kwasniewski M., Kretowski A. Molecular Signature of Subtypes of Non-Small-Cell Lung Cancer by Large-Scale Transcriptional Profiling: Identification of Key Modules and Genes by Weighted Gene Co-Expression Network Analysis (WGCNA) Cancers. 2019;12:37. doi: 10.3390/cancers12010037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Cheng Y., Liu C., Liu Y., Su Y., Wang S., Jin L., Wan Q., Liu Y., Li C., Sang X., et al. Immune Microenvironment Related Competitive Endogenous RNA Network as Powerful Predictors for Melanoma Prognosis Based on WGCNA Analysis. Front. Oncol. 2020;10:577072. doi: 10.3389/fonc.2020.577072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Shi Z., Derow C.K., Zhang B. Co-expression module analysis reveals biological processes, genomic gain, and regulatory mechanisms associated with breast cancer progression. BMC Syst. Biol. 2010;4:74. doi: 10.1186/1752-0509-4-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Karami H., Derakhshani A., Ghasemigol M., Fereidouni M., Miri-Moghaddam E., Baradaran B., Tabrizi N.J., Najafi S., Solimando A.G., Marsh L.M., et al. Weighted Gene Co-Expression Network Analysis Combined with Machine Learning Validation to Identify Key Modules and Hub Genes Associated with SARS-CoV-2 Infection. J. Clin. Med. 2021;10:3567. doi: 10.3390/jcm10163567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Zhao W., Langfelder P., Fuller T., Dong J., Li A., Hovarth S. Weighted gene coexpression network analysis: State of the art. J. Biopharm. Stat. 2010;20:281–300. doi: 10.1080/10543400903572753. [DOI] [PubMed] [Google Scholar]
- 168.Xu J., Bankov G., Kim M., Wretlind A., Lord J., Green R., Hodges A., Hye A., Aarsland D., Velayudhan L., et al. Integrated lipidomics and proteomics network analysis highlights lipid and immunity pathways associated with Alzheimer’s disease. Transl. Neurodegener. 2020;9:36. doi: 10.1186/s40035-020-00215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Pei G., Chen L., Zhang W. WGCNA Application to Proteomic and Metabolomic Data Analysis. Methods Enzymol. 2017;585:135–158. doi: 10.1016/bs.mie.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 170.Coupland S.E., Anastassiou G., Stang A., Schilling H., Anagnostopoulos I., Bornfeld N., Stein H. The prognostic value of cyclin D1, p53, and MDM2 protein expression in uveal melanoma. J. Pathol. 2000;191:120–126. doi: 10.1002/(SICI)1096-9896(200006)191:2<120::AID-PATH591>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 171.Liu Y., Li M., Shi D., Zhu Y. Higher expression of cation transport regulator-like protein 1 (CHAC1) predicts of poor outcomes in uveal melanoma (UM) patients. Int. Ophthalmol. 2019;39:2825–2832. doi: 10.1007/s10792-019-01129-1. [DOI] [PubMed] [Google Scholar]
- 172.Wong S.C., Lo E.S., Lee K.C., Chan J.K., Hsiao W.L. Prognostic and diagnostic significance of beta-catenin nuclear immunostaining in colorectal cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2004;10:1401–1408. doi: 10.1158/1078-0432.CCR-0157-03. [DOI] [PubMed] [Google Scholar]
- 173.Bian J., Dannappel M., Wan C., Firestein R. Transcriptional Regulation of Wnt/beta-Catenin Pathway in Colorectal Cancer. Cells. 2020;9:2125. doi: 10.3390/cells9092125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Tetsu O., McCormick F. Beta-catenin regulates expression of cyclin D1 in colon carcinoma cells. Nature. 1999;398:422–426. doi: 10.1038/18884. [DOI] [PubMed] [Google Scholar]
- 175.De La Coste A., Romagnolo B., Billuart P., Renard C.A., Buendia M.A., Soubrane O., Fabre M., Chelly J., Beldjord C., Kahn A., et al. Somatic mutations of the beta-catenin gene are frequent in mouse and human hepatocellular carcinomas. Proc. Natl. Acad. Sci. USA. 1998;95:8847–8851. doi: 10.1073/pnas.95.15.8847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Miyoshi Y., Iwao K., Nagasawa Y., Aihara T., Sasaki Y., Imaoka S., Murata M., Shimano T., Nakamura Y. Activation of the beta-catenin gene in primary hepatocellular carcinomas by somatic alterations involving exon 3. Cancer Res. 1998;58:2524–2527. [PubMed] [Google Scholar]
- 177.Khalaf A.M., Fuentes D., Morshid A.I., Burke M.R., Kaseb A.O., Hassan M., Hazle J.D., Elsayes K.M. Role of Wnt/beta-catenin signaling in hepatocellular carcinoma, pathogenesis, and clinical significance. J. Hepatocell. Carcinoma. 2018;5:61–73. doi: 10.2147/JHC.S156701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kageshita T., Hamby C.V., Ishihara T., Matsumoto K., Saida T., Ono T. Loss of beta-catenin expression associated with disease progression in malignant melanoma. Br. J. Dermatol. 2001;145:210–216. doi: 10.1046/j.1365-2133.2001.04336.x. [DOI] [PubMed] [Google Scholar]
- 179.Gajos-Michniewicz A., Czyz M. WNT Signaling in Melanoma. Int. J. Mol. Sci. 2020;21:4852. doi: 10.3390/ijms21144852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Kovacs D., Migliano E., Muscardin L., Silipo V., Catricala C., Picardo M., Bellei B. The role of Wnt/beta-catenin signaling pathway in melanoma epithelial-to-mesenchymal-like switching: Evidences from patients-derived cell lines. Oncotarget. 2016;7:43295–43314. doi: 10.18632/oncotarget.9232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.McKenney J.K., Hornick J.L. Immunohistochemistry in Surgical Pathology. Adv. Anat. Pathol. 2018;25:373. doi: 10.1097/PAP.0000000000000212. [DOI] [PubMed] [Google Scholar]
- 182.Taylor C.R. Immunohistochemistry in surgical pathology: Principles and practice. Methods Mol. Biol. 2014;1180:81–109. doi: 10.1007/978-1-4939-1050-2_5. [DOI] [PubMed] [Google Scholar]
- 183.Farquhar N., Thornton S., Coupland S.E., Coulson J.M., Sacco J.J., Krishna Y., Heimann H., Taktak A., Cebulla C.M., Abdel-Rahman M.H., et al. Patterns of BAP1 protein expression provide insights into prognostic significance and the biology of uveal melanoma. J. Pathology. Clin. Res. 2018;4:26–38. doi: 10.1002/cjp2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Broggi G., Musumeci G., Puzzo L., Russo A., Reibaldi M., Ragusa M., Longo A., Caltabiano R. Immunohistochemical Expression of ABCB5 as a Potential Prognostic Factor in Uveal Melanoma. Appl. Sci. 2019;9:1316. doi: 10.3390/app9071316. [DOI] [Google Scholar]
- 185.Tura A., Thieme C., Brosig A., Merz H., Ranjbar M., Vardanyan S., Zuo H., Maassen T., Kakkassery V., Grisanti S. Lower Levels of Adiponectin and Its Receptor Adipor1 in the Uveal Melanomas With Monosomy-3. Investig. Ophthalmol. Vis. Sci. 2020;61:12. doi: 10.1167/iovs.61.5.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kashyap S., Jha J., Singh M.K., Singh L., Sen S., Kaur J., Bajaj M.S., Pushker N. DNA damage response proteins and its role in tumor progression of uveal melanoma with patient outcome. Clin. Transl. Oncol. Off. Publ. Fed. Span. Oncol. Soc. Natl. Cancer Inst. Mex. 2020;22:1472–1480. doi: 10.1007/s12094-019-02281-x. [DOI] [PubMed] [Google Scholar]
- 187.Jha J., Singh M.K., Singh L., Pushker N., Bajaj M.S., Sen S., Kashyap S. Prognostic relevance of ATM protein in uveal melanoma and its association with clinicopathological factors. Int. J. Clin. Oncol. 2019;24:1526–1535. doi: 10.1007/s10147-019-01519-6. [DOI] [PubMed] [Google Scholar]
- 188.Broggi G., Ieni A., Russo D., Varricchio S., Puzzo L., Russo A., Reibaldi M., Longo A., Tuccari G., Staibano S., et al. The Macro-Autophagy-Related Protein Beclin-1 Immunohistochemical Expression Correlates With Tumor Cell Type and Clinical Behavior of Uveal Melanoma. Front. Oncol. 2020;10:589849. doi: 10.3389/fonc.2020.589849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Jiang Z., Yu F., Li M. Upregulation of BCL2 19 kD Protein-Interacting Protein 3 (BNIP3) is Predictive of Unfavorable Prognosis in Uveal Melanoma. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2018;24:4711–4717. doi: 10.12659/MSM.907679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Jiang Z., Liu F. Butyrophilin-Like 9 (BTNL9) Suppresses Invasion and Correlates with Favorable Prognosis of Uveal Melanoma. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019;25:3190–3198. doi: 10.12659/MSM.914074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Singh M.K., Singh L., Pushker N., Chosdol K., Bakhshi S., Meel R., Sen S., Kashyap S. Constitutive expression of c-REL in uveal melanoma patients: Correlation with clinicopathological parameters and patient outcome. Clin. Transl. Oncol. Off. Publ. Fed. Span. Oncol. Soc. Natl. Cancer Inst. Mex. 2020;22:1193–1204. doi: 10.1007/s12094-019-02247-z. [DOI] [PubMed] [Google Scholar]
- 192.Gajdzis M., Theocharis S., Gajdzis P., Cassoux N., Gardrat S., Donizy P., Klijanienko J., Kaczmarek R. Ephrin Receptors (Eph): EphA1, EphA5, and EphA7 Expression in Uveal Melanoma-Associations with Clinical Parameters and Patient Survival. Life. 2020;10:225. doi: 10.3390/life10100225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Levidou G., Gajdzis P., Cassoux N., Donizy P., Masaoutis C., Gajdzis M., Gardrat S., Pergaris A., Danas E., Klijanienko J., et al. Histone Deacetylase (HDAC)-1, -2, -4, and -6 in Uveal Melanomas: Associations with Clinicopathological Parameters and Patients’ Survival. Cancers. 2021;13:4763. doi: 10.3390/cancers13194763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Djirackor L., Shakir D., Kalirai H., Petrovski G., Coupland S.E. Nestin expression in primary and metastatic uveal melanoma—Possible biomarker for high-risk uveal melanoma. Acta Ophthalmol. 2018;96:503–509. doi: 10.1111/aos.13645. [DOI] [PubMed] [Google Scholar]
- 195.Singh M.K., Singh L., Pushker N., Saini N., Meel R., Chosdol K., Bakhshi S., Sen S., Venkatesh P., Chawla B., et al. Identification of canonical NFkappaB (C-NFkappaB) pathway in uveal melanoma and their relation with patient outcome. Clin. Exp. Metastasis. 2019;36:271–290. doi: 10.1007/s10585-019-09969-y. [DOI] [PubMed] [Google Scholar]
- 196.Singh M.K., Singh L., Chosdol K., Pushker N., Saini N., Meel R., Bakhshi S., Sen S., Kashyap S. Differential expression of p52 and RelB proteins in the metastatic and non-metastatic groups of uveal melanoma with patient outcome. J. Cancer Res. Clin. Oncol. 2019;145:2969–2982. doi: 10.1007/s00432-019-03052-5. [DOI] [PubMed] [Google Scholar]
- 197.Gajdzis M., Theocharis S., Klijanienko J., Cassoux N., Gardrat S., Donizy P., Kaczmarek R., Gajdzis P. The Prognostic Values of PARP-1 Expression in Uveal Melanoma. Cells. 2021;10:285. doi: 10.3390/cells10020285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Jiang Z., Yan Y., Dong J., Duan L. PD-1 expression on uveal melanoma induces tumor proliferation and predicts poor patient survival. Int. J. Biol. Markers. 2020;35:50–58. doi: 10.1177/1724600820943610. [DOI] [PubMed] [Google Scholar]
- 199.Singh L., Singh M.K., Kenney M.C., Jager M.J., Rizvi M.A., Meel R., Lomi N., Bakhshi S., Sen S., Kashyap S. Prognostic significance of PD-1/PD-L1 expression in uveal melanoma: Correlation with tumor-infiltrating lymphocytes and clinicopathological parameters. Cancer Immunol. Immunother. CII. 2021;70:1291–1303. doi: 10.1007/s00262-020-02773-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Berus T., Markiewicz A., Kobylinska K., Biecek P., Orlowska-Heitzman J., Romanowska-Dixon B., Donizy P. Downregulation of Polo-like kinase-1 (PLK-1) expression is associated with poor clinical outcome in uveal melanoma patients. Folia Histochem. Cytobiol. 2020;58:108–116. doi: 10.5603/FHC.a2020.0017. [DOI] [PubMed] [Google Scholar]
- 201.Ramasamy P., Larkin A.M., Linge A., Tiernan D., McAree F., Horgan N., Moriarty P., Beatty S., Murphy C.C., Clynes M., et al. PRDX3 is associated with metastasis and poor survival in uveal melanoma. J. Clin. Pathol. 2020;73:408–412. doi: 10.1136/jclinpath-2019-206173. [DOI] [PubMed] [Google Scholar]
- 202.Salvatorelli L., Puzzo L., Russo A., Reibaldi M., Longo A., Ragusa M., Aldo C., Rappazzo G., Caltabiano R., Salemi M. Immunoexpression of SPANX-C in metastatic uveal melanoma. Pathol. Res. Pract. 2019;215:152431. doi: 10.1016/j.prp.2019.04.023. [DOI] [PubMed] [Google Scholar]
- 203.Kadioglu O., Saeed M.E.M., Munder M., Spuller A., Greten H.J., Efferth T. Effect of ABC transporter expression and mutational status on survival rates of cancer patients. Biomed. Pharmacother. 2020;131:110718. doi: 10.1016/j.biopha.2020.110718. [DOI] [PubMed] [Google Scholar]
- 204.Tangella L.P., Arooj M., Deplazes E., Gray E.S., Mancera R.L. Identification and characterisation of putative drug binding sites in human ATP-binding cassette B5 (ABCB5) transporter. Comput. Struct. Biotechnol. J. 2021;19:691–704. doi: 10.1016/j.csbj.2020.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Guo Q., Grimmig T., Gonzalez G., Giobbie-Hurder A., Berg G., Carr N., Wilson B.J., Banerjee P., Ma J., Gold J.S., et al. ATP-binding cassette member B5 (ABCB5) promotes tumor cell invasiveness in human colorectal cancer. J. Biol. Chem. 2018;293:11166–11178. doi: 10.1074/jbc.RA118.003187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Gambichler T., Petig A.L., Stockfleth E., Stucker M. Expression of SOX10, ABCB5 and CD271 in melanocytic lesions and correlation with survival data of patients with melanoma. Clin. Exp. Dermatol. 2016;41:709–716. doi: 10.1111/ced.12928. [DOI] [PubMed] [Google Scholar]
- 207.Wang S., Tang L., Lin J., Shen Z., Yao Y., Wang W., Tao S., Gu C., Ma J., Xie Y., et al. ABCB5 promotes melanoma metastasis through enhancing NF-kappaB p65 protein stability. Biochem. Biophys. Res. Commun. 2017;492:18–26. doi: 10.1016/j.bbrc.2017.08.052. [DOI] [PubMed] [Google Scholar]
- 208.Cheung S.T., Cheung P.F., Cheng C.K., Wong N.C., Fan S.T. Granulin-epithelin precursor and ATP-dependent binding cassette (ABC)B5 regulate liver cancer cell chemoresistance. Gastroenterology. 2011;140:344–355. doi: 10.1053/j.gastro.2010.07.049. [DOI] [PubMed] [Google Scholar]
- 209.Kleffel S., Lee N., Lezcano C., Wilson B.J., Sobolewski K., Saab K.R., Mueller H., Zhan Q., Posch C., Elco C.P., et al. ABCB5-Targeted Chemoresistance Reversal Inhibits Merkel Cell Carcinoma Growth. J. Investig. Dermatol. 2016;136:838–846. doi: 10.1016/j.jid.2015.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Chartrain M., Riond J., Stennevin A., Vandenberghe I., Gomes B., Lamant L., Meyer N., Gairin J.E., Guilbaud N., Annereau J.P. Melanoma chemotherapy leads to the selection of ABCB5-expressing cells. PLoS ONE. 2012;7:e36762. doi: 10.1371/journal.pone.0036762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Bueno R.C., Canevari R.A., Villacis R.A., Domingues M.A., Caldeira J.R., Rocha R.M., Drigo S.A., Rogatto S.R. ATM down-regulation is associated with poor prognosis in sporadic breast carcinomas. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2014;25:69–75. doi: 10.1093/annonc/mdt421. [DOI] [PubMed] [Google Scholar]
- 212.AlDubayan S.H., Giannakis M., Moore N.D., Han G.C., Reardon B., Hamada T., Mu X.J., Nishihara R., Qian Z., Liu L., et al. Inherited DNA-Repair Defects in Colorectal Cancer. Am. J. Hum. Genet. 2018;102:401–414. doi: 10.1016/j.ajhg.2018.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Petersen L.F., Klimowicz A.C., Otsuka S., Elegbede A.A., Petrillo S.K., Williamson T., Williamson C.T., Konno M., Lees-Miller S.P., Hao D., et al. Loss of tumour-specific ATM protein expression is an independent prognostic factor in early resected NSCLC. Oncotarget. 2017;8:38326–38336. doi: 10.18632/oncotarget.16215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Klionsky D.J., Abdel-Aziz A.K., Abdelfatah S., Abdellatif M., Abdoli A., Abel S., Abeliovich H., Abildgaard M.H., Abudu Y.P., Acevedo-Arozena A., et al. Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition) Autophagy. 2021;17:1–382. doi: 10.1080/15548627.2020.1797280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Mizushima N., Levine B. Autophagy in Human Diseases. N. Engl. J. Med. 2020;383:1564–1576. doi: 10.1056/NEJMra2022774. [DOI] [PubMed] [Google Scholar]
- 216.Amaravadi R.K., Kimmelman A.C., Debnath J. Targeting Autophagy in Cancer: Recent Advances and Future Directions. Cancer Discov. 2019;9:1167–1181. doi: 10.1158/2159-8290.CD-19-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Yun C.W., Jeon J., Go G., Lee J.H., Lee S.H. The Dual Role of Autophagy in Cancer Development and a Therapeutic Strategy for Cancer by Targeting Autophagy. Int. J. Mol. Sci. 2020;22:179. doi: 10.3390/ijms22010179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Rangel M., Kong J., Bhatt V., Khayati K., Guo J.Y. Autophagy and tumorigenesis. FEBS J. 2021 doi: 10.1111/febs.16125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Chourasia A.H., Macleod K.F. Tumor suppressor functions of BNIP3 and mitophagy. Autophagy. 2015;11:1937–1938. doi: 10.1080/15548627.2015.1085136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Ney P.A. Mitochondrial autophagy: Origins, significance, and role of BNIP3 and NIX. Biochim. Biophys. Acta. 2015;1853:2775–2783. doi: 10.1016/j.bbamcr.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 221.Chourasia A.H., Tracy K., Frankenberger C., Boland M.L., Sharifi M.N., Drake L.E., Sachleben J.R., Asara J.M., Locasale J.W., Karczmar G.S., et al. Mitophagy defects arising from BNip3 loss promote mammary tumor progression to metastasis. EMBO Rep. 2015;16:1145–1163. doi: 10.15252/embr.201540759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Vijayalingam S., Pillai S.G., Rashmi R., Subramanian T., Sagartz J.E., Chinnadurai G. Overexpression of BH3-Only Protein BNIP3 Leads to Enhanced Tumor Growth. Genes Cancer. 2010;1:964–971. doi: 10.1177/1947601910386110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Chen Z., Wu H., Huang S., Li W., Zhang S., Zheng P., Zhou X., Liu W., Zhang D. Expression of BNIP3 and its correlations to hypoxia-induced autophagy and clinicopathological features in salivary adenoid cystic carcinoma. Cancer Biomark. 2015;15:467–475. doi: 10.3233/CBM-150474. [DOI] [PubMed] [Google Scholar]
- 224.Vara-Perez M., Rossi M., Van den Haute C., Maes H., Sassano M.L., Venkataramani V., Michalke B., Romano E., Rillaerts K., Garg A.D., et al. BNIP3 promotes HIF-1alpha-driven melanoma growth by curbing intracellular iron homeostasis. EMBO J. 2021;40:e106214. doi: 10.15252/embj.2020106214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Lebrero-Fernandez C., Wenzel U.A., Akeus P., Wang Y., Strid H., Simren M., Gustavsson B., Borjesson L.G., Cardell S.L., Ohman L., et al. Altered expression of Butyrophilin (BTN) and BTN-like (BTNL) genes in intestinal inflammation and colon cancer. Immun. Inflamm. Dis. 2016;4:191–200. doi: 10.1002/iid3.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Mo Q., Xu K., Luo C., Zhang Q., Wang L., Ren G. BTNL9 is frequently downregulated and inhibits proliferation and metastasis via the P53/CDC25C and P53/GADD45 pathways in breast cancer. Biochem. Biophys. Res. Commun. 2021;553:17–24. doi: 10.1016/j.bbrc.2021.03.022. [DOI] [PubMed] [Google Scholar]
- 227.Ren H., Li S., Liu X., Li W., Hao J., Zhao N. Multi-omics analysis of the expression and prognostic value of the butyrophilins in breast cancer. J. Leukoc. Biol. 2021;110:1181–1195. doi: 10.1002/JLB.5MA0321-158RR. [DOI] [PubMed] [Google Scholar]
- 228.Pergaris A., Danas E., Goutas D., Sykaras A.G., Soranidis A., Theocharis S. The Clinical Impact of the EPH/Ephrin System in Cancer: Unwinding the Thread. Int. J. Mol. Sci. 2021;22:8412. doi: 10.3390/ijms22168412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Anderton M., van der Meulen E., Blumenthal M.J., Schafer G. The Role of the Eph Receptor Family in Tumorigenesis. Cancers. 2021;13:206. doi: 10.3390/cancers13020206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Laussu J., Khuong A., Gautrais J., Davy A. Beyond boundaries--Eph:ephrin signaling in neurogenesis. Cell Adhes. Migr. 2014;8:349–359. doi: 10.4161/19336918.2014.969990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Wilkinson D.G. Regulation of cell differentiation by Eph receptor and ephrin signaling. Cell Adhes. Migr. 2014;8:339–348. doi: 10.4161/19336918.2014.970007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Cayuso J., Xu Q., Wilkinson D.G. Mechanisms of boundary formation by Eph receptor and ephrin signaling. Dev. Biol. 2015;401:122–131. doi: 10.1016/j.ydbio.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 233.Klein R. Eph/ephrin signalling during development. Development. 2012;139:4105–4109. doi: 10.1242/dev.074997. [DOI] [PubMed] [Google Scholar]
- 234.Lodola A., Giorgio C., Incerti M., Zanotti I., Tognolini M. Targeting Eph/ephrin system in cancer therapy. Eur. J. Med. Chem. 2017;142:152–162. doi: 10.1016/j.ejmech.2017.07.029. [DOI] [PubMed] [Google Scholar]
- 235.Tejido C., Pakravan D., Bosch L.V.D. Potential Therapeutic Role of HDAC Inhibitors in FUS-ALS. Front. Mol. Neurosci. 2021;14:686995. doi: 10.3389/fnmol.2021.686995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Klingl Y.E., Pakravan D., Van Den Bosch L. Opportunities for histone deacetylase inhibition in amyotrophic lateral sclerosis. Br. J. Pharmacol. 2021;178:1353–1372. doi: 10.1111/bph.15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Zhang T., Sun B., Zhong C., Xu K., Wang Z., Hofman P., Nagano T., Legras A., Breadner D., Ricciuti B., et al. Targeting histone deacetylase enhances the therapeutic effect of Erastin-induced ferroptosis in EGFR-activating mutant lung adenocarcinoma. Transl. Lung Cancer Res. 2021;10:1857–1872. doi: 10.21037/tlcr-21-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Damaskos C., Tomos I., Garmpis N., Karakatsani A., Dimitroulis D., Garmpi A., Spartalis E., Kampolis C.F., Tsagkari E., Loukeri A.A., et al. Histone Deacetylase Inhibitors as a Novel Targeted Therapy Against Non-small Cell Lung Cancer: Where Are We Now and What Should We Expect? Anticancer. Res. 2018;38:37–43. doi: 10.21873/anticanres.12189. [DOI] [PubMed] [Google Scholar]
- 239.Strub T., Ballotti R., Bertolotto C. The “ART” of Epigenetics in Melanoma: From histone “Alterations, to Resistance and Therapies”. Theranostics. 2020;10:1777–1797. doi: 10.7150/thno.36218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Chen I.C., Sethy B., Liou J.P. Recent Update of HDAC Inhibitors in Lymphoma. Front. Cell Dev. Biol. 2020;8:576391. doi: 10.3389/fcell.2020.576391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Bondarev A.D., Attwood M.M., Jonsson J., Chubarev V.N., Tarasov V.V., Schioth H.B. Recent developments of HDAC inhibitors: Emerging indications and novel molecules. Br. J. Clin. Pharmacol. 2021 doi: 10.1111/bcp.14889. [DOI] [PubMed] [Google Scholar]
- 242.Shukla S., Tekwani B.L. Histone Deacetylases Inhibitors in Neurodegenerative Diseases, Neuroprotection and Neuronal Differentiation. Front. Pharmacol. 2020;11:537. doi: 10.3389/fphar.2020.00537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Souri Z., Jochemsen A.G., Versluis M., Wierenga A.P.A., Nemati F., van der Velden P.A., Kroes W.G.M., Verdijk R.M., Luyten G.P.M., Jager M.J. HDAC Inhibition Increases HLA Class I Expression in Uveal Melanoma. Cancers. 2020;12:3690. doi: 10.3390/cancers12123690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Souri Z., Jochemsen A.G., Wierenga A.P.A., Kroes W.G.M., Verdijk R.M., van der Velden P.A., Luyten G.P.M., Jager M.J. Expression of HDACs 1, 3 and 8 Is Upregulated in the Presence of Infiltrating Lymphocytes in Uveal Melanoma. Cancers. 2021;13:4146. doi: 10.3390/cancers13164146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Levinzon L., Madigan M., Nguyen V., Hasic E., Conway M., Cherepanoff S. Tumour Expression of Histone Deacetylases in Uveal Melanoma. Ocul. Oncol. Pathol. 2019;5:153–161. doi: 10.1159/000490038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Ny L., Jespersen H., Karlsson J., Alsen S., Filges S., All-Eriksson C., Andersson B., Carneiro A., Helgadottir H., Levin M., et al. The PEMDAC phase 2 study of pembrolizumab and entinostat in patients with metastatic uveal melanoma. Nat. Commun. 2021;12:5155. doi: 10.1038/s41467-021-25332-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Lendahl U., Zimmerman L.B., McKay R.D. CNS stem cells express a new class of intermediate filament protein. Cell. 1990;60:585–595. doi: 10.1016/0092-8674(90)90662-X. [DOI] [PubMed] [Google Scholar]
- 248.Bernal A., Arranz L. Nestin-expressing progenitor cells: Function, identity and therapeutic implications. Cell. Mol. Life Sci. CMLS. 2018;75:2177–2195. doi: 10.1007/s00018-018-2794-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Thill M., Berna M.J., Grierson R., Reinhart I., Voelkel T., Piechaczek C., Galambos P., Jager M.J., Richard G., Lange C., et al. Expression of CD133 and other putative stem cell markers in uveal melanoma. Melanoma Res. 2011;21:405–416. doi: 10.1097/CMR.0b013e328348db10. [DOI] [PubMed] [Google Scholar]
- 250.Neradil J., Veselska R. Nestin as a marker of cancer stem cells. Cancer Sci. 2015;106:803–811. doi: 10.1111/cas.12691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Zhang X., Xing C., Guan W., Chen L., Guo K., Yu A., Xie K. Clinicopathological and prognostic significance of nestin expression in patients with breast cancer: A systematic review and meta-analysis. Cancer Cell Int. 2020;20:169. doi: 10.1186/s12935-020-01252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Szymanska-Chabowska A., Swiatkowski F., Jankowska-Polanska B., Mazur G., Chabowski M. Nestin Expression as a Diagnostic and Prognostic Marker in Colorectal Cancer and Other Tumors. Clin. Med. Insights. Oncol. 2021;15:11795549211038256. doi: 10.1177/11795549211038256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Sone K., Maeno K., Masaki A., Kunii E., Takakuwa O., Kagawa Y., Takeuchi A., Fukuda S., Uemura T., Fukumitsu K., et al. Nestin Expression Affects Resistance to Chemotherapy and Clinical Outcome in Small Cell Lung Cancer. Front. Oncol. 2020;10:1367. doi: 10.3389/fonc.2020.01367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Sharma P., Alsharif S., Fallatah A., Chung B.M. Intermediate Filaments as Effectors of Cancer Development and Metastasis: A Focus on Keratins, Vimentin, and Nestin. Cells. 2019;8:497. doi: 10.3390/cells8050497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Djirackor L., Kalirai H., Coupland S.E., Petrovski G. CD166high Uveal Melanoma Cells Represent a Subpopulation With Enhanced Migratory Capacity. Investig. Ophthalmol. Vis. Sci. 2019;60:2696–2704. doi: 10.1167/iovs.18-26431. [DOI] [PubMed] [Google Scholar]
- 256.Liu T., Zhang L., Joo D., Sun S.C. NF-kappaB signaling in inflammation. Signal Transduct. Target. Ther. 2017;2:17023. doi: 10.1038/sigtrans.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Taniguchi K., Karin M. NF-κB, inflammation, immunity and cancer: Coming of age. Nat. Rev. Immunol. 2018;18:309–324. doi: 10.1038/nri.2017.142. [DOI] [PubMed] [Google Scholar]
- 258.Zhang Q., Lenardo M.J., Baltimore D. 30 Years of NF-kappaB: A Blossoming of Relevance to Human Pathobiology. Cell. 2017;168:37–57. doi: 10.1016/j.cell.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Gilmore T.D. NF-kappaB and Human Cancer: What Have We Learned over the Past 35 Years? Biomedicines. 2021;9:889. doi: 10.3390/biomedicines9080889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Eluard B., Thieblemont C., Baud V. NF-kappaB in the New Era of Cancer Therapy. Trends Cancer. 2020;6:677–687. doi: 10.1016/j.trecan.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 261.Barnabei L., Laplantine E., Mbongo W., Rieux-Laucat F., Weil R. NF-kappaB: At the Borders of Autoimmunity and Inflammation. Front. Immunol. 2021;12:716469. doi: 10.3389/fimmu.2021.716469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Van Beek L., McClay E., Patel S., Schimpl M., Spagnolo L., Maia de Oliveira T. PARP Power: A Structural Perspective on PARP1, PARP2, and PARP3 in DNA Damage Repair and Nucleosome Remodelling. Int. J. Mol. Sci. 2021;22:5112. doi: 10.3390/ijms22105112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Rizvi A., Merlin M.A., Shah G.M. Poly (ADP-ribose) polymerase (PARP) inhibition in cancer: Potential impact in cancer stem cells and therapeutic implications. Eur. J. Pharmacol. 2021;911:174546. doi: 10.1016/j.ejphar.2021.174546. [DOI] [PubMed] [Google Scholar]
- 264.Chan W.Y., Brown L.J., Reid L., Joshua A.M. PARP Inhibitors in Melanoma-An Expanding Therapeutic Option? Cancers. 2021;13:4520. doi: 10.3390/cancers13184520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Iams W.T., Porter J., Horn L. Immunotherapeutic approaches for small-cell lung cancer. Nat. Rev. Clin. Oncol. 2020;17:300–312. doi: 10.1038/s41571-019-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Trojaniello C., Luke J.J., Ascierto P.A. Therapeutic Advancements Across Clinical Stages in Melanoma, With a Focus on Targeted Immunotherapy. Front. Oncol. 2021;11:670726. doi: 10.3389/fonc.2021.670726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Mei Z., Huang J., Qiao B., Lam A.K. Immune checkpoint pathways in immunotherapy for head and neck squamous cell carcinoma. Int. J. Oral Sci. 2020;12:16. doi: 10.1038/s41368-020-0084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Okazaki T., Honjo T. PD-1 and PD-1 ligands: From discovery to clinical application. Int. Immunol. 2007;19:813–824. doi: 10.1093/intimm/dxm057. [DOI] [PubMed] [Google Scholar]
- 269.Lucibello G., Mograbi B., Milano G., Hofman P., Brest P. PD-L1 regulation revisited: Impact on immunotherapeutic strategies. Trends Mol. Med. 2021;27:868–881. doi: 10.1016/j.molmed.2021.06.005. [DOI] [PubMed] [Google Scholar]
- 270.Kleffel S., Posch C., Barthel S.R., Mueller H., Schlapbach C., Guenova E., Elco C.P., Lee N., Juneja V.R., Zhan Q., et al. Melanoma Cell-Intrinsic PD-1 Receptor Functions Promote Tumor Growth. Cell. 2015;162:1242–1256. doi: 10.1016/j.cell.2015.08.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Algazi A.P., Tsai K.K., Shoushtari A.N., Munhoz R.R., Eroglu Z., Piulats J.M., Ott P.A., Johnson D.B., Hwang J., Daud A.I., et al. Clinical outcomes in metastatic uveal melanoma treated with PD-1 and PD-L1 antibodies. Cancer. 2016;122:3344–3353. doi: 10.1002/cncr.30258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Basile M.S., Mazzon E., Fagone P., Longo A., Russo A., Fallico M., Bonfiglio V., Nicoletti F., Avitabile T., Reibaldi M. Immunobiology of Uveal Melanoma: State of the Art and Therapeutic Targets. Front. Oncol. 2019;9:1145. doi: 10.3389/fonc.2019.01145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Piulats J.M., Espinosa E., de la Cruz Merino L., Varela M., Alonso Carrion L., Martin-Algarra S., Lopez Castro R., Curiel T., Rodriguez-Abreu D., Redrado M., et al. Nivolumab Plus Ipilimumab for Treatment-Naive Metastatic Uveal Melanoma: An Open-Label, Multicenter, Phase II Trial by the Spanish Multidisciplinary Melanoma Group (GEM-1402) J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2021;39:586–598. doi: 10.1200/JCO.20.00550. [DOI] [PubMed] [Google Scholar]
- 274.Zoroquiain P., Esposito E., Logan P., Aldrees S., Dias A.B., Mansure J.J., Santapau D., Garcia C., Saornil M.A., Belfort Neto R., et al. Programmed cell death ligand-1 expression in tumor and immune cells is associated with better patient outcome and decreased tumor-infiltrating lymphocytes in uveal melanoma. Mod. Pathol. Off. J. United States Can. Acad. Pathol. Inc. 2018;31:1201–1210. doi: 10.1038/s41379-018-0043-5. [DOI] [PubMed] [Google Scholar]
- 275.Iliaki S., Beyaert R., Afonina I.S. Polo-like kinase 1 (PLK1) signaling in cancer and beyond. Biochem. Pharmacol. 2021;193:114747. doi: 10.1016/j.bcp.2021.114747. [DOI] [PubMed] [Google Scholar]
- 276.Cunningham C.E., MacAuley M.J., Vizeacoumar F.S., Abuhussein O., Freywald A., Vizeacoumar F.J. The CINs of Polo-Like Kinase 1 in Cancer. Cancers. 2020;12:2953. doi: 10.3390/cancers12102953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Colicino E.G., Hehnly H. Regulating a key mitotic regulator, polo-like kinase 1 (PLK1) Cytoskeleton. 2018;75:481–494. doi: 10.1002/cm.21504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Zhang Y., Wu Z., Liu D., Wang M., Xiao G., Wang P., Sun X., Ren H., Tang S.C., Du N. Augmented expression of polo-like kinase 1 indicates poor clinical outcome for breast patients: A systematic review and meta-analysis. Oncotarget. 2017;8:57723–57732. doi: 10.18632/oncotarget.17301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Shin S.B., Jang H.R., Xu R., Won J.Y., Yim H. Active PLK1-driven metastasis is amplified by TGF-beta signaling that forms a positive feedback loop in non-small cell lung cancer. Oncogene. 2020;39:767–785. doi: 10.1038/s41388-019-1023-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Murga-Zamalloa C., Inamdar K.V., Wilcox R.A. The role of aurora A and polo-like kinases in high-risk lymphomas. Blood Adv. 2019;3:1778–1787. doi: 10.1182/bloodadvances.2019000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Liu Z., Sun Q., Wang X. PLK1, A Potential Target for Cancer Therapy. Transl. Oncol. 2017;10:22–32. doi: 10.1016/j.tranon.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Gutteridge R.E., Ndiaye M.A., Liu X., Ahmad N. Plk1 Inhibitors in Cancer Therapy: From Laboratory to Clinics. Mol. Cancer Ther. 2016;15:1427–1435. doi: 10.1158/1535-7163.MCT-15-0897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Ismail T., Kim Y., Lee H., Lee D.S., Lee H.S. Interplay Between Mitochondrial Peroxiredoxins and ROS in Cancer Development and Progression. Int. J. Mol. Sci. 2019;20:4407. doi: 10.3390/ijms20184407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Lee Y.J. Knockout Mouse Models for Peroxiredoxins. Antioxidants. 2020;9:182. doi: 10.3390/antiox9020182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Westbrook V.A., Diekman A.B., Klotz K.L., Khole V.V., von Kap-Herr C., Golden W.L., Eddy R.L., Shows T.B., Stoler M.H., Lee C.Y., et al. Spermatid-specific expression of the novel X-linked gene product SPAN-X localized to the nucleus of human spermatozoa. Biol. Reprod. 2000;63:469–481. doi: 10.1093/biolreprod/63.2.469. [DOI] [PubMed] [Google Scholar]
- 286.Salemi M., Calogero A.E., Di Benedetto D., Cosentino A., Barone N., Rappazzo G., Vicari E. Expression of SPANX proteins in human-ejaculated spermatozoa and sperm precursors. Int. J. Androl. 2004;27:134–139. doi: 10.1111/j.1365-2605.2004.00461.x. [DOI] [PubMed] [Google Scholar]
- 287.Urizar-Arenaza I., Osinalde N., Akimov V., Puglia M., Munoa-Hoyos I., Gianzo M., Rodriguez J.A., Ganzabal T., Blagoev B., Kratchmarova I., et al. SPANX-A/D protein subfamily plays a key role in nuclear organisation, metabolism and flagellar motility of human spermatozoa. Sci. Rep. 2020;10:5625. doi: 10.1038/s41598-020-62389-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Maine E.A., Westcott J.M., Prechtl A.M., Dang T.T., Whitehurst A.W., Pearson G.W. The cancer-testis antigens SPANX-A/C/D and CTAG2 promote breast cancer invasion. Oncotarget. 2016;7:14708–14726. doi: 10.18632/oncotarget.7408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Lazar I., Fabre B., Feng Y., Khateb A., Turko P., Martinez Gomez J.M., Frederick D.T., Levesque M.P., Feld L., Zhang G., et al. SPANX Control of Lamin A/C Modulates Nuclear Architecture and Promotes Melanoma Growth. Mol. Cancer Res. MCR. 2020;18:1560–1573. doi: 10.1158/1541-7786.MCR-20-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Urizar-Arenaza I., Benedicto A., Perez-Valle A., Osinalde N., Akimov V., Munoa-Hoyos I., Rodriguez J.A., Asumendi A., Boyano M.D., Blagoev B., et al. The multifunctional role of SPANX-A/D protein subfamily in the promotion of pro-tumoural processes in human melanoma. Sci. Rep. 2021;11:3583. doi: 10.1038/s41598-021-83169-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Jang G.F., Crabb J.S., Hu B., Willard B., Kalirai H., Singh A.D., Coupland S.E., Crabb J.W. Proteomics of Primary Uveal Melanoma: Insights into Metastasis and Protein Biomarkers. Cancers. 2021;13:3520. doi: 10.3390/cancers13143520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Song J., Zhang Z., Chan D.W. Detection of Uveal Melanoma by Multiplex Immunoassays of Serum Biomarkers. Methods Mol. Biol. 2021;2265:447–459. doi: 10.1007/978-1-0716-1205-7_32. [DOI] [PubMed] [Google Scholar]
- 293.Song J., Merbs S.L., Sokoll L.J., Chan D.W., Zhang Z. A multiplex immunoassay of serum biomarkers for the detection of uveal melanoma. Clin. Proteom. 2019;16:10. doi: 10.1186/s12014-019-9230-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Velez G., Nguyen H.V., Chemudupati T., Ludwig C.A., Toral M., Reddy S., Mruthyunjaya P., Mahajan V.B. Liquid biopsy proteomics of uveal melanoma reveals biomarkers associated with metastatic risk. Mol. Cancer. 2021;20:39. doi: 10.1186/s12943-021-01336-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Honavar S.G. Is Collaborative Ocular Melanoma Study (COMS) still relevant? Indian J. Ophthalmol. 2018;66:1385–1387. doi: 10.4103/ijo.IJO_1588_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Damato B., Eleuteri A., Hussain R., Kalirai H., Thornton S., Taktak A., Heimann H., Coupland S.E. Parsimonious Models for Predicting Mortality from Choroidal Melanoma. Investig. Ophthalmol. Vis. Sci. 2020;61:35. doi: 10.1167/iovs.61.4.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Vaquero-Garcia J., Lalonde E., Ewens K.G., Ebrahimzadeh J., Richard-Yutz J., Shields C.L., Barrera A., Green C.J., Barash Y., Ganguly A. PRiMeUM: A Model for Predicting Risk of Metastasis in Uveal Melanoma. Investig. Ophthalmol. Vis. Sci. 2017;58:4096–4105. doi: 10.1167/iovs.17-22255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Martel A., Baillif S., Nahon-Esteve S., Gastaud L., Bertolotto C., Romeo B., Mograbi B., Lassalle S., Hofman P. Liquid Biopsy for Solid Ophthalmic Malignancies: An Updated Review and Perspectives. Cancers. 2020;12:3284. doi: 10.3390/cancers12113284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Ignatiadis M., Sledge G.W., Jeffrey S.S. Liquid biopsy enters the clinic—Implementation issues and future challenges. Nat. Rev. Clin. Oncol. 2021;18:297–312. doi: 10.1038/s41571-020-00457-x. [DOI] [PubMed] [Google Scholar]
- 300.Heitzer E., Haque I.S., Roberts C.E.S., Speicher M.R. Current and future perspectives of liquid biopsies in genomics-driven oncology. Nat. Rev. Genet. 2019;20:71–88. doi: 10.1038/s41576-018-0071-5. [DOI] [PubMed] [Google Scholar]
- 301.Im Y.R., Tsui D.W.Y., Diaz L.A., Jr., Wan J.C.M. Next-Generation Liquid Biopsies: Embracing Data Science in Oncology. Trends Cancer. 2021;7:283–292. doi: 10.1016/j.trecan.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Heeke S., Hofman V., Ilie M., Allegra M., Lespinet V., Bordone O., Benzaquen J., Boutros J., Poudenx M., Lalvee S., et al. Prospective evaluation of NGS-based liquid biopsy in untreated late stage non-squamous lung carcinoma in a single institution. J. Transl. Med. 2020;18:87. doi: 10.1186/s12967-020-02259-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Heeke S., Benzaquen J., Hofman V., Ilie M., Allegra M., Long-Mira E., Lassalle S., Tanga V., Salacroup C., Bonnetaud C., et al. Critical Assessment in Routine Clinical Practice of Liquid Biopsy for EGFR Status Testing in Non-Small-Cell Lung Cancer: A Single-Laboratory Experience (LPCE, Nice, France) Clin. Lung Cancer. 2020;21:56–65.e8. doi: 10.1016/j.cllc.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 304.Hofman P. Liquid Biopsy and Therapeutic Targets: Present and Future Issues in Thoracic Oncology. Cancers. 2017;9:154. doi: 10.3390/cancers9110154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Hofman P. Next-Generation Sequencing with Liquid Biopsies from Treatment-Naive Non-Small Cell Lung Carcinoma Patients. Cancers. 2021;13:2049. doi: 10.3390/cancers13092049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Hofman P. Detecting Resistance to Therapeutic ALK Inhibitors in Tumor Tissue and Liquid Biopsy Markers: An Update to a Clinical Routine Practice. Cells. 2021;10:168. doi: 10.3390/cells10010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Jin E., Burnier J.V. Liquid Biopsy in Uveal Melanoma: Are We There Yet? Ocul. Oncol. Pathol. 2021;7:1–16. doi: 10.1159/000508613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Beasley A., Isaacs T., Khattak M.A., Freeman J.B., Allcock R., Chen F.K., Pereira M.R., Yau K., Bentel J., Vermeulen T., et al. Clinical Application of Circulating Tumor Cells and Circulating Tumor DNA in Uveal Melanoma. JCO Precis. Oncol. 2018;2:1–12. doi: 10.1200/PO.17.00279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Park J.J., Diefenbach R.J., Byrne N., Long G.V., Scolyer R.A., Gray E.S., Carlino M.S., Rizos H. Circulating Tumor DNA Reflects Uveal Melanoma Responses to Protein Kinase C Inhibition. Cancers. 2021;13:1740. doi: 10.3390/cancers13071740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Le Guin C.H.D., Bornfeld N., Bechrakis N.E., Jabbarli L., Richly H., Lohmann D.R., Zeschnigk M. Early detection of metastatic uveal melanoma by the analysis of tumor-specific mutations in cell-free plasma DNA. Cancer Med. 2021;10:5974–5982. doi: 10.1002/cam4.4153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Krishna Y., McCarthy C., Kalirai H., Coupland S.E. Inflammatory cell infiltrates in advanced metastatic uveal melanoma. Hum. Pathol. 2017;66:159–166. doi: 10.1016/j.humpath.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 312.Wierenga A.P.A., Cao J., Mouthaan H., van Weeghel C., Verdijk R.M., van Duinen S.G., Kroes W.G.M., Dogrusoz M., Marinkovic M., van der Burg S.S.H., et al. Aqueous Humor Biomarkers Identify Three Prognostic Groups in Uveal Melanoma. Investig. Ophthalmol. Vis. Sci. 2019;60:4740–4747. doi: 10.1167/iovs.19-28309. [DOI] [PubMed] [Google Scholar]
- 313.Berry J.L., Xu L., Murphree A.L., Krishnan S., Stachelek K., Zolfaghari E., McGovern K., Lee T.C., Carlsson A., Kuhn P., et al. Potential of Aqueous Humor as a Surrogate Tumor Biopsy for Retinoblastoma. JAMA Ophthalmol. 2017;135:1221–1230. doi: 10.1001/jamaophthalmol.2017.4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Gerrish A., Stone E., Clokie S., Ainsworth J.R., Jenkinson H., McCalla M., Hitchcott C., Colmenero I., Allen S., Parulekar M., et al. Non-invasive diagnosis of retinoblastoma using cell-free DNA from aqueous humour. Br. J. Ophthalmol. 2019;103:721–724. doi: 10.1136/bjophthalmol-2018-313005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Kuiper J., Ten Dam-van Loon N., Domanian A., Schellekens P., Nierkens S., Radstake T., de Boer J. Correlation between measurement of IL-10 and IL-6 in paired aqueous humour and vitreous fluid in primary vitreoretinal lymphoma. Acta Ophthalmol. 2015;93:e680–e681. doi: 10.1111/aos.12733. [DOI] [PubMed] [Google Scholar]
- 316.Pochat-Cotilloux C., Bienvenu J., Nguyen A.M., Ohanessian R., Ghesquieres H., Seve P., Garnier L., Kodjikian L. Use of a Threshold of Interleukin-10 and Il-10/Il-6 Ratio in Ocular Samples for the Screening of Vitreoretinal Lymphoma. Retina. 2018;38:773–781. doi: 10.1097/IAE.0000000000001922. [DOI] [PubMed] [Google Scholar]
- 317.Midena E., Parrozzani R., Midena G., Trainiti S., Marchione G., Cosmo E., Londei D., Frizziero L. In vivo intraocular biomarkers: Changes of aqueous humor cytokines and chemokines in patients affected by uveal melanoma. Medicine. 2020;99:e22091. doi: 10.1097/MD.0000000000022091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Shaw A., Gullerova M. Home and Away: The Role of Non-Coding RNA in Intracellular and Intercellular DNA Damage Response. Genes. 2021;12:1475. doi: 10.3390/genes12101475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Statello L., Guo C.J., Chen L.L., Huarte M. Gene regulation by long non-coding RNAs and its biological functions. Nat. Rev. Mol. Cell Biol. 2021;22:96–118. doi: 10.1038/s41580-020-00315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Acha-Sagredo A., Uko B., Pantazi P., Bediaga N.G., Moschandrea C., Rainbow L., Marcus M.W., Davies M.P.A., Field J.K., Liloglou T. Long non-coding RNA dysregulation is a frequent event in non-small cell lung carcinoma pathogenesis. Br. J. Cancer. 2020;122:1050–1058. doi: 10.1038/s41416-020-0742-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Wozniak M., Czyz M. The Functional Role of Long Non-Coding RNAs in Melanoma. Cancers. 2021;13:4848. doi: 10.3390/cancers13194848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Bande M., Fernandez-Diaz D., Fernandez-Marta B., Rodriguez-Vidal C., Lago-Baameiro N., Silva-Rodriguez P., Paniagua L., Blanco-Teijeiro M.J., Pardo M., Pineiro A. The Role of Non-Coding RNAs in Uveal Melanoma. Cancers. 2020;12:2944. doi: 10.3390/cancers12102944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Milan-Rois P., Quan A., Slack F.J., Somoza A. The Role of LncRNAs in Uveal Melanoma. Cancers. 2021;13:4041. doi: 10.3390/cancers13164041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Aughton K., Kalirai H., Coupland S.E. MicroRNAs and Uveal Melanoma: Understanding the Diverse Role of These Small Molecular Regulators. Int. J. Mol. Sci. 2020;21:5648. doi: 10.3390/ijms21165648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Sharma A., Biswas A., Liu H., Sen S., Paruchuri A., Katsonis P., Lichtarge O., Chand Dakal T., Maulik U., Gromiha M.M., et al. Mutational Landscape of the BAP1 Locus Reveals an Intrinsic Control to Regulate the miRNA Network and the Binding of Protein Complexes in Uveal Melanoma. Cancers. 2019;11:1600. doi: 10.3390/cancers11101600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Yang C., Wang Y., Hardy P. Emerging roles of microRNAs and their implications in uveal melanoma. Cell. Mol. Life Sci. CMLS. 2021;78:545–559. doi: 10.1007/s00018-020-03612-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Wroblewska J.P., Lach M.S., Ustaszewski A., Kulcenty K., Ibbs M., Jagiello I., Suchorska W.M., Marszalek A. The Potential Role of Selected miRNA in Uveal Melanoma Primary Tumors as Early Biomarkers of Disease Progression. Genes. 2020;11:271. doi: 10.3390/genes11030271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Yang C., Wang R., Hardy P. Potential of miRNA-Based Nanotherapeutics for Uveal Melanoma. Cancers. 2021;13:5192. doi: 10.3390/cancers13205192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Krishna Y., Acha-Sagredo A., Sabat-Pospiech D., Kipling N., Clarke K., Figueiredo C.R., Kalirai H., Coupland S.E. Transcriptome Profiling Reveals New Insights into the Immune Microenvironment and Upregulation of Novel Biomarkers in Metastatic Uveal Melanoma. Cancers. 2020;12:2832. doi: 10.3390/cancers12102832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Kelly D., Rose A.A.N., Muniz T.P., Hogg D., Butler M.O., Saibil S.D., King I., Kamil Z.S., Ghazarian D., Ross K., et al. Development of a Metastatic Uveal Melanoma Prognostic Score (MUMPS) for Use in Patients Receiving Immune Checkpoint Inhibitors. Cancers. 2021;13:3640. doi: 10.3390/cancers13143640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Bol K.F., Ellebaek E., Hoejberg L., Bagger M.M., Larsen M.S., Klausen T.W., Kohler U.H., Schmidt H., Bastholt L., Kiilgaard J.F., et al. Real-World Impact of Immune Checkpoint Inhibitors in Metastatic Uveal Melanoma. Cancers. 2019;11:1489. doi: 10.3390/cancers11101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Figueiredo C.R., Kalirai H., Sacco J.J., Azevedo R.A., Duckworth A., Slupsky J.R., Coulson J.M., Coupland S.E. Loss of BAP1 expression is associated with an immunosuppressive microenvironment in uveal melanoma, with implications for immunotherapy development. J. Pathol. 2020;250:420–439. doi: 10.1002/path.5384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Stalhammar G., Seregard S., Grossniklaus H.E. Expression of immune checkpoint receptors Indoleamine 2,3-dioxygenase and T cell Ig and ITIM domain in metastatic versus nonmetastatic choroidal melanoma. Cancer Med. 2019;8:2784–2792. doi: 10.1002/cam4.2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Durante M.A., Rodriguez D.A., Kurtenbach S., Kuznetsov J.N., Sanchez M.I., Decatur C.L., Snyder H., Feun L.G., Livingstone A.S., Harbour J.W. Single-cell analysis reveals new evolutionary complexity in uveal melanoma. Nat. Commun. 2020;11:496. doi: 10.1038/s41467-019-14256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Souri Z., Wierenga A.P.A., Kroes W.G.M., van der Velden P.A., Verdijk R.M., Eikmans M., Luyten G.P.M., Jager M.J. LAG3 and Its Ligands Show Increased Expression in High-Risk Uveal Melanoma. Cancers. 2021;13:4445. doi: 10.3390/cancers13174445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Li Z., Li Y., Gao J., Fu Y., Hua P., Jing Y., Cai M., Wang H., Tong T. The role of CD47-SIRPalpha immune checkpoint in tumor immune evasion and innate immunotherapy. Life Sci. 2021;273:119150. doi: 10.1016/j.lfs.2021.119150. [DOI] [PubMed] [Google Scholar]
- 337.Jia X., Yan B., Tian X., Liu Q., Jin J., Shi J., Hou Y. CD47/SIRPalpha pathway mediates cancer immune escape and immunotherapy. Int. J. Biol. Sci. 2021;17:3281–3287. doi: 10.7150/ijbs.60782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Sun J., Chen Y., Lubben B., Adebayo O., Muz B., Azab A.K. CD47-targeting antibodies as a novel therapeutic strategy in hematologic malignancies. Leuk. Res. Rep. 2021;16:100268. doi: 10.1016/j.lrr.2021.100268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Xu Y., Li J., Tong B., Chen M., Liu X., Zhong W., Zhao J., Wang M. Positive tumour CD47 expression is an independent prognostic factor for recurrence in resected non-small cell lung cancer. ESMO Open. 2020;5:e000823. doi: 10.1136/esmoopen-2020-000823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Kosaka A., Ishibashi K., Nagato T., Kitamura H., Fujiwara Y., Yasuda S., Nagata M., Harabuchi S., Hayashi R., Yajima Y., et al. CD47 blockade enhances the efficacy of intratumoral STING-targeting therapy by activating phagocytes. J. Exp. Med. 2021;218:e20200792. doi: 10.1084/jem.20200792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Petralia M.C., Mazzon E., Fagone P., Russo A., Longo A., Avitabile T., Nicoletti F., Reibaldi M., Basile M.S. Characterization of the Pathophysiological Role of CD47 in Uveal Melanoma. Molecules. 2019;24:2450. doi: 10.3390/molecules24132450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Lu Q., Chen X., Wang S., Lu Y., Yang C., Jiang G. Potential New Cancer Immunotherapy: Anti-CD47-SIRPalpha Antibodies. OncoTargets Ther. 2020;13:9323–9331. doi: 10.2147/OTT.S249822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Marin-Acevedo J.A., Kimbrough E.O., Lou Y. Next generation of immune checkpoint inhibitors and beyond. J. Hematol. Oncol. 2021;14:45. doi: 10.1186/s13045-021-01056-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Lee J.B., Ha S.J., Kim H.R. Clinical Insights Into Novel Immune Checkpoint Inhibitors. Front. Pharmacol. 2021;12:681320. doi: 10.3389/fphar.2021.681320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Pelster M.S., Gruschkus S.K., Bassett R., Gombos D.S., Shephard M., Posada L., Glover M.S., Simien R., Diab A., Hwu P., et al. Nivolumab and Ipilimumab in Metastatic Uveal Melanoma: Results From a Single-Arm Phase II Study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2021;39:599–607. doi: 10.1200/JCO.20.00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Hofman P., Badoual C., Henderson F., Berland L., Hamila M., Long-Mira E., Lassalle S., Roussel H., Hofman V., Tartour E., et al. Multiplexed Immunohistochemistry for Molecular and Immune Profiling in Lung Cancer-Just About Ready for Prime-Time? Cancers. 2019;11:283. doi: 10.3390/cancers11030283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Wharton K.A., Jr., Wood D., Manesse M., Maclean K.H., Leiss F., Zuraw A. Tissue Multiplex Analyte Detection in Anatomic Pathology—Pathways to Clinical Implementation. Front. Mol. Biosci. 2021;8:672531. doi: 10.3389/fmolb.2021.672531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Grossniklaus H.E., Zhang Q., You S., McCarthy C., Heegaard S., Coupland S.E. Metastatic ocular melanoma to the liver exhibits infiltrative and nodular growth patterns. Hum. Pathol. 2016;57:165–175. doi: 10.1016/j.humpath.2016.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Grossniklaus H.E. Understanding Uveal Melanoma Metastasis to the Liver: The Zimmerman Effect and the Zimmerman Hypothesis. Ophthalmology. 2019;126:483–487. doi: 10.1016/j.ophtha.2018.09.031. [DOI] [PubMed] [Google Scholar]
- 350.Bustamante P., Piquet L., Landreville S., Burnier J.V. Uveal melanoma pathobiology: Metastasis to the liver. Semin. Cancer Biol. 2021;71:65–85. doi: 10.1016/j.semcancer.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 351.Lin W., Beasley A.B., Ardakani N.M., Denisenko E., Calapre L., Jones M., Wood B.A., Warburton L., Forrest A.R.R., Gray E.S. Intra- and inter-tumoral heterogeneity of liver metastases in a patient with uveal melanoma revealed by single-cell RNA sequencing. Cold Spring Harb. Mol. Case Stud. 2021;7:a006111. doi: 10.1101/mcs.a006111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Pandiani C., Strub T., Nottet N., Cheli Y., Gambi G., Bille K., Husser C., Dalmasso M., Beranger G., Lassalle S., et al. Single-cell RNA sequencing reveals intratumoral heterogeneity in primary uveal melanomas and identifies HES6 as a driver of the metastatic disease. Cell Death Differ. 2021;28:1990–2000. doi: 10.1038/s41418-020-00730-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Strub T., Martel A., Nahon-Esteve S., Baillif S., Ballotti R., Bertolotto C. Translation of single-cell transcriptomic analysis of uveal melanomas to clinical oncology. Prog. Retin. Eye Res. 2021;85:100968. doi: 10.1016/j.preteyeres.2021.100968. [DOI] [PubMed] [Google Scholar]
- 354.Simian M., Bissell M.J. Organoids: A historical perspective of thinking in three dimensions. J. Cell Biol. 2017;216:31–40. doi: 10.1083/jcb.201610056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Lamas N.J., Roybon L. Harnessing the potential of human pluripotent stem cell-derived motor neurons for drug discovery in Amyotrophic Lateral Sclerosis (ALS): From the clinic to the laboratory and back to the patient. Front. Drug Discov. 2021;1:1–26. doi: 10.3389/fddsv.2021.773424. [DOI] [Google Scholar]
- 356.Lucey B.P., Nelson-Rees W.A., Hutchins G.M. Henrietta Lacks, HeLa cells, and cell culture contamination. Arch. Pathol. Lab. Med. 2009;133:1463–1467. doi: 10.5858/133.9.1463. [DOI] [PubMed] [Google Scholar]
- 357.Jager M.J., Magner J.A., Ksander B.R., Dubovy S.R. Uveal Melanoma Cell Lines: Where do they come from? (An American Ophthalmological Society Thesis) Trans. Am. Ophthalmol. Soc. 2016;114:T5. [PMC free article] [PubMed] [Google Scholar]
- 358.Angi M., Versluis M., Kalirai H. Culturing Uveal Melanoma Cells. Ocul. Oncol. Pathol. 2015;1:126–132. doi: 10.1159/000370150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Fiorentzis M., Viestenz A., Siebolts U., Seitz B., Coupland S.E., Heinzelmann J. The Potential Use of Electrochemotherapy in the Treatment of Uveal Melanoma: In Vitro Results in 3D Tumor Cultures and In Vivo Results in a Chick Embryo Model. Cancers. 2019;11:1344. doi: 10.3390/cancers11091344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Aughton K., Shahidipour H., Djirackor L., Coupland S.E., Kalirai H. Characterization of Uveal Melanoma Cell Lines and Primary Tumor Samples in 3D Culture. Transl. Vis. Sci. Technol. 2020;9:39. doi: 10.1167/tvst.9.7.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Richards J.R., Yoo J.H., Shin D., Odelberg S.J. Mouse models of uveal melanoma: Strengths, weaknesses, and future directions. Pigment. Cell Melanoma Res. 2020;33:264–278. doi: 10.1111/pcmr.12853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Stei M.M., Loeffler K.U., Holz F.G., Herwig M.C. Animal Models of Uveal Melanoma: Methods, Applicability, and Limitations. BioMed Res. Int. 2016;2016:4521807. doi: 10.1155/2016/4521807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Yamanaka S. Pluripotent Stem Cell-Based Cell Therapy-Promise and Challenges. Cell Stem Cell. 2020;27:523–531. doi: 10.1016/j.stem.2020.09.014. [DOI] [PubMed] [Google Scholar]
- 364.Bharathan S.P., Ferrario A., Stepanian K., Fernandez G.E., Reid M.W., Kim J.S., Hutchens C., Harutyunyan N., Marks C., Thornton M.E., et al. Characterization and staging of outer plexiform layer development in human retina and retinal organoids. Development. 2021;148:dev199551. doi: 10.1242/dev.199551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Castro-Perez E., Rodriguez C.I., Mikheil D., Siddique S., McCarthy A., Newton M.A., Setaluri V. Melanoma Progression Inhibits Pluripotency and Differentiation of Melanoma-Derived iPSCs Produces Cells with Neural-like Mixed Dysplastic Phenotype. Stem Cell Rep. 2019;13:177–192. doi: 10.1016/j.stemcr.2019.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Karagiannis P., Kim S.I. iPSC-Derived Natural Killer Cells for Cancer Immunotherapy. Mol. Cells. 2021;44:541–548. doi: 10.14348/molcells.2021.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Bhan A., Ansari K., Chen M.Y., Jandial R. Human induced pluripotent stem cell-derived platelets loaded with lapatinib effectively target HER2+ breast cancer metastasis to the brain. Sci. Rep. 2021;11:16866. doi: 10.1038/s41598-021-96351-2. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 368.Lamas N.J., Johnson-Kerner B., Roybon L., Kim Y.A., Garcia-Diaz A., Wichterle H., Henderson C.E. Neurotrophic requirements of human motor neurons defined using amplified and purified stem cell-derived cultures. PLoS ONE. 2014;9:e110324. doi: 10.1371/journal.pone.0110324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Li H., Kuwajima T., Oakley D., Nikulina E., Hou J., Yang W.S., Lowry E.R., Lamas N.J., Amoroso M.W., Croft G.F., et al. Protein Prenylation Constitutes an Endogenous Brake on Axonal Growth. Cell Rep. 2016;16:545–558. doi: 10.1016/j.celrep.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 370.Rodrigues T., Kundu B., Silva-Correia J., Kundu S.C., Oliveira J.M., Reis R.L., Correlo V.M. Emerging tumor spheroids technologies for 3D in vitro cancer modeling. Pharmacol. Ther. 2018;184:201–211. doi: 10.1016/j.pharmthera.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 371.Monteiro M.V., Zhang Y.S., Gaspar V.M., Mano J.F. 3D-bioprinted cancer-on-a-chip: Level-up organotypic in vitro models. Trends Biotechnol. 2021 doi: 10.1016/j.tibtech.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Liu X., Fang J., Huang S., Wu X., Xie X., Wang J., Liu F., Zhang M., Peng Z., Hu N. Tumor-on-a-chip: From bioinspired design to biomedical application. Microsyst. Nanoeng. 2021;7:50. doi: 10.1038/s41378-021-00277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Marton R.M., Pasca S.P. Organoid and Assembloid Technologies for Investigating Cellular Crosstalk in Human Brain Development and Disease. Trends Cell Biol. 2020;30:133–143. doi: 10.1016/j.tcb.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 374.Andersen J., Revah O., Miura Y., Thom N., Amin N.D., Kelley K.W., Singh M., Chen X., Thete M.V., Walczak E.M., et al. Generation of Functional Human 3D Cortico-Motor Assembloids. Cell. 2020;183:1913–1929.e26. doi: 10.1016/j.cell.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Panoutsopoulos A.A. Organoids, Assembloids, and Novel Biotechnology: Steps Forward in Developmental and Disease-Related Neuroscience. Neuroscientist. 2020;27:463–472. doi: 10.1177/1073858420960112. [DOI] [PubMed] [Google Scholar]
- 376.Nathan P., Hassel J.C., Rutkowski P., Baurain J.F., Butler M.O., Schlaak M., Sullivan R.J., Ochsenreither S., Dummer R., Kirkwood J.M., et al. Overall Survival Benefit with Tebentafusp in Metastatic Uveal Melanoma. N. Engl. J. Med. 2021;385:1196–1206. doi: 10.1056/NEJMoa2103485. [DOI] [PubMed] [Google Scholar]
- 377.Killock D. Tebentafusp for uveal melanoma. Nat. Rev. Clin. Oncol. 2021;18:747. doi: 10.1038/s41571-021-00572-3. [DOI] [PubMed] [Google Scholar]
- 378.Damato B.E., Dukes J., Goodall H., Carvajal R.D. Tebentafusp: T Cell Redirection for the Treatment of Metastatic Uveal Melanoma. Cancers. 2019;11:971. doi: 10.3390/cancers11070971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Goebeler M.E., Bargou R.C. T cell-engaging therapies—BiTEs and beyond. Nat. Rev. Clin. Oncol. 2020;17:418–434. doi: 10.1038/s41571-020-0347-5. [DOI] [PubMed] [Google Scholar]
- 380.Zhao Q., Jiang Y., Xiang S., Kaboli P.J., Shen J., Zhao Y., Wu X., Du F., Li M., Cho C.H., et al. Engineered TCR-T Cell Immunotherapy in Anticancer Precision Medicine: Pros and Cons. Front. Immunol. 2021;12:658753. doi: 10.3389/fimmu.2021.658753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Han A., Purwin T.J., Bechtel N., Liao C., Chua V., Seifert E., Sato T., Schug Z.T., Speicher D.W., William Harbour J., et al. BAP1 mutant uveal melanoma is stratified by metabolic phenotypes with distinct vulnerability to metabolic inhibitors. Oncogene. 2021;40:618–632. doi: 10.1038/s41388-020-01554-y. [DOI] [PMC free article] [PubMed] [Google Scholar]