Abstract
In 1978, G. Klerman published an essay in which he named the then‐nascent “neo‐Kraepelinian” movement and formulated a “credo” of nine propositions expressing the movement's essential claims and aspirations. Klerman's essay appeared on the eve of the triumph of neo‐Kraepelinian ideas in the DSM‐III. However, this diagnostic system has subsequently come under attack, opening the way for competing proposals for the future of psychiatric nosology. To better understand what is at stake, in this paper I provide a close reading and consideration of Klerman's credo in light of the past forty years of research and reflection. The credo is placed in the context of two equally seminal publications in the same year, one by S. Guze, the leading neo‐Kraepelinian theorist, and the other by R. Spitzer and J. Endicott, defining mental disorder. The divergences between Spitzer and standard neo‐Kraepelinianism are highlighted and argued to be much more important than is generally realized. The analysis of Klerman's credo is also argued to have implications for how to satisfactorily resolve the current nosological ferment in psychiatry. In addition to issues such as creating descriptive syndromal diagnostic criteria, overthrowing psychoanalytic dominance of psychiatry, and making psychiatry more scientific, neo‐Kraepelinians were deeply concerned with the conceptual issue of the nature of mental disorder and the defense of psychiatry's medical legitimacy in response to antipsychiatric criticisms. These issues cannot be ignored, and I argue that proposals currently on offer to replace the neo‐Kraepelinian system, especially popular proposals to replace it with dimensional measures, fail to adequately address them.
Keywords: Neo‐Kraepelinian movement, Klerman's credo, DSM‐III, mental disorder, harmful dysfunction, antipsychiatry, dimensional approaches, Research Domain Criteria, Hierarchical Taxonomy of Psychopathology, R. Spitzer
After four decades of dominance of psychiatry by the neo‐Kraepelinian symptom‐based categorical vision of nosology, formally embraced in the DSM‐III 1 , there is a growing perception that neo‐Kraepelinianism has failed and is unable to yield its expected dividends in etiological understanding and treatment progress. This perceived failure has left a vacuum that various alternative proposals and research programs are attempting to fill, ranging from the US National Institute of Mental Health (NIMH)'s Research Domain Criteria (RDoC) initiative2, 3, 4, 5, focused on identifying brain circuitry etiologies, to multiple research programs to dimensionalize or factor‐analyze away rigid diagnostic categories such as the Hierarchical Taxonomy of Psychopathology (HiTOP) project6, 7, 8, 9, and many other proposals as well, such as network theory10, 11, 12, 13 and comprehensive risk factor analyses 14 .
This nosological ferment provides an ideal time to reconsider the neo‐Kraepelinian program's origins, aspirations, and its present condition as a prelude to grappling with the future of psychiatric nosology and mediating among the many competing proposals. A natural way to start such a reassessment is with G. Klerman's pivotal 1978 essay, The Evolution of a Scientific Nosology 15 , in which he coined the term “neo‐Kraepelinian”. In his article, Klerman prepared his readers for the radical changes to come by elaborating a neo‐Kraepelinian “credo” of nine propositions that constituted the movement's central claims and goals (Table 1). After some preliminaries, I will comment on and evaluate each of these propositions both in terms of the arguments they put forward and in light of thinking during the four decades since their formulation. I focus on conceptual issues rather than sociological or other motivational determinants.
Table 1.
The neo‐Kraepelinian credo 15
| 1. | Psychiatry is a branch of medicine. |
|---|---|
| 2. | Psychiatry should utilize modem scientific methodologies and base its practice on scientific knowledge. |
| 3. | Psychiatry treats people who are sick and who require treatment for mental illnesses. |
| 4. | There is a boundary between the normal and the sick. |
| 5. | There are discrete mental illnesses. Mental illnesses are not myths. There is not one but many mental illnesses. It is the task of scientific psychiatry, as of other medical specialties, to investigate the causes, diagnosis, and treatment of these mental illnesses. |
| 6. | The focus of psychiatric physicians should be particularly on the biological aspects of mental illness. |
| 7. | There should be an explicit and intentional concern with diagnosis and classification. |
| 8. | Diagnostic criteria should be codified, and a legitimate and valued area of research should be to validate such criteria by various techniques. Further, departments of psychiatry in medical schools should teach these criteria and not depreciate them, as has been the case for many years. |
| 9. | In research efforts directed at improving the reliability and validity of diagnosis and classification, statistical techniques should be utilized. |
In fact, 1978 was a remarkable year for foundations of psychiatry even beyond Klerman's essay. In considering Klerman's nine principles, I will draw on two additional seminal events of that year that must be part of a perspicuous account. First, S. Guze, a Washington University psychiatrist who was the leading neo‐Kraepelinian theorist, published a defense of the movement's most basic claim, that psychiatry is a branch of medicine 16 , an argument he elaborated in a later article and book17, 18. Second, R. Spitzer and J. Endicott published the most ambitious of a series of attempts to define the concept of mental disorder as a foundation for nosology 19 .
A WORD ABOUT G. KLERMAN AND HIS STANCE TOWARD THE NEO‐KRAEPELINIAN MOVEMENT
In his 1978 article, Klerman spoke with considerable authority about the direction of psychiatry because he had been appointed the year before as head of the US Alcohol, Drug Abuse and Mental Health Administration (ADAMHA) by President J. Carter. Klerman had a distinguished career as a research psychiatrist specializing in mood and anxiety disorders, and as a gifted administrator as well, holding appointments at Yale, Harvard and Cornell Universities. In the course of his research on combined medication and psychotherapy treatment of depression, he developed – with his collaborator and wife, M. Weissman – interpersonal psychotherapy 20 , which remains a leading empirically supported treatment.
Klerman was very sympathetic to neo‐Kraepelinian ideas, seeing them as a scientific advance that promised enormous progress in psychiatry. The wordings of his credo's propositions are often paraphrases of assertions in neo‐Kraepelinian articles. However, his article's tone is more that of a summary of the movement's doctrines by an appreciative witness to history rather than an insider's fervent personal manifesto. Klerman even suggests at one point that there is bound to be a reaction against what will be perceived as the movement's excesses. Klerman identifies the leading neo‐Kraepelinians as including S. Guze, E. Robins, G. Winokur, D. Klein and R. Spitzer (but see below regarding Spitzer), along with others trained during that period at the Psychiatry Department of Washington University in St. Louis. However, Klerman himself, despite giving the movement a name and a credo, did not become identified as a central figure in the movement. As we shall see, although taken with the scientific rigor of the neo‐Kraepelinians, Klerman, like Spitzer, was reluctant to adopt the movement's strictly biological ideological stance to the detriment of other forms of etiological theory and research.
THE TWO PRIMARY TARGETS OF NEO‐KRAEPELINIANISM
The neo‐Kraepelinians’ positive scientific agenda was intertwined with a negative polemical agenda of refuting two other prominent positions that they considered to be undermining the status of psychiatry. These were the antipsychiatric movement and psychoanalysis.
The antipsychiatric challenge
The philosophical motivations for neo‐Kraepelinianism are often underestimated. Its central preoccupation was to justify locating psychiatry within medicine, as stated in Klerman's proposition 1. For today's younger clinicians who grew up professionally in a neo‐Kraepelinian world in which the medical nature of psychiatry was obvious and respected, the neo‐Kraepelinian concerns about antipsychiatry must be placed in context.
Antipsychiatrists argued that psychiatry used bogus medical categories to justify the use of medical authority and technology for the social control of disapproved behavior21, 22, 23, 24, 25, 26, 27. In an unlikely alliance with antipsychiatrists, behaviorists, who were a powerful constituency within psychology at the time, argued that deviant behavior is shaped by normal learning processes in deviant environments and thus that “mental disorders” are not literally medical disorders but merely socially disapproved behavioral outcomes 28 . Psychiatrists of the biopsychosocial school who were trying to integrate the multiple perspectives relevant to mental disorder added to the confusion by lacking a clear conceptual distinction between normal‐range psychological distress and psychiatric disorder, leading, for example, to an argument that perhaps standard grief is a mental disorder after all 29 . This multipronged conceptual/ideological onslaught was combined with devastating empirical demonstrations of the unreliability and arbitrariness of psychiatric diagnosis23, 30, 31.
The undermining of psychiatry's medical credentials took an increasing toll on the profession's credibility, morale, and public support. There was a concern that psychiatry was becoming much less appealing as a specialty as a result. For example, B. Brown, NIMH Director, observed that “the proportion of medical school graduates entering psychiatric residency dropped by approximately 15% between 1972 and 1974” 32 , p.490.
The neo‐Kraepelinians recognized antipsychiatry as a fundamental threat and were absorbed by the need to rebut antipsychiatric arguments and legitimize psychiatry's medical status. Guze spent considerable time rebutting the antipsychiatrists in his paper, observing that the antipsychiatrists’ arguments cut to the heart of psychiatry as a medical discipline: “Attacks on the medical model for psychiatric disorders often reflect the belief that there is no such thing as psychiatric illness. According to this view, psychiatric diagnosis is merely a way that society labels its deviants… and only serves as a means of social control” 16 , p.301. Klerman, too, reviews the various antipsychiatrists’ positions, commenting on Foucault, Szasz, Scheff, Laing, Rosenhan, and labeling theorists, and attempts to characterize their fundamental challenge: “common to these schools of criticism is an attack on the basic concept that mental illnesses… are appropriately treated within the medical model and that psychiatry and its treatments… are legitimate medical activities” 15 , pp.108‐109.
The challenge of psychoanalytic dominance
The second primary target of neo‐Kraepelinianism was psychoanalysis. Neo‐Kraepelinians were opposed to all approaches to etiology and diagnosis that they considered non‐medical, including behaviorism, socioculturalism, and even integrative biopsychosocialism that placed the psychological and social domains on an equal footing with the biological. However, their main concern was to challenge and replace psychoanalysis as the dominant force in psychiatry.
Psychoanalytic dominance in the pre‐DSM‐III era was indisputable. Psychoanalysts chaired most psychiatry departments, determined the content of most graduate training, and authored the most widely used textbooks 33 . In a 1960 survey, 95% of medical schools reported teaching psychodynamic psychiatry, and “virtually every chairperson of a department of psychiatry stated unequivocally that the psychodynamic frame of reference (as contrasted with the descriptive or organic) was dominant” 34 , pp.429‐430.
Despite the advent of some research‐oriented psychoanalytic approaches such as attachment theory 35 , American psychoanalysis at the time still primarily adhered to Freud's classic Oedipal theory of neurosogenesis, according to which neurotic symptoms of varying kinds emerged due to unsuccessful defenses against anxiety produced by inner conflict generated during the Oedipal period of childhood psychosexual development. Psychoanalysts thus tended to downplay differential diagnosis based on symptom presentation as not very relevant to etiological understanding or treatment choice. In considering Klerman's credo, we shall find that the wording of his neo‐Kraepelinian propositions often contains implicit barbs against psychoanalysis to hasten its decline.
R. SPITZER AND NEO‐KRAEPELINIANISM: SOUL MATES OR MARRIAGE OF CONVENIENCE?
In the course of examining Klerman's neo‐Kraepelinian propositions, I am going to incrementally develop what I will call a “Spitzerian” view of psychiatric nosology. Although Spitzer's views have generally been equated with neo‐Kraepelinianism, in fact they are importantly different. Spitzer explicitly rejected some of Klerman's propositions and clearly framed the DSM‐III as differing from standard neo‐Kraepelinianism in its assumptions. I will argue that the DSM‐III is a Spitzerian document that has often been misinterpreted as a straightforward neo‐Kraepelinian document in ways that distort its nature.
This perspective may come as a surprise, because Spitzer is often asserted to be a prominent neo‐Kraepelinian or even the leading neo‐Kraepelinian, and is credited with conquering psychiatric nosology on behalf of the neo‐Kraepelinian cause. Klerman refers to him as a “New York investigator identified with the neo‐Kraepelinian approach” who was responsible for the DSM‐III's “strong descriptive approach” 15 , p.105. Blashfield, following Klerman, labels Spitzer one of the five “most prominent members of the neo‐Kraepelinian movement”, despite his not being at the institutional heart of the movement at Washington University but at “an associated setting for this invisible college” at Columbia University and New York State Psychiatric Institute 36 , p.3. Such attributions continue todaye.g., 4,13.
It is easy to see why this view is appealing. Spitzer was Chairperson of the Task Force that generated the DSM‐III revolution in diagnosis, which was hailed by neo‐Kraepelinians as accomplishing their signature goal of reinstituting descriptive diagnosis in psychiatry. As well, in eliminating a generic category of psychoneuroses that presupposed psychoanalytic assumptions about anxiety and defense, Spitzer accomplished the neo‐Kraepelinian goal of freeing psychiatry from the claimed nosological sins of the psychodynamic era. Moreover, in their nature and sometimes their literal content, Spitzer's DSM‐III descriptive diagnostic criteria sets were descended, by way of the intermediate Research Diagnostic Criteria 37 , from the so‐called Feighner criteria formulated by members of the Washington University Department of Psychiatry in pursuit of neo‐Kraepelinian research measures 38 . Spitzer also placed several leading neo‐Kraepelinian adherents on his Task Force to help oversee the development of DSM‐III 39 .
On most substantive points, Spitzer and the neo‐Kraepelinians were in agreement. Spitzer wanted to place psychiatry on a more secure scientific foundation by using the neo‐Kraepelinians’ Feighner‐style descriptive research criteria as clinical diagnostic criteria that could serve as a starting point for bootstrapping to etiological understanding, in roughly the way neo‐Kraepelinians envisioned. The overlap in scientific sensibilities and the passionate belief in shared goals meant that the neo‐Kraepelinians made ideal allies in the many battles Spitzer had to fight with various entrenched powers within psychiatry to realize the shared vision of a scientific psychiatry.
However, as I will show in the course of my coverage of the nine propositions of Klerman's neo‐Kraepelinian credo, Spitzer and the neo‐Kraepelinians were not soul mates. Instead, they entered into a marriage of convenience. Perhaps the limits of the relationship were ambiguous at the beginning, but with time it became apparent that, on important conceptual issues about the nature of psychiatry and psychiatric diagnosis, there was considerable daylight between them.
I now turn to Klerman's propositions.
1. PSYCHIATRY IS A BRANCH OF MEDICINE
The claim that psychiatry is a branch of medicine is the most basic and momentous neo‐Kraepelinian claim. I therefore examine it in some detail.
The proposition's significance may not be immediately apparent. Psychiatry is obviously a branch of medicine in a sociological or organizational sense. However, what is being raised is a conceptual question about whether psychiatry deals with medical disorders, which is the essential defining mission of medicine, whatever else it does. There can be many other reasons for being a branch of medicine in the organizational sense. Neither cosmetic surgery nor obstetrics have as their primary activity the treatment of diseases, yet those are both branches of medicine, one because the skills to be used in pursuit of aesthetic ideals are possessed uniquely by physicians, and the other for preventive reasons because pregnancy and childbirth hold many dangers to the health of mother and child.
Klerman and Schechter distinguish between the core of psychiatry as the treatment of mental disorder versus the use of psychiatric skills to help people deal with distress or realize their potential 40 (see Figure 1). Similarly, I elsewhere distinguish the essential tasks of a profession from a profession's derived tasks that result from the application of its skills to areas other than its essential domain 41 . The sense of “branch of medicine” in Klerman's proposition is intended to refer to being concerned with medicine's essential core task of treating medical disorders. This is evident from the title of Guze's paper published the same year, Nature of Psychiatric Illness: Why Psychiatry is a Branch of Medicine 16 .
Figure 1.
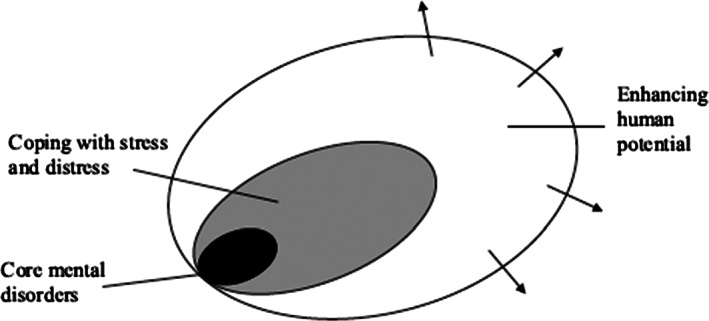
The core of psychiatry as the treatment of mental disorder versus the use of psychiatric skills to help people deal with distress or realize their potential (adapted from Klerman and Schechter 40 )
The “medical model” as a conceptual red herring
Given the way the debates about medicine were framed at the time, the neo‐Kraepelinians decided that the way to argue that psychiatry treats medical disorders and thus is a legitimate medical discipline is to argue that it appropriately adheres to the “medical model”. As Klerman explains, “The Kraepelinian revival is part of the general movement of psychiatry towards greater integration with medicine… To better understand these developments requires exploration of the ‘medical model’” 15 , p.105. However, Klerman also points out that “medical model” can mean many different things and is “a code word for controversy and debate” 15 , p.106.
Indeed, at the time – and, one could argue, also todaye.g., 42 – the expression “medical model” was often used pejoratively to refer to the asymmetric authority of the physician over the patient, the expansion of medical authority into areas of life such as giving birth and dying, the emphasis on biological processes rather than the patient's feelings and values, and the claimed dehumanizing effects of the technology‐driven physician‐patient interaction (hence, the rise of the field of “medical humanities” as an antidote).
How do Guze and Klerman think they can argue from the premise that psychiatry uses the “medical model” to the conclusion that it uses that model to treat genuine medical disorders? The argument is not crystal clear. Brilliant as they were, neither Guze nor Klerman were particularly talented conceptual analysts in the way that Spitzer proved himself to be. The usefulness of the “medical model” in treating psychiatric conditions is a pragmatic or sociological observation that cannot be equated with whether the treated conditions are genuine medical disorders, which is a conceptual‐scientific question. As Spitzer came to understand, it is ultimately the conceptual question of the criterion for psychiatric conditions being genuine medical disorders, not what model one finds most useful in treating the conditions, that determines whether psychiatry is legitimately a branch of medicine in the relevant sense that would rebut the antipsychiatrists.
Klerman suggests that there are three components to the “medical model” in a modern society: a) the disease concept; b) the sick role, consisting of certain prerogatives (you are relieved of some usual obligations) and responsibilities (you try to get better); and c) the health care system, which decides who is to be considered sick and obtain the sick role. He notes that bringing the “medical model” to mental illness was an achievement of the 19th century, and that the antipsychiatric movement wants to undo this achievement. However, Klerman's second and third features – whether society decides to place someone in the sick role, and judgments that a problem should be addressed by the health care system – should follow rather than determine the judgment that a condition is a medical disorder. Only Klerman's first feature, that psychiatry's target conditions fall under the concept of disease, determines whether psychiatry is a branch of medicine in the sense relevant to antipsychiatric claims.
Guze promisingly starts his 1978 article with the questions “Are psychiatric conditions diseases?” and “How is disease defined?” 16 , p.295 (Guze and the neo‐Kraepelinians decidedly preferred the biologically connotative term “disease” to “disorder”, a point to which I will return). But, he immediately shifts to exploring the nature of the “medical model”. This path of analysis repeatedly leads him to confront the fact that the one feature of the “medical model” that is relevant to deciding whether psychiatry is a branch of medicine is whether it is used to address genuine diseases. The “medical model”, he finally concludes, “is clearly related to the concept of disease” and its most basic feature is a “concern for the symptoms and signs of illness” 16 , p.296.
Unfortunately, when Guze refocuses on the concept of disease, he is not able to make much headway. He notes that those who argue against psychiatric conditions being diseases often rely on a definition of disease that “requires the presence of consistent pathologic changes in one or another bodily organ or evidence of a qualitative deviation from the normal in some function or process” 16 , p.297. He argues that this anatomical/physiological definition is too narrow even as a definition of physical disease, thus should not be used to exclude psychiatric conditions from disease status. However, throughout his discussion, he seems to confuse the definition of disease – what it is for a condition to be a disease – with what we happen to know about a condition at a given time. Guze uses epilepsy and cardiac dysrhythmias as examples of conditions that were long recognized as diseases based on apparent functional impairment despite lack of understanding of their pathophysiology and etiology, concluding that “among conditions most physicians and most laymen regard as medical disorders are states for which consistent anatomical changes have not yet been recognized” 16 , p.297. He is of course quite correct: medicine generally recognizes conditions as disorders on the basis of indirect evidence long before the actual etiology is known. However, Guze's understanding that one may not yet know the etiology of a condition and nevertheless from circumstantial evidence one may justifiably judge it a disorder does not resolve the problem of what makes it a disorder – that is, what we need to infer from the circumstantial evidence to conclude that there is a disorder.
Guze also refers to a definition of disease that he had proposed in an earlier paper: “any condition associated with discomfort, pain, disability, death, or an increased liability to these states, regarded by physicians and the public as properly the responsibility of the medical profession, may be considered a disease’” 16 , p.296. This definition is invalid, because it would encompass, for example, childbirth pain, pregnancy, and cosmetic concerns addressed by surgery. The sheer fact of discomfort or pain that physicians try to ameliorate cannot be used as a sufficient criterion for medical disorder. Even antipsychiatrists could agree that conditions targeted by psychiatric treatment often cause discomfort and are regarded as the responsibility of the medical profession. Their point is that these conditions are not genuine medical disorders.
Klerman's attempts to respond to antipsychiatry
Klerman presents various arguments to rebut the antipsychiatrists and show that psychiatric conditions can be genuine medical disorders, but these arguments tend to be weak. For example, he argues: “From research evidence and clinical experience it is concluded that certain of the experiences and behaviors of individuals labeled schizophrenic are abnormal. They are distressing to the individual and to those around him, and are profoundly maladaptive for the individual in relation to his family and his social grouping” 15 , p.110. The fact that purported disorders are “profoundly maladaptive”, “distressing”, or “abnormal” in a statistical sense is consistent with the antipsychiatric position. If “abnormal” is intended to mean “psychopathological”, then Klerman's argument begs the question of whether the conditions are really disorders.
Klerman comments on Laing's analysis, according to which “the locus of pathology is in the family or in the society at large”, by arguing that “it is a bizarre form of sophistry to deny the sick role and the opportunity of being treated to the patient by placing blame on the family or society” 15 , p.110. Again, this answer begs the question: it is sophistry only if in fact these individuals have disorders rather than unfortunate suffering due to oppressive familial or social structures.
In rejecting Szasz's view that mental disorder is a myth, Klerman argues: “If it is a myth, then… it is also a myth with a genetic transmission and a pharmacological antidote” 15 , p.110. This quip is a non sequitur. Antipsychiatrists such as Szasz and Laing never claimed that the condition that we call schizophrenia is a myth, although perhaps some labeling theorists came close to this. The “myth” is supposed to be that the condition is a mental disorder in a medical sense. Non‐disordered conditions can be real, genetically transmitted, painful, and alterable by psychotropic medication.
R. Spitzer's approach to the question of psychiatry's medical status
In grappling with the rationale for eliminating the category of homosexuality as a disorder from the DSM, R. Spitzer was forced to confront the question of what it means for a condition to be a medical disorder. He continued to pursue this question after the homosexuality debate had been resolved. After some false starts in which he argued that a medical disorder was defined in terms of certain kinds of harm, such as suffering or social role impairment, his thinking changed.
His broader goal, like the neo‐Kraepelinians, was to define mental disorder in a way that would convincingly locate mental disorders within medicine and counter the antipsychiatrists. In considering obvious counterexamples to his earlier definitional attempts, as well as objections from his colleagues, he concluded that the only way to accomplish this was to first clarify the meaning of medical disorder and then define mental disorder as a subdomain of medical disorder 43 . This led to his analysis of the concept of mental disorder, coauthored with J. Endicott, that was published in the same year as Klerman's article.
Spitzer and Endicott argued that the basic intuition behind the concept of a medical disorder is that “something has gone wrong with the organism” that yields harmful symptoms. They expressed the necessary condition that something has gone wrong by the phrase “organismic dysfunction”. The attempt to explain why mental disorders are best understood as a subcategory of medical disorders led them to a dysfunction requirement: negative consequences alone are insufficient as a definition of disorder, due to the existence of many painful conditions that are not medical disorders. The expression “organismic dysfunction” was shortened to “dysfunction” in the definition that appeared in Spitzer's introduction to the DSM‐III, which required that “there is an inference that there is a behavioral, psychological, or biological dysfunction” 44 , p.6. The dysfunction requirement has then appeared in the definition of disorder in every subsequent DSM edition, as well as in the ICD‐11 45 . Whereas the symptoms are manifest, the presence of dysfunction – that something has gone wrong in the organism – is inferred from the symptoms, with the nature of the inferred dysfunction generally unknown.
Spitzer and Endicott did not yet have an evolutionary understanding of dysfunction. Indeed, Spitzer later admitted that he was quite baffled by the problem of how to explicate the idea that something has gone wrong inside the organism. However, he eventually endorsed my evolutionarily based “harmful dysfunction analysis” of medical – including mental – disorder, according to which the relevant dysfunctions are failures of internal physical or psychological mechanisms to perform natural functions for which they were biologically designed (i.e., naturally selected)46, 47, 48, 49, 50, 51, 52. Spitzer concluded that this is the only plausible way to scientifically ground the notion of dysfunction53, 54.
A glance at DSM confirms that the categories of disorders do seem to capture what are prima facie failures of biological design. That is, the categories tend to correspond to domains in which it seems highly plausible that there are biologically designed mechanisms and natural functions, and the described conditions appear to be ways in which those mechanisms can go awry. For example, human developmental processes, thought, emotions, appetite and sexuality are all areas in which one would expect that complex adaptive mechanisms have been naturally selected, so that failures of expectable functions tend to be dysfunctions.
Spitzer's analysis has to some extent reshaped the discussion on psychiatry's status. Skeptical challenges raised today, as in the neurodiversity movement's claims that autism is illegitimate pathologization of normal brain variation, in critiques of attention‐deficit/hyperactivity disorder (ADHD) as pathologizing normal child rambunctious behavior, or in objections to eliminating the major depression bereavement exclusion55, 56, 57, generally do not question psychiatry's legitimacy as a branch of medicine. Rather, they question whether the concept of mental disorder is being applied correctly to the specific category at issue and argue that psychiatric diagnostic practices are generating false positive diagnoses.
However, antipsychiatric attitudes are still powerful in some constituencies, and this struggle is hardly resolved. Even today there are sometimes reactions against the “biomedical” approach, and the argument against biomedicalization is often misdirected due to conceptual confusion. On the one hand, psychiatrists are accused of “medicalizing” various aspects of life that are not strictly disorders, and on the other they are accused of applying a narrow “biomedical” approach which neglects the broader mental health needs of the population that extend well beyond disorder.
2. PSYCHIATRY SHOULD UTILIZE MODERN SCIENTIFIC METHODOLOGIES AND BASE ITS PRACTICE ON SCIENTIFIC KNOWLEDGE
This is a proposition that anyone interested in advancing psychiatric knowledge, neo‐Kraepelinian or not, could endorse. More sophisticated science is undeniably the most promising pathway to optimal diagnosis and treatment of those suffering from mental disorder. A major benefit of neo‐Kraepelinianism has been the focus on generating cumulative and relevant scientific knowledge about etiology and treatment using the most advanced research methods.
Proposition 2 also appears intended as a rebuke to the American classic psychoanalytic school that was perceived as unscientific. Such criticisms seem justified. It was the sad fate of classical clinical psychoanalytic theory of that era to fail to transcend the unscientific sexual etiological theories of Freud 58 .
The DSM‐III's embrace of the syndromal approach to diagnosis, whatever its problems, has yielded an explosion of scientific research on mental disorders using the most advanced methodologies and data‐analytic techniques. A major benefit of neo‐Kraepelinianism is that the psychiatry profession's use of research‐style criteria in clinical diagnosis has allowed for the generation of an increasing amount of scientific research on psychiatric conditions that is directly relevant to the clinical categories used by clinicians. Because research from varying approaches use the same criteria for sample selection, the results can be compared and accumulated into a picture of treatment effectiveness.
On the other hand, the yield in terms of major breakthroughs in etiological understanding or treatment effectiveness is much less than one might wish. Although we base practice on scientific knowledge to the degree that we can, our decision making is far from being fully scientifically based, because we know so little.
3. PSYCHIATRY TREATS PEOPLE WHO ARE SICK AND WHO REQUIRE TREATMENT FOR MENTAL ILLNESSES
Proposition 3 is a corollary of proposition 1. For psychiatry to be a branch of medicine, it must treat medical disorders as its defining core mission. However, this proposition requires interpretation because, if taken in a logically strong sense – as asserting that psychiatrists appropriately treat only mental disorders – it is obviously false. Psychiatrists appropriately treat many problematic psychological conditions that are not mental disorders, as the DSM‐ICD systems officially recognize in their large sets of psychological “Z Codes”, i.e. problematic psychosocial conditions that are not disorders but for which psychiatrists are frequently consulted.
Klerman subsequently corrected any possible misunderstanding on this score in a follow‐up article with Schechter in which he explained that, in addition to its core domain of mental disorders, psychiatry is also mandated to treat “problems involving significant amounts of psychological and emotional distress associated with the stress of daily life but that do not meet the criteria for a diagnosable mental disorder” as well as “people… who seek to enhance their own potential, heighten their awareness, or improve their mental health” 40 , p.122 (see Figure 1).
However, to make treatment of mental disorder the core of psychiatry's mission, one must be able to distinguish the mentally disordered from the non‐disordered. This is precisely the assumption to which the antipsychiatrists objected, claiming that any such distinction consists of arbitrary labels serving social control purposes. This brings us to the neo‐Kraepelinian assumption that disorder can be distinguished from non‐disorder, and thus to Klerman's proposition 4.
4. THERE IS A BOUNDARY BETWEEN THE NORMAL AND THE SICK
The neo‐Kraepelinians understood that a defensible disorder/non‐disorder boundary, even if fuzzy, is essential for distinguishing mental disorder from normal‐range socially deviant, disapproved, or problematic behavior or distress, and so is required to respond adequately to antipsychiatric critics.
Physicians clearly have the ability to at least roughly distinguish disorder from normality in most domains. Despite all the controversies and missteps in the history of medicine, if one examines the diagnostic compendiums of antiquity, one finds that, despite lack of knowledge and wildly incorrect theories of underlying dysfunctions and normal physiology, almost all the conditions classified as medical disorders still would be seen as such today. This suggests that physicians are pretty good at using circumstantial evidence to judge that something has gone wrong with how individuals are biologically designed to function. Proposition 4 thus reflects a point basic to the bootstrapping process on which neo‐Kraepelinian progress in nosology rests. On the basis of syndromal symptoms, one can often (fallibly) distinguish a category of clearly disordered conditions from clear normality. This provides a starting point for research to establish one or more etiologies present in the disordered group – although carrying out this part of the program has thus far proven more difficult than envisioned.
Proposition 4 thus concerns only a disorder category's conceptual validity, which refers to the category's including only disordered conditions 46 . Conceptual validity is a much more limited initial goal than the more demanding ultimate goal of construct validity, which refers to the category's including only disorders with a homogeneous etiology based on the same type of underlying dysfunction.
DSM syndromal diagnostic criteria sets are designed to achieve conceptual validity. Every feature of the diagnostic criteria sets, including duration requirements, symptom thresholds, the specific nature of the symptoms, the frequency, intensity and persistence of the symptoms, and even contextual exclusions for scenarios in which symptoms can be better understood as normal reactions to a challenging environment, are all attempts to operationalize the notion that something has gone wrong and allow an inference to dysfunction versus a normal‐range form of distress or problem in living59, 60, 61. There is of course also a hope, usually forlorn, that the criteria may have construct validity.
To see the two forms of validity at work, consider the first sentence of Robins and Guze's classic article on validating diagnostic categories: “Since Bleuler, psychiatrists have recognized that the diagnosis of schizophrenia includes a number of different disorders” 62 , p.983. The assumption is that one conceptually valid disorder category, schizophrenia, can be refined into multiple construct valid disorders. Klerman, too, explains that schizophrenia is a syndrome that likely encompasses multiple etiologies, so that refinement into more construct valid categories is called for. Kraepelin suggested that one way to increase construct validity from initial syndromal categories is by a gradual refinement process of addition and subtraction based on syndromal features and etiological discoveries 63 . To make the mistake of thinking that the initial syndromes are already the individuated disorders that are the end‐goal of the process is to illegitimately “reify” syndromes into disorders 64 .
The challenge of conceptual validity: was uniting research and clinical criteria a mistake?
Achieving conceptual validity has turned out to be surprisingly difficult, once psychiatry focused less on the asylum, with its extreme clearly disordered conditions, and more on the community, with its many varying forms of normal distress and deviance that are often difficult to distinguish from disorder strictly on symptomatic grounds. Under these circumstances, the neo‐Kraepelinian vision called for an aggressive and systematic anti‐false‐positives stance if validity goals were to be preserved. However, such a stance was not forthcoming.
The pursuit of conceptual validity is one place that suffered possible negative side effects from Spitzer's remarkable accomplishment of uniting clinical and research criteria. The Feighner and Research Diagnostic Criteria that preceded the DSM‐III were formulated with research in mind. However, Spitzer quickly recognized the potential for a revolution in psychiatric diagnosis by re‐conceptualizing neo‐Kraepelinian research diagnostic criteria as clinical diagnostic criteria as well. This brilliant tactic created a novel direct link between research studies and the clinician's need for guidance in treatment choice. Rather than by a gradual process of rectification of clinical and research needs, in one fell swoop clinical diagnosis was brought to the greater level of precision required in research.
The problem is that, once this link was forged, the influence went in both directions. The formulation of research criteria was now influenced by feedback from the practical concerns of the clinician. The relentless process of addition to and subtraction from diagnostic categories that might have led from initial syndromal categories to etiologically more homogeneous categories or at least more conceptually valid categories was impeded by a host of clinical utility concerns.
In clinical intervention, fear of false negatives often outweighs concerns about false positives when treatment is not risky. In the US, many clinicians need a disorder diagnosis to obtain insurance reimbursement, so there is pressure to have categories that encompass the problems for which people seek help even if they are not disorders. An admirable humanitarian impulse causes clinicians to want to help as many people as they can, and thus DSM work groups are biased toward inclusion independent of strict etiological considerations. As N. Ghaemi trenchantly put the problem: “Why should neuroanatomy correlate with wishes for insurance reimbursement?” 65 . This is precisely the opposite of what is needed for advancing the neo‐Kraepelinian research agenda. The uniting of research and clinical criteria may have exacerbated the false positives problem to the point of being the death‐knell for the serious pursuit of the neo‐Kraepelinian program.
There are many illustrations of the approach to validity gone awry due to clinical utility considerations taking precedence, but one of the most striking concerns the category of substance abuse. Whereas addiction can be understood as a genuine mental disorder, sheer use of a substance in a way that may be excessive or harmful or causes arguments with one's family or leads to legal difficulties does not imply mental disorder. This was sufficiently apparent that the category of substance abuse, introduced in the DSM‐III, was slated to be eliminated from the DSM‐III‐R 66 . This decision was reversed at the last minute due to the consideration that the categories and criteria should allow treatment for as many people as possible who could be helped by it.
Remarkably, during succeeding DSM revisions, this pragmatic consideration repeatedly won out over scientific validity considerations, and the substance abuse category was retained, inflating disorder estimates and confusing scientific endeavors. Finally, in the DSM‐5, the category of substance abuse was eliminated. However, the work group argued that “the substance use disorders criteria represent a dimensional condition with no natural threshold”. So, “to avoid a marked perturbation in prevalence without justification, the work group sought a threshold for DSM‐5 substance use disorders that would yield the best agreement with the prevalence of DSM‐IV substance abuse and dependence disorders combined” – that is, they attempted to match the previous dependence and abuse prevalence despite abuse's invalidity. Challenged on the grounds that such a low threshold would not represent true cases and would reduce etiological homogeneity, the committee answered: “These understandable concerns were weighed against the competing need to identify all cases meriting intervention” 67 , p.841. That is, clinical utility outweighed concerns about conceptual validity, let alone construct validity.
It is true that each DSM revision has corrected some obvious false‐positive mistakes in the diagnostic criteria. For example, the DSM‐5 added to insomnia disorder the requirement that “the sleep difficulty occurs despite adequate opportunity for sleep”, to eliminate false positives due, for example, to a neighbor's late‐night television viewing; DSM‐5 oppositional defiant disorder newly excludes diagnosis if the defiant behavior is directed only toward a sibling, because sibling relations can normally include such behavior; and the DSM‐5 finally introduced the requirement that a sexual dysfunction can be diagnosed only if lack of sexual response in a relationship is not better explained as a consequence of severe relationship distress such as partner abuse or violence. Such ad‐hoc corrections are useful. However, they are no substitute for systematic category‐by‐category attention to the problem of false positives.
Implications of the failure to confront the false positives problem
The failure to aggressively confront the false positives problem raises a disturbing question. As unlikely as it may seem after four decades of perceived neo‐Kraepelinian diagnostic hegemony, it is nonetheless possible that neo‐Kraepelinianism, to borrow G.K. Chesterton's remark about Christianity, “has not been tried and found wanting; it has been found difficult and not tried” 68 . The neo‐Kraepelinian program – including Klerman's pivotal proposition 1, that psychiatry is inherently medical – rests on proposition 4's claim that disorders can be separated from problematic non‐disorders, so that scientific identification of homogeneous dysfunction etiologies can proceed. If psychiatry has not taken the boundary between disorder and non‐disorder seriously enough to avoid having admixtures of normal distress and true disorder in many of its central categories, then that makes scientific bootstrapping to identification of distinct dysfunctions extremely difficult.
Kraepelin was well aware of the false positives problem. Although unmentioned in recent articles analyzing his approach to diagnosis, Kraepelin attended to identifying potential false positive cases and sometimes explained the basis for judging a potentially ambiguous condition to be a true case: “Morbid emotions are distinguished from healthy emotions chiefly through the lack of a sufficient cause, as well as by their intensity and persistence… Again, morbid emotions sometimes attach themselves to certain external occasions, but they do not vanish with the cause like normal feelings, and they acquire a certain independence” 69 , p.68.
Sometimes, Kraepelin made a difficult judgment about a first episode that was only justified by later developments, with the benefit of time having passed. For example, he admits that some women's intense depressive episodes after the death of their husbands could be seen as a normal‐range depressive reaction except for evidence that emerged later: “A woman fell ill three times of depression after the death first of her husband, next of her dog, and then of her dove. Another patient was depressed after the death of her husband, manic after a confinement and after a dental operation” 70 , pp.179‐180.
Kraepelin likely would have been shocked to hear the eminent psychiatric epidemiologist R. Kessler explain to an interviewer the then‐controversial findings of a major psychiatric epidemiological study indicating that 50% of Americans experience mental disorders: “Well, we found that… about half the population meets criteria for at least some mental disorder at some point in their life, but I think it's important to put this in context…. There are many people who have minor phobias, who, for three or four weeks, get depressed after they move from one town to another or break up with a relationship. Perhaps they have some panic problems for a month or two after they get into a life‐threatening automobile accident. But most of these things are very minor. They're self‐limiting. They go away on their own. And they're the stuff of day‐to‐day life that we all experience at some time or another” 71 .
This answer was evidently troubling enough that the then‐President of the American Psychiatric Association, S. Sharfstein, felt the need to comment on the obvious doubts it raised about psychiatric diagnosis: “The study raises many questions and issues about the nature of psychiatric disorders… Does our DSM nosology have too low a threshold in selecting symptoms of mental disorders? Many of these disorders may be self‐limiting and mild in response to life stresses… How much credibility does our diagnostic system lose by attaching a psychiatric diagnosis to these relatively mild and self‐limiting problems?” 72 .
Ultimately, however, it is not just public credibility but also scientific validity that is sacrificed if diagnostic categories are not conceptually valid. D. Regier, later the DSM‐5 Task Force Vice‐Chair, suggested that there was indeed a problem: “Based on the high prevalence rates… it is reasonable to hypothesize that some syndromes in the community represent transient homeostatic responses to internal or external stimuli that do not represent true psychopathologic disorders” 73 , pp.112,114. Since Kessler's and Regier's remarks, studies using superior longitudinal epidemiological methods have shown that the prevalence rates of individuals meeting DSM criteria for disorder is much higher even than Kessler's 50%74, 75.
An initial step toward taking false positives seriously was taken by P. Clayton, in her classic study of false‐positive diagnoses of depression during normal grief 76 . Whereas depressive criteria had been validated previously by showing that they differentiated depression cases from cases of physical illness and from normal individuals77, 78, Clayton realized that this did not directly address the false positives problem. She adopted the strategy of studying a group of presumptively non‐disordered individuals that was feared might be falsely diagnosed, namely, grief‐stricken people who had recently lost a loved one. Her research established that many of these individuals did indeed satisfy standard diagnostic criteria despite presumed lack of disorder.
Clayton's work resulted in the DSM‐III incorporating a bereavement exclusion to reduce false positives for major depression. Her work was not followed up with research targeting other stressful sources of transient normal‐range depressive feelings, even though she herself urged such expansion 76 . Despite recent replicated epidemiological evidence that the bereavement exclusion picked out conditions that were dramatically more benign in outcome than other depressed individuals79, 80, 81, 82, 83, 84, 85, the exclusion was eliminated in the DSM‐5 as a formal part of the diagnostic criteria and replaced by an ambiguous note suggesting that clinicians identify false positives without guidance from diagnostic criteria. The resulting number of possible false positives is unknown. One hint is that a recent analysis found that about 13% of all the individuals classified as depressively disordered by DSM‐5 criteria in a major epidemiological study had experienced their episodes only after the death of loved ones and lasting less than two months – and that is just for bereavement and not including the larger domain of potentially normal‐range reactions to other stressors to which Clayton alluded 86 .
The general lack of adequate attention to context distinguishes the DSM criteria for major depression from the way physicians from ancient times to Kraepelin thought about depressive pathology. For example, the major risk factor by far for an initial episode of major depression in an adolescent is the breakup of a romantic relationship. Classic physicians would have looked askance at any easy equation of these conditions. Galen himself provides a case in which he ponders whether a woman is suffering from melancholia or unrequited love (it turns out to be the latter). Our fascination with the symptom approach has seemingly been elevated into a fetish that has defeated the seriousness of the neo‐Kraepelinian aspirations that started us down this path.
There are, of course, many ways to study false positives other than Clayton's simple and direct method (see, for instance, the later discussion on the DRD4 gene in the section on proposition 6). Moreover, this is clearly not an issue unique to depression. The point is that the problem of false positives has simply not been pursued systematically, undercutting the possibility of giving neo‐Kraepelinian aspirations a chance of being realized.
The threat to proposition 4 from dimensional approaches to diagnosis
I noted in the introduction that, in response to the perceived failure of the neo‐Kraepelinian program, a variety of nosological proposals have emerged to compete as its replacement. Prominent among these options is the view that syndromes may be decomposed into a hierarchy of factor‐analytically determined dimensions, yielding a fully dimensionalized classification system.
Dimensional and factor analytic explorations of the psychometric structure of the space of symptoms of mental disorders are a welcome development. However, beyond potential scientific contributions, there is a push to fully transform our nosology into a dimensional system. This movement has gathered momentum and is endorsed by many leading researchers and nosologists, as in the HiTOP version of dimensionalization6, 7, 8, 9. In fact, dimensionalization was embraced as one of the prime goals of the DSM‐5 Task Force: “We have decided that one, if not the major, difference between DSM‐IV and DSM‐V will be the more prominent use of dimensional measures in DSM‐V” 87 , p.649.
The most common dimensional proposals simply arrange the conditions that fall within a pre‐defined DSM category according to the severity of symptoms, as was done, for example, with autism spectrum disorder and substance use disorder in the DSM‐5 and personality disorder in the ICD‐11. The DSM‐5 Task Force intended to add such symptom‐severity dimensional measures to all the major disorders, but decided against it for reasons that were scientific (the scales were not adequately validated), of clinical utility (there was inadequate understanding of how treatment choice should vary with severity rating), as well as pragmatic (reimbursers might decide to set their own severity thresholds for treatment reimbursement). Dimensionalization of this kind presupposes a symptomatically defined category of disorder on which the severity measure is imposed, and such severity scales are frequently imposed on disorders in physical medicine as well. This sort of dimensionalization involves no challenge to categorical diagnosis and is entirely consistent with neo‐Kraepelinianism.
Stronger forms of dimensionalization replace and transcend the pre‐existing diagnostic categories. For example, some members of the DSM‐5 Task Force at one point imagined replacing the entire categorical system with a system of severity dimensions of various types of symptoms that are applied to the entire population and would yield a unique “diagnosis” for each individual consisting of a point in the multidimensional severity grid, replacing all current categorical diagnoses. A major criticism of DSM‐ICD by those who want to replace the categorical nosological system with a dimensional system is that DSM‐ICD categories provide “scientifically arbitrary diagnostic cut‐offs” 4 or “arbitrary boundaries between psychopathology and normality” 6 .
The problem with strong dimensionalism from a neo‐Kraepelinian perspective is that it lacks a concept of dysfunction that locates the extreme conditions within the medical domain. Dysfunctions and normal variations alike may be on the extreme of a dimension. So, without some additional dysfunction criterion, strong dimensionalism would dislocate psychiatry from medicine. The antipsychiatrists would be delighted with this account: what else is social deviance than being extreme on some socially defined dimensions? In fact, one typically sees dimensionalists shifting their terminology from “pathological” to “maladaptive” to reflect these presuppositions, and “maladaptive” is just one step away from “socially disapproved” and the reawakening of antipsychiatric forces. Dimensionalists criticize the DSM‐ICD for having arbitrary boundaries – which, we shall see, is only partly true – and then propose a system that formally does away with non‐arbitrary boundaries.
In this approach, a disorder is nothing but being extreme on a dimension, or perhaps being extreme on a dimension in a problematic or harmful way. An unappreciated problem with this approach is that the essence of a population‐distribution dimension is different from the essence of a disorder. There are populationally distributed traits such as sadness, anxiety and weird thinking that are mostly features of non‐disordered individuals. Without some additional explanation as to why those same features in their extreme versions should be considered disordered, the strong dimensionalist program yields to arbitrariness. Consider, for example, H. Eysenck, who also went down the path of dimensionalization and found that, no matter how high up he went on the psychoticism scale, it was not equivalent to psychotic disorder 88 .
Nevertheless, psychologists regularly argue for strong population‐based dimensional approaches based on the greater statistical analytical power they yield 4 , generally ignoring the impact that such a system would have on the medical status of psychiatry, while nevertheless continuing to use medical language. Other dimensionalists, like behaviorists before them, are honest enough to confront the antipsychiatric implications of a strong dimensionalist view that offers no non‐arbitrary boundary between disorder and normality. Thus, for example, the eminent geneticist and psychologist R. Plomin dramatically claims that “there are no disorders” 89 , p.23, and that “the abnormal is normal, meaning that there are no qualitative disorders, only quantitative dimensions” 90 , p.128.
A group of leading researchers and nosologists conclude: “all thresholds in mental illness should be regarded as arbitrary”5, p.74. Yet, at another point, the same authors note that “such categories as infant, toddler, child, and so on represent semiarbitrary but useful divisions along the continuum of age”5, p.75. Surely such divisions are not arbitrary; a normal individual at age 3 is a child and a normal individual at age 25 is an adult by the very meaning of the concepts “child” and “adult”. What they presumably mean is that the distinction is fuzzy – it is non‐arbitrary within extensive domains but arbitrary for a fuzzy boundary zone (and perhaps for some pathological instances or instances in which development is intentionally medically manipulated). So, if a precise line must be drawn, then there is some arbitrariness. But, the substantial non‐arbitrariness due to clear cases exists for most real distinctions, including disorder versus non‐disorder. The concept “extreme on a population dimension” has no such non‐arbitrary domains corresponding to clear cases of disorder and non‐disorder.
The dimensionalist critique of DSM‐ICD includes several other standard complaints that the proposed approach is claimed to address. It is claimed that dimensionalism eliminates diagnostically messy and puzzling comorbidity because everyone falls at one multidimensional point on the system of dimensions, so everyone has just one condition. This “solution” evades all the interesting causal questions that need to be addressed about comorbidity and provides merely a technical terminological “solution” without advancing understanding. The comorbidity questions will just reappear in the statistical analyses of the co‐occurrence of various factors, even if it is no longer called comorbidity. There are all sorts of reasons – e.g., common risk factors, unusually stressful environments that trigger multiple dysfunctions – why more than one disorder might occur at the same time. For comparison, about 77% of older individuals have two or more chronic physical disorders at any one time, not including additional transient disorders. Given the high level of interaction and integration among psychological modules, dysfunction in one module could tend to cause unusual behavior or even dysfunction in another linked module, even though “pure” one‐module dysfunctions are also possible.
It is also claimed that dimensionalism addresses problematic heterogeneity within disorder categories. Dimensionalization provides a technical sidestepping of this issue without resolving or addressing the scientific substance. The various symptom realizations of a disorder are based on theory and clinical experience, and are supposed to reflect possible alternative ways that an inferred common type of dysfunction might manifest itself. That is correct or incorrect in each case, but is ultimately an empirical question not resolved by dimensional reorganization.
The number of different syndromal conditions satisfying some DSM‐ICD diagnostic criteria sets is frequently cited to show the absurdity of the DSM‐ICD system. However, this is an empirical question, and it is the criticism that is absurd. Just to take a simple example all too close at hand: upon searching, I get a list of 16 possible COVID‐19 symptoms and, if any two or more of them is considered cause for inferring possible disease, that means there are 65,519 symptom profiles, many non‐overlapping, that get you a likely diagnosis. It is a scientific question whether the evidence of causation from the same underlying cause is solid, not a matter of ridicule because a single dysfunction may have such a wide array of presentations. Certainly diagnostic heterogeneity will be a scientific focus as genetic studies give us the power to tease apart syndromal variations that were mistakenly lumped together under one postulated dysfunction type, and also to unite syndromal presentations that look like they are products of different dysfunctions. None of these substantive issues are addressed by sheer dimensionalization.
To become a profession concerned with dimensionally extreme maladaptive behaviors would take psychiatry into a morally controversial terrain. If it is true that “revenge is a dish best served cold”, then many psychologists who objected to Spitzer's implicit medicalizing of psychiatry to end the antipsychiatric threat must be salivating now, as the totally non‐medical psychological mainstay of statistical studies of populations is perhaps poised to encompass psychiatry.
5. THERE ARE DISCRETE MENTAL ILLNESSES. MENTAL ILLNESSES ARE NOT MYTHS. THERE IS NOT ONE BUT MANY MENTAL ILLNESSES. IT IS THE TASK OF SCIENTIFIC PSYCHIATRY, AS OF OTHER MEDICAL SPECIALTIES, TO INVESTIGATE THE CAUSES, DIAGNOSIS, AND TREATMENT OF THESE MENTAL ILLNESSES
Are there many mental disorders?
We already dealt with the issue of “mental illnesses are not myths” when considering the proposition 1 of Klerman's credo. Moreover, if there are mental disorders, then it surely follows that “it is the task of scientific psychiatry… to investigate the causes, diagnosis, and treatment of these mental illnesses”. So, consideration of proposition 5 comes down to two further claims that can be combined into one: “there are many discrete mental disorders”.
Guze elaborated the idea in his 1978 paper: “there are many psychiatric disorders, each with a different clinical picture, natural history, etiology, pathogenesis, and response to treatment” 16 , p.306. This claim was basic to the diagnostic aspirations of the neo‐Kraepelinians in opposition to psychoanalytic theories postulating one Oedipal etiology, and behaviorist theories claiming that all behavior is normal learning.
How many distinct mental disorders there are is ultimately an empirical question. The neo‐Kraepelinians were, of course, well aware of the many‐to‐many relationship of biological etiologies and symptomatic presentations in physical medicine. Even among biologically oriented psychiatrists in the 19th century, there were some who argued that all mental disorder was likely due to just one or a few fundamental pathologies. Kraepelin himself wondered toward the end of his career whether his basic division of dementia praecox and manic‐depressive insanity did not hide one condition emerging in varying presentations. So, other than anti‐psychoanalytic animus, what were the grounds for the neo‐Kraepelinians’ claim that there exist many discrete mental disorders?
One answer is that the neo‐Kraepelinians were impressed by what at that time seemed to be a promising specificity of the effects of psychopharmacological medications on various psychiatric conditions, although confidence in “pharmacological dissection” has waned considerably over time. In any event, there is a more basic theoretical argument implicit in Guze's writings that suggests the plausibility of there being many discrete mental disorders. Guze argues for an evolutionary perspective on the brain as the complexly biologically designed basis for our many distinct psychological capacities and thus as a foundation for biological psychiatric theory: “I start my argument with evolution, the bedrock of modern biology. Of central interest to psychiatry is the fact that evolution has shaped the development of the brain – the organ of mental functions or what we call the mind… All brain functions, including perception, learning, thought, memory, emotions, communication, language, etc. reflect the results of such evolution. The capacity to feel, to be aware, to recognize, to remember, to learn, to talk, to think all depend upon this wonderfully evolved brain with its still mysterious complexity, made possible by what we must take to be a finite genotype… devoted to programming the brain”17, pp.315‐316.
Guze's evolutionary arguments are primarily aimed at supporting the primacy of brain functions in determining mental functions and thus a biological foundation for psychiatry. However, they also presuppose that the brain must have many distinct mechanisms to support so many distinct mental capacities. For example, thinking, perception and hunger are so different from fear, sadness and joy to lead one to suppose that the brain mechanisms which are programmed to provide these presumably evolved capacities must be distinct, whether in actual structure or in differential response capacities of the same structure. It seems plausible and indeed inevitable that dysfunctions can occur in each of these psychological domains independently of problems with the others – high rates of comorbidity notwithstanding, as that could be due to the rich interactions among the various brain features underlying the functional capacities.
In current philosophical and evolutionary‐theoretical terms, the postulation of many distinct brain processes devoted to various evolved capacities is known as the “modularity of mind” hypothesis91, 92, 93, 94, 95, 96. If one combines a recognition of the complexity of the brain's many different biologically designed processing domains with the view that disorders are individuated by underlying dysfunctions, and one adds the commonsense observation that “whatever can go wrong, will go wrong”, the conclusion follows that there must be many different mental disorders. Experience seems to confirm that complexly designed entities with many designed sub‐processes, whether biological or artifactual, can go wrong in many different ways.
Spitzer versus the neo‐Kraepelinians on discreteness
The claim that mental disorders are discrete can have various meanings. From the time of the DSM‐III through today, the generally accepted understanding of discreteness within psychiatry is in terms of the “zones of rarity” account elaborated by R. Kendell97, 98. In early studies of depression, Kendell defined discreteness in terms of discontinuities along dimensions either of symptoms or of observable correlates of symptoms such as course, outcome, or response to treatment: “Proof that two clinical syndromes are distinct entities depends on a demonstration that patients with features of both syndromes are less common than those with features only of the one or the other… a bimodal distribution of scores must be demonstrated on some chosen dimension” 99 , p.257. Such discontinuities are evidence of natural boundaries: “Diagnostic categories defined by their syndromes should be regarded as valid only if they have been shown to be discrete entities with natural boundaries that separate them from other disorders” 100 , p.4. The wide acceptance of Kendell's zones‐of‐rarity test has had momentous consequences for nosology. The frequent failure to find such zones has accelerated the trend toward dimensionalization.
No doubt Spitzer had Kendell's work in mind when he renounced any commitment to the discreteness of mental disorders and thus his view became distinct from standard neo‐Kraepelinianism. Soon after the appearance of the DSM‐III, R. Blashfield published a paper citing the Feighner criteria and Klerman's nine propositions as the basis for an inordinately influential neo‐Kraepelinian “invisible college” within psychiatry 36 . Blashfield cited Spitzer as a leading neo‐Kraepelinian, so Spitzer decided to publicly clarify his position and make explicit the differences between him and the neo‐Kraepelinians.
In his published commentary, Spitzer notes that Blashfield says he adheres to Klerman's “neo‐Kraepelinian credo, nine articles of faith”, and states unequivocally: “I take this opportunity… to offer my resignation publicly from the neo‐Kraepelinian college as I do not subscribe to two of these articles of faith”. The first one that Spitzer rejects is Klerman's proposition 5, that there are discrete mental illnesses. In his explanation, Spitzer quotes directly from his own introduction to the DSM‐III as proof: “Article five states: ‘There are discrete mental illnesses’. As stated in one of the required texts of this college, DSM‐III, ‘In DSM‐III there is no assumption that each mental disorder is a discrete entity with sharp boundaries (discontinuity) between it and other mental disorders, as well as between it and No Mental Disorder’. This is an empirical issue and the available evidence supporting discontinuity… is far less than compelling”101, p.592.
It may seem incomprehensible that the designer of the DSM‐III categorical system denied that such a system presupposed discrete categories of disorder. Spitzer clearly intended the categories of DSM to be taken in a more flexible way than critics have construed it. For Spitzer, we have seen, the crucial test of conceptual validity – that is, that the categorized conditions fall within the medical realm, even if not yet sorted into construct‐valid individual disorders – is that they are caused by something‐gone‐wrong dysfunctions. Dysfunctions or their symptoms might conceivably be continuous with each other, so discreteness of categories of disorder is largely independent of the deeper discreteness issue of dysfunction versus normality.
6. THE FOCUS OF PSYCHIATRIC PHYSICIANS SHOULD BE PARTICULARLY ON THE BIOLOGICAL ASPECTS OF MENTAL ILLNESS
Neo‐Kraepelinianism was inspired by discoveries of brain‐based etiologies for prominent mental disorders, including general paresis, pellagra and Alzheimer's disease. The neo‐Kraepelinians paid lip service to various psychological, family, developmental and cultural influences on mental disorder, as well as to the fact that almost all human features result from some degree of genetic or biological interaction with environmental influences. However, when they consider the concept of mental disease, they sideline all of the non‐biological factors and affirm the unique primacy of specifically biological etiologies as supporting the attribution of medical and psychiatric disorder.
“Biological” can be understood here in the sense of anatomical or physiological features. It appears that Guze, lacking Spitzer's “dysfunction” criterion, mistakenly thought that the presence of a biological substrate was needed to guarantee that a mental condition was a medical disorder. He systematically defends such a biological view, concluding: “There is no such thing as a psychiatry that is too biological… The conclusion appears inescapable to me that what is called psychopathology is the manifestation of disordered processes in various brain systems that mediate psychological functions. Psychopathology thus involves biology”17, pp.315,317.
Guze puts forward many rather weak arguments for biological etiology. He argues that nobody has yet demonstrated a non‐biological etiology for a mental disorder, but, with few exceptions, the same is true for biological etiology. He argues that the non‐biological psychological and social factors often cited as causes of mental disorder are generally experiences too common in human life to be the specific cause of disorder, but does not consider the possibility of more specific factors. He argues that, even where some non‐biological determinant might be shown to play a causal role, one still has to explain why some exposed to the determinant develop a disorder and most do not in terms of differential biological factors. However, he fails to mention that the same holds true for many biological determinants and that there is no reason to assume that the missing part of the explanation must be biological. Indeed, Freud used precisely the same argument to justify the Oedipal interpretation of Little Hans's development of a horse phobia after witnessing a horse accident, because, he pointed out, not all boys who witnessed such an accident would fall ill 102 .
Guze exiles all non‐biological factors to the scientific periphery, as influencing the disease process but not being the specific etiology: “An individual's socioeconomic circumstances, education, job, marital status, religion, and temperament may influence his risk of developing a given disorder, may play a role in determining when and whether he will seek medical care, may color the way he describes his symptoms, and may be important in determining treatment and its outcome. But the diagnosis… is not based upon this background” 16 , p.299. Guze develops an extended analogy of psychosocial factors in mental disorder to non‐specific factors in heart disease: “Certain symptoms of coronary atherosclerosis, those of myocardial ischaemia, are frequently and regularly precipitated by physical activity and emotion. But no one therefore challenges the belief that coronary artery disease is a biological phenomenon and that trying to understand the genetic and epigenetic factors that lead to differential vulnerability to coronary atherosclerosis is the most promising strategy for research and hope for truly effective intervention. And no one is likely to suggest that intervening to reduce physical activity or emotion‐provoking experiences is likely to be of more than marginal importance… It seems highly likely that the same overall conceptual strategies will prove to be appropriate for conditions such as schizophrenia, obsessional disorders, depression, mania, etc.” 17 , p.317.
Klerman does not offer much in the way of explicit argument for the neo‐Kraepelinian belief in the necessary biological focus of a medical psychiatry. In fact, he seems uncomfortable with it. He makes clear that the syndromal approach to diagnosis is designed to serve the goal of creating homogeneous categories with shared biological causes. However, he observes that there is a certain arbitrariness to the seeming fixation of neo‐Kraepelinians on biological explanation: “In principle, there is no reason why this approach cannot be applied to the search for psychogenic causation in early childhood experience, or to family interaction, or to communication defects, or to social deprivation. There is no reason why this approach cannot be used for the study of non‐biological treatments such as individual or group psychotherapy or milieu therapy. It is an interesting observation in the history of psychiatry that those investigators who have attempted to apply these procedures most vigorously have had a biological bias… and an interest in biological treatments… Very few of the neo‐Kraepelinians are willing to give other than lip service to developmental causation. They are just vitriolic about it… Very few… are personally interested in, or willing to entertain, on principle, a developmental or psychogenic causation to the major psychoses” 15 , pp.115,117.
Why mental disorders need not be brain disorders
Surely, some of the more severe mental disorders are likely due to biologically describable dysfunctions. Nonetheless, Guze's biologicalism is, as Spitzer chided, an article of faith, and it remains so even today. For example, despite the fact that there is not one clearly established consensus on brain pathophysiology for a major mental disorder, N. Andreasen asserts that “people who suffer from mental illness suffer from a sick or broken brain” 103 , p.8 and Nobel Prize winner E. Kandel argues: “All mental processes are brain processes, and therefore all disorders of mental functioning are biological diseases… The brain is the organ of the mind. Where else could [mental illness] be if not in the brain?” 104 . One finds naïve assertions such as the following one occurring in scientific journals: “We confirm, with high‐powered analysis, that patients with ADHD have altered brains; therefore ADHD is a disorder of the brain” 105 , p.311.
Of course, the latter inference that brain differences mean mental disorder is spurious; brain differences occur in normal conditions as well 106 . As to Kandel's “locational” argument that psychological meanings occur “in the brain”, thus mental disorders must be brain diseases, the problem is that there is an equivocation in moving from the correct premise that all mental disorders are brain diseases in the locational sense to the conclusion that all mental disorders are brain diseases in the narrower sense that the underlying dysfunction is describable sheerly in anatomical/physiological terms. The invalidity of “all mental disorders are located in the brain, therefore all mental disorders are brain diseases” is suggested by the manifest invalidity of the analogous argument: all computer software runs in computer hardware, therefore all software malfunctions must be hardware malfunctions 107 .
It seems entirely possible for a mental disorder to be caused by problematic meanings that cause a psychological dysfunction without causing a brain dysfunction. It might be, as in Janoff‐Bulman's theory 108 , that certain meanings are so central that we are not biologically designed to process them in the rare event that they are seriously challenged, so there is a breakdown in psychological processing capabilities. This notion is reflected in the characterization of post‐traumatic stress disorder in the DSM‐III as requiring that “the person has experienced an event that is outside the range of usual human experience” 1 , p.250. The mix of successful psychotherapeutic and psychopharmacological treatments we have today argues against a narrow biologicalist thesis and suggests that Klerman was right to be skeptical of neo‐Kraepelinian biologicalist ideology.
Spitzer's rejection of neo‐Kraepelinian biologicalism
The second of Klerman's propositions that Spitzer rejected in his reply to Blashfield was proposition 6. Spitzer rather bluntly rejected the claim that psychiatry, to be a part of medicine, must be distinctively and primarily about biological etiology as opposed to being about whatever is empirically established to be causing mental disorders: “Article six states: ‘The focus of psychiatric physicians should be particularly on the biological aspects of mental illness.’ Nonsense. Psychiatrists should concern themselves with all aspects of mental illness, including the psychological and social aspects” 101 , p.592.
Spitzer completed his disengagement from neo‐Kraepelinianism by tartly suggesting that, in taking an open‐minded empirical approach, he had joined a different college with a credo much simpler than Klerman's: “I hope that my resignation from the neo‐Kraepelinian college will be accepted, as I have already joined the faculty of a much larger institution of higher learning. The faculty of this university is multidisciplinary and its credo is simple and easy to remember: it is ‘data oriented’… Faculty and students of this university are harmoniously committed to the pursuit of data that will help us understand the multiple determinants of mental illness and the relative effectiveness of various biological, psychological, and social treatments” 101 , p.592.
The same year, in a paper with J. Williams, Spitzer reiterated the DSM‐III's etiological neutrality and potential eclecticism: “DSM‐III makes no assumption that a biological abnormality accounts for each of the mental disorders. There is only one class of mental disorders for which a specific biological etiology is established, the Organic Mental Disorders. In some of the other categories, such as the psychotic disorders and the severe forms of Affective Disorder, a biological abnormality is assumed by many, although not included in the DSM‐III description. It is also widely assumed that whatever biological abnormality may eventually be discovered for these disorders, it is only one component of a multifactorial etiology that almost certainly involves environmental and psychological factors” 109 , p.23.
Spitzer's understanding emerged explicitly in his DSM‐III definition of mental disorder, which specifies that “there is an inference that there is a behavioral, psychological, or biological dysfunction” 44 , p.6 – a direct rejection of the narrower biological‐etiological vision of his neo‐Kraepelinian partners. He made the point even more abundantly clear in his explanation of DSM‐III's revolutionary descriptive diagnostic system. Even though the system was derived from the work of the neo‐Kraepelinians, Spitzer interpreted it differently. As Klerman had observed, the logic of the system was entirely theory‐neutral and therefore was not inherently biological, psychological, behavioral, and so on. It was a level playing field of operationally identified consensus disordered conditions about which the various approaches and theories – including biological theories – could now compete over etiology and treatment efficacy.
Spitzer went so far as to emphasize how competing theories were encompassed by the syndromal approach: “For most of the DSM‐III disorders… the etiology is unknown. A variety of theories have been advanced, buttressed by evidence – not always convincing – to explain how these disorders come about. The approach taken in DSM‐III is atheoretical with regard to etiology or pathophysiological process except for those disorders for which this is well established and therefore included in the definition of the disorder. Undoubtedly, with time, some of the disorders of unknown etiology will be found to have specific biological etiologies, others to have specific psychological causes, and still others to result mainly from a particular interplay of psychological, social and biological factors. The major justification for the generally atheoretical approach taken in DSM‐III with regard to etiology is that the inclusion of etiological theories would be an obstacle to use of the manual by clinicians of varying theoretical orientations… Clinicians can agree on the identification of mental disorders on the basis of their clinical manifestations without agreeing on how the disturbances come about” 44 , pp.6‐7. The DSM system can be interpreted as neo‐Kraepelinian in the strict bioetiological sense if one so wishes. But, that is not inherent in the structure of the manual or in the intentions of its primary creator, R. Spitzer.
There may be a concern that allowing psychogenic dysfunctions into the medical domain creates a fuzzy line between psychiatry and clinical psychology and opens the way to jurisdictional threats from non‐physicians. Fortunately, Guze and the neo‐Kraepelinians recognized that this is a dispute that need not be decided for now. Despite claiming mental disorders for the medical field in a conceptual sense, the neo‐Kraepelinians did not claim that their arguments delegitimized treatment of mental disorder by other mental health professions, such as psychologists and social workers, given their skills in some areas of psychotherapy.
“Disease” versus “disorder”
The difference between standard neo‐Kraepelinians and Spitzer also emerges in a much‐discussed matter of terminology. Neo‐Kraepelinians, we have seen, preferred the term “disease” because of its manifest biological‐disorder implications. Contrary to a common impression, the use instead of the generic term “disorder” for mental pathological conditions did not start with the DSM but rather has a long history. “Disease” is sometimes used for all medical problems, but its dominant use is to refer to a subcategory including infectious, genetic, and some other biologically based conditions, and so tends to exclude, for example, injuries, poisonings, and other genuine medical conditions 110 . To avoid ambiguities or premature etiological assumptions, “disorder” has long been the generic term of choice for mental and physical pathology. It was already in use in S. Johnson's Dictionary published in 1755, which includes entries in which, for example, “megrim” (migraine) is “a painful disorder of the head” and the “hypochondriack” is “disordered in the imagination” 111 .
Psychiatry has long used “disorder” in this way. For example, in the second issue, October 1844, of the American Journal of Insanity (later the American Journal of Psychiatry), the editor, A. Brigham, published an essay on The Definition of Insanity that begins: “By Insanity is generally understood some disorder of the faculties of the mind” 112 , p.97. The bibliography notes that H. Johnson recently published a book titled On the Arrangement and Nomenclature of Mental Disorders 113 . DSM merely adopted this long‐standard usage.
However, there is more to the continued use of “disorder” versus “disease” in DSM‐III than mere tradition. Spitzer early expressed preference for this term specifically because it allows a slimmed‐down understanding of “medical model” that rejects the ideologically loaded neo‐Kraepelinian notion that requires all psychiatric conditions to be biological brain diseases. According to Spitzer and Wilson, in a 1975 handbook entry, the use of “disorder” rather than “disease” is a disavowal of the neo‐Kraepelinian demand for biological etiology and treatment: “This conception of the medical model makes no a priori assumptions as to what etiological factors – physical, social, genetic, psychological, developmental – are responsible for the development of these conditions nor what kind of treatment – somatic, psychological, social, behavioral – will be most effective… However, since the word ‘disease’ usually does connote manifest physical dysfunction, the appropriate generic term for a psychiatric illness is ‘mental disorder’” 114 , p.827.
Because disorder attribution implies an inferred dysfunction, whether its nature is known or not, it is a confusion to think that disorder represents a non‐theoretical “nominalist view of mental illness” 115 , p.386 or that “the explicitly vague term ‘disorder’ reflects post‐modernist cynicism about the disease concept” 65 , p.36. Disorders are not merely syndromes, they are syndromes caused by dysfunctions.
RDoC as an alternative neo‐Kraepelinian strategy
With the rise of biological psychiatry as the dominant force in American psychiatry, there has been a transfer of power in departments of psychiatry from psychoanalysts to biologicalists. In reflecting further on where we stand with regard to proposition 6, I first comment briefly on RDoC and then turn to the broader picture.
RDoC is a major research initiative by the US NIMH that primarily focuses on brain circuitry activation patterns as dimensional variables linked to fundamental psychological functions2, 3, 4, 5. The circuits’ functions and dysfunctions need not correspond in any simple way to DSM‐ICD categories, allowing for new insights unconstrained by DSM‐ICD syndromal formulations. Rather than starting from syndromally defined disorders with implicit assumptions about normality in the background, RDoC starts from the identification of psychological adaptive systems that are presumably naturally selected and anchored in neural circuitry but subject to disruption, such as response to threat or loss, motivation to approach or avoid, reward responsiveness, attentional and memory systems, dominance/submission, theory of mind, appetitive systems, and other arousal, consummatory and regulating systems. After identifying brain circuitry that supports biologically designed behavior and studying the range of activation of such circuits, RDoC hopes to identify psychopathological outcomes of excessive or defective activation.
The RDoC initiative is well‐timed and potentially highly fruitful due to a raft of new methods and technologies for brain research. Because of its focus on brain‐level variables rather than standard DSM‐ICD categories or psychological‐level variables, RDoC has been controversial in the psychological and psychiatric community. However, any attempt to better understand the brain‐physiological underpinnings of psychological functioning and psychopathology is desirable from both a scientific and clinical perspective, especially given recent failures to make substantial progress in etiological research.
RDoC is generally seen, and initially was presented by its creators, as a potential replacement for the DSM‐ICD system, with dimensional brain‐circuitry activation measures supplanting DSM‐ICD syndromal categories. However, RDoC is best understood as a continuation of the neo‐Kraepelinian program, with a change of tactics rather than a basic change of overall conception. The neo‐Kraepelinian vision was to start with categories of disorders based on observable symptom syndromes that prima facie indicated failures of biologically designed functioning, then to work conceptually and empirically to eliminate false positives and create conceptually valid categories of disorder, and finally to work to refine the categories into more etiologically homogeneous construct‐valid categories for which biological etiologies could be identified, and to use the discovered biological etiologies to refine the syndromal categories. The biological step of this syndrome‐to‐etiology process has been largely unsuccessful thus far. RDoC is a push to revive the neo‐Kraepelinian vision by moving directly to the search for biological dysfunctions. Given that the relationship between symptoms and etiologies appears to be much more complicated than anticipated 116 , RDoC abandons the attempt to work from syndromes to bio‐etiologies and instead attempts to start directly at the brain level. The goal is not to redefine the current DSM‐ICD categories according to identified alterations in the functioning of brain circuitry, but rather to reorganize classification and diagnosis around novel brain‐level constructs.
RDoC thus can be understood as a realization of the neo‐Kraepelinian dream of identifying brain‐physiological etiologies, but approached by a different route than the syndrome refinement pathway. The neo‐Kraepelinian system did not require the initial syndromal categories to remain fixed once etiologies are discovered and linked to clinical presentations; Kraepelin himself maintained flexibility about the proper syndromal organization as his etiological theories changed. Shifting to the brain level when the syndromal level presents seemingly intractable obstacles is entirely consistent with the neo‐Kraepelinian vision. In the harmful dysfunction analysis's terms, RDoC investigates function and dysfunction without initial focus on harm.
However, there are several caveats to this neo‐Kraepelinian perspective on RDoC 117 . First, a fundamental problem with RDoC is its commitment to biological‐level etiologies and downplaying of psychological‐level dysfunctions. RDoC would benefit from more Spitzerian open‐mindedness; some dysfunctions at the psychological level may not be reflected in circuitry dysfunction.
Second, RDoC lacks any explicit evolutionary perspective that would provide a context for understanding which circuit activations are functional versus dysfunctional. Syndromal features often support prima facie judgments of failure of biological design, but brain circuit activations in themselves tell one little about which types and domains of circuit activation are normal and which disordered. For example, certain circuitry activations in the male rat brain cause aggression toward an interloping male, overlapping activations inhibit those aggressive behaviors and cause mating approaches to an interloping receptive female, and intensive activation of an overlapping region causes aggression against males and receptive females 118 . Circuitry activation in itself does not tell you that two of these are normal‐range processes whereas the third is a potential disorder; for that, you need to know something about normal evolved functioning.
Third, RDoC is committed to a dimensional analysis of circuit activation across the entire normal and disordered range. The whole‐population dimensional approach is valuable for the advance of knowledge of normality and disorder, and is appealing as a systematic way to approach each domain and gain a perspicuous understanding. However, this approach also presents potential obstacles to the understanding of disorder in a medical sense. Dimensions provide no non‐arbitrary thresholds for disorder and thus place medical legitimacy in question. The often‐stated idea that extremes on dimensions define disorder is conceptually vacuous: must it be in the top 50% or the top 1%? Adding impairment is not a solution: normal grief, normal pregnancy, and, for that matter, normal sleep are impairing. Moreover, deleterious genotypes or endophenotypes may not be at the extreme of a dimension but just a happenstance pathogenic combination. Focus on disorder as the extreme on dimensions can distract from the search for underlying discontinuities such as deleterious mutations explaining all or part of a distribution's extreme, as has been found in several mental disorder categories (see below), as well as among some physical disorder categories119, 120.
Finally and most fundamentally, RDoC appears to assume that clinically relevant brain‐physiological etiological analyses can proceed without any reference to symptom syndromes. However, symptoms provide the harms that make dysfunctions into mental disorders rather than mere anomalies. It is not possible to illuminatingly explore the etiology of disorder while being blind to symptoms, because etiologies do not have their pathogenicity written on their sleeves. Even most infectious diseases, from the common cold to tuberculosis and polio, actually cause disease in only some of those who are infected. Understanding of disorder comes from studying the etiological level and symptom level simultaneously; neither alone provides the basis for judging harmful dysfunction.
The current pessimism about neo‐Kraepelinian biologicalist aspirations
Despite massive amounts of biologicalist research filling our late‐neo‐Kraepelinian‐era journals, there is not one clear discovery of a biological etiology for a major mental disorder. Modern efforts have focused on genetic determinants, but attempts to identify relatively straightforward genetic etiologies have failed, and it appears that highly polygenic solutions with many genes of small effect are generally the best we can find for disease risk. A mood of pessimism has set in, prompting philosophical rumination about whether our goals made sense to begin with 121 . Skeptics argue that we were misled by early discoveries of biological etiologies of general paresis and pellagra and that we need to find a different path. One might be tempted to respond that it has been only a few decades since the neo‐Kraepelinian revolution occurred, that science rarely goes in a straight line, and that patience is a virtue in a science dealing with complexities at the level of the etiology of mental disorder. Fortunately, there is a more constructive response to biologicalist pessimism.
We stand today in an excellent position to advance our understanding of biological causes of mental disorder due to the development of novel technologies and data analytic techniques. In particular, it has only recently become possible to perform genetic analyses that allow us to infer the history of natural selection of specific genes and gene combinations without the need for a time machine, and genome‐wide genetic risk analyses have become routine. Genetic analysis can provide an alternative to the current enthusiasm for dimensionalization, as the following examples illustrate.
Intellectual disability
Klerman, defending the possibility that statistical analysis of syndromes could eventually reveal etiologically homogeneous subtypes, pointed to successes in identifying genetic determinants of intellectual disability that caused individuals to fall in the extreme lower area of the IQ distribution: “The logic of the partialing out syndromes has been successful, for example, in mental retardation” 15,p.119 .
Since then, genetic analysis has enormously refined our understanding of IQ and intellectual disability. There is a roughly smooth normal distribution of intelligence in the population that is polygenically determined in a way that accounts for the upper reaches, although the nature of extreme genius remains disputed 122 . The extreme low end of the distribution, on the other hand, appears to consist of two components. The larger group, accounting for most of intellectually disabled people, represents the extreme lower end of the same polygenic distribution. The remaining smaller group consists of conditions caused by many different genetic mutations that are qualitatively distinct from the genes that are responsible for the normal distribution of intelligence in the population 123 .
Premenstrual dysphoric disorder
Premenstrual dysphoric disorder (PMDD) is a depressive condition occurring primarily during the days just prior to menstruation, in the late luteal phase of the cycle. In many ways, it is an extreme form of the premenstrual syndrome (PMS) that afflicts the vast majority of women in varying degrees. However, in a small percentage of women, the emotional symptoms of sadness, irritability and anxious tension, as well as physical symptoms, are so severe as to interfere with basic functioning, disrupt relationships, and block the performance of usual social roles.
Long proposed as a category of mood disorder, several concerns led to resistance to its being included among DSM categories 124 . The distribution of premenstrual symptom severity is dimensional without obvious discontinuities, so there was a validity concern that any threshold was arbitrary and would pathologize the extreme of normal variation. Skepticism about there being a dysfunction underlying PMDD was supported by studies disconfirming the standard theory that women with PMDD experienced abnormally high levels of menstruation‐related hormones. Moreover, the dimensionality of PMS/PMDD meant that classification of PMDD as a disorder could easily lead to pathologization of milder PMS, perhaps reinforcing traditional stereotypes that emotional variations associated with the menstrual cycle rendered women unsuitable to certain responsibilities. Due to these controversies, PMDD was not a stand‐alone category of disorder, but instead listed under DSM‐IV's Appendix B of “Criteria sets provided for further study”, when the revision leading to DSM‐5 began.
PMDD was finally made a full criterial category of depressive disorder in DSM‐5 after a panel of experts concluded that there was sufficient empirical evidence to support such a move125, 126. The evidence that justified the DSM‐5 change of PMDD to full disorder status was not evidence of severity, because that was already established by definition. Rather, evidence emerged that the severity was caused by a dysfunction, so that the extreme on the PMS dimension constituted a discontinuous and distinct condition. In ovarian steroid suppression and addback studies, women reporting PMDD and a control group were administered agonists that rid the bloodstream of circulating hormone, then gradually added back hormone into the bloodstream, simulating changing hormone levels during the menstrual cycle127, 128. The result was that women with PMDD histories displayed pronounced behavioral and brain over‐reactivity to hormone fluctuation, whereas other women did not. So, women with PMDD did not have different hormone levels, but rather different reactions to changing hormone levels. Researchers then established that the greater reactivity was due to specific genetic variations that led to overexpression of some cellular responses and underexpression of others 129 . These findings were replicated in animal models of PMDD 130 . This research revealed an underlying dysfunction of genetic response to hormone fluctuation that supports the idea that PMDD is a categorical disorder.
Autism spectrum disorder
A recent study of the genetics of autism spectrum disorder (ASD) 131 found that individual risk genes for autism are associated with cognitive advantages, and linkage studies indicate that each of these genes was individually positively selected: “Using genome‐wide data, we observed that common alleles associated with increased risk for ASD present a signature of positive selection. ASD risk alleles could positively affect these [cognitive] mechanisms, causing better cognitive ability in carriers as a consequence”. However, for reasons as yet unknown, certain polygenic combinations to the contrary yielded autism: “an excessive burden of these risk variants is correlated with the onset of the developmental disorders included in the autism spectrum as the evolutionary cost”. Thus, “according to our interpretation of our data, such small‐effect alleles were accumulated across the genome (polygenic adaptation) to the benefit of most but to the detriment of some” 131 , pp.4,8,9.
This work illustrates the important point that the dimensionalist's hope that disorder can be identified as an extreme on a dimension has no basis in genetic theory. Although extremes on etiological variables may correlate with disorder, in principle seemingly arbitrary confluences of otherwise benign etiological variables can yield pathology. Dysfunction‐causing combinations of what are individually positive traits may occur at non‐genetic levels as well. For example, there can be several personality traits that are individually advantageous but, when they occur together and interact in a certain way, create a personality disorder.
ADHD
The Centers for Disease Control and Prevention report that about one in five high school boys in the US have been diagnosed with ADHD, with most taking stimulant medication 132 . Multiple lines of evidence suggest that such rates are inflated by substantial false‐positive diagnoses. For example, of children in a given school grade, the youngest have much higher rates of ADHD diagnosis133, 134, 135, suggesting that normal variation in developmental rate is being misdiagnosed as disorder. Consistent with this interpretation, the majority of children with ADHD exit from the diagnosis as they get older136, 137, 138, 139, 140. This has suggested a “brain maturation developmental delay” hypothesis to explain ADHD, a theory that is ambiguous between disorder and misdiagnoses due to normal variation in developmental rate occurring in a school environment which demands behavior that slower‐developing children are not ready to provide.
Critics of the DSM‐ICD criteria for ADHD commonly argue that normal‐range children who are naturally more active than others are misdiagnosed with ADHD due to constrained school environments. The results of a multifaceted research program supports this possibility. It concerns the “seven repeat” polymorphism of the DRD4 gene, DRD4‐7R, which codes for aspects of the structure of the brain's dopamine receptors. This variation is considerably more common in ADHD‐diagnosed children than in other children141, 142, 143, 144. DRD4‐7R slows uptake and metabolism of dopamine, thus decreasing experience of reward and heightening response to negative stimuli145, 146, 147, 148. ADHD in this group can thus be seen as inattention and impulsive activity due to lessened reward and consequent boredom when sedentary, and the search for novel sources of reward. This fits with the fact that stimulants used to successfully treat ADHD enhance dopamine metabolism.
Rather than these discoveries implying that DRD4‐7R‐related ADHD is a genetic disorder, research indicates just the opposite. The occurrences of 7R variants of DRD4 in the general population are too common to be random mutations, and there is strong evidence that 7R was naturally selected149, 150. The 7R polymorphism is also associated with personality traits of sensation‐seeking and novelty‐seeking which are plausibly adaptive 151 . The gene has higher incidence in populations that resulted from geographic dispersal, is associated with risk‐taking, and appears to yield a longevity benefit as well152, 153.
This polymorphism seems to adaptively increase exploration and activity, by creating the need for more intense dopamine responses that come with novel stimuli. However, in an environment such as a modern school system that demands long periods of focused and sedentary behavior, the same gene is problematic. Rather than revealing a genetic disorder, the research on DRD4‐7R has revealed a likely naturally selected normal variation in dopamine metabolism that is being treated as a disorder due to the demands of our society. Some ADHD individuals are not disordered but have natures mismatched to the demands we make on them.
Spitzerian open‐mindedness about the nature of dysfunctions and their etiologies is certainly more plausible and appealing than the fervent neo‐Kraepelinian biologicalism expressed in Klerman's proposition 6. Yet, any pessimism about the power of biological discovery to help us to understand the etiological terrain, and even to help to better define the boundary between normal variation and disorder, is premature.
7. THERE SHOULD BE AN EXPLICIT AND INTENTIONAL CONCERN WITH DIAGNOSIS AND CLASSIFICATION
This proposition appears to be primarily intended as a rebuke to psychoanalysis. The oft‐repeated neo‐Kraepelinian narrative was that diagnosis became irrelevant in psychoanalytically‐dominated American psychiatry. This issue played a role in the run‐up to the DSM‐III. Despite repeated overtures to the psychoanalytic community to contribute to the DSM‐III, Spitzer refused to build into the nosology the unscientific assumption that a single Oedipal etiology existed for disparate conditions, and so he eliminated neuroses as a formal category 39 .
Proposition 7 was particularly persuasive in the wake of progress in psychopharmacology. For example, some medications worked for panic disorder but not as well for generalized anxiety disorder. This suggested that the medications might be working to correct dysfunctional mechanisms specific to the etiology of the particular disorder. However, most of these medication results have weakened over time.
During the subsequent decades, neo‐Kraepelinianism has transformed psychiatry exactly as envisioned by proposition 7. Moreover, if taken in a broad sense, even the challenges to various aspects of neo‐Kraepelinianism do not necessarily alter this perception. The dimensionalist and RDoC challenges are born of a continued concern for diagnosis but dissatisfaction with the current system.
8. DIAGNOSTIC CRITERIA SHOULD BE CODIFIED, AND A LEGITIMATE AND VALUED AREA OF RESEARCH SHOULD BE TO VALIDATE SUCH CRITERIA BY VARIOUS TECHNIQUES. FURTHER, DEPARTMENTS OF PSYCHIATRY IN MEDICAL SCHOOLS SHOULD TEACH THESE CRITERIA AND NOT DEPRECIATE THEM, AS HAS BEEN THE CASE FOR MANY YEARS
Proposition 8 fires a broadside against the psychoanalytic domination of psychiatric education. As to codification, once psychiatry possessed a formal, complex diagnostic system that was the basis for everything, from insurance reimbursement to research sample selection, codification inevitably followed.
9. IN RESEARCH EFFORTS DIRECTED AT IMPROVING THE RELIABILITY AND VALIDITY OF DIAGNOSIS AND CLASSIFICATION, STATISTICAL TECHNIQUES SHOULD BE UTILIZED
The advisability of using statistical analysis to improve reliability and validity of diagnostic criteria is indisputable and has become routine. Reliability has been improved under the DSM system, although the magnitude of the improvement remains controversial 154 .
The neo‐Kraepelinians, including Klerman, explicitly envisioned epidemiology as providing the primary statistical basis for improving the identification and validation of true medical psychiatric conditions and separating conditions with divergent etiologies. For reasons presented earlier, it is arguable that thus far epidemiology has failed in this quest for true prevalence of disorders due to massive overinflation of prevalence rates by false positives.
CONCLUSIONS
The DSM‐ICD nosological system has many problems, and I have spent a good deal of scholarly and research effort pointing some of them out. However, a close look at the neo‐Kraepelinian movement and especially its Spitzerian realization, out of which the DSM‐III was born, reveals the complexity of the aspirations behind the manual that must be taken into account in its assessment. The DSM‐III emerged in an attempt to defeat a threat to the legitimacy of psychiatry. This discipline deals with sensitive areas of human relationships, and it will always be in danger of being seen as social control rather than medicine, as the recent neurodiversity movement reminds us. It would be easy to forget those challenges, but to do so would be a mistake. I argued that some proposed changes to our nosology, especially stronger forms of dimensionalization, do not appear to understand or address this fundamental issue. A sliding scale in clinical practice is a good thing, but an arbitrarily sliding threshold between disorder and non‐disorder on an all‐encompassing set of dimensions of population distributions of a variety of traits is potentially a frightening prospect sure to reawaken public worries about the legitimacy of psychiatry.
Many standard views of the DSM‐ICD system are based on misimpressions that do not correspond to the system as Spitzer conceived it. For example, the diagnostic categories are not assumed to be discrete entities with zones of symptom rarity between them; etiology is not exiled forever from the manual's criteria but only excluded until the science reaches a consensus view; and the categories are not final and written in stone but instead represent provisional groups of disorders that may need to be eventually separated, and are expected to change over time to achieve greater conceptual and construct validity 155 .
As a general nosological doctrine expressed in the nine propositions of Klerman's credo, neo‐Kraepelinianism has three aspects. First, it makes the conceptual claim that psychiatry as its core mission treats genuine mental disorders in the medical sense, that are distinct from normal deviance, stress reactions and problems in living, because they are caused by dysfunctions. Second, it lays out a theoretical agenda that the many different biologically designed psychological capacities that humans possess imply the likelihood that there are many different ways through which psychological functioning can go wrong, even if they share upstream risk factors. Finally, it lays out a methodological program based on the assumption that the best way to achieve understanding of mental disorders is through scientific research starting with clinical syndromes that are conceptually face‐valid as disorders. Then, through the use of epidemiology, statistical analysis, and other data‐based scientific investigations, the goal is to gradually improve and revise diagnostic criteria so as to yield refined categories that are etiologically increasingly homogeneous and thus support even more productive research. In this bootstrapping process, initial syndromes transform by addition and subtraction into more construct valid etiologically understood diagnostic categories.
It is apparent that the neo‐Kraepelinian methodological bootstrapping vision has not been working, or at least not working as rapidly as desired. I argued that this is partly because, in uniting research and clinical diagnostic criteria, the envisioned process was undermined. Like most well‐intentioned actions, this one had unexpected side effects. The expectation, I think, was that researchers would gain their insights on the mountain of science and come down unto the clinicians and put forth the scientific law. It has not worked that way. The many truly bewildering decisions that afflicted the DSM‐5 revision process, especially in failing to address false positives57, 60, 156, 157, have made neo‐Kraepelinian bootstrapping much more difficult. The false positives problem loomed large because, once clinical intervention and research moved from the asylum to the community, aggressive steps were needed but not undertaken to control false positives, and bootstrapping to homogeneous dysfunction etiologies was undermined.
I also argued that the Spitzerian version of neo‐Kraepelinianism is correct on two points of divergence. First, biological research has much to offer, but strict biologicalism about etiology cannot be taken a priori as the only ultimate form of etiology. Second, the degree of discreteness versus continuity of both symptom and latent factor distributions cannot be judged ahead of time, because that is an empirical issue. Until etiologies are understood, the syndrome‐to‐etiology bootstrapping scheme is founded on intuitions that something has gone wrong with the way people are supposed to function. This is how it was in physical medicine, but there was clearer separation of biological design versus social demands. Even so, the bootstrapping process took millennia for many disorders, and for many others we are not there yet.
Nonetheless, pessimism is not warranted. We have remarkable new technologies at our disposal that are already yielding deep insights. Although etiologies are an elusive quarry, this is what science is designed to do and what it does well – namely, it formulates competing theories about a domain and then formulates tests, the outcomes of which add evidential weight and explanatory power to one competing theory over another. True, “dysfunction” is still a broad and vague notion referring to a largely unknown domain. But, this is how science works. It starts with terms that allude to types of processes defined with minimal specified features, and then it gradually fills in the picture. For example, despite developing a radically different understanding of circulation than Galen, Harvey more or less agreed with Galen on the point that the lungs must add some “spirit” to the blood and eject some “soot”. It took millennia to figure out that, roughly speaking, the added spirit is oxygen and the soot is carbon dioxide. The clever use of a variety of research strategies will hopefully allow psychiatry to go a bit faster than that.
REFERENCES
- 1. American Psychiatric Association . Diagnostic and statistical manual of mental disorders, 3rd ed. Washington: American Psychiatric Association, 1980. [Google Scholar]
- 2. Insel TR, Cuthbert B, Garvey M et al. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 2010;167:748‐51. [DOI] [PubMed] [Google Scholar]
- 3. Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry 2014;13:28‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lilienfeld SO, Treadway MT. Clashing diagnostic approaches: DSM‐ICD versus RDoC. Annu Rev Clin Psychol 2016;12:435‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clark LA, Cuthbert B, Lewis‐Fernández R et al. Three approaches to understanding and classifying mental disorder: ICD‐11, DSM‐5, and the National Institute of Mental Health's Research Domain Criteria (RDoC). Psychol Sci Public Interest 2017;18:72‐145. [DOI] [PubMed] [Google Scholar]
- 6. Kotov R, Krueger RF, Watson D et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol 2017;126:454‐77. [DOI] [PubMed] [Google Scholar]
- 7. Kotov R, Jonas KG, Carpenter WT et al. Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): I. Psychosis superspectrum. World Psychiatry 2020;19:151‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krueger RF, Hobbs KA, Conway CC et al. Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): II. Externalizing superspectrum. World Psychiatry 2021;20:171‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ruggero CJ, Kotov R, Hopwood CJ et al. Integrating the Hierarchical Taxonomy of Psychopathology (HiTOP) into clinical practice. J Consult Clin Psychol 2019;87:1069‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Borsboom D. A network theory of mental disorders. World Psychiatry 2017;16:5‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol 2013;9:91‐121. [DOI] [PubMed] [Google Scholar]
- 12. Borsboom D, Cramer AOJ, Kalis A. Brain disorders? Not really: why network structures block reductionism in psychopathology research. Behav Brain Sci 2019;42:1‐63. [DOI] [PubMed] [Google Scholar]
- 13. McNally RJ. Network analysis of psychopathology: controversies and challenges. Annu Rev Clin Psychol 2021;17:31‐53. [DOI] [PubMed] [Google Scholar]
- 14. Kendler KS. Levels of explanation in psychiatric and substance use disorders: implications for the development of etiologically based nosology. Mol Psychiatry 2012;17:11‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Klerman GL. The evolution of a psychiatric nosology. In: Shershow JC (ed). Schizophrenia: science and practice. Cambridge: Harvard University Press, 1978:99‐121. [Google Scholar]
- 16. Guze SB. Nature of psychiatric illness: why psychiatry is a branch of medicine. Compr Psychiatry 1978;19:295‐307. [DOI] [PubMed] [Google Scholar]
- 17. Guze SB. Biological psychiatry: is there any other kind? Psychol Med 1989;19:315‐23. [DOI] [PubMed] [Google Scholar]
- 18. Guze SB. Why psychiatry is a branch of medicine. New York: Oxford University Press, 1992. [Google Scholar]
- 19. Spitzer RL, Endicott J. Medical and mental disorder: proposed definition and criteria. In: Spitzer RL, Klein DF (eds). Critical issues in psychiatric diagnosis. New York: Raven Press, 1978:15‐39. [Google Scholar]
- 20. Klerman GL, Weissman MM, Roundaville BJ et al. Interpersonal psychotherapy of depression. New York: Basic Books, 1984. [Google Scholar]
- 21. Foucault M. Madness and civilization: a history of insanity in the Age of Reason. New York: Pantheon, 1965. [Google Scholar]
- 22. Laing RD. The politics of experience. London: Penguin Books, 1967. [Google Scholar]
- 23. Rosenhan D. On being sane in insane places. Science 1973;179:250‐8. [DOI] [PubMed] [Google Scholar]
- 24. Sarbin T. On the futility of the proposition that some people be labeled “mentally ill”. J Consult Psychol 1967;31:447‐53. [DOI] [PubMed] [Google Scholar]
- 25. Scheff TJ. Being mentally ill: a sociological theory. Chicago: Aldine, 1966. [Google Scholar]
- 26. Scheff TJ. Labeling madness. Englewood Cliffs: Prentice Hall, 1975. [Google Scholar]
- 27. Szasz TS. The myth of mental illness: foundations of a theory of personal conduct. New York: Hoeber‐Harper, 1961. [Google Scholar]
- 28. Ullman LP, Krasner L. A psychological approach to abnormal behavior. Englewood Cliffs: Prentice‐Hall, 1975. [Google Scholar]
- 29. Engel G L. Is grief a disease?: A challenge for medical research. Psychosom Med 1961;23:18‐22. [DOI] [PubMed] [Google Scholar]
- 30. Professional Staff of the United States‐United Kingdom Cross‐National Project. The diagnosis and psychopathology of schizophrenia in New York and London. Schizophr Bull 1974;1:80‐102. [DOI] [PubMed] [Google Scholar]
- 31. Strauss JS, Carpenter WT, Bartko JJ. The diagnosis and understanding of schizophrenia: summary and conclusions. Schizophr Bull 1974;1:70‐80. [PubMed] [Google Scholar]
- 32. Brown BS. The life of psychiatry. Am J Psychiatry 1976;133:489‐95. [DOI] [PubMed] [Google Scholar]
- 33. Shorter E. The history of nosology and the rise of the Diagnostic and Statistical Manual of Mental Disorders. Dialogues Clin Neurosci 2015;17:59‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Grob GN. From asylum to community: mental health policy in modern America. Princeton: Princeton University Press, 2014. [Google Scholar]
- 35. Bowlby J. The nature of the child's tie to his mother. Int J Psychoanal 1958;39:350‐73. [PubMed] [Google Scholar]
- 36. Feighner Blashfield RK. et al., invisible colleges, and the Matthew effect. Schizophr Bull 1982;8:1‐6. [DOI] [PubMed] [Google Scholar]
- 37. Spitzer RL, Endicott J, Robins E. Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry 1978;34:773‐82. [DOI] [PubMed] [Google Scholar]
- 38. Feighner JP, Robins E, Guze SB et al. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972;26:57‐63. [DOI] [PubMed] [Google Scholar]
- 39. Decker HS. The making of DSM‐III: a diagnostic manual's conquest of American psychiatry. New York: Oxford, 2013. [Google Scholar]
- 40. Klerman G, Schechter G. Ethical aspects of drug treatment. In: Bloch S, Chodof P (eds). Psychiatric ethics. Oxford: Oxford University Press, 1981:117‐30. [Google Scholar]
- 41. Wakefield JC. Psychological justice: DSM‐5, false positive diagnosis, and fair equality of opportunity. Pub Affairs Q 2015;29:32‐75. [Google Scholar]
- 42. Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health. Mental health and human rights: setting a rights‐based global agenda. A/HRC/44/48. Geneva: Office of the United Nations High Commissioner for Human Rights, 2020. [Google Scholar]
- 43. Wakefield JC. From Ribot and Dupré to Spitzer and RDoC, does the harmful dysfunction analysis possess historical explanatory power? Reply to Steeves Demazeux. Defining mental disorder: Jerome Wakefield and his critics. Cambridge: MIT Press, 2021:27‐46.
- 44. Spitzer RL. Introduction. In: American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 3rd ed. Washington: American Psychiatric Association, 1980:1‐12. [Google Scholar]
- 45. World Health Organization . International classification of diseases, 11th revision. https://icd.who.int/en.
- 46. Wakefield JC. The concept of mental disorder: on the boundary between biological facts and social values. Am Psychol 1992;47:373‐88. [DOI] [PubMed] [Google Scholar]
- 47. Wakefield JC. Evolutionary versus prototype analyses of the concept of disorder. J Abnorm Psychol 1999;108:374‐99. [DOI] [PubMed] [Google Scholar]
- 48. Wakefield JC. Mental disorder as a black box essentialist concept. J Abnorm Psychol 1999;108:465‐72. [DOI] [PubMed] [Google Scholar]
- 49. Wakefield JC. Evolutionary history versus current causal role in the definition of disorder: reply to McNally. Behav Res Ther 2001;39:347‐66. [DOI] [PubMed] [Google Scholar]
- 50. Wakefield JC. The concept of mental disorder: diagnostic implications of the harmful dysfunction analysis. World Psychiatry 2007;6:149‐56. [PMC free article] [PubMed] [Google Scholar]
- 51. Wakefield JC. The concepts of biological function and dysfunction: toward a conceptual foundation for evolutionary psychopathology, 2nd ed. In: Buss D (ed). Handbook of evolutionary psychology. Oxford: Oxford University Press, 2016:988‐1006. [Google Scholar]
- 52. Wakefield JC. Darwin, functional explanation, and the philosophy of psychiatry. In: Andriaens PR, De Block A (eds). Maladapting minds: philosophy, psychiatry, and evolutionary theory. Oxford: Oxford University Press, 2011:143‐172. [Google Scholar]
- 53. Spitzer RL. Brief comments from a psychiatric nosologist weary from his own attempts to define mental disorder: why Ossorio's definition muddles and Wakefield's “harmful dysfunction” illuminates the issues. Clin Psychol 1997;4:259‐61. [Google Scholar]
- 54. Spitzer RL. Harmful dysfunction and the DSM definition of mental disorder. J Abnorm Psychol 1999;108:430‐2. [DOI] [PubMed] [Google Scholar]
- 55. Wakefield JC. DSM‐5 grief scorecard: assessment and outcomes of proposals to pathologize grief. World Psychiatry 2013;12:171‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wakefield JC, First MB. Validity of the bereavement exclusion to major depression: does the evidence support the proposed elimination of the exclusion in DSM‐5? World Psychiatry 2012;11:3‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wakefield JC. The DSM‐5 debate over the bereavement exclusion: psychiatric diagnosis and the future of empirically supported practice. Clin Psychol Rev 2013;33:825‐45. [DOI] [PubMed] [Google Scholar]
- 58. Wakefield JC. The day the horse fell down: rethinking Freud's argument for the Oedipus complex in the case of Little Hans. New York: Routledge, 2021. [Google Scholar]
- 59. Wakefield JC. Diagnostic issues and controversies in DSM‐5: return of the false positives problem. Annu Rev Clin Psychol 2016;12:105‐32. [DOI] [PubMed] [Google Scholar]
- 60. First MB, Wakefield JC. Diagnostic criteria as dysfunction indicators: bridging the chasm between the definition of mental disorder and diagnostic criteria for specific disorders. Can J Psychiatry 2013;58:663‐9. [DOI] [PubMed] [Google Scholar]
- 61. Wakefield JC, First MB. Placing symptoms in context: the role of contextual criteria in reducing false positives in DSM diagnosis. Compr Psychiatry 2012;53:130‐9. [DOI] [PubMed] [Google Scholar]
- 62. Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 1970;126:107‐11. [DOI] [PubMed] [Google Scholar]
- 63. Kendler KS, Jablensky A. Kraepelin's concept of psychiatric illness. Psychol Med 2011;41:1119‐26. [DOI] [PubMed] [Google Scholar]
- 64. Hyman SE. The diagnosis of mental disorders: the problem of reification. Annu Rev Clin Psychol 2010;6:155‐79. [DOI] [PubMed] [Google Scholar]
- 65. Ghaemi SN. Utility without validity is useless. World Psychiatry 2016;15:35‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Rounsaville BJ, Spitzer RL, Williams JB. Proposed changes in DSM‐III substance use disorders: description and rationale. Am J Psychiatry 1986;143:463‐8. [DOI] [PubMed] [Google Scholar]
- 67. Hasin DS, O'Brien CP, Auriacombe M et al. DSM‐5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry 2013;170:834‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Chesterton GK. What's wrong with the world. New York: Gassell, 1910. [Google Scholar]
- 69. Kraepelin E. Clinical psychiatry: a text‐book for students and physicians. New York: Macmillan, 1915. [Google Scholar]
- 70. Kraepelin E. Textbook of Psychiatry. Edinburgh: Livingstone, 1921. [Google Scholar]
- 71. Flatow I, Kessler R. Survey: Half of U.S. residents will suffer mental illness. NPR, June 10, 2005.
- 72. Sharfstein S. Prevalence, treatment data raise troubling questions. Psychiatr News 2006;41:3. [Google Scholar]
- 73. Regier DA, Kaelber CT, Rae DS et al. Limitations of diagnostic criteria and assessment instruments for mental disorders: implications for research and policy. Arch Gen Psychiatry 1998;55:109‐15. [DOI] [PubMed] [Google Scholar]
- 74. Moffitt TE, Caspi A, Taylor AW et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med 2010;40:899‐909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Rohde P, Lewinsohn PM, Klein DN et al. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clin Psychol Sci 2013;1:41‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Clayton P, Desmarais L, Winokur G. A study of normal bereavement. Am J Psychiatry 1968;125:168‐78. [DOI] [PubMed] [Google Scholar]
- 77. Cassidy WL, Flanagan NB, Spellman M et al. Clinical observations in manic‐depressive disease: a quantitative study of one hundred manic‐depressive patients and fifty medically sick controls. JAMA 1957;164:1535‐46. [DOI] [PubMed] [Google Scholar]
- 78. Stone TT, Burris BC. Melancholia: clinical study of 50 selected cases. JAMA 1950;142:165‐8. [DOI] [PubMed] [Google Scholar]
- 79. Mojtabai R. Bereavement‐related depressive episodes: characteristics, 3‐year course, and implications for DSM‐5. Arch Gen Psychiatry 2011;68:920‐8. [DOI] [PubMed] [Google Scholar]
- 80. Wakefield JC, Schmitz MF. When does depression become a disorder? Using recurrence rates to evaluate the validity of proposed changes in major depression diagnostic thresholds. World Psychiatry 2013;12:44‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Wakefield JC, Schmitz MF. Can the DSM's major depression bereavement exclusion be validly extended to other stressors?: Evidence from the NCS. Acta Psychiatr Scand 2013;128:294‐305. [DOI] [PubMed] [Google Scholar]
- 82. Wakefield JC, Schmitz MF. Normal vs. disordered bereavement‐related depression: are the differences real or tautological? Acta Psychiatr Scand 2013;127:159‐68. [DOI] [PubMed] [Google Scholar]
- 83. Wakefield JC, Schmitz MF, First MB et al. Should the bereavement exclusion for major depression be extended to other losses? Evidence from the National Comorbidity Survey. Arch Gen Psychiatry 2007;64:433‐40. [DOI] [PubMed] [Google Scholar]
- 84. Wakefield JC, Schmitz M. Predictive validation of single‐episode uncomplicated depression as a benign subtype of unipolar major depression. Acta Psychiatr Scand 2014;129:445‐57. [DOI] [PubMed] [Google Scholar]
- 85. Wakefield JC, Schmitz MF. Uncomplicated depression is normal sadness, not depressive disorder: further evidence from the NESARC. World Psychiatry 2014;13:317‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Grant BF, Saha TD, Ruan WJ et al. Epidemiology of DSM‐5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA Psychiatry 2016;73:39‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Regier DA, Narrow WE, Kuhl EA et al. The conceptual development of DSM‐5. Am J Psychiatry 2009;166:645‐50. [DOI] [PubMed] [Google Scholar]
- 88. Wakefield JC. Diagnosing DSM‐IV, part 2: Eysenck (1986) and the essentialist fallacy. Behav Res Ther 1997;35:651‐66. [DOI] [PubMed] [Google Scholar]
- 89. Plomin R. Genes and behavior: cognitive abilities and disabilities in normal populations. In: Ron M, Robbins T (eds). Disorders of brain and mind, Vol. 2. Cambridge: Cambridge University Press, 2003:3‐29. [Google Scholar]
- 90. Plomin R. Blueprint: how DNA makes us who we are. Cambridge: MIT Press, 2018. [Google Scholar]
- 91. Fodor JA. The modularity of mind. Cambridge: MIT Press, 1983. [Google Scholar]
- 92. Carruthers P. The architecture of the mind. Oxford: Oxford University Press, 2006. [Google Scholar]
- 93. Pinker S. How the mind works. New York: Norton, 1997. [DOI] [PubMed] [Google Scholar]
- 94. Cosmides L, Tooby J. Cognitive adaptations for social exchange. In: Barkow J, Cosmides L, Tooby J (eds). The adapted mind. Oxford: Oxford University Press, 1992:163‐228. [Google Scholar]
- 95. Barrett HC, Kurzban R. Modularity in cognition: framing the debate. Psychol Rev 2006;113:628‐47. [DOI] [PubMed] [Google Scholar]
- 96. Sperber D. In defense of massive modularity. In Mehler J, Dupoux E (eds). Language, brain, and cognitive development: essays in honor of Jacques Mehler. Cambridge: MIT Press, 2001:47‐57. [Google Scholar]
- 97. Kendell RE. The classification of depressive illness. Maudsley Monograph No. 18. London: Oxford University Press, 1968. [Google Scholar]
- 98. Kendell RE, Gourley J. The clinical distinction between the affective psychoses and schizophrenia. Br J Psychiatry 1970;117:261‐6. [PubMed] [Google Scholar]
- 99. Kendell RE, Gourley J. The clinical distinction between psychotic and neurotic depression. Br J Psychiatry 1970;117:257‐60. [PubMed] [Google Scholar]
- 100. Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry 2003;160:4‐12. [DOI] [PubMed] [Google Scholar]
- 101. Spitzer RL. Letter to the editor. Schizophr Bull 1982;8:592. [Google Scholar]
- 102. Freud S. Analysis of a phobia in a five‐year‐old boy. In: Strachey J (ed), The standard edition of the complete psychological works of Sigmund Freud, Vol. 10. London: Hogarth Press, 1955:1‐150. [Google Scholar]
- 103. Andreasen N. The broken brain: the biological revolution in psychiatry. New York: Harper Collins, 1984. [Google Scholar]
- 104. Weir K. The roots of mental illness: how much of mental illness can the biology of the brain explain? APA Monitor 2012;43:30. [Google Scholar]
- 105. Hoogman M, Bralten J, Hibar DP et al. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross‐sectional mega‐analysis. Lancet Psychiatry 2017;4:310‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. George MS, Ketter TA, Parekh PI et al. Brain activity during transient sadness and happiness in healthy women. Am J Psychiatry 1995;152:341‐51. [DOI] [PubMed] [Google Scholar]
- 107. Wakefield JC. Addiction and the concept of disorder, Part 2: Is every mental disorder a brain disorder? Neuroethics 2017;10:55‐67. [Google Scholar]
- 108. Janoff‐Bulman R. Assumptive worlds and the stress of traumatic events: applications of the schema construct. Soc Cogn 1989;7:113‐36. [Google Scholar]
- 109. Spitzer RL, Williams JB. The definition and diagnosis of mental disorder. In: Grove WR (ed). Deviance and mental illness. Beverly Hills: Sage, 1982:15‐31. [Google Scholar]
- 110. Campbell EJM, Scadding JG, Roberts RS. The concept of disease. BMJ 1979;2:757‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Johnson S. Dictionary of the English language. London: Strahan, 1755. [Google Scholar]
- 112. Brigham A. Definition of insanity – nature of the disease. Am J Insanity 1844;1:97‐116. [DOI] [PubMed] [Google Scholar]
- 113. Johnson H. On the arrangement and nomenclature of mental disorders. London: Longman, Brown, Green, and Longmans, 1843. [Google Scholar]
- 114. Spitzer RL, Wilson PT. Nosology and the official psychiatric nomenclature. In: Freedman AM, Kaplan HI, Sadock BJ (eds). Comprehensive textbook of psychiatry, Vol. 2. Baltimore: Williams & Wilkins, 1975:826‐45. [Google Scholar]
- 115. Heckers S, Kendler KS. The evolution of Kraepelin's nosological principles. World Psychiatry 2020;19:381‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wakefield JC. Limits of operationalization: a critique of Spitzer and Endicott's (1978) proposed operational criteria for mental disorder. J Abnorm Psychol 1993;102:160‐72. [DOI] [PubMed] [Google Scholar]
- 117. Wakefield JC. Wittgenstein's nightmare: why the RDoC grid needs a conceptual dimension. World Psychiatry 2014;13:38‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Lin D, Boyle MP, Dollar P et al. Functional identification of an aggression locus in the mouse hypothalamus. Nature 2011;470:221‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Fejzo MS, Sazonova OV, Sathirapongsasuti JF et al. Placenta and appetite genes GDF15 and IGFBP7 are associated with hyperemesis gravidarum. Nat Commun 2018;9:1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Fejzo MS, Fasching PA, Schneider MO et al. Analysis of GDF15 and IGFBP7 in hyperemesis gravidarum support causality. Geburtshilfe Frauenheilkd 2019;79:382‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Kendler KS. The nature of psychiatric disorders. World Psychiatry 2016;15:5‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Shakeshaft NG, Trzaskowski M, McMillan A et al. Thinking positively: the genetics of high intelligence. Intelligence 2015;48:123‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Reichenberg A, Cederlöf M, McMillan A et al. Discontinuity in the genetic and environmental causes of the intellectual disability spectrum. Proc Natl Acad Sci USA 2016;113:1098‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Zachar P, Kendler KS. A diagnostic and statistical manual of mental disorders history of premenstrual dysphoric disorder. J Nerv Ment Dis 2014;202:346‐52. [DOI] [PubMed] [Google Scholar]
- 125. Epperson CN, Steiner M, Hartlage SA et al. Premenstrual dysphoric disorder: evidence for a new category for DSM‐5. Am J Psychiatry 2012;169:465‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Epperson CN. Premenstrual dysphoric disorder and the brain. Am J Psychiatry 2013;170:248‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Baller EB, Wei S‐M, Kohn PD et al. Abnormalities of dorsolateral prefrontal function in women with premenstrual dysphoric disorder: a multimodal neuroimaging study. Am J Psychiatry 2013;170:305‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Schmidt PJ, Nieman LK, Danaceau MA et al. Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med 1998;338:209‐16. [DOI] [PubMed] [Google Scholar]
- 129. Dubey N, Hoffman JF, Schuebel K et al. The ESC/E(Z) complex, an effector of response to ovarian steroids, manifests an intrinsic difference in cells from women with premenstrual dysphoric disorder. Mol Psychiatry 2017;22:1172‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Marrocco J, Einhorn NR, Petty GH et al. Epigenetic intersection of BDNF Val66Met genotype with premenstrual dysphoric disorder transcriptome in a cross‐species model of estradiol add‐back. Mol Psychiatry 2020;25:572‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Polimanti R, Gelernter J. Widespread signatures of positive selection in common risk alleles associated to autism spectrum disorder. PLoS Genet 2017;13:e1006618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Visser SN, Danielson ML, Bitsko RH et al. Trends in the parent‐report of health care provider‐diagnosed and medicated in attention‐deficit/hyperactivity disorder: United States, 2003‐2011. J Am Acad Child Adolesc Psychiatry 2014,53:34‐46.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Elder TE. The importance of relative standards in ADHD diagnoses: evidence based on exact birth dates. J Health Econ 2010;29:641‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Evans WN, Morrill MS, Parente ST. Measuring inappropriate medical diagnosis and treatment in survey data: the case of ADHD among school‐age children. J Health Econ 2010;29:657‐73. [DOI] [PubMed] [Google Scholar]
- 135. Zoëga H, Valdimarsdóttir UA, Hernández‐Díaz S. Age, academic performance, and stimulant prescribing for ADHD: a nationwide cohort study. Pediatrics 2012;130:1012‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Shaw P, Malek M, Watson B et al. Trajectories of cerebral cortical development in childhood and adolescent and adult attention‐deficit/hyperactivity disorder. Biol Psychiatry 2013;74:599‐606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Moffitt TE, Houts R, Asherson P et al. Is adult ADHD a childhood‐onset neurodevelopmental disorder? Evidence from a four‐decade longitudinal cohort study. Am J Psychiatry 2015;172:967‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Klein RG. Thinning of the cerebral cortex during development: a dimension of ADHD. Am J Psychiatry 2011;168:111‐3. [DOI] [PubMed] [Google Scholar]
- 139. Hill JC, Schoener EP. Age‐dependent decline of attention deficit hyperactivity disorder. Am J Psychiatry 1996;153:1143‐6. [DOI] [PubMed] [Google Scholar]
- 140. Biederman J, Petty CR, Evans M et al. How persistent is ADHD? A controlled 10‐year follow‐up study of boys with ADHD. Psychiatry Res 2010;177:299‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Faraone SV, Doyle AE, Mick E et al. Meta‐analysis of the association between the 7‐repeat allele of the dopamine D4 receptor gene and attention deficit hyperactivity disorder. Am J Psychiatry 2001;158:1052‐7. [DOI] [PubMed] [Google Scholar]
- 142. Rapoport JL. Association of the dopamine receptor D4 (DRD4) gene 7‐repeat allele with children with attention‐deficit/hyperactivity disorder (ADHD): an update. Am J Med Genet 2007;144B:379‐82. [DOI] [PubMed] [Google Scholar]
- 143. Grady DL, Chi H‐C, Ding Y‐C et al. High prevalence of rare dopamine receptor D4 alleles in children diagnosed with attention‐deficit hyperactivity disorder. Mol Psychiatry 2003;8:536‐45. [DOI] [PubMed] [Google Scholar]
- 144. Grady DL, Harxhi A, Smith M et al. Sequence variants of the DRD4 gene in autism: further evidence that rare DRD4 7R haplotypes are ADHD specific. Am J Med Genet 2005;136B:33‐5. [DOI] [PubMed] [Google Scholar]
- 145. González S, Rangel‐Barajas C, Peper M et al. Dopamine D4 receptor, but not the ADHD‐associated D4.7 variant, forms functional heteromers with the dopamine D 2S receptor in the brain. Mol Psychiatry 2012;17:650‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Volkow ND, Wang G, Kollins SH et al. Evaluating dopamine reward pathway in ADHD. JAMA 2009;302:1084‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Volkow ND, Wang G‐J, Newcorn JH et al. Motivation deficit in ADHD is associated with dysfunction of the dopamine reward pathway. Mol Psychiatry 2011;16:1147‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Gehricke J‐G, Swanson JM, Duong S et al. Increased brain activity to unpleasant stimuli in individuals with the 7R allele of the DRD4 gene. Psychiatry Res 2015;231:58‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Ding Y‐C, Chi H‐C, Grady DL et al. Evidence of positive selection acting at the human dopamine receptor D4 gene locus. Proc Natl Acad Sci USA 2002;99:309‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Wang E, Ding Y‐C, Flodman P et al. The genetic architecture of selection at the human dopamine receptor D4 (DRD4) gene locus. Am J Hum Genet 2004;74:931‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Kluger AN, Siegfried Z, Ebstein RP. A meta‐analysis of the association between DRD4 polymorphism and novelty seeking. Mol Psychiatry 2002;7:712‐7. [DOI] [PubMed] [Google Scholar]
- 152. Dreber A, Apicella CL, Eisenberg DTA et al. The 7R polymorphism in the dopamine receptor D4 gene (DRD4) is associated with financial risk taking in men. Evol Hum Behav 2009;30:85‐92. [Google Scholar]
- 153. Grady DL, Thanos PK, Corrada MM et al. DRD4 genotype predicts longevity in mouse and human. J Neurosci 2013;33:286‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Kirk SA, Kutchins H. The selling of DSM: the rhetoric of science in psychiatry. New York: Aldine de Gruyter, 1992. [Google Scholar]
- 155. Maj M. The need for a conceptual framework in psychiatry acknowledging complexity while avoiding defeatism. World Psychiatry 2016;15:1‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Wakefield JC. DSM‐5 substance use disorder: how conceptual missteps weakened the foundations of the addictive disorders field. Acta Psychiatr Scand 2015;132:327‐34. [DOI] [PubMed] [Google Scholar]
- 157. Wakefield JC. DSM‐5, psychiatric epidemiology, and the false positive problem. Epidemiol Psychiatr Sci 2015;24:188‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]


