Abstract
Antimicrobial peptides are an attractive alternative to traditional antibiotics, due to their physicochemical properties, activity toward a broad spectrum of bacteria, and mode-of-actions distinct from those used by current antibiotics. In general, antimicrobial peptides kill bacteria by either disrupting their membrane, or by entering inside bacterial cells to interact with intracellular components. Characterization of their mode-of-action is essential to improve their activity, avoid resistance in bacterial pathogens, and accelerate their use as therapeutics. Here we review experimental biophysical tools that can be employed with model membranes and bacterial cells to characterize the mode-of-action of antimicrobial peptides.
Keywords: peptide-lipid interactions, bacterial membrane, cellular uptake, biophysical methodologies, peptide therapeutics
Introduction
Antibiotic resistant bacteria are rapidly emerging while the development of new antimicrobial agents is decelerating (1–3). To fight infections caused by resistant bacteria, it is essential to develop new compounds. Antimicrobial peptides (AMPs) have attracted attention as potential alternative antimicrobial agents, as these small biological molecules kill bacteria using a mode-of-action (MOA) distinct from those used by traditional antibiotics (4).
AMPs are produced in almost all species (5), kill a broad spectrum of bacteria, fungi, protozoa and viruses, have anticancer properties (6, 7), and can kill antibiotic-resistant bacteria (8, 9). In general, AMPs are positively charged amphipathic molecules able to selectively target bacteria and kill them using two broad MOAs. In the first mechanism AMPs induce membrane disruption, leading to cell lysis and death. In the second MOA, AMPs enter cells without membrane disruption and inhibit essential intracellular functions by binding to nucleic acids or intracellular proteins (10–12).
Peptide-based antimicrobials, such as Tyrothricin, Gramicidin S (13), Vancomycin and Telavancin (14), are used in the clinic as therapeutics. Nevertheless, the widespread application of AMPs is limited by a perception that peptides are expensive to produce, susceptible to proteases, and display high cytotoxicity (15–17). Peptide production costs have decreased over the past years due to advances in solid- and liquid-phase peptide synthesis (18, 19), and production of recombinant peptides in Escherichia coli (20) and yeast (21). Peptides can be engineered to increase their chemical and proteolytic stability via backbone cyclization (22), side chain-to-side chain cyclization (23), or the inclusion of stereochemical amino acids (24). Furthermore, toxicity to the host can be reduced, and potency can be improved, if we understand their MOA (16, 25–28).
In this mini-review, we highlight some experimental biophysical techniques that can be employed to investigate the complex MOA of AMPs. Identifying whether particular AMPs act by disrupting bacterial membranes, or by interfering with an intracellular pathway, is key to rationally improve efficacy, stability and safety of AMPs, and develop novel antimicrobial therapeutics.
Characterization of Peptide-Lipid Binding Using Model Membranes
AMPs generally target and bind bacterial membranes via peptide-lipid interactions. Model membrane systems, including Langmuir monolayers, liposomes, and solid supported bilayers, have been used to screen peptide-membrane interactions and investigate the effect of peptides on the structure of lipid bilayers. Although they are less complex than bacterial membranes, model membranes are useful to investigate individual membrane components (29, 30). They can be produced with defined lipid compositions, biophysical properties, and conditions (e.g., size, charge, pH, ionic strength); thereby reducing the variables present in biological assays.
Liposomes are particularly useful as a model membrane: they are versatile, easy to prepare, and can be used in several methodologies. Liposomes can be prepared with synthetic lipids present in bacterial membranes, such as phospholipids with phosphatidylglycerol-, or phosphatidylethanolamine-headgroups and cardiolipin (31) or can be prepared with lipids extracted directly from bacterial membranes. Liposomes are unilamellar or multilamellar structures obtained by suspending lipids in an aqueous solution and by sonicating, or extruding them through a membrane filter with a defined pore size, such as 50 nm, 100 nm and 1 μm, to prepare small, large and giant vesicles, respectively.
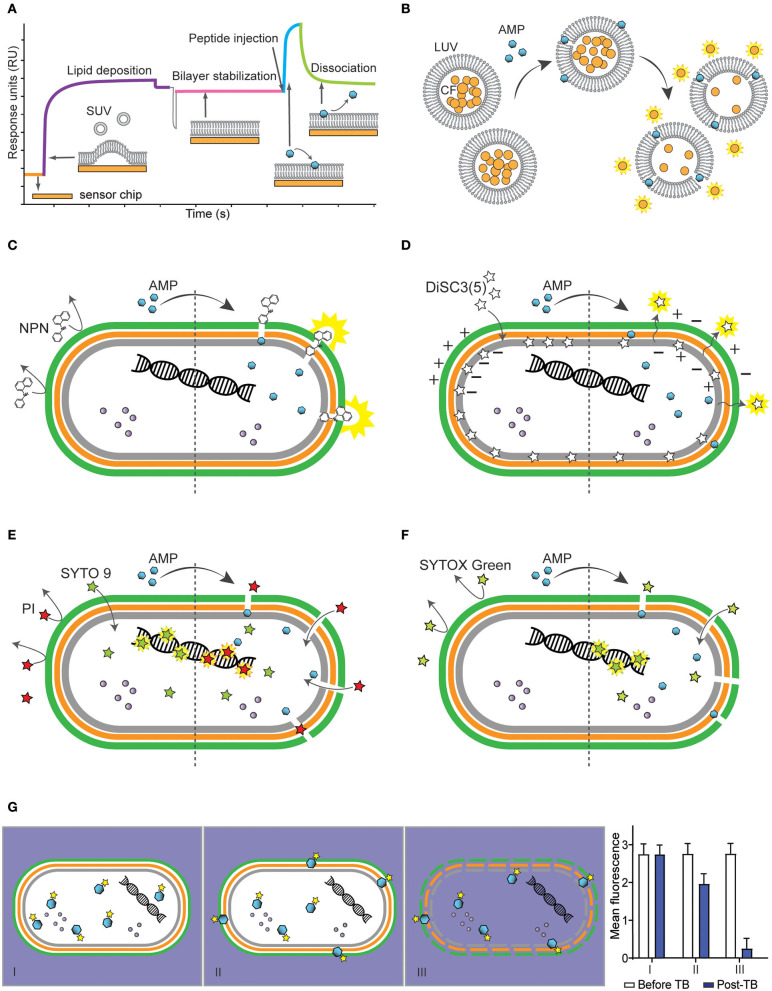
Surface plasmon resonance (SPR) (Figure 1A) can be used to study peptide-lipid binding affinity in real-time and without requiring fluorescently labeled peptide. In this assay, liposomes are deposited onto the surface of a sensor chip covered with polydextran (e.g., L1 Sensor Chip from GE Biacore systems) to form a stable lipid bilayer (32). Peptide solution is injected over the lipid bilayer and peptide-lipid binding is monitored via variation of refractive index over time. Sensorgrams can be used to calculate peptide-lipid binding association (kon), dissociation (koff) rate constants, equilibrium dissociation constant (KD) and membrane partition coefficients (Kp) (32, 33). It is possible to predict cytotoxic properties of AMPs by comparing their peptide-lipid binding affinity. AMPs with high binding affinity for negatively charged membranes and with weak affinity for zwitterionic membranes are normally selective toward bacteria and not toxic to host cells (34).
Figure 1.
Methodologies to determine interactions of antimicrobial peptides (AMPs) with bacterial membranes using model membranes (A,B) and bacterial cells (C-G). (A) Schematic representation of a sensorgram obtained with surface plasmon resonance (SPR) to monitor peptide-lipid interactions. The response units (RU) increase when small unilamellar vesicles (SUV) are injected to cover the chip (orange) and form a bilayer (purple). Once the bilayer is stabilized (pink), AMPs are injected and association with the lipid bilayer (blue) is monitored in real time. The stronger the binding of the antimicrobial peptide (AMP) to the lipid system, the higher the response units. When the peptide injection stops, it is possible to monitor the dissociation of the peptides from the lipid bilayer (green). (B) Illustration of the leakage assay using large unilamellar vesicles (LUV) filled with carboxyfluorescein (CF), whose fluorescence is self-quenched when packed inside LUVs at high concentration. In the presence of permeabilizing AMPs, CF escapes into the aqueous environment and becomes fluorescent. (C–F) Schematic of a Gram-negative bacterium with inner membrane (gray), peptidoglycan layer (orange), outer membrane (green) and intracellular content such as proteins (purple spheres) and nucleic acids (helix) and the effect of fluorescent dyes before (left) and after (right) treatment with a membrane-active AMP. (C) Illustration of N-phenyl-1-napthylamine (NPN) becoming highly fluorescent when in hydrophobic environment such as lipid membranes, subsequently damaged by AMPs. (D) Illustration of 3,3′-Dipropylthiadicarbocyanine iodide [DiSC3(5)] packed within inner membrane of bacterium. DiSC3(5) is released into the aqueous environment and becomes highly fluorescent (right) once membrane is depolarized by binding of AMPs. (E) Illustration of bacterial cells incubated with propidium iodide (PI) and SYTO 9, to label lysed/dead and viable cells, respectively. Left side shows PI unable to go through intact membrane, unlike SYTO 9 that can penetrate intact membrane and bind to DNA. Once AMP damages membrane, PI enters the cell and displaces SYTO 9 (right). (F) Illustration of SYTOX Green which is highly fluorescent if bound to DNA, however, unable to go through bacterial membrane unless membrane is damaged by the AMP. (G) Schematic of internalization of bacterial cell by fluorescently labeled AMP and graph showing fluorescence measurement before and after addition of trypan blue (TB). Panel I shows an AMP able to enter bacteria cells without damaging membrane, panel II shows an AMP entering cells with a portion located on the membrane, and panel III shows internalization of an AMP and permeabilization of bacterial membrane resulting in drop of fluorescence readings after addition of TB quenching fluorescence of labeled AMP.
Many AMPs kill bacteria by inducing membrane disruption and leakage of bacterial content. Leakage assays with model membranes (Figure 1B) can be used to investigate the ability of AMPs to disrupt lipid bilayers. In these assays, an aqueous soluble fluorescent dye, such as carboxyfluorescein (35–37) or calcein (38, 39), is entrapped into large unilamellar vesicles at self-quenching concentrations. Dye-loaded vesicles are resuspended in buffer by gel filtration and their lipid concentration quantified using the Stewart assay (40). If peptides permeabilize vesicles, the fluorescent dye is released into solution, resulting in increased fluorescence emission signal. This assay can be performed in a 96-well plate format to reduce the volume of reagents and peptides (41). It can also be used to investigate membrane selectivity in a competitive lipid environment (42). For example, AMPs can be incubated with a mixture of liposomes of distinct composition to quantify selective disruption of negatively charged over neutral liposomes. Although leakage assays do not provide information about the disruption mechanism involved (e.g., toroidal pore, barrel pore, or carpet mechanism), they inform on whether AMPs can disrupt lipid bilayers, can be used to investigate membrane selectivity (42).
Molecular dynamic simulations using atomistic or coarse-grained models of lipid bilayers, can also be used to characterize peptide-lipid interactions and to gain information on the disruption mechanism used by specific AMPs (43–46). More complex bacterial cell wall models (e.g., peptidoglycan network, outer membrane of Gram-negative bacteria) (47–49) have been developed and can be used to simulate interactions of peptides with bacterial cell walls, and predict membrane disruption properties (50).
Examining Integrity and Function of Bacterial Membranes Using Membrane Dyes
Membrane dyes and fluorescence spectrophotometer plate readers can be used with bacteria cells to study the effect of AMPs on the integrity of specific layers of bacterial membranes. For instance, the fluorescence of the lipophilic dye N-phenyl-1-napthylamine (NPN) can inform on the ability of AMPs to permeabilize the outer membrane of Gram-negative bacteria (Figure 1C). NPN emits weak fluorescence in aqueous environment and is highly fluorescent in hydrophobic environment found in lipid membranes. NPN cannot insert into intact bacteria membranes; however, when AMPs disturb the outer membrane of Gram-negative bacteria, NPN gains access to lipid layers in the outer membrane and/or in the cytoplasmic membrane (51–53) and its fluorescence emission intensity increases. This assay can be done using a 96-well plate format in a fluorescence spectrophotometer plate reader, in which peptides are added to bacterial suspensions.
Cell membranes of viable bacteria are polarized (i.e., they have a negative transmembrane potential), and some cationic AMPs kill bacteria by depolarizing their membranes (10, 54). The dye 3,3′-Dipropylthiadicarbocyanine iodide [DiSC3(5)] is cationic, membrane-permeable, fluorescent in aqueous environment and can be used to examine the ability of specific AMPs to depolarize bacterial membranes (53, 55, 56). DiSC3(5) has a stable and low fluorescence emission signal when bound to viable bacteria with polarized membranes; if an AMP induces membrane depolarization, the dye is released, and its fluorescence emission intensity increases (Figure 1D). In this assay, it is important to optimize cell density, dye concentration and ensure that tested AMPs do not quench the fluorescence of the dye, as this assay is based on fluorescence quenching (57).
Examining Bacterial Membrane Integrity Using Flow Cytometry
Flow cytometry combines fluidic, optical and electronic parameters to analyze physical properties (e.g., size and granularity) and fluorescence of individual cells within a population of cells. Each cell goes through a set of lasers and produces scattered and fluorescent light signals that are detected and analyzed by a computer (58).
Bacteria with permeabilized membranes can be distinguished from viable bacterial cells using two fluorescent dyes [e.g., propidium iodide (PI) and SYTO 9] and by analyzing cells using flow cytometry (59). PI and SYTO 9 become fluorescent when intercalating with DNA. However, PI is a red-fluorescent dye, non-permeable to intact plasma membranes and cannot enter viable cells, whereas SYTO 9 is a green-fluorescent dye that can enter both live and dead bacterial cells (Figure 1E). PI has stronger affinity for nucleic acids than SYTO 9; therefore, when both dyes have access to nucleic acids inside bacteria, PI displaces SYTO 9 (60).
There are some factors that might interfere with correct readings, such as photobleaching of SYTO 9, variable binding affinities of SYTO 9 to live and dead cells, background fluorescence and bleed-through (61). Moreover, some bacteria strains have efflux pumps that can remove PI from the cell (60). Nevertheless, this is a rapid and high-throughput assay to quantify the effect of AMPs on the cell membrane integrity within a large population of cells (62).
SYTOX Green is another high-affinity nucleic acid stain that can be used to investigate cell membrane integrity in bacteria using flow cytometry. This dye only enters cells with compromised plasma membrane (Figure 1F). The binding of SYTOX green to nucleic acids results in >500-fold increase in fluorescence emission intensity (63). SYTOX green and PI have similar molecular weight (i.e., 600 and 688 Da), and entry of these two dyes into bacteria is unlikely to be discriminated based on their size. Nevertheless, the detection of permeabilized cells and distinction from non-permeabilized cells is superior when using SYTOX Green. This dye has a higher quantum yield and molar extinction coefficient compared to that of PI (63). These advantages might explain why many studies used SYTOX green to investigate bacterial membrane integrity in the presence of AMPs, instead of the combination of SYTO 9 and PI (53, 64–69).
Confirming Whether Membrane Disruption is the Cause of Death
It is important to investigate whether peptide concentrations required to lyse bacterial membranes correlate with concentrations required to kill bacteria. Some AMPs display a minimal inhibitory concentration (MIC) below the concentration required to disrupt membranes, suggesting that bacteria are being killed/inactivated by a mechanism not directly related to cell membrane disruption. This can be investigated by treating bacteria with various concentrations of peptide and quantifying viable cells (e.g., using plate colony count method) in parallel with permeabilized cells (e.g., using a flow cytometry assay with SYTOX Green) (67, 70). Interestingly, some bacteria species seem to be more resistant to membrane damage, as suggested by a study with the AMP maculatin 1.1. This peptide induces uptake of SYTOX Green in E. coli and Staphylococcus aureus at similar concentrations, but is more potent at inhibiting the growth of S. aureus (67).
When AMPs inhibit bacterial growth at non-permeabilizing concentrations, their MOA is likely to involve entry in the cell and ability to interact with an intracellular target; therefore, it is important to investigate whether they can enter inside bacteria. These non-lytic AMPs able to cross bacterial membranes can also be referred to as cell-penetrating peptides (66).
Distinguishing Internalized and Membrane-Bound Peptide Via Flow Cytometry
Uptake into bacterial cells can be investigated using flow cytometry and peptides labeled with a fluorophore, such as Alexa Fluor® 488, fluorescein isothiocyanate (FITC), bodipy or rhodamine. Care must be taken when choosing the fluorophore, as some can alter peptide physicochemical properties (e.g., increase of overall hydrophobicity), peptide-peptide intermolecular interactions, binding affinity for lipid bilayers, activity, or cellular uptake (71–75).
There are also some challenges in conjugating peptides with fluorescent labels, as the most common strategies involve amide bond ligation with labels derivatized with succinimidyl esters and require a free amine (66, 69). Therefore, the peptide requires an uncapped N-terminal, or a Lys residue within the amino acid sequence if the peptide is backbone-cyclised. Moreover, when the peptide has more than one Lys, several isomers with one or more label molecules might be obtained (76). To decrease the number of possible isomers and avoid changes in the overall charge of Lys-rich peptides after labeling, the dye can be conjugated using site-directed strategies. Some examples include conjugation of alkyne-derivatized dyes onto azide-containing peptides with copper-catalyzed azide-alkyne cycloaddition, and conjugation of dyes containing hydroxylamine with acetone-linked peptides using oxime ligation (77).
Fluorescently labeled AMP molecules located inside bacteria can be distinguished from those bound to the bacteria surface by screening peptide-treated cells via flow cytometry (Figure 1G). Fluorescence emission intensity and percentage of fluorescent bacteria are recorded before and after addition of trypan blue (TB), an aqueous fluorescence quencher unable to enter cells with intact membranes. A similar fluorescence emission signal before and after addition of TB indicates that the peptide is inside the bacteria. A decrease in fluorescence emission signal suggests that a proportion of peptide molecules is surface exposed and accessible to TB. A significant decrease in the percentage of fluorescent bacteria and in the fluorescence emission intensity indicate that cells are permeabilized, which enabled TB to enter and quench the fluorescence emission of peptide inside cells (66, 78, 79).
Using Microscopy to Visualize Bacteria Morphology and Peptide Location
Changes in cell morphology induced by AMPs can be visualized using electron microscopy and atomic force microscopy (AFM). Bacterial cells incubated with sub-lethal and/or lethal concentrations of AMPs are imaged to identify whether the membrane surface is intact, becomes wrinkly, has blebs, or is lysed (28, 80–82). AMPs inducing visible damages are likely to act on the membrane, whereas lack of morphological changes at lethal concentrations suggests interference with an internal component.
The location of labeled AMPs inside bacteria can be visualized using confocal microscopy. For instance, AMPs NCR247 and NCR235 bind to the membrane of both Salmonella and Listeria, but can only reach the cytosol of Salmonella (83, 84). In another study, the authors showed localization of an AMP inside E. coli using confocal microscopy, SYTOX green and rhodamine-labeled AMP, and confirmed changes in the E. coli morphology using AFM (70). These examples demonstrate how diverse and versatile microscopy techniques are to evaluate peptide location within bacteria, and effect on their membrane.
Detection of Amp and Nucleic Acid Interactions Using Electrophoretic Mobility Shift Assays
Some AMPs kill bacteria by interacting with DNA or RNA, and therefore interfere with their synthesis, replication, and translational processes (10, 85). It is debatable whether AMPs can target specific portions of DNA/RNA, as positively charged AMPs might bind unspecifically to negatively charged nucleic acids via strong electrostatic attractions (86). In addition, binding to nucleic acids can be unrelated to the cell death mechanism, as it can occur as a result of AMPs entering bacteria after disrupting their membranes. Thus, studies to investigate interaction with DNA/RNA are more appropriate with non-lytic AMPs.
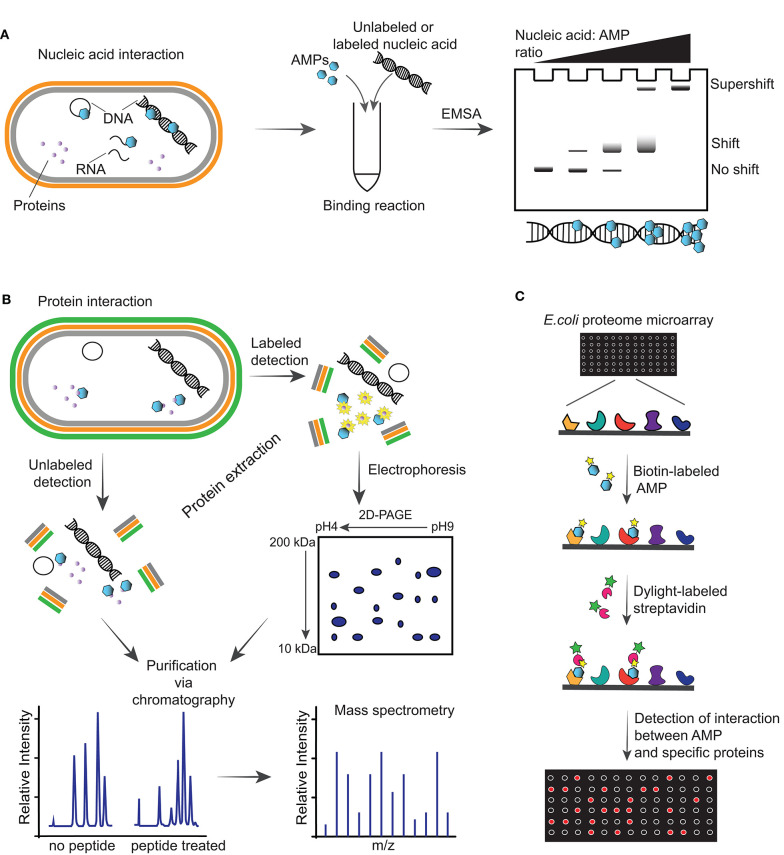
The gel electrophoretic mobility shift assay (EMSA) is a rapid and sensitive methodology used to detect interactions between proteins, or peptides, with DNA/RNA (87). In this assay, the peptide is incubated with nucleic acids and the reaction is electrophoresed on an agarose or native polyacrylamide gel to detect whether a peptide-nucleic acid complex is formed based on a slower migration than that of free nucleic acid. The complex can be detected using a range of approaches, including fluorescence, chemiluminescence, immunohistochemical and highly sensitive radioisotope-labeled nucleic acids (Figure 2A). One limitation to consider during the electrophoresis is that samples are not at chemical equilibrium and therefore rapid dissociation during this time might prevent detection of the complex. Antimicrobial peptides such as indolicin (88), LL-37 (89), Burforin II (90) and Frenatin 2.3S peptide (91) have been shown to bind bacterial DNA using EMSAs.
Figure 2.
Illustrations of methodologies for detection of intracellular targets of antimicrobial peptides (AMPs). (A) Schematic of detection of an AMP able to interact with nucleic acid including DNA, plasmid DNA and RNA of a Gram-negative bacterium via electrophoretic mobility shift assay (EMSA). This assay consists of running incubation reactions between increasing ratios of AMPs with specific nucleic acid (labeled or unlabeled) and running the reactions through an agarose gel. Depending on the affinity of the AMP with the nucleic acid, a shift or supershift in the EMSA is observed. (B) Interaction of AMPs with intracellular proteins can be detected by incubating the peptides with bacteria, followed by protein extraction, purification, and mass spectrometry analysis. Alternatively, cells can be incubated with AMPs followed by addition of radioactive labels to incorporate labels to the newly synthesized proteins and performing a two-dimensional polyacrylamide gel (2D-PAGE), from which spots are analyzed via mass spectrometry. (C) Schematic representation of E. coli proteome microarray and workflow. Biotinylated AMPs are probed on the microarray followed by Dylight-labeled streptavidin to tag the biotin linked on the AMPs and signals are obtained by scanning the chip with a laser scanner to show interaction between AMPs and specific proteins on the chip.
Proteomics to Search For a Putative Intracellular Target Or/and Differences in Protein Expression
Non-lytic AMPs that translocate through bacterial membranes might inhibit intracellular processes by interacting with essential proteins and enzymes (92). Mass spectrometry and proteome microarray are examples of methodologies used to identify protein targets of AMPs and/or the subsequent changes in protein expression due to peptide entry inside bacteria.
Mass spectrometry is a powerful tool to examine changes in protein expression of bacteria treated with AMPs. In the unlabeled approach, after co-incubation of bacteria with AMPs, proteins are extracted, digested and fractionated, and the whole proteome is analyzed by mass spectrometry (Figure 2B). A recent study used this approach to show the effect of LL-37 peptide on the proteome of Streptococcus pneumoniae D39, and identified alteration in the expression of 105 proteins (93). Treatment with LL-37 induced upregulation of proteins involved in cell surface modification, including increasing membrane surface charge, and an abundance of ABC transporters. These modifications are likely to help removing LL-37 from the bacterial membrane. Using a similar workflow, lipidomics studies can be used to investigate changes in the lipid composition of bacterial membranes after treatment with AMPs, as recently reviewed (94).
Wenzel et al. (95) reported a radio-labeling approach to facilitate the identification of proteins that are up/down regulated upon treatment with peptide (Figure 2B). In this study, Bacillus subtilis cultures were incubated with RW-rich peptides, followed by addition of radioactive methionine to incorporate a radioactive label into newly synthesized proteins. Proteins were extracted from cells and separated on a two-dimensional polyacrylamide gel (2D-PAGE) where up/down regulated proteins were identified, excised from the gel and identified by mass spectrometry (95).
Proteome microarray is another powerful and high-throughput tool with potential to screen the entire proteome and identify targets in a single experiment. This has been exemplified with a biotin-labeled AMP and incubated with an E. coli K12 proteome microarray chip, followed by detection of the biotinylated AMPs with Dylight-labeled streptavidin (92) (Figure 2C). The signals detected on a microarray scanner show binding between specific proteins and AMPs. Fabricated E. coli K12 proteome microarrays have been used to identify intracellular protein targets of several AMPs, such as bactenecin 7, a hybrid of pleurocidin and dermaseptin, and proline-arginine-rich peptide (96). However, the coverage of the microarray, differences between the proteins immobilized on microarrays and their counterpart in physiological conditions, and the cost are limitations for a broader use of protein microarrays (97).
Discussion
AMPs are promising leads to develop new antimicrobial drugs to treat bacterial infections. The number of AMPs reported to date is high, and some candidates reached clinical trials (98, 99). Understanding the MOA used by AMPs to kill bacteria is important to advance their development. Here we describe some experimental biophysical tools that can be used to investigate whether AMPs act by disrupting bacterial membranes, or by modulating intracellular activities. An overview of multiple AMPs, their MOA and the biophysical techniques employed to characterize them, is summarized in a recent review (100).
Determining whether an AMP disrupts bacterial membranes can be straightforward; however, finding specific intracellular targets is more complex. Pinpointing whether AMPs act by interfering with DNA, RNA or proteins remains challenging, as some AMPs not only act on the membrane they can also activate a cascade of reactions within the bacteria (12, 85). Advances in transcriptomics, proteomics, lipidomics and continued development of high-throughput techniques will facilitate these MOA studies.
Computational tools, such as molecular dynamics simulations, machine learning, and AMPs databases [such as https://dbaasp.org/ (101)] are also important to identify new AMPs, characterize their MOA, and predict lead candidates (102, 103). Computer-based and wet-lab based methodologies can be integrated to better understand the MOA of AMPs, and to rationally design novel AMPs with a required MOA. For example, when searching for AMPs to target intracellular pathogens, it is desirable to have peptides with cell-penetrating properties able to enter host cells and kill bacteria by modulating specific bacterial components, without disrupting the membrane of host cells. On the other hand, when targeting mixed-species biofilms, membrane-lytic AMPs with a broad-spectrum activity are likely to be more effective at the infection site, compared to AMPs that selectively inhibit an intracellular target.
MOA studies in vitro and in silico, together with efficacy, safety and pharmacology studies in vivo and ex vivo, are essential to convert AMP leads into therapeutics used in the clinic. In particular, MOA studies help in identifying off-targets in host cells, understanding spectrum of activity, finding intrinsically resistant bacteria, and overcoming challenges associated with delivery of peptides. Therefore, the biophysical tools here described can assist the development of novel antibiotics.
Author Contributions
AB and STH conceptualized the manuscript. AB wrote the original draft. STH reviewed and edited the manuscript. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. STH was an Australian Research Council (ARC) Future Fellow (FT150100398). The Translational Research Institute was supported by a grant from the Australian Government. The authors are supported by the Australian Research Council Centre of Excellence for Innovations in Peptide and Protein Science (CE200100012).
References
- 1.Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. (2015) 40:277–83. [PMC free article] [PubMed] [Google Scholar]
- 2.Ghosh C, Sarkar P, Issa R, Haldar J. Alternatives to conventional antibiotics in the era of antimicrobial resistance. Trends Microbiol. (2019) 27:323–38. 10.1016/j.tim.2018.12.010 [DOI] [PubMed] [Google Scholar]
- 3.Ventola CL. The antibiotic resistance crisis: part 2: management strategies and new agents. P T. (2015) 40:344–52. [PMC free article] [PubMed] [Google Scholar]
- 4.Lei J, Sun L, Huang S, Zhu C, Li P, He J, et al. The antimicrobial peptides and their potential clinical applications. Am J Transl Res. (2019) 11:3919–31. [PMC free article] [PubMed] [Google Scholar]
- 5.Zasloff M. Antimicrobial peptides of multicellular organisms. Nature. (2002) 415:389–95. 10.1038/415389a [DOI] [PubMed] [Google Scholar]
- 6.Hancock RE, Diamond G. The role of cationic antimicrobial peptides in innate host defences. Trends Microbiol. (2000) 8:402–10. 10.1016/S0966-842X(00)01823-0 [DOI] [PubMed] [Google Scholar]
- 7.Zhang LJ, Gallo RL. Antimicrobial peptides. Curr Biol. (2016) 26:R14–R19. 10.1016/j.cub.2015.11.017 [DOI] [PubMed] [Google Scholar]
- 8.Ageitos JM, Sanchez-Perez A, Calo-Mata P, Villa TG. Antimicrobial peptides (AMPs): ancient compounds that represent novel weapons in the fight against bacteria. Biochem Pharmacol. (2017) 133:117–38. 10.1016/j.bcp.2016.09.018 [DOI] [PubMed] [Google Scholar]
- 9.Mourtada R, Herce HD, Yin DJ, Moroco JA, Wales TE, Engen JR, et al. Design of stapled antimicrobial peptides that are stable, nontoxic and kill antibiotic-resistant bacteria in mice. Nat Biotechnol. (2019) 37:1186–97. 10.1038/s41587-019-0222-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brogden KA. Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat Rev Microbiol. (2005) 3:238–50. 10.1038/nrmicro1098 [DOI] [PubMed] [Google Scholar]
- 11.Sani MA, Separovic F. How membrane-active peptides get into lipid membranes. Acc Chem Res. (2016) 49:1130–8. 10.1021/acs.accounts.6b00074 [DOI] [PubMed] [Google Scholar]
- 12.Le CF, Fang CM, Sekaran SD. Intracellular targeting mechanisms by antimicrobial peptides. Antimicrob Agents Chemother. (2017) 61:e02340–16. 10.1128/AAC.02340-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wenzel M, Rautenbach M, Vosloo JA, Siersma T, Aisenbrey CHM, Zaitseva E, et al. The multifaceted antibacterial mechanisms of the pioneering peptide antibiotics tyrocidine and gramicidin S. mBio. (2018) 9:e00802–18. 10.1128/mBio.00802-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Binda E, Marinelli F, Marcone GL. Old and new glycopeptide antibiotics: action and Resistance. Antibiotics. (2014) 3:572–94. 10.3390/antibiotics3040572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahlapuu M, Hakansson J, Ringstad L, Bjorn C. Antimicrobial peptides: an emerging category of therapeutic agents. Front Cell Infect Microbiol. (2016) 6:194. 10.3389/fcimb.2016.00194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mishra B, Reiling S, Zarena D, Wang G. Host defense antimicrobial peptides as antibiotics: design and application strategies. Curr Opin Chem Biol. (2017) 38:87–96. 10.1016/j.cbpa.2017.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen CH, Lu TK. Development and challenges of antimicrobial peptides for therapeutic applications. Antibiotics. (2020) 9:24. 10.3390/antibiotics9010024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isidro-Llobet A, Kenworthy MN, Mukherjee S, Kopach ME, Wegner K, Gallou F, et al. Sustainability challenges in peptide synthesis and purification: from RandD to production. J Org Chem. (2019) 84:4615–28. 10.1021/acs.joc.8b03001 [DOI] [PubMed] [Google Scholar]
- 19.Magana M, Pushpanathan M, Santos AL, Leanse L, Fernandez M, Ioannidis A, et al. The value of antimicrobial peptides in the age of resistance. Lancet Infect Dis. (2020) 20:e216–e230. 10.1016/S1473-3099(20)30327-3 [DOI] [PubMed] [Google Scholar]
- 20.Gaglione R, Pane K, Dell'olmo E, Cafaro V, Pizzo E, Olivieri G, et al. Cost-effective production of recombinant peptides in Escherichia coli. N Biotechnol. (2019) 51:39–48. 10.1016/j.nbt.2019.02.004 [DOI] [PubMed] [Google Scholar]
- 21.Cao J, De La Fuente-Nunez C, Ou RW, Torres MT, Pande SG, Sinskey AJ, et al. Yeast-based synthetic biology platform for antimicrobial peptide production. ACS Synth Biol. (2018) 7:896–902. 10.1021/acssynbio.7b00396 [DOI] [PubMed] [Google Scholar]
- 22.Clark RJ, Fischer H, Dempster L, Daly NL, Rosengren KJ, Nevin ST, et al. Engineering stable peptide toxins by means of backbone cyclization: stabilization of the alpha-conotoxin MII. Proc Natl Acad Sci USA. (2005) 102:13767–72. 10.1073/pnas.0504613102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schafmeister CE, Po J, Verdine GL. An all-hydrocarbon cross-linking system for enhancing the helicity and metabolic stability of peptides. J Am Chem Soc. (2000) 122:5891–2. 10.1021/ja000563a [DOI] [Google Scholar]
- 24.Tugyi R, Uray K, Ivan D, Fellinger E, Perkins A, Hudecz F. Partial D-amino acid substitution: improved enzymatic stability and preserved Ab recognition of a MUC2 epitope peptide. Proc Natl Acad Sci USA. (2005) 102:413–8. 10.1073/pnas.0407677102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zelezetsky I, Tossi A. Alpha-helical antimicrobial peptides–using a sequence template to guide structure-activity relationship studies. Biochim Biophys Acta. (2006) 1758:1436–49. 10.1016/j.bbamem.2006.03.021 [DOI] [PubMed] [Google Scholar]
- 26.Badosa E, Ferre R, Planas M, Feliu L, Besalu E, Cabrefiga J, et al. A library of linear undecapeptides with bactericidal activity against phytopathogenic bacteria. Peptides. (2007) 28:2276–85. 10.1016/j.peptides.2007.09.010 [DOI] [PubMed] [Google Scholar]
- 27.Mangoni ML, Shai Y. Short native antimicrobial peptides and engineered ultrashort lipopeptides: similarities and differences in cell specificities and modes of action. Cell Mol Life Sci. (2011) 68:2267–80. 10.1007/s00018-011-0718-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Torcato IM, Huang YH, Franquelim HG, Gaspar D, Craik DJ, Castanho MA, et al. Design and characterization of novel antimicrobial peptides, R-BP100 and RW-BP100, with activity against gram-negative and gram-positive bacteria. Biochim Biophys Acta. (2013) 1828:944–55. 10.1016/j.bbamem.2012.12.002 [DOI] [PubMed] [Google Scholar]
- 29.Knobloch J, Suhendro DK, Zieleniecki JL, Shapter JG, Koper I. Membrane-drug interactions studied using model membrane systems. Saudi J Biol Sci. (2015) 22:714–8. 10.1016/j.sjbs.2015.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hollmann A, Martinez M, Maturana P, Semorile LC, Maffia PC. Antimicrobial peptides: interaction with model and biological membranes and synergism with chemical antibiotics. Front Chem. (2018) 6:204. 10.3389/fchem.2018.00204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Epand RM, Epand RF. Bacterial membrane lipids in the action of antimicrobial agents. J Pept Sci. (2011) 17:298–305. 10.1002/psc.1319 [DOI] [PubMed] [Google Scholar]
- 32.Figueira TN, Freire JM, Cunha-Santos C, Heras M, Goncalves J, Moscona A, et al. Quantitative analysis of molecular partition towards lipid membranes using surface plasmon resonance. Sci Rep. (2017) 7:45647. 10.1038/srep45647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Benfield AH, Defaus S, Lawrence N, Chaousis S, Condon N, Cheneval O, et al. Cyclic gomesin, a stable redesigned spider peptide able to enter cancer cells. Biochim Biophys Acta Biomembr. (2020) 1863:183480. 10.1016/j.bbamem.2020.183480 [DOI] [PubMed] [Google Scholar]
- 34.Maturana P, Martinez M, Noguera ME, Santos NC, Disalvo EA, Semorile L, et al. Lipid selectivity in novel antimicrobial peptides: implication on antimicrobial and hemolytic activity. Colloids Surf B Biointerfaces. (2017) 153:152–9. 10.1016/j.colsurfb.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 35.Weinstein JN, Klausner RD, Innerarity T, Ralston E, Blumenthal R. Phase transition release, a new approach to the interaction of proteins with lipid vesicles. Application to lipoproteins. Biochim Biophys Acta. (1981) 647:270–84. 10.1016/0005-2736(81)90255-8 [DOI] [PubMed] [Google Scholar]
- 36.Rex S. Pore formation induced by the peptide melittin in different lipid vesicle membranes. Biophys Chem. (1996) 58:75–85. 10.1016/0301-4622(95)00087-9 [DOI] [PubMed] [Google Scholar]
- 37.Ambroggio EE, Separovic F, Bowie JH, Fidelio GD, Bagatolli LA. Direct visualization of membrane leakage induced by the antibiotic peptides: maculatin, citropin, and aurein. Biophys J. (2005) 89:1874–81. 10.1529/biophysj.105.066589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kendall DA, Macdonald RC. A fluorescence assay to monitor vesicle fusion and lysis. J Biol Chem. (1982) 257:13892–5. [PubMed] [Google Scholar]
- 39.Won A, Ianoul A. Interactions of antimicrobial peptide from C-terminus of myotoxin II with phospholipid mono- and bilayers. Biochim Biophys Acta. (2009) 1788:2277–83. 10.1016/j.bbamem.2009.07.012 [DOI] [PubMed] [Google Scholar]
- 40.Stewart JC. Colorimetric determination of phospholipids with ammonium ferrothiocyanate. Anal Biochem. (1980) 104:10–4. 10.1016/0003-2697(80)90269-9 [DOI] [PubMed] [Google Scholar]
- 41.Huang YH, Colgrave ML, Daly NL, Keleshian A, Martinac B, Craik DJ. The biological activity of the prototypic cyclotide kalata b1 is modulated by the formation of multimeric pores. J Biol Chem. (2009) 284:20699–707. 10.1074/jbc.M109.003384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sani MA, Gagne E, Gehman JD, Whitwell TC, Separovic F. Dye-release assay for investigation of antimicrobial peptide activity in a competitive lipid environment. Eur Biophys J. (2014) 43:445–50. 10.1007/s00249-014-0970-0 [DOI] [PubMed] [Google Scholar]
- 43.Cruz VL, Ramos J, Melo MN, Martinez-Salazar J. Bacteriocin AS-48 binding to model membranes and pore formation as revealed by coarse-grained simulations. Biochim Biophys Acta. (2013) 1828:2524–31. 10.1016/j.bbamem.2013.05.036 [DOI] [PubMed] [Google Scholar]
- 44.Bennett WF, Hong CK, Wang Y, Tieleman DP. Antimicrobial peptide simulations and the influence of force field on the free energy for pore formation in lipid bilayers. J Chem Theory Comput. (2016) 12:4524–33. 10.1021/acs.jctc.6b00265 [DOI] [PubMed] [Google Scholar]
- 45.Aghazadeh H, Ganjali Koli M, Ranjbar R, Pooshang Bagheri K. Interactions of GF-17 derived from LL-37 antimicrobial peptide with bacterial membranes: a molecular dynamics simulation study. J Comput Aided Mol Des. (2020) 34:1261–73. 10.1007/s10822-020-00348-4 [DOI] [PubMed] [Google Scholar]
- 46.Su J, Marrink SJ, Melo MN. Localization preference of antimicrobial peptides on liquid-disordered membrane domains. Front Cell Dev Biol. (2020) 8:350. 10.3389/fcell.2020.00350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Piggot TJ, Holdbrook DA, Khalid S. Electroporation of the E. coli and S Aureus membranes: molecular dynamics simulations of complex bacterial membranes. J Phys Chem B. (2011) 115:13381–8. 10.1021/jp207013v [DOI] [PubMed] [Google Scholar]
- 48.Kim S, Pires MM, Im W. Insight into elongation stages of peptidoglycan processing in bacterial cytoplasmic membranes. Sci Rep. (2018) 8:17704. 10.1038/s41598-018-36075-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vaiwala R, Sharma P, Puranik M, Ayappa KG. Developing a coarse-grained model for bacterial cell walls: evaluating mechanical properties and free energy barriers. J Chem Theory Comput. (2020) 16:5369–84. 10.1021/acs.jctc.0c00539 [DOI] [PubMed] [Google Scholar]
- 50.Jiang X, Yang K, Yuan B, Gong B, Wan L, Patil NA, et al. Simulations of octapeptin-outer membrane interactions reveal conformational flexibility is linked to antimicrobial potency. J. Biol. Chem. (2020) 295:15902–12. 10.1074/jbc.RA120.014856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hancock RE, Farmer SW. Mechanism of uptake of deglucoteicoplanin amide derivatives across outer membranes of Escherichia coli and Pseudomonas aeruginosa. Antimicrob Agents Chemother. (1993) 37:453–6. 10.1128/AAC.37.3.453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee DL, Powers JP, Pflegerl K, Vasil ML, Hancock RE, Hodges RS. Effects of single D-amino acid substitutions on disruption of beta-sheet structure and hydrophobicity in cyclic 14-residue antimicrobial peptide analogs related to gramicidin S. J Pept Res. (2004) 63:69–84. 10.1046/j.1399-3011.2003.00106.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Velkov T, Gallardo-Godoy A, Swarbrick JD, Blaskovich M. A. T., Elliott A. G., et al. (2018). Structure, function, and biosynthetic origin of octapeptin antibiotics active against extensively drug-resistant gram-negative bacteria. Cell Chem Biol. 25:380–391.e5. 10.1016/j.chembiol.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yeaman MR, Yount NY. Mechanisms of antimicrobial peptide action and resistance. Pharmacol Rev. (2003) 55:27–55. 10.1124/pr.55.1.2 [DOI] [PubMed] [Google Scholar]
- 55.Wu M, Maier E, Benz R, Hancock RE. Mechanism of interaction of different classes of cationic antimicrobial peptides with planar bilayers and with the cytoplasmic membrane of Escherichia coli. Biochemistry. (1999) 38:7235–42. 10.1021/bi9826299 [DOI] [PubMed] [Google Scholar]
- 56.Cheng M, Huang JX, Ramu S, Butler MS, Cooper MA. Ramoplanin at bactericidal concentrations induces bacterial membrane depolarization in Staphylococcus aureus. Antimicrob Agents Chemother. (2014) 58:6819–27. 10.1128/AAC.00061-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Te Winkel JD, Gray DA, Seistrup KH, Hamoen LW, Strahl H. Analysis of antimicrobial-triggered membrane depolarization using voltage sensitive dyes. Front Cell Dev Biol. (2016) 4:29. 10.3389/fcell.2016.00029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mckinnon KM. Flow cytometry: an overview. Curr Protoc Immunol. (2018) 120:5.1.1–5.1.11. 10.1002/cpim.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Freire JM, Gaspar D, De La Torre BG, Veiga AS, Andreu D, Castanho MA. Monitoring antibacterial permeabilization in real time using time-resolved flow cytometry. Biochim Biophys Acta. (2015) 1848:554–60. 10.1016/j.bbamem.2014.11.001 [DOI] [PubMed] [Google Scholar]
- 60.Stocks SM. Mechanism and use of the commercially available viability stain, BacLight. Cytometry A. (2004) 61:189–95. 10.1002/cyto.a.20069 [DOI] [PubMed] [Google Scholar]
- 61.Stiefel P, Schmidt-Emrich S, Maniura-Weber K, Ren Q. Critical aspects of using bacterial cell viability assays with the fluorophores SYTO9 and propidium iodide. BMC Microbiol. (2015) 15:36. 10.1186/s12866-015-0376-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O'Brien-Simpson NM, Pantarat N, Attard TJ, Walsh KA, Reynolds EC. A rapid and quantitative flow cytometry method for the analysis of membrane disruptive antimicrobial activity. PLoS ONE. (2016) 11:e0151694. 10.1371/journal.pone.0151694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roth BL, Poot M, Yue ST, Millard PJ. Bacterial viability and antibiotic susceptibility testing with SYTOX green nucleic acid stain. Appl Environ Microbiol. (1997) 63:2421–31. 10.1128/AEM.63.6.2421-2431.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rathinakumar R, Walkenhorst WF, Wimley WC. Broad-spectrum antimicrobial peptides by rational combinatorial design and high-throughput screening: the importance of interfacial activity. J Am Chem Soc. (2009) 131:7609–17. 10.1021/ja8093247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kaplan CW, Sim JH, Shah KR, Kolesnikova-Kaplan A, Shi W, Eckert R. Selective membrane disruption: mode of action of C16G2, a specifically targeted antimicrobial peptide. Antimicrob Agents Chemother. (2011) 55:3446–52. 10.1128/AAC.00342-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Torcato IM, Huang YH, Franquelim HG, Gaspar DD, Craik DJ, Castanho MA, et al. The antimicrobial activity of Sub3 is dependent on membrane binding and cell-penetrating ability. Chembiochem. (2013) 14:2013–22. 10.1002/cbic.201300274 [DOI] [PubMed] [Google Scholar]
- 67.Sani MA, Henriques ST, Weber D, Separovic F. Bacteria may cope differently from similar membrane damage caused by the australian tree frog antimicrobial peptide maculatin 1.1. J Biol Chem. (2015) 290:19853–62. 10.1074/jbc.M115.643262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dias SA, Freire JM, Perez-Peinado C, Domingues MM, Gaspar D, Vale N, et al. New potent membrane-targeting antibacterial peptides from viral capsid proteins. Front Microbiol. (2017) 8:775. 10.3389/fmicb.2017.00775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Troeira Henriques S, Lawrence N, Chaousis S, Ravipati AS, Cheneval O, Benfield AH, et al. Redesigned spider peptide with improved antimicrobial and anticancer properties. ACS Chem Biol. (2017) 12:2324–34. 10.1021/acschembio.7b00459 [DOI] [PubMed] [Google Scholar]
- 70.Perez-Peinado C, Dias SA, Domingues MM, Benfield AH, Freire JM, Radis-Baptista G, et al. Mechanisms of bacterial membrane permeabilization by crotalicidin (Ctn) and its fragment Ctn(15-34), antimicrobial peptides from rattlesnake venom. J Biol Chem. (2018) 293:1536–49. 10.1074/jbc.RA117.000125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Henriques ST, Costa J, Castanho MA. Re-evaluating the role of strongly charged sequences in amphipathic cell-penetrating peptides: a fluorescence study using pep-1. FEBS Lett. (2005) 579:4498–502. 10.1016/j.febslet.2005.06.085 [DOI] [PubMed] [Google Scholar]
- 72.Szeto HH, Schiller PW, Zhao K, Luo G. Fluorescent dyes alter intracellular targeting and function of cell-penetrating tetrapeptides. FASEB J. (2005) 19:118–20. 10.1096/fj.04-1982fje [DOI] [PubMed] [Google Scholar]
- 73.Hughes LD, Rawle RJ, Boxer SG. Choose your label wisely: water-soluble fluorophores often interact with lipid bilayers. PLoS ONE. (2014) 9:e87649. 10.1371/journal.pone.0087649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hedegaard SF, Derbas MS, Lind TK, Kasimova MR, Christensen MV, Michaelsen MH, et al. Fluorophore labeling of a cell-penetrating peptide significantly alters the mode and degree of biomembrane interaction. Sci Rep. (2018) 8:6327. 10.1038/s41598-018-24154-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cavaco M, Perez-Peinado C, Valle J, Silva RDM, Correia JDG, Andreu D, et al. To what extent do fluorophores bias the biological activity of peptides? A practical approach using membrane-active peptides as models. Front Bioeng Biotechnol. (2020) 8:552035. 10.3389/fbioe.2020.552035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Philippe GJ, Gaspar D, Sheng C, Huang YH, Benfield AH, Condon ND, et al. Cell membrane composition drives selectivity and toxicity of designed cyclic helix-loop-helix peptides with cell penetrating and tumor suppressor properties. ACS Chem Biol. (2019) 14:2071–87. 10.1021/acschembio.9b00593 [DOI] [PubMed] [Google Scholar]
- 77.Lawrence N, Philippe GJB, Harvey PJ, Condon ND, Benfield AH, Cheneval O, et al. Cyclic peptide scaffold with ability to stabilize and deliver a helical cell-impermeable cargo across membranes of cultured cancer cells. RSC Chem Biol. (2020). 10.1039/D0CB00099J [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Benincasa M, Pacor S, Gennaro R, Scocchi M. Rapid and reliable detection of antimicrobial peptide penetration into gram-negative bacteria based on fluorescence quenching. Antimicrob Agents Chemother. (2009) 53:3501–4. 10.1128/AAC.01620-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mardirossian M, Perebaskine N, Benincasa M, Gambato S, Hofmann S, Huter P, et al. The dolphin proline-rich antimicrobial peptide Tur1A inhibits protein synthesis by targeting the bacterial ribosome. Cell Chem Biol. (2018) 25:530–539.e7. 10.1016/j.chembiol.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hartmann M, Berditsch M, Hawecker J, Ardakani MF, Gerthsen D, Ulrich AS. Damage of the bacterial cell envelope by antimicrobial peptides gramicidin S and PGLa as revealed by transmission and scanning electron microscopy. Antimicrob Agents Chemother. (2010) 54:3132–42. 10.1128/AAC.00124-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schneider VA, Coorens M, Ordonez SR, Tjeerdsma-Van Bokhoven JL, Posthuma G, Van Dijk A, et al. Imaging the antimicrobial mechanism(s) of cathelicidin-2. Sci Rep. (2016) 6:32948. 10.1038/srep32948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen RB, Zhang K, Zhang H, Gao CY, Li CL. Analysis of the antimicrobial mechanism of porcine beta defensin 2 against E. coli by electron microscopy and differentially expressed genes. Sci Rep. (2018) 8:14711. 10.1038/s41598-018-32822-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Farkas A, Maroti G, Durgo H, Gyorgypal Z, Lima RM, Medzihradszky KF, et al. Medicago truncatula symbiotic peptide NCR247 contributes to bacteroid differentiation through multiple mechanisms. Proc Natl Acad Sci USA. (2014) 111:5183–8. 10.1073/pnas.1404169111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Farkas A, Maroti G, Kereszt A, Kondorosi E. Comparative analysis of the bacterial membrane disruption effect of two natural plant antimicrobial peptides. Front Microbiol. (2017) 8:51. 10.3389/fmicb.2017.00051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cardoso MH, Meneguetti BT, Costa BO, Buccini DF, Oshiro KGN, Preza SLE, et al. Non-lytic antibacterial peptides that translocate through bacterial membranes to act on intracellular targets. Int J Mol Sci. (2019) 20:4877. 10.3390/ijms20194877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Snoussi M, Talledo JP, Del Rosario NA, Mohammadi S, Ha BY, Kosmrlj A, et al. Heterogeneous absorption of antimicrobial peptide LL37 in Escherichia coli cells enhances population survivability. eLife. (2018) 7:e38174. 10.7554/eLife.38174.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hellman LM, Fried MG. Electrophoretic mobility shift assay (EMSA) for detecting protein-nucleic acid interactions. Nat Protoc. (2007) 2:1849–61. 10.1038/nprot.2007.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hsu CH, Chen C, Jou ML, Lee AY, Lin YC, Yu YP, et al. Structural and DNA-binding studies on the bovine antimicrobial peptide, indolicidin: evidence for multiple conformations involved in binding to membranes and DNA. Nucleic Acids Res. (2005) 33:4053–64. 10.1093/nar/gki725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Limoli DH, Rockel AB, Host KM, Jha A, Kopp BT, Hollis T, et al. Cationic antimicrobial peptides promote microbial mutagenesis and pathoadaptation in chronic infections. PLoS Pathog. (2014) 10:e1004083. 10.1371/journal.ppat.1004083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Park CB, Kim HS, Kim SC. Mechanism of action of the antimicrobial peptide buforin II: buforin II kills microorganisms by penetrating the cell membrane and inhibiting cellular functions. Biochem Biophys Res Commun. (1998) 244:253–7. 10.1006/bbrc.1998.8159 [DOI] [PubMed] [Google Scholar]
- 91.Munoz-Camargo C, Salazar VA, Barrero-Guevara L, Camargo S, Mosquera A, Groot H, et al. Unveiling the multifaceted mechanisms of antibacterial activity of buforin II and frenatin 2.3S peptides from skin micro-organs of the orinoco lime treefrog (Sphaenorhynchus lacteus). Int J Mol Sci. (2018) 19:2170. 10.3390/ijms19082170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shah P, Hsiao FS, Ho YH, Chen CS. The proteome targets of intracellular targeting antimicrobial peptides. Proteomics. (2016) 16:1225–37. 10.1002/pmic.201500380 [DOI] [PubMed] [Google Scholar]
- 93.Mucke PA, Maass S, Kohler TP, Hammerschmidt S, Becher D. Proteomic adaptation of streptococcus pneumoniae to the human antimicrobial peptide LL-37. Microorganisms. (2020) 8:413. 10.3390/microorganisms8030413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lee TH, Hofferek V, Separovic F, Reid GE, Aguilar MI. The role of bacterial lipid diversity and membrane properties in modulating antimicrobial peptide activity and drug resistance. Curr Opin Chem Biol. (2019) 52:85–92. 10.1016/j.cbpa.2019.05.025 [DOI] [PubMed] [Google Scholar]
- 95.Wenzel M, Schriek P, Prochnow P, Albada HB, Metzler-Nolte N, Bandow JE. Influence of lipidation on the mode of action of a small RW-rich antimicrobial peptide. Biochim Biophys Acta. (2016) 1858:1004–11. 10.1016/j.bbamem.2015.11.009 [DOI] [PubMed] [Google Scholar]
- 96.Ho YH, Shah P, Chen YW, Chen CS. Systematic analysis of intracellular-targeting antimicrobial peptides, bactenecin 7, hybrid of pleurocidin and dermaseptin, proline-arginine-rich peptide, and lactoferricin b, by using Escherichia coli proteome microarrays. Mol Cell Proteomics. (2016) 15:1837–47. 10.1074/mcp.M115.054999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Qi H, Wang F, Tao SC. Proteome microarray technology and application: higher, wider, and deeper. Expert Rev Proteomics. (2019) 16:815–27. 10.1080/14789450.2019.1662303 [DOI] [PubMed] [Google Scholar]
- 98.Koo HB, Seo J. Antimicrobial peptides under clinical investigation. Peptide Sci. (2019) 111:e24122. 10.1002/pep2.24122 [DOI] [Google Scholar]
- 99.Browne K, Chakraborty S, Chen R, Willcox MD, Black DS, Walsh WR, et al. A new era of antibiotics: the clinical potential of antimicrobial peptides. Int J Mol Sci. (2020) 21:7047. 10.3390/ijms21197047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Raheem N, Straus SK. Mechanisms of action for antimicrobial peptides with antibacterial and antibiofilm functions. Front Microbiol. (2019) 10:2866. 10.3389/fmicb.2019.02866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pirtskhalava M, Amstrong AA, Grigolava M, Chubinidze M, Alimbarashvili E, Vishnepolsky B, et al. DBAASP v3: database of antimicrobial/cytotoxic activity and structure of peptides as a resource for development of new therapeutics. Nucleic Acids Res. (2020) 5:gkaa991. 10.1093/nar/gkaa991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lee EY, Lee MW, Fulan BM, Ferguson AL, Wong GCL. What can machine learning do for antimicrobial peptides, and what can antimicrobial peptides do for machine learning? Interface Focus. (2017) 7:20160153. 10.1098/rsfs.2016.0153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cardoso MH, Orozco RQ, Rezende SB, Rodrigues G, Oshiro KGN, Candido ES, et al. Computer-aided design of antimicrobial peptides: are we generating effective drug candidates? Front Microbiol. (2019) 10:3097. 10.3389/fmicb.2019.03097 [DOI] [PMC free article] [PubMed] [Google Scholar]