Abstract
Objective:
Sexual assault is associated with higher rates of posttraumatic stress disorder (PTSD) than other traumas, and the course of PTSD may differ by trauma type. However, the course of PTSD after sexual assault has not been summarized. The aim of this meta-analysis was to identify the prevalence and severity of PTSD and changes to the average rate of recovery in the 12 months following sexual assault.
Method:
Authors searched four databases for prospective studies published before April 2020 and sought relevant unpublished data. Eligible studies assessed PTSD in at least 10 survivors of sexual assault in at least two time points, starting within three months post-assault. Random effects linear-linear piecewise models were used to identify changes in average recovery rate and produce model-implied estimates of monthly point prevalence and mean symptom severity.
Results:
Meta-analysis of 22 unique samples (N = 2106) indicated that 74.58% (95% CI: 67.21, 81.29) and 41.49% (95% CI: 32.36, 50.92) of individuals met diagnostic criteria for PTSD at the first and twelfth month following sexual assault, respectively. PTSD symptom severity was 47.94% (95% CI: 41.27, 54.61) and 29.91% (95% CI: 23.10, 36.73) of scales’ maximum severity at the first and twelfth month following sexual assault, respectively. Most symptom recovery occurred within the first three months following sexual assault, after which point the average rate of recovery slowed.
Conclusions:
Findings indicate that PTSD is common and severe following sexual assault, and the first three months post-assault may be a critical period for natural recovery.
Keywords: sexual violence, rape, posttraumatic stress disorder, meta-analysis, victimization
Sexual assault—defined as unwanted, nonconsensual sexual contact achieved via force, incapacitation, and/or coercion—is a common form of trauma. Epidemiological data indicate that, in their lifetime, 12.3-13.5% of women and 0.9-1.6% of men in the United States experience forced penetration, and 8.0%-11.0% of women and 0.6-5.5% of men experience alcohol/drug-facilitated penetration (Black et al., 2011; Smith et al., 2018;). In addition, 12.5-16.0% of women and 2.0-2.4% of men experience lifetime sexual coercion (Black et al., 2011; Breiding et al., 2014; Smith et al., 2018).
Sexual assault is associated with heightened risk for posttraumatic stress disorder (PTSD) (Dworkin et al., 2017), which is characterized by re-experiencing (i.e., reliving the event), avoidance behavior, negative changes to thoughts and emotions, and hyperarousal (American Psychiatric Association [APA], 2013). Studies assessing PTSD in relation to any trauma exposure (not necessarily due to sexual assault) indicate that 36% of sexual assault survivors meet criteria for lifetime PTSD (Dworkin, 2020) and 12-25% meet criteria for current PTSD (Kilpatrick et al., 2007; Resnick et al., 1993; Zinzow et al., 2012).
Immediately following sexual assault, the majority of survivors experience PTSD symptoms (Rothbaum et al., 1992; Steenkamp et al., 2012). Prospective studies demonstrate that, over the months following sexual assault, many survivors experience at least some natural remission of their initial symptoms (e.g., Gutner, et al., 2006; Riggs et al., 1995; Rothbaum et al., 1992), and PTSD is only diagnosed when sufficient symptoms are present for at least one continuous month (APA, 2013). Accordingly, PTSD is considered to be a disorder of non-recovery from initial symptoms (Monson & Friedman, 2006).
Compared to other potentially traumatic events (e.g., physical assault, accidents, natural disasters), for which only a minority of survivors experience significant levels of PTSD (Galatzer-Levy et al., 2018; Lowe et al., 2020), sexual assault appears to carry relatively greater risk for PTSD (Brewin et al., 2000; Dworkin, 2020; Kessler et al., 2014; Kilpatrick et al., 2003), and may be associated with unique trajectories of recovery. According to cognitive-behavioral theories of PTSD, negative attributions regarding the cause and meaning of trauma (e.g., self-blame, the world is dangerous) and avoidance of trauma reminders (e.g., thoughts/feelings associated with the assault, situations that remind the individuals of the assault) prevent natural recovery from PTSD symptoms (Ehlers & Clark, 2000; Foa & Kozak, 1986; Foa et al., 2006; Resick et al., 2017). Stigma associated with sexual assault (e.g., victim blame; Kennedy & Prock, 2018; Lebowitz & Roth, 1994) may contribute to inaccurate or unhelpful negative attributions or encourage avoidance of discussing the assault with others (Kelley et al., 2009; see for exception Smith et al., 2016), uniquely obstructing PTSD recovery.
Two prior meta-analyses of prospective studies have summarized the prevalence of PTSD within the first year after exposure to a range of potentially traumatic events, although neither focused specifically on sexual assault. First, Hiller et al. (2016) conducted a meta-analysis of recovery from childhood trauma involving 27 peer-reviewed studies and 1 unpublished dataset (including 3 studies that sampled at least some children exposed to interpersonal violence). The aggregate prevalence of PTSD was 21% at 1 month, 15% at 3 months, 12% at 6 months, and 11% at one year (Hiller et al., 2016). Analyses of the subset of studies that examined reductions in symptomatology identified that the greatest reductions in symptom severity occurred between 1 and 3 months, although there was a greater reduction in prevalence of PTSD diagnosis from 3 to 6 months (32%) than 1 to 3 months (17%). Second, by pooling item-level data from 13 studies of acutely-hospitalized trauma survivors (7.7% of whom were hospitalized following interpersonal violence), Qi et al. (2018) found that PTSD prevalence ranged from 3-62% at studies’ baseline assessment; 4-38% at studies’ first follow-up assessment, and 4–27% at studies’ third follow-up assessment. These wide prevalence ranges reflected the inclusion of studies that explicitly selected participants on the basis of elevated symptom severity, as well as studies that enrolled participants regardless of symptom severity. Results were not presented as a function of time since trauma.
Similar results have been identified in reviews of published prospective studies. Santiago et al. (2013) reviewed 58 published studies of various trauma types. Although this review included mixed physical and sexual assault samples, no studies specific to sexual assault were included. Consistent with the notion of natural recovery, they reported decreases in the median prevalence of PTSD between 1 month (28.8%) and 3 months (17.8%) post-trauma, followed by a stabilization in prevalence through 12 months (17.0%; Santiago et al., 2013). Differences in trajectories were observed for different types of trauma: whereas PTSD prevalence decreased over time for non-violent traumas (20.1% at month 1 and 14.0% at month 12), the median prevalence increased from 11.8% at month 1 to 23.3% at month 12 for violent traumas. More recently, MacGregor and colleagues (2019) reviewed 10 published studies of sexual assault recovery in young people (ages 10-24). PTSD prevalence was 65-88% at month 1 (based on 2 studies), 35-71% at 3 months (based on 3 studies), and 58-60% at month 12 (based on 2 studies).
These meta-analyses and systematic reviews generally provide evidence for the presence of high levels of initial post-trauma symptoms that tend to stabilize by the end of the first year post-trauma. However, they have two major limitations. First, although the Santiago and Hiller reviews found that large reductions in PTSD symptomatology occurred between 1 and 3 months post-trauma, neither statistically determined if there was a time point at which the average rate of recovery slowed (Hiller et al., 2016; Santiago et al., 2013). This information would be critical to inform the timing of early assessment and intervention efforts. Second, despite evidence that sexual assault is more strongly associated with PTSD than other forms of trauma (Brewin et al., 2000; Dworkin, 2020; Kessler et al., 2014; Kilpatrick et al., 2003), no prior work has quantitatively summarized the natural course of PTSD recovery specifically for adolescent and adult sexual assault survivors. Aggregating across samples would clarify average rates of recovery in the acute aftermath of sexual assault, which would in turn inform clinical practice and help to contextualize individual responses.
Thus, the goal of this study was to characterize the average month-to-month rates of PTSD in adolescents and adults in the year following sexual assault. We aimed to use random-effects meta-analysis to (1) statistically summarize the point prevalence and average symptom severity of PTSD in the 12 months following sexual assault and (2) empirically test whether there is a point at which the average rate of recovery changes. Building on prior reviews of PTSD following other types of trauma, we focused specifically on samples exposed to adolescent and/or adult sexual assault. We also sought to address the reliance of prior reviews on published literature by seeking unpublished data to supplement published reports.
Method
Procedures
We undertook an extensive search strategy to identify published and unpublished literature on this topic. First, we searched PsycInfo, PsycArticles, Academic Search Complete, and PubMed on November 20th, 2018 and April 6th, 2020 using the following search terms and Boolean operators: (“posttraumatic stress” OR “post-traumatic stress” OR ptsd) AND (“sexual assault” OR rape OR “sexual violence” OR “sexual victimization”) AND (prospective OR recent OR month* OR year* OR week* OR trajector*). This search yielded 929 unique results, which were each independently subject to abstract and/or full-text review by two authors using the eligibility criteria (discussed next). Kappa values for eligibility decisions of “yes” versus “maybe” or “no” ranged from .82 to .87 across coders. Disagreements were discussed collaboratively, and 58 articles were ultimately retained for coding from this step. Second, the first author reviewed the citations of the articles retained for coding and the citations of prior reviews on related topics (i.e., Bryant, 2011; Dworkin et al., 2017; Guay et al., 2019; Forneris et al., 2013; MacGregor et al., 2019), and the third author reviewed a database of articles collected for a prior review, which yielded an additional 12 articles. Third, requests for unpublished data were posted to relevant listservs, which did not yield any additional studies. Finally, when full information was not included in a published report, we emailed authors to request supplemental PTSD data, and alerted these authors that we sought any other unpublished datasets available to them. We ultimately sent 29 emails requesting data, 13 of which yielded supplemental data, but no previously unidentified datasets were obtained through this step.
Eligible studies were those where: 1) results were reported in English; 2) at least 10 survivors of sexual assault were included (we contacted authors to request sexual-assault-specific data for mixed-trauma samples); 3) the sample included at least some survivors who were not receiving an active treatment meant to reduce PTSD as a part of study participation (we contacted authors to request data for control conditions in clinical trials); 4) survivors were recruited because they experienced a past-year trauma; 5) PTSD symptoms were first assessed within 3 months of sexual assault; 6) PTSD was assessed prospectively, 7) the sample was not primarily comprised of children (defined as a sample mean age of 13 years old or younger); and 8) the study did not exclude participants on the basis of symptom level cutoffs (i.e., the study did not have a PTSD symptom maximum or minimum as an inclusion criterion). From the 70 studies that met these criteria, we selected the 22 unique samples in which relevant outcome data could be obtained (i.e., the percent of survivors with PTSD or means and standard deviations on a measure of PTSD at multiple time points were published or provided by authors).
Data Extraction
All articles were coded independently by at least two coders. Discrepancies were resolved by group discussion.
Effect sizes.
For studies that reported proportions, we coded the n with PTSD, the proportion with PTSD, and the sample size (N) on which this proportion was based. When N was not reported for a time point, we carried forward the last available N from a prior time point, and calculated n based on the reported proportion with PTSD at that time point.1 Consistent with recommendations for meta-analyses of single proportions (Schwarzer et al., 2019), arcsine square root transformations were used for analyses to normalize and stabilize sampling distributions. Transformed proportions were back-transformed to percentages (range: 0 to 100) for presentation of model-predicted values using the formula (sin(transformed proportion))2 *100.
For studies that reported means, we recorded the mean and its associated standard deviation, the scale minimum and scale maximum, and the sample size on which the mean was based (or the last available N from a prior time point). We rescaled all means to a 0 to 1 scale using the formula: Mrescaled = (Mraw - scale minimum)/(scale maximum - scale minimum). Rescaled variance was calculated as vrescaled = SDraw2/(n(scale maximum - scale minimum)2). We multiplied model-predicted mean scores by 100% when presenting month-by-month point estimates to represent a percent of maximum severity.
Time since assault.
Each assessment time point was coded in units of months since assault. When assessment time points were reported in the source in a unit smaller than months (i.e., hours, days, or weeks), we transformed into a ratio variable representing months since assault. For assessments that were stated to be performed within a certain time frame (e.g., within one month of the assault), we took the midpoint of that time frame.
Descriptive variables.
With regard to study methods, we coded the type of source (e.g., peer-reviewed journal article, dissertation) in which the study was made publicly available, even when unpublished data were obtained, the country of data collection, the site from which the majority (at least 67%) of participants were recruited, the name of the PTSD measure, whether PTSD point prevalence was determined by a cut score or meeting Diagnostic Statistical Manual of Mental Disorders (DSM) diagnostic criteria (e.g., based on the number of symptoms in clusters B, C, and D in the DSM-IV; APA, 2000), the DSM version on which the PTSD measure was based, and whether an interview or self-report measure was used to assess PTSD. The following sample characteristics were coded: the percent of participants who were women, participant mean age, the majority (>67%) racial composition of samples in the United States, and the percent of participants with a prior history of sexual assault. With regard to characteristics of the index assault, we coded the percent of participants presenting with assaults involving alcohol/drug use by the survivor, weapon use by the perpetrator, physical injury, a stranger perpetrator (i.e., unknown to the survivor), and a police report. Finally, attrition was calculated as the percent reduction in sample size at each follow-up time point relative to the N at baseline. Attrition was not coded for two samples that presented outcomes only for the subsample of individuals who completed all study visits and one sample that enrolled participants in an ongoing manner after baseline.
Study quality.
Methodological quality of studies was rated using a 9-item adapted version of the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (National Heart, Lung, and Blood Institute, 2014; see Appendix A).
Analyses
Analyses were conducted in R version 3.6.3 (R Core Team, 2020). We employed a multilevel modeling approach to the meta-analysis using the package metafor (Viechtbauer, 2010). All models used inverse-variance weights, which is a strategy to give more weight to more precise effect sizes (e.g., those obtained from larger studies). We first undertook a process of comparing models to select the most appropriate models. The method used to compute the values for the parameters in these models (e.g., summary estimates and variances) was maximum likelihood estimation, which maximizes the likelihood that the model parameters could have generated the observed data (i.e., the effect sizes obtained from studies included in the analysis). We selected models by comparing their fit statistics (e.g.,−2 log likelihood, information criteria) against each other and selecting the best-fitting model. The method used to compute the values for the parameters in our final models was restricted maximum likelihood estimation, which is a variant of maximum likelihood estimation that reduces the risk of bias that can arise with small sample sizes.
Results
Descriptive Statistics
A total of 22 unique samples representing 2,106 participants met eligibility criteria and were included in analyses (see Table 1 for full sample characteristics; the full dataset and corresponding syntax and output are available in Appendices B & C, respectively). The majority (19 samples) were published in peer-reviewed journal articles, 2 samples were only represented in dissertations, and 1 sample was only reported in a government-funded report. Across these samples, 75 effects were computed for PTSD diagnostic point prevalence (including 26 unpublished effects) from 20 samples, and 57 effects were computed for average symptom severity (including 42 unpublished effects) from 17 samples.
Table 1:
Characteristics of Samples Included in Meta-Analysis
| Source | Country | Na | Recruitment Siteb | Time Post-Assaultc | PTSD Assessment | Quality Ratingd |
|---|---|---|---|---|---|---|
| Armour et al. (2012), Hansen et al. (2017), Hyland et al. (2016) – Sample 1 | Denmark | 355 | Hospital | 3, 6, & 12 months | HTQ | 44 |
| Darves-Bornoz et al. (1998) | France | 67 | Hospital | 1, 3, 6, & 12 months | Structured interview | 78 |
| Foa & Riggs (1995) – Study 2, Gilboa-Schectman & Foa (2001) – Study 2 (sexual assault group) | US | 57 | Hospital | within 2 weeks; 4 & 12 weeks; 6 months | PSS-I | 43 |
| Frazier (1988) - Sample 1 (diagnostic assessment) | US | 184 | Hospital | 3 days; 3 & 6 weeks; 3 & 6 months; 1 year | Study-specific checklist | 25 |
| eFrazier (1988) - Sample 2 (clinical assessment) | US | 253 | Hospital | 3 & 7 days; 3 & 6 weeks; 3, 6, & 12 months | Study-specific checklist | 14 |
| Frazier (2000) - Study 3 | US | 69 | Hospital | 1 week; 1, 3, 6, 9, & 12 months | Study-specific checklist | 25 |
| Frazier et al. (2001) | US | 97 | Hospital | 2 weeks; 2 & 6 months, 1 year | Study-specific checklist | 44 |
| fGilmore et al. (2019a, 2019b), Walsh et al. (2017) (control condition) | US | 52 | Hospital | 1.5, 3, & 6 months | PDS | 67 |
| f Gutner et al. (2006) | US | 121 | Mixed | within 1 month, 3 months | CAPS | 75 |
| fKaysen et al. (2010, 2011) | US | 24 | Community | within 2-5 weeks; 3 & 6 months | CAPS | 75 |
| f Khadr et al. (2018) | England | 135 | Rape crisis center | within 6 weeks, 4-5 months | CRIES-13 | 67 |
| f Koss & Figueredo (2004) | US | 59 | Mixed | within 3 months, 6 & 12 months | PDS | 56 |
| f Machado et al. (2011) | Brazil | 67 | Hospital | within 1 month, 6 months | CAPS | 75 |
| Mathews et al. (2013) | South Africa | 31 | Rape crisis center | 4, 8-12, & 16-20 weeks | Child PTSD Checklist | 67 |
| fMiller et al. (2015) (control condition) | US | 71 | Hospital | within 72 hours, 1 week, 2 months | PSS-SR | 50 |
| Nickerson et al. (2013), Steenkamp et al. (2012) | US | 126 | Community | 1, 2, 3, & 4 months | PCL-C | 50 |
| f Quidé et al. (2018) | France | 27 | Mixed | within 1 month, 6 months | CAPS | 63 |
| f Resick (1988) | US | 68 | Police | 1, 3, 6, & 12 months | IES | 22 |
|
fResnick et al. (2007a, 2007b) (control condition) |
US | 91 | Hospital | within 3 months, 3-6 & 6+ months | PSS-SR | 67 |
|
Rothbaum et al. (1992)
|
US | 64 | Hospital | 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, & 12 weeks |
Assault Reactions Weekly Interview | 38 |
| fRothbaum et al. (2012) (sexual assault group within control condition) | US | 13 | Hospital | 4 & 12 weeks | PSS-I | 56 |
| Ulirsch et al. (2013) | US | 75 | Hospital | 6 weeks, 3 months | PSS-I | 56 |
Note. PTSD = posttraumatic stress disorder; US = United States; CRIES-13 = Child Revised Impact of Events Scale; CAPS = Clinician-Administered PTSD Scale; HTQ = Harvard Trauma Questionnaire; IES = Impact of Events Scale; PDS = Posttraumatic Diagnostic Scale; PSS-SR = Posttraumatic Symptom Scale-Self-Report version; PCL-C = PTSD Checklist-Civilian; PSS-I = PTSD Symptom Scale – Interview Version.
N reported for the PTSD assessment generating effect sizes with the most participants.
The site from which the majority (>67%) of participants were recruited, including hospitals (including forensic nursing programs), rape crisis centers (i.e., any non-hospital-based victim assistance agency), police, general community, or mixed (i.e., no majority site).
Timepoints listed reflect those from which effect sizes were drawn and are described in the terms used in published articles; precise time periods were estimated for analyses as described in the methods.
Range: 0-100; higher scores indicate higher methodological quality and lower risk of bias.
Frazier (1988) presents means data for both samples separately and proportions data for the combined samples.
Unpublished data sent from authors were used for some or all effect sizes.
Study quality.
As indicated in Table 1, study quality ratings ranged from 14 to 78 on a 0-100 scale (M = 52.59, SD = 18.95; higher ratings indicate superior quality). Common issues with study quality (Appendix A) were participation-related issues (low participation rates, attrition, lack of sample size justification or power description) and lack of standardized measures.
Study methods.
Most samples (72.7%; n = 16) were recruited in the U.S. The most common recruitment site (for 63.6% of samples; n = 14) was a hospital, including hospital-based sexual assault services (e.g., during a sexual assault medical forensic exam); other recruitment sites were the general community (n = 2), rape crisis centers and other non-hospital-based victim assistance agencies (n = 2), the police (n = 1), or multiple sites (n = 3). PTSD was assessed by interview in 14 samples and self-report in 8 samples. All PTSD assessments were based on the DSM-IV-TR or earlier (DSM-III2: n = 4; DSM-III-R: n = 4; DSM-IV or DSM-IV-TR: n = 14). Of the 20 samples with PTSD diagnostic point prevalence reported, this was based only on cut scores in 2 samples, and only on diagnostic criteria in 17 samples; one additional sample provided separate frequencies for PTSD point prevalence according to both scoring approaches.
Sample and assault characteristics.
Race/ethnic composition was coded for U.S. samples only. Among the 15 U.S. samples with information about racial/ethnic composition, 40.0% (n = 6) were at least two-thirds majority White, 20.0% (n = 3) were at least two-thirds majority African American, and the remaining 40.0% (n = 6) had no majority race or ethnic group. Sample average age ranged from 13.5 to 35.6 (M = 26.6; SD = 5.4). Additionally, 81.0% (n = 17) of samples consisted exclusively of participants who identified as women. Information about proportion of the sample who had a history of sexual assault prior to the recent sexual assault was available for 9 samples and ranged from 10.3% to 76.9% (M = 43.7%, SD = 19.2%).
Sample-level characteristics of the index sexual assault were coded when available. On average, across samples with relevant information reported, the sexual assault occurred while the survivor was under the influence of drugs or alcohol in 39.7% of cases (SD = 14.7%; based on n = 7 samples). The sexual assault was perpetrated by a stranger in 41.2% of cases (SD = 17.2%; based on n = 13 samples). Additionally, the sexual assault involved a weapon in 25.7% of cases (SD = 13.9%; based on n = 5 samples), and the sexual assault resulted in physical injury for 63.6% of survivors (SD = 18.2%; based on n = 7 samples). Finally, 76.1% of participants made a police report for the sexual assault (SD = 31.8%; based on n = 6 samples).
Publication Bias
We examined publication bias in two ways. First, we compared published to unpublished effects at 1, 3, and 6 months post-assault (due to low numbers of effects at other months) using t-tests and identified no significant differences in point prevalence or average symptom severity. Second, we removed unpublished effects from the dataset and examined funnel plots for each month at which there were at least 10 published effects. Funnel plots are scatter plots in which the x-axis represents effect size magnitude, and the y-axis represents an indicator of effect size precision (e.g., standard error), with the assumption that the most precise effect sizes (i.e., the peak of the funnel) will be closest to the “true” effect size. If the funnel is symmetrical, that means that effect sizes that are larger than the true effect size (i.e., to the right of the peak) are as likely to be published as effect sizes that are smaller than the true effect size (i.e., to the left of the peak). If publication bias is present, one would expect to see an asymmetrical plot, with fewer effect sizes present that are smaller than the true effect size. Using Egger’s regression test in a model with standard error as a predictor (Egger et al., 1997), we found no evidence for publication bias indicated by asymmetry in the funnel plots for point prevalence at 1 month, z = −0.48, p = .63, or 3 months, z = 1.06, p = .29 (Appendices D & E). Funnel plot asymmetry was not examined for severity because the majority of means were unpublished.
Modeling Change Over Time
A multilevel modeling approach was used to evaluate separate models for the two outcomes: point prevalence (i.e., proportion of the sample with a PTSD diagnosis) and average PTSD symptom severity. This was necessary because all studies contributed multiple effect sizes across time. Thus, effect sizes were nested in samples. Failing to use a multilevel model (i.e., using a “fixed effects” approach) would mean that every effect size would be treated independently, as if it came from a different sample, even though effect sizes obtained from the same sample should be more similar to each other than effect sizes obtained from different sample. In contrast, a multilevel model can include “random effects” to model variability between samples. For both point prevalence and symptom severity, likelihood ratio tests revealed that a multilevel (random-effects) model was superior to a fixed-effects model.
Further, we recognized that several studies assessed PTSD prevalence or severity in multiple ways, which meant that some studies reported multiple effect sizes even within a given time point. This could indicate the need to model a third level of nesting (i.e., effect sizes nested in time points nested in studies). We considered the need for a third level of nesting. However, likelihood ratio tests revealed that a third level did not improve model fit, likely because there were few samples with multiple assessment types. Thus, the 2-level random-effects model with effect sizes nested within samples was retained for both PTSD prevalence and severity models. All available data were retained in these models, including multiple effect sizes at a given time point when available.
We then examined the amount of heterogeneity present in the data. If there is substantial heterogeneity, this can indicate the need for moderator analyses to identify potential sources of the heterogeneity. As indicated by I2 (Higgins & Thompson, 2002) for the intercept-only multilevel model, 90.1% of the variance in PTSD point prevalence and 98.2% of the variance in PTSD symptom severity was due to differences across studies and across effect sizes within the same study (i.e., combined between- and within-group heterogeneity) rather than chance. This suggested that there was heterogeneity in the data that could potentially be accounted for by moderator analyses.
Next, we considered various approaches to model the course of symptom changes over time. First, we considered modeling linear change, which would indicate that average symptoms changed at a constant rate over time, and quadratic change, which would indicate that the average rate of symptom change itself changed over time. We did this by testing both linear and quadratic fixed effects for time (operationalized as the number of months since assault). For both point prevalence and symptom severity, likelihood ratio tests revealed that a model containing a quadratic term was a superior fit to a model containing only a linear term. This suggested that the rate of change in average symptoms over time was not linear; instead, the rate of change itself changed over time.
Given this evidence for a change over time in the rate of average symptom change, we investigated whether there was a particular point in time at which the trajectory of symptoms changed. To do this, we evaluated linear-linear piecewise models, where symptom change over time was modeled as two lines connected by an elbow, or “knot,” which could be placed at various points in time. Drawing on algorithmic approaches to detect unknown knots (e.g., Marcoulides, 2018), we specified model parameters to test in advance. First, based on theoretical conceptualizations of PTSD suggesting symptoms decrease substantially in the months following assault and stabilize thereafter (Monson & Friedman, 2006), we decided to consider at most one knot. Second, for ease of conceptual interpretation, we only considered knots at the monthly level (i.e., integer time values). Third, because there were few samples with multiple assessments after 6 months, and because prior studies suggested that decreases happen prior to 6 months post-trauma (Hiller et al., 2016; Santiago et al., 2013), we only considered knots up to 6 months. Thus, there were seven potential models to consider, including a model with no knots, as well as models with knots at 1, 2, 3, 4, 5, and 6 months. We compared the fit of these models to the data using fit indices appropriate for non-nested models, Akaike Information Criteria (AIC; Akaike, 1974) and Bayesian Information Criteria (BIC; Raftery, 1995), where lower values represented better fit.
As seen in Appendix F, model fit statistics indicated that a knot at 3-months post sexual assault fit the data best, for both PTSD point prevalence and symptom severity. These models suggested that, on average, both PTSD point prevalence and symptom severity declined most rapidly within the first 3 months after a sexual assault, and continued to decline, but at a slower average rate, in months 3 through 12. All subsequent analyses used models with knots at 3-months post sexual assault.
Month-by-Month Estimates of Point Prevalence and Symptom Severity
Based on the model with a knot at 3 months, model-predicted estimates of PTSD point prevalence and average symptom severity were computed at each time point3 (Table 2). With regard to the percent meeting PTSD diagnostic criteria, point prevalence decreased from 74.58% at 1 month post-assault to 41.49% at 12 months post-assault. Mean symptom severity reduced from 47.94% of maximum severity on average at 1 month post-assault to 29.91% at 12 months post-assault. Model-predicted estimates for PTSD point prevalence and mean symptom severity can be viewed alongside sample-level data in Figures 1 and 2, respectively.
Table 2:
Model-Implied Estimates at Each Month Post-Assault
| Time since assault | Proportion with PTSD % (95% CI) | PTSD symptom severity % of maximum (95% CI) |
|
| ||
| 1 weeka | 81.42 (74.49, 87.47) | 52.68 (45.95, 59.42) |
| 2 weeksa | 79.23 (72.14, 85.51) | 51.10 (44.39, 57.81) |
| 3 weeksa | 76.94 (69.71, 83.45) | 49.52 (42.83, 56.21) |
| 1 month | 74.58 (67.21, 81.29) | 47.94 (41.27, 54.61) |
| 2 months | 64.44 (56.58, 71.92) | 41.61 (34.96, 48.26) |
| 3 months | 53.60 (45.31, 61.78) | 35.28 (28.58, 41.97) |
| 4 months | 52.25 (44.06, 60.37) | 34.68 (28.00, 41.37) |
| 5 months | 50.90 (42.76, 59.01) | 34.09 (27.41, 40.76) |
| 6 months | 49.55 (41.40, 57.70) | 33.49 (26.81, 40.17) |
| 9 months | 45.50 (37.04, 54.09) | 31.70 (24.98, 38.42) |
| 12 months | 41.49 (32.36, 50.92) | 29.91 (23.10, 36.73) |
Note. PTSD = posttraumatic stress disorder, CI = confidence interval.
Represents the presence of posttraumatic stress symptoms before the 1-month duration criterion required for a diagnosis of PTSD has been met.
Figure 1: PTSD Point Prevalence by Sample and Overall (color version available in Appendix I).
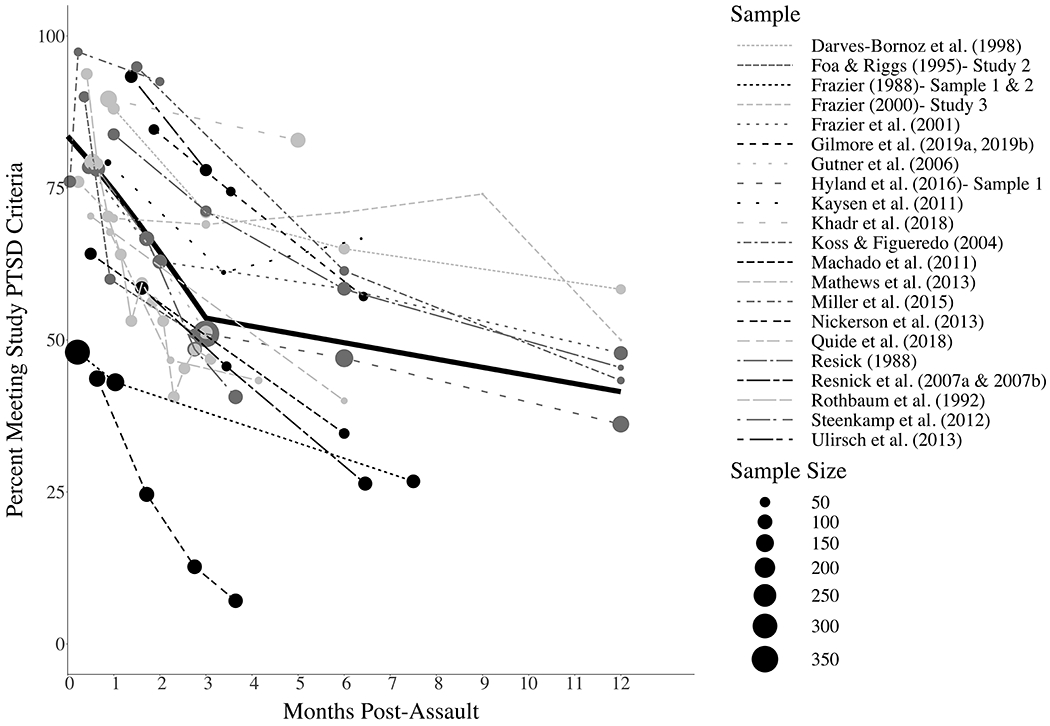
Note: The solid black line represents the overall (i.e., model-predicted) estimates of PTSD point prevalence. A 95% confidence interval for these estimates is additionally presented in the color version of this figure (Appendix I).
Figure 2: PTSD Mean Severity by Sample and Overall (color version available in Appendix J).
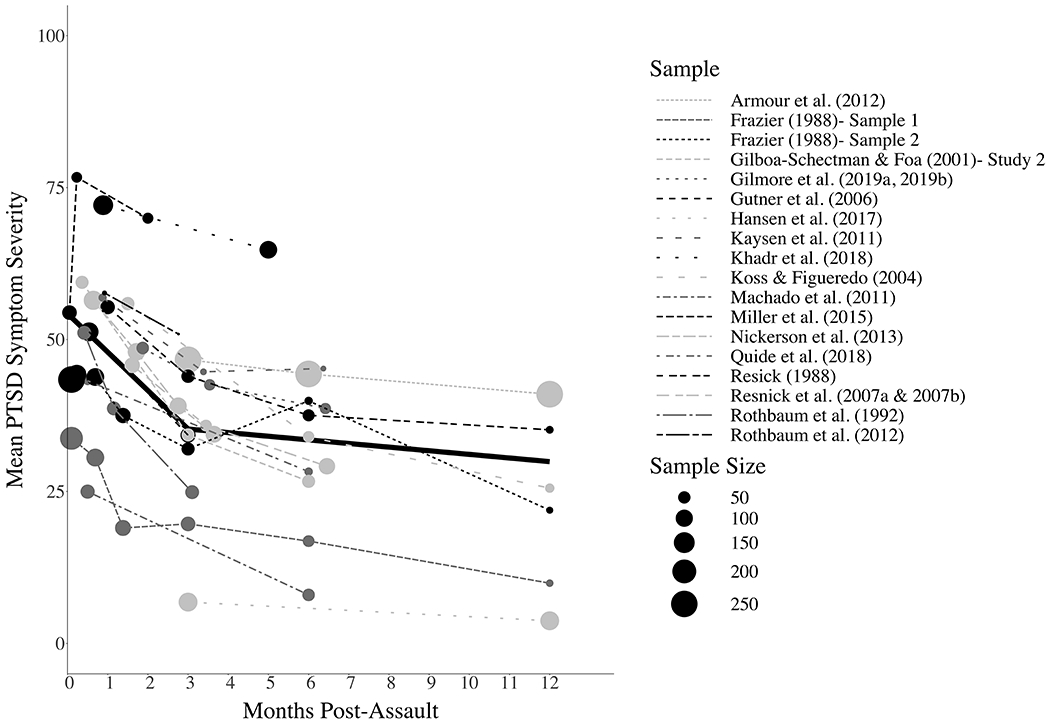
Note: The solid black line represents the overall (i.e., model-predicted) estimates of average PTSD symptom severity. A 95% confidence interval for these estimates is additionally presented in the color version of this figure (Appendix J).
The Effects of Attrition on Point Prevalence
As described above, the percent of the sample that dropped out at follow-up assessments relative to the study’s baseline was computed for each effect size. Attrition varied over time within a given sample. Across the 19 samples (for effects which were not limited to completers and did not allow for ongoing enrollment) and all post-baseline timepoints, maximum attrition ranged from 3.23% to 92.49% (M = 45.50%, SD = 26.54%), with greater maximum attrition at later follow-ups, r = .44, p < .001. The average attrition was 33.73% for follow-ups that occurred within the first 6 months post-assault and 54.58% for follow-ups that occurred in months 6-12.
The month-by-month estimates of PTSD point prevalence presented in the prior section were based on calculations assuming that people with PTSD were no more or less likely to drop out of a given study between observations (henceforth, the standard assumption). Correlations were not statistically significant between baseline point prevalence and attrition rates at 3 months, r = −0.33, p = .35, and 6 months, r = −0.18, p = .62, and between baseline symptom severity and attrition rates at 3 months, r = −0.25, p = .48, and 6 months, r = −0.29, p = .38. However, given that these analyses likely had low power to detect statistical significance and effect sizes were in the medium range, we next tested the degree to which these findings are robust to violations of the standard assumption.
We recalculated model-implied effects in the models with knots at 3 months post-assault under two alternative assumptions, similar to the approach used by Hiller and colleagues (2016). First, we tested the assumption that survivors with PTSD would be less likely to be lost to follow-up (alternative assumption 1). To calculate point prevalence under this assumption, we divided the n with PTSD at a given observation by the total sample size (N) at the first observation, which treats all dropouts as if they did not have PTSD. Second, we tested the assumption that survivors with PTSD would be more likely to be lost to follow-up (alternative assumption 2). To calculate point prevalence under this assumption, we added the number of people who dropped out by a given observation to the n with PTSD at that observation, up to n with PTSD at the baseline observation, and divided this figure by the total sample size (N) at the first observation. We did not allow the numerator to surpass the n with PTSD at the baseline observation given evidence that it is unlikely for the prevalence of PTSD to increase over time (Galatzer-Levy et al., 2018; Smid et al., 2009). Data from three studies involving completer analyses and two studies that enrolled new participants post-baseline were included uncorrected in these analyses to maximize comparability to the original analysis. Appendix G includes results under each of the three assumptions. Confidence intervals overlapped for the standard assumption and each of the two alternative assumptions through month 5, but confidence intervals were non-overlapping for alternative assumption 1 at month 6, and both alternative assumptions at months 9 and 12. This indicates that point prevalence estimates for months 0-5 are robust to violations of the assumption that attrition is unbiased by PTSD, but later estimates should be interpreted with caution.
Moderator Analyses
In unconditional models with knots at 3 months tested using the standard attrition assumption, significant residual heterogeneity was observed in both the point prevalence model, QE(72)= 892.03, p < .0001, and the mean severity model, QE(54)= 3156.43, p < .0001, suggesting the presence of heterogeneity that could potentially be explained by moderators. Because moderation models would test differences in pre- and post-3-month slopes at each level of the moderator, we only considered moderators for which we had data at each level of the moderator from at least 3 samples both before and after 3 months post-assault in both mean and point prevalence models. Results are presented in Table 3. We used a Bonferroni-corrected p value of .004 to interpret the significance of effects in these models. In all, no moderator reduced heterogeneity to non-significance.
Table 3:
Moderator Analysis
| Moderator | Number of samples | Number of effects | Main Effect of Pre-3 Month Slope | Main Effect of Post-3 Month Slope | Main Effect of Moderator: Estimate (SE) | Moderator * Pre-3 Month Slope: Estimate (SE) | Moderator * Post-3 Month Slope: Estimate (SE) | Residual Heterogeneity: QE |
|---|---|---|---|---|---|---|---|---|
| Point prevalence model | ||||||||
| None (unconditional model) | 19 | 75 | −0.111 (0.008) * | −0.014 (0.004) * | -- | -- | -- | 892.03 * |
| Study quality (mean-centered) | 19 | 72 | −0.117 (0.009) * | −0.016 (0.003) * | 0.001 (0.001) | 0.000 (0.001) | 0.000 (0.000) | 704.03 * |
| PTSD assessment method | 19 | 75 | −0.124 (0.012) * | −0.013 (0.007) | 857.26 * | |||
| Interview | 11 | 42 | -- | -- | -- | -- | -- | |
| Self-report (vs. interview) | 8 | 33 | -- | -- | −0.075 (0.091) | 0.028 (0.017) | −0.001 (0.008) | |
| PTSD diagnosis determination | 19 | 75 | −0.112 (0.009) * | −0.013 (0.004) * | 819.43 * | |||
| Diagnostic criteria | 16 | 65 | -- | -- | -- | -- | -- | |
| Cut score (vs. diagnostic criteria) | 3 | 10 | -- | -- | 0.120 (0.122) | 0.007 (0.022) | −0.005 (0.013) | |
| Country | 19 | 75 | −0.081 (0.019) * | −0.017 (0.005) * | 847.36 * | |||
| Non-US | 6 | 16 | -- | -- | -- | -- | -- | |
| US (vs. non-US) | 13 | 59 | -- | -- | 0.059 (0.102) | −0.038 (0.021) | 0.005 (0.007) | |
| Mean age (mean-centered) | 17 | 69 | −0.104 (0.009) * | −0.014 (0.004) * | 0.004 (0.009) | −0.006 (0.002) * | 0.000 (0.001) | 740.16 * |
| Percent women (mean-centered) | 18 | 69 | −0.116 (0.009) * | −0.014 (0.004) * | −0.010 (0.014) | −0.003 (0.003) | 0.000 (0.001) | 783.78 * |
| Percent stranger perpetrators (mean-centered) | 11 | 42 | −0.103 (0.011) * | −0.013 (0.005) | −0.004 (0.004) | 0.001 (0.001) | 0.001 (0.001) | 660.79 * |
| Mean severity model | ||||||||
| None (unconditional model) | 17 | 57 | −0.063 (0.004) * | −0.006 (0.001) * | -- | -- | -- | 3156.43 * |
| Study quality (mean-centered) | 17 | 57 | −0.064 (0.004) * | −0.007 (0.002) * | 0.002 (0.002) | 0.000 (0.000) | 0.000 (0.000) | 2987.27 * |
| PTSD assessment method | 17 | 57 | −0.060 (0.005) * | −0.011 (0.002) * | 2686.38 * | |||
| Interview | 11 | 36 | -- | -- | -- | -- | -- | |
| Self-report (vs. interview) | 6 | 21 | -- | -- | 0.082 (0.070) | −0.001 (0.008) | 0.006 (0.003) | |
| Country | 17 | 57 | −0.052 (0.007) * | −0.004 (0.001) | 3037.65 * | |||
| Non-US | 4 | 11 | -- | -- | -- | -- | -- | |
| US (vs. non-US) | 13 | 46 | -- | -- | 0.094 (0.079) | −0.010 (0.008) | −0.007 (0.003) | |
| Mean age (mean-centered) | 15 | 51 | −0.060 (0.004) * | −0.013 (0.002) * | 0.005 (0.008) | −0.002 (0.001) | −0.002 (0.001) * | 2695.62 * |
| Percent women (mean-centered) | 17 | 57 | −0.059 (0.004) * | −0.005 (0.002) | −0.002 (0.005) | −0.002 (0.001) | −0.000 (0.001) | 2188.09 * |
| Percent stranger perpetrators (mean-centered) | 8 | 29 | −0.053 (0.005) * | −0.014 (0.003) * | −0.007 (0.003) | 0.000 (0.000) | 0.001 (0.000) | 778.87 * |
p < .004 (p value cutoff corrected for multiple tests)
Study quality.
There were no statistically significant main or interaction effects for study quality in either model.
Study methods.
There were no statistically significant main or interaction effects for PTSD assessment method (interview vs. self-report) or study country in either model. The method used to determine whether participants met study criteria for PTSD was tested in the point prevalence model only (given that study criteria for determining PTSD diagnosis are irrelevant in estimates of severity), and no significant main or interaction effects were identified.
Sample and assault characteristics.
Mean age significantly moderated the pre-3-month trajectory in the point prevalence model, such that point prevalence decreased more quickly from 0 to 3 months among older samples. Age also moderated the post-3-month trajectory in the mean severity model, such that mean severity decreased more quickly from 3 to 12 months among older samples. See Appendix H for interaction plots. There were no main or interaction effects for gender or the percent of participants assaulted by a stranger in either model.
Discussion
Sexual assault is prevalent (Black et al., 2011; Breiding et al., 2014; Smith et al., 2018) and debilitating (Dworkin et al., 2017). Sexual assault is associated with higher rates of PTSD than other traumas (Brewin et al., 2000; Dworkin, 2020; Kessler et al., 2014; Kilpatrick et al., 2003) and there is evidence that the course of PTSD differs by trauma type (Santiago et al., 2013). However, the unique course of PTSD onset and recovery after sexual assault specifically had not been summarized prior to this study. This was the first known meta-analysis to summarize the month-by-month point prevalence and symptom severity of PTSD, and test the timing of changes in average recovery rates, during the year after sexual assault. The current meta-analysis aggregated studies not previously reviewed, as past meta-analyses of post-trauma trajectories (Hiller et al., 2016; Qi et al., 2018) did not include any of the sexual assault-specific samples included in the current analysis. These findings on the unique course of PTSD onset and recovery after sexual assault specifically provide novel information that can be applied to improve prevention and intervention efforts for a vulnerable group of trauma survivors.
Point Prevalence and Severity of PTSD Following Sexual Assault
Our findings underscore prior findings that PTSD is common and severe in the immediate aftermath of sexual assault, but strengthen this assertion by representing prospective studies. Specifically, at one month after a sexual assault, a majority (74.58%) met criteria for PTSD, and at the twelfth month, two out of five individuals (41.49%) met criteria. Mean symptom severity was 47.94 out of 100 at one month post-assault and 29.91 out of 100 at 12 months post-assault. Although assessments of PTSD included in this analysis reflect DSM-IV-TR and earlier, to assist with interpretation of these findings, we calculated comparable scores on the Clinician-Administered Posttraumatic Stress Disorder Scale (CAPS-5; Weathers et al., 2018) and the PTSD Checklist (PCL-5; Blevins et al., 2015), which has a recommended clinical cutoff of 31 to 33 (Bovin et al., 2016). Both scales range from 0 to 80. With acknowledgment that this comparison is not exact given changes to DSM diagnostic criteria, average symptom severity scores identified in this analysis were comparable to a CAPS-5 or PCL-5 score of 38.35 at 1 month, 28.22 at 3 months, and 23.93 at 12 months.
PTSD prevalence was high. For example, the 12-month prevalence of 41.49% identified in this prospective meta-analysis—which is the lowest rate observed in the year post-assault—is still higher than the lifetime prevalence of PTSD (36.2%, 95% CI: 31.4%-41.1%) identified in a prior retrospective meta-analysis on this topic (Dworkin, 2020). One would expect the true lifetime prevalence of PTSD in sexual assault survivors to be higher than the prevalence at 12 months post-assault, given that the 12-month prevalence rate focuses on a shorter timeframe, does not capture PTSD with onset more than one year after the assault (though rare; Galatzer-Levy et al., 2018; Smid et al., 2009), and is linked to a specific sexual assault (whereas lifetime prevalence can be linked to any sexual assault or other past traumatic event). Yet, PTSD prevalence rates were higher in the current prospective meta-analysis compared to the Dworkin (2020) retrospective meta-analysis. One potential explanation for this unexpected finding is that the prevalence of PTSD obtained in the prior meta-analysis may be an underestimate due to retrospective reporting biases (e.g., recall failure). Indeed, lifetime prevalence estimates have been critiqued (Streiner et al., 2009) and one study found that the prevalence of common mental disorders obtained from prospective studies was double the prevalence obtained from retrospective studies (Moffitt et al., 2010). Therefore, although prevalence estimates in the current prospective meta-analysis are high, they may be more accurate than retrospectively assessed lifetime prevalence rates. An alternate explanation is differences in sample selection. Specifically, the prospective studies included in the current analysis largely consisted of help-seeking samples, whereas the retrospective studies included in the prior meta-analysis included more college and community-recruited samples. Survivors seeking help might be in more distress, might have more risk factors for the development of PTSD (e.g., greater life threat associated with the assault, fewer social resources; Ozer et al., 2003), or may be subject to additional stressors related to engagement with the criminal justice system.
The rates of PTSD identified in the current study are also much higher than in prior meta-analyses that reflected multiple types of trauma (none of which included any studies reviewed here). For example, in the first month post-trauma, PTSD prevalence was 74.58% following sexual assault in the current analysis. In prior meta-analyses, one-month PTSD prevalence was 28.8% following mixed trauma exposure (Santiago et al., 2013) and 21.3% following childhood trauma (Hiller et al., 2016). PTSD prevalence at the twelfth month post-trauma was 41.5% following sexual assault in this study, as compared to prior meta-analyses, which found 17.0% following mixed trauma exposure (Santiago et al., 2013) and 10.9% following childhood trauma (Hiller et al., 2016). Thus, although the present work did not directly compare the rates and severity of PTSD following sexual assault to that of other trauma types, these comparisons of our findings to prior meta-analyses indirectly corroborate extant literature suggesting sexual assault may be associated with greater prevalence and symptom severity of PTSD relative to other forms of trauma (Brewin et al., 2000; Dworkin, 2020; Kessler et al., 2014; Kilpatrick et al., 2003).
There are several reasons why high rates of PTSD might be observed following sexual assault. First, it is possible that societal stigma and myths related to sexual assault contribute to the development of cognitive changes in survivors that are more substantial or inflexible than those following other forms of trauma. Specifically, cognitive theories of PTSD posit that, following any form of trauma, survivors often develop negative and unhelpful beliefs regarding the trauma itself (e.g., self-blame), oneself (e.g., “I am permanently damaged”), others (e.g., “others cannot be trusted”), and the world (e.g., “the world is totally unsafe”) that prevent natural resolution of PTSD symptoms (Ehlers & Clark, 2000; Janoff-Bulman, 1992; Resick et al., 2017). Commonly-held societal myths about sexual assault (e.g., victim blame; Kennedy & Prock, 2018; Lebowitz & Roth, 1994) may contribute to the development of these negative beliefs following sexual assault (Dworkin & Weaver, in press), which may create greater obstructions to PTSD recovery. Second, when survivors disclose sexual assault to others, they may be more likely to receive negative social reactions than survivors of non-stigmatized traumas (Kennedy & Prock, 2018). Meta-analytic findings indicate that these negative social reactions are cross-sectionally and prospectively associated with PTSD symptom severity (Dworkin et al., 2019). Third, sexual assault is more likely than other traumas to produce specific emotional reactions, such as anger, guilt, and shame (Amstadter & Vernon, 2008), which may theoretically obstruct PTSD recovery by inhibiting processing of other emotions that naturally occur in response to trauma (e.g., fear, sadness; Resick et al., 2017). Fourth, sexual assault—unlike many other forms of trauma— occurs primarily to women, who are more likely to develop PTSD following trauma (Tolin & Foa, 2006). Some research suggests that higher rates of PTSD in women are not accounted for by the higher likelihood of sexual assault, but rather by the presence of psychological risk factors for the development of PTSD in the wake of trauma that are more common among women (e.g., pre-existing depression or anxiety) (Breslau, 2009; Tolin & Foa, 2006). In addition, risk factors in women’s sociocultural contexts (e.g., sexism) may increase their risk for the development of post-trauma psychopathology (Dworkin & Weaver, in press). Given that most of the samples (81%) in this study exclusively consisted of women, it is possible that risk factors that differ by gender, rather than sexual assault specifically, contributed to the high rates of PTSD observed in this meta-analysis. Additional literature reviews with greater representation of men and gender minorities are required to fully understand differential symptom trajectories by trauma type and gender.
Trajectory of PTSD Recovery Following Sexual Assault
Our findings also corroborate the extant theoretical and empirical literature by suggesting the majority of PTSD recovery occurs within the first few months following sexual assault, after which point the average rate of recovery slows. These findings are consistent with a past review of mixed traumas which indicated that the prevalence of PTSD stabilizes after three months exposure (Santiago et al., 2013). Similarly, Hiller and colleagues’ (2016) meta-analysis of mixed trauma in youth suggested that PTSD symptom severity plateaued after three months, although the prevalence of PTSD stabilized at approximately six months. Thus, although sexual assault is associated with a particularly high point prevalence and severity of PTSD, the timing of recovery for adolescents and adults appears to be comparable to that of other traumas.
Of note, observed trajectories of symptom recovery could only be assessed for participants who completed longitudinal assessments. Samples varied widely in their maximum attrition, with an average of 45.5% of sexual assault survivors not returning for a follow-up assessment across timepoints, highlighting the difficulties of retaining participants in the early aftermath of sexual assault. This rate is higher than Qi and colleagues’ (2018) meta-analysis of PTSD in the 4 to 36 months after acute hospitalization (average attrition of 13%), where the most frequently represented traumatic event was a motor vehicle collision. It is possible that the stigmatized nature of sexual assault relative to other forms of trauma (Kennedy & Prock, 2018) may make it more difficult to retain these survivors in assault-related research.
We found no evidence that attrition rates were significantly associated with baseline PTSD in a given sample. Additionally, sensitivity analyses indicated that, even if individual-level attrition differed as a function of PTSD status, estimates for the first six months post-trauma were unlikely to be substantially changed, but later estimates may be affected. We considered possibilities at both extremes – that either all or no participants with missing follow-up data had PTSD. Although neither extreme assumption is likely to be true, and the subset of individuals who dropout is likely to be comprised of people both with and without PTSD, our sensitivity analyses focused on these extremes to give a range of possibilities. We can further narrow in on the possibilities that appear most likely by interpreting our results in the context of prior work. For example, assuming that all dropouts had PTSD led to very high point prevalence estimates (64.07% and 65.41% at 9 and 12 months, respectively) that are unlikely to be accurate, especially in light of cross-sectional studies that show 12-25% of survivors meet criteria for current PTSD at any given time (Kilpatrick et al., 2007; Resnick et al., 1993; Zinzow et al., 2012). Instead, true point prevalence estimates may be closer to those estimates obtained under the assumption that no dropouts had PTSD, which would be consistent with prior meta-analytic results revealing individuals with lower baseline PTSD scores were more likely to drop out of prospective post-trauma studies (Shalev et al., 2019). It is also notable that all correlations that we obtained for the association between baseline PTSD and attrition were negative. Although these bivariate tests were based on a small number of samples and thus were likely underpowered to detect statistical significance, this implies that it is possible that samples with higher baseline PTSD might have lower dropout. Thus, 9 months after a sexual assault, the point prevalence of PTSD is likely between 23.04% and 45.49%, and by 12 months, the point prevalence is likely between 14.75% and 41.49%.
Moderators of Trajectory of Recovery
In general, we found little evidence that characteristics of studies or samples variables moderated the average rate of recovery. Only age was a significant moderator, such that samples that were older on average tended to evidence quicker recovery. Although prior research on risk of PTSD in relation to age has been somewhat mixed, there is some evidence from cross-sectional studies that younger individuals have higher risk of PTSD (Brewin et al., 2000; Kessler et al., 2017), as one would expect to see for a group that recovers more slowly. In addition, in the only prospective study to our knowledge that examined age in relation to PTSD outcomes, a study of hospitalized trauma survivors found that younger patients were more likely to have PTSD at 3 months post trauma (Powers et al., 2014), suggesting that—consistent with the current study—younger individuals may have a slower average rate of recovery. When understanding this finding, it is important to note that, in general, samples included in this meta-analysis consisted mostly of adolescents and young adults; indeed, the maximum average age was 35.6 years. Younger sexual assault survivors may have fewer coping skills that could promote their resilience, or may be more likely to disclose to parents, who tend to offer more negative reactions to disclosure than other types of confidants (Reitsema & Grietens, 2016). It is possible that differences in the types of assaults experienced by younger samples (i.e., ongoing child sexual abuse) could account for differences in average rates of recovery, but this possibility has not been tested empirically. Future prospective research should test these possibilities, and also explore average rates of recovery among older adults, who also evidence high risk of PTSD following trauma exposure (Kessler et al., 2017) but are minimally reflected in the studies included in this analysis.
Strengths and Limitations
This was the first prospective meta-analysis to examine and clarify the course of recovery from sexual assault. Our inclusion of a substantial amount of unpublished data—representing 52% of the effects analyzed—addresses limitations of past meta-analyses in this area, helps to overcome publication biases that obstruct the dissemination of anomalous findings, and increases the representation of studies, sexual assaults, and survivors with varied characteristics. Additionally, our statistical evaluation of linear-linear piecewise models allowed us to empirically corroborate past work and common perceptions that PTSD recovery slows three months after a sexual assault. Finally, our examination of potential bias due to attrition increases confidence in study findings, and our tests of moderators help to contextualize results.
However, this study also had limitations. First, this meta-analysis used aggregate (rather than individual-level) data, which prohibits examination of distinct trajectories in recovery. Indeed, the point prevalence of PTSD at follow-up timepoints may comprise individuals who have not yet recovered from PTSD, individuals who experienced a new emergence of delayed-onset PTSD, or some combination of the two. Second, we were unable to test some relevant moderators that were unreported for many studies (e.g., percent seeking treatment, frequency of police reporting, weapon use in the assault, physical injury due to the assault, prior history of sexual assault). This is consistent with prior meta-analyses on related topics (e.g., Hiller et al., 2016), and reflects the relatively small number of studies and inconsistent reporting of key characteristics. As a result, it is unclear to what extent these characteristics of studies and samples affected observed results. Future studies should consistently report characteristics of their methods and samples, and use novel methodological approaches (e.g., recruitment at non-hospital sites) against which the current results can be compared. We also encourage future researchers to study whether comorbidities moderate average rates of PTSD recovery after sexual assault.
We identified several strengths of the body of research on which this analysis was based. In terms of strengths, the U.S.-based studies were relatively diverse in terms of race and ethnicity: most studies were not comprised primarily of White participants. In addition, although most studies were comprised exclusively of women, approximately a fifth of studies included survivors regardless of gender. This representation is especially important given that the intersection of racism, sexism, and other sociocultural systems of oppression may affect recovery from sexual assault (Bryant-Davis et al., 2009; Dworkin & Weaver, in press). Although we did not have sufficient data to test gender or race/ethnicity as moderators of PTSD symptom trajectories, future studies should explore this these factors as well as other aspects of diversity. It is possible that rates of recovery may differ as a function of survivors’ intersecting identities, and an individual patient meta-analysis could more effectively disentangle such patterns.
We also identified weaknesses of the primary studies used in this analysis. First, the majority of studies recruited individuals who were seeking some medical or rape crisis services following sexual assault, which may not be representative of survivors who specifically do not disclose their assaults to, or seek help from, healthcare providers, or who choose not to seek help at all. Non-help-seeking individuals may (a) recover at a more rapid rate than others, and therefore may not perceive a need to seek healthcare, or (b) experience much more severe forms of PTSD that prohibit adaptive help-seeking behavior. Future researchers are advised to study sexual assault recovery using recruitment methods that do not rely on individuals seeking some form of services in order to disentangle these effects. Second, there was substantial variation in the methods used to assess PTSD. In particular, studies varied in terms of whether they used DSM diagnostic criteria or cut scores to establish PTSD diagnoses, so the point prevalence at each month post-assault reflects a combination of these methods. The measures used to assess average PTSD symptom severity also varied between studies. We addressed this by transforming all measures to a common scale, but a rescaled score on different measures could have different meanings. We encourage the use of standardized PTSD measures, such as the CAPS-5 or PCL-5, in future work. Third, although not an inclusion criterion, all included samples assessed PTSD with criteria from DSM-IV-TR or earlier. Given that there is evidence that the prevalence of PTSD may change somewhat with DSM-5 criteria (Kilpatrick et al., 2013), this analysis is limited in the conclusions that can be drawn about the prevalence of PTSD using current DSM-5 criteria. Prospective studies using updated criteria are needed to address this gap.
Clinical Implications
Current findings offer important clinical implications. First, our findings suggest that PTSD is common and severe following sexual assault, which may help to normalize survivors’ distress following sexual assault. Second, our results suggest that on average, PTSD symptom severity continues to decline up to a year after a sexual assault. This suggests natural recovery is an ongoing process that may continue, however slowly, beyond the immediate aftermath of a trauma, and could be used by clinicians to combat negative attributions regarding symptoms (e.g., reduce beliefs such as “I will never feel better”; Ehlers & Clark, 2000).
Efforts to prevent PTSD in the aftermath of trauma exposure have long focused on the first three months post-trauma as a critical period for delivering interventions (Roberts et al., 2019). A recent meta-analysis indicates that certain such interventions (especially trauma-focused cognitive behavioral therapy) are effective at preventing PTSD (Roberts et al., 2019), and there is some evidence that these interventions are more effective at preventing PTSD after sexual assault as compared to other types of traumas (Rothbaum et al., 2012). Although the current results cannot not speak to the efficacy of early versus later intervention, they suggest that the first three months following sexual assault appear to be a period in which substantial symptom change is occurring, which could potentially increase malleability to intervention. Intervening in this period of time could change trauma-related thoughts and behaviors before they become habitual. Given prior research suggesting that societal stigma and negative social reactions may explain higher PTSD prevalence and severity after sexual assault versus other traumas (Dworkin et al., 2019; Kennedy & Prock, 2018), such interventions could potentially be more effective by explicitly attending to the societal context of sexual assault recovery.
In light of the finding that recovery may slow after three months following trauma exposure, providers of intensive treatments may consider adopting an approach of “watchful waiting” in the months following sexual assault in order to identify who may not quickly recover without subsequent clinical intervention and thus may be in need of more intensive services. Our provision of average scores on commonly used PTSD measures may help clinicians determine if their clients are experiencing more severe symptoms than typical at each month post-assault.
Conclusions and Directions for Future Research
In conclusion, this meta-analysis examined the point prevalence, severity, and trajectory of recovery from PTSD following sexual assault. Findings suggested that PTSD is common and severe following sexual assault, and the average rate of recovery slows (but continues) after three months. Building on the present work, future researchers are advised to prospectively study sexual assault recovery in survivors who are not actively seeking help in order to identify whether their PTSD prevalence, severity, and average recovery rates differ between survivors who do and do not seek services. To further disentangle unique trajectories following sexual assault, an individual patient meta-analysis drawing on archived data is recommended.
Supplementary Material
Summary Tables.
Critical Findings
One month after a sexual assault, 75% of survivors met criteria for PTSD. Twelve months after sexual assault, 41% of survivors met criteria for PTSD.
The majority of PTSD recovery occurs within the first three months following sexual assault, after which point the average rate of recovery slows.
Implications for Practice, Policy, & Research
Future prospective studies should examine recovery trajectories among survivors who are not seeking help, and explore the role of intersecting social identities (e.g., race, gender) in post-assault outcomes.
Many survivors will recover without intervention within 3 months of assault, suggesting that low-burden interventions may be more appropriate than resource-intensive treatments for survivors presenting for services immediately after assault.
Acknowledgements:
The authors would like to thank the researchers who submitted unpublished data or facilitated these requests: John B. Barnes, Venetia Clarke, Patricia Frazier, Amanda Gilmore, Debra Kaysen, Sophie Khadr, Mary Koss, Katherine Miller, Jani Nöthling, Matthew Price, Yan Quidé, Patricia Resick, Barbara Rothbaum, Arlete Maria dos Santos Fernandes, Soraya Seedat, Brian Smith, Maria Steenkamp, and Kate Walsh. The authors report no conflicts of interest.
Funding:
Manuscript preparation for this article was supported by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) grants T32AA007455 (PI: Larimer), K99AA026317 (PI: Dworkin), R00AA026317 (PI: Dworkin), and R01AA027499 (PI: Bedard-Gilligan). The views expressed in this article are those of the authors and do not necessarily reflect the positions or policies of the University of Washington or the NIAAA.
Footnotes
Because the sample size as well as the n with PTSD were needed to compute transformed proportions for analyses, we sometimes needed to calculate n with PTSD by multiplying N by the proportion reported in the article and rounding to the nearest integer. We then checked this calculation by dividing it by N and comparing it to the proportion reported in the article. When this check yielded a different proportion than reported in the article, we retained the unrounded n to 2 decimals.
Resick (1988) used the Impact of Events Scale, which reflected the DSM-III intrusions and avoidance symptom clusters, and did not assess the hyperarousal cluster.
Although we considered aggregating estimates via month-specific subgroup analyses (i.e., in which we aggregated only those effects available at each month), these estimates would be biased by the studies available at a given month. For example, if a study of an especially low-severity population had an observation at 3 months but not 1 month, the 1-month estimate would be biased upward. Subgroup analyses would have also involved averaging across change that occurred during a given month, and therefore would have reduced precision compared to point-specific model predicted values.
Contributor Information
Emily R. Dworkin, University of Washington School of Medicine, 1100 NE 45th St., Ste. 300, Seattle, WA, USA, 98105
Anna E. Jaffe, University of Nebraska- Lincoln
Michele Bedard-Gilligan, University of Washington School of Medicine, Skye Fitzpatrick, York University.
References
- Akaike H (1974). A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19, 716–723. 10.1109/TAC.1974.1100705 [DOI] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Amstadter AB, & Vernon LL (2008). Emotional reactions during and after trauma: A comparison of trauma types. Journal of Aggression, Maltreatment & Trauma, 16, 391–408. 10.1080/10926770801926492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armour C, Shevlin M, Elklit A, & Mroczek D (2012). A latent growth mixture modeling approach to PTSD symptoms in rape victims. Traumatology, 18(1), 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Chen J, & Stevens MR (2011). National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, & Merrick MT (2014). Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization - National Intimate Partner and Sexual Violence Survey, United States, 2011. MMWR Surveillance Summaries, 63(1), 1–18. [PMC free article] [PubMed] [Google Scholar]
- Breslau N (2009). The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse, 10, 198–210. 10.1177/1524838009334448 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, & Valentine JD (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. 10.1037/0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Bryant RA (2011). Psychological interventions for trauma exposure and PTSD. In Stein DJ, Friedman MJ, & Blanco C (Eds.), World Psychiatric Association evidence and experience in psychiatry series: Post-traumatic stress disorder (pp. 171–202). Wiley-Blackwell. 10.1002/9781119998471.ch5 [DOI] [Google Scholar]
- Bryant-Davis T, Chung H, Tillman S, & Belcourt A (2009). From the margins to the center: Ethnic minority women and the mental health effects of sexual assault. Trauma, Violence & Abuse, 10(4), 330–357. 10.1177/1524838009339755 [DOI] [PubMed] [Google Scholar]
- Darves-Bornoz JM, Lépine JP, Choquet M, Berger C, Degiovanni A, & Gaillard P (1998). Predictive factors of chronic post-traumatic stress disorder in rape victims. European Psychiatry, 13, 281–287. 10.1016/S0924-9338(98)80045-X [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Brill CD, & Ullman SE (2019). Social reactions to disclosure of interpersonal violence and psychopathology: A systematic review and meta-analysis. Clinical Psychology Review, 72, 101750. 10.1016/j.cpr.2019.101750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER (2020). Risk for mental disorders associated with sexual assault: A meta-analysis. Trauma, Violence, & Abuse, 21(5), 1011–1028. 10.1177/1524838018813198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER, Menon SV, Bystrynski J, & Allen NE (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. 10.1016/j.cpr.2017.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER, & Weaver TL (in press). The impact of sociocultural contexts on mental health following sexual violence: A conceptual model. Psychology of Violence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315, 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behavior Research and Therapy, 38, 319–345. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. 10.1037/0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Foa EB, & Riggs DS (1995). Posttraumatic stress disorder following assault: Theoretical considerations and empirical findings. Current Directions in Psychological Science, 4, 61–65. 10.1111/1467-8721.ep10771786 [DOI] [Google Scholar]
- Foa EB, Huppert JD, & Cahill SP (2006). Emotional processing theory: An update. In Rothbaum BO (Ed.), Pathological anxiety: Emotional processing in etiology and treatment (pp. 3–24). New York: Guilford Press. [Google Scholar]
- Forneris CA, Gartlehner G, Brownley KA, Gaynes BN, Sonis J, Coker-Schwimmer E, Jonas DE, Greenblatt A, Wilkins TM, Woodell CL, Lohr KN (2013). Interventions to prevent post-traumatic stress disorder: A systematic review. American Journal of Preventive Medicine, 44(6), 635–650. 10.1017/CBO9781107415324.004 [DOI] [PubMed] [Google Scholar]
- Frazier PA (1988). Attributions and adjustment to rape (Unpublished doctoral dissertation). University of Minnesota, Minneapolis, MN. [Google Scholar]
- Frazier PA (2000). The role of attributions and perceived control in recovery from rape. Journal of Personal & Interpersonal Loss, 5, 203–225. [Google Scholar]
- Frazier P, Conlon A, & Glaser T (2001). Positive and negative life changes following sexual assault. Journal of Consulting and Clinical Psychology, 69, 1048–1055. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Harlow T, Schauben L, & Byrne C (1993, August). Predictors of postrape trauma. Paper presented at the 1993 meeting of the American Psychological Association, Toronto, Ontario, Canada. Retrieved from https://files.eric.ed.gov/fulltext/ED370032.pdf [Google Scholar]
- Galatzer-Levy IR, Huang SH, & Bonanno GA (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55. [DOI] [PubMed] [Google Scholar]
- Gilboa-Schechtman E, & Foa EB (2001). Patterns of recovery from trauma: The use of intraindividual analysis. Journal of Abnormal Psychology, 110, 392–400. [DOI] [PubMed] [Google Scholar]
- Gilmore AK, Walsh K, Frazier P, Ledray L, Acierno R, Ruggiero KJ, Kilpatrick DG, & Resnick HS (2019a). Prescription opioid misuse after a recent sexual assault: A randomized clinical trial of a video intervention. American Journal on Addictions, 28, 376–381. 10.1111/ajad.12922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore AK, Walsh K, Frazier P, Meredith L, Ledray L, Davis J, Acierno R, Ruggiero KJ, Kilpatrick DG, Jaffe AE, & Resnick HS (2019b). Post-sexual assault mental health: A randomized clinical trial of a video-based intervention. Journal of Interpersonal Violence. Advance online publication. 10.1177/0886260519884674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guay S, Beaulieu-Prévost D, Sader J, & Marchand A (2019). A systematic literature review of early posttraumatic interventions for victims of violent crime. Aggression and Violent Behavior, 46, 15–24. 10.1016/j.avb.2019.01.004 [DOI] [Google Scholar]
- Gutner CA, Rizvi SL, Monson CM, & Resick PA (2006). Changes in coping strategies, relationship to the perpetrator, and posttraumatic distress in female crime victims. Journal of Traumatic Stress, 19, 813–823. 10.1002/jts.20158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen NB, Hansen M, Nielsen LH, & Elklit A (2017). Positive or negative change in outlook on life following sexual assault and associations to PTSD severity. Sexual and Relationship Therapy, 32, 36–45. 10.1080/14681994.2016.1169266 [DOI] [Google Scholar]
- Higgins JPT, & Thompson SG (2002). Quantifying heterogeneity in meta-analysis. Statistics in Medicine, 21, 1539–1558. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- Hiller RM, Meiser-Stedman R, Fearon P, Lobo S, MacKinnon A, Fraser A, & Halligan SL (2016). Changes in the prevalence and symptom severity of child PTSD in the year following trauma: A meta-analytic study. Journal of Child Psychology and Psychiatry, 57, 884–898. 10.1111/jcpp.12566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, Hansen M, Vallières F, Murphy J, & Elklit A (2016). The temporal relations of PTSD symptoms among treatment-seeking victims of sexual assault: A longitudinal study. Journal of Loss and Trauma, 21, 492–506. [Google Scholar]
- Janoff-Bulman R (1992). Shattered assumptions: Towards a new psychology of trauma. New York, NY: Free Press. [Google Scholar]
- Kaysen D, Atkins D, Moore S, Lindgren K, Dillworth T, & Simpson T (2011). Alcohol use, problems, and the course of posttraumatic stress disorder: A prospective study of female crime victims. Journal of Dual Diagnosis, 7, 262–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen DL, Lindgren KP, Lee CM, Lewis MA, Fossos N, & Atkins DC (2010). Alcohol-involved assault and the course of PTSD in female crime victims. Journal of Traumatic Stress, 23, 523–527. 10.1002/jts.20542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, & Flood AM (2009). A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress, 22, 227–235. 10.1002/jts.20406 [DOI] [PubMed] [Google Scholar]
- Kennedy AC, & Prock KA (2018). “I still feel like I am not normal”: A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma, Violence, & Abuse, 19, 512–527. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV, Ferry F, Florescu S, Gureje O, Haro JM, Huang Y, Karam EG, Kawakami N, Lee S, Lepine J-P, Levinson D, … Koenen KC (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Rose S, Koenen KC, Karam EG, Stang PE, Stein DJ, Heeringa SG, Hill ED, Liberzon I, McLaughlin KA, McLean SA, Pennell BE, Petukhova M, Rosellini AJ, Ruscio AM, Shahly V, Shalev AY, Silove D, Zaslavsky AM, … Viana MC (2014). How well can post-traumatic stress disorder be predicted from pre-trauma risk factors? An exploratory study in the WHO World Mental Health Surveys. World Psychiatry, 13(3), 265–274. 10.1002/wps.20150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadr S, Clarke V, Wellings K, Villalta L, Goddard A, Welch J, Bewley S, Kramer T, & Viner R (2018). Mental and sexual health outcomes following sexual assault in adolescents: A prospective cohort study. The Lancet. Child & Adolescent Health, 2(9), 654–665. 10.1016/S2352-4642(18)30202-5 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Ruggiero KJ, Conoscenti LM, & McCauley J (2007). Drug-facilitated, incapacitated, and forcible rape: A national study. Charleston, SC: Medical University of South Carolina, National Crime Victims Research & Treatment Center. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology, 71, 692–700. 10.1037/0022-006X.71.4.692 [DOI] [PubMed] [Google Scholar]
- Koss MP, & Figueredo AJ (2004). Change in cognitive mediators of rape’s impact on psychosocial health across 2 years of recovery. Journal of Consulting and Clinical Psychology, 72, 1063–1072. 10.1037/0022-006X.72.6.1063 [DOI] [PubMed] [Google Scholar]
- Lebowitz L, & Roth S (1994). “I felt like a slut”: The cultural context and women’s response to being raped. Journal of Traumatic Stress, 7, 363–390. [DOI] [PubMed] [Google Scholar]
- Lowe SR, Ratanatharathorn A, Lai BS, Van Der Mei W, Barbano AC, Bryant RA, Delahanty DL, Matsuoka YJ, Olff M, Schnyder U, Laska E, Koenen KC, Shalev AY, & Kessler RC (2020). Posttraumatic stress disorder symptom trajectories within the first year following emergency department admissions: Pooled results from the International Consortium to predict PTSD. Psychological Medicine. 10.1017/S0033291719004008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGregor KE, Villalta L, Clarke V, Viner R, Kramer T, & Khadr SN (2019). A systematic review of short and medium-term mental health outcomes in young people following sexual assault. Journal of Child & Adolescent Mental Health, 31(3), 161–181. [DOI] [PubMed] [Google Scholar]
- Machado CL, de Azevedo RCS, Facuri CO, Vieira M-JN, Fernandes A-MS, & Vieira M-JN (2011). Posttraumatic stress disorder, depression, and hopelessness in women who are victims of sexual violence. International Journal of Gynecology & Obstetrics, 113, 58–62. 10.1016/j.ijgo.2010.10.016 [DOI] [PubMed] [Google Scholar]
- Marcoulides KM (2018). Automated latent growth curve model fitting: A segmentation and knot selection approach. Structural Equation Modeling, 25, 687–699. 10.1080/10705511.2018.1424548 [DOI] [Google Scholar]
- Mathews S, Abrahams N, & Jewkes R (2013). Exploring mental health adjustment of children post sexual assault in South Africa. Journal of Child Sexual Abuse, 22, 639–657. [DOI] [PubMed] [Google Scholar]
- Miller KE, Cranston CC, Davis JL, Newman E, & Resnick H (2015). Psychological outcomes after a sexual assault video intervention: A randomized trial. Journal of Forensic Nursing, 11, 129–136. 10.1097/JFN.0000000000000080 [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, & Poulton R (2010). How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine, 40, 899–909. 10.1017/S0033291709991036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, & Friedman MJ (2006). Back to the future of understanding trauma: Implications for cognitive-behavioral therapies for trauma. In Follette VM & Ruzek JI (Eds.), Cognitive behavioral therapies for trauma (pp. 1–15). New York: Guilford Press. [Google Scholar]
- National Heart, Lung, and Blood Institute. (2014). Quality assessment tool for observational cohort and cross-sectional studies. Bethesda: National Institutes of Health, Department of Health and Human Services. Retrieved from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Google Scholar]
- Nickerson A, Steenkamp M, Aerka IM, Salters PK, Carper TL, Barnes JB, & Litz BT (2013). Prospective investigation of mental health following sexual assault. Depression and Anxiety, 30, 444–450. 10.1002/da.22023 [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, & Weiss DS (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73. [DOI] [PubMed] [Google Scholar]
- Powers MB, Warren AM, Rosenfield D, Roden-Foreman K, Bennett M, Reynolds MC, Davis ML, Foreman ML, Petrey LB, & Smits JAJ (2014). Predictors of PTSD symptoms in adults admitted to a Level I trauma center: A prospective analysis. Journal of Anxiety Disorders, 28(3), 301–309. 10.1016/j.janxdis.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi W, Ratanatharathorn A, Gevonden M, Bryant R, Delahanty D, Matsuoka Y, Olff M, DeRoon-Cassini T, Schnyder U, Seedat S, Laska E, Kessler RC, Koenen K, & Shalev A (2018). Application of data pooling to longitudinal studies of early post-traumatic stress disorder (PTSD): The International Consortium to Predict PTSD (ICPP) project. European Journal of Psychotraumatology, 9(1). 10.1080/20008198.2018.1476442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quidé Y, Andersson F, Dufour-Rainfray D, Descriaud C, Brizard B, Gissot V, Cléry H, Carrey Le Bas M, Osterreicher S, Ogielska M, Saint-Martin P, & El-Hage W (2018). Smaller hippocampal volume following sexual assault in women is associated with post-traumatic stress disorder. Acta Psychiatrica Scandinavica, 138(4), 312–324. 10.0.4.87/acps.12920 [DOI] [PubMed] [Google Scholar]
- R Core Team. (2020). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Retrieved from https://www.R-project.org/. [Google Scholar]
- Raftery AE (1995). Bayesian model selection in social research. Sociological Methodology, 25, 111–163. 10.2307/271063 [DOI] [Google Scholar]
- Reitsema AM, & Grietens H (2016). Is anybody listening? The literature on the dialogical process of child sexual abuse disclosure reviewed. Trauma, Violence, & Abuse, 17(3), 330–340. [DOI] [PubMed] [Google Scholar]
- Resick PA (1988). Reactions of female and male victims of rape or robbery (Final report, NIJ Grant No. 85-IJ-CV-0042). Washington, DC: National Institute of Justice. [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2017). Cognitive processing therapy for PTSD: A comprehensive manual. New York, NY: Guilford Press. [Google Scholar]
- Resnick HS, Acierno R, Amstadter AB, Self-Brown S, & Kilpatrick DG (2007a). An acute post-sexual assault intervention to prevent drug abuse: Updated findings. Addictive Behaviors, 32, 2032–2045. 10.1016/j.addbeh.2007.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick H, Acierno R, Waldrop AE, King L, King D, Danielson C, Ruggiero KJ, & Kilpatrick D (2007b). Randomized controlled evaluation of an early intervention to prevent post-rape psychopathology. Behaviour Research and Therapy, 45, 2432–2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, & Best CL (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61, 984–991. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Rothbaum BO, & Foa EB (1995). A prospective examination of symptoms of posttraumatic stress disorder in victims of nonsexual assault. Journal of Interpersonal Violence, 10, 201–214. 10.1177/0886260595010002005 [DOI] [Google Scholar]
- Roberts NP, Kitchiner NJ, Kenardy J, Lewis CE, & Bisson JI (2019). Early psychological intervention following recent trauma: A systematic review and meta-analysis. European Journal of Psychotraumatology, 10(1), 1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, & Walsh W (1992). A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress, 5, 455–475. 10.1002/jts.2490050309 [DOI] [Google Scholar]
- Rothbaum BO, Kearns MC, Price M, Malcoun E, Davis M, Ressler KJ, Lang D, & Houry D (2012). Early intervention may prevent the development of posttraumatic stress disorder: A randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry, 72, 957–963. 10.1016/j.biopsych.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubel NL (1989). The relationship between social adjustment and posttraumatic stress symptomatology following sexual assault (Unpublished doctoral dissertation). Temple University, Philadelphia, PA. [Google Scholar]
- Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, Friedman MJ, & Fullerton CS (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS ONE, 8(4), 1–5. 10.1371/journal.pone.0059236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer G, Chemaitelly H, Abu-Raddad LJ, & Rücker G (2019). Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Research Synthesis Methods, 10, 476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalev AY, Gevonden M, Ratanatharathorn A, Laska E, van der Mei WF, Qi W, Lowe S, Lai BS, Bryant RA, Delahanty D, Matsuoka YJ, Olff M, Schnyder U, Seedat S, DeRoon-Cassini TA, Kessler RC, Koenen KC, Errera-Ankri Y, Barbano AC, … van Zuiden M (2019). Estimating the risk of PTSD in recent trauma survivors: Results of the International Consortium to Predict PTSD (ICPP). World Psychiatry, 18(1), 77–87. 10.1002/wps.20608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smid GE, Mooren TT, van der Mast RC, Gersons BP, & Kleber RJ (2009). Delayed posttraumatic stress disorder: Systematic review, meta-analysis, and meta-regression analysis of prospective studies. The Journal of Clinical Psychiatry, 70, 1572–1582. [DOI] [PubMed] [Google Scholar]
- Smith HL, Summers BJ, Dillon KH, & Cougle JR (2016). Is worst-event trauma type related to PTSD symptom presentation and associated features? Journal of Anxiety Disorders, 38, 55–61. 10.1016/j.janxdis.2016.01.007 [DOI] [PubMed] [Google Scholar]
- Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, Chen J (2018). The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief – Updated Release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Steenkamp MM, Dickstein BD, Salters PK, Hofmann SG, & Litz BT (2012). Trajectories of PTSD symptoms following sexual assault: Is resilience the modal outcome? Journal of Traumatic Stress, 25, 469–474. 10.1002/jts.21718 [DOI] [PubMed] [Google Scholar]
- Streiner DL, Patten SB, Anthony JC, & Cairney J (2009). Has ‘lifetime prevalence’ reached the end of its life? An examination of the concept. International Journal of Methods in Psychiatric Research, 18, 221–228. 10.1002/mpr.296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, & Foa EB (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132, 959–992. [DOI] [PubMed] [Google Scholar]
- Ulirsch JC, Ballina LE, Soward AC, Rossi C, Hauda W, Holbrook D, Wheeler R, Foley KA, Batts J, Collette R, Goodman E, & McLean SA (2014). Pain and somatic symptoms are sequelae of sexual assault: Results of a prospective longitudinal study. European Journal of Pain, 18(4), 559–566. 10.1002/j.1532-2149.2013.00395.x [DOI] [PubMed] [Google Scholar]
- Viechtbauer W (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36, 1–48. [Google Scholar]
- Walsh K, Gilmore AK, Frazier P, Ledray L, Acierno R, Ruggiero KJ, Kilpatrick DG, & Resnick HS (2017). A randomized clinical trial examining the effect of video-based prevention of alcohol and marijuana use among recent sexual assault victims. Alcoholism: Clinical and Experimental Research, 41, 2163–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, & Marx BP (2018). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30, 383–395. 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, McCauley JL, Amstadter AB, Ruggiero KJ, & Kilpatrick DG (2012). Prevalence and risk of psychiatric disorders as a function of variant rape histories: Results from a national survey of women. Social Psychiatry and Psychiatric Epidemiology, 47, 893–902. 10.1007/s00127-011-0397-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


