Abstract
As of May 2021, the current COVID-19 pandemic is still plaguing the world, challenging all the countries and their health systems, globally. In this context, conditions typical of low-resource settings surfaced also in high-resource ones (e.g., the lack of essential medical equipment, of resources etc.), while exacerbating in the already resource-scarce settings, because of COVID-19. This is the case of oxygen concentrators that are one of the first-line medical devices for treating COVID-19 patients. Since the beginning of 2020, their demand has been rapidly growing worldwide, aggravating the situation for low-resource settings, where the availability of devices providing oxygen-enriched air was already scarce. In fact, due to their delicacy, the lack of spare parts and of an appropriate health technology management system, oxygen concentrators can often be found broken or not working properly in these settings. The underlying problems have deep roots. The current regulatory frameworks and standards, which are set by high-income countries, are too stringent, and do not take into account the limited resources of poorer settings. Thus, they are often inapplicable in such settings. One of the main issues affecting the oxygen concentrators, is that related to the filters, which are designed to filter out dust, particles, bacteria, and to be used in medical locations complying with international standards (e.g., the air filtration level in a surgical theatre in Italy is at 99.97%). When used in low-resource settings, which do not comply with these standards and face several challenges (e.g., dust), these filters have a much-reduced lifespan.
For these reasons, this paper aims to present the redesign of the inlet filter of an oxygen concentrator, which is used to prevent gross particles to enter the device. The redesign is based on a reverse engineering approach, and on the use of 3D-printing along with activated charcoal. After testing the filtration efficiency with a particle counter, the filter design has been refined through several iterations. The final prototype performs particularly well when filtering particles above 1 μm (with a filtration efficiency of 64.2%), and still has a satisfactory performance with any particle size over 0.3 μm (with a filtration efficiency of 38.8%). Following the United Nations Sustainable Development Goals, this project aims to empower local communities, and start a positive trend of self-sustained supply chain of simple spare parts for medical devices, leveraging on frugal engineering, 3D-printing, locally produced activated charcoal, and circular economy.
Keywords: Oxygen concentrator, Filter, Clinical engineering, Supply chain, Circular economy, Sustainable development
Abbreviations: (LMIC), Low- and Middle-Income Country; (MD), Medical Device; (WHO), World Health Organization; (LRS), Low-Resource Setting; (SDG), Sustainable Development Goal
1. Introduction and background
Over the 21st century, the industrial and public healthcare sectors of low-income countries (LMICs) tend to rely on scarce funding when compared to high-income ones. This results in a lack of availability of medical devices (MDs) and the exclusion of the poorest populations from basic health care. This often leads hospitals and other healthcare centres lacking sufficient MDs to effectively administer healthcare resources, from expensive equipment such as X-ray machines to even the most basic MDs (Shah et al., 2015; Piaggio et al., 2019; Di Pietro et al., 2020, Pecchia et al., 2020).
In LMICs, where the public sector is unable to provide healthcare support, donations of MDs by many organizations and companies from high-income countries cover approximately the 80% of the entire medical equipment supply (in line with a World Health Organization (WHO) estimation) (WHO, 2010; Arasaratnam and Humphreys 2013, Gauthier et al., 2013; Piaggio et al., 2019). Hypothetically, this high volume of donated equipment should drastically improve the efficacy of medical sectors across sub-Saharan Africa and other low-income settings. However, several critical factors are still holding back progress and MD donations proved to be not the ideal solution (Piaggio et al., 2019). The lack of a good health technology management program in addition to the harsh environmental conditions, that are typical of these settings (e.g., dust, high temperatures, high humidity), and the lack of efficient supply chains are the most significant issues (Di Pietro et al., 2020, Pecchia et al., 2020; Piaggio et al., 2021).
Moreover, WHO recently estimates that about 40% of the donated medical equipment, is non-functioning (Marks et al., 2019). This estimate can also be considered conservative as many hospitals in LMICs do not keep up to date records of their inventories (Medenou et al., 2019). Whilst this statistic is concerning, the real situation is even more alarming. The low levels of funding in these settings, indeed, has been causing staff shortages across hospitals and other medical centres. The lack of qualified professionals licensed to use advanced MDs and to carry out preventive maintenance, often results in underuse of MDs due to damaged parts or, in the worst case, in permanent equipment damage (Piaggio et al., 2019; Di Pietro et al., 2020, Pecchia et al., 2020). Furthermore, the safe and efficient use of MDs is often hindered by the lack of a reliable power supply (Chawla et al., 2018; Di Pietro et al., 2020, Pecchia et al., 2020).
Donors and other organizations are attempting to mitigate the problem of non-functioning MDs through a variety of methods, such as providing free education and staff training needed for the use and maintenance of donated devices. However, as it can be seen from the various challenges described above, this will not be enough to solve the problem of the donated equipment, which is not manufactured in/for LMICs. In fact, in addition to the limited availability of qualified staff to make repairs, there is often no obtainable access to spare parts, resulting in one malfunctioning part hindering the use of the entire device (Kaplan et al., 2011; Di Pietro et al., 2020, Pecchia et al., 2020). Representative of this scenario is the oxygen concentrators’ supply.
Despite the WHO defined medical oxygen as an “essential medicine”, the access to it remains critical in the healthcare systems of most LMICs (Di Pietro et al., 2020, Pecchia et al., 2020; Howie et al., 2020). Currently, this situation is being exacerbated by the spread of COVID-19 pandemic. Over the last year, in fact, the demand for oxygen concentrators and ventilators by health facilities drastically increased, as they can play a vital role in the treatment of critical-condition patients infected with COVID-19 (Andellini et al., 2020; Bhisey 2020, Howie et al., 2020; WHO 2021). Currently, oxygen concentrators are enlisted in the WHO's priority MDs list for the COVID-19 response. Oxygen concentrators are MDs that deliver oxygen to patients with blood oxygen concentration levels below normal and that are used to treat individuals with breathing related disorders or conditions including but not limited to asthma attacks, pneumonia, and respiratory stress syndrome. Furthermore, oxygen concentrators are more suitable for LMICs than alternative such as oxygen canisters, as they concentrate oxygen from ambient air without requiring an artificial oxygen supply, significantly reducing costs and the problems related to the oxygen supply chain.
Bradley et al. (Bradley et al., 2013; Bradley et al., 2015) proved the cost-effectiveness of oxygen concentrators when compared to other oxygen systems (e.g., cylinders). In fact, they estimated that even when replaced every 5 years, the use of oxygen concentrators reduced the costs by 75%. Based on the field studies performed in Gambia, they also proved that, a good health technology management is at the base of a functioning oxygen concentrator service (Bradley et al., 2015). Moreover, they pinpointed how the most frequent issues affecting oxygen concentrators, i.e., those related to batteries and filters, are easy and cheap to fix.
However, in (Bradley et al., 2015) they also state the fact that the resources for and the access to spare parts are among the key elements of an oxygen concentrator support ecosystem. In the specific case of The Gambia unit, the access to such spare parts was guaranteed through a long-standing relationship with manufacturers. Nonetheless, this might not be the case for other low-resource settings (LRSs). Mongolia and Malawi, for example, have difficulty in retrieving spare parts, as well as Benin and Uganda (Di Pietro et al., 2020, Pecchia et al., 2020).
Moreover, the constant power supply that oxygen concentrators require to function could be a disadvantage because of the lack of/unreliability of the electrical power in LRSs. However, the amount of power they consume is relatively low (i.e., 280–600W depending on the model) (WHO 2016) and this cost is much lower than the cost to refill and transport oxygen cylinders (Friesen et al., 1999). The WHO estimates, indeed, that the operating costs of an oxygen concentrator are between 2 and 8 US dollar equivalent for every 1000 L of oxygen supplied, compared to oxygen cylinders that cost from 10 to 30 US dollars for the same amount of oxygen supplied (WHO 2016).
Howie et al. (Howie et al., 2020) and Bradley et al. (Bradley et al., 2016) presented oxygen concentrators systems relying on batteries and solar panels, that proved to be able to provide for a continuous supply of oxygen for two days, as well as to be more reliable and easier to use.
When it comes to battery-based device, it is also essential to take into consideration the limitations of local contexts, such as the extreme environmental conditions. High temperatures challenge and reduce the battery life by 16% (Bradley et al., 2012).
Despite the above-mentioned limitations and advantages, the presence of one to three filters within the oxygen concentrators (i.e., the gross particle filter, the inlet filter, and the output filter) is the source of one of the main issues in LRSs. The filters, in fact, are designed to work a limited number of hours in ideal conditions (e.g., a surgical theatre where there is a 99.97% air filtration level). These ideal conditions cannot be found in LRSs, where these devices are bound to last much less, also because of the lack of a working supply chain for spare parts (Piaggio et al., 2019). To the authors’ best knowledge, there has been no attempt to design a replacement filter that can readily and rapidly be manufactured locally at a LRS medical facility. Due to its many advantages with regard to small scale local manufacturing, additive manufacturing appears to be an ideal process to tailor this aim towards. In fact, additive manufacturing is used to some extent in almost every major manufacturing industry and is widely used across a large array of disciplines, from the motor industry to medicine. Today, 3D printers are even accessible and affordable for members of the public in developed countries and are now also beginning to be adopted by organizations in low-income settings (Rismani et al., 2015; Beroza 2019).
For this reason, this project aims to present the redesign of the inlet filter of an oxygen concentrator, based on a reverse engineering approach, and on the use of 3D-printing along with activated charcoal, following the design paradigm presented in (Piaggio et al., 2021). Moreover, this project aims to set out a sample process that, together with 3D printing and protocycling (i.e., the act of recycling used filament and prints to create new filament), can foster capacity building in local communities, especially in LRSs, empowering them to create a local supply chain for affordable and environmental-friendly inlet filters for oxygen concentrators. As the project focuses on important aspects such as empowering local communities, diminishing the environmental impact, kickstart a local supply chain, increase the lifespan of oxygen concentrators (and the amount of available oxygen for those who need it), it is perfectly aligned with several of the United Nations’ sustainable development goals (SDGs) (e.g., SDG 3 – Good health and wellbeing; SDG 9 – industry, innovation and infrastructure; SDG 10 – Reduced inequalities; SDG 12 – Responsible consumption and production; SDG 15 – Life on land) (UN, 2020).
2. Methodology (design and manufacturing)
This section presents the methods that were used for prototyping and validating our filter. The filter design was partially based on the existing inlet filter of EverFlo by Philips, which was selected because of availability in our laboratory.
2.1. 3D data acquisition and post processing
In order to have a casing compatible with the inlet of EverFlo, two methods of 3D data acquisition were used, i.e., handheld 3D scanning and microcomputed tomography scanning. The results from these two techniques were then compared and analysed, so that the superior method could be recommended for oxygen concentrator filters as well as other small-scale MDs future applications.
2.2. Handheld 3D scanning
2.2.1. Data acquisition
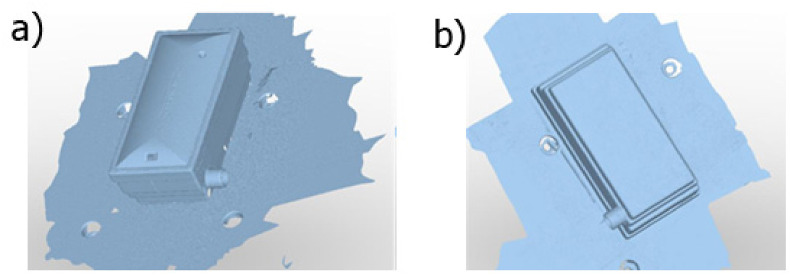
The Nikon h120 handheld scanner, mounted on a MCAx25 scanning tripod setup was used for 3D handheld scanning. The Nikonh120 is still a highly accurate scanner, with a combined accuracy of 0.028 mm. This process is important as it allows for the Computer-Aided Design (CAD) that will be created to have as close dimensions as possible to the original filter, which will ensure that the new filters fit comfortably into the oxygen concentrator. Each filter was scanned twice, because, as the parts were scanned on a measuring table, a second scan of the underside was required to capture every surface (see Fig. 1 a and b). The scanning software used was Nikon Focus. Each scan also captured part of the surface of the measuring table, so the scan data was all exported as an.STL File into Geomagic Studio2 and the measuring table data was removed (as well as any other noise present).
Fig. 1.
Handheld scan data of the filter, prior to the application of post processing techniques. Top of the filter (a) Bottom of the filter (b).
2.2.2. Post processing
The two scans were then combined, by first carrying out a manual registration. Manual registration is when a number of common points (in this case 3) between two scan sets are selected. The software then uses these common points to align the two scans together, forming one combined item. A global registration was then carried out, which moves the two scan sets relative to each other until the highest overlap is located. The combined filter scans were then meshed (see Fig. 2 ). A side effect of conducting an alignment of two separate scans is that it will induce an additional nominal error into the model, meaning that the dimensions of the object will not be as accurate.
Fig. 2.
Handheld scan data of the filter, after post processing.
2.3. Micro computed tomography (CT) scanning
2.3.1. Data acquisition
The inlet filter was also scanned using a micro–Computed Tomography (CT) X-ray scanner. This method is able to capture internal data without having to move or damage any parts. The scan was carried out with specific scan parameters (see Table 1 ) in order to produce the cleanest data.
Table 1.
The parameters used during micro-CT scanning.
| Parameter | Value |
|---|---|
| Voltage | 40 Kilovolts |
| Exposure | 50 ms |
| Power | 65 Kilowatts |
| Projections | 2879 |
| Resolution | 150 μm |
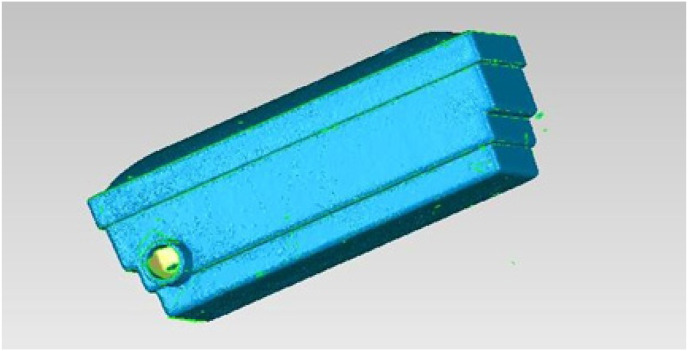
The filter data is initially presented as a set of 2879 2D projections. A voxel resolution of 150 μm was achieved, as this was the maximum possible resolution available that could also scan the filter in a single scan. A greater resolution could be achieved by dividing the filter into multiple scans and stitching them together in post processing, but this was not deemed as necessary in this application. From the 2D data projections the internal structures are visible, i.e., a pleated paper structure across the center of the internal area (see Fig. 3 ).
Fig. 3.
2D projections of the inlet filters showing the internal structure: a) frontal, b) transverse, c) sagittal.
The post processing phase consists of stitching together the 2D stack into a 3D model which was then meshed via a reconstruction process. Similar to the handheld scanning technique, the 3D model was then converted into an.STL File. The.STL file type allows for easy analysis, measurement and editing of the model using CAD software. As well as providing an.STL File for future design like the handheld scanning method, the CT scan data also provided important context as to the design of the original EverFlo filter, as it also shows the internal structure of the filter, something which handheld scanning is not able to achieve.
2.4. Filter material manufacture
From the micro-CT scan data, it resulted that the internal structure of the inlet filter is a folded paper structure, which acts to trap gross particles in the air to prevent them getting into the oxygen concentrator and contaminating the air. Paper air filters are cheap and effective but require regular maintenance in order to clean out the residue that gets caught between folds. Failure to clean paper air inlet filters will reduce the effectiveness of the filter considerably, and in an oxygen concentrator may result in the oxygen delivered to the patient being contaminated with particulates. Before making changes to the reverse engineered data in order to produce an ideal CAD model for the new filter, a filter material must be selected, so that when the new model is designed it is done so with the specific material in mind. A number of different filter materials were considered, including cotton gauze, paper, sponge and activated carbon. Of these materials, activated carbon was selected due to the unique criteria presented by LRSs. In fact, charcoal is the main source of domestic fuel in several sub-Saharan African countries, which produce 65% of the world's charcoal.3 Activated carbon filters are filters that use small pieces of powdered or granular carbon to filter air, have an extremely high surface area to volume ratio and are very porous (more so than regular carbon due to the activation process) (Dillon et al., 1989).
The process to locally manufacture activated carbon, in fact, is easy to carry out, low cost and accessible. First wood is heated in a closed container until it forms a charcoal. After the charcoal is cleaned with water and left to dry, it is ground into a fine powder or pellets. To activate the charcoal, calcium chloride, either as a premixed solution or as flakes hydrated with water, is mixed with water in a 1:3 ratio. Alternatively, the citric acid contained in lemon juice can be used instead of calcium chloride. This mixed solution is then added to the charcoal, sealed for 24 h, and then heated again to form the final activated carbon product (Nubie,).
2.5. Filter modelling
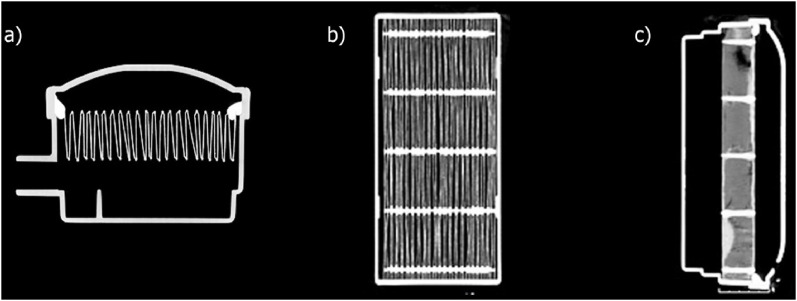
With the filter material selected and the 3D data of the pre-existing oxygen concentrator inlet filter obtained, a new version of the digital model was made. Due to the changing of the filter material from a paper structure to activated carbon, some changes to the 3D model were required. These changes were also depending on the fact that the filter would be created using additive manufacturing, which implied that the filter material should be installed after manufacturing of the case is complete. The most simple and straightforward design solution that would allow filter material to be installed afterwards, was to simply split the filter casing into two distinct sections with a tight tolerance, namely a “base” and a “lid”. Other designs were also considered including one with a hinge mechanism (see Fig. 4 a), keeping the base and lid of the filter casing connected. All CAD design work for this project was carried out using Solidworks Education Edition20194 .
Fig. 4.
CAD model of the initial hinge-based prototype (a), later replaced with the “snap fit” model (b).
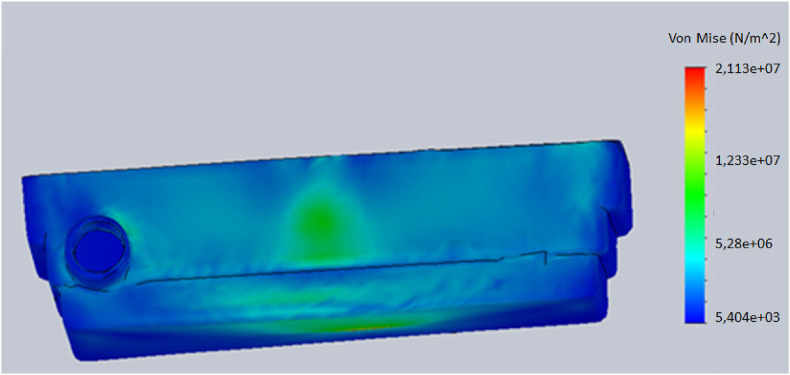
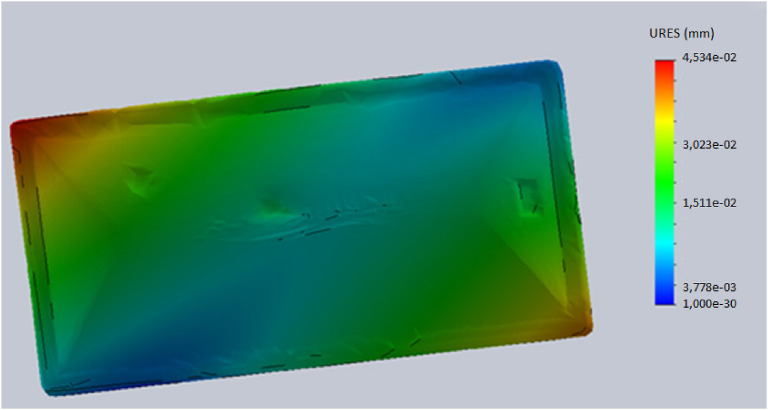
2.6. Finite element methods analysis
With the filter casing redesigned, a short simulation study was carried out using finite element methods analysis to ensure that there were no structural weaknesses, as it is important to confirm that the casing will not fail, excessively deform or otherwise be rendered ineffective during its life span. Consequently, Von Mises stress, strain and displacement values were measured against expected impacts, such as from the filter being accidently dropped, or the oxygen concentrator with the filter inside being knocked over. An additional safety factor of 10% was also implemented. Results are displayed as concentrations on the subject model, with a key that can be read to determine the regions of high and low stress, strain or deformation. Solidworks Education Edition 2019 was used to carry out this simulation.
2.7. Filter manufacturing
After the simulation testing process is completed, the inlet filter product can now proceed to the next stage, manufacture. Before printing, the right 3D printer should be selected to use, as there are many variations in model, with each being adapted for specific applications. This decision can be used both to manufacture the initial test model for this project but throughout the selection process it is important to take into consideration the suitability of the printer or similar model for a LRS facility.
Among the 3D printers available at the UK facility, Warwick Manufacturing Group, there were the Fortus 360mc, the Stratasys J750, the Markforged Mark Two and the Connex Objet 260. Table 2 shows the available printers and their relevant characteristics.
Table 2.
The relevant characteristics of the available printers.
| FORTUS 360 MC | STRATASYS J750 | MARKFORGED MARK TWO | CONNEX OBJET 260 | |
|---|---|---|---|---|
| MAX BUILD SIZE (MM) | 406 × 355 × 406 | 490 × 390 × 200 | 320 × 132 × 154 | 255 × 252 × 200 |
| PRINTABLE MATERIALS |
|
|
|
|
| PRINT ACCURACY (MM) | 0.127 | 0.125 | 0.2 | |
| SMALLEST LAYER THICKNESS (MM) | 0.127 | 0.014 | 0.1 | 0.016 |
| OTHER ATTRIBUTES | Has multiple model tips, each capable of producing a different slice thickness. | Able to print in over 500,000 colours | Able to integrate carbon fibre alongside other materials | Fast print time |
The printer that was selected for this application was the Fortus 360mc. The Markforged Mark Two was discarded as it cannot print with ABS plastic, that is the material selected for the printer casing due to its durability and cost. The Stratasys J750 has the advantage of being able to print in colour but uses an ‘in-house’ version of ABS that is more expensive, and as the aesthetics of the filter are irrelevant this printer can be discarded. Between the Connex object 260 and the Fortus, the Fortus was selected due to its superior print accuracy. The Fortus (or a similar model) would also be more useful to a LRS setting medical facility, as it is cheaper than the Connex, and swaps the ability to print in resin for other advantages more applicable to MD manufacturing, such as interchangeable printing tips of various sizes, and a larger build area.
After selecting and confirming the manufacturing method, the filter casing could be printed. The material of ABS plastic was used. This material was selected as it has excellent mechanical properties (e.g., good impact resistance and tensile strength) for its price (15–20 US Dollars per kg of ABS filament), which is an important consideration when designing MDs for LRS. ABS plastic is also extremely viable with 3D printing and is accepted by the majority of plastic using printers without complication, or loss of structural integrity. Using a more niche material would likely introduce complications in a LRS, including but not limited to increased costs, limited stock, and the risk of the material not being useable by the 3D printer at the LRS. The 3D printing software Insight was used to slice the model. The default build parameters and other settings were used, as the filter casing product does not require any special treatment such as thermal forming. The print time was approximately 3 h. After the manufacturing of the filter casing is complete, the filter material (activated carbon) could then be manually installed. In this case, a piece of nylon tights was used as an extra container surrounded by a small layer of cotton wool, within the inlet filter casing. The filter material is positioned so that the edges of the casing are covered by it. This should help filter the amount of air that is leaking through the edges, if any. These air leaks should already be minimised by the “snap-fit” design, which should provide for good adherence between the edges of both parts of the casing. Future designs may further look into the airtightness of the edges and, if needed, improve it by using sealing techniques (i.e., v-seal, plug seal) (Oberk, 2021) or by using polyvinyl acetate as an additional sealant.
2.8. Bench tests
The whole design and validation process followed the relevant standards for oxygen concentrators. In particular, once the final prototype was manufactured and assembled, bench tests were designed to validate our filter. These standards report the specifications and testing method for the so-called “outlet filter”, which is the final component of the filtering system before oxygen is delivered. The testing requires the measurements of the number of particles within the oxygen-enriched gas sampled at the output of the oxygen concentrator. This testing should be performed by means of a light scattering particle counter, and the number of particles should be within the limits of ISO5 (max 832 particles greater than 1 μm per cube meter). No testing procedure nor specific requirements were found in the literature, nor in the relevant standards, nor in the maintenance manuals of common oxygen concentrators. Further feedback was also sought after by contacting international experts of clinical engineering and ventilatory systems.
As, to the best of our knowledge, no specific requirement exists for the inlet filters, we decided to refer to the WHO's definition of inlet filter, i.e., a filter that “filters fine particles to protect compressor and/or valves” (WHO 2020), and to estimate the filtration efficiency of our 3D-printed filter comparing it to the original one, as well as its pressure drop (airflow resistance). To this purpose, a light scattering airborne particle counter (Trotec PC200) was used to sample a volume of 2.83 L in 60s, i.e., the maximum allowed by the device, by connecting it to the filter via a 3D-printed junction.
The experiments were undertaken in a normal environment, subject to no air filtering nor air pollution control. The actual flow of air generated by the device was measured in different conditions, i.e., alone, with the original filter and with the Warwick filter, in order to adjust the filtration efficiency calculations according to the sampled volume. In fact, different filters will introduce different pressure drops, affecting the overall flow. In order to quantify the real flow and the pressure drop through each filter, a gas flow analyser (Fluke VT650) was used in series with the filter and the particle counter.
Since the above-mentioned standards refer to the number of particles per m3, we estimated the number of particles in 1 m3 by multiplying our values by 1000 (in fact, 1 m3 equals 1000 L) and dividing by the respective volume sampled in 60 s (measured with the flowmeter). In order to make the measurements more reliable, 10 subsequent measurements were taken both using the original filter and our solution. Moreover, 10 measurements of the air of the room were taken similarly and dispersed through the filter experiments, i.e., a few at the start, a few in the middle and a few in the end, to have a reliable measurement of the “pollution” of the background.
Data were averaged, and the filtration efficiency was calculated as follows ( stands for filtration efficiency, Particles in the ambient, residual particles coming out of the filter):
In the end, additionally, a similar procedure was performed to measure the gas outputted by the oxygen concentrator with either the original filter or our solution installed.
3. Results
3.1. Design and manufacturing
The data from the micro-CT scanner was selected to model the filter due to the data being less noisy, more accurate, and due to the additional compounded errors, that are introduced during the post processing stage of 3D handheld scanning, such as the global and manual data registrations. Fig. 4b shows the 3D model of the final filter, devised as two separate parts, i.e., the base and the lid.
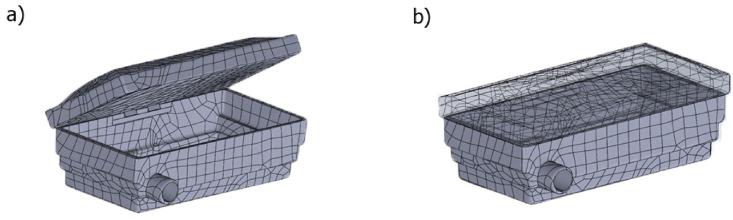
Some simulations were run on this model using finite element methods analysis, the results of which can be found in Fig. 5, Fig. 6 . From this analysis, it resulted that when impacted by reasonable expected force, the filter casing performs adequately well, presenting around the point of impact acceptable stress and strain levels (note that ABS plastic has a yield strength of 29.6–48Mpa). These low values imply that deformation levels will be minimal, meaning that the efficacy of the filter will be unaffected by the impact, as the filter casing will still be able to fit into its assigned slot on the oxygen concentrator completely. The simulation also confirms the suitability of ABS plastic as the material for the prototype, as ABS material properties were applied to the model before applying the force. The simulation results (Fig. 5, Fig. 6) highlight the most likely failure points by displaying the regions of greatest stress (shown in red), however, even at these points the stress values were well within acceptable limits. Finally, Fig. 7 shows the 3D printed filter casing, filled with the filter material.
Fig. 5.
The results of the simulation, Von Mises stresses.
Fig. 6.
The results of the simulation, resulting displacement (URES).
Fig. 7.
The 3D printed filter with the filtering material inside.
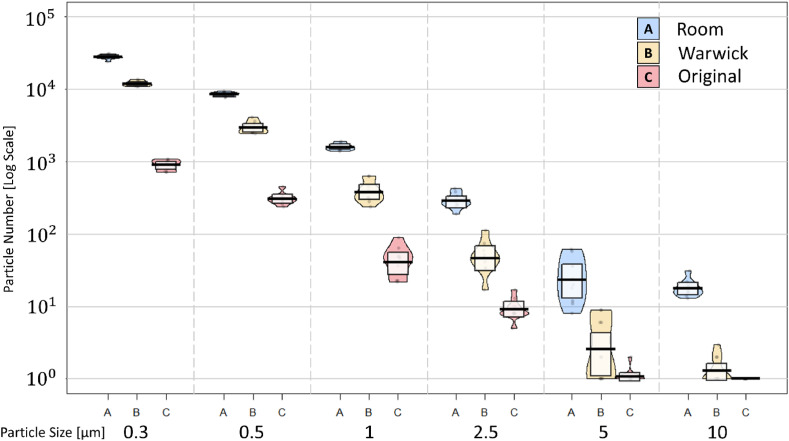
3.2. Bench tests
The results from the bench tests are summarised in Fig. 8 and Table 3 . Fig. 8 reports the pirateplots for the distributions of the particles per particle size, comparing the different filters. It can be noted that, both filters effectively produced a significant reduction in the number of particles with respect to those naturally present in the test room.
Fig. 8.
The pirateplots for the distribution of the particles per particle size for the Warwick filter (Yellow), the Original filter (Pink), and the room (Light blue).
Table 3.
The table reports the average number of particles per m3 per particle size as well as the total and the filtration efficiency. The total filtration efficiency is presented outside of the brackets; the filtration efficiency on particles greater than or equal to 1 μm is between brackets.
| Particle size (MICRONS) | Average particles per M3 - Room | Average particles per M3 - Original | Average particles per M3 – Warwick |
|---|---|---|---|
| 0.3 | 9.94E+06 | 3.55E+05 | 6.49E+06 |
| 0.5 | 3.00E+06 | 1.22E+05 | 1.61E+06 |
| 1 | 5.66E+05 | 1.77E+04 | 2.15E+05 |
| 2.5 | 1.04E+05 | 3.73E+03 | 2.81E+04 |
| 5 | 1.01E+04 | 7.84E+01 | 1.84E+03 |
| 10 | 6.46E+03 | 1.18E+02 | 5.95E+02 |
| Total | 1.36E+07 | 4.99E+05 | 8.34E+06 |
| Filtration efficiency | 96.3% (96.9%) | 38.8% (64.2%) |
The detailed distribution of such particles is available in Table 3, which reports their average number per m3 per particle size, and the resulting filtration efficiency, adjusted according to the actual flow. In fact, from the measurements of the flow it resulted that the flows were: 2.83 L per minute without any filter, 2.55 with the original filter and 1.85 with the Warwick filter, respectively. This was due to the airflow resistance linked to the presence of filtering material, which can be estimated by the pressure drop induced by each filter. In particular, the pressure drop related to the use of the Warwick filter was 0.035 mmHg, that linked to the use of the original filter was 0.011 mmHg. The relative pressure increase, due to the more resistance offered to the airflow by the activated charcoal granules, is 0.024 mmHg (0.0032 kPa). This small increase is negligible when compared to the capacity of oxygen concentrators of generating at least 55 kPa at all flows, to overcome pressure drops linked to long oxygen delivery tubing (WHO 2016).
Table 3 also reports both the overall filtration efficiency and the filtration efficiency for particles greater than or equal to 1 μm. This is because, by observing the reduction of the particles induced by the Warwick filter, it can be noted that it is more effective for those particle sizes. Although the overall filtration efficiency is 38.8% (compared to the 96.3% of the original filter), in fact, the filtration efficiency for particles over 1 μm is almost double, i.e., 64.2% (96.9% for the original filter).
As regards the tests done on the whole system, i.e., oxygen concentrator with different inlet filters installed and the same original micro-filter installed, the output gas was of ISO Class 5 quality for particles greater than 1 μm, as required by ISO BS EN ISO 80601-2-69:2020 (Medical electrical equipment. Particular requirements for the basic safety and essential performance of oxygen concentrator equipment). In fact, on average, the system with the original filter installed presented 0 particles per m3, while that with the Warwick filter installed 177, both much lower than the limit, i.e., 832.
4. Discussions and conclusions
This paper presented the design and technical validation of a 3D-printed activated charcoal filter for oxygen concentrators. One of the core aims of this project, was to set out a sample process that can be followed by others, particularly in LRSs. The design started with a reverse engineering phase through the use of both a 3D handheld scanner and micro-CT scanning in order to obtain essential dimensional data for the specific housing within the selected oxygen concentrators (EverFlo). Ideally, Handheld scanners appear adequate for small scale MDs as the scanning object is small by definition, and the scan data does not need to be as detailed as the data obtained when using slower but more accurate scanners such as Computed Tomography (CT) scanners. Results showed, indeed, that the sets of data from both scanning techniques resulted to be highly accurate and more than suitable for this application. However, the latter gave less noisy and more detailed results and was selected for our application. The most important advantage that this method has over 3D handheld scanning is its ability to capture internal data, without having to move or damage any parts. Given the high costs of micro-CT scanners and probably lower availability in LRSs, 3D scanning should be used instead. Although the CT data is less noisy and will contain less error, handheld scanning data is still more than acceptable for this application. It is only when dealing with MDs that require extreme levels of precision, for example medical stents, that the extremely minimal error of CT scanning becomes a determining factor. It is important to note that in most applications, handheld scanning still delivers highly accurate, low error data, just not quite as good as CT scan data. Therefore, as both scanning techniques were more than adequate for this application, other factors (bearing in mind LRS applications) determined the final selection of handheld 3D scanning. These factors included cost, amount of training required to operate, ease of maintenance, portability and the - size of the two scanners. While handheld scanning was recommended for LRS after comparing the data sets, validating the applicability of micro-CT methods opens avenues for future MDs research, design and local manufacture, as it is able to obtain high resolution internal structure data through non-invasive means. 3D-printing, given its advantages and the wide availability of 3D printers, was selected to manufacture the prototypes of our filter casing. Nonetheless, despite being less accurate, the handheld scanning data would have been adequate for the external body data, and as the technique is cheaper, faster and more accessible, is to be considered for future real applications of this manufacturing method.
Another essential step was to select and produce the filtering material. After careful considerations, activated charcoal resulted to be the best option, given its high impurity-absorbing capacities and its easy production. In fact, although primarily manufactured in large quantities, activated carbon can also be locally manufactured in small quantities, with a minimal cost and without the need of any expensive equipment, such as the large vats used by manufacturers when making activated carbon in bulk. This manufacturing method presented in method section allows producing activated charcoal in any kind of setting by using commonly available materials, such as wood and lemon juice. It is ideal for this project as only a small amount of activated carbon will be required for an oxygen concentrator inlet filter, and the same method can easily be carried out by facilities in LRS to due to the methods’ low cost and accessibility. Furthermore, the wide availability and affordability of 3D printers make this design adapt for lower resource settings, keeping to the project aim to create a filter that is entirely locally manufacturable.
Four 3D printers were compared to select the one that meet the essential requirement for our application. Overall, it would be unreasonable for a 3D printer to be obtained just to manufacture replacement filters for oxygen concentrators, but as already covered in this report 3D printers can be used in multiple different medical applications, particularly the manufacturing of small-scale MDs. Finally, the 3D printer Fortus 360mc (or an equivalent model) was selected as it was considered more useful to a LRS setting medical facility. It resulted cheaper than the other options, and it swaps the ability to print in resin for other advantages more applicable to MD manufacturing, such as interchangeable printing tips of various sizes, and a larger build area. Finally, another important step was to technically validate our device, by assessing its performance and comparing it against that of a commercial inlet filter for oxygen concentrators. Overall, the results of this phase are satisfactory. In particular, it resulted that the Warwick filter has a mediocre overall filtration efficiency and performs even better on all the particles over 1 μm. Although the performance is not comparable to the Original filter, it is still a satisfactory result, because the aim of the inlet filter is that of filtering out the gross particles to provide a cleaner airflow to the concentrating means of oxygen concentrator. It is then the second filter, i.e., the output filter that further purifies the oxygen-enriched airflow. Currently, only the oxygen-enriched gas outputted by the oxygen concentrator, downstream of all the filters, is regulated by relevant standards. In fact, while output filters should be high-efficiency particulate arrestance filters, according to the WHO Technical Specifications for oxygen concentrators, there is no specification or no specific standard for inlet filters. This highlights the current inadequacy and/or incompleteness of some existing standards and regulatory frameworks, as reported and explained in another publication (Pecchia et al., 2020) concerning personal protective equipment.
For these reasons, the filtration efficiency provided by this prototype, i.e., 38.8% overall, and 64.2% at particles equal to or greater than 1 μm, is a good result, as its use as well as its much easier supply and servicing would indefinitely extend the lifespan of the output filter, as well as of the oxygen concentrator, in respect to no inlet filter at all, or to an overused paper-based one. This envisioned specific clinical benefit can only be confirmed by an in-loco clinical evaluation, in which several prototypes could be trialled in existing oxygen concentrators working in typically harsh environments of LRSs. This could be potentially done in those healthcare locations of LRSs, which already receive (or could benefit from) the support of local universities/research centres. Such centres could be the local incubators for small enterprises that could provide the local health centres with the novel production of 3D-printed activated charcoal inlet filters.
Before such clinical evaluations, the filter prototypes could also be challenge tested by measuring their performance and filtration efficiency in simulated harsher environments, i.e., labs with the possibility control cycles of high temperatures and humidity, as well as the amount of “pollution particles” present. However, such labs are not available at the University of Warwick and not trivial to reproduce. Thus, such “extreme” tests were not taken into consideration for this particular study. Should there be the opportunity to access such labs, further tests could be performed. As presented in a previous publication, in fact, the reliance on external factors, as well as other domains, should be taken into considerations when designing MDs for LRSs (Piaggio et al., 2021).
As the filtering material choice was limited to one, i.e., activated charcoal, due to its ease of production, other filtering materials, on the conditions that they are widely available in LRSs, could also be individuated and investigated in further experiments. Possibly, in the current circumstances (i.e., COVID-19 pandemic) one could leverage the wide distribution of either surgical masks, cloth masks, or FFP2 respirators, to use them as filtering material. As regards different inlet filters of oxygen concentrators of different makes, the same exercise of scanning, remodelling, and 3D-printing could be performed on them, too. Ideally, there could be a shared database or open-source platform, where such scans and models could be uploaded, or where different experts from across the world could collaborate towards the creation of a novel inlet filter for a specific oxygen concentrator.
One final consideration about the filter concerns the fluid dynamics within the filter, i.e., how and where the air will flow within the filter through and around the filtering media. This study did not investigate such matter, and, thus, did not look into the optimisation of the filter shape or filtering media shape/disposition. However, further studies could also investigate the enhancement of the design of a filter based on such considerations, relying on FEM simulations.
Beyond presenting our activated charcoal filter, this paper wants to introduce a reproducible approach for designing, prototyping and manufacturing spare parts of MDs, particularly feasible for LRSs. The empowerment of local realities with ad-hoc technological centres within universities, private companies or hospitals, equipped with 3D printers, protocyclers and skilled staff, can improve the quality of life and healthcare, by bypassing an often inexistent/poor supply chain. Such centres could also be supported by/cooperate with centres set in higher resource settings, which could rely on costly technologies, such as the CT scanner. In that case, the centre with such technologies available could be in charge of the scanning (and the CAD modelling, if needed) of the filter, which could then be shared through open-source platforms.
Furthermore, the reliance of these local production centres on protocyclers would allow the introduction of resource recycling and reuse, and the reduction of the environmental impact, following a circular economy approach, which is suitable to the typical approach of LRSs of reutilising the few available resources.
However, it is worth reminding that our envisioned solution, i.e., both the filter and its local production, should not be the first choice, in case the healthcare locations, in which they would be used, can rely on working agreements with manufacturers for the prompt delivery of spare parts and maintenance, as well as on non-harsh environmental conditions.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
All the data and materials are available upon reasonable request.
Funding
D. Piaggio and L. Pecchia received funding from the University of Warwick with two Warwick Impact Found grants supported by the EPSRC Impact Accelerator Award (EP/K503848/1 and EP/R511808/1).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Footnotes
References
- Andellini M., De Santis S., Nocchi F., Bassanelli E., Pecchia L., Ritrovato M. Clinical needs and technical requirements for ventilators for COVID-19 treatment critical patients: an evidence-based comparison for adult and pediatric age. Health Technol. 2020;10(6):1403–1411. doi: 10.1007/s12553-020-00467-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arasaratnam A., Humphreys G. Emerging economies drive frugal innovation. World Health Organization. Bulletin of the World Health Organization. 2013;91(1):6. doi: 10.2471/BLT.13.020113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beroza A. 2019. (3D printing IN low resource healthcare settings: analysis OF potential implementations). [Google Scholar]
- Bhisey R. Portable oxygen concentrators market: covid-19 impact on global market demand, opportunities, and analysis & forecast to 2026. 2020. https://www.biospace.com/article/portable-oxygen-concentrators-market-covid-19-impact-on-global-market-demand-opportunities-and-analysis-and-forecast-to-2026/ Retrieved 26/02/2021, from.
- Bradley B., Light J., Ebonyi A., N'Jai P., Ideh R., Ebruke B., Nyassi E., Peel D., Howie S. Implementation and 8-year follow-up of an uninterrupted oxygen supply system in a hospital in the Gambia. Int. J. Tubercul. Lung Dis. 2016;20(8):1130–1134. doi: 10.5588/ijtld.15.0889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley B., Light J., Singhateh B., Koli D., Peel D., Cheng Y.-L., Howie S. 7th International Conference on Appropriate Healthcare Technologies for Developing Countries. IET; 2012. Temperature and humidity trends in a health centre in the Gambia: implications for back up battery-life in tropical settings. [Google Scholar]
- Bradley B.D., Chow S., Cheng Y.-L., Nyassi E., Howie S.R., Peel D. WHO Second Global Forum on Medical Devices; Geneva, Switzerland: 2013. The Use of Oxygen Concentrators in the Gambia: A Study of over 5 Years of Experience in. [Google Scholar]
- Bradley B.D., Chow S., Nyassi E., Cheng Y.-L., Peel D., Howie S.R. A retrospective analysis of oxygen concentrator maintenance needs and costs in a low-resource setting: experience from the Gambia. Health Technol. 2015;4(4):319–328. [Google Scholar]
- Chawla S., Kurani S., Wren S.M., Stewart B., Burnham G., Kushner A., McIntyre T. Electricity and generator availability in LMIC hospitals: improving access to safe surgery. J. Surg. Res. 2018;223:136–141. doi: 10.1016/j.jss.2017.10.016. [DOI] [PubMed] [Google Scholar]
- Di Pietro L., Piaggio D., Oronti I., Maccaro A., Houessouvo R.C., Medenou D., De Maria C., Pecchia L., Ahluwalia A. A framework for assessing healthcare facilities in low-resource settings: field studies in Benin and Uganda. J. Med. Biol. Eng. 2020:1–9. [Google Scholar]
- Dillon E.C., Jr., Wilton J.H., Barlow J.C., Watson W.A. Large surface area activated charcoal and the inhibition of aspirin absorption. Ann. Emerg. Med. 1989;18(5):547–552. doi: 10.1016/s0196-0644(89)80841-8. [DOI] [PubMed] [Google Scholar]
- Friesen R., Raber M., Reimer D. Oxygen concentrators: a primary oxygen supply source. Can. J. Anesth. 1999;46(12):1185. doi: 10.1007/BF03015531. [DOI] [PubMed] [Google Scholar]
- Gauthier A.K., Cruz G., Medina L., Duke S. IIE Annual Conference. Proceedings, Institute of Industrial and Systems Engineers (IISE); 2013. Design factors for medical device functionality in developing countries. [Google Scholar]
- Howie S.R., Ebruke B.E., Gil M., Bradley B., Nyassi E., Edmonds T., Boladuadua S., Rasili S., Rafai E., Mackenzie G. The development and implementation of an oxygen treatment solution for health facilities in low and middle-income countries. J. Global Health. 2020;10(2) doi: 10.7189/jgh.10.020425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan W.A., Ritz L.S., Vitello M. Local production of medical technologies and its effect on access in low and middle income countries: a systematic review of the literature. South Med. Rev. 2011;4(2):51–61. doi: 10.5655/smr.v4i2.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks I.H., Thomas H., Bakhet M., Fitzgerald E. Medical equipment donation in low-resource settings: a review of the literature and guidelines for surgery and anaesthesia in low-income and middle-income countries. BMJ Glob Health. 2019;4(5) doi: 10.1136/bmjgh-2019-001785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medenou D., Fagbemi L.A., Houessouvo R.C., Jossou T.R., Ahouandjinou M.H., Piaggio D., Kinnouezan C.-D.A., Monteiro G.A., Idrissou M.A., Iadanza E. Medical devices in sub-Saharan Africa: optimal assistance via a computerized maintenance management system (CMMS) in Benin. Health Technol. 2019;9(3):219–232. [Google Scholar]
- Nubie S. How to make activated charcoal (with pictures) https://homesteadsurvivalsite.com/make-activated-charcoal/ Retrieved 26/02/2021, from.
- Oberk How different seals work and best applications of each. 2021. https://www.oberk.com/packaging-crash-course/dispensing-closures-sealing-systems Retrieved 22/02/2021 from.
- Pecchia L., Piaggio D., Maccaro A., Formisano C., Iadanza E. The inadequacy of regulatory frameworks in time of crisis and in low-resource settings: personal protective equipment and COVID-19. Health Technol. 2020:1. doi: 10.1007/s12553-020-00429-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piaggio D., Castaldo R., Cinelli M., Cinelli S., Maccaro A., Pecchia L. A framework for designing medical devices resilient to low-resource settings. Glob. Health. 2021;17(1):1–13. doi: 10.1186/s12992-021-00718-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piaggio D., Medenou D., Houessouvo R.C., Pecchia L. International Conference on Medical and Biological Engineering. Springer; 2019. Donation of medical devices in low-income countries: preliminary results from field studies. [Google Scholar]
- Rismani S., der Loos V., Machiel H. 2015. (The competitive advantage of using 3D-printing in Low-resource healthcare settings). [Google Scholar]
- Shah M.T., Joshipura M., Singleton J., LaBarre P., Desai H., Sharma E., Mock C. Assessment of the availability of technology for trauma care in India. World J. Surg. 2015;39(2):363–372. doi: 10.1007/s00268-014-2805-7. [DOI] [PubMed] [Google Scholar]
- UN Transforming our world: the 2030 agenda for sustainable development. 2020. https://sustainabledevelopment.un.org/post2015/transformingourworld Retrieved 22/02/2021.
- WHO . WHO; Geneva, Switzerland: 2010. Barriers to Innovation in the Field of Medical Devices. [Google Scholar]
- WHO . World Health Organization; 2016. Technical Specifications for Oxygen Concentrators: WHO Medical Device Technical Series. [Google Scholar]
- WHO . World Health Organization; 2020. Technical Specifications for Invasive and Non-invasive Ventilators for COVID-19: Interim Guidance, 15 April 2020. [Google Scholar]
- WHO The life-saving power of medical oxygen. 2021. https://www.who.int/news-room/feature-stories/detail/the-life-saving-power-of-medical-oxygen Retrieved 26/02/2021, from.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data and materials are available upon reasonable request.