Abstract
Objectives:
To present the consensus statements with supporting literature for plasma and platelet transfusions in critically ill neonates and children with malignancy, acute liver disease and/or following liver transplantation, and sepsis and/or disseminated intravascular coagulation (DIC) from the Transfusion and Anemia EXpertise Initiative – Control/Avoidance of Bleeding (TAXI-CAB).
Design:
Systematic review and consensus conference of international, multidisciplinary experts in platelet and plasma transfusion management of critically ill children.
Setting:
Not applicable.
Patients:
Critically ill neonates and children with malignancy, acute liver disease and/or following liver transplantation, and sepsis and/or DIC
Interventions:
None
Measurements and Main Results:
A panel of 13 experts developed evidence-based and, when evidence was insufficient, expert based statements for plasma and platelet transfusions in critically ill neonates and children with malignancy, acute liver disease and/or following liver transplantation, and sepsis and/or DIC. These statements were reviewed and ratified by the 29 TAXI-CAB experts. A systematic review was conducted using MEDLINE, EMBASE, and Cochrane Library databases, from inception to December 2020. Consensus was obtained using the Research and Development/University of California, Los Angeles (UCLA) Appropriateness Method. Results were summarized using the Grading of Recommendations Assessment, Development, and Evaluation method. We developed 12 expert consensus statements.
Conclusions:
In the TAXI-CAB program, the current absence of evidence for use of plasma and/or platelet transfusion in critically ill children with malignancy, acute liver disease and/or following liver transplantation, and sepsis, means that only expert consensus statements are possible for these areas of practice.
MeSH Terms: platelet transfusion, plasma, transfusion, hemostasis, critical illness, child, sepsis, oncology, malignancy, liver transplant, evidence based guidelines
INTRODUCTION
Platelet and plasma transfusions are commonly administered to neonates and children admitted to pediatric intensive care units (PICUs), especially those with malignancy, acute liver disease, and sepsis [1–3]. Plasma and platelet transfusions may be given to prevent or treat active bleeding attributable to acquired coagulation factor deficiencies or thrombocytopenia. Recent studies demonstrate that most transfusions are prescribed as prophylaxis to non-bleeding children with limited evidence demonstrating beneficial effect. At present, clinical practice is largely based on expert consensus and adult studies [4–7]. Extrapolation of adult results to pediatric settings may be inappropriate given the differences in underlying diagnoses, coagulation systems [8, 9], and the likelihood of bleeding [10].
There are concerns about short and long-term complications of transfusion in children. In the PICU, the rate of acute transfusion reaction (ATR) is 2%, [11] and children are more likely to experience an ATR as compared to adults [12–14]. In the PICU, plasma transfusions are associated with increased length of stay, nosocomial infections and multi-organ failure (MOF) and mortality [15]. For children with leukemia, the number of transfusions received is an independent risk factor for poor survival [16]. Given these risks, short and long-term risks and benefits of platelet and plasma transfusions should be carefully considered prior to use.
The objective of this study was to develop evidence-based recommendations, or expert-based consensus statements when there was insufficient evidence for recommendations, to address the following question: For critically ill neonates and children (i.e., those admitted to the intensive care unit) with malignancy, acute liver disease and/or following liver transplantation, and sepsis, what strategies are used when ordering plasma or platelet transfusions to prevent or treat bleeding?
METHODS
The search strategy, item selection and recommendation generation used to identify and select references for systematic review and to develop recommendation are detailed in the general manuscript of TAXI-CAB [17]. Briefly, we searched Ovid MEDLINE®, Ovid EMBASE, and Cochrane Library (Wiley) from inception through December 2020 using a combination of medical subject heading terms and text words to define concepts of plasma or platelet transfusion, transfusion triggers, laboratory tests to assess efficacy of transfusion in children admitted to the pediatric intensive care unit (PICU) malignancy, acute liver disease and/or following liver transplantation, and sepsis and/or DIC. For articles selected for inclusion, reference lists and citing articles were selected from Scopus (Elsevier) and screened. Two reviewers independently reviewed all citations and performed data extraction and assessments of bias. Literature was reviewed for relevance to this subgroup. Research Electronic Data Capture (REDCap) hosted at Weill Cornell Medicine was used for standardized data extraction. We used a standardized data extraction form to construct evidence tables and graded the evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system [18].
Thirteen experts participated in the development of recommendations from this subgroup. A panel of 29 experts convened in an on-line format over 18 months to develop good practice statements, recommendations and, when evidence was lacking, expert consensus statements. Good practice statements are those in which there is high-level of certainty that the practice will do more good than harm, but there is little in the way of supporting literature evidence. Expert consensus statements are based on the expert opinion of the group, but in areas where research is likely needed. All statements from each subgroup were reviewed by the full panel of experts and voted on using the Research and Development/University of California, Los Angeles (UCLA) Appropriateness Method. Agreement was defined a priori as >80% of all experts. The recommendations and statements are intended to apply to infants, children and adolescents. Malignancy included children receiving chemotherapy or radiation for either solid tumors or hematological malignancies within the previous six months or receipt of hematopoietic stem cell transplant (HSCT) within the previous year. Sepsis, DIC and acute liver failure were defined in the citations [19]. Acute liver failure includes fulminant liver failure and acute on chronic liver failure. Bleeding definitions included the World Health Organization (WHO) bleeding classification or the Bleeding Assessment Scale in critically Ill Children (BASIC) scale [20,21]. Prophylactic transfusions are those prescribed to patients at risk of bleeding, whereas therapeutic transfusions are given to those with active bleeding.
RESULTS
Searching 1) malignancy, 2) acute liver failure/liver transplantation and 3) sepsis/DIC, identified 1) 3076, 2) 2677, and 3) 3028 abstracts, respectively. After duplicates were removed, a total of 1) 2653, 2) 2332, and 3) 2600 abstracts were screened. Then, out of 1) 162, 2) 52, and 3) 86 full text manuscripts about malignancy, acute liver failure/liver transplantation, and sepsis/DIC respectively, we selected 1) 6, 2) 3, and 3) 8 papers for detailed review (see Figures 1–3). These papers underwent data extraction and assessment of bias in order to generate recommendations and statements (see Supplemental Data Tables 1–3); twelve expert consensus statements were produced. The voting data, including the number of voting experts and median score, are provided for each statement and recommendation.
Figure 1.

Papers Flow Chart Critically ill children with malignancy
Figure 3.

Papers flow chart for critically ill children with sepsis and/or DIC
Indications for Plasma and Platelet Transfusions in Critically Ill Children with Malignancy
1. In critically ill neonatal or pediatric oncology/HSCT patients, there is insufficient evidence to make a recommendation regarding specific indications or transfusion strategies to direct plasma and platelet transfusion. 95% Agreement (n=22), Median 8, IQR 7.75–9.
2. In critically ill pediatric oncology/HSCT patients, prophylactic platelet transfusions might be considered for a platelet count < 10 × 109/L (10,000/mm3). 100% Agreement (n=22), Median 8, IQR 7–9.
Rationale:
There are few studies that provide evidence to guide prophylactic platelet indications in children with leukemia and none in critically ill oncology children. The guidance for transfusion with mild or no bleeding and a pre-transfusion platelet threshold of < 10×109/L has been extrapolated from limited adult and pediatric oncology literature [22–25] and published guidelines [7, 26–31]. Randomized controlled trials (RCTs) performed in adults and children demonstrated that a prophylactic platelet transfusion threshold of 10×109/L is as safe as thresholds of 20×109/L [23, 25, 32] or 30×109/L [33] and is not associated with increased bleeding risk. The two largest RCTs performed in adults and adolescents reported no difference in mortality when transfusing platelets prophylactically at a threshold of 10×109/L compared with only transfusing for therapeutic indications [22, 34], although higher rates of WHO grade 2 to 4 bleeding events occurred in the therapeutic platelet transfusion groups. A Cochrane review reported that a therapeutic-only platelet transfusion strategy was associated with increased risk of bleeding, but a reduced number of platelet transfusions per patient [35]. The suggestions for a prophylactic over therapeutic transfusion approach in critically ill oncology patients was developed, recognizing the optimal threshold for prophylactic transfusion in these patients has not been identified.
3. In critically ill pediatric oncology/HSCT patients, therapeutic platelet transfusions might be considered for moderate or severe bleeding. 82% Agreement (n=22), Median 8, IQR 7–9.
Rationale:
Bleeding is commonly encountered in the pediatric critical care patient. An observational study of 405 children, reported that 9% experienced clinically relevant bleeding and platelets were transfused in 16% with a median (IQR) platelet count 181 (108–257) ×109/L [36]. Oncology patients represent a common cohort of patients who receive platelet transfusions in the PICU [2, 37]. A recent point prevalence study of platelet transfusion practice of 237 inpatient PICU oncology patients, found that 30% of transfusions were administered for therapeutic indications (major bleeding 9%, minor bleeding 16%) at a median (IQR) pre-transfusion platelet count of 56 (37–89) ×109/L and that 60% were administered prophylactically at thresholds of >20 ×109/L [2]. This study could not establish any association of platelet transfusions with improvement in bleeding outcomes. No additional studies have evaluated the role of therapeutic platelet transfusions to treat bleeding in critically ill oncology patients with thrombocytopenia.
Minimum platelet count is a frequently employed indicator of bleeding risk in both pediatric and adult oncology patients [38–41]. Even with prophylactic platelet transfusions, some children will still experience moderate to severe bleeding events [10, 24, 41]. Children may have an increased rate of bleeding compared to adults. A sub-analysis of pediatric patients (n =198) within the Platelet Dose Optimization (PLADO) trial demonstrated that children experienced additional days with bleeding and a higher rate of WHO (≥ grade 2) bleeding (p<0.001) compared to adults. These findings were more marked in younger children undergoing HSCT and interpreted to be a consequence of aggressive pediatric therapy regimens. In addition, different patterns of bleeding were seen, with more oropharyngeal and gastrointestinal bleeding [10].
A number of guidelines suggest more generous platelet transfusion strategies with higher thresholds in children with malignancy in the presence of perceived risk factors for bleeding [7, 27, 28, 30]. Some pediatric oncology guidelines recommend a threshold of 40×109/L in the presence of fever, hyperleukocytosis, a rapid fall in platelet count, coagulopathy, acute promyelocytic leukemia, critical illness and/or impaired platelet functions [28]. However, other pediatric transfusion guidelines suggest higher thresholds when a child is clinically unstable and/or bleeding, targeting 20×109/L in the context of sepsis, severe mucositis, DIC and anticoagulant therapy. Australian guidelines advise a threshold of < 20×109/L with risk factors such as fever or minor bleeding [7]. French Intensive Care guidelines advise platelet transfusions, without specifying a threshold, in critically ill patients with iatrogenic thrombocytopenia after chemotherapy when there are signs of bleeding [26].
Our expert consensus statement to consider platelet transfusions to pediatric oncology patients with moderate to severe bleeding took into context the high rates of clinically significant bleeding seen in pediatric oncology patients, the different patterns of bleeding compared to adults [10], the results of RCTs performed in both pediatric and adult patients and guidance provided from international guidelines [10,22,24,34,41]. Although platelets may be beneficial in bleeding patients, a specific pre-transfusion platelet threshold could not be provided in the consensus statement.
4. In critically ill pediatric oncology/HSCT patients, prophylactic plasma transfusions for minor coagulopathy (INR ≤ 1.5, aPTT ≤ 1.5) may not be beneficial unless performing surgery in a critical site (orbit, brain, facial nerve, spinal column, etc.). 86% Agreement (n=22), Median 8, IQR 7–9.
Rationale:
In general, plasma is transfused to critically ill oncology patients for two reasons: to correct coagulation factor deficiencies in actively bleeding patients (therapeutic transfusions) or to prevent bleeding before invasive procedures or surgeries (prophylactic transfusions) [3,42]. Literature about adult patients reports that minor abnormalities in INR or PT are poorly predictive of bleeding [43] and may not correct with plasma transfusion [3,44,45]. Studies in children have demonstrated that plasma transfusion to treat minor or moderate coagulopathy result in only modest INR changes [3,42].
Multiple observational studies note that plasma transfusions are associated with an increased risk of respiratory failure, multiorgan failure (MOF), and prolonged PICU length of stay [15]. Given these risks and limited evidence of benefit, prophylactic plasma transfusions for minor coagulopathy may not be beneficial. Consensus statements could not be made regarding plasma transfusion in bleeding oncology patients due to sparse published literature. The risks of pre-surgical plasma transfusions need to be weighed against the child’s underlying co-morbidities, severity of illness, etiology of the coagulopathy, type of surgical procedure, risk of bleeding, and additional hemostatic measures. Formal hematology consultation is advised prior to any surgery if a coagulopathy is suspected.
Indications for Plasma or Platelet Transfusions in Critically Ill Infants or Children with Acute Liver Failure or Following Liver Transplantation
5. In critically ill pediatric patients with acute liver failure and/or following liver transplantation, there is insufficient evidence to make a recommendation regarding the specific indications or transfusion strategies to direct plasma or platelet transfusion. 96% Agreement (n=23), Median 8, IQR 8–9.
6. In critically ill pediatric patients with acute liver failure and/or following liver transplantation, prophylactic plasma and platelet transfusions may not be beneficial in the absence of moderate or severe bleeding. 87% Agreement (n=23), Median 8, IQR 7–9.
7. In critically ill pediatric patients with acute liver failure and/or following liver transplantation, restrictive plasma and platelet transfusion strategies might be considered including not treating a laboratory number alone, but taking into consideration the overall clinical hemostatic status of the infant or child. 96% Agreement (n=23), Median 8, IQR 7–9.
Rationale:
Plasma and platelet transfusion decisions in children with acute liver failure or following liver transplantation are complicated by a number of factors including: 1) an inability of standard coagulation tests to predict bleeding; 2) increased risk of thrombosis; 3) difference in the etiology of liver disease between adults and children and the reliance on guidelines from adults; and 4) the scarcity of published data in children with liver disease.
An understanding of coagulopathy in patients with severe acute liver disease has evolved over time. In the past, prophylactic plasma transfusions were administered liberally with the goal of supplementing coagulation factor deficits to prevent significant hemorrhage. The coagulopathy of severe acute liver disease is now believed to be an unstable balance between thrombosis and hemorrhage. The liver has a central role in the hemostatic system as it produces the majority of coagulation factors, anticoagulation factors and fibrinolytic proteins found in plasma. Multiple changes in the hemostatic system are found in patients with liver disease including thrombocytopenia, decreased levels of coagulation factors and anticoagulation proteins, vitamin K deficiency and decreased levels of fibrinolytic proteins. Although routine diagnostic tests of hemostasis may be abnormal, these results do not necessarily indicate an increased bleeding risk [46,47]. Studies in adult patients have shown rebalanced coagulation with normal thrombin generation in the presence of thrombomodulin suggesting acquired Protein C resistance [48]. Bleeding is likely a consequence of many factors including local vascular abnormalities, portal hypertension, increased vascular pressure [49] and/or fluctuation between a hypo- and/or hypercoagulable balance accompanying infections or renal failure [50].
Prior to surgery, these children often present in a hypercoagulable state due to an imbalance between pro- and anticoagulant factors, placing the patient at risk of thrombosis. In addition, the use of plasma to correct INR values alone may falsely affect the prognostication of a child’s condition and ability to list for transplant as scores typically use INR values in their prognostic models [51]. Intraoperative plasma transfusions contribute to the pro-coagulant state, which increases the risk of thrombotic events [52] and acts as an independent risk factor for the development of patient and graft survival and postoperative complications, including acute kidney injury [53–55]. A RCT comparing a restrictive to a liberal transfusion policy (to maintain a low or high central venous pressure) found that the restrictive policy led to a significant reduction in intraoperative blood loss and transfusion requirements [56,57]. A North American survey that identified best practices leading to the lowest hepatic artery thrombosis rate included a restrictive transfusion strategy without prophylactic plasma transfusions [58]. These retrospective data suggests that restrictive plasma transfusion strategies might be considered as plasma transfusion may enhance usual post-operative complications leading to increased morbidity and mortality.
From the limited research available, expert consensus concludes that plasma transfusions do not decrease the overall plasma pro-thrombotic profile and may increase the risk of postoperative thrombosis and hence should not be used prophylactically to prevent bleeding in pediatric patients with acute liver failure or post liver transplantation. Literature that focuses on pediatric liver transplantation patients is sparse and recommendations are based on adult data. Given that the etiology of liver failure in children differs from those of adults, applicability of these suggestions may be limited [57].
To date, no studies have specifically assessed use of platelet transfusions in this population. However, a single center retrospective study found an association between platelet count < 100×109/L (OR 7.92, 95% CI 1.46–43.05) and INR >1.5 (OR 11.62, 95% CI 2.36–57.26) and increased odds of perioperative (including the first postoperative day in the ICU) massive bleeding (defined as blood loss > 1 circulating blood volume) in children undergoing liver transplantation perioperatively [59].
Indications for Plasma or Platelet Transfusion in Critically Ill Children with Sepsis and/or DIC
8. In critically ill pediatric patients with sepsis and/or DIC, there is insufficient evidence to make a recommendation regarding specific indications or transfusion strategies to direct plasma or platelet transfusion. 95% Agreement (n=20), Median 8, IQR 8–9.
Rationale:
The development of recommendations is particularly challenging for neonates and children with sepsis. The 2005 pediatric consensus definition of sepsis is now replaced by the 2020 pediatric surviving sepsis campaign guidelines [60]. There is a range of severity of clinical symptoms related to sepsis, with the degree and severity of DIC and MOF differing between patients on presentation. DIC is a clinico-pathological diagnosis and includes multiple underlying causes and their laboratory features [61]. Our systematic review did not identify RCTs evaluating the effects of plasma transfusions in critically ill children with DIC. Therefore, it is not possible to make a recommendation about using plasma or platelet transfusions to prevent or treat DIC.
9. In critically ill pediatric patients with sepsis and/or DIC, in the absence of moderate or severe bleeding, prophylactic plasma transfusion may not be beneficial. 83% Agreement (n=23), Median 8, IQR 8–9.
10. In critically ill pediatric patients with sepsis and/or DIC and moderate bleeding, plasma transfusion may not be beneficial if the INR is ≤ 1.5. 96% Agreement (n=23), Median 8, IQR 8–9.
Rationale:
Karam et al reported that following plasma transfusion in the PICU, significant decreases in INR were only noted in cases with baseline INR >2.5 and APTT > 60 seconds [3]. INRs of 1.5 – 2.4 showed minimal correction following plasma transfusion, whereas there was no measurable effect for INRs between 0.5 and 1.4. Given this information, practitioners should recognize that plasma transfusions may not be beneficial when children and neonates experience non-severe bleeding (as per BASIC definition) with only minimally abnormal coagulation test results (PTR or INR ≤1.5). Additionally, in critically ill children, observational studies suggest an independent association between plasma transfusions and increased mortality [62], increased odds of MOF, nosocomial infections, and length of stay [15]. Although these studies did not specifically evaluate children with sepsis, decisions to transfuse plasma to children must take into account the risk of bleeding along with the risk of transfusion. This statement is supported by the Surviving Sepsis Guidelines which state: “We suggest against prophylactic plasma transfusion in nonbleeding children with septic shock or other sepsis- associated organ dysfunction and coagulation abnormalities (weak recommendation, very low quality of evidence)” [60].
In the neonatal intensive care unit (NICU), retrospective data confirm that abnormal coagulation results are not associated with an increased risk of bleeding. Christensen et al assessed the relationship between hemorrhage and abnormal coagulation results in neonates (n = 375) and noted that coagulation tests did not independently affect the odds of developing an intraventricular hemorrhage (IVH) [9]. A second study assessed the relationship between plasma transfusion, morbidity and mortality in low birth weight infants. Preterm neonates (N = 776) were randomized to receive plasma, gelatin plasma substitute or dextrose (in saline). No significant difference was noted in IVH rates or short term developmental outcomes [63]. A systematic review (12 RCTs and 1052 neonates) reported no significant improvement in clinical outcomes with plasma compared with colloid or no transfusion [64]. These studies highlight that the current laboratory toolkit used to assess bleeding risk is inadequate and future efforts should focus on different testing platforms.
11. In critically ill pediatric patients with sepsis and/or DIC, in the absence of moderate or severe bleeding, platelet transfusion might be considered when the platelet count is <10 × 109/L (10,000/mm3). 87% Agreement (n=23), Median 8, IQR 7–9.
Rationale:
In general, the pathophysiology related to thrombocytopenia in children with DIC and severe sepsis, leads to massive platelet consumption. The mechanisms that normally tightly regulate thrombin formation become overwhelmed, and thrombin circulates freely causing widespread platelet activation. Platelets are consumed in response to the bleeding associated with DIC. However, DIC can also be associated with thrombosis and, therefore, caution needs to be taken when making decisions regarding both platelet and plasma transfusions. Critically ill septic children consume transfused platelets quickly which may lead to thrombosis and transfusion-associated MOF [65]. In this population, it is unclear whether platelet transfusions lead to improved hemostasis, decreased bleeding risk and/or mortality.
The current literature supports a pre-transfusion platelet threshold of 10×109/L in non-bleeding oncology patients [22–25,34]; there is no specific evidence regarding transfusion threshold for critically ill children with sepsis but it “might be considered” at this threshold as well. Considering platelet transfusions are independently associated with increased mortality in critically ill children [1], it seems reasonable to refrain from transfusing platelets if the platelet count is > 10×109/L, in non-bleeding critically ill children with sepsis. This statement is supported by the Surviving Sepsis Guidelines which state: “We suggest against prophylactic platelet transfusion based solely on platelet levels in non-bleeding children with septic shock or other sepsis-associated organ dysfunction and thrombocytopenia (weak recommendation, very low quality of evidence)” [60].
12. In critically ill pediatric patients with sepsis and/or DIC and moderate bleeding, platelet transfusion might be considered when the platelet count is < 50×109/L (50,000/mm3). 87% Agreement (n=23), Median 8, IQR 7–9.
Rationale:
The consensus opinion that platelet transfusion “might be considered” in critically ill septic children with moderate bleeding and a pre-transfusion platelet count of 50×109/L is based on three types of evidence: our understanding of sepsis related thrombocytopenia; results from a systematic review of adult patient data [66]; and expert consensus statements [26,30,67].
DISCUSSION
The TAXI-CAB collaborative sought to develop recommendations, good practice statements and expert consensus statements about platelet and plasma transfusions in critically ill pediatric patients. Three TAXI-CAB subgroups, oncology/HSCT, acute liver failure/liver transplant and sepsis/DIC, were clustered together because of the overlap in underlying mechanisms of end-organ injury, infection and toxicity. Platelet and plasma products are often administered to these patients with either prophylactic or therapeutic intent. Although there are numerous articles of varying scientific quality exploring transfusion practice, the articles reviewed to develop the consensus are very limited. The most informative studies are two prospective point prevalence studies that provide a snapshot of practice in a large number of PICUs internationally [1,3]. Limitations of these studies to address the questions about transfusion include: 1) lack of pre-transfusion platelet and coagulopathy thresholds specific for oncology, liver failure and septic children; 2) limited data regarding the number of oncologic, liver failure and septic patients who were not transfused; and 3) no correlation between transfusion and outcomes including bleeding and transfusion reactions. Given the limited high quality data, no specific recommendations regarding platelet and plasma strategies for the subgroups of interest could be made. Instead, we developed expert consensus statements based on information from data in adult and neonatal patients.
The practice of declaring “thresholds” as indications for transfusion is suboptimal. Laboratory coagulation values and platelet counts are ex vivo measures applied to in vitro expectations of hemostatic balance. A complex in vitro interaction between circulating procoagulant factors, coagulation inhibitors, fibrinolytic and anti-fibrinolytic factors, platelet functions and breakdown components from all these factors in combination with any underlying vasculopathy and flow/viscosity physics together all determine a patient’s local, regional and global hemostatic balance. Certainly, in the subgroups included in the discussion points, vascular contributions to hemostatic balance are expected to be significant, whether from chemotherapy toxicity, bacterial sepsis or viral hepatitis. Until definitions and measures of functional hemostatic balance are designed, challenges using current laboratory measures as isolated indicators for transfusion will be difficult to overcome and evidence-based recommendations will be difficult to develop.
CONCLUSIONS
Despite the widespread use of platelet and plasma transfusions for critically ill pediatric patients with malignancy, sepsis/DIC and acute liver failure/transplantation, the evidence base underpinning this practice is scarce. This review highlighted the paucity of data which is primarily retrospective in nature.
Supplementary Material
Figure 2.
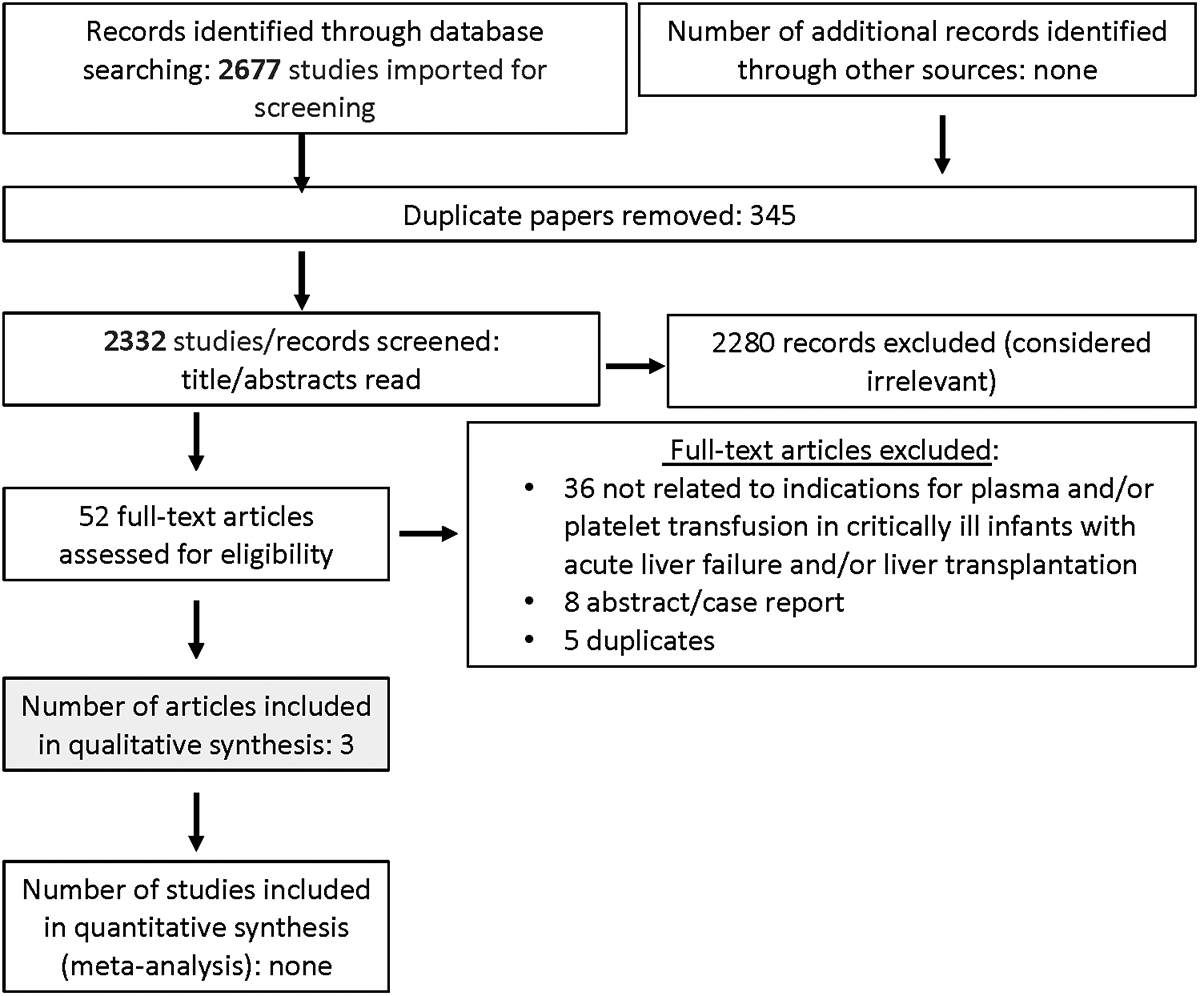
Papers Flow Chart for Critically ill children with acute liver failure and/or liver transplantation
ACKNOWLEDGMENTS
We would like to thank all members of TAXI-CAB for their support and input, especially during the COVID-19 pandemic. In addition, we thank the Chaire Héma-Québec-Bayer en médecine transfusionnelle de l’Université de Montréal, the Society for the Advancement of Blood Management, the Network for the Advancement of Patient Blood Management, Haemostasis and Thrombosis, the International Society of Blood Transfusion, the Society for Critical Care Medicine, and the AABB for their support.
Financial Support:
The Transfusion and Anemia EXpertise Initiative - Control/Avoidance of Bleeding (TAXI-CAB) was supported, in part, by the National Institutes of Health National Heart, Lung and Blood Institute under award number R13 HL154544-01.
Abbreviations:
- DIC
disseminated intravascular coagulopathy
- HSCT
hematologic stem cell transplant
- MOF
multi-organ failure
- NICU
Neonatal intensive care unit
- PICU
Pediatric intensive care unit
- RCT
randomized control study
- TAXI-CAB
Transfusion and Anemia Expertise Initiative – Control/Avoidance of Bleeding
- ATR
acute transfusion reaction
APPENDIX 1. Transfusion and Anemia EXpertise Initiative – Control/Avoidance of Bleeding (TAXI-CAB) Members
(* for executive committee) Co-chairs: Marianne E. Nellis, MD, MS*, Weill Cornell Medicine, New York, NY, and Robert I. Parker, MD*, Renaissance School of Medicine, State University of New York at Stony Brook, Stony Brook, NY; Content Experts: Section 1. Laboratory assays used to assess need for plasma and/or platelet transfusions: Scot T. Bateman, MD*, University of Massachusetts Medical School, Worcester, MA, Meghan Delaney, DO, MPH, The George Washington University Health Sciences, Washington, DC, Kenneth E. Remy, MD, MHSc, MSCI, Washington University of St. Louis, St. Louis, MO, Katherine Steffen, MD, Stanford University, Palo Alto, CA; Section 2. Traumatic brain injury and intracranial hemorrhage: David F. Bauer, MD, MPH, Baylor College of Medicine, Houston, TX, Jacques Lacroix, MD, Université de Montréal, Montreal, QC, Canada, Daniel Nishijima, MD, Davis School of Medicine, Davis, CA; Section 3. Following cardiopulmonary bypass: Jill M. Cholette, MD, University of Rochester Golisano Children’s Hospital, Rochester, NY, Sitaram Emani, MD, Harvard Medical School, Boston, MA, Juan Ibla, MD, Harvard Medical School, Boston, MA, Marie E. Steiner, MD, MS, University of Minnesota, Minneapolis, MN; Section 4. Supported by extracorporeal membrane oxygenation: Melania M. Bembea, MD, PhD, Johns Hopkins University School of Medicine, Baltimore, MD, Jill M. Cholette, MD, University of Rochester Golisano Children’s Hospital, Rochester, NY, Jennifer A. Muszynski, MD, MPH, Nationwide Children’s Hospital, Columbus, OH, Adam M. Vogel, MD, Baylor College of Medicine, Houston, TX; Section 5. Following severe trauma: Susan M. Goobie, MD, Harvard Medical School, Boston, MA, Thorsten Haas, MD, University Children’s Hospital Zurich, Switzerland, Daniel Nishijima, MD, Davis School of Medicine, Davis, CA, Robert T. Russell, MD, MPH, University of Alabama Birmingham, Birmingham, AL, Adam M. Vogel, MD, Baylor College of Medicine, Houston, TX; Section 6. With oncologic diagnosis or following hematopoietic stem cell transplantation: Gemma Crighton, MD, Royal Children’s Hospital, Melbourne, Australia, Ruchika Goel, MD, MPH, Johns Hopkins University, Baltimore, MD, Jacques Lacroix, MD, Université de Montréal, Montreal, QC, Canada, Lani Lieberman, MD, University of Toronto, Canada, Simon J. Stanworth, MD, University of Oxford, UK, Marie E. Steiner, MD, MS, University of Minnesota, Minneapolis, MN; Section 7. With acute liver failure or following liver transplantation: Susan M. Goobie, MD, Harvard Medical School, Boston, MA, Oliver Karam, MD, PhD*, Children’s Hospital of Richmond at VCU, Richmond, VA, Paul A. Stricker, MD, Perelman School of Medicine at the University of Pennsylvania, PA; Section 8. Following non-cardiac surgery: Susan M. Goobie, MD, Harvard Medical School, Boston, MA, Thorsten Haas, MD, University Children’s Hospital Zurich, Switzerland, Marisa Tucci, MD, Université de Montréal, Montreal, QC, Canada, Adam M. Vogel, MD, Baylor College of Medicine, Houston, TX; Section 9. Invasive procedures outside of the operating room: Gemma Crighton, MD, Royal Children’s Hospital, Melbourne, Australia, Jacques Lacroix, MD, Université de Montréal, Montreal, QC, Canada, Robert T. Russell, MD, MPH, University of Alabama Birmingham, Birmingham, AL, Paul A. Stricker, MD, Perelman School of Medicine at the University of Pennsylvania, PA; Section 10. Sepsis and/or disseminated intravascular coagulation: Oliver Karam, MD, PhD*, Children’s Hospital of Richmond at VCU, Richmond, VA, Simon J. Stanworth, MD, University of Oxford, UK, Katherine Steffen, MD, Stanford University, Palo Alto, CA, Stacey L. Valentine, MD, MPH*, University of Massachusetts Medical School, Worcester, MA; Section 11. Product processing and selection: Meghan Delaney, DO, MPH, The George Washington University Health Sciences, Washington, DC, Ruchika Goel, MD, MPH, Johns Hopkins University, Baltimore, MD, Oliver Karam, MD, PhD*, Children’s Hospital of Richmond at VCU, Richmond, VA, Jennifer A. Muszynski, MD, MPH, Nationwide Children’s Hospital, Columbus, OH; Evidence-based medicine: Melania M. Bembea, MD, PhD, Johns Hopkins University School of Medicine, Baltimore, MD, Diana Delgado and Michelle Demetres, Weill Cornell Medicine, New York, NY; Implementation science: Katherine Steffen, MD, Stanford University, Palo Alto, CA.
Footnotes
Copyright Form Disclosure:
Dr. Crighton disclosed that she is employed by the Royal Children’s Hospital of Melbourne, Australia and she was the Australian and New Zealand Society of Blood Transfusion President. Dr. Nellis received support for article research from the National Institutes of Health. Dr. Steiner received funding from PumpKIN DSMB and HealthCore. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Nellis ME, Karam O, Mauer E, et al. Platelet Transfusion Practices in Critically Ill Children. Crit Care Med 2018; 46:1309–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nellis ME, Goel R, Karam O, et al. International Study of the Epidemiology of Platelet Transfusions in Critically Ill Children With an Underlying Oncologic Diagnosis. Pediatr Crit Care Med 2019; 20:e342–e351. [DOI] [PubMed] [Google Scholar]
- 3.Karam O, Demaret P, Shefler A, et al. Indications and Effects of Plasma Transfusions in Critically Ill Children. Am J Respir Crit Care Med 2015; 191:1395–1402. [DOI] [PubMed] [Google Scholar]
- 4.New HV, Stanworth SJ, Gottstein R, et al. British Society for Haematology Guidelines on transfusion for fetuses, neonates and older children (Br J Haematol. 2016;175:784–828). Addendum August 2020. Br J Haematol 2020;191:725–727. [DOI] [PubMed] [Google Scholar]
- 5.New HV, Berryman J, Bolton-Maggs PH, et al. Guidelines on transfusion for fetuses, neonates and older children. Br J Haematol 2016; 175:784–828. [DOI] [PubMed] [Google Scholar]
- 6.Liumbruno G, Bennardello F, Lattanzio A, Piccoli P, Rossetti G; Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) Work Group. Recommendations for the transfusion of plasma and platelets. Blood Transfus 2009; 7:132–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Blood Authority: Patient Blood Management Guidelines: Module 6 - Neonatal and Paediatrics. Available at: https://www.blood.gov.au/pbm-module-6. Accessed March 22, 2021.
- 8.Pal S, Curley A, Stanworth SJ. Interpretation of clotting tests in the neonate. Arch Dis Child Fetal Neonatal Ed 2015; 100:F270–F274. [DOI] [PubMed] [Google Scholar]
- 9.Christensen RD, Baer VL, Lambert DK, Henry E, Ilstrup SJ, Bennett ST. Reference intervals for common coagulation tests of preterm infants (CME). Transfusion 2014; 54:627–632. [DOI] [PubMed] [Google Scholar]
- 10.Josephson CD, Granger S, Assmann SF, et al. Bleeding risks are higher in children versus adults given prophylactic platelet transfusions for treatment-induced hypoproliferative thrombocytopenia. Blood 2012; 120:748–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gauvin F, Lacroix J, Robillard P, Lapointe H, Hume H. Acute transfusion reactions in the pediatric intensive care unit. Transfusion 2006; 46:1899–1908. [DOI] [PubMed] [Google Scholar]
- 12.Stainsby D, Jones H, Wells AW, Gibson B, Cohen H; SHOT Steering Group. Adverse outcomes of blood transfusion in children: analysis of UK reports to the serious hazards of transfusion scheme 1996–2005. Br J Haematol 2008; 141:73–79. [DOI] [PubMed] [Google Scholar]
- 13.Vossoughi S, Perez G, Whitaker BI, Fung MK, Stotler B. Analysis of pediatric adverse reactions to transfusions. Transfusion 2018; 58:60–69. [DOI] [PubMed] [Google Scholar]
- 14.Oakley FD, Woods M, Arnold S, Young PP. Transfusion reactions in pediatric compared with adult patients: a look at rate, reaction type, and associated products. Transfusion 2015; 55:563–570. [DOI] [PubMed] [Google Scholar]
- 15.Karam O, Lacroix J, Robitaille N, Rimensberger PC, Tucci M. Association between plasma transfusions and clinical outcome in critically ill children: a prospective observational study. Vox Sang 2013; 104:342–349. [DOI] [PubMed] [Google Scholar]
- 16.Jaime-Pérez JC, Colunga-Pedraza PR, Gómez-Almaguer D. Is the number of blood products transfused associated with lower survival in children with acute lymphoblastic leukemia? Pediatr Blood Cancer 2011; 57:217–223. [DOI] [PubMed] [Google Scholar]
- 17.Nellis ME, Karam O, Valentine S, et al. Executive Summary of Recommendations and Expert Consensus for Plasma and Platelet Transfusion Practice in Critically Ill Children: From the Transfusion and Anemia EXpertise Initiative – Control/Avoidance of Bleeding (TAXI-CAB). Pediatr Crit Care Med to complete [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed) 2008, 336:924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 2005; 6:2–8. [DOI] [PubMed] [Google Scholar]
- 20.Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer 1981; 47:207–214. [DOI] [PubMed] [Google Scholar]
- 21.Nellis ME, Tucci M, Lacroix J, et al. Bleeding Assessment Scale in Critically Ill Children (BASIC): Physician-Driven Diagnostic Criteria for Bleeding Severity. Crit Care Med 2019; 47:1766–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wandt H, Schaefer-Eckart K, Wendelin K, et al. Therapeutic platelet transfusion versus routine prophylactic transfusion in patients with haematological malignancies: an open-label, multicentre, randomised study. Lancet 2012; 380:1309–1316. [DOI] [PubMed] [Google Scholar]
- 23.Rebulla P, Finazzi G, Marangoni F, et al. The threshold for prophylactic platelet transfusions in adults with acute myeloid leukemia. Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto. N Engl J Med 1997; 337:1870–1875. [DOI] [PubMed] [Google Scholar]
- 24.Murphy S, Litwin S, Herring LM, et al. Indications for platelet transfusion in children with acute leukemia. Am J Hematol 1982; 12:347–356. [DOI] [PubMed] [Google Scholar]
- 25.Zumberg MS, del Rosario ML, Nejame CF, et al. A prospective randomized trial of prophylactic platelet transfusion and bleeding incidence in hematopoietic stem cell transplant recipients: 10,000/L versus 20,000/microL trigger. Biol Blood Marrow Transplant 2002; 8:569–576. [DOI] [PubMed] [Google Scholar]
- 26.Van der Linden T, Souweine B, Dupic L, Soufir L, Meyer P. Management of thrombocytopenia in the ICU (pregnancy excluded). Ann Intensive Care 2012; 2:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schiffer CA, Bohlke K, Delaney M, et al. Platelet Transfusion for Patients With Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 2018; 36:283–299. [DOI] [PubMed] [Google Scholar]
- 28.Barnard D, Portwine C, Members of the C17 Standards and Guidelines Group. Guideline for platelet transfusion thresholds for pediatric hematology/oncology patients. Edmonton, C17 Council and Children’s Cancer & Blood Disorders, 2010. [Google Scholar]
- 29.Nahirniak S, Slichter SJ, Tanael S, et al. Guidance on platelet transfusion for patients with hypoproliferative thrombocytopenia. Transfus Med Rev 2015; 29:3–13. [DOI] [PubMed] [Google Scholar]
- 30.Estcourt LJ, Birchall J, Allard S, et al. Guidelines for the use of platelet transfusions. Br J Haematol 2017; 176:365–394. [DOI] [PubMed] [Google Scholar]
- 31.Kaufman RM, Djulbegovic B, Gernsheimer T, et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann Intern Med 2015; 162:205–213. [DOI] [PubMed] [Google Scholar]
- 32.Heckman KD, Weiner GJ, Davis CS, Strauss RG, Jones MP, Burns CP. Randomized study of prophylactic platelet transfusion threshold during induction therapy for adult acute leukemia: 10,000/microL versus 20,000/microL. J Clin Oncol 1997; 15:1143–1149. [DOI] [PubMed] [Google Scholar]
- 33.Diedrich B, Remberger M, Shanwell A, Svahn BM, Ringdén O. A prospective randomized trial of a prophylactic platelet transfusion trigger of 109/L versus 30 × 109/L in allogeneic hematopoietic progenitor cell transplant recipients. Transfusion 2005; 45:1064–1072. [DOI] [PubMed] [Google Scholar]
- 34.Stanworth SJ, Estcourt LJ, Powter G, et al. A no-prophylaxis platelet-transfusion strategy for hematologic cancers. N Engl J Med 2013; 368:1771–1780. [DOI] [PubMed] [Google Scholar]
- 35.Crighton GL, Estcourt LJ, Wood EM, Trivella M, Doree C, Stanworth S. A therapeutic-only versus prophylactic platelet transfusion strategy for preventing bleeding in patients with haematological disorders after myelosuppressive chemotherapy or stem cell transplantation. Cochrane Database Syst Rev 2015; 9:CD010981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White LJ, Fredericks R, Mannarino CN, Janofsky S, Faustino EVS. Epidemiology of Bleeding in Critically Ill Children. J Pediatr 2017; 184:114–119. [DOI] [PubMed] [Google Scholar]
- 37.Alsheikh B, Chegondi M, Totapally B. Platelet Transfusion Thresholds Among Children Admitted to a Pediatric Intensive Care Unit. Cureus 2017; 9:e1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gaydos LA, Freireich EJ, Mantel N. The quantitative relation between platelet count and hemorrhage in patients with acute leukemia. N Engl J Med 1962; 266:905–909. [DOI] [PubMed] [Google Scholar]
- 39.Uhl L, Assmann SF, Hamza TH, Harrison RW, Gernsheimer T, Slichter SJ. Laboratory predictors of bleeding and the effect of platelet and RBC transfusions on bleeding outcomes in the PLADO trial. Blood 2017; 130:1247–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Slichter SJ, Kaufman RM, Assmann SF, et al. Dose of prophylactic platelet transfusions and prevention of hemorrhage. N Engl J Med 2010; 362:600–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roy AJ, Jaffe N, Djerassi I. Prophylactic platelet transfusions in children with acute leukemia: a dose response study. Transfusion 1973; 13:283–290. [DOI] [PubMed] [Google Scholar]
- 42.Stanworth SJ, Grant-Casey J, Lowe D, et al. The use of fresh-frozen plasma in England: high levels of inappropriate use in adults and children. Transfusion 2011; 51:62–70. [DOI] [PubMed] [Google Scholar]
- 43.Segal JB, Dzik WH; Transfusion Medicine/Hemostasis Clinical Trials Network. Paucity of studies to support that abnormal coagulation test results predict bleeding in the setting of invasive procedures: an evidence-based review. Transfusion 2005; 45:1413–1425. [DOI] [PubMed] [Google Scholar]
- 44.Abdel-Wahab OI, Healy B, Dzik WH. Effect of fresh-frozen plasma transfusion on prothrombin time and bleeding in patients with mild coagulation abnormalities. Transfusion 2006; 46:1279–1285. [DOI] [PubMed] [Google Scholar]
- 45.Holland LL, Brooks JP. Toward rational fresh frozen plasma transfusion: The effect of plasma transfusion on coagulation test results. Am J Clin Pathol 2006; 126:133–139. [DOI] [PubMed] [Google Scholar]
- 46.Lisman T, Caldwell SH, Leebeek FW, Porte RJ. Is chronic liver disease associated with a bleeding diathesis?. J Thromb Haemost 2006; 4:2059–2060. [DOI] [PubMed] [Google Scholar]
- 47.Tripodi A, Mannucci PM. Abnormalities of hemostasis in chronic liver disease: reappraisal of their clinical significance and need for clinical and laboratory research. J Hepatol 2007; 46:727–733. [DOI] [PubMed] [Google Scholar]
- 48.Habib M, Roberts LN, Patel RK, Wendon J, Bernal W, Arya R. Evidence of rebalanced coagulation in acute liver injury and acute liver failure as measured by thrombin generation. Liver Int 2014; 34:672–8. [DOI] [PubMed] [Google Scholar]
- 49.Sharara AI, Rockey DC. Gastroesophageal variceal hemorrhage. N Engl J Med 2001; 345:669–681. [DOI] [PubMed] [Google Scholar]
- 50.Lisman T, Porte RJ. Rebalanced hemostasis in patients with liver disease: evidence and clinical consequences. Blood 2010; 116:878–885. [DOI] [PubMed] [Google Scholar]
- 51.Jain V, Dhawan A. Prognostic modeling in pediatric acute liver failure. Liver Transpl 2016; 22:1418–30. [DOI] [PubMed] [Google Scholar]
- 52.Arni D, Wildhaber BE, McLin V, et al. Effects of plasma transfusions on antithrombin levels after paediatric liver transplantation. Vox Sang 2018; 10.1111/vox.12664. [DOI] [PubMed] [Google Scholar]
- 53.Nacoti M, Cazzaniga S, Lorusso F, et al. The impact of perioperative transfusion of blood products on survival after pediatric liver transplantation. Pediatr Transplant 2012; 16:357–366. [DOI] [PubMed] [Google Scholar]
- 54.Nacoti M, Cazzaniga S, Colombo G, et al. Postoperative complications in cirrhotic pediatric deceased donor liver transplantation: Focus on transfusion therapy. Pediatr Transplant 2017;21: 10.1111/petr.13020. [DOI] [PubMed] [Google Scholar]
- 55.Hilmi IA, Damian D, Al-Khafaji A, et al. Acute kidney injury following orthotopic liver transplantation: incidence, risk factors, and effects on patient and graft outcomes. Br J Anaesth 2015; 114:919–26. [DOI] [PubMed] [Google Scholar]
- 56.Feng ZY, Xu X, Zhu SM, Bein B, Zheng SS. Effects of low central venous pressure during preanhepatic phase on blood loss and liver and renal function in liver transplantation. World J Surg 2010; 34:1864–1873. [DOI] [PubMed] [Google Scholar]
- 57.Massicotte L, Beaulieu D, Thibeault L. Con: low central venous pressure during liver transplantation. J Cardiothorac Vasc Anesth 2008; 22:315–317. [DOI] [PubMed] [Google Scholar]
- 58.Englesbe MJ, Kelly B, Goss J, et al. Reducing pediatric liver transplant complications: a potential roadmap for transplant quality improvement initiatives within North America. Am J Transplant 2012; 12:2301–2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kloesel B, Kovatsis PG, Faraoni D, et al. Incidence and predictors of massive bleeding in children undergoing liver transplantation: A single-center retrospective analysis. Paediatr Anaesth 2017; 27:718–725. [DOI] [PubMed] [Google Scholar]
- 60.Weiss SL, Peters MJ, Alhazzani W, et al. Surviving Sepsis Campaign International Guidelines for the Management of Septic Shock and Sepsis-Associated Organ Dysfunction in Children. Pediatr Crit Care Med 2020; 21:e52–e106. [DOI] [PubMed] [Google Scholar]
- 61.Toh CH, Hoots WK; SSC on Disseminated Intravascular Coagulation of the ISTH. The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost 2007; 5:604–606. [DOI] [PubMed] [Google Scholar]
- 62.Church GD, Matthay MA, Liu K, Milet M, Flori HR. Blood product transfusions and clinical outcomes in pediatric patients with acute lung injury. Pediatr Crit Care Med 2009; 10:297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Randomised trial of prophylactic early fresh-frozen plasma or gelatin or glucose in preterm babies: outcome at 2 years. Northern Neonatal Nursing Initiative Trial Group. Lancet 1996; 348:229–232. [PubMed] [Google Scholar]
- 64.Stanworth SJ, Brunskill SJ, Hyde CJ, McClelland DB, Murphy MF. Is fresh frozen plasma clinically effective? A systematic review of randomized controlled trials. Br J Haematol 2004; 126:139–152. [DOI] [PubMed] [Google Scholar]
- 65.Nguyen T, Hall M, Han Y, et al. Microvascular thrombosis in pediatric multiple organ failure: Is it a therapeutic target? Pediatr Crit Care Med 2001; 2:187–196. [DOI] [PubMed] [Google Scholar]
- 66.Kumar A, Mhaskar R, Grossman BJ, et al. Platelet transfusion: a systematic review of the clinical evidence. Transfusion 2015; 55:1116–1115. [DOI] [PubMed] [Google Scholar]
- 67.Science M, Robinson PD, MacDonald T, Rassekh SR, Dupuis LL, Sung L. Guideline for Primary Antifungal Prophylaxis for Pediatric Patients with Cancer or Hematopoietic Stem Cell Transplant Recipients. Edmonton, C17 Council, 2014. [DOI] [PubMed] [Google Scholar]
- 68.Du Pont-Thibodeau G, Tucci M, Robitaille N, Ducruet T, Lacroix J. Platelet Transfusions in Pediatric Intensive Care. Pediatr Crit Care Med 2016; 17:e420–9. [DOI] [PubMed] [Google Scholar]
- 69.Saini A, West AN, Harrell C, et al. Platelet Transfusions in the PICU: Does Disease Severity Matter? Pediatr Crit Care Med 2018; 19:e472–e478. [DOI] [PubMed] [Google Scholar]
- 70.Nellis ME, Goel R, Karam O, et al. Effects of ABO Matching of Platelet Transfusions in Critically Ill Children. Pediatr Crit Care Med 2019; 20:e61–e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu SC, Chen CL, Wang CH, et al. Predictive factors associated with re-exploration for hemostasis in living donor liver transplantation. Ann Transplant 2012; 17:64–71. [DOI] [PubMed] [Google Scholar]
- 72.Gross SJ, Filston HC, Anderson JC. Controlled study of treatment for disseminated intravascular coagulation in the neonate. J Pediatr 1982; 100:445–8. [DOI] [PubMed] [Google Scholar]
- 73.Kabra SK, Jain Y, Madhulika, et al. Role of platelet transfusion in dengue hemorrhagic fever. Indian Pediatr 1998; 35:452–5. [PubMed] [Google Scholar]
- 74.El-Nawawy AA, Elshinawy MI, Khater DM, et al. Outcome of Early Hemostatic Intervention in Children With Sepsis and Nonovert Disseminated Intravascular Coagulation Admitted to PICU: A Randomized Controlled Trial. Pediatr Crit Care Med 2021; 22:e168–e177. [DOI] [PubMed] [Google Scholar]
- 75.Go H, Ohto H, Nollet KE, et al. Risk factors and treatments for disseminated intravascular coagulation in neonates. Ital J Pediatr 2020; 46:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


