This randomized clinical trial evaluates the improvement in the 6-minute walk distance test and in leg and hand muscle endurance after use of urolithin A in patients aged 65 to 90 years.
Key Points
Question
What is the effect of supplementation with urolithin A, a natural gut microbiome–derived food metabolite, on skeletal muscle performance and mitochondrial health in older adults?
Findings
In this randomized clinical trial of 66 older adults, those who received supplementation with 1000 mg of urolithin A had a significant improvement in muscle endurance (number of muscle contractions until fatigue) for both hand and leg skeletal muscles compared with those who used placebo. Plasma levels of several acylcarnitines, ceramides (biomarkers of mitochondrial health), and C-reactive protein were decreased after urolithin A supplementation.
Meaning
These findings indicate that urolithin A was safe and well tolerated as well as beneficial for muscle endurance and mitochondrial health in older adults; it may also be a promising approach to counteracting age-associated muscle decline.
Abstract
Importance
Aging is associated with a decline in mitochondrial function and reduced exercise capacity. Urolithin A is a natural gut microbiome–derived food metabolite that has been shown to stimulate mitophagy and improve muscle function in older animals and to induce mitochondrial gene expression in older humans.
Objective
To investigate whether oral administration of urolithin A improved the 6-minute walk distance, muscle endurance in hand and leg muscles, and biomarkers associated with mitochondrial and cellular health.
Design, Setting, and Participants
This double-blind, placebo-controlled randomized clinical trial in adults aged 65 to 90 years was conducted at a medical center and a cancer research center in Seattle, Washington, from March 1, 2018, to July 30, 2020. Muscle fatigue tests and plasma analysis of biomarkers were assessed at baseline, 2 months, and 4 months. Six-minute walk distance and maximal ATP production were assessed using magnetic resonance spectroscopy at baseline and at the end of study at 4 months. The analysis used an intention-to-treat approach.
Interventions
Participants were randomized to receive daily oral supplementation with either 1000 mg urolithin A or placebo for 4 months.
Main Outcomes and Measures
The primary end point was change from baseline in the 6-minute walk distance and change from baseline to 4 months in maximal ATP production in the hand skeletal muscle. The secondary end points were change in muscle endurance of 2 skeletal muscles (tibialis anterior [TA] in the leg and first dorsal interosseus [FDI] in the hand). Cellular health biomarkers were investigated via plasma metabolomics. Adverse events were recorded and compared between the 2 groups during the intervention period.
Results
A total of 66 participants were randomized to either the urolithin A (n = 33) or the placebo (n = 33) intervention group. These participants had a mean (SD) age of 71.7 (4.94) years, were predominantly women (50 [75.8%]), and were all White individuals. Urolithin A, compared with placebo, significantly improved muscle endurance (ie, increase in the number of muscle contractions until fatigue from baseline) in the FDI and TA at 2 months (urolithin A: FDI, 95.3 [115.5] and TA, 41.4 [65.5]; placebo: FDI, 11.6 [147.4] and TA, 5.7 [127.1]). Plasma levels of several acylcarnitines, ceramides, and C-reactive protein were decreased by urolithin A, compared with placebo, at 4 months (baseline vs 4 mo: urolithin A, 2.14 [2.15] vs 2.07 [1.46]; placebo, 2.17 [2.52] vs 2.65 [1.86]). The mean (SD) increase from baseline in the 6-minute walk distance was 60.8 (67.2) m in the urolithin A group and 42.5 (73.3) m in the placebo group. The mean (SD) change from baseline to 4 months in maximal ATP production in the FDI was 0.07 (0.23) mM/s in the urolithin A group and 0.06 (0.20) mM/s in the placebo group; for the TA, it was −0.03 (0.10) mM/s in the urolithin A group and 0.03 (0.10) mM/s in the placebo group. These results showed no significant improvement with urolithin A supplementation compared with placebo. No statistical differences in adverse events were observed between the 2 groups.
Conclusions and Relevance
This randomized clinical trial found that urolithin A supplementation was safe and well tolerated in the assessed population. Although the improvements in the 6-minute walk distance and maximal ATP production in the hand muscle were not significant in the urolithin A group vs the placebo group, long-term urolithin A supplementation was beneficial for muscle endurance and plasma biomarkers, suggesting that urolithin A may counteract age-associated muscle decline; however, future work is needed to confirm this finding.
Trial Registration
ClinicalTrials.gov Identifier: NCT03283462
Introduction
Older adults (aged ≥60 years) are the fastest growing age group in the world and projected to represent 1 in every 4 adults by 2050.1,2 Aging is associated with a progressive loss of muscle mass and strength that manifests as reduced physical performance and endurance capacity, imposing a burden on both the individual and society.3,4 Evidence has shown that mitochondrial dysfunction plays an important role in age-related diseases.5 In skeletal muscle, the decline in mitochondrial efficiency and capacity for adenosine triphosphate (ATP) production is associated with decreased performance and increased fatigue.6,7,8,9 With age, a progressive decline in the cell’s capacity to eliminate its dysfunctional mitochondria by a selective autophagy process named mitophagy contributes to poor mitochondrial quality.10,11 Therefore, restoring levels of mitophagy is an interesting approach to improving mitochondrial function. Urolithin A is a natural food metabolite of the gut microbiome12,13,14 that has been shown to stimulate mitophagy and improve muscle function in aged animals15 and in models of muscular dystrophy,16 while also being safe, bioavailable, and able to induce mitochondrial gene expression in older adults.17
The current study was designed to test the hypothesis that long-term supplementation with urolithin A would improve mitochondrial function and muscle performance in older adults. Specifically, we aimed to investigate whether oral administration of urolithin A improved the 6-minute walk distance, the muscle endurance in hand and leg muscles, and the biomarkers associated with mitochondrial and cellular health. Potential participants were screened for average physical performance using the 6-minute walk distance test and mitochondrial function using magnetic resonance spectroscopy (MRS) in the skeletal muscle. A supplementation period of 4 months, with efficacy readouts at 2 and 4 months, was chosen as the earliest time point at which improvements in muscle function end points would be likely observed.
Methods
This double-blind, placebo-controlled randomized clinical trial (Bioenergetics and Muscle Function Improvement With AMAZ-02 in Elderly Skeletal Muscle [ENERGIZE]) was conducted at the University of Washington Medical Center and the Fred Hutchison Cancer Research Center in Seattle, Washington, from March 1, 2018, to July 30, 2020. Study approval was obtained from both the University of Washington Institutional Review Board and the Western Institutional Review Board. The trial protocol and the statistical analysis plan are available in Supplement 1. All participants signed an informed consent form. The trial was conducted in accordance with the guidelines of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practice and the Declaration of Helsinki.18 We followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Participants, Randomization, and Dosing
Older adults aged 65 to 90 years were recruited through advertisements, social media platforms, and referrals from previous studies. To be included, individuals had to be healthy; ambulatory; and able to perform activities of daily living without assistance, to speak and read English fluently, and to sign the informed consent form. Race and ethnicity were self-reported by participants. All participants identified as White individuals. No other race and ethnicity data were collected.
Individuals were screened on average physical performance (6-minute walk distance ≤550 m) and low-average mitochondrial health using MRS that evaluated the maximal ATP synthesis rate (≤1.0 mM/s) in the hand skeletal muscle (first dorsal interosseus [FDI]). Major exclusion criteria were the presence of any existing chronic uncontrolled medical conditions (eg, uncontrolled hypertension or chronic kidney disease requiring dialysis), any major cardiac events in the last 3 months, and any metallic implants in the limbs or a cardiac pacemaker. Five individuals had a medical history of diabetes that was well controlled when they were enrolled. A complete list of the inclusion and exclusion criteria is provided in the trial protocol (Supplement 1). Ten individuals could not fully complete the intermediate and final study tests because of COVID-19 restrictions.
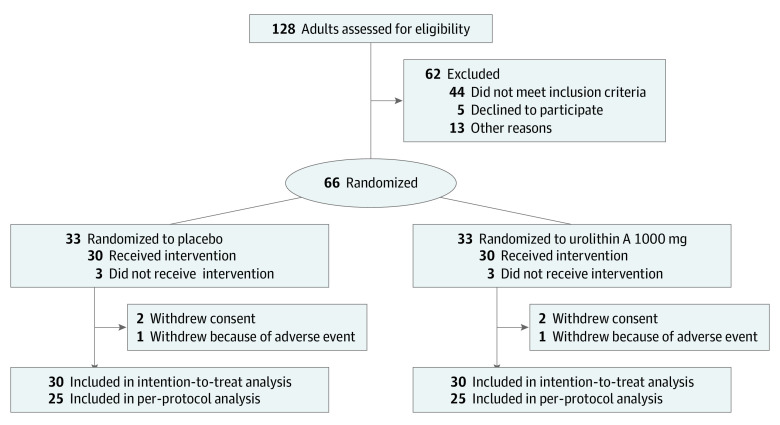
Participants who met all of the inclusion criteria were randomized using a random number generator in a 1:1 ratio to either urolithin A (Mitopure; Amazentis SA) or placebo intervention groups (Figure 1). The following measures were taken to avoid bias: the study was double blinded, and the softgels containing the active product or placebo were made to be indistinguishable in appearance. Each softgel contained either 250 mg of urolithin A along with excipients or only excipients for the placebo. To reach the daily dose of 1000 mg urolithin A, each participant consumed 4 softgels (containing the active drug or placebo) in the morning on an empty stomach with a glass of water. The softgels were provided in blistered wallet cards for the duration of the trial. Compliance to the intervention was ascertained by counting the number of leftover or unused softgels.
Figure 1. CONSORT Diagram of Participant Flow Through the Study .
In this trial, the primary end point was change in the 6-minute walk distance and maximal ATP production in the hand skeletal muscle from baseline measurement to the end of the study at 4 months. The secondary end points were change in the muscle endurance of the tibialis anterior (TA) in the leg and the FDI in the hand.
Muscle Performance Test
Muscle endurance (ie, resistance to fatigue) was assessed on the right hand (FDI) and leg skeletal (TA) muscles by measuring the number of contractions during repeated isometric contractions until fatigue using a custom-built exercise apparatus19,20 at baseline, 2 months, and 4 months. The contraction intensity was set at 70% of the maximum voluntary contraction, and the exercise began at a frequency of 60 contractions per minute (cpm) for the first minute and increased at a rate of 10 cpm each minute until exhaustion. Muscle strength, which was defined as the maximum voluntary contraction, was measured as the mean of 3 maximum contractions separated by 5 seconds, with each contraction sustained for 3 to 5 seconds.
Muscle Maximal ATP Production and Cross-sectional Area
The mitochondrial oxidative phosphorylation capacity (maximal ATP production) was determined using 31P MRS20 at baseline and 4 months. Briefly, a short exercise bout (20-30 seconds) involving the index finger for the hand and dorsiflexion of the foot for the leg was used to reduce the concentration of phosphocreatine (PCr) in the muscle by approximately 30% to 50% from the resting state while maintaining muscle pH that was higher than 6.8.21 The PCr recovery was measured for 6 minutes to determine a time constant of recovery to yield a maximal ATP production that was equal to the resting concentration of PCr in the muscle divided by the time constant of recovery, where the resting-level PCr was 24.5 mM.
The FDI and TA muscle cross-sectional areas (eTable in Supplement 2) were assessed at baseline and 4 months using magnetic resonance imaging (4.7-T magnet with Biospin console; Bruker Corporation). The axial plane T1-weighted, 2-dimensional gradient-echo images were collected with the following parameters: 500-ms repetition time, 2.5-ms echo time, 3-mm slice thickness with 1-mm interslice interval, 192 × 192 matrix, and 2 excitations. Five slices of each right limb were analyzed with Image J, version 1.50e (National Institutes of Health) using manual planimetry to determine the muscle cross-sectional area.
6-Minute Walk Distance Test
Participant performance in 6-minute walk distance test was measured at baseline and 4 months. A distance of 15 m was marked on the floor of an indoor hallway, which was regulated for temperature and humidity, and markers were placed at each end of the course. Participants completed as many laps of the course as possible for 6 minutes. Participants were provided time updates at 1-minute intervals for the duration of the test. At the 6-minute mark, participants were asked to stop where they were standing and the total distance walked in meters was calculated.
Adverse Events, Compliance, and Plasma Collection
Adverse events (AEs) were recorded and coded according to the Medical Dictionary for Regulatory Activities. The AEs were classified as mild, moderate, or severe by the study physicians (J.M.G. and A.S.), and the relationship of the AEs to the study product was assessed. Compliance to the intervention was evaluated at the 2-month and 4-month visits. Possible differences in compliance by intervention groups between each visit and overall were assessed by analysis of variance.
Blood samples were drawn from all participants at screening (baseline) and at the 2-month and 4-month visits. Ten mL of blood was collected in lavender EDTA tubes until the vacuum was exhausted and blood ceased to flow. Tubes were gently inverted 8 to 10 times to disperse the anticoagulant and then labeled and centrifuged immediately at 2500 rpm for 15 minutes at 25 °C.
Bioavailability Assessment of Urolithin A and Plasma Cytokine Measurement
Concentrations of urolithin A and its metabolite, urolithin A glucuronide, were analyzed in plasma at baseline and 4 months (end of the study) using a validated method, as described previously.17 The limit of quantification was 5.00 pg/mL for urolithin A in plasma and 5.00 ng/mL for urolithin A glucuronide. For mean value calculations, all values below the limit of quantification were set to 0.
Human plasma samples were evaluated for levels of C-reactive protein (CRP) with a kit (V-Plex K151STD; Meso Scale Diagnostics LLC), following manufacturing instructions. These samples were analyzed in a blinded manner using a dilution ratio of 1:2. Standard curve concentration points on each plate were used to compare the calculated lower limit of quantification for a particular analyte against the published lower limit of quantification.
Plasma Metabolomics
Metabolomics of plasma were performed by Metabolon Inc, according to published methods.17 Briefly, sample preparation was conducted using a proprietary series of organic and aqueous extractions to remove the protein fraction while allowing maximum recovery of small molecules. The extracted samples were split into equal parts for analysis by gas chromatography–mass spectroscopy and liquid chromatography–tandem mass spectroscopy platforms. For liquid chromatography–tandem mass spectroscopy, samples were either analyzed in positive (acidic solvent) or negative (basic solvent) ionization mode. Gas chromatography–mass spectroscopy was performed on bis(trimethylsilyl)triflouroacetamide-derivatized samples in a 5% phenyl gas chromatography column.
Statistical Analysis
One of us (D.J.M.) reported the clinical data using a web-based electronic case report form. After the study started, the original primary end points of change from baseline of hand maximal ATP production and of hand muscle endurance were replaced by change from baseline of 6-minute walk distance and hand maximal ATP production. The reason for this amendment was that the 6-minute walk distance end point was determined to be more functionally important. The trial was powered to detect a change (>30 m) in the 6-minute walk distance from baseline measurement between the 2 intervention groups. Assuming a higher dropout rate in older adults, we calculated that each group required 33 participants. A statistical analysis plan (Supplement 1) was prepared before unblinding the data.
The analysis of primary efficacy parameters was performed using analysis of covariance, with treatment as the independent factor, baseline measurement as the covariable, and change from baseline as the dependent variable. The 95% CIs for treatment differences and corresponding nonadjusted P values were calculated. A 5% significance level (α = .05 or 2-sided P < .05) was applied for the comparison of urolithin A to placebo groups. To account for the 2 primary efficacy end points, an a priori–ordered hypothesis was stated: the percentage of maximal ATP production was only to be tested for confirmatory decisions if the 6-minute walk distance test resulted in a statistically significant difference between urolithin A and placebo groups.
Changes in plasma levels of acylcarnitines and ceramides were assessed using repeated-measures analysis of variance. Missing values were imputed with the observed minimum for that particular compound. The statistical analyses were performed on natural log–transformed data. For plasma CRP, the postbaseline markers were analyzed in the log10 scale using analysis of covariance, correcting for baseline value and intervention group. If the observed values were below the limit of detection, left censoring was applied. Point estimates, 80% CIs, and 95% CIs were extracted from the analysis of covariance model. No correction for multiplicity testing was applied. This intention-to-treat analysis was performed using R, version 4.0.3 (R Foundation for Statistical Computing).
Results
Of the 128 adults aged 65 to 90 years screened for this trial, 66 (51.6%) were included and randomized to either the urolithin A (n = 33) or placebo (n = 33) intervention. These participants had a mean (SD) age of 71.7 (4.94) years; were predominantly women, with 50 women (75.8%) and 16 men (24.2%); and were all White individuals. The BMI and vital signs were similar between urolithin A and placebo groups (Table 1). At baseline, participants had a mean (SD) 6-minute walk distance of 450.6 (59.21) m and a mean (SD) maximal ATP production in hand muscle of 0.678 (0.20) mM/s, showing that the population enrolled had average physical performance and suboptimal mitochondrial function.20,22 Six participants were lost to follow-up, and 10 participants did not complete functional tests that were linked to secondary end points because of COVID-19-related restrictions. Compliance was high, with 96% in the placebo group and 97% in the urolithin A group adhering to the intervention.
Table 1. Demographic Characteristics of Participants at Baseline.
| Characteristic | Mean (SD) | ||
|---|---|---|---|
| Placebo (n = 33) | Urolithin A (n = 33) | Total (n = 66) | |
| Age, y | 71 (4.58) | 72.5 (5.24) | 71.7 (4.94) |
| Sex, No. (%) | |||
| Female | 23 (69.7) | 27 (81.8) | 50 (75.8) |
| Male | 10 (30.3) | 6 (18.2) | 16 (24.2) |
| White race and ethnicity, No. (%)a | 33 (100) | 33 (100) | 66 (100) |
| BMI | 26.7 (3.77) | 25.7 (3.45) | 26.2 (3.62) |
| Blood pressure | |||
| Systolic, mm Hg | 132.1 (13.03) | 132.9 (13.59) | 132.5 (13.21) |
| Diastolic, mm Hg | 75.5 (7.96) | 76.8 (9.23) | 76.1 (8.57) |
| Heart rate, bpm | 64.4 (9.95) | 65.4 (9.61) | 64.9 (9.72) |
| 6-min Walking distance, m | 464.6 (59.66) | 436.6 (56.26) | 450.6 (59.21) |
| Maximal ATP production, mM/s | 0.703 (0.22) | 0.653 (0.22) | 0.678 (0.20) |
Abbreviations: ATP, adenosine triphosphate; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Race and ethnicity were self-reported by participants. All participants identified as White individuals.
Safety and Efficacy End Points
Urolithin A was found to be safe and well tolerated. In total, 33 AEs were recorded during the study, of which a total of 31 treatment-emergent AEs (93.9%) were reported by participants in the urolithin A (n = 16) and placebo (n = 15) groups (Table 2). The AEs were diverse in nature, with no statistical differences between the groups. No serious AEs were reported. In addition, no significant changes in vital signs, blood biochemistry parameters, hematology, and urinalysis were found between groups.
Table 2. Differences in Reported AEs Between Study Groups .
| AE classification | Placebo group (n = 33), No. | Urolithin A group (n = 33), No. | Total No. (n = 66) |
|---|---|---|---|
| All AEs | 15 | 18 | 33 |
| Treatment-emergent AEs | 15 | 16 | 31 |
| Serious AEs | 0 | 0 | 0 |
| AEs leading to study withdrawal | 1 | 1 | 2 |
| Hematologic investigations | 10 | 13 | 23 |
| Creatinine phosphokinase increased | 2 | 3 | 5 |
| Lipids increased | 3 | 2 | 5 |
| Triglycerides increased | 3 | 1 | 4 |
| Cholesterol increased | 1 | 2 | 3 |
| LDL-C increased | 1 | 2 | 3 |
| Liver enzymes increased | 0 | 2 | 2 |
| Alkaline phosphatase increased | 0 | 1 | 1 |
| Cardiac disorders | 0 | 2 | 2 |
| Angina pectoris | 0 | 1 | 1 |
| Sinus bradycardia | 0 | 1 | 1 |
| Gastrointestinal disorders | 2 | 0 | 2 |
| Abdominal pain | 1 | 0 | 1 |
| Diarrhea | 1 | 0 | 1 |
| Infections and infestations | 1 | 1 | 2 |
| Bronchitis | 0 | 1 | 1 |
| UTI | 1 | 0 | 1 |
| Eye disorders | 1 | 0 | 1 |
| Glaucoma | 1 | 0 | 1 |
| Metabolism and nutrition disorders | 1 | 0 | 1 |
| Hyperglycemia | 1 | 0 | 1 |
Abbreviations: AEs, adverse events; LDL-C, low-density lipoprotein cholesterol; UTI, urinary tract infection.
Primary
The mean (SD) change from baseline in the 6-minute walk distance, the primary end point, was 60.8 (67.2) m (n = 30; percentage change from baseline: 14.9%) among participants who were supplemented with a 1000-mg/d dosage of urolithin A for 120 days, compared with 42.5 (73.3) m (n = 30; percentage change from baseline: 10.1%) in the placebo group (Figure 2A). This increase with urolithin A was not a significant improvement over that observed in the placebo group. However, both the placebo group (464.6 [59.7] m vs 507.2 [76.5] m) and the urolithin A group (436.6 [56.3] m vs 497.4 [70.3] m) demonstrated significant improvements in the 6-minute walk distance that were greater than the clinically relevant improvement of 30 m.23 A further subgroup analysis of the change in the 6-minute walk distance among those with a maximal ATP production of 0.7 mM/s or less at baseline revealed a bigger difference between the placebo group (n = 16) and the urolithin A group (n = 19). These differences, however, did not reach statistical significance (33.8 m vs 56.1 m; P = .36) (Figure 2B).
Figure 2. Effect of Urolithin A Supplementation on the 6-Minute Walk Distance and Maximal Adenosine Triphosphate (ATP) Production in Hand Muscles and Muscle Endurance .
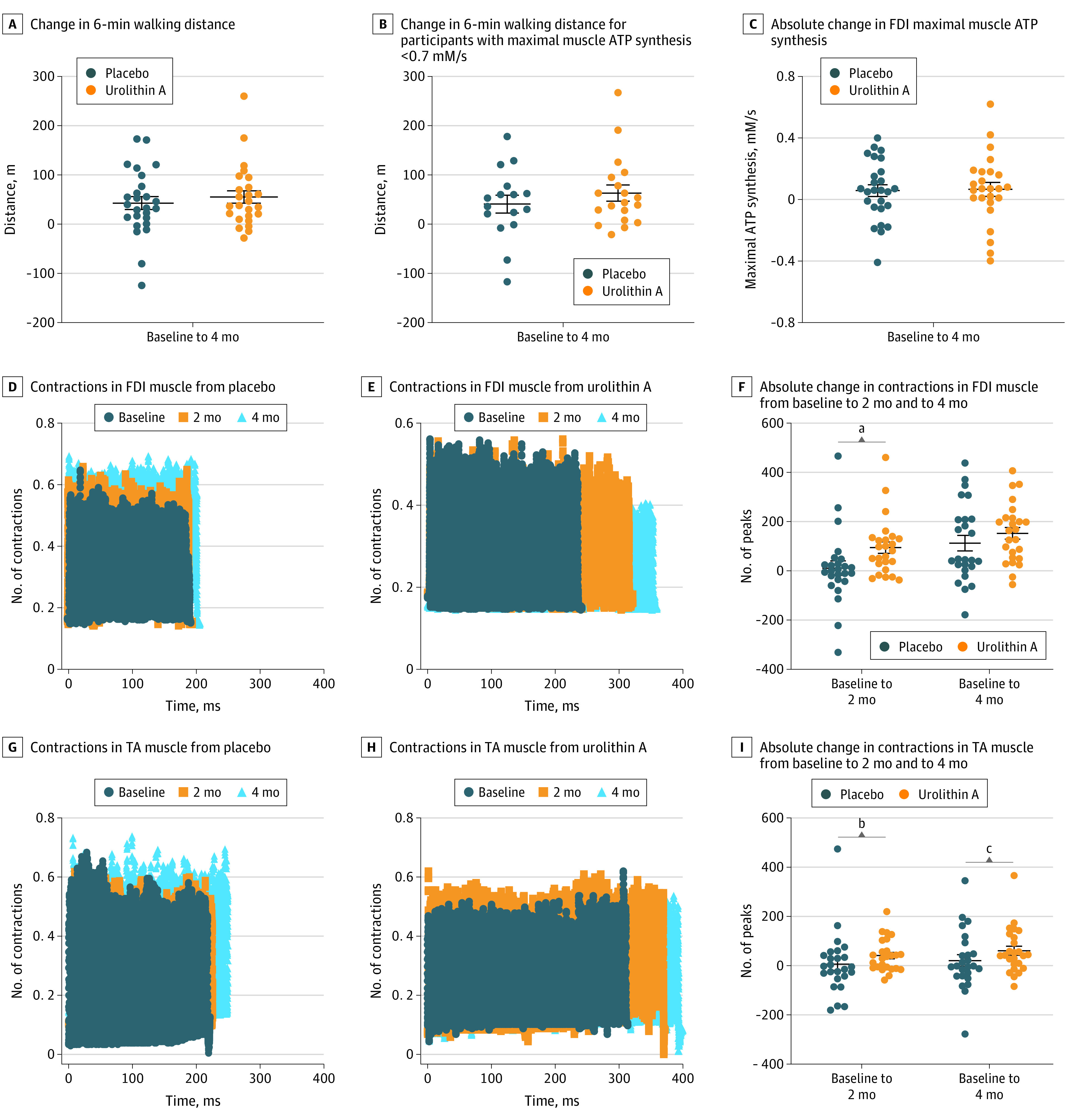
Data were analyzed using an analysis of covariance with 95% CIs for treatment differences. The center horizontal line represents the mean and the top and bottom lines represent the SEM. FDI indicates first dorsal interosseus; TA, tibialis anterior.
aP <.01 with post hoc 2-sided Wilcoxon 2-sample test.
bP = .05.
cP = .07 with post hoc 2-sided Wilcoxon 2-sample test.
To test whether urolithin A supplementation improved mitochondrial capacity in aged skeletal muscle, we measured the maximal ATP production using MRS. There was no significant effect of treatment on the mean (SD) change in maximal ATP production from baseline to 4 months in either the hand FDI (urolithin A group vs placebo group: 0.07 [0.23] mM/s vs 0.06 [0.20] mM/s) or the leg TA (urolithin A group vs placebo group: −0.03 [10] mM/s vs 0.03 [0.10] mM/s) (Figure 2C; eFigure 1 in Supplement 2).
Secondary
To assess the effect of urolithin A supplementation on muscle endurance, we measured the ability to maintain repeated voluntary contractions to 70% of maximum voluntary contraction in the FDI and TA. At the 2-month visit, urolithin A supplementation significantly improved endurance in both muscles compared with placebo (urolithin A: FDI, 95.3 [115.5] and TA, 41.4 [65.5]; placebo: FDI, 11.6 [147.4] and TA, 5.7 [127.1]) (Figure 2D-I; eFigure 2A and B in Supplement 2). At the 4-month visit, endurance in the urolithin A group continued to improve, but a parallel increase in the placebo group led to no significant effect of treatment.
Supportive Biomarkers
Plasma samples were collected from study participants to assess urolithin A bioavailability. High levels of parent urolithin A (1038 pg/mL at 4 months) and its conjugated form urolithin A glucuronide (1014 ng/mL at 4 months) were detected 4 months after administration of urolithin A compared with baseline levels (eFigure 3 in Supplement 2). Plasma levels were consistent with those measured in previous trials with urolithin A.17
We further analyzed plasma samples to investigate the effect of urolithin A on biomarkers of mitochondrial health and inflammation. Urolithin A supplementation led to a significant reduction in several acylcarnitines, primarily long-chain and polyunsaturated species, at both the 2-month and 4-month visits compared with baseline (Figure 3A-D; eFigure 4A and B in Supplement 2). In addition, several species from a panel of ceramides that were analyzed via plasma metabolomics showed a significant reduction from baseline measurement in the urolithin A group but not the placebo group at both 2 and 4 months (Figure 3E and F; and eFigure 4C and D in Supplement 2).
Figure 3. Effect of Urolithin A on Biomarkers of Mitochondrial Health and Inflammation.
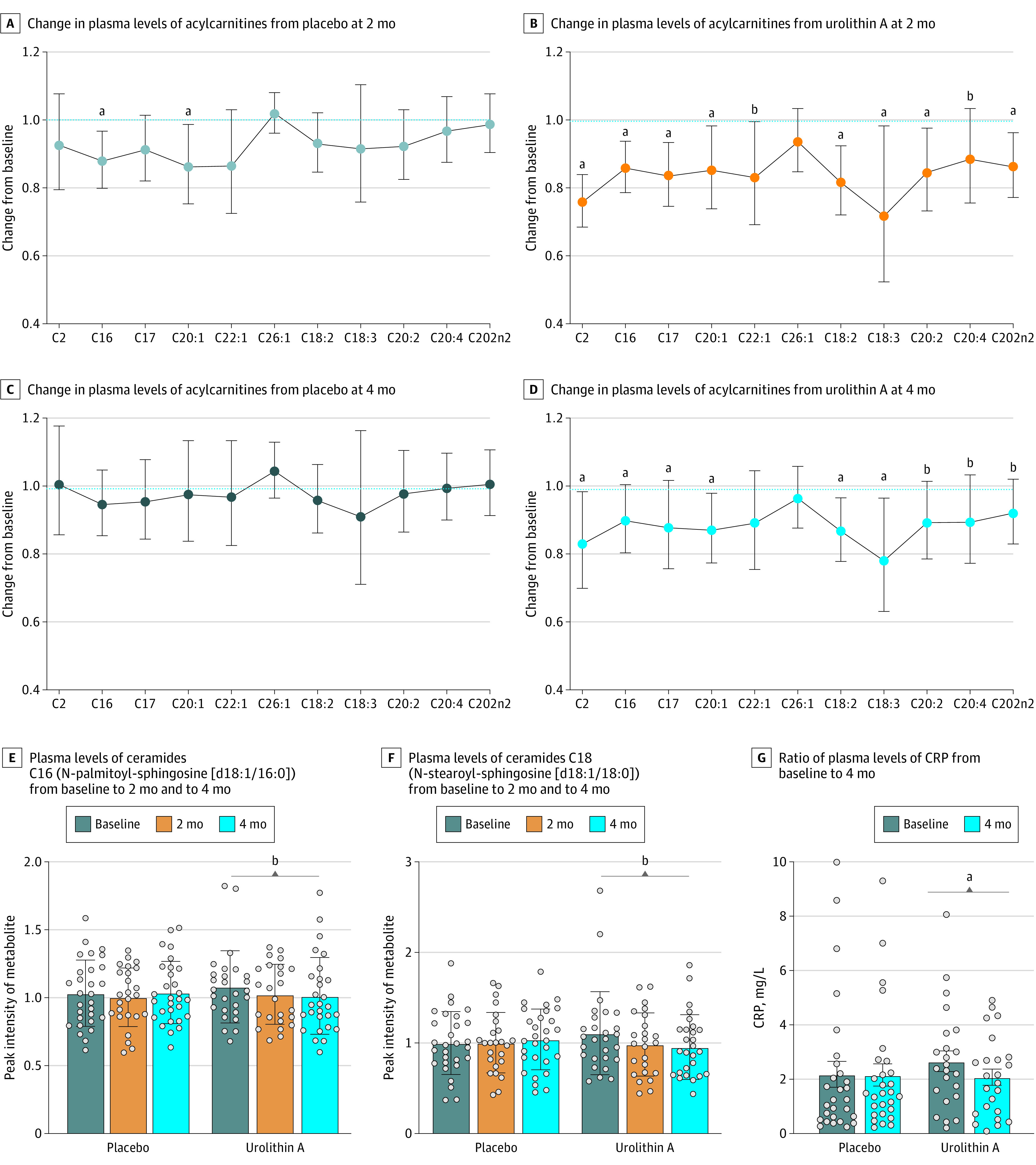
A-F, Data represent geometric mean (95% CI). A 2-way repeated-measures analysis of variance was used. G, Data represent mean (95% CI). An analysis of covariance model was used. BL indicates baseline; CRP indicates C-reactive protein. Light gray circles indicate change in plasma levels in the control group at 2 months; dark blue circles, change in plasma levels in the control group at 4 months; orange circles, change in plasma levels in the urolithin A group at 2 months; bright blue circles, change in plasma levels in the urolithin A group at 4 months.
aP <.05.
b.05 is less than P < .10.
To further test the effect of urolithin A on inflammation, we measured plasma levels of the inflammatory biomarker CRP. As for ceramides, a significant reduction from baseline in plasma CRP was observed in participants in the urolithin A group but not the placebo group (baseline vs 4 months: urolithin A, 2.14 [2.15] vs 2.07 [1.46]; placebo, 2.17 [2.52] vs 2.65 [1.86]) (Figure 3G).
Discussion
Urolithin A has been shown to boost mitochondrial health by triggering mitophagy in both preclinical models of aging and in older adults.15,16,17 In this follow-up, double-blind, placebo-controlled randomized clinical trial, we found that the improvements in the 6-minute walk distance and maximal ATP production in hand muscles were not significant for urolithin A. However, we found that long-term supplementation with urolithin A significantly enhanced skeletal muscle–specific endurance and improved the metabolic markers of mitochondrial function in older adults.
In this trial, both the placebo and urolithin A groups showed clinically meaningful improvements (>30 m) from baseline23 in the 6-minute walk distance. Nevertheless, no significant benefits of urolithin A over placebo were observed because of a higher-than-anticipated placebo effect. To exclude participants who were least likely to benefit from improved mitochondrial quality control, we excluded individuals from this study with the highest functioning mitochondria using a maximal ATP production of 1.0 mM/s as a cutoff. Previous studies have reported a mean maximal ATP production of 0.5 to 0.6 mM/s in the quadricep of older adults,7 and a cutoff of 0.7 mM/s has been employed in previous studies to select older participants with compromised muscle mitochondrial function.20 Thus, the participants in this trial still included well-functioning individuals, as was also observed from the mean (SD) range of the 6-minute walk distance at baseline (450.6 [59.21] m), who would be less likely to benefit from improved mitochondrial function. Furthermore, the improvement in the placebo group likely confounded the ability to detect a significant effect of urolithin A supplementation on the 6-minute walk distance. These results suggest that higher powering, a longer intervention regimen of more than 6 months, or combining urolithin A supplementation with exercise training19 may be required to detect the effects of urolithin A on whole-body performance.
Despite the absence of a significant effect on the 6-minute walk distance, the observation that urolithin A supplementation significantly improved muscle endurance in both the hand and leg skeletal muscle is important because it demonstrated a direct functional effect on muscle performance in the absence of exercise training in 2 functionally and anatomically diverse skeletal muscles. The TA tends toward a slower twitch (75% type I fiber) phenotype and is involved in locomotion and thus more likely to be affected by activity level.24 In contrast, the FDI tends toward a faster twitch (approximately 50% type II fibers)24 and is not directly related to mobility. The fatigue test in this trial was designed to isolate the effects on skeletal muscle by minimizing the potential confounding effects of changes in cardiovascular or lung function that could influence whole-body performance measures, such as the 6-minute walk distance. The increased muscle endurance in both the hand and leg muscles at the 2-month visit and further increases at the 4-month visit support the conclusion that urolithin A supplementation directly improved skeletal muscle performance. These measures are functionally important because the ability to perform repeated submaximal muscle contractions is a key aspect of activities of daily living. The dissociation between maximal ATP production and muscle fatigue resistance observed in this study suggests that the maximum capacity for ATP production in skeletal muscle may not be the sole limiting factor associated with poor muscle performance in aging. A previous randomized clinical trial that targeted mitochondrial function in aged skeletal muscle with a pharmaceutical compound found that the greatest effect on FDI muscle endurance occurred several days after treatment, after maximal ATP production had returned to baseline levels.20
The decrease in circulating biomarkers in this trial supports the improved mitochondrial health in participants who used the urolithin A supplement. Metabolomics data were consistent with findings from a previous clinical study that showed urolithin A decreased plasma acylcarnitines, which was indicative of improved mitochondrial metabolic efficiency, in older adults after 4 weeks of supplementation.17 Impaired mitochondrial health has been associated with higher low-grade systemic inflammation or inflamm-aging.25 The link between urolithin A, mitochondrial health, and inflammation is supported by the finding of a decline in plasma ceramides, a class of molecules belonging to the sphingolipid family whose levels are associated with inflammation state and the risk of age-associated diseases. Urolithin A reduced levels of C16 (N-palmitoyl-sphingosine [d18:1/16:0]) and C18 (N-stearoyl-sphingosine [d18:1/18:0]) ceramides (Figure 3E and F), 2 species that are part of a clinically validated ceramide score whose accumulation in the blood is indicative of a higher risk for future cardiovascular diseases26 and is associated with several age-associated diseases, such as Alzheimer disease and diabetes.27 In addition, urolithin A reduced plasma CRP levels. Stable levels of CRP were associated with healthy aging outcomes in a large longitudinal study,28 and findings from this trial further support the benefits of urolithin A in this older population. However, CRP is a general biomarker of inflammation; thus, future studies should include additional measures, such as inflammatory cytokines, to test the anti-inflammatory activity of urolithin A.
This trial suggests that urolithin A may be a promising approach to counteract age-associated muscle decline. Future study is needed to confirm the role of urolithin A supplementation in healthy aging.
Limitations
This study has several limitations. First, the 6-minute walk distance significantly improved from baseline in both the placebo and the urolithin A groups. One potential explanation is that participation in the study motivated an increase in activity in some participants. An effect of increased physical activity on muscle and metabolic health would confound the ability to detect a significant effect of urolithin A. However, monitoring daily participant physical activity was not part of the trial protocol. Because physical function is a complex trait, detecting an effect of urolithin A supplementation is further limited by our decision to use only the 6-minute walk distance to assess function. Second, because of the relatively small sample size of only White participants from the Seattle, Washington, area, these results should be considered preliminary if extrapolating to the general older population. Future studies should have a longer intervention of more than 6 months, track daily physical activity levels, and select participants with lower physical performance (eg, 6-minute walk distance in the range of 350-400 m) to assess the effect of urolithin A.
Conclusions
This randomized clinical trial found that urolithin A was safe and well tolerated by older adults. The improvements in the primary end point of the 6-minute walk distance and maximal ATP production in hand muscles were not significant for urolithin A, but long-term urolithin A supplementation had a beneficial effect on the secondary end points of muscle endurance and biomarkers of mitochondrial health. The findings from this exploratory work suggest that urolithin A is a promising approach to counteracting age-associated muscle decline. However, future work is needed to confirm the beneficial role of urolithin A supplementation in healthy aging.
Trial Protocol
eTable. No Impact on Muscle Size During the Study Intervention Period
eFigure 1. Change in TA ATPmax
eFigure 2. Percent Change in Number of Muscle Contractions in Skeletal Muscle
eFigure 3. UA Bioavailability in the Study Population
eFigure 4. UA Impact on Plasma Acylcarnitine and Ceramide Levels
Data Sharing Statement
References
- 1.Atella V, Piano Mortari A, Kopinska J, et al. Trends in age-related disease burden and healthcare utilization. Aging Cell. 2019;18(1):e12861. doi: 10.1111/acel.12861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, Johnson KS. Actualizing better health and health care for older adults. Health Aff (Millwood). 2021;40(2):219-225. doi: 10.1377/hlthaff.2020.01470 [DOI] [PubMed] [Google Scholar]
- 3.von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle. 2010;1(2):129-133. doi: 10.1007/s13539-010-0014-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landi F, Liperoti R, Fusco D, et al. Prevalence and risk factors of sarcopenia among nursing home older residents. J Gerontol A Biol Sci Med Sci. 2012;67(1):48-55. doi: 10.1093/gerona/glr035 [DOI] [PubMed] [Google Scholar]
- 5.Moon HE, Paek SH. Mitochondrial dysfunction in Parkinson’s disease. Exp Neurobiol. 2015;24(2):103-116. doi: 10.5607/en.2015.24.2.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coen PM, Jubrias SA, Distefano G, et al. Skeletal muscle mitochondrial energetics are associated with maximal aerobic capacity and walking speed in older adults. J Gerontol A Biol Sci Med Sci. 2013;68(4):447-455. doi: 10.1093/gerona/gls196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conley KE, Jubrias SA, Esselman PC. Oxidative capacity and ageing in human muscle. J Physiol. 2000;526(pt 1):203-210. doi: 10.1111/j.1469-7793.2000.t01-1-00203.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Short KR, Bigelow ML, Kahl J, et al. Decline in skeletal muscle mitochondrial function with aging in humans. Proc Natl Acad Sci U S A. 2005;102(15):5618-5623. doi: 10.1073/pnas.0501559102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santanasto AJ, Glynn NW, Jubrias SA, et al. Skeletal muscle mitochondrial function and fatigability in older adults. J Gerontol A Biol Sci Med Sci. 2015;70(11):1379-1385. doi: 10.1093/gerona/glu134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fivenson EM, Lautrup S, Sun N, et al. Mitophagy in neurodegeneration and aging. Neurochem Int. 2017;109:202-209. doi: 10.1016/j.neuint.2017.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi R, Guberman M, Kirshenbaum LA. Mitochondrial quality control: the role of mitophagy in aging. Trends Cardiovasc Med. 2018;28(4):246-260. doi: 10.1016/j.tcm.2017.11.008 [DOI] [PubMed] [Google Scholar]
- 12.D’Amico D, Andreux PA, Valdés P, Singh A, Rinsch C, Auwerx J. Impact of the natural compound urolithin A on health, disease, and aging. Trends Mol Med. 2021;27(7):687-699. doi: 10.1016/j.molmed.2021.04.009 [DOI] [PubMed] [Google Scholar]
- 13.Cerdá B, Periago P, Espín JC, Tomás-Barberán FA. Identification of urolithin A as a metabolite produced by human colon microflora from ellagic acid and related compounds. J Agric Food Chem. 2005;53(14):5571-5576. doi: 10.1021/jf050384i [DOI] [PubMed] [Google Scholar]
- 14.Singh A, D’Amico D, Andreux PA, et al. Direct supplementation with urolithin A overcomes limitations of dietary exposure and gut microbiome variability in healthy adults to achieve consistent levels across the population. Eur J Clin Nutr. 2021. doi: 10.1038/s41430-021-00950-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryu D, Mouchiroud L, Andreux PA, et al. Urolithin A induces mitophagy and prolongs lifespan in C. elegans and increases muscle function in rodents. Nat Med. 2016;22(8):879-888. doi: 10.1038/nm.4132 [DOI] [PubMed] [Google Scholar]
- 16.Luan P, D’Amico D, Andreux PA, et al. Urolithin A improves muscle function by inducing mitophagy in muscular dystrophy. Sci Transl Med. 2021;13(588):eabb0319. doi: 10.1126/scitranslmed.abb0319 [DOI] [PubMed] [Google Scholar]
- 17.Andreux PA, Blanco-Bose W, Ryu D, et al. The mitophagy activator urolithin A is safe and induces a molecular signature of improved mitochondrial and cellular health in humans. Nat Metab. 2019;1(6):595-603. doi: 10.1038/s42255-019-0073-4 [DOI] [PubMed] [Google Scholar]
- 18.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 19.Liu SZ, Valencia AP, VanDoren MP, et al. Astaxanthin supplementation enhances metabolic adaptation with aerobic training in the elderly. Physiol Rep. 2021;9(11):e14887. doi: 10.14814/phy2.14887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roshanravan B, Liu SZ, Ali AS, et al. In vivo mitochondrial ATP production is improved in older adult skeletal muscle after a single dose of elamipretide in a randomized trial. PLoS One. 2021;16(7):e0253849. doi: 10.1371/journal.pone.0253849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jubrias SA, Crowther GJ, Shankland EG, Gronka RK, Conley KE. Acidosis inhibits oxidative phosphorylation in contracting human skeletal muscle in vivo. J Physiol. 2003;553(pt 2):589-599. doi: 10.1113/jphysiol.2003.045872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: six-minute walk test, Berg balance scale, timed up & go test, and gait speeds. Phys Ther. 2002;82(2):128-137. doi: 10.1093/ptj/82.2.128 [DOI] [PubMed] [Google Scholar]
- 23.Bohannon RW, Crouch R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. J Eval Clin Pract. 2017;23(2):377-381. doi: 10.1111/jep.12629 [DOI] [PubMed] [Google Scholar]
- 24.Johnson MA, Polgar J, Weightman D, Appleton D. Data on the distribution of fibre types in thirty-six human muscles: an autopsy study. J Neurol Sci. 1973;18(1):111-129. doi: 10.1016/0022-510X(73)90023-3 [DOI] [PubMed] [Google Scholar]
- 25.Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014;69(suppl 1):S4-S9. doi: 10.1093/gerona/glu057 [DOI] [PubMed] [Google Scholar]
- 26.Hilvo M, Meikle PJ, Pedersen ER, et al. Development and validation of a ceramide- and phospholipid-based cardiovascular risk estimation score for coronary artery disease patients. Eur Heart J. 2020;41(3):371-380. [DOI] [PubMed] [Google Scholar]
- 27.Kurz J, Parnham MJ, Geisslinger G, Schiffmann S. Ceramides as novel disease biomarkers. Trends Mol Med. 2019;25(1):20-32. doi: 10.1016/j.molmed.2018.10.009 [DOI] [PubMed] [Google Scholar]
- 28.Lassale C, Batty GD, Steptoe A, et al. Association of 10-year C-reactive protein trajectories with markers of healthy aging: findings from the English Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci. 2019;74(2):195-203. doi: 10.1093/gerona/gly028 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable. No Impact on Muscle Size During the Study Intervention Period
eFigure 1. Change in TA ATPmax
eFigure 2. Percent Change in Number of Muscle Contractions in Skeletal Muscle
eFigure 3. UA Bioavailability in the Study Population
eFigure 4. UA Impact on Plasma Acylcarnitine and Ceramide Levels
Data Sharing Statement