Abstract
Obesity is a worrisomely escalating public health problem globally and one of the leading causes of morbidity and mortality from noncommunicable disease. The epidemiological link between obesity and a broad spectrum of cardiometabolic disorders has been well documented; however, the underlying pathophysiological mechanisms are only partially understood, and effective treatment options remain scarce. Given its critical role in glucose metabolism, skeletal muscle has increasingly become a focus of attention in understanding the mechanisms of impaired insulin function in obesity and the associated metabolic sequelae. We examined the current evidence on the relationship between microvascular dysfunction and insulin resistance in obesity. A growing body of evidence suggest an intimate and reciprocal relationship between skeletal muscle microvascular and glucometabolic physiology. The obesity phenotype is characterized by structural and functional changes in the skeletal muscle microcirculation which contribute to insulin dysfunction and disturbed glucose homeostasis. Several interconnected etiologic molecular mechanisms have been suggested, including endothelial dysfunction by several factors, extracellular matrix remodelling, and induction of oxidative stress and the immunoinflammatory phenotype. We further correlated currently available pharmacological agents that have deductive therapeutic relevance to the explored pathophysiological mechanisms, highlighting a potential clinical perspective in obesity treatment.
Keywords: obesity, microvascular dysfunction, insulin resistance, skeletal muscle, obesity treatment
1. Introduction
Obesity (body mass index (BMI) ≥ 30.0 kg/m2) [1] is an escalating global health challenge affecting 13% of the world’s population, according to recent World Health Organization estimates [2]. Over the past five decades, the global prevalence of obesity has risen to pandemic proportions [3,4]. The rising global trend of obesity is associated with the increasing prevalence of diabetes mellitus (DM) type 2, hypertension and other cardiovascular morbidities, liver disease, and malignancies [5,6]. Much of the obesity-related mortality is due to cardiovascular disease, but although the epidemiological links between obesity and a broad spectrum of cardiometabolic disorders are clearly recognised, the specific pathophysiological mechanisms are not yet fully understood [6,7].
Skeletal muscle accounts for 40–50% of the total body mass and structurally consists of multiple fascicles or bundles of different physiochemically and metabolically distinct fibre types, classified based on the expression of different myosin heavy-chain isoforms [8,9]. The skeletal muscle represents the largest endocrine tissue involved in glucose metabolism, mediating ~80% of insulin-stimulated glucose uptake under euglycemic hyperinsulinaemic conditions [10]. Decreased sensitivity for insulin-mediated glucose uptake in skeletal muscle is a core pathophysiological denominator in obesity-related alterations in metabolic phenotype [11]. However, the exact mechanisms of such attenuated biological response are not fully understood. Skeletal muscle microvascular and metabolic physiology and pathophysiology are closely linked, and a growing body of evidence has confirmed the critical role of microvascular dysfunction (inadequate microvascular response to physiologic metabolic demand or challenge) in the mediation of obesity-related insulin resistance [12,13,14,15]. Several pathophysiological mechanisms in obesity, e.g., oxidative stress, alterations in adipokine secretion, decreased adiponectin levels, increased inflammatory mediators, and increased activation of the renin–angiotensin system, may contribute to impaired microvascular dilatation and insulin-mediated capillary recruitment, leading to suboptimal glucose and insulin delivery to the skeletal muscle, and subsequent impaired glucose homeostasis [16,17,18,19,20]. Previously, microvascular dysfunction was merely regarded as a diabetic sequela, manifesting as classical microangiopathic complications such as retinopathy, nephropathy, and neuropathy. Current evidence, however, demonstrates that microvascular dysfunction and hyperglycaemia exhibit a bidirectional relationship: microvascular dysfunction antedates and mediates hyperglycaemia in insulin-resistant states, while being a known consequence of prediabetic and diabetic levels of hyperglycaemia [21,22]. It has equally been shown that microvascular and macrovascular complications share similar risk factors and reciprocal pathophysiological mechanisms [23].
In chronic obesity, microvascular dysfunction has been shown to mediate impaired insulin sensitivity and β-cell dysfunction via multifactorial mechanisms, providing scaffolding for subsequent hyperglycaemic sequelae and complications, including multiorgan microangiopathy [13,21,24,25]. Therefore, targeting microvascular dysfunction in this vicious cycle may provide an important pharmacotherapeutic window for preventing or abrogating obesity-related insulin resistance and its ramifications. Recent clinical evidence shows that optimizing glycaemic control improved microvascular function in early but not advanced phase of DM type 2, suggesting a strong benefit of initiating early aggressive interventions to prevent or attenuate the progression of microvascular complications and insulin-resistant phenotypes [26]. The aim of this paper was to review the general background of the relationship between skeletal muscle microvascular and metabolic physiology, as a point of departure to explore the etiological role of microvascular dysfunction in obesity-related insulin resistance. Furthermore, it also highlights the therapeutic implications of the elucidated pathophysiological mechanisms and correlates the currently available or potential pharmacological agents that bear important therapeutic relevance.
2. Vascular and Metabolic Physiology of Skeletal Muscle Microcirculation
2.1. Anatomical Background
Microcirculation includes all vessels less than 150 μm in diameter, namely capillaries, venules, and third- or fourth-order arterioles [27]. However, this definition excludes larger arterioles with important microcirculatory function. A more inclusive definition based on vessel physiology considers all vessels that myogenically alter the luminal diameter in response to increased pressure as part of the microvasculature [14,27]. Arterioles consist of a layer of smooth muscle cells surrounding a layer of endothelial cells, while capillaries consist of a monolayer of squamous endothelial cells without a muscle layer. The microcirculation represents much of the total vascular surface area and controls the delivery of oxygen and nutrients to tissues by regulating capillary vascular resistance and trans-endothelial exchange of blood solutes.
Although the skeletal muscle’s microvascular histological architecture varies according to muscle typology and location, the basic gross anatomical characteristics are shared. One or more feed arteries in the epimysium ramify into an intertwined network of arterioles in the perimysium, which then branch at regular intervals into transverse arterioles that pierce the endomysium and asymmetrically divide into terminal arterioles that give rise to capillary networks running parallel to the muscle fibres. The venules arise from the contralateral loop of the capillary arcade and ramify progressively into larger venules in tandem with the arteriolar branching. Each muscle fibre is perfused by multiple terminal arterioles and capillary units along its length, and the loop of capillaries supplied by one terminal arteriole and drained by a venule constitutes the microvascular unit which represents the basic functional unit of skeletal muscle microcirculation [28].
2.2. The Microvascular Endothelium Is the Key Regulator of Vascular Homeostasis
The regulation of microvascular function is controlled by the balance in the activation of the sympathetic and parasympathetic nervous system, as well as by local metabolic and myogenic autoregulatory mechanisms. The microvascular endothelium plays multifaceted biological functions, including serving as a semipermeable physiological barrier and component of innate immunity, as well as regulation of vascular tone, mechano-transduction, procoagulant/anticoagulant balance, endothelial repair, and angiogenesis, among other functions [29]. It produces both vasodilators/anti-thrombogenic factors and vasoconstrictors/prothrombotic factors. The former include nitric oxide (NO), prostacyclin, bradykinin, and endothelium-derived hyperpolarizing factor, while the latter consists of endothelin-1 (ET-1), angiotensin II (Ang II), thromboxane A2 (TXA2), prostacyclin H2, and superoxide [30]. These vasoactive molecules may act in autocrine, paracrine, or endocrine fashion to regulate vessel tone and diameter, proliferation of vascular smooth muscle cells (VSMC), and activation and adhesion of platelets and leukocytes.
NO is the most characterized endothelium-derived relaxing factor and is synthesized by the calcium-calmodulin-dependent endothelial nitric oxide synthase (eNOS) from L-arginine substrate, with tetrahydrobiopterin (BH4) as co-factor. Various mechanisms of eNOS activation have been identified, including phosphorylation, glutathionylation, S-nitrosylation, and N-acetyl glycosylation [31]. Insulin induces insulin receptor substrates (IRS) 1 and 2 signalling, which activates the phosphatidylinositol 3-kinase (PI3K) and protein kinase B (Akt), to phosphorylate eNOS at Ser1177 (in humans), catalysing the conversion of L-arginine to L-citrulline and NO [32]. Several cofactors, including calmodulin, flavinmononucleotide, flavin adenine dinucleotide, and nicotinamide adenine dinucleotide phosphate, are involved in this reaction [33]. NO diffuses to the vascular smooth muscle cells, where it mediates vasodilatation by activating guanylate cyclase to catalyse increased cyclic guanosine monophosphate (cGMP) synthesis [34].
2.3. Role of Insulin in the Regulation of Microvascular Tone
Vascular smooth muscle tone is maintained by the dynamic balance of the endothelium-derived relaxing and contracting factors. This vasomotor balance may shift in response to both mechanical factors such as enhanced shear stress, and endocrine factors such as insulin. Insulin is a potent hormone produced by the pancreatic β-cell of the Islets of Langerhans, which exerts a wide range of anabolic effects, including promoting glucose uptake in skeletal muscles and adipocytes, glycogen synthesis in skeletal muscles, and triacylglycerol synthesis in adipocytes and suppressing glucose production in hepatocytes and lipolysis in adipocytes [35].
In healthy vasculature, insulin predominantly mediates microvascular dilatation by activating PI3K with consequent eNOS activation and NO production, although it can also mediate vasoconstriction by increasing ET-1 and vasoconstrictor eicosanoids via the intracellular mitogen-activated protein kinase (MAPK) signalling pathway and the extracellular signal-regulated kinase-1/2 (ERK-1/2) pathway [30,36,37]. Insulin signal transduction via the PI3K/Akt pathway also modulates vascular immuno-inflammation by increasing vascular endothelial growth factor (VEGF) and hemeoxygenase-1 expression and decreasing vascular cell adhesion molecule 1(VCAM-1) expression [38].
The ET-1/NO balance is maintained in favour of insulin-stimulated vasodilatation, which enhances downstream capillary perfusion and trans-endothelial transport of insulin. Direct visualisation of the trans-endothelial transport of fluorescent insulin shows that the movement to the skeletal muscle interstitium occurs by a fluid-phase transport mechanism that is receptor-dependent and regulated by the balance of oncotic and hydrostatic pressures [39]. The ability of insulin to dose- and time-dependently increase total skeletal muscle blood flow and consequent insulin-mediated glucose uptake via dilatation of resistance vessels was first reported by Baron and colleagues about three decades ago and demonstrates the link between the vascular and metabolic function of insulin [40,41,42].
2.4. Functional Capillary Recruitment
Furthermore, it has also been established that without increasing total blood flow, insulin can selectively redirect microvascular circulation in favour of perfusion of nutritive capillary beds by decreasing precapillary arteriolar tone or altering arteriolar vasomotor response, facilitating glucose delivery and uptake in skeletal muscle [43,44]. During physiologic hyperinsulinaemia or glucose challenge, contrast-enhanced ultrasound has been used to demonstrate in vivo that capillary recruitment is an early forerunner phenomenon to muscle glucose uptake, ensuring a maximal metabolic effect of insulin [45]. The resistance arterioles that regulate total blood flux were shown to be less insulin-sensitive than the precapillary arterioles mediating microvascular recruitment [44]. This functional capillary recruitment which accounts for about 40% of insulin-mediated muscle glucose uptake is dependent on the activation of endothelial PI3K pathway including autophosphorylation of the insulin receptor, phosphorylation of tyrosine residues of the IRS-1 and 2, and phosphorylation of phosphoinositide-dependent kinase 1 (PDK-1) and Akt, leading to the translocation of glucose transporter-4 (GLUT-4) to the cell membrane, which is the rate-limiting process for skeletal muscles’ insulin-mediated glucose uptake [14,15,46].
2.5. Assessment of Skeletal Muscle Microvascular Structure and Function
Microvasculature research remains relatively underdeveloped, largely on account the limitations in techniques for morphological and functional studies. Accordingly, it is hoped that our understanding of the physiological mechanisms of microvascular function will continue to evolve as new study techniques emerge. Currently, microvascular function in skeletal muscles can be measured by plethysmography, contrast-enhanced ultrasonography, intravital microscopy, plasma concentration of several endothelial biomarkers, and other surrogate clinical markers such as urinary albumin excretion [36,44,45,47,48,49,50,51]. Additionally, application of various stimuli including local ischaemia, temperature changes, and vasoactive agents such as acetylcholine, adenosine, serotonin, bradykinin, and sodium nitroprusside, can be used to study microvascular response. Histological assessment of skeletal muscle microvasculature is conventionally accomplished by two-dimensional (2D) analyses of tissue cross-sections [52,53], although recently, a three-dimensional (3D) analytic technique that overcomes the usual technical biases and inconsistencies associated with the traditional 2D approach has been proposed [54,55,56].
3. Skeletal Muscle Microvascular Dysfunction in Obesity
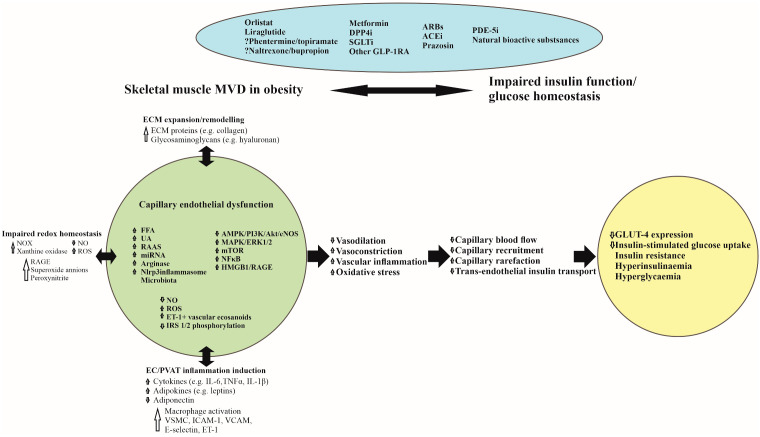
Obesity is associated with a broad spectrum of metabolic derangements including hyperglycaemia, insulin resistance, and a proinflammatory milieu, all of which contribute to vascular endothelial vasodilator and fibrinolytic dysfunction and extracellular matrix remodelling [47]. Insulin resistance precedes the development of hyperglycaemia and DM type 2 and results in compensatory hyperinsulinaemia, which contributes to increased inflammation and oxidative stress. Elevated plasma free fatty acids (FFAs) is considered an important etiologic factor linking insulin resistance, oxidative stress, and inflammation with obesity and other cardiometabolic disorders, and impaired insulin-mediated glucose uptake correlates with circulating FFA levels [57,58]. The increased circulating free fatty acids in obesity probably triggers the early phase of microvascular dysfunction via downregulation of the of the endothelial AMPK-PI3K-Akt-eNOS pathway [59], while other factors such as alterations in adipokines (e.g., leptins, adiponectin, monocyte chemotactic protein-1, and retinol binding protein 4) and inflammatory cytokines (e.g., interleukin-6 (IL-6), and tumour necrosis factor-alpha (TNFα)) released from both visceral and perivascular adipose tissue, help to drive the progression of the dysfunction (Figure 1) [60,61,62]. Besides visceral or extracellular lipids, accumulation of saturated lipid droplets, mainly triglycerides, in skeletal muscle fibres has been shown to have a pathogenic role in insulin resistance [63]. It was recently demonstrated that such intramyocellular lipid accumulation exhibit both muscle- and fibre-type specificity in obese mice, meaning that similar muscle fibres in different muscles may show different pattern of lipid accumulation [9]. Moreover, it was also shown that capillary network changes in obesity are muscle-fibre-specific, being more pronounced around small and more oxidative muscle fibres than around large fibres [56].
Figure 1.
Pathophysiological mechanisms linking skeletal muscle microvascular dysfunction with glucometabolic disorder in obesity and potential therapeutic agents. ACEi, Angiotensin-Converting Enzyme inhibitors; AMPK 5’-, Adenosine Monophosphate-activated Protein Kinase; ARBs, Angiotensin Receptor Blockers; Akt, Protein Kinase B; DPP4i, Dipeptidyl-Peptidase-4 inhibitors; EC, Endothelial Cell; ECM, Extracellular Matrix; eNOS, endothelial Nitric Oxide Synthase; ERK, Extracellular-signal-regulated Kinase; ET-1, Endothelin 1; FFA, Free Fatty Acids; GLP-1RA, Glucagon-like Peptide-1 Receptor Agonists; GLUT-4, Glucose Transporter 4; HMGB 1, High Mobility Group Box chromosomal protein 1; IRS, Insulin Receptor Substrate; ICAM1, Intercellular Adhesion Molecule 1; IL-1β, Interleukin-1Beta; IL-6, Interleukin-6; MAPK, Mitogen-Activated Protein Kinase; miRNAs, Micro RNAs; mTOR, Mammalian Target of Rapamycin; MVD, Microvascular Dysfunction; NF-κB, Nuclear Factor-Kappa B; NO, Nitric Oxide; NOX, Nicotinamide Adenine Dinucleotide Phosphate (NADPH) Oxidase; PDE-5i, Phosphodiesterase-5 inhibitors; PI3K, Phosphatidylinositol 3 Kinase; RAAS, Renin-Angiotensin-Aldosterone System; ROS, Reactive Oxygen Species; RAGE, Receptor for Advanced Glycation End products; SGLT2i, Sodium Glucose co-Transporter 2 inhibitors; TNF-α, Tumour Necrosis Factor-alpha; UA, Uric Acid; VCAM1, Vascular Cell Adhesion Molecule 1; VSMC, Vascular Smooth Muscle Cells.
3.1. Skeletal Muscle Microvascular Functional and Structural Dynamics in Obesity
Skeletal muscle microvascular perfusion, blood flow dynamics, and insulin permeability are critical determinants of insulin action in skeletal muscles and have become a compelling focus of investigation in studying disorders of glucose metabolism. While some studies have described relatively preserved skeletal muscle blood flow in obese young adult humans [64,65,66], several other investigations in obese humans and animal models suggest a blunted vascular conductance that is independent of age and vascular bed [24,67,68,69,70,71]. In a systematic review and meta-analysis probing the association between BMI and retinal vascular calibre, a surrogate marker of microvascular disease, Boillot et al. noted a narrower retinal arteriolar and wider venular calibres in both adults and children with increasing BMI, affirming that the biological mechanisms of microvascular dysfunction are similar across organs and independent of age [16].
Obesity is associated with decreased endothelial NO production, decreased insulin-stimulated vasomotion, and reduced capillary density, leading to impaired insulin-mediated capillary recruitment and microvascular dilatation [24]. During an insulin clamp, impaired capillary insulin delivery in humans with prediabetes and mouse models of insulin resistance results in increased insulin concentration gradient from plasma to the interstitial fluid [51,72,73]. Skeletal muscle perfusion is determined by changes in the flux rate through individual capillaries and the number of actively perfused capillaries. The capacity of vasodilators such as the phosphodiesterase (PDE5) inhibitor sildenafil to improve vascular function and prevent diet-induced insulin resistance in obese mice [74,75] provides indirect evidence that impaired capillary blood flow is an important mechanism of the development of obesity-related insulin resistance and the progression of prediabetes to diabetes. Conversely, Chadderdon et al. noted that in the early phase of high-fat diet-induced obesity in rhesus macaques, an increased basal and glucose-mediated capillary blood volume via endothelial-derived vasodilator pathways, may represent a compensatory mechanism for insulin resistance [76].
Besides changes in microvascular blood flow dynamics, structural changes in capillaries may contribute to insulin resistance [56]. In obesity, actual reduction of microvessel per given tissue volume, or structural capillary regression, has been suggested to be biphasic: an early phase characterized by increased leukocyte adhesion/rolling, oxidant stress, tumour necrosis factor-alpha (TNF-α) levels, and vascular TXA2 and a later phase mediated by impaired NO-bioavailability [71,77]. Several mechanisms including endothelial dysfunction, oxidative stress, apoptosis, and other antiangiogenic factors are thought to underlie capillary regression. Capillary rarefaction in skeletal muscle vascular endothelial growth factor (VEGF)-knockout mice was associated with reduced skeletal muscle insulin-stimulated glucose uptake and glucose tolerance [78]. In contrast to the suggestions that capillary regression contributes to the pathogenesis of skeletal muscle insulin resistance, increased skeletal muscle capillarisation has been demonstrated both in a mouse model of early-stage obesity with insulin resistance [56,79] and in middle-aged men with impaired glucose tolerance precedent to the development of DM type 2 [80]. Thus, the precise role of skeletal muscle capillary rarefaction in the pathophysiology of insulin resistance remains a subject for continued investigation.
Remarkably, sexual dimorphism in skeletal muscle functional and metabolic properties have been well-described in animal models in terms of fibre typology, microvascular architecture, and transcriptomics profile, reflecting the genomic and non-genomic influences of reproductive hormones and sex-specific gene expression [81,82]. In obesity, sex differences have been reported in the interplay of skeletal muscle microvascular dysfunction and metabolic dysregulation. High-fat-diet-induced obesity in male C57BL/6 mice was associated with impaired vasoconstriction in second-order arterioles compared to male control, whereas diet-induced obesity in the female model resulted in significant alterations in both arteriolar vasodilation and vasoconstrictor responses compared to a female control [83].
3.2. Endothelial Dysfunction Is the Key Driver of Microvascular Dysfunction in Obesity
As already noted, the vascular endothelium plays a critical role in the regulation of vascular permeability and tone, and endothelial vasodilator dysfunction in the peripheral microcirculation is a hallmark of chronic obesity and insulin resistance and precedes the development of DM type 2 [18,24,68,69,70]. Using peripheral arterial tonometry and laser Doppler flowmetry, van der Heijden et al. recently demonstrated that higher BMI was significantly associated with impaired endothelial function even after adjustment for confounding risk factors such as diabetes mellitus, hypertension, hypercholesterolemia, and smoking [18]. Endothelial cell dysfunction results in impaired NO bioavailability, and enhanced platelet activation, smooth muscle cell proliferation, and adhesion molecule expression [17,84,85,86,87]. In addition, obesity is associated with ultrastructural alterations in the skeletal muscle capillary endothelium, which impair trans-endothelial insulin transport, a critical step in skeletal muscle glucose uptake [51].
Insulin-stimulated NO-dependent skeletal muscle microvascular dilatation involves several mechanisms including activation of the insulin receptor, IRS1 and 2, and the PI3K-Akt-eNOS pathway [32,88]. Decreased expression of IRS-1 and 2 and decreased phosphorylation of Akt and eNOS are key hallmarks of vascular insulin resistance [37,48]. Attenuation of insulin-induced capillary recruitment and consequent reduction in glucose uptake by skeletal muscle was demonstrated in tissue-specific knockout mice lacking endothelial IRS-2 [73]. In obesity, insulin-mediated vasoconstriction via the activation of the ERK1/2 pathway becomes dominant, as its activation of the PI3K pathway in endothelial cells is selectively inhibited, consequently blocking downstream capillary recruitment [36,61].
Increased circulating free fatty acids seen in obesity mediates endothelial dysfunction through several mechanisms including decreased tyrosine phosphorylation of IRS-1/2, impaired phosphorylation of eNOS via inhibition of the PI3K/Akt pathway, impaired ATP-induced mobilization, and influx of calcium in endothelial cells, increased ROS production via protein kinase C (PKC)-dependent activation of NADPH oxidase and consequent stimulation of inflammation via NF-κB activation [57,58,62]. Additionally, the role of inflammasome activation in free-fatty-acid-induced endothelial injury in obesity has been increasingly demonstrated [89,90,91]. It was shown that palmitate markedly induces Nlrp3 inflammasome complex formation in microvascular endothelial cells, leading to downregulation of inter-endothelial tight junction proteins ZO-1/ZO-2, which correlates with increased paracellular endothelial permeability [91]. Additionally, chronic exposure to palmitate has been shown to impair autophagic turnover by decreasing lysosomal acidification via suppressed mitochondrial bioenergetics and cellular ATP levels [92]. Autophagy plays a critical role in the maintenance of endothelial NO bioavailability and regulation of oxido-inflammatory balance, and defective autophagic flux contributes to endothelial dysfunction [93].
Obesity and other insulin-resistant phenotypes are associated with hyperuricaemia [94,95,96]. High uric acid concentration has been suggested to induce endothelial dysfunction via the interaction of high-mobility group box chromosomal protein 1 with the receptor for advanced glycation end products (HMGB1/RAGE pathway). In human umbilical vein, uric acid was shown to inhibit eNOS expression and NO production by increasing the intracellular expression and extracellular secretion of HMGB1, enhancing the expression of RAGE, activating NF-κB, and upregulating the levels of adhesion molecules and inflammatory cytokines including ICAM-1, VCAM-1, TNF-α, and IL-6 [97].
Recent studies have indicated that the upregulation of arginase, a dual isoform manganese metalloenzyme of the urea cycle, represents another important mechanism of endothelial dysfunction. Arginase hydrolyses L-arginine to urea and L-ornithine, and because L-arginine is a common substrate of eNOS and arginase, increased expression or activity of the latter reduces eNOS-dependent NO synthesis in the vascular endothelium via substrate competition [98,99,100]. An enhanced vascular activity and expression of arginase has been demonstrated in obesity [101,102,103]; however, the contribution of this to microvascular endothelial dysfunction is attenuated by aging due to the overriding modulation by the high levels of vascular reactive oxygen species (ROS) from age-dependent increased activity of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase [103].
The enhanced activation of the renin–angiotensin–aldosterone system in obesity further contributes to vascular insulin resistance and endothelial dysfunction. Both Ang II and aldosterone induce degradation of IRS-1; the former via the proto-oncogene tyrosine-protein kinase Src, and the latter via a mineralocorticoid receptor-, ROS-, and Src-dependent mechanism [104,105]. Aldosterone promotes insulin resistance via increased insulin-like growth factor (IGF)-1 receptor expression and hybridization with IRS-1, in addition to mediating Ang II-stimulated ERK1/2 phosphorylation in vascular smooth muscle cells [106,107]. Furthermore, more recent evidence suggests that increased expression of Ang II and the activation of mineralocorticoid receptor by aldosterone may activate the mammalian target of rapamycin (mTOR)–S6K1 signal transduction pathway and promote insulin resistance by inducing phosphorylation of serine residues of IRS [108].
Vascular endothelial dysfunction related to glucometabolic dysregulation may also result from enhanced expression of several endothelial miRNAs (short, single-stranded, non-coding RNA molecules) which mediate gene-regulatory mechanisms in angiogenesis, vascular repair, and inflammation. Obesity has been associated with enhanced expression of miR-24, miR-155, miR-15b, miR-16, miR-221/222, and miR-765, which mediate endothelial dysfunction via direct inhibition of eNOS translation [109,110].
Furthermore, gut microbiota and their metabolites have been suggested to play an important role in vascular homeostasis through different mechanisms, notably by influencing endothelial NO production and bioavailability and the expression of immunoinflammatory mediators [111,112,113,114]. It was shown that gut microbiota can impair endothelium-dependent vasorelaxation by remotely downregulating Sirtuin1 (Sirt 1) and stimulating the expression of vascular miRNA-204, while broad-spectrum antibiotic administration was shown to reverse high-fat diet induced endothelial dysfunction mediated via the microRNA–Sirt 1 nexus [115]. A study of obese children and adolescents noted a significant positive association between endothelial dysfunction markers such as ICAM-1 and VCAM-1 and changes in gut microbiota [116]. Similarly, a cross-sectional study of aging overweight and obese individuals found that independently of BMI, gut microbiota phenotypes correlated positively with vascular endothelial dysfunction as assessed by reactive hyperaemia index [117].
3.3. Endothelial and Perivascular Adipose Tissue Inflammatory Mediators
The endothelium and perivascular adipose tissue both secrete vasoactive substances and share important common pathways in the regulation of vascular function (NO, prostaglandins, K+ channels, hydrogen peroxide, and hydrogen sulphide) [33]. However, while the role of the endothelium in the regulation of vascular tone has been well established, the mechanisms by which perivascular adipose tissue contributes to microvascular function and dysfunction remains an active area of investigation. Obesity-related chronic inflammatory phenotype is characterized by release of an array of proinflammatory mediators including cytokines (e.g., interleukin-6 (IL-6), interleukin 1β, tumour necrosis factor-α (TNF-α)), and adipokines (e.g., leptins) [118], which promote insulin resistance through alterations in the extracellular matrix, capillary network architecture, and glucose uptake mechanisms. TNF-α regulates insulin-mediated cell signalling, and its increased expression may decrease both insulin-mediated capillary recruitment and glucose uptake in the skeletal muscle by activating the intracellular c-Jun N-terminal kinase (JNK), which attenuates the PI3K pathway and promotes vasoconstriction by activating endothelial ERK-1/2 phosphorylation [119]. Both TNF-α and IL-6 derived from peripheral vascular tissue can stimulate ROS production via activation of NAD(P)H oxidase. Additionally, both inflammatory cytokines can also enhance ROS generation by activating nuclear transcription factor-kappa B (NF-κB) and xanthine oxidase, respectively. It has been further suggested that TNF-α, IL-6, and other inflammatory mediators reduce the production of adiponectin [120,121], an anti-inflammatory adipokine which promotes insulin-mediated vasodilatation through increased eNOS phosphorylation [122]. In concert, these pro-inflammatory mechanisms result in the activation of macrophages, migration, and proliferation of VSMCs, induction of endothelial adhesion molecules such as intercellular adhesion molecule-1 (ICAM1), VCAM-1 and E-selectin, and increased synthesis of endothelin [16,17,123,124]. This suggests that perivascular adipose tissue is an important regulator of vascular homeostasis, and that induction of inflammation represents a pivotal mechanism by which pathological perivascular adipose tissue promotes deleterious effect on the microvasculature [125].
3.4. Dysregulation of Redox Homeostasis
The production of ROS in the mitochondria plays a key role in regulating the cellular redox status. Superoxide is the proximal mitochondrial ROS and rapidly undergoes dismutation to yield hydrogen peroxide, which modulates retrograde redox signalling from the organelle to the cytosol and nucleus. Overproduction of ROS in the mitochondria (superoxide and hydrogen peroxide) induces oxidative damage to mitochondrial proteins, membranes, and DNA, consequently impairing mitochondrial ATP synthesis as well as mitochondrial pathways for fatty acid, urea, and amino acid metabolism [126]. Impaired mitochondrial oxidative phosphorylation tilts the cellular metabolism towards greater reliance on glycolytic ATP production with consequent lactic acid accumulation. It has been suggested that endothelial dysfunction and vascular insulin resistance may result from the impairment of cellular adaptive mechanisms against mitochondrial dysfunction and oxidative stress such as the redox-sensitive transcription factor nuclear factor E2-related factor 2 (Nrf2) and the antioxidant response element (ARE), which modulate cellular antioxidant activity [127,128]. Insulin resistance and persistent hyperglycaemia further exacerbate redox dysregulation through a positive feedback loop [129].
The balance between the vaso-protective NO and the vaso-deleterious ROS is disrupted in the setting of hyperglycaemia and insulin resistance [130]. Hyperglycaemia alters the endothelial redox environment by inducing increased ROS generation via several mechanisms, including PKC-dependent activation of vascular NAD(P)H oxidase [62,131]. Skeletal muscles express three isoforms of NAD(P)H oxidases (NOX1, NOX2, and NOX4), which are critically important in the modulation of redox homeostasis [132]. NOX2 generates most of the skeletal muscle ROS during contractions and is involved in insulin signalling and glucose transport [133,134]. In the setting of hyperglycaemia and hyperinsulinaemia, endothelial NOX2 activation promotes vasoconstriction by altering the balance between MAPK-dependent vasoconstriction and PI3K/Akt-dependent vasodilation [133].
In addition to uncoupling eNOS and impairing endothelium-dependent vasodilation, excess ROS derived from NOX1 and NOX2 in the setting of hyperglycaemia also impairs NO production and bioavailability by increasing the production of superoxide anion, which reacts with NO to form peroxynitrite, which in turn oxidises the eNOS cofactor BH4 [30]. The superoxide anion further enhances ROS generation via increased formation of glucose-derived advanced glycation end products (AGEs) and activation of the AGE receptor on vascular cells [135]. The build-up of AGEs is pathogenically important in the development of arteriosclerosis. Obesity and insulin resistance also decrease NO production via different mechanisms, including blunting of skeletal muscle eNOS expression and activity, consequently impairing the NO-driven endothelium-dependent vasoreactivity [62]. On the other hand, recent studies have suggested that NO can mediate vasoconstriction rather than vasorelaxation in certain conditions, notably hypoxia, via activation of soluble guanylyl cyclase and consequent production of cyclic inosine monophosphate (cIMP) rather than cGMP [30,136].
Much of the highlighted mechanisms have been derived from preclinical studies, and it therefore remains unclear if the findings can be translated to humans. Other areas requiring clarification in this regard include the relative contribution of hyperglycaemia vs. hyperinsulinaemia in the induction of NOX-derived superoxide production, and the interactions and coordination between the different NOX isoforms and between NOX family and other sources of pathological ROS generation [137].
3.5. The Role of Extracellular Matrix Remodelling
The extracellular matrix (ECM) is an important structure in the microvascular environment composed of proteins and proteoglycans. Alterations in this dynamic structure as seen in an inflammatory milieu may mediate skeletal muscle insulin resistance by causing capillary regression and endothelial dysfunction [47]. The chronic inflammatory phenotype seen in obesity and DM type 2 induces compositional changes in the ECM, including increased expression of ECM proteins such as collagen, and glycosaminoglycans such as hyaluronan, which are a major constituent of the capillary luminal endothelial cell glycocalyx [138,139]. The expansion and remodelling of the ECM is associated with capillary rarefaction and insulin resistance. ECM collagen level is inversely related to muscle capillarisation and insulin sensitivity [138,140]. Similarly, decreasing hyaluronan expression using PEGylated hyaluronidase or antibodies against CD44, which is the main hyaluronan cell surface receptor, is associated with improved insulin action [139,141,142].
4. Crossroads of Microvascular Pathophysiology and Pharmacology: Clinical Perspectives in Obesity Treatment
4.1. Current Paradigm
While lifestyle adjustments like increased physical activity and dietary modification and vigilance remain the fundamental treatment modalities for obesity, such conservative approaches are often insufficient, and adjunctive pharmacological or surgical treatment is usually indicated to realise target clinical outcomes [7,143,144]. Remarkably, conservative obesity treatment measures such as physical activity and healthy dietary habits were even further negatively impacted by the series of lockdown measures instituted to limit the spread of the novel coronavirus [145,146], further highlighting the practical need for supportive medical therapy for obesity and related complications. Unfortunately, although several drugs have been approved for the treatment of obesity over the past few decades, most have been withdrawn due to safety concerns, and only a very limited number are currently available for clinical use [147,148]. Even more far-fetched are treatments rationally designed to counteract the pathways and mechanisms of the chronic effects of obesity. Accordingly, an enhanced understanding of the multiple pathophysiological pathways in obesity will be critical in developing or adapting targeted therapies for obesity-related complications.
Current medications approved by the United States Food and Drug Administration (US-FDA) for the treatment of chronic obesity include orlistat (lipase inhibitor, decreases lipid absorption), phentermine/topiramate (norepinephrine/GABA agonist and glutamate antagonist, which suppress appetite), naltrexone/bupropion (opioid receptor antagonist/dopamine agonist and norepinephrine reuptake inhibitor, which increase satiety and suppress appetite), and liraglutide (glucagon-like peptide-1 (GLP-1) agonist, which promotes slow gastric emptying and satiety) [149,150]. However, phentermine/topiramate is currently not approved by the European Medicines Agency (EMA). In February 2020, the US-FDA ordered the withdrawal of lorcaserin, which until then was one of the most frequently prescribed weight-loss drugs since its approval in 2012, following evidence of increased cancer risks by safety clinical trials [149,151]. Other promising anti-obesity drugs that were withdrawn from the market due to life-threatening adverse effects include aminorex, fenfluramine, dexfenfluramine, phenylpropanolamine, rimonabant, and sibutramine (respectively associated with pulmonary hypertension, cardiac valvopathy, valvopathy, stroke, suicidal ideation and behaviour, and myocardial infarction and stroke) [152]. Although the development and maintenance of obesity and its sequelae are mediated by both central and peripheral mechanisms, most of the currently available pharmacological agents for treatment of obesity act primarily on pathways in the central nervous system, and thus expectedly show a wider potential adverse effect profile in both short- and long-term use [148,149]. Furthermore, the recruitment of alternate and counter-regulatory pathways significantly reduces the long-term efficacy of most of the anti-obesity monotherapies [153].
4.2. Targeting Microvascular Inflammatory Phenotype and Endothelial Dysfunction as a Therapeutic Strategy for Insulin Dysfunction in Obesity
Given the limitations of centrally acting anti-obesity medications, specific or adapted therapies targeting the peripheral mechanisms of obesity-related complications seems attractive in terms of risk/benefit balance and the possibilities of tailoring therapy towards the specific downstream metabolic effects of chronic obesity. The mechanisms of the intimate reciprocal relationship between microvascular and metabolic pathophysiology in obesity provides a promising window for pharmacotherapeutic exploitation.
4.2.1. Current Anti-Obesity Drugs
A few studies have evaluated the effects of some of the currently available anti-obesity drugs on inflammatory markers in obese and insulin-resistant patients. The modulation of visceral and vascular inflammatory phenotypes may bear indirect therapeutic relevance to microvascular dysfunction. It was shown that treatment with orlistat for at least 6 months was associated with reduction in serum IL-6, TNFα and high-sensitivity C-reactive protein (hsCRP) levels [154,155]. This anti-inflammatory effect appears to strongly correlate with the degree of weight loss over the treatment duration. Data on the anti-inflammatory properties of naltrexone/bupropion are inconsistent with different trials reporting reductions in hsCRP or no significant change [156]. In the CONQUER trial, phentermine/topiramate was associated with decreased hsCRP and increased adiponectin levels [157].
A randomized, double-blind, placebo-controlled trial in DM type 2 patients with persistent albuminuria showed that liraglutide treatment for 12 weeks reduced TNFα and mid-regional pro-adrenomedullin levels [158]. Liraglutide was also shown to mediate modulatory effects on inflammatory gene expression in peripheral blood mononuclear cells [159]. Using [64Cu] DOTATATE, a novel high-resolution PET tracer, it was recently suggested in a randomized placebo-controlled study that liraglutide treatment reduced vascular inflammation, which is a probable mechanistic explanation of the clinically observed cardiovascular protective effect of GLP-1 receptor agonists [160]. However, this study was limited by a small sample size and the lack of statistical significance in the observed effect. In obese patients with DM type 2, Liraglutide treatment was associated with inhibition of NF-κB pathways and up-regulation of Sirt1 expression, and decreased levels of inflammatory markers such as TNFα and ceruloplasmin [161]. Conversely, compared to the placebo group, 26-week liraglutide treatment in a low- to moderate-risk population DM type 2 patients did not change vascular inflammation as assessed by [18F]-fluorodeoxyglucose PET-CT, although an explorative analysis indicated a possible effect in patients with pre-existing background of cardiovascular disease [162]. Similarly, a 12-week treatment with liraglutide yielded no effect on capillary perfusion or vasomotion in diabetic patients, suggesting that the glycaemic effects of GLP-1-based therapies may be independent of microvascular responses [163]. Further investigations are therefore warranted to clarify the role of GLP-1 receptor agonists in microvascular response.
4.2.2. Anti-Hyperglycaemic and Other Agents
Several other antihyperglycemic agents, notably metformin, dipeptidyl-peptidase (DPP)-4 inhibitors (e.g., vildagliptin, linagliptin), GLP-1 analogues (e.g., exenatide), and sodium-glucose cotransporter 2 inhibitors (SGLT2i) (e.g., empagliflozin), have also been suggested to confer microvascular protective benefit related to, or independent of, glycaemic control mechanisms. Metformin is the first-line drug for treating patients with DM type 2 and is increasingly also used for clinical management of other insulin-resistant states such as prediabetes and polycystic ovarian disease [164] on account of known cardiovascular benefits and pleiotropic effects. A growing body of evidence suggests that metformin improves vascular endothelial dysfunction via AMPK dependent and independent mechanisms, including downregulation of NF-κB and upregulation of PI3K-Akt-eNOS, Sirt1, forkhead box O1 (FOXO1), and krüppel-like factors (KLF) 2 and 4 [29]. Compared to control, obese diabetic patients treated with metformin expressed lower levels of inflammatory markers such as hsCRP, TNF-α, and Toll-like receptors 2/4 [165]. In a recent study on obese newly diagnosed drug-naïve DM type 2 women, metformin treatment for 30 days was associated with increased nutritive microvascular reactivity and functional capillary density during post-occlusive reactive hyperaemia [166].
Metformin and vildagliptin have been suggested to exert microvascular effects via distinct but potentially complementary mechanisms. Following ingestion of a lipid-rich meal, metformin, but not vildagliptin, was shown to increase functional capillary recruitment in obese patients with DM type 2 [167]. Vildagliptin on the other hand increased endothelial-dependent and -independent vasodilatations at the arteriolar level, following 30 days of treatment in obese diabetic women [166]. Conversely, a multicentre, prospective, randomized, parallel-group comparison of double-dose metformin (1–1.5 g/d) vs. low-dose metformin (0.5–0.75 g/d) plus add-on vildagliptin in DM type 2 patients found that combination therapy of vildagliptin and metformin had no effect on endothelial function as assessed by flow-mediated dilation before and after 12 weeks of treatment, although favourable effects on adipokine levels were noted [168]. Furthermore, Petrie et al. also noted that regardless of a wider role in cardiovascular risk management, metformin treatment in patients with long-standing DM type 1 had no effect on endothelial function as assessed by reactive hyperaemia index, or on retinopathy [169]. While linagliptin showed no effect on macrovascular function, it was significantly associated with improved fasting-state microvascular function in DM type 2 patients [170]. An ongoing multinational, randomised, partially double-blind, placebo-controlled clinical trial on the effect of lifestyle and pharmacological interventions on early prevention of hyperglycaemia-related microvascular complications will hopefully shed new light on the effects of metformin and linagliptin on microvascular function in people with prediabetes [171].
Three-month therapy with the GLP-1 receptor agonist exenatide showed a similar effect to metformin on microvascular endothelial function, inflammatory phenotype, and redox homeostasis, as assessed by reactive hyperaemic index, C-reactive protein (CRP), circulating oxidized low-density lipoprotein, and VCAM-1 [172]. However, in obese patients with insulin resistance, acute treatment with exenatide following a high-fat meal was associated with blunted postprandial vasodilatory response [173]. On the other hand, SGLT2 inhibitors such as empagliflozin, canagliflozin, and dapagliflozin, which are clinically remarkable for their favourable cardiovascular and renal profile in diabetic patients [174], have additionally been suggested to have benefits in obesity. In high-fat-diet-induced obese C57BL/6J mice, it was shown that empagliflozin significantly reduced whole body weight and fat, improved metabolic function, and ameliorated obesity-related myocardial hypertrophy/fibrosis and dysfunction [175]. These effects were mediated via upregulation of Sestrin2-mediated increase in AMPK and eNOS phosphorylation and inhibition of Akt and mTOR phosphorylation. Sestrin2 is a stress-inducible protein that regulates AMPK-mTOR signalling and redox homeostasis. However, in patients with DM type 2 and cardiovascular morbidity, empagliflozin treatment for 24 weeks had no effect on peripheral endothelial function, suggesting that its cardiovascular benefits may be attributed to other mechanisms rather than improvement in endothelial function [176].
Targeting the mammalian Sirt1, which reciprocally activates AMPK to inhibit lipid accumulation and stimulate fatty acid oxidation, has also been proposed as a therapeutic option in obesity. L-leucine and metformin are a known allosteric activator and a synergistic coactivator of Sirt1, respectively, while sildenafil is a phosphodiesterase-5 inhibitor and vasodilator which indirectly stimulates Sirt1 by increasing NO bioavailability. The Leucine–Metformin–Sildenafil fixed-dose combination is a pharmacologic attempt to synergistically exploit these mechanisms, and recent randomized control trials noted significant weight reduction in obese non-diabetic patients treated for 16 and 24 weeks [177,178].
It has also been shown that alpha adrenergic blockers (e.g., prazosin) can mediate capillary growth in human skeletal muscles via increased shear stress [179,180]. While this angiogenic effect may beneficially counteract structural capillary regression and its metabolic sequelae in obesity, the pharmacodynamic mechanisms exploited here are not directly related to the microvascular metabolic mechanisms described in the pathogenesis of obesity-related insulin resistance. Furthermore, given the contribution of the renin–angiotensin–aldosterone system to the pathogenesis of endothelial dysfunction, angiotensin-converting enzyme inhibitors (ACEi, e.g., lisinopril) and angiotensin receptor blockers (ARBs, e.g., losartan) have been shown to exert microvascular protective and insulin resistance counteractive effects beyond their basic antihypertensive actions. Besides improving endothelial function and redox homeostasis, the peripheral vasodilatory actions of ACE inhibitors and ARBs contribute to enhanced skeletal muscle blood flow. A meta-analysis of 12 randomized controlled clinical trials of ACEi or ARBs found that both antihypertensive medication types decreased the incidence of new-onset diabetes by 27% and 23%, respectively, highlighting a significant clinical benefit in patients with prediabetic conditions such as obesity and metabolic syndrome [181].
4.2.3. Experimental Phytochemicals and Dietary Interventions
Several medicinal herbs have been suggested to have therapeutic benefit in vascular endothelial dysfunction, notably via anti-inflammatory, anti-oxidative, and anti-apoptotic effects. For example, traditional Chinese medicinal herbs like Danshen (Salvia miltiorrhiza), Shanchi (Panax notoginseng), Shanzai (Hawthorn), and Heshouwu (Polygonum multiflorum Thunb) were shown to decrease apoptosis and inhibit adhesion molecule expression in human umbilical vein endothelial cells [182]. Similarly, Naoxintong, a compound herbal mixture containing Radix Astragali, Angelicae sinensis, Paeoniae radix rubra, and Ligusticum wallichii, was shown to improve the protective effect of high-density lipoprotein on endothelial function in DM type 2 patients [183]. Hydroalcoholic extract of Teucrium polium, a traditional antidiabetic medicinal herb, improved endothelial dysfunction by regulating vasoreactivity and eNOS and VCAM-1 genes’ expression in streptozocin-induced diabetic rats [184]. However, the specific chemical compounds responsible for the putative pharmacologic effect of the herbal extracts, and their toxicological properties, are yet to be identified and characterized.
Other bioactive compounds have also been suggested to exert microvascular protective actions in obesity via favourable effects on various microvascular dysfunction pathophysiological mechanisms described above. A typical example is resveratrol, a naturally occurring polyphenolic phytoalexin found in red wine that modulates endothelial function by targeting AMPK, eNOS, nuclear factor-erythroid-derived 2-related factor-2 (Nrf2), KLF2, and NF-κB [185]. In addition, polyphenol compounds such as chlorogenic acid, piceatannol, taxifolin, quercetin, fisetin, kaempferol, and caffeic acid have been shown to inhibit arginase activity and enhance endothelial function by increasing NO levels and decreasing ROS generation [186]. Other naturally occurring bioactive compounds with suggested beneficial effects in microvascular dysfunction include garlic, cinnamon, olive, extra virgin olive oil, ginger, cocoa (modulation of endothelial function), hydroxytyrosol, oleocanthal, and quercetin (modulation of inflammation and oxidative stress) [187]. Furthermore, given the increasing recognition of the role of gut microbiota in pathogenesis of vascular endothelial dysfunction, several interventions targeting gut dysbiosis have been suggested, including high-fibre diet, zinc supplementation, use of pre- or probiotics and faecal microbiota transplantation [188].
5. Conclusions
In this review, we discussed the current evidence on the relationship between skeletal muscle microvascular dysfunction and insulin resistance in obesity. Several reciprocal and interconnected pathways were shown to intimately link microvascular physiology and metabolic functions, with the delicate balance in these pathways disrupted in obesity. Several intertwined mechanisms, including endothelial cell dysfunction from various factors, induction of immuno-inflammatory cascades in endothelial cells and perivascular adipocytes, dysregulation of redox hemostasias and extracellular matrix remodelling, are thought to mediate obesity-related structural and functional alterations in skeletal muscle microcirculation and contribute to insulin dysfunction and glucose dysregulation. We further reviewed the therapeutic implications thereof by correlating the explored peripheral pathophysiological mechanisms with clinical and pharmacodynamic data on both currently approved and adapted medications for treatment of obesity and its complications.
While several preclinical studies have suggested a close link between microvascular and metabolic dysfunction in obesity, overall, the paucity of clearcut prospective evidence for many of the suggested mechanisms means that direct causal effect awaits conclusive proof. Similarly, while many of the examined anti-obesity medications appear to make pathophysiological sense, remarkable inconsistencies in the clinical data question suggested effects and benefits. Nevertheless, adapting existing or developing novel therapies targeting peripheral mechanisms such as the pathophysiological interface between skeletal muscle microvascular and metabolic function in obesity still represents a rational perspective in obesity pharmacotherapy requiring further exploration.
Acknowledgments
We are thankful to Thomas Puhov for assistance with graphics and to Ida Eržen for many stimulating discussions.
Abbreviations
| AMPK | 5’-Adenosine Monophosphate-activated Protein Kinase |
| Akt | Protein Kinase B |
| AGEs | Advanced Glycation End Products |
| Ang | Angiotensin II |
| ARBs | Angiotensin Receptor Blockers |
| ARE | Antioxidant response element |
| BMI | Body Mass Index |
| CRP | C-Reactive Protein |
| DM | Diabetes Mellitus |
| DPP4i | Dipeptidyl-Peptidase-4 inhibitors |
| ERK | Extracellular-signal-regulated Kinase |
| eNOS | Endothelial Nitric Oxide Synthase |
| ET-1 | Endothelin 1 |
| FOXO1 | Forkhead Box O1 |
| GABA | Gamma-Aminobutyric acid |
| GLP-1 RA | Glucagon-like Peptide-1 Receptor Agonists |
| GLUT-4 | Glucose Transporter 4 |
| hCRP | High-Sensitivity CRP |
| HMGB 1 | High Mobility Group Box chromosomal protein 1 |
| IRS | Insulin Receptor Substrate |
| ICAM1 | Intercellular Adhesion Molecule 1 |
| IL-1β | Interleukin-1Beta |
| IL-6 | Interleukin-6 |
| JNK | C-Jun N-terminal Kinase |
| KLF2 | Krüppel-Like Factor 2 |
| KLF4 | Krüppel-Like Factor 4 |
| mTOR | Mammalian Target of Rapamycin |
| MAPK | Mitogen-Activated Protein Kinase |
| MCP1 | Monocyte Chemoattractant Protein 1 |
| miRNAs | MicroRNAs |
| NADPH | Nicotinamide Adenine Dinucleotide Phosphate |
| NF-κB | Nuclear Factor-KappaB |
| NO | Nitric Oxide |
| NOX | NADPH Oxidase |
| Nrf2 | E2-related factor 2 |
| PDE-5i | Phosphodiesterase-5 inhibitors |
| PET-CT | Positron emission tomography—computed tomography |
| PI3K | Phosphatidylinositol 3 Kinase |
| PKC | Protein Kinase C |
| ROS | Reactive Oxygen Species |
| RAGE | Receptor for AGEs |
| SGLT2i | Sodium Glucose Cotransporter 2 inhibitors |
| SIRT1 | Sirtuin 1 |
| TXA2 | Thromboxane A2 |
| TNF-α | Tumour Necrosis Factor-A |
| VCAM1 | Vascular Cell Adhesion Molecule 1 |
| VEGF | Vascular Endothelial Growth Factor |
| VSMCs | Vascular Smooth Muscle Cells |
Author Contributions
Conceptualization, C.K.U., E.C., and N.U.; writing—original draft preparation, C.K.U.; writing—review and editing, C.K.U., E.C., and N.U.; visualization, C.K.U. and N.U.; supervision, E.C. All authors have read and agreed to the submitted version of the manuscript.
Funding
The authors gratefully acknowledge financial support from the Slovenian Research Agency (ARRS), Slovenia, through the research core funding No. P3-0043.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no known conflict of interest that could have appeared to influence the work reported in this paper.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Weir C.B., Jan A. BMI Classification Percentile and Cut Off Points. StatPearls Publishing; Treasure Island, FL, USA: 2021. [PubMed] [Google Scholar]
- 2.Obesity and Overweight. [(accessed on 9 December 2021)]. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 3.Abarca-Gómez L., Abdeen Z.A., Hamid Z.A., Abu-Rmeileh N.M., Acosta-Cazares B., Acuin C., Adams R.J., Aekplakorn W., Afsana K., Aguilar-Salinas C.A., et al. Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yanovski J.A. Obesity: Trends in Underweight and Obesity-Scale of the Problem. Nat. Rev. Endocrinol. 2018;14:5–6. doi: 10.1038/nrendo.2017.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sung H., Siegel R.L., Torre L.A., Pearson-Stuttard J., Islami F., Fedewa S.A., Goding Sauer A., Shuval K., Gapstur S.M., Jacobs E.J., et al. Global Patterns in Excess Body Weight and the Associated Cancer Burden. CA Cancer J. Clin. 2018 doi: 10.3322/caac.21499. [DOI] [PubMed] [Google Scholar]
- 6.GBD 2015 Obesity Collaborators. Afshin A., Forouzanfar M.H., Reitsma M.B., Sur P., Estep K., Lee A., Marczak L., Mokdad A.H., Moradi-Lakeh M., et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017;377:13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blüher M. Obesity: Global Epidemiology and Pathogenesis. Nat. Rev. Endocrinol. 2019;15:288–298. doi: 10.1038/s41574-019-0176-8. [DOI] [PubMed] [Google Scholar]
- 8.Schiaffino S. Muscle Fiber Type Diversity Revealed by Anti-Myosin Heavy Chain Antibodies. FEBS J. 2018;285:3688–3694. doi: 10.1111/febs.14502. [DOI] [PubMed] [Google Scholar]
- 9.Umek N., Horvat S., Cvetko E. Skeletal Muscle and Fiber Type-Specific Intramyocellular Lipid Accumulation in Obese Mice. Bosn. J. Basic Med. Sci. 2021;21 doi: 10.17305/bjbms.2021.5876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thiebaud D., Jacot E., DeFronzo R.A., Maeder E., Jequier E., Felber J.P. The Effect of Graded Doses of Insulin on Total Glucose Uptake, Glucose Oxidation, and Glucose Storage in Man. Diabetes. 1982;31:957–963. doi: 10.2337/diacare.31.11.957. [DOI] [PubMed] [Google Scholar]
- 11.Czech M.P. Insulin Action and Resistance in Obesity and Type 2 Diabetes. Nat. Med. 2017;23:804–814. doi: 10.1038/nm.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levy B.I., Schiffrin E.L., Mourad J.J., Agostini D., Vicaut E., Safar M.E., Struijker-Boudier H.A.J. Impaired Tissue Perfusion: A Pathology Common to Hypertension, Obesity, and Diabetes Mellitus. Circulation. 2008;118:968–976. doi: 10.1161/CIRCULATIONAHA.107.763730. [DOI] [PubMed] [Google Scholar]
- 13.Serné E.H., DeJongh R.T., Eringa E.C., Ijzerman R.G., DeBoer M.P., Stehouwer C.D.A. Microvascular Dysfunction: Causative Role in the Association between Hypertension, Insulin Resistance and the Metabolic Syndrome? Essays Biochem. 2006;42:163–176. doi: 10.1042/bse0420163. [DOI] [PubMed] [Google Scholar]
- 14.De Boer M.P., Meijer R.I., Wijnstok N.J., Jonk A.M., Houben A.J., Stehouwer C.D., Smulders Y.M., Eringa E.C., Serné E.H. Microvascular Dysfunction: A Potential Mechanism in the Pathogenesis of Obesity-Associated Insulin Resistance and Hypertension. Microcirculation. 2012;19:5–18. doi: 10.1111/j.1549-8719.2011.00130.x. [DOI] [PubMed] [Google Scholar]
- 15.Jonk A.M., Houben A.J.H.M., de Jongh R.T., Serné E.H., Schaper N.C., Stehouwer C.D.A. Microvascular Dysfunction in Obesity: A Potential Mechanism in the Pathogenesis of Obesity-Associated Insulin Resistance and Hypertension. Physiology. 2007;22:252–260. doi: 10.1152/physiol.00012.2007. [DOI] [PubMed] [Google Scholar]
- 16.Boillot A., Zoungas S., Mitchell P., Klein R., Klein B., Ikram M.K., Klaver C., Wang J.J., Gopinath B., Tai E.S., et al. Obesity and the Microvasculature: A Systematic Review and Meta-Analysis. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0052708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Virdis A., Masi S., Colucci R., Chiriacò M., Uliana M., Puxeddu I., Bernardini N., Blandizzi C., Taddei S. Microvascular Endothelial Dysfunction in Patients with Obesity. Curr. Hypertens. Rep. 2019;21:32. doi: 10.1007/s11906-019-0930-2. [DOI] [PubMed] [Google Scholar]
- 18.van der Heijden D.J., van Leeuwen M.A.H., Janssens G.N., Lenzen M.J., van de Ven P.M., Eringa E.C., van Royen N. Body Mass Index Is Associated With Microvascular Endothelial Dysfunction in Patients With Treated Metabolic Risk Factors and Suspected Coronary Artery Disease. J. Am. Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.006082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Villalobos-Labra R., Subiabre M., Toledo F., Pardo F., Sobrevia L. Endoplasmic Reticulum Stress and Development of Insulin Resistance in Adipose, Skeletal, Liver, and Foetoplacental Tissue in Diabesity. Mol. Asp. Med. 2019;66:49–61. doi: 10.1016/j.mam.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Muris D.M.J., Houben A.J.H.M., Schram M.T., Stehouwer C.D.A. Microvascular Dysfunction: An Emerging Pathway in the Pathogenesis of Obesity-Related Insulin Resistance. Rev. Endocr. Metab. Disord. 2013;14:29–38. doi: 10.1007/s11154-012-9231-7. [DOI] [PubMed] [Google Scholar]
- 21.Stehouwer C.D.A. Microvascular Dysfunction and Hyperglycemia: A Vicious Cycle with Widespread Consequences. Diabetes. 2018;67:1729–1741. doi: 10.2337/dbi17-0044. [DOI] [PubMed] [Google Scholar]
- 22.Horton W.B., Barrett E.J. Microvascular Dysfunction in Diabetes Mellitus and Cardiometabolic Disease. Endocr. Rev. 2021;42:29–55. doi: 10.1210/endrev/bnaa025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krentz A.J., Clough G., Byrne C.D. Interactions between Microvascular and Macrovascular Disease in Diabetes: Pathophysiology and Therapeutic Implications. Diabetes Obes. Metab. 2007;9:781–791. doi: 10.1111/j.1463-1326.2007.00670.x. [DOI] [PubMed] [Google Scholar]
- 24.De Jongh R.T., Serné E.H., Ijzerman R.G., de Vries G., Stehouwer C.D.A. Impaired Microvascular Function in Obesity: Implications for Obesity-Associated Microangiopathy, Hypertension, and Insulin Resistance. Circulation. 2004;109:2529–2535. doi: 10.1161/01.CIR.0000129772.26647.6F. [DOI] [PubMed] [Google Scholar]
- 25.Karaca Ü., Schram M.T., Houben A.J.H.M., Muris D.M.J., Stehouwer C.D.A. Microvascular Dysfunction as a Link between Obesity, Insulin Resistance and Hypertension. Diabetes Res. Clin. Pract. 2014;103:382–387. doi: 10.1016/j.diabres.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 26.Casanova F., Adingupu D.D., Adams F., Gooding K.M., Looker H.C., Aizawa K., Dove F., Elyas S., Belch J.J.F., Gates P.E., et al. The Impact of Cardiovascular Co-Morbidities and Duration of Diabetes on the Association between Microvascular Function and Glycaemic Control. Cardiovasc. Diabetol. 2017;16 doi: 10.1186/s12933-017-0594-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levy B.I., Ambrosio G., Pries A.R., Struijker-Boudier H.A.J. Microcirculation in Hypertension: A New Target for Treatment? Circulation. 2001;104:735–740. doi: 10.1161/hc3101.091158. [DOI] [PubMed] [Google Scholar]
- 28.Latroche C., Gitiaux C., Chrétien F., Desguerre I., Mounie R., Chazaud B. Skeletal Muscle Microvasculature: A Highly Dynamic Lifeline. Physiology. 2015;30:417–427. doi: 10.1152/physiol.00026.2015. [DOI] [PubMed] [Google Scholar]
- 29.Ding Y., Zhou Y., Ling P., Feng X., Luo S., Zheng X., Little P.J., Xu S., Weng J. Metformin in Cardiovascular Diabetology: A Focused Review of Its Impact on Endothelial Function. Theranostics. 2021;11:9376–9396. doi: 10.7150/thno.64706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vanhoutte P.M., Shimokawa H., Feletou M., Tang E.H.C. Endothelial Dysfunction and Vascular Disease-a 30th Anniversary Update. Acta Physiol. (Oxf. Engl.) 2017;219:22–96. doi: 10.1111/apha.12646. [DOI] [PubMed] [Google Scholar]
- 31.Tejero J., Shiva S., Gladwin M.T. Sources of Vascular Nitric Oxide and Reactive Oxygen Species and Their Regulation. Physiol. Rev. 2019;99:311–379. doi: 10.1152/physrev.00036.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeng G., Nystrom F.H., Ravichandran L.V., Cong L.N., Kirby M., Mostowski H., Quon M.J. Roles for Insulin Receptor, PI3-Kinase, and Akt in Insulin-Signaling Pathways Related to Production of Nitric Oxide in Human Vascular Endothelial Cells. Circulation. 2000;101:1539–1545. doi: 10.1161/01.CIR.101.13.1539. [DOI] [PubMed] [Google Scholar]
- 33.Zaborska K.E., Wareing M., Austin C. Comparisons between Perivascular Adipose Tissue and the Endothelium in Their Modulation of Vascular Tone. Br. J. Pharmacol. 2017;174:3388–3397. doi: 10.1111/bph.13648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Daiber A., Steven S., Weber A., Shuvaev V.V., Muzykantov V.R., Laher I., Li H., Lamas S., Münzel T. Targeting Vascular (Endothelial) Dysfunction. Br. J. Pharmacol. 2017;174:1591–1619. doi: 10.1111/bph.13517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Janus A., Szahidewicz-Krupska E., Mazur G., Doroszko A. Insulin Resistance and Endothelial Dysfunction Constitute a Common Therapeutic Target in Cardiometabolic Disorders. Mediat. Inflamm. 2016;2016 doi: 10.1155/2016/3634948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chadderdon S.M., Belcik J.T., Bader L., Kievit P., Grove K.L., Lindner J.R. Vasoconstrictor Eicosanoids and Impaired Microvascular Function in Inactive and Insulin-Resistant Primates. Int. J. Obes. 2016;40:1600–1603. doi: 10.1038/ijo.2016.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Samuel V.T., Shulman G.I. The Pathogenesis of Insulin Resistance: Integrating Signaling Pathways and Substrate Flux. J. Clin. Investig. 2016;126:12–22. doi: 10.1172/JCI77812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barrett E.J., Liu Z., Khamaisi M., King G.L., Klein R., Klein B.E.K., Hughes T.M., Craft S., Freedman B.I., Bowden D.W., et al. Diabetic Microvascular Disease: An Endocrine Society Scientific Statement. J. Clin. Endocrinol. Metab. 2017;102:4343–4410. doi: 10.1210/jc.2017-01922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams I.M., Valenzuela F.A., Kahl S.D., Ramkrishna D., Mezo A.R., Young J.D., Sam Wells K., Wasserman D.H. Insulin Exits Skeletal Muscle Capillaries by Fluid-Phase Transport. J. Clin. Investig. 2018;128:699–714. doi: 10.1172/JCI94053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baron A.D. Cardiovascular Actions of Insulin in Humans. Implications for Insulin Sensitivity and Vascular Tone. Bailliere’s Clin. Endocrinol. Metab. 1993;7:961–987. doi: 10.1016/S0950-351X(05)80241-1. [DOI] [PubMed] [Google Scholar]
- 41.Baron A.D., Steinberg H., Brechtel G., Johnson A. Skeletal Muscle Blood Flow Independently Modulates Insulin-Mediated Glucose Uptake. Am. J. Physiol. 1994;266 doi: 10.1152/ajpendo.1994.266.2.E248. [DOI] [PubMed] [Google Scholar]
- 42.Laakso M., Edelman S.V., Brechtel G., Baron A.D. Decreased Effect of Insulin to Stimulate Skeletal Muscle Blood Flow in Obese Man. A Novel Mechanism for Insulin Resistance. J. Clin. Investig. 1990;85:1844–1852. doi: 10.1172/JCI114644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clark A.D.H., Barrett E.J., Rattigan S., Wallis M.G., Clark M.G. Insulin Stimulates Laser Doppler Signal by Rat Muscle in Vivo, Consistent with Nutritive Flow Recruitment. Clin. Sci. 2001;100:283–290. doi: 10.1042/CS20000104. [DOI] [PubMed] [Google Scholar]
- 44.Zhang L., Vincent M.A., Richards S.M., Clerk L.H., Rattigan S., Clark M.G., Barrett E.J. Insulin Sensitivity of Muscle Capillary Recruitment in vivo. Diabetes. 2004;53:447–453. doi: 10.2337/diabetes.53.2.447. [DOI] [PubMed] [Google Scholar]
- 45.Vincent M.A., Clerk L.H., Lindner J.R., Klibanov A.L., Clark M.G., Rattigan S., Barrett E.J. Microvascular Recruitment Is an Early Insulin Effect That Regulates Skeletal Muscle Glucose Uptake in vivo. Diabetes. 2004;53:1418–1423. doi: 10.2337/diabetes.53.6.1418. [DOI] [PubMed] [Google Scholar]
- 46.Shulman G.I. Cellular Mechanisms of Insulin Resistance. J. Clin. Investig. 2000;106:171–176. doi: 10.1172/JCI10583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wasserman D.H., Wang T.J., Brown N.J. The Vasculature in Prediabetes. Circ. Res. 2018;122:1135–1150. doi: 10.1161/CIRCRESAHA.118.311912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jiang Z.Y., Lin Y.W., Clemont A., Feener E.P., Hein K.D., Igarashi M., Yamauchi T., White M.F., King G.L. Characterization of Selective Resistance to Insulin Signaling in the Vasculature of Obese Zucker (Fa/Fa) Rats. J. Clin. Investig. 1999;104:447–457. doi: 10.1172/JCI5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martens R.J.H., Henry R.M.A., Houben A.J.H.M., van der Kallen C.J.H., Kroon A.A., Schalkwijk C.G., Schram M.T., Sep S.J.S., Schaper N.C., Dagnelie P.C., et al. Capillary Rarefaction Associates with Albuminuria: The Maastricht Study. J. Am. Soc. Nephrol. 2016;27:3748–3757. doi: 10.1681/ASN.2015111219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Martens R.J.H., Houben A.J.H.M., Kooman J.P., Berendschot T.T.J.M., Dagnelie P.C., van der Kallen C.J.H., Kroon A.A., Leunissen K.M.L., van der Sande F.M., Schaper N.C., et al. Microvascular Endothelial Dysfunction Is Associated with Albuminuria: The Maastricht Study. J. Hypertens. 2018;36:1178–1187. doi: 10.1097/HJH.0000000000001674. [DOI] [PubMed] [Google Scholar]
- 51.Williams I.M., McClatchey P.M., Bracy D.P., Bonner J.S., Valenzuela F.A., Wasserman D.H. Transendothelial Insulin Transport Is Impaired in Skeletal Muscle Capillaries of Obese Male Mice. Obesity. 2020;28:303–314. doi: 10.1002/oby.22683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krogh A. The Number and Distribution of Capillaries in Muscles with Calculations of the Oxygen Pressure Head Necessary for Supplying the Tissue. J. Physiol. 1919;52:409–415. doi: 10.1113/jphysiol.1919.sp001839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hepple R.T., Mathieu-Costello O. Estimating the Size of the Capillary-to-Fiber Interface in Skeletal Muscle: A Comparison of Methods. J. Appl. Physiol. 2001;91:2150–2156. doi: 10.1152/jappl.2001.91.5.2150. [DOI] [PubMed] [Google Scholar]
- 54.Eržen I., Janáček J., Kreft M., Kubínová L., Cvetko E. Capillary Network Morphometry of Pig Soleus Muscle Significantly Changes in 24 Hours After Death. J. Histochem. Cytochem. 2018;66:23–31. doi: 10.1369/0022155417737061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schaad L., Hlushchuk R., Barré S., Gianni-Barrera R., Haberthür D., Banfi A., Djonov V. Correlative Imaging of the Murine Hind Limb Vasculature and Muscle Tissue by MicroCT and Light Microscopy. Sci. Rep. 2017;7 doi: 10.1038/srep41842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Umek N., Horvat S., Cvetko E., Kreft M., Janáček J., Kubínová L., Stopar Pintarič T., Eržen I. 3D Analysis of Capillary Network in Skeletal Muscle of Obese Insulin-Resistant Mice. Histochem. Cell Biol. 2019;152:323–331. doi: 10.1007/s00418-019-01810-7. [DOI] [PubMed] [Google Scholar]
- 57.Dresner A., Laurent D., Marcucci M., Griffin M.E., Dufour S., Cline G.W., Slezak L.A., Andersen D.K., Hundal R.S., Rothman D.L., et al. Effects of Free Fatty Acids on Glucose Transport and IRS-1-Associated Phosphatidylinositol 3-Kinase Activity. J. Clin. Investig. 1999;103:253–259. doi: 10.1172/JCI5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xing L.W., Zhang L., Youker K., Zhang M.X., Wang J., LeMaire S.A., Coselli J.S., Shen Y.H. Free Fatty Acids Inhibit Insulin Signaling-Stimulated Endothelial Nitric Oxide Synthase Activation through Upregulating PTEN or Inhibiting Akt Kinase. Diabetes. 2006;55:2301–2310. doi: 10.2337/DB05-1574. [DOI] [PubMed] [Google Scholar]
- 59.García-Prieto C.F., Hernández-Nuño F., del Rio D., Ruiz-Hurtado G., Aránguez I., Ruiz-Gayo M., Somoza B., Fernández-Alfonso M.S. High-Fat Diet Induces Endothelial Dysfunction through a down-Regulation of the Endothelial AMPK-PI3K-Akt-ENOS Pathway. Mol. Nutr. Food Res. 2015;59:520–532. doi: 10.1002/mnfr.201400539. [DOI] [PubMed] [Google Scholar]
- 60.Sorop O., Olver T.D., van DeWouw J., Heinonen I., van Duin R.W., Duncker D.J., Merkus D. The Microcirculation: A Key Player in Obesity-Associated Cardiovascular Disease. Cardiovasc. Res. 2017;113:1035–1045. doi: 10.1093/cvr/cvx093. [DOI] [PubMed] [Google Scholar]
- 61.Meijer R.I., Serné E.H., Korkmaz H.I., van der Peet D.L., de Boer M.P., Niessen H.W.M., van Hinsbergh V.W.M., Yudkin J.S., Smulders Y.M., Eringa E.C. Insulin-Induced Changes in Skeletal Muscle Microvascular Perfusion Are Dependent upon Perivascular Adipose Tissue in Women. Diabetologia. 2015;58:1907–1915. doi: 10.1007/s00125-015-3606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Inoguchi T., Li P., Umeda F., Yu H.Y., Kakimoto M., Imamura M., Aoki T., Etoh T., Hashimoto T., Naruse M., et al. High Glucose Level and Free Fatty Acid Stimulate Reactive Oxygen Species Production through Protein Kinase C--Dependent Activation of NAD(P)H Oxidase in Cultured Vascular Cells. Diabetes. 2000;49:1939–1945. doi: 10.2337/diabetes.49.11.1939. [DOI] [PubMed] [Google Scholar]
- 63.Savage D.B., Watson L., Carr K., Adams C., Brage S., Chatterjee K.K., Hodson L., Boesch C., Kemp G.J., Sleigh A. Accumulation of Saturated Intramyocellular Lipid Is Associated with Insulin Resistance. J. Lipid Res. 2019;60:1323–1332. doi: 10.1194/jlr.M091942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Limberg J.K., Johansson R.E., Carter K.J., Peltonen G., Harrell J.W., Kellawan J.M., Eldridge M.W., Sebranek J.J., Walker B.J., Schrage W.G. Preserved β-Adrenergic Mediated Vasodilation in Skeletal Muscle of Young Obese Adults despite Shifts in Cyclooxygenase and Nitric Oxide Synthase. Am. J. Physiol. Heart Circ. Physiol. 2021 doi: 10.1152/AJPHEART.00449.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Limberg J.K., Morgan B.J., Schrage W.G. Peripheral Blood Flow Regulation in Human Obesity and Metabolic Syndrome. Exerc. Sport Sci. Rev. 2016;44:116–122. doi: 10.1249/JES.0000000000000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Limberg J.K., de Vita M.D., Blain G.M., Schrage W.G. Muscle Blood Flow Responses to Dynamic Exercise in Young Obese Humans. J. Appl. Physiol. 2010;108:349–355. doi: 10.1152/japplphysiol.00551.2009. [DOI] [PubMed] [Google Scholar]
- 67.Bender S.B., de Beer V.J., Tharp D.L., van Deel E.D., Bowles D.K., Duncker D.J., Laughlin M.H., Merkus D. Reduced Contribution of Endothelin to the Regulation of Systemic and Pulmonary Vascular Tone in Severe Familial Hypercholesterolaemia. J. Physiol. 2014;592:1757–1769. doi: 10.1113/jphysiol.2013.267351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Karpoff L., Vinet A., Schuster I., Oudot C., Goret L., Dauzat M., Obert P., Perez-Martin A. Abnormal Vascular Reactivity at Rest and Exercise in Obese Boys. Eur. J. Clin. Investig. 2009;39:94–102. doi: 10.1111/j.1365-2362.2008.02068.x. [DOI] [PubMed] [Google Scholar]
- 69.Vinet A., Karpoff L., Walther G., Startun A., Obert P., Goret L., Dauzat M., Perez-Martin A. Vascular Reactivity at Rest and during Exercise in Middle-Aged Obese Men: Effects of Short-Term, Low-Intensity, Exercise Training. Int. J. Obes. 2011;35:820–828. doi: 10.1038/ijo.2010.206. [DOI] [PubMed] [Google Scholar]
- 70.Agapitov A.V., Correia M.L.G., Sinkey C.A., Dopp J.M., Haynes W.G. Impaired Skeletal Muscle and Skin Microcirculatory Function in Human Obesity. J. Hypertens. 2002;20:1401–1405. doi: 10.1097/00004872-200207000-00027. [DOI] [PubMed] [Google Scholar]
- 71.Frisbee J.C., Goodwill A.G., Frisbee S.J., Butcher J.T., Brock R.W., Olfert I.M., DeVallance E.R., Chantler P.D. Distinct Temporal Phases of Microvascular Rarefaction in Skeletal Muscle of Obese Zucker Rats. Am. J. Physiol. Heart Circ. Physiol. 2014;307:H1714–H1728. doi: 10.1152/ajpheart.00605.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sjöstrand M., Gudbjörnsdottir S., Holmäng A., Lönn L., Strindberg L., Lönnroth P. Delayed Transcapillary Transport of Insulin to Muscle Interstitial Fluid in Obese Subjects. Diabetes. 2002;51:2742–2748. doi: 10.2337/diabetes.51.9.2742. [DOI] [PubMed] [Google Scholar]
- 73.Kubota T., Kubota N., Kumagai H., Yamaguchi S., Kozono H., Takahashi T., Inoue M., Itoh S., Takamoto I., Sasako T., et al. Impaired Insulin Signaling in Endothelial Cells Reduces Insulin-Induced Glucose Uptake by Skeletal Muscle. Cell Metab. 2011;13:294–307. doi: 10.1016/j.cmet.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 74.Ayala J.E., Bracy D.P., Julien B.M., Rottman J.N., Fueger P.T., Wasserman D.H. Chronic Treatment with Sildenafil Improves Energy Balance and Insulin Action in High Fat-Fed Conscious Mice. Diabetes. 2007;56:1025–1033. doi: 10.2337/db06-0883. [DOI] [PubMed] [Google Scholar]
- 75.Schäfer A., Fraccarollo D., Pförtsch S., Flierl U., Vogt C., Pfrang J., Kobsar A., Renné T., Eigenthaler M., Ertl G., et al. Improvement of Vascular Function by Acute and Chronic Treatment with the PDE-5 Inhibitor Sildenafil in Experimental Diabetes Mellitus. Br. J. Pharmacol. 2008;153:886–893. doi: 10.1038/sj.bjp.0707459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chadderdon S.M., Belcik J.T., Bader L., Peters D.M., Kievit P., Alkayed N.J., Kaul S., Grove K.L., Lindner J.R. Temporal Changes in Skeletal Muscle Capillary Responses and Endothelial-Derived Vasodilators in Obesity-Related Insulin Resistance. Diabetes. 2016;65:2249–2257. doi: 10.2337/db15-1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lemaster K.A., Farid Z., Brock R.W., Shrader C.D., Goldman D., Jackson D.N., Frisbee J.C. Altered Post-Capillary and Collecting Venular Reactivity in Skeletal Muscle with Metabolic Syndrome. J. Physiol. 2017;595:5159–5174. doi: 10.1113/JP274291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bonner J.S., Lantier L., Hasenour C.M., James F.D., Bracy D.P., Wasserman D.H. Muscle-Specific Vascular Endothelial Growth Factor Deletion Induces Muscle Capillary Rarefaction Creating Muscle Insulin Resistance. Diabetes. 2013;62:572–580. doi: 10.2337/db12-0354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Messa G.A.M., Piasecki M., Hurst J., Hill C., Tallis J., Degens H. The Impact of a High-Fat Diet in Mice Is Dependent on Duration and Age, and Differs between Muscles. J. Exp. Biol. 2020;223 doi: 10.1242/jeb.217117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Eriksson K.F., Saltin B., Lindgarde F. Increased Skeletal Muscle Capillary Density Precedes Diabetes Development in Men with Impaired Glucose Tolerance. A 15-Year Follow-Up. Diabetes. 1994;43:805–808. doi: 10.2337/diab.43.6.805. [DOI] [PubMed] [Google Scholar]
- 81.O’Reilly J., Ono-Moore K.D., Chintapalli S.V., Rutkowsky J.M., Tolentino T., Lloyd K.C.K., Olfert I.M., Adams S.H. Sex Differences in Skeletal Muscle Revealed through Fiber Type, Capillarity, and Transcriptomics Profiling in Mice. Physiol. Rep. 2021;9 doi: 10.14814/phy2.15031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huxley V.H., Kemp S.S. Sex-Specific Characteristics of the Microcirculation. Adv. Exp. Med. Biol. 2018;1065:307–328. doi: 10.1007/978-3-319-77932-4_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sidsworth D.A., Sellers S.L., Reutens-Hernandez J.P., Dunn E.A., Gray S.L., Payne G.W. Impact of Sex on Microvascular Reactivity in a Murine Model of Diet-Induced Obesity and Insulin Resistance. Heliyon. 2021;7 doi: 10.1016/j.heliyon.2021.e06217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.de Vriese A.S., Verbeuren T.J., van de Voorde J., Lameire N.H., Vanhoutte P.M. Endothelial Dysfunction in Diabetes. Br. J. Pharmacol. 2000;130:963–974. doi: 10.1038/sj.bjp.0703393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Scioli M.G., Storti G., D’Amico F., Rodríguez Guzmán R., Centofanti F., Doldo E., Céspedes Miranda E.M., Orlandi A. Oxidative Stress and New Pathogenetic Mechanisms in Endothelial Dysfunction: Potential Diagnostic Biomarkers and Therapeutic Targets. J. Clin. Med. 2020;9:1995. doi: 10.3390/jcm9061995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kaur R., Kaur M., Singh J. Endothelial Dysfunction and Platelet Hyperactivity in Type 2 Diabetes Mellitus: Molecular Insights and Therapeutic Strategies. Cardiovasc. Diabetol. 2018;17 doi: 10.1186/s12933-018-0763-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dhananjayan R., Koundinya K.S.S., Malati T., Kutala V.K. Endothelial Dysfunction in Type 2 Diabetes Mellitus. Indian J. Clin. Biochem. IJCB. 2016;31:372–379. doi: 10.1007/s12291-015-0516-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dimmeler S., Fleming I., Fisslthaler B., Hermann C., Busse R., Zeiher A.M. Activation of Nitric Oxide Synthase in Endothelial Cells by Akt-Dependent Phosphorylation. Nature. 1999;399:601–605. doi: 10.1038/21224. [DOI] [PubMed] [Google Scholar]
- 89.Ke B., Shen W., Fang X., Wu Q. The NLPR3 Inflammasome and Obesity-Related Kidney Disease. J. Cell. Mol. Med. 2018;22:16–24. doi: 10.1111/jcmm.13333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chen Y., Wang L., Pitzer A.L., Li X., Li P.L., Zhang Y. Contribution of Redox-Dependent Activation of Endothelial Nlrp3 Inflammasomes to Hyperglycemia-Induced Endothelial Dysfunction. J. Mol. Med. 2016;94:1335–1347. doi: 10.1007/s00109-016-1481-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang L., Chen Y., Li X., Zhang Y., Gulbins E., Zhang Y. Enhancement of Endothelial Permeability by Free Fatty Acid through Lysosomal Cathepsin B-Mediated Nlrp3 Inflammasome Activation. Oncotarget. 2016;7:73229–73241. doi: 10.18632/oncotarget.12302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Las G., Serada S.B., Wikstrom J.D., Twig G., Shirihai O.S. Fatty Acids Suppress Autophagic Turnover in β-Cells. J. Biol. Chem. 2011;286:42534. doi: 10.1074/jbc.M111.242412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mameli E., Martello A., Caporali A. Autophagy at the Interface of Endothelial Cell Homeostasis and Vascular Disease. FEBS J. 2021 doi: 10.1111/febs.15873. [DOI] [PubMed] [Google Scholar]
- 94.Tsushima Y., Nishizawa H., Tochino Y., Nakatsuji H., Sekimoto R., Nagao H., Shirakura T., Kato K., Imaizumi K., Takahashi H., et al. Uric Acid Secretion from Adipose Tissue and Its Increase in Obesity. J. Biol. Chem. 2013;288:27138–27149. doi: 10.1074/jbc.M113.485094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Niu Y., Tang Q., Zhao X., Zhao X., Mao X., Sheng J., Cai W., Feng Y. Obesity-Induced Insulin Resistance Is Mediated by High Uric Acid in Obese Children and Adolescents. Front. Endocrinol. 2021;12:773820. doi: 10.3389/fendo.2021.773820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Liu F., Chen S., Zhao W., Chen M., Ke J., Zhang Z., Lu J., Li L. Urine Uric Acid Excretion Levels Are Positively Associated with Obesity and Abdominal Obesity in Type 2 Diabetes Patients without Chronic Kidney Disease. Diabetes Metab. Syndr. Obes. Targets Ther. 2021;14:4691–4703. doi: 10.2147/DMSO.S335558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cai W., Duan X.M., Liu Y., Yu J., Tang Y.L., Liu Z.L., Jiang S., Zhang C.P., Liu J.Y., Xu J.X. Uric Acid Induces Endothelial Dysfunction by Activating the HMGB1/RAGE Signaling Pathway. BioMed Res. Int. 2017;2017:4391920. doi: 10.1155/2017/4391920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Johnson F.K., Peyton K.J., Liu X.M., Azam M.A., Shebib A.R., Johnson R.A., Durante W. Arginase Promotes Endothelial Dysfunction and Hypertension in Obese Rats. Obesity. 2015;23:383–390. doi: 10.1002/oby.20969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chung J.H., Moon J., Lee Y.S., Chung H.K., Lee S.M., Shin M.J. Arginase Inhibition Restores Endothelial Function in Diet-Induced Obesity. Biochem. Biophys. Res. Commun. 2014;451:179–183. doi: 10.1016/j.bbrc.2014.07.083. [DOI] [PubMed] [Google Scholar]
- 100.Xia N., Horke S., Habermeier A., Closs E.I., Reifenberg G., Gericke A., Mikhed Y., Münzel T., Daiber A., Förstermann U., et al. Uncoupling of Endothelial Nitric Oxide Synthase in Perivascular Adipose Tissue of Diet-Induced Obese Mice. Arterioscler. Thromb. Vasc. Biol. 2016;36:78–85. doi: 10.1161/ATVBAHA.115.306263. [DOI] [PubMed] [Google Scholar]
- 101.Bhatta A., Yao L., Xu Z., Toque H.A., Chen J., Atawia R.T., Fouda A.Y., Bagi Z., Lucas R., Caldwell R.B., et al. Obesity-Induced Vascular Dysfunction and Arterial Stiffening Requires Endothelial Cell Arginase 1. Cardiovasc. Res. 2017;113:1664–1676. doi: 10.1093/cvr/cvx164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.el Assar M., Angulo J., Santos-Ruiz M., Ruiz de Adana J.C., Pindado M.L., Sánchez-Ferrer A., Hernández A., Rodríguez-Mañas L. Asymmetric Dimethylarginine (ADMA) Elevation and Arginase up-Regulation Contribute to Endothelial Dysfunction Related to Insulin Resistance in Rats and Morbidly Obese Humans. J. Physiol. 2016;594:3045–3060. doi: 10.1113/JP271836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Masi S., Colucci R., Duranti E., Nannipieri M., Anselmino M., Ippolito C., Tirotta E., Georgiopoulos G., Garelli F., Nericcio A., et al. Aging Modulates the Influence of Arginase on Endothelial Dysfunction in Obesity. Arterioscler. Thromb. Vasc. Biol. 2018;38:2474–2483. doi: 10.1161/ATVBAHA.118.311074. [DOI] [PubMed] [Google Scholar]
- 104.Taniyama Y., Hitomi H., Shah A., Alexander R.W., Griendling K.K. Mechanisms of Reactive Oxygen Species-Dependent Downregulation of Insulin Receptor Substrate-1 by Angiotensin II. Arterioscler. Thromb. Vasc. Biol. 2005;25:1142–1147. doi: 10.1161/01.ATV.0000164313.17167.df. [DOI] [PubMed] [Google Scholar]
- 105.Hitomi H., Kiyomoto H., Nishiyama A., Hara T., Moriwaki K., Kaifu K., Ihara G., Fujita Y., Ugawa T., Kohno M. Aldosterone Suppresses Insulin Signaling via the Downregulation of Insulin Receptor Substrate-1 in Vascular Smooth Muscle Cells. Hypertension. 2007;50:750–755. doi: 10.1161/HYPERTENSIONAHA.107.093955. [DOI] [PubMed] [Google Scholar]
- 106.Mazak I., Fiebeler A., Muller D.N., Park J.K., Shagdarsuren E., Lindschau C., Dechend R., Viedt C., Pilz B., Haller H., et al. Aldosterone Potentiates Angiotensin II-Induced Signaling in Vascular Smooth Muscle Cells. Circulation. 2004;109:2792–2800. doi: 10.1161/01.CIR.0000131860.80444.AB. [DOI] [PubMed] [Google Scholar]
- 107.Sherajee S.J., Fujita Y., Rafiq K., Nakano D., Mori H., Masaki T., Hara T., Kohno M., Nishiyama A., Hitomi H. Aldosterone Induces Vascular Insulin Resistance by Increasing Insulin-like Growth Factor-1 Receptor and Hybrid Receptor. Arterioscler. Thromb. Vasc. Biol. 2012;32:257–263. doi: 10.1161/ATVBAHA.111.240697. [DOI] [PubMed] [Google Scholar]
- 108.Jia G., DeMarco V.G., Sowers J.R. Insulin Resistance and Hyperinsulinaemia in Diabetic Cardiomyopathy. Nat. Rev. Endocrinol. 2016;12:144–153. doi: 10.1038/nrendo.2015.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ait-Aissa K., Nguyen Q.M., Gabani M., Kassan A., Kumar S., Choi S.K., Gonzalez A.A., Khataei T., Sahyoun A.M., Chen C., et al. MicroRNAs and Obesity-Induced Endothelial Dysfunction: Key Paradigms in Molecular Therapy. Cardiovasc. Diabetol. 2020;19 doi: 10.1186/s12933-020-01107-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Caporali A., Meloni M., Völlenkle C., Bonci D., Sala-Newby G.B., Addis R., Spinetti G., Losa S., Masson R., Baker A.H., et al. Deregulation of MicroRNA-503 Contributes to Diabetes Mellitus-Induced Impairment of Endothelial Function and Reparative Angiogenesis after Limb Ischemia. Circulation. 2011;123:282–291. doi: 10.1161/CIRCULATIONAHA.110.952325. [DOI] [PubMed] [Google Scholar]
- 111.Murphy K., O’Donovan A.N., Caplice N.M., Ross R.P., Stanton C. Exploring the Gut Microbiota and Cardiovascular Disease. Metabolites. 2021;11:493. doi: 10.3390/metabo11080493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang B., Wang X., Xia R., Li C. Gut Microbiota in Coronary Artery Disease: A Friend or Foe? Biosci. Rep. 2020;40 doi: 10.1042/BSR20200454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Malik M., Suboc T.M., Tyagi S., Salzman N., Wang J., Ying R., Tanner M.J., Kakarla M., Baker J.E., Widlansky M.E. Lactobacillus Plantarum 299v Supplementation Improves Vascular Endothelial Function and Reduces Inflammatory Biomarkers in Men with Stable Coronary Artery Disease. Circ. Res. 2018;123:1091–1102. doi: 10.1161/CIRCRESAHA.118.313565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rovella V., Rodia G., di Daniele F., Cardillo C., Campia U., Noce A., Candi E., Della-Morte D., Tesauro M. Association of Gut Hormones and Microbiota with Vascular Dysfunction in Obesity. Nutrients. 2021;13:613. doi: 10.3390/nu13020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Vikram A., Kim Y.R., Kumar S., Li Q., Kassan M., Jacobs J.S., Irani K. Vascular MicroRNA-204 Is Remotely Governed by the Microbiome and Impairs Endothelium-Dependent Vasorelaxation by Downregulating Sirtuin1. Nat. Commun. 2016;7 doi: 10.1038/ncomms12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Nirmalkar K., Murugesan S., Pizano-Zárate M.L., Villalobos-Flores L.E., García-González C., Morales-Hernández R.M., Nuñez-Hernández J.A., Hernández-Quiroz F., Romero-Figueroa M.D.S., Hernández-Guerrero C., et al. Gut Microbiota and Endothelial Dysfunction Markers in Obese Mexican Children and Adolescents. Nutrients. 2018;10:2009. doi: 10.3390/nu10122009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Johnson S., Litwin N., van Ark H., Hartley S., Fischer E., Michell K., Vazquez A., Lee D., Trikha S.R., Wrigley S., et al. The Gut Microbiota Is Associated with Vascular Function and Blood Pressure Phenotypes in Overweight and Obese Middle-Aged/Older Adults (P21-024-19) Curr. Dev. Nutr. 2019;3 doi: 10.1093/cdn/nzz041.P21-024-19. [DOI] [Google Scholar]
- 118.King R.J., Ajjan R.A. Vascular Risk in Obesity: Facts, Misconceptions and the Unknown. Diabetes Vasc. Dis. Res. 2017;14:2–13. doi: 10.1177/1479164116675488. [DOI] [PubMed] [Google Scholar]
- 119.Eringa E.C., Stehouwer C.D.A., Walburg K., Clark A.D., van Nieuw Amerongen G.P., Westerhof N., Sipkema P. Physiological Concentrations of Insulin Induce Endothelin-Dependent Vasoconstriction of Skeletal Muscle Resistance Arteries in the Presence of Tumor Necrosis Factor-Alpha Dependence on c-Jun N-Terminal Kinase. Arterioscler. Thromb. Vasc. Biol. 2006;26:274–280. doi: 10.1161/01.ATV.0000198248.19391.3e. [DOI] [PubMed] [Google Scholar]
- 120.Zheng Q., Yuan Y., Yi W., Lau W.B., Wang Y., Wang X., Sun Y., Lopez B.L., Christopher T.A., Peterson J.M., et al. C1q/TNF-Related Proteins, a Family of Novel Adipokines, Induce Vascular Relaxation through the Adiponectin Receptor-1/AMPK/ENOS/Nitric Oxide Signaling Pathway. Arterioscler. Thromb. Vasc. Biol. 2011;31:2616–2623. doi: 10.1161/ATVBAHA.111.231050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Houben A.J., Eringa E.C., Jonk A.M., Serne E.H., Smulders Y.M., Stehouwer C.D. Perivascular Fat and the Microcirculation: Relevance to Insulin Resistance, Diabetes, and Cardiovascular Disease. Curr. Cardiovasc. Risk Rep. 2012;6:80–90. doi: 10.1007/s12170-011-0214-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sena C.M., Pereira A., Fernandes R., Letra L., Seiça R.M. Adiponectin Improves Endothelial Function in Mesenteric Arteries of Rats Fed a High-Fat Diet: Role of Perivascular Adipose Tissue. Br. J. Pharmacol. 2017;174:3514–3526. doi: 10.1111/bph.13756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Serné E.H., de Jongh R.T., Eringa E.C., IJzerman R.G., Stehouwer C.D.A. Microvascular Dysfunction. Hypertension. 2007;50:204–211. doi: 10.1161/HYPERTENSIONAHA.107.089680. [DOI] [PubMed] [Google Scholar]
- 124.Virdis A., Colucci R., Bernardini N., Blandizzi C., Taddei S., Masi S. Microvascular Endothelial Dysfunction in Human Obesity: Role of TNF-α. J. Clin. Endocrinol. Metab. 2019;104:341–348. doi: 10.1210/jc.2018-00512. [DOI] [PubMed] [Google Scholar]
- 125.Schinzari F., Tesauro M., Cardillo C. Endothelial and Perivascular Adipose Tissue Abnormalities in Obesity-Related Vascular Dysfunction: Novel Targets for Treatment. J. Cardiovasc. Pharmacol. 2017;69:360–368. doi: 10.1097/FJC.0000000000000469. [DOI] [PubMed] [Google Scholar]
- 126.Murphy M.P. How Mitochondria Produce Reactive Oxygen Species. Biochem. J. 2009;417:1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Thiruvengadam M., Venkidasamy B., Subramanian U., Samynathan R., Ali Shariati M., Rebezov M., Girish S., Thangavel S., Dhanapal A.R., Fedoseeva N., et al. Bioactive Compounds in Oxidative Stress-Mediated Diseases: Targeting the NRF2/ARE Signaling Pathway and Epigenetic Regulation. Antioxidants. 2021;10:1859. doi: 10.3390/antiox10121859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ramprasath T., Freddy A.J., Velmurugan G., Tomar D., Rekha B., Suvekbala V., Ramasamy S. Context-Dependent Regulation of Nrf2/ARE Axis on Vascular Cell Function during Hyperglycemic Condition. Curr. Diabetes Rev. 2020;16:797–806. doi: 10.2174/1573399816666200130094512. [DOI] [PubMed] [Google Scholar]
- 129.Lennicke C., Cochemé H.M. Redox Regulation of the Insulin Signalling Pathway. Redox Biol. 2021;42 doi: 10.1016/j.redox.2021.101964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Creager M.A., Lüscher T.F., Cosentino F., Beckman J.A. Diabetes and Vascular Disease: Pathophysiology, Clinical Consequences, and Medical Therapy: Part I. Circulation. 2003;108:1527–1532. doi: 10.1161/01.CIR.0000091257.27563.32. [DOI] [PubMed] [Google Scholar]
- 131.Inoguchi T., Sonta T., Tsubouchi H., Etoh T., Kakimoto M., Sonoda N., Sato N., Sekiguchi N., Kobayashi K., Sumimoto H., et al. Protein Kinase C-Dependent Increase in Reactive Oxygen Species (ROS) Production in Vascular Tissues of Diabetes: Role of Vascular NAD(P)H Oxidase. J. Am. Soc. Nephrol. 2003;14 doi: 10.1097/01.ASN.0000077407.90309.65. [DOI] [PubMed] [Google Scholar]
- 132.Ferreira L.F., Laitano O. Regulation of NADPH Oxidases in Skeletal Muscle. Free Radic. Biol. Med. 2016;98:18–28. doi: 10.1016/j.freeradbiomed.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mahmoud A.M., Ali M.M., Miranda E.R., Mey J.T., Blackburn B.K., Haus J.M., Phillips S.A. Nox2 Contributes to Hyperinsulinemia-Induced Redox Imbalance and Impaired Vascular Function. Redox Biol. 2017;13:288–300. doi: 10.1016/j.redox.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cully T.R., Rodney G.G. Nox4–RyR1–Nox2: Regulators of Micro-Domain Signaling in Skeletal Muscle. Redox Biol. 2020;36 doi: 10.1016/j.redox.2020.101557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nishikawa T., Edelstein D., Du X.L., Yamagishi S.I., Matsumura T., Kaneda Y., Yorek M.A., Beebe D., Oates P.J., Hammes H.P., et al. Normalizing Mitochondrial Superoxide Production Blocks Three Pathways of Hyperglycaemic Damage. Nature. 2000;404:787–790. doi: 10.1038/35008121. [DOI] [PubMed] [Google Scholar]
- 136.Chen Z., Zhang X., Ying L., Dou D., Li Y., Bai Y., Liu J., Liu L., Feng H., Yu X., et al. CIMP Synthesized by SGC as a Mediator of Hypoxic Contraction of Coronary Arteries. Am. J. Physiol. Heart Circ. Physiol. 2014;307 doi: 10.1152/ajpheart.00132.2014. [DOI] [PubMed] [Google Scholar]
- 137.Meza C.A., la Favor J.D., Kim D.H., Hickner R.C. Endothelial Dysfunction: Is There a Hyperglycemia-Induced Imbalance of NOX and NOS? Int. J. Mol. Sci. 2019;20:3775. doi: 10.3390/ijms20153775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kang L., Ayala J.E., Lee-Young R.S., Zhang Z., James F.D., Neufer P.D., Pozzi A., Zutter M.M., Wasserman D.H. Diet-Induced Muscle Insulin Resistance Is Associated with Extracellular Matrix Remodeling and Interaction with Integrin A2β 1in Mice. Diabetes. 2011;60:416–426. doi: 10.2337/db10-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kang L., Lantier L., Kennedy A., Bonner J.S., Mayes W.H., Bracy D.P., Bookbinder L.H., Hasty A.H., Thompson C.B., Wasserman D.H. Hyaluronan Accumulates with High-Fat Feeding and Contributes to Insulin Resistance. Diabetes. 2013;62:1888–1896. doi: 10.2337/db12-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Berria R., Wang L., Richardson D.K., Finlayson J., Belfort R., Pratipanawatr T., de Filippis E.A., Kashyap S., Mandarino L.J. Increased Collagen Content in Insulin-Resistant Skeletal Muscle. Am. J. Physiol. -Endocrinol. Metab. 2006;290:560–565. doi: 10.1152/ajpendo.00202.2005. [DOI] [PubMed] [Google Scholar]
- 141.Fogelstrand P., Borén J. Treatment of Hyaluronan Accumulation Ameliorates High-Fat Diet-Induced Insulin Resistance in Mice. Diabetes. 2013;62:1816–1817. doi: 10.2337/db13-0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kodama K., Toda K., Morinaga S., Yamada S., Butte A.J. Anti-CD44 Antibody Treatment Lowers Hyperglycemia and Improves Insulin Resistance, Adipose Inflammation, and Hepatic Steatosis in Diet-Induced Obese Mice. Diabetes. 2015;64:867–875. doi: 10.2337/db14-0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Saunders K.H., Shukla A.P., Igel L.I., Aronne L.J. Obesity: When to Consider Medication. J. Fam. Pract. 2017;66:608–617. [PubMed] [Google Scholar]
- 144.Gadde K.M., Martin C.K., Berthoud H.R., Heymsfield S.B. Obesity: Pathophysiology and Management. J. Am. Coll. Cardiol. 2018;71:69–84. doi: 10.1016/j.jacc.2017.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., Mead B.R., Noonan R., Hardman C.A. Obesity, Eating Behavior and Physical Activity during COVID-19 Lockdown: A Study of UK Adults. Appetite. 2021;156 doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Deschasaux-Tanguy M., Druesne-Pecollo N., Esseddik Y., de Edelenyi F.S., Allès B., Andreeva V.A., Baudry J., Charreire H., Deschamps V., Egnell M., et al. Diet and Physical Activity during the Coronavirus Disease 2019 (COVID-19) Lockdown (March-May 2020): Results from the French NutriNet-Santé Cohort Study. Am. J. Clin. Nutr. 2021;113:924–938. doi: 10.1093/ajcn/nqaa336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Rodríguez J.E., Campbell K.M. Past, Present, and Future of Pharmacologic Therapy in Obesity. Prim. Care. 2016;43:61–67. doi: 10.1016/j.pop.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 148.Khera R., Murad M.H., Chandar A.K., Dulai P.S., Wang Z., Prokop L.J., Loomba R., Camilleri M., Singh S. Association of Pharmacological Treatments for Obesity Withweight Loss and Adverse Events a Systematic Review and Meta-Analysis. JAMA-J. Am. Med. Assoc. 2016;315:2424–2434. doi: 10.1001/jama.2016.7602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tak Y.J., Lee S.Y. Long-Term Efficacy and Safety of Anti-Obesity Treatment: Where Do We Stand? Curr. Obes. Rep. 2021;10:14–30. doi: 10.1007/s13679-020-00422-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Daneschvar H.L., Aronson M.D., Smetana G.W. FDA-Approved Anti-Obesity Drugs in the United States. Am. J. Med. 2016;129:879.e1–879.e6. doi: 10.1016/j.amjmed.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 151.Sharretts J., Galescu O., Gomatam S., Andraca-Carrera E., Hampp C., Yanoff L. Cancer Risk Associated with Lorcaserin-The FDA’s Review of the CAMELLIA-TIMI 61 Trial. N. Engl. J. Med. 2020;383:1000–1002. doi: 10.1056/NEJMp2003873. [DOI] [PubMed] [Google Scholar]
- 152.Coulter A.A., Rebello C.J., Greenway F.L. Centrally Acting Agents for Obesity: Past, Present, and Future. Drugs. 2018;78:1113–1132. doi: 10.1007/s40265-018-0946-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Narayanaswami V., Dwoskin L.P. Obesity: Current and Potential Pharmacotherapeutics and Targets. Pharmacol. Ther. 2017;170:116–147. doi: 10.1016/j.pharmthera.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bougoulia M., Triantos A., Koliakos G. Effect of Weight Loss with or without Orlistat Treatment on Adipocytokines, Inflammation, and Oxidative Markers in Obese Women. Hormones. 2006;5:259–269. doi: 10.14310/horm.2002.11190. [DOI] [PubMed] [Google Scholar]
- 155.Hsieh C.J., Wang P.W., Liu R.T., Tung S.C., Chien W.Y., Chen J.F., Chen C.H., Kuo M.C., Hu Y.H. Orlistat for Obesity: Benefits beyond Weight Loss. Diabetes Res. Clin. Pract. 2005;67:78–83. doi: 10.1016/j.diabres.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 156.Vorsanger M.H., Subramanyam P., Weintraub H.S., Lamm S.H., Underberg J.A., Gianos E., Goldberg I.J., Schwartzbard A.Z. Cardiovascular Effects of the New Weight Loss Agents. J. Am. Coll. Cardiol. 2016;68:849–859. doi: 10.1016/j.jacc.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 157.Gadde K.M., Allison D.B., Ryan D.H., Peterson C.A., Troupin B., Schwiers M.L., Day W.W. Effects of Low-Dose, Controlled-Release, Phentermine plus Topiramate Combination on Weight and Associated Comorbidities in Overweight and Obese Adults (CONQUER): A Randomised, Placebo-Controlled, Phase 3 Trial. Lancet. 2011;377:1341–1352. doi: 10.1016/S0140-6736(11)60205-5. [DOI] [PubMed] [Google Scholar]
- 158.von Scholten B.J., Persson F., Rosenlund S., Eugen-Olsen J., Pielak T., Faber J., Hansen T.W., Rossing P. Effects of Liraglutide on Cardiovascular Risk Biomarkers in Patients with Type 2 Diabetes and Albuminuria: A Sub-Analysis of a Randomized, Placebo-Controlled, Double-Blind, Crossover Trial. Diabetes Obes. Metab. 2017;19:901–905. doi: 10.1111/dom.12884. [DOI] [PubMed] [Google Scholar]
- 159.Zobel E.H., Ripa R.S., von Scholten B.J., Rotbain Curovic V., Kjaer A., Hansen T.W., Rossing P., Størling J. Effect of Liraglutide on Expression of Inflammatory Genes in Type 2 Diabetes. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-97967-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zobel E.H., Ripa R.S., von Scholten B.J., Curovic V.R., Diaz L.J., Hansen T.W., Rossing P., Kjaer A. Effect of Liraglutide on Vascular Inflammation Evaluated by [64 Cu] DOTATATE. Diagnostics. 2021;11:1431. doi: 10.3390/diagnostics11081431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Savchenko L.G., Digtiar N.I., Selikhova L.G., Kaidasheva E.I., Shlykova O.A., Vesnina L.E., Kaidashev I.P. Liraglutide Exerts an Anti-Inflammatory Action in Obese Patients with Type 2 Diabetes. Rom. J. Intern. Med. Rev. Roum. Med. Interne. 2019;57:233–240. doi: 10.2478/rjim-2019-0003. [DOI] [PubMed] [Google Scholar]
- 162.Ripa R.S., Zobel E.H., von Scholten B.J., Jensen J.K., Binderup T., Diaz L.J., Curovic V.R., Hansen T.W., Rossing P., Kjaer A. Effect of Liraglutide on Arterial Inflammation Assessed as [18 F] FDG Uptake in Patients With Type 2 Diabetes: A Randomized, Double-Blind, Placebo-Controlled Trial. Circulation. Cardiovasc. Imaging. 2021;14:632–644. doi: 10.1161/CIRCIMAGING.120.012174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Smits M.M., Tonneijck L., Muskiet M.H.A., Hoekstra T., Kramer M.H.H., Diamant M., Serné E.H., van Raalte D.H. GLP-1-Based Therapies Have No Microvascular Effects in Type 2 Diabetes Mellitus: An Acute and 12-Week Randomized, Double-Blind, Placebo-Controlled Trial. Arterioscler. Thromb. Vasc. Biol. 2016;36:2125–2132. doi: 10.1161/ATVBAHA.116.307930. [DOI] [PubMed] [Google Scholar]
- 164.Heidari B., Lerman A., Lalia A.Z., Lerman L.O., Chang A.Y. Effect of Metformin on Microvascular Endothelial Function in Polycystic Ovary Syndrome. Mayo Clin. Proc. 2019;94:2455–2466. doi: 10.1016/j.mayocp.2019.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Andrews M., Soto N., Arredondo M. [Effect of Metformin on the Expression of Tumor Necrosis Factor-α, Toll like Receptors 2/4 and C Reactive Protein in Obese Type-2 Diabetic Patients] Rev. Med. Chile. 2012;140:1377–1382. doi: 10.4067/S0034-98872012001100001. [DOI] [PubMed] [Google Scholar]
- 166.Schiapaccassa A., Maranhão P.A., de Souza M.D.G.C., Panazzolo D.G., Nogueira Neto J.F., Bouskela E., Kraemer-Aguiar L.G. 30-Days Effects of Vildagliptin on Vascular Function, Plasma Viscosity, Inflammation, Oxidative Stress, and Intestinal Peptides on Drug-Naïve Women with Diabetes and Obesity: A Randomized Head-to-Head Metformin-Controlled Study. Diabetol. Metab. Syndr. 2019;11 doi: 10.1186/s13098-019-0466-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Schiappacassa A., Maranhão P.A., de Souza M.D.G.C., Panazzolo D.G., Neto J.F.N., Bouskela E., Kraemer-Aguiar L.G. Acute Effects of Metformin and Vildagliptin after a Lipid-Rich Meal on Postprandial Microvascular Reactivity in Patients with Type 2 Diabetes and Obesity: A Randomized Trial. J. Clin. Med. 2020;9:3228. doi: 10.3390/jcm9103228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kitao N., Miyoshi H., Furumoto T., Ono K., Nomoto H., Miya A., Yamamoto C., Inoue A., Tsuchida K., Manda N., et al. The Effects of Vildagliptin Compared with Metformin on Vascular Endothelial Function and Metabolic Parameters: A Randomized, Controlled Trial (Sapporo Athero-Incretin Study 3) Cardiovasc. Diabetol. 2017;16 doi: 10.1186/s12933-017-0607-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Petrie J.R., Chaturvedi N., Ford I., Brouwers M.C.G.J., Greenlaw N., Tillin T., Hramiak I., Hughes A.D., Jenkins A.J., Klein B.E.K., et al. Cardiovascular and Metabolic Effects of Metformin in Patients with Type 1 Diabetes (REMOVAL): A Double-Blind, Randomised, Placebo-Controlled Trial. Lancet. Diabetes Endocrinol. 2017;5:597–609. doi: 10.1016/S2213-8587(17)30194-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jax T., Stirban A., Terjung A., Esmaeili H., Berk A., Thiemann S., Chilton R., Eynatten M., Marx N. A Randomised, Active- and Placebo-Controlled, Three-Period Crossover Trial to Investigate Short-Term Effects of the Dipeptidyl Peptidase-4 Inhibitor Linagliptin on Macro- and Microvascular Endothelial Function in Type 2 Diabetes. Cardiovasc. Diabetol. 2017;16 doi: 10.1186/s12933-016-0493-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gabriel R., Abdelkader N.B., Acosta T., Gilis-Januszewska A., Gómez-Huelgas R., Makrilakis K., Kamenov Z., Paulweber B., Satman I., Djordjevic P., et al. Early Prevention of Diabetes Microvascular Complications in People with Hyperglycaemia in Europe. EPREDICE Randomized Trial. Study Protocol, Recruitment and Selected Baseline Data. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0231196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kelly A.S., Bergenstal R.M., Gonzalez-Campoy J.M., Katz H., Bank A.J. Effects of Exenatide vs. Metformin on Endothelial Function in Obese Patients with Pre-Diabetes: A Randomized Trial. Cardiovasc. Diabetol. 2012;11 doi: 10.1186/1475-2840-11-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Hamidi V., Riggs K., Zhu L., Bermudez Saint Andre K., Westby C., Coverdale S., Dursteler A., Wang H., Miller C., Taegtmeyer H., et al. Acute Exenatide Therapy Attenuates Postprandial Vasodilation in Humans with Prediabetes: A Randomized Controlled Trial. Metab. Syndr. Relat. Disord. 2020;18:225–233. doi: 10.1089/met.2019.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Thomas M.C., Cherney D.Z.I. The Actions of SGLT2 Inhibitors on Metabolism, Renal Function and Blood Pressure. Diabetologia. 2018;61:2098–2107. doi: 10.1007/s00125-018-4669-0. [DOI] [PubMed] [Google Scholar]
- 175.Sun X., Han F., Lu Q., Li X., Ren D., Zhang J., Han Y., Xiang Y.K., Li J. Empagliflozin Ameliorates Obesity-Related Cardiac Dysfunction by Regulating Sestrin2-Mediated AMPK-MTOR Signaling and Redox Homeostasis in High-Fat Diet-Induced Obese Mice. Diabetes. 2020;69:1292–1305. doi: 10.2337/DB19-0991. [DOI] [PubMed] [Google Scholar]
- 176.Tanaka A., Shimabukuro M., Machii N., Teragawa H., Okada Y., Shima K.R., Takamura T., Taguchi I., Hisauchi I., Toyoda S., et al. Secondary Analyses to Assess the Profound Effects of Empagliflozin on Endothelial Function in Patients with Type 2 Diabetes and Established Cardiovascular Diseases: The Placebo-Controlled Double-Blind Randomized Effect of Empagliflozin on Endothelial Function in Cardiovascular High Risk Diabetes Mellitus: Multi-Center Placebo-Controlled Double-Blind Randomized Trial. J. Diabetes Investig. 2020;11:1551–1563. doi: 10.1111/JDI.13289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Zemel M.B., Kolterman O., Rinella M., Vuppalanchi R., Flores O., Barritt A.S., Siddiqui M., Chalasani N. Randomized Controlled Trial of a Leucine-Metformin-Sildenafil Combination (NS-0200) on Weight and Metabolic Parameters. Obesity. 2019;27:59–67. doi: 10.1002/oby.22346. [DOI] [PubMed] [Google Scholar]
- 178.Rebello C.J., Zemel M.B., Kolterman O., Fleming G.A., Greenway F.L. Leucine and Sildenafil Combination Therapy Reduces Body Weight and Metformin Enhances the Effect at Low Dose: A Randomized Controlled Trial. Am. J. Ther. 2021;28:e1–e13. doi: 10.1097/MJT.0000000000001303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mortensen S.P., Egginton S., Madsen M., Hansen J.B., Munch G.D.W., Iepsen U.W., Åkerström T., Pedersen B.K., Hellsten Y. Alpha Adrenergic Receptor Blockade Increases Capillarization and Fractional O 2 Extraction and Lowers Blood Flow in Contracting Human Skeletal Muscle. Acta Physiol. (Oxf. Engl.) 2017;221:32–43. doi: 10.1111/apha.12857. [DOI] [PubMed] [Google Scholar]
- 180.Dunford E.C., Leclair E., Aiken J., Mandel E.R., Haas T.L., Birot O., Riddell M.C. The Effects of Voluntary Exercise and Prazosin on Capillary Rarefaction and Metabolism in Streptozotocin-Induced Diabetic Male Rats. J. Appl. Physiol. 2017;122:492. doi: 10.1152/japplphysiol.00762.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Abuissa H., Jones P.G., Marso S.P., O’Keefe J.H. Angiotensin-Converting Enzyme Inhibitors or Angiotensin Receptor Blockers for Prevention of Type 2 Diabetes: A Meta-Analysis of Randomized Clinical Trials. J. Am. Coll. Cardiol. 2005;46:821–826. doi: 10.1016/j.jacc.2005.05.051. [DOI] [PubMed] [Google Scholar]
- 182.Ling S., Nheu L., Dai A., Guo Z., Komesaroff P. Effects of Four Medicinal Herbs on Human Vascular Endothelial Cells in Culture. Int. J. Cardiol. 2008;128:350–358. doi: 10.1016/j.ijcard.2007.05.111. [DOI] [PubMed] [Google Scholar]
- 183.Lv P., Tong X., Peng Q., Liu Y., Jin H., Liu R., Sun W., Pan B., Zheng L., Huang Y. Treatment with the Herbal Medicine, Naoxintong Improves the Protective Effect of High-Density Lipoproteins on Endothelial Function in Patients with Type 2 Diabetes. Mol. Med. Rep. 2016;13:2007–2016. doi: 10.3892/mmr.2016.4792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Khodadadi S., Zabihi N.A., Niazmand S., Abbasnezhad A., Mahmoudabady M., Rezaee S.A. Teucrium Polium Improves Endothelial Dysfunction by Regulating ENOS and VCAM-1 Genes Expression and Vasoreactivity in Diabetic Rat Aorta. Biomed. Pharmacother. Biomed. Pharmacother. 2018;103:1526–1530. doi: 10.1016/j.biopha.2018.04.158. [DOI] [PubMed] [Google Scholar]
- 185.Parsamanesh N., Asghari A., Sardari S., Tasbandi A., Jamialahmadi T., Xu S., Sahebkar A. Resveratrol and Endothelial Function: A Literature Review. Pharmacol. Res. 2021;170 doi: 10.1016/j.phrs.2021.105725. [DOI] [PubMed] [Google Scholar]
- 186.Minozzo B.R., Fernandes D., Beltrame F.L. Phenolic Compounds as Arginase Inhibitors: New Insights Regarding Endothelial Dysfunction Treatment. Planta Med. 2018;84:277–295. doi: 10.1055/s-0044-100398. [DOI] [PubMed] [Google Scholar]
- 187.Noce A., di Lauro M., di Daniele F., Zaitseva A.P., Marrone G., Borboni P., di Daniele N. Natural Bioactive Compounds Useful in Clinical Management of Metabolic Syndrome. Nutrients. 2021;13:630. doi: 10.3390/nu13020630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Xu H., Wang X., Feng W., Liu Q., Zhou S., Liu Q., Cai L. The Gut Microbiota and Its Interactions with Cardiovascular Disease. Microb. Biotechnol. 2020;13:637–656. doi: 10.1111/1751-7915.13524. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.