Abstract
Spinal cord injuries (SCI) are disruptive neurological events that severly affect the body leading to the interruption of sensorimotor and autonomic pathways. Recent research highlighted SCI-related alterations extend beyond than the expected network, involving most of the central nervous system and goes far beyond primary sensorimotor cortices. The present perspective offers an alternative, useful way to interpret conflicting findings by focusing on the deafferented and deefferented body as the central object of interest. After an introduction to the main processes involved in reorganization according to SCI, we will focus separately on the body regions of the head, upper limbs, and lower limbs in complete, incomplete, and deafferent SCI participants. On one hand, the imprinting of the body’s spatial organization is entrenched in the brain such that its representation likely lasts for the entire lifetime of patients, independent of the severity of the SCI. However, neural activity is extremely adaptable, even over short time scales, and is modulated by changing conditions or different compensative strategies. Therefore, a better understanding of both aspects is an invaluable clinical resource for rehabilitation and the successful use of modern robotic technologies.
Keywords: spinal cord injury, neural plasticity, central nervous system, face representation, limb representation, phantom limb, neuropathic pain, rehabilitation, disembodied, deafferentation, body representation, somatotopy
1. Introduction
Spinal cord injury (SCI) is a devastating neurological injury that mostly affects young individuals, severely limiting their normal life activities. SCIs are commonly attributed to sudden trauma, acute/chronic disease processes, or degeneration of the vertebrae [1]. Unfortunately, there is no satisfactory treatment for SCI victims yet. The degree of impairment depends on the level and entity of the lesion, with partial or complete loss of sensation and loss of voluntary movements of the body below the level of the lesion. Early clinical treatment at the primary lesion site, such as surgical decompression, is frequently associated with significant clinical improvements [2]. However, the injury is also immediately accompanied by a sustained cascade of biological events [3,4,5], termed “secondary injuries.” These dynamic effects lead to neuroplastic changes below and above the lesion throughout the central nervous system (CNS), including the brain [4]. Therefore, understanding the subsequent reorganization entails placing emphasis on the specific damaged tissues, studying the ensuing events from a pathophysiological perspective [5]. Alternatively, the rehabilitation-based perspective, in its widest and most multidisciplinary sense, focuses on enabling the body to recover and regain its ability to interact physically and socially with the world [6]. Here we explore yet a third method, not considered as an alternative but encompassing different approaches, whereby the body and its representations in the nervous system, act as a bridge between neurobiological and clinical/behavioral outcomes.
We provide a comprehensive yet concise summary of the current knowledge on how SCI impacts the representation of the entire body, both above and below the injury. The first section summarizes the main structural and functional neuroplastic events that typically occur throughout the CNS following SCI and that unfolds at different spatial and temporal scales. The second section discusses the most relevant studies relating to body representation for the three main parts of the body: (i) lower limbs, (ii) trunk and upper limbs, and (iii) head and face. Only a better understanding of the neurobiological and clinical/behavioral outcomes will allow the development of appropriate therapeutic strategies.
2. Neural Plasticity following SCI
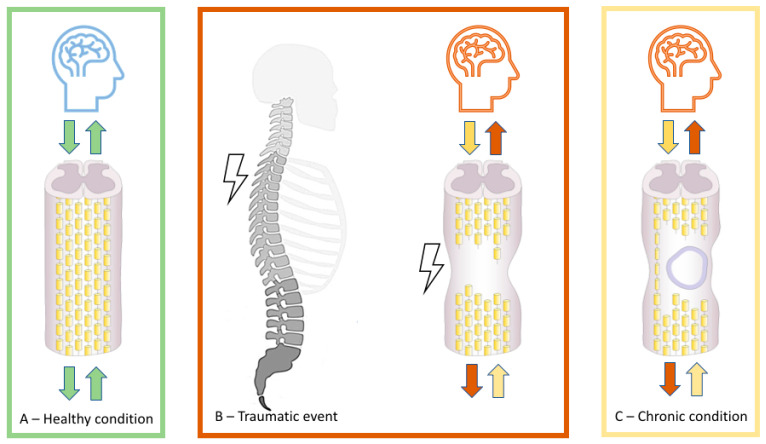
At the neural systems level, an altered signal initiated at the lesion’s origin in the spinal cord spreads until the endpoint of the sensorimotor tract [7,8,9] in the cortex causing changes at all levels of CNS circuitry (i.e., the spinal cord, brainstem, and brain). These dynamic processes in the CNS circuitry involve modification of cortical somatotopy, requiring changes in body self-perception [10]. The immediate damage to neurons, axonal circuits, and to the tissue in the injured area cause the formation of a glial scar that limits tissue loss but also acts as a barrier for axonal growth [4]. Neurodegenerative process occurs along the dorsal columns and in the descending corticospinal tracts presumably, driving the activity of large cortical networks [11,12,13]. Neuroimaging techniques are the most powerful methods for mapping on human brain the consequences of “disconnected” spinal segments. These spinal changes (Figure 1) are the main trigger of neuroplasticity in neural centers supraspinal can lead to abnormal cortical excitability, altered connectivity and neural changes [13,14,15,16,17,18,19,20,21,22,23,24]. Specific brain morphometric differences with a reduction in white matter and gray matter, involve but are not limited to, the primary motor [11,13] and sensory cortices [11]. Resting-state functional magnetic resonance imaging studies have revealed that the strength of intra- and inter-hemispheric functional connectivity within sensorimotor cortex is dependent on ascending and descending altered signals from spinal and immediately supraspinal structures [10,13]. Brain activity alterations [23,24] can be recorded even in incomplete SCI injuries [25] and are correlated with the number of “disconnected” spinal segments [21,24,26,27,28]. Progressive atrophic, microstructural, and biochemical changes after SCI has also been associated with altered motor and sensory body behaviour [29,30,31,32,33]. Given the reduction in body efferent and afferent signals, the entire cortex is also exposed to reduced functional connectivity, that constantly includes different areas [34,35,36,37]. Structures, such as the fusiform gyrus or the orbitofrontal cortex, may also be at play in anatomical and functional reorganization also occurs in the sensorimotor cortex [38]. However, it is possible that despite the morphometric changes of sensorimotor activity after SCI, somatotopically typical representations of the paralysed and sensory deprived body parts can be initially preserved but deteriorates across time.
Figure 1.
Schematic representation of the pathophysiology of a normal (A) and an injured spinal cord (B,C). The initial mechanical trauma to the spinal cord (B) initiates a secondary injury cascade that is characterized by edema, hemorrhage, inflammatory cells (B), and the persistence of scar tissue (C), which can lead to further cell death, demyelination, and neurological impairments in orthograde and retrograde directions, including brain areas.
In addition, cortical reorganization after SCI has also been associated with neuropathic or phantom limb pain [37,38,39]. The onset and evolution of pain in SCI and its effects on the nervous system remain unclear. Huynh, et al. [39], reviewed imaging studies to assess supraspinal neuroplasticity differences between groups of SCI patients with and without neuropathic pain in the resting condition. They found changes in the concentration of metabolites in sensory and pain-related areas, such as the thalamus and the anterior cingulate cortex, that depended on the presence and intensity of neuropathic pain [40,41]. Furthermore, grey matter volume alterations in the same areas have also been observed in SCI patients with neuropathic pain [23]. Differences in gray matter volume of motor and somatosensory primary cortices indicate other possible sites related to neuropathic pain [23]. Finally, differences associated with neuropathic pain have been observed in activity patterns within the insula, making it a possible target for future clinical research [41].
Important information on the over time evolution of SCI also comes from the perceptual symptoms reported by patients. Phantom limb sensations are common after SCI [42], both for upper and lower limbs (depending on the lesion level), but less well-characterized and studied than in amputations and other neurological deafferentations such as brachial plexus avulsion [43,44,45,46]. Understanding such symptoms and their spontaneous and rehabilitation-driven evolution may help reveal the brain-body coupling mechanisms, improving clinical outcomes. In this context, different studies have clearly shown a seemingly contradictory contribution of processes promoting stability, remapping, and reorganization. To integrate the two perspectives, Muret and Makin (2020) have recently proposed that homeostasis can be scaled up from an intra-cellular level to a neuronal network level. That is, the representation of adjacent body parts in the somatosensory Penfield’s homunculus may overlap and borders fade. Finally, the loss of sensory input alters normal lateral cortical inhibitory processes, emphasizing latent activity in the deafferented areas as well as homeostasis [47].
This analysis introduces new factors that may help disentangle the complex dynamics of brain adaptation post-SCI and may assist in understanding phenomena such as phantom limbs or the long-term somatotopic stability of the deafferented body.
3. Body Reorganization and Body Stability of Somatosensory-Motor Topographies
Currently, the most effective technique for addressing body-brain disconnection in SCI is brain activity registration [48] during three main activities: mental imagery, sensory stimulation, and motor activity. However, the mechanisms through which the brain interprets and fails to record the signals from affected and non-affected body parts remain controversial. We examine the evidence in favor of somatotopic rearrangement as a possible representational rule underlying the loss of extension, reductions, or absence of activity in the affected body, while considering how movements and sensations of the body are expanded and shifted.
3.1. Reorganization and Stability of the Lower Limb Representation
The traditional view of this problem suggests that severe sensorimotor impairment should correspond to shifts, loss of extension, and reductions in cortical thickness and/or activation in lower-limb corresponding areas of the brain. However, this represents an over-simplification caused mainly by over-interpreting the results of early studies in the field due to the clinical need to categorize sensory and motor residual functions. According to the American Spinal Cord Injury Association (ASIA) classification, a complete SCI lesion is classified as AIS Grade A, meaning that the patient does not feel any sensation—or cannot produce any motor activity—in the part of the body below the lesion. Meanwhile, an AIS Grade B lesion means that while body sensations from below the SCI are spared, complete motor loss is present. AIS grades C–E describe different levels of sensorimotor impairment. However, more recent evidence suggests that at least one more level exists between AIS grade A and B; over 30 years ago, such a condition was known as a discomplete lesion whereby at least sensory information was able to reach the brain, even in the absence of a patient’s awareness [49]. Importantly, recent studies have shown that sensory connections are spared in approximately half of the lesions considered to be complete [50,51]. The purpose of these brief considerations is to highlight the risk of relevant biases that occur in most studies regarding the consequences of an SCI on the CNS, in line with a recent review [52].
A procedure seeking to identify changes in the cortical representation of the lower limbs consists of simple sensory stimulation. Gentle toe brushing of patients with clinically complete SCIs (AIS Grade A) was used to evoke S1 activation, making it possible to discriminate between complete and incomplete lesions [50]. In 11 of the 23 participants with complete lesions, significant S1 activation was produced by toe brushing, which was not correlated to the presence of neuropathic pain. Furthermore, the location did not differ between the subjects with discomplete lesions and healthy control participants. Moreover, activity was recorded in the contralateral S2, contralateral thalamus, and ipsilateral cerebellum, without any significant location differences. A subsequent study confirmed how different types of sub-lesional sensory stimulations (touch and nociception) correlate with brain activation in the expected contralateral somatosensory areas [51]. Activation was also recorded in the bilateral S2 region and contralateral Brodmann area 5, the insula, and anterior cingulate cortex for nociceptive stimuli.
Depending on the level and severity of SCI, researchers have used various experimental paradigms, including motor activity, motor attempt, and mental/motor imagery tasks, to study lower limb-related brain activity in humans. For example, Sharp et al. [53] using fMRI, offered important insights into the main characteristics of lower limb-related brain activity changes during ankle dorsiflexion. In patients with incomplete spinal cord lesions, the authors found a correlation between higher activation levels and more severe impairment of the lower limbs. Moreover, the chronicity of an SCI plays a major role in the exacerbation of these changes, especially in the supplementary motor area and left frontoparietal regions, pointing to the occurrence of a process of adaptation. In this study, the researchers observed enhanced recruitment of the expected correct sensorimotor areas (i.e., non-dominant) during voluntary movement of the right ankle, and a higher level of brain activity correlated with a higher impairment level. Recently, new studies have been conducted on body-related cortical reorganization that have explored the impact of mental imagery repetitive tapping task of both upper- and lower-limbs in patients with complete SCI [54]. When compared to healthy controls, the blood oxygenation level-dependent (BOLD) response in SCI patients showed both stronger and weaker responses to upper-limb mental imagery tasks. Healthy controls showed strong signals in the left middle frontal gyrus, left anterior cingulate, and left medial frontal gyrus. Patients with complete SCI have stronger activation in the left inferior parietal gyrus, left precentral gyrus, and left postcentral gyrus. A stronger BOLD response in the SCI group was also evident in the right globus pallidus, right thalamus, right superior temporal gyrus, right inferior parietal gyrus, and right precentral gyrus. In the lower-limb version of the imagery task, controls produced stronger signals in the right anterior cingulate, right medial frontal gyrus, right superior temporal gyrus, and right superior frontal gyrus. However, patients with SCI demonstrated more intense activity in the left lingual gyrus and right globus pallidus [54]. The authors found a negative correlation between time since injury and signal intensity in the left precentral gyrus and left lingual gyrus, suggesting that this may be a consequence of compensatory mechanisms triggered by motor and sensory loss. Therefore, a generalized compensatory process may be found in the stronger activation of visual and auditory subcortical processing areas for both upper-and lower-limb motor imagery tasks. Despite the contradictory findings in activation intensity and patterns in fMRI studies, it appears appropriate to consider the cortical structural representation of the areas of the body below the lesion as mostly stable throughout both the acute and chronic phases. When assessed, somatotopy of the lower limbs––specifically the ankle and toes––corresponds to that of healthy controls. However, in terms of activation patterns and intensity, while it remains too early to provide precise answers, compensatory processes likely play a fundamental role in the recruitment of contralateral sensorimotor areas as well as in the involvement of more distant cortical and subcortical structures.
3.2. Reorganization and Stability of Upper Limb Representation
The upper body, specifically the upper limbs, offers a wider range of experimental opportunities to assess changes in body representations in the brain following a SCI, when compared to the lower limbs. TMS is a non-invasive brain stimulation technique that produces different effects depending on the target area. For example, stimulation of the primary motor cortex with TMS produces motor-evoked potentials that can be recorded in the muscles [55]. TMS has long since been used to explore the effects of deafferentation and has helped confirm changes in the cortical representation of the body showing how, in SCI patients, to produce motor evoked potentials of muscles surface and position of the stimulation site can be different than in healthy controls [56]. As previously mentioned, the results from past studies are not entirely consistent; however, differences continue to be found in the extent, intensity, and pattern of brain activity related to movements of the upper body in the case of SCI. For example, in their fMRI research, Curt et al. found a substantial stability of the somatotopic organization of the upper limbs in M1 during a controlled movement task of the upper limb and tongue free movement. However, the pattern and extent of activation differed from those of healthy participants [36].
In the primary motor area, only the movement of the fingers produced a change, which consisted of more extensive activations that expand medially and laterally compared to that in the controls. Movements of both the wrist and elbow in SCI patients are related to greater activation of non-primary cortical areas involved in movement, such as the supplementary motor area, the dorsal premotor area, the primary somatosensory cortex, and the cerebellum. Just a few years earlier, a PET study, using a hand movement task to control a joystick, identified, albeit in less detail, differences in activation patterns, also differentiating paraplegic and tetraplegic participants in comparison with healthy controls [21]. The activation areas shared with healthy subjects, in the case of SCI, presented greater and more extensive activations for both paraplegics and tetraplegics, which also involved cortical areas normally associated with the legs. Furthermore, both SCI groups also showed activation of the parietal, cerebellar, and thalamic areas. Counter-intuitively, the paraplegics showed more intense and extensive activity, which was explained by the greater sensorimotor impairment of the hand in tetraplegics. The shift in hand-related somatosensory areas was subsequently confirmed in larger groups of patients with SCI using fMRI during a tactile stimulation of the mouth, fingers and toe [24]. This shift mainly occurs towards the medial areas that correspond to the legs, or, more generally, the sub-lesion part of the body. This phenomenon is particularly affected by the area corresponding to the little finger, which extends its activation area by 13 mm towards the cortical areas directly involved in SCI and therefore is “disconnected” from the body. It is noteworthy that the loss of gray matter that occurs in most of the deafferented S1 areas was not seen in individuals in whom hand-related activity was extended. This is likely due not only to the exceptional recruitment of dormant neuronal populations found in the short term after the injury [57] but also to a real trophic process of sprouting that leads to an increase in lateral cortical connections [24]. Using TMS, Fassett, Turco, El-Sayes and Nelson [56] found alterations in somatotopic organization in the bilateral primary motor cortex of the biceps, flexor carpi radialis, and abductor pollicis brevis in participants with an incomplete cervical SCI. While the overall somatotopic organization between the parts studied does not present substantial differences between SCI patients and healthy controls, the entire region is medially shifted in SCI. A further change concerns the extension of the cortical territory relating to the abductor pollicis brevis, which is more accentuated than that in healthy participants. Researchers attribute these aspects to two major possible factors: learning of motor skills related to the need to adapt to new physical conditions and compensatory mechanisms of plasticity due to the need to optimize the neural output necessary to control muscles whose functionality is compromised [56]. In some tetraplegic patients, finger movement is no longer possible, depending on the level of the lesion, while the arms can still be controlled. However, surgical transfer of the distal brachioradialis tendon to the flexor pollicis longus can restore the pinch grip of the flexion of the thumb [58]. After a long training period, patients learn to move their thumb, controlling a muscle normally used only in elbow movements. Interestingly, the movement change corresponds to a change in the areas activated in motor cortices [59]. Furthermore, researchers have shown that in patients with SCI, cortical activity related to the brachioradialis muscle shifts from the elbow area (before the surgical tendon transfer) to the wrist-related area. This suggests that the motor cortical areas and their connections remain intact, even after prolonged disconnection from the corresponding body areas.
In addition, the ability of plastic reorganization is maintained to allow these areas to participate in long-lost motor activity (i.e., at the time of spinal injury), even when using a muscle that was previously not directly involved in this movement. After some time, in the same group of patients, it was possible to study the morphological changes in the cortical areas involved in thumb movement. That is, the primary motor cortex showed a general condition of atrophy, but when specifically considering only the area “reactivated”, because of the tendon transfer procedure, there was no difference in cortical thickness between tetraplegic patient and healthy controls [60].
3.3. Reorganization and Stability of Face Representation
Dorsal column lesions [61,62,63,64] or dorsal root transections [65] of the spinal cord in non-human primates are prominent models for large-scale face cortical reorganization of the primary somatosensory cortex. During this reorganization, the facial inputs for hand deafferented representation expand by 7–20 mm [61,63,64,66], shifting the face/hand map boundaries [63].
In fact, somatotopic remapping processes occur with the establishment of new connections between the face and the deafferented hand region in the primary somatosensory cortex [67,68]. Reorganization is also seen in the ventroposterior nucleus of the thalamus [63,69,70,71] and in the spinal cord and dorsal column nuclei [72], despite the fact that selective somatotopic interference, cortical dynamics, and neuroplasticity, based on competitive interaction from a normally innervated territory, are common and widely accepted. However, there remains no objective evidence supporting a link between neural topographic substitution and peripheral loss in humans, as has been observed in monkeys. Brain-imaging studies of humans show contradictory findings, reporting possible reorganization of the cortex after SCI with expansion of the representation of the face into the hand region [38,47,73]. Specifically, it has been shown that, in patients with cervical lesions, tongue movement is displaced medially, posteriorly, and superiorly (12 mm) toward the adjacent cortical deafferented hand area compared to that in controls, with a strong correlation between displacement and the level of SCI [73]. Similar cortical remapping was found by Corbetta et al. [37], who used visuomotor monitoring to assess a patient with cervical SCI. The patient had to synchronize his tongue movements with a video image, after which he received vibrotactile stimulation in the palm of his hand. They found stronger and more widespread BOLD responses in the patient than in the control subject. The activity of brain responses to tongue movement spread dorsally in the hand area and broadly in the second somatosensory cortex and frontal operculum. In addition, the SI/M1 face area was activated in the ventral precentral gyrus, central sulcus, and postcentral gyrus.
Overlapping fMRI scans of the SCI patient and the control revealed that the active facial region was similarly active in the two participants; however, in the SCI subject, it invaded the hand area. While reorganization patterns following SCI in humans suggest a topographical remapping in the region closer to the site of deafferentation, the tactile threshold required to elicit a neural response of the new face map, and whether reorganization of face representation occurs in higher somatosensory areas, remains unknown in humans after cervical SCI. However, behaviorally, greater susceptibility to the modified rubber hand illusion paradigm (applying sensory stimulation to the face with the observed touches on the fake hand) seems to drive tetraplegics’ sense of hand ownership [74], supporting topographic remapping of the face on the hand territory. Moreover, “somatotopic interference” of the face–hand is suggested by vivid and clear “phantom” limb experiences in SCI, which implicitly confirm topographical remapping of cortical territories following peripheral disconnection [75]. However, these previous studies were unable to determine whether such activity represents functional reorganization, supporting the sensorimotor hand. Therefore, some descriptions of face-hand remapping may be misleading [76]. For example, Curt et al. (2002) did not report the topographical reorganization of M1 but did observe increased activation during tongue movements [36]. In addition, fMRI studies found no apparent expansion in the somatotopic cortical representation during attempted face movement in individuals with SCI and revealed no significant differences when compared with healthy controls [36,77]. It is also noteworthy that advanced studies using MRI with VMB and DTI analysis [24], despite reports of cortical reorganization of the hand, found no evidence of a shift following tongue movements. It is worth noting that discrepancies between human and animal neuroplasticity arise from biological differences between species, including variations in the way different species experience their bodies when interacting with the world. Beyond these differences, many changes in the relevant functional networks may be related to the extent of neurological injury and the severity of the lesion, which determine the inconsistency in results for the heterogeneous sample. Time is another critical factor related to remapping, and longitudinal studies are required to understand the progressive development of processes that, by their very definition, extend across different time scales. Shift occurs at a minimum of one year following SCI, depending on the severity of the SCI [78] indicating less chaotic reorganization subsequent to the absence of hand inputs. Changes in cortical activity may lead to the convergence of metabolic and neural processes, such as aberrant signaling [79], altered cellular metabolism [80], axonal sprouting, and fluctuations in synaptic strength due to upstream reorganization [33]. Numerous subcortical changes also play a role in reorganization, specifically thalamic reorganization, in which facial afferents in the trigeminal nucleus may grow within the cuneate nucleus [62]. For example, a study by Kambi, et al. [81] sought to identify a causal relationship between all these changes and cortical reorganization in non-human primates. Their results showed that cortical reorganization following sprouting of chin input in deafferent areas does not affect reorganization. In contrast, when the cuneate nucleus was blocked by lidocaine, there were no longer any responses from the chin region, which had previously expanded into the hand region following stimulation of the chin. Therefore, it could be assumed that humans possess the same control of the cuneate nucleus. If so, brainstem could represent a starting point for controlling cortical reorganization of somatosensory cortex [81].
4. Conclusions
The studies discussed in this paper show that peripheral and CNS lesions can induce neural reorganization within the central somatosensory and motor/body representations. However, how the brain processes the flow of signals following a body-brain disconnection due to a complete SCI remains largely unknown. How deep severe neurological traumas affect typical sensory and motor signals of single body parts and their appropriate integration by brain mechanisms and structures is unclear. In fact, there are discrepancies in the observed brain activity changes in patients with SCI. This can be attributed to heterogeneity in the extent of the neurological injury and lesion severity, to disease duration, age, as well as to the degree of altered sensory and pain experience, to compensatory learning, and to exposure to rehabilitation [82]. Importantly, the mechanisms underlying SCI are multifactorial, and changes to a patient’s temporal dynamics and experiences as well as spinal and supraspinal modifications may be the main drivers of neuroplasticity in the sensorimotor centers [11,12]. Furthermore, reorganization of the neural system appears to represent a response to body pain [83,84,85]. The approach proposed in this paper offers new insight for the body rehabilitation and the use of assistive devices [84,86,87,88]. It proposes that it is advantageous to consider somatotopically head, upper-limb, and lower limbs body areas for focal stimulation, to boost the sense of embodiment and agency in body parts with reduced access to sensori-motor information [89]. Yet, this may produce positive residual responses, improving the effects of treatment rehabilitative [90,91].
Acknowledgments
This work was supported by Ania Foundation.
Author Contributions
Conceptualization and writing—original draft preparation: E.L., G.F., V.G., M.L.D.M. and M.P.; critical revision of the article: E.L.,G.F., A.P., L.D.G., A.M.G. and M.P.; funding acquisition: M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Italian Ministry of Health, grant number RF-2018-12365682.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alizadeh A., Dyck S.M., Karimi-Abdolrezaee S. Traumatic Spinal Cord Injury: An Overview of Pathophysiology, Models and Acute Injury Mechanisms. Front. Neurol. 2019;10:282. doi: 10.3389/fneur.2019.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tykocki T., Poniatowski Ł.A., Czyz M., Wynne-Jones G. Oblique corpectomy in the cervical spine. Spinal Cord. 2017;56:426–435. doi: 10.1038/s41393-017-0008-4. [DOI] [PubMed] [Google Scholar]
- 3.Wojdasiewicz P., Poniatowski Ł.A., Turczyn P., Frasuńska J., Paradowska-Gorycka A., Tarnacka B. Significance of Omega-3 Fatty Acids in the Prophylaxis and Treatment after Spinal Cord Injury in Rodent Models. Mediat. Inflamm. 2020;2020:3164260. doi: 10.1155/2020/3164260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silva N., Sousa N., Reis R.L., Salgado A.J. From basics to clinical: A comprehensive review on spinal cord injury. Prog. Neurobiol. 2014;114:25–57. doi: 10.1016/j.pneurobio.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Ahuja C.S., Wilson J.R., Nori S., Kotter M.R.N., Druschel C., Curt A., Fehlings M. Traumatic spinal cord injury. Nat. Rev. Dis. Prim. 2017;3:17018. doi: 10.1038/nrdp.2017.18. [DOI] [PubMed] [Google Scholar]
- 6.Nas K. Rehabilitation of spinal cord injuries. World J. Orthop. 2015;6:8–16. doi: 10.5312/wjo.v6.i1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Longo M.R., Azañón E., Haggard P. More than skin deep: Body representation beyond primary somatosensory cortex. Neuropsychologia. 2010;48:655–668. doi: 10.1016/j.neuropsychologia.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 8.Cadotte D.W., Bosma R., Mikulis D., Nugaeva N., Smith K., Pokrupa R., Islam O., Stroman P.W., Fehlings M.G. Plasticity of the Injured Human Spinal Cord: Insights Revealed by Spinal Cord Functional MRI. PLoS ONE. 2012;7:e45560. doi: 10.1371/journal.pone.0045560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsubayashi K., Nagoshi N., Komaki Y., Kojima K., Shinozaki M., Tsuji O., Iwanami A., Ishihara R., Takata N., Matsumoto M., et al. Assessing cortical plasticity after spinal cord injury by using resting-state functional magnetic resonance imaging in awake adult mice. Sci. Rep. 2018;8:14406. doi: 10.1038/s41598-018-32766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Min Y.-S., Park J.W., Jin S.U., Jang K.E., Nam H.U., Lee Y.-S., Jung T.-D., Chang Y. Alteration of Resting-State Brain Sensorimotor Connectivity following Spinal Cord Injury: A Resting-State Functional Magnetic Resonance Imaging Study. J. Neurotrauma. 2015;32:1422–1427. doi: 10.1089/neu.2014.3661. [DOI] [PubMed] [Google Scholar]
- 11.Freund P., Weiskopf N., Ashburner J., Wolf K., Sutter R., Altmann D.R., Friston K., Thompson A., Curt A. MRI investigation of the sensorimotor cortex and the corticospinal tract after acute spinal cord injury: A prospective longitudinal study. Lancet Neurol. 2013;12:873–881. doi: 10.1016/S1474-4422(13)70146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hou J., Xiang Z., Yan R., Zhao M., Wu Y., Zhong J., Guo L., Li H., Wang J., Wu J., et al. Motor recovery at 6 months after admission is related to structural and functional reorganization of the spine and brain in patients with spinal cord injury. Hum. Brain Mapp. 2016;37:2195–2209. doi: 10.1002/hbm.23163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oni-Orisan A., Kaushal M., Li W., Leschke J., Ward B.D., Vedantam A., Kalinosky B., Budde M.D., Schmit B.D., Li S.-J., et al. Alterations in Cortical Sensorimotor Connectivity following Complete Cervical Spinal Cord Injury: A Prospective Resting-State fMRI Study. PLoS ONE. 2016;11:e0150351. doi: 10.1371/journal.pone.0150351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bunge R.P., Puckett W.R., Becerra J.L., Marcillo A., Quencer R.M. Observations on the pathology of human spinal cord injury. A review and classification of 22 new cases with details from a case of chronic cord compression with extensive focal demyelination. Adv. Neurol. 1993;59:75–89. [PubMed] [Google Scholar]
- 15.Bunge R.P., Puckett W.R., Hiester E.D. Observations on the pathology of several types of human spinal cord injury, with emphasis on the astrocyte response to penetrating injuries. Adv. Neurol. 1997;72:305–315. [PubMed] [Google Scholar]
- 16.Guest J., Hiester E., Bunge R. Demyelination and Schwann cell responses adjacent to injury epicenter cavities following chronic human spinal cord injury. Exp. Neurol. 2005;192:384–393. doi: 10.1016/j.expneurol.2004.11.033. [DOI] [PubMed] [Google Scholar]
- 17.Anderson A.J., Robert S., Huang W., Young W., Cotman C.W. Activation of Complement Pathways after Contusion-Induced Spinal Cord Injury. J. Neurotrauma. 2004;21:1831–1846. doi: 10.1089/neu.2004.21.1831. [DOI] [PubMed] [Google Scholar]
- 18.Grabher P., Blaiotta C., Ashburner J., Freund P. Relationship between brainstem neurodegeneration and clinical impairment in traumatic spinal cord injury. NeuroImage Clin. 2017;15:494–501. doi: 10.1016/j.nicl.2017.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grabher P., Callaghan M.F., Ashburner J., Weiskopf N., Thompson A., Curt A., Freund P. Tracking sensory system atrophy and outcome prediction in spinal cord injury. Ann. Neurol. 2015;78:751–761. doi: 10.1002/ana.24508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen Q., Zheng W., Chen X., Li X., Wang L., Qin W., Li K., Chen N. Reorganization of the somatosensory pathway after subacute incomplete cervical cord injury. NeuroImage Clin. 2019;21:101674. doi: 10.1016/j.nicl.2019.101674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bruehlmeier M., Dietz V., Leenders K.L., Roelcke U., Missimer J., Curt A. How does the human brain deal with a spinal cord injury? Eur. J. Neurosci. 1998;10:3918–3922. doi: 10.1046/j.1460-9568.1998.00454.x. [DOI] [PubMed] [Google Scholar]
- 22.Aguilar J., Humanes-Valera D., Calviño E.A., Yague J.G., Moxon K.A., Oliviero A., Foffani G. Spinal Cord Injury Immediately Changes the State of the Brain. J. Neurosci. 2010;30:7528–7537. doi: 10.1523/JNEUROSCI.0379-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jutzeler C.R., Huber E., Callaghan M.F., Luechinger R., Curt A., Kramer J.L.K., Freund P. Association of pain and CNS structural changes after spinal cord injury. Sci. Rep. 2016;6:18534. doi: 10.1038/srep18534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henderson L.A., Gustin S.M., Macey P.M., Wrigley P.J., Siddall P.J. Functional Reorganization of the Brain in Humans Following Spinal Cord Injury: Evidence for Underlying Changes in Cortical Anatomy. J. Neurosci. 2011;31:2630–2637. doi: 10.1523/JNEUROSCI.2717-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pan Y., Dou W.-B., Wang Y.-H., Luo H.-W., Ge Y.-X., Yan S.-Y., Xu Q., Tu Y.-Y., Xiao Y.-Q., Wu Q., et al. Non-concomitant cortical structural and functional alterations in sensorimotor areas following incomplete spinal cord injury. Neural Regen. Res. 2017;12:2059–2066. doi: 10.4103/1673-5374.221165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adams M.M., Hicks A.L. Spasticity after spinal cord injury. Spinal Cord. 2005;43:577–586. doi: 10.1038/sj.sc.3101757. [DOI] [PubMed] [Google Scholar]
- 27.Burchiel K.J., Hsu F.P.K. Pain and Spasticity After Spinal Cord Injury. Spine. 2001;26:S146–S160. doi: 10.1097/00007632-200112151-00024. [DOI] [PubMed] [Google Scholar]
- 28.Karlsson A.-K. Overview: Autonomic dysfunction in spinal cord injury: Clinical presentation of symptoms and signs. Glial Cell Funct. 2006;152:1–8. doi: 10.1016/s0079-6123(05)52034-x. [DOI] [PubMed] [Google Scholar]
- 29.Yoon E.J., Kim Y.K., Shin H.I., Lee Y., Kim S.E. Cortical and white matter alterations in patients with neuropathic pain after spinal cord injury. Brain Res. 2013;1540:64–73. doi: 10.1016/j.brainres.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 30.Gustin S.M., Wrigley P.J., Youssef A.M., McIndoe L., Wilcox S.L., Rae C.D., Edden R.A., Siddall P.J., Henderson L.A. Thalamic activity and biochemical changes in individuals with neuropathic pain after spinal cord injury. Pain. 2014;155:1027–1036. doi: 10.1016/j.pain.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao P., Hill M., Liu S., Chen L., Bangalore L., Waxman S.G., Tan A.M. Dendritic spine remodeling following early and late Rac1 inhibition after spinal cord injury: Evidence for a pain biomarker. J. Neurophysiol. 2016;115:2893–2910. doi: 10.1152/jn.01057.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park J., Zheng L., Acosta G., Vega-Alvarez S., Chen Z., Muratori B., Cao P., Shi R. Acrolein contributes to TRPA1 up-regulation in peripheral and central sensory hypersensitivity following spinal cord injury. J. Neurochem. 2015;135:987–997. doi: 10.1111/jnc.13352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meisner J.G., Marsh A.D., Marsh D.R. Loss of GABAergic Interneurons in Laminae I–III of the Spinal Cord Dorsal Horn Contributes to Reduced GABAergic Tone and Neuropathic Pain after Spinal Cord Injury. J. Neurotrauma. 2010;27:729–737. doi: 10.1089/neu.2009.1166. [DOI] [PubMed] [Google Scholar]
- 34.Lucci G., Pazzaglia M. Towards multiple interactions of inner and outer sensations in corporeal awareness. Front. Hum. Neurosci. 2015;9:9. doi: 10.3389/fnhum.2015.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Martino M.L., De Bartolo M., Leemhuis E., Pazzaglia M. Rebuilding Body–Brain Interaction from the Vagal Network in Spinal Cord Injuries. Brain Sci. 2021;11:1084. doi: 10.3390/brainsci11081084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Curt A., Alkadhi H., Crelier G.R., Boendermaker S.H., Hepp-Reymond M.-C., Kollias S.S. Changes of non-affected upper limb cortical representation in paraplegic patients as assessed by fMRI. Brain. 2002;125:2567–2578. doi: 10.1093/brain/awf250. [DOI] [PubMed] [Google Scholar]
- 37.Corbetta M., Burton H., Sinclair R.J., Conturo T.E., Akbudak E., McDonald J.W. Functional reorganization and stability of somatosensory-motor cortical topography in a tetraplegic subject with late recovery. Proc. Natl. Acad. Sci. USA. 2002;99:17066–17071. doi: 10.1073/pnas.262669099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li X., Chen Q., Zheng W., Chen X., Wang L., Qin W., Li K., Lu J., Chen N. Inconsistency between cortical reorganization and functional connectivity alteration in the sensorimotor cortex following incomplete cervical spinal cord injury. Brain Imaging Behav. 2019;14:2367–2377. doi: 10.1007/s11682-019-00190-9. [DOI] [PubMed] [Google Scholar]
- 39.Huynh V., Rosner J., Curt A., Kollias S., Hubli M., Michels L. Disentangling the Effects of Spinal Cord Injury and Related Neuropathic Pain on Supraspinal Neuroplasticity: A Systematic Review on Neuroimaging. Front. Neurol. 2020;10 doi: 10.3389/fneur.2019.01413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Widerström-Noga E., Cruz-Almeida Y., Felix E.R., Pattany P.M. Somatosensory phenotype is associated with thalamic metabolites and pain intensity after spinal cord injury. Pain. 2015;156:166–174. doi: 10.1016/j.pain.0000000000000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li X., Wang L., Chen Q., Hu Y., Du J., Chen X., Zheng W., Lu J., Chen N. The Reorganization of Insular Subregions in Individuals with Below-Level Neuropathic Pain following Incomplete Spinal Cord Injury. Neural Plast. 2020;2020:2796571. doi: 10.1155/2020/2796571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bors E. Phantom limbs of patients with spinal cord injury. AMA Arch. Neurol. Psychiatry. 1951;66:610–631. doi: 10.1001/archneurpsyc.1951.02320110075007. [DOI] [PubMed] [Google Scholar]
- 43.Pazzaglia M., Leemhuis E., Giannini A.M., Haggard P. The Homuncular Jigsaw: Investigations of Phantom Limb and Body Awareness Following Brachial Plexus Block or Avulsion. J. Clin. Med. 2019;8:182. doi: 10.3390/jcm8020182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pazzaglia M., Scivoletto G., Giannini A.M., Leemhuis E. My hand in my ear: A phantom limb re-induced by the illusion of body ownership in a patient with a brachial plexus lesion. Psychol. Res. 2018;83:196–204. doi: 10.1007/s00426-018-1121-5. [DOI] [PubMed] [Google Scholar]
- 45.Pazzaglia M., Galli G., Lucci G., Scivoletto G., Molinari M., Haggard P. Phantom limb sensations in the ear of a patient with a brachial plexus lesion. Cortex. 2019;117:385–395. doi: 10.1016/j.cortex.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 46.Diaz-Segarra N., McKay O., Kirshblum S., Yonclas P. Management of nonpainful supernumerary phantom limbs after incomplete spinal cord injury with visual–tactile feedback therapy: A case report. Spinal Cord Ser. Cases. 2020;6:1–6. doi: 10.1038/s41394-020-0312-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Muret D., Makin T.R. The homeostatic homunculus: Rethinking deprivation-triggered reorganisation. Curr. Opin. Neurobiol. 2021;67:115–122. doi: 10.1016/j.conb.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 48.Wang W., Xie W., Zhang Q., Liu L., Liu J., Zhou S., Shi J., Chen J., Ning B. Reorganization of the brain in spinal cord injury: A meta-analysis of functional MRI studies. Neuroradiology. 2019;61:1309–1318. doi: 10.1007/s00234-019-02272-3. [DOI] [PubMed] [Google Scholar]
- 49.Dimitrijević M.R. Residual motor functions in spinal cord injury. Adv. Neurol. 1988;47:138–155. [PubMed] [Google Scholar]
- 50.Wrigley P.J., Siddall P.J., Gustin S. New evidence for preserved somatosensory pathways in complete spinal cord injury: A fMRI study. Hum. Brain Mapp. 2018;39:588–598. doi: 10.1002/hbm.23868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Awad A., Levi R., Waller M., Westling G., Lindgren L., Eriksson J. Preserved somatosensory conduction in complete spinal cord injury: Discomplete SCI. Clin. Neurophysiol. 2020;131:1059–1067. doi: 10.1016/j.clinph.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 52.Melo M.C., Macedo D.R., Soares A.B. Divergent Findings in Brain Reorganization After Spinal Cord Injury: A Review. J. Neuroimaging. 2020;30:410–427. doi: 10.1111/jon.12711. [DOI] [PubMed] [Google Scholar]
- 53.Sharp K.G., Gramer R., Page S.J., Cramer S.C. Increased Brain Sensorimotor Network Activation after Incomplete Spinal Cord Injury. J. Neurotrauma. 2017;34:623–631. doi: 10.1089/neu.2016.4503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gao F., Guo Y., Chu H., Yu W., Chen Z., Chen L., Li J., Yang D., Yang M., Du L., et al. Lower-Limb Sensorimotor Deprivation-Related Brain Activation in Patients with Chronic Complete Spinal Cord Injury. Front. Neurol. 2020;11:555733. doi: 10.3389/fneur.2020.555733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Krings T., Naujokat C., Keyserlingk D.G.V. Representation of cortical motor function as revealed by stereotactic transcranial magnetic stimulation. Electroencephalogr. Clin. Neurophysiol. Mot. Control. 1998;109:85–93. doi: 10.1016/S0924-980X(97)00078-7. [DOI] [PubMed] [Google Scholar]
- 56.Fassett H.J., Turco C.V., El-Sayes J., Nelson A.J. Alterations in Motor Cortical Representation of Muscles Following Incomplete Spinal Cord Injury in Humans. Brain Sci. 2018;8:225. doi: 10.3390/brainsci8120225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Björkman A., Weibull A., Rosén B., Svensson J., Lundborg G. Rapid cortical reorganisation and improved sensitivity of the hand following cutaneous anaesthesia of the forearm. Eur. J. Neurosci. 2009;29:837–844. doi: 10.1111/j.1460-9568.2009.06629.x. [DOI] [PubMed] [Google Scholar]
- 58.Waters R., Moore K.R., Graboff S.R., Paris K. Brachioradialis to flexor pollicis longus tendon transfer for active lateral pinch in the tetraplegic. J. Hand Surg. 1985;10:385–391. doi: 10.1016/S0363-5023(85)80040-X. [DOI] [PubMed] [Google Scholar]
- 59.Wester K., Hove L.M., Barndon R., Craven A.R., Hugdahl K. Cortical Plasticity After Surgical Tendon Transfer in Tetraplegics. Front. Hum. Neurosci. 2018;12:234. doi: 10.3389/fnhum.2018.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Käll L.B., Fridén J., Björnsdotter M. Regional estimates of cortical thickness in brain areas involved in control of surgically restored limb movement in patients with tetraplegia. J. Spinal Cord Med. 2018;43:462–469. doi: 10.1080/10790268.2018.1535639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jain N., Catania K.C., Kaas J.H. Deactivation and reactivation of somatosensory cortex after dorsal spinal cord injury. Nat. Cell Biol. 1997;386:495–498. doi: 10.1038/386495a0. [DOI] [PubMed] [Google Scholar]
- 62.Jain N., Florence S.L., Qi H.-X., Kaas J.H. Growth of new brainstem connections in adult monkeys with massive sensory loss. Proc. Natl. Acad. Sci. USA. 2000;97:5546–5550. doi: 10.1073/pnas.090572597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jain N., Qi H.-X., Collins C.E., Kaas J.H. Large-Scale Reorganization in the Somatosensory Cortex and Thalamus after Sensory Loss in Macaque Monkeys. J. Neurosci. 2008;28:11042–11060. doi: 10.1523/JNEUROSCI.2334-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tandon S., Kambi N., Lazar L., Mohammed H., Jain N. Large-Scale Expansion of the Face Representation in Somatosensory Areas of the Lateral Sulcus after Spinal Cord Injuries in Monkeys. J. Neurosci. 2009;29:12009–12019. doi: 10.1523/JNEUROSCI.2118-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pons T.P., Garraghty P.E., Ommaya A.K., Kaas J.H., Taub E., Mishkin M. Massive Cortical Reorganization After Sensory Deafferentation in Adult Macaques. Science. 1991;252:1857–1860. doi: 10.1126/science.1843843. [DOI] [PubMed] [Google Scholar]
- 66.Pollin B., Albe-Fessard D. Organization of somatic thalamus in monkeys with and without section of dorsal spinal tracts. Brain Res. 1979;173:431–449. doi: 10.1016/0006-8993(79)90240-3. [DOI] [PubMed] [Google Scholar]
- 67.Garraghty P., Florence S., Kaas J. Ablations of areas 3a and 3b of monkey somatosensory cortex abolish cutaneous responsivity in area 1. Brain Res. 1990;528:165–169. doi: 10.1016/0006-8993(90)90213-U. [DOI] [PubMed] [Google Scholar]
- 68.Merzenich M.M., Nelson R.J., Stryker M.P., Cynader M.S., Schoppmann A., Zook J.M. Somatosensory cortical map changes following digit amputation in adult monkeys. J. Comp. Neurol. 1984;224:591–605. doi: 10.1002/cne.902240408. [DOI] [PubMed] [Google Scholar]
- 69.Florence S., Kaas J. Large-scale reorganization at multiple levels of the somatosensory pathway follows therapeutic amputation of the hand in monkeys. J. Neurosci. 1995;15:8083–8095. doi: 10.1523/JNEUROSCI.15-12-08083.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Garraghty P.E., Kaas J.H. Functional reorganization in adult monkey thalamus after peripheral nerve injury. NeuroReport. 1991;2:747–750. doi: 10.1097/00001756-199112000-00004. [DOI] [PubMed] [Google Scholar]
- 71.Lenz F.A., Kwan H.C., Martin R., Tasker R., Richardson R.T., Dostrovsky J.O. Characteristics of somatotopic organization and spontaneous neuronal activity in the region of the thalamic principal sensory nucleus in patients with spinal cord transection. J. Neurophysiol. 1994;72:1570–1587. doi: 10.1152/jn.1994.72.4.1570. [DOI] [PubMed] [Google Scholar]
- 72.Florence S.L., Taub H.B., Kaas J.H. Large-Scale Sprouting of Cortical Connections After Peripheral Injury in Adult Macaque Monkeys. Science. 1998;282:1117–1121. doi: 10.1126/science.282.5391.1117. [DOI] [PubMed] [Google Scholar]
- 73.Mikulis D.J., Jurkiewicz M.T., McIlroy W.E., Staines W.R., Rickards L., Kalsi–Ryan S., Crawley A.P., Fehlings M.G., Verrier M.C. Adaptation in the motor cortex following cervical spinal cord injury. Neurology. 2002;58:794–801. doi: 10.1212/WNL.58.5.794. [DOI] [PubMed] [Google Scholar]
- 74.Scandola M., Tidoni E., Avesani R., Brunelli G., Aglioti S.M., Moro V. Rubber hand illusion induced by touching the face ipsilaterally to a deprived hand: Evidence for plastic “somatotopic” remapping in tetraplegics. Front. Hum. Neurosci. 2014;8:404. doi: 10.3389/fnhum.2014.00404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moore C.I., Stern C.E., Dunbar C., Kostyk S., Gehi A., Corkin S. Referred phantom sensations and cortical reorganization after spinal cord injury in humans. Proc. Natl. Acad. Sci. USA. 2000;97:14703–14708. doi: 10.1073/pnas.250348997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Makin T., Bensmaia S. Stability of Sensory Topographies in Adult Cortex. Trends Cogn Sci. 2017;21:195–204. doi: 10.1016/j.tics.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Turner J., Lee J., Martinez O., Medlin A., Schandler S., Cohen M. Somatotopy of the motor cortex after long-term spinal cord injury or amputation. IEEE Trans. Neural Syst. Rehabil. Eng. 2001;9:154–160. doi: 10.1109/7333.928575. [DOI] [PubMed] [Google Scholar]
- 78.Lotze M., Laubis-Herrmann U., Topka H. Combination of TMS and fMRI reveals a specific pattern of reorganization in M1 in patients after complete spinal cord injury. Restor. Neurol. Neurosci. 2006;24:97–107. [PubMed] [Google Scholar]
- 79.Vaso A., Adahan H.-M., Gjika A., Zahaj S., Zhurda T., Vyshka G., Devor M. Peripheral nervous system origin of phantom limb pain. Pain. 2014;155:1384–1391. doi: 10.1016/j.pain.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 80.Cirstea C.M., Choi I.-Y., Lee P., Peng H., Kaufman C.L., Frey S.H. Magnetic resonance spectroscopy of current hand amputees reveals evidence for neuronal-level changes in former sensorimotor cortex. J. Neurophysiol. 2017;117:1821–1830. doi: 10.1152/jn.00329.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kambi N., Halder P., Rajan R., Arora V., Chand P., Arora M., Jain N. Large-scale reorganization of the somatosensory cortex following spinal cord injuries is due to brainstem plasticity. Nat. Commun. 2014;5:3602. doi: 10.1038/ncomms4602. [DOI] [PubMed] [Google Scholar]
- 82.Leemhuis E., De Gennaro L., Pazzaglia A.M. Disconnected Body Representation: Neuroplasticity Following Spinal Cord Injury. J. Clin. Med. 2019;8:2144. doi: 10.3390/jcm8122144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zantedeschi M., Pazzaglia M. Commentary: Non-invasive Brain Stimulation, a Tool to Revert Maladaptive Plasticity in Neuropathic Pain. Front. Hum. Neurosci. 2016;10:544. doi: 10.3389/fnhum.2016.00544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leemhuis E., Esposito R., Gennaro L., Pazzaglia M. Go Virtual to Get Real: Virtual Reality as a Resource for Spinal Cord Treatment. Int. J. Environ. Res. Public Health. 2021;18:1819. doi: 10.3390/ijerph18041819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Leemhuis E., Giuffrida V., Giannini A.M., Pazzaglia M.A. Therapeutic Matrix: Virtual Reality as a Clinical Tool for Spinal Cord Injury-Induced Neuropathic Pain. Brain Sci. 2021;11:1201. doi: 10.3390/brainsci11091201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pazzaglia M., Galli G., Lewis J.W., Scivoletto G., Giannini A.M., Molinari M. Embodying functionally relevant action sounds in patients with spinal cord injury. Sci. Rep. 2018;8:15641. doi: 10.1038/s41598-018-34133-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Scivoletto G., Galli G., Torre M., Molinari M., Pazzaglia M. The Overlooked Outcome Measure for Spinal Cord Injury: Use of Assistive Devices. Front. Neurol. 2019;10:272. doi: 10.3389/fneur.2019.00272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pazzaglia M., Molinari M. The re-embodiment of bodies, tools, and worlds after spinal cord injury: An intricate picture. Phys. Life Rev. 2016;16:191–194. doi: 10.1016/j.plrev.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 89.Pazzaglia M., Galli G. Loss of agency in apraxia. Front. Hum. Neurosci. 2014;8:751. doi: 10.3389/fnhum.2014.00751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pazzaglia M., Galli G. Action Observation for Neurorehabilitation in Apraxia. Front. Neurol. 2019;10:309. doi: 10.3389/fneur.2019.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pazzaglia M., Galli G. Translating novel findings of perceptual-motor codes into the neuro-rehabilitation of movement disorders. Front. Behav. Neurosci. 2015;9:222. doi: 10.3389/fnbeh.2015.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.