Abstract
This systematic review and meta-analysis evaluated the extent of sleep disturbances during the COVID-19 pandemic. Eleven databases and six preprint repositories were searched for the period from November 1, 2019, to July 15, 2021. The DerSimonian and Laird method was used to develop random-effect meta-analyses. Two hundred and fifty studies comprising 493,475 participants from 49 countries were included. During COVID-19, the estimated global prevalence of sleep disturbances was 40.49% [37.56; 43.48%]. Bayesian meta-analysis revealed an odds of 0.68 [0.59; 0.77] which translates to a rate of approximately 41%. This provides reassurance that the estimated rate using classical meta-analysis is robust. Six major populations were identified; the estimated prevalence of sleep problem was 52.39% [41.69; 62.88%] among patients infected with COVID-19, 45.96% [36.90; 55.30%] among children and adolescents, 42.47% [37.95; 47.12%] among healthcare workers, 41.50% [32.98; 50.56%] among special populations with healthcare needs, 41.16% [28.76; 54.79%] among university students, and 36.73% [32.32; 41.38%] among the general population. Sleep disturbances were higher during lockdown compared to no lockdown, 42.49% versus 37.97%. Four in every ten individuals reported a sleep problem during the COVID-19 pandemic. Patients infected with the disease, children, and adolescents appeared to be the most affected groups.
Keywords: Sleep disorder, Sleep disturbance, Pandemic, Insomnia, Sleep hygiene, Circadian rhythm
Abbreviations: AIS, Athens insomnia scale; Decimal, data extraction for complicated meta-analysis; DOI, digital object identification; GOSH, Graphic display of study heterogeneity; IPD, individual patient data; ISI, Insomnia severity index; MeSH, Medical Subjects Headings; NOS, Newcastle–Ottawa Scale; Prisma, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PSQI, Pittsburgh sleep quality index
Introduction
Because sufficient sleep is necessary for humans to sustain everyday functioning [1], numerous research studies of sleep disturbances were conducted during the COVID-19 pandemic, most using self-report data [2]. These studies have reported a range of results on the prevalence and associated factors of sleep disturbances during COVID-19 in various populations.
Several systematic reviews and meta-analyses examining the impact of COVID-19 on sleep disturbances have been conducted. The first review reported a systematic review and meta-analysis of the pooled prevalence rate of sleep disturbances during the COVID-19 pandemic [2]. The review concluded that the global prevalence of sleep disturbances was approximately 36%; the least affected group was the general population with a rate of 32%, followed by healthcare workers with a rate of 36%, and patients with COVID-19 were the most affected with a rate of 75% [2]. A more recent systematic review and meta-analysis estimated a similar prevalence of sleep disturbances among the general population, 31% [3] to the 32% initially reported by Jahrami and colleagues (2). Similar findings of healthcare workers were confirmed by two independent meta-analyses that reported a pool rate of 35% [4] and 38% [5]. Nurses appeared to have a slightly higher rate of sleep disturbances with a reported rate of 43% [6]. According to the same review, the adjusted pooled estimated prevalence of sleep disturbances was 24% for females and 27%, for males [3]. A review focused on children and adolescents reported a combined prevalence of any sleep disruption in children was 54% [7]. Furthermore, a high rate of sleep disturbances was reported among Chinese healthcare workers, with a reported rate of 45% [8]. Reviews of sleep disturbances in patients infected with COVID-19 produced heterogenous findings as follows 34% [9], 57% [10], and 75% [2].
In all previous systematic reviews and meta-analyses, heterogeneity or variation in study outcomes between studies was high despite efforts to control moderators using subgroup analysis or a meta-regression analysis. While results of moderator analyses resulted in better fit indices of heterogeneity; nonetheless, it remained high. Previous reviews typically controlled for one moderator at the time, and no review has attempted a multiple meta-regression analysis to correct for interaction between variables at the metadata level. Risk of bias assessment was examined coarsely as part of some of the previous systematic reviews and meta-analyses with findings presented as aggregate scores and not utilized to influence the synthesis of the studies' conclusions or to factor into the overall reliability evaluation of the evidence.
Ten previous systematic reviews and meta-analyses were performed and published before our review [∗[2], ∗[3], ∗[4], ∗[5], ∗[6], ∗[7], ∗[8], ∗[9], ∗[10], ∗[11]]; and were critically appraised as a preparatory step. While there is some value in independent replications of meta-analyses by different teams, the specific purpose of this review was not to perform an updated systematic review and meta-analysis but to fill identified gaps in previous multiple overlapping meta-analyses covering the topic of sleep disturbances during COVID-19. Several important information gaps were identified in evaluating the previously published reviews. First, seven out of ten were narrowly focused on a single population, mainly healthcare workers [∗[4], ∗[5], ∗[6],8,11], children and adolescents [7], or patients with COVID-19 [9]. Therefore, several significant populations were missed, for example, university students or those with medical comorbidities. Second, previous studies that focused on healthcare workers did not control for the line of work, i.e., frontline healthcare workers vs. non-frontline healthcare workers. Thus, it remained unknown if the proportion of frontline healthcare workers in the analyzed study or nursing staff (as the primary direct care providers) during the pandemic will affect the reported estimated rate. Third, previous work examined the role of lockdown during the COVID-19 pandemic and reported an association between lockdown status, per se, and prevalence of sleep disturbances [10] but did not explicitly quantify or report the magnitudes of sleep disturbances during lockdown compared to no lockdown. Accordingly, neither lockdown status nor the year of publication as a proxy for the longitudinal effect were analyzed or reported in previously published studies. Finally, all previously published reviews relied exclusively on classical meta-analytic techniques. Consequently, statistical approaches (e.g., Bayesian analysis) guided by combining prior information about what is already known with data in a new sample were not previously utilized to ensure the stability of results.
Given the now large number of published studies on the topic, the current systematic review was designed and conducted to estimate the raw and weighted prevalence rates of sleep disturbances during the pandemic taking into account the effect of a single moderator and simultaneous interaction of several moderators on the prevalence of sleep disorders in diverse populations. The findings provide a more precise prevalence estimate of sleep disturbances during COVID-19 across multiple at-risk populations and may aid in the development of customized screening and intervention techniques to reduce the harmful consequences of these sleep disturbances.
Methodology
Registration and protocol
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Prisma) criteria were used to design and perform this systematic review and meta-analysis [12]. The protocol was registered into the PROSPERO International Prospective Register of Systematic Reviews (Prospero) database (Registration number: CRD42021268440). Before registering our protocol, a careful review of the Prospero and the COVID-19 evidence network to support decision-making (COVID-END) resources was performed to verify if a similar systematic review already existed to avoid duplication.
Search strategy
Eleven electronic academic databases (American Psychological Association PsycINFO; Cochrane Library; Cumulative Index to Nursing and Allied Health Literature (CINAHL); EBSCOhost Research Platform; Embase; Google Scholar; MEDLINE; ProQuest Medical; ScienceDirect; Scopus; and Web of Science were searched systematically between November 1, 2019 and July 15, 2021. Additionally, the COVID-19 Global literature on coronavirus disease database by World Health Organization was also searched to cover six preprint repositories (arXiv.org; biorxiv.org; medRxiv.org; Preprints.org; psyarxiv.com; and SSRN.com) for publications that have been peer-reviewed and accepted but not yet indexed. There was no limit on the language used.
The search strategy involved crossmatching keywords selected based on key terms and the PubMed Medical Subjects Headings (MeSH). The Boolean logic operators of (OR, AND, NOT) were used to develop the search in an [All Fields] search. Each database's advanced search characteristics were used to change the search syntax. In the search, the following keywords were used: “COVID-19″ OR “2019-nCoV” OR “2019 coronavirus” OR “Wuhan coronavirus” OR “2019 novel coronavirus” OR “SARS-CoV-2” AND “sleep” OR “sleep medicine” OR “sleep disturbances” OR “sleep disorders” OR “sleep problems” OR “polysomnography” OR “sleep quality” OR “PSQI” OR “Pittsburg Sleep Quality Index” OR “insomnia” OR “circadian rhythm” OR “restless leg syndrome” OR “sleep apnea” OR “narcolepsy” OR “daytime dysfunction” OR “daytime sleepiness” OR “ESS” or “Epworth Sleepiness Scale” AND “prevalence” OR “incidence” OR “epidemiology” OR “rate” OR “frequency” OR “risk factors” OR “interventions” OR “treatment” OR “therapy” OR “management”.
To enhance the chance of obtaining relevant original studies, the reference lists of included studies and previous systematic reviews and meta-analyses of published articles were manually searched.
Finally, the final search results were converted into a Microsoft Excels spreadsheet 2019 to filter and eliminate duplicates. Research Information Systems, incorporated files were saved to manage the citations using EndNote X9.3.3.
Inclusion and exclusion criteria
The magnitude of sleep disturbances during the COVID-19 pandemic was the primary outcome of the current meta-analysis. As a result, we included: First, all observational studies that looked at the impact of COVD-19 on sleep quantity and quality in a variety of groups, including the general population, healthcare workers, COVD-19-infected patients, children and adolescents, university students, and people with special healthcare needs (e.g., pregnant women or people with chronic medical conditions). Second, studies that reported numerical values of the prevalence of sleep disturbances expressed in event counts and total sample size. We used an artificial intelligence application - WebPlotDigitizer [13] - to obtain the underlying numerical data, reverse plots of data visualizations if they were not reported in the text of the original studies. Third, only English language, peer-reviewed studies published between November 1, 2019, and July 15, 2021, were included.
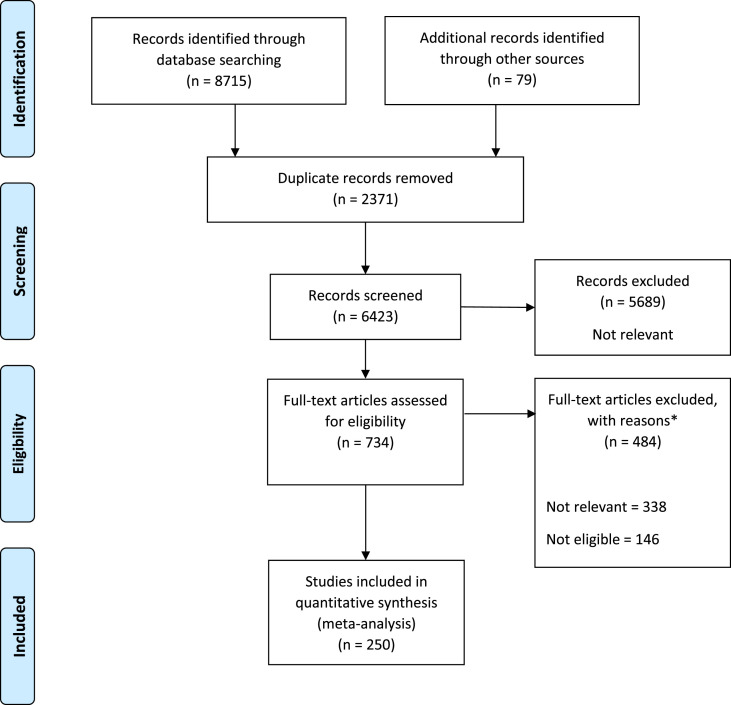
There were no restrictions on the characteristics of the participants. Abstracts, case reports, editorials, infographics, letters, narrative reviews, opinions, position statements, and systematic reviews and meta-analyses were excluded from the retrieved articles. Fig. 1 shows the Prisma flow diagram for study selection.
Fig. 1.
PRISMA flow diagram of study inclusion.
Outcomes
The primary outcome was the estimated prevalence of sleep disturbances during the COVID-19 pandemic. Sleep disturbances refer to a group of disturbances characterized by trouble falling or staying asleep, which can result in excessive drowsiness throughout the day as a result of sleep deprivation or change in terms of quantity, quality, or timing [10]. Sleep disturbances as an outcome had to be measured with valid and reliable psychometric instruments or validated with established cut-off points before being labeled as such. For example, on the Pittsburgh sleep quality index [14], a global score of five or above indicates poor sleep quality indicative of a “sleep problem”.
Study screening and selection
In the first phase, two reviewers independently evaluated the title and abstract of all retrieved publications based on the inclusion criteria (HJ, AH, AFA, FFR). Based on the aforementioned criteria, the complete texts of possibly relevant papers were studied further. Relevant studies were chosen during this procedure. Disagreements between reviewers were addressed by a third member of the study team (AB) through discussion and consensus.
Data extraction
The recommendations for data extraction for complicated meta-analysis (Decimal) [15] were used to design data extraction for this review. To extract data from the studies that were included, a pre-designed electronic form was created in a Microsoft Excel Spreadsheet. To facilitate the work of geographically dispersed researchers, the form was available live online within a secure, shared workspace for the extraction team members.
Study information, epidemiological findings, and the article's reference were all part of the data extraction process. The research information included the last author, year of publication, country of origin, kind of study, study goals, sample size, recruitment strategy, and basic sample characteristics such as mean age and proportion of females. The prevalence rate for sleep quality (count of events and sample size) and other noteworthy findings were the epidemiological findings. The complete citation information of the publication, including the digital object identification (DOI), was provided in the citation. We contacted the corresponding authors for clarifications and to seek more information when necessary. Each entry was extracted by two reviewers independently (OH, AH, AFA, FFR) and was matched by (ZS); discrepancies/disagreements between reviewers were settled through discussion and consensus with a third author (HJ).
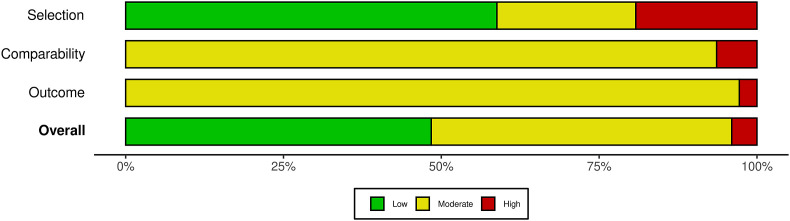
Quality assessment and risk of bias
The Newcastle–Ottawa Scale (NOS) was used to evaluate the methodological quality and assess the risk of bias of the studies included in the current review. The NOS checklist was used to look at three aspects (participants selection, comparability, and outcome and statistics). There are three variants of the checklist: for cross-sectional studies (seven items), for case–control studies (eight items), and for cohort or longitudinal studies (eight items). NOS is based on a star rating system, with each study receiving a maximum of nine stars (cross-sectional and cohort studies) or ten stars (case–control studies). A study with a score ≥8 has good quality and low risk of bias, a score of 5–7 has moderate quality and moderate risk of bias), and a score of 0–4 has low quality and high risk of bias [16]. Based on this quality ranking, no studies were eliminated. On the other hand, subgroup analysis was used to examine the impact of quality on the pooled effect size. Quality evaluation was done in parallel with data extraction by the same researchers, and the quality score for each study was determined using a consensus method.
Quality assessment results are presented visually using the traffic light plot, which tabulates the judgment for each study in each area of the NOS. A summary plot (weighted) was also created to depict the proportion of information within each judgment for each domain for all studies.
Data analysis
Because the studies included were of diverse populations, a random effect model was used to account for both within-study and between-study variations. Our meta-analysis utilized the general inverse variance approach [17], the logit transformed proportions, and corresponding standard errors with the DerSimonian and Laird estimates of effect size [18]. Clopper-Pearson interval was used for the 95% confidence interval calculation [19]. The I 2 statistic was used to quantify the variability of sample size impact estimates across these investigations [20]. The I 2 statistic indicates how much variance between research is attributable to heterogeneity rather than chance [21]. Heterogeneity is classified as 1) mild when the I 2 is less than 25%, 2) moderate when the I 2 is 25–50%, 3) severe when the I 2 is 50–75%, and 4) extremely severe when the I 2 is higher than 75% [21].
Cochran's Q test [22] and τ2 [23] statistics were used to determine the degree of heterogeneity between the studies. The weighted sum of squared differences between individual study effects and the pooled effect across studies was computed as Cochran's Q, with the weights being those used in the pooling technique [22]. The chi-square statistic with k (number of studies) minus 1 degree of freedom was used to distribute Q [22]. The τ2 statistic is the variation of effect size parameters across all studies in a population, and it represents the variance of real effect sizes; τ refers to the square root of this integer. To further examine heterogeneity, the H statistic was defined as the ratio of the standard deviation of a random-effects meta-analysis' estimated overall effect size to the standard deviation of a fixed-effects meta-analysis [20].
In our meta-analysis, the Baujat plot was employed to investigate heterogeneity [24]. Each study's contribution to the total heterogeneity statistic is displayed on the x-axis. The standardized difference of the total prevalence of sleep disturbances with and without each study is displayed on the y-axis; this amount represents the impact of each study on the overall treatment effect.
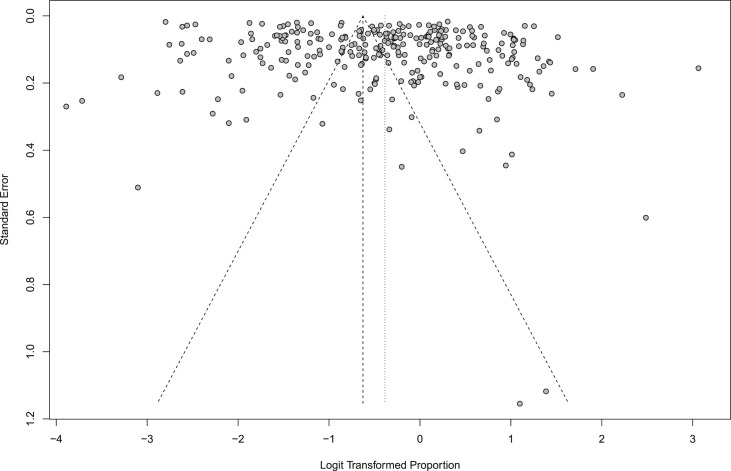
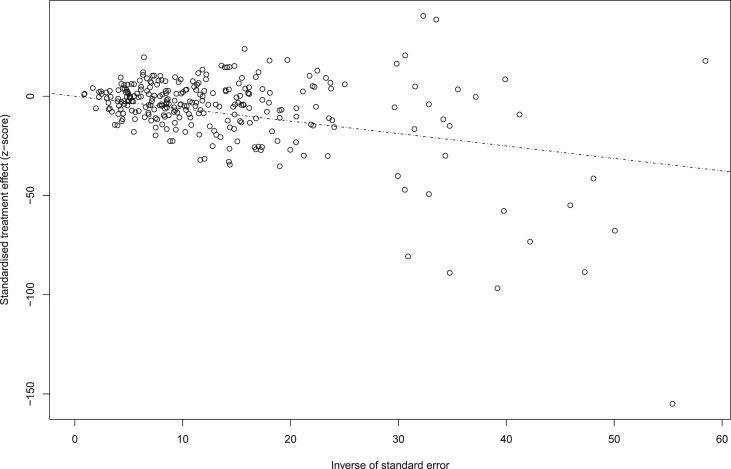
The findings of meta-analyses are plotted as a point estimate with 95% confidence intervals in a forest plot [25]. A jackknife approach was used to establish that no single study drove our findings by doing a leave-one-out sensitivity analysis [26]. The inclusion of outliers and influential studies may compromise the validity and robustness of the meta-analysis results. Thus, outliers were identified and removed. An outlier is labeled if the study's confidence interval does not coincide with the pooled effect's confidence interval [27]. Funnel plots were used as a visual approach to examine publication bias [28]. A funnel plot is a basic scatter plot of individual study intervention effect estimates versus some metric of study size or precision. The impact estimates are plotted on the horizontal scale, with the study size measured on the vertical axis, as with forest plots. This is the polar opposite of traditional scatter plot graphical presentations, which exhibit the result (e.g., effect size) on the vertical axis and the covariate (e.g., study size) on the horizontal axis [28]. Kendall's τ rank-order correlations [29] and Egger's regression [30] were used to analyze publication bias in a formal way. The use of Duval and Tweedie's trim and fill technique [31] to produce modified point estimates to account for funnel plot asymmetry due to possible publication bias was planned a priori. Because the most extreme findings on one side of the funnel plot are suppressed, the technique may be used to estimate the number of studies missing from a meta-analysis [31]. The technique then adds data to the funnel plot to make it more symmetric. The approach should not be thought of as a way to get a more valid assessment of the overall effect or outcome, but rather as a tool to see how sensitive the results are to one specific selection process [31]. The adjusted prevalence rate was reported if both Kendall's τ rank order correlation and Egger's regression were significant.
The p-curve approach, which focuses on p-values as the major driver of publication bias, was used to determine whether there is a real impact behind our meta-analysis data and to estimate its size [32,33]. Importantly, unlike small-study impact approaches, it accounts for dubious research procedures such as p-hacking. Graphic display of study heterogeneity (GOSH) plots was also utilized as a diagnostic plot to examine effect size heterogeneity [34]. Within the modeled data, GOSH charts make it easier to find outliers as well as clear homogenous groupings [34].
To explain the dispersion of effect sizes or heterogeneity, a moderator analysis was done. Because estimates of the prevalence of sleep disturbances differ depending on the types of populations studied, subgroup meta-analyses were performed to see if sleep disorders in each of the groups had an impact on the overall pooled estimate. Subgroup analysis was used to look at variations between groups based on categorical factors, such as the study population and the research measure. When three or more studies were available for analysis, subgroup analysis was conducted, and results were presented. We reported subgroup analysis based on country, population, used sleep measure, lockdown status, year of publication (time effect), research design, and quality assessment. The different aspects of sleep disturbances described, such as insomnia or sleep quality, were analyzed and presented separately according to the sleep measurement tool utilized in the included studies. The primary two disturbances reported were poor sleep quality measured using the Pittsburgh sleep quality index (PSQI); and insomnia measured using the insomnia severity index (ISI), the Athens insomnia scale (AIS).
For countries, we reported results if ≥ 10 studies were available for a given country. Special populations were defined as pregnant women, the elderly, and individuals with chronic diseases. Healthcare workers include physicians, nurses, emergency medical personnel, dental professionals, diagnostics professionals, pharmacists, and administrative staff. Those personnel in organizations committed to the assessment, quarantine, isolation, and treatment of established COVID-19 cases are designated as frontline healthcare workers in our analysis.
We utilized meta-regression approaches to look for continuous variables of sleep difficulties; we used four covariates, mean age, female sex proportion, front-line staff proportion (for studies involving healthcare workers) and proportion of nurses (for studies involving healthcare workers), and the interaction term of the proportion of nurses working on the front-line (for studies involving healthcare workers).
To further strengthen the results of the classical meta-analysis, Bayesian meta-analysis was also conducted. Meta-analysis using Bayesian methods has some advantages over many classical methods [35]. First, the analysis naturally considers the imprecision of the estimated between-study variance estimates [35]. Second, the analysis includes the impact of data on people's beliefs [20]. Finally, the analysis includes external evidence, such as information about the effects of interventions or likely differences between studies. Bayesian meta-analysis uses the Bayesian hierarchical model [36]. As with the conventional random-effects model, this model relies on the same basic assumptions [36]. There is a difference, however, in that prior distribution (informative, weakly informative, or uninformative) is assumed for μ and . The prior distribution describes the uncertainty surrounding a particular effect measure within a meta-analysis, such as the odds ratio or the mean difference [36]. There may be subjective beliefs about the size of the effect, or it may be based on sources of evidence excluded from the meta-analysis, such as non-randomized studies. Quantity uncertainty is reflected by the width of the prior distribution [37]. It is possible to use a ‘non-informative prior when there is little or no available information, in which all values are equally likely [37]. Meta-analysis likelihood summarizes both the data from included studies and the model of the meta-analysis (assuming random effects) [35,37].
All data analyses and visualizations were performed using R for statistical computing version 4.1.0 [38]. The packages ‘meta’ [39] and ‘metafor’ [40] were used to perform all meta-analytics. The package ‘bayesmeta’ [41] was used to perform Bayesian meta-analysis. Quality assessment plots were produced using risk-of-bias visualization ‘robvis’ [42].
Role of the funding source
No governmental, commercial, or non-profit sector has provided support for this systematic review and meta-analysis.
Results
Features of the studies included
The search was performed for the period between November 1, 2019, and July 15, 2021. Through electronic database searches and other sources, a total of 8715 records were identified. There were 6771 records left after duplicates were removed. A total of 734 prospective articles were evaluated in their entirety. Narrative and systematic reviews, editorials, comments, letters to the editor, position statements, irrelevant literature, duplicates, and incorrectly categorized publications were among the 485 papers eliminated. The search procedure is depicted in Fig. 1 using the PRISMA flowchart.
A total of 250 studies [285 subgroups, i.e., multiple populations, multiple tools, or multiple data points] comprising 493,475 participants from 49 countries were included in the analyses [[43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110], [111], [112], [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135], [136], [137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150], [151], [152], [153], [154], [155], [156], [157], [158], [159], [160], [161], [162], [163], [164], [165], [166], [167], [168], [169], [170], [171], [172], [173], [174], [175], [176], [177], [178], [179], [180], [181], [182], [183], [184], [185], [186], [187], [188], [189], [190], [191], [192], [193], [194], [195], [196], [197], [198], [199], [200], [201], [202], [203], [204], [205], [206], [207], [208], [209], [210], [211], [212], [213], [214], [215], [216], [217], [218], [219], [220], [221], [222], [223], [224], [225], [226], [227], [228], [229], [230], [231], [232], [233], [234], [235], [236], [237], [238], [239], [240], [241], [242], [243], [244], [245], [246], [247], [248], [249], [250], [251], [252], [253], [254], [255], [256], [257], [258], [259], [260], [261], [262], [263], [264], [265], [266], [267], [268], [269], [270], [271], [272], [273], [274], [275], [276], [277], [278], [279], [280], [281], [282], [283], [284], [285], [286], [287], [288], [289], [290], [291], [292]]. The countries included Argentina (K = 3), Australia (K = 3), Austria (K = 1), Bahrain (K = 1), Bangladesh (K = 4), Belgium (K = 1), Brazil (K = 7), Canada (K = 5), China (K = 84), Colombia (K = 2), Cyprus (K = 1), Egypt (K = 6), Ethiopia (K = 2), Finland (K = 1), France (K = 4), Germany (K = 2), Greece (K = 5), India (K = 16), Indonesia (K = 2), Iran (K = 3), Iraq (K = 2), Israel (K = 2), Italy (K = 34), Jordan (K = 2), Kuwait (K = 1), Libya (K = 1), Mali (K = 1), Morocco (K = 2), Multicountry (K = 17), México (K = 1), Nepal (K = 2), Netherlands (K = 1), Nigeria (K = 1), Oman (K = 3), Pakistan (K = 1), Poland (K = 2), Qatar (K = 2), Russia (K = 1), Saudi Arabia (K = 10), Slovenia (K = 1), Spain (K = 10), Sweden (K = 1), Taiwan (K = 1), Thailand (K = 1), Tunis (K = 2), Turkey (K = 12), UK (K = 2), USA (K = 15), and Vietnam (K = 1). A total of 249 (99.60%) of the studies collected data online; only one study used a telephone survey and aimed to include the elderly [123]. In 139 (55.60%) studies the data were obtained during the specific countries' national lockdown periods. In terms of included studies, the top three countries were China, Italy, India with (84, 33.60%), (34, 13.60%), and (16, 6.40%), respectively.
The mean sample size was 1804 [95%CI 1237; 2376 participants]. Participants were mainly females 64% [95%CI 62%; 66%], and the mean age of participants was 35 years [95%CI 33; 37 years]. A total of six participants grouping clusters were identified: general population 98 (39%), healthcare workers 84 (34%), special population 22 (9%), university students 18 (7%), COVID-19 patients 15 (6%), and children and adolescents 13 (5%). Participants from the healthcare workers included: 37% [95%CI 28%; 45%] from the frontline workforce, and 40% [95%CI 32%; 47%] were from nursing staff only. Cross-sectional design 229 (91%) was the most common, followed by longitudinal 12 (5%) or case–control 9 (4%) designs. Sleep disturbances were assessed using a variety of measures; the most common were: the PSQI, 95 (38%) of the studies, the ISI 94 (37.60%) of the studies, the AIS 12 (4.80%) of the studies, and other sleep measures 49 (19.60%) of the remaining studies. A prevalence rate was calculated as the number of people with sleep disturbances divided by all the individuals in a sample. All studies were published after March 2020, and 93 (37%) were released in 2021. Studies published in 2020 and 2021 did not differ significantly in terms of populations, P = 0.32, or used research design, P = 0.90. However, studies published in 2021 compared to those published in 2020 were mostly during lockdown periods P = 0.001 and relied mainly on the PSQI as a research measure P = 0.001. Furthermore, more studies in 2021 came from the countries that did not publish in 2020, P = 0.002. The mean NOS quality score was 7.10 ± 1.12 and ranged from 4.0 to 8.0. Detailed examination of quality assessment for each study included in the meta-analysis is presented in Fig. S1. Summary results indicate that 95% of the studies were of high or moderate quality. According to Fig. 2 , most of the risk bias is observed in the selection dimension, specifically regarding the sample size and representativeness of the sample. The summary features of all included studies are listed in Table 1 .
Fig. 2.
The summary risk of bias plot of included studies.
Table 1.
Key features, methodologies, and measures of studies that were included in this review about sleep disturbances during COVID-19.
| ID | Authors, year (Ref.) | Country | Lockdown Period | Population | Methodology | Measuresa | Quality scoreb |
|---|---|---|---|---|---|---|---|
| 1 | Abbas et al., 2021 [43] | Kuwait | Yes | Healthcare workers [Frontline = 64.98%, Nurses = 0%] | Cross-sectional design, N = 217, Female = 43.8%, Age = 35.8 years. | PSQI | 5 |
| 2 | Abdellah et al., 2021 [44] | Multi | Yes | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 344, Female = 71.5%, Age = 35.6 years. | PSQI | 7 |
| 3 | Abdulah et al., 2020 [45] | Iraq | No | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 268, Female = 29.9%, Age = 35.1 years. | AIS | 8 |
| 4 | Agberotimi et al., 2020 [46] | Nigeria | Yes | General Population | Cross-sectional design, N = 884, Female = 45.5%, Age = 28.8 years. | ISI | 8 |
| 5 | Ahmad et al., 2020 [47] | India | Yes | General Population | Cross-sectional design, N = 393, Female = 47.2%, Age = 30.3 years. | SD | 6 |
| 6 | Akıncı et al., 2021 [48] | Turkey | No | COVID-19 patients | Cross-sectional design, N = 189, Female = 41%, Age = 46.3 years. | PSQI | 7 |
| 7 | Al Ammari et al., 2021 [49] | Saudi Arabia | No | Healthcare workers [Frontline = 27.78%, Nurses = 36.39%] | Cross-sectional design, N = 720, Female = 64.2%, Age = 18–40 years. | ISI | 8 |
| 8 | Al Maqbali et al., 2021 [50] | Oman | Yes | Healthcare workers [Frontline = 81.4%, Nurses = 100%] | Cross-sectional design, N = 1130, Female = 91.2%, Age = 36.9 years. | PSQI | 7 |
| 9 | Al-Ajlouni et al., 2020 [51] | Jordan | Yes | General Population | Cross-sectional design, N = 1240, Female = 47.1%, Age = 37.4 years. | PSQI | 7 |
| 10 | Alamrawy et al., 2021 [52] | Egypt | No | General Population | Cross-sectional design, N = 447, Female = 70.2%, Age = 20.7 years. | ISI | 8 |
| 11 | AlAteeq et al., 2021 [53] | Saudi Arabia | Yes | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 1313, Female = 44.2%, Age = 34.8 years. | ISI | 7 |
| 12 | Alessi et al., 2020 [54] | Brazil | No | Special Population | Cross-sectional design, N = 120, Female = 55.8%, Age = 54.8 years. | MSQ | 6 |
| 13 | Alfonsi et al., 2021 [55] | Italy | Yes | General Population | Longitudinal design, N = 217, Female = 72%, Age = 35.7 years. | PSQI | 7 |
| 14 | Alharbi et al., 2021 [56] | Saudi Arabia | Yes | General Population | Cross-sectional design, N = 790, Female = 53.1%, Age = 40–60 years. | PSQI, AIS | 7 |
| 15 | Ali et al., 2021 [57] | Bangladesh | No | Healthcare workers [Frontline = 4.1%, Nurses = 9.5%] | Cross-sectional design, N = 294, Female = 43.5%, Age = 28.9 years. | ISI | 5 |
| 16 | Almater et al., 2020 [58] | Saudi Arabia | No | Healthcare workers [Frontline = 64.5%, Nurses = 0%] | Cross-sectional design, N = 107, Female = 43.9%, Age = 32.9 years. | ISI | 6 |
| 17 | Alnofaiey et al., 2020 [59] | Saudi Arabia | No | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 462, Female = 49.1%, Age = 20–60 years. | PSQI | 8 |
| 18 | Alomayri et al., 2020 [60] | Saudi Arabia | No | Special Population | Cross-sectional design, N = 400, Female = 86%, Age = 18–55 years. | PSQI | 8 |
| 19 | Alqahtani et al., 2021 [61] | Saudi Arabia | Yes | General Population | Cross-sectional design, N = 593, Female = 42.3%, Age = 36.5 years. | PSQI | 7 |
| 20 | AlRasheed et al., 2021 [62] | Saudi Arabia | Yes | General Population | Cross-sectional design, N = 344, Female = 63%, Age = 27.5 years. | PSQI | 7 |
| 21 | Alshekaili et al., 2020 [63] | Oman | Yes | Healthcare workers [Frontline = 50.4%, Nurses = 39.5%] | Cross-sectional design, N = 1139, Female = 80%, Age = 36.3 years. | ISI | 7 |
| 22 | Ammar et al., 2020 [64] | Multi | No | General Population | Longitudinal design, N = 1047, Female = 53.8%, Age = 18–55 years. | PSQI | 8 |
| 23 | Amra et al., 2021 [65] | Iran | Yes | Healthcare workers [Frontline = 0%, Nurses = 65.1%] | Cross-sectional design, N = 372, Female = 65.8%, Age = 34.5 years. | PSQI, ISI | 7 |
| 24 | Assenza et al., 2020 [66] | Italy | No | General Population | Cross-sectional design, N = 928, Female = 74.5%, Age = 18–86 years. | PSQI | 8 |
| 25 | Atas et al., 2021 [67] | Turkey | Yes | Special Population | Cross-sectional design, N = 106, Female = 38.7%, Age = 44.2 years. | PSQI, ISI | 5 |
| 26 | Bacaro et al., 2020 [68] | Italy | Yes | General Population | Cross-sectional design, N = 1989, Female = 76.2%, Age = 38.4 years. | ISI | 8 |
| 27 | Badellino et al., 2020 [69] | Argentina | No | General Population | Cross-sectional design, N = 1985, Female = 75.9%, Age = 36.8 years. | PSQI | 8 |
| 28 | Bai et al., 2020 [70] | China | Yes | Healthcare workers [Frontline = 0%, Nurses = 74.6%] | Cross-sectional design, N = 118, Female = 63.6%, Age = 33.1 years. | PSQI | 5 |
| 29 | Bajaj et al., 2020 [71] | India | Yes | General Population | Cross-sectional design, N = 391, Female = 53.5%, Age = 19–41 years. | ISI | 8 |
| 30 | Barrea et al., 2020 [72] | Italy | Yes | General Population | Longitudinal design, N = 121, Female = 64.5%, Age = 44.9 years. | PSQI | 6 |
| 31 | Barua et al., 2021 [73] | Bangladesh | No | Healthcare workers [Frontline = 100%, Nurses = 0%] | Cross-sectional design, N = 370, Female = 39.7%, Age = 30.5 years. | SCI-02 | 8 |
| 32 | Baskan et al., 2021 [74] | Turkey | Yes | General Population | Cross-sectional design, N = 1909, Female = 69%, Age = 31.9 years. | PSQI | 7 |
| 33 | Beck et al., 2020 [75] | France | Yes | General Population | Cross-sectional design, N = 1005, Female = 52%, Age = NR years. | SD | 6 |
| 34 | Benham et al., 2020 [76] | USA | Yes | University Students | Longitudinal, N = 1222, Female = 69%, Age = 21.3 years. | PSQI, ISI | 7 |
| 35 | Bezerra et al., 2020 [77] | Brazil | Yes | General Population | Cross-sectional design, N = 3836, Female = 73.5%, Age = 18-7 years. | SD | 6 |
| 36 | Bhat et al., 2020 [78] | India | No | General Population | Cross-sectional design, N = 264, Female = 27.7%, Age = 18–60 years. | PSQI | 8 |
| 37 | Bigalke et al., 2020 [79] | USA | Yes | General Population | Cross-sectional design, N = 103, Female = 59%, Age = 38 years. | PSQI | 6 |
| 38 | Blekas et al., 2020 [80] | Greece | No | Healthcare workers [Frontline = 0%, Nurses = 50%] | Cross-sectional design, N = 270, Female = 73.7%, Age = 18–75 years. | AIS | 8 |
| 39 | Bohlken et al., 2020 [81] | Germany | Yes | General Population | Cross-sectional design, N = 396, Female = NR%, Age = 23.9 years. | SD | 6 |
| 40 | Brito-Marques et al., 2021 [82] | Brazil | Yes | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 332, Female = 68.4%, Age = 36 years. | PSQI | 6 |
| 41 | Caballero-Domínguez et al., 2020 [83] | Colombia | Yes | General Population | Cross-sectional design, N = 700, Female = 68%, Age = 37.1 years. | AIS | 8 |
| 42 | Cai et al., 2020 [84] | China | No | Healthcare workers [Frontline = 50%, Nurses = 50%] | Case-Control design, N = 2346, Female = 70%, Age = 30.6 years. | ISI | 8 |
| 43 | Cai et al., 2020 [85] | China | No | Healthcare workers [Frontline = 45.9%, Nurses = 100%] | Cross-sectional design, N = 1330, Female = 97%, Age = 18–40 years. | ISI | 8 |
| 44 | Casagrande et al., 2020 [86] | Italy | No | General Population | Cross-sectional design, N = 2291, Female = 74.6%, Age = 18–50 years. | PSQI | 8 |
| 45 | Cellini et al., 2021 [87] | Italy | No | General Population Children and Adolescents |
Cross-sectional design, N = 299, Female = 100%, Age = 40.1 years. Cross-sectional design, N = 299, Female = 46.5%, Age = 8.0 years. |
PSQI SDSC |
8 |
| 46 | Cellini et al., 2020 [88] | Italy | Yes | COVID-19 patients | Cross-sectional design, N = 1310, Female = 67.2%, Age = 23.9 years. | PSQI | 8 |
| 47 | Cellini et al., 2021 [89] | Multi | No | General Population | Cross-sectional design, N = 2272, Female = 73.9%, Age = 38.6 years. | PSQI | 8 |
| 48 | Chatterjee et al., 2021 [90] | India | Yes | Healthcare workers [Frontline = 0%, Nurses = 32.9%] | Cross-sectional design, N = 140, Female = 56.7%, Age = 37.7 years. | ISI | 7 |
| 49 | Chen et al., 2021 [91] | China | No | Special Population | Cross-sectional design, N = 834, Female = 100%, Age = NR years. | ISI | 8 |
| 50 | Cheng et al., 2020 [92] | China | No | Healthcare workers [Frontline = 0%, Nurses = 45.88%] | Cross-sectional design, N = 534, Female = 82.4%, Age = 20–50 years. | PSQI | 8 |
| 51 | Cheng et al., 2021b [93] | Multi | No | General Population | Cross-sectional design, N = 2278, Female = 53.5%, Age = NR years. | PROMIS | 8 |
| 52 | Chi et al., 2021 [94] | China | No | Children and Adolescents | Cross-sectional design, N = 1794, Female = 43.9%, Age = 15.3 years. | YSIS | 8 |
| 53 | Chouchou et al., 2021 [95] | France | No | General Population | Cross-sectional design, N = 400, Female = 58.3%, Age = 29.8 years. | PSQI | 8 |
| 54 | Coiro et al., 2021 [96] | Multi | Yes | General Population | Cross-sectional design, N = 2541, Female = 50.2%, Age = 38.7 years. | PSQI | 7 |
| 55 | Cui et al., 2020 [97] | China | No | COVID-19 patients | Cross-sectional design, N = 891, Female = 100%, Age = 18–40 years. | ISI | 8 |
| 56 | Czeisler et al., 2021 [98] | Australia | No | General Population | Cross-sectional design, N = 1531, Female = 48.3%, Age = 38.7 years. | SD | 5 |
| 57 | Dai et al., 2020 [99] | China | No | COVID-19 patients | Cross-sectional design, N = 307, Female = 43.3%, Age = 44–60 years. | PSQI | 8 |
| 58 | Das et al., 2021 [100] | Bangladesh | Yes | General Population | Cross-sectional design, N = 672, Female = 43%, Age = 34.4 years. | PSQI | 7 |
| 59 | Dasdemir et al., 2021 [101] | Turkey | Yes | Special Population | Cross-sectional design, N = 44, Female = 70.5%, Age = 34.3 years. | PSQI | 5 |
| 60 | de Medeiros et al., 2021 [102] | Brazil | Yes | General Population | Cross-sectional design, N = 5, Female = 60%, Age = 40 years. | PSQI | 4 |
| 61 | Demartini et al., 2020 [103] | Italy | No | General Population | Cross-sectional design, N = 432, Female = 72%, Age = 35.9 years. | PSQI | 8 |
| 62 | Du et al., 2021 [104] | Multi | Yes | University Students | Cross-sectional design, N = 2254, Female = 66.6%, Age = 22.5 years. | PSQI | 7 |
| 63 | Duran et al., 2021 [105] | Turkey | No | General Population | Cross-sectional design, N = 405, Female = 70.9%, Age = NR years. | PSQI | 8 |
| 64 | Elhadi et al., 2021 [106] | Libya | Yes | General Population | Cross-sectional design, N = 10,296, Female = 77.6%, Age = 28.9 years. | ISI | 6 |
| 65 | ElHafeez et al., 2021 [107] | Egypt | Yes | General Population Healthcare workers [Frontline = 0%, Nurses = 50%] |
Cross-sectional design, N = 538, Female = 66.2%, Age = 35 years. Cross-sectional design, N = 462, Female = 66.2%, Age = 35 years. |
PSQI | 7 |
| 66 | Elkholy et al., 2021 [108] | Egypt | No | Healthcare workers [Frontline = 100%, Nurses = 40%] | Cross-sectional design, N = 502, Female = 50%, Age = 20–40 years. | ISI | 8 |
| 67 | Essangri et al., 2021 [109] | Morocco | No | University Students | Cross-sectional design, N = 549, Female = 74%, Age = 22 years. | ISI | 8 |
| 68 | Falkingham et al., 2020 [110] | UK | Yes | General Population | Cross-sectional design, N = 15,360, Female = 53.9%, Age = 36.5 years. | SD | 6 |
| 69 | Fekih-Romdhane et al., 2020 [111] | Tunis | No | Healthcare workers [Frontline = 48.3%, Nurses = 0.65%] | Cross-sectional design, N = 210, Female = 70.5%, Age = 28.6 years. | ISI | 8 |
| 70 | Fidanci et al., 2020 [112] | Turkey | No | Healthcare workers [Frontline = 0%, Nurses = 1%] | Cross-sectional design, N = 153, Female = 67.3%, Age = 33.4 years. | PSQI | 7 |
| 71 | Filippo et al., 2021 [113] | Italy | Yes | Healthcare workers [Frontline = 0%, Nurses = 8.57%] | Cross-sectional design, N = 175, Female = 76.6%, Age = 37 years. | PSQI | 5 |
| 72 | Florin et al., 2020 [114] | France | Yes | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 1515, Female = 44.3%, Age = 45.2 years. | ISI | 8 |
| 73 | Franceschini et al., 2020 [115] | Italy | Yes | General Population | Cross-sectional design, N = 6439, Female = 73.1%, Age = 33.9 years. | MOS-SS | 8 |
| 74 | Fu et al., 2020 [116] | China | No | General Population | Cross-sectional design, N = 1242, Female = 69.7%, Age = 18–64 years. | AIS | 8 |
| 75 | Garcia-Priego et al., 2020 [117] | México | Yes | General Population | Cross-sectional design, N = 561, Female = 71%, Age = 30.7 years. | SD | 6 |
| 76 | Garriga-Baraut et al., 2021 [118] | Multi | Yes | Children and Adolescents | Longitudinal design, N = 25, Female = 64%, Age = 14 years. | SDSC | 4 |
| 77 | Gas et al., 2021 [119] | Turkey | Yes | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 699, Female = 64.7%, Age = 21.3 years. | PSQI | 7 |
| 78 | Ge et al., 2020 [120] | China | No | University Students | Cross-sectional design, N = 2009, Female = 51%, Age = NR years. | ISI | 8 |
| 79 | Genta et al., 2021 [121] | Brazil | Yes | Children and Adolescents | Longitudinal design, N = 94, Female = 64%, Age = 15 years. | PSQI | 6 |
| 80 | Giardino et al., 2020 [122] | Argentina | No | Healthcare workers [Frontline = 0%, Nurses = 7.5%] | Cross-sectional design, N = 1059, Female = 72.7%, Age = 41.7 years. | ISI | 8 |
| 81 | Goodman-Casanova et al., 2020 [123] | Spain | Yes | Special Population | Cross-sectional design, N = 93, Female = 65%, Age = 73.3 years. | SD | 4 |
| 82 | Goularte et al., 2021 [124] | Brazil | Yes | General Population | Cross-sectional design, N = 1996, Female = 84.5%, Age = 34.2 years. | PSQI | 7 |
| 83 | Gu et al., 2020 [125] | China | No | Healthcare workers [Frontline = 0%, Nurses = 77.9%] | Cross-sectional design, N = 522, Female = 77.6%, Age = 18–40 years. | ISI | 8 |
| 84 | Gualano et al., 2020 [126] | Italy | Yes | General Population | Cross-sectional design, N = 1515, Female = 65.6%, Age = 42 years. | ISI | 8 |
| 85 | Guo et al., 2020 [127] | China | No | General Population | Cross-sectional design, N = 2441, Female = 52.4%, Age = 18–50 years. | PSQI | 8 |
| 86 | Gupta et al., 2020 [128] | India | Yes | General Population Healthcare workers [Frontline = 0%, Nurses = 50%] |
Cross-sectional design, N = 579, Female = 37.7%, Age = 38.8 years. Cross-sectional design, N = 379, Female = 46.2%, Age = 35.7 years. |
ISI | 7 |
| 87 | Hao et al., 2020 [129] | China | Yes | Special Population | Case-Control design, N = 185, Female = 49.8%, Age = 33 years. | ISI | 7 |
| 88 | Haravuori et al., 2020 [130] | Finland | No | General Population | Longitudinal design, N = 4804, Female = 87.5%, Age = 45 years. | ISI | 8 |
| 89 | He et al., 2020 [131] | China | No | COVID-19 patients General Population Healthcare workers [Frontline = NR%, Nurses = NR%] |
Cross-sectional design, N = 1912, Female = 70.1%, Age = 56.8 years. Cross-sectional design, N = 374, Female = 77.4%, Age = 56.8 years. Cross-sectional design, N = 403, Female = 49.6%, Age = 56.8 years. |
PSQI | 8 |
| 90 | Hendrickson et al., 2020 [132] | USA | Yes | Healthcare workers [Frontline = 44%, Nurses = 34.59%] | Cross-sectional design, N = 118, Female = NR%, Age = 41 years. | ISI | 5 |
| 91 | Herrero San Martin et al., 2020 [133] | Spain | No | General Population Healthcare workers [Frontline = 58.82%, Nurses = 15.29%] |
Cross-sectional design, N = 70, Female = 58.8%, Age = 36.4 years. Cross-sectional design, N = 100, Female = 59%, Age = 36.4 years. |
PSQI | 7 |
| 92 | Huang et al., 2020 [134] | China | No | Healthcare workers [Frontline = 100%, Nurses = 100%] | Cross-sectional design, N = 966, Female = 91.2%, Age = 31.9 years. | PSQI | 8 |
| 93 | Huang et al., 2020 [135] | China | No | General Population | Cross-sectional design, N = 1172, Female = 69.3%, Age = 18–40 years. | ISI | 8 |
| 94 | Huang et al., 2020 [136] | China | No | General Population | Cross-sectional design, N = 7236, Female = 54.6%, Age = 36.6 years. | PSQI | 8 |
| 95 | Hussen et al., 2021 [137] | Iraq | Yes | General Population | Cross-sectional design, N = 320, Female = NR%, Age = NR years. | SD | 6 |
| 96 | Idrissi et al., 2020 [138] | Morocco | Yes | General Population | Cross-sectional design, N = 827, Female = 52.2%, Age = 35.9 years. | AIS | 8 |
| 97 | Innocenti et al., 2020 [139] | Italy | Yes | General Population | Cross-sectional design, N = 1035, Female = 82.9%, Age = NR years. | PSQI | 7 |
| 98 | Iqbal et al., 2020 [140] | Qatar | Yes | COVID-19 patients | Cross-sectional design, N = 50, Female = 52%, Age = 39.5 years. | SD | 4 |
| 99 | Jahrami et al., 2020 [141] | Bahrain | No | Healthcare workers [Frontline = 50%, Nurses = 50%] | Cross-sectional design, N = 257, Female = 70%, Age = 40.2 years. | PSQI | 8 |
| 100 | Jain et al., 2020 [142] | India | No | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 512, Female = 44.3%, Age = 18–60 years. | ISI | 8 |
| 101 | Jiang et al., 2021 [143] | China | Yes | Healthcare workers [Frontline = 35.2%, Nurses = 50.2%] | Cross-sectional design, N = 4245, Female = 77.5%, Age = 38 years. | SRSS | 8 |
| 102 | Jin et al., 2021 [144] | China | Yes | Healthcare workers [Frontline = 0%, Nurses = 50%] | Cross-sectional design, N = 404, Female = NR%, Age = 30–50 years. | PSQI | 7 |
| 103 | Juanjuan et al., 2020 [145] | China | No | Special Population | Cross-sectional design, N = 658, Female = 100%, Age = 40–65 years. | ISI | 8 |
| 104 | Jung et al., 2020 [146] | Germany | Yes | General Population | Cross-sectional design, N = 3545, Female = 83.1%, Age = 41.4 years. | SD | 6 |
| 105 | Kaparounaki et al., 2020 [147] | Greece | Yes | University Students | Cross-sectional design, N = 1000, Female = 68.1%, Age = 22.1 years. | SRSS | 7 |
| 106 | Khaled et al., 2021 [148] | Qatar | No | General Population | Cross-sectional design, N = 1161, Female = 53.2%, Age = NR years. | SCI | 8 |
| 107 | Khalil et al., 2020 [149] | Egypt | No | Children and Adolescents | Cross-sectional design, N = 83, Female = 74.7%, Age = 12.8 years. | PSQI | 4 |
| 108 | Khamis et al., 2020 [150] | Oman | No | Healthcare workers [Frontline = 27.9%, Nurses = 71.6%] | Cross-sectional design, N = 402, Female = 100%, Age = 36.4 years. | SQS | 8 |
| 109 | Khanal et al., 2020 [151] | Nepal | No | Healthcare workers [Frontline = 45.3%, Nurses = 35.2%] | Cross-sectional design, N = 475, Female = 52.6%, Age = 28.2 years. | ISI | 8 |
| 110 | Khoury et al., 2021 [152] | Canada | No | Special Population | Cross-sectional design, N = 303, Female = 100%, Age = 32.1 years. | ISI | 8 |
| 111 | Kilani et al., 2020 [153] | Multi | No | General Population | Cross-sectional design, N = 1723, Female = 46.8%, Age = 34.9 years. | PSQI | 8 |
| 112 | Killgore et al., 2020 [154] | USA | Yes | General Population | Cross-sectional design, N = 1013, Female = 56%, Age = 18–35 years. | ISI | 7 |
| 113 | Kocevska et al., 2020 [155] | Netherlands | Yes | General Population | Cross-sectional design, N = 667, Female = NR%, Age = NR years. | ISI | 8 |
| 114 | Kokou-Kpolou et al., 2020 [156] | France | Yes | General Population | Cross-sectional design, N = 556, Female = 75.5%, Age = 30.1 years. | ISI | 7 |
| 115 | Kolokotroni et al., 2021 [157] | Cyprus | Yes | General Population | Cross-sectional design, N = 745, Female = 73.8%, Age = 39 years. | PSQI | 7 |
| 116 | Lahiri et al., 2021 [158] | India | Yes | General Population | Cross-sectional design, N = 1081, Female = 41.7%, Age = 32 years. | ISI | 8 |
| 117 | Lai et al., 2020 [159] | China | No | Healthcare workers [Frontline = 41.5%, Nurses = 60.8%] | Cross-sectional design, N = 1257, Female = 76.7%, Age = 18–40 years. | ISI | 8 |
| 118 | Lai et al., 2020 [160] | UK | No | University Students | Cross-sectional design, N = 124, Female = 63.7%, Age = NR years. | ISI | 6 |
| 119 | Lavigne-Cerván et al., 2021 [161] | Spain | Yes | Children and Adolescents | Cross-sectional design, N = 1028, Female = 46.5%, Age = 10.5 years. | BEARS | 7 |
| 120 | Li et al., 2021 [162] | Australia | Yes | Children and Adolescents | Cross-sectional design, N = 760, Female = 72%, Age = 14.8 years. | ISI | 7 |
| 121 | Li et al., 2020 [163] | Taiwan | Yes | General Population | Cross-sectional design, N = 1970, Female = 66.2%, Age = 37.8 years. | SD | 6 |
| 122 | Li et al., 2021 [164] | China | Yes | COVID-19 patients | Cross-sectional design, N = 51, Female = 58%, Age = 46.1 years. | PSQI | 5 |
| 123 | Li et al., 2020 [165] | China | Yes | Healthcare workers [Frontline = 23.3%, Nurses = 55.1%] | Cross-sectional design, N = 606, Female = 81.2%, Age = 35.8 years. | ISI | 7 |
| 124 | Li et al., 2021 [166] | China | No | Special Population | Cross-sectional design, N = 1063, Female = 67.4%, Age = 62.8 years. | ISI | 8 |
| 125 | Liang et al., 2020 [167] | China | No | General Population Healthcare workers [Frontline = 100%, Nurses = 50.0%] |
Cross-sectional design, N = 1104, Female = 69.5%, Age = 20–60 years. Cross-sectional design, N = 889, Female = 74.8%, Age = 20–60 years. |
ISI | 8 |
| 126 | Liguori et al., 2020 [168] | Italy | Yes | COVID-19 patients | Cross-sectional design, N = 103, Female = 42.7%, Age = 55 years. | SNS | 5 |
| 127 | Lin et al., 2021 [169] | China | Yes | General Population | Cross-sectional design, N = 5461, Female = 70.1%, Age = 37.6 years. | ISI | 7 |
| 128 | Liu et al., 2020 [170] | China | Yes | General Population | Cross-sectional design, N = 285, Female = 54.5%, Age = NR years. | PSQI | 7 |
| 129 | Liu et al., 2021 [171] | China | No | Healthcare workers [Frontline = 0%, Nurses = 63.8%] | Cross-sectional design, N = 2126, Female = 97.7%, Age = NR years. | ISI | 8 |
| 130 | Liu et al., 2021 [172] | China | No | General Population | Cross-sectional design, N = 2858, Female = 53.6%, Age = NR years. | PSQI | 8 |
| 131 | Liu et al., 2020 [173] | China | No | Healthcare workers [Frontline = 0%, Nurses = 63.8%] | Cross-sectional design, N = 606, Female = 81.2%, Age = 35.8 years. | ISI | 8 |
| 132 | Liu et al., 2020 [174] | USA | No | General Population | Cross-sectional design, N = 898, Female = 81.3%, Age = 24.5 years. | MOS-SS | 8 |
| 133 | Lu et al., 2020 [175] | China | No | Children and Adolescents | Cross-sectional design, N = 965, Female = 42.4%, Age = 15.3 years. | YSRIS | 8 |
| 134 | Machón et al., 2021 [176] | Spain | Yes | Special Population | Cross-sectional design, N = 38, Female = 71%, Age = 83 years. | EQ-5D-5L | 5 |
| 135 | Magnavita et al., 2020 [177] | Italy | No | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 90, Female = 52.2%, Age = NR years. | SCI | 6 |
| 136 | Majumdar et al., 2021 [178] | India | Yes | General Population University Students |
Cross-sectional design, N = 203, Female = 18.2%, Age = 33.1 years. Cross-sectional design, N = 325, Female = 60.9%, Age = 22.1 years. |
ESS | 6 |
| 137 | Mandelkorn et al., 2021 [179] | Multi USA |
Yes | General Population General Population |
Cross-sectional design, N = 2562, Female = 68%, Age = 45.2 years. Cross-sectional design, N = 971, Female = 52.8%, Age = 40.4 years. |
PSQI | 8 |
| 138 | Marelli et al., 2020 [180] | Italy | No | University Students | Longitudinal design, N = 400, Female = 75.8%, Age = 29.9 years. | PSQI | 8 |
| 139 | Marroquín et al., 2020 [181] | USA | No | General Population | Cross-sectional design, N = 435, Female = 46.4%, Age = 39.2 years. | ISI | 8 |
| 140 | Martínez-de-Quel et al., 2021 [182] | Spain | No | General Population | Longitudinal design, N = 161, Female = 37%, Age = 35 years. | PSQI | 7 |
| 141 | Martínez-Lezaun et al., 2020 [183] | Spain | Yes | University Students | Cross-sectional design, N = 75, Female = 80.4%, Age = 21.8 years. | PSQI | 7 |
| 142 | Massicotte et al., 2021 [184] | Canada | No | Special Population | Cross-sectional design, N = 36, Female = 100%, Age = 53.6 years. | ISI | 6 |
| 143 | Mazza et al., 2020 [185] | Italy | No | COVID-19 patients | Cross-sectional design, N = 402, Female = 34.4%, Age = 57.8 years. | MOS-SS | 8 |
| 144 | McCall et al., 2020 [186] | USA | No | Healthcare workers [Frontline = 0%, Nurses = 55.5%] | Cross-sectional design, N = 573, Female = 72%, Age = 43.4 years. | SD | 6 |
| 145 | McCracken et al., 2020 [187] | Sweden | No | General Population | Cross-sectional design, N = 1212, Female = 73.8%, Age = 36.1 years. | ISI | 8 |
| 146 | Meo et al., 2021 [188] | Saudi Arabia | Yes | Healthcare workers [Frontline = 71.5%, Nurses = 15.4%] | Cross-sectional design, N = 1678, Female = 51.2%, Age = 34.1 years. | PSQI | 7 |
| 147 | Miaskowski et al., 2020 [189] | USA | Yes | Special Population | Cross-sectional design, N = 187, Female = 97.9%, Age = 63.3 years. | SD | 4 |
| 148 | Mongkhon et al., 2021 [190] | Thailand | Yes | General Population | Cross-sectional design, N = 4004, Female = 65.4%, Age = 29.1 years. | ISI | 8 |
| 149 | Murata et al., 2020 [191] | USA | Yes | Children and Adolescents General Population |
Cross-sectional design, N = 583, Female = 80%, Age = 15.8 years. Cross-sectional design, N = 4326, Female = 80%, Age = 43.6 years. |
SD | 5 |
| 150 | Necho et al., 2020 [192] | Ethiopia | No | Special Population | Cross-sectional design, N = 423, Female = 40.7%, Age = 36.7 years. | ISI | 8 |
| 151 | Osiogo et al., 2021 [193] | Canada | Yes | General Population | Cross-sectional design, N = 6041, Female = 86.8%, Age = 20–60 years. | SD | 6 |
| 152 | Ozluk et al., 2021 [194] | Turkey | Yes | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 347, Female = 24.2%, Age = 20–65 years. | ISI | 7 |
| 153 | Parlapani et al., 2020 [195] | Greece | No | Special Population | Cross-sectional design, N = 103, Female = 61.2%, Age = 69.9 years. | AIS | 6 |
| 154 | Pedrozo-Pupo et al., 2020 [196] | Colombia | No | Special Population | Cross-sectional design, N = 292, Female = 64.7%, Age = 60.4 years. | AIS | 8 |
| 155 | Petrov et al., 2021 [197] | Multi | Yes | General Population | Cross-sectional design, N = 991, Female = 72.5%, Age = 37.9 years. | ISI | 8 |
| 156 | Pieh et al., 2020 [198] | Austria | Yes | General Population | Cross-sectional design, N = 1005, Female = 52.7%, Age = 18–65 years. | ISI | 8 |
| 157 | Poyraz et al., 2020 [199] | Turkey | No | COVID-19 patients | Cross-sectional design, N = 284, Female = 49.8%, Age = 39.7 years. | PSQI | 8 |
| 158 | Qi et al., 2020 [200] | China | No | Healthcare workers [Frontline = 61.33%, Nurses = 0%] | Cross-sectional design, N = 1306, Female = 80.4%, Age = 33.1 years. | PSQI, ISI | 8 |
| 159 | Que et al., 2020 [201] | China | No | Healthcare workers [Frontline = 0%, Nurses = 9.1%] | Cross-sectional design, N = 2285, Female = 69.1%, Age = 31.1 years. | ISI | 8 |
| 160 | Ren et al., 2020 [202] | China | No | General Population | Cross-sectional design, N = 1172, Female = 69.3%, Age = 22 years. | ISI | 8 |
| 161 | Repon et al., 2021 [203] | Bangladesh | Yes | Healthcare workers [Frontline = 0%, Nurses = 26%] | Cross-sectional design, N = 355, Female = 43%, Age = 20–60 years. | PSQI | 7 |
| 162 | Robillard et al., 2020 [204] | Canada | Yes | General Population | Cross-sectional design, N = 5525, Female = 67.1%, Age = 55.6 years. | PSQI | 8 |
| 163 | Rossi et al., 2020 [205] | Italy | No | General Population Healthcare workers [Frontline = 52.1%, Nurses = 36%] |
Case-control design, N = 21,342, Female = 80.4%, Age = 38.95 years. Case-control design, N = 2706, Female = 79.5%, Age = 42 years. |
ISI ISI |
8 |
| 164 | Rossi et al., 2020 [206] | Italy | No | General Population | Cross-sectional design, N = 18,147, Female = 79.5%, Age = 38 years. | ISI | 8 |
| 165 | Roy et al., 2020 [207] | India | Yes | General Population | Cross-sectional design, N = 662, Female = 51.2%, Age = 29 years. | SD | 6 |
| 166 | Saadeh et al., 2021 [208] | Jordan | Yes | University Students | Cross-sectional design, N = 6157, Female = 71.3%, Age = 19.8 years. | PSQI | 8 |
| 167 | Sadeghniiat-Haghighi et al., 2021 [209] | Iran | No | General Population | Cross-sectional design, N = 1223, Female = 67.6%, Age = 39.8 years. | ISI | 7 |
| 168 | Sagaon-Teyssier et al., 2020 [210] | Mali | Yes | Healthcare workers [Frontline = 0%, Nurses = 14.8%] | Cross-sectional design, N = 135, Female = 39.3%, Age = 40 years. | ISI | 5 |
| 169 | Sagherian et al., 2020 [211] | USA | No | Healthcare workers [Frontline = 63.2%, Nurses = 100%] | Cross-sectional design, N = 564, Female = 94.1%, Age = 18–40 years. | ISI | 8 |
| 170 | Saguem et al., 2021 [212] | Tunis | Yes | University Students | Cross-sectional design, N = 251, Female = 82.5%, Age = 21 years. | PSQI | 8 |
| 171 | Şahin et al., 2020 [213] | Turkey | No | Healthcare workers [Frontline = 60.6%, Nurses = 27.1%] | Cross-sectional design, N = 939, Female = 66%, Age = 18–40 years. | ISI | 8 |
| 172 | Salfi et al., 2021 [214] | Italy | Yes | General Population | Cross-sectional design, N = 13,989, Female = 77.6%, Age = 34.8 years. | PSQI, ISI | 8 |
| 173 | Sañudo et al., 2020 [215] | Spain | No | General Population | Cross-sectional design, N = 20, Female = 47%, Age = 22.6 years. | PSQI | 5 |
| 174 | Saracoglu et al., 2020 [216] | Turkey | No | Healthcare workers [Frontline = 0%, Nurses = 67.3%] | Cross-sectional design, N = 208, Female = 27.9%, Age = 29 years. | PSQI | 7 |
| 175 | Saraswathi et al., 2020 [217] | India | No | University Students | Longitudinal design, N = 217, Female = 64%, Age = 20 years. | PSQI | 7 |
| 176 | Scotta et al., 2020 [218] | Argentina | Yes | University Students | Cross-sectional design, N = 584, Female = 81%, Age = 22.5 years. | ISI | 8 |
| 177 | Sekartaji et al., 2021 [219] | Indonesia | Yes | University Students | Cross-sectional design, N = 101, Female = 58.4%, Age = 21–26 years. | ISI | 4 |
| 178 | Sharma et al., 2020 [220] | Nepal | Yes | General Population | Cross-sectional design, N = 204, Female = 32.8%, Age = 32 years. | SD | 5 |
| 179 | Sharma et al., 2020 [221] | India | No | Healthcare workers [Frontline = 60.9%, Nurses = 41.8%] | Cross-sectional design, N = 184, Female = 58.7%, Age = 20–50 years. | ISI | 7 |
| 180 | Sharma et al., 2021 [222] | India | Yes | Healthcare workers [Frontline = 0%, Nurses = 0%] | Cross-sectional design, N = 100, Female = 0%, Age = 30–60 years. | SQS | 4 |
| 181 | Shi et al., 2020 [223] | China | No | General Population | Cross-sectional design, N = 56,679, Female = 52.1%, Age = 36 years. | ISI | 8 |
| 182 | Shillington et al., 2021 [224] | Canada | Yes | General Population | Cross-sectional design, N = 2192, Female = 89.6%, Age = 43 years. | PSQI | 7 |
| 183 | Simonetti et al., 2021 [225] | Italy | Yes | Healthcare workers [Frontline = 80.8%, Nurses = 100%] | Cross-sectional design, N = 1005, Female = 65.9%, Age = 40.2 years. | PSQI | 7 |
| 184 | Song et al., 2020 [226] | China | No | General Population | Cross-sectional design, N = 709, Female = 74.2%, Age = 35.4 years. | ISI | 8 |
| 185 | Stanton et al., 2020 [227] | Australia | Yes | General Population | Cross-sectional design, N = 1491, Female = NR%, Age = NR years. | SD | 6 |
| 186 | Stewart et al., 2021 [228] | USA | Yes | Healthcare workers [Frontline = 100%, Nurses = 0%] | Cross-sectional design, N = 963, Female = 73.4%, Age = 18–50 years. | PSQI, ISI | 7 |
| 187 | Sun et al., 2020 [229] | China | Yes | General Population | Cross-sectional design, N = 2091, Female = 60.8%, Age = 16–60 years. | SD | 6 |
| 188 | Sunil et al., 2021 [230] | India | No | Healthcare workers [Frontline = 0%, Nurses = 47.6%] | Cross-sectional design, N = 313, Female = 35.5%, Age = 21–61 years. | ISI | 8 |
| 189 | Tan Wanqiu et al., 2020 [231] | China | No | Healthcare workers [Frontline = NR%, Nurses = NR%] | Cross-sectional design, N = 673, Female = 25.6%, Age = 30.8 years. | ISI | 8 |
| 190 | Tang et al., 2020 [232] | China | Yes | University Students | Cross-sectional design, N = 2485, Female = 60.8%, Age = 19.8 years. | SD | 6 |
| 191 | Than et al., 2020 [233] | Vietnam | No | Healthcare workers [Frontline = 100%, Nurses = 63%] | Cross-sectional design, N = 173, Female = 68.2%, Age = 31 years. | ISI | 7 |
| 192 | Tiete et al., 2020 [234] | Belgium | Yes | Healthcare workers [Frontline = 50.4%, Nurses = 72.3%] | Cross-sectional design, N = 647, Female = 78.4%, Age = 20–50 years. | ISI | 7 |
| 193 | Totskiy et al., 2021 [235] | Russia | Yes | University Students | Cross-sectional design, N = 39, Female = 64.1%, Age = 20.6 years. | ISI | 5 |
| 194 | Trabelsi et al., 2021a [236] | Multi | Yes | General Population | Longitudinal design, N = 517, Female = 52.2%, Age = 63.2 years. | PSQI | 7 |
| 195 | Trabelsi et al., 2021b [237] | Multi | No | General Population | Longitudinal design, N = 5056, Female = 59.4%, Age = 18–55 years. | PSQI | 8 |
| 196 | Tselebis et al., 2020 [238] | Greece | No | Healthcare workers [Frontline = 0%, Nurses = 100%] | Cross-sectional design, N = 150, Female = 80%, Age = 42.3 years. | AIS | 7 |
| 197 | Tu et al., 2020 [239] | China | No | Healthcare workers [Frontline = 100%, Nurses = 100%] | Cross-sectional design, N = 100, Female = 100%, Age = 34.4 years. | PSQI | 6 |
| 198 | Varma et al., 2021 [240] | Multi | Yes | General Population | Cross-sectional design, N = 1653, Female = 67.7%, Age = 42.9 years. | PSQI | 8 |
| 199 | Vitale et al., 2020 [241] | Italy | Yes | COVID-19 patients | Cross-sectional design, N = 4, Female = 25%, Age = 54 years. | PSQI | 4 |
| 200 | Voitaidis et al., 2020 [242] | Greece | Yes | General Population | Cross-sectional design, N = 2427, Female = 76.2%, Age = 18–30 years. | AIS | 7 |
| 201 | Wang et al., 2021a [243] | China | Yes | General Population COVID-19 patients |
Case-control design, N = 1743, Female = 47.8%, Age = 32.7 years. Case-control design, N = 1674, Female = 49.8%, Age = 32.6 years. |
ISI | 7 |
| 202 | Wang et al., 2020 [244] | China | Yes | Healthcare workers [Frontline = 50%, Nurses = 59.2%] | Cross-sectional design, N = 274, Female = 77.4%, Age = 37 years. | PSQI | 7 |
| 203 | Wang et al., 2021 [245] | China | Yes | Children and Adolescents | Cross-sectional design, N = 11,072, Female = 47.9%, Age = 11.5 years. | SD | 6 |
| 204 | Wang et al., 2020 [246] | China | No | General Population | Cross-sectional design, N = 19,372, Female = 52%, Age = 11–87 years. | ISI | 8 |
| 205 | Wang et al., 2021 [247] | China | No | General Population | Cross-sectional design, N = 5676, Female = 71.4%, Age = NR years. | ISI | 8 |
| 206 | Wang et al., 2020 [248] | China | No | General Population | Cross-sectional design, N = 4191, Female = 62%, Age = 36.2 years. | ISI | 8 |
| 207 | Wang et al., 2020 [249] | China | No | University Students | Cross-sectional design, N = 3092, Female = 66.4%, Age = NR years. | SRSS | 8 |
| 208 | Wang et al., 2020 [250] | China | No | COVID-19 patients | Cross-sectional design, N = 484, Female = 50.2%, Age = 52.5 years. | ISI | 8 |
| 209 | Wang et al., 2020 [251] | China | No | General Population | Cross-sectional design, N = 6437, Female = 56.1%, Age = 31.5 years. | PSQI | 8 |
| 210 | Wang et al., 2020 [252] | China | No | Healthcare workers [Frontline = 33%, Nurses = 0%] | Cross-sectional design, N = 2001, Female = 64.5%, Age = 33 years. | PSQI | 8 |
| 211 | Wang et al., 2020 [253] | China | No | Healthcare workers [Frontline = 0%, Nurses = 61%] | Cross-sectional design, N = 123, Female = 90%, Age = 33.8 years. | PSQI | 6 |
| 212 | Wańkowicz et al., 2020 [254] | Poland | No | Healthcare workers [Frontline = 46.7%, Nurses = 0%] | Cross-sectional design, N = 441, Female = 52.2%, Age = 40 years. | ISI | 8 |
| 213 | Wańkowicz et al., 2020 [255] | Poland | No | Special Population | Case-control design, N = 723, Female = 54.4%, Age = 39.1 years. | ISI | 8 |
| 214 | Wasim et al., 2020 [256] | Pakistan | No | Healthcare workers [Frontline = 0%, Nurses = 20.8%] | Cross-sectional design, N = 356, Female = 52%, Age = NR years. | ISI | 8 |
| 215 | Windiani et al., 2021 [257] | Indonesia | No | Children and Adolescents | Cross-sectional design, N = 204, Female = 48.5%, Age = 16 years. | PSQI | 4 |
| 216 | Wu et al., 2020 [258] | China | No | Healthcare workers [Frontline = 100%, Nurses = 0%] | Case-control design, N = 120, Female = 74.2%, Age = 33.7 years. | PSQI | 6 |
| 217 | Xia et al., 2021 [259] | China | No | Special Population | Case-control design, N = 288, Female = 54.8%, Age = 60.5 years. | PSQI | 8 |
| 218 | Xu et al., 2021 [260] | China | Yes | Special Population | Cross-sectional design, N = 274, Female = 100%, Age = 30.4 years. | PSQI | 7 |
| 219 | Yadav et al., 2021 [261] | India | Yes | COVID-19 patients | Cross-sectional design, N = 100, Female = 27%, Age = 42.9 years. | PSQI | 5 |
| 220 | Yang et al., 2020 [262] | China | Yes | General Population | Cross-sectional design, N = 2410, Female = 49.2%, Age = 36.3 years. | PSQI | 7 |
| 221 | Yang et al., 2020 [263] | China | No | General Population Healthcare workers [Frontline = 100%, Nurses = 84.4%] |
Case-control design, N = 15,000, Female = 57.1%, Age = NR years. Case-control design, N = 1036, Female = 72.9%, Age = 20–50 years. |
ISI | 8 |
| 222 | Yang et al., 2021 [264] | China | No | Healthcare workers [Frontline = 100%, Nurses = 84.4%] | Cross-sectional design, N = 1036, Female = 72.9%, Age = 20–50 years. | ISI | 8 |
| 223 | Yifan et al., 2020 [265] | China | Yes | Healthcare workers [Frontline = 100%, Nurses = 100%] | Cross-sectional design, N = 140, Female = 84.3%, Age = 29.4 years. | SD | 5 |
| 224 | Yitayih et al., 2020 [266] | Ethiopia | No | Healthcare workers [Frontline = 0%, Nurses = 52.2%] | Cross-sectional design, N = 249, Female = 52.6%, Age = 27.4 years. | ISI | 7 |
| 225 | Youssef et al., 2020 [267] | Egypt | No | Healthcare workers [Frontline = 10.2%, Nurses = 9.1%] | Cross-sectional design, N = 540, Female = 45.6%, Age = 37.3 years. | ISI | 8 |
| 226 | Yu et al., 2020 [268] | China | Yes | General Population | Cross-sectional design, N = 1138, Female = 65.6%, Age = NR years. | ISI | 8 |
| 227 | Yuksel et al., 2021 [269] | Multi | Yes | General Population | Cross-sectional design, N = 6882, Female = 78.8%, Age = 42.3 years. | SD | 6 |
| 228 | Zanghì et al., 2020 [270] | Italy | No | Special Population | Cross-sectional design, N = 432, Female = 64.1%, Age = 40.4 years. | ISI | 8 |
| 229 | Zhan et al., 2020 [271] | China | No | Healthcare workers [Frontline = 100%, Nurses = 100%] | Cross-sectional design, N = 1794, Female = 97%, Age = 25–65 years. | AIS | 8 |
| 230 | Zhang et al., 2020 [272] | China | Yes | General Population | Cross-sectional design, N = 2027, Female = 61.2%, Age = 35.5 years. | PSQI | 7 |
| 231 | Zhang et al., 2021 [273] | China | Yes | COVID-19 patients | Cross-sectional design, N = 205, Female = 48.3%, Age = 58 years. | PSQI | 5 |
| 232 | Zhang et al., 2020 [274] | China | Yes | Healthcare workers [Frontline = 0%, Nurses = 11.3%] | Cross-sectional design, N = 2182, Female = 64.2%, Age = NR years. | ISI | 7 |
| 233 | Zhang et al., 2020 [275] | China | No | COVID-19 patients | Cross-sectional design, N = 135, Female = 42.2%, Age = 63 years. | PSQI | 6 |
| 234 | Zhang et al., 2021 [276] | China | No | Healthcare workers [Frontline = 100%, Nurses = 46.7%] | Cross-sectional design, N = 319, Female = 62.1%, Age = 30.4 years. | PSQI | 8 |
| 235 | Zhang et al., 2021 [277] | China | No | Special Population | Cross-sectional design, N = 456, Female = 100%, Age = NR years. | PSQI | 8 |
| 236 | Zhang et al., 2020 [278] | China | No | Healthcare workers [Frontline = 28.6%, Nurses = 55.7%] | Cross-sectional design, N = 524, Female = 74.4%, Age = 34.9 years. | ISI | 8 |
| 237 | Zhang et al., 2020 [279] | China | No | COVID-19 patients | Cross-sectional design, N = 30, Female = 50%, Age = 42.5 years. | ISI | 6 |
| 238 | Zhang et al., 2020 [280] | China | No | General Population | Cross-sectional design, N = 3237, Female = 47.1%, Age = NR years. | ISI | 8 |
| 239 | Zhang et al., 2020 [281] | China | No | Healthcare workers [Frontline = 50%, Nurses = 62.9%] | Cross-sectional design, N = 1563, Female = 82.7%, Age = 18–60 years. | ISI | 8 |
| 240 | Zhang et al., 2020 [282] | China | No | University Students | Longitudinal design, N = 66, Female = 62.1%, Age = 20.7 years. | PSQI | 6 |
| 241 | Zhao et al., 2020 [283] | China | Yes | Healthcare workers [Frontline = 100%, Nurses = 46%] | Cross-sectional design, N = 215, Female = 76.2%, Age = 35.9 years. | PSQI | 5 |
| 242 | Zheng et al., 2020 [284] | China | Yes | Healthcare workers [Frontline = 63.77%, Nurses = 74.88%] | Cross-sectional design, N = 207, Female = 84.5%, Age = 37 years. | PSQI | 5 |
| 243 | Zheng et al., 2021 [285] | China | Yes | General Population | Cross-sectional design, N = 631, Female = 61.2%, Age = 21.1 years. | PSQI | 7 |
| 244 | Zhou et al., 2020 [286] | China | Yes | Children and Adolescents | Cross-sectional design, N = 11,835, Female = 57.7%, Age = 17.4 years. | PSQI | 7 |
| 245 | Zhou et al., 2020 [287] | China | No | General population Healthcare workers [Frontline = 100%, Nurses = NR %] |
Case-control design, N = 1099, Female = 69.4%, Age = 28.3 years. Case-control design, N = 606, Female = 81.2%, Age = 35.8 years. |
ISI | 8 |
| 246 | Zhou et al., 2020 [288] | China | No | Healthcare workers [Frontline = 100%, Nurses = 83.6%] | Cross-sectional design, N = 1931, Female = 95.4%, Age = 35.1 years. | PSQI | 8 |
| 247 | Zhou et al., 2020 [289] | China | No | Special Population | Cross-sectional design, N = 859, Female = 100%, Age = 33.3 years. | ISI | 8 |
| 248 | Zhuo et al., 2020 [290] | China | No | Healthcare workers [Frontline = 100%, Nurses = NR %] | Cross-sectional design, N = 26, Female = 46.2%, Age = 41.9 years. | ISI | 5 |
| 249 | Zreik et al., 2021 [291] | Israel | Yes | General Population Children and Adolescents |
Cross-sectional design, N = 264, Female = 100%, Age = 34 years Cross-sectional design, N = 264, Female = 54.4%, Age = 0.5 years. |
ISI BICQ |
7 |
| 250 | Zupancic et al., 2021 [292] | Slovenia | Yes | Healthcare workers [Frontline = 27.03%, Nurses = NR%] | Cross-sectional design, N = 1019, Female = 73.3%, Age = NR years. | ESS | 8 |
Measures: AIS = Athens insomnia scale. BEARS = Bedtime issues, excessive daytime sleepiness, night awakenings, regularity and duration of sleep, and snoring. ISI = Insomnia severity index. MOS-SS = Medical outcomes study sleep scale. MSQ = Mini sleep questionnaire. PROMIS = Patient-reported outcomes measurement information system-sleep disturbance. PSQI = Pittsburgh sleep quality index. SCI = Sleep condition indicator. SCI-02 = Sleep condition indicator-02. SD = Self-developed. SDSC = Bruni scale/sleep disturbance scale for children. SNS = Subjective neurological symptoms. SQS = Sleep quality scale. SRSS = Self-rating scale of sleep. YSIS = Youth self-rating insomnia scale.
The Newcastle–Ottawa Scale (NOS) was used to evaluate the methodological quality and assess the risk of bias of the studies included in the current review. The look at three aspects (participants selection, comparability, and outcome and statistics).
Sleep disturbances: a meta-analysis
Global assessment of sleep disturbances
Using all available studies, a random-effects meta-analysis evaluated the prevalence of sleep disturbances in all populations (K = 285, N = 493,475) generated a pooled prevalence rate of 40.49% [37.56; 43.48%], heterogeneity (Q = 87,213 (284), P = 0.001), = 1.09 [0.86; 1.30], = 1.04 [0.93; 1.14], I 2 = 99.7%; H = 17.52 [17.28; 17.78]. Using any sleep measure in all populations, the raw prevalence estimates for sleep disturbances varied from 2% to 95%. The forest plot of the meta-analysis of sleep disturbances in all populations using all measures is shown in Fig. S2.
A (leave-one-out) sensitivity analysis found that no study had a greater than 1% impact on the global prevalence estimate, Fig. S3. Influence analysis was used to identify and eliminate outliers in our meta-analyses. Results of influence meta-analysis yielded a pooled prevalence rate of 40.70% [39.81; 41.59%], heterogeneity (Q = 270 (76), P = 0.001), = 0.02 [0.01; 0.04], = 0.12 [0.10; 0.19], I 2 = 72.20% [65.10%; 77.90%], H = 1.90 [1.69; 2.13]. The influence on pooled result and overall heterogeneity contribution from the analysis is shown in a Baujat plot in Figure S4.
After using the leave-one-out method and influence analyses to test the robustness of our meta-analysis, the GOSH plot in Fig. S5 revealed several distinct clusters, indicating that there may be more than one effect size population in our data, necessitating a subgroup analysis and the preservation of outliers. GOSH diagnostics indicated that the number of K-means clusters detected ≥3 is shown in Fig. S6.
Visual inspection to funnel plot indicated a slight publication bias (Fig. 3 ), Egger's regression P = 0.001 confirmed the publication bias; however, this was not evident in the radial plot (Fig. 4 ) and rank correlation by Kendall's τ without continuity correction, P = 0.06. The trim-and-fill technique was used to estimate and compensate for the quantity and findings of missing studies, and results showed that adjusted prevalence of sleep disturbances with K = 353 (68 added studies) is 30.50% [27.93; 33.19%], heterogeneity (Q = 124,771 (352), P = 0.001), = 1.39 [1.27; 1.84], = 1.18 [1.12; 1.35], I 2 = 99.70%; H = 18.83 [18.60; 19.06].
Fig. 3.
Funnel plot of sleep disturbances (all populations, all countries, all measures).
Fig. 4.
Radial plot of sleep disturbances (all populations, all countries, all measures).
Meta-regression analysis revealed that neither age nor sex moderates the global prevalence rate of sleep disturbances during the COVID-19 pandemic P = 0.15 and P = 0.92, respectively. Detailed results are presented in Table 2 .
Table 2.
Sleep disturbances during COVID-19: a meta-analysis, a moderator analysis and assessment of heterogeneity.
| Component | K | N | Random-effects meta-analysis |
Heterogeneity |
Moderators |
Publication Bias | Adjusted results [95%CI] | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pooled results [95%CI] | Forest Plot | I2 | H | τ2 | Q (Within) | Q (Between) | Age | Sex (%Female) | |||||
| Global assessment of sleep disturbances during COVID-19 | |||||||||||||
| Sleep disturbances (all populations, all countries, all measuresa) | 285 | 493,475 | 40.49% [37.56; 43.48%] | Fig. S2. | 99.7% | 17.52 | 1.09 | 87,213 (284) | NA | 0.15 | 0.92 | Egger's P = 0.001 | 30.50% [27.93; 33.19%] |
| Assessment of sleep disturbances during COVID-19 by country | |||||||||||||
| Sleep disturbances (all populations, all measures) China | 84 | 223,196 | 30.32% [26.26; 34.72%] | Fig. S8. | 99.7% | 17.45 | 0.86 | 25,281 (83) | 54 (7) P = 0.001 |
0.02 | 0.14 | Egger's P = 0.003 | 20.14% [17.02; 23.65%] |
| Sleep disturbances (all populations, all measures) Italy | 34 | 91,878 | 38.64% [28.86; 49.44%] | 99.8% | 23.99 | 1.67 | 18,997 (33) | 0.66 | 0.19 | NS | NI | ||
| Sleep disturbances (all populations, all measures) India | 16 | 5842 | 27.25% [19.00; 37.43%] | 98.2% | 7.39 | 0.89 | 819 (15) | 0.89 | 0.78 | NS | NI | ||
| Sleep disturbances (all populations, all measures) USA | 15 | 13,022 | 50.21% [41.06; 59.35%] | 98.8% | 9.18 | 0.52 | 1181 (14) | 0.35 | 0.83 | NS | NI | ||
| Sleep disturbances (all populations, all measures) Turkey | 12 | 5389 | 44.18% [33.41; 55.53%] | 98.0% | 7.03 | 0.62 | 543 (11) | 0.10 | 0.83 | Egger's P = 0.03 | 60.67% [49.31; 70.98%] | ||
| Sleep disturbances (all populations, all measures) Spain | 10 | 1848 | 58.59% [47.64; 68.76%] | 92.8% | 3.72 | 0.45 | 124 (9) | 0.04 | 0.66 | NS | NI | ||
| Sleep disturbances (all populations, all measures) Saudi Arabia | 10 | 7197 | 51.10% [36.67; 65.35%] | 99.2% | 11.17 | 0.90 | 1122 (9) | 0.19 | 0.39 | NS | NI | ||
| Sleep disturbances (all populations, all measures) all other countries | 104 | 145,103 | 47.69% [43.67; 51.75%] | 99.5% | 14.04 | 0.69 | 20,316 (103) | 0.85 | 0.78 | NS | NI | ||
| Assessment of sleep disturbances during COVID-19 by population | |||||||||||||
| Sleep disturbances (general population, all measures) | 121 | 364,060 | 36.73% [32.32; 41.38%] | Fig. S9. | 99.8% | 23.17 | 1.18 | 64,436 (120) | 9 (5) P = 0.10 |
0.12 | 0.34 | NS | NI |
| Sleep disturbances (healthcare workers, all measures) | 90 | 63,685 | 42.47% [37.95; 47.12%] | 99.1% | 0.47 | 0.81 | 9749 (89) | 0.03 | 0.74 | NS | NI | ||
| Sleep disturbances (COVID-19 patients, all measures) | 16 | 6821 | 52.39% [41.69; 62.88%] | 98.1% | 7.31 | 0.70 | 802 (15) | 0.60 | 0.34 | Egger's P = 0.006 | 33.20% [24.17; 43.66%] | ||
| Sleep disturbances (university students, all measures) | 22 | 21,880 | 41.16% [28.76; 54.79%] | 99.6% | 16.08 | 1.69 | 5432 (21) | 0.52 | 0.04 | NS | NI | ||
| Sleep disturbances (special populations, all measures) | 23 | 8023 | 41.50% [32.98; 50.56%] | 98.1% | 7.19 | 0.77 | 1136 (22) | 0.10 | 0.05 | NS | NI | ||
| Sleep disturbances (children and adolescents, all measures) | 13 | 29,006 | 45.96% [36.90; 55.30%] | 99.3% | 12.29 | 0.45 | 1812 (12) | 0.64 | 0.15 | NS | NI | ||
| Assessment of sleep disturbances during COVID-19 by used measure | |||||||||||||
| Sleep disturbances (all populations, PSQI only) | 114 | 134,177 | 51.87% [47.87; 55.84%] | Fig. S10. | 99.4% | 13.11 | 0.73 | 19,414 (113) | 52 (3) P = 0.001 |
0.76 | 0.78 | NS | NI |
| Sleep disturbances (all populations, ISI only) | 110 | 256,673 | 30.98% [26.77; 35.54%] | 99.7% | 18.39 | 1.19 | 36,874 (109) | 0.69 | 0.56 | Kendall's P = 0.04 Egger's P = 0.01 |
18.38% [15.36; 21.85%] | ||
| Sleep disturbances (all populations, AIS only) | 12 | 10,169 | 47.22% [41.37; 53.15%] | 96.9% | 5.69 | 0.17 | 356 (11) | 0.45 | 0.09 | NS | NI | ||
| Sleep disturbances (all populations, other measures) | 49 | 92,456 | 35.70% [30.38; 41.39%] | 96.9% | 16.00 | 0.72 | 12,294 (48) | 0.054 | 0.055 | NS | NI | ||
| Assessment of sleep disturbances during COVID-19 by lockdown status | |||||||||||||
| Sleep disturbances (all populations, all measures, no lockdown) | 123 | 325,653 | 37.97% [34.42; 41.66%] | Fig. S11. | 99.4% | 13.13 | 0.74 | 21,033 (122) | 3 (1) P = 0.1 |
0.008 | 0.51 | Egger's P = 0.001 | 26.68% [23.59; 30.01%] |
| Sleep disturbances (all populations, all measures, during lockdown) | 162 | 166,275 | 42.49% [38.21; 46.89%] | 99.8% | 20.33 | 1.31 | 65,459 (161) | 0.78 | 0.39 | Kendall's P = 0.03 Egger's P = 0.03 |
33.01% [29.20; 37.06%] | ||
| Assessment of sleep disturbances during COVID-19 by year of publication | |||||||||||||
| Sleep disturbances (all populations, all measures, 2020) | 171 | 321,988 | 36.20% [32.52; 40.04%] | Fig. S12. | 99.7% | 17.55 | 1.16 | 52,374 (170) | 15 (1) P = 0.001 |
0.04 | 0.99 | Kendall's P = 0.01 Egger's P = 0.001 |
23.54% [20.68; 26.66%] |
| Sleep disturbances (all populations, all measures, 2021) | 114 | 171,487 | 47.14% [43.01; 51.30%] | 99.6% | 15.34 | 0.80 | 26,601 (113) | 0.90 | 0.56 | NS | NI | ||
| Assessment of sleep disturbances during COVID-19 by research design | |||||||||||||
| Sleep disturbances assessed using cross-sectional design | 249 | 445,950 | 40.26% [37.10; 43.49%] | Fig. S13. | 99.7% | 17.93 | 1.12 | 79,699 (248) | 8 (2) P = 0.01 |
0.15 | 0.66 | Egger's P = 0.002 | 29.65% [26.91; 32.54%] |
| Sleep disturbances assessed using case–control design | 11 | 24,820 | 31.57% [18.23; 48.85%] | 99.7% | 18.99 | 1.50 | 3607 (10) | 0.15 | 0.39 | NS | NI | ||
| Sleep disturbances assessed using longitudinal design | 25 | 22,705 | 48.36% [43.14; 53.61%] | 98.0% | 6.98 | 0.26 | 1171 (24) | 0.37 | 0.001 | NS | NI | ||
| Assessment of sleep disturbances during COVID-19 by methodological quality | |||||||||||||
| High quality (low risk of bias) | 137 | 348,278 | 34.59% [30.58; 38.83%] | Fig. S14. | 99.8% | 21.01 | 1.18 | 60,013 (136) | 16 (2) P = 0.001 |
0.59 | 0.94 | Egger's P = 0.049 | 21.80% [18.56; 25.43%] |
| Moderate quality (moderate risk of bias) | 138 | 144,345 | 46.49% [42.64; 50.39%] | 99.4% | 13.01 | 0.85 | 23,172 (137) | 0.06 | 0.27 | Egger's P = 0.04 | 30.50% [27.93; 33.19%] | ||
| Low quality (high risk of bias) | 10 | 852 | 42.60% [29.20; 57.19%] | 91.8% | 3.50 | 0.72 | 110 (9) | 0.93 | 0.58 | NS | NI | ||
Abbreviations: CI, Confidence interval. K = denotes the number of studies. N = denotes the number of participants. NA = Not applicable. NI = Not indicated. NS = Not Significant.
Methodological details.
I2 statistic describes the percentage of variation across studies due to heterogeneity rather than chance.
In a random-effects meta-analysis, the extent of variation among the effects observed in different studies (between-study variance) is referred to as -squared.
Cochran's Q, which is calculated as the weighted sum of squared differences between individual study effects and the pooled effect across studies, with the weights being those used in the pooling method.
Meta-regression was performed using Method of Moments Estimator for Random Effect Multivariate Meta-Analysis.
Publication bias was not observed in the Funnel plot.
Adjusted results were calculated using trill-and-fill.
Measures: AIS = Athens insomnia scale. BEARS = Bedtime issues, excessive daytime sleepiness, night awakenings, regularity and duration of sleep, and snoring. ISI = Insomnia severity index. MOS-SS = Medical outcomes study sleep scale. MSQ = Mini sleep questionnaire. PROMIS = Patient-reported outcomes measurement information system-sleep disturbance. PSQI = Pittsburgh sleep quality index. SCI = Sleep condition indicator. SCI-02 = Sleep condition indicator-02. SD = Self-developed. SDSC = Bruni scale/sleep disturbance scale for children. SNS = Subjective neurological symptoms. SQS = Sleep quality scale. SRSS = Self-rating scale of sleep. YSIS = Youth self-rating insomnia scale.
Bayesian meta-analysis of the global assessment of sleep disturbances revealed that the mean odds of quotes estimate was 0.68 [0.59; 0.77], = 1.09 [1.00; 1.18]. Thus, converting the odds obtained by Bayesian meta-analysis translates to an overall proportion of approximately 41%; detailed results are shown in Figure S7.
Assessment of sleep disturbances during COVID-19 by country
Seven countries had 10 or more studies and showed a statistically significant difference between the groups Q = 4808 (48), P = 0.001. Prevalence rate of sleep disturbances were as follow: China 30.32% [26.26; 34.72%], = 0.87, It = 99.70%; Italy 38.64% [28.86; 49.44%], = 1.67, I 2 = 99.80%; India 27.25% [19.00; 37.43%], = 0.89, It2 = 98.20%; USA 50.21% [41.06; 59.35%], τ2 = 0.52, I 2 = 98.80%; Turkey 44.18% [33.41; 55.53%], = 0.62, I 2 = 98.0%; Spain 58.59% [47.64; 68.76%], = 0.45, I 2 = 92.80%; and Saudi Arabia 51.10% [36.67; 65.35%], = 0.89, I 2 = 99.20%.
Age (older age) was a statistically significant moderator in China and Spain, P = 0.02 and P = 0.04, respectively. Detailed results are presented in Table 2 and Figure S8.
Assessment of sleep disturbances during COVID-19 by population
Subgroup analysis by population revealed that: patients infected with COVID-19 are the most affected population group by sleep disturbances with an overall pooled rate of 52.39% [41.69; 62.88%], K = 16, N = 6821, I 2 = 98.10%, H = 7.31, = 0.70, and τ = 0.84. Children and adolescents appeared the second most affected population group by sleep disturbances with an overall pooled rate of 45.96% [36.90; 55.30%], K = 13, N = 29,006, I 2 = 99.30%, H = 12.29, = 0.45, and = 0.67. Healthcare workers, special populations, and university students had a similar pooled prevalence rate of sleep disturbances during COVID-19. Specifically, data for healthcare workers K = 90, N = 63,685 showed an overall rate of sleep disturbances during COVID-19 pandemic of 42.47% [37.95; 47.12%], I 2, 99.1%, H = 0.47, = 0.82, and = 0.90. Special populations K = 23, N = 8023, showed an overall rate of sleep disturbances during COVID-19 pandemic of 41.50% [32.98; 50.56%], I 2 = 98.1%, H = 7.19, = 0.77, and = 0.88. University students K = 22, N = 21,880, showed an overall rate of sleep disturbances during COVID-19 pandemic of 41.16% [28.76; 54.79%], I 2 = 99.6%, H = 16.08, = 1.69, and = 1.30. Finally, the general population K = 121, N = 364,060 had the lowest rate of sleep disturbances during COVID-19 pandemic with an overall rate of 36.73% [32.32; 41.38%], I 2 = 99.8%, H = 23.17, = 1.18, and = 1.09. Forest plots of the results are shown in Fig. S9. Assessment of publication bias using funnel plots revealed no significant publication bias within each group, results was confirmed by Kendall's and Egger's tests. Detailed results are presented in Table 2.
Moderator analysis revealed that age (older age) was associated with a higher risk of sleep disturbances in healthcare workers P = 0.03; and sex (larger proportion of female) was associated with a higher risk of sleep disturbances in university students and special populations P = 0.04 and P = 0.05, respectively. Detailed results are presented in Table 2.
For the healthcare workers population, being a nurse or frontline or a nurse working in frontline (interaction term) was not a moderator of the size of sleep disturbances during the pandemic COVID-19 P = 0.15, P = 0.78, and P = 0.98, respectively.
Assessment of sleep disturbances during COVID-19 by used measure
Random-effects subgroup meta-analysis of sleep disturbances doing the COVID-19 pandemic by research measure used showed statistically different results between the groups Q = 51.81 (3), P = 0.001. The largest magnitude of sleep disturbances (poor sleep quality) was obtained by studies that have used the PSQI, K = 114 studies and yielded a prevalence rate of 51.87% [47.87; 55.84%], = 0.73, I 2 = 99.40%. ISI (moderate to severe insomnia) was used in K = 110 studies and yielded a prevalence rate of 30.98% [26.77; 35.54%], = 1.19, I 2 = 99.7%. AIS (insomnia) was used in K = 12 studies and yielded a prevalence rate of 47.22% [41.37; 53.15%], = 0.16, I 2 = 96.9%. Finally, other measures were used in K = 49 studies and yielded a prevalence rate 35.70% [30.38; 41.39%], = 0.72, I 2 = 99.6%.
Moderator analysis revealed that neither age (older age) nor sex (larger proportion of female) was associated with higher rates of sleep disturbances using any research measure.
Publication bias was detected in the studies that have used ISI and adjusted prevalence rate of sleep disturbances with K = 147 (with 37 added studies) is 18.38% [15.36; 21.85%], = 1.76 [1.58; 2.75], τ = 1.32 [1.25; 1.66], I 2 = 99.8%; H = 21.36 [20.99; 21.73], Q = 66,590 (146), P = 0.001. Detailed results are presented in Table 2, and Fig. S10.
Assessment of sleep disturbances during COVID-19 by lockdown status
About half the studies 123 (49.2%) collected data during no lockdown period and about 162 (64.8%) collected data during a local lockdown. Results for subgroups based on lockdown status using random-effects modelling showed that the prevalence rate of sleep disturbances during lockdown periods was higher 42.49% [38.21; 46.89%], = 1.31, I 2 = 99.8% compared to periods of non-lockdown 37.97% [34.42; 41.66%], = 0.74, I 2 = 99.4%. Test for subgroup differences showed that between groups differences did not reach statistical significance Q = 2.45 (1), P = 0.11. Detailed results are presented in Table 2, and Fig. S11.
Assessment of sleep disturbances during COVID-19 by year of publication
Papers published in 2021 reported a higher prevalence rate of sleep disturbances compared to papers published in 2020. The overall rate of sleep disturbances during COVID-19 pandemic in 2021 was 47.14% [43.01; 51.30%], = 0.80, I 2 = 99.6%. In 2020 the rate was lower with an overall prevalence of 36.20% [3252; 40.04%], = 1.16, I 2 = 99.7%. Test for subgroup differences between groups indicated that the difference is statistically significant Q = 14.42 (1), P = 0.001. Detailed results are presented in Table 2 and Fig. S12.
Assessment of sleep disturbances during COVID-19 by research design
Most 249 (87.4%) of the data were collected using a cross-sectional design; on the other hand, 25 (8.8) were collected using longitudinal designs, and only 11 (3.8%) were collected using case–control studies. The overall pooled prevalence rate obtained by longitudinal studies was the highest, 48.36% [43.14; 53.61%], = 0.25 [0.28; 1.26], τ = 0.51 [0.50; 1.12, I 2 = 98.0% [97.5%; 98.3%], H = 6.98 [6.37; 7.66], Q = 1171 (24), P = 0.001. Results obtained by cross-sectional studies followed, 40.26% [37.10; 43.49%], = 1.12 [0.86; 1.34], τ = 1.06 [0.92; 1.15], I 2 = 99.7%; H = 17.93 [17.66; 18.20], Q = 79,698 (248), P = 0.001. Case-control studies produced the lowest overall prevalence rate of sleep disturbances during the COVID-19 pandemic with an overall rate of 31 57% [18.23; 48.85%], = 1.50 [0.58; 4.33], = 1.22 [0.76; 2.08], I 2 = 99.7% [99.7%; 99.8%], H = 18.99 [17.68; 20.40], Q = 3606 (10), P = 0.001. Sex (larger proportion of female sex) was a statistically significant moderator in longitudinal studies P = 0.001. Detailed results are presented in Table 2, and Fig. S13.
Assessment of sleep disturbances during COVID-19 by methodological quality/risk of bias
Studies of moderate and low quality produced similar results, while studies of high quality produced a lower overall rate of sleep disturbances. Specifically, low quality studies K = 10, N = 852 showed an overall rate of sleep disturbances of 42.60% [29.20; 57.19%], = 0.7182 [0.34; 3.56], = 0.84 [0.58; 1.88], I 2 = 91.8% [87.1%; 94.8%], H = 3.50 [2.79; 4.40], Q = 110 (9), P = 0.001. Medium quality studies K = 138, N = 144,345 showed an overall rate of sleep disturbances of 46.49% [42.64; 50.39%], = 0.84 [0.74; 1.36], = 0.92 [0.86; 1.16], I 2 = 99.4%; H = 13.01 [12.68; 13.34], Q = 23,172 (137), P = 0.001. Finally, high quality studies K = 137, N = 348,278 showed an overall rate of sleep disturbances of 34.59% [30.58; 38.83%], = 1.17 [0.78; 1.37], = 1.08 [0.88; 1.17], I 2 = 99.8%; H = 21.01 [20.63; 21.39], Q = 60,013 (136), P = 0.001. Detailed results are presented in Table 2, and Fig. S14.
Discussion
The current systematic review and meta-analysis of 250 studies comprising about half-million participants revealed that during the COVID-19 pandemic, the pooled estimated prevalence of sleep disturbances (including poor sleep quality and insomnia), independent of any covariate, was 40%. Bayesian meta-analysis revealed the same overall estimate of sleep disturbances, providing reassurance that this is likely a reasonable estimate of COVID-19 related sleep disturbance. Publication bias was minimal, and neither age nor gender moderated the overall pooled prevalence rate. A statistically significant variation was observed between countries, and overall results ranged from approximately 30% in China and India to 60% in Spain. Patients infected with COVID-19 appeared the most affected by sleep disturbances, with an overall pooled rate of 52%. Children and adolescents were the second most affected group, with an overall rate of sleep disturbances of approximately 46%. Healthcare workers, university students, and special populations had a similar magnitude of the problem, with an overall rate of approximately 41%. The general population appeared the least affected by the pandemic, with an overall prevalence of sleep disturbances of about 36%. Poor sleep quality appeared as the main problem and explained 52% of the variance in the data.
Meeting clinical diagnostic scores for insomnia was observed in 30%–40% of the overall participants; therefore, accounting for approximately 80% of the variance of total sleep disturbances. Sleep disturbances were more prevalent during lockdown periods than non-lockdown periods, 38% and 43%, respectively. The difference according to lockdown status did not reach statistical significance. Finally, a statistically significant increase was observed in studies published in 2021 compared to studies published in 2020, 36% and 47%, respectively.
Our global finding on the pooled prevalence rate of sleep disturbances during COVID-19 (40%) is consistent with two previous meta-analyses [2,10]. In the review, meta-regression revealed that age and sex had no bearing on the estimated prevalence of sleep disturbances. This finding was also reported in previous reviews [2,3,10].
Statistically significant differences were observed between countries, implying that the emergence of COVID-19, the local community transmission rate of the disease, measures taken to control the virus, and the pattern of media use [293] contributed to the magnitude of sleep disturbances. Recent data from COVIDiSTRESS Global Survey showed that stress and stress-related symptoms are positively associated with living in a nation or region where COVID-19 is more severe [294]. Additionally, cross-country discrepancies in public perception of stress have been reported [295]. The overlapping prevalence between psychological distress symptoms [296] and our findings on sleep disturbances suggests that there is a two-way relationship between sleep disturbances and psychiatric comorbidities, which indicates sleep experts should consider treating comorbidities in sleep disturbances and vice versa.
COVID19 patients can be expected to have the highest frequency of sleep disturbances (about 52%) because of the core symptoms of the disease, including cough, fever, inflammation, and shortness of breath, all of which are related to sleep disturbances [2]. The increased risk of sleep disturbances in COVID19 patients is likely also the result of body pain and the side effects of used medications.
Before the pandemic, a meta-analysis documented that 25% of normally developing children had sleep disturbances [297]. Therefore, the high prevalence of sleep disturbances among children (46%) observed during the pandemic is alarming. The most significant negative effect of the lockdown (schools closures), according to several studies, was a delay in the start of sleep and wake-up time [7]. Increased anxiety, inability to do outdoor activities, remote learning, and lack of in-person social connections all led to more time spent using technology, especially during the pre-sleep period [298]. Limited exposure to sunshine and extended exposure to screen blue and bright light from phones and computer screens (for school or play) may lead to disturbed circadian rhythms [299].
Previous reviews concluded that healthcare workers are among the populations most affected by sleep disturbances during the pandemic [2,4,5,10]. In addition, recent data demonstrated that during the pandemic, healthcare workers have a high prevalence of perceived stress, anxiety, and depression [53,300]. The present review documented that healthcare workers, university students, and special populations had a similar magnitude of sleep disturbances, with an overall rate of approximately 41%.
A key component in understanding sleep disturbances during the pandemic was shown to be lockdown. Current evidence suggests that social isolation and loneliness can harm mental health [301], and affect sleep quality [302,303].
Another interesting finding is that the reported prevalence of sleep disturbances in publications in 2021 appeared to be higher than in 2020, suggesting that the COVID-19 pandemic is continuing to have a negative impact on sleep. Since 2020, multiple epidemic waves with increasing infected cases [304], and the identification, spread, and impact of new COVID variants have led to “pandemic fatigue” [305]. Despite the availability of COVID-19 vaccines at the end of 2020, new waves could not be avoided across the globe, and the expected return to normal life now appears to be delayed or even uncertain. Moreover, several populations have experienced successive lockdowns since, which the current meta-analysis demonstrates is one of the major factors associated with COVID-19-related sleep disturbances. Hence, as the pandemic persists, more people are likely to develop sleep disturbances [193]. Findings that emerged from longitudinal follow-up studies revealed a significant worsening of sleep parameters over observational waves [306].
The findings of this review have several practical and research implications. First, screening programs and countermeasures for sleep disturbances must be developed and executed to help various groups detect and overcome sleep-related impairment. Specific programs need to be tailored for different populations, e.g., healthcare workers, children and adolescents, university students, and special populations, such as pregnant women, etc. Evidence-based strategies, e.g., cognitive behavioral therapy for insomnia [307], meditation [308], sports interventions [309], and wellness interventions [310], can be included in self-help applications, and healthcare staff can be trained to detect and treat sleep issues in various populations [311]. Second, special attention needs to be paid to insomnia as a formal disorder accounting for approximately 80% of the variance of sleep disturbances. Future primary and secondary research need to identify the magnitude of insomnia by severity; longitudinal studies are required to determine if insomnia is short-term or long-term. Third, our review showed that data saturation is achieved in certain populations, e.g., healthcare workers and the general populations; therefore, at least some research focus needs to be shifted to novel populations, e.g., post-COVID-19 populations, homeless individuals, those rough sleeping, and others. Fourthly, formal sleep assessment needs to be part of the comprehensive psychiatric evaluation for individuals seeking psychiatric services. Empirical results of a recent review documented the strong association between psychological distress and sleep disturbances [10], implying that both issues are best assessed and treated simultaneously.
The current review has several strengths. First, the rate of sleep disturbances has been assessed across several new populations that never received attention in previous reviews, e.g., special populations, university students, and children and adolescents. Second, robust statistical tests were used to handle bias, detect outliers, and examine heterogeneity. Third, because the pooled sample size was very large and the participants were recruited from many countries, the generalizability of the current review's conclusions is likely to be strong.
There are a few drawbacks to this review. First, the magnitude of heterogeneity in this meta-analysis was large. This is to be expected in a large epidemiological meta-analysis. The use of random-effects modeling was anticipated to deal with issues related to the effects of evaluating many studies that do not all follow the same pattern, but instead follow a distribution. Future reviews need finetuned aggregate data, and individual patient data (IPD) meta-analyses are desirable and should be encouraged to work out, analyze and present different aspects of sleep disturbances. Second, we included only limited moderators. When correcting for moderators, future reviews should expand this exploration using other lifestyle variables, including physical activity, smoking, and substance use, focusing on adjusting for stress-related illnesses such as posttraumatic stress disorder, adjustment disorders, anxiety, and depression. Besides sleep disturbances, there are many types of wakefulness disturbances that all have to do with staying awake at a time that is desirable or socially appropriate. These were beyond the scope of our analyses and discussion. Further reviewers are encouraged to address this under-investigated topic.
Conclusion
During the COVID-19 pandemic, sleep disturbances are common. Four in every ten individuals reported a sleep problem, and the main complaint is insomnia. Patients infected with COVID-19 and children and adolescents appeared to be the most affected groups. Healthcare workers, special populations, and university students had a similar but somewhat lower rate of sleep disturbances, while the general population appears to be the least affected. Lockdown is associated with a larger magnitude of sleep disturbances. More research is needed, particularly longitudinal studies, to establish the courses of sleep disturbances over time in these and populations, and such studies should pay particular attention to moderators, which may exacerbate sleep problem prevalence.
Practice points.
• Sleep disturbances are common during the COVID-19 pandemic. The most affected groups were patients infected with the disease, children and adolescents, and university students. It is essential to develop and implement screening programs and countermeasures to help various groups detect and overcome sleep disturbances.
• There is a need to pay special attention to insomnia as a formal sleep disorder that accounts for 80% of sleep loss.
• During the pandemic, individuals seeking psychiatric treatment need a formal sleep assessment as part of their comprehensive evaluation.
Research agenda.
• It is necessary to conduct future primary and secondary research to identify the severity of insomnia; longitudinal studies are needed to determine if insomnia is short-term or long-term.
• Meta-analyses of individual patient data (IPD) should be encouraged in future reviews and fine-tuned aggregate parameters should be included.
• The process of adjusting for moderators should expand the analysis by adding physical activity, smoking, and substance use, focusing on the prevalence of stress-related disorders.
Author agreement
All authors were involved in writing the paper and have seen and approved the manuscript.
Ethical statement
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study (meta-analysis) formal consent is not required.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors do not have any conflicts of interest to disclose.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.smrv.2022.101591.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Ramar K., Malhotra R.K., Carden K.A., Martin J.L., Abbasi-Feinberg F., Aurora R.N., et al. Sleep is essential to health: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2021 Oct 1;17(10):2115–2119. doi: 10.5664/jcsm.9476. PMID: 34170250; PMCID: PMC8494094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrami H., BaHammam A.S., Bragazzi N.L., Saif Z., Faris M., Vitiello M.V. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17:299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimoradi Z., Gozal D., Tsang H.W.H., Lin C.Y., Broström A., Ohayon M.M., et al. Gender-specific estimates of sleep problems during the COVID-19 pandemic: systematic review and meta-analysis. J Sleep Res. 2021 doi: 10.1111/jsr.13432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Khazaie H., Hosseinian-Far A., Ghasemi H., Mohammadi M., Shohaimi S., et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Glob Health. 2020;16:92. doi: 10.1186/s12992-020-00620-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Ripoll M.J., Zamanillo-Campos R., Castro A., Fiol-de Roque M.A., Ricci-Cabello I. Insomnia and sleep quality in healthcare workers fighting against COVID-19: a systematic review of the literature and meta-analysis. Actas Esp Psiquiatr. 2021;49:155–179. [PubMed] [Google Scholar]
- Al Maqbali M., Al Sinani M., Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J Psychosom Res. 2021;141:110343. doi: 10.1016/j.jpsychores.2020.110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma M., Aggarwal S., Madaan P., Saini L., Bhutani M. Impact of COVID-19 pandemic on sleep in children and adolescents: a systematic review and meta-analysis. Sleep Med. 2021;84:259–267. doi: 10.1016/j.sleep.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia L., Chen C., Liu Z., Luo X., Guo C., Liu Z., et al. Prevalence of sleep disturbances and sleep quality in Chinese healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatr. 2021;12:646342. doi: 10.3389/fpsyt.2021.646342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. 2021;1486:90–111. doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimoradi Z., Broström A., Tsang H.W.H., Griffiths M.D., Haghayegh S., Ohayon M.M., et al. Sleep problems during COVID-19 pandemic and its' association to psychological distress: a systematic review and meta-analysis. Eclin Med. 2021:36. doi: 10.1016/j.eclinm.2021.100916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 13.PLOTCON. WebPlotDigitizer. 2017. https://automeris.io/WebPlotDigitizer/ Accessed September 2021. [Google Scholar]
- 14.Buysse D.J., Reynolds C.F., 3rd, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 15.Pedder H., Sarri G., Keeney E., Nunes V., Dias S. Data extraction for complex meta-analysis (DECiMAL) guide. Syst Rev. 2016;5:212. doi: 10.1186/s13643-016-0368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luchini C., Stubbs B., Solmi M., Veronese N. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa scale. World J Meta-Anal. 2017;5:80–84. [Google Scholar]
- 17.Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 18.DerSimonian R., Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clopper C.J., Pearson E.S. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404–413. [Google Scholar]
- 20.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cochran W.G. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. [Google Scholar]
- 23.Higgins J.P., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., et al. John Wiley & Sons; 2019. Cochrane handbook for systematic reviews of interventions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baujat B., Mahé C., Pignon J.-P., Hill C. A graphical method for exploring heterogeneity in meta-analyses: application to a meta-analysis of 65 trials. Stat Med. 2002;21:2641–2652. doi: 10.1002/sim.1221. [DOI] [PubMed] [Google Scholar]
- 25.Lewis S., Clarke M. Forest plots: trying to see the wood and the trees. BMJ. 2001;322:1479–1480. doi: 10.1136/bmj.322.7300.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hedges L.V., Olkin I. Academic Press; 2014. Statistical methods for meta-analysis. [Google Scholar]
- 27.Viechtbauer W., Cheung M.W. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- 28.Sterne J.A.C., Sutton A.J., Ioannidis J.P.A., Terrin N., Jones D.R., Lau J., et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- 29.Kendall M., Gibbons J.D. A Charles Griffin Title; London: 1990. Rank correlation methods edward arnold. A division of Hodder & Stoughton; pp. 29–50. [Google Scholar]
- 30.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duval S., Tweedie R. A nonparametric "trim and fill" method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95:89–98. [Google Scholar]
- 32.Simonsohn U., Nelson L.D., Simmons J.P. P-curve: a key to the file-drawer. J Exp Psychol Gen. 2014;143:534–547. doi: 10.1037/a0033242. [DOI] [PubMed] [Google Scholar]
- 33.Simonsohn U., Nelson L.D., Simmons J.P. p-Curve and effect size: correcting for publication bias using only significant results. Perspect Psychol Sci. 2014;9:666–681. doi: 10.1177/1745691614553988. [DOI] [PubMed] [Google Scholar]
- 34.Olkin I., Dahabreh I.J., Trikalinos T.A. GOSH - a graphical display of study heterogeneity. Res Synth Methods. 2012;3:214–223. doi: 10.1002/jrsm.1053. [DOI] [PubMed] [Google Scholar]
- 35.Sutton A.J., Abrams K.R. Bayesian methods in meta-analysis and evidence synthesis. Stat Methods Med Res. 2001;10:277–303. doi: 10.1177/096228020101000404. [DOI] [PubMed] [Google Scholar]
- 36.Spiegelhalter D.J. Incorporating Bayesian ideas into health-care evaluation. Stat Sci. 2004;19:156–174. [Google Scholar]
- 37.Lunn D., Barrett J., Sweeting M., Thompson S. Fully Bayesian hierarchical modelling in two stages, with application to meta-analysis. J Roy Stat Soc: C Appl Stat. 2013;62:551–572. doi: 10.1111/rssc.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.R. 4.1.0 . In: R foundation for statistical computing. Team R.C., editor. Language and Environment Forstatistical Computing; Vienna, Austria A: 2021. [Google Scholar]
- 39.Balduzzi S., Rücker G., Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Base Ment Health. 2019;22:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Software. 2010;36:1–48. [Google Scholar]
- 41.Röver C. 2017. Bayesian random-effects meta-analysis using the bayesmeta R package. arXiv preprint arXiv:171108683. [Google Scholar]
- 42.McGuinness L.A., Higgins J.P. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12:55–61. doi: 10.1002/jrsm.1411. [DOI] [PubMed] [Google Scholar]
- 43.Abbas A., Al-Otaibi T., Gheith O.A., Nagib A.M., Farid M.M., Walaa M. Sleep quality among healthcare workers during the COVID-19 pandemic and its impact on medical errors: Kuwait experience. Turk Thorac J. 2021;22:142. doi: 10.5152/TurkThoracJ.2021.20245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abdellah M.M., Khalil M.F., Alhafiz A. Prevalence of poor sleep quality among physicians during the COVID-19 pandemic. Cureus. 2021;13 doi: 10.7759/cureus.12948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abdulah D.M., Musa D.H. Insomnia and stress of physicians during COVID-19 outbreak. Sleep Med X. 2020;2:100017. doi: 10.1016/j.sleepx.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Agberotimi S.F., Akinsola O.S., Oguntayo R., Olaseni A.O. Interactions between socioeconomic status and mental health outcomes in the nigerian context amid covid-19 pandemic: a comparative study. Front Psychol. 2020;11:2655. doi: 10.3389/fpsyg.2020.559819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ahmad A., Rahman I., Agarwal M. Early psychosocial predictors of mental health among Indians during coronavirus disease 2019 outbreak. J Health Sci. 2020;10(2):147–156. doi: 10.17532/jhsci.2020.950. [DOI] [Google Scholar]
- 48.Akıncı T., Başar H.M. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep Med. 2021;80:167–170. doi: 10.1016/j.sleep.2021.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al Ammari M., Sultana K., Thomas A., Al Swaidan L., Al Harthi N. Mental health outcomes amongst health care workers during COVID 19 pandemic in Saudi Arabia. Front Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.619540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Al Maqbali M., Al Khadhuri J. Psychological impact of the coronavirus 2019 (COVID-19) pandemic on nurses. Jpn J Nurs Sci. 2021 doi: 10.1111/jjns.12417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Al-Ajlouni Y.A., Park S.H., Alawa J., Shamaileh G., Bawab A., El-Sadr W.M., et al. Anxiety and depressive symptoms are associated with poor sleep health during a period of COVID-19-induced nationwide lockdown: a cross-sectional analysis of adults in Jordan. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-041995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alamrawy R.G., Fadl N., Khaled A. Psychiatric morbidity and dietary habits during COVID-19 pandemic: a cross-sectional study among Egyptian Youth (14–24 years) Middle East Curr Psychiatr. 2021;28:1–10. [Google Scholar]
- 53.AlAteeq D., Almokitib A., Mohideen M., AlBlowi N., Fayed A., Alshahrani S.M. Stress, sleep, and use of sleep aids among physicians during the COVID-19 pandemic. J Nat Sci Med. 2021;4:197. [Google Scholar]
- 54.Alessi J., De Oliveira G.B., Franco D.W., Do Amaral B.B., Becker A.S., Knijnik C.P., et al. Mental health in the era of COVID-19: prevalence of psychiatric disorders in a cohort of patients with type 1 and type 2 diabetes during the social distancing. Diabetol Metab Syndrome. 2020;12:1–10. doi: 10.1186/s13098-020-00584-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alfonsi V., Gorgoni M., Scarpelli S., Zivi P., Sdoia S., Mari E., et al. COVID-19 lockdown and poor sleep quality: not the whole story. J Sleep Res. 2021 doi: 10.1111/jsr.13368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alharbi A.S., Alshahrani S.M., Alsaadi M.M., Al-Jahdali H.H., Wali S.O., BaHammam A.S. Sleep quality and insomnia during the COVID-19 lockdown among the Saudi public. Saudi Med J. 2021;42:384–390. doi: 10.15537/smj.2021.42.4.20200735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ali M., Uddin Z., Ahsan N.F., Haque M.Z., Bairagee M., Khan S.A., et al. Prevalence of mental health symptoms and its effect on insomnia among healthcare workers who attended hospitals during COVID-19 pandemic: a survey in Dhaka city. Heliyon. 2021;7 doi: 10.1016/j.heliyon.2021.e06985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Almater A.I., Tobaigy M.F., Younis A.S., Alaqeel M.K., Abouammoh M.A. Effect of 2019 coronavirus pandemic on ophthalmologists practicing in Saudi Arabia: a psychological health assessment. Middle East Afr J Ophthalmol. 2020;27:79. doi: 10.4103/meajo.MEAJO_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alnofaiey Y.H., Alshehri H.A., Alosaimi M.M., Alswat S.H., Alswat R.H., Alhulayfi R.M., et al. Sleep disturbances among physicians during COVID-19 pandemic. BMC Res Notes. 2020;13:1–7. doi: 10.1186/s13104-020-05341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alomayri W., Alanazi N., Faraj F. Correlation between atopic dermatitis and sleep quality among adults in Saudi Arabia. Cureus. 2020;12 doi: 10.7759/cureus.12051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alqahtani S.S., Banji D., Banji O.J. Saudi Pharmaceutical Journal; 2021. A survey assessing sleep efficiency among Saudis during COVID-19 home confinement using the Pittsburgh sleep quality index: a call for health education. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.AlRasheed M.M., Alkadir A.M., Shuqiran K.I.B., Al-Aqeel S., Jahrami H.A., BaHammam A.S. The impact of quarantine on sleep quality and psychological distress during the COVID-19 pandemic. Nat Sci Sleep. 2021;13:1037. doi: 10.2147/NSS.S313373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alshekaili M., Hassan W., Al-Said N., Alsulimani F., Kumar Jayapal S., Al-Mawali A., et al. 2020. Factors associated with mental health outcomes in Oman during COVID-19: frontline vs non-frontline healthcare workers. Available at: SSRN 3624265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ammar A., Trabelsi K., Brach M., Chtourou H., Boukhris O., Masmoudi L., et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: insights from the ECLB-COVID19 multicentre study. Biol Sport. 2021;38:9. doi: 10.5114/biolsport.2020.96857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Amra B., Salmasi M., Soltaninejad F., Sami R., Nickpour M., Mansourian M., et al. Healthcare workers' sleep and mood disturbances during COVID-19 outbreak in an Iranian referral center. Sleep Breath. 2021:1–8. doi: 10.1007/s11325-021-02312-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Assenza G., Lanzone J., Brigo F., Coppola A., Di Gennaro G., Di Lazzaro V., et al. Epilepsy care in the time of COVID-19 pandemic in Italy: risk factors for seizure worsening. Front Neurol. 2020;11:737. doi: 10.3389/fneur.2020.00737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barutcu Atas D., Aydin Sunbul E., Velioglu A., Tuglular S. The association between perceived stress with sleep quality, insomnia, anxiety and depression in kidney transplant recipients during Covid-19 pandemic. PLoS One. 2021;16 doi: 10.1371/journal.pone.0248117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bacaro V., Chiabudini M., Buonanno C., De Bartolo P., Riemann D., Mancini F., et al. Insomnia in the Italian population during Covid-19 Outbreak: a snapshot on one major risk factor for Depression and Anxiety. Front Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.579107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Badellino H., Gobbo M.E., Torres E., Aschieri M.E. Early indicators and risk factors associated with mental health problems during COVID-19 quarantine: is there a relationship with the number of confirmed cases and deaths? Int J Soc Psychiatr. 2020;67(5):567–575. doi: 10.1177/0020764020966020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang X., Jiang X., Huang Q., Wang H., Gurarie D., Ndeffo-Mbah M., et al. Risk factors of SARS-CoV-2 infection in healthcare workers: a retrospective study of a nosocomial outbreak. Sleep Med X. 2020;2:100028. doi: 10.1016/j.sleepx.2020.100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bajaj S., Blair K.S., Schwartz A., Dobbertin M., Blair R.J.R. Worry and insomnia as risk factors for depression during initial stages of COVID-19 pandemic in India. PLoS One. 2020;15 doi: 10.1371/journal.pone.0243527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barrea L., Pugliese G., Framondi L., Di Matteo R., Laudisio D., Savastano S., et al. Does Sars-Cov-2 threaten our dreams? Effect of quarantine on sleep quality and body mass index. J Transl Med. 2020;18:1–11. doi: 10.1186/s12967-020-02465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barua L., Zaman M.S., Omi F.R., Faruque M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: a cross-sectional study. F1000Research. 2020;9 doi: 10.12688/f1000research.27189.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Başkan S.A., Güneş D. The effect of stress perceived by adults due to the COVID-19 pandemic on their sleep quality. J Turk Sleep Med. 2021;1:57–66. [Google Scholar]
- 75.Beck F., Léger D., Fressard L., Peretti-Watel P., Verger P., Group C. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J Sleep Res. 2021;30:e13119. doi: 10.1111/jsr.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Benham G. Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Health. 2021 Aug;37(3):504–515. doi: 10.1002/smi.3016. Epub 2020 Dec 19. PMID: 33315301. [DOI] [PubMed] [Google Scholar]
- 77.Bezerra C.B., Saintrain MVdL., Braga D.R.A., Santos FdS., Lima A.O.P., Brito EHSd, et al. Psychosocial impact of COVID-19 self-isolation on the Brazilian population: a preliminary cross-sectional analysis. Saúde Soc. 2020;29 [Google Scholar]
- 78.Bhat B.A., Mir R.A., Hussain A., Shah I.R. Depressive and anxiety symptoms, quality of sleep, and coping during the 2019 coronavirus disease pandemic in general population in Kashmir. Middle East Curr Psychiatr. 2020;27:1–10. [Google Scholar]
- 79.Bigalke J.A., Greenlund I.M., Carter J.R. Sex differences in self-report anxiety and sleep quality during COVID-19 stay-at-home orders. Biol Sex Differ. 2020;11:1–11. doi: 10.1186/s13293-020-00333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Blekas A., Voitsidis P., Athanasiadou M., Parlapani E., Chatzigeorgiou A.F., Skoupra M., et al. COVID-19: PTSD symptoms in Greek health care professionals. Psycol Trauma: Theor, Res, Pract, Pol. 2020;12:812. doi: 10.1037/tra0000914. [DOI] [PubMed] [Google Scholar]
- 81.Bohlken J., Schömig F., Seehagen T., Köhler S., Gehring K., Roth-Sackenheim C., et al. Experience of practice-based psychiatrists and neurologists during the COVID-19 pandemic. Psychiatr Prax. 2020;47:214–217. doi: 10.1055/a-1159-5575. [DOI] [PubMed] [Google Scholar]
- 82.Brito-Marques JMdAM., Franco C.M.R., Brito-Marques PRd, Martinez S.C.G., Prado GFd. Impact of COVID-19 pandemic on the sleep quality of medical professionals in Brazil. Arq Neuro Psiquiatr. 2021;79:149–155. doi: 10.1590/0004-282X-anp-2020-0449. [DOI] [PubMed] [Google Scholar]
- 83.Caballero-Domínguez C.C., De Luque-Salcedo J.G., Campo-Arias A. Social capital and psychological distress during Colombian coronavirus disease lockdown. J Community Psychol. 2021;49:691–702. doi: 10.1002/jcop.22487. [DOI] [PubMed] [Google Scholar]
- 84.Cai Q., Feng H., Huang J., Wang M., Wang Q., Lu X., et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J Affect Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cai Z., Cui Q., Liu Z., Li J., Gong X., Liu J., et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. 2020;131:132–137. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cellini N., Di Giorgio E., Mioni G., Di Riso D. Sleep and psychological difficulties in Italian school-age children during COVID-19 lockdown. J Pediatr Psychol. 2021;46:153–167. doi: 10.1093/jpepsy/jsab003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29 doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cellini N., Conte F., De Rosa O., Giganti F., Malloggi S., Reyt M., et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021;77:112–119. doi: 10.1016/j.sleep.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chatterjee S.S., Chakrabarty M., Banerjee D., Grover S., Chatterjee S.S., Dan U. Stress, sleep and psychological impact in healthcare workers during the early phase of COVID-19 in India: a factor analysis. Front Psychol. 2021;12:473. doi: 10.3389/fpsyg.2021.611314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen X., Wang L., Liu L., Jiang M., Wang W., Zhou X., et al. Factors associated with psychological distress among patients with breast cancer during the COVID-19 pandemic: a cross-sectional study in Wuhan, China. Support Care Cancer. 2021:1–10. doi: 10.1007/s00520-021-05994-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cheng F.-F., Zhan S.-H., Xie A.-W., Cai S.-Z., Hui L., Kong X.-X., et al. Anxiety in Chinese pediatric medical staff during the outbreak of Coronavirus Disease 2019: a cross-sectional study. Transl Pediatr. 2020;9:231. doi: 10.21037/tp.2020.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cheng C., Ebrahimi O.V., Lau Yc. Maladaptive coping with the infodemic and sleep disturbance in the COVID-19 pandemic. J Sleep Res. 2020:e13235. doi: 10.1111/jsr.13235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chi X., Liang K., Chen S.-T., Huang Q., Huang L., Yu Q., et al. Mental health problems among Chinese adolescents during the COVID-19: the importance of nutrition and physical activity. Int J Clin Health Psychol. 2021;21:100218. doi: 10.1016/j.ijchp.2020.100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chouchou F., Augustini M., Caderby T., Caron N., Turpin N.A., Dalleau G. The importance of sleep and physical activity on well-being during COVID-19 lockdown: reunion island as a case study. Sleep Med. 2021;77:297–301. doi: 10.1016/j.sleep.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Coiro M.J., Asraf K., Tzischinsky O., Hadar-Shoval D., Tannous-Haddad L., Wolfson A.R. Sleep quality and COVID-19-related stress in relation to mental health symptoms among Israeli and US adults. Sleep Health. 2021;7:127–133. doi: 10.1016/j.sleh.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 97.Cui Q., Cai Z., Li J., Liu Z., Sun S., Chen C., et al. The psychological pressures of breast cancer patients during the COVID-19 outbreak in China—a comparison with frontline female nurses. Front Psychiatr. 2020;11:1462. doi: 10.3389/fpsyt.2020.559701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Czeisler M.É., Wiley J.F., Facer-Childs E.R., Robbins R., Weaver M.D., Barger L.K., et al. Mental health, substance use, and suicidal ideation during a prolonged COVID-19-related lockdown in a region with low SARS-CoV-2 prevalence. J Psychiatr Res. 2021 Aug;140:533–544. doi: 10.1016/j.jpsychires.2021.05.080. PMCID: PMC8177437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dai L.-L., Wang X., Jiang T.-C., Li P.-F., Wang Y., Wu S.-J., et al. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang shelter hospital in Wuhan, China. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Das R., Hasan M.R., Daria S., Islam M.R. Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Daşdemir K.A., Suner Keklik S. Physical activity, sleep and quality of life of patients with asthma during the COVID-19 pandemic. J Asthma. 2021:1–11. doi: 10.1080/02770903.2021.1931303. [DOI] [PubMed] [Google Scholar]
- 102.de Medeiros G., Artismo R.S., Coelho P., da Silveira B., Souza Filho V.P.P., Branco J.H.L., et al. Did social isolation due to COVID-19 interfere with the quality of sleep and excessive daytime sleepiness in individuals with grade III obesity about to enter a surgical prehabilitation program? An observational study. Metabol Open. 2021:100104. doi: 10.1016/j.metop.2021.100104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Demartini B., Nisticò V., D'Agostino A., Priori A., Gambini O. Early psychiatric impact of COVID-19 pandemic on the general population and healthcare workers in Italy: a preliminary study. Front Psychiatr. 2020:11. doi: 10.3389/fpsyt.2020.561345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Du C., Zan M.C.H., Cho M.J., Fenton J.I., Hsiao P.Y., Hsiao R., et al. Health behaviors of higher education students from 7 countries: poorer sleep quality during the COVID-19 pandemic predicts higher dietary risk. Clock Sleep. 2021;3:12–30. doi: 10.3390/clockssleep3010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Duran S., Ö Erkin. Psychologic distress and sleep quality among adults in Turkey during the COVID-19 pandemic. Prog Neuro Psychopharmacol Biol Psychiatr. 2021;107:110254. doi: 10.1016/j.pnpbp.2021.110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Elhadi M., Alsoufi A., Msherghi A., Alshareea E., Ashini A., Nagib T., et al. Psychological health, sleep quality, behavior, and internet use among people during the COVID-19 pandemic: a cross-sectional study. Front Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.632496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Abd-ElHafeez S., Meira e Cruz M., Gouda S., Nofal M., Fayed A., Ghazy R., et al. Sleep quality and anxiety among Egyptian population during COVID-19 pandemic. Sleep Sci. 2021 doi: 10.5935/1984-0063.20210020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Elkholy H., Tawfik F., Ibrahim I., Salah El-din W., Sabry M., Mohammed S., et al. Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: a call for action. Int J Soc Psychiatr. 2020 doi: 10.1177/0020764020960192. [DOI] [PubMed] [Google Scholar]
- 109.Essangri H., Sabir M., Benkabbou A., Majbar M.A., Amrani L., Ghannam A., et al. Predictive factors for impaired mental health among medical students during the early stage of the COVID-19 pandemic in Morocco. Am J Trop Med Hyg. 2021;104:95. doi: 10.4269/ajtmh.20-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Falkingham J., Evandrou M., Qin M., Vlachantoni A. 2020. Sleepless in lockdown': unpacking differences in sleep loss during the coronavirus pandemic in the UK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fekih-Romdhane F., Snene H., Jebri A., Rhouma M.B., Cheour M. Psychological impact of the pandemic COVID-19 outbreak among medical residents in Tunisia. Asian J Psychiatr. 2020;53:102349. doi: 10.1016/j.ajp.2020.102349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fidanci I., derinöz Güleryüz O., Fidanci I. An analysis on sleep quality of the healthcare professionals during the covid-19 pandemic. Acta Med. 2020;36:3797. [Google Scholar]
- 113.Di Filippo P., Attanasi M., Dodi G., Porreca A., Raso M., Di Pillo S., et al. Evaluation of sleep quality and anxiety in Italian pediatric healthcare workers during the first wave of COVID-19 pandemic. BMC Res Notes. 2021;14:1–8. doi: 10.1186/s13104-021-05621-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Florin M., Pinar U., Chavigny E., Bouaboula M., Jarboui L., Coulibaly A., et al. Socio-economic and psychological impact of the COVID-19 outbreak on private practice and public hospital radiologists. Eur J Radiol. 2020;132:109285. doi: 10.1016/j.ejrad.2020.109285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Franceschini C., Musetti A., Zenesini C., Palagini L., Scarpelli S., Quattropani M.C., et al. Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy. Front Psychol. 2020;11:3072. doi: 10.3389/fpsyg.2020.574475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S., et al. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl Psychiatry. 2020;10:1–9. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Garcia-Priego B.A., Triana-Romero A., Pinto-Galvez S.M., Duran-Ramos C., Salas-Nolasco O., Reyes M.M., et al. Anxiety, depression, attitudes, and internet addiction during the initial phase of the 2019 coronavirus disease (COVID-19) epidemic: a cross-sectional study in México. medRxiv. 2020 doi: 10.1101/2020.05.10.20095844. [DOI] [Google Scholar]
- 118.Garriga-Baraut T. COVID-19 pandemic and sleep disorders among pediatric and adolescent asthmatic patients. TP73 TP073 Pediatr Sleep: Am Thorac Soc. 2021:A3344. [A] [Google Scholar]
- 119.Gaş S., Ekşi Özsoy H., Cesur Aydın K. The association between sleep quality, depression, anxiety and stress levels, and temporomandibular joint disorders among Turkish dental students during the COVID-19 pandemic. CRANIO®. 2021:1–6. doi: 10.1080/08869634.2021.1883364. [DOI] [PubMed] [Google Scholar]
- 120.Ge F., Di Zhang L.W., Mu H. Predicting psychological state among Chinese Undergraduate Students in the COVID-19 Epidemic: a longitudinal study using a machine learning. Neuropsychiatric Dis Treat. 2020;16:2111. doi: 10.2147/NDT.S262004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Genta F.D., Neto G.B.R., Sunfeld J.P.V., Porto J.F., Xavier A.D., Moreno C.R.C., et al. COVID-19 pandemic impact on sleep habits, chronotype, and health-related quality of life among high school students: a longitudinal study. J Clin Sleep Med. 2021;17:1371–1377. doi: 10.5664/jcsm.9196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Giardino D.L., Huck-Iriart C., Riddick M., Garay A. The endless quarantine: the impact of the COVID-19 outbreak on healthcare workers after three months of mandatory social isolation in Argentina. Sleep Med. 2020;76:16–25. doi: 10.1016/j.sleep.2020.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Goodman-Casanova J.M., Dura-Perez E., Guzman-Parra J., Cuesta-Vargas A., Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. J Med Internet Res. 2020;22 doi: 10.2196/19434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Goularte J.F., Serafim S.D., Colombo R., Hogg B., Caldieraro M.A., Rosa A.R. COVID-19 and mental health in Brazil: psychiatric symptoms in the general population. J Psychiatr Res. 2021;132:32–37. doi: 10.1016/j.jpsychires.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gu Y., Zhu Y., Xu G. Factors associated with mental health outcomes among health care workers in the Fangcang shelter hospital in China. Int J Soc Psychiatr. 2020 doi: 10.1177/0020764020975805. [DOI] [PubMed] [Google Scholar]
- 126.Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Publ Health. 2020;17:4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Guo J., Feng X.L., Wang X.H., van IJzendoorn M.H. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int J Environ Res Publ Health. 2020;17:3857. doi: 10.3390/ijerph17113857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gupta R., Grover S., Basu A., Krishnan V., Tripathi A., Subramanyam A., et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatr. 2020;62:370. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Haravuori H., Junttila K., Haapa T., Tuisku K., Kujala A., Rosenström T., et al. Personnel well-being in the Helsinki university hospital during the COVID-19 pandemic—a prospective cohort study. Int J Environ Res Publ Health. 2020;17:7905. doi: 10.3390/ijerph17217905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.He Q., Fan B., Xie B., Liao Y., Han X., Chen Y., et al. Mental health conditions among the general population, healthcare workers and quarantined population during the coronavirus disease 2019 (COVID-19) pandemic. Psychol Health Med. 2021:1–13. doi: 10.1080/13548506.2020.1867320. [DOI] [PubMed] [Google Scholar]
- 132.Hendrickson R.C., Slevin R.A., Chang B.P., Sano E., McCall C.A., Raskind M.A. The impact of working during the Covid-19 pandemic on health care workers and first responders: mental health, function, and professional retention. medRxiv. 2020 doi: 10.1101/2020.12.16.20248325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.San Martin A.H., Serrano J.P., Cambriles T.D., Arias E.M.A., Méndez J.M., del Yerro Álvarez M.J., et al. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Med. 2020;75:388–394. doi: 10.1016/j.sleep.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Huang L., Lei W., Liu H., Hang R., Tao X., Zhan Y. Nurses' sleep quality of “Fangcang” hospital in China during the COVID-19 pandemic. Int J Ment Health Addiction. 2020:1–11. doi: 10.1007/s11469-020-00404-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Huang Y., Wang Y., Zeng L., Yang J., Song X., Rao W., et al. Prevalence and correlation of anxiety, insomnia and somatic symptoms in a Chinese population during the COVID-19 epidemic. Front Psychiatr. 2020;11:894. doi: 10.3389/fpsyt.2020.568329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hussen B., Qader S., Aziz K., Hazha J., Qader A., Jamal A. 2021. The assessment of lifestyle change due to COVID-19 pandemic in northern Iraq. [Google Scholar]
- 138.Idrissi A.J., Lamkaddem A., Benouajjit A., El Bouaazzaoui M.B., El Houari F., Alami M., et al. Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep Med. 2020;74:248–253. doi: 10.1016/j.sleep.2020.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Innocenti P., Puzella A., Mogavero M.P., Bruni O., Ferri R. Letter to editor: CoVID-19 pandemic and sleep disorders—a web survey in Italy. Neurol Sci. 2020;41:2021–2022. doi: 10.1007/s10072-020-04523-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Iqbal Y., Al Abdulla M.A., Albrahim S., Latoo J., Kumar R., Haddad P.M. Psychiatric presentation of patients with acute SARS-CoV-2 infection: a retrospective review of 50 consecutive patients seen by a consultation-liaison psychiatry team. BJPsych Open. 2020;6 doi: 10.1192/bjo.2020.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Jahrami H., BaHammam A.S., AlGahtani H., Ebrahim A., Faris M., AlEid K., et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021;25:503–511. doi: 10.1007/s11325-020-02135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jain A., Singariya G., Kamal M., Kumar M., Jain A., Solanki R.K. COVID-19 pandemic: psychological impact on anaesthesiologists. Indian J Anaesth. 2020;64:774. doi: 10.4103/ija.IJA_697_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Jiang F., Xiao Y., Dong H., Liu S., Guo F., Gong Z., et al. Sleep quality in medical staffs during the outbreak of coronavirus disease 2019 in China: a web-based cross-sectional study. Front Psychiatr. 2021;12:630330. doi: 10.3389/fpsyt.2021.630330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Jin L.-R., Zhou S., Yuan H. Investigation on sleep quality in Chinese medical staff during the COVID-19 pandemic. Psychol Health Med. 2021:1–7. doi: 10.1080/13548506.2021.1922722. [DOI] [PubMed] [Google Scholar]
- 145.Juanjuan L., Santa-Maria C.A., Hongfang F., Lingcheng W., Pengcheng Z., Yuanbing X., et al. Patient-reported outcomes of patients with breast cancer during the COVID-19 outbreak in the epicenter of China: a cross-sectional survey study. Clin Breast Cancer. 2020;20:e651–e662. doi: 10.1016/j.clbc.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jung S., Kneer J., Kruger T.H. The German COVID-19 survey on mental health: primary results. medRxiv. 2020 doi: 10.1101/2020.05.06.20090340. [DOI] [Google Scholar]
- 147.Kaparounaki C.K., Patsali M.E., Mousa D.-P.V., Papadopoulou E.V., Papadopoulou K.K., Fountoulakis K.N. University students' mental health amidst the COVID-19 quarantine in Greece. Psychiatr Res. 2020;290:113111. doi: 10.1016/j.psychres.2020.113111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Khaled S.M., Petcu C., Al-Thani M.A., Al-Hamadi A.M.H., Daher-Nashif S., Zolezzi M., et al. Prevalence and associated factors of DSM-5 insomnia disorder in the general population of Qatar. BMC Psychiatr. 2021;21:1–10. doi: 10.1186/s12888-020-03035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Khalil11 A.M.S., Elsayed Z.E.H. Children dietary habits and quality of sleep during COVID-19 pandemic. Int J Nurs. 2020;7:80–86. [Google Scholar]
- 150.Khamis F., Al Mahyijari N., Al Lawati F., Badahdah A.M. The mental health of female physicians and nurses in Oman during the COVID-19 pandemic. Oman Med J. 2020;35 doi: 10.5001/omj.2020.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Khanal P., Devkota N., Dahal M., Paudel K., Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob Health. 2020;16:1–12. doi: 10.1186/s12992-020-00621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Khoury J.E., Atkinson L., Bennett T., Jack S.M., Gonzalez A. COVID-19 and mental health during pregnancy: the importance of cognitive appraisal and social support. J Affect Disord. 2021;282:1161–1169. doi: 10.1016/j.jad.2021.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kilani H.A., Bataineh MaF., Al-Nawayseh A., Atiyat K., Obeid O., Abu-Hilal M.M., et al. Healthy lifestyle behaviors are major predictors of mental wellbeing during COVID-19 pandemic confinement: a study on adult Arabs in higher educational institutions. PLoS One. 2020;15 doi: 10.1371/journal.pone.0243524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Killgore W.D., Cloonan S.A., Taylor E.C., Fernandez F., Grandner M.A., Dailey N.S. Suicidal ideation during the COVID-19 pandemic: the role of insomnia. Psychiatr Res. 2020;290:113134. doi: 10.1016/j.psychres.2020.113134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kocevska D., Blanken T.F., Van Someren E.J., Rösler L. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 2020;76:86–88. doi: 10.1016/j.sleep.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kokou-Kpolou C.K., Megalakaki O., Laimou D., Kousouri M. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatr Res. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kolokotroni O., Mosquera M.C., Quattrocchi A., Heraclides A., Demetriou C., Philippou E. Lifestyle habits of adults during the COVID-19 pandemic lockdown in Cyprus: evidence from a cross-sectional study. BMC Publ Health. 2021;21:1–11. doi: 10.1186/s12889-021-10863-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Lahiri A., Jha S.S., Acharya R., Dey A., Chakraborty A. Correlates of insomnia among the adults during COVID19 pandemic: evidence from an online survey in India. Sleep Med. 2021;77:66–73. doi: 10.1016/j.sleep.2020.11.020. [DOI] [PubMed] [Google Scholar]
- 159.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976–e. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lai AY-k, Lee L., Wang M-p, Feng Y., Lai TT-k, Ho L-m, et al. Mental health impacts of the COVID-19 pandemic on international university students, related stressors, and coping strategies. Front Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.584240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lavigne-Cerván R., Costa-López B., Juárez-Ruiz de Mier R., Real-Fernández M., Sánchez-Muñoz de León M., Navarro-Soria I. Consequences of COVID-19 confinement on anxiety, sleep and executive functions of children and adolescents in Spain. Front Psychol. 2021;12:334. doi: 10.3389/fpsyg.2021.565516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Li S.H., Beames J.R., Newby J.M., Maston K., Christensen H., Werner-Seidler A. The impact of COVID-19 on the lives and mental health of Australian adolescents. Eur Child Adolesc Psychiatr. 2021:1–13. doi: 10.1007/s00787-021-01790-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Li D.-J., Ko N.-Y., Chen Y.-L., Wang P.-W., Chang Y.-P., Yen C.-F., et al. COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: a Facebook survey. Int J Environ Res Publ Health. 2020;17:4479. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Li X., Cai Q., Jia Z., Zhou Y., Liu L., Zhou Y., et al. The correlation between mental health status, sleep quality, and inflammatory markers, virus negative conversion time among patients confirmed with 2019-nCoV during the COVID-19 outbreak in China: an observational study. Medicine. 2021;100 doi: 10.1097/MD.0000000000026520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Li H., Zhang Y., Wang H., Liang J., Zhou Y., Huang Y., et al. The relationship between symptoms of anxiety and somatic symptoms in health professionals during the coronavirus disease 2019 Pandemic. Neuropsychiatric Dis Treat. 2020;16:3153. doi: 10.2147/NDT.S282124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Li W., Zhao N., Yan X., Zou S., Wang H., Li Y., et al. The prevalence of depressive and anxiety symptoms and their associations with quality of life among clinically stable older patients with psychiatric disorders during the COVID-19 pandemic. Transl Psychiatry. 2021;11:1–8. doi: 10.1038/s41398-021-01196-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Liang Y., Wu K., Zhou Y., Huang X., Zhou Y., Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int J Environ Res Publ Health. 2020;17:6550. doi: 10.3390/ijerph17186550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Liguori C., Pierantozzi M., Spanetta M., Sarmati L., Cesta N., Iannetta M., et al. Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav Immun. 2020;88:11–16. doi: 10.1016/j.bbi.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lin L-y, Wang J., Ou-Yang X.-Y., Miao Q., Chen R., Liang F-x, et al. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021;77:348–354. doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatr Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Liu T., Zheng Z., Sha X., Liu H., Zheng W., Su H., et al. Psychological impact in non-infectious disease specialists who had direct contact with patients with COVID-19. BJPsych Open. 2021;7 doi: 10.1192/bjo.2020.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Liu C., Liu D., Huang N., Fu M., Ahmed J.F., Zhang Y., et al. The combined impact of gender and age on post-traumatic stress symptoms, depression, and insomnia during COVID-19 outbreak in China. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.620023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Liu D., Liu S., Zhu L., Li D., Huang D., Deng H., et al. Prevalence and related factors of insomnia among Chinese medical staff in the middle and late stage of COVID-19. Front Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.602315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Liu C., Stevens C., Conrad R., Hahm H. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among US young adults with suspected and reported psychiatric diagnoses. Psychiatr Res. 2020;292:113345. doi: 10.1016/j.psychres.2020.113345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lu C., Chi X., Liang K., Chen S.-T., Huang L., Guo T., et al. Moving more and Sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychol Res Behav Manag. 2020;13:1223. doi: 10.2147/PRBM.S284103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sobrado M.M., Mateo-Abad M., Vrotsou K., Vergara I. Health status and lifestyle habits of vulnerable, community-dwelling older people during the COVID-19 lockdown. J Frailty Aging. 2021:1–4. doi: 10.14283/jfa.2021.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Magnavita N., Soave P.M., Ricciardi W., Antonelli M. Occupational stress and mental health among anesthetists during the COVID-19 pandemic. Int J Environ Res Publ Health. 2020;17:8245. doi: 10.3390/ijerph17218245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Majumdar P., Biswas A., Sahu S. COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol Int. 2020;37:1191–1200. doi: 10.1080/07420528.2020.1786107. [DOI] [PubMed] [Google Scholar]
- 179.Mandelkorn U., Genzer S., Choshen-Hillel S., Reiter J., Meira e Cruz M., Hochner H., et al. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med. 2021;17:45–53. doi: 10.5664/jcsm.8800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Marelli S., Castelnuovo A., Somma A., Castronovo V., Mombelli S., Bottoni D., et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2021;268:8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Marroquín B., Vine V., Morgan R. Mental health during the COVID-19 pandemic: effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatr Res. 2020;293:113419. doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Martínez-de-Quel Ó., Suárez-Iglesias D., López-Flores M., Pérez C.A. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: a longitudinal study. Appetite. 2021;158:105019. doi: 10.1016/j.appet.2020.105019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Martínez-Lezaun I., Santamaría-Vázquez M., Del Líbano M. Influence of confinement by COVID-19 on the quality of sleep and the interests of university students. Nat Sci Sleep. 2020;12:1075. doi: 10.2147/NSS.S280892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Massicotte V., Ivers H., Savard J. COVID-19 pandemic stressors and psychological symptoms in breast cancer patients. Curr Oncol. 2021;28:294–300. doi: 10.3390/curroncol28010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Mazza M.G., De Lorenzo R., Conte C., Poletti S., Vai B., Bollettini I., et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.McCall W.V., Mensah-Bonsu D., Withers A.E., Gibson R.W. Short-term insomnia disorder in health care workers in an academic medical center before and during COVID-19: rates and predictive factors. J Clin Sleep Med. 2021;17:749–755. doi: 10.5664/jcsm.9034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. Psychological impact of COVID-19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur Psychiatr. 2020;63 doi: 10.1192/j.eurpsy.2020.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Meo S.A., Alkhalifah J.M., Alshammari N.F., Alnufaie W.S. Comparison of generalized anxiety and sleep disturbance among frontline and second-line healthcare workers during the COVID-19 pandemic. Int J Environ Res Publ Health. 2021;18:5727. doi: 10.3390/ijerph18115727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Miaskowski C., Paul S.M., Snowberg K., Abbott M., Borno H., Chang S., et al. Stress and symptom burden in oncology patients during the COVID-19 pandemic. J Pain Symptom Manag. 2020;60:e25–e34. doi: 10.1016/j.jpainsymman.2020.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Mongkhon P., Ruengorn C., Awiphan R., Thavorn K., Hutton B., Wongpakaran N., et al. Exposure to COVID-19-related information and its association with mental health problems in Thailand: Nationwide, cross-sectional survey study. J Med Internet Res. 2021 Feb 12;23(2):e25363. doi: 10.2196/25363. PMID: 33523828; PMCID: PMC7886375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Murata S., Rezeppa T., Thoma B., Marengo L., Krancevich K., Chiyka E., et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38:233–246. doi: 10.1002/da.23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Necho M., Birkie M., Gelaye H., Beyene A., Belete A., Tsehay M. Depression, anxiety symptoms, Insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. PLoS One. 2020;15 doi: 10.1371/journal.pone.0244530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Osiogo F., Shalaby R., Adegboyega S., Hrabok M., Gusnowski A., Vuong W., et al. COVID-19 pandemic: demographic and clinical correlates of disturbed sleep among 6,041 Canadians. Int J Psychiatr Clin Pract. 2021:1–8. doi: 10.1080/13651501.2021.1881127. [DOI] [PubMed] [Google Scholar]
- 194.Ozluk O., Ekici B., Zoghi M., Yuce E., Ozmen C., Yenercag M., et al. An assessment of the anxiety, depression, and sleep disorders experienced by cardiologists during the COVID-19 pandemic. Int J Clin Exp Med. 2021:1936–1942. [Google Scholar]
- 195.Parlapani E., Holeva V., Nikopoulou V.A., Sereslis K., Athanasiadou M., Godosidis A., et al. Intolerance of uncertainty and loneliness in older adults during the COVID-19 pandemic. Front Psychiatr. 2020;11:842. doi: 10.3389/fpsyt.2020.00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Pedrozo-Pupo J.C., Campo-Arias A. Depression, perceived stress related to COVID, post-traumatic stress, and insomnia among asthma and COPD patients during the COVID-19 pandemic. Chron Respir Dis. 2020;17 doi: 10.1177/1479973120962800. 1479973120962800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Petrov M.E., Pituch K.A., Kasraeian K., Jiao N., Mattingly J., Hasanaj K., et al. Impact of the COVID-19 pandemic on change in sleep patterns in an exploratory, cross-sectional online sample of 79 countries. Sleep Health. 2021 Aug;7(4):451–458. doi: 10.1016/j.sleh.2021.05.007. Epub 2021 Jun 27. PMID: 34193394. [DOI] [PubMed] [Google Scholar]
- 198.Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Poyraz B.Ç., Poyraz C.A., Olgun Y., Gürel Ö., Alkan S., Özdemir Y.E., et al. Psychiatric morbidity and protracted symptoms after COVID-19. Psychiatr Res. 2021;295:113604. doi: 10.1016/j.psychres.2020.113604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Qi J., Xu J., Li B.-Z., Huang J.-S., Yang Y., Zhang Z.-T., et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020;72:1–4. doi: 10.1016/j.sleep.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Que J., Le Shi J.D., Liu J., Zhang L., Wu S., Gong Y., et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr. 2020;33 doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Ren Y., Qian W., Li Z., Liu Z., Zhou Y., Wang R., et al. Public mental health under the long-term influence of COVID-19 in China: geographical and temporal distribution. J Affect Disord. 2020;277:893–900. doi: 10.1016/j.jad.2020.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Repon M.A.U., Pakhe S.A., Quaiyum S., Das R., Daria S., Islam M.R. Effect of COVID-19 pandemic on mental health among Bangladeshi healthcare professionals: a cross-sectional study. Sci Prog. 2021;104 doi: 10.1177/00368504211026409. 00368504211026409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Robillard R., Dion K., Pennestri M.H., Solomonova E., Lee E., Saad M., et al. Profiles of sleep changes during the COVID-19 pandemic: demographic, behavioural and psychological factors. J Sleep Res. 2021;30 doi: 10.1111/jsr.13231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Rossi R., Socci V., Pacitti F., Mensi S., Di Marco A., Siracusano A., et al. Mental health outcomes among healthcare workers and the general population during the COVID-19 in Italy. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.608986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatr. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Saadeh H., Saadeh M., Almobaideen W., Al Refaei A., Shewaikani N., Al Fayez R.Q., et al. Effect of COVID-19 quarantine on the sleep quality and the depressive symptom levels of university students in Jordan during the spring of 2020. Front Psychiatr. 2021;12:131. doi: 10.3389/fpsyt.2021.605676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sadeghniiat-Haghighi KM M., Najafi A., Shabani M., Akbarpour S. Cluster analysis of insomnia symptoms during COVID-19 pandemic: a general population web-based survey in Iran. Sleep Sci. 2021:1–6. doi: 10.5935/1984-0063.20200087. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Sagaon-Teyssier L., Kamissoko A., Yattassaye A., Diallo F., Castro D.R., Delabre R., et al. Assessment of mental health outcomes and associated factors among workers in community-based HIV care centers in the early stage of the COVID-19 outbreak in Mali. Health Pol Open. 2020;1:100017. doi: 10.1016/j.hpopen.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Sagherian K., Steege L.M., Cobb S.J., Cho H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: a cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. 2020 Nov 20 doi: 10.1111/jocn.15566. Epub ahead of print. PMID: 33219569; PMCID: PMC7753687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Saguem B.N., Nakhli J., Romdhane I., Nasr S.B. L'encephale; 2021. Predictors of sleep quality in medical students during COVID-19 confinement. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Şahin M.K., Aker S., Şahin G., Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J Community Health. 2020;45:1168–1177. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Salfi F., Lauriola M., D'Atri A., Amicucci G., Viselli L., Tempesta D., et al. Demographic, psychological, chronobiological, and work-related predictors of sleep disturbances during the COVID-19 lockdown in Italy. Sci Rep. 2021;11:1–12. doi: 10.1038/s41598-021-90993-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Sañudo B., Fennell C., Sánchez-Oliver A.J. Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns pre-and during-COVID-19 quarantine in young adults from Spain. Sustainability. 2020;12:5890. [Google Scholar]
- 216.Saracoglu K.T., Simsek T., Kahraman S., Bombaci E., Sezen Ö., Saracoglu A., et al. The psychological impact of Covid-19 disease is more severe on Intensive Care Unit healthcare providers: a cross-sectional study. Clin Psychopharmacol Neurosci. 2020;18:607. doi: 10.9758/cpn.2020.18.4.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Saraswathi I., Saikarthik J., Kumar K.S., Srinivasan K.M., Ardhanaari M., Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8 doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Scotta A.V., Cortez M.V., Miranda A.R. Insomnia is associated with worry, cognitive avoidance and low academic engagement in Argentinian university students during the COVID-19 social isolation. Psychol Health Med. 2021:1–16. doi: 10.1080/13548506.2020.1869796. [DOI] [PubMed] [Google Scholar]
- 219.Sekartaji M., Sari R.P., Irsan M., Adnan M., Aquaira L.P., Farahiya S.R., et al. Relationship between anxiety and insomnia in clinical clerkship students during COVID-19 pandemic. J Commun Empower Health. 2021;4:21–28. [Google Scholar]
- 220.Sharma R., Sharma S.C., Sharma P., Pradhan S.N., Chalise P., Regmee J., et al. Effect of lockdown on mental health during the COVID-19 pandemic among individuals attending services at a tertiary care center. Indian J Psychiatr. 2020;62:S431. doi: 10.4103/psychiatry.IndianJPsychiatry_1038_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Sharma R., Seth S., Solanki H.K., Mishra N., Srivastava A., Jakhar K. COVID-19 and obstetrical care: coping with new stress. Cureus. 2020;12 doi: 10.7759/cureus.12116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Sharma V., Kumar N., Gupta B., Mahajan A. Impact of COVID-19 pandemic on orthopaedic surgeons in terms of anxiety, sleep outcomes and change in management practices: a cross-sectional study from India. J Orthop Surg. 2021;29 doi: 10.1177/23094990211001621. 23094990211001621. [DOI] [PubMed] [Google Scholar]
- 223.Shi L., Lu Z.-A., Que J.-Y., Huang X.-L., Liu L., Ran M.-S., et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053. e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Shillington K.J., Vanderloo L.M., Burke S.M., Ng V., Tucker P., Irwin J.D. Not so sweet dreams: adults' quantity, quality, and disruptions of sleep during the initial stages of the COVID-19 pandemic. Sleep Med. 2021 Feb 19 doi: 10.1016/j.sleep.2021.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Simonetti V., Durante A., Ambrosca R., Arcadi P., Graziano G., Pucciarelli G., et al. Anxiety, sleep disorders and self-efficacy among nurses during COVID-19 pandemic: a large cross-sectional study. J Clin Nurs. 2021;30:1360–1371. doi: 10.1111/jocn.15685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Song L., Wang Y., Li Z., Yang Y., Li H. Mental health and work attitudes among people resuming work during the COVID-19 pandemic: a cross-sectional study in China. Int J Environ Res Publ Health. 2020;17:5059. doi: 10.3390/ijerph17145059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Stanton R., To Q.G., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Publ Health. 2020;17:4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Stewart N.H., Koza A., Dhaon S., Shoushtari C., Martinez M., Arora V.M. Sleep disturbances in frontline health care workers during the COVID-19 pandemic: social media survey study. J Med Internet Res. 2021;23 doi: 10.2196/27331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Sun L., Sun Z., Wu L., Zhu Z., Zhang F., Shang Z., et al. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv. 2020:1–17. [Google Scholar]
- 230.Sunil R., Bhatt M.T., Bhumika T.V., Thomas N., Puranik A., Chaudhuri S., et al. Weathering the storm: psychological impact of COVID-19 pandemic on clinical and nonclinical healthcare workers in India. Indian J Crit Care Med: Peer-Reviewed, Off Publ Ind Soc Crit Care Med. 2021;25:16. doi: 10.5005/jp-journals-10071-23702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Than H.M., Nong V.M., Nguyen C.T., Dong K.P., Ngo H.T., Doan T.T., et al. Mental health and health-related quality-of-life outcomes among frontline health workers during the peak of COVID-19 outbreak in Vietnam: a cross-sectional study. Risk Manag Healthc Pol. 2020;13:2927. doi: 10.2147/RMHP.S280749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Tiete J., Guatteri M., Lachaux A., Matossian A., Hougardy J.-M., Loas G., et al. Mental health outcomes in healthcare workers in COVID-19 and non-COVID-19 care units: a cross-sectional survey in Belgium. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.612241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Totskiy D., Alekhin A., Leonenko N., Pultcina C., Belyaeva S., Guzi L. E3S web of conferences. EDP Sciences; 2021. The psychological hardiness of students with a high insomnia index during the covid-19 pandemic; p. 7092. [Google Scholar]
- 236.Trabelsi K., Ammar A., Masmoudi L., Boukhris O., Chtourou H., Bouaziz B., et al. Sleep quality and physical activity as predictors of mental wellbeing variance in older adults during COVID-19 lockdown: ECLB COVID-19 international online survey. Int J Environ Res Publ Health. 2021;18:4329. doi: 10.3390/ijerph18084329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Trabelsi K., Ammar A., Masmoudi L., Boukhris O., Chtourou H., Bouaziz B., et al. 2021. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Tselebis A., Lekka D., Sikaras C., Tsomaka E., Tassopoulos A., Ilias I., et al. Multidisciplinary Digital Publishing Institute; Healthcare: 2020. Insomnia, perceived stress, and family support among nursing staff during the pandemic crisis; p. 434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Tu Z-h, He J-w, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine. 2020;99 doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Varma P., Junge M., Meaklim H., Jackson M.L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog Neuro Psychopharmacol Biol Psychiatr. 2021;109:110236. doi: 10.1016/j.pnpbp.2020.110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Vitale J.A., Perazzo P., Silingardi M., Biffi M., Banfi G., Negrini F. Is disruption of sleep quality a consequence of severe Covid-19 infection? A case-series examination. Chronobiol Int. 2020;37:1110–1114. doi: 10.1080/07420528.2020.1775241. [DOI] [PubMed] [Google Scholar]
- 242.Voitsidis P., Gliatas I., Bairachtari V., Papadopoulou K., Papageorgiou G., Parlapani E., et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatr Res. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Wang C., Song W., Hu X., Yan S., Zhang X., Wang X., et al. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: a case-controlled study. BMC Psychiatr. 2021;21:1–9. doi: 10.1186/s12888-021-03108-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Wang L.-Q., Zhang M., Liu G.-M., Nan S.-Y., Li T., Xu L., et al. Psychological impact of coronavirus disease (2019)(COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J Psychiatr Res. 2020;129:198–205. doi: 10.1016/j.jpsychires.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Wang L., Zhang Y., Chen L., Wang J., Jia F., Li F., et al. Psychosocial and behavioral problems of children and adolescents in the early stage of reopening schools after the COVID-19 pandemic: a national cross-sectional study in China. Transl Psychiatry. 2021;11:1–12. doi: 10.1038/s41398-021-01462-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Wang S., Zhang Y., Ding W., Meng Y., Hu H., Liu Z., et al. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur Psychiatr. 2020;63 doi: 10.1192/j.eurpsy.2020.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Wang M., Zhao Q., Hu C., Wang Y., Cao J., Huang S., et al. Prevalence of psychological disorders in the COVID-19 epidemic in China: a real world cross-sectional study. J Affect Disord. 2021;281:312–320. doi: 10.1016/j.jad.2020.11.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Wang Q., Feng H., Wang M., Xie Y., Hou B., Lu X., et al. Mental health and psychological responses during the coronavirus disease 2019 epidemic: a comparison between Wuhan and other areas in China. Psychosom Med. 2021;83:322–327. doi: 10.1097/PSY.0000000000000892. [DOI] [PubMed] [Google Scholar]
- 249.Wang X., Chen H., Liu L., Liu Y., Zhang N., Sun Z., et al. Anxiety and sleep problems of college students during the outbreak of COVID-19. Front Psychiatr. 2020:11. doi: 10.3389/fpsyt.2020.588693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Wang Y., Zhu L.-Y., Ma Y.-F., Bo H.-X., Deng H.-B., Cao J., et al. Association of insomnia disorder with sociodemographic factors and poor mental health in COVID-19 inpatients in China. Sleep Med. 2020;75:282–286. doi: 10.1016/j.sleep.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Wang J., Gong Y., Chen Z., Wu J., Feng J., Yan S., et al. Sleep disturbances among Chinese residents during the Coronavirus Disease 2019 outbreak and associated factors. Sleep Med. 2020;74:199–203. doi: 10.1016/j.sleep.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Wang W., Song W., Xia Z., He Y., Tang L., Hou J., et al. Sleep disturbance and psychological profiles of medical staff and non-medical staff during the early outbreak of COVID-19 in Hubei Province, China. Front Psychiatr. 2020;11:733. doi: 10.3389/fpsyt.2020.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Wang S., Xie L., Xu Y., Yu S., Yao B., Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med. 2020;70:364–369. doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Wańkowicz P., Szylińska A., Rotter I. Assessment of mental health factors among health professionals depending on their contact with COVID-19 patients. Int J Environ Res Publ Health. 2020;17:5849. doi: 10.3390/ijerph17165849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Wańkowicz P., Szylińska A., Rotter I. Evaluation of mental health factors among people with systemic lupus erythematosus during the SARS-CoV-2 pandemic. J Clin Med. 2020;9:2872. doi: 10.3390/jcm9092872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Wasim T., e Raana G., Bushra N., Riaz A. vol. 26. Annals of King Edward Medical University; 2020. pp. 140–144. (Effect of COVID-19 pandemic on mental wellbeing of healthcare workers in tertiary care hospital). [Google Scholar]
- 257.Windiani I.G.A.T., Noviyani N.M.R., Adnyana I.G.A.N.S., Murti N.L.S.P., Soetjiningsih S. Prevalence of sleep disorders in adolescents and its relation with screen time during the COVID-19 pandemic era. Open Access Macedonian J Med Sci. 2021;9:297–300. [Google Scholar]
- 258.Wu K., Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Mon Basic Res. 2020;26:e924085. doi: 10.12659/MSMBR.924085. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Xia Y., Kou L., Zhang G., Han C., Hu J., Wan F., et al. Investigation on sleep and mental health of patients with Parkinson's disease during the Coronavirus disease 2019 pandemic. Sleep Med. 2020;75:428–433. doi: 10.1016/j.sleep.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Xu K., Zhang Y., Zhang Y., Xu Q., Lv L., Zhang J. Mental health among pregnant women under public health interventions during COVID-19 outbreak in Wuhan, China. Psychiatr Res. 2021;301:113977. doi: 10.1016/j.psychres.2021.113977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Yadav R., Yadav P., Kumar S.S., Kumar R. Assessment of depression, anxiety, and sleep disturbance in COVID-19 patients at tertiary care center of north India. J Neurosci Rural Pract. 2021;12:316–322. doi: 10.1055/s-0040-1722811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Yang Y., Zhu J-f, Yang S-y, Lin H-j, Chen Y., Zhao Q., et al. Prevalence and associated factors of poor sleep quality among Chinese returning workers during the COVID-19 pandemic. Sleep Med. 2020;73:47–52. doi: 10.1016/j.sleep.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Yang B.X., Xia L., Huang R., Chen P., Luo D., Liu Q., et al. Relationship between eHealth literacy and psychological status during COVID-19 pandemic: a survey of Chinese residents. J Nurs Manag. 2021;29:805–812. doi: 10.1111/jonm.13221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Yang G., Li C., Zhu X., Yan J., Liu J. Prevalence of and risk factors associated with sleep disturbances among HPCD exposed to COVID-19 in China. Sleep Med. 2021;80:16–22. doi: 10.1016/j.sleep.2020.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Yifan T., Ying L., Chunhong G., Jing S., Rong W., Zhenyu L., et al. Symptom cluster of ICU nurses treating COVID-19 pneumonia patients in Wuhan, China. J Pain Symptom Manag. 2020;60:e48–e53. doi: 10.1016/j.jpainsymman.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Yitayih Y., Mekonen S., Zeynudin A., Mengistie E., Ambelu A. Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. BJPsych Open. 2021;7 doi: 10.1192/bjo.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Youssef N., Mostafa A., Ezzat R., Yosef M., El Kassas M. Mental health status of health-care professionals working in quarantine and non-quarantine Egyptian hospitals during the COVID-19 pandemic. East Mediterr Health J. 2020:1155–1164. doi: 10.26719/emhj.20.116. [DOI] [PubMed] [Google Scholar]
- 268.Yu B.Y.-M., Yeung W.-F., Lam J.C.-S., Yuen S.C.-S., Lam S.C., Chung V.C.-H., et al. Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: a cross-sectional study. Sleep Med. 2020;74:18–24. doi: 10.1016/j.sleep.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Yuksel D., McKee G.B., Perrin P.B., Alzueta E., Caffarra S., Ramos-Usuga D., et al. Sleeping when the world locks down: correlates of sleep health during the COVID-19 pandemic across 59 countries. Sleep Health. 2021;7:134–142. doi: 10.1016/j.sleh.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Zanghì A., D'Amico E., Luca M., Ciaorella M., Basile L., Patti F. Mental health status of relapsing-remitting multiple sclerosis Italian patients returning to work soon after the easing of lockdown during COVID-19 pandemic: a monocentric experience. Mult Scler Relat Disord. 2020;46:102561. doi: 10.1016/j.msard.2020.102561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Zhan Y., Liu Y., Liu H., Li M., Shen Y., Gui L., et al. Factors associated with insomnia among Chinese front-line nurses fighting against COVID-19 in Wuhan: a cross-sectional survey. J Nurs Manag. 2020;28:1525–1535. doi: 10.1111/jonm.13094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Zhang F., Shang Z., Ma H., Jia Y., Sun L., Guo X., et al. Epidemic area contact history and sleep quality associated with posttraumatic stress symptoms in the first phase of COVID-19 outbreak in China. Sci Rep. 2020;10:1–10. doi: 10.1038/s41598-020-80649-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Zhang L., Li T., Chen L., Wu F., Xia W., Huang M., et al. Association of sleep quality before and after SARS-CoV-2 infection with clinical outcomes in hospitalized patients with COVID-19 in China. EXCLI J. 2021;20:894. doi: 10.17179/excli2021-3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Zhang W-r, Wang K., Yin L., Zhao W-f, Xue Q., Peng M., et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Zhang J., Xu D., Xie B., Zhang Y., Huang H., Liu H., et al. Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: a retrospective cohort study. Brain Behav Immun. 2020;88:50–58. doi: 10.1016/j.bbi.2020.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Zhang X., Zou R., Liao X., Bernardo A.B., Du H., Wang Z., et al. Perceived stress, hope, and health outcomes among medical staff in China during the COVID-19 pandemic. Front Psychiatr. 2021;11:1646. doi: 10.3389/fpsyt.2020.588008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Zhang X., Liu J., Han N., Yin J. Social media use, unhealthy lifestyles, and the risk of miscarriage among pregnant women during the COVID-19 pandemic: prospective observational study. JMIR Publ Health Surveill. 2021;7 doi: 10.2196/25241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Zhang X., Zhao K., Zhang G., Feng R., Chen J., Xu D., et al. Occupational stress and mental health: a comparison between frontline medical staff and non-frontline medical staff during the 2019 novel coronavirus disease outbreak. Front Psychiatr. 2020;11:1543. doi: 10.3389/fpsyt.2020.555703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Zhang H., Qin S., Zhang L., Feng Z., Fan C. A psychological investigation of coronavirus disease 2019 (COVID-19) patients in mobile cabin hospitals in Wuhan. Ann Transl Med. 2020;8 doi: 10.21037/atm-20-4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Zhang Y., Wang S., Ding W., Meng Y., Hu H., Liu Z., et al. Status and influential factors of anxiety depression and insomnia symptoms in the work resumption period of COVID-19 epidemic: a multicenter cross-sectional study. J Psychosom Res. 2020;138:110253. doi: 10.1016/j.jpsychores.2020.110253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatr. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Zhang Y., Zhang H., Ma X., Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int J Environ Res Publ Health. 2020;17:3722. doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Zhao X., Zhang T., Li B., Yu X., Ma Z., Cao L., et al. Job-related factors associated with changes in sleep quality among healthcare workers screening for 2019 novel coronavirus infection: a longitudinal study. Sleep Med. 2020;75:21–26. doi: 10.1016/j.sleep.2020.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Zheng C., Huang W., Sheridan S., Sit C., Chen X., Wong S. COVID-19 pandemic brings a sedentary lifestyle: a cross-sectional and longitudinal study. medRxiv. May. 2020;24 doi: 10.3390/ijerph17176035. Preprint posted online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Zheng Y., Wang L., Feng L., Ye L., Zhang A., Fan R. Sleep quality and mental health of medical workers during the coronavirus disease 2019 pandemic. Sleep Biol Rhythm. 2021;19:173–180. doi: 10.1007/s41105-020-00304-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Zhou S.-J., Wang L.-L., Yang R., Yang X.-J., Zhang L.-G., Guo Z.-C., et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020;74:39–47. doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Zhou Y., Wang W., Sun Y., Qian W., Liu Z., Wang R., et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in China under the COVID-19 epidemic: workload should be concerned. J Affect Disord. 2020;277:510–514. doi: 10.1016/j.jad.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Zhou Y., Yang Y., Shi T., Song Y., Zhou Y., Zhang Z., et al. Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID-19 outbreak. Front Psychiatr. 2020;11:520. doi: 10.3389/fpsyt.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Zhou Y., Shi H., Liu Z., Peng S., Wang R., Qi L., et al. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl Psychiatry. 2020;10:1–7. doi: 10.1038/s41398-020-01006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Zhuo K., Gao C., Wang X., Zhang C., Wang Z. Stress and sleep: a survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID-19 pandemic. Gen Psychiatr. 2020:33. doi: 10.1136/gpsych-2020-100260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Zreik G., Asraf K., Haimov I., Tikotzky L. Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID-19) pandemic in Israel. J Sleep Res. 2021;30 doi: 10.1111/jsr.13201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Zupancic N., Bucik V., Ihan A., Dolenc-Groselj L. Sleep and safety improve physicians' psychological functioning at work during covid-19 epidemic. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.569324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Pahayahay A., Khalili-Mahani N. What media helps, what media hurts: a mixed methods survey study of coping with COVID-19 using the media repertoire framework and the appraisal theory of stress. J Med Internet Res. 2020;22 doi: 10.2196/20186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Kowal M., Coll-Martín T., Ikizer G., Rasmussen J., Eichel K., Studzińska A., et al. Who is the most stressed during the COVID-19 pandemic? Data from 26 countries and areas. Appl Psychol: Health Well-Being. 2020;12:946–966. doi: 10.1111/aphw.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Souza-Talarico J.N., Wan N., Santos S., Fialho P.P.A., Chaves E.C., Caramelli P., et al. Cross-country discrepancies on public understanding of stress concepts: evidence for stress-management psychoeducational programs. BMC Psychiatr. 2016;16:181. doi: 10.1186/s12888-016-0886-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Liu X., Zhu M., Zhang R., Zhang J., Zhang C., Liu P., et al. Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence. Transl Psychiatry. 2021;11:384. doi: 10.1038/s41398-021-01501-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Horwood L., Li P., Mok E., Shevell M., Constantin E. A systematic review and meta-analysis of the prevalence of sleep problems in children with cerebral palsy: how do children with cerebral palsy differ from each other and from typically developing children? Sleep Health. 2019;5:555–571. doi: 10.1016/j.sleh.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 298.Becker S.P., Gregory A.M. Editorial Perspective: perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. JCPP (J Child Psychol Psychiatry) 2020;61:757–759. doi: 10.1111/jcpp.13278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: literature review and case study. Environ Res. 2018;164:149–157. doi: 10.1016/j.envres.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 300.Aly H.M., Nemr N.A., Kishk R.M., Elsaid N. Stress, anxiety and depression among healthcare workers facing COVID-19 pandemic in Egypt: a cross-sectional online-based study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-045281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Publ Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 302.Smith S.S., Kozak N., Sullivan K.A. An investigation of the relationship between subjective sleep quality, loneliness and mood in an Australian sample: can daily routine explain the links? Int J Soc Psychiatr. 2012;58:166–171. doi: 10.1177/0020764010387551. [DOI] [PubMed] [Google Scholar]
- 303.Kurina L.M., Knutson K.L., Hawkley L.C., Cacioppo J.T., Lauderdale D.S., Ober C. Loneliness is associated with sleep fragmentation in a communal society. Sleep. 2011;34:1519–1526. doi: 10.5665/sleep.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Hassan E.M., Mahmoud H.N. Impact of multiple waves of COVID-19 on healthcare networks in the United States. PLoS One. 2021;16 doi: 10.1371/journal.pone.0247463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Reicher S., Drury J. Pandemic fatigue? How adherence to covid-19 regulations has been misrepresented and why it matters. BMJ. 2021;372:n137. doi: 10.1136/bmj.n137. [DOI] [PubMed] [Google Scholar]
- 306.Lam C.S., Yu B.Y.-M., Cheung D.S.T., Cheung T., Lam S.C., Chung K.-F., et al. Sleep and mood disturbances during the COVID-19 outbreak in an urban Chinese population in Hong Kong: a longitudinal study of the second and third waves of the outbreak. Int J Environ Res Publ Health. 2021;18:8444. doi: 10.3390/ijerph18168444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Ballesio A., Aquino M., Feige B., Johann A.F., Kyle S.D., Spiegelhalder K., et al. The effectiveness of behavioural and cognitive behavioural therapies for insomnia on depressive and fatigue symptoms: a systematic review and network meta-analysis. Sleep Med Rev. 2018;37:114–129. doi: 10.1016/j.smrv.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 308.Rusch H.L., Rosario M., Levison L.M., Olivera A., Livingston W.S., Wu T., et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. 2019;1445:5–16. doi: 10.1111/nyas.13996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Jahrami H., BaHammam A.S., Stubbs B., Sabah A., Saif Z., Bragazzi N.L., et al. Eight-week high-intensity interval training is associated with improved sleep quality and cardiorespiratory fitness in patients with depressive disorders. Sleep Breath. 2021 May 27 doi: 10.1007/s11325-021-02388-y. Epub ahead of print. PMID: 34046817. [DOI] [PubMed] [Google Scholar]
- 310.Magnavita N., Garbarino S. Sleep, health and wellness at work: a scoping review. Int J Environ Res Publ Health. 2017;14:1347. doi: 10.3390/ijerph14111347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Choi Y.K., Demiris G., Lin S.-Y., Iribarren S.J., Landis C.A., Thompson H.J., et al. Smartphone applications to support sleep self-management: review and evaluation. J Clin Sleep Med : JCSM: Off Publ Am Acad Sleep Med. 2018;14:1783–1790. doi: 10.5664/jcsm.7396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.