Abstract
A new episode of urticaria and/or angioedema can be an anxiety-inducing event for both the patient and the physician(s) seeing them in primary care, urgent care, or the emergency department. These events are commonly mistaken for “allergic” reactions and often mistreated. The most common causes of new onset urticaria in older children and adults, with or without angioedema, and normal vital signs or hypertension, are post-infection or acute idiopathic urticaria. These patients are not helped by systemic steroids, which may cause morbidity. An IgE-mediated allergy is almost never the cause. These episodes are easy to manage and virtually never life-threatening. Acute idiopathic urticaria is treated with high-dose nonsedating antihistamines acute avoidance of alcohol and nonsteroidal anti-inflammatory drugs, and time. An epinephrine prescription is not indicated for onset acute urticaria or angioedema, unless there is a strong suspicion of anaphylaxis, and they have been acutely treated with epinephrine. When anaphylaxis is suspected, because of hypotension or hypoxia, the treatment of choice is intramuscular epinephrine and supportive care. An acute tryptase then needs to be obtained within 1 to 3 hours of symptom onset, prior to a referral to Allergy. Most angioedema, without itching or hives, is idiopathic. Treatment is supportive care and time. Antihistamines, epinephrine, and systemic corticosteroids are completely ineffective in treating idiopathic or bradykinin-mediated angioedema. Suspect hereditary or acquired angioedema if there is recurrent non-itchy swelling with abdominal pain triggered by mechanical trauma. Only check a C4 prior to a referral to Allergy for a formal diagnosis and long-term management.
Keywords: adverse drug reaction, angioedema, bradykinin, itching, management, mast cell, urticaria
INTRODUCTION
Allergy is almost never the cause of a new episode of urticaria and/or angioedema in older children or adults presenting in primary care, urgent care, or the emergency department.1 Having a new episode of urticaria and/or angioedema can be an anxiety inducing event for both the patient and the physician(s) treating them, because there is a subliminal and pervasive fear of progression to life-threatening anaphylaxis. These relatively common, often quite benign, events are frequently misdiagnosed as “allergic” reactions. Following current standard practices, often based on dated practice parameters, may result in the patient being confused as to what is happening and acute treatment and management that results in avoidable morbidity.1
DEFINITIONS
Hypersensitivity
The term hypersensitivity is used to describe an immunologically mediated adverse reaction.
Allergy is an important subgroup of hypersensitivity, mediated through mast cell activation caused by pre-existing antigen-specific IgE bound to mast cells. In order to have an allergic reaction, one needs to have been sensitized by a previous exposure to the relevant antigen. Individuals either start to develop clinically significant IgE-mediated allergies in childhood, or they do not, and many true allergies wane with increasing age. This is unlike delayed-onset T-cell–mediated hypersensitivities that are gradually accumulated over time.
Tolerance and Intolerance
Tolerance means that an individual did not have a problem with the last exposure. If a clinically significant IgE-mediated allergy is present, then the person will fail to tolerate that antigen with every exposure the same size as the dose triggering dose for the index reaction. Most suspected “allergies,” with penicillin being the classic example, are misdiagnosed. Acute idiopathic urticaria commonly occurs after viral infections.1 Individuals with viral infections are commonly given antibiotics. Post-infection urticaria is then mistakenly attributed to the antibiotic. Less than 5% of individuals with a penicillin “allergy” will react to an oral challenge with a therapeutic dose of penicillin.2 Intolerance is what really should be labeled in the electronic health record most of the time, not allergy.3 New-onset food allergy almost never occurs in adults, without previously confirmed food and/or environmental allergies that started in early childhood.4
Allergic Reactions
A key characteristic of an allergic reaction is that they are essentially immediate-onset because of the existence of pre-formed antigen-specific IgE already bound on mast cells.5 Typical onset is within minutes of parenteral exposures, generally 10s of minutes after oral exposures, almost always less than 1 hour, but up to 6 hours, by international consensus.6 A reaction occurs with every exposure over the threshold dose with clinically significant IgE-mediated allergy. Antigen-specific IgE or IgG and complement can cause mast cell activation, and in both cases, it is possible to desensitize individuals with drug allergies by giving doubling doses. It is not possible to reliably desensitize individuals with clinically significant food allergies at this time.
Anaphylaxis
Anaphylaxis is a potentially life-threatening systemic reaction caused by systemic mast cell activation, either IgE-mediated, IgG- and complement-mediated, or direct activation through other mast cell surface receptors such as MAS-related GPR family member X2 (MRGPRX2).7,8 Direct mast cell activation through MRGPRX2 is thought to contribute to many of the acute hypersensitivity events observed with fluoroquinolones, opiates, and radiocontrast.8 Nonsteroidal anti-inflammatory drugs (NSAIDs) can induce anaphylaxis through leukotrienes in rare individuals who are metabolically intolerant of NSAIDs.9 Individuals with anaphylaxis must have at least 2 organ systems involved.7 Serious episodes of anaphylaxis presenting to the emergency department are virtually always associated with hypotension, dyspnea, and/or hypoxia. Treatment is with intramuscular epinephrine. Systemic steroids do not help any of the symptoms associated with anaphylaxis and cause potentially avoidable morbidity. Obtain an acute tryptase 1 to 3 hours after onset of symptoms whenever anaphylaxis is suspected, or when the individual is treated or has been treated with intramuscular epinephrine prior to arrival to help determine if systemic mast cell activation has occurred and to help guide future management. If the tryptase is normal or negative, then IgE-mediated anaphylaxis is unlikely the cause of the episode. Tryptase is a mast cell mediator that is measurable 1 to 3 hours after onset of anaphylaxis. An elevated acute tryptase provides strong support for mast cell activation. It can take up to a week for an acute tryptase to be available. If the tryptase is normal or negative, then IgE-mediated anaphylaxis becomes a much less likely diagnosis. Refer all individuals with newly suspected or confirmed anaphylaxis to Allergy. Virtually all food-, drug-, or venom-associated anaphylaxis occurs within 1 hour of exposure. Most NSAID-associated anaphylaxis starts within 2 hours. Almost all anaphylaxis cases occur within 6 hours of exposure, including rare, delayed-onset cases associated with α-gal hypersensitivity after oral exposures.10
Delayed-Onset T Cell-Mediated Hypersensitivity
Non-immediate hypersensitivity reactions are mediated by antigen-specific T cells. These delayed-type reactions, analogous to what is happening in contact dermatitis, typically have an onset of more than a day, but down to 6 hours by international consensus.5,6 The time to onset can be longer, 4 to 24 days, for serious cutaneous adverse reactions. One cannot desensitize individuals with T-cell–mediated hypersensitivity. T-cell–mediated hypersensitivity can mimic angioedema but can take weeks instead of days to resolve. Corticosteroid therapy, by inhibiting T-cell activation, may help speed clearing of the swelling and inflammation. T cells are not involved in angioedema or urticaria.5
Urticaria
The key point when attempting to distinguish urticaria from all other rashes is answering the question, “how long do the spots last”.1 With urticaria the answer must be minutes to hours, and by definition, always less than 24 hours. Because urticaria is due to dilation of blood vessels caused by histamine and other mediator release from mast cells or bradykinin activation, there is no tissue damage, other than scratch damage, and basically no pathologic cellular infiltration. If there are painful lesions lasting for more than 24 hours, even if they look like “hives”, consider alternative diagnoses such as contact dermatitis or urticarial vasculitis.
Angioedema
Angioedema is localized, non-pitting, often asymmetric, and does not typically involve depending regions, like the ankles. Angioedema is caused by vascular leakage of plasma into the surrounding tissues. Angioedema may affect the deeper layers of the skin, mucus membranes, the upper airway, and the gastrointestinal tract. It is most common on the face, larynx, abdomen, genitalia, and extremities.11 The plasma reabsorbs within hours, at most within 72 hours, and leaves no evidence of skin damage. Other rashes that are caused by cellular infiltrates or mechanical tissue damage take longer to resolve. It is important to distinguish histamine-mediated versus bradykinin-mediated or other non-histamine-mediated angioedema.12,13 Antihistamines only help itchy swelling mediated by histamine. Epinephrine can be helpful with histamine-mediated angioedema, typically with associated hypotension. Epinephrine, antihistamines, and corticosteroids are completely ineffective against non–histamine-mediated, bradykinin-mediated, or idiopathic angioedema.14 The clinical features distinguishing histamine- and bradykinin-mediated or idiopathic non–histamine-mediated angioedema are displayed in Table 1.
Table 1.
Clinical features associated with histamine- and bradykinin-mediated angioedema
| Histamine-mediated | Bradykinin-mediated | |
|---|---|---|
| Itching | Commonly | Never |
| Hives | Commonly | Never |
| Abdominal pain | Rarely | Commonly |
| Exacerbated by heat | Commonly | Rarely |
| Exacerbated by alcohol | Commonly | Possibly |
| Exacerbated by NSAIDs | About 30% of the time | Rarely |
| Exacerbated by ACE inhibitors | Occasionally | Commonly |
| Triggered by surgery | No | Commonly |
| Triggered by physical factors such as mechanical pressure on the skin or vibration | Occasionally | Commonly |
| Triggered by stress or hormonal changes | No | Commonly |
| Triggered by acute infections | Yes | Yes |
ACE = angiotensin-converting enzyme; NSAIDs = nonsteroidal anti-inflammatory drugs.
Short-term Systemic Corticosteroid-Associated Morbidity
There is significant, but often overlooked, delayed-onset, morbidity associated with short-term systemic corticosteroid use, often given for “allergic” reactions.15–17 Waljee and coworkers reported in 2017 on a 3-year study involving over 1.5 million patients receiving less than 30 days of systemic corticosteroids.15 They noted that within 30 days of corticosteroid initiation, there was an increase in rates of sepsis (incidence rate ratio 5.30, 95% confidence interval [CI] 3.80-7.41), venous thromboembolism (3.33, 2.78-3.99), and fracture (1.87, 1.69-2.07), which diminished over the subsequent 31-90 days. The increased risk persisted at prednisone equivalent doses of less than 20 mg/d (incidence rate ratio 4.02 for sepsis, 3.61 for venous thromboembolism, and 1.83 for fracture; all p < 0.001). Thus, even relatively short courses of systemic corticosteroids, given for conditions where they provide no therapeutic benefit, cause significant morbidity. Yao and coworkers in 2020 and 2021 reported on short-course steroid-associated morbidity in nationwide Taiwanese cohorts in children and adults and noted similar findings.16,17
EPIDEMIOLOGY
Urticaria
Acute Urticaria
The incidence of acute urticaria, with or without associated angioedema, is about 1 in 5 per lifetime.1 The vast majority, 99.5%, of all episodes of urticaria come and go within 6 weeks, and those that resolve are defined as acute. The vast majority of new onset episodes of urticaria in older children or adults presenting in primary care, urgent care, or the emergency department are idiopathic. The most commonly identified “cause” or association is post viral, or other, infection. The size of the hives and what part of the body they occur on are not helpful clues in finding a “cause” of or treatment for hives. Topical exposures to materials are almost never the cause of acute idiopathic urticaria. Medications, foods, and insect bites or stings are the most common allergic causes identified, but only when there is a pattern of recurrent urticaria associated with recurrent systemic exposures to one of these agents that meets the 1-1-1 rule (hives starting within 1 hour of the index exposure and completely clearing within 1 day).18 IgE-mediated allergy is almost never the cause of newly presenting cases of acute urticaria seen in primary care, urgent care, or the emergency department.
Chronic Urticaria
Chronic urticaria, with or without associated angioedema, by definition last longer than 6 weeks.1 The most common subgroups of chronic urticaria, with or without angioedema, are physical urticaria, autoimmune, and idiopathic.1 In some individuals, physical factors such as scratching the skin, vibration, changes in temperature, sun exposure, and/or pressure will induce hives. People with physical urticaria often have hives on and off for decades. Cold urticaria is a special type of chronic urticaria where the primary trigger is the rewarming after skin exposure to cold. The average episode of autoimmune chronic urticaria takes about 3 years to resolve, but 20% of episodes can remain active for more than 10 years.1
Fricke and coworkers reported in 2020 on a meta-analysis of the world-wide prevalence of chronic urticaria.19 They noted that Asian studies showed a higher point prevalence of chronic urticaria (1.4%, 95% CI 0.5-2.9) than those from Europe (0.5%, 95% CI 0.2-1.0) or Northern American (0.1%, 95% CI 0.1-0.1). Women were slightly more affected than men in all regions, whereas in children < 15 years, they did not find a sex-specific difference in the prevalence. Chronic urticaria has a point prevalence estimate in the United States of about 1 in 1,000. Thus, with around 4 million members, Kaiser Permanente Southern California (KPSC) would be expected to have about 4,000 patients annually with chronic urticaria. If this was coded accurately, a much larger fraction of the chronic urticaria patients would be expected to have the diagnosis in all 3 years compared to what is observed.
Angioedema
Most newly presenting cases of isolated angioedema, without any itching or hives, seen in primary care, urgent care, or the emergency department are idiopathic.20 Angioedema will occur in about 0.1% to 0.7% of patients receiving angiotensin-converting enzyme (ACE) inhibitors over the long term.21 ACE inhibitors are the leading cause of drug-induced angioedema, accounting for up to 30% of emergency department visits for angioedema.20 Individuals treated with HMG-CoA reductase inhibitors, dipeptidyl peptidase IV inhibitors, and rarely risperidone may also be at higher risk to present with angioedema.21 Only about 1% to 2% of cases of angioedema are caused by hereditary angioedema (HAE) or acquired angioedema (AAE).22 HAE, associated with reduce C1q inhibitor function, has a population prevalence of about 1 in 30,000 to 80,000 in the United States. AAE, often secondary to an underlying hematopoietic malignancy, is about 10-fold rarer than HAE.23
Rare individuals with NSAID hypersensitivity can get leukotriene-mediated angioedema, without the typical nasal and respiratory symptoms associated with NSAID-exacerbated respiratory disease. Mast cells may contribute to the pathogenesis of this rare type of angioedema.9
The coding for angioedema and urticaria-related diagnoses in KPSC at times appears almost random. Using the KPSC Research Preliminary Data Application Program, the number of unique individuals given angioedema and urticaria-related diagnoses in 2018 through 2020 are displayed in Table 2.24 If individuals with chronic urticaria were truly chronic, then those given a diagnosis in 2018 would be very likely to have the same diagnosis in 2019 and 2020. With around 4 million members, KPSC would be expected to have about 4,000 patients annually with chronic urticaria. If chronic urticaria was coded accurately, a much larger fraction of the chronic urticaria patients would be expected to have the diagnosis in all 3 years, compared to what is observed. KPSC cares for a much larger than predicted group of individuals with HAE based on the fraction of the United States population we care for.
Table 2.
Unique patients coded for urticaria- and angioedema-related diagnoses in 2019 and 2020 in Kaiser Permanente Southern California
| Diagnosis [ICD-10 code] | 2018 Unique patients | 2019 Unique patients | 2020 Unique patients (% of mean of 2019 and 2018) | Total patients [unique patients] (ratio)a |
|---|---|---|---|---|
| Acute urticaria [L50.9] | 38,237 | 40,307 | 28,461 (72.5%) | 107,005 [101,546] (1.05) |
| Chronic urticaria [L50.8] | 6,603 | 7,215 | 5,946 (86.1%) | 19,764 [16,758] (1.18) |
| Angioedema [T78.3] | 7,368 | 7,391 | 6,069 (82.2%) | 20,828 [19,339] (1.08) |
| Allergy-unspecified [T78.4] | 31,130 | 32,661 | 23,189 (72.7%) | 86,980 [83,708] (1.04) |
| Hereditary angioedema [D84.1] | 211 | 211 | 211 (100%) | 633 [248] (2.55) |
| ACE inhibitor intolerance [T46.4X5A] | 860 | 834 | 549 (64.8%) | 2,243 [2,235] (1.00) |
| Upper respiratory infection [J06.9] | 455,219 | 501,781 | 304,125 (63.6%) | 126,125 [1,044,107] (1.21) |
With the same patients every year, ratio = 3. With different patients every year, ratio = 1.
ACE = angiotensin-converting enzyme.
MANAGEMENT OF URTICARIA
Urticaria is defined as an itchy raised rash, with surrounding erythema, with spots that move around and never stay in the same place for more than several hours, and by definition less than 24 hours.1 One cannot accurately identify a hive, unless one knows how long the spot lasts. Urticaria often presents with hypertension when seen in urgent care or the emergency department. It often presents with associated angioedema, particularly if there has been recent high dose NSAID or alcohol use. New onset urticaria in older children or adults is almost never from an IgE-mediated food or drug allergy.
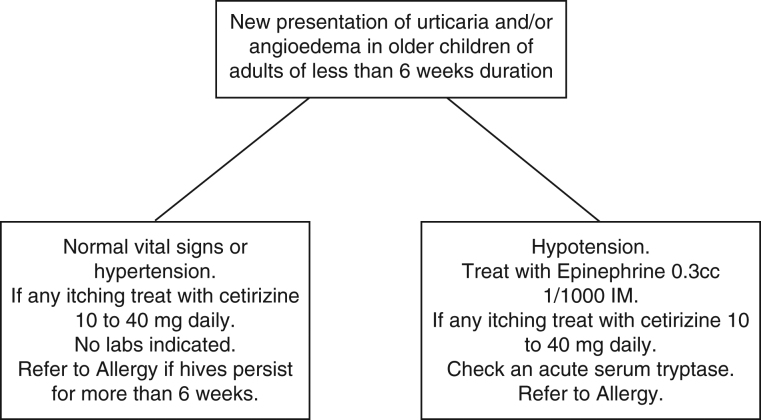
The essential elements for the management of newly presenting urticaria are displayed in Figure 1. The treatment of choice for both the itching and the hives associated with both acute and chronic urticaria is a high-dose nonsedating antihistamine, typically cetirizine up to 40 mg.25-28 Cetirizine is significantly more effective than loratadine of fexofenadine.29 Cetirizine is as effective in blocking itching as sedating antihistamines, including diphenhydramine and hydroxyzine, but without the anti-cholinergic side-effects. Cetirizine is the active metabolic breakdown product of hydroxyzine. Systemic corticosteroids do not help any of the symptoms associated with urticaria and may cause avoidable morbidity.15-17,27,28 Systemic steroids can induce acne and are associated with weight gain, gastrointestinal bleeding, and infections. Topical steroids do not help urticaria and can cause skin thinning.
Figure 1.
Simplified management plan for the new presentation of hives and/or angioedema in older children and adults presenting in primary care, urgent care, or the emergency department.
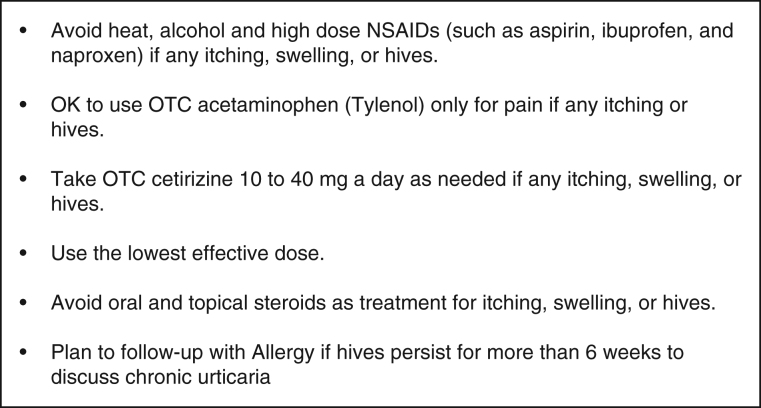
The smart phrase that I use in my management plan for all of my urticaria patients contains the information noted in Figure 2.
Figure 2.
Essential elements in a management plan for urticaria. NSAIDs = nonsteroidal anti-inflammatory drugs.
An epinephrine injector is rarely indicated in patients with acute idiopathic urticaria or chronic urticaria, with or without angioedema. An epinephrine prescription is indicated if anaphylaxis was treated. High dose NSAIDs used for pain control such as aspirin, ibuprofen, and naproxen can amplify urticaria in up to 30% of individuals.30 One 81 mg baby aspirin daily typically does not make urticaria worse. ACE inhibitors can make associated angioedema worse. Alcohol and heat can also amplify urticaria by dilating blood vessels near the surface of the skin. All patients with chronic urticaria, daily hives lasting more than 6 weeks, should be referred to Allergy for long-term follow-up and to determine if an additional therapy such as omalizumab (anti-IgE) may be warranted. There is no cure for chronic urticaria, only symptom management until the course resolves on its own.
ACUTE IDIOPATHIC URTICARIA MIMIC: SCOMBROID POISONING
Scombroid food poisoning mimics both fish food allergy and acute idiopathic urticaria.31 Scombroid food poisoning can occur with a variety of fresh, smoked, or canned fish products that have developed high histamine levels because of improper processing or storage. Histamine does not change the smell or appearance of the affected fish. Symptoms typically begin within 10 to 90 minutes of ingestion. Often multiple individuals are affected by the implicated food, though sometimes one individual is more sensitive or has a high exposure than others at the same meal. Treatment is just symptomatically with nonsedating antihistamine and scombroid poisoning is typically self-limiting over a 3- to 36-hour period.
MANAGEMENT OF ANGIOEDEMA
When angioedema presents without itching or hives, it is often bradykinin mediated.8 See Table 1. One of the most common angioedema presentations is associated with ACE inhibitor use. There is typically no effective treatment for a newly presenting case of angioedema, unless it has been confirmed to be from HAE or AAE, a complement system defect. Epinephrine, antihistamines, and systemic steroids do not help idiopathic or bradykinin-mediated angioedema and can have severe side-effects. The most useful treatment is watchful waiting, maintaining the airway, discontinuation of the implicated ACE inhibitor, and allowing normal homeostasis to return. If there is suspected HAE based on family history and associated abdominal pain, check a C4 and consult the allergist on call for treatment options. Do not send any C1q inhibitor testing. This will be done by Allergy if indicated based on an abnormally low C4 level.
There are at least 3 general categories of non–mast cell-mediated angioedema syndromes, all of which are very rare:
-
1.
HAE due to C1-inhibitor deficiency
-
2.
AAE associated with a hematopoietic malignancy
-
3.
Other angioedema syndromes induced by the renin-angiotensin-aldosterone system
Bradykinin-mediated angioedema, specifically with laryngeal angioedema, may be life-threatening. C1-inhibitor concentrates, icatibant, or ecallantide are the drugs of choice for the acute treatment of HAE and AAE in the emergency department. There are now a variety of drugs approved for the prevention bradykinin-mediated angioedema, including C1-INH concentrates, the bradykinin B2-receptor antagonist, icatibant, and the kallikrein inhibitors, ecallantide, lanadelumab, and berotralstat, all of which are managed by the allergy department.22
ANGIOEDEMA MIMIC: CHEILITIS
Cheilitis is typically caused by a T-cell–mediated delayed-type hypersensitivity reaction and may occur after years of using the eventual contact sensitizer.32 It can also be caused by exposure to a direct contact irritant, without antigen-specific T-cells present. Cheilitis is not caused by IgE-mediated allergy. There is typically a 2- to 5-day lag between the chemical exposure and the initial lip inflammation. With a single exposure, the lips can be inflamed and swollen for days to weeks.
Management starts with avoidance of all chemical exposure to the lips if any active cheilitis. Only use pure petrolatum on the lips. Do not use topical steroids on the lips. Avoid licking lips if active swelling or inflammation. When there is no active cheilitis, advise the patient to only reintroduce any one new material in any 1 week. If the cheilitis returns, stop the last thing restarted and repeat the process noted above.
SUMMARY
The treatment of choice for acute idiopathic urticaria and chronic urticaria in and adults is cetirizine 10-40 mg/d and avoidance of heat, alcohol, and NSAIDs when the hives are active. Individuals with chronic urticaria should be referred to allergy for long-term management. Systemic corticosteroids are not helpful for acute or chronic urticaria and can cause avoidable morbidity
When an NSAID is the suspected cause of angioedema, the therapy of choice is intramuscular epinephrine and antihistamines. Systemic corticosteroids are not helpful for angioedema caused by NSAID hypersensitivity and can cause morbidity.
The acute treatment of a new episode of angioedema, where an NSAID is not the suspected cause or a specific known HAE or AAE syndrome that has an approved therapy has not been confirmed, is maintenance of the airway and watchful waiting. Do not use epinephrine or antihistamines in the setting of angioedema without itching or hives. The use of systemic corticosteroids for angioedema, with or without urticaria, is not helpful and causes morbidity.
Any episode of new-onset acute idiopathic hives seen in primary care, urgent care, or the emergency department, with or without angioedema, should be coded as urticaria [L50.9]. If the patient has had more than 42 days of hives, with or without angioedema, then it should be coded as chronic urticaria [L50.8]. If there is non-itchy angioedema, then it should be coded as angioedema [T78.3]. Whenever there is non-itchy angioedema and an ACE inhibitor is being used, then the ACE inhibitor is the presumptive cause. The ACE inhibitor should be stopped immediately, and the event coded as an adverse effect of ACE inhibitors [T46.4 × 5A]. When it is unclear which code to use, the default code should be urticaria [L50.9]. The code allergic reaction [T78.4] should essentially never be used in patients seen for a new episode of hives or swelling in primary care, urgent care, or the emergency department. If an IgE-mediated event has been previously confirmed, then the specific reaction code linked to that specific food, venom, drug, or other agent should be used.
Footnotes
Disclosure Statement: The author has no conflicts of interest to disclose.
Funding: The author has received no funding for this manuscript.
Author Contributions: The author contributed entirely to the writing of this manuscript.
Abbreviations: AAE, acquired angioedema; ACE, angiotensin-converting enzyme; HAE, hereditary angioedema; KPSC, Kaiser Permanente Southern California; MRGPRX2, MAS-related GPR family member X2; NSAID, nonsteroidal anti-inflammatory drug
References
- 1.Bernstein JA, Lang DM, Khan DA, et al. The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol 2014. May;133(5):1270–7. DOI: 10.1016/j.jaci.2014.02.036 [DOI] [PubMed] [Google Scholar]
- 2.Macy E. Addressing the epidemic of antibiotic “allergy” over-diagnosis. Ann Allergy Asthma Immunol 2020. Jun;124(6):550–7. DOI: 10.1016/j.anai.2019.12.016 [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal KG, Park MA, Macy EM. Redesigning the allergy module of the electronic health record. Ann Allergy Asthma Immunol 2016. Aug;117(2):126–31. DOI: 10.1016/j.anai.2016.05.017 [DOI] [PubMed] [Google Scholar]
- 4.Savage J, Sicherer S, Wood R. The natural history of food allergy. J Allergy Clin Immunol Pract 2016. Mar-Apr;4(2):196–203. DOI: 10.1016/j.jaip.2015.11.024 [DOI] [PubMed] [Google Scholar]
- 5.Macy E. Immune-related adverse drug reactions and immunologically mediated drug hypersensitivity. Immunol Allergy Clin North Am 2020. Nov;40(4):635–47. DOI: 10.1016/j.iac.2020.06.003 [DOI] [PubMed] [Google Scholar]
- 6.Macy E, Romano A, Khan D. Practical management of antibiotic hypersensitivity in 2017. J Allergy Clin Immunol Pract 2017. May-Jun;5(3):577–86. DOI: 10.1016/j.jaip.2017.02.014 [DOI] [PubMed] [Google Scholar]
- 7.Turner PJ, Worm M, Ansotegui IJ, et al. ; WAO Anaphylaxis Committee. Time to revisit the definition and clinical criteria for anaphylaxis? World Allergy Organ J 2019. Oct; 12(10):100066. DOI: 10.1016/j.waojou.2019.100066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu R, Hu S, Zhang Y, et al. Mast cell-mediated hypersensitivity to fluoroquinolone is MRGPRX2 dependent. Int Immunopharmacol 2019. May;70:417–27. DOI: 10.1016/j.intimp.2019.02.001 [DOI] [PubMed] [Google Scholar]
- 9.Macy E, Bernstein JA, Castells MC, et al. ; Aspirin Desensitization Joint Task Force. Aspirin challenge and desensitization for aspirin-exacerbated respiratory disease: a practice paper. Ann Allergy Asthma Immunol 2007. Feb;98(2):172–4. DOI: 10.1016/S1081-1206(10)60692-8 [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Alpha-gal Syndrome. Accessed Jul 23, 2021. https://www.cdc.gov/ticks/alpha-gal/index.html
- 11.Pines JM, Poarch K, Hughes S. Recognition and differential diagnosis of hereditary angioedema in the emergency department. J Emerg Med 2021. Jan;60(1):35–43. DOI: 10.1016/j.jemermed.2020.09.044 [DOI] [PubMed] [Google Scholar]
- 12.Obtułowicz K. Bradykinin-mediated angioedema. Pol Arch Med Wewn 2016;126(1-2):76–85. DOI: 10.20452/pamw.3273 [DOI] [PubMed] [Google Scholar]
- 13.Andersen MF, Longhurst HJ, Rasmussen ER, Bygum A. How not to be misled by disorders mimicking angioedema: a review of pseudoangioedema. Int Arch Allergy Immunol 2016;169(3):163–70. DOI: 10.1159/000445835 [DOI] [PubMed] [Google Scholar]
- 14.Maurer M, Magerl M. Differences and similarities in the mechanisms and clinical expression of bradykinin-mediated vs. mast cell-mediated angioedema. Clin Rev Allergy Immunol 2021. Aug;61(1):40–9. DOI: 10.1007/s12016-021-08841-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waljee AK, Rogers MAM, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: Population based cohort study. BMJ 2017. Apr;357:j1415. DOI: 10.1136/bmj.j1415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yao T-C, Wang J-Y, Chang S-M, et al. Association of oral corticosteroid bursts with severe adverse events in children. JAMA Pediatr 2021. Jul;175(7):723–9. DOI: 10.1001/jamapediatrics.2021.0433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yao T-C, Huang Y-W, Chang S-M, Tsai S-Y, Wu AC, Tsai H-J. Association between oral corticosteroid bursts and severe adverse events: A nationwide population-based cohort study. Ann Intern Med 2020. Sep;173(5):325–30. DOI: 10.7326/M20-0432 [DOI] [PubMed] [Google Scholar]
- 18.Sabato V, Gaeta F, Valluzzi RL, Van Gasse A, Ebo DG, Romano A. Urticaria: The 1-1-1 criterion for optimized risk stratification in β-lactam allergy delabeling. J Allergy Clin Immunol Pract 2021. Jun 16;S2213-2198(21)00664-4. DOI: 10.1016/j.jaip.2021.05.037. Online ahead of print. [DOI] [PubMed]
- 19.Fricke J, Ávila G, Keller T, et al. Prevalence of chronic urticaria in children and adults across the globe: Systematic review with meta-analysis. Allergy 2020. Feb;75(2):423–32. DOI: 10.1111/all.14037 [DOI] [PubMed] [Google Scholar]
- 20.Kalambay J, Ghazanfar H, Martes Pena KA, Munshi RA, Zhang G, Patel JY. Pathogenesis of drug induced non-allergic angioedema: a review of unusual etiologies. Cureus 2017. Aug;9(8):e1598. DOI: 10.7759/cureus.1598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Long BJ, Koyfman A, Gottlieb M. Evaluation and management of angioedema in the emergency department. West J Emerg Med 2019. Jul;20(4):587–600. DOI: 10.5811/westjem.2019.5.42650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lumry WR. Hereditary angioedema: The economics of treatment of an orphan disease. Front Med (Lausanne) 2018. Feb;5:22 DOI: 10.3389/fmed.2018.00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swanson TJ, Patel BC. Acquired angioedema. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2021. Jan. Accessed Jul 23, 2021. https://www.ncbi.nlm.nih.gov/books/NBK430889/ [PubMed] [Google Scholar]
- 24.The Kaiser Permanente Research Preliminary Data Application. Accessed. https://kpscresapp.kp-scalresearch.org/signon.jsp
- 25.Staevska M, Gugutkova M, Lazarova C, et al. Night-time sedating H1-antihistamine increases daytime somnolence but not treatment efficacy in chronic spontaneous urticaria: A randomized controlled trial. Br J Dermatol 2014. Jul;171(1):148–54. DOI: 10.1111/bjd.12846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Staevska M, Popov TA, Kralimarkova T, et al. The effectiveness of levocetirizine and desloratadine in up to 4 times conventional doses in difficult-to-treat urticaria. J Allergy Clin Immunol 2010. Mar;125(3):676–82. DOI: 10.1016/j.jaci.2009.11.047 [DOI] [PubMed] [Google Scholar]
- 27.Barniol C, Dehours E, Mallet J, Houze-Cerfon CH, Lauque D, Charpentier S. Levocetirizine and prednisone are not superior to levocetirizine alone for the treatment of acute urticaria: A randomized double-blind clinical trial. Ann Emerg Med 2018. Jan; 71(1):125–131.e1. DOI: 10.1016/j.annemergmed.2017.03.006 [DOI] [PubMed] [Google Scholar]
- 28.Palungwachira P, Vilaisri K, Musikatavorn K, Wongpiyabovorn J. A randomized controlled trial of adding intravenous corticosteroids to H1 antihistamines in patients with acute urticaria. Am J Emerg Med 2021. Apr;42:192–7. DOI: 10.1016/j.ajem.2020.02.025 [DOI] [PubMed] [Google Scholar]
- 29.Sharma M, Bennett C, Cohen SN, Carter B. H1-antihistamines for chronic spontaneous urticaria. Cochrane Database Syst Rev 2014. Nov;2014(11):CD006137. DOI: 10.1002/14651858.CD006137.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asero R. Intolerance to nonsteroidal anti-inflammatory drugs might precede by years the onset of chronic urticaria. J Allergy Clin Immunol 2003. May;111(5):1095–8. DOI: 10.1067/mai.2003.1444 [DOI] [PubMed] [Google Scholar]
- 31.Stratta P, Badino G. Scombroid poisoning. CMAJ 2012. Apr;184(6):674. DOI: 10.1503/cmaj.111031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheilitis MC. Accessed Jul 23, 2021. https://www.uptodate.com/contents/cheilitis