Introduction
France is a country in Western Europe with a population of 6706 million in 2020 (1). This country has a universal health care system financed by a compulsory health insurance taxation on the basis of worker income, which refunds patients 70% of most health care costs and 100% for costly or long-term diseases, such as Chronic kidney disease (CKD). CKD affects nearly 3 million people, and the prevalence increases by 2% each year (1). Among them, 89,692 are treated by dialysis or received a kidney transplant. France has been a pioneer in transplantation, with the first living donor kidney transplant performed in 1952 (2). After two decades of transplants with living donors, the first bioethics laws were enacted in 1976, authorizing deceased donor procurement and instituting three rules for organ donation: (1) all adult residents are presumed to be consenting to donate except in case of expression of refusal during lifetime, (2) donation is anonymized, and (3) donation is free of charge. Since 2004, organ procurement is organized by the Biomedicine Agency, which is in charge of ensuring equity and safety of organ allocation and collecting donor characteristics, recipient characteristics, and follow-up through the French national database called CRISTAL. The national allocation system for deceased donors is made on the basis of a scoring system from the local and national levels and also, some national allocation priorities (Figure 1). Kidney transplantation is currently performed in 47 centers, mostly public university hospitals, of which 14 perform 60% of the transplants (3).
Figure 1.
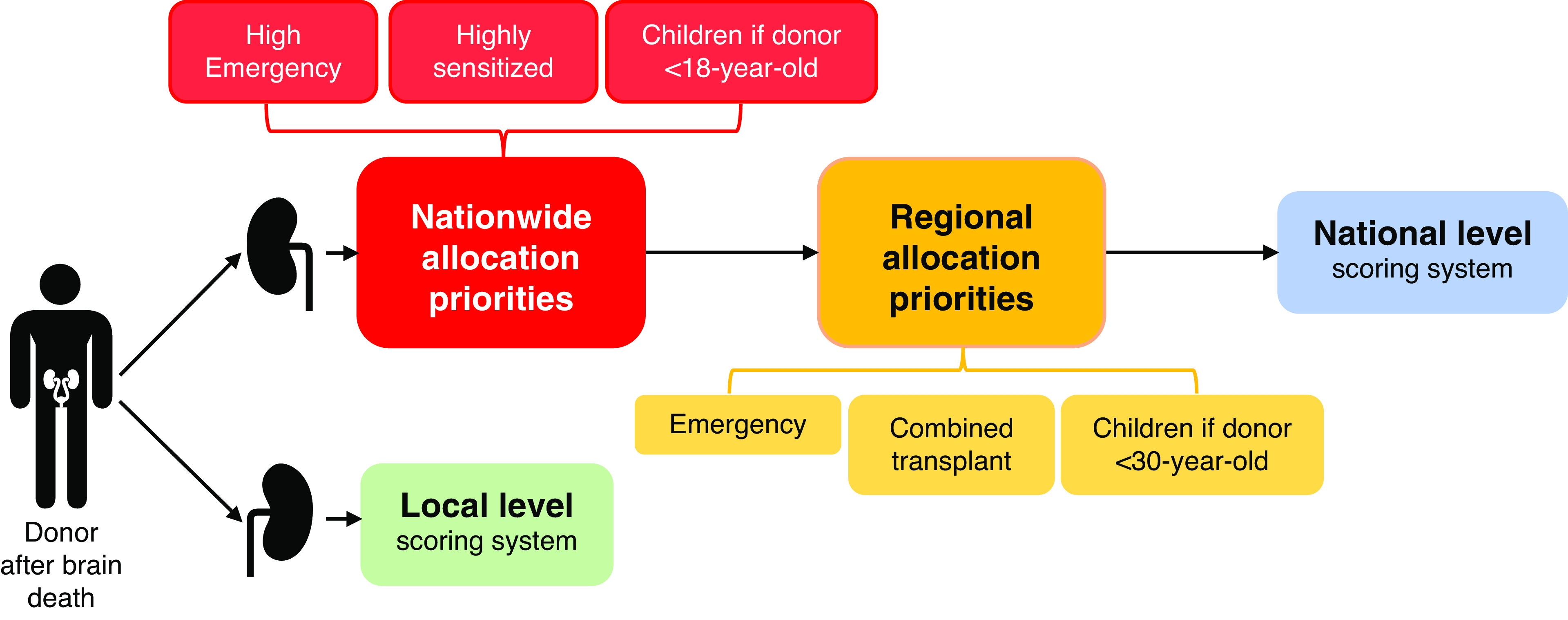
French national allocation policy for kidney from deceased donors. Adapted from the (rules of allocation of organs from deceased donor), Agence de la biomédecine, 2015. The French allocation system for deceased donors is on the basis of a scoring system, from the local and national levels and also, some regional priorities. One kidney is allocated at the local level, i.e., referred to the transplant center located in the district where the kidney is procured. The other kidney is allocated at the national level, according to nationwide priorities (high emergency, highly sensitized patients, children if donor <18-year-old). Then, according to the regional priorities (emergency, combined transplants, children if donor <30-year-old). Finally, in the absence of national or regional priorities, the kidney is allocated at the national level according to the French scoring system, which takes into account dialysis duration, time on the waiting list, recipient age, donor recipient HLA and age matching, and travel time between procurement and transplant centers.
Number of Kidney Transplant Recipients
Since the start of the French national registry in 1959, a total of 91,565 kidneys have been transplanted. Among them, 42,409 are still functional, corresponding to a prevalence of 628 per million people in the general population (3), whereas 50,501 patients are on dialysis. In 2019, 3643 kidney transplants were performed, representing a ratio of 53.9 per million people and placing France in second place in Europe behind Spain (3). Kidney transplantation activity, although increasing continuously, is far from covering the rising demand, and inexorably, patients accumulate on the waiting list (4) (Supplemental Table 1). To tackle this challenging obstacle, France has made considerable efforts to promote transplants from living donors, and the organ procurement of donors after cardiac arrest was reintroduced in 2006 (4). In 2014, a significant milestone was also reached with the opening of a program authorizing the recovery of kidneys from Maastricht III non-heart-beating donors, allowing doctors to perform 826 new transplants in 5 years with similar or even better early outcomes than those from brain-dead donors (3,5,6).
Number of Kidney Transplant Candidates on the Waiting List
The growth rate of the number of people on the waiting list increases from year to year (further details are provided in Supplemental Table 1), with 16,181 patients waiting for a transplant on January 1, 2020, including 5269 new patients on the waiting list compared with 4557 new patients in 2013 (+16%). Among these candidates, 8642 are active and 7539 are inactive (temporary contraindication) on the list (3). The median waiting time between registration and transplantation increased progressively in recent years and has reached 22.6 months (3). It is important to note that there are discrepancies according to age categories and regional registration areas, reflecting various appreciations in indications for kidney transplantation (7). In order to mitigate these discrepancies, the Biomedicine Agency modified its allocation system score in 2015 by improving the quality of age pairing and integrating road distances in minutes between the sampling and transplant locations for assigning the graft.
Percentage of Live Donor Versus Deceased Donor Transplants
In 2019, 510 kidney allotransplantations from a living donor were performed, representing 14% of the total number of kidney transplants (3). This ratio remains insufficient, so two main efforts were made for increasing this activity. First, French bioethics laws were revised in 2011 to allow people with a close and emotional bond for at least 2 years with the recipient to donate a kidney. Second, a paired kidney exchange program was introduced in the event of blood group incompatibility between the donor and the recipient. However, this program is struggling to develop because it requires complex logistics, and some centers also perform ABO-incompatible transplants. Consequently, it allowed only 12 kidneys transplants since it was set up in 2013 (3). Facing the predictable increase in the number of candidates, all efforts should be put together for increasing the number of living donor transplants, and this activity is largely promoted by the Biomedicine Agency. Concerning deceased donors, 89% were brain-dead donors, 1% were Maastricht II non-heart-beating donors, and 10% were Maastricht III non-heart-beating donors in 2019. Furthermore, among the donors after brain death, 52% were expanded criteria donors (3). Further details on the evolution of organ procurement according to the donor type during the last 10 years are provided in Supplemental Table 2.
Length of Hospital Stay After Kidney Transplantation
The median length of hospital stay after kidney transplantation is 14 days (interquartile range, 11–19) (8). It manly depends on hospital logistics, medical resources, donor type, and recipients’ characteristics. Moreover, the absence of ambulatory facilities, like outpatient clinics, or day hospitalization significantly increases length of stay. To note, some patients, especially elderly or frail patients, can be hospitalized much longer, with a median of 16 days (interquartile range, 12–22) after 65 years old (8). Hence, some centers are organizing close care networks with rehabilitation centers for reinforcing the postoperative period and improving morbidity, mortality, and quality of life after such transplant.
Surgeons Who Perform the Kidney Transplants
Since 1952, kidney transplants are historically performed by urologists in France (2). Kidney procurements and low–surgical risk transplants from deceased donors are mainly performed by junior urologists. High–surgical risk transplants and living donor transplants are usually performed by senior urologists, accompanied by a junior urologist. In case of a high-risk vascular transplant, such as a transplantation on vascular prothesis, the surgery can also be performed with the help of a vascular surgeon. To note, kidney transplant surgery is rarely an exclusive activity for surgeons, this may increase cold ischemia time. However, the mean cold ischemia time was 15.4 hours in 2019 and has tended to decrease in the past 10 years (3).
Transplant Surgery Costs
France is made on the basis of a national solidarity system and takes in charge a list of serious and/or chronic diseases requiring a prolonged and costly treatment. Chronic kidney failure is one of them and is fully covered for the care related to this pathology. The effective surgery costs from the removal to the transplantation are estimated at 13,835.44€ ($16,340.90) for a deceased donor and 13,601.66€ ($16,064.78) for a living donation (including the follow-up) (9). However, these amounts could significantly increase according to the patient's postoperative complications and comorbidities. These costs are integrally covered without out-of-pocket expenses or advance payment from the patient.
Post-Transplant Care for Kidney Transplant Recipients
Historically, post-transplant care is usually provided by the transplant nephrologist (2). The recipient is hospitalized in a nephrology/kidney transplant department before and right after the transplant surgery. Then, the follow-up is carried out in the transplant center, with the nephrologist who followed the patient before the transplant, or jointly. Some guidelines of good practices were published for the management of a kidney transplant recipient by the French High Authority for Health in 2007 (10). The initial follow-up is weekly during the first 3 months, then bimonthly until 6 months, and monthly until 1 year. After 1 year, the follow-up is variable depending on the centers and the patients’ condition, and it is usually every 1–4 months according to the centers and the patients’ conditions.
Costs of Immunosuppression
The costs of immunosuppression and other medications related to the transplant are covered by national insurance. Therefore, patients have few out-of-pocket expenses, with a fixed price per box of medication up to a limit of 50€ ($59) per year for medical expenses related to their pathology.
Graft and Patient Survival after Transplant
The short-term allograft survival has steadily improved in France, with a current survival rate of 92% at 1 year. However, long-term survival has quietly decreased over the last 20 years, with a current allograft survival rate of 78% at 5 years and 60% at 10 years (Supplemental Figure 1) (3). It is also observed concerning patient survival, with a current survival rate of 97% at 1 year, 88% at 5 years, and 75% at 10 years (3). The main hypothesis for this relative decrease is that the ages of donors and recipients have increased, as well as the complexity of recipients with more comorbidities and a growing immunologic risk.
Major Barrier to Successful Kidney Transplantation
The major barrier to successful kidney transplantation in France is the constant increase in the immunologic risk of patients. Many barriers have been crossed with the desensitization protocols and the multiple transplantations, but antibody-mediated rejection remains the main cause of allograft failure in kidney transplants (11). For this purpose, national priorities have been created for hypersensitized patients (i.e., with a virtual calculated panel reactive antibody ≥85% or 70% at time of transplant). These programs represent 13% of transplants performed in 2019 (Table 1). The main program since 2005 is the Authorized Antigens Program, similar to the Acceptable Mismatch Program from Eurotransplant. To be included in this program, patients must have a calculated panel-reactive antibody (cPRA) ≥85% and a serum tested with Single Antigen Flow Beads assays every 3 months to detect potential anti-HLA antibodies emergence and then, prevent unexpected positive crossmatches. This program initially caused several problems by authorizing the transfer of young donor grafts to immunized elderly recipients; a rule with an age criterion was added later to solve this problem. Another problem was the exponential increase of patients in this program with the advent of high-definition techniques to detect anti-HLA antibodies, especially for class 2 anti-HLA antibodies, and the heterogeneity of practices across HLA laboratories to classify antigens as prohibited. The Biomedicine Agency is working to homogenize practices across HLA laboratories.
Table 1.
Type of allocation of kidney transplants from donors after brain death in 2019
| Type of Allocation | No. of Transplants (%) |
|---|---|
| Local or regional on the basis of the scoring systema | 1384 (50) |
| National on the basis of the scoring systema | 788 (28) |
| Dual kidney transplant | 19 (1) |
| Priorities | 592 (21) |
| Urgent | 11 (0.4) |
| Highly sensitized patients | 371 (13) |
| Sensitized patients | 30 (1) |
| Combined transplant | 115 (4) |
| Children | 64 (2) |
On the basis of the data from the French National Report 2019 (3).
The French scoring system takes into account dialysis duration, time on the waiting list, recipient age, donor recipient HLA and age matching, and travel time between procurement and transplant centers.
Disclosures
G. Divard received grants from the French Foundation for Medical Research and the French-Speaking Society of Nephrology, Dialysis and Transplantation. V. Goutaudier received a grant from the French-Speaking Society of Transplantation.
Funding
None.
Acknowledgments
The authors thank the French Biomedicine Agency for the completeness of data contained in its annual reports, which was very valuable for the realization of this work.
The content of this article reflects the personal experience and views of the author and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author(s).
Footnotes
This article contains a podcast at https://www.asn-online.org/media/podcast/K360/2021_10_28_KID0002402021.mp3
Author Contributions
G. Divard and V. Goutaudier wrote the original draft, and reviewed and edited the manuscript.
Supplemental Material
This article contains supplemental material online at http://kidney360.asnjournals.org/lookup/suppl/doi:10.34067/KID.0002402021/-/DCSupplemental.
Graft survival according to the transplant period. Download Supplemental Figure 1, PDF file, 190 KB (189.6KB, pdf)
Evolution of the number of kidney transplants and the number of candidates on the waiting (active and inactive) list during the last 10 years. Download Supplemental Table 1, PDF file, 190 KB (189.6KB, pdf)
Evolution of organ procurement according to the donor type in France during the last 10 years. Download Supplemental Table 2, PDF file, 190 KB (189.6KB, pdf)
References
- 1.The National Institute of Statistics and Economic Studies , [Bilan démographique 2020], Montrouge, France, 2021
- 2.Michon L, Hamburger J, Oeconomos N, Delinotte P, Richet G, Vaysse J, Antoine B: Une tentative de transplantation renale chez l’homme. Aspects Medicaux et Biologiques Presse Med 61: 1419, 1953 [PubMed] [Google Scholar]
- 3.Agence de la biomédecine : The French National Report 2019. France, Saint-Denis La Plaine, 2020 [Google Scholar]
- 4.Hiesse C: [Kidney transplantation epidemiology in France]. Nephrol Ther 9: 441–450, 2013 [DOI] [PubMed] [Google Scholar]
- 5.Antoine C, Mourey F, Prada-Bordenave E; Steering committee on DCD program : How France launched its donation after cardiac death program. Ann Fr Anesth Reanim 33: 138–143, 2014 [DOI] [PubMed] [Google Scholar]
- 6.Savoye E, Legeai C, Branchereau J, Gay S, Riou B, Gaudez F, Veber B, Bruyere F, Cheisson G, Kerforne T, Badet L, Bastien O, Antoine C; cDCD National Steering Committee : Optimal donation of kidney transplants after controlled circulatory death. Am J Transplant 21: 2424–2436, 2021 [DOI] [PubMed] [Google Scholar]
- 7.Bayat S, Macher MA, Couchoud C, Bayer F, Lassalle M, Villar E, Caillé Y, Mercier S, Joyeux V, Noel C, Kessler M, Jacquelinet C; REIN registry : Individual and regional factors of access to the renal transplant waiting list in France in a cohort of dialyzed patients. Am J Transplant 15: 1050–1060, 2015 [DOI] [PubMed] [Google Scholar]
- 8.Tuppin P, Bessou A, Legeai C, Vigneau C, Couchoud C: Two-year management after renal transplantation in 2013 in France: Input from the French national health system database. Nephrol Ther 14: 207–216, 2018 [DOI] [PubMed] [Google Scholar]
- 9.Sainsaulieu Y, Sambuc C, Logerot H, Bongiovanni I, Couchoud C: [Cost of a renal transplant: Medico-economic analysis of the amount reimbursed by the French national health program to finance renal transplantation]. Nephrol Ther 10: 228–235, 2014 [DOI] [PubMed] [Google Scholar]
- 10.Haute Autorité de Santé HAS : [Suivi ambulatoire de l’adulte transplanté rénal au-delà de 3 mois après transplantation. Recommandation de bonne pratique]. France, Saint-Denis La Plaine, 2007 [Google Scholar]
- 11.Lohéac C, Aubert O, Loupy A, Legendre C: [Identifying the specific causes of kidney allograft loss: A population-based study]. Nephrol Ther 14: S39–S50, 2018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Graft survival according to the transplant period. Download Supplemental Figure 1, PDF file, 190 KB (189.6KB, pdf)
Evolution of the number of kidney transplants and the number of candidates on the waiting (active and inactive) list during the last 10 years. Download Supplemental Table 1, PDF file, 190 KB (189.6KB, pdf)
Evolution of organ procurement according to the donor type in France during the last 10 years. Download Supplemental Table 2, PDF file, 190 KB (189.6KB, pdf)


