Abstract
This paper aims to develop a telehealth success model and discusses three critical components: (1) health information quality, (2) electronic health record system quality, and (3) telehealth service quality to ensure effective telehealth service delivery, reduce professional burnout, and enhance access to care. The paper applied a policy analysis method and discussed telehealth applications in rural health, mental health, and veterans health services. The results pointed out the fact that, although telehealth paired with semantic/organizational interoperability facilitates value-based and team-based care, challenges remain to enhance user (both patients and clinicians) experience and satisfaction. The conclusion indicates that approaches at systemic and physician levels are needed to reduce disparities in health technology adoption and improve access to telehealth care.
Keywords: Electronic Health Records, Telehealth, Telemental health, Pandemic, Health outcomes, Health Policy
Executive Summary
A telehealth platform integrated with an interoperable electronic health record (EHR) system can contribute directly toward achieving the often-discussed “quadruple aim” [1]—better health outcomes, improved patient experience, lower costs, and improved clinician experience. This paper develops a telehealth success model and discusses three critical components: (1) health information quality, (2) EHR system quality, and (3) telehealth service quality to ensure effective health care service delivery, reduce professional burnout, and enhance access to care.
Despite the benefits of telehealth in rural health, mental health, and Veterans Administration health services, disparities continue to exist in access to care. Patients without internet service, appropriate devices, or digital literacy skills experience greater challenges in accessing care via telehealth. The COVID-19 pandemic has also caused substantial financial strain on hospitals, and it is uncertain if the current reimbursement and payment model for telehealth service/devices and regulation flexibility for virtual consulting will continue after the pandemic is over.
To help integrate telehealth into clinical practice and improve patient care, health policy at the systemic level should accelerate the uptake of telehealth. On the industry level, hospitals should identify adoption strategies for different types of telehealth services and evaluate telehealth products for health care delivery. On the physician level, health providers should offer the same level of care and follow the same treatment guidelines for telehealth services as with in-person visits and ensure that their practices are compliant with applicable regulations.
Development of Telehealth
Telehealth has become a rapidly growing sector of health care delivery systems. Previous studies show evidence that telehealth tools and services increase the overall effectiveness of physicians in (1) counseling patients with chronic conditions, (2) psychotherapy support for behavioral interventions, and (3) remote monitoring of patients [2].
The shortage of health providers and increasing consumer demand (from the aging population and people diagnosed with chronic diseases) were key factors in expanding the scope and scale of telehealth services [3]. The 2019 annual report of the Association of American Medical Colleges projected a shortfall of 40,000 to 122,000 physicians in the United States over the next decade, with a shortage of 29,000 to 42,900 doctors in 2020 [4]. To use telehealth as a new strategy to stretch the physician supply, the Interstate Medical Licensure Compact standardized licensing requirements that allow physicians to practice in multiple states and provide remote digitalized services [5]. To further remove regulatory and reimbursement barriers to telehealth services, telehealth parity laws require commercial health insurers to provide equal coverage for telehealth and in-person services in 38 states and the District of Columbia [6]. By January 2017, all state Medicaid programs reimburse teleradiology, 49 cover tele–mental health services, and 36 states cover various remote telehealth services [2].
The COVID-19 pandemic accelerated the adoption of telehealth tools and services. Amid the pandemic, some hospitals are seeing 500 to 600 patients per day via video or telephone visits [7]. To enable providers to use telehealth services, Medicare implemented temporary payment flexibility to allow more beneficiaries to benefit from virtual care services and more providers to be eligible to bill for telehealth services at the same payment rate as they would receive for in-person services [8]. The Centers for Medicare and Medicaid Services (CMS) added 135 allowable services, including emergency department visits; initial nursing facility and discharge visits; home visits; and physical, occupational, and speech therapy services [9]. With these initiatives, US provider systems are rapidly deploying digitalized services for two main goals:
Forward triage to screen patients with COVID-19 symptoms before arrival to a health care facility so as to reduce exposure to the virus [10]
Continue patient care and provide virtual consultation to nonvirus patients, especially those with chronic diseases
Telehealth Success Model
This paper applies a conceptual model (Figure 1) based on Delone and McLean’s [11] model of information systems success to assess the impact of hospital medical record interoperability on telehealth service outcomes. As framed by Delone and McLean [11], a sustainable information system depends on positive results from the quality of information, service, and systems, as well as interrelated measures of user satisfaction, use, and net benefits.
Figure 1.
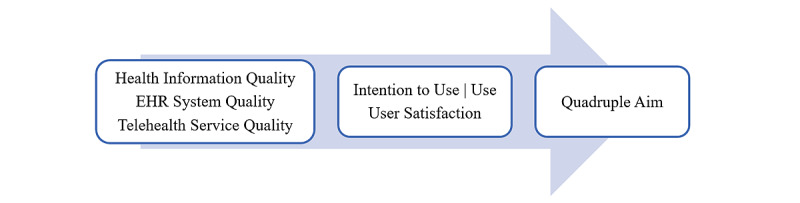
Telehealth success model. EHR: electronic health record.
Health Information Quality
Device interoperability and data integration are key aspects of telehealth delivery. Hospital interoperability (Figure 2) covers three types of information exchange: (1) sending, receiving, and incorporating health records that support electronic referral loops; (2) electronic access for both physicians and patients to their health information; and (3) public health surveillance that collects and integrates health-related data to assist planning, implementing, and evaluating public health practice [12].
Figure 2.
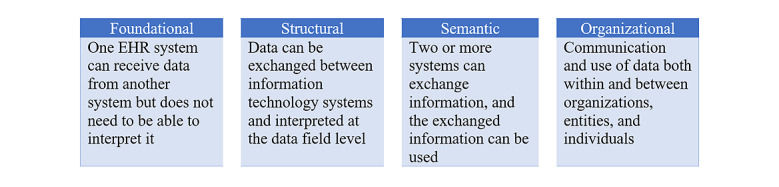
Hospital interoperability levels. EHR: electronic health record.
For value-based care to achieve and protect patient safety, the EHR system needs to deliver accurate and clinically appropriate data across care settings to both physicians and patients. Studies suggest that hospital sharing of diagnostic data with providers within their system is associated with lower patient mortality, and the hospital interoperability level is associated with improved process quality related to conditions of acute myocardial infarction, heart failure, and pneumonia at acute care hospitals [13-15].
However, establishing a telehealth platform in a short period of time amid pandemic conditions could put health information—patient names, address, dates, diagnoses, and more—at higher risks to safety and security [16]. The introduction of increasingly complicated technology into already complex work environments may trigger various unintended interactions that undermine or outweigh the potential benefits of the new technology [17]. Moreover, with an exponential growth in clinical data, it becomes critical to code symptoms (eg, allergies) and medications correctly to ensure patient safety and care quality [18].
EHR System Quality: Maximizing the Benefits of Telehealth
Integrating telehealth programs into a hospital’s existing EHR system infrastructure helps maximize the benefits of telemedicine, as providers and staff already have experience working with the baseline system [19]. Over 95% of US hospitals reported using a certified EHR platform [12]. However, many hospitals run separate systems for doctors, labs, radiologists, and remote monitoring devices; the technical and data incompatibilities between different vendors make data sharing more vulnerable to cybersecurity threats [20]. Suboptimally integrated systems also added clerical burdens on physicians that can help lead to professional burnout. For every hour of clinical work, physicians spent 2 hours on EHR-related tasks, threatening the capacity and performance of the health system [21].
In 2020, the US Office of the National Coordinator for Health Information Technology (ONC) established requirements for a secure standards-based application programming interface (API) to support each individual patient’s access and control of their electronic health information [22,23]. The increasing data volumes, new data types, and various data sources collected from telehealth services can make it difficult and labor-intensive to match or identify the correct patient between systems [24]. Thus, a wide-scale adoption of common standards would drive data sharing and make integration more consistent and efficient, thereby providing clinically useful information and mitigating physician burnout [25].
Telehealth Service Quality
Advanced interoperability—especially at semantic and organizational levels—can enable telehealth to expand access, exchange information, and provide user-centered services to both physicians and patients [26]. Current telehealth services use devices such as wearable monitors, smartphones, mobile apps, video, email, and web portals to deliver three types of care: (1) remote monitoring of patients and collecting vital signs and health data for care plan management, (2) counseling and interacting with patients at home, and (3) triaging patients to screen them to reduce exposures to viruses and thereby free up hospital resources during emergencies [27].
Telehealth Use in Clinical Practice
Rural Health Services
Approximately 80% of rural areas in the United States are classified as medically underserved and in health professional shortage areas [28,29]. These regions are lacking the physicians, registered nurses, and behavioral health providers (including psychiatrists, psychologists, and therapists) [30]. The patient-to-primary care physician ratio in rural areas is only 39.8 physicians per 100,000 people, compared to 53.3 in urban areas [31]. The shortage disproportionately impacts rural residents who tend to be older, have lower socioeconomic status, are more reliant on public insurance, and have worse health outcomes [32,33].
For rural residents, telehealth care increased access to experienced providers and high-quality care [34,35], improved continuity of care and health outcomes [36], and reduced health disparities [37]. Studies have shown that greater adoption of telehealth was associated with facilities in rural locations [38]. Between 2010 and 2017, telehealth visits have increased among rural Medicare beneficiaries, with a 425% increase for tele–mental health services [36].
Tele–Mental Health Services
There are two primary uses for tele–mental health: provider consultations with mental health specialists in primary care and emergency department settings, and the direct provision of mental health services including home-based services [37,38].
For people experiencing serious mental illness, telehealth has the potential to improve quality of life and general mental health, reduce depressive symptoms, build more confidence in managing depression, and increase satisfaction with mental health and coping skills compared to treatment offered in-person only [36,39]. For people experiencing substance use disorders (SUDs), treatments delivered through telehealth have resulted in reductions in alcohol consumption, increased tobacco cessation, and increased engagement and retention in opioid use disorder treatment [36]. Between 2016 and 2019, SUD treatment offered through telehealth increased from 13.5% to 17.4% [40].
Veterans’ Health Services
As one of the early adopters of telehealth, the Veterans Health Administration (VHA) is currently the largest telehealth provider in the United States [41]. In 2018, VHA conducted over a million telehealth visits [42]. A total 10% of the visits used VA Video Connect (VVC), a secure video teleconferencing platform that allows providers to treat veterans on their mobile devices or personal computers at a location of the veteran’s choice [43,44]. The 2018 “Maintaining Internal Systems and Strengthening Integrated Outside Networks” (“MISSION”) Act included mandates for VHA to establish an “Anywhere to Anywhere” telehealth network, where VHA providers in outpatient mental health and primary care service lines nationwide will be both capable and experienced with providing telehealth (VVC) to non-VA locations [43]. The demands for VA telehealth services also increased during the pandemic [45]. Tele–mental health sessions via VVC increased 42% at one VA medical center in South Carolina, from 1429 appointments in January 2020 to 2034 in March 2020 [43,45].
Patient-Centered Care
A telehealth program paired with the right EHR system can serve as a care collaboration platform and help optimize team-based care delivery [13,46]. It connects off-site specialists in the fields of cardiology, psychiatry and behavioral health, oncology, and infectious disease with patients at home or intensive care units (ICUs) [2]. Physicians can easily access and send health records from one interface to another (mobile, computer, or tablet) remotely using a protected account to diagnose and assess symptoms as an in-person consultation [47].
Telehealth interventions, particularly remote monitoring and SMS text messaging, were associated improvements in obstetric outcomes, perinatal smoking cessation, breastfeeding, and schedule optimization for high-risk obstetrics [48]. For at-risk patients with chronic disease, remote monitoring devices continuously capture physiological data such as heart rate, blood glucose, oxygen saturation level, body temperature, blood pressure, and weight over time [2,49]. Evidence also suggests telehealth services allowed physicians to better communicate with patients on treatment plans that are appropriate for their culture, race, gender, sexual orientation, and lived experience [35,48,50].
Population Health Management
An EHR system with organizational interoperability allows institutions to aggregate community-level data from disparate sources to track influenza/disease trends for population health [51,52]. For example, CMS requires hospitals to electronically report public health data such as syndromic surveillance data, electronic case reporting, reportable laboratory results, and more. Sharing critical data among health care systems, especially during a pandemic, assists public health authorities to predict clusters of outbreaks and make timely and efficient guidance for quarantine and better containment [53,54].
Postpandemic Health Care Needs and Challenges
Regulation Uncertainties
The COVID-19 pandemic in the United States is affecting different areas at different times and levels: cases spike in some states while others face the threats of both COVID-19 resurgence and seasonal flu [55]. Many hospitals are providing a combination of traditional in-person visits and telehealth services that allow remote virtual consultations to patients [34].
Early in March 2020, CMS modified policies to lift originating site restrictions and expand the type of visits allowed virtually [56]. However, after the pandemic, hospitals may shift telehealth services from urgent care and COVID-19 screenings and treatment to regular care visits [57]; it is unclear how current more flexible regulation and payment arrangements will change [56,58]. Will there be permanent polices to reimburse virtual care and remote monitoring devices? Will telehealth reimbursement rates be set at the same level with in-person visits? Will there be financial incentives to provide reliable broadband access to rural or small hospitals [59]?
With hospitals and the health care system faced with uncertainties about the duration of this pandemic and the structure of future telehealth benefits, the development of clear regulatory requirements and timetables could help reduce administrative and technological constraints associated with virtual health care delivery and encourage further investment in health care information technology (IT) infrastructure [60,61].
Hospital Financing Challenges
The COVID-19 pandemic has created substantial financial difficulties for both hospitals and the health system [62,63]. As a result of cancelled elective surgeries and nonessential medical procedures, which often generate more revenues than ICU and emergency care, US hospitals continue to experience substantial losses in revenue [64]. Expenses also have increased sharply from purchasing needed for personal protective equipment, COVID-19–associated hospitalizations, and providing additional support to frontline health workers [62]. The American Hospital Association estimates a total 4-month financial impact of US $202.6 billion in losses for US hospitals and health systems, or an average of US $50.7 billion per month [62]. These financial loss and additional system maintenance/implementation costs for telehealth and EHR systems will require decision makers to establish more effective strategies to use hospital resources and workforce [64,65].
Disparities in Telehealth Access
Although most hospitals in the United States have adopted interoperable EHR systems, there is little evidence about whether small, rural, and safety net hospitals are keeping up [66]. Compared to more technologically advanced hospitals, smaller and rural hospitals have limited broadband access [59], less interoperability and health care IT management experience [67], and staff with less technological familiarity [68,69]. Because of the uneven adoption of telemedicine services, some small clinics and postacute care facilities are unable to receive or share patient data [70,71].
Substantial disparities in access to telehealth services also remain [72]. Evidence suggests geographical disparities, profit-based discrimination, technology deployment cost, and socioeconomic factors played key roles in the telehealth use gap [59,72,73]. Moreover, people 65 years and older, with disabilities, experiencing poverty, and who are non-White are less likely to use telehealth services because of lower smartphone or computer ownership, limited (home) broadband internet access, and low digital literacy [36]. A recent study of 134,225 completed primary care visits also reported that early adopters of online scheduling were more likely to be young, White, and commercially insured [74].
Regulatory Process for EHR Market
To ensure that EHRs cooperate effectively in an interoperable structure, substantial governmental regulation has been put into place. In the United States, CMS and the ONC regulate EHR privacy, security, and standards for hospitals or health providers and health IT developers [75,76]. In July 2021, the Interoperability and Patient Access final rule began to require CMS-regulated payers to remove industry siloes and support Patient Access API, Provider Directory API, and Payer-to-Payer Data Exchange to achieve greater semantic interoperability within the health care system while complying with existing Health Insurance Portability and Accountability Act (HIPAA) requirements [75,77]. On the technical level, CMS adopted Health Level 7 Fast Healthcare Interoperability Resources Release 4.0.1 to standardize implementing privacy and security features for provider organizations [78].
In the European Union, to facilitate cross-border EHR interoperability, the General Data Protection Regulation established explicit rules to process and protect patient health data [79]. On the technical level, the eHealth Digital Service Infrastructure has enabled provider organizations to exchange patient summaries and e-prescriptions [78]. In the Asia-Pacific region, Singapore, Japan, and Australia have instituted regulations on software qualification, software as a medical device, and presubmission consultation by regulatory authorities to facilitate EHR interoperability [80-82]. In Singapore, for example, the National Electronic Health Record system sets technical standards (including architecture, security, and operations) for the digital health market and monitors user functionality and risk to protect data security [83].
Discussion
Studies suggest that telehealth programs paired with the right EHR system enhance care access, increase patient satisfaction, and reduce medical spending [84,85], and by improving clinician experience, the integrated system can contribute to achieving the quadruple aim.
To help integrate telehealth into clinical practice and improve patient care, on a systemic level, health policies should accelerate the uptake of telehealth, including tele–mental health, to improve care quality, cost-effectiveness, and value of care [86]. Federal and state governments can use disruptive reimbursement and funding strategies on training primary and mental health care providers, workforce, licensure, and cultural sensitivity for long-term telehealth practice [34,87]. Regulators also need to assess and set standards for malpractice liability and protect patient safety and confidentiality that may result from telehealth deployment [88].
On an industry/organization level, hospitals need to identify strategies to adopt and integrate different types of telehealth services, and evaluate telehealth products for health care delivery [66,70]. Future studies are needed to provide evidence on telehealth practice guidelines and service models.
On the physician level, clinicians who provide telehealth should offer the same level of care and follow the same treatment guidelines they would follow for in-person visits [89]. Moreover, physicians should closely follow HIPAA rules, state laws, and medical board definitions to ensure their practices are compliant with applicable regulations while implementing telehealth [57].
Abbreviations
- API
application programming interface
- CMS
Centers for Medicare and Medicaid Services
- EHR
electronic health record
- HIPAA
Health Insurance Portability and Accountability Act
- ICU
intensive care unit
- IT
information technology
- MISSION
Maintaining Internal Systems and Strengthening Integrated Outside Networks
- ONC
Office of the National Coordinator for Health Information Technology
- SUD
substance use disorder
- VHA
Veterans Health Administration
- VVC
VA Video Connect
Footnotes
Conflicts of Interest: None declared.
References
- 1.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–6. doi: 10.1370/afm.1713. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=25384822 .12/6/573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017 Oct 19;377(16):1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 3.Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV. An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff (Millwood) 2013 Nov;32(11):2013–20. doi: 10.1377/hlthaff.2013.0714.32/11/2013 [DOI] [PubMed] [Google Scholar]
- 4.The complexities of physician supply and demand: projections from 2018 to 2033. Association of American Medical Colleges. [2021-02-17]. https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf .
- 5.Frieden J. COVID-19 is making the physician shortage worse, groups say. Medpage Today. [2021-01-15]. https://www.medpagetoday.com/infectiousdisease/covid19/85661 .
- 6.Abuzeineh M, Muzaale AD, Crews DC, Avery RK, Brotman DJ, Brennan DC, Segev DL, Al Ammary F. Telemedicine in the care of kidney transplant recipients with coronavirus disease 2019: case reports. Transplant Proc. 2020 Nov;52(9):2620–2625. doi: 10.1016/j.transproceed.2020.07.009. http://europepmc.org/abstract/MED/32798002 .S0041-1345(20)32629-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Redford G. Delivering more care remotely will be critical as COVID-19 races through communities. Association of American Medical Colleges. 2020. Mar 23, [2020-03-28]. https://www.aamc.org/news-insights/delivering-more-care-remotely-will-be-critical-covid-19-races-through-communities .
- 8.Physicians and other clinicians: CMS flexibilities to fight COVID-19. Centers for Medicare and Medicaid Services. 2020. Mar 30, [2020-05-20]. https://www.endocrine.org/-/media/endocrine/files/membership/cms--covid-phys-fact-sheet.pdf .
- 9.Verma S. Early impact of CMS expansion of Medicare telehealth during COVID-19. Health Affairs. 2020. Jul 15, [2020-08-12]. https://www.healthaffairs.org/do/10.1377/forefront.20200715.454789/full/
- 10.COVID-19: a physician guide to keeping your practice open. American Medical Association. 2020. Dec, [2021-02-16]. https://www.ama-assn.org/delivering-care/public-health/covid-19-physician-guide-keeping-your-practice-open .
- 11.DeLone H, McLean E. The DeLone and McLean model of information systems success: a ten-year update. J Manage Inf Syst. 2014 Dec 23;19(4):9–30. doi: 10.1080/07421222.2003.11045748. [DOI] [Google Scholar]
- 12.What is HIE? HealthIT.gov. 2020. Jul 24, [2020-08-19]. https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/what-hie .
- 13.Deyo D, Khaliq A, Mitchell D, Hughes DR. Electronic sharing of diagnostic information and patient outcomes. Am J Manag Care. 2018 Jan;24(1):32–37. https://www.ajmc.com/pubMed.php?pii=87415 .87415 [PubMed] [Google Scholar]
- 14.Appari A, Eric Johnson M, Anthony DL. Meaningful use of electronic health record systems and process quality of care: evidence from a panel data analysis of U.S. acute-care hospitals. Health Serv Res. 2013 Apr;48(2 Pt 1):354–75. doi: 10.1111/j.1475-6773.2012.01448.x. http://europepmc.org/abstract/MED/22816527 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lammers EJ, McLaughlin CG. Meaningful use of electronic health records and Medicare expenditures: evidence from a panel data analysis of U.S. health care markets, 2010-2013. Health Serv Res. 2017 Aug;52(4):1364–1386. doi: 10.1111/1475-6773.12550. http://europepmc.org/abstract/MED/27546309 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ozair FF, Jamshed N, Sharma A, Aggarwal P. Ethical issues in electronic health records: a general overview. Perspect Clin Res. 2015;6(2):73–6. doi: 10.4103/2229-3485.153997. http://www.picronline.org/article.asp?issn=2229-3485;year=2015;volume=6;issue=2;spage=73;epage=76;aulast=Ozair .PCR-6-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greenhalgh T, Potts HWW, Wong G, Bark P, Swinglehurst D. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Q. 2009 Dec;87(4):729–88. doi: 10.1111/j.1468-0009.2009.00578.x. http://europepmc.org/abstract/MED/20021585 .MILQ578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Computerized Prescriber Order Entry Medication Safety (CPOEMS): uncovering and learning from issues and errors. US Food and Drug Administration. 2015. Dec 15, [2020-09-05]. https://www.fda.gov/media/95234/download .
- 19.Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J Am Coll Surg. 2020 Aug;231(2):216–222.e2. doi: 10.1016/j.jamcollsurg.2020.04.030. http://europepmc.org/abstract/MED/32360960 .S1072-7515(20)30375-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams P, Woodward A. Cybersecurity vulnerabilities in medical devices: a complex environment and multifaceted problem. Med Devices (Auckl) 2015;8:305–16. doi: 10.2147/MDER.S50048.mder-8-305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel R, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: a review. Behav Sci (Basel) 2018 Oct 25;8(11):98. doi: 10.3390/bs8110098. https://www.mdpi.com/resolver?pii=bs8110098 .bs8110098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HHS finalizes historic rules to provide patients more control of their health data. Centers for Medicare and Medicaid Services. 2020. Mar 09, [2020-07-12]. https://www.cms.gov/newsroom/press-releases/hhs-finalizes-historic-rules-provide-patients-more-control-their-health-data .
- 23.Lipinski M, Knee M. 21st Century Cures Act: interoperability, information blocking, and the ONC Health IT Certification Program proposed rule. HealthIT.gov. 2019. Mar 22, [2020-06-15]. https://www.healthit.gov/sites/default/files/facas/2019-03-22_ONC_Cures_Act_NPRM_IB_%20HITAC_IB_Task_Force_508.pdf .
- 24.Luxton DD, Kayl RA, Mishkind MC. mHealth data security: the need for HIPAA-compliant standardization. Telemed J E Health. 2012 May;18(4):284–8. doi: 10.1089/tmj.2011.0180. [DOI] [PubMed] [Google Scholar]
- 25.Chervitz S, Deutsch EW, Field D, Parkinson H, Quackenbush J, Rocca-Serra P, Sansone SA, Stoeckert CJ, Taylor CF, Taylor R, Ball CA. Data standards for Omics data: the basis of data sharing and reuse. Methods Mol Biol. 2011;719:31–69. doi: 10.1007/978-1-61779-027-0_2. http://europepmc.org/abstract/MED/21370078 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Interoperability in Healthcare. Healthcare Information and Management Systems Society. [2020-05-17]. https://www.himss.org/resources/interoperability-healthcare .
- 27.Coronavirus (COVID-19) update: FDA allows expanded use of devices to monitor patients’ vital signs remotely. US Food and Drug Administration. 2020. Mar 20, [2020-08-12]. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-allows-expanded-use-devices-monitor-patients-vital-signs-remotely .
- 28.What is shortage designation? Health Resources and Services Administration: Bureau of Health Workforce. 2021. Feb, [2021-04-12]. https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation .
- 29.Shortage areas. data.HRSA.gov. [2021-02-18]. https://data.hrsa.gov/topics/health-workforce/shortage-areas .
- 30.The psychiatric shortage: causes and solutions. The National Council for Mental Wellbeing. 2018. Mar 01, [2020-05-17]. https://www.thenationalcouncil.org/wp-content/uploads/2017/03/Psychiatric-Shortage_National-Council-.pdf?daf=375ateTbd56 .
- 31.About rural health care. National Rural Health Association. [2021-06-01]. https://www.ruralhealth.us/about-nrha/about-rural-health-care .
- 32.Medicaid and rural health. Medicaid and CHIP Payment and Access Commission. 2021. Apr, [2021-05-01]. https://www.macpac.gov/wp-content/uploads/2021/04/Medicaid-and-Rural-Health.pdf .
- 33.Mueller JT, McConnell K, Burow PB, Pofahl K, Merdjanoff AA, Farrell J. Impacts of the COVID-19 pandemic on rural America. Proc Natl Acad Sci U S A. 2021 Jan 05;118(1):2019378118. doi: 10.1073/pnas.2019378118. http://www.pnas.org/cgi/pmidlookup?view=long&pmid=33328335 .2019378118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.CDC Using telehealth to expand access to essential health services during the COVID-19 pandemic. Centers for Disease Control and Prevention. 2020. Jun 10, [2020-09-16]. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html .
- 35.Totten AM, Womack DM, Eden KB, McDonagh MS, Griffin JC, Grusing S, Hersh WR. Telehealth: Mapping the Evidence for Patient Outcomes From Systematic Reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2016. Jun, https://www.ncbi.nlm.nih.gov/books/NBK379320/ [PubMed] [Google Scholar]
- 36.Telehealth for the treatment of serious mental illness and substance use disorders. Substance Abuse and Mental Health Services Administration. [2021-06-15]. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP21-06-02-001.pdf .
- 37.Patel SY, Huskamp HA, Busch AB, Mehrotra A. Telemental health and US rural-urban differences in specialty mental health use, 2010-2017. Am J Public Health. 2020 Sep;110(9):1308–1314. doi: 10.2105/AJPH.2020.305657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Myers CR. Using telehealth to remediate rural mental health and healthcare disparities. Issues Ment Health Nurs. 2019 Mar;40(3):233–239. doi: 10.1080/01612840.2018.1499157. [DOI] [PubMed] [Google Scholar]
- 39.Dixon LB, Holoshitz Y, Nossel I. Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry. 2016 Mar;15(1):13–20. doi: 10.1002/wps.20306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Uscher-Pines L, Cantor J, Huskamp HA, Mehrotra A, Busch A, Barnett M. Adoption of telemedicine services by substance abuse treatment facilities in the U.S. J Subst Abuse Treat. 2020 Oct;117:108060. doi: 10.1016/j.jsat.2020.108060. http://europepmc.org/abstract/MED/32811631 .S0740-5472(20)30316-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elliott VL. Telehealth and telemedicine: description and issues. United States Senate. 2016. Mar 29, [2020-09-21]. https://www.senate.gov/CRSpubs/757e3b90-ff10-497c-8e8c-ac1bdbdb3aaf.pdf .
- 42.Spotlight on telehealth. US Department of Veterans Affairs: Health Services Research and Development. 2020. Jul, [2020-08-12]. https://www.hsrd.research.va.gov/news/feature/telehealth-0720.cfm .
- 43.Myers US, Birks A, Grubaugh AL, Axon RN. Flattening the curve by getting ahead of it: how the VA healthcare system is leveraging telehealth to provide continued access to care for rural veterans. J Rural Health. 2021 Jan;37(1):194–196. doi: 10.1111/jrh.12449. http://europepmc.org/abstract/MED/32282955 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Department of Veterans Affairs (VA): a primer on telehealth. Federation of American Scientists: Project on Government Secrecy. 2019. Jul 26, [2020-08-15]. https://sgp.fas.org/crs/misc/R45834.pdf .
- 45.VA Video Connect visits increase 1000% during COVID-19 pandemic. US Department of Veterans Affairs. [2021-04-18]. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5467 .
- 46.Adler-Milstein J, Everson J, Lee SD. Sequencing of EHR adoption among US hospitals and the impact of meaningful use. J Am Med Inform Assoc. 2014;21(6):984–91. doi: 10.1136/amiajnl-2014-002708. http://europepmc.org/abstract/MED/24853066 .amiajnl-2014-002708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014 May;39(5):356–64. http://europepmc.org/abstract/MED/24883008 . [PMC free article] [PubMed] [Google Scholar]
- 48.Dinesen B, Nonnecke B, Lindeman D, Toft E, Kidholm K, Jethwani K, Young HM, Spindler H, Oestergaard CU, Southard JA, Gutierrez M, Anderson N, Albert NM, Han JJ, Nesbitt T. Personalized telehealth in the future: a global research agenda. J Med Internet Res. 2016 Mar 01;18(3):e53. doi: 10.2196/jmir.5257. https://www.jmir.org/2016/3/e53/ v18i3e53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tomasic I, Tomasic N, Trobec R, Krpan M, Kelava T. Continuous remote monitoring of COPD patients-justification and explanation of the requirements and a survey of the available technologies. Med Biol Eng Comput. 2018 Apr;56(4):547–569. doi: 10.1007/s11517-018-1798-z. http://europepmc.org/abstract/MED/29504070 .10.1007/s11517-018-1798-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sharing data, saving lives. American Hospital Association. 2019. Jan, [2020-08-16]. https://www.aha.org/system/files/2019-01/Infographic01_18__19_Sharing-Data-Saving-Lives_infographic_FINAL.pdf .
- 51.Diamond CC, Mostashari F, Shirky C. Collecting and sharing data for population health: a new paradigm. Health Aff (Millwood) 2009;28(2):454–66. doi: 10.1377/hlthaff.28.2.454.28/2/454 [DOI] [PubMed] [Google Scholar]
- 52.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, Curtis S, Roman M, Poon EG, Ferranti J, Katz JN, Tcheng J. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020 Jun 01;27(6):957–962. doi: 10.1093/jamia/ocaa067. http://europepmc.org/abstract/MED/32311034 .5822868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McClellan M, Gottlieb S, Mostashari F, Rivers C, Silvis L. A national COVID-19 surveillance system: achieving containment. Margolis Center for Health Policy. 2020. Apr 07, [2020-07-21]. https://healthpolicy.duke.edu/sites/default/files/2020-06/a_national_covid_surveillance_system.pdf .
- 54.Budd J, Miller BS, Manning EM, Lampos V, Zhuang M, Edelstein M, Rees G, Emery VC, Stevens MM, Keegan N, Short MJ, Pillay D, Manley E, Cox IJ, Heymann D, Johnson AM, McKendry RA. Digital technologies in the public-health response to COVID-19. Nat Med. 2020 Aug;26(8):1183–1192. doi: 10.1038/s41591-020-1011-4.10.1038/s41591-020-1011-4 [DOI] [PubMed] [Google Scholar]
- 55.Maragakis L. Coronavirus second wave, third wave and beyond: what causes a COVID surge. Johns Hopkins Medicine. [2021-04-12]. https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/first-and-second-waves-of-coronavirus .
- 56.Medicare coverage and payment of virtual services. Centers for Medicare and Medicaid Services. 2020. May 08, [2020-07-12]. https://www.cms.gov/outreach-and-educationmedicare-learning-network-mlnmlnproductsmln-multimedia/medicare-coverage-and-payment-virtual-services .
- 57.Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020 Jun 16;323(23):2375–2376. doi: 10.1001/jama.2020.7943.2766369 [DOI] [PubMed] [Google Scholar]
- 58.COVID-19 frequently asked questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. Centers for Medicare and Medicaid Services. [2021-11-18]. https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf .
- 59.Perzynski A, Roach MJ, Shick S, Callahan B, Gunzler D, Cebul R, Kaelber DC, Huml A, Thornton JD, Einstadter D. Patient portals and broadband internet inequality. J Am Med Inform Assoc. 2017 Sep 01;24(5):927–932. doi: 10.1093/jamia/ocx020. http://europepmc.org/abstract/MED/28371853 .3079333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Strategy on reducing burden relating to the use of health IT and EHRs. HealthIT.gov. 2020. Mar 11, [2020-08-15]. https://www.healthit.gov/topic/usability-and-provider-burden/strategy-reducing-burden-relating-use-health-it-and-ehrs .
- 61.COVID-19 emergency declaration blanket waivers for health care providers. Centers for Medicare and Medicaid Services. 2021. May 24, [2021-06-12]. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf .
- 62.Hospitals and health systems face unprecedented financial pressures due to COVID-19. American Hospital Association. 2020. May, [2020-06-01]. https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf .
- 63.Bojdani E, Rajagopalan A, Chen A, Gearin P, Olcott W, Shankar V, Cloutier A, Solomon H, Naqvi NZ, Batty N, Festin FED, Tahera D, Chang G, DeLisi LE. COVID-19 pandemic: impact on psychiatric care in the United States. Psychiatry Res. 2020 May 06;289:113069. doi: 10.1016/j.psychres.2020.113069.S0165-1781(20)31226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020 Jun 02;323(21):2127–2128. doi: 10.1001/jama.2020.6269.2765698 [DOI] [PubMed] [Google Scholar]
- 65.Druss BG, Cohen AN, Brister T, Cotes RO, Hendry P, Rolin D, Torous J, Ventura J, Gorrindo T. Supporting the mental health workforce during and after COVID-19. Psychiatr Serv. 2021 Oct 01;72(10):1222–1224. doi: 10.1176/appi.ps.202000509. [DOI] [PubMed] [Google Scholar]
- 66.Adler-Milstein J, Holmgren AJ, Kralovec P, Worzala C, Searcy T, Patel V. Electronic health record adoption in US hospitals: the emergence of a digital "advanced use" divide. J Am Med Inform Assoc. 2017 Nov 01;24(6):1142–1148. doi: 10.1093/jamia/ocx080. http://europepmc.org/abstract/MED/29016973 .4091350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cohen MF. Impact of the HITECH financial incentives on EHR adoption in small, physician-owned practices. Int J Med Inform. 2016 Oct;94:143–54. doi: 10.1016/j.ijmedinf.2016.06.017.S1386-5056(16)30146-0 [DOI] [PubMed] [Google Scholar]
- 68.Garrett P, Brown CA, Hart-Hester S, Hamadain E, Dixon C, Pierce W, Rudman WJ. Identifying barriers to the adoption of new technology in rural hospitals: a case report. Perspect Health Inf Manag. 2006 Oct 25;3:9. http://europepmc.org/abstract/MED/18066367 . [PMC free article] [PubMed] [Google Scholar]
- 69.Reisman M. EHRs: the challenge of making electronic data usable and interoperable. P T. 2017 Sep;42(9):572–575. http://europepmc.org/abstract/MED/28890644 . [PMC free article] [PubMed] [Google Scholar]
- 70.Adler-Milstein J, DesRoches CM, Kralovec P, Foster G, Worzala C, Charles D, Searcy T, Jha AK. Electronic health record adoption in US hospitals: progress continues, but challenges persist. Health Aff (Millwood) 2015 Dec;34(12):2174–80. doi: 10.1377/hlthaff.2015.0992.hlthaff.2015.0992 [DOI] [PubMed] [Google Scholar]
- 71.Pylypchuk Y, Alvarado CS, Patel V, Searcy T. Uncovering differences in interoperability across hospital size. Healthc (Amst) 2019 Dec;7(4):S2213-0764(18)30185-4. doi: 10.1016/j.hjdsi.2019.04.001.S2213-0764(18)30185-4 [DOI] [PubMed] [Google Scholar]
- 72.Mack D, Zhang S, Douglas M, Sow C, Strothers H, Rust G. Disparities in primary care EHR adoption rates. J Health Care Poor Underserved. 2016 Mar;27(1):327–338. doi: 10.1353/hpu.2016.0016. http://europepmc.org/abstract/MED/27587942 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Heisey-Grove DM, Carretta HJ. Disparities in secure messaging uptake between patients and physicians: longitudinal analysis of two national cross-sectional surveys. J Med Internet Res. 2020 May 01;22(5):e12611. doi: 10.2196/12611. https://www.jmir.org/2020/5/e12611/ v22i5e12611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ganguli I, Orav EJ, Lupo C, Metlay JP, Sequist TD. Patient and visit characteristics associated with use of direct scheduling in primary care practices. JAMA Netw Open. 2020 Aug 03;3(8):e209637. doi: 10.1001/jamanetworkopen.2020.9637. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.9637 .2769839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Policies and technology for interoperability and burden reduction. Centers for Medicare and Medicaid Services. [2021-11-15]. https://www.cms.gov/Regulations-and-Guidance/Guidance/Interoperability/index .
- 76.McCue M. Financial performance of health plans in Medicaid managed care. Medicare Medicaid Res Rev. 2012;2(2):mmrr.002.02.a07. doi: 10.5600/mmrr.002.02.a07. http://europepmc.org/abstract/MED/24800142 .mmrr2012-002-02-a07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.CMS Interoperability and patient access fact sheet. Centers for Medicare and Medicaid Services. 2020. Mar 09, [2020-06-12]. https://www.cms.gov/newsroom/fact-sheets/interoperability-and-patient-access-fact-sheet .
- 78.Exchange of electronic health records across the EU. European Commission: Shaping Europe’s Digital Future. [2021-11-12]. https://digital-strategy.ec.europa.eu/en/policies/electronic-health-records .
- 79.What is GDPR, the EU’s new data protection law? General Data Protection Regulation. [2021-11-12]. https://gdpr.eu/what-is-gdpr/
- 80.Teo P, Yeoh BS, Ong SN. SARS in Singapore: surveillance strategies in a globalising city. Health Policy. 2005 Jun;72(3):279–91. doi: 10.1016/j.healthpol.2004.11.004. http://europepmc.org/abstract/MED/15862636 .S0168-8510(04)00242-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Consultation on Regulatory Guidelines for Classification of Standalone Medical Mobile Applications (SaMD) and Qualification of Clinical Decision Support Software. Singapore Health Sciences Authority. [2021-11-12]. https://tinyurl.com/4rztun6j .
- 82.Digital health regulation in Asia-Pacific: overview and best practices. APACMed. 2021. Jan, [2021-02-15]. https://apacmed.org/content/uploads/2021/01/APACMed-Digital-Health-Regulation-in-APAC.pdf .
- 83.International health care system profiles. The Commonwealth Fund. 2020. [2021-01-09]. https://www.commonwealthfund.org/international-health-policy-center/system-profiles .
- 84.Ashwood JS, Mehrotra A, Cowling D, Uscher-Pines L. Direct-to-consumer telehealth may increase access to care but does not decrease spending. Health Aff (Millwood) 2017 Mar 01;36(3):485–491. doi: 10.1377/hlthaff.2016.1130.36/3/485 [DOI] [PubMed] [Google Scholar]
- 85.McLendon S. Interactive video telehealth models to improve access to diabetes specialty care and education in the rural setting: a systematic review. Diabetes Spectr. 2017 May;30(2):124–136. doi: 10.2337/ds16-0004. http://europepmc.org/abstract/MED/28588379 .124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Telepsychiatry and COVID-19: update on telehealth restrictions in response to COVID-19. American Psychiatric Association. 2020. May 01, [2020-06-12]. https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/blog/apa-resources-on-telepsychiatry-and-covid-19 .
- 87.List of telehealth services. Centers for Medicare and Medicaid Services. [2021-05-16]. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes .
- 88.Fahey RA, Hino A. COVID-19, digital privacy, and the social limits on data-focused public health responses. Int J Inf Manage. 2020 Dec;55:102181. doi: 10.1016/j.ijinfomgt.2020.102181. http://europepmc.org/abstract/MED/32836638 .102181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lammers EJ, McLaughlin CG, Barna M. Physician EHR adoption and potentially preventable hospital admissions among Medicare beneficiaries: panel data evidence, 2010-2013. Health Serv Res. 2016 Dec;51(6):2056–2075. doi: 10.1111/1475-6773.12586. http://europepmc.org/abstract/MED/27766628 . [DOI] [PMC free article] [PubMed] [Google Scholar]


