Abstract
This position paper provides a comprehensive guide for optimal follow-up of patients with acute pulmonary embolism (PE), covering multiple relevant aspects of patient counselling. It serves as a practical guide to treating patients with acute PE complementary to the formal 2019 European Society of Cardiology guidelines developed with the European Respiratory Society. We propose a holistic approach considering the whole spectrum of serious adverse events that patients with acute PE may encounter on the short and long run. We underline the relevance of assessment of modifiable risk factors for bleeding, of acquired thrombophilia and limited cancer screening (unprovoked PE) as well as a dedicated surveillance for the potential development of chronic thromboembolic pulmonary hypertension as part of routine practice; routine testing for genetic thrombophilia should be avoided. We advocate the use of outcome measures for functional outcome and quality of life to quantify the impact of the PE diagnosis and identify patients with the post-PE syndrome early. Counselling patients on maintaining a healthy lifestyle mitigates the risk of the post-PE syndrome and improves cardiovascular prognosis. Therefore, we consider it important to discuss when and how to resume sporting activities soon after diagnosing PE. Additional patient-relevant topics that require Focused counselling are travel and birth control.
Keywords: Pulmonary embolism, Anticoagulation therapy, Bleeding, Contraceptive agents, Neoplasms, Cardiovascular diseases, Thrombophilia, Travel, Sports, Pulmonary hypertension
Graphical Abstract
Introduction
The 2019 European Society of Cardiology guidelines on the diagnosis and treatment of acute pulmonary embolism (PE), developed with the European Respiratory Society, provide recommendations on the optimal management of acute PE, including diagnostic algorithms, risk stratification, initial and extended treatment, and follow-up strategy.1 Some important aspects of the treatment and overall care of patients after acute PE were mentioned, but their detailed discussion was beyond the scope of the guideline document. These issues relate to: management of bleeding risk, screening for cancer, screening for thrombophilia, treatment of PE in women, dealing with sports and travel, detection and management of the post-PE syndrome (PPES), and screening for and management of risk factors for arterial cardiovascular disease. This position paper highlights these key aspects of patient counselling, summarizes best available evidence and provides guidance for clinical practice. It serves as a practical guide to treating patients with acute PE that is intended to be complementary to the formal guideline.1 The rationale for the conclusions presented is provided in the Supplementary material online, Appendix. This review will not deal with PE and COVID-19, for which the reader is referred to the dedicated European Society of Cardiology (ESC) consensus document.2
Management of bleeding risk
From the start of anticoagulant treatment, patients with acute PE are at increased bleeding risk.3 Therefore, management of bleeding risk is relevant throughout the course of treatment, beginning with ruling out absolute contraindications to anticoagulant treatment at diagnosis, identifying the optimal anticoagulant strategy, and avoiding unnecessary interventions. Alternative treatment strategies in PE patients who have an absolute contraindication to anticoagulation include (repeated) platelet transfusions to deal with ‘critical’ thrombocytopenia aiming to keep the platelet count above 30–50 × 109/L, or the use of a retrievable vena cava filter in selected cases.1 Appropriate action should be taken to ensure drug adherence and optimal dosing, while avoiding relevant drug-drug interactions. Risk factors for bleeding need to be screened for and—when modifiable—reversed before patients are discharged. The most relevant potentially modifiable risk factors are: renal insufficiency, liver disease, thrombocytopenia, anaemia, hypertension, and use of antiplatelet or nonsteroidal anti-inflammatory drugs. After the first 3–6 months, estimation of the risk of bleeding over the long term becomes relevant for patients at high risk of recurrent venous thromboembolism (VTE), for whom indefinite treatment is considered.1 This bleeding risk can be estimated by either implicit judgement, weighing individual risk factors, or by risk prediction schemes. The currently available evidence supports the application of the American College of Chest Physicians bleeding risk tool or VTE-BLEED to identify patients at lowest risk of bleeding complications, in whom long-term anticoagulant treatment is likely safe.3–5 There is however no evidence supporting the avoidance of long-term anticoagulation in patients with a high estimated bleeding risk based on either of these risk stratification tools.3 Instead, such knowledge should be discussed with the patient and incorporated into a shared decision-making process regarding continuation or discontinuation of anticoagulation. Moreover, we propose a reduced dose of apixaban or rivaroxaban for patients at higher risk of bleeding, in whom it is decided to continue treatment. Of note, according to the ESC PE guideline, a reduced dose of apixaban or rivaroxaban for extended anticoagulation after the first 6 months should generally be considered.
During long-term anticoagulation, drug tolerance, drug-drug interactions, blood pressure, renal function and adherence to treatment need to be assessed on a regular basis (e.g. once a year in patients at low risk, and every 3 or 6 months in patients at high risk for bleeding) to optimize both the efficacy and safety of the treatment.1 Moreover, emerging modifiable risk factors for bleeding should be reversed and the appropriateness of continued anticoagulation evaluated following expert judgement and considering the patient’s preference. A drastic transition between bleeding risk classes may provide justification for (temporarily) discontinuing treatment.
Cancer screening
The overall incidence of a new cancer diagnosis is up to six-fold higher in patients with VTE than in sex- and age-matched controls.6 The absolute risk is highest during the first months after VTE diagnosis, in patients with unprovoked VTE, and in patients aged older than 50 years. The 1-year incidence of cancer is ∼1% in patients with provoked VTE compared to 5% in patients with unprovoked VTE, an incidence that gradually decreases to the risk of the general population over a 2-year period.7 , 8 Given these facts, we propose limited cancer screening in patients with unprovoked VTE to detect cancer at an early stage. Screening should include a thorough medical history, physical examination, basic laboratory testing (including a complete blood count, calcium, and liver function tests), and lung imaging (unless computed tomography [CT] pulmonary angiography was performed to diagnose PE). Age- and gender-specific testing (e.g. mammography, cervical smear, and prostate specific antigen testing) should be implemented in accordance with national guidelines and local practice. During follow-up after acute PE, the threshold to suspect cancer should be low in patients with a relatively recent history of cured cancer (e.g. within 5 years, as VTE can be a sign of recurrent cancer), early VTE progression/recurrence despite anticoagulant treatment, and anticoagulant-related bleeding shortly after start of treatment (particularly gastrointestinal bleeding or haematuria).9 If cancer is detected in the course of PE treatment, the choice and dosage of the anticoagulant as well as the duration of treatment should be adjusted accordingly.1 , 10
Although (extensive) screening for cancer leads to an earlier cancer diagnosis, evidence that screening reduces cancer-related morbidity or mortality is lacking.11 Extensive imaging-based screening with chest CT imaging, abdominal CT imaging, and/or 18-fluorodeoxyglucose positron emission tomography/CT imaging may further increase the number of cancers detected at VTE diagnosis but should be avoided, since the survival benefit of such an approach has never been demonstrated, and at the same time it carries the considerable costs and risks of invasive tests, false-positive findings, and overdiagnosis.
Inherited and acquired thrombophilia
Inherited thrombophilia can be detected in up to 30% of VTE patients. However, screening for inherited thrombophilia should only be performed if the results of testing are expected to modify (i) patient management in terms of type, dosage, or duration of anticoagulant therapy or (ii) counselling on oral contraception or prophylactic measures during pregnancy for female first degree relatives.1 In particular, the presence of inherited thrombophilia should not drive the choice of anticoagulant drug class or its intensity.12 Notably, in younger patients without identifiable strong risk factors for VTE recurrence and without a strong family history of VTE, in whom the physician and patient are considering anticoagulant treatment discontinuation, the absence of inherited thrombophilia might support the latter decision. Seven of 16 panel members would use the results of genetic thrombophilia testing to support clinical decisions for young patients (e.g. age <50 years) with unprovoked PE if validated risk assessment models suggest a low risk of recurrence. In their opinion, the presence of inherited thrombophilia may, under those circumstances, support a decision in favour of indefinite anticoagulation. The remaining nine panel members considered available evidence insufficient to support this practice.
The prevalence of confirmed antiphospholipid antibody syndrome (APS) can be as high as 9% in patients with a first unprovoked VTE.13 Non-vitamin K antagonist oral anticoagulants (NOACs) are currently not recommended in patients with acute PE and APS, particularly in the presence of a double or triple positive APS.14 , 15 Therefore, we propose limiting APS screening to patients with unprovoked PE presenting with signs or concomitant conditions that may raise the suspicion of APS. Twelve of the 16 panel members proposed to test patients with unprovoked PE for APS (only) in case of prior episodes of arterial or small-vessel thrombosis, prior thrombosis at unusual sites, pregnancy complications such as recurrent miscarriage or pre-eclampsia/eclampsia, autoimmune diseases, younger age (<50 years), or patients with an unexplained pre-treatment prolonged activated partial thromboplastin time. The panel suggests to avoid testing for APS during the first 4-6 weeks after the PE diagnosis because of potential unwanted interfering with the test, which may lead to both false-positive as well as false-negative results.16 For the interpretation of the type and titre of antiphospholipid antibodies, we refer to the statement made by the International Society on Thrombosis and Haemostasis (ISTH) as the present position paper does not aim at exploring laboratory issues in detail. All panel members agree that the ISTH document sets the standards for this specific point.16 , 17 We further propose that the option of switching to a vitamin K antagonist (VKA) should be discussed with patients with confirmed APS who are already on a NOAC and who have remained free of recurrent thromboembolic events. Preliminary long-term follow-up data from a phase III trial suggest that switching from NOAC to VKA may be beneficial also within 2 years of VTE diagnosis.18
Treatment of pulmonary embolism in women
Hormonal contraceptives may be continued during anticoagulant treatment to prevent pregnancy and mitigate the risk of abnormal uterine bleeding (AUB).19 Current evidence suggests that the risk of recurrent VTE in women receiving combined hormonal contraceptives or progestin-only contraceptives during anticoagulation for acute PE is not increased.19–21 For women with anticoagulant-associated AUB in the setting of PE treatment, management options include omission of NOAC for a single day (for example if bleeding is extremely heavy at a particular day of the cycle), modification of the dose or type of anticoagulant therapy, e.g. switching from an oral factor Xa inhibitor to an oral thrombin inhibitor, commencement of hormonal therapy, addition of tranexamic acid or application of local interventional strategies (including intrauterine devices), with multidisciplinary discussion where appropriate.22
Importantly, hormone treatment increases the risk of a recurrent VTE event after discontinuation of anticoagulant treatment. Available evidence suggests that the risk of recurrent VTE after discontinuation of hormonal contraception (the latter which is associated with a higher VTE risk, mostly relevant to combined hormonal contraceptives) and anticoagulant therapy is lower after hormonal contraception-associated VTE than after unprovoked VTE. Therefore, we propose a limited duration of anticoagulation, rather than indefinite anticoagulation, in these patients after hormonal contraception is discontinued, particularly if the bleeding risk is high and/or if no risk factors for recurrent VTE are present.23 , 24
Lastly, we suggest that pregnant women with prior VTE associated with hormonal contraceptive use who are not receiving long-term anticoagulant therapy should receive prophylactic or intermediate intensity anticoagulation in the antepartum and postpartum period, pending the results of a large multinational randomized trial (NCT01828697).
Sports, lifestyle and travel
Air travel and sporting activities are important topics that require discussion when counselling patients with acute PE. For both, caution should be taken in the initial period following PE diagnosis. Right ventricular (RV) dysfunction may persist for days to weeks, putting patients at risk of cardiac failure if the right ventricle is subjected to stress. During air travel, susceptible patients may be at risk of developing hypoxia-induced pulmonary hypertension and ultimately right heart failure.25 The pulmonary circulation will have relatively limited capacity to adapt and accommodate the increased blood flow induced by exercise, if it is already compromised by the presence of acute PE and associated RV overload. Hence, we suggest that before resuming strenuous exercise and air travel soon after a PE diagnosis, it should be ensured that the right ventricle has recovered. In low-risk PE patients, this may only take a few days, while in patients with intermediate to high-risk PE, several weeks may need to elapse. In this latter specific circumstances, the panel members perform echocardiography and look for favourable evolution of RV parameters if abnormal at baseline.1
Patients should be advised to resume their regular sporting activities in a stepwise manner after hospital discharge. Generally, to avoid deconditioning, we consider it reasonable to encourage and support PE patients in maintaining a healthy lifestyle including adequate physical activity in accordance with European Guidelines on cardiovascular disease prevention.26 This includes adequate physical activity, e.g. at least 150–300 min of moderate-intensity per week, or 75–150 min vigorous-intensity aerobic physical activity per week, or an equivalent combination of moderate- and vigorous-intensity aerobic activity.26–28
Sexuality is one aspect of quality of life that is important for many patients and partners, and may be adversely affected by cardiovascular disease. Although studies on this topic are unavailable for patients with acute PE, routine assessment of sexual problems and sexual counselling may be of benefit as part of effective management of PE patients.29
It should be noted that some sporting or other leisure activities are associated with direct bodily contact or prone to trauma, and as such of major bleeding. Such activities should generally be avoided for the duration of anticoagulant therapy, as has also been advised for patients with atrial fibrillation.30 Personalized anticoagulation schedules during the long-term anticoagulation phase may be discussed on an individual basis with high-level athletes. These may include consideration of occasional anticoagulation dose delays or omission prior to high-risk activities.
Long-haul air travel is associated with an increased risk of PE after discontinuation of anticoagulation.31 We propose the use of either compression stockings or prophylactic intensity anticoagulation in all patients with prior PE who have discontinued anticoagulant therapy and plan long-haul air flights (>4 h).32 , 33 Twelve of the 16 panel members would prescribe a NOAC when it is decided to treat with pharmacological thromboprophylaxis, while four preferred low molecular weight heparin. Fifteen of 16 panel members would start pharmacological thromboprophylaxis on the day of the flight rather than the day before, and 10 would extend the duration of pharmacological thromboprophylaxis to 2–4 days following the flight in light of the increased risk of VTE that may persist for several days.
Post-pulmonary embolism syndrome
The PPES is defined as new or progressive dyspnoea, exercise intolerance, and/or impaired functional or mental status after at least 3 months of adequate anticoagulation following acute PE, which cannot be explained by other (pre-existing) comorbidities.34 , 35 It is reported in up to 40–60% of PE survivors. Incomplete thrombus resolution occurs in 25–50% of patients after acute PE despite adequate anticoagulation, but bears no clinical significance in most cases.36 Notably, follow-up studies have shown that ∼40% of PE survivors have persistent perfusion defects, although only a very small proportion of these patients are ultimately diagnosed with chronic thromboembolic pulmonary hypertension (CTEPH), the most severe clinical presentation of PPES.34 , 36 , 37 The prevalence of CTEPH in PE survivors is 2–3%, and 5–8% in PE survivors with persistent dyspnoea, but it is unclear whether CTEPH develops from acute PE, or presents as acute PE.34 , 36 , 38–40 Therefore, current guidelines do not recommend routine follow-up of asymptomatic PE patients by imaging methods, but suggest to evaluate the index imaging test used to diagnose acute PE for signs of CTEPH.36
Chronic thromboembolic pulmonary disease (CTEPD) is defined as chronic pulmonary vascular obstruction with normal mean pulmonary artery pressure at rest, but with limited exercise tolerance which is attributed, at least in part, to an increased slope of the pulmonary arterial pressure–flow relationship (>3 mmHg/L/min) during exercise or dead space ventilation.41 , 42 Dead space fraction is decreased with exercise, while ventilatory efficiency, measured by the ventilatory equivalent for carbon dioxide slope, is decreased.36 , 43–45 It is obvious today that the majority of patients diagnosed with CTEPH are derived from cohorts with acute PE. This is why diagnostic evaluation of CTEPD/CTEPH is one of the crucial topics in post-PE care. Especially in suspected CTEPH, diagnostic delay should be prevented as it associated with poor clinical outcomes.36 Application of a dedicated screening programme for CTEPH allows for the diagnosis of most CTEPH patients within 4 months after the PE diagnosis.46 Patients with (suspected) CTEPH should be referred to an expert centre for multidisciplinary assessment and treatment. Echocardiography is the preferred first-line diagnostic test in patients with suspected CTEPH.1 Because echocardiographic findings may be inconclusive or even normal, especially early in the course of CTEPH, all patients with CTEPD, after confirmation of persistence of chronic pulmonary vascular obstruction preferably by ventilation perfusion scanning, should be referred to expert centres to allow for proper exclusion of CTEPH and advanced treatment, e.g. pulmonary endarterectomy or balloon pulmonary angioplasty.
In patients with PPES, cardiopulmonary exercise testing (CPET) can be a very useful diagnostic test, provided it is performed by physicians experienced in its interpretation. It allows for identification of changes in the cardiovascular, pulmonary, and skeletal muscle systems causing the symptoms.47 In particular, CPET may point to deconditioning. The latter is the most prevalent explanation of persisting functional limitations, followed by mental health problems such as depression or post-VTE panic syndrome. Depending on the results of CPET, other relevant (cardiopulmonary) comorbidities can be diagnosed and treated.
The presence of functional limitations and chronic dyspnoea should ideally be assessed in a standardized way using validated (patient-reported) outcome measures, such as the Post-VTE Functional Status (PVFS) scale.1 , 48 Based on current evidence, every patient with PPES should be analysed carefully, in particular if exercise limitation is a predominant feature of PPES. Individual treatment decisions should be made based on symptoms and findings of CPET, and could include cardiopulmonary rehabilitation especially if no other treatable comorbidities have been identified. Psychological support could also be of value. It is likely that targeted treatment of depression or panic disorders is equally effective for PE patients as it is in other settings.
Cardiovascular risk factors
Population-level and cohort studies have suggested a two- to three-fold increased incidence of arterial cardiovascular disease in patients with PE or deep vein thrombosis (DVT) compared to age- and sex- matched control patients without VTE.49–53 Underlying mechanisms remain poorly understood. On one hand, several studies have suggested that conventional risk factors for atherosclerosis may be associated with VTE as well.54 , 55 This hypothesis is underlined by studies that observed a higher prevalence of atherosclerosis in VTE patients than in matched controls without VTE.49 On the other hand, myocardial infarction and stroke may coexist with PE, e.g. in the setting of paradoxical embolism via an open foramen ovale.56 Since observations of a clear association between VTE and arterial cardiovascular disease could not be confirmed in all studies, it remains unknown whether VTE and arterial cardiovascular disease share a common pathophysiological mechanism or if the increased incidence should be regarded as an epiphenomenon.54–58 Of note, the incidence of arterial cardiovascular disease has been consistently reported to be higher in the first year after the VTE event, in obese subjects, in patients with PE (vs. DVT) and in patients with unprovoked VTE.54–58
Since no biomarkers and surrogate measures to refine cardiovascular risk assessment in patients with PE have been established, we propose to perform systematic cardiovascular risk assessment in all PE patients, using validated scores and risk calculators, and according to current guidelines.26 Patients with PE and a high cardiovascular risk score, especially in case of unprovoked PE and/or obesity, may require urgent attention to controlling risk factors. We propose that a holistic assessment of risk factors is performed at the routine 3-month follow-up visit, while individual risk factors such as smoking and hypertension should be targeted at the earliest convenience.
In PE patients with established cardiovascular disease, cardiovascular drugs may be discontinued or modified during the acute phase of treatment. This is particularly relevant for beta-blockers and antihypertensive drugs, the administration of which should be carefully re-evaluated in acute PE presenting with hypotension and/or severe RV dysfunction. Careful assessment of the expected benefits vs. risks of such drugs should guide management decisions in the individual patient. Similar anticoagulant strategies based on assessment of the risk of bleeding and ischaemic complications as in patients with atrial fibrillation can be followed.59 Triple therapy for longer than 1 week should be considered when risk of stent thrombosis outweighs the bleeding risk, with the total duration (<1 month) decided according to assessment of these risks.59 Triple therapy may be considered for up to 6 months in selected patients with high ischaemic risk.60 The treatment plan should be clearly specified at hospital discharge, and this strategy should be re-evaluated at regular intervals during follow-up. i.e. with a short period of overlapping antiplatelet therapy after myocardial infarction or percutaneous coronary intervention with stenting, to mitigate the risk of bleeding.61 For PE patients with established ischaemic cardiovascular disease, the full dose of anticoagulation should be continued for as long as indicated; a dose reduction in accordance with the label of rivaroxaban and apixaban after a treatment period of 6 months is not applicable in these patients.
Conclusions
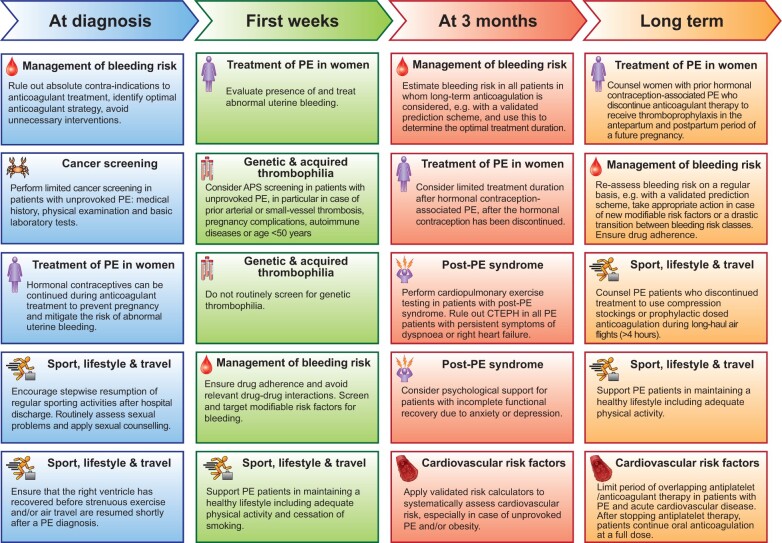
PE is a potentially life-altering, lifelong diagnosis. The treatment of patients with confirmed acute PE reaches far beyond the early phase of initial anticoagulant therapy. PE patients may experience serious adverse events during the course of disease and in particular in the first year after diagnosis, including major bleeding, recurrent VTE, arterial cardiovascular disease and CTEPH. Targeted management of risk factors and optimal choice of anticoagulant drugs early in the course of disease are likely to improve the patient’s prognosis. Advice on resuming sporting activities, sexual activities, travel and birth control needs to be discussed with the patient soon after diagnosing PE and built into a holistic care pathway that includes a dedicated recovery programme. Limited screening of selected patients for cancer and acquired thrombophilia, risk factors for arterial cardiovascular disease and early detection of CTEPH should be part of routine practice. Emphasis on maintaining a healthy lifestyle mitigates the risk of PPES and improves long-term cardiovascular prognosis. By adopting measures of functional outcomes and quality of life in routine practice, PPES can be identified early and targeted with appropriate treatment strategies such as cardiopulmonary rehabilitation. This position paper is a call to action, supporting a holistic approach to managing the lifelong spectrum of PE and providing a comprehensive guide for optimal follow-up of patients with acute PE (Graphical Abstract).
Graphical Abstract.
Overview of main conclusions of the position paper. APS, antiphospholipid antibody syndrome; aPTT, activated partial thromboplastin time; CTEPH, chronic thromboembolic pulmonary hypertension; PE, pulmonary embolism.
Supplementary material
Supplementary material is available at European Heart Journal online.
Conflict of interest: none declared.
Supplementary Material
Contributor Information
Frederikus A. Klok, Department of Medicine—Thrombosis and Hemostasis, Leiden University Medical Center, Leiden, Netherlands Center for Thrombosis and Hemostasis, University Medical Center Mainz, Mainz, Germany.
Walter Ageno, Department of Medicine and Surgery, University of Insubria, Varese, Italy.
Cihan Ay, Clinical Division of Haematology and Haemostaseology, Department of Medicine I, Medical University of Vienna, Vienna, Austria; I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
Magnus Bäck, Center for Molecular Medicine and Department of Cardiology, Karolinska University Hospital, Solna, Sweden, Stockholm; INSERM U1116, Université de Lorraine, Centre Hospitalier Régional Universitaire de Nancy, Vandoeuvre les Nancy, France.
Stefano Barco, Center for Thrombosis and Hemostasis, University Medical Center Mainz, Mainz, Germany; Clinic of Angiology, University Hospital Zurich, Zurich, Switzerland.
Laurent Bertoletti, Service de Médecine Vasculaire et Thérapeutique, CHU de St-Etienne, Saint-Etienne 42055, France; INSERM, UMR1059, Université Jean-Monnet, Saint-Etienne 42055, France; INSERM, CIC-1408, CHU de Saint-Etienne, Saint-Etienne 42055, France; INNOVTE, CHU de Saint-Etienne, Saint-Etienne 42055, France.
Cecilia Becattini, Internal and Cardiovascular Medicine-Stroke Unit, University of Perugia, Perugia, Italy.
Jørn Carlsen, Department of Cardiology, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark; Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark.
Marion Delcroix, Clinical Dept. of Respiratory Diseases, Pulmonary Hypertension Center, UZ Leuven, Leuven, Belgium; BREATHE, Dept CHROMETA, KU Leuven, Leuven, Belgium.
Nick van Es, Department of Vascular Medicine, Amsterdam Cardiovascular Sciences, Amsterdam University Medical Center, Amsterdam, Netherlands.
Menno V. Huisman, Department of Medicine—Thrombosis and Hemostasis, Leiden University Medical Center, Leiden, Netherlands
Luis Jara-Palomares, Medical Surgical Unit of Respiratory Diseases, Instituto de Biomedicina de Sevilla (IBiS). Hospital Universitario Virgen del Rocio, Seville, Spain; Centro de Investigación Biomédica en Red de Enfermedades Respiratorias (CIBERES), Instituto de Salud Carlos III, Madrid, Spain.
Stavros Konstantinides, Center for Thrombosis and Hemostasis, University Medical Center Mainz, Mainz, Germany; Department of Cardiology, Democritus University of Thrace, Greece.
Irene Lang, Department of Internal Medicine II, Cardiology and Center of Cardiovascular Medicine, Medical University of Vienna, Währinger Gürtel 18-20, Vienna 1090, Austria.
Guy Meyer, Respiratory Medicine Department, Hôpital Européen Georges Pompidou, Aphp, Paris, France; Université Paris Descartes, Paris 75006, France.
Fionnuala Ní Áinle, Dept. of Hematology, Mater University Hospital and Rotunda Hospital, Dublin, Ireland; School of Medicine, University College Dublin, Dublin, Ireland.
Stephan Rosenkranz, Dept. of Cardiology, Heart Center at the University of Cologne, Germany; Cologne Cardiovascular Research Center (CCRC), University of Cologne, Köln 50937, Germany.
Piotr Pruszczyk, Dept. of Internal Medicine and Cardiology Medical University of Warsaw, Lindley St 4, Warsaw 00-005, Poland.
References
- 1. Konstantinides SV, Meyer G, Becattini C et al. ; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 2020;41:543–603. [DOI] [PubMed] [Google Scholar]
- 2. Task Force for the management of COVID-19 of the European Society of Cardiology. ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 2-care pathways, treatment, and follow-up. Eur Heart J 2021;ehab697. doi: 10.1093/eurheartj/ehab697. [DOI] [PMC free article] [PubMed]
- 3. Klok FA, Huisman MV. How I assess and manage the risk of bleeding in patients treated for venous thromboembolism. Blood 2020;135:724–734. [DOI] [PubMed] [Google Scholar]
- 4. Kearon C, Akl EA, Ornelas J et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016;149:315–352. [DOI] [PubMed] [Google Scholar]
- 5. Klok FA, Hosel V, Clemens A et al. Prediction of bleeding events in patients with venous thromboembolism on stable anticoagulation treatment. Eur Respir J 2016;48:1369–1376. [DOI] [PubMed] [Google Scholar]
- 6. van Es N, Le Gal G, Otten HM et al. Screening for occult cancer in patients with unprovoked venous thromboembolism: a systematic review and meta-analysis of individual patient data. Ann Intern Med 2017;167:410–417. [DOI] [PubMed] [Google Scholar]
- 7. Marks MA, Engels EA. Venous thromboembolism and cancer risk among elderly adults in the United States. Cancer Epidemiol Biomarkers Prev 2014;23:774–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sorensen HT, Mellemkjaer L, Steffensen FH, Olsen JH, Nielsen GL. The risk of a diagnosis of cancer after primary deep venous thrombosis or pulmonary embolism. N Engl J Med 1998;338:1169–1173. [DOI] [PubMed] [Google Scholar]
- 9. Eikelboom JW, Connolly SJ, Bosch J et al. Bleeding and new cancer diagnosis in patients with atherosclerosis. Circulation 2019;140:1451–1459. [DOI] [PubMed] [Google Scholar]
- 10. Lyman GH, Carrier M, Ay C et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv 2021;5:927–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Robertson L, Yeoh SE, Broderick C, Stansby G, Agarwal R. Effect of testing for cancer on cancer- or venous thromboembolism (VTE)-related mortality and morbidity in people with unprovoked VTE. Cochrane Database Syst Rev 2018;11:Cd010837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elsebaie MAT, van Es N, Langston A, Buller HR, Gaddh M. Direct oral anticoagulants in patients with venous thromboembolism and thrombophilia: a systematic review and meta-analysis. J Thromb Haemost 2019;17:645–656. [DOI] [PubMed] [Google Scholar]
- 13. Miranda S, Park J, Le Gal G et al. Prevalence of confirmed antiphospholipid syndrome in 18-50 years unselected patients with first unprovoked venous thromboembolism. J Thromb Haemost 2020;18:926–930. [DOI] [PubMed] [Google Scholar]
- 14. Pengo V, Denas G, Zoppellaro G et al. Rivaroxaban vs warfarin in high-risk patients with antiphospholipid syndrome. Blood 2018;132:1365–1371. [DOI] [PubMed] [Google Scholar]
- 15. Ordi-Ros J, Saez-Comet L, Perez-Conesa M et al. Rivaroxaban versus vitamin K antagonist in antiphospholipid syndrome: a randomized noninferiority trial. Ann Intern Med 2019;171:685–694. [DOI] [PubMed] [Google Scholar]
- 16. Devreese KMJ, de Groot PG, de Laat B et al. Guidance from the Scientific and Standardization Committee for lupus anticoagulant/antiphospholipid antibodies of the International Society on Thrombosis and Haemostasis: update of the guidelines for lupus anticoagulant detection and interpretation. J Thromb Haemost 2020;18:2828–2839. [DOI] [PubMed] [Google Scholar]
- 17. Devreese KMJ, Ortel TL, Pengo V, de Laat B; Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibodies. Laboratory criteria for antiphospholipid syndrome: communication from the SSC of the ISTH. J Thromb Haemost 2018;16:809–813. [DOI] [PubMed] [Google Scholar]
- 18. Pengo V, Hoxha A, Andreoli L et al. Trial of Rivaroxaban in AntiPhospholipid Syndrome (TRAPS): two-year outcomes after the study closure. J Thromb Haemost 2021;19:531–535. [DOI] [PubMed] [Google Scholar]
- 19. Klok FA, Barco S. Optimal management of hormonal contraceptives after an episode of venous thromboembolism. Thromb Res 2019;181 Suppl 1:S1–S5. [DOI] [PubMed] [Google Scholar]
- 20. Huisman MV, Ferreira M, Feuring M, Fraessdorf M, Klok FA. Less abnormal uterine bleeding with dabigatran than warfarin in women treated for acute venous thromboembolism. J Thromb Haemost 2018;16:1775–1778. [DOI] [PubMed] [Google Scholar]
- 21. Scheres L, Brekelmans M, Ageno W et al. Abnormal vaginal bleeding in women of reproductive age treated with edoxaban or warfarin for venous thromboembolism: a post hoc analysis of the Hokusai-VTE study. BJOG 2018;125:1581–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Samuelson Bannow B. Management of heavy menstrual bleeding on anticoagulation. Hematol Am Soc Hematol Educ Program 2020;2020:533–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rodger MA, Le Gal G, Anderson DR et al. ; REVERSE II Study Investigators. Validating the HERDOO2 rule to guide treatment duration for women with unprovoked venous thrombosis: multinational prospective cohort management study. BMJ 2017;356:j1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kiconco S, Abdul Sultan A, Grainge MJ. Recurrence risk of venous thromboembolism and hormone use in women from England: a cohort study using clinical practice research datalink. Br J Haematol 2017;177:127–135. [DOI] [PubMed] [Google Scholar]
- 25. Smith TG, Talbot NP, Chang RW et al. Pulmonary artery pressure increases during commercial air travel in healthy passengers. Aviat Space Environ Med 2012;83:673–676. [DOI] [PubMed] [Google Scholar]
- 26. Piepoli MF, Hoes AW, Agewall S et al. ; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rolving N, Brocki BC, Bloch-Nielsen JR et al. Effect of a physiotherapist-guided home-based exercise intervention on physical capacity and patient-reported outcomes among patients with acute pulmonary embolism: a randomized clinical trial. JAMA Netw Open 2020;3:e200064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Piercy KL, Troiano RP. Physical activity guidelines for Americans from the US Department of Health and Human Services. Circ Cardiovasc Qual Outcomes 2018;11:e005263. [DOI] [PubMed] [Google Scholar]
- 29. Steinke EE, Jaarsma T, Barnason SA et al. ; Council on Cardiovascular and Stroke Nursing of the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP). Sexual counselling for individuals with cardiovascular disease and their partners: a consensus document from the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP). Eur Heart J 2013;34:3217–3235. [DOI] [PubMed] [Google Scholar]
- 30. Pelliccia A, Sharma S, Gati S et al. ; ESC Scientific Document Group. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J 2021;42:17–96. [DOI] [PubMed] [Google Scholar]
- 31. Saleh B, Paul C, Combes X et al. Pulmonary embolism after a long-haul flight. Intern Emerg Med 2021; [DOI] [PubMed] [Google Scholar]
- 32. Clarke MJ, Broderick C, Hopewell S, Juszczak E, Eisinga A. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst Rev 2016;9:CD004002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cesarone MR, Belcaro G, Nicolaides AN et al. Venous thrombosis from air travel: the LONFLIT3 study –prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: a randomized trial. Angiology 2002;53:1–6. [DOI] [PubMed] [Google Scholar]
- 34. Klok FA, van der Hulle T, den Exter PL, Lankeit M, Huisman MV, Konstantinides S. The post-PE syndrome: a new concept for chronic complications of pulmonary embolism. Blood Rev 2014;28:221–226. [DOI] [PubMed] [Google Scholar]
- 35. Boon G, Huisman MV, Klok FA. Determinants and management of the post-pulmonary embolism syndrome. Semin Respir Crit Care Med 2021;42:299–307. [DOI] [PubMed] [Google Scholar]
- 36. Delcroix M, Torbicki A, Gopalan D et al. ERS statement on chronic thromboembolic pulmonary hypertension. Eur Respir J 2021;57:2002828. [DOI] [PubMed] [Google Scholar]
- 37. Gerges C, Gerges M, Friewald R et al. Microvascular disease in chronic thromboembolic pulmonary hypertension: hemodynamic phenotyping and histomorphometric assessment. Circulation 2020;141:376–386. [DOI] [PubMed] [Google Scholar]
- 38. Ende-Verhaar YM, Meijboom LJ, Kroft LJM et al. Usefulness of standard computed tomography pulmonary angiography performed for acute pulmonary embolism for identification of chronic thromboembolic pulmonary hypertension: results of the InShape III study. J Heart Lung Transplant 2019;38:731–738. [DOI] [PubMed] [Google Scholar]
- 39. Guerin L, Couturaud F, Parent F et al. Prevalence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Prevalence of CTEPH after pulmonary embolism. Thromb Haemost 2014;112:598–605. [DOI] [PubMed] [Google Scholar]
- 40. Ende-Verhaar YM, Cannegieter SC, Vonk Noordegraaf A et al. Incidence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: a contemporary view of the published literature. Eur Respir J 2017;49:1601792. [DOI] [PubMed] [Google Scholar]
- 41. Kim NH, Delcroix M, Jais X et al. Chronic thromboembolic pulmonary hypertension. Eur Respir J 2019;53:1801915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Le Gal G, Carrier M, Castellucci LA et al. ; ISTH CDE Task Force. Development and implementation of common data elements for venous thromboembolism research: on behalf of SSC Subcommittee on official Communication from the SSC of the ISTH. J Thromb Haemost 2021;19:297–303. [DOI] [PubMed] [Google Scholar]
- 43. Claeys M, Claessen G, La Gerche A et al. Impaired cardiac reserve and abnormal vascular load limit exercise capacity in chronic thromboembolic disease. JACC Cardiovasc Imaging 2019;12:1444–1456. [DOI] [PubMed] [Google Scholar]
- 44. Held M, Kolb P, Grun M et al. Functional characterization of patients with chronic thromboembolic disease. Respiration 2016;91:503–509. [DOI] [PubMed] [Google Scholar]
- 45. Boon G, Bogaard HJ, Klok FA. Essential aspects of the follow-up after acute pulmonary embolism: an illustrated review. Res Pract Thromb Haemost 2020;4:958–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Boon G, Ende-Verhaar YM, Bavalia R et al. ; InShape II Study Group. Non-invasive early exclusion of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: the InShape II study. Thorax 2021;76:1002–1009. [DOI] [PubMed] [Google Scholar]
- 47. Radtke T, Crook S, Kaltsakas G et al. ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur Respir Rev 2019;28:180101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Boon G, Barco S, Bertoletti L et al. Measuring functional limitations after venous thromboembolism: optimization of the Post-VTE Functional Status (PVFS) scale. Thromb Res 2020;190:45–51. [DOI] [PubMed] [Google Scholar]
- 49. Prandoni P, Bilora F, Marchiori A et al. An association between atherosclerosis and venous thrombosis. N Engl J Med 2003;348:1435–1441. [DOI] [PubMed] [Google Scholar]
- 50. Prandoni P, Ghirarduzzi A, Prins MH et al. Venous thromboembolism and the risk of subsequent symptomatic atherosclerosis. J Thromb Haemost 2006;4:1891–1896. [DOI] [PubMed] [Google Scholar]
- 51. Sørensen HT, Horvath-Puho E, Pedersen L, Baron JA, Prandoni P. Venous thromboembolism and subsequent hospitalisation due to acute arterial cardiovascular events: a 20-year cohort study. Lancet 2007;370:1773–1779. [DOI] [PubMed] [Google Scholar]
- 52. Klok FA, Zondag W, van Kralingen KW et al. Patient outcomes after acute pulmonary embolism. A pooled survival analysis of different adverse events. Am J Respir Crit Care Med 2010;181:501–506. [DOI] [PubMed] [Google Scholar]
- 53. Klok FA, Mos IC, Broek L et al. Risk of arterial cardiovascular events in patients after pulmonary embolism. Blood 2009;114:1484–1488. [DOI] [PubMed] [Google Scholar]
- 54. Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation 2008;117:93–102. [DOI] [PubMed] [Google Scholar]
- 55. Ageno W, Di Minno MN, Ay C et al. Association between the metabolic syndrome, its individual components, and unprovoked venous thromboembolism: results of a patient-level meta-analysis. Arterioscler Thromb Vasc Biol 2014;34:2478–2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Le Moigne E, Timsit S, Ben Salem D et al. Patent foramen ovale and ischemic stroke in patients with pulmonary embolism: a prospective cohort study. Ann Intern Med 2019;170:756–763. [DOI] [PubMed] [Google Scholar]
- 57. Noumegni SR, Hoffmann C, Tromeur C et al. Frequency and incidence of arterial events in patients with venous thromboembolism compared to the general population: a systematic review and meta-analysis of cohort studies. Thromb Res 2021;203:172–185. [DOI] [PubMed] [Google Scholar]
- 58. Delluc A, Lacut K, Rodger MA. Arterial and venous thrombosis: what's the link? A narrative review. Thromb Res 2020;191:97–102. [DOI] [PubMed] [Google Scholar]
- 59. Steffel J, Collins R, Antz M et al. 2021 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace 2021;23:1612–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Collet JP, Thiele H, Barbato E et al. ; ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289–1367. [DOI] [PubMed] [Google Scholar]
- 61. Hindricks G, Potpara T, Dagres N et al. ; ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC). Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 2021;42:373–498. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.