Abstract
BACKGROUND:
Medically compromised nursing home residents continue to be prescribed statins, despite questionable benefits.
OBJECTIVE:
To describe regional variation in statin use among residents with life-limiting illness.
RESEARCH DESIGN:
Cross-sectional study using 2016 Minimum Data Set 3.0 assessments linked to Medicare administrative data and health service utilization area resource files.
SETTING:
Nursing homes (n=14,147) within hospital referral regions (n=306) across the U.S.
SUBJECTS:
Long-stay residents (≥65 years old) with life-limiting illness (e.g., serious illness, palliative care, or prognosis < 6 months to live) (n= 361,170).
MEASURES:
Prevalent statin use was determined by Medicare Part D claims. Stratified by age (65–75, ≥76 years), multilevel logistic models provided odds ratios with 95% confidence intervals.
RESULTS:
Statin use was prevalent (age 65–75: 46.0%, ≥76: 31.6%). For both age groups, nearly all resident-level variables evaluated were associated with any and high-intensity statin use and three facility level variables (i.e., higher proportions of Black residents, skilled nursing care provided, average number of medications per resident) were associated with increased odds of statin use. While in residents 65–75 years, no associations were observed, residents aged ≥76 years located in HRRs with the highest healthcare utilization had higher odds of statin use than those in nursing homes in HRRs with the lowest health care utilization.
CONCLUSIONS:
Our findings suggest extensive geographic variation in U.S. statin prescribing across HRRs, especially for those aged ≥76 years. This variation may reflect clinical uncertainty given the largely absent guidelines for statin use in nursing home residents.
Keywords: statins, pharmacoepidemiology, geographic variation, long-term care, nursing homes
INTRODUCTION
Statins are one of the most commonly prescribed medications in the United States (US).1 Prescriptions for statin pharmacotherapy have continued to increase.2 This has, in turn, disproportionately impacted older adults.3 From 2012 to 2013, almost half of all U.S. adults over age 75 years were prescribed a statin, nearly double the rate a decade earlier.2 While the clinical benefit of statin pharmacotherapy for adults in the general population is well documented, the benefit for clinically complex, older adults is less clear.4–7 For example, the United States Preventative Services Task Force guidelines report insufficient evidence to make any statin recommendations for adults over age 75 years.8 Even so, statin use persists among clinically complex older adults including nursing home residents.9,10
In nursing homes, statin use is widespread even among those with life-limiting illness.10–13 One in three U.S. nursing home residents with life-limiting illness are on statins.12 However, statins appear unlikely to benefit these older, clinically compromised nursing home residents.4,14,15 Moreover, common musculoskeletal statin side effects often reported in the general adult population could be particularly harmful to compromised nursing home residents, exacerbating frailty and physical decline.16 This use of statins with questionable benefits and known harms may contribute to concerns regarding polypharmacy and overprescribing in nursing homes.12 To address the potential overprescribing of statins in this setting, we must understand what else beyond clinical indication is driving statin use. Among Medicare beneficiaries, contextual factors such as facility or regional practice characteristics appear to influence statin prescribing.17–19 Nonetheless, research on the contextual forces driving use of statins for those in nursing homes is lacking.
The purpose of this study was to evaluate the extent to which potential overuse of statins in U.S. nursing homes varies by contextual factors on the facility- and regional- level. Using a national sample of nursing home facilities, we focused on statin use in clinically complex older adult residents with a limited life expectancy or life-limiting illness as this subset of the population is less likely to benefit from statins. We hypothesized that in the absence of clear clinical statin guidelines for adults over age 75 years, regional factors would play a larger role in use for this older portion of the nursing home population.
METHODS
Study Design
This study used a cross-sectional design to evaluate statin use in the nursing homes via multilevel modeling with resident-, facility-, and regional- levels. The study was approved by the University of Massachusetts Medical School Institutional Review Board.
Data Sources
Nursing home assessment data from the Minimum Data Set (MDS) 3.0 were linked to Medicare administrative data including the Beneficiary Summary File (Medicare eligibility), Medicare Part A inpatient claims, and Medicare Part D prescription drug claims. These data were merged to Nursing Home Compare 2016 annual files,20 the 2016 Provider of Service file,21 and the 2016 Dartmouth Atlas End-of-life Chronically Ill Care file (Methods Appendix).22 The Nursing Home Compare and Provider of Services files are largely based on information from the Certification and Survey Provider Enhanced Reports, comprised of survey reports from mandatory inspections of all U.S. Medicare- and Medicaid- certified nursing home facilities. The files include operational characteristics, regulatory compliance, and quality of care measurements for each facility. Nursing Home Compare uses these data to assign facilities quality star ratings. The Dartmouth Atlas End-of-life Chronical Ill Care data files provided data at the Hospital Referral Region (HRR) level. The Dartmouth Atlas files are built largely from figures provided by the Medicare files, specifically Medicare fee-for-service beneficiary eligibility and claims files, in addition to regional files from US Census reports and Tele Atlas zip code boundary files. Nursing home facilities were matched by their zip codes to HRRs.
Setting
In the United States, all nursing homes that receive federal funding from the Center for Medicare and Medicaid Services (CMS) must complete standardized nursing home assessments for all admitted residents. This pertains to 98% of all U.S. nursing home facilities. CMS-certified facilities were included if MDS data on residents eligible for the study were linkable to the facility and regional level.
Life-Limiting Illness Definition
Life-limiting illness was used to identify nursing home residents not likely to benefit from statins, specifically those clinically compromised near the end of life. Conceptually, life-limiting illness was defined as a progressive, incurable condition that results in a prognosis less than one year.23 While mortality risk scores have been developed for nursing home residents,24,25 an operational definition matching the conceptualization of life-limiting illness used in this study has yet to be validated. Given that most long-stay nursing home residents have a limited average remaining life expectancy,11,26 multiple definitions were used to avoid excluding appropriate residents. A diagnosis of a life-limiting illness or condition was confirmed if ≥ one criterion was met (Supplemental Table 1):
Physician documentation of life expectancy <6 months based on MDS 3.0 prognosis item J1400
Receipt of hospital palliative care consultation based on ICD-10 diagnosis code Z51.5
≥1 condition on the Veterans Health Administration Palliative Care Index13,27
≥1 “serious illness” as defined by Kelley et al. (2019)28
Study Population
Nursing home residents were included if they: 1) resided in a CMS- certified nursing home facility on September 30, 2016 (last date of the year prior to implementation of MDS 3.0 changes), 2) had a quarterly assessment, 3) were aged ≥65 years, 4) had continuous Medicare Fee-for-Service coverage in July, August, September 2016, and 4) had a life-limiting illness. Exclusion criteria included: 1) hospital-based facility residence due to substantial practice differences from free-standing nursing homes, and 2) receipt of skilled nursing or hospice services (no Medicare Part D claims). Supplemental Figure 1 shows the construction of study sample (n= 361,170).
Resident-level Variables
Resident-level variables included: age (65–75, ≥76 years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic/Latino, other), functional dependence (none to limited assistance required, extensive assistance required, complete assistance required/dependent), cognitive impairment (none/intact, mild, moderate, severe), and atherosclerotic cardiovascular disease (ASCVD) risk (no risk factors, ≥1 risk factors, ASCVD diagnosis).
Facility-level Variables
Facility-level variables included organizational and operational (process, staffing, and outcome) nursing home characteristics that could affect quality of care provided.29,30 Categorization of continuous variables was informed by previous literature.29,31 Organizational variables included structural characteristics such as facility ownership status, facility size by number of beds, % occupancy, etc. Operational variables included process variables (% residents with skilled nursing care, % residents on hospice, and average number of medications per resident), staffing variables (full-time medical director availability, physician extender availability, and average staff care time per resident-day), and outcome variables (quality indicators, number of facility deficiencies, and overall Nursing Home Compare star ratings quality score).
Regional-level Variables
Regional-level variables included: census-defined regions (Northeast, Midwest, South, West), U.S. states (+ DC), and HRR end-of-life healthcare utilization (quartiles).32 Per the Dartmouth Atlas,22 HRRs are regional health care markets for tertiary care, with each HRR having ≥ one hospital where neurosurgery and major CVD procedures can be performed. The HRR end-of-life variables included: hospital days per decedent, % deaths occurring in the hospital, % deaths with included time in the intensive care unit, intensive care unit days per decedent, skilled nursing facility days per decedent, % enrolled in hospice, total physician visits per decedent, % patients seeing ≥10 physicians, and ratio of medical specialty to primary care.
Statin Use
Statin use was defined as a binary (yes/no) variable for any use or high-intensity use as of September 30th 2016 (target date). High-intensity statin use was based on a daily dose LDL-C reduction >50%, outlined in the recent American College of Cardiology/American Heart Association (ACC/AHA) guidelines for each generic statin available (Supplemental Table 2).33 Statin use was defined by the presence of Medicare Part D prescription claim for any generic statin or combination in the 90 days preceding the target date, in which the fill date + number of days supply overlapped with the target date.
Statistical Analysis
Analyses were stratified by age categories based on commonly defined guideline age groups:34 65–75 years and ≥76 years. Descriptive analyses were initially run to estimate the distribution of resident, facility, and regional characteristics in the sample. This was in addition to crude estimates of any statin use and high intensity statin use. To visually evaluate the geographic variation of statins, figures of statin use prevalence were generated by U.S. census regions, states, and HRRs. This included U.S. maps of statin use by HRRs with statin use categorized into quartiles.
Before multilevel modeling, the potential for multicollinearity was evaluated in several ways. First, correlations between the determinants of interest were examined. Second, regression models with binary outcome variables (separate models for any and high intensity statin use) were used to generate variance inflation factors for all determinants of interest. No variables exceeded the threshold of 10 for the variance inflation factors. Lastly, the standard errors in the multilevel models were evaluated as additional variables were added to the models to see if any appeared inflated.
Separate multilevel logistic models with random intercepts that account for HRR and state variation were developed for each age group and the outcomes of interest (i.e., any statin use, high intensity statin use). This process included first estimating crude odds ratios (OR) and 95% confidence intervals (CI) followed by models which included all resident- and facility- level variables, with separate models for each HRR variable.
Lastly, to estimate the amount of between HRR variation explained by model covariates, models were run with the random intercept only in addition to those fit sequentially for resident-, facility-, and HRR- level variables. We then calculated the proportional change in cluster variation and intraclass correlation coefficients.35 For more detail, see Methods Appendix.
RESULTS
Sample Characteristics
Table 1 shows that the sample was mostly women, non-Hispanic white with functional and/or cognitive impairment. Most (90.8%) had diagnosis of cardiovascular disease (CVD) or at least one risk factor. In terms of facility characteristics, most were for-profit with ≥100 beds and ≥80% occupancy. The majority of facilities were concentrated in non-rural regions. For distributions of all quartiles in regional HRR variables, see Supplemental Table 4.
Table 1.
Characteristics of long-stay nursing home residents with life-limiting illness. N= 361,170 residents, 14,147 facilities, 306 hospital referral regions (HRRs)
| Characteristics (%*) | Overall (n=361,170) | 65–75 years-olds (n=77,819) | ≥76 years-olds (n=283,351) |
|---|---|---|---|
| Resident- level | |||
| Women | 71.5 | 54.5 | 76.1 |
| Race/ethnicity | |||
| Non-Hispanic white | 79.8 | 72.3 | 81.8 |
| Non-Hispanic black | 13.0 | 20.1 | 11.1 |
| Hispanic/Latino | 5.0 | 5.6 | 4.9 |
| Other | 2.3 | 2.1 | 2.3 |
| Functional dependence | |||
| None to limited assistance required | 21.2 | 26.3 | 19.8 |
| Extensive assistance required | 57.9 | 51.7 | 59.6 |
| Complete assistance required/dependent | 20.9 | 22.0 | 20.6 |
| Cognitive impairment | |||
| None/Intact | 25.1 | 41.2 | 20.7 |
| Mild | 24.3 | 25.2 | 24.0 |
| Moderate | 42.2 | 26.9 | 46.4 |
| Severe | 8.4 | 6.7 | 8.9 |
| Atherosclerotic Cardiovascular Disease (ASCVD) risk | |||
| ASCVD diagnosis | 29.9 | 35.9 | 28.2 |
| ≥1 risk factor for ASCVD without the dx | 60.9 | 55.6 | 62.3 |
| No risk factors for ASCVD | 9.3 | 8.5 | 9.5 |
| Facility- level | |||
| Ownership | |||
| For-profit | 71.0 | 79.5 | 68.7 |
| Government | 21.3 | 13.6 | 23.4 |
| Non-profit | 7.7 | 6.9 | 7.9 |
| Chain status | |||
| Part of chain | 56.1 | 59.9 | 55.0 |
| Facility specialty services | |||
| Alzheimer/dementia care unit | 21.0 | 18.3 | 21.7 |
| No special care unit | 76.7 | 78.6 | 76.2 |
| Facility size (no. beds) | |||
| <50 | 3.5 | 2.5 | 3.8 |
| 50–100 | 27.5 | 25.6 | 28.0 |
| 100–200 | 55.4 | 57.4 | 54.8 |
| >200 | 13.6 | 14.6 | 13.4 |
| Occupancy | |||
| <80% | 28.1 | 31.5 | 27.2 |
| % Black/African American residents | |||
| 0 to <15% | 73.2 | 62.5 | 76.2 |
| 15 to <50% | 21.0 | 28.3 | 19.0 |
| ≥50% | 5.8 | 9.2 | 4.8 |
| % of residents dependent in activities of daily living (ADLs) | |||
| >50% | 11.0 | 11.6 | 10.8 |
| % skilled nursing care | |||
| ≥50% | 36.0 | 30.0 | 37.7 |
| % hospice use | |||
| <5% | 15.3 | 13.8 | 15.7 |
| 5–10% | 15.8 | 14.8 | 16.1 |
| 10–20% | 30.1 | 29.7 | 30.2 |
| ≥20% | 38.9 | 41.8 | 38.0 |
| Facility average # of medications per resident | |||
| ≥6 medications | 71.5 | 73.5 | 70.9 |
| Staffing | |||
| No Full-time medical director | 95.3 | 95.0 | 95.4 |
| No physician extender | 27.1 | 25.8 | 27.5 |
| Registered nurse < 30 minutes per resident per day | 53.7 | 59.7 | 52.0 |
| Direct care < 3 hours per resident per day | 7.9 | 10.0 | 7.3 |
| Nursing homes quality measures | |||
| ≥5% bed sores | 53.3 | 59.1 | 51.7 |
| ≥5% residents restrained | 3.6 | 4.2 | 3.5 |
| Facility average # of deficiencies in 2016 survey | |||
| 0–1 | 17.8 | 15.8 | 18.3 |
| 2–5 | 31.9 | 29.5 | 32.5 |
| ≥6 | 50.4 | 54.7 | 49.2 |
| Overall Nursing Home Compare Star rating | |||
| 1 | 18.6 | 23.5 | 17.3 |
| 2 | 19.4 | 21.7 | 18.7 |
| 3 | 19.3 | 19.6 | 19.2 |
| 4 | 23.2 | 20.4 | 24.0 |
| 5 | 19.6 | 14.8 | 20.9 |
| Regional- level | |||
| Rural location | 26.7 | 24.9 | 27.2 |
| US census region | |||
| Northeast | 23.2 | 20.1 | 24.0 |
| Midwest | 27.5 | 25.0 | 28.2 |
| South | 39.2 | 43.4 | 38.0 |
| West | 10.2 | 11.5 | 9.8 |
| Highest HRR quartile of end-of-life healthcare | |||
| Hospital days per decedent | 33.5 | 33.6 | 33.5 |
| % deaths occurring in the hospital | 26.6 | 25.8 | 26.8 |
| % deaths with included time in intensive care unit | 27.0 | 28.3 | 26.7 |
| Intensive care days per decedent | 24.6 | 25.7 | 24.2 |
| SNF days per decedent | 35.5 | 34.7 | 35.7 |
| % enrolled in hospice | 22.3 | 23.6 | 21.9 |
| Total physician visits per decedent | 31.3 | 32.6 | 30.9 |
| % of patients seeing ≥10 different physicians | 37.2 | 37.1 | 37.2 |
| Ratio of medical specialty to primary care | 30.6 | 31.2 | 30.5 |
May not round to 100% because of rounding.
ADL indicates activities of daily living; ASCVD, atherosclerotic cardiovascular disease; HRR, hospital referral regions; SNF, skilled nursing facility.
Overall Statin Use
Overall, the rate of any statin use was 34.7% (65–75 years: 46.0%, ≥76 years: 31.6%) and high-intensity use was 6.6% (65–75 years: 11.4%, ≥76 years: 5.3%). Table 2 (any statin use) and Table 3 (high-intensity statin use) provide the percent use and odds ratios for selected resident-, (structural) facility-, and regional- level characteristics typically of interest, with the complete list given on Supplemental Table 5. A summary of these findings by level of analysis is provided below.
Table 2.
Association between select nursing home resident, facility, and hospital referral region (HRR) characteristics and any statin use by age.
| 65–75 years-old | ≥76 years-old | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | No.a | Row % on statins | ORb | aOR (95% CI)c | No.a | Row % on statins | ORb | aOR (95% CI)c |
| Overall | 77,819 | 46.0 | - | - | 283,351 | 31.6 | - | - |
| Resident- level | ||||||||
| Atherosclerotic Cardiovascular Disease (ASCVD) risk | ||||||||
| ASCVD diagnosis | 27,924 | 54.7 | * | *referent | 79,942 | 39.1 | * | *referent |
| ≥1 risk factor for ASCVD | 43,267 | 46.1 | 0.71 | 0.69 (0.67–0.71) | 176,488 | 32.2 | 0.75 | 0.74 (0.73–0.76) |
| No risk factors for ASCVD | 6,628 | 9.3 | 0.08 | 0.09 (0.08–0.10) | 26,921 | 5.7 | 0.10 | 0.10 (0.10–0.11) |
| Facility- level | ||||||||
| Ownership | ||||||||
| For-profit | 61,866 | 46.1 | * | *referent | 194,671 | 32.4 | * | *referent |
| Government | 10,544 | 46.8 | 1.O3 | 1.05 (1.00–1.10) | 66,431 | 29.5 | 0.91 | 0.96 (0.94–0.98) |
| Non-profit | 5,399 | 44.4 | 0.93 | 0.95 (0.89–1.02) | 22,249 | 30.4 | 0.95 | 0.95 (0.92–0.98) |
| Facility size (no. beds) | ||||||||
| <50 | 1,913 | 43.9 | 0.92 | 0.93 (0.83–1.04) | 10,770 | 27.6 | 0.90 | 0.96 (0.91–1.02) |
| 50–100 | 19,940 | 46.1 | 1.01 | 0.97 (0.92–1.03) | 79,363 | 31.1 | 1.00 | 1.02 (0.99–1.06) |
| 100–200 | 44,640 | 46.1 | 1.00 | 0.97 (0.92–1.02) | 155,387 | 31.9 | 1.01 | 1.01 (0.98–1.04) |
| >200 | 11,326 | 46.2 | * | *referent | 37,831 | 32.5 | * | *referent |
| Occupancy | ||||||||
| <80% | 24,481 | 46.1 | 1.01 | 1.01 (0.96–1.06) | 77,127 | 31.6 | 1.02 | 1.02 (0.99–1.05) |
| 80 to <90% | 23,515 | 46.2 | 1.02 | 0.99 (0.95–1.04) | 85,795 | 31.6 | 1.01 | 1.01 (0.98–1.03) |
| 90 to <95% | 16,655 | 46.0 | 1.02 | 1.01 (0.96–1.06) | 65,738 | 31.4 | 0.99 | 0.99 (0.97–1.02) |
| ≥95% | 13,168 | 45.7 | * | *referent | 54,691 | 31.7 | * | *referent |
| % Black/African American residents | ||||||||
| 0 to <15% | 48,644 | 45.5 | * | *referent | 215,795 | 30.6 | * | *referent |
| 15 to <50% | 22,030 | 46.5 | 1.03 | 1.05 (1.00–1.09) | 53,828 | 34.0 | 1.09 | 1.06 (1.03–1.09) |
| ≥50% | 7,145 | 48.3 | 1.10 | 1.13 (1.06–1.21) | 13,728 | 37.3 | 1.23 | 1.14 (1.09–1.20) |
| Overall Nursing Home Compare Star rating | ||||||||
| 1 | 18,305 | 45.5 | * | *referent | 48,958 | 31.7 | * | *referent |
| 2 | 16,886 | 46.7 | 1.06 | 1.03 (0.98–1.08) | 53,011 | 32.3 | 1.03 | 1.04 (1.01–1.07) |
| 3 | 15,213 | 47.1 | 1.08 | 1.05 (1.00–1.10) | 54,409 | 32.0 | 1.01 | 1.04 (1.01–1.07) |
| 4 | 15,882 | 45.2 | 1.00 | 0.98 (0.93–1.03) | 67,862 | 31.5 | 0.99 | 1.04 (1.01–1.07) |
| 5 | 11,533 | 45.7 | 1.03 | 1.01 (0.96–1.07) | 59,111 | 30.7 | 0.95 | 1.02 (0.99–1.06) |
| Regional- level | ||||||||
| Rural location | 19,399 | 46.3 | 1.02 | 1.01 (0.97–1.06) | 77,141 | 30.4 | 1.02 | 0.99 (0.96–1.01) |
| US census region | ||||||||
| Northeast | 15,666 | 46.4 | * | *referent | 68,013 | 31.5 | * | *referent |
| Midwest | 19,462 | 47.4 | 1.06 | 0.96 (0.87–1.07) | 79,861 | 30.8 | 0.98 | 0.83 (0.71–0.98) |
| South | 33,767 | 45.9 | 1.01 | 0.86 (0.78–0.94) | 107,731 | 32.2 | 1.09 | 0.85 (0.73–1.00) |
| West | 8,924 | 43.2 | 0.86 | 0.91 (0.81–1.02) | 27,746 | 31.7 | 0.82 | 0.80 (0.67–0.95) |
| Hospital days/decedent | ||||||||
| Q1 | 11,366 | 44.7 | * | *referent | 47,800 | 27.0 | * | *referent |
| Q2 | 17,569 | 46.9 | 1.07 | 1.03 (0.96–1.10) | 64,071 | 31.1 | 1.14 | 1.11 (1.03–1.19) |
| Q3 | 22,734 | 45.3 | 1.02 | 0.95 (0.88–1.02) | 76,604 | 32.3 | 1.21 | 1.15 (1.07–1.24) |
| Q4 | 26,150 | 46.8 | 1.10 | 1.03 (0.96–1.11) | 94,876 | 33.7 | 1.32 | 1.27 (1.18–1.38) |
| % deaths occurring in the hospital | ||||||||
| Q1 | 15,807 | 46.2 | * | *referent | 58,662 | 31.2 | * | *referent |
| Q2 | 21,318 | 46.8 | 1.07 | 1.05 (0.98–1.12) | 77,346 | 31.9 | 1.06 | 1.03 (0.96–1.11) |
| Q3 | 20,658 | 45.3 | 0.99 | 0.96 (0.89–1.02) | 71,356 | 30.9 | 1.01 | 0.99 (0.92–1.06) |
| Q4 | 20,036 | 45.9 | 1.02 | 1.02 (0.94–1.10) | 75,987 | 32.3 | 1.10 | 1.09 (1.00–1.18) |
| % deaths w/included time in intensive care unit | ||||||||
| Q1 | 12,250 | 45.7 | * | *referent | 50,129 | 28.7 | * | *referent |
| Q2 | 18,091 | 46.8 | 1.04 | 1.01 (0.94–1.08) | 66,904 | 31.5 | 1.09 | 1.07 (1.00–1.15) |
| Q3 | 25,493 | 46.1 | 1.00 | 0.97 (0.91–1.04) | 90,793 | 31.8 | 1.10 | 1.07 (1.00–1.15) |
| Q4 | 21,985 | 45.6 | 0.99 | 0.95 (0.88–1.03) | 75,525 | 33.4 | 1.21 | 1.15 (1.06–1.25) |
| Intensive care days/decedent | ||||||||
| Q1 | 12,729 | 45.1 | * | *referent | 54,038 | 27.6 | * | *referent |
| Q2 | 21,646 | 46.5 | 1.04 | 1.02 (0.96–1.09) | 82,276 | 30.7 | 1.08 | 1.06 (0.99–1.14) |
| Q3 | 23,432 | 46.1 | 1.03 | 0.99 (0.92–1.06) | 78,376 | 32.4 | 1.21 | 1.16 (1.08–1.25) |
| Q4 | 20,012 | 46.1 | 1.04 | 0.99 (0.92–1.07) | 68,661 | 34.9 | 1.29 | 1.22 (1.13–1.32) |
| Skilled nursing facility days/decedent | ||||||||
| Q1 | 10,046 | 45.2 | * | *referent | 37,678 | 27.3 | * | *referent |
| Q2 | 16,640 | 45.0 | 1.00 | 0.97 (0.90–1.04) | 58,059 | 30.5 | 1.12 | 1.06 (0.98–1.14) |
| Q3 | 24,107 | 46.6 | 1.05 | 1.00 (0.93–1.07) | 86,467 | 31.8 | 1.16 | 1.09 (1.01–1.18) |
| Q4 | 27,026 | 46.6 | 1.08 | 1.01 (0.93–1.09) | 101,147 | 33.7 | 1.33 | 1.22 (1.12–1.32) |
| % enrolled in hospice | ||||||||
| Q1 | 18,787 | 45.3 | * | *referent | 74,465 | 30.8 | * | *referent |
| Q2 | 21,209 | 45.8 | 1.01 | 1.00 (0.94–1.07) | 79,719 | 31.1 | 1.01 | 0.99 (0.92–1.06) |
| Q3 | 19,423 | 45.8 | 1.03 | 1.01 (0.94–1.09) | 67,191 | 31.6 | 1.05 | 1.03 (0.95–1.11) |
| Q4 | 18,400 | 47.3 | 1.10 | 1.06 (0.98–1.15) | 61,976 | 33.3 | 1.08 | 1.05 (0.97–1.14) |
| Total physician visits/decedent | ||||||||
| Q1 | 10,010 | 44.8 | * | *referent | 42,755 | 25.9 | * | *referent |
| Q2 | 19,031 | 46.2 | 1.05 | 0.99 (0.92–1.07) | 71,339 | 30.2 | 1.14 | 1.08 (1.00–1.16) |
| Q3 | 23,380 | 46.3 | 1.06 | 0.96 (0.89–1.04) | 81,802 | 32.2 | 1.29 | 1.18 (1.09–1.27) |
| Q4 | 25,398 | 46.2 | 1.08 | 0.98 (0.90–1.06) | 87,455 | 35.0 | 1.43 | 1.31 (1.21–1.42) |
| % of patients seeing ≥10 different physicians | ||||||||
| Q1 | 11,078 | 45.3 | * | *referent | 46,678 | 27.8 | * | *referent |
| Q2 | 16,222 | 45.5 | 1.01 | 0.96 (0.89–1.03) | 56,632 | 30.8 | 1.12 | 1.07 (1.00–1.15) |
| Q3 | 21,672 | 45.8 | 1.01 | 0.94 (0.88–1.01) | 74,699 | 31.1 | 1.16 | 1.09 (1.01–1.18) |
| Q4 | 28,847 | 46.9 | 1.07 | 1.00 (0.83–1.08) | 105,342 | 34.1 | 1.36 | 1.27 (1.18–1.38) |
| Ratio of medical specialty to primary care | ||||||||
| Q1 | 13,333 | 45.3 | * | *referent | 53,702 | 28.1 | * | *referent |
| Q2 | 18,795 | 45.3 | 0.97 | 0.98 (0.92–1.05) | 65,442 | 30.0 | 1.03 | 1.02 (0.96–1.09) |
| Q3 | 21,399 | 46.6 | 1.01 | 1.01 (0.94–1.08) | 77,864 | 31.7 | 1.11 | 1.09 (1.02–1.16) |
| Q4 | 24,292 | 46.5 | 1.02 | 1.02 (0.95–1.09) | 86,343 | 34.9 | 1.24 | 1.22 (1.14–1.31) |
No. = number of residents with each characteristic in the sample- serves as a denominator for the row %, indicating the % of residents on statin pharmacotherapy;
OR = crude odds ratio;
aOR (95% CI) = adjusted odds ratio (95% Confidence Interval), All odds ratios were estimated via cross-classified multilevel logistic models with random intercepts for state and HRR. Crude models that failed to converge without adjustments included the following for the ≥76 year-old age group: ASCVD risk (sex-adjusted), occupancy (sex-, race-, functional dependence- adjusted), hospital days/decedent (sex-, race- adjusted), skilled nursing facility/decedent (sex-, race-, functional dependence- adjusted), % enrolled in hospice (sex- adjusted), total physician visits/decedent (sex- adjusted). For resident-level and facility-level variables, adjusted odds ratios are derived from models that include adjustments for all resident-level and facility-level variables included in Supplemental Table 5 and the rural/urban indicator variable. For HRR-level variables, adjusted odds ratios are derived from separate models for each HRR-level variable that include all the resident- and facility- level variables adjusted for previously.
Table 3.
Association between select nursing home resident, facility, and hospital referral region (HRR) characteristics and high intensity statin use by age
| Characteristics | 65–75 years-old | ≥76 years-old | ||||||
|---|---|---|---|---|---|---|---|---|
| No.a | Row % on statins | ORb | aOR (95% CI)c | No.a | Row % on statins | ORb | aOR (95% CI)c | |
| Overall | 77,819 | 11.4 | - | - | 283,351 | 5.3 | - | - |
| Resident- level | ||||||||
| Atherosclerotic Cardiovascular Disease (ASCVD) risk | ||||||||
| ASCVD diagnosis | 27,924 | 15.1 | * | *referent | 79,942 | 7.7 | * | *referent |
| ≥1 risk factor for ASCVD | 43,267 | 10.4 | 0.64 | 0.64 (0.61–0.67) | 176,488 | 5.0 | 0.62 | 0.64 (0.62–0.66) |
| No risk factors for ASCVD | 6,628 | 1.9 | 0.11 | 0.12 (0.10–0.14) | 26,921 | 0.9 | 0.11 | 0.12 (0.11–0.14) |
| Facility- level | ||||||||
| Ownership | ||||||||
| For-profit | 61,866 | 11.4 | * | *referent | 194,671 | 5.4 | * | *referent |
| Government | 10,544 | 11.8 | 1.01 | 1.03 (0.96–1.10) | 66,431 | 5.1 | 0.96 | 1.02 (0.98–1.07) |
| Non-profit | 5,399 | 10.4 | 0.88 | 0.94 (0.84–1.04) | 22,249 | 5.2 | 0.98 | 1.01 (0.94–1.09) |
| Facility size (no. beds) | ||||||||
| <50 | 1,913 | 11.6 | 1.00 | 1.02 (0.86–1.21) | 10,770 | 4.4 | 0.81 | 0.91 (0.81–1.02) |
| 50–100 | 19,940 | 11.5 | 1.02 | 0.98 (0.89–1.07) | 79,363 | 5.3 | 0.97 | 1.01 (0.95–1.08) |
| 100–200 | 44,640 | 11.4 | 1.01 | 0.97 (0.90–1.04) | 155,387 | 5.4 | 0.98 | 0.99 (0.94–1.05) |
| >200 | 11,326 | 10.9 | * | *referent | 37,831 | 5.3 | * | *referent |
| Occupancy | ||||||||
| <80% | 24,481 | 11.3 | 1.00 | 0.99 (0.92–1.06) | 77,127 | 5.4 | 1.08 | 1.06 (1.00–1.12) |
| 80 to <90% | 23,515 | 11.5 | 1.02 | 0.99 (0.92–1.06) | 85,795 | 5.3 | 1.03 | 1.02 (0.97–1.07) |
| 90 to <95% | 16,655 | 11.3 | 1.00 | 0.98 (0.91–1.06) | 65,738 | 5.3 | 1.01 | 1.00 (0.95–1.06) |
| ≥95% | 13,168 | 11.2 | * | *referent | 54,691 | 5.2 | * | *referent |
| % Black/African American residents | ||||||||
| 0 to <15% | 48,644 | 11.2 | * | *referent | 215,795 | 5.1 | * | *referent |
| 15 to <50% | 22,030 | 11.4 | 1.05 | 1.06 (0.99–1.12) | 53,828 | 5.9 | 1.17 | 1.13 (1.07–1.19) |
| ≥50% | 7,145 | 12.3 | 1.12 | 1.12 (1.01–1.23) | 13,728 | 7.0 | 1.38 | 1.28 (1.17–1.39) |
| Overall Nursing Home Compare Star rating | ||||||||
| 1 | 18,305 | 10.8 | * | *referent | 48,958 | 5.5 | * | *referent |
| 2 | 16,886 | 11.7 | 1.10 | 1.07 (1.00–1.14) | 53,011 | 5.5 | 1.00 | 1.00 (0.95–1.06) |
| 3 | 15,213 | 11.7 | 1.10 | 1.08 (1.00–1.16) | 54,409 | 5.2 | 0.95 | 0.97 (0.92–1.03) |
| 4 | 15,882 | 11.1 | 1.04 | 1.02 (0.95–1.10) | 67,862 | 5.4 | 0.98 | 1.01 (0.95–1.07) |
| 5 | 11,533 | 11.5 | 1.09 | 1.07 (0.98–1.17) | 59,111 | 5.1 | 0.92 | 0.97 (0.91–1.04) |
| Regional- level | ||||||||
| Rural location | 19,399 | 11.3 | 0.97 | 0.99 (0.93–1.05) | 77,141 | 5.1 | 0.99 | 0.98 (0.94–1.03) |
| US census region | ||||||||
| Northeast | 15,666 | 11.4 | * | *referent | 68,013 | 5.5 | * | *referent |
| Midwest | 19,462 | 12.1 | 1.03 | 0.98 (0.83–1.15) | 79,861 | 5.2 | 0.82 | 0.73 (0.60–0.89) |
| South | 33,767 | 11.0 | 0.94 | 0.83 (0.72–0.97) | 107,731 | 5.3 | 0.91 | 0.75 (0.62–0.90) |
| West | 8,924 | 11.0 | 0.94 | 0.97 (0.81–1.17) | 27,746 | 5.1 | 0.77 | 0.78 (0.62–0.97) |
| Hospital days per decedent | ||||||||
| Q1 | 11,366 | 11.8 | * | *referent | 47,800 | 4.7 | * | *referent |
| Q2 | 17,569 | 11.8 | 1.00 | 0.96 (0.86–1.07) | 64,071 | 5.3 | 1.11 | 1.07 (0.96–1.20) |
| Q3 | 22,734 | 11.0 | 0.94 | 0.89 (0.80–0.99) | 76,604 | 5.4 | 1.13 | 1.06 (0.95–1.19) |
| Q4 | 26,150 | 11.2 | 1.01 | 0.93 (0.83–1.05) | 94,876 | 5.6 | 1.25 | 1.14 (1.01–1.29) |
| % deaths occurring in the hospital | ||||||||
| Q1 | 15,807 | 11.6 | * | *referent | 58,662 | 5.3 | * | *referent |
| Q2 | 21,318 | 11.3 | 1.01 | 0.99 (0.90–1.10) | 77,346 | 5.2 | 1.05 | 1.02 (0.92–1.14) |
| Q3 | 20,658 | 11.3 | 0.99 | 0.97 (0.87–1.07) | 71,356 | 5.4 | 1.11 | 1.07 (0.97–1.20) |
| Q4 | 20,036 | 11.2 | 1.00 | 0.98 (0.87–1.10) | 75,987 | 5.5 | 1.18 | 1.16 (1.03–1.31) |
| % deaths with included time in intensive care unit | ||||||||
| Q1 | 12,250 | 12.0 | * | *referent | 50,129 | 4.8 | * | *referent |
| Q2 | 18,091 | 11.7 | 1.00 | 0.97 (0.88–1.07) | 66,904 | 5.3 | 1.12 | 1.09 (0.98–1.21) |
| Q3 | 25,493 | 11.4 | 0.95 | 0.93 (0.84–1.02) | 90,793 | 5.5 | 1.16 | 1.12 (1.01–1.24) |
| Q4 | 21,985 | 10.7 | 0.92 | 0.87 (0.78–0.98) | 75,525 | 5.4 | 1.23 | 1.15 (1.02–1.29) |
| Intensive care days per decedent | ||||||||
| Q1 | 12,729 | 11.9 | * | *referent | 54,038 | 4.7 | * | *referent |
| Q2 | 21,646 | 11.4 | 0.94 | 0.91 (0.82–1.01) | 82,276 | 5.4 | 1.09 | 1.05 (0.95–1.17) |
| Q3 | 23,432 | 11.2 | 0.97 | 0.93 (0.84–1.03) | 78,376 | 5.4 | 1.16 | 1.09 (0.97–1.21) |
| Q4 | 20,012 | 11.0 | 0.92 | 0.87 (0.78–0.98) | 68,661 | 5.7 | 1.21 | 1.12 (1.00–1.26) |
| SNF days per decedent | ||||||||
| Q1 | 10,046 | 12.0 | * | *referent | 37,678 | 4.8 | * | *referent |
| Q2 | 16,640 | 11.4 | 0.96 | 0.94 (0.85–1.05) | 58,059 | 5.0 | 1.01 | 0.96 (0.86–1.07) |
| Q3 | 24,107 | 11.1 | 0.94 | 0.91 (0.81–1.01) | 86,467 | 5.4 | 1.06 | 1.01 (0.90–1.13) |
| Q4 | 27,026 | 11.3 | 0.97 | 0.93 (0.83–1.04) | 101,147 | 5.6 | 1.14 | 1.05 (0.93–1.18) |
| % enrolled in hospice | ||||||||
| Q1 | 18,787 | 11.0 | * | *referent | 74,465 | 5.2 | * | *referent |
| Q2 | 21,209 | 11.5 | 0.96 | 0.95 (0.86–1.05) | 79,719 | 5.3 | 0.95 | 0.92 (0.83–1.02) |
| Q3 | 19,423 | 11.2 | 1.00 | 0.98 (0.88–1.10) | 67,191 | 5.3 | 0.99 | 0.95 (0.85–1.06) |
| Q4 | 18,400 | 11.7 | 1.05 | 1.02 (0.90–1.15) | 61,976 | 5.6 | 0.99 | 0.95 (0.84–1.07) |
| Total physician visits per decedent | ||||||||
| Q1 | 10,010 | 12.3 | * | *referent | 42,755 | 4.6 | * | *referent |
| Q2 | 19,031 | 11.5 | 0.92 | 0.88 (0.79–0.98) | 71,339 | 5.2 | 1.06 | 1.00 (0.89–1.12) |
| Q3 | 23,380 | 11.5 | 0.92 | 0.86 (0.77–0.96) | 81,802 | 5.6 | 1.14 | 1.02 (0.91–1.15) |
| Q4 | 25,398 | 10.7 | 0.91 | 0.83 (0.74–0.94) | 87,455 | 5.5 | 1.17 | 1.04 (0.92–1.17) |
| % of patients seeing ≥10 different physicians | ||||||||
| Q1 | 11,078 | 11.7 | * | *referent | 46,678 | 4.6 | * | *referent |
| Q2 | 16,222 | 11.3 | 0.98 | 0.93 (0.84–1.04) | 56,632 | 5.2 | 1.09 | 1.04 (0.93–1.16) |
| Q3 | 21,672 | 11.3 | 0.97 | 0.91 (0.82–1.02) | 74,699 | 5.4 | 1.15 | 1.07 (0.95–1.20) |
| Q4 | 28,847 | 11.3 | 1.00 | 0.93 (0.82–1.04) | 105,342 | 5.6 | 1.20 | 1.08 (0.95–1.22) |
| Ratio of medical specialty to primary care | ||||||||
| Q1 | 13,333 | 11.2 | * | *referent | 53,702 | 4.8 | * | *referent |
| Q2 | 18,795 | 11.3 | 1.05 | 1.05 (0.95–1.16) | 65,442 | 5.1 | 1.04 | 1.01 (0.91–1.12) |
| Q3 | 21,399 | 11.7 | 1.05 | 1.04 (0.94–1.25) | 77,864 | 5.4 | 1.03 | 0.98 (0.89–1.09) |
| Q4 | 24,292 | 11.1 | 1.04 | 1.02 (0.91–1.13) | 86,343 | 5.8 | 1.18 | 1.11 (1.00–1.24) |
No. = number of residents with each characteristic in the sample- serves as a denominator for the row %, indicating the % of residents on statin pharmacotherapy;
OR = crude odds ratio;
aOR (95% CI) = adjusted odds ratio (95% Confidence Interval). All odds ratios were estimated via cross-classified multilevel logistic models with random intercepts for state and HRR. For resident-level and facility-level variables, adjusted odds ratios are derived from models that include adjustments for all resident-level and facility-level variables included in Supplemental Table 5 and the rural/urban indicator variable. For HRR-level variables, adjusted odds ratios are derived from separate models for each HRR-level variable that include all the resident- and facility- level variables adjusted for previously.
Resident-level Statin Use Associations
On the resident-level, almost all variables evaluated appeared to be associated with any and high-intensity statin use for both age groups. In residents ≥ 76 years, men and racial/ethnic minorities (versus non-Hispanic Whites) had higher odds of statin use. For both age groups, residents with functional dependence, severe cognitive impairment, and those without a CVD diagnosis or risk factors had reduced odds of statin use. (Supplemental Table 5). However, residents without a CVD diagnosis and no risk factors comprised <10% of the sample.
Facility- Level Statin Use Associations
Both age groups appeared to have some facility-level characteristics that were associated with any and high-intensity statin use. The extent to which facility variables were associated with any statin use differed by age group (65–75 years: 5 of 18 facility variables; ≥76 years: 13 of 18 facility variables) (Supplement Table 5). There were few associations with high-intensity statin use across age. For both age groups and statin types, three facility level variables (i.e., higher proportions of African American/Black residents, skilled nursing care provided, and average number of medications per resident) were consistently associated with increased odds of statin use (Supplemental Table 5).
Regional- Level Statin Use Associations
Census Regions. For the regional-level data, patterns of statin use appeared to have the most variation on the HRR-level (Figure 1) as opposed to larger scaled analyses with U.S. census regions (Figure 2) and states (Supplemental Figures 2 and 3). Residents living in facilities other than those in the Northeast had lower odds of high-intensity statin use (e.g., vs. South for any statins, 65–75 years: aOR 0.86, 95% CI 0.78–0.94; ≥76 years: aOR 0.85, 95% CI 0.73–1.00).
U.S. States. When breaking down census regions by U.S. state, statin use appeared to remain relatively consistent with the exception of some outlier states (Supplemental Figures 2 and 3). For those 65–75 years, Arkansas appeared to have the highest average statin prescribing rates for any and high-intensity use. For those ≥76 years, DC appeared to have the highest average statin prescribing for any statin use and Delaware for high-intensity use.
HRRs. When the U.S. is further divided into HRRs, rates appear most variable, crossing state lines. Referring to geographic maps of HRR-level statin use (Figure 1), statin use (any and high-intensity) appeared most concentrated in the eastern half of the United States in both age groups. However, use varied widely across HRRs, even those in neighboring states. For those aged 65–75 years, any statin use ranged from 25% (Hickory, NC) to 63% (Lacrosse, WI) across HRRs with a range of 0% to 33% for high-intensity statin use. For the ≥76 age cohort, any statin use ranged from 7% (St Cloud, MN) to 49% (Houma, LA) with a range of 0% to 12% for high-intensity statin use (Supplemental Table 3).
Figure 1.
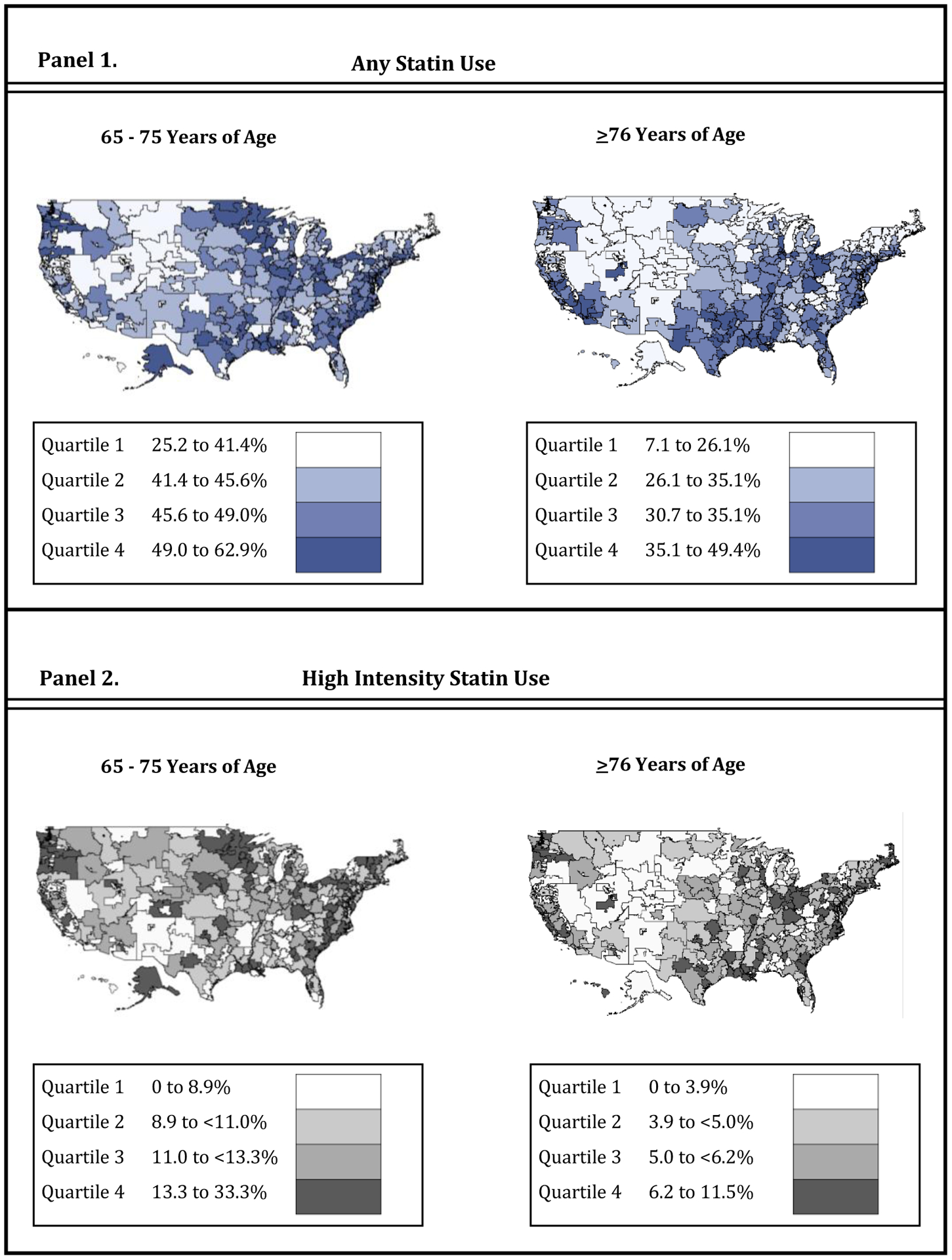
Prevalence of statin: 1. any use and 2. high intensity use, among long stay nursing home residents with life limiting illness across hospital referral regions stratified by age (65–75 years and ≥76 years). High intensity statin use is defined as LDL-C daily dose reduction >50%.
In reference to statin use by HRR characteristics (end-of-life healthcare utilization variables; Tables 2–3), distinct patterns in variation emerged via age group and statin type. With regards to age, the most variation in statin use by HRR characteristics appeared in residents aged ≥76 years, with all but one factor associated with use. More specifically, nursing home residents ≥76 years residing in nursing homes located in HRRs with the highest quartile of healthcare utilization consistently had higher odds of statin utilization than residents living in nursing homes located in HRRs with the lowest quartile (with the exception of hospice utilization). No associations between HRR end-of-life utilization variables and statin use were observed among residents aged 65–75 years. For high-intensity statin use, HRR characteristics were associated with use in some categories for both age groups.
Proportional Change in Regional Variation
When evaluating proportional change in variation (PCV) in cross-classified models for any statin use (Table 4), adding regional- level variables to resident- and facility- adjusted models resulted in reductions in between-HRR and between-state variation. This was especially true for any statin use in the older 76+ age group, in which HRR characteristics alone (PCVHRR: 26.5%, PCVSTATE: 37.2%) appeared to explain a larger percentage of the between-HRR and between-state variation than facility or resident characteristics alone (resident: PCVHRR: 22.9%, PCVSTATE: 21.8%; facility: PCVHRR: 23.9%, PCVSTATE: 26.0%). For high-intensity statin use, resident- level characteristics alone appeared to explain a larger portion of between-region variation than the other levels of characteristics alone. The intraclass correlation coefficients (ICCs) were small (e.g., age ≥76 – high-intensity statin use: ICCHRR: 0.014, ICCSTATE: 0.011).
Table 4.
Cross-classified model variance components including proportional change* estimates in between-hospital referral region (HRR) and between-state variation, explained by resident-, facility-, and regional- level characteristics. N= 361,170 residents, 14,147 facilities, 306 HRRs
| Age 65–75 years | ||||||
|---|---|---|---|---|---|---|
| Model Classification: | Null | |||||
| any statin | ||||||
| T2HRR | 0.01533 | 0.01201 | 0.01194 | 0.01436 | 0.01044 | 0.00991 |
| T2STATE | 0.00979 | 0.00651 | 0.00987 | 0.01002 | 0.00872 | 0.0065 |
| ICCHRR | 0.004624 | 0.003630 | 0.003605 | 0.004333 | 0.003155 | 0.002997 |
|
high-intensity statin |
||||||
| T2HRR | 0.02654 | 0.0236 | 0.02551 | 0.03105 | 0.02342 | 0.02772 |
| T2STATE | 0.01682 | 0.01512 | 0.02188 | 0.01569 | 0.01900 | 0.01523 |
| ICCHRR | 0.007962 | 0.007090 | 0.007644 | 0.009306 | 0.007028 | 0.008317 |
| Age ≥76 years | ||||||
| Model Classification: | Null | |||||
|
any statin |
||||||
| T2HRR | 0.04110 | 0.03167 | 0.03126 | 0.03020 | 0.02691 | 0.02149 |
| T2STATE | 0.04109 | 0.03215 | 0.03040 | 0.02582 | 0.02583 | 0.01902 |
| ICCHRR | 0.01219 | 0.00944 | 0.00933 | 0.00903 | 0.00805 | 0.00645 |
|
high-intensity statin |
||||||
| T2HRR | 0.05135 | 0.04364 | 0.04948 | 0.04907 | 0.04513 | 0.04558 |
| T2STATE | 0.03779 | 0.03288 | 0.04057 | 0.03604 | 0.03576 | 0.03716 |
| ICCHRR | 0.01520 | 0.01296 | 0.01464 | 0.01454 | 0.01339 | 0.01351 |
Proportional change was estimated via cross-classified multilevel logistic models with random intercepts for state and HRR, systematically fit using resident-, facility-, and regional HRR- level characteristics
Abbreviations defined: T2 is the variance of the random intercept; PCV is the proportion change in variation (PCV) explained by the multilevel model with the following formula: (T2 in null model - T2 in adjusted model)/T2 in null model; ICC is the intraclass correlation coefficient (ICC); ICCHRR estimates the correlation in the propensity to use statins between two randomly selected individuals from each HRR, but different states; ICCSTATE estimates the correlation in the propensity to use statins between two individuals in the same state, but different HRR.
DISCUSSION
U.S. nursing home statin use varied by HRRs, crossing state lines. While overall prevalence of statin use was 35%, rates varied across HRRs including up to 63% in residents aged 65–75 years and 49% in residents aged ≥76 years. The resident-level factors associated with statin use in this study (e.g., sex, race/ethnicity, functional limitations, cognitive impairment, and ASCVD) were consistent with previous research.10 The most variation by HRRs was observed in the ≥76 age group, in which HRR-level variables appeared to explain more variation compared to resident and facility variables.
We found that statin use persisted in the nursing home even among those with life-limiting illness, which is consistent with our previous work.12 Moreover, variation in statin use by geographic region among U.S. older adults has been shown in other studies.17,19,36,37 However, these other studies focused on dually eligible Medicare and Medicaid beneficiaries on dialysis,19 Medicare beneficiaries after hospitalization for a myocardial infarction,17,18,36 and all Medicare Part D beneficiaries.37 None evaluated older adults near the end of life or in nursing homes. In addition, none evaluated their target population on the HRR level, instead measuring statin use by U.S. census region,17 state,19 county,37 and zipcode.18 Our study shows that clustering was strongest within HRRs than within states, of which end-of-life healthcare spending measured at the HRR level appeared to explain most of the variation in statin prescribing for residents aged ≥76 years. Interestingly, a study on the geographic variation in carotid endarterectomy and carotid stenting (treatment for extracranial carotid artery disease) showed similar use patterns across HRRs as in our study.38 Perhaps this is because coronary artery disease and peripheral artery disease are risk factors for the metabolic manifestations that statins are designed to treat and thus, treatment patterns are similar. This supports our hypothesis that in the absence of clinical guidelines for advanced age adults, regional prescribing practices rather may drive statin utilization patterns.
Facility level variables associated with increased statin use include having a high proportion of skilled nursing care residents and the average number of medications per resident in the facility ≥ 6. It is possible that in nursing homes with high volume of skilled nursing care (post-acute care), there is less emphasis on considering deprescribing in residents with life-limiting illness than in homes predominantly servicing long stay residents. Further, residents in nursing homes with a greater medication burden per resident overall may be indicative of less focus on reducing the complexity of drug regimens. Our data did not allow us to explore the reasons for the facility-level associations observed.
We found that HRR characteristics relating to end-of-life healthcare utilization appeared to affect statin use in residents aged ≥76 years. This pattern is consistent with the fact that U.S. national guidelines for statin pharmacotherapy largely excludes older adults beyond 75 years of age, often using this age as the upper limit for population-level recommendations. Guidelines, such as the United States Preventative Services Task Force, have cited insufficient evidence as a justification to abstain from providing any statin use recommendations for adults older than 75 years of age. This pattern suggests that clinical uncertainty could lead to more variation in prescribing, allowing other contextual factors to potentially drive prescribing behavior. Our findings highlight the need for evidence to inform U.S. recommendations for statin use in adults beyond age 75 years, especially those most vulnerable to overtreatment, particularly the long-term care population near the end of life. With evidence regarding the risks and benefits of statins in nursing home residents, guidelines should be updated to include recommendations for nursing home residents. Guidelines affect healthcare utilization, including that of statins.39–41 In addition, there should be a concerted effort to elicit a standard of regular patient-provider communication with goals of care and risk-benefit discussions to aid in deprescribing efforts and reduce potential for overprescribing.
Strengths and Limitations
This is the first study to evaluate geographic variation in statin use in a national sample of U.S. nursing home residents, particularly those with life-limiting illness. We were able to evaluate statin use on a more specific geographic scale than previous studies, specifically on the HRR level using multilevel analyses. This study is not without limitations. Analyses are based on data from 2016. Nevertheless, although guidelines and regulations around Medicare are quickly changing, any recent updates seem unlikely to have significantly changed statin prescribing. Our study is observational and therefore at risk for unmeasured confounding. Aside from lacking prescriber information, the inclusion of a limited number of resident variables may have lessened the power of resident-level variables in the ICC analyses. While HRR- level data appear more effective in evaluating regional variation associated with healthcare utilization compared to larger regions of analysis (e.g., states), interventions may be more effectively targeted at smaller levels than HRRs. A 2012 study showed that there was substantial variation in drug spending between hospital service areas within HRRs.42
CONCLUSION
For nursing home residents with life-limiting illness and over ≥76 years of age, there is substantial geographic variation in statin prescribing. HRR regional characteristics appeared to play a role in statin utilization for this population. Our findings highlight the need to implement interventions and policies to better manage prescribing practices for older populations with clinical uncertainty.
Supplementary Material
ACKLOWLEDGMENTS
The data set forth at https://atlasdata.dartmouth.edu of the 2016 Dartmouth Atlas Chronically Ill Care file and the Hospital Referral Region zip code crosswalk file was obtained from The Dartmouth Atlas, which is funded by the Robert Wood Johnson Foundation and the Dartmouth Clinical and Translational Science Institute, under award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH).
Disclosure of funding:
Support for this work included the National Center for Advancing Translational Sciences, National Institutes of Health (TL1 TR001454), the National Institute on Aging (AGK24068300), and the Agency for Healthcare Research and Quality (R36 HS026840). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Disclosure of potential conflicts of interest:
Mack, DS: No potential conflicts exist.
Baek, JB: No potential conflicts exist.
Tjia, J: Dr. Tjia is a consultant for CVS Health and Omnicare Long Term Care Pharmacy.
Lapane, KL: Dr. Lapane serves on an external advisory board to the University of Maryland Lamy Center on work funded by Emperion. Her role is to review and provide comments on monographs for medications used in post-acute care settings.
REFERENCES
- 1.Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in Prescription Drug Use Among Adults in the United States From 1999–2012. JAMA. 2015;314(17):1818–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salami JA, Warraich H, Valero-Elizondo J, et al. National Trends in Statin Use and Expenditures in the US Adult Population From 2002 to 2013: Insights From the Medical Expenditure Panel Survey. JAMA Cardiol. 2017;2(1):56–65. [DOI] [PubMed] [Google Scholar]
- 3.Ngo-Metzger Q, Zuvekas SH, Bierman AS. Estimated Impact of US Preventive Services Task Force Recommendations on Use and Cost of Statins for Cardiovascular Disease Prevention. J Gen Intern Med. 2018;33(8):1317–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chou R, Dana T, Blazina I, Daeges M, Jeanne TL. Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;316(19):2008–2024. [DOI] [PubMed] [Google Scholar]
- 5.Han BH, Sutin D, Williamson JD, et al. Effect of Statin Treatment vs Usual Care on Primary Cardiovascular Prevention Among Older Adults: The ALLHAT-LLT Randomized Clinical Trial. 2017(2168–6114 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armitage J, Baigent C, Barnes E. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. 2019(1474–547X (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zullo AR, Ofori-Asenso R, Wood M, et al. Effects of Statins for Secondary Prevention on Functioning and Other Outcomes Among Nursing Home Residents. 2020(1538–9375 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Final Update Summary: Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: Preventive Medication - US Preventive Services Task Force. . https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/statin-use-in-adults-preventive-medication1. Published 2016. Accessed Accessed December 10, 2018.
- 9.Thorpe CA-O, Sileanu FE, Mor MK, et al. Discontinuation of Statins in Veterans Admitted to Nursing Homes near the End of Life. LID - 10.1111/jgs.16727 [doi]. 2020(1532–5415 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tjia J, Cutrona SL, Peterson D, Reed G, Andrade SE, Mitchell SL. Statin discontinuation in nursing home residents with advanced dementia. J Am Geriatr Soc. 2014;62(11):2095–2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly A, Conell-Price J Fau - Covinsky K, Covinsky K Fau - Cenzer IS, et al. Length of stay for older adults residing in nursing homes at the end of life. 2010(1532–5415 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mack DS, Tjia J, Hume AL, Lapane KL. Prevalent Statin Use in Long-Stay Nursing Home Residents with Life-Limiting Illness. J Am Geriatr Soc. 2020;68(4):708–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silveira MJ, Kazanis As Fau - Shevrin MP, Shevrin MP. Statins in the last six months of life: a recognizable, life-limiting condition does not decrease their use. 2008(1557–7740 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 14.Holmes HM, Min Lc Fau - Yee M, Yee M Fau - Varadhan R, et al. Rationalizing prescribing for older patients with multimorbidity: considering time to benefit. 2013(1179–1969 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kutner JS, Blatchford PJ, Taylor DH Jr., et al. Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med. 2015;175(5):691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curfman G. Risks of Statin Therapy in Older Adults. 2017(2168–6114 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 17.Bittner V, Colantonio LD, Dai Y, et al. Association of Region and Hospital and Patient Characteristics With Use of High-Intensity Statins After Myocardial Infarction Among Medicare Beneficiaries. 2019(2380–6591 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brooks JM, Cook Ea Fau - Chapman CG, Chapman Cg Fau - Kulchaitanaroaj P, et al. Geographic variation in statin use for complex acute myocardial infarction patients: evidence of effective care? 2014(1537–1948 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wetmore JB, Mahnken Jd Fau - Mukhopadhyay P, Mukhopadhyay P Fau - Hou Q, et al. Geographic variation in HMG-CoA reductase inhibitor use in dialysis patients. 2012(1525–1497 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nursing Home Compare - 2016 Annual Files. Nursing Home Compare Data Archive. https://data.medicare.gov/data/archives/nursing-home-compare. Published 2016. Accessed October 18, 2019.
- 21.Provider of Services (POS) - 2016 POS File https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/POS2016.html. Published 2016. Accessed October 18, 2019.
- 22.EOL Chronic Illness. https://atlasdata.dartmouth.edu/static/eol_chronic_illness. Accessed October 18, 2019.
- 23.Hui D, Nooruddin Z, Didwaniya N, et al. Concepts and definitions for “actively dying,” “end of life,” “terminally ill,” “terminal care,” and “transition of care”: a systematic review. 2014(1873–6513 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niznik JD, Zhang S, Mor MK, et al. Adaptation and Initial Validation of Minimum Data Set (MDS) Mortality Risk Index to MDS Version 3.0. 2018(1532–5415 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Porock D, Parker-Oliver D Fau - Petroski GF, Petroski Gf Fau - Rantz M, Rantz M. The MDS Mortality Risk Index: The evolution of a method for predicting 6-month mortality in nursing home residents. 2020(1756–0500 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flacker JM, Kiely DK. Mortality-related factors and 1-year survival in nursing home residents. 2003(0002–8614 (Print)). [DOI] [PubMed] [Google Scholar]
- 27.Kumar G, Hayes K. Hospice and Palliative Care Strategic Plan for an Inpatient Unit: The Dayton Example. In: Office of Academic Affiliations (OAA), Geriatrics and Extended Care in the Office of Patient Service, eds. A Toolkit for Developing Hospice and Palliative Care Programs in the Department of Veterans Affairs Medical Centers. www.va.gov/oaa/flp. Published 2001. Accessed August 13, 2019. [Google Scholar]
- 28.Kelley AS, Ferreira KB, Bollens-Lund E, Mather H, Hanson LC, Ritchie CS. Identifying Older Adults With Serious Illness: Transitioning From ICD-9 to ICD-10. 2019(1873–6513 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bostick JE, Rantz Mj Fau - Flesner MK, Flesner Mk Fau - Riggs CJ, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. 2006(1525–8610 (Print)). [DOI] [PubMed] [Google Scholar]
- 30.Unruh L, Wan TT. A systems framework for evaluating nursing care quality in nursing homes. 2004;30(0148–5598 (Print)). [DOI] [PubMed] [Google Scholar]
- 31.Nursing Home Data Compendium 2015 Edition Nursing Home Data Compendium 2015. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/nursinghomedatacompendium_508-2015.pdf. Published 2015. Accessed August 21, 2017.
- 32.Statistical Abstract of the United States (115th Edition) In: Census USBot, ed. Washington, DC: 1995. [Google Scholar]
- 33.Stone N, Robinson J, Lichtenstein A. ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;63(25):2889–2934. [DOI] [PubMed] [Google Scholar]
- 34.Mortensen MB, Nordestgaard BG. Comparison of Five Major Guidelines for Statin Use in Primary Prevention in a Contemporary General Population. 2018(1539–3704 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 35.Austin PA-OX, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. 2017(1097–0258 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fang G, Robinson J, Lauffenburger J, Roth MT, Brookhart MA. Prevalent but moderate variation across small geographic regions in patient nonadherence to evidence-based preventive therapies in older adults after acute myocardial infarction. 2014(1537–1948 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karpinski SA, Look KA, Vanness DJ. Factors Associated with County-Level Variation in the Prescription of Statins. 2019(2376–1032 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patel MR, Greiner Ma Fau - DiMartino LD, DiMartino Ld Fau - Schulman KA, et al. Geographic variation in carotid revascularization among Medicare beneficiaries, 2003–2006. 2010(1538–3679 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 39.New Cholesterol Guidelines Would Significantly Increase Statin Use If Implemented. https://www.mdedge.com/jcomjournal/article/146995/cardiology/new-cholesterol-guidelines-would-significantly-increase-statin. Accessed February 12, 2019.
- 40.Pagidipati NJ, Navar AM, Mulder H, Sniderman AD, Peterson ED, Pencina MJ. Comparison of Recommended Eligibility for Primary Prevention Statin Therapy Based on the US Preventive Services Task Force Recommendations vs the ACC/AHA Guidelines. 2017(1538–3598 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mack D, Hume A, Tjia J, Lapane K. National Trends in Statin Use among the United States Nursing Home Population (2011 – 2016). Drugs and Aging. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang Y, Baik Sh Fau - Fendrick AM, Fendrick Am, Fau - Baicker K, Baicker K. Comparing local and regional variation in health care spending. 2012(1533–4406 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


