Abstract
Fluconazole and voriconazole MICs were determined for 114 clinical Candida isolates, including isolates of Candida albicans, Candida glabrata, Candida krusei, Candida lusitaniae, Candida parapsilosis, and Candida tropicalis. All strains were susceptible to voriconazole, and most strains were also susceptible to fluconazole, with the exception of C. glabrata and C. krusei, the latter being fully fluconazole resistant. Single-strain regression analysis (SRA) was applied to 54 strains, including American Type Culture Collection reference strains. The regression lines obtained were markedly different for the different Candida species. Using an MIC limit of susceptibility to fluconazole of ≤8 μg/ml, according to NCCLS standards, the zone breakpoint for susceptibility for the 25-μg fluconazole disk was calculated to be ≥18 mm for C. albicans and ≥22 mm for C. glabrata and C. krusei. SRA results for voriconazole were used to estimate an optimal disk content according to rational criteria. A 5-μg disk content of voriconazole gave measurable zones for a tentative resistance limit of 4 μg/ml, whereas a 2.5-μg disk gave zones at the same MIC level for only three of the species. A novel SRA modification, multidisk testing, was also applied to the two major species, C. albicans and C. glabrata, and the MIC estimates were compared with the true MICs for the isolates. There was a significant correlation between the two measurements. Our results show that disk diffusion methods might be useful for azole testing of Candida isolates. The method can be calibrated using SRA. Multidisk testing gives direct estimations of the MICs for the isolates.
Infections with Candida species are common complications in immunocompromised patients and require adequate treatment, often with newer azole drugs. Particularly in AIDS patients with oropharyngeal and/or esophageal candidiasis there have been reports of increased azole resistance among Candida isolates (6, 14, 24, 29, 32–34, 44). This emergence of resistance to drugs has led to a growing demand for susceptibility testing of clinical yeast isolates (14, 32, 41, 43). Comparisons between the standardized NCCLS broth macrodilution method (27) and microdilution methods (12, 22, 33, 38), E-tests (7, 8, 12, 25, 33, 38), and disk diffusion methods (2, 3, 26, 35, 36, 41) suggest a possibility of using the less expensive disk method in clinical microbiology laboratories. We have extended the analysis of azole disk diffusion tests by using single-strain regression analysis (SRA) for studying azole regression lines among Candida species and for calibration of the disk test. Such a calibration method is required since no interpretive zone breakpoints are yet available. The SRA-derived multidisk test (M-test) was also used for MIC estimations of susceptibility to fluconazole and voriconazole, the two azole drugs included. Voriconazole is a new azole with more avid binding to the sterol 14α-demethylase, thereby more effectively inhibiting ergosterol synthesis (22, 34).
MATERIALS AND METHODS
Candida isolates, species identification and culture conditions.
The clinical isolates of Candida species were obtained from blood cultures at the Karolinska Hospital, Stockholm, Sweden, during the years 1994 to 1998. A total of 118 consecutive strains were included and comprised 86 Candida albicans strains, 19 Candida glabrata strains, 3 Candida krusei strains, 2 Candida lusitaniae strains, 5 Candida parapsilosis strains, and 3 Candida tropicalis strains. Four strains of C. albicans were excluded because of poor growth. The following reference strains were also included in the studies: C. albicans ATCC 90028, C. glabrata ATCC 90030, C. krusei ATCC 6258, C. parapsilosis ATCC 22019, and C. tropicalis ATCC 750. For SRA calculations 24 C. albicans strains, 12 C. glabrata strains, 3 C. krusei strains, 2 C. lusitaniae strains, 5 C. parapsilosis strains, and 3 C. tropicalis strains were studied, in all 54 strains including the reference strains. Speciation of clinical isolates was performed using colony characteristics on Sabouraud dextrose agar and CHROM agar Candida differential plates (ILS AB Laboratories, Sollentuna, Sweden) and conventional biochemical and assimilation tests according to established procedures (1, 42).
For E-tests and disk diffusion tests Candida isolates were grown on Sabouraud dextrose agar, and from each strain five colonies were picked and suspended to a 0.5 McFarland density, which was then diluted 1:5 in saline. This suspension was flooded onto RPMI 1640 (AB Biodisk, Solna, Sweden) agar medium plates including MOPS (morpholinepropanesulfonic acid) and 2% glucose, and the excess suspension was aspirated, and this was followed by drying at 37°C for 15 min. E-test strips or disks were then applied, and the plates were incubated and read as described below. The flooding method was used instead of swabbing for inoculation because of improved readability of results with more clear-cut zone edges. This variant has also been suggested by the producer of the E-test (AB Biodisk, oral communication). For many years the flooding method of inoculation was the recommended procedure in Scandinavia for disk testing of clinical bacterial isolates (11).
MIC determinations.
E-tests were performed according to the instructions from the manufacturer (AB Biodisk), using substrates and inoculates as described above and with readings after 24 and 48 h. The E-test strips with fluconazole and voriconazole were kindly provided by AB Biodisk. Criteria for defining the edge of growth followed recommendations by AB Biodisk (E-test technical guide, 1994). MIC determinations were performed once for each strain. Studies have shown good correlations between E-test results and reference dilution method MICs (7, 8, 12, 13, 24, 33, 38). A similar correlation between the NCCLS macrodilution method and the E-test was obtained for fluconazole by E. Chryssanthou (in our laboratory), who tested 29 C. albicans isolates and 110 strains of other Candida species. She found 80% agreement within 1 dilution step and 88% within 2 dilution steps (E. Chryssanthou, personal communication). The E-test was therefore used as the reference method in the present comparisons with M-test MIC estimations.
Range and median MICs for groups were calculated using the full range of E-test values. For the geometric mean value and the MICs at which 50 and 90% of isolates tested were inhibited (MIC50 and MIC90 values, respectively) the E-test results were adjusted to the nearest higher regular 2-log dilution. The 48-h results gave less edge-reading problems for C. albicans, whereas all other species were more easily read after 24 h of incubation. The 48-h results were, however, used throughout the studies in conformity with established procedures (25; AB Biodisk E-test technical guide). When the discrepancy between the 24- and 48-h results was more than fourfold (fluconazole, three strains; voriconazole, four strains) this difference could be attributed to endpoint reading difficulties. In accordance with recent studies by Rex et al. (30) these results were corrected toward the 24-h readings by measuring the outer zone of inhibition in the E-test.
MIC limits for interpretation of susceptibility to fluconazole were ≤8 μg/ml (susceptible) and ≥64 μg/ml (resistant) according to NCCLS guidelines (12, 26, 27, 31). The intermediate category is called S-DD, which stands for susceptible dependent upon dose, i.e., 400 mg or more of fluconazole per day (27). Studies of the MIC correlation with response to fluconazole gave an MIC limit for susceptibility of <25 μg/ml and for resistance of ≥25 μg/ml (34). Similar studies with voriconazole indicated an MIC limit for voriconazole resistance of ≥6.25 μg/ml, but proper interpretive guidelines from the NCCLS or other reference authorities are yet to come (34).
SRA and M-test.
The SRA equation was developed from early equations describing the formation of the inhibition zone in diffusion tests. In the SRA equation the disk content is retained as a variable, which makes it possible to calculate a regression line for a bacterial species using one single, representative strain and several different disk contents of the antibiotic (15, 19). SRA permits the calibration of disk diffusion tests and the calculation of species-related interpretive zone breakpoints (4, 19, 21, 28), as well as the evaluation of an optimal disk potency for susceptibility testing (16, 18, 21). A modification of the SRA equation, the so called M-test, has shown a potential for MIC estimations (17). In the M-test the Q-zero value is first calculated directly from the modified SRA equation (17). This value is proportional to the MIC for the strains. The Q-zero value multiplied by a conversion factor gives the MIC. In the first description of the M-test the conversion factor was around 2, but other figures (unpublished data) have been found for other combinations of antibiotics and microorganisms (17). These methods have now been applied in the present studies to azole susceptibility testing of Candida species.
Disk diffusion antibiotic susceptibility tests.
Disk diffusion testing of Candida species to determine antibiotic susceptibility has been evaluated by several investigators and shown to have potential (2, 3, 12, 23, 35, 36, 41). We applied SRA for the calculation of interpretive zone diameter equivalents of MIC limits for the susceptibility categories and also for estimation of MICs for strains using the M-test (15, 17–20). For SRA experiments two series of disks were produced, containing 2.5, 5.0, 10, 20, 40, and 80 μg of fluconazole and 0.64, 1.25, 2.5, 5.0, 10, 20, and 40 μg of voriconazole, respectively. The production of disks and their control followed established procedures in our laboratory (21). Fluconazole and voriconazole substance was kindy provided by Pfizer (Pfizer Ltd., Sandwich, Kent, England). All clinical isolates were tested by SRA once and the reference strains were tested four times. The fluconazole disk content for routine disk testing has tentatively been set to 25 μg (2, 3, 26, 36, 37). No disk recommendations are available for voriconazole testing.
RESULTS
Determination of MICs of fluconazole and voriconazole for Candida isolates.
The MICs of Candida isolates were determined using E-tests, and the results are shown in Table 1. All Candida species showed homogeneous populations of fluconazole susceptibility, and all strains were within the susceptible category except for strains belonging to C. glabrata and C. krusei. C. glabrata isolates clustered in the S-DD interpretation region, with only 5 of 19 strains falling in the susceptible category. The MIC50 of fluconazole was 16 μg/ml, and the MIC90 for C. glabrata was 32 μg/ml. The three strains of C. krusei were fully resistant. The MIC for one strain of C. albicans was 4 μg/ml, higher than that for the main population of strains of this species.
TABLE 1.
Fluconazole and voriconazole susceptibility of Candida isolatesa
| Species (no. of isolates) | MIC (μg/ml) of fluconazoleb
|
MIC (μg/ml) of voriconazoleb
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Range | Median | Geometric mean | 50% | 90% | Range | Median | Geometric mean | 50% | 90% | |
| C. albicans (82) | 0.094–4 | 0.25 | 0.28 | 0.25 | 0.5 | 0.004–0.38 | 0.012 | 0.013 | 0.015 | 0.015 |
| C. glabrata (19) | 2–32 | 12 | 14 | 16 | 32 | 0.125–2 | 0.5 | 0.52 | 0.5 | 2 |
| C. krusei (3) | 64–128 | 64 | 80 | 64 | 128 | 0.75–1.5 | 0.75 | 1.26 | 1 | 2 |
| C. lusitaniae (2) | 1.5–3 | 2.25 | 2.83 | 2 | 4 | 0.047–0.064 | 0.0555 | 0.06 | 0.06 | 0.06 |
| C. parapsilosis (5) | 0.38–2 | 0.75 | 1 | 1 | 2 | 0.016–0.032 | 0.032 | 0.027 | 0.03 | 0.03 |
| C. tropicalis (3) | 0.5–1 | 0.625 | 0.707 | 0.5 | 1 | 0.032–0.125 | 0.095 | 0.073 | 0.06 | 0.125 |
MICs of strains were determined using the E-test according to the instructions of the manufacturer.
Range and median calculated on full range of MICs from E-tests. 50% and 90%, MIC50 and MIC90, respectively.
For voriconazole the MIC results of the different Candida species were of a magnitude 10 to more than 100 times lower (Table 1). For no clinical isolate was the voriconazole MIC >2 μg/ml. The increase in susceptibility to voriconazole compared to fluconazole was parallel in the different species, and this drug was therefore also least effective against C. glabrata and C. krusei in comparison to the other Candida species. No MIC limits for interpretations are available for this drug, but judging from a tentative resistance limit obtained from clinical outcome studies (34), all strains would belong to the susceptible category. When the fluconazole and voriconazole MICs for all individual strains were plotted on a logarithmic scale there was a significant correlation between the MICs for the two drugs (R2 = 0.848), with a five-step 2-log difference between the two.
Fluconazole SRA studies of Candida species.
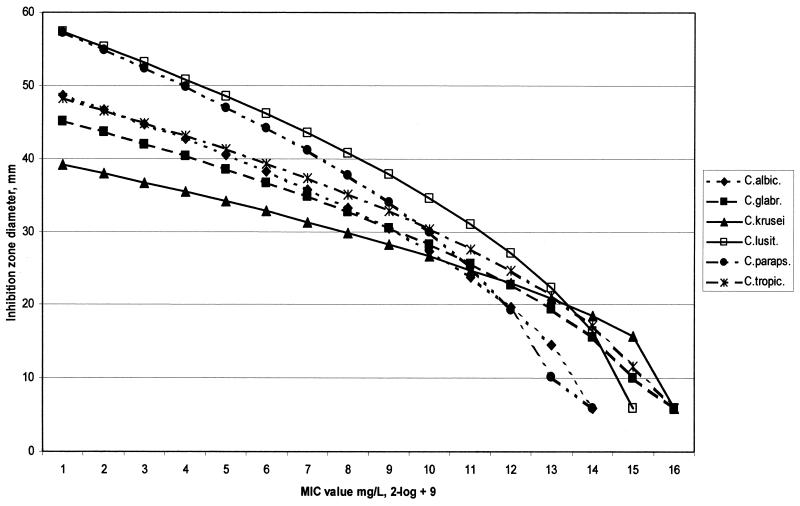
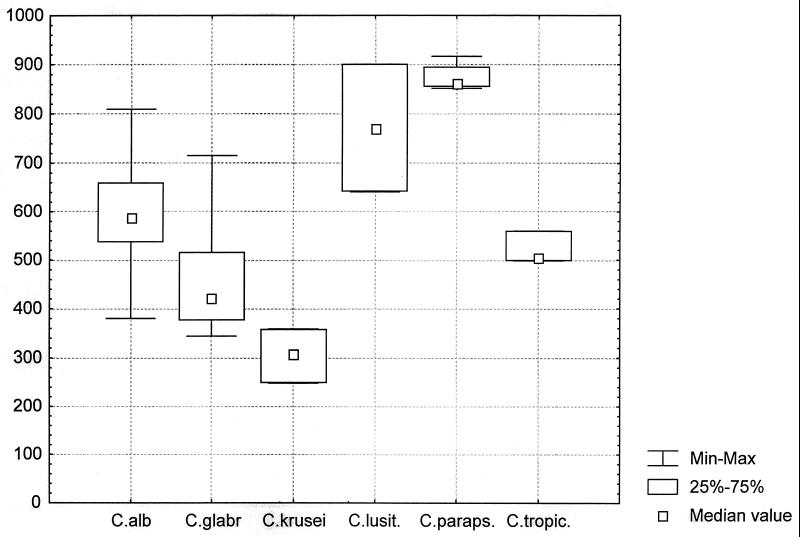
SRA was applied to Candida isolates including 24 C. albicans, 12 C. glabrata, 3 C. krusei, 2 C. lusitaniae, 5 C. parapsilosis, and 3 C. tropicalis strains. Five American Type Culture Collection (ATCC) reference Candida strains were also analyzed. Fluconazole regression lines calculated for a 25-μg disk content from the means of the constants for the clinical isolates specieswise showed a substantial variation between the different species (Fig. 1). A statistical analysis showed that the species differed significantly in their constant A values (Kruskal-Wallis test and Mann-Whitney U test after Bonferroni correction). A box-plot of the constant A values is shown in Fig. 2. C. krusei gave the lowest value for the slope constant A (A = 305) whereas C. lusitaniae and C. parapsilosis showed the steepest curves (A = 771 and A = 876, respectively [Fig. 2]). Among isolates from the same species the A constants were relatively homogeneous, with coefficients of variation between 3 and 25%. The results indicated that the different Candida species should be treated separately. Results for the ATCC reference strains showed a similar pattern, with C. parapsilosis giving the steepest curve. The A constants were within the 25 to 75% range of the clinical isolates for only C. glabrata, and C. krusei. The C. parapsilosis and C. tropicalis values were outside the full range of the clinical isolates of the same species and the C. albicans constant A was just within this range. Therefore, these reference strains should perhaps not be used as representatives without further investigations. In these studies the mean values of the constants from the clinical isolates were used for calibrations.
FIG. 1.
Regression lines for a 25-μg fluconazole disk and different Candida species, calculated using the mean SRA equation constants A and B obtained from tests of clinical isolates. The SRA equation uses the zone size squared, which gives a curved appearance of the regression lines in this linear plot. Abbreviations: C.albic., C. albicans; C.glabr., C. glabrata; C.lusit., C. lusitaniae; C.paraps., C. parapsilosis; C.tropic., C. tropicalis.
FIG. 2.
Box plot of SRA constant A values from clinical isolates in fluconazole SRA tests using an M-test series of disks containing 2.5, 5.0, 10, 20, 40, and 80 μg of fluconazole, respectively. C. alb, C. albicans (see the legend to Fig. 1 for other abbreviations).
Calibration of fluconazole disk diffusion testing of Candida species.
Using the fluconazole regression lines shown in Fig. 1 the zone diameter interpretive breakpoints corresponding to the MIC limits (for susceptibility, ≤8 μg/ml, and for resistance, ≥64 μg/ml for fluconazole, according to NCCLS guidelines) were calculated for the most common species. For the 25-μg fluconazole disk the calculated zone breakpoints for susceptibility were ≥18 mm for C. albicans and ≥22 mm for C. glabrata and C. krusei. A disk content of 20 μg of fluconazole will give zone diameters just below the results obtained using a 25-μg disk, i.e., about 1 mm less. When the zone breakpoints were tested on the available 20-μg disk results, all C. albicans strains were susceptible in accordance with the MIC results. The C. glabrata isolates clustered around the susceptibility breakpoint, in line with the MIC results. C. krusei isolates were all resistant. It was thus apparent that calibration of the disk test yielded results which corresponded to MIC results.
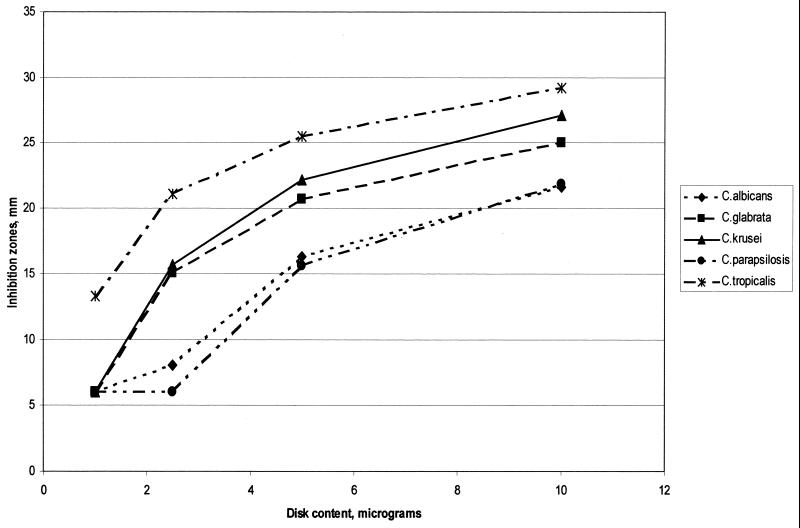
Determination of an optimal disk potency for voriconazole disk testing.
A rational definition of an optimal disk content has been proposed in earlier studies (16, 21). It was defined as the smallest amount of antibiotic in the disk still capable of producing measurable inhibition zones corresponding to the MIC limit for resistance and for all bacterial species encountered. The interesting point is that this criterion can be tested using SRA. Since no recommendations on MIC susceptibility limits are yet available, a resistance breakpoint of ≥6.25 μg/ml given in studies of voriconazole (34) was taken as an indication of the level of the MIC limit. We therefore used 4 μg/ml as an MIC limit for calculation of an optimal disk content, but there is reason to believe that the limit might be set at a lower level. The zone equivalents of 4 μg/ml were then calculated for five Candida species using regression lines with mean equation constants from SRA studies of the clinical isolates (Fig. 3). Both 10- and a 5-μg voriconazole disks gave adequate zones at 4 μg/ml for all five Candida species, whereas a 2.5-μg disk gave zones at the same MIC for only three of the species (Fig. 3). A 5-μg voriconazole disk seems optimal if an MIC limit for voriconazole resistance is around 4 μg/ml. Calibration of voriconazole disk diffusion testing of Candida species would also be possible, analogous to the calibration for fluconazole, but such calculations await the proper announcement of MIC limits for the susceptibility categories.
FIG. 3.
Calculated inhibition zone diameter equivalents of a voriconazole MIC of 4 μg/ml around disks with 1, 2.5, 5, and 10 μg of voriconazole, respectively.
M-test of azole MICs for Candida species.
SRA will permit the estimation of the MICs for strains according to recent modifications and the development of the M-test (17). We applied the M-test principle to fluconazole and voriconazole testing of the two most frequent Candida species in the present studies. The Q-zero values were determined for 24 strains of C. albicans and for 12 strains of C. glabrata. Comparisons with the true MICs obtained by E-tests permitted a calculation of the conversion factors required to convert Q-zero to an MIC. Their mean values were 1.55 (standard deviation [SD], 1.0) and 4.12 (SD, 1.9), respectively, for fluconazole and 2.71 (SD, 3.1) and 7.41 (SD, 11.2), respectively, for voriconazole. Earlier studies have shown mean conversion values of ca. 2, and until further studies have confirmed the species-related conversion factors above, a factor of two was used in the present studies for estimating the MICs for the strains (17). When the estimated MICs were compared with the E-test-generated MICs there was a positive correlation between the two, for both Candida species and the two antibiotics. The r value was 0.859 for the fluconazole-C. glabrata combination and 0.70 for the fluconazole-C. albicans combination and was lower for voriconazole testing. These results are very interesting and should be further evaluated using reference methods for MIC determinations and with particular emphasis on the possible correlation between different conversion factors and Candida species.
DISCUSSION
Using the E-test for MIC determinations we could confirm the susceptibility of 114 clinical Candida isolates to voriconazole, including the species C. albicans, C. glabrata, C. krusei, C. lusitaniae, C. parapsilosis, and C. tropicalis (Table 1) (22, 34). The fluconazole MICs for the 114 Candida isolates were as expected from earlier reports, with all species susceptible, except C. glabrata, which was susceptible to S-DD, and C. krusei, which was fully resistant (22, 33, 34, 38). When we compared the results for MICs of fluconazole and voriconazole for each strain there was a correlation between the two as reported earlier for azole drugs including voriconazole (5, 29, 34, 40). The five 2-log steps by which MICs of voriconazole were lower brought the less fluconazole-susceptible species C. glabrata and C. krusei into the range of voriconazole susceptibility. This azole cross-resistance in Candida isolates might suggest that earlier azole drugs with lower activity should be avoided and that the more potent azoles should be used in all instances, calling for this kind of drug.
Earlier studies have indicated that disk diffusion might be used for the susceptibility testing of Candida isolates (2, 3, 23, 26, 35–37, 41). There are, however, problems with the reading of the results as pointed out by others, which we can verify. The E-test is also a diffusion-based method, and the instructions for Candida E-testing can serve as a useful guide for the determination of the proper edge of the inhibition zone (AB Biodisk E-test technical guide). The other problem with azole disk testing of Candida isolates is the lack of proper guidelines for disk contents and susceptibility interpretations. In the present studies we have shown that this problem can be solved by calculating the zone diameter equivalent of the MIC limit for susceptibility using SRA (15, 19–21, 28). The regression lines can be determined for the individual species, and the laboratory-specific influence is automatically included when this analysis is performed in the individual clinical microbiology setting. This method seems promising as a new tool for calibration of disk testing in those laboratories where large volumes of isolated pathogens are tested daily for antibiotic susceptibility. Often, the ATCC reference strain for a species shares the characteristics of most clinical isolates and can therefore be used as the reference strain for SRA calibration. For the Candida species studied here this does not seem to be the case, and further studies are therefore required in order to select representative ATCC or National Collection of Type Cultures strains for SRA reference purposes in disk test calibration.
A rational definition of the optimal disk content of an antibiotic for disk testing has recently been proposed by Kronvall and Holst (18; see also references 16 and 21): “the lowest disk content of antibiotic which will distinguish resistant strains of any bacterial species from strains of the intermediate or susceptible category.” This means that measurable inhibition zones should be produced corresponding to the MIC limit for resistance, a criterion which can easily be tested using SRA calculations. This definition ensures that the disk content will not be too low but will not be unnecessarily high either. We applied this definition to voriconazole susceptibility testing, assuming an MIC limit for voriconazole resistance of 4 μg/l based on levels obtained by oral medication (34). The results indicated that a 5-μg disk content of voriconazole would suffice. However, a lower MIC limit for resistance might be possible, and then a 2- to 2.5-μg disk content could be sufficient. A final calculation awaits the NCCLS guidelines for voriconazole testing when the MIC limits for susceptibility have been decided upon.
A novel SRA modification based on principles known for several years (9, 10, 39) was also tested in the present studies, the M-test (17). When the antibiotic applications are made on a strip it might look like the E-test, but the latter is based on the diffusion of a predefined continous gradient of antibiotic whereas in contrast the M-test uses three to five different disk contents of antibiotics and the MICs are calculated using the modified SRA equation (17). The M-test was applied to the two major species, C. albicans and C. glabrata, and the MIC estimates (using a general conversion factor of 2.0) were compared with the true MICs of the isolates. There was a significant correlation between the two measurements. We also found clear species-related differences for the conversion factor. Reports have shown that E-test results indicate MICs that are higher than true MIC for some species, e.g., C. albicans, but lower for other species, e.g., C. glabrata, C. tropicalis, and C. parapsilosis (7, 25, 43). Species-related conversion factors might remedy such deviations in M-tests.
The results of the present studies on azole susceptibility testing of Candida species have shown that voriconazole might be a first-choice azole in treating Candida infections. It was also clear that the lack of proper zone diameter breakpoints for susceptibility interpretations can be remedied by SRA calibration of the azole disk test. This calibration procedure will also provide species-related and laboratory-specific interpretive breakpoints corresponding to the reference authority-recommended MIC limits for the susceptibility categories. Moreover, a novel modification of SRA, the M-test, will permit the direct estimation of MICs for clinical isolates. However, there are still some uncertainties regarding the proper conversion factors to be used for the different combinations of drugs and species, and these uncertainties have to be solved by extended studies on the applicability of the M-test.
ACKNOWLEDGMENTS
This research work was supported by a grant from Pfizer AB, Täby, Sweden; by funds from the Karolinska Institute; and by the Scandinavian Society for Antimicrobial Chemotherapy Foundation.
We acknowledge Erja Chryssanthou for valuable advice and fruitful discussions and Anne Bolmström, AB Biodisk, for providing E-test strips for MIC determinations.
REFERENCES
- 1.Barnett J A, Payne R W, Yarrow D. Yeasts: characteristics and identification. Cambridge, England: Cambridge University Press; 1990. [Google Scholar]
- 2.Barry A L, Brown S D. Fluconazole disk diffusion procedure for determining susceptibility of Candida species. J Clin Microbiol. 1996;34:2154–2157. doi: 10.1128/jcm.34.9.2154-2157.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bille J, Glauser M P. Evaluation of the susceptibility of pathogenic Candida species to fluconazole. Fluconazole Global Susceptibility Study Group. Eur J Clin Microbiol Infect Dis. 1997;16:924–928. doi: 10.1007/BF01700561. [DOI] [PubMed] [Google Scholar]
- 4.Björklind A, Ringertz S, Kronvall G. Types of interpretive errors in susceptibility testing. APMIS. 1989;97:941–948. doi: 10.1111/j.1699-0463.1989.tb00502.x. [DOI] [PubMed] [Google Scholar]
- 5.Cartledge J D, Midgley J, Gazzard B G. Clinically significant azole cross-resistance in Candida isolates from HIV-positive patients with oral candidosis. AIDS. 1997;11:1839–1844. doi: 10.1097/00002030-199715000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Chryssanthou E, Torssander J, Petrini B. Oral Candida albicans isolates with reduced susceptibility to fluconazole in Swedish HIV-infected patients. Scand J Infect Dis. 1995;27:391–395. doi: 10.3109/00365549509032737. [DOI] [PubMed] [Google Scholar]
- 7.Colombo A L, Barchiesi F, McGough D A, Fothergill A W, Rinaldi M G. Evaluation of the E test system versus a microtitre broth method for antifungal susceptibility testing of yeasts against fluconazole and itraconazole. J Antimicrob Chemother. 1995;36:93–100. doi: 10.1093/jac/36.1.93. [DOI] [PubMed] [Google Scholar]
- 8.Colombo A L, Barchiesi F, McGough D A, Rinaldi M G. Comparison of Etest and National Committee for Clinical Laboratory Standards broth macrodilution method for azole antifungal susceptibility testing. J Clin Microbiol. 1995;33:535–540. doi: 10.1128/jcm.33.3.535-540.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delignette-Muller M L, Flandrois J P. An accurate diffusion method for determining bacterial sensitivity to antibiotics. J Antimicrob Chemother. 1994;34:73–81. doi: 10.1093/jac/34.1.73. [DOI] [PubMed] [Google Scholar]
- 10.Drugeon H B, Juvin M-E, Caillon J, Courtieu A-L. Assessment of formulas for calculating critical concentration by the agar diffusion method. Antimicrob Agents Chemother. 1987;31:870–875. doi: 10.1128/aac.31.6.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ericsson H M, Sherris J C. Antibiotic sensitivity testing. Report of an international collaborative study. Acta Pathol Microbiol Scand Sect B. 1971;(Suppl. 217:1–90. [PubMed] [Google Scholar]
- 12.Espinel-Ingroff A, Barchiesi F, Hazen K C, Martinez-Suarez J V, Scalise G. Standardization of antifungal susceptibility testing and clinical relevance. Med Mycol. 1998;36(Suppl. 1):68–78. [PubMed] [Google Scholar]
- 13.Espinel-Ingroff A, Pfaller M, Erwin M E, Jones R N. Interlaboratory evaluation of Etest method for testing antifungal susceptibilities of pathogenic yeasts to five antifungal agents by using Casitone agar and solidified RPMI 1640 medium with 2% glucose. J Clin Microbiol. 1996;34:848–852. doi: 10.1128/jcm.34.4.848-852.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Franz R, Kelly S L, Lamb D C, Kelly D E, Ruhnke M, Morschhauser J. Multiple molecular mechanisms contribute to a stepwise development of fluconazole resistance in clinical Candida albicans strains. Antimicrob Agents Chemother. 1998;42:3065–3072. doi: 10.1128/aac.42.12.3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kronvall G. Analysis of a single reference strain for determination of gentamicin regression line constants and inhibition zone diameter breakpoints in quality control of disk diffusion antibiotic susceptibility testing. J Clin Microbiol. 1982;16:784–793. doi: 10.1128/jcm.16.5.784-793.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kronvall G. Improving the accuracy of disc diffusion antibiotic susceptibility testing using species-related interpretive zone breakpoints. Indian J Med Microbiol. 1998;16:138–142. [Google Scholar]
- 17.Kronvall G. MIC determination of fusidic acid and of ciprofloxacin using multidisk diffusion tests. Clin Microbiol Infect. 2000;6:483–489. doi: 10.1046/j.1469-0691.2000.00135.x. [DOI] [PubMed] [Google Scholar]
- 18.Kronvall G, Holst E. Calibration of the disk diffusion test for trovafloxacin susceptibility testing of four anaerobic species. Clin Microbiol Infect. 2000;6:195–201. doi: 10.1046/j.1469-0691.2000.00031.x. [DOI] [PubMed] [Google Scholar]
- 19.Kronvall G, Ringertz S. Antibiotic disk diffusion testing revisited. Single strain regression analysis. APMIS. 1991;99:295–306. doi: 10.1111/j.1699-0463.1991.tb05153.x. [DOI] [PubMed] [Google Scholar]
- 20.Kronvall G, Ringertz S, Karlsson I, Göransson E, Dornbusch K. Laboratory- and species-specific interpretive breakpoints for disk diffusion tests of chloramphenicol susceptibility of Haemophilus influenzae. Antimicrob Agents Chemother. 1988;32:1484–1489. doi: 10.1128/aac.32.10.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kronvall G, Rylander M, Walder M, Lind-Brandberg L, Larsson P, Törnqvist E, Monsen T. Calibration of disk diffusion antibiotic susceptibility testing: species-related trovafloxacin interpretive zone breakpoints and selection of disk potency. Scand J Infect Dis. 1999;31:573–578. doi: 10.1080/00365549950164463. [DOI] [PubMed] [Google Scholar]
- 22.Lozano-Chiu M, Arikan S, Paetznick V L, Anaissie E J, Rex J H. Optimizing voriconazole susceptibility testing of Candida: effects of incubation time, endpoint rule, species of Candida, and level of fluconazole susceptibility. J Clin Microbiol. 1999;37:2755–2759. doi: 10.1128/jcm.37.9.2755-2759.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lozano-Chiu M, Nelson P W, Paetznick V L, Rex J H. Disk diffusion method for determining susceptibilities of Candida spp. to MK-0991. J Clin Microbiol. 1999;37:1625–1627. doi: 10.1128/jcm.37.5.1625-1627.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin M V. The use of fluconazole and itraconazole in the treatment of Candida albicans infections: a review. J Antimicrob Chemother. 1999;44:429–437. doi: 10.1093/jac/44.4.429. [DOI] [PubMed] [Google Scholar]
- 25.Martin-Mazuelos E, Gutierrez M J, Aller A I, Bernal S, Martinez M A, Montero O, Quindos G. A comparative evaluation of Etest and broth microdilution methods for fluconazole and itraconazole susceptibility testing of Candida spp. J Antimicrob Chemother. 1999;43:477–481. doi: 10.1093/jac/43.4.477. [DOI] [PubMed] [Google Scholar]
- 26.Meis J, Petrou M, Bille J, Ellis D, Gibbs D Global Antifungal Surveillance Group. A global evaluation of the susceptibility of Candida species to fluconazole by disk diffusion. Diagn Microbiol Infect Dis. 2000;36:215–223. doi: 10.1016/s0732-8893(99)00152-2. [DOI] [PubMed] [Google Scholar]
- 27.National Committee for Clinical Laboratory Standards. Reference method for broth dilution antifungal susceptibility testing of yeasts. 1997. pp. 1–29. . Approved standard. Document M27-A. National Committee for Clinical Laboratory Standards, Wayne, Pa. [Google Scholar]
- 28.Oppenheimer M, Kronvall G, Karlsson I, Holst E. Fusidic acid disk diffusion testing of Clostridium difficile can be calibrated using SRA, single strain regression analysis. Scand J Infect Dis. 2000;32:633–637. doi: 10.1080/003655400459540. [DOI] [PubMed] [Google Scholar]
- 29.Pelletier R, Peter J, Antin C, Gonzalez C, Wood L, Walsh T J. Emergence of resistance of Candida albicans to clotrimazole in human immunodeficiency virus-infected children: in vitro and clinical correlations. J Clin Microbiol. 2000;38:1563–1568. doi: 10.1128/jcm.38.4.1563-1568.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rex J H, Nelson P W, Paetznick V L, Lozano-Chiu M, Espinel-Ingroff A, Anaissie E J. Optimizing the correlation between results of testing in vitro and therapeutic outcome in vivo for fluconazole by testing critical isolates in a murine model of invasive candidiasis. Antimicrob Agents Chemother. 1998;42:129–134. doi: 10.1128/aac.42.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rex J H, Pfaller M A, Galgiani J N, Bartlett M S, Espinel-Ingroff A, Ghannoum M A, Lancaster M, Odds F C, Rinaldi M G, Walsh T J, Barry A L. Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro-in vivo correlation data for fluconazole, itraconazole, and candida infections. Subcommittee on Antifungal Susceptibility Testing of the National Committee for Clinical Laboratory Standards. Clin Infect Dis. 1997;24:235–247. doi: 10.1093/clinids/24.2.235. [DOI] [PubMed] [Google Scholar]
- 32.Rex J H, Rinaldi M G, Pfaller M A. Resistance of Candida species to fluconazole. Antimicrob Agents Chemother. 1995;39:1–8. doi: 10.1128/aac.39.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ruhnke M, Schmidt-Westhausen A, Engelmann E, Trautmann M. Comparative evaluation of three antifungal susceptibility test methods for Candida albicans isolates and correlation with response to fluconazole therapy. J Clin Microbiol. 1996;34:3208–3211. doi: 10.1128/jcm.34.12.3208-3211.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruhnke M, Schmidt-Westhausen A, Trautmann M. In vitro activities of voriconazole (UK-109,496) against fluconazole-susceptible and -resistant Candida albicans isolates from oral cavities of patients with human immunodeficiency virus infection. Antimicrob Agents Chemother. 1997;41:575–577. doi: 10.1128/aac.41.3.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sandven P. Detection of fluconazole-resistant Candida strains by a disc diffusion screening test. J Clin Microbiol. 1999;37:3856–3859. doi: 10.1128/jcm.37.12.3856-3859.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scheven M. Testing susceptibility of fungi to fluconazole. Eur J Clin Microbiol Infect Dis. 1993;12:393–395. doi: 10.1007/BF01964441. [DOI] [PubMed] [Google Scholar]
- 37.Schmalreck A F, Kottmann I. Empfindlichkeitsprüfung von Hefen gegenüber Fluconazol: Vorschlag für eine standardisierte Agardiffusions-Methode mit 25-μg-Fluconazol-Testblättchen. Mycoses. 1996;39(Suppl. 2):27–30. doi: 10.1111/j.1439-0507.1996.tb00524.x. [DOI] [PubMed] [Google Scholar]
- 38.Sewell D L, Pfaller M A, Barry A L. Comparison of broth macrodilution, broth microdilution, and E test antifungal susceptibility tests for fluconazole. J Clin Microbiol. 1994;32:2099–2102. doi: 10.1128/jcm.32.9.2099-2102.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shannon R, Hedges A J, Edwards R J. Distribution of levels of penicillin resistance among freshly isolated strains of N. gonorrhoeae. Application of a novel sensitivity assay. Br J Venereal Dis. 1975;51:246–250. doi: 10.1136/sti.51.4.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stevens D A, Stevens J A. Cross-resistance phenotypes of fluconazole-resistant Candida species: results with 655 clinical isolates with different methods. Diagn Microbiol Infect Dis. 1996;26:145–148. doi: 10.1016/s0732-8893(96)00199-x. [DOI] [PubMed] [Google Scholar]
- 41.Troillet N, Durussel C, Bille J, Glauser M P, Chave J P. Correlation between in vitro susceptibility of Candida albicans and fluconazole-resistant oropharyngeal candidiasis in HIV-infected patients. Eur J Clin Microbiol Infect Dis. 1993;12:911–915. doi: 10.1007/BF01992164. [DOI] [PubMed] [Google Scholar]
- 42.Warren N G, Hazen K C. Candida, Cryptococcus, and other yeasts of medical importance. In: Murray P R, Baron E J, Pfaller M A, Tenover F C, Yolken R H, editors. Manual of Clinical Microbiology. Washington, D.C.: ASM Press; 1999. pp. 1184–1199. [Google Scholar]
- 43.White T C, Marr K A, Bowden R A. Clinical, cellular, and molecular factors that contribute to antifungal drug resistance. Clin Microbiol Rev. 1998;11:382–402. doi: 10.1128/cmr.11.2.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu J, Ramos A R, Vilgalys R, Mitchell T G. Clonal and spontaneous origins of fluconazole resistance in Candida albicans. J Clin Microbiol. 2000;38:1214–1220. doi: 10.1128/jcm.38.3.1214-1220.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]