Key Points
Question
How common and expensive are medical services that can require prior authorization?
Findings
This cross-sectional study examined medical services paid for by government-administered Medicare Part B, which lacks prior authorization requirements, for approximately 6.5 million beneficiaries; 2.2 services per beneficiary per year would have been subject to prior authorization under the coverage rules of a large Medicare Advantage insurer, and these services accounted for 25% of annual Part B spending.
Meaning
In Medicare, the scope of prior authorization policies differs considerably between government-administered insurance and privately administered insurance.
Abstract
Importance
Health insurers use prior authorization to evaluate the medical necessity of planned medical services. Data challenges have precluded measuring the frequency with which medical services can require prior authorization, the spending on these services, the types of services and clinician specialties affected, and differences in the scope of prior authorization policies between government-administered and privately administered insurance.
Objectives
To measure the extent of prior authorization requirements for medical services and to describe the services and clinician specialties affected by them using novel data on private insurer coverage policies.
Design, Setting, and Participants
Fee-for-service Medicare claims from 2017 were analyzed for beneficiaries in Medicare Part B, which lacks prior authorization. We measured the use of services that would have been subject to prior authorization according to the coverage rules of a large Medicare Advantage insurer and calculated the associated spending. We report the rates of these services for 14 clinical categories and 27 clinician specialties.
Main Outcomes and Measures
Annual count per beneficiary and associated spending for 1151 services requiring prior authorization by the Medicare Advantage insurer; likelihood of providing 1 or more such service per year, by clinician specialty.
Results
Of 6 497 534 beneficiaries (mean [SD] age, 72.1 [12.1] years), 41% received at least 1 service per year that would have been subject to prior authorization under Medicare Advantage prior authorization requirements. The mean (SD) number of services per beneficiary per year was 2.2 (8.9) (95% CI, 2.17-2.18), corresponding to a mean (SD) of $1661 ($8900) in spending per beneficiary per year (95% CI, $1654-$1668), or 25% of total annual Part B spending. Part B drugs constituted 58% of the associated spending, mostly accounted for by hematology or oncology drugs. Radiology was the largest source of nondrug spending (16%), followed by musculoskeletal services (9%). Physician specialties varied widely in rates of services that required prior authorization, with highest rates among radiation oncologists (97%), cardiologists (93%), and radiologists (91%) and lowest rates among pathologists (2%) and psychiatrists (4%).
Conclusions and Relevance
In this cross-sectional study, a large portion of fee-for-service Medicare Part B spending would have been subject to prior authorization under private insurance coverage policies. Prior authorization requirements for Part B drugs have been an important source of difference in coverage policy between government-administered and privately administered Medicare.
This cross-sectional study measures the extent of prior authorization requirements for medical services and describes the services and clinician specialties affected by them using novel data on private insurer coverage policies
Introduction
Since the 1980s, health insurers in the United States have used prior authorization to evaluate prospectively whether a medical service will meet coverage criteria.1 The rationale for prior authorization is to identify and discourage costly low-value services, thereby reducing health care spending without impairing health care quality. By targeting medical services that insurers view as susceptible to inappropriate use, prior authorization differs from other insurer tools that broadly incentivize lower health care spending, such as patient cost sharing or risk-based third-party payment. The persistent role of prior authorization and its expansion in prescription drug policy between 2007 and 2017 suggest that these programs can produce savings.2 However, citing administrative burdens, provider groups and policy scholars have sought prior authorization reforms.3,4,5
Despite the enduring presence of prior authorization, basic facts about the practice remain unknown. For example, it is unclear how often a clinician’s diagnosis or treatment plan falls under a prior authorization policy in general or in particular clinical domains. Such information could inform policy makers’ understanding of prior authorization’s potential for savings and its administrative burden. Although there have been quasi-experimental studies of prior authorization for specific prescription drug classes,6,7,8,9 data challenges have been an obstacle to measuring the overall scope of prior authorization. Data sets used to track health care use tend to include only final approved transactions.10 Even when data on prior authorization requests are available, they can be inaccurate11 and will fail to include whatever services were deterred by prior authorization without an explicit insurer denial, the so-called sentinel effect.
Prior authorization also represents a difference in insurance design between private insurers and government-administered insurance in Medicare. In Medicare Part D, private insurers administer prescription drug plans, and approximately 1 in 4 drugs on the plans’ formularies requires prior authorization.2 In Medicare Advantage, private insurers administer both medical and drug benefits, and 80% of plans require prior authorization for some types of nonprescription services.12 In contrast, fee-for-service Medicare has used minimal prior authorization, generally limited to demonstration projects for select nonphysician services (eg, durable medical equipment),13 although expansions are underway for select outpatient services.14 The absence of prior authorization in fee-for-service Medicare provides an opportunity to quantify the scope of private insurers’ prior authorization policies and to better understand their role in US health care.
In this study, we measured the scope of prior authorization by applying a private insurer’s Medicare Advantage prior authorization rules to the medical services provided to fee-for-service Medicare beneficiaries under Medicare Part B. We quantified the frequency of services delivered in fee-for-service Medicare that would have required prior authorization in Medicare Advantage and calculated the associated spending. We categorized the clinical types of services subject to prior authorization and the differential rates across clinicians by specialty.
Methods
Data Sources and Sample Population
We analyzed claims and enrollment data for a random 20% sample of Medicare fee-for-service beneficiaries in 2017. The purpose of employing fee-for-service claims in an analysis of Medicare Advantage coverage policy was to allow more complete detection of services that would require prior authorization under Medicare Advantage. Our aim was to detect medical services that would be subject to prior authorization regardless of whether prior authorization for the service (1) would be approved, (2) would be denied, or (3) would not be sought owing to the sentinel effect of the prior authorization policy. The lack of prior authorization in fee-for-service Medicare ensured that all these services would be present in claims even though some would have been deterred had they been subject to Medicare Advantage prior authorization policies. In contrast, alternate data sources, such as Medicare Advantage paid claims, would not include deterred services in the second and third categories, the sources of savings from prior authorization. Data containing prior authorization applications would also lack the third category of services. Fee-for-service Medicare is therefore an ideal setting to estimate the scope of prior authorization policies. We restricted our beneficiary sample to those continuously enrolled in Medicare Part B while alive throughout 2017. The demographic categories used to describe sample characteristics were defined according to Medicare administrative enrollment files.15
We obtained proprietary prior authorization data from a large Medicare Advantage insurer, Aetna.16 The data included all services for which Aetna required prior authorization in 2017 according to the Aetna Participating Provider Precertification List, the Healthcare Common Procedure Coding System (HCPCS) code used to identify the service, and the 2017 approval rate for prior authorization requests for the service. Aetna uses prior authorization for the same services in Medicare Advantage and non-Medicare plans, although approval criteria may differ owing to Medicare coverage requirements. Notably, Aetna’s prior authorization policies for Part B drugs did not involve step therapy or a pharmacy benefits manager during the study period.
We restricted our analysis to Part B covered services (physician and other professional services, ambulance, durable medical equipment, and Part B drugs) that were active nationally in the precertification program for all of 2017 and required medical review. We excluded steerage reviews, which encourage service delivery by an in-network clinician or provider institution. We refer to included services as “prior authorization services” throughout the remainder of the study. Whether a service required prior authorization was generally based on its HCPCS code alone. For some services, prior authorization requirements depended on other clinical information, such as diagnosis or place of service. We excluded 2 service codes whose requirement for prior authorization could not be readily obtained from claims data. A total of 1151 HCPCS codes satisfied these inclusion criteria. The study protocol was approved by the institutional review board of the Harvard Faculty of Medicine, who waived the requirement for informed consent because they deemed that the use or disclosure of protected health information would not adversely affect the privacy rights and the welfare of the individuals.
Detection of Prior Authorization Services
We detected prior authorization services using the HCPCS procedure codes present in Medicare claims from the 2017 Carrier (professional) file, Outpatient (institutional) file, and Durable Medical Equipment (supplier) file. We excluded noncovered services according to guidance from the Centers for Medicare & Medicaid Services (R. Gbadebo, MPH, MS, Research Data Assistance Center, email, August 2020) using claim processing codes, modifier codes, and indicators for noncovered charges. To avoid potential duplicate claims, we collapsed multiple claims for the same HCPCS code, beneficiary, and service date to a single observation and defined this observation as a single instance of a prior authorization service. We also used service-specific exclusion criteria when the prior authorization requirement for a service depended on additional criteria.
We calculated the mean number of prior authorization services per beneficiary and the mean associated spending per beneficiary. The spending associated with each instance of a prior authorization service and the components of spending (beneficiary cost sharing, Medicare spending, and spending by other payers) were calculated using service-level claim line and revenue center data. Because covered services paid via the Outpatient Prospective Payment System may not have service-level spending recorded in facility claims (eg, for non–pass-through drugs), we imputed spending when necessary. See the eAppendix in the Supplement for details on service-specific exclusion criteria, assigning place of service, and spending imputation.
Although these methods allowed us to calculate the spending associated with prior authorization services, they cannot provide a causal estimate of savings if fee-for-service Medicare were to expand its scope of services requiring prior authorization. Such an estimate would require additional assumptions, such as the magnitudes of any deterrence effects and offsetting spending on substitute services. We detail these assumptions and a provide a range of approximate savings estimates in the eAppendix in the Supplement.
We summarized the number of prior authorization services and the associated spending by service types by assigning services to 1 of 14 clinical categories. Service categories were assigned based on a proprietary HCPCS mapping crosswalk provided by Aetna, augmented by manual assignment of drug categories by clinical specialty. All service category definitions are presented in eTable 1 in the Supplement. For brevity, we combined smaller service categories, specifically drug categories encompassing less than 1.3% of prior authorization drug spending and nondrug service categories consisting of less than 0.05% of total prior authorization spending. We calculated the proportion of prior authorization services and the proportion of prior authorization spending in each clinical category, with 95% CIs obtained via bootstrapping with resampling at the beneficiary level. For more detailed classification of prior authorization services, we also tabulated HCPCS-level service counts and associated spending.
To characterize prior authorization across clinician specialties, we calculated, by physician specialty, the annual likelihood of a clinician performing 1 or more prior authorization services. Our clinician sample included clinicians listed as performing providers or attending providers in covered Carrier or Outpatient claims. We assigned clinician specialty based on the modal specialty code listed in claims for each National Provider Identifier (NPI) during the study period, with ties broken by temporal recency. We excluded clinicians with specialty codes denoting institutions or nonphysician clinicians. For brevity, our main analysis excludes clinician specialties in pediatrics or other categories encompassing less than 0.5% of remaining clinicians, resulting in a sample of 641 928 clinicians. In a supplemental analysis (eTable 2 in the Supplement), we include all specialties containing more than 0.01% of clinicians.
Results
Among 6 497 534 Medicare beneficiaries (mean [SD] age, 72.1 [12.1] years), we detected 14 128 272 instances of services that would qualify for prior authorization in Medicare Advantage, corresponding to 2.174 services per beneficiary per year (95% CI, 2.168-2.181); 41.24% of beneficiaries received at least 1 of these services (95% CI, 41.20%-41.28%). Spending associated with these services totaled $10.8 billion, corresponding to $1661 per beneficiary per year (95% CI, $1654-$1668), or 24.8% of total annual Part B spending. Medicare payments accounted for 72% of the associated spending, while beneficiary cost sharing accounted for 20% and other insurers accounted for 9%. The majority of prior authorization services occurred in an outpatient hospital setting (59%), with most of the remainder in an office setting (34%). Table 1 illustrates characteristics of the beneficiary sample overall and stratified by receipt of prior authorization services. Among those receiving at least 1 prior authorization service, the mean number (SD) of such services was 5.3 (13.3) per beneficiary per year, corresponding to $4027 in spending per beneficiary per year.
Table 1. Sample Characteristics.
| Characteristic | Beneficiaries | ||
|---|---|---|---|
| All (n = 6 497 534) | Without prior authorization services (n = 3 818 074) | With prior authorization services (n = 2 679 460) | |
| Age, mean (SD), y | 72.1 (12.1) | 71.7 (12.8) | 72.6 (10.9) |
| Sex, % | |||
| Male | 45.1 | 46.0 | 43.8 |
| Female | 54.9 | 54.0 | 56.2 |
| Race/ethnicity, % | |||
| White | 82.6 | 81.4 | 84.4 |
| Black | 9.4 | 9.9 | 8.6 |
| Asian | 2.0 | 2.3 | 1.7 |
| Hispanic | 2.1 | 2.3 | 1.8 |
| Native American | 0.6 | 0.6 | 0.5 |
| Othera | 1.6 | 1.8 | 1.4 |
| Unknown | 1.6 | 1.8 | 1.4 |
| Medicaid dual eligibility, % | 21.1 | 22.2 | 19.4 |
| Disability as original Medicare eligibility, % | 23.9 | 23.9 | 23.8 |
| Census region, % | |||
| Northeast | 18.2 | 17.8 | 18.6 |
| Midwest | 22.6 | 23.2 | 21.7 |
| South | 39.5 | 38.4 | 40.9 |
| West | 19.4 | 20.0 | 18.5 |
| Other | 0.4 | 0.5 | 0.2 |
| No. of chronic conditions, mean (SD) | 5.9 (4.0) | 5.1 (4.0) | 7.0 (3.8) |
| Annual Part B spending, mean (SD), $ | 6685 (13 728) | 2834 (6678) | 12 172 (18 500) |
| No. of prior authorization services, mean (SD) | 2.2 (8.9) | 5.3 (13.3) | |
| Spending on prior authorization services, mean (SD), $ | 1661 (8900) | 4027 (13 512) | |
As defined according to Medicare administrative enrollment files.
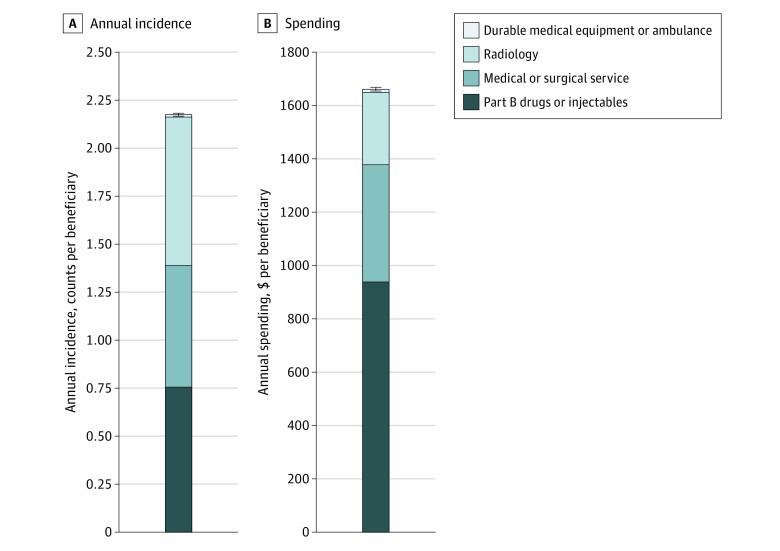
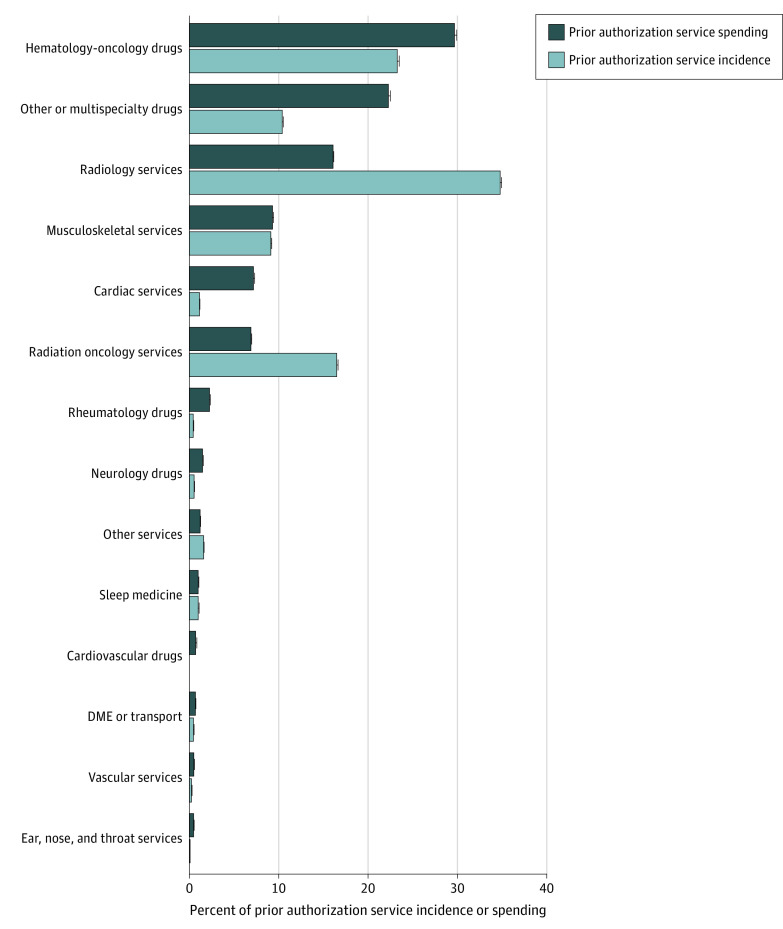
The majority of spending on prior authorization services was for Part B drugs/injectables (Figure 1). These accounted for 35% of prior authorization services and 57% of associated spending. Figure 2 shows the distribution of prior authorization services and their associated spending across clinical categories. Hematology or oncology drugs and multispecialty or other drugs accounted for the greatest share of spending (30% and 22%, respectively). The most common and expensive nondrug services were radiology services and musculoskeletal services, which constituted 37% and 21% of nondrug spending, respectively. Musculoskeletal services include laminectomy or laminotomy, spinal fusion, and dorsal column neurostimulation. Table 2 presents the 10 prior authorization services with the largest associated spending. These 10 services, 8 of which are injectable drugs, accounted for 36% of all spending on prior authorization services. eTable 1 in the Supplement presents the incidence and associated spending for each of the 918 different services that we detected, as well as the range of projected savings estimates. Savings estimates incorporated rejection rates calculated based on HCPCS-level rejection rates for Aetna plans; the mean rejection rate across HCPCS codes was 4.2% when weighted by HCPCS-level spending in fee-for-service Medicare.
Figure 1. Annual Incidence (A) and Spending (B) for Prior Authorization Services.
Prior authorization services include all services covered by fee-for-service Medicare Part B that would have been subject to prior authorization in Medicare Advantage. Count refers to the number of unique incidences of service provision. Error bars indicate 95% CIs.
Figure 2. Shares of Incidence and Spending for Prior Authorization Services, by Service Type.
Count refers to the number of unique incidences of service provision. See the eAppendix in the Supplement for all service category assignments. “Other services” consists of nondrug services contributing to less than 0.05% of prior authorization spending, including nondrug services in dermatology, gastroenterology, hematology or oncology, laboratory medicine, obstetrics or gynecology, ophthalmology, pulmonology, and urology. Error bars indicate 95% CIs. DME indicates durable medical equipment.
Table 2. Prior Authorization Services With the Greatest Spending.
| Spending ranka | Service | Annual spending, $/beneficiary | Annual incidence, count/100 beneficiaries |
|---|---|---|---|
| 1 | Epoetin beta | 136 | 4.3 |
| 2 | Epoetin alfa | 86 | 31.3 |
| 3 | Aflibercept | 76 | 3.5 |
| 4 | Rituximab | 54 | 0.8 |
| 5 | Nivolumab | 45 | 0.7 |
| 6 | Echocardiography, transthoracic, complete with doppler | 44 | 14.4 |
| 7 | Pegfilgrastim | 43 | 1.0 |
| 8 | Infliximab | 42 | 1.0 |
| 9 | Denosumab | 39 | 3.0 |
| 10 | MPI SPECT, multiple studies | 39 | 5.3 |
Abbreviation: MPI SPECT, myocardial perfusion imaging single-photon emission computed tomography.
Each row corresponds to a single procedure code.
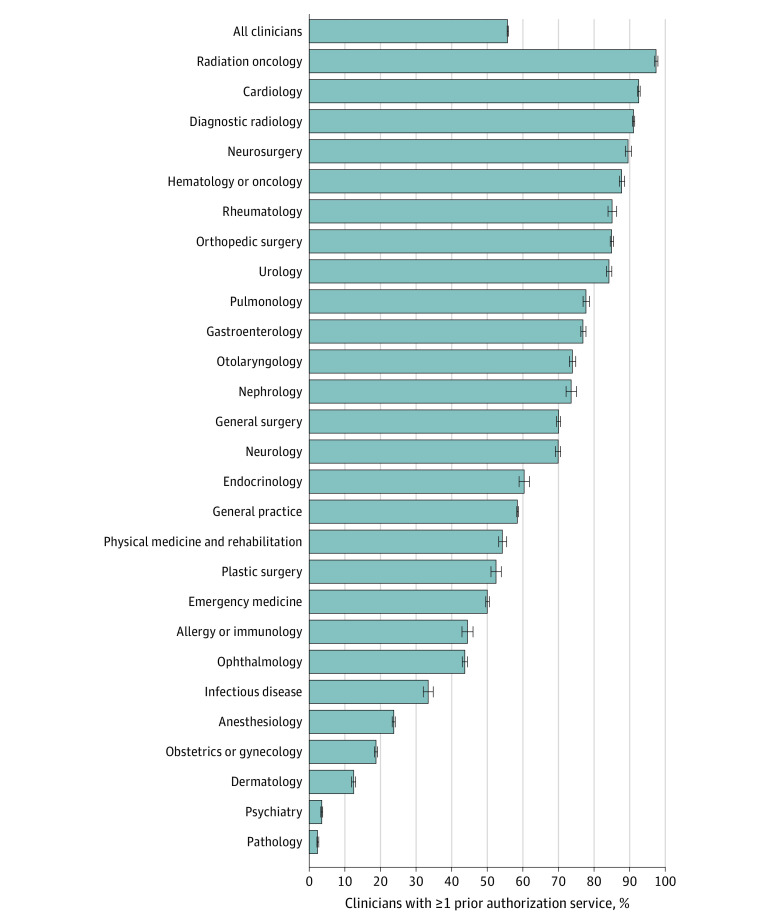
Figure 3 presents the annual risk of encountering prior authorization by clinician specialty. On average, 55.7% (95% CI, 55.6%-55.9%) of clinicians performed 1 or more prior authorization service per year for our sampled Medicare beneficiaries. This percentage, however, varied widely across clinician specialties. The highest rates were observed in radiation oncology (97%), cardiology (93%), diagnostic radiology (91%), neurosurgery (90%), hematology or oncology (88%), and rheumatology (85%). The lowest rates were observed in pathology (2%), psychiatry (4%), and dermatology (12%).
Figure 3. Clinician Annual Risk of Prior Authorization, by Specialty.
General practice includes clinicians in family practice, internal medicine, and hospital medicine. Error bars indicate 95% CIs.
Discussion
Although prior authorization has long been a part of managed care in the United States, there are no recent estimates of either how often or which medical services fall under prior authorization policies. In this national cross-sectional study, fee-for-service Medicare beneficiaries commonly received Part B services that would be subject to prior authorization in Medicare Advantage. These services contributed to a large amount of health care spending, encompassing 1 in 4 dollars covered by fee-for-service Medicare Part B. Our results suggest that prior authorization is widespread as a managed care strategy used within private health insurance. These findings also indicate that fee-for-service Medicare and private insurers differ substantially in this aspect of coverage design.
Our findings add to previous research showing differences in the processing of physician claims between fee-for-service Medicare and Medicare Advantage.17 Our work differs because it focused on clinical coverage criteria applied before services occur, rather than all-inclusive challenges to reimbursement after a service is rendered. Also, our study design allowed us to detect services that would not appear in submitted claims because coverage restrictions deterred claim submission. Our results are consistent with prior findings that Medicare Advantage reduces health care spending relative to fee-for-service Medicare by reducing health care use.18,19,20,21 Given the large proportion of spending subject to prior authorization, it is possible that prior authorization produces substantial savings, although the magnitude of savings remains uncertain (eAppendix and eFigure in the Supplement).
Our finding of extensive Medicare spending on services that insurers may not view as appropriate is also consistent with recent studies on the prevalence of suspected low-value medical services in fee-for-service Medicare.22,23,24 For prior authorization and other coverage policies, Medicare Advantage insurers cover services under a “reasonable and necessary” legal standard, whereas low-value services lack a uniform definition or legal standard. We did not quantify the number of low-value services among the services we detected. However, had we found very few services that private insurers would subject to the scrutiny of prior authorization, this result would have undermined the hypothesis that there are many identifiable unnecessary health care services in fee-for-service Medicare.
The spending associated with prior authorization services was concentrated in particular clinical domains. Accordingly, prior authorization services varied substantially across clinician specialty, suggesting an uneven administrative burden for different specialties and institutions. Prior authorization service spending was concentrated in Part B drugs (typically, injectable drugs), particularly hematology and oncology drugs. Insurers’ targeting of such drugs may reflect their high prices and frequency of off-label use.25 Developing and applying appropriateness criteria may also be more complex for nondrug services. Although assigning appropriateness criteria to imaging studies proved challenging in a recent Medicare demonstration project,26 Aetna has broad prior authorization requirements for outpatient radiology.
Our work introduces a simple and generalizable method for evaluating the scope of coverage limitations for health care services. Applying coverage rules in a setting without such restrictions allows services to be observed even if they would be deterred and thus unobservable in settings where the restrictions are active. Future studies could compare the coverage policies of multiple insurers using a single patient population for benchmarking. This method could also be applied to managed care tools other than prior authorization, such as formulary restrictions. Quantifying the savings from coverage policies will require research designs that account for the effects of coverage denials and deterrence not only on restricted services but also on cascading spending from services complementary to restricted services,27 on offsetting spending from substitute services delivered instead of restricted services,28 and on administrative costs. These administrative costs may be exacerbated by a lack of standardization among prior authorization policies.
Limitations
Our study has several limitations. First, we do not address the scope of prior authorization for Part D prescription drugs, a topic of recent government and industry reports.11,29 Our focus on Part B services reflects the policy-relevant difference between fee-for-service Medicare and private insurers in prior authorization policies for nonprescription services. Furthermore, our research design, which requires a setting that lacks prior authorization, would not be feasible if studying prescription drugs because prescription prior authorization is ubiquitous across Part D.2,29,30 We also did not examine Aetna coverage policies for Part A services such as inpatient hospitalization and postacute care, for which Aetna has prior authorization and concurrent review restrictions.
Second, we studied a single insurer’s prior authorization rules, which may differ from those of other insurers. We expect, however, that Aetna’s coverage policies are generally representative of Medicare Advantage insurers given Aetna’s market share,16 insurers’ shared incentives to use prior authorization, and the public availability of competitors’ prior authorization policies.31 Nonetheless, because Aetna has modestly lower rates of challenging physician claims for any reason (ie, not only prior authorization),17 we may have underestimated the scope of prior authorization in Medicare Advantage if the rate of challenging claims is indicative of less prior authorization within Aetna than within other insurers.
Third, our data were not clinically nuanced enough to identify services that, by federal regulation,32 are exempt from prior authorization because they were delivered in emergent situations. Although such services do not require prospective prior authorization, they are subject to retrospective review by the insurer to confirm that they met criteria for emergency exemption.
Finally, fee-for-service Medicare was not entirely insulated from prior authorization policies during the study period. Private insurers’ prior authorization policies may have caused spillover effects in fee-for-service Medicare,33,34,35 which would have led us to underestimate the scope of these policies. In addition, prior authorization policies were not entirely absent from fee-for-service Medicare during the study period. However, the only 2 HCPCS codes requiring prior authorization nationally in fee-for-service Medicare were for 2 types of motorized wheelchairs,13 and they constituted only 0.1% of the spending we detected. The difference we observed between fee-for-service Medicare and Medicare Advantage in prior authorization policy is unlikely to narrow significantly following a recent expansion of prior authorization for fee-for-service Medicare, which applies to only 5 types of outpatient hospital services.14 A Medicare demonstration project introducing prior authorization for hyperbaric oxygen ended in 2018.36 Beyond its limited use of prior authorization, fee-for-service Medicare uses other forms of coverage limits, including local and national coverage determinations, which restrict payment for services based on medical necessity standards.13
Conclusions
In this cross-sectional study, a large portion of fee-for-service Medicare Part B spending would have been subject to prior authorization under private insurance coverage policies. Prior authorization and other forms of clinical coverage policy present opportunities and challenges for health insurers. Explicitly focusing on the clinical appropriateness of medical services can allow insurers to manage care with more clinical nuance than blunt cost-sharing tools or blanket restrictions on service coverage. However, the complexity of assessing the clinical appropriateness of a particular medical service involves distinct administrative and compliance costs. Our study illustrates how private insurers have faced this trade-off differently than fee-for-service Medicare by adopting a broad scope of prior authorization policies.
eAppendix. Methods
eReferences.
eTable 1. Service Codes, Category, Annual Spending and Annual Incidence
eTable 2. Clinician Annual Risk of PA Service, by Specialty
eFigure. Projected Savings From Prior Authorization in Fee-For-Service Medicare
References
- 1.Brook RH. Assessing the appropriateness of care—its time has come. JAMA. 2009;302(9):997-998. doi: 10.1001/jama.2009.1279 [DOI] [PubMed] [Google Scholar]
- 2.Medicare Payment Advisory Commission . Health Care Spending and the Medicare Program: A Data Book; 2019.
- 3.Resneck JS Jr. Refocusing medication prior authorization on its intended purpose. JAMA. 2020;323(8):703-704. doi: 10.1001/jama.2019.21428 [DOI] [PubMed] [Google Scholar]
- 4.American Hospital Association, America’s Health Insurance Plans, American Medical Association, American Pharmacists Association, BlueCross BlueShield Association, Medical Group Management Associa. Consensus Statement on Improving the Prior Authorization. Published online 2018. Accessed April 21, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/arc-public/prior-authorization-consensus-statement.pdf
- 5.Cutler DM. Reducing Administrative Costs in U.S. Health Care. The Hamilton Project. Accessed October 26, 2020. https://www.hamiltonproject.org/papers/reducing_administrative_costs_in_u.s_health_care
- 6.Smalley WE, Griffin MR, Fought RL, Sullivan L, Ray WA. Effect of a prior-authorization requirement on the use of nonsteroidal antiinflammatory drugs by Medicaid patients. N Engl J Med. 1995;332(24):1612-1617. doi: 10.1056/NEJM199506153322406 [DOI] [PubMed] [Google Scholar]
- 7.Fischer MA, Choudhry NK, Winkelmayer WC. Impact of Medicaid prior authorization on angiotensin-receptor blockers: can policy promote rational prescribing? Health Aff (Millwood). 2007;26(3):800-807. doi: 10.1377/hlthaff.26.3.800 [DOI] [PubMed] [Google Scholar]
- 8.Fischer MA, Schneeweiss S, Avorn J, Solomon DH. Medicaid prior-authorization programs and the use of cyclooxygenase-2 inhibitors. N Engl J Med. 2004;351(21):2187-2194. doi: 10.1056/NEJMsa042770 [DOI] [PubMed] [Google Scholar]
- 9.Dillender M. What happens when the insurer can say no? assessing prior authorization as a tool to prevent high-risk prescriptions and to lower costs. J Public Econ. 2018;165:170-200. doi: 10.1016/j.jpubeco.2018.07.006 [DOI] [Google Scholar]
- 10.Data documentation: Part D Event (PDE) file. Part D Drug Event Characteristics File.xlsx. Research Data Assitance Center. Accesed April 21, 2021. https://www.resdac.org/cms-data/files/pde/data-documentation
- 11.Office of the Inspector General; Murrin S. US Department of Health and Human Services. Some Medicare Part D beneficiaries face avoidable extra steps that can delay or prevent access to prescribed drugs. OEI-09-16-00411. Published September 2019. Accessed April 21, 2021. https://oig.hhs.gov/oei/reports/oei-09-16-00411.pdf
- 12.Jacobson G, Neuman T. Prior authorization in Medicare Advantage plans: how often is it used? KFF. Published October 24, 2018. Accessed October 9, 2020. https://www.kff.org/medicare/issue-brief/prior-authorization-in-medicare-advantage-plans-how-often-is-it-used/
- 13.Medicare Payment Advisory Commission . Medicare coverage policy and use of low-value care. In: Medicare and the Health Care Delivery System; 2018:293-363. Accessed April 21, 2021. http://www.medpac.gov/docs/default-source/reports/jun18_ch10_medpacreport_sec.pdf?sfvrsn=0
- 14.Centers for Medicare & Medicaid Services . CMS-1717-FC Notice of Final Rulemaking with Comment- Hospital Outpatient Prospective Payment; 2020. Accessed April 21, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices-Items/CMS-1717-FC
- 15.Jarrín OF, Nyandege AN, Grafova IB, Dong X, Lin H. Validity of race and ethnicity codes in Medicare administrative data compared with gold-standard self-reported race collected during routine home health care visits. Med Care. 2020;58(1):e1-e8. doi: 10.1097/MLR.0000000000001216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacobson G, Damico A, Neuman T. Medicare Advantage 2017 spotlight: enrollment market update. Published June 6, 2017. Accessed October 12, 2020. https://www.kff.org/medicare/issue-brief/medicare-advantage-2017-spotlight-enrollment-market-update/
- 17.Gottlieb JD, Shapiro AH, Dunn A. The complexity of billing and paying for physician care. Health Aff (Millwood). 2018;37(4):619-626. doi: 10.1377/hlthaff.2017.1325 [DOI] [PubMed] [Google Scholar]
- 18.Curto V, Einav L, Finkelstein A, Levin J, Bhattacharya J. Health care spending and utilization in public and private medicare. Am Econ J Appl Econ. 2019;11(2):302-332. doi: 10.1257/app.20170295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP, Ayanian JZ. Analysis of Medicare Advantage HMOs compared with traditional Medicare shows lower use of many services during 2003-09. Health Aff (Millwood). 2012;31(12):2609-2617. doi: 10.1377/hlthaff.2012.0179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duggan M, Gruber J, Vabson B. The consequences of health care privatization: evidence from medicare advantage exits. Am Econ J Econ Policy. 2018;10(1):153-186. doi: 10.1257/pol.20160068 [DOI] [Google Scholar]
- 21.Geruso M, Layton T. Upcoding: Evidence from Medicare on squishy risk adjustment. J Polit Econ. 2020;12(3):984-1026. doi: 10.1086/704756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174(7):1067-1076. doi: 10.1001/jamainternmed.2014.1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing wisely: prevalence and correlates of low-value health care services in the United States. J Gen Intern Med. 2015;30(2):221-228. doi: 10.1007/s11606-014-3070-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Segal JB, Bridges JFP, Chang HY, et al. Identifying possible indicators of systematic overuse of health care procedures with claims data. Med Care. 2014;52(2):157-163. doi: 10.1097/MLR.0000000000000052 [DOI] [PubMed] [Google Scholar]
- 25.Saiyed MM, Ong PS, Chew L. Off-label drug use in oncology: a systematic review of literature. J Clin Pharm Ther. 2017;42(3):251-258. doi: 10.1111/jcpt.12507 [DOI] [PubMed] [Google Scholar]
- 26.Timbie JW, Hussey PS, Burgette LF, et al. Medicare Imaging Demonstration final evaluation: report to congress. Rand Heal Q. 2015;5(1):4. [PMC free article] [PubMed] [Google Scholar]
- 27.Ganguli I, Lupo C, Mainor AJ, et al. Prevalence and cost of care cascades after low-value preoperative electrocardiogram for cataract surgery in fee-for-service Medicare beneficiaries. JAMA Intern Med. 2019;179(9):1211-1219. doi: 10.1001/jamainternmed.2019.1739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parikh RB, Fishman E, Chi W, et al. Association of utilization management policy with uptake of hypofractionated radiotherapy among patients with early-stage breast cancer. JAMA Oncol. 2020;6(6):839-846. doi: 10.1001/jamaoncol.2020.0449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dieguez G, Mirchandani H. Evolution of the use of restrictions in commercial formularies. Published November 3, 2016. Accessed October 18, 2020. https://www.milliman.com/en-GB/insight/evolution-of-the-use-of-restrictions-in-commercial-formularies
- 30.VA National Formulary. Pharmacy Benefits Management Services. Accessed October 19, 2020. https://www.pbm.va.gov/nationalformulary.asp
- 31.Precertification Lists. Search by CPT code Lookup. Aetna. Accessed October 18, 2020. https://www.aetna.com/health-care-professionals/precertification/precertification-lists.html
- 32.42 CFR § 422.113 (b) (2); 2020.
- 33.Baicker K, Chernew ME, Robbins JA. The spillover effects of Medicare managed care: Medicare Advantage and hospital utilization. J Health Econ. 2013;32(6):1289-1300. doi: 10.1016/j.jhealeco.2013.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Callison K. Medicare managed care spillovers and treatment intensity. Health Econ. 2016;25(7):873-887. doi: 10.1002/hec.3191 [DOI] [PubMed] [Google Scholar]
- 35.Feyman Y, Pizer SD, Frakt AB. The persistence of Medicare Advantage spillovers in the post–Affordable Care Act era. Health Econ. 2021;30(2):311-327. doi: 10.1002/hec.4199 [DOI] [PubMed] [Google Scholar]
- 36.Asher A, Contreary K, Coopersmith J, Haile G, Chen T. Evaluation of the Medicare Prior Authorization Model for Non-Emergent Hyperbaric Oxygen (HBO): Final Report. Publication HHSM-500-2014-00034. Published May 2019. Accessed April 21, 2021. https://innovation.cms.gov/files/reports/mpa-hbo-fnlevalrpt.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Methods
eReferences.
eTable 1. Service Codes, Category, Annual Spending and Annual Incidence
eTable 2. Clinician Annual Risk of PA Service, by Specialty
eFigure. Projected Savings From Prior Authorization in Fee-For-Service Medicare