Abstract
Despite remarkable progress in the reduction of under-five mortality, the rate of perinatal and neonatal mortality is still high especially in developing countries. The adverse outcome associated with preterm birth is one of the major public health challenges in Africa. However, there are limited and inconsistent studies conducted on the effect of preterm birth on adverse perinatal and neonatal outcomes in Ethiopia. Therefore, this systematic review and meta-analysis aimed to investigate the association between preterm birth and its adverse perinatal and neonatal outcomes in Ethiopia. We systematically searched several electronic databases like PubMed, Web of Science, SCOPUS, CINAHL, Google Scholar, African Journals Online databases and Science Direct. All identified observational studies were included. The I 1 statistics were used to assess the heterogeneity among the studies. A random-effects model was computed to estimate the pooled effect of preterm birth on adverse perinatal and neonatal outcomes. Thirty-three studies with a total of 20 109 live births were included in the final meta-analysis. Our meta-analysis showed that preterm birth increased the odds of perinatal mortality by 10-folds [POR = 9.56 (95% CI: 5.47, 19.69)] and there was a 5.44-folds risk of stillbirth [Odds Ratio = 5.44 (95% CI: 3.57, 8.28)] among women who gave birth before 37 weeks of gestation. In addition, preterm birth was significantly associated with neonatal hypothermia [OR=3.54 (95% CI: 2.41, 5.21)], neonatal mortality [OR= 3.16 (95% CI: 1.57, 6.34). The sub-group analysis of this meta-analysis showed that there was an increased risk of neonatal sepsis [OR=2.33 (95% CI: 1.15, 4.71)] among preterm babies. Preterm births significantly increased the risk of adverse perinatal and neonatal outcomes in Ethiopia. Therefore, scale-up strategies and improving the quality of maternal and child health care providers should be an area of intervention to reduce adverse outcomes associated with preterm birth. The Federal Ministry of Health and concerned bodies should work towards the prevention of preterm birth and its adverse outcomes.
Keywords: perinatal mortality, adverse outcomes, preterm birth, meta-analysis, Ethiopia
Background
In 2015, 2.8 million (44%) of the 6.3 million deaths in under-five children during the neonatal period and 4.5 million perinatal deaths (2.1 million stillbirths and 2.4 million early neonatal deaths) occurred globally. 2 Preterm birth is the leading cause of neonatal morbidity and mortality. It is the largest single condition in the Global Burden of Disease due to the high mortality and the risk of lifelong impairment among survivors.1,3 Preterm birth is the single leading direct cause of neonatal deaths resulting in 35% of the world’s deaths annually, cause of under-5 deaths and child death in all high- and middle-income countries.3,4 Neonatal and perinatal death associated with preterm birth is an important public health challenge across a range of countries mainly in Sub-Saharan Africa (SSA).5,6 It also imposes an economic burden on the health system due to the most common cause of readmission7–9 and increased length of hospital stay. 10
Preterm birth causes severe neonatal morbidity including the need for assisted ventilation (45.7%),10,11 respiratory distress, 12 sepsis, 10 need for phototherapy and newborn’s morbidity rate doubled in infants for each gestational week earlier than 38 weeks. 13 Premature birth was also associated with mortality during infancy10,14–16 and adulthood.15,17 Additionally, preterm birth affects the likelihood of parenthood; the decreased likelihood of parenthood,18,19 decrease romantic partnership and sexual life of partners.19,20 Preterm birth also increases the risk of malnutrition; underweight or wasted, more often screened positively for disability and neonatal mortality. 21
Different interventions were done in the perinatal and neonatal periods to reduce adverse perinatal and neonatal outcomes of preterm birth. 22 The Global strategy plans to reduce stillbirth at least 25 per 1000 live births and neonatal mortality at least 12 per 1000 live births in every country by 2030. The rate of morbidity and mortality associated with preterm birth was higher and varies in Ethiopia.23–28 There is growing national attention focused on neonatal mortality. Though, adverse perinatal and neonatal outcomes attributed to preterm birth remains high in Ethiopia. There are different studies conducted in Ethiopia on predictors of adverse perinatal and neonatal outcomes. Evidence on the effect of preterm birth on adverse outcomes is inconsistent and inconclusive for national-level health policy and managers across available epidemiologic studies. Unfortunately, there is no pooled study on the effect preterm birth on perinatal mortality, neonatal hypothermia and neonatal sepsis. Therefore, this systematic review and meta-analysis were conducted to estimate the effect of preterm birth on adverse perinatal and neonatal outcomes in Ethiopia.
Methods
Reporting of Systematic Review, Data Sources and Search Strategies
The findings of this systematic review and meta-analysis are reported based on the recommendation of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2009 statement checklist 29 (SupplementaryTable1). All published articles were searched from major international databases like PubMed, Web of Science, SCOPUS, CINAHL, Google Scholar, Science Direct, African Journals Online databases and Google hand searches. Additionally, a search was made for the reference list of studies already identified to retrieve additional articles.
For each of the selected components of adverse outcomes, electronic databases were searched using keyword search and the Medical Subject Heading [MeSH] words. The keywords include adverse perinatal or neonatal outcomes, perinatal mortality, stillbirth, sepsis, hypothermia OR neonatal mortality as well as Ethiopia. The search terms were combined by the Boolean operators ‘OR’ and ‘AND’.
Population and Outcomes of the Study
The population of interest was all live births from 28 weeks of gestation to 7 days of postpartum period for perinatal outcomes and the first 28 days for neonatal outcomes respectively in Ethiopia. The exposure was preterm birth. Comparisons were defined for each perinatal and neonatal outcome of preterm delivery for each outcome.
The outcome lists were adverse perinatal and neonatal outcomes of preterm birth. The adverse perinatal outcomes included were perinatal mortality and stillbirth. However, neonatal sepsis, hypothermia and neonatal mortality were adverse neonatal outcomes.
Eligibility Criteria and Study Selection
This review included studies that reported adverse outcomes, which included perinatal mortality, neonatal sepsis, hypothermia and neonatal mortality. All studies published from inception to the end of our search, July 27, 2020 published in the English language were retrieved to assess eligibility for inclusion. Case reports of populations, abstracts of conferences, articles without full access and not reported outcomes of interest were excluded. The article selection process passed through different steps. Retrieved articles were screened using their title, abstract and full article review. Study screening and full review of the studies were conducted by two reviewers (MD and GMK). Any disagreement between the two reviewers regarding the selection and inclusion of the studies was resolved by consensus. There was then a full-text analysis of the studies that passed abstract review and whether or not the specified set of criteria had been met and for duplicated records.
Quality Assessment and Data Abstraction
The Newcastle-Ottawa Scale quality assessment tool was used to assess the quality of the included studies based on the 3 components; the selection of the study groups, comparability of the study groups and ascertainment of exposure or outcome. 30 The NOS has 3 categorical criteria with a maximum score of 9 points. The first component emphasized the methodological quality of primary studies, the second component was concerned with the comparability and the third component was used to evaluate the results and statistical analysis of each study. The quality of each study was assessed using the following scoring algorithm: ≥7 points were considered as ‘good’, 4 to 6 points were considered as ‘moderate’, and ≤3 points was considered as ‘poor’ quality studies. Additionally, to improve the validity of the results of this systematic review, only primary studies of fair to good quality were included in the final meta-analysis. Two reviewers (MD and NBY) independently assessed the quality and extracted data from these articles using a standardized data extraction format. The data extraction format included primary author, year of publication, geographic region of the study, sample size, the reported number of cases (live birth who develop the respective outcomes).
Publication Bias and Statistical Analysis
The publication bias was assessed using Egger’s 31 and Begg’s 32 tests with a P-value of less than .05. The I 1 test statistic was used to assess heterogeneity between studies and a P-value of less than .05 was used to declare heterogeneity. Due to the presence of heterogeneity among studies, a random-effects method of the meta-analysis was utilized to estimate the pooled effect based on the metan software of the double arcsine transformations. 33,34 Data were extracted in Microsoft Excel and exported to Stata version 11 for analysis. Sub-group analysis was conducted by study design. The effect of selected adverse outcomes was analysed using separate categories of meta-analysis. 34 The findings of the meta-analysis were presented using forest plots and Odds Ratio (OR) with its 95% Confidence intervals (CIs). In addition, we conducted a sensitivity analysis to assess whether the pooled estimates were influenced by individual studies.
Results
Study Identification and Characteristics of Studies
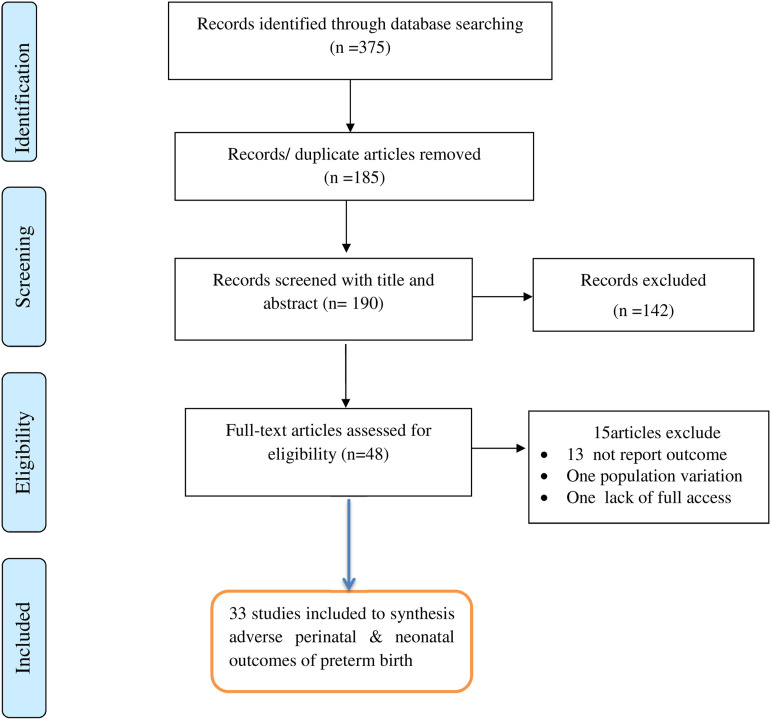
This systematic review and meta-analysis included published studies on the pooled effect of preterm birth on adverse perinatal and neonatal outcomes in Ethiopia using published studies. A total of 375 studies were found from the review. Of these, 185 duplicated records were deleted and 142 articles were excluded by the screening of titles and abstracts. Subsequently, a total of 48 full-text papers were assessed for eligibility based on the inclusion and exclusion criteria. Thus, thirteen studies were excluded due to lack of the outcome of interest,22,35–46 population difference 47 and 1 article was excluded due to lack of access to the full text. 48 Finally, a total of 33 studies were included in the final quantitative meta-analysis (Figure 1).
Figure 1.
PRISMA flow diagram of the studies in the systematic review and meta-analysis.
The review was conducted among 20 109 live births delivered after 28 weeks of gestation to estimate the pooled effect of preterm birth on adverse outcomes. Of those, 8 studies reported perinatal mortality,24,25,49–52 3 studies53–55 reported stillbirth, 9 studies27,56–63 reported neonatal sepsis, 4 studies26,64–66 were on neonatal hypothermia and 8 studies28,67–74 reported neonatal mortality. Regarding the design of the included studies, sixteen (48.5%) were cross-sectional studies,26,49,51,53,56,58,60,64,66,68,72–74 8 (24.2%) studies were case-control24,25,50,52,54,59,60,65 and 7 (21.2%)were cohort studies.28,55,67,69,71,73 The articles were published between 2014 and 2020. To estimate neonatal mortality, the largest sample size was 3463 live births in a prospective follow-up study conducted in Oromia region 73 followed by 1770 sample size in a study conducted in Tigray. 72 However, the smallest sample size was 219 from a study conducted in Oromia region 25 and 249 from a case-control study in Tigray region. 59 Seven geographic regions of Ethiopia were represented in the current review. Of which, 7 (21.2%) studies were from the Amhara region, 9 (27.3%) were from the Tigray region, 4 (12.1%) were from Southern Nations, Nationalities and Peoples Region (SNNPR), 6 (18.2%) were from Oromia, 4 (12.1%) were from Addis Ababa, 2 from Harar region and the remaining 1 study was represented from Somali region (Table 1). The included studies had fair to good quality scores based on the NOS assessment tool, with a maximum of 9 scores and the minimum was with a score of 5 (Supplementaryfile 2).
Table 1.
Characteristics of included studies on the effect of preterm birth adverse outcomes.
|
Author |
Year | Region | Design | Reported Outcomes | Number of Cases with the Outcome | Sample | |||
|---|---|---|---|---|---|---|---|---|---|
| a | b | C | day | ||||||
| Roro BM et al 25 | 2018 | Oromia | Case-c | Perinatal mortality | 11 | 7 | 62 | 139 | 219 |
| Yirgu R et al 24 | 2016 | Amhara | Case-c | Perinatal mortality | 14 | 2 | 88 | 202 | 306 |
| Aragaw YH 49 | 2016 | Oromia | Cross-s | Perinatal mortality | 23 | 14 | 59 | 925 | 1025 |
| Tesfaye H | 2019 | AA | Case-c | Perinatal mortality | 110 | 89 | 164 | 458 | 821 |
| Getiye and Fentahun 50 | 2017 | AA | Case-c | Perinatal mortality | 139 | 59 | 211 | 655 | 1064 |
| Tilahun S et al 51 | 2008 | AA | Cross-s | Perinatal mortality | 35 | 8 | 41 | 179 | 263 |
| Goba GK et al 52 | 2018 | Tigray | Case-c | Perinatal mortality | 37 | 9 | 89 | 243 | 378 |
| Mihiretu A et al | 2017 | SNNPR | Cross-s | Perinatal mortality | 18 | 10 | 34 | 248 | 310 |
| Berhe T et al 53 | 2019 | Tigray | Cross-s | Stillbirth | 10 | 62 | 14 | 487 | 570 |
| Tasew H et al 54 | 2019 | Tigray | Cross-s | Stillbirth | 40 | 68 | 23 | 184 | 315 |
| GSlasie KZ et al 55 | 2020 | Tigray | Cohort | Stillbirth | 10 | 60 | 13 | 564 | 648 |
| Geyesus T et al 56 | 2017 | Amhara | Cross-s | Neonatal sepsis | 65 | 27 | 42 | 101 | 251 |
| Getabelew A et al 58 | 2018 | Oromia | Cross-s | Neonatal sepsis | 46 | 23 | 148 | 31 | 244 |
| Woldu MA et al 57 | 2014 | Oromia | Cross-s | Neonatal sepsis | 39 | 25 | 178 | 50 | 306 |
| Gebremedhin D et al 59 | 2016 | Tigray | Case-c | Neonatal sepsis | 29 | 37 | 52 | 112 | 234 |
| Ketema E et al 60 | 2019 | SNNPR | Case-c | Neonatal sepsis | 40 | 58 | 72 | 165 | 335 |
| Sorsa A et al 61 | 2019 | Oromia | Cross-s | Neonatal sepsis | 30 | 49 | 68 | 170 | 317 |
| Alemu M et al 27 | 2019 | Amhara | Case-c | Neonatal sepsis | 50 | 40 | 32 | 124 | 246 |
| Mustafa A et al 62 | 2020 | SNNPR | Cross-s | Neonatal sepsis | 89 | 52 | 186 | 24 | 351 |
| Weldu Y et al 63 | 2020 | Tigray | Cross-s | Neonatal sepsis | 54 | 74 | 62 | 127 | 317 |
| Bayih WA et al 26 | 2019 | Harar | Cross-s | N. hypothermia | 86 | 13 | 181 | 123 | 403 |
| Tasew H et al 65 | 2018 | Tigray | Case-c | N. hypothermia | 27 | 20 | 61 | 156 | 264 |
| Seyum and Ebrahim 66 | 2015 | Amhara | Cross-s | N. hypothermia | 49 | 9 | 245 | 118 | 421 |
| Demissie BW et al 64 | 2018 | AA | Cross-s | N. hypothermia | 155 | 47 | 73 | 81 | 356 |
| Kokeb and Desta 68 | 2016 | Amhara | Cross-s | Neonatal mortality | 36 | 49 | 36 | 186 | 307 |
| Demisse AG et al 74 | 2017 | Amhara | Cross-s | Neonatal mortality | 49 | 201 | 48 | 408 | 706 |
| Debelew GT et al 73 | 2014 | Oromia | Cohort | Neonatal mortality | 20 | 323 | 90 | 3030 | 3463 |
| Farah AE et al 70 | 2018 | Somali | Cohort | Neonatal mortality | 14 | 143 | 31 | 604 | 792 |
| Orsido TT et al 67 | 2019 | SNNPR | Cohort | Neonatal mortality | 84 | 128 | 77 | 677 | 966 |
| Mengesha HG et al 28 | 2016 | Tigray | Cohort | Neonatal mortality | 42 | 51 | 26 | 1033 | 1152 |
| Desalew A et al 69 | 2020 | Harar | Cohort | Neonatal mortality | 82 | 78 | 233 | 96 | 489 |
| Hadgu FB et al 72 | 2020 | Tigray | Cross-s | Neonatal mortality | 139 | 292 | 150 | 1190 | 1770 |
| Gudayu TW et al 71 | 2020 | Amhara | Cohort | Neonatal mortality | 57 | 150 | 30 | 267 | 504 |
Impact of Preterm Birth on Adverse Perinatal Outcomes
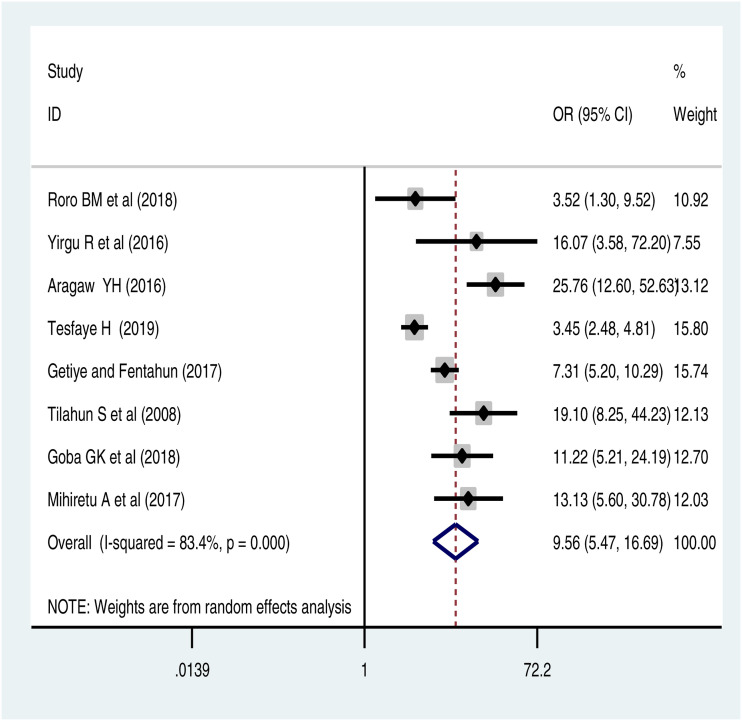
The pooled random effect analysis of 8 studies showed that neonates born preterm were 10 times [POR = 9.56 (95%CI: 5.47, 19.69)] more likely to die in the perinatal period than babies born after 37 weeks of gestation. The heterogeneity test showed very high variability among the included studies (I1= 83.4% at P-value < .0001). To account for the high heterogeneity, a random effect meta-analysis was used (Figure 2). However, there was no publication bias based on Egger’s and Begg’s tests. It was supported by Funnel plot (Supplementary file 3). The sub-group analysis also showed that the minimum highest odds of perinatal mortality among preterm neonates were reported in a case-control study design than cross-sectional. Interestingly, both study designs have a nearly comparable significant association between preterm birth and perinatal mortality (Table 2).
Figure 2.
Forest pot of association of preterm birth and perinatal mortality: meta-analysis.
Table 2.
Sub-group analysis of the impact of preterm birth on adverse outcomes by study design.
| Outcomes | Design | Included Studies, n | POR [95%CI] | I 1 , % | P-value |
|---|---|---|---|---|---|
| Perinatal mortality | Case control | 5 | 9.44 (3.64, 24.4) | 89.6 | <.0001 |
| Cross-sectional | 3 | 8.09 (5.96, 10.9) | 0 | 0.4 | |
| Neonatal sepsis | Case control | 3 | 2.33 (1.15, 4.71) | 79.8 | .05 |
| Cross-sectional | 5 | .9 (.36, 2.29) | 94.1 | <.0001 | |
| Neonatal mortality | Cohort | 6 | 3.20 (1.01, 10.1) | 97.2 | <.0001 |
| Cross-sectional | 3 | 3.12 (2.10, 4.64) | 65 | <.005 |
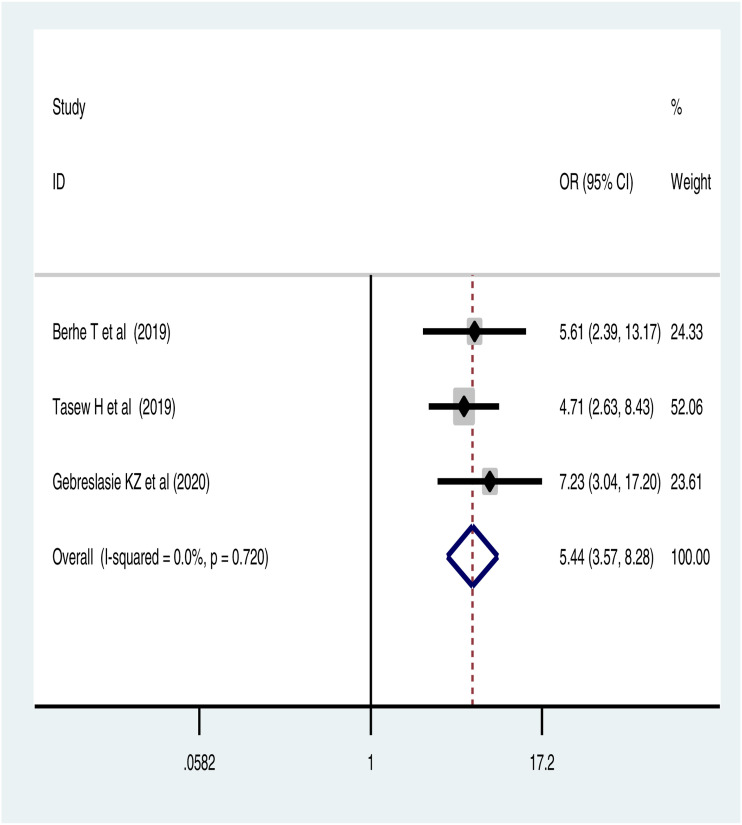
The pooled effect of 3 studies showed that the odds of stillbirth was 5.44 [POR=5.44 (95%CI: 3.57, 8.28)] times higher among preterm live births than their counterparts. The fixed-effects model was used due to the absence of a significant source of heterogeneity (I1=0%, at P-value = .72) (Figure 3).
Figure 3.
Forest pot of association of preterm birth and stillbirth in Ethiopia: meta-analysis.
Impact of Preterm Birth on Adverse Neonatal Outcomes
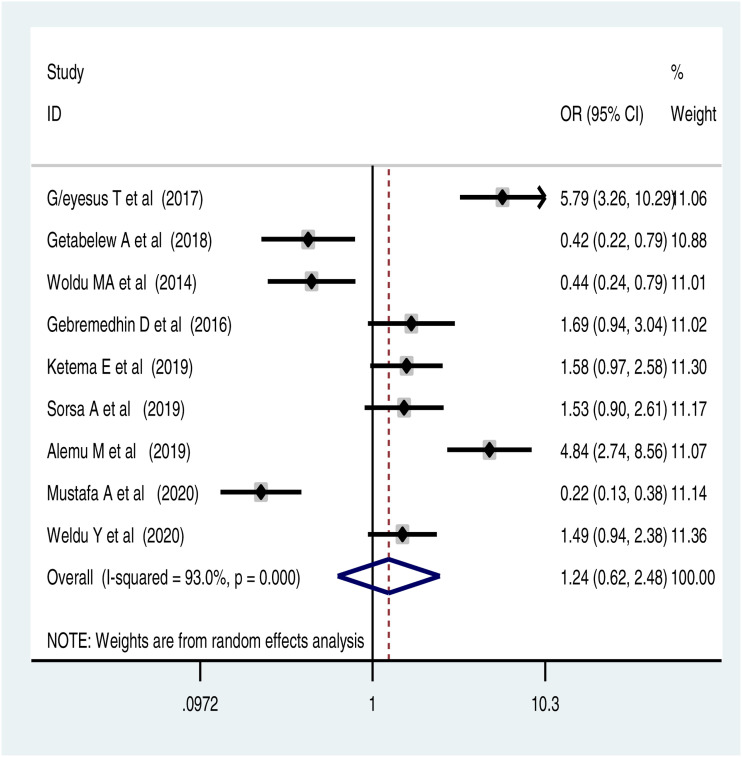
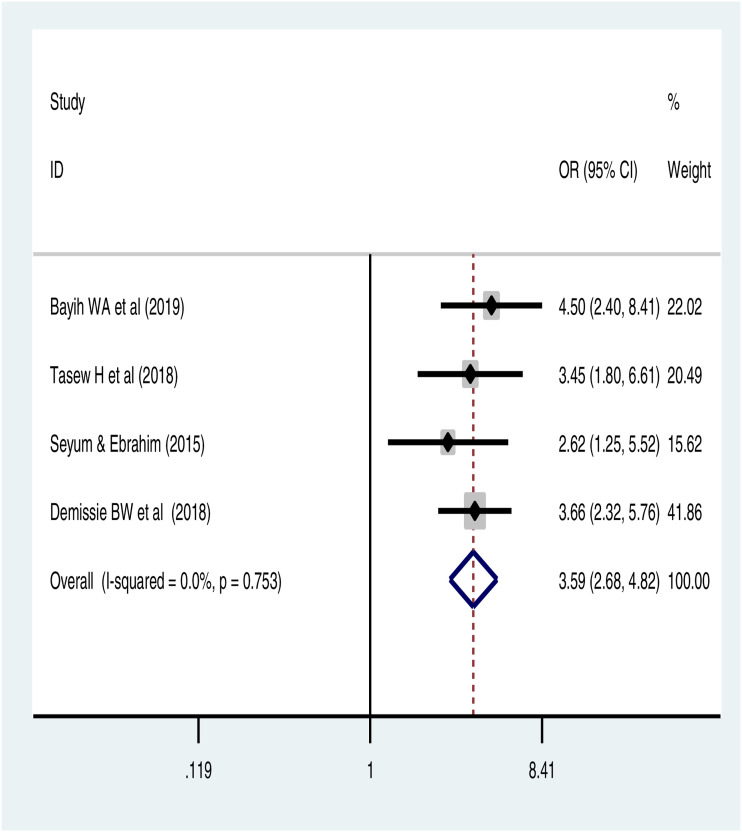
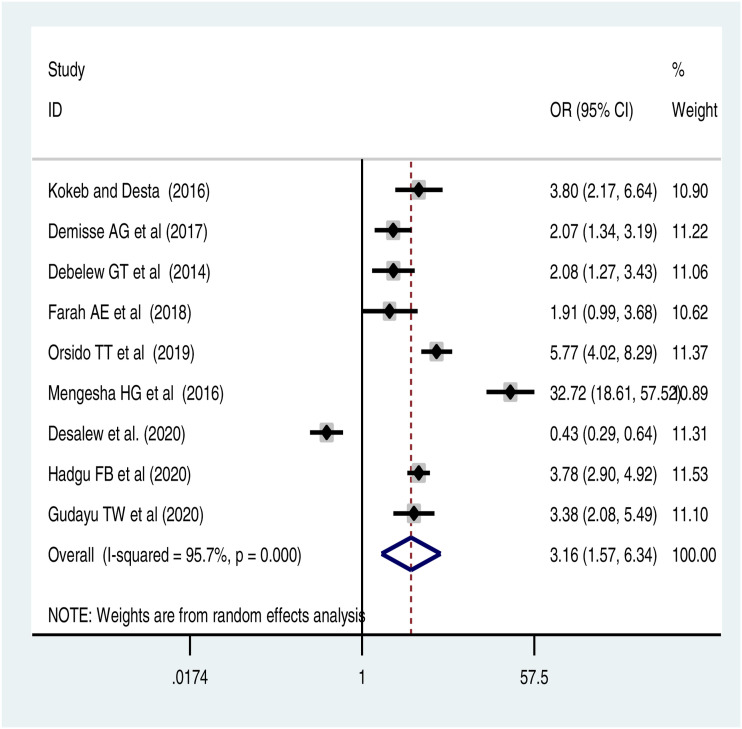
The pooled effect of this meta-analysis also showed that preterm birth was significantly associated with neonatal hypothermia and neonatal mortality. This meta-analysis also indicated that there was no significant association between preterm birth and neonatal sepsis (Figure 4). There was no publication bias (Supplementary file 4). The pooled effect of 4 studies revealed that preterm babies had 3.54 times higher odds of neonatal hypothermia than those delivered after 37 weeks of gestational age [POR = 3.54 (95% CI: 2.41, 5.21)]. The fixed-effects model of analysis was used due to the absence of a significant source of heterogeneity (I 1 = 0%, at P-value = .55) (Figure 5). There was no significant publication bias based on the Eggers test and funnel plot (Supplementary 5). Moreover, this meta-analysis found that preterm babies had 3 times higher odds of dying in the neonatal period than babies born after 37 weeks of gestation [POR = 3.16 (95% CI: 1.57, 6.34). There was a significant source of heterogeneity, and therefore, a random effect model was used (Figure 6). There was no publication bias based on the Eggers test and Funnel plot (supplementaryfile 6).
Figure 4.
Forest pot of association of preterm birth and neonatal sepsis: meta-analysis.
Figure 5.
Pooled odds ratio of association of preterm birth and neonatal hypothermia.
Figure 6.
Forest plot of the impact of preterm birth on neonatal mortality: meta-analysis.
The sub-group analysis based on study design on the role of preterm birth on neonatal sepsis and neonatal mortality was investigated. The pooled effect of 3 case-control studies showed that preterm birth significantly increased the risk of neonatal sepsis by 2-folds [OR=2.33 (95%CI: 1.15, 4.71)] and neonatal mortality was significantly associated with preterm birth based on the sub-group analysis of 6 cohort studies [OR = 3.20 (95% CI: 1.01, 10.1)] and 3 cross-sectional studies [OR = 3.12 (95% CI: 2.10, 4.64)] (Table 2).
Discussion
This systematic review and meta-analysis estimated the association between preterm birth and adverse perinatal and neonatal outcomes using studies conducted in Ethiopia. The current review underscored the significant association between preterm birth and adverse birth outcomes in Ethiopia. The findings of this study showed that the odds of perinatal mortality were higher among preterm babies than those with normal gestational age. This finding is in line with findings reported in Low and Middle-Income Countries (LMICs).75,76 This could be because those neonates born before 37 weeks of gestation might be more likely to have perinatal morbidities mainly due to the high burden of maternal near miss mainly hypertensive disorders and antepartum haemorrhage. Hence, hypertension disorders and antepartum haemorrhage are significantly associated with preterm birth and are known to decrease the feto-maternal perfusion that reduces blood supply to the foetus, asphyxiated and ultimately resulting in death in the perinatal period. This can be also explained because the health services delivery system and a health care system to improve the survival of preterm neonates is limited in the setting 77 including poor uptake of maternity waiting home in the health facility.78–80 Since a systematic review and meta-analysis were done in Africa revealed that maternity waiting for home utilization significantly reduced the risk of perinatal mortality.81,82
This study found that a significant higher odd of stillbirth among preterm babies. This may indicate the preterm newborns might be due to low birth weight and growth-restricted 83 and the poor quality of care in the peripartum period, lack of skilled health personnel, and increased unassisted births and a lack of timely provision of life-saving emergency perinatal services leading to an increased risk of stillbirth. 84 Hence, an improved antepartum care 85 and intrapartum care interventions can reduce stillbirths by 46%. 86 Therefore, the improved survival of preterm babies and the reduction of perinatal mortality rate by providing appropriate care and improvements in the quality of care offered by the health facilities during pregnancy, during labour and after birth are needed.
The present systematic review and meta-analysis also found that preterm birth significantly increased the odds of neonatal hypothermia. This was following with other studies done in Eastern Africa. 87 This finding can be explained by the fact that preterm babies have lower brown body tissue or fat, decrease the potential to maintain body temperature and are easily exposed for hypothermia.88,89 The narrative review of this study also showed higher odds of neonatal near misses among preterm babies than their counterparts. This finding was supported by a study conducted in Brazil.90,91 The neonatal near miss rate was almost 8 times higher than the neonatal mortality rate based on the findings of the systematic review done by Santos JP and his collaborators. 92 Thus, a strategy to reduce the burden of hypothermia and neonatal sepsis among preterm neonates should be scaled up by governmental and non-governmental institutions.
Moreover, the results of our systematic review and meta-analysis also found increased odds of neonatal mortality among preterm babies. This finding is in line with other studies done in Eastern Africa 93 and Europe. 94 This can be explained by the fact that preterm babies have immature lungs and other vital organs, which exposed them to respiratory problems including infections, facing difficulty to adapt the extra-uterine life. Premature newborns are at risk for death during the neonatal period 21 due to higher rates of associated neonatal morbidities such as neonatal sepsis, 95 neonatal near miss and foetal malformations, 96 leukaemia, 97 retinopathy of prematurity,12,21 respiratory distress, feed intolerance and jaundice 98 and neonatal sepsis.98–100
A recent study conducted in Ethiopia also showed the highest rate of preterm mortality was attributed to respiratory problems distress syndrome (45%), infections (30%) and asphyxia (14%). 101 Thus, to reduce morbidity and mortality of preterm neonates improving the interventions during the antenatal, intrapartum and postpartum period for the women and the newborn like optimal care in temperature maintenance, adequate feeding, hygienic cord and skincare, and early detection is needed. Also, treatment of morbidities including respiratory distress syndrome and infections associated with preterm birth is paramount. The observed strong association between preterm birth and adverse perinatal and neonatal outcomes might be linked with an increased risk of ill-health and negative feelings about their baby 102 including anxiety and postpartum depression.103–106 This because depression and anxiety are known factors to reduce caring for themselves and neonates, reduce health care service utilization for the sick newborn, absence of breastfeeding, increase febrile illnesses and malnutrition 107 and increases the risk of near miss, ultimately to mortality.
Therefore, an integrated interdisciplinary approach and interventions on the maternal continuum of care and neonatal care is needed. Scale-up of such interventions to prevent adverse outcomes and long-term impacts of the offspring associated with preterm birth are also recommended. However, the multiple clinical and research disciplines are not practically integrated significantly, mainly obstetricians are more concerned with labour and delivery complications and mental health experts are concerned with mental health problems like antenatal and postnatal depression. A narrative review on the reported outcomes that were unable to do a meta-analysis was conducted, the review showed that preterm birth significantly increased neonatal jaundice, 108 respiratory distress syndrome and neonatal near miss. 109
The current systematic review and meta-analysis are not without limitations. The highest heterogeneity among studies might be explained by the heterogeneity in the characteristics of the studies and may have led to insufficient statistical power to detect statistically significant association. However, a meta-regression analysis was conducted to identify the source of heterogeneity, and, it revealed that there was no variation due to sample size and publication year. The studies were conducted only on the 7 regions which may reduce the representativeness of the country. Future researchers should address the main predictors of preterm neonatal mortality to develop a package of interventions to reduce mortality.
Conclusions
This systematic review and meta-analysis indicated that preterm birth was significantly associated with perinatal mortality, stillbirth, neonatal hypothermia and neonatal mortality. Therefore, improving the quality of intervention programs during antenatal care, intrapartum and neonatal period are essential to reduce preterm birth and its adverse outcomes. The Federal Ministry of Health and other stakeholders should also work towards reduction of adverse perinatal and neonatal outcomes associated with preterm birth.
Availability of Data and Materials
Data will be available from the corresponding author upon reasonable request.
Supplemental Material
Supplemental Material, sj-pdf-1-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-2-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-3-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-4-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-5-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-6-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplementary files
Supplementary file 1 (S1): Effect of preterm birth on the risk of adverse perinatal and neonatal outcomes in Ethiopia: a systematic review and meta-analysis
Supplementary file 2: The Newcastle – Ottawa Scale (NOS) quality assessment of studies
Supplementary file 3: funnel plot on the association of preterm birth and perinatal mortality
Supplementary file 4: funnel plot on the association of preterm birth and neonatal sepsis
Supplementary file 5: funnel plot on the association of preterm birth and neonatal hypothermia
Supplementary file 6: funnel plot on the association of preterm birth and neonatal mortality
Appendix A
Abbreviations
- ANC
Antenatal Care
- LMICs
Low- and Middle-Income Countries
- POR
Pooled Odds Ratio
- SNNPR
Southern Nations Nationalities and Peoples Region
Author Contributions: MD: conceived and designed the study protocol, literature review, data extraction, data analysis, interpretation and wrote up the manuscript.
YGY, BTM, KA, MA and MAA have extracted and analysis data.
GMK and NBY have review and edit the manuscript.
All authors read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Melaku Desta https://orcid.org/0000-0002-4955-2346
Getachew Kassa https://orcid.org/0000-0002-8095-7376
References
- 1.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197-2223. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2015 Child Mortality Collaborators . Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1725-1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151-2161. [DOI] [PubMed] [Google Scholar]
- 4.GBD 2016 Causes of Death Collaborators . Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: A systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1151-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oza S, Cousens SN, Lawn JE. Estimation of daily risk of neonatal death, including the day of birth, in 186 countries in 2013: a vital-registration and modelling-based study. Lancet Global Health. 2014;2(e635–44):e635-44. [DOI] [PubMed] [Google Scholar]
- 6.Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. The Lancet Global Health. 2016;4(2):e98-e108. [DOI] [PubMed] [Google Scholar]
- 7.Paul IM, Lehman EB, Hollenbeak CS, Maisels MJ. Preventable newborn readmissions since passage of the newborns' and mothers' health protection act. Pediatrics. 2006;118(6):2349-2358. [DOI] [PubMed] [Google Scholar]
- 8.Tseng YH, Chen CW, Huang HL, Chen CC, Lee MD, Ko MC, et al. Incidence of and predictors for short-term readmission among preterm low-birthweight infants. Pediatr Int. 2010;52(5):711-717. [DOI] [PubMed] [Google Scholar]
- 9.Kunle-Olowu OE, Peterside O, Adeyemi OO. Prevalence and outcome of preterm admissions at the neonatal unit of a tertiary health centre in Southern Nigeria. Open J Pediatr. 2014;04(01):67-75. [Google Scholar]
- 10.Khashu M, Narayanan M, Bhargava S, Osiovich H. Perinatal outcomes associated with preterm birth at 33 to 36 weeks' gestation: A population-based cohort study. Pediatrics. 2009;123(1):109-113. [DOI] [PubMed] [Google Scholar]
- 11.Escobar GJ, McCormick MC, Zupancic JA, Coleman-Phox K, Armstrong MA, Greene JD, et al. Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2006;91(4):F238-F244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). Br Med J Int Ed. 2012;345:e7976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J, et al. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics. 2008;121(2):e223-e232. [DOI] [PubMed] [Google Scholar]
- 14.Fellman V, Hellström-Westas L, Norman M, Westgren M, Källén K, Lagercrantz H, et al. One-year survival of extremely preterm infants after active perinatal care in Sweden. Obstet Anesth Digest. 2010;30(1):22-23. [DOI] [PubMed] [Google Scholar]
- 15.Swamy GK, Østbye T, Skjærven R. Association of preterm birth with long-term survival, reproduction, and next-generation preterm birth. J Am Med Assoc. 2008;299(12):1429-1436. [DOI] [PubMed] [Google Scholar]
- 16.Kramer MS, Demissie K, Yang H, Platt RW, PSauvé R, PListon R. The contribution of mild and moderate preterm birth to infant mortality. JAMA. 2000;284(7):843-849. [DOI] [PubMed] [Google Scholar]
- 17.Crump C, Sundquist K, Sundquist J, Winkleby MA. Gestational age at birth and mortality in young adulthood. JAMA. 2011;306(11):1233-1240. [DOI] [PubMed] [Google Scholar]
- 18.D'Onofrio BM, Class QA, Rickert ME, Larsson H, Långström N, Lichtenstein P. Preterm birth and mortality and morbidity: a population-based quasi-experimental study. JAMA Psychiatry. 2013;70(11):1231-1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mendonça M, Bilgin A, Wolke D. Association of preterm birth and low birth weight with romantic partnership, sexual intercourse, and parenthood in adulthood: A systematic review and meta-analysis. JAMA Network Open. 2019;2(7):e196961-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mannisto T, Vaarasmaki M, Sipola-Leppanen M, Tikanmaki M, Matinolli H-M, Pesonen A-K, et al. Independent living and romantic relations among young adults born preterm. Pediatrics. 2015;135(2):290-297. [DOI] [PubMed] [Google Scholar]
- 21.Askie LM, Darlow BA, Davis PG, Finer N, Stenson B, Vento M, et al. Effects of targeting lower versus higher arterial oxygen saturations on death or disability in preterm infants. Cochrane Database Syst Rev. 2017;4:Cd011190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ballard K, Belete Z, Kinfu H, Tadesse M, Amin M, Atnafu H. The effect of prenatal and intrapartum care on the stillbirth rate among women in rural Ethiopia. Int J Gynecol Obstet. 2016;133(2):164-167. [DOI] [PubMed] [Google Scholar]
- 23.Aynalem YA. Survival status and predictor of mortality among premature neonate that was admitted to neonatal intensive care unit from 2013-2017 at Tikur Anbessa Hospital, Addis Ababa Ethiopia: a retrospective cohort study with survival analysis. Prim Health Care. 2018;8. [Google Scholar]
- 24.Yirgu R, Molla M, Sibley L, Gebremariam A. Perinatal mortality magnitude, determinants and causes in west Gojam: population-based nested case-control study. PLoS One. 2016;11(7):e0159390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roro EM, Sisay MM, Sibley LM. Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia Region, Ethiopia: Community based nested case control study. BMC Publ Health. 2018;18(1):888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alebachew Bayih W, Assefa N, Dheresa M, Minuye B, Demis S. Neonatal hypothermia and associated factors within six hours of delivery in eastern part of Ethiopia: a cross-sectional study. BMC Pediatrics. 2019;19(1):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alemu M, Ayana M, Abiy H, Minuye B, Alebachew W, Endalamaw A. Determinants of neonatal sepsis among neonates in the northwest part of Ethiopia: case-control study. Ital J Pediatr. 2019;45(1):150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region, Northern Ethiopia: prospective cohort study. BMC Pregnancy and Childbirth. 2016;16(1):202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088-1101. [PubMed] [Google Scholar]
- 33.Nyaga VN, Arbyn M, Aerts M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch Publ Health. 2014;72(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deeks JJ, Higgins JP, Altman DG. Analysing data and undertaking meta‐analyses. Cochrane Handbook Systemat Rev Interv. 2008:241-284. [Google Scholar]
- 35.Soubeiga D, Gauvin L, Hatem MA, Johri M. Birth Preparedness and Complication Readiness (BPCR) interventions to reduce maternal and neonatal mortality in developing countries: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2014;14(1):129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Demise A, Gebrehiwot Y, Worku B, Spector JM. Prospective audit of avoidable factors in institutional stillbirths and early neonatal deaths at Tikur Anbessa Hospital in Addis Ababa, Ethiopia. Afr J Reprod Health. 2015;19(4):78-86. [PubMed] [Google Scholar]
- 37.Welegebriel TK, Dadi TL, Mihrete KM. Determinants of stillbirth in Bonga General and Mizan Tepi University Teaching Hospitals southwestern Ethiopia, 2016: a case-control study. BMC Res Notes. 2017;10(1):713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Worede DT, Dagnew GW. Determinants of stillbirth in Felege-Hiwot comprehensive specialized referral hospital, North-west, Ethiopia, 2019. BMC Res Notes. 2019;12(1):579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berhie KA, Gebresilassie HG. Multilevel logistic regression analysis of the determinants of stillbirth in Ethiopia using EDHS 2011 data. Turkiye Klinikleri J Biostat. 2017;9(2):121-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mersha A, Worku T, Shibiru S, Bante A, Molla A, Seifu G, et al. Neonatal sepsis and associated factors among newborns in hospitals of Wolaita Sodo Town, Southern Ethiopia. Res Rep Neonatol. 2019;Volume 9:1-8. [Google Scholar]
- 41.G/Eyesus T, Moges F, Eshetie S, Yeshitela B, Abate E. Bacterial etiologic agents causing neonatal sepsis and associated risk factors in Gondar, Northwest Ethiopia. BMC Pediatrics. 2017;17(1):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tewabe T, Mohammed S, Tilahun Y, Melaku B, Fenta M, Dagnaw T, et al. Clinical outcome and risk factors of neonatal sepsis among neonates in Felege Hiwot referral Hospital, Bahir Dar, Amhara Regional State, North West Ethiopia 2016: a retrospective chart review. BMC Research Notes. 2017;10(1):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ukke GG, Diriba K. Prevalence and factors associated with neonatal hypothermia on admission to neonatal intensive care units in Southwest Ethiopia - A cross-sectional study. PLoS One. 2019;14(6):e0218020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Seid SS, Ibro SA, Ahmed AA, Olani Akuma A, Reta EY, Haso TK, et al. Causes and factors associated with neonatal mortality in neonatal intensive care unit (NICU) of Jimma University medical center, Jimma, south West Ethiopia. Pediatr Health Med Therapeut. 2019;Volume 10:39-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alemu AY, Belay GM, Berhanu M, Minuye B. Determinants of neonatal mortality at neonatal intensive care unit in Northeast Ethiopia: Unmatched case-control study. Trop Med Health. 2020;48(1):40-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mengesha HG, Lerebo WT, Kidanemariam A, Gebrezgiabher G, Berhane Y. Pre-term and post-term births: Predictors and implications on neonatal mortality in Northern Ethiopia. BMC Nursing. 2016;15(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tura AK, Scherjon S, van Roosmalen J, Zwart J, Stekelenburg J, van den Akker T. Surviving mothers and lost babies - burden of stillbirths and neonatal deaths among women with maternal near miss in eastern Ethiopia: a prospective cohort study. Journal of global health. 2020;10(1):01041310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Demissie S, Asrat D, Yimtubezinash W, Bogale W. Risk factors and etiology of neonatal sepsis in Tikur Anbessa University Hospital, Ethiopia. Ethiop Med J. 2010;48(1):11-21. [PubMed] [Google Scholar]
- 49.Aragaw Y. Perinatal mortality and associated factor in Jimma university specialized hospital, South West Ethiopia. Gynecol Obstet. 2016;6(409):2161-0932. [Google Scholar]
- 50.Getiye Y, Fantahun M. Factors associated with perinatal mortality among public health deliveries in Addis Ababa, Ethiopia, an unmatched case control study. BMC Pregnancy Childbirth. 2017;17(1):245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tilahun S, Gaym A. Past reproductive performance and its correlation with perinatal mortality in the current gestation at teaching hospitals in Addis Ababa, Ethiopia. Ethiop Med J. 2008;46(4):313-324. [PubMed] [Google Scholar]
- 52.Goba GK, Tsegay H, Gebregergs GB, Mitiku M, Kim KA, Alemayehu M. A facility-based study of factors associated with perinatal mortality in Tigray, northern Ethiopia. Int J Gynecol Obstet. 2018;141(1):113-119. [DOI] [PubMed] [Google Scholar]
- 53.Berhe T, Gebreyesus H, Teklay H. Prevalence and determinants of stillbirth among women attended deliveries in Aksum General Hospital: a facility based cross-sectional study. BMC Research Notes. 2019;12(1):368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tasew H, Zemicheal M, Teklay G, Mariye T. Risk factors of stillbirth among mothers delivered in public hospitals of Central Zone, Tigray, Ethiopia. Afr Health Sci. 2019;19(2):1930-1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gebreslasie KZ, Weldemariam S, Gebre G, Mehari MA. Intimate partner violence during pregnancy and risk of still birth in hospitals of Tigray region Ethiopia. Ital J Pediatr. 2020;46(1):107-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Geyesus T, Moges F, Eshetie S, Yeshitela B, Abate E. Bacterial etiologic agents causing neonatal sepsis and associated risk factors in Gondar, Northwest Ethiopia. BMC Pediatr. 2017;17(1):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Woldu M, Guta M, Lenjisa J, Tegegne G, Tesafye G, Dinsa H. Assessment of the incidence of neonatal sepsis, its risk factors, antimicrobial use and clinical outcomes in Bishoftu General Hospital. Int J Contem Pediatr. 2014;4(214):2161-0665. [Google Scholar]
- 58.Getabelew A, Aman M, Fantaye E, Yeheyis T. Prevalence of neonatal sepsis and associated factors among neonates in neonatal intensive care unit at selected governmental hospitals in Shashemene town, Oromia regional state, Ethiopia, 2017. Int J Pediatr. 20172018;2018:7801272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gebremedhin D, Berhe H, Gebrekirstos K. Risk factors for neonatal sepsis in public hospitals of Mekelle City, North Ethiopia, 2015: Unmatched case control study. PLoS One. 2016;11(5):e0154798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ketema E, Mamo M, Miskir D, Hussen S, Boti N. Determinants of neonatal sepsis among neonates admitted in a neonatal intensive care unit at Jinka General Hospital, Southern Ethiopia. Int J Nurs Midwifery. 2019;11(3):18-24. [Google Scholar]
- 61.Sorsa A. Epidemiology of neonatal sepsis and associated factors implicated: Observational study at neonatal intensive care unit of Arsi University Teaching and Referral Hospital, South East Ethiopia. Ethiopian J Health Sci. 2019;29(3):333-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mustefa A, Abera A, Aseffa A. Prevalence of neonatal sepsis and associated factors amongst neonates admitted in arbaminch general hospital, arbaminch, southern Ethiopia, 2019. J Pediatr Neonatal Care. 2020;10(1):1-7. [Google Scholar]
- 63.Weldu Y, Naizgi M, Hadgu A, Desta AA, Kahsay A, Negash L, et al. Neonatal septicemia at intensive care unit, Ayder Comprehensive Specialized Hospital, Tigray, North Ethiopia: Bacteriological profile, drug susceptibility pattern, and associated factors. PLoS One. 2020;15(6):e0235391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Demissie BW, Abera BB, Chichiabellu TY, Astawesegn FH. Neonatal hypothermia and associated factors among neonates admitted to neonatal intensive care unit of public hospitals in Addis Ababa, Ethiopia. BMC Pediatr. 2018;18(1):263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tasew H, Gebrekristos K, Kidanu K, Mariye T, Teklay G. Determinants of hypothermia on neonates admitted to the intensive care unit of public hospitals of Central Zone, Tigray, Ethiopia 2017: unmatched case-control study. BMC Res Notes. 2018;11(1):576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seyum T, Ebrahim E. Proportion of neonatal hypothermia and associated factors among new-borns at Gondar university teaching and refferal hospital, Northwest Ethiopia: a hospital based cross sectional study. Gen Med: Open Access. 2015;2015. [Google Scholar]
- 67.Orsido TT, Asseffa NA, Berheto TM. Predictors of neonatal mortality in neonatal intensive care unit at referral hospital in southern Ethiopia: A retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kokeb M, Desta T. Institution based prospective cross-sectional study on patterns of neonatal morbidity at gondar university hospital neonatal unit, North-West Ethiopia. Ethiopian J Health Sci. 2016;26(1):73-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Desalew A, Sintayehu Y, Teferi N, Amare F, Geda B, Worku T, et al. Cause and predictors of neonatal mortality among neonates admitted to neonatal intensive care units of public hospitals in eastern Ethiopia: a facility-based prospective follow-up study. BMC Pediatrics 2020;20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Elmi Farah A, Abbas AH, Tahir Ahmed A. Trends of admission and predictors of neonatal mortality: A hospital based retrospective cohort study in Somali region of Ethiopia. PLoS One. 2018;13(9):e0203314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gudayu TW, Zeleke EG, Lakew AM. Time to death and its predictors among neonates admitted in the intensive care unit of the university of gondar comprehensive specialized hospital, Northwest Ethiopia. Res Rep Neonatol. 2020;Volume 10:1-10. [Google Scholar]
- 72.Hadgu FB, Gebretsadik LG, Mihretu HG, Berhe AH. Prevalence and factors associated with neonatal mortality at ayder comprehensive specialized hospital, northern Ethiopia. A Cross-Sectional Study. Pediatr Health Med Therapeut. 2020;Volume 11:29-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma zone, southwest Ethiopia: a multilevel analysis of prospective follow up study. PLoS One. 2014;9(9):e107184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Demisse AG, Alemu F, Gizaw MA, Tigabu Z. Patterns of admission and factors associated with neonatal mortality among neonates admitted to the neonatal intensive care unit of University of Gondar Hospital, Northwest Ethiopia. Pediatr Health Med Therapeut. 2017;Volume 8:57-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Berhan Y, Berhan A. Meta-analysis of selected maternal and fetal factors for perinatal mortality. Ethiopian journal of health sciences. 2014;24:55-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bayou G, Berhan Y. Perinatal mortality and associated risk factors: a case control study. Ethiopian J Health Sciences. 2012;22(3):153-162. [PMC free article] [PubMed] [Google Scholar]
- 77.Kirigia JM, Barry SP. Health challenges in Africa and the way forward. Int Arch Med. 2008;1(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tenaw Z, Fikre R, Gemeda H, Astatkie A. Poverty Reduces Maternity Waiting Home Utilization in Sidama Zone, Southern Ethiopia; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Getachew B, Liabsuetrakul T, Gebrehiwot Y. Association of maternity waiting home utilization with women's perceived geographic barriers and delivery complications in Ethiopia. Int J Health Plann Manag. 2020;35(1):e96-e107. [DOI] [PubMed] [Google Scholar]
- 80.Kurji J, Gebretsadik LA, Wordofa MA, Sudhakar M, Asefa Y, Kiros G, et al. Factors associated with maternity waiting home use among women in Jimma Zone, Ethiopia: a multilevel cross-sectional analysis. BMJ open. 2019;9(8):e028210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bekele BB, Dadi TL, Tesfaye T. The significant association between maternity waiting homes utilization and perinatal mortality in Africa: Systematic review and meta-analysis. BMC Res Notes. 2019;12(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dadi TL, Bekele BB, Kasaye HK, Nigussie T. Role of maternity waiting homes in the reduction of maternal death and stillbirth in developing countries and its contribution for maternal death reduction in Ethiopia: A systematic review and meta-analysis. BMC Health Services Res. 2018;18(1):748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A. Maternal and fetal risk factors for stillbirth: Population based study. Br Med J Int Ed. 2013;346:f108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Praxton A, Maine D, Freedman L, Frey D, Lobis S. The evidence for emergency obstetrics. Int J Gynacol Obstetric. 2004;88(2):181-193. [DOI] [PubMed] [Google Scholar]
- 85.Ballard K, Belete Z, Kinfu H, Tadesse M, Amin M, Atnafu H. The effect of prenatal and intrapartum care on the stillbirth rate among women in rural Ethiopia. Int J Gynecol Obstet. 2016;133(2):164-167. [DOI] [PubMed] [Google Scholar]
- 86.Lindtjørn B, Mitike D, Zidda Z, Yaya Y. Reducing stillbirths in Ethiopia: Results of an intervention programme. PLoS One. 2018;13(5):e0197708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Beletew B Mengesha A Wudu Mand Abate M. Prevalence of neonatal hypothermia and its associated factors in East Africa: a systematic review and meta-analysis. BMC Pediatrics 2020;20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ramel SE, Gray HL, Ode KL, Younge N, Georgieff MK, Demerath EW. Body composition changes in preterm infants following hospital discharge. J Pediatr Gastroenterol Nutr. 2011;53(3):333-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ringer SA. Core concepts: thermoregulation in the newborn, part II: prevention of aberrant body temperature. Neo reviews. 2013;14(5):e221-e226. [Google Scholar]
- 90.Silva AAMD, Leite ÁJM, Lamy ZC, Moreira MEL, Gurgel RQ, Cunha AJLAD, et al. Morbidade neonatal near miss na pesquisa Nascer no Brasil. Cad Saúde Pública. 2014;30:S182-S191. [Google Scholar]
- 91.Pileggi C, Souza JAOP, Cecatti JG, Faúndes A. Neonatal near miss approach in the 2005 WHO Global Survey Brazil. J Pediatr. 2010;86(1):21-26. [DOI] [PubMed] [Google Scholar]
- 92.Santos JP, Pileggi-Castro C, Camelo JS, Silva AA, Duran P, Serruya SJ, et al. Neonatal near miss: a systematic review. BMC Pregnancy Childbirth. 2015;15(1):320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Marchant T, Willey B, Katz J, Clarke S, Kariuki S, Kuile FT, et al. Neonatal mortality risk associated with preterm birth in East Africa, adjusted by weight for gestational age: individual participant level meta-analysis. PLoS Med. 2012;9(8):e1001292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Buekens P, Wilcox AJ, Kiely J, Masuy-Stroobant G. Birthweight, preterm births and neonatal mortality in Belgium and the United States. Paediatr Perinat Epidemiol. 1995;9(3):273-280. [DOI] [PubMed] [Google Scholar]
- 95.Liang LD, Kotadia N, English L, Kissoon N, Ansermino JM, Kabakyenga J, et al. Predictors of mortality in neonates and infants hospitalized with sepsis or serious infections in developing countries: A systematic review. Front Pediatr. 2018;6(277):277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.de Lima THB, Katz L, Kassar SB, Amorim MM. Neonatal near miss determinants at a maternity hospital for high-risk pregnancy in Northeastern Brazil: a prospective study. BMC Pregnancy Childbirth. 2018;18(1):401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang YF, Wu LQ, Liu YN, Bi YY, Wang H. Gestational age and childhood leukemia: A meta-analysis of epidemiologic studies. Hematology. 2018;23(5):253-262. [DOI] [PubMed] [Google Scholar]
- 98.Hassan N, Mukhopadhyay S, Mohan S. Morbidity and mortality profile of preterm neonates admitted in neonatal intensive care unit of a tertiary care centre in Western Uttar Pradesh, India. Int J Contemp Pediatr. 2019;6(5). [Google Scholar]
- 99.Ochoga MO, Michael A, Abah RO, Dabit O, Ikuren I, Ebonyi A. Risk factors and outcome of preterm admissions in a special care baby unit of a tertiary hospital in north central Nigeria. Open J Pediatr. 2018;08(02):117-125. [Google Scholar]
- 100.Undela K, Mohammed BTS, Gurumurthy P, Doreswamy SM. Impact of preterm birth and low birth weight on medical conditions, medication use and mortality among neonates: a prospective observational cohort study. World J Pediatr. 2019;15:281-288. [DOI] [PubMed] [Google Scholar]
- 101.Muhe LM, McClure EM, Nigussie AK, Mekasha A, Worku B, Worku A, et al. Major causes of death in preterm infants in selected hospitals in Ethiopia (SIP): a prospective, cross-sectional, observational study. Lancet Global Health. 2019;7(8):e1130-e1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Henderson J, Carson C, Redshaw M. Impact of preterm birth on maternal well-being and women's perceptions of their baby: a population-based survey. BMJ Open. 2016;6(10):e012676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Helle N, Barkmann C, Bartz-Seel J, Diehl T, Ehrhardt S, Hendel A, et al. Very low birth-weight as a risk factor for postpartum depression four to six weeks postbirth in mothers and fathers: Cross-sectional results from a controlled multicentre cohort study. J Affect Disord. 2015;180:154-161. [DOI] [PubMed] [Google Scholar]
- 104.Pace CC, Spittle AJ, Molesworth CML, Lee KJ, Northam EA, Cheong JLY, et al. Evolution of depression and anxiety symptoms in parents of very preterm infants during the newborn period. Jama Pediatrics. 2016;170(9):863-870. [DOI] [PubMed] [Google Scholar]
- 105.Ihongbe TO, Masho SW. Do Successive Preterm Births Increase the Risk of Postpartum Depressive Symptoms? Journal of Pregnancy. 2017;2017:4148136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vigod S, Villegas L, Dennis CL, Ross L. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG An Int J Obstet Gynaecol. 2010;117(5):540-550. [DOI] [PubMed] [Google Scholar]
- 107.Dadi AF, Miller ER, Mwanri L. Postnatal depression and its association with adverse infant health outcomes in low- and middle-income countries: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20(1):416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lake EA, Abera GB, Azeze GA, Gebeyew NA, Demissie BW. Magnitude of neonatal jaundice and its associated factor in neonatal intensive care units of mekelle city public hospitals, northern Ethiopia. Int J Pediatr. 2019;2019:1054943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yohannes E, Assefa N, Dessie Y. Determinants of neonatal near miss among neonates admitted to ambo university referral hospital and ambo general hospital, Ethiopia. J Preg Child Health. 20192020;77:42511-42518. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-2-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-3-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-4-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-5-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental Material, sj-pdf-6-inq-10.1177_00469580211064125 for Effect of Preterm Birth on the Risk of Adverse Perinatal and Neonatal Outcomes in Ethiopia: A Systematic Review and Meta-Analysis by Melaku Desta, Melaku Admas, Yordanos Yeshitila, Belsity Meselu, Keralem Bishaw, Moges Assemie, Nigus Yimer and GetachewKassa Kassa in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Data Availability Statement
Data will be available from the corresponding author upon reasonable request.