ABSTRACT
Findings from earlier studies on the association between adherence to a Mediterranean diet and risk of overweight/obesity were inconsistent. We summarized cohort studies investigating the association between the Mediterranean diet and risk of overweight and/or obesity and weight change in adults. A systematic search of PubMed, Scopus, ISI Web of Science, and Google Scholar was conducted up to May 2021. Prospective cohorts that examined the Mediterranean diet adherence in adults as the exposure, and overweight and/or obesity or weight change as the outcomes, and reported RRs or β coefficients and 95% CIs as the effect sizes were included. Seven prospective cohort studies were included of which 6 studies (with 244,678 adult participants) reported the risk of overweight and/or obesity, and 4 cohorts (with 436,617 participants) reported the weight change (3 cohorts reported both overweight and/or obesity risk and weight change). Combining 15 effect sizes from 6 cohorts revealed that greater adherence to the Mediterranean diet was significantly associated with a 9% decreased risk of overweight and/or obesity (RR: 0.91; 95% CI: 0.88, 0.94; I2 = 44.7%; PQ-test = 0.031). This association was significant in the case of studies investigating combined overweight and obesity (RR: 0.92; 95% CI: 0.88, 0.96; I2 = 29.4%; PQ-test = 0.166), but not for studies that reported on obesity (RR: 0.68; 95% CI: 0.43, 1.10, I2 = 50.6%, PQ-test = 0.132). Linear dose–response analysis of 6 studies showed a 2% decreased risk of overweight and/or obesity for 1 additional Mediterranean diet score (RR: 0.98; 95% CI: 0.96, 0.99). Each unit increase in the Mediterranean diet score was associated with 0.04 kg less weight gain over 5 y (−0.04 kg; 95% CI: −0.07, −0.02 kg; 13 effect sizes from 4 cohorts). In conclusion, Mediterranean diet adherence is inversely associated with risk of overweight and/or obesity as well as 5-y weight gain and thus has practical importance for public health.
Keywords: Mediterranean diet, overweight, obesity, weight change, meta-analysis, cohort studies
Statement of Significance: This meta-analysis of prospective cohort studies revealed that Mediterranean diet adherence was associated with lower risk of overweight and/or obesity and less weight gain.
Introduction
The Mediterranean diet, as a healthy plant-based diet, is characterized by high consumption of fruits and vegetables, nuts and seeds, whole grains and olive oil; moderate consumption of fish and poultry; and low consumption of dairy products, red meats, and processed meats (1). So far, the association between the long-term adherence to this dietary pattern and health conditions including cardiovascular disease (CVD), diabetes, cancer, metabolic syndrome, and neurodegenerative diseases has been shown (2). In a meta-analysis, an inverse association was reported between Mediterranean diet score and risk of mortality (3).
Overweight and obese individuals are more likely to develop type 2 diabetes, CVD, many cancers, and even musculoskeletal disorders (4). Furthermore, a large meta-analysis showed that overweight and obesity could increase the risk of mortality in different populations (5). Because of the high fat and carbohydrate content of the Mediterranean diet, the association between adherence to a Mediterranean diet and obesity has gained great attention (6, 7). Moreover, the prevalence of obesity in the Mediterranean countries is considerable, but the mortality from CVD is significantly lower in these nations than in other parts of the world (8, 9). Findings from earlier studies on the association between adherence to a Mediterranean diet and risk of obesity have been inconsistent (10–12). In a Seguimiento Universidad de Navarra (SUN) cohort study, no significant association was seen between adherence to a Mediterranean diet and risk of weight gain in Spanish adults (10). The same finding was also reported from a European Prospective Investigation into Cancer and Nutrition (EPIC)-Spain cohort in normal-weight participants; however, adherence to a Mediterranean diet in that study was significantly associated with reduced risk of becoming obese in overweight subjects (12). Reports from clinical trials, focusing on the effect of a Mediterranean diet on weight loss, have also been inconsistent (13). Given that findings from clinical trials cannot easily be extrapolated to normal populations in their routine life, focusing on prospective cohort studies and summarizing their results might provide additional information on the role of diet in preventing obesity incidence in the community. We are aware of no study summarizing earlier prospective cohort studies on the association between adherence to a Mediterranean diet and risk of obesity. This study was therefore done to systematically review published prospective cohort studies on the association between adherence to a Mediterranean diet and risk of overweight and obesity as well as weight change in the adult population and to quantify these associations through meta-analysis.
Methods
Search strategy
We performed a comprehensive search of articles published up to May 2021 using databases including MEDLINE (PubMed), Scopus, ISI Web of Science, and Google Scholar with no restriction in language or time of publication. Detailed information on the search terms is provided in Supplemental Table 1. Briefly, the following Medical Subject Headings (MeSH) and non-MeSH terms were used: (“Mediterranean diet” OR “Med diet”) AND (“Body Weight” OR Obesity OR overweight OR “Body Weight”) AND (cohort OR follow up OR longitudinal OR prospective). Two independent investigators (KL and ZH) selected the articles and any disagreement was resolved by the principal investigator (AE). Furthermore, manual searches of the bibliographies of relevant investigations were performed to identify additional studies. Then, duplicate citations were removed. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The study was registered at http://www.crd.york.ac.uk/Prospero (registration no. CRD42020221658).
Inclusion criteria
Published studies were included if they had the following criteria: 1) prospective cohort studies conducted in adults (≥18 y); 2) considered baseline adherence to the Mediterranean diet as the exposure, and general overweight and/or obesity and weight change as the outcomes; 3) reported RRs with corresponding 95% CIs for the association of adherence to the Mediterranean diet with overweight and/or obesity; and 4) reported β coefficients with corresponding 95% CIs regarding the association between adherence to the Mediterranean diet and weight change. Investigations on unhealthy populations (with a history of diabetes, CVD, or cancer) were not included.
Exclusion criteria
We excluded these studies: 1) studies that were conducted in children and adolescents; 2) investigations with overweight/obese people at study baseline when we considered overweight and/or obesity as the outcome; and 3) studies that reported mean and SD for the association between the Mediterranean diet and weight change but did not provide regression coefficients. Three studies (14–16) were excluded because they considered change in the Mediterranean diet in relation to change in weight. Two reports were published from the SUN cohort study (10, 17) with the same study population. We included only 1 of these studies (10) with the largest sample size. In addition, 4 reports were published based on the EPIC cohort (12, 18–20), and we included the study with the largest sample (19). A more recent study published on EPIC-Italy with longer follow-up (21) was considered instead of the EPIC cohort (19) for Italians. In the study of Ford et al. (22) the OR for >10% weight gain from baseline was reported in normal weight, overweight, or obese individuals; because the average BMI at baseline was 27.4 kg/m2, a 10% increase in weight was the smallest increment that could shift the average BMI to the obese range (30.1). However, some individuals with a 10% increase in their baseline weight in the follow-up might have had normal weight. For example, an individual with a BMI of 20 at baseline and 22 in the follow-up was considered as having the outcome of interest, but still was categorized in normal-weight subjects. So, the outcome of interest in this investigation was different from other cohorts included in our analysis and the mentioned study was not included in the current analysis. Supplemental Table 2 summarizes some of the excluded publications and the reason for their exclusion.
Data extraction
Data of included studies were independently extracted by 2 researchers (KL and PS). The following information was extracted from each eligible article: first author's name, publication year, cohort name, country, mean age or age range at entry, gender, sample size, duration of follow-up, dietary pattern components, method of assessing outcome, number of obesity cases, weight change scale, RRs for overweight and/or obesity, or β coefficients for weight change, and their 95% CIs, and adjustments for confounding variables.
Assessment of quality of studies
To evaluate the quality of included studies, we used the Newcastle–Ottawa scale (NOS) for cohort studies (23). The NOS is a 9-point scoring scale: 4 for selection, 2 for comparability, and 3 for assessment of outcomes. Thus, a maximum score of 9 could be assigned to each study; when a study got more than a median score of 6, it was considered as relatively high quality; otherwise it was considered as a low-quality study. Any disagreements were resolved by discussion. Results from a quality assessment of studies included in the meta-analysis are presented in Supplemental Tables 3 and 4.
Statistical analysis
Log RR ± SE was calculated using reported RRs (and 95% CIs) for the top categories of adherence to the Mediterranean diet compared with the bottom categories as the reference. When the studies reported RRs per an SD increase in Mediterranean diet score, we converted the data to the top tertile compared with the bottom tertile by previously published methods (24, 25). Briefly, assuming a normal distribution in the exposure and a log-linear association with the outcome risk, log RRs for the comparison between the highest and the lowest tertile are equivalent to per SD increment values multiplied by 2.18. The same approach was applied for their SEs. Because of different scales of weight change among studies, we converted them to a 5-y weight change. In this regard, regression coefficients were divided by the mean time interval in each cohort and then multiplied by 5. Furthermore, 95% CIs of the unstandardized β coefficients were used to calculate SEs. For 1 study that reported standardized β coefficients (11), we used previously described formulas (26) to calculate an unstandardized regression coefficient and SE. Because included studies were not identical in design, participants, applied methods, and other factors, they were considered nonhomogeneous. So, the overall effect size for each outcome was calculated by a random-effects model to take between-study variations into account. The I2 test and Q-test were used to investigate heterogeneity between the studies (27) and were considered significant if the P value of the Q test was <0.05 and/or I2 >50%. For overweight and/or obesity as the outcome, subgroup analysis (based on gender, country, follow-up duration, dietary assessment method, the Mediterranean diet definition, quality score of the studies, energy adjustment, and outcome) was performed to find out the possible sources of heterogeneity. Overall effect size in each subgroup was calculated by a random-effects model. Also, a fixed-effect model was applied to obtain a P value for heterogeneity between subgroups and to determine whether the examined variable could be a possible source of heterogeneity or not. To examine publication bias, funnel plots were visually observed. Also, funnel plot asymmetry was statistically assessed, using the Begg test. Sensitivity analysis was also performed to explore the influence of each study on the overall estimate.
A previous method, as described by Greenland and Longnecker (28) and Orsini et al. (29), was applied for doing a dose–response analysis per 1 unit of traditional Mediterranean score. This score ranged from 0 to 9. If a study had a different score range, we recalculated the reported effect sizes based on the 0–9 scale. For example, if the Mediterranean score ranged from 0 to 55 in a cohort, we multiplied the reported effect size by 9 and then divided by 55. To evaluate study-specific slopes (linear trends) and 95% CIs in 2 cohort studies, the natural logs of the RRs and corresponding CIs across levels of the Mediterranean diet score were applied (10, 21). This method required the distribution of participants with general overweight/obesity and the RRs with the variance estimates for ≥3 categories of the independent variable. We assigned a mean score of the Mediterranean diet in each category to the corresponding RR of the category for each study. If RRs had not been provided for ≥3 categories, as well as other required information for this method, we used the continuous RRs reported in the studies for linear dose–response analysis. Statistical analyses were performed with Stata version 14.0 (StataCorp LLC). P values <0.05 were considered as statistically significant.
Results
Literature search
In the initial search 5255 articles were identified for screening. After excluding the articles that did not meet our inclusion criteria and those that were duplicates, 24 potentially relevant articles remained (Figure 1). Full-text articles were reviewed and 17 additional studies were excluded based on inclusion and exclusion criteria. Finally, 7 prospective cohort studies, of which 6 reported on overweight and/or obesity and 4 reported on weight change (3 studies had both reports), were eligible for this systematic review and meta-analysis.
FIGURE 1.
Flowchart of the study selection process.
Study characteristics
Table 1 presents details of 6 cohort studies, with 15 effect sizes including a total of 244,678 participants aged 18 to 70, that investigated the association between the Mediterranean diet and risk of overweight and/or obesity. These cohorts were conducted in Italy (21), Spain (10), France (11), Greece (30), and China (31), and 1 of the studies (19) was conducted in 9 countries including France, Spain, the United Kingdom, the Netherlands, Greece, Germany, Sweden, Norway, and Denmark. Among these studies, 1 separately investigated the relation between Mediterranean diet and overweight and/or obesity in men and women, whereas 5 others were conducted on both genders. Also, 1 study separately reported effect sizes for 9 different countries. The number of study participants varied from 343 to 197,522. Most studies used FFQs to assess dietary intakes; however, 24-h dietary recall (11) and a country-specific validated dietary questionnaire (19) were applied in 2 investigations. For scoring of the Mediterranean diet, 4 studies used the method of Trichopoulou et al. (1), whereas 2 others used other methods (19, 30). One study (21) used the modified version of the Trichopoulou et al. method. Weight and height values were self-reported in 4 studies (10, 19, 21, 30), whereas in 2 other cohorts (11, 31) they were measured by trained individuals. Three cohorts reported RRs for combined overweight and obesity, 2 for obesity, and 1 for overweight. Reported RRs for overweight and/or obesity ranged from 0.45 to 1.35. Most studies considered age (n = 5), physical activity (n = 5), energy intake (n = 4), sex (n = 4), education (n = 4), and smoking (n = 3) as the potential confounding variables. However, 1 of these cohorts (30) did not control for any confounder. According to the NOS, 2 studies were of high quality, whereas 4 others were of low quality.
TABLE 1.
Main characteristics of prospective studies examining the association of adherence to the Mediterranean diet with risk of overweight and/or obesity in adults1
| First author (year) | Cohort name | Country | Age,2 y | Sex | Sample size, n; person-year | Duration follow-up, y | Exposure assessment | Dietary pattern components3 | Outcome assessment | Cases | RR (95% CI) | Comparison | Score | Adjustments4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Agnoli (2018) (21) | EPIC | Italy | 50.3 ± 7.7 (35–65) | M/F | 32,119; NR | 11.97 | FFQ | Italian Mediterranean index (Agnoli) | Overweight or obesity (BMI ≥25 kg/m2) | 3563 | 0.89 (0.80, 0.99) | T3 vs. T1 | 7 | 1–8 |
| Lassale (2012) (11) | SU.VI.MAX | France | 52.3 ± 4.6 (45–60) | M | 1569; NR | 13.0 | 24 h- recall | Mediterranean dietary scale (Trichopoulou) | Obesity (BMI ≥30) | 123 | 0.45 (0.27, 0.76) | Q4 vs. Q1 | 7 | 2, 6, 7, 9–12 |
| 51.0 ± 4.5 (35–60) | F | 1385; NR | Obesity (BMI ≥30) | 84 | 1.04 (0.52, 2.10) | |||||||||
| Beunza (2010) (10) | SUN | Spain | 38.0 ± 11.0 (NR) | M/F | 10,376; 36,495 | 5.70 | FFQ | Mediterranean dietary score (Trichopoulou) | Overweight or obesity (BMI ≥25) | 1026 | 0.90 (0.75, 1.06) | Highest score (6–9) vs. lowest score (0–3) | 5 | 2, 3, 7, 9, 11, 13–15 |
| Romaguera (2010) (19) | EPIC | 9 countries5 | NR (25–70) | M/F | 197,522; NR | 5.0 | Country specific validated dietary questionnaire (FFQ, dietary record) | Relative Mediterranean diet score (Buckland) | Overweight or obesity (BMI ≥25) | NR | EPIC-France: 0.96 (0.94, 0.98) | Per 2 unit increase | 5 | 2, 3, 6–9, 11, 13, 16, 17 |
| EPIC-Spain: 1.01 (0.96, 1.05) | ||||||||||||||
| EPIC-UK: 0.99 (0.94, 1.05) | ||||||||||||||
| EPIC-UK: 1.00 (0.95, 1.04) | ||||||||||||||
| EPIC-UK: 0.96 (0.87, 1.06) | ||||||||||||||
| EPIC-NL: 1.07 (0.96, 1.20) | ||||||||||||||
| EPIC-NL: 0.89 (0.82, 0.96) | ||||||||||||||
| EPIC-NL: 0.94 (0.88, 0.99) | ||||||||||||||
| EPIC-Greece: 0.99 (0.92, 1.06) | ||||||||||||||
| EPIC-Germany: 0.93 (0.89, 0.98) | ||||||||||||||
| EPIC-Germany: 0.95 (0.88, 1.02) | ||||||||||||||
| EPIC-Sweden: 0.95 (0.90, 1.00) | ||||||||||||||
| EPIC-Sweden: 1.03 (0.96, 1.11) | ||||||||||||||
| EPIC-Denmark: 0.99 (0.95, 1.03) | ||||||||||||||
| EPIC-Norway: 0.98 (0.93, 1.02) | ||||||||||||||
| Yannakoulia (2008) (30) | ATTICA | Greece | 45.0 ± 14.0 (>18) | M/F | 1364; NR | 5.0 | FFQ | Mediterranean dietary score (Panagiotakos) | Obesity (BMI ≥30) | 152 | 0.98 (0.95, 1.03) | Per 1 unit increase | 3 | — |
| Woo (2007) (31) | NR | China | 43.7 ± 11.1 (25–74) | M/F | 343; NR | 5.0–9.0 | FFQ | Mediterranean dietary score (Trichopoulou) | Overweight (BMI ≥23) | 49 | 1.35 (0.94, 1.93) | Per 1 SD increase | 4 | 2, 3, 6, 7 |
EPIC, European Prospective Investigation into Cancer and Nutrition; NL, Netherlands; NR, not reported; Q, quartile; SUN, Seguimiento Universidad de Navarra; SU.VI.MAX, SUpplementation en Vitamines et Mineraux AntioXydants; T, tertile; UK, United Kingdom; (+), high intake; (−), low intake; (m), moderate intake.
Values are mean ± SD (range).
Dietary pattern components: Agnoli 2018: (+): pasta, vegetables, fruit, pulses, olive oil, and fish, (−): soft drinks, butter, red and processed meat, and potatoes, (m): alcohol. Lassale 2012: (+): fruit, vegetables, legumes, grains, fish, ratio of MUFA to SFA, (−): meat, dairy products, (m): alcohol. Beunza 2010: (+): vegetables, fruit and nuts, legumes, cereals, bread and potatoes, ratio of MUFA to SFA, (−): meat and poultry, dairy products, (m): alcohol. Romaguera 2010: (+): vegetables, legumes, fruit and nuts, cereals, fish and seafood, olive oil, (−): meat and meat products and dairy products, (m): alcohol. Yannakoulia 2008: (+): nonrefined cereals, vegetables, fruit, legumes, fish, olive oil, and potatoes, (−): meat and meat products, poultry, full-fat dairy products, (m): alcohol. Woo 2007: (+): cereals, vegetables, fruit and nuts, legumes, fish, (−): meat, poultry, dairy products, (m): ethanol.
Adjustments: center (1), age (2), sex (3), nonalcoholic energy intake (4), distance between baseline and recall (5), education (6), physical activity (7), menopausal status for women (8), energy intake (9), number of 24-h records (10), smoking status (11), supplementation group (12), baseline BMI (13), sedentary behavior (14), snacking (15), follow-up duration (16), misreporting of energy intake (17).
France, Spain, UK, NL, Greece, Germany, Sweden, Denmark, Norway.
Detailed information regarding the association between the Mediterranean diet and weight change is provided in Table 2. Four cohorts with 13 effect sizes including 436,617 healthy participants with a follow-up duration of 5 to 13 y were examined. These studies were conducted in Italy (21), Sweden (32), and France (11). The last cohort was conducted in 9 countries including France, Spain, the United Kingdom, the Netherlands, Greece, Germany, Sweden, Norway, and Denmark (19). The age range of participants was between 25 and 70. One investigation separately assessed the link between Mediterranean diet and weight change in men and women, another cohort consisted only of women, and 2 others were conducted in both genders. Also, 1 study separately provided effect sizes for 9 different countries. The number of study participants ranged from 3151 to 373,803. Most studies used FFQs and the Trichopoulou method (1) for assessment of usual dietary intake and Mediterranean diet score, respectively. However, 2 studies used other methods. Three cohorts (19, 21, 32) used self-reported weight and height values, and anthropometric values in the last cohort (11) were measured by trained individuals. Weight change was reported over 5 y in 2 cohorts, whereas others reported weight change over 12 and 13 y. Potential confounders mostly controlled for were age (n = 4), physical activity (n = 4), energy intake (n = 4), menopausal status for women (n = 3), smoking (n = 2), and baseline BMI (n = 2). Three cohort studies were of high quality and 1 was of low quality, based on the NOS.
TABLE 2.
Main characteristics of prospective studies examining the association of adherence to the Mediterranean diet with weight-change in adults1
| First author (year) | Cohort name | Country | Age,2 y | Sex | Sample size, n | Duration follow-up, y | Exposure assessment | Dietary pattern components3 | Outcome assessment | β coefficient (95% CI) | Comparison | Score | Adjustments4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Agnoli (2018) (21) | EPIC | Italy | 50.3 ± 7.7 (35–65) | M/F | 32,119 | 11.97 | FFQ | Italian Mediterranean index (Agnoli) | 5-y weight change | −0.03 (−0.06, 0.01) | Per 1 tertile increase | 7 | 1–9 |
| Li (2015) (32) | WLH | Sweden | 40.0 ± 2.5 (29–49) | F | 27,544 | 12.0 | FFQ | Mediterranean diet score (Trichopoulou) | 12-y weight change | 0.03 (−0.03, 0.09) | Per 1 unit | 6 | 2, 6, 7, 10, 11–13 |
| Lassale (2012) (11) | SU.VI.MAX | France | 52.3 ± 4.6 (45–60) | M | 1680 | 13.0 | 24-h recall | Mediterranean dietary scale (Trichopoulou) | 13-y weight change | −0.77 (−1.06, −0.48)5 | Per 1 SD | 7 | 2, 7, 8, 10, 13–16 |
| 51.0 ± 4.5 (35–60) | F | 1471 | −0.43 (−0.86, 0.00)5 | ||||||||||
| Romaguera (2010) (19) | EPIC | 9 countries6 | NR (25–70) | M/F | 373,803 | 5.0 | Country-specific validated dietary questionnaire (FFQ, dietary record) | Relative Mediterranean diet score (Buckland) | 5-y weight change | EPIC-France: −0.04 (−0.07, −0.01) | Per 2 unit increase | 5 | 2, 6–10, 13, 17–19 |
| EPIC-Spain: −0.15 (−0.20, −0.10) | |||||||||||||
| EPIC-UK: 0.07 (0.00, 0.14) | |||||||||||||
| EPIC-UK: −0.04 (−0.09, 0.00) | |||||||||||||
| EPIC-UK: −0.11 (−0.21, −0.01) | |||||||||||||
| EPIC-NL: 0.08 (−0.04, 0.20) | |||||||||||||
| EPIC-NL: −0.07 (−0.14, 0.01) | |||||||||||||
| EPIC-NL: −0.09 (−0.17, −0.01) | |||||||||||||
| EPIC-Greece: −0.04 (−0.10, 0.01) | |||||||||||||
| EPIC-Germany: −0.13 (−0.22, −0.05) | |||||||||||||
| EPIC-Germany: −0.02 (−0.06, 0.02) | |||||||||||||
| EPIC-Sweden: −0.03 (−0.08, 0.02) | |||||||||||||
| EPIC-Sweden: 0.04 (−0.01, 0.09) | |||||||||||||
| EPIC-Denmark: −0.02 (−0.05, 0.01) | |||||||||||||
| EPIC-Norway: −0.05 (−0.09, −0.00) |
EPIC, European Prospective Investigation into Cancer and Nutrition; NL, Netherlands; NR, not reported; SU.VI.MAX, SUpplementation en VItamines et Mineraux AntioXydants; UK, United Kingdom; WLH: Swedish Women's Lifestyle and Health; (+), high intake; (−), low intake; (m), moderate intake.
Values are mean ± SD (range).
Dietary pattern components: Agnoli 2018: (+): pasta, vegetables, fruit, pulses, olive oil, and fish, (−): soft drinks, butter, red and processed meat, and potatoes, (m): alcohol. Li 2015: (+): cereals, vegetables, fruits/nuts, legumes, fish/seafood, and a high ratio of unsaturated fat:SFA, (−): dairy and meat products, (m): alcohol. Lassale 2012: (+): fruit, vegetables, legumes, grains, fish, ratio of MUFA to SFA, (−): meat, dairy products, (m): alcohol. Romaguera 2010: (+): vegetables, legumes, fruit and nuts, cereals, fish and seafood, olive oil, (−): meat and meat products and dairy products, (m): alcohol.
Adjustments: center (1), age (2), sex (3), nonalcoholic energy intake (4), distance between baseline and recall (5), education (6), physical activity (7), menopausal status for women (8), baseline BMI (9), smoking status (10), height (11), baseline outcome (12), energy intake (13), number of 24-h records (14), supplementation group (15), baseline weight and height (16), sex (17), follow-up time (18), misreporting of energy intake (19).
Standardized β coefficient.
France, Spain, Italy, United Kingdom, Netherlands, Greece, Germany, Sweden, Denmark, Norway.
Findings from the meta-analysis on overweight and/or obesity
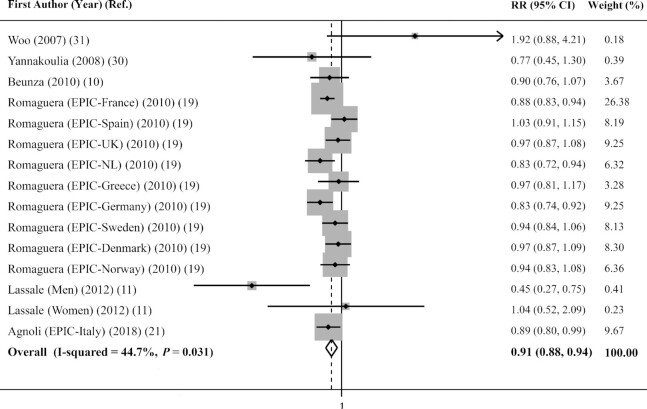
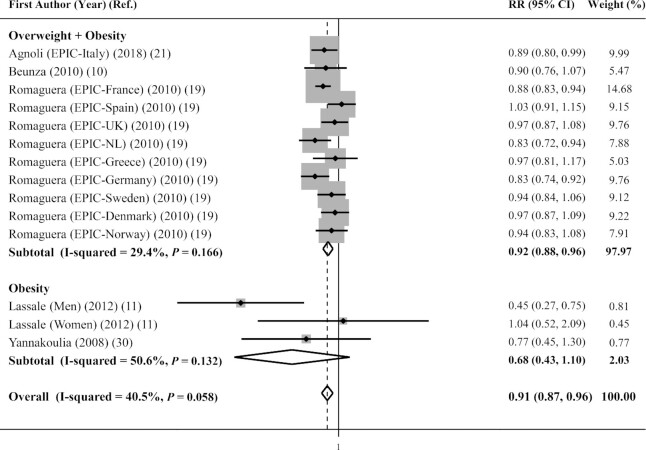
Combining 15 effect sizes from 6 prospective cohort studies (9 additional effect sizes were from 1 cohort that separately reported RRs for 9 different countries and another study that separately reported RR for males and females), which included 244,678 subjects, revealed that greater adherence to the Mediterranean diet was significantly associated with a 9% decreased risk of overweight and/or obesity (pooled RR = 0.91; 95% CI: 0.88, 0.94) (Figure 2). However, moderate heterogeneity was observed between studies (I2 = 44.7%; PQ-test = 0.031). To explore the source of heterogeneity, subgroup analysis was done based on the outcome of interest (combined overweight and obesity compared with obesity) (the only effect size for overweight was not included in this analysis). As shown in Figure 3, combining 11 effect sizes from 3 cohorts that combined overweight and obesity as their outcome revealed that a high score on the Mediterranean diet, compared with a low score, was associated with an 8% lower risk (pooled RR = 0.92; 95% CI: 0.88, 0.96), whereas such an association was not observed for cohort studies that considered obesity as the outcome (3 effect sizes from 2 cohorts; pooled RR = 0.68; 95% CI: 0.43, 1.10) (Pheterogeneity between subgroups = 0.057). Subgroup analysis based on other covariates (including gender, country, energy adjustment, dietary assessment method, Mediterranean diet definition, follow-up duration, and quality score of cohorts) was also conducted (Table 3). Greater adherence to the Mediterranean diet, compared with low adherence, was protectively associated with overweight and/or obesity in most subgroups. Sensitivity analysis revealed that pooled RR was not significantly influenced by any individual cohort. No asymmetry was seen in the funnel plot and no evidence for publication bias was found according to the Begg test (P = 0.921).
FIGURE 2.
Forest plot of cohort studies examining the association between Mediterranean diet adherence and risk of overweight and/or obesity in adults. The area of each shaded box is proportional to the weight of the study.
FIGURE 3.
Forest plot of cohort studies examining the association between Mediterranean diet adherence and risk of overweight and/or obesity in adults, stratified by outcome of interest. The area of each shaded box is proportional to the weight of the study.
TABLE 3.
Results of subgroup analysis for adherence to the Mediterranean diet and overweight and/or obesity risk and weight change
| Subgroup analysis for adherence to the Mediterranean diet and risk of overweight and/or obesity | |||||
|---|---|---|---|---|---|
| Effect sizes, n | RR (95% CI)1 | P within2 | I 2 (%) | P between3 | |
| Overall | 15 | 0.91 (0.88, 0.94) | 0.031 | 44.7 | |
| Gender | 0.019 | ||||
| Male | 1 | 0.45 (0.27, 0.75) | — | — | |
| Female | 3 | 0.89 (0.84, 0.95) | 0.597 | 0.0 | |
| Both | 11 | 0.92 (0.87, 0.98) | 0.089 | 38.9 | |
| Country | 0.061 | ||||
| European | 14 | 0.91 (0.87, 0.96) | 0.058 | 40.5 | |
| Non-European | 1 | 1.92 (0.88, 4.21) | — | — | |
| Energy adjustment | 0.601 | ||||
| Adjustment | 13 | 0.91 (0.87, 0.96) | 0.044 | 44.0 | |
| No adjustment | 2 | 1.16 (0.47, 2.84) | 0.057 | 72.4 | |
| Dietary assessment method | 0.088 | ||||
| FFQ | 6 | 0.93 (0.87, 0.99) | 0.391 | 4.0 | |
| 24-h recall | 2 | 0.66 (0.29, 1.50) | 0.059 | 72.0 | |
| Country-specific questionnaires | 5 | 0.90 (0.82, 0.97) | 0.042 | 59.6 | |
| FFQ + food record | 2 | 0.96 (0.88, 1.04) | 0.746 | 0.0 | |
| Mediterranean diet definition | 0.630 | ||||
| Trichopoulou | 4 | 0.89 (0.56, 1.42) | 0.014 | 71.6 | |
| Others | 11 | 0.92 (0.88, 0.96) | 0.150 | 31.3 | |
| Follow-up duration | 0.350 | ||||
| <10 y | 12 | 0.92 (0.88, 0.97) | 0.086 | 38.2 | |
| ≥10 y | 3 | 0.75 (0.48, 1.18) | 0.036 | 70.0 | |
| Quality score of cohorts3 | 0.350 | ||||
| Low quality | 12 | 0.92 (0.88, 0.97) | 0.086 | 38.2 | |
| High quality | 3 | 0.75 (0.48, 1.18) | 0.036 | 70.0 | |
| Subgroup analysis for adherence to the Mediterranean diet and 5-y weight change | |||||
|---|---|---|---|---|---|
| Effect sizes, n | β coefficient (95% CI) | P within1 | I 2 (%) | P between2 | |
| Overall | 13 | −0.04 (−0.07, −0.02) | <0.001 | 83.3 | |
| Gender | <0.001 | ||||
| Male | 1 | −0.53 (−0.73, −0.33) | — | — | |
| Female | 4 | −0.03 (−0.07, 0.02) | 0.003 | 78.2 | |
| Both | 8 | −0.04 (−0.06, −0.01) | <0.001 | 78.8 | |
| Dietary assessment method | <0.001 | ||||
| FFQ | 4 | −0.01 (−0.03, 0.01) | 0.061 | 59.4 | |
| 24-h recall | 2 | −0.48 (−0.65, −0.31) | 0.335 | 0.0 | |
| Country-specific questionnaires | 5 | −0.06 (−0.10, −0.02) | 0.003 | 74.6 | |
| FFQ + food record | 2 | −0.01 (−0.03, 0.01) | 0.395 | 0.0 | |
| Mediterranean diet definition | 0.062 | ||||
| Trichopoulou | 3 | −0.27 (−0.68, 0.13) | <0.001 | 93.7 | |
| Others | 10 | −0.04 (−0.06, −0.02) | <0.001 | 75.4 | |
| Follow-up duration | 0.001 | ||||
| <10 y | 9 | −0.04 (−0.07, −0.02) | 0.001 | 70.5 | |
| ≥10 y | 4 | −0.06 (−0.13, 0.01) | <0.001 | 90.8 | |
| Quality score of cohorts4 | 0.001 | ||||
| Low quality | 9 | −0.04 (−0.07, −0.02) | 0.001 | 70.5 | |
| High quality | 4 | −0.06 (−0.13, 0.01) | <0.001 | 90.8 | |
Values were obtained from random-effects model.
P for heterogeneity within subgroup obtained from random-effects model.
P for heterogeneity between subgroups obtained from fixed-effect model.
Quality scores were according to the Newcastle–Ottawa scale.
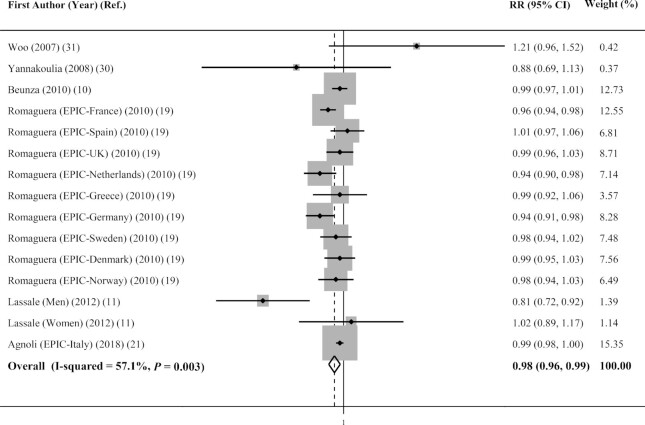
Findings from linear dose–response analysis on overweight and/or obesity
Six publications (10, 11, 19, 21, 30, 31) including 243,314 participants were included in the linear dose–response analysis. This analysis revealed that there was a 2% decreased risk of general overweight and/or obesity per 1 additional Mediterranean diet score (pooled RR = 0.98; 95% CI: 0.96, 0.99) (Figure 4). We did not perform a nonlinear meta-analysis because the number of eligible studies was limited (n = 2).
FIGURE 4.
Forest plot of cohort studies examining the linear dose–response association between Mediterranean diet adherence and risk of overweight and/or obesity in adults. The area of each shaded box is proportional to the weight of the study.
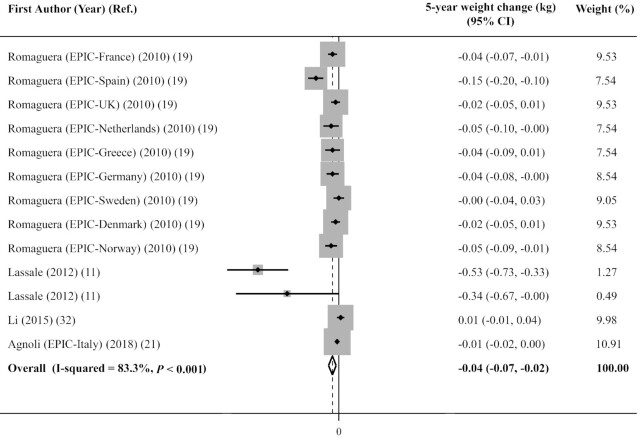
Findings from the meta-analysis on 5-y weight change
Figure 5 illustrates the combination of 13 effect sizes from 4 cohorts with 436,617 adults (9 additional effect sizes were from 1 cohort that separately reported effect sizes for 9 different countries and another study that separately reported effect sizes for males and females); we found that each unit increase in the Mediterranean diet score was significantly associated with 0.04 kg less weight gain over 5 y (−0.04 kg; 95% CI: −0.07, −0.02 kg). However, between-studies heterogeneity was high (I2 = 83.3%; PQ-test < 0.001). This heterogeneity remained significant even after subgroup analysis based on different variables (gender, dietary assessment method, Mediterranean diet definition, follow-up duration, and quality score of cohorts), as reported in Table 3. Sensitivity analysis showed that none of the included studies significantly influenced the overall effect size. There was evidence of potential publication bias based on the Begg test (P = 0.005) and Egger test (P = 0.006). The overall effect size did not change after trim-and-fill analysis.
FIGURE 5.
Forest plot of cohort studies examining the association between Mediterranean diet adherence and 5-y weight change in adults. The area of each shaded box is proportional to the weight of the study.
Discussion
This meta-analysis revealed that among 6 prospective cohort studies higher adherence to the Mediterranean diet was associated with a lower risk of overweight and/or obesity. Stratified analysis also showed that the highest adherence to the Mediterranean diet was associated with a lower risk of combined overweight and obesity (BMI ≥25), but not with obesity (BMI ≥30). Also, a weak, but significant, linear association was observed between the Mediterranean diet score and overweight and/or obesity. In addition, we found that the Mediterranean diet was significantly associated with less weight gain during 5 y of follow-up among 4 cohort studies. This association was present in almost all subgroups.
Considering the high prevalence of obesity and its relation to chronic disease, it is clinically necessary to maintain a healthful weight. Based on our findings, higher adherence to the Mediterranean diet was associated with a decreased risk of overweight and/or obesity as well as less weight gain in adults. Given these findings, adhering to the Mediterranean dietary pattern could be recommended to decrease the risk of overweight and obesity.
The association between the Mediterranean diet components and the risk of obesity and weight gain has been previously investigated. Based on the Mediterranean diet recommendations, meat and dairy intakes should be lowered. The Italian cohort study by Agnoli et al. (21) showed that removing meat products from the Mediterranean diet score made the association between this score and less weight gain and obesity nonsignificant. Therefore, meat products might have a significant influence on weight gain and obesity. Similarly, 2 meta-analyses found that higher consumption of both red and processed meat was significantly associated with increased risk of general and abdominal obesity as well as weight gain (33, 34). This might be due to the high energy density and fat content of red meat, which might alter appetite signaling (35). Furthermore, consuming high amounts of red meat might be a reflection of an unhealthy dietary pattern and more detrimental lifestyle habits (35). In the aforementioned meta-analysis, no association between dairy products and overweight and/or obesity was found (34). However, it did show an inverse association between highly recommended components of the Mediterranean diet and overweight and/or obesity (34). Moreover, results from 3 prospective studies showed that unlike fruits and vegetables, starchy foods and refined grains were related to higher weight gain (36). These controversies might be attributed to different components and methods used to assess the Mediterranean diet score and different confounders controlled in each study. Several methods have been developed to evaluate adherence to the Mediterranean diet. These methods are mostly based on the dietary components, which reflect local food intake patterns. Moreover, some food groups are combined to define a single component. Also, these scoring methods are based on the amounts consumed of each food group, which differ considerably in each population. Therefore, the above-mentioned differences could potentially change the level of adherence to the Mediterranean diet in different populations. In addition, controlling confounders is necessary to find the independent association between 2 variables of interest; however, taking different confounders into account might shift the results to either a significant or nonsignificant association.
We found an inverse association between Mediterranean diet and risk of overweight and/or obesity and weight gain. Two reports on the EPIC cohort study have also revealed a significant association between higher adherence to the Mediterranean diet and waist circumference (21, 37); however, 2 other cohorts did not confirm this finding (32, 38). Another cohort study of postmenopausal women observed no significant association between the highest adherence to Mediterranean diet and risk of weight gain (22). It is worth noting that underreporting of diet and weight is common in overweight/obese individuals, especially female individuals (39). This might be why previous studies mostly found a strong inverse association between the Mediterranean diet and weight gain in normal-weight individuals (19, 21). Unlike most prior cohorts, which considered baseline adherence to the Mediterranean diet as the exposure of interest, Fung et al. (14) investigated the change in adherence to the Mediterranean diet over the follow-up duration to decrease the possibility of reverse causation. Remarkably, they found a stronger inverse association between the Mediterranean diet and weight gain in the individuals who were overweight and obese at baseline (14). This means that people change their diet in an effort to lose weight; therefore, the association in individuals with BMI ≥25 was stronger.
Findings of previous randomized control trials (RCTs) are in agreement with our findings. A recent meta-analysis showed that following a Mediterranean diet significantly reduced body weight (−1.72 kg; 95% CI: −2.40, −1.05 kg), BMI (−0.41; 95% CI: −0.71, −0.10), and waist circumference (−1.47 cm; 95% CI: −2.54, −0.39 cm) (40). In contrast, no significant effect was found in case of the total fat mass (−0.47 kg; 95% CI: −1.53, 0.60 kg) or percentage of body fat (−0.12%; 95% CI: −1.60%, 1.37%). Another meta-analysis revealed that a 6-mo intervention with the Mediterranean diet could lower body weight by 2.87 kg (41). It should be considered that these interventions are usually conducted on obese individuals or individuals at high risk of CVDs. Furthermore, RCTs cannot reflect the routine dietary intakes of people. Therefore, findings of interventions could not be compared directly with those from prospective cohort studies.
Several mechanisms might clarify the linkage between adherence to a Mediterranean diet and weight status. Most previous findings have focused on the satiety-inducing properties of the Mediterranean diet and, therefore, its ability to lower energy intake. This characteristic is mainly attributed to the Mediterranean diet components. On the one hand, high consumption of fruits and vegetables is recommended in the Mediterranean diet. Therefore, this diet contains relatively large amounts of dietary fiber. High-fiber foods need more mastication, which could increase cholecystokinin release (42, 43). This, in turn, could provoke satiety and the sensation of fullness. Furthermore, consuming high-fiber foods leads to increased bacterial production of SCFAs in the intestine (43). SCFAs in the liver might activate AMP-activated protein kinase (43). This enzyme might have positive effects on abdominal obesity because of its role in metabolic homeostasis (43). On the other hand, the Mediterranean diet consists mostly of low glycemic index (GI) carbohydrates (such as whole grains). Lower-GI foods attenuate insulin secretion, which is an anabolic hormone (44), and result in less weight gain (44). Moreover, lower-GI foods might delay the hunger sensation, and therefore lead to decreased energy intake (45). It is also worth mentioning that the Mediterranean diet mostly recommends beneficial fat sources, including olive oil and fish (10). Therefore, this could minimize concerns about its high fat content (10).
There are some strengths in the present meta-analysis. This is the first and most comprehensive meta-analysis that examines the association between the Mediterranean diet and overweight and/or obesity and weight change in adults. Also, only prospective studies were included; thus, recall and selection bias are trivial. In addition, subgroup analyses based on several confounders were done. Furthermore, a dose–response meta-analysis was performed and revealed a linear association between the Mediterranean diet and the risk of overweight and/or obesity. Besides these strengths, we need to acknowledge some limitations in our investigation. Dietary intake and anthropometric values have been assessed with self-reported questionnaires in most eligible studies. The assessment methods for the Mediterranean diet adherence varied among the studies. Also, different questionnaires were used to assess individuals’ dietary intake. Not all the investigations reported the association between the Mediterranean diet and outcomes of interest in males and females separately. These limitations could lead to the observed between-study heterogeneity that did not completely resolve in subgroup analyses. Most of the eligible studies were conducted in the Mediterranean nations; therefore, we should cautiously extrapolate our findings to other non-Mediterranean countries. Furthermore, ignoring potential confounders including energy intake in some included studies might result in misleading conclusions about the effect of Mediterranean diet adherence on the outcomes of interest. Moreover, the overall effect size in low-quality studies was smaller than that in high-quality investigations (RR = 0.92 compared with 0.75). This overall effect size for low-quality studies was significant, but the pooled RR for high-quality studies was nonsignificant, probably due to the low number of included studies. Low-quality investigations were those in which >20% of their participants were lost to follow-up, studied nonrepresentative populations, and did not consider energy intake as the major confounder in their analysis. Therefore, more high-quality prospective studies without these limitations are required to shed light on the associations.
Conclusion
In conclusion, we found that the Mediterranean diet adherence was inversely associated with risk of overweight and/or obesity. Moreover, a significant inverse association was found between the Mediterranean diet score and 5-y weight gain. Considering the pandemic prevalence of overweight and obesity, even a minimal advantage of Mediterranean diet adherence to reduce this prevalence would have a substantial clinical impact for the entire population.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—KL: contributed to the literature search, screening, data extraction, and drafting of the manuscript; PS: contributed to the literature search, data extraction, statistical analyses, interpretation of data, and drafting of the manuscript; ZH: contributed to the literature search, screening, and data extraction; AE: contributed to the conception, design, statistical analyses, interpretation of the data, and drafting of the manuscript, and supervised the study; and all authors: read and approved the final manuscript.
Notes
Financial support for conception, design, data analysis, and manuscript drafting comes from the Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran (no. 240043).
Author disclosures: The authors report no conflicts of interest.
Supplemental Tables 1–4 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
Abbreviations used: CVD, cardiovascular disease; EPIC, European Prospective Investigation into Cancer and Nutrition; GI, glycemic index; MeSH, Medical Subject Headings; NOS, Newcastle–Ottawa scale; RCT, randomized control trial; SUN, Seguimiento Universidad de Navarra.
Contributor Information
Keyhan Lotfi, Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran.
Parvane Saneei, Department of Community Nutrition, School of Nutrition and Food Science, Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Zahra Hajhashemy, Department of Community Nutrition, School of Nutrition and Food Science, Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Ahmad Esmaillzadeh, Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran; Department of Community Nutrition, School of Nutrition and Food Science, Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran; Obesity and Eating Habits Research Center, Endocrinology and Metabolism Molecular-Cellular Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
References
- 1. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608. [DOI] [PubMed] [Google Scholar]
- 2. Dernini S, Berry EM, Serra-Majem L, La Vecchia C, Capone R, Medina F, Aranceta-Bartrina J, Belahsen R, Burlingame B, Calabrese G et al. Med diet 4.0: the Mediterranean diet with four sustainable benefits. Public Health Nutr. 2017;20(7):1322–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eleftheriou D, Benetou V, Trichopoulou A, La Vecchia C, Bamia C. Mediterranean diet and its components in relation to all-cause mortality: meta-analysis. Br J Nutr. 2018;120(10):1081–97. [DOI] [PubMed] [Google Scholar]
- 4. GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Di Angelantonio E, Bhupathiraju SN, Wormser D, Gao P, Kaptoge S, de Gonzalez AB, Cairns BJ, Huxley R, Jackson CL, Joshy G et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bertoli S, Leone A, Vignati L, Bedogni G, Martínez-González MÁ, Bes-Rastrollo M, Spadafranca A, Vanzulli A, Battezzati A. Adherence to the Mediterranean diet is inversely associated with visceral abdominal tissue in Caucasian subjects. Clin Nutr. 2015;34(6):1266–72. [DOI] [PubMed] [Google Scholar]
- 7. Zappalà G, Buscemi S, Mulè S, La Verde M, D'Urso M, Corleo D, Marranzano M. High adherence to Mediterranean diet, but not individual foods or nutrients, is associated with lower likelihood of being obese in a Mediterranean cohort. Eat Weight Disord. 2018;23(5):605–14. [DOI] [PubMed] [Google Scholar]
- 8. Buckland G, Bach A, Serra-Majem L. Obesity and the Mediterranean diet: a systematic review of observational and intervention studies. Obes Rev. 2008;9(6):582–93. [DOI] [PubMed] [Google Scholar]
- 9. Grosso G, Marventano S, Yang J, Micek A, Pajak A, Scalfi L, Galvano F, Kales SN. A comprehensive meta-analysis on evidence of Mediterranean diet and cardiovascular disease: are individual components equal?. Crit Rev Food Sci Nutr. 2017;57(15):3218–32. [DOI] [PubMed] [Google Scholar]
- 10. Beunza J-J, Toledo E, Hu FB, Bes-Rastrollo M, Serrano-Martínez M, Sanchez-Villegas A, Martínez JA, Martínez-González MA. Adherence to the Mediterranean diet, long-term weight change, and incident overweight or obesity: the Seguimiento Universidad de Navarra (SUN) cohort. Am J Clin Nutr. 2010;92(6):1484–93. [DOI] [PubMed] [Google Scholar]
- 11. Lassale C, Fezeu L, Andreeva V, Hercberg S, Kengne A, Czernichow S, Kesse-Guyot E. Association between dietary scores and 13-year weight change and obesity risk in a French prospective cohort. Int J Obes. 2012;36(11):1455–62. [DOI] [PubMed] [Google Scholar]
- 12. Mendez MA, Popkin BM, Jakszyn P, Berenguer A, Tormo MJ, Sanchéz MJ, Quirós JR, Pera G, Navarro C, Martinez C et al. Adherence to a Mediterranean diet is associated with reduced 3-year incidence of obesity. J Nutr. 2006;136(11):2934–8. [DOI] [PubMed] [Google Scholar]
- 13. Esposito K, Kastorini C-M, Panagiotakos DB, Giugliano D. Mediterranean diet and weight loss: meta-analysis of randomized controlled trials. Metab Syndr Relat Disord. 2011;9(1):1–12. [DOI] [PubMed] [Google Scholar]
- 14. Fung TT, Pan A, Hou T, Chiuve SE, Tobias DK, Mozaffarian D, Willett WC, Hu FB. Long-term change in diet quality is associated with body weight change in men and women. J Nutr. 2015;145(8):1850–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kang M, Boushey CJ, Shvetsov YB, Setiawan VW, Paik H-Y, Wilkens LR, Le Marchand L, Park S-Y. Changes in diet quality and body weight over 10 years: the Multiethnic Cohort Study. Br J Nutr. [Internet] 2021. doi:10.1017/S000711452100012X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tobias DK, Zhang C, Chavarro J, Olsen S, Bao W, Bjerregaard AA, Fung TT, Manson J, Hu FB. Healthful dietary patterns and long-term weight change among women with a history of gestational diabetes mellitus. Int J Obes. 2016;40(11):1748–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sanchez-Villegas A, Bes-Rastrollo M, Martinez-Gonzalez M, Serra-Majem L. Adherence to a Mediterranean dietary pattern and weight gain in a follow-up study: the SUN cohort. Int J Obes. 2006;30(2):350–8. [DOI] [PubMed] [Google Scholar]
- 18. May AM, Romaguera D, Travier N, Ekelund U, Bergmann MM, Kaaks R, Teucher B, Steffen A, Boeing H, Halkjaer J et al. Combined impact of lifestyle factors on prospective change in body weight and waist circumference in participants of the EPIC-PANACEA study. PLoS One. 2012;7(11):e50712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Romaguera D, Norat T, Vergnaud A-C, Mouw T, May AM, Agudo A, Buckland G, Slimani N, Rinaldi S, Couto E et al. Mediterranean dietary patterns and prospective weight change in participants of the EPIC-PANACEA project. Am J Clin Nutr. 2010;92(4):912–21. [DOI] [PubMed] [Google Scholar]
- 20. Roswall N, Ängquist L, Ahluwalia TS, Romaguera D, Larsen SC, Østergaard JN, Halkjaer J, Vimaleswaran KS, Wareham NJ, Bendinelli B et al. Association between Mediterranean and Nordic diet scores and changes in weight and waist circumference: influence of FTO and TCF7L2 loci. Am J Clin Nutr. 2014;100(4):1188–97. [DOI] [PubMed] [Google Scholar]
- 21. Agnoli C, Sieri S, Ricceri F, Giraudo MT, Masala G, Assedi M, Panico S, Mattiello A, Tumino R, Giurdanella MC et al. Adherence to a Mediterranean diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr Diabetes. 2018;8(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ford C, Chang S, Vitolins MZ, Fenton JI, Howard BV, Rhee JJ, Stefanick M, Chen B, Snetselaar L, Urrutia R et al. Evaluation of diet pattern and weight gain in postmenopausal women enrolled in the Women's Health Initiative Observational Study. Br J Nutr. 2017;117(8):1189–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: 2000. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- 24. Chêne G, Thompson SG. Methods for summarizing the risk associations of quantitative variables in epidemiologic studies in a consistent form. Am J Epidemiol. 1996;144(6):610–21. [DOI] [PubMed] [Google Scholar]
- 25. Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279(18):1477–82. [DOI] [PubMed] [Google Scholar]
- 26. Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. London (UK): Routledge; 2013. [Google Scholar]
- 27. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. 2nd edition. Chichester (UK): John Wiley & Sons; 2019. [Google Scholar]
- 28. Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135(11):1301–9. [DOI] [PubMed] [Google Scholar]
- 29. Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose–response data. Stata J. 2006;6(1):40–57. [Google Scholar]
- 30. Yannakoulia M, Panagiotakos D, Pitsavos C, Lentzas Y, Chrysohoou C, Skoumas I, Stefanadis C. Five-year incidence of obesity and its determinants: the ATTICA study. Public Health Nutr. 2009;12(1):36–43. [DOI] [PubMed] [Google Scholar]
- 31. Woo J, Cheung B, Ho S, Sham A, Lam T. Influence of dietary pattern on the development of overweight in a Chinese population. Eur J Clin Nutr. 2008;62(4):480–7. [DOI] [PubMed] [Google Scholar]
- 32. Li Y, Roswall N, Ström P, Sandin S, Adami H-O, Weiderpass E. Mediterranean and Nordic diet scores and long-term changes in body weight and waist circumference: results from a large cohort study. Br J Nutr. 2015;114(12):2093–102. [DOI] [PubMed] [Google Scholar]
- 33. Rouhani M, Salehi-Abargouei A, Surkan P, Azadbakht L. Is there a relationship between red or processed meat intake and obesity? A systematic review and meta-analysis of observational studies. Obes Rev. 2014;15(9):740–8. [DOI] [PubMed] [Google Scholar]
- 34. Schlesinger S, Neuenschwander M, Schwedhelm C, Hoffmann G, Bechthold A, Boeing H, Schwingshackl L. Food groups and risk of overweight, obesity, and weight gain: a systematic review and dose-response meta-analysis of prospective studies. Adv Nutr. 2019;10(2):205–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vergnaud A-C, Norat T, Romaguera D, Mouw T, May AM, Travier N, Luan Ja, Wareham N, Slimani N, Rinaldi S et al. Meat consumption and prospective weight change in participants of the EPIC-PANACEA study. Am J Clin Nutr. 2010;92(2):398–407. [DOI] [PubMed] [Google Scholar]
- 36. Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Romaguera D, Norat T, Mouw T, May AM, Bamia C, Slimani N, Travier N, Besson H, Luan Ja, Wareham N et al. Adherence to the Mediterranean diet is associated with lower abdominal adiposity in European men and women. J Nutr. 2009;139(9):1728–37. [DOI] [PubMed] [Google Scholar]
- 38. Esfandiari S, Bahadoran Z, Mirmiran P, Tohidi M, Azizi F. Adherence to the dietary approaches to stop hypertension trial (DASH) diet is inversely associated with incidence of insulin resistance in adults: the Tehran lipid and glucose study. J Clin Biochem Nutr. 2017;61(2):123–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Robinson E. Overweight but unseen: a review of the underestimation of weight status and a visual normalization theory. Obes Rev. 2017;18(10):1200–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Papadaki A, Nolen-Doerr E, Mantzoros CS. The effect of the Mediterranean diet on metabolic health: a systematic review and meta-analysis of controlled trials in adults. Nutrients. 2020;12(11):3342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ge L, Sadeghirad B, Ball GD, da Costa BR, Hitchcock CL, Svendrovski A, Kiflen R, Quadri K, Kwon HY, Karamouzian M et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ. 2020;369:m969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Miquel-Kergoat S, Azais-Braesco V, Burton-Freeman B, Hetherington MM. Effects of chewing on appetite, food intake and gut hormones: a systematic review and meta-analysis. Physiol Behav. 2015;151:88–96. [DOI] [PubMed] [Google Scholar]
- 43. Burton-Freeman B, Davis PA, Schneeman BO. Plasma cholecystokinin is associated with subjective measures of satiety in women. Am J Clin Nutr. 2002;76(3):659–67. [DOI] [PubMed] [Google Scholar]
- 44. Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002;287(18):2414–23. [DOI] [PubMed] [Google Scholar]
- 45. Chang KT, Lampe JW, Schwarz Y, Breymeyer KL, Noar KA, Song X, Neuhouser ML. Low glycemic load experimental diet more satiating than high glycemic load diet. Nutr Cancer. 2012;64(5):666–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.