Abstract
Background
Cyclooxygenase (COX) enzymes oxidise arachidonic acid to prostaglandins, which modulate neuronal function and inflammation in the central nervous system. Consensus guidelines suggest non-steroidal anti-inflammatory drugs as a possible adjunctive approach in adults with obsessive–compulsive disorder (OCD) and in children with acute-onset OCD subtypes. However, there is limited evidence to support this approach. The primary objective of this study is to determine the efficacy of the COX-2-selective inhibitor celecoxib as an adjunct to treatment-as-usual in children and youth with moderate-to-severe OCD. The safety of this intervention including adverse events will also be systematically assessed.
Methods
The Adjunctive CElecoxib in childhood-onset OCD (ACE-OCD) study is a single-centre randomised, quadruple-blind, placebo-controlled superiority trial with two parallel groups: celecoxib 100 mg twice daily and placebo. Treatments will be added to participants’ routine clinical care, which will not change over the course of the study. Target recruitment is 80 participants ages 7–18 with no recent treatment changes. The primary outcome is OCD severity after 12 weeks of treatment, measured by clinician-administered Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS). Secondary outcomes include CY-BOCS score after 6 weeks; difference in the proportion of participants achieving a clinically meaningful response or remission; mean clinical global impression of severity and improvement after 6 and 12 weeks; and proportion of participants reporting adverse events possibly or probably related to the study intervention. The primary analyses, carried out according to intention-to-treat principles, will compare the celecoxib to placebo group on each outcome of interest, adjusting for baseline scores using analysis of covariance or logistic regression. Participants will be offered a 12-week open-label celecoxib extension and will be invited to participate in an ancillary study for biomarker analyses.
Ethics and dissemination
This protocol has been approved by the University of British Columbia Children’s and Women’s Research Ethics Board and has received a No Objection Letter from Health Canada. The findings will be disseminated in peer-reviewed journals and presentations to multiple stakeholders including patients, parents and healthcare providers.
Trial registration number
Keywords: child & adolescent psychiatry, immunology, mental health
Strengths and limitations of this study.
This study is the first randomised, placebo-controlled trial to evaluate the efficacy and safety of adjunctive non-steroidal anti-inflammatory drug therapy in childhood-onset obsessive–compulsive disorder and does not restrict participants to a diagnosis of paediatric acute-onset neuropsychiatric syndrome or paediatric autoimmune neuropsychiatric disorder associated with streptococcal infections.
Study visits may occur virtually and screening blood work can be completed in participants’ local communities, increasing accessibility for participants.
Participants will have the option to consent to an ancillary study involving biosample collection for correlative biology; this will provide preliminary longitudinal data allowing measurement of associations between inflammatory biomarkers and clinical phenotype.
This study incorporates assessment of participants’ and parents’ perspectives on participation, including their experience of virtual visits, to inform future studies of psychopharmacologic interventions in this population.
While heterogeneity of usual therapy may limit power to detect differences between arms, this represents a more pragmatic approach than contemporaneous initiation of a selective serotonin reuptake inhibitor as described in preliminary studies in adults.
Introduction
Obsessive–compulsive disorder (OCD) is a common neuropsychiatric condition identified by the World Health Organisation as one of the leading causes of worldwide medical disability.1 It affects 1%–3% of the population and places significant burden on patients, families and healthcare systems.2 Childhood-onset OCD (CO-OCD) represents a specific subtype with unique epidemiological, aetiological and clinical characteristics.3 4 Although cognitive–behavioural therapy and serotonin reuptake inhibitors (SRIs) are effective treatments, there is a critical need to develop novel and augmenting agents for patients with enduring symptoms.
A large body of work suggests an association between infection and an abrupt, early-onset form of OCD, termed paediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS),5 as well as paediatric acute neuropsychiatric syndrome (PANS).6 Recent epidemiological data suggest that recurrent episodes of infection and inflammation are associated with the development of multiple mental disorders in children,7 including ‘classic’ OCD.8 Moreover, patients with autoimmune disorders have higher rates of comorbid OCD compared with the general population.9 10 A recent cohort study based on Swedish National Register data suggested increased rates of multiple autoimmune diseases among patients with OCD and their first-degree relatives11; we have also described higher-than-expected rates of immune-related conditions in individuals with CO-OCD.12 Positron emission tomography imaging in adults with OCD has demonstrated increased volume of translocator protein-18 distribution in cortico-striato-thalamo-cortical circuits, implicating widespread microglial activation.13 It is unclear whether changes in cellular and soluble inflammatory markers represent underlying aetiology, a consequence of disease progression or associated epiphenomena.
Non-steroidal anti-inflammatory drugs (NSAIDs) inhibit cyclooxygenase (COX) enzymes, which catalyse the metabolism of arachidonic acids to prostanoids. COX-2 and its products play an important physiological role in synaptic plasticity and long-term potentiation and may also contribute to neuropathology by enhancing glutamate excitotoxicity, promoting neuronal cell death and oxidising endogenous cannabinoids.14 15 Recent meta-analyses suggest a potential role of adjunctive COX-2 inhibitors in the treatment of depression16 and first-episode schizophrenia,17 18 with additional small studies suggesting possible benefit in neurodevelopmental conditions including autism spectrum disorder.19 20 Behavioural effects of COX inhibition may relate not only to anti-inflammatory activity but also to direct effects on neuronal function and synaptic transmission. Consensus guidelines on the use of anti-inflammatory therapy in children with PANDAS suggest NSAIDs as first-line options for patients with mild impairment.21 However, a recent systematic review of treatment for PANS/PANDAS found insufficient evidence to support this practice.22 In adults with OCD, three small randomised controlled trials (RCTs) have suggested modest symptom improvement with celecoxib as an adjunct to fluoxetine,21 fluvoxamine23 24 or other selective serotonin reuptake inhibitors.25 This raises the possibility that COX-2 inhibition may be effective in a general OCD population.26 However, no controlled studies to date have tested the effects of COX inhibitors in CO-OCD. This study will determine the efficacy of the COX-2-selective inhibitor celecoxib as an adjunct to treatment-as-usual in children and youth with moderate-to-severe OCD. There is no cost to participate in the study.
Methods and design
Study design
The ACE-OCD trial is a randomised, quadruple-blind, placebo-controlled, single-site study comparing a 12-week course of twice daily celecoxib with placebo as an adjunct to treatment-as-usual in children and youth with moderate-to-severe OCD between the ages of 7 and 18. The protocol was drafted in accordance with the Standard Protocol Items: Recommendations for Interventional Trials statement.27 All parents/guardians participating in the study will give electronically-documented informed consent; child and youth participants will provide informed assent or consent.
Study setting
This is a single-site study based at the British Columbia Children’s Hospital (BCCH) Provincial OCD Program in Vancouver, BC, Canada. Study visits will be conducted virtually, using electronic-consent and survey platforms through Research Electronic Data Capture (REDCap) and Zoom, an online videoconference platform that complies with the Personal Information Protection and Electronic Documents Act and the Personal Health Information Protection Act. Participants will continue to receive treatment-as-usual from their regular healthcare providers, which will not change as a result of participation in this study.
Patient selection
Participants will be recruited from BCCH and based on self-referral through community paediatrics, psychiatry, and psychology practices. Participants may be receiving concurrent pharmacotherapy or psychotherapy according to their routine clinical care, constituting ‘treatment-as-usual’ as long as there have been no changes in the preceding 4 weeks and during the study period. They must have a previous diagnosis of OCD. Participants with PANS or PANDAS who also meet diagnostic criteria for OCD are eligible to participate. Refer to table 1 for full inclusion and exclusion criteria.
Table 1.
Inclusion and exclusion criteria
| Criterion | Items |
| Inclusion |
|
| Exclusion |
|
BCCH, British Columbia Children’s Hospital; CBT, cognitive–behavioural therapy; NSAIDs, non-steroidal anti-inflammatory drugs; OCD, obsessive–compulsive disorder.
Allocation and randomisation
Participants will be randomly assigned to either placebo or celecoxib with a 1:1 allocation as per a computer-generated randomisation schedule stratified by baseline CY-BOCS score (16–23 versus ≥24) using permuted blocks of random sizes of 2 and 4. Specific information regarding the allocation sequence will be stored in a separate document with access restricted to the study’s statistician, the research pharmacist and a research assistant (RA) not involved in the study. The block sizes will not be disclosed to trial implementers.
Blinding
Trial participants, investigators, care providers and outcome assessors will be blinded to treatment allocation. Placebo capsules will be identical in appearance to celecoxib capsules. Unique randomisation codes will be used for each participant to avoid inadvertent loss of blinding for all participants in the event that one is unblinded. Data analysis and manuscript writing will be performed after unblinding once data have been cleaned for primary and secondary endpoints and adverse events (AEs). Participants will be provided with an option to be contacted and informed of their allocation at that time. Emergency unblinding will occur only in exceptional circumstances when required to maintain participant safety—that is, when knowledge of the actual treatment is essential for further management. The blind will be maintained as far as possible and will not be disclosed to other study personnel unless required for patient management. Unblinding will not be a reason for study drug discontinuation.
Sample size calculation
The sample size of 80 participants (40 per arm) was estimated on the basis of the primary hypothesis. If we assume a power to detect a minimally clinically significant between-group difference in CY-BOCS scores of 2.5 with an SD of 5 (equivalent to a Cohen’s d effect size of 0.5 and roughly based on two existing studies of adjunctive celecoxib in adults23 24) a correlation of 0.5 between baseline and final CY-BOCS score, and a sample size of 40 participants per arm, we will have power of 80% to detect a between-group difference using a directional, one-tailed alpha (celecoxib<placebo) using analysis of covariance. Missing follow-up data due to attrition will be imputed (as described in detail in the Statistical Analysis section below). Our recruitment target is similar to pilot studies of adjunctive celecoxib in other psychiatric disorders.19
Interventions
Eligible patients will be randomised to a 12-week course of either celecoxib (generic form) or placebo containing microcrystalline cellulose. Participants receiving celecoxib with weight between 10 and 25 kg, inclusive, will receive 50 mg two times per day (2–5 mg/kg per dose); those >25 kg will receive 100 mg two times per day as per Food and Drug Administration (FDA)-approved paediatric dosing in children (maximum 4 mg/kg per dose). The placebo capsule is effectively indistinguishable from that of the drug. Participants will be instructed to take the capsule with food to reduce the risk of gastrointestinal side effects. Those unable to swallow a capsule may sprinkle the contents on moist food, given similar pharmacokinetics compared with an intact capsule.28 Adherence will be documented by capsule count and adherence questionnaires. Weekly adherence reminders will be provided by email or text. Participants will also be asked to maintain an electronic diary documenting the first dose, missed doses, AEs and changes to the usual way they take the capsule.
Participant schedule and follow-up
Prior to their first study visit, parents/guardians of participants who provide informed consent will complete a full eligibility screening questionnaire followed by a diagnostic interview that includes the Mini International Neuropsychiatric Interview for Children and Adolescents, a short structured interview that covers a broad range of Diagnostic and Statistical Manual of Mental Disorders (DSM-5) psychiatric diagnoses in children and adolescents.29 Participants and their parents who are eligible to proceed to the first study visit will complete a demographic/medical questionnaire and Participant Perspective Questionnaire (PPQ) via REDCap prior to the first study visit.
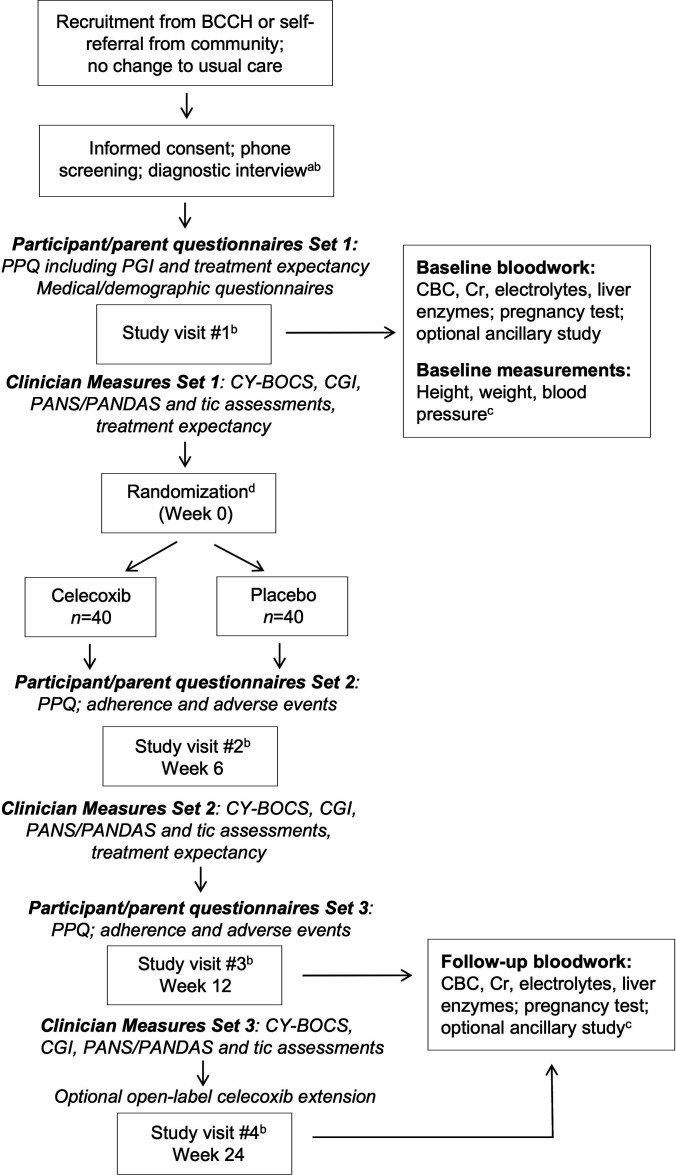
Study visits will proceed according to the flow chart in figure 1. Measures completed by a study physician at the first visit include the CY-BOCS30; Clinical Global Impression (CGI) scales31; review of diagnostic criteria for PANS/PANDAS, tic disorders and restricted food intake6 clinician treatment expectancy and clinician experience of remote study visits. Participants who continue to meet eligibility criteria after study visit 1 will be provided with a requisition for monitoring blood work if not already completed (complete blood count, creatinine, aspartate aminotransferase, alanine aminotransferase, electrolytes, pregnancy test). Participants will have the option to consent to participation in an ancillary study for biosample collection (blood, saliva, buccal swab and stool) for future analyses of inflammatory markers.
Figure 1.
Flow diagram of study visits and assessments. aMINI-Kid diagnostic interview administered by phone with the participant and parent present. bScreening and study visits may be conducted virtually according to patient preference and current COVID-19 restrictions. cHeight, weight and blood pressure will be determined either on-site or by a participant’s regular care provider. dParticipants will inform study staff of the date and time of their first dose. Weekly reminders regarding adherence and completion of the participant e-diary as required will be sent via email, phone or text according to participant preference and consent. CY-BOCS, Children’s Yale-Brown Obsessive Compulsive Scale; BCCH, British Columbia Children’s Hospital; CGI, Clinical Global Impression; PANDAS, paediatric autoimmune neuropsychiatric disorder associated with streptococcal infections; PANS, paediatric acute-onset neuropsychiatric syndrome; PGI, Patient/Parent Global Impression; PPQ, Participant Perspective Questionnaire.
For participants who remain eligible for randomisation, the BCCH Pharmacy will dispense the study drug or placebo according to an allocation sequence provided to them by the team’s statistician at a dose based on the patient’s weight. For visits 2-4, parents/participants will again complete a REDCap survey prior to each visit, including adherence and AE questionnaires. Participants will be provided with a requisition for blood work to be completed following visit 3. Participants with ongoing symptoms (CY-BOCS >8) at visit 3 will have the option to continue with a 12-week open-label extension with celecoxib, with a follow-up visit and monitoring blood work at 24 weeks.
Outcome parameters and statistical analyses
Primary outcome
The primary outcome is OCD severity as measured by total CY-BOCS score after 12 weeks in the celecoxib compared with placebo arm, adjusted for baseline OCD severity. This is a more powerful statistical approach in comparison to analysis of change scores.32
Secondary outcomes
Secondary outcomes include the following: (1) OCD severity after 6 weeks of treatment in the celecoxib compared with placebo arm, adjusted for baseline OCD severity; (2) difference in the proportion of participants achieving a clinically meaningful response (defined as a 25% reduction in the CY-BOCS score or CGI-I of 1 or 2 based on previous meta-analyses33 after 6 and 12 weeks of treatment in the celecoxib compared with placebo arm; (3) difference in the proportion of participants achieving clinical remission (CY-BOCS ≤14) after 6 and 12 weeks of treatment in the celecoxib compared with placebo arm; (4) mean CGI of severity (CGI-S) after 6 and 12 weeks in the celecoxib compared with placebo arm, adjusted for baseline OCD severity; (5) mean CGI of improvement (CGI-I) after 6 and 12 weeks in the celecoxib compared with placebo arm, adjusted for baseline OCD severity and (6) difference between celecoxib and placebo arms in the proportion of participants reporting AEs that are possibly, probably or definitely related to the study intervention. Definitions of response and remission are applied as described previously to allow for cross-study comparability.34
Exploratory outcomes
Exploratory analyses will include determination of the associations among age, sex, race/ethnicity, body mass index (BMI) percentile, treatment at baseline, severity at baseline, presence/severity of PANS/PANDAS symptoms or tics at any time point based on clinician assessment, medical/psychiatric comorbidities, time since diagnosis, scores on parent perspective questionnaire items, clinician treatment expectancy, and the primary and secondary outcomes. Additional measures of severity will be included in exploratory analyses and collected at all time points, including self-report and parent-report versions of the CY-BOCS and Obsessive Compulsive Inventory-Child Version (table 2).
Table 2.
Description of measures included in the parent/participant perspective questionnaire
| Measure | Outcome |
| Patient/Parent Global Impression Scales for Severity and Improvement | Severity and improvement in OCD and tic symptoms, based on a standard 7-point Likert scale derived from the Clinician Global Impression scales.53 |
| PANS rating scale | Severity and change in PANS/PANDAS symptoms38 |
| National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS) measures | Patient-reported measures of (1) global health and (2) pain intensity, including 8 items overall.54 55 |
| Treatment expectancy | Two items assuming assignment of the participant to either placebo or active drug. Rated on a 7-point Likert scale, previously linked with treatment response and lower attrition in a clinical trial of CBT for youth with OCD.56 |
| Self-reported OCD severity | Self-report CY-BOCS, combining scores for obsessions and compulsions to generate a total score out of 20, consistent with recommendations based on a recent study of CY-BOCS construct validity.57 |
| Self-report and parent-report versions of the Obsessive Compulsive Inventory-Child Version | 21-item self-report measure that assesses obsessive-compulsive symptoms in children and adolescents aged 7–17 years over the preceding month.58 |
| Postvisit questionnaire items | Likert-scale and open-ended items querying participant experiences with virtual visits and trial participation, based on previous work but tailored to this current study.59 |
CBT, cognitive–behavioural therapy; CY-BOCS, Children’s Yale-Brown Obsessive Compulsive Scale; OCD, obsessive–compulsive disorder; PANDAS, paediatric autoimmune neuropsychiatric disorder associated with streptococcal infections; PANS, paediatric acute-onset neuropsychiatric syndrome.
Outcome measures
Children’s Yale-Brown Obsessive Compulsive Scale
OCD severity will be assessed using the CY-BOCS, a gold-standard clinician report measure.30 The CY-BOCS is the most widely used measure of clinician-rated OCD and its psychometric properties including validity and reliability have been supported across many studies.35 It is composed of two subscale total scores, Obsessions and Compulsions, each ranging from 0 to 20, with a higher score indicating greater symptom severity. These subscale scores are summed to provide a total score, ranging from 0 to 40, that is used to measure overall OCD symptom severity. We have also included additional items in the clinician assessment forms to allow calculation of a score for CY-BOCS-II, which has been recently validated and may be used in future studies.36
Clinical Global Impression
The CGI scale includes single-item, clinician-rated, 7-point Likert-type scales of severity and improvement. The CGI-S is a frequently-used measure for assessment of symptom severity across multiple psychiatric illnesses. Both face-to-face and video scoring are considered valid outcome measures suitable for use in trials of OCD treatment.37 The CGI-I typically but not always tracks with CGI-S31 and has been used to define treatment response in treatment trials of paediatric OCD.33
Participant Perspective Questionnaire
This is a study-specific questionnaire to be completed online by the participant and parent in conjunction with each study visit. Included measures are listed in table 2.
PANDAS/PANS scale
Included in the PPQ, this rating scale assesses severity and change in PANS/PANDAS symptoms and is a parent-report form based on criteria proposed by the PANS Consortium and described previously.38 This measure has also been used to capture PANS exacerbation, as it asks the rater whether each current symptom had been possibly worse (1 point), dramatically worse (2 points), new (3 points) or better/same (0 points) within the past week. The maximum score possible is 54.38
Clinician assessment
In addition to assessment of OCD severity, PANS/PANDAS diagnosis and review of tic symptoms/severity will be conducted by the clinician at all study visits. This will include CGI measures for tics and for food intake restriction (a PANS criterion). Clinicians will also complete several questions related to treatment expectancy and their experience of virtual study visits.
Adverse events
AEs will be systematically assessed at study visits 2-4 using a questionnaire adaptation of the Safety Monitoring Uniform Research Form (SMURF).39 The SMURF is an AE-elicitation tool specifically aimed at paediatric populations, developed by the NIMH-funded Research Units on Paediatric Psychopharmacology.39 A checklist will also be included in participant electronic diaries to allow for standardisation of reporting and to facilitate recall when completing the AE Questionnaire prior to the visit.
Adherence
Medication adherence questionnaires will be completed on REDCap by participants prior to visits 2-4 and will be reviewed with the family by the RA and study physician. This will consist of two questions regarding the frequency with which participants have taken all doses or missed one dose, with the response rated on a visual analogue scale. An open-ended question will be included regarding the reason for any missed doses. Adherence will also be assessed by capsule count at the end of the study.
Safety monitoring and interim analysis
This study will be reviewed by a data safety and monitoring board (DSMB). An interim analysis of recruitment rates and AEs will be conducted after the first 10 patients or the first year of recruitment. Unblinding of data will occur only at the request of the DSMB by a statistician not directly involved in the conduct of the study. No interim efficacy analysis is planned. Individual participants may be asked to leave the study for their own safety, in which case consensus of at least two study physicians will be required. Individual participants who withdraw from or complete the study will continue follow-up with their regular care providers.
Statistical analyses
Analyses will be carried out according to the intention-to-treat principle such that participants will be analysed according to the group to which they were randomised regardless of adherence. Descriptive statistics will be conducted on baseline variables to evaluate the characteristics of the total sample and subsamples in each treatment condition. The primary analyses will be conducted on two sets of data. First, the analyses will be conducted on complete case data, which is defined as the set of subjects without missing data on the variables included in the particular statistical model. Second, missing data will be multiply imputed using the multivariate imputation by chained equations approach, which is appropriate when data are missing at random or are missing completely at random.40 The imputation method for all variables will be semi-parametric predictive mean matching, which restricts imputations to the observed values in the data set. Common diagnostics, including visual inspection of trace plots and examination of R-hat values, will be used to ensure the validity of the imputation procedure. The imputation model will include baseline demographic and clinical characteristics used to form subgroups for exploratory analyses, treatment condition, baseline scores on outcomes measures, as well as observed follow-up scores on the outcomes of interest. The imputation model will create forty imputed data sets, on which statistical analyses will be performed. Statistical estimates will be pooled over the 40 imputed data sets using the Barnard-Rubin procedure to estimate pooled SEs and df.41
Primary analysis
The primary analyses will compare the celecoxib to the placebo group on the outcome of interest at weeks 6 and 12, adjusting for baseline scores on the outcome, using analysis of covariance (ANCOVA) for continuous outcomes and logistic regression for categorical outcomes. Additionally, baseline CY-BOCS will be included as a covariate in all analyses, even when CY-BOCS is not the outcome variable. ANCOVA produces unbiased treatment effect estimates and less variance in the treatment effect as compared with the commonly-used linear mixed model, resulting in superior statistical power.32 All continuous outcomes believed to be generated from a Gaussian distribution will be analysed using this approach.
The primary contrast for this study will be the between-group difference (celecoxib vs placebo) in CY-BOCS score at 12 weeks, adjusted for baseline CY-BOCS score, using multiply imputed data and complete case data. The estimated between-group difference using the multiply imputed data will be considered the primary estimate; the estimated between-group difference using complete case data will be considered secondary. The statistical significance threshold for this analysis will be set at a one-sided alpha=0.05, to test whether the celecoxib group has lower adjusted 12-week CY-BOCS scores compared with the placebo group. For this analysis, we will report the between-group point estimate, 95% CI, and p value to three decimal places. A pvalue less than 0.001 will be reported as p<0.001. Additional analyses of between-group differences in secondary outcomes and in symptom severity at the midpoint assessment will be considered descriptive and will be described using point estimates and 95% CIs.
Secondary analysis
Secondary analyses will include analysis of the proportion of patients in each group who achieve a 25% reduction in CY-BOCS score from baseline or CGI-I of 1 or 2 (treatment response) and who achieve a CY-BOCS score ≤14 (remission). Logistic regression will analyse between-group differences in this binary outcome (achieved ≥25% reduction vs did not), adjusting for baseline CY-BOCS score. Similarly, logistic regression will examine group differences in a binary AE variable (experienced at least one AE vs did not), also adjusting for baseline CY-BOCS score. Association between OCD symptoms, Patient/Parent Global Impression (PGI), and treatment expectancy will be estimated using linear regression modelling with treatment group, age, sex, BMI percentile, race/ethnicity, PANS/PANDAS status and tic status as covariates.
Other analysis
Data collected during the 12-week extension period will be reported in a descriptive fashion, for example, number of observations, percentages, means and SDs.
Patient and public involvement
The research question addressed by the study has been informed by discussions with families interested in trialling NSAID therapy and the current lack of evidence base to inform treatment recommendations. Feedback from families has been incorporated into trial design, including addition of an open-label phase. Procedures for recruitment, assessment, BioBank sample collection, outcome assessments, follow-up and results dissemination are common to other studies in the BCCH Provincial OCD Program that have provided both patients and families with an opportunity for input. Because this trial is unique in incorporating virtual/remote study visits for a pharmacological intervention within a paediatric psychiatric population in BC, participants’ perspectives on their participation may provide critical information relevant to the design of future studies.
Ethics and dissemination
Data collection and confidentiality
All data are handled confidentially and the information in the datasets for analyses is non-identifiable.
Ethics
A no objection letter has been received from Health Canada. This study has been approved by the University of British Columbia/Children’s and Women’s Health Centre of British Columbia Research Ethics Board.
Withdrawal
Patients will be informed of their right to withdraw from the study without explanation at any time.
Dissemination plan
The findings will be disseminated in peer-reviewed academic journals and presentations to multiple stakeholders including patients, parents and healthcare providers.
Discussion
This study will be the first to assess the efficacy of celecoxib in paediatric OCD. Multiple lines of evidence suggest behavioural effects of COX inhibition, which may relate not only to anti-inflammatory activity but also to direct effects on neuronal function and synaptic transmission. While clinical phenotyping will identify children meeting criteria for PANS/PANDAS, this work will also bring much-needed attention to a heterogeneous population of patients with OCD and may inform future trials of immune-modulating therapies. Participant perspectives on treatment expectancy, outcomes, and trial participation will be used to inform the design of future studies in this population.
Rationale for use of a COX-2-selective versus COX-1-selective inhibitor
While all NSAIDS appear to have anti-inflammatory, antipyretic, and analgesic properties attributable to prostaglandin inhibition, they vary with respect to COX selectivity42 and may have neuroprotective effects not directly related to their classic anti-inflammatory activity.43 44 In the CNS, modulation of glutamate, serotonin, norepinephrine and endocannabinoid signalling has been primarily demonstrated with COX-2 rather than COX-1 inhibitors.14 15 45–47 Other than a negative RCT of naproxen in geriatric depression48 and a study of adjuvant aspirin in schizophrenia,49 few RCTs have evaluated non-selective NSAIDs in primary psychiatric disorders. Given the significance of different COX isoforms and their unknown relative ‘potencies’ in the CNS, careful attention must be given to selection and evaluation of specific NSAIDs to better understand their neurobiology and clinical efficacy. This study uses celecoxib rather than naproxen given evidence of benefit in adults with OCD and preclinical data pointing to modulation of serotonin and glutamate. Celecoxib is also associated with fewer gastrointestinal side effects in adults.
Rationale for dosing regimen
The US FDA has approved the use of celecoxib in the paediatric population for the management of juvenile idiopathic arthritis (JIA)50 and it is available in the US to children from ages two and up based on a non-inferiority study comparing celecoxib with naproxen.51 A follow-up registry study from routine clinical practice included 274 children on NSAIDs and found that AEs were similar for non-selective NSAIDs and celecoxib, and that no serious AEs were attributed to NSAID use over a mean duration of treatment of 11–13 months.52 The dosages used were within the range of those tested in children with JIA over 12 weeks (3–6 mg/kg two times per day).51 To avoid exceeding plasma levels associated with the 6 mg/kg suspension, the FDA-approved capsule dosing will be used in this study.
Strengths and limitations of this study
While an RCT of naproxen in PANDAS is currently recruiting (NCT04015596), this study has broader inclusion criteria based on emerging evidence for inflammatory dysregulation in ‘classic’ OCD and existing data in adults. The pragmatic approach of adding celecoxib to treatment-as-usual is a potential strength reflecting typical use in clinical practice. Because of this, our study population is likely to be more heterogeneous than that of existing adult studies. It is difficult to predict to what extent and in which direction selection bias will affect the representativeness of the study population, as in our clinical experience families often consider anti-inflammatory therapy at all stages and severities of the disorder.
A subset of children may benefit from immune-modulating therapies, but there are no validated strategies for identifying these individuals. This study incorporates biosample collection preintervention and postintervention, allowing not only for safety monitoring but also for future analyses of pro-inflammatory markers. Given the paucity of data from interventional trials examining longitudinal markers of inflammation and treatment response in paediatric OCD, this will generate much-needed preliminary data to inform further studies of immune-related biomarkers. Due to funding limitations, these samples will be allocated for future analyses.
This study incorporates questionnaires aimed at better understanding participants’ experiences of virtual study visits, which is a novel format for psychopharmaceutical trials at our centre in the context of the COVID-19 pandemic and will increase equitable access to opportunities for research participation. We expect that these data will inform the design of future studies incorporating remote research visits and clinical care.
Conclusions
NSAIDs are common in clinical practice and referenced in both adult and paediatric treatment guidelines for OCD, but no controlled studies have evaluated the effects of COX inhibitors in CO-OCD. This study will be the first to assess the efficacy and safety of adjunctive celecoxib in this population and will inform clinical management of children and youth with OCD.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge clinical trial support provided by the BC Children’s Hospital Clinical Research Support Unit, including consultation on study design and methodology by Peter Subrt and Jennifer Claydon. We also thank BCCH Research Pharmacist Erin Adams, Delta Prescriptions Pharmacist Michael Millman and BCCH Clinical Laboratory/BioBank staff Veronica Chow and Vi Nguyen for input on protocol design and implementation.
Footnotes
Twitter: @cwestwellroper
Contributors: CW-R drafted the initial protocol under the supervision of SES, who revised for significant content. JRB created the statistical analysis plan. MM, SB, DE and LT provided clinical input into study design and monitoring. AA, ZN, BL and CL drafted subsections of the initial protocol and facilitated research ethics board submission. All authors revised the protocol and approved of the final version to be submitted.
Funding: This work is supported by an International OCD Foundation Young Investigator Award to CW-R.
Competing interests: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet 1997;349:1436–42. 10.1016/S0140-6736(96)07495-8 [DOI] [PubMed] [Google Scholar]
- 2.Hollander E, Doernberg E, Shavitt R, et al. The cost and impact of compulsivity: a research perspective. Eur Neuropsychopharmacol 2016;26:800–9. 10.1016/j.euroneuro.2016.02.006 [DOI] [PubMed] [Google Scholar]
- 3.do Rosario-Campos MC, Leckman JF, Curi M, et al. A family study of early-onset obsessive-compulsive disorder. Am J Med Genet B Neuropsychiatr Genet 2005;136B:92–7. 10.1002/ajmg.b.30149 [DOI] [PubMed] [Google Scholar]
- 4.Chabane N, Delorme R, Millet B, et al. Early-onset obsessive-compulsive disorder: a subgroup with a specific clinical and familial pattern? J Child Psychol Psychiatry 2005;46:881–7. 10.1111/j.1469-7610.2004.00382.x [DOI] [PubMed] [Google Scholar]
- 5.Swedo SE, Leonard HL, Garvey M, et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am J Psychiatry 1998;155:264–71. 10.1176/ajp.155.2.264 [DOI] [PubMed] [Google Scholar]
- 6.Chang K, Frankovich J, Cooperstock M, et al. Clinical evaluation of youth with pediatric acute-onset neuropsychiatric syndrome (PANS): recommendations from the 2013 PANS consensus conference. J Child Adolesc Psychopharmacol 2015;25:3–13. 10.1089/cap.2014.0084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Köhler-Forsberg O, Petersen L, Gasse C, et al. A nationwide study in Denmark of the association between treated infections and the subsequent risk of treated mental disorders in children and adolescents. JAMA Psychiatry 2019;76:271–9. 10.1001/jamapsychiatry.2018.3428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orlovska S, Vestergaard CH, Bech BH, et al. Association of streptococcal throat infection with mental disorders: testing key aspects of the PANDAS hypothesis in a nationwide study. JAMA Psychiatry 2017;74:740–6. 10.1001/jamapsychiatry.2017.0995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slattery MJ, Dubbert BK, Allen AJ, et al. Prevalence of obsessive-compulsive disorder in patients with systemic lupus erythematosus. J Clin Psychiatry 2004;65:301–6. 10.4088/JCP.v65n0303 [DOI] [PubMed] [Google Scholar]
- 10.Hounie AG, Pauls DL, do Rosario-Campos MC, et al. Obsessive-compulsive spectrum disorders and rheumatic fever: a family study. Biol Psychiatry 2007;61:266–72. 10.1016/j.biopsych.2006.02.021 [DOI] [PubMed] [Google Scholar]
- 11.Mataix-Cols D, Frans E, Perez-Vigil A. A total-population multigenerational family clustering study of autoimmune diseases in obsessive-compulsive disorder and Tourette’s/chronic tic disorders. Mol Psychiatry 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westwell-Roper C, Williams KA, Samuels J, et al. Immune-related comorbidities in childhood-onset obsessive compulsive disorder: lifetime prevalence in the obsessive compulsive disorder collaborative genetics association study. J Child Adolesc Psychopharmacol 2019;29:615–24. 10.1089/cap.2018.0140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Attwells S, Setiawan E, Wilson AA, et al. Inflammation in the neurocircuitry of obsessive-compulsive disorder. JAMA Psychiatry 2017;74:833–40. 10.1001/jamapsychiatry.2017.1567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang H, Chen C. Cyclooxygenase-2 in synaptic signaling. Curr Pharm Des 2008;14:1443–51. 10.2174/138161208784480144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen C, Magee JC, Bazan NG. Cyclooxygenase-2 regulates prostaglandin E2 signaling in hippocampal long-term synaptic plasticity. J Neurophysiol 2002;87:2851–7. 10.1152/jn.2002.87.6.2851 [DOI] [PubMed] [Google Scholar]
- 16.Faridhosseini F, Sadeghi R, Farid L, et al. Celecoxib: a new augmentation strategy for depressive mood episodes. A systematic review and meta-analysis of randomized placebo-controlled trials. Hum Psychopharmacol 2014;29:216–23. 10.1002/hup.2401 [DOI] [PubMed] [Google Scholar]
- 17.Marini S, De Berardis D, Vellante F, et al. Celecoxib adjunctive treatment to antipsychotics in schizophrenia: a review of randomized clinical add-on trials. Mediators Inflamm 2016;2016:1–8. 10.1155/2016/3476240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zheng W, Cai D-B, Yang X-H, et al. Adjunctive celecoxib for schizophrenia: a meta-analysis of randomized, double-blind, placebo-controlled trials. J Psychiatr Res 2017;92:139–46. 10.1016/j.jpsychires.2017.04.004 [DOI] [PubMed] [Google Scholar]
- 19.Sethi R, Gómez-Coronado N, Walker AJ, et al. Neurobiology and therapeutic potential of cyclooxygenase-2 (COX-2) inhibitors for inflammation in neuropsychiatric disorders. Front Psychiatry 2019;10:605. 10.3389/fpsyt.2019.00605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asadabadi M, Mohammadi M-R, Ghanizadeh A, et al. Celecoxib as adjunctive treatment to risperidone in children with autistic disorder: a randomized, double-blind, placebo-controlled trial. Psychopharmacology 2013;225:51–9. 10.1007/s00213-012-2796-8 [DOI] [PubMed] [Google Scholar]
- 21.Thienemann M, Murphy T, Leckman J, et al. Clinical management of pediatric acute-onset neuropsychiatric syndrome: part I-Psychiatric and behavioral interventions. J Child Adolesc Psychopharmacol 2017;27:566–73. 10.1089/cap.2016.0145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sigra S, Hesselmark E, Bejerot S. Treatment of PANDAS and PANS: a systematic review. Neurosci Biobehav Rev 2018;86:51–65. 10.1016/j.neubiorev.2018.01.001 [DOI] [PubMed] [Google Scholar]
- 23.Sayyah M, Boostani H, Pakseresht S, et al. A preliminary randomized double-blind clinical trial on the efficacy of celecoxib as an adjunct in the treatment of obsessive-compulsive disorder. Psychiatry Res 2011;189:403–6. 10.1016/j.psychres.2011.01.019 [DOI] [PubMed] [Google Scholar]
- 24.Shalbafan M, Mohammadinejad P, Shariat S-V, et al. Celecoxib as an adjuvant to fluvoxamine in moderate to severe obsessive-compulsive disorder: a double-blind, placebo-controlled, randomized trial. Pharmacopsychiatry 2015;48:136–40. 10.1055/s-0035-1549929 [DOI] [PubMed] [Google Scholar]
- 25.Shahini N, Talaei A, Shalbafan M, et al. Effects of celecoxib adjunct to selective serotonin reuptake inhibitors on obsessive-compulsive disorder. BCN 2021;12:489–98. 10.32598/bcn.2021.1998.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katzman MA, Bleau P, Blier P, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry 2014;14:S1. 10.1186/1471-244X-14-S1-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krishnaswami S, Hutmacher MM, Robbins JL, et al. Dosing celecoxib in pediatric patients with juvenile rheumatoid arthritis. J Clin Pharmacol 2012;52:1134–49. 10.1177/0091270011412184 [DOI] [PubMed] [Google Scholar]
- 29.Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). J Clin Psychiatry 2010;71:313–26. 10.4088/JCP.09m05305whi [DOI] [PubMed] [Google Scholar]
- 30.Goodman WK, et al. The Yale-Brown obsessive compulsive scale. Arch Gen Psychiatry 1989;46:1006–11. 10.1001/archpsyc.1989.01810110048007 [DOI] [PubMed] [Google Scholar]
- 31.Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry 2007;4:28–37. [PMC free article] [PubMed] [Google Scholar]
- 32.O'Connell NS, Dai L, Jiang Y, et al. Methods for analysis of pre-post data in clinical research: a comparison of five common methods. J Biom Biostat 2017;8:1–8. 10.4172/2155-6180.1000334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McGuire JF, Piacentini J, Lewin AB, et al. A meta-analysis of cognitive behavior therapy and medication for child obsessive-compulsive disorder: MODERATORS of treatment efficacy, response, and remission. Depress Anxiety 2015;32:580–93. 10.1002/da.22389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Storch EA, Lewin AB, De Nadai AS, et al. Defining treatment response and remission in obsessive-compulsive disorder: a signal detection analysis of the children's Yale-Brown obsessive compulsive scale. J Am Acad Child Adolesc Psychiatry 2010;49:708–17. 10.1016/j.jaac.2010.04.005 [DOI] [PubMed] [Google Scholar]
- 35.Rapp AM, Bergman RL, Piacentini J, et al. Evidence-Based assessment of obsessive-compulsive disorder. J Cent Nerv Syst Dis 2016;8:JCNSD.S38359. 10.4137/JCNSD.S38359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Storch EA, McGuire JF, Wu MS, et al. Development and psychometric evaluation of the children's yale-brown obsessive-compulsive scale second edition. J Am Acad Child Adolesc Psychiatry 2019;58:92–8. 10.1016/j.jaac.2018.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bourredjem A, Pelissolo A, Rotge J-Y, et al. A video clinical global impression (CGI) in obsessive compulsive disorder. Psychiatry Res 2011;186:117–22. 10.1016/j.psychres.2010.06.021 [DOI] [PubMed] [Google Scholar]
- 38.Murphy TK, Patel PD, McGuire JF, et al. Characterization of the pediatric acute-onset neuropsychiatric syndrome phenotype. J Child Adolesc Psychopharmacol 2015;25:14–25. 10.1089/cap.2014.0062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Greenhill LL, Vitiello B, Fisher P, et al. Comparison of increasingly detailed elicitation methods for the assessment of adverse events in pediatric psychopharmacology. J Am Acad Child Adolesc Psychiatry 2004;43:1488–96. 10.1097/01.chi.0000142668.29191.13 [DOI] [PubMed] [Google Scholar]
- 40.Buuren Svan, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw 2011;45:1. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 41.Barnard J, Rubin DB. Miscellanea. small-sample degrees of freedom with multiple imputation. Biometrika 1999;86:948–55. 10.1093/biomet/86.4.948 [DOI] [Google Scholar]
- 42.Gan TJ. Diclofenac: an update on its mechanism of action and safety profile. Curr Med Res Opin 2010;26:1715–31. 10.1185/03007995.2010.486301 [DOI] [PubMed] [Google Scholar]
- 43.Calvo-Rodríguez M, Núñez L, Villalobos C. Non-steroidal anti-inflammatory drugs (NSAIDs) and neuroprotection in the elderly: a view from the mitochondria. Neural Regen Res 2015;10:1371–2. 10.4103/1673-5374.165219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Díaz-González F, Sánchez-Madrid F. NSAIDs: learning new tricks from old drugs. Eur J Immunol 2015;45:679–86. 10.1002/eji.201445222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin T-Y, Lu C-W, Wang C-C, et al. Cyclooxygenase 2 inhibitor celecoxib inhibits glutamate release by attenuating the PGE2/EP2 pathway in rat cerebral cortex endings. J Pharmacol Exp Ther 2014;351:134–45. 10.1124/jpet.114.217372 [DOI] [PubMed] [Google Scholar]
- 46.Sandrini M, Vitale G, Pini LA. Effect of rofecoxib on nociception and the serotonin system in the rat brain. Inflamm Res 2002;51:154–9. 10.1007/PL00000287 [DOI] [PubMed] [Google Scholar]
- 47.Johansson D, Falk A, Marcus MM, et al. Celecoxib enhances the effect of reboxetine and fluoxetine on cortical noradrenaline and serotonin output in the rat. Prog Neuropsychopharmacol Biol Psychiatry 2012;39:143–8. 10.1016/j.pnpbp.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 48.Fields C, Drye L, Vaidya V, et al. Celecoxib or naproxen treatment does not benefit depressive symptoms in persons age 70 and older: findings from a randomized controlled trial. Am J Geriatr Psychiatry 2012;20:505–13. 10.1097/JGP.0b013e318227f4da [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Laan W, Grobbee DE, Selten J-P, et al. Adjuvant aspirin therapy reduces symptoms of schizophrenia spectrum disorders: results from a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 2010;71:520–7. 10.4088/JCP.09m05117yel [DOI] [PubMed] [Google Scholar]
- 50.Young D. FDA advisers endorse Celebrex for juvenile rheumatoid arthritis: lack of studies in children raises safety concerns. Am J Health Syst Pharm 2007;64:11–12. 10.2146/news070001 [DOI] [PubMed] [Google Scholar]
- 51.Foeldvari I, Szer IS, Zemel LS, et al. A prospective study comparing celecoxib with naproxen in children with juvenile rheumatoid arthritis. J Rheumatol 2009;36:174–82. 10.3899/jrheum.080073 [DOI] [PubMed] [Google Scholar]
- 52.Sobel RE, Lovell DJ, Brunner HI, et al. Safety of celecoxib and nonselective nonsteroidal anti-inflammatory drugs in juvenile idiopathic arthritis: results of the phase 4 registry. Pediatr Rheumatol Online J 2014;12:29. 10.1186/1546-0096-12-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stewart SE, Stack DE, Farrell C, et al. Effectiveness of intensive residential treatment (IRT) for severe, refractory obsessive-compulsive disorder. J Psychiatr Res 2005;39:603–9. 10.1016/j.jpsychires.2005.01.004 [DOI] [PubMed] [Google Scholar]
- 54.Forrest CB, Bevans KB, Pratiwadi R, et al. Development of the PROMIS ® pediatric global health (PGH-7) measure. Qual Life Res 2014;23:1221–31. 10.1007/s11136-013-0581-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mara CA, Kashikar-Zuck S, Cunningham N, et al. Development and psychometric evaluation of the PROMIS pediatric pain intensity measure in children and adolescents with chronic pain. J Pain 2021;22:48–56. 10.1016/j.jpain.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lewin AB, Peris TS, Lindsey Bergman R, et al. The role of treatment expectancy in youth receiving exposure-based CBT for obsessive compulsive disorder. Behav Res Ther 2011;49:536–43. 10.1016/j.brat.2011.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.De Nadai A, Nagpal PS, Piacentini J, et al. Contemporary models of pediatric obsessive-compulsive disorder: an evaluation with a large clinical sample. Psychiatry Res 2015;229:620–2. 10.1016/j.psychres.2015.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Foa EB, Coles M, Huppert JD, et al. Development and validation of a child version of the obsessive compulsive inventory. Behav Ther 2010;41:121–32. 10.1016/j.beth.2009.02.001 [DOI] [PubMed] [Google Scholar]
- 59.Pflugeisen BM, Rebar S, Reedy A, et al. Assessment of clinical trial participant patient satisfaction: a call to action. Trials 2016;17:483. 10.1186/s13063-016-1616-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.